Abstract
OBJECTIVE:
To assess the effectiveness of a comprehensive rehabilitation approach combining Traditional Chinese Medicine Daoyin with lower limb robotics during the recovery phase of stroke patients.
METHODS:
Stroke patients meeting the specified criteria were randomly assigned to one of four groups using a random number table: Control group, Daoyin group, lower limb robot group (LLR group), and Daoyin and lower limb robot group (DLLR group). Each group received distinct treatments based on conventional rehabilitation training. The treatment duration spanned two weeks with two days of rest per week. Pre- and post-intervention assessments included various scales: Fugl-Meyer Assessment (FMA), Berg balance scale (BBS), Barthel index (BI), Fatigue Scale-14 (FS-14), Pittsburgh sleep quality index (PSQI), Hamilton Anxiety Scale (HAMA), and Hamilton Depression Scale (HAMD).
RESULTS:
Statistically significant differences were observed in the lower limb function measured by FAM between the Control group (15 ± 5) and the DLLR group (18 ± 5) (P = 0.049). In the Barthel index, a statistically significant difference was noted between the Control group (54 ± 18) and the DLLR group (64 ± 11) (P = 0.041). Additionally, significant differences were found in the Berg balance scale between the Control group (21 ± 10) and the DLLR group (27 ± 8) (P = 0.024), as well as between the Control group (21 ± 10) and the LLR group (26 ± 10) (P = 0.048).
CONCLUSION:
The findings of this study suggest that the combined use of Daoyin and robotics not only enhances motor function in stroke patients but also has a positive impact on fatigue, sleep quality, and mood. This approach may offer a more effective rehabilitation strategy for stroke patients.
Keywords: stroke, rehabilitation, Daoyin, lower limb robot, randomized controlled trial
1. INTRODUCTION
Stroke, as widely recognized, stands as the second leading global cause of mortality and the primary cause of acquired adult disabilities, despite notable advancements in primary prevention and acute treatment over recent decades.1,2 It is worth noting that stroke not only entails a high morbidity rate but also a significant mortality rate, with over 50% of survivors enduring chronic disabilities.3,⇓,⇓-6
The physical disabilities resulting from stroke profoundly affect the psychological well-being and overall quality of life of patients. Among the various goals of stroke rehabilitation, the recovery of walking ability assumes paramount importance.7 Moreover, post-stroke depression (PSD) is a prevalent complication, afflicting approximately 31.1% of stroke patients.8 PSD not only prolongs the course of post-stroke neurological disorders but also exacerbates physical disabilities, further diminishing the quality of life. It significantly undermines the efficacy of therapeutic and rehabilitative measures, thereby increasing the risk of mortality.9 Notably, PSD may independently predict stroke recurrence among ischemic stroke patients and has been associated with a markedly elevated mortality risk in stroke survivors.10,11
Enhancing lower limb walking function and alleviating depression represent enduring and challenging objectives in stroke rehabilitation. To mitigate the costs of traditional rehabilitation training and enhance its reproducibility, rehabilitation robots designed to assist with limb dyskinesia post-stroke have emerged as a timely innovation.12,13 The primary advantage of these robots lies in their ability to provide patients with high-dose, high-intensity, and rhythmic training, thereby enhancing motor function and balance. This technology holds significant promise in the realm of stroke rehabilitation.14,15 Research indicates that the combined use of rehabilitation robots and conventional rehabilitation training yields superior therapeutic outcomes compared to conventional training alone.16,17
While current rehabilitation robot technology has reached a relatively advanced stage, ensuring the safety of human-robot interactions remains a paramount objective in rehabilitation robot research. The inherent complexity of human movement introduces disparities between rehabilitation robots and human motion. These disparities can lead to disturbances during the rehabilitation process, resulting in increased muscle tension and fatigue in patients and, in some cases, unintentional harm. And fatigue is one of the most serious sequelae of stroke, which also may limit the rehabilitation process and quality of life.18 This significantly compromises the safety of the human-robot interaction. To mitigate the adverse effects of robotic training on lower limbs, we have incorporated a traditional training method rooted in the principles of traditional Chinese exercises, known as "Daoyin."
The term "Dao" in Daoyin signifies the guidance of Qi, while "Yin" pertains to bodily movement and simultaneous breath adjustment, ultimately promoting both physical and mental well-being.19 Daoyin encompasses various modalities such as Tai Chi, Baduanjin, Yijinjing, and others. These practices not only fortify the body but also play a supportive role in disease treatment, particularly during the rehabilitation process following a stroke. In addition to enhancing the function of limbs affected by hemiplegia, Daoyin can alleviate fatigue, ameliorate depression, and improve sleep. It is commonly acknowledged that post-stroke depression can often impede the effectiveness of rehabilitation training. Therefore, incorporating Daoyin training can significantly enhance the outcomes of rehabilitation training. According to existing literature studies, both Tai Chi and Baduanjin not only enhance balance, gait, and reduce fall rates in stroke patients.19,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓-28 but also improve sleep quality and alleviate post-stroke depression.20,24,26 To date, there have been no similar studies combining Daoyin and lower limb robotics for stroke treatment. Our team's innovative approach of merging Daoyin with lower limb robotics seeks to explore a novel, comprehensive rehabilitation intervention that can benefit a larger population of stroke patients.
2. MATERIALS AND METHODS
2.1. Study design and participants
This study was a randomized controlled clinical trial conducted at the First Department of Rehabilitation, Wangjing Hospital of China Academy of Chinese Medical Sciences from January 1, 2017, to December 31, 2019. Recruitment for the study commenced in March 2018. The study participants were individuals in the recovery phase following a stroke, and their essential information, including gender, age, and duration of illness, was documented. Subsequently, participants were randomly allocated into four groups using a random number table: the control group, Daoyin group, lower limb robot group (LLR group), and Daoyin and lower limb robot group (DLLR group). Allocation was carried out on a 1:1:1:1 ratio for each group. Allocation Concealment: (a) The trial participants' allocation into groups was concealed. A designated individual generated a table of 80 random numbers, where each number represented one of the 80 participants. Importantly, the researchers responsible for determining these random numbers were not involved in the subject inclusion or subsequent trials. (b) A sequence list for assignment preparation was created, divided into three columns. The first column contained the participant sequence number, the second column had the random numbers, and the third column indicated the group sequence number (Group 1 for control, Group 2 for Daoyin, Group 3 for LLR, and Group 4 for DLLR). For example, No. 1 corresponded to 26, indicating Group 1; No. 2 corresponded to 45, indicating Group 2, and so forth. (c) The random numbers in the second column were derived from the random number table, ensuring that the sequence number for each included participant aligned with the generated random number in sequential order and without any alteration (e.g., the fifth random number matched the participant with the number 5). (d) Group assignment was based on the random numbers. For example, a participant with number 1 and number 26 was assigned to Group 1, while a participant with number 7 and number 69 was assigned to Group 3. (e) Three copies of the assignment sequences were prepared: one for the project leader, one for the researcher, and one for the individual who generated the random numbers. Each copy was sealed and secured in an opaque envelope. To address the small sample size, we added 20 additional participants while adhering to the above allocation concealment procedures, resulting in a total of 100 participants in this study. The inclusion and exclusion criteria for this study are as follows:
2.1.1. Inclusion criteria
Patients meeting the following criteria were eligible for inclusion: (a) Diagnosis in accordance with cerebral hemorrhage or cerebral infarction criteria. (b) Age between 25 and 75 years. (c) Disease duration ranging from 2 weeks to 6 months post-stroke, with a stable condition. (d) Lower limb dysfunction due to stroke, with spasticity grade < 2 (modified Ashworth scale). (e) Adequate cognitive function to follow instructions, indicated by an MMSE (Mini Mental State Examination, MMSE) score > 24. (f) Signed informed consent.
2.1.2. Exclusion criteria
Patients meeting the following criteria were excluded from the study: (a) Hemiplegia caused by cerebral trauma, brain tumor, or craniocerebral surgery. (b) Cerebral infarction complicated with cerebral hemorrhage. (c) Severe primary cardiovascular, liver, kidney, or hematopoietic system diseases. (d) Severe aphasia, profound hearing impairment, cognitive impairment, or an inability to communicate effectively. (e) Prior history of stroke and/or residual limb dysfunction. (f) Pregnant or lactating women. (g) Participation in other concurrent clinical trials.
Stroke patients, along with their families, were provided with comprehensive information about the study's particulars prior to enrollment. Informed consent was obtained only after careful screening based on the inclusion and exclusion criteria.
2.2. Ethics committee approval
This study protocol received approval from the Ethics Committee of Wangjing Hospital, China Academy of Chinese Medicine Sciences. The trial will be conducted under the supervision of the Clinical Trials Center at Wangjing Hospital, adhering to the principles of the Declaration of Helsinki. The Ethics Committee will oversee all study processes, including recruitment, randomization, intervention, and data storage. Participants will provide written informed consent, and all collected data will be anonymized. Participants may withdraw from the study at any time without facing any constraints.
2.3. Ethics approval and consent to participate
This study adheres to the principles of the Declaration of Helsinki. The Ethics Committee of Wangjing Hospital, affiliated with China Academy of Chinese Medicine Sciences (WJEC-KT-2017-016-P001), has approved the study protocol. All participants in this study provided written informed consent.
2.4. Clinical registration information
This trial has been registered clinically, with registration available at the International Traditional Medicine Clinical Trial Registry (http://itmctr.ccebtcm.org.cn/). The registration number is ITMCTR2023000038.
2.5. Intervention
Once all preparatory tasks were completed, each group received distinct intervention treatments based on the designated plan. The control group received standard conventional rehabilitation treatment. In addition to conventional treatment, the Daoyin group received combined Daoyin treatment, the LLR group received combined lower limb robot treatment, and the DLLR group received a combination of both Daoyin and lower limb robot treatment. Both Daoyin and lower limb robot treatments were administered over a two-week period, with sessions conducted five days a week, twice daily. Daoyin sessions lasted for 40 min, while lower limb robot sessions were 20 min in duration. Following the two-week treatment period, participants underwent a reassessment using the relevant assessment scales, and the data were meticulously recorded in the CRF manual. All interventions were administered under the supervision of a professional physician who closely monitored the participants' condition to ensure their safety and prevent any accidental falls.
2.6. Equipment
A lower limb robot, developed by Beijing Ai-Robotics Technology Co., Ltd., known as AI-ROBOTICS (www.ai-robotics.cn), was employed for lower limb movement training post-stroke. This robot is commonly referred to as AIWALKER and is suitable for rehabilitation training in the early to middle stages for patients with various types of lower limb dysfunction. The Aiwalker, a frame-type Ai-robot, primarily comprises a waist support device and a suspension system designed to securely and stably immobilize the user's trunk and pelvis without necessitating active efforts to maintain balance.30,31 Refer to supplementary Figure 1 for the specific donning process. The Aiwalker boasts extensive functional integration, enabling weight-bearing, stationary standing, indoor and outdoor flat-ground walking, gait training, functional assessment, and more. It combines both active and passive training methods, facilitating comprehensive and multi-dimensional rehabilitation training that accelerates the rehabilitation process. The ease of operation of this rehabilitation equipment simplifies lower limb motor function training and can also alleviate the manual training burden on physical therapists. Lower limb robot training sessions were conducted once daily, each lasting 20 min, with medical professionals assisting patients during the exercises. The training adhered to a standard gait pattern and was adjusted based on the specific leg length coefficient of each patient. Training consisted of 10 min of treadmill exercise followed by 10 min of flat-ground walking. Under the guidance of professional TCM doctors, lower limb robot training occurred twice daily for 14 consecutive days, with 2 d of rest provided every 5 d.
2.7. Daoyin
In response to the specific requirements of stroke patients and through consultation with relevant experts, field training, and expert discussions, our team developed a TCM Daoyin program based on the traditional principles of Tai Chi and Baduanjin. The Daoyin program comprises seven primary movements: Rise form, Lift separately to regulate spleen and stomach, Wave hands like a cloud, Hands on the heavenly three jiao, Step up on your knees, Seven upheavals in the back, and Close form. To ensure the effective implementation of the program, we took a dual approach. Firstly, we engaged specialized researchers to provide guidance to participants, explaining the key elements of the Daoyin movements. Secondly, we created instructional Daoyin videos for participants to watch and practice.
Under the supervision of a professional Chinese medicine practitioner, the Daoyin exercises were conducted over a two-week period, 5 d a week, with two sessions per day, each lasting 40 min. This included 5 min for Commencing form and Closing form to regulate breathing and prepare and cool down the body. Additionally, we provided training to patients and their caregivers, and recorded instructional videos to facilitate independent practice. Prior to the intervention, patients and their caregivers received 1-2 d of instruction in Daoyin, ensuring their familiarity and proficiency with the movements before commencing the actual intervention. Throughout the entire Daoyin exercise program, professional TCM doctors were present to oversee and safeguard the patients, monitoring their physical condition to prevent accidents such as falls.
2.8. Outcome indictors
All groups received treatment based on conventional methods. Participants who met the inclusion and exclusion criteria underwent scale assessments and were then assigned to groups according to corresponding random numbers. Scale assessments were conducted again after two weeks of intervention, with professional physicians responsible for the evaluations. To minimize subjective bias, two professional physicians scored the assessments, and disagreements were resolved through expert consultation. Primary outcomes were measured using the FMA, and secondary outcomes included the BBS, BI, PSQI, FS-14, HAMA, HAMD.
2.9. Statistical analysis
Data analysis for this study was conducted using SPSS 23.0 statistical software (IBM Corp., Armonk, NY, USA). Grouped data were summarized as mean ± standard deviation (). Between-group comparisons at each follow-up point were carried out using analysis of variance (ANOVA) for data with a normal distribution, with post hoc least significant difference testing. In all analyses, a significance level of P < 0.05 was deemed statistically significant.
3. RESULTS
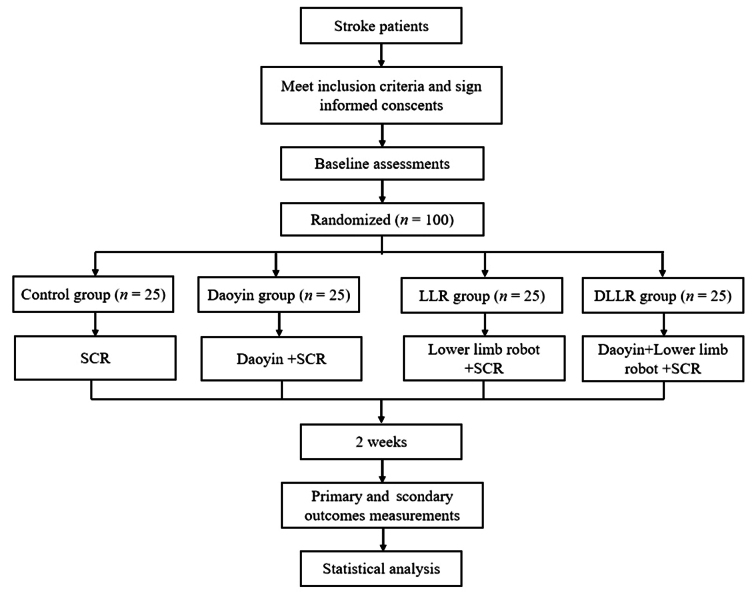
In total, 100 stroke patients were enrolled in this study, comprising 84 men and 16 women, with no dropouts during the study. The data collected from the relevant scales for these patients were recorded in the case report form (CRF) manual. Refer to Figure 1 for a summary of the study design flow chart.
Figure 1. Flow chart of the study.
LLR group: lower limb robot group; DLLR group: Daoyin and lower limb robot group; SCR: standard conventional rehabilitation.
3.1. Physical data
All 100 stroke patients successfully completed the study. At baseline, there were no significant differences in gender, time since stroke, age, FMA score, BBS score, BI score, FS-14 score, PSQI score, HAMA score, and HAMD score among the four distinct groups. The significance level (P) exceeded 0.05, indicating no significant differences between the groups (Table 1).
Table 1.
Demographic data of the participants (n = 25, )
| Item | Control group | Daoyin group | LLR group | DLLR group |
|---|---|---|---|---|
| Sex (n) | 25 | 25 | 25 | 25 |
| Men | 22 | 21 | 20 | 21 |
| Women | 3 | 4 | 5 | 4 |
| Time after stroke (weeks) | 7±4 | 9±5 | 8±8 | 8±5 |
| Age (years) | 58±12 | 58±9 | 59±10 | 60±11 |
| Body mass (kg) Body height (cm) Hemiparesis side (left/right, n) Stroke type (ISC/Hem, n) |
71±12 170±6 15/10 19/6 |
71±10 169±6 16/9 17/8 |
69±8 168±7 13/12 20/5 |
70±9 166±7 18/7 21/4 |
Notes: LLR group: lower limb robot group; DLLR group: Daoyin and lower limb robot group;Isc: Ischemic; Hem: hemorrhagic. Continuous variables are statistically summarized through statistical description or analysis of variance.
3.2. Primary outcome: FMA
After the intervention, there was no significant difference in upper limb FMA among the four groups. However, a statistically significant difference was observed between the Control group and the DLLR group (P = 0.049), with no significant differences found between the other groups (Table 2).
Table 2.
Primary Outcomes of FMA in the Participants (n = 25, )
| Item | Control group | Daoyin group | LLR group | DLLR group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | |||||
| Upper limb | 17±12 | 20±13 | 15±9 | 20±10 | 13±12 | 18±12 | 16±10 | 22±9 | ||||
| Lower limb | 13±4 | 15±5 | 13±4 | 17±4 | 11±5 | 16±6 | 13±5 | 18±5a | ||||
Notes: LLR group: lower limb robot group; DLLR group: Daoyin and lower limb robot group; FMA: Fugl-Meyer Assessment. Continuous variables are statistically summarized through analysis of variance. Compared with the Control group, aP < 0.05.
3.3. Secondary outcomes included BBS, BI, PSQI, FS-14, HAMA, HAMD and 10- meters pace
3.3.1. BBS and BI
After two weeks of treatment, a statistically significant difference was noted between the Control group and the LLR group (P = 0.048) in BBS scores, as well as between the Control group and the DLLR group (P = 0.024). A significant difference in BI change was observed between the Control group and the DLLR group (P = 0.036) (Table 3).
Table 3.
Secondary outcomes of the participants (n = 25, )
| Item | Control group | Daoyin group | LLR group | DLLR group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | ||||||
| BBS | 16±10 | 21±10 | 17±11 | 23±11 | 16±10 | 26±10a | 16±8 | 27±8a | |||||
| BI | 46±18 | 54±18 | 47±18 | 60±16 | 45±17 | 62±16 | 48±12 | 64±11a | |||||
Notes: LLR group: lower limb robot group; DLLR group: Daoyin and lower limb robot group; BBS: Berg balance scale; BI: Barthel index. Continuous variables are statistically summarized through analysis of variance. Compared with the Control group, aP < 0.05.
3.3.2. PSQI and FS-14
Following the intervention, statistically significant differences were found in PSQI scores between the Control group and the Daoyin group (P = 0.012), the Control group and the DLLR group (P = 0.021), and the Daoyin group and the LLR group (P = 0.037). Similarly, significant differences in FS-14 scores were noted between the Control group and the Daoyin group (P = 0.015), the Control group and the DLLR group (P = 0.033), and the Daoyin group and the LLR group (P = 0.015) (Table 4).
Table 4.
Secondary outcomes of the participants (n = 25, )
| Item | Control group | Daoyin group | LLR group | DLLR group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | Pre-test | Post-test | ||||||
| FS-14 | 10.1±2.1 | 8.6±1.9 | 9.6±2.8 | 6.6±2.7ab | 9.6±3.5 | 8.3±3.5 | 9.8±2.6 | 6.9±2.5a | |||||
| PSQI | 12.3±5.3 | 8.6±4.0 | 10.9±4.0 | 6.3±2.8a | 10.9±3.9 | 8.2±2.6 | 11.0±3.5 | 6.5±2.8a | |||||
| HAMA | 9.1±4.3 | 6.0±3.0 | 8.5±3.8 | 4.4±2.0ab | 8.9±3.4 | 5.9±2.6 | 9.2±3.0 | 4.4±2.2ab | |||||
| HAMD | 9.3±3.1 | 5.8±2.7 | 8.0±3.4 | 4.2±1.6ab | 8.3±3.4 | 5.5±3.0 | 8.8±2.9 | 4.2±2.3ab | |||||
Notes: LLR group: lower limb robot group; DLLR group: Daoyin and lower limb robot group; FS-14: Fatigue Scale-14; PSQI: Pittsburgh sleep quality index; HAMA: Hamilton Anxiety Scale; HAMD: Hamilton Depression Scale. Continuous variables are statistically summarized through analysis of variance. Compared with the Control group, aP < 0.05; compared with the LLR group, bP < 0.05.
3.3.3. HAMA and HAMD
After two weeks of treatment, significant differences were observed in HAMA scores between the Control group and the Daoyin group (P = 0.035), the Control group and the DLLR group (P = 0.027), the Daoyin group and the LLR group (P = 0.040), and the LLR group and the DLLR group (P = 0.030). Similarly, significant differences in HAMD scores were found between the Control group and the Daoyin group (P = 0.024), the Control group and the DLLR group (P = 0.027), the Daoyin group and the LLR group (P = 0.041), and the LLR group and the DLLR group (P = 0.046) (Table 4).
4. DISCUSSION
The results demonstrated that significant statistical differences were observed in various parameters. Specifically, when comparing the control group to the DLLR group, there were statistically significant differences in FMA (P = 0.049), BBS (P = 0.024), and BI (P = 0.036). Similarly, when comparing the control group to the LLR group, a statistically significant difference was found in BBS (P = 0.048). These findings suggest that the robot intervention may enhance lower limb motor function by improving balance and gait rhythm in the lower limbs. Robot-assisted therapy has become a crucial component of stroke rehabilitation, and this study reaffirmed its positive impact. Moreover, ensuring the safety of human-machine interaction is a paramount objective in robot-assisted therapy research. In this study, all participants successfully completed the entire treatment process without experiencing notable fatigue or injury interruptions. We attribute this outcome to the incorporation of Daoyin before and after robot training. Daoyin serves to balance Yin and Yang, soothe meridians, promote Qi and blood circulation, and fortify the body. It exerts a substantial regulatory effect on various bodily systems. The use of these guiding techniques can facilitate ligament stretching and muscle relaxation before and after robot-assisted treatment, preventing soft tissue injuries, reducing muscle fatigue and stiffness, and enabling uninterrupted robot training. This experiment ensures the safety of interaction in robot-assisted rehabilitation therapy.
Additionally, the results also revealed statistically significant differences when comparing various groups. In particular, when comparing the control group to the DLLR group, there were significant differences in PSQI (P = 0.021), Fatigue Scale-14 (FS-14) (P = 0.033), HAMA (P = 0.027), and HAMD (P = 0.027). Similarly, when comparing the control group to the Daoyin group, significant differences were observed in PSQI (P = 0.012), FS-14 (P = 0.015), HAMA (P = 0.035), and HAMD (P = 0.024). These findings suggest that Daoyin can relax muscles and improve mood through limb traction and breathing adjustments, subsequently alleviating fatigue and improving sleep quality while reducing depression. Previous research has indicated that Tai Chi and Baduanjin can mitigate depression and enhance mood by influencing brain regions associated with emotional regulation.32,⇓,⇓-35 The Daoyin approach employed in this study was developed based on Tai Chi and Baduanjin, tailored to the specific needs of stroke patients, aiming to harmonize the mind and body.34 In comparison to activities such as swimming and running, Tai Chi has a more pronounced impact on cognitive function and mood in the elderly, even increasing gray matter volume in the insula.35,36 Moreover, stroke patients with hemiplegia can enhance the excitability of motor areas in the cerebral cortex and nerve cells through consistent and active Daoyin practice. During Daoyin practice, noticeable changes in skin temperature were observed, suggesting potential effects on autonomic nerve function. EEG studies have indicated that long-term Daoyin practice leads to more orderly brainwaves and potential improvements in memory and attention. Therefore, the multidimensional and multilevel effects of Daoyin make it a valuable component in stroke rehabilitation. We propose that combining Daoyin with lower limb robots as a novel comprehensive rehabilitation intervention not only effectively enhances lower limb motor function but also alleviates fatigue, improves mood, and enhances sleep quality. These improvements boost patients' motivation, confidence in rehabilitation training, and ultimately contribute to enhanced rehabilitation outcomes.
Naturally, this study does possess certain limitations. Firstly, the nature of the study made it impossible to blind participants and interveners. Nonetheless, to mitigate potential bias in the data results, the assessors of the scales and the statisticians handling the data were kept blinded. Secondly, due to the specific location of the experiment, the study conditions, and the influence of the COVID-19 pandemic, it may not provide the same level of comprehensiveness as a multicenter large-sample experimental study. Thirdly, during the early stages of this study, it became apparent that the sample size was relatively small. Following consultations with experts in relevant fields and a thorough literature review, a decision was made to augment the sample size by an additional 20 cases, distributing them evenly across the four groups with 5 cases per group. The study continued to select 20 random numbers for grouping in accordance with the previously established principles of random concealment and blinding. Consequently, we intend to enhance the study's design and aim for more standardized implementation in future research endeavors.
Presently, Daoyin, as a secure, efficacious, and straightforward Traditional Chinese Medicine exercise method, has gained widespread acceptance among professionals and patients both domestically and internationally. It is poised to emerge as a prominent research focal point in the rehabilitation field, boasting considerable potential for development and application in the future.
5. SUPPORTING INFORMATION
Supporting data to this article can be found online at http://journaltcm.cn.
REFERENCES
- 1. Bejot Y, Bailly H, Durier J, Giroud M. . Epidemiology of stroke in Europe and trends for the 21st century. Presse Med 2016; 45: e391-8. [DOI] [PubMed] [Google Scholar]
- 2. Collaborators GBDS. . Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795-820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Caimmi M, Giovanzana C, Gasperini G, Molteni F, Molinari Tosatti L. . Robot fully assisted upper-limb functional movements against gravity to drive recovery in chronic stroke: a pilot study. Front Neurol 2021; 12: 782094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Donkor ES. . Stroke in the 21(st) century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat 2018; 2018: 3238165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. . Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367: 1747-57. [DOI] [PubMed] [Google Scholar]
- 6. Xie YH, Gu H, Zhao Q, et al. Efficacy of meridian massage for motor function after a stroke: a systematic review and Meta-analysis. J Tradit Chin Med 2022; 42: 321-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Rooij IJM, Riemens MMR, Punt M, Meijer JG, Visser-Meily JMA, van de Port IGL.. To what extent is walking ability associated with participation in people after stroke? J Stroke Cerebrovasc Dis 2021; 30: 106081. [DOI] [PubMed] [Google Scholar]
- 8. Schottke H, Giabbiconi CM. . Post-stroke depression and post-stroke anxiety: prevalence and predictors. Int Psychogeriatr 2015; 27: 1805-12. [DOI] [PubMed] [Google Scholar]
- 9. Sivolap YP, Damulin IV. . Stroke and depression. Zh Nevrol Psikhiatr Im S S Korsakova 2019; 119: 143-7. [DOI] [PubMed] [Google Scholar]
- 10. Cai W, Mueller C, Li YJ, Shen WD, Stewart R. . Post stroke depression and risk of stroke recurrence and mortality: a systematic review and Meta-analysis. Ageing Res Rev 2019; 50: 102-9. [DOI] [PubMed] [Google Scholar]
- 11. Wu QE, Zhou AM, Han YP, et al. Poststroke depression and risk of recurrent stroke: a Meta-analysis of prospective studies. Medicine (Baltimore) 2019; 98: e17235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chien WT, Chong YY, Tse MK, Chien CW, Cheng HY. . Robot-assisted therapy for upper-limb rehabilitation in subacute stroke patients: a systematic review and Meta-analysis. Brain Behav 2020; 10: e01742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li L, Fu Q, Tyson S, Preston N, Weightman A. . A scoping review of design requirements for a home-based upper limb rehabilitation robot for stroke. Top Stroke Rehabil 2022; 29: 449-63. [DOI] [PubMed] [Google Scholar]
- 14. Chen ZJ, Wang C, Fan W, et al. Robot-assisted arm training versus therapist-mediated training after stroke: a systematic review and Meta-analysis. J Healthc Eng 2020; 2020: 8810867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li YQ, Fan T, Qi Q, et al. Efficacy of a novel exoskeletal robot for locomotor rehabilitation in stroke patients: a multi-center, non-inferiority, randomized controlled trial. Front Aging Neurosci 2021; 13: 706569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mehrholz J, Thomas S, Kugler J, Pohl M, Elsner B. . Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev 2020; 10: CD006185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moucheboeuf G, Griffier R, Gasq D, et al. Effects of robotic gait training after stroke: a Meta-analysis. Ann Phys Rehabil Med 2020; 63: 518-34. [DOI] [PubMed] [Google Scholar]
- 18. You JY, Li HY, Xie DY, Chen MR, Chen RX. . Efficacy of acupuncture therapy for Post-Stroke Fatigue: A systematic review and Meta-analysis. J Tradit Chin Med 2023; 43: 27-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li R, Jin L, Hong P, et al. The effect of baduanjin on promoting the physical fitness and health of adults. Evid Based Complement Alternat Med 2014; 2014: 784059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xie GL, Rao T, Lin LL, et al. Effects of Tai Chi Yunshou exercise on community-based stroke patients: a cluster randomized controlled trial. Eur Rev Aging Phys Act 2018; 15 :17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim H, Kim YL, Lee SM. . Effects of therapeutic Tai Chi on balance, gait, and quality of life in chronic stroke patients. Int J Rehabil Res 2015; 38: 156-61. [DOI] [PubMed] [Google Scholar]
- 22. Taylor-Piliae RE, Hoke TM, Hepworth JT, Latt LD, Najafi B, Coull BM. . Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch Phys Med Rehabil 2014; 95: 816-24. [DOI] [PubMed] [Google Scholar]
- 23. Yuen M, Ouyang HX, Miller T, Pang MYC. . Baduanjin Qigong improves balance, leg strength, and mobility in individuals with chronic stroke: a randomized controlled study. Neurorehabil Neural Repair 2021; 35: 444-56. [DOI] [PubMed] [Google Scholar]
- 24. Li YF, Zhang YJ, Cui CY, et al. The effect of Tai Chi exercise on motor function and sleep quality in patients with stroke: a Meta-analysis. Int J Nurs Sci 2017; 4: 314-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lyu DY, Lyu XX, Zhang Y, et al. Tai Chi for stroke rehabilitation: a systematic review and Meta-analysis of randomized controlled trials. Front Physiol 2018; 9: 983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lyu DY, Wang JC, Yang F, et al. Effect of Tai Chi on post-stroke non-motor disorders: a systematic review and Meta-analysis of randomized controlled trials. Clin Rehabil 2021; 35: 26-38. [DOI] [PubMed] [Google Scholar]
- 27. Zheng G, Fang Q, Chen B, Yi H, Lin Q, Chen L. . Qualitative evaluation of Baduanjin (Traditional Chinese Qigong) on health promotion among an elderly community population at risk for ischemic stroke. Evid Based Complement Alternat Med 2015; 2015: 893215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zou L, Wang C, Chen X, Wang H. . Baduanjin exercise for stroke rehabilitation: a systematic review with Meta-analysis of randomized controlled trials. Int J Environ Res Public Health 2018; 15: 600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zou L, Yeung A, Quan X, Boyden S, Wang H. . A systematic review and Meta-analysis of mindfulness-based (Baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. Int J Environ Res Public Health 2018; 15: 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chen SJ, Wang ZB, Li YQ, et al. Safety and feasibility of a novel exoskeleton for locomotor rehabilitation of subjects with spinal cord injury: a prospective, multi-center, and cross-over clinical trial. Front Neurorobot 2022; 16: 848443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang F, Li K, Wu D, Chen P, Dou Z. . Therapeutic effect of AiWalker on balance and walking ability in patients with stroke: a pilot study. Top Stroke Rehabil 2021; 28: 236-240. [DOI] [PubMed] [Google Scholar]
- 32. Li MY, Fang QY, Li JZ, et al. The effect of Chinese traditional exercise-Baduanjin on physical and psychological well-being of college students: a randomized controlled trial. PLoS One 2015; 10: e0130544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tao J, Liu J, Liu WL, et al. Tai Chi Chuan and Baduanjin increase grey matter volume in older adults: a brain imaging study. J Alzheimers Dis 2017; 60: 389-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wei GX, Xu T, Fan FM, et al. Can Taichi reshape the brain? A brain morphometry study. PLoS One 2013; 8: e61038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang X, Ni X, Chen P. . Study about the effects of different fitness sports on cognitive function and emotion of the aged. Cell Biochem Biophys 2014; 70: 1591-6. [DOI] [PubMed] [Google Scholar]
- 36. Menon V, Uddin LQ. . Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct 2010; 214: 655-67. [DOI] [PMC free article] [PubMed] [Google Scholar]