Abstract
Purpose of Review
Autistic adults frequently require treatment of mental health problems. Increased rates of suicidality and diminished quality of life among autistic people may be partially attributable to psychiatric symptoms. Some risk factors for mental health problems in autistic people are likely the same as risk factors present in neurotypical individuals, but unique factors that are specific to neurodivergent individuals, and some even more specific to autistic people, may exist. Understanding pathways from autism to mental health problems could inform intervention efforts at the individual and societal levels.
Recent Findings
We review a growing body of research identifying risk processes across the affective, cognitive, and social domains. Consistent with the principle of equifinality, different processes appear to independently and jointly lead to heightened risk for the onset of mental health problems.
Summary
Autistic adults frequently utilize mental healthcare services, and experience heightened risk for chronic impairment as a result of mental health problems. Understanding causal and developmental risk processes in autism should inform personalized treatment. We synthesize extant research on these processes and offer suggestions for addressing them therapeutically and societally.
Keywords: Autism, Mental health, Risk, Mechanism
Introduction
The autism spectrum is a multifaceted collection of traits including symptoms that contribute to formal diagnoses [1]; many individuals self-identify as autistic without the level of symptoms that would qualify for a formal diagnosis [2]. Psychiatric symptoms, such as social avoidance, repetitive behaviors, and difficulties in emotion perception are key diagnostic features of autism, and they are also symptoms of other mental health conditions [1]. In addition, common aspects of autism such as inattention, sleep disruption, and frequent heightened levels of stress / worry are diagnostic for many psychiatric conditions, leading to inherent overlap of autism with mental health diagnoses. Many psychiatric disorders are more common among autistic adults than in the general population. Over > 70% of autistic adults meet criteria for additional diagnoses [1]. Throughout the lifespan, autistic people face heightened risk in particular for mood and anxiety problems [3]. Psychiatric problems, widely observed in autistic individuals [4, 5], directly contribute to the high healthcare costs for this population, and adversely impact their quality of life [6–8].
This review focuses on psychiatric disorders named in the Diagnostic and Statistical Manual for Mental Disorders (DSM); we consider myriad distress-linked characteristics commonly present in autistic people, such as sensory issues, pain sensitivity, synesthesia, and social exclusion, as potential vulnerability or exacerbating factors for these disorders, but do not focus on them explicitly as outcomes. We also offer recommendations as to how processes can be targeted therapeutically and societally, capitalizing on preserved strengths and capacities. Comprehensive review of all risk processes is beyond the scope of this paper. As such, the focus herein is on those processes that are likely more specific, or unique, to Autism Spectrum Disorder (ASD). The authors draw on prior research from our labs and others, direct clinical and personal family experience with this population, and personal lived experience as an autistic adult (GS).
There is a high need for care and services in autism, across functional domains (e.g., psychiatric, social, occupational), and this need goes unmet for most autistic adults. In a recent meta-analysis, ADHD was the most common co-occurring condition in autism, followed by depression and anxiety disorders, with estimated prevalence of 18.8% and 17.8%, respectively [9]. Among autistic adults with lower needs for services, up to 25% meet criteria for obsessive–compulsive disorder [10]and up to 50% meet criteria for obsessive compulsive personality disorder [11]. There has been less research on presence of personality disorders in autism; however, co-occurrence with schizoid personality disorder has been observed [12].
Autistic adults visit emergency rooms for psychiatric reasons 4 times more frequently than non-autistic adults [13], which has high costs for both those individuals and their families, and for the healthcare system [14]. Research has also documented heightened risk for suicide and self-harm among autistic people. In a nationwide study in Denmark, autistic people had a threefold greater rate of suicide attempt [15].
Though our focus is psychiatric symptoms associated with autism, consistent with the prevailing medical model, autism is also associated with preserved capacities and strengths [16]. The medical model, which has dominated clinical science and intervention research, views the ‘problem’ as residing within the affected or disabled person. In contrast, the social model of disability recognizes that many of the problems experienced by a person with a disability, including autism, are the result of oppression or exclusion by society. Thus, increasingly, autism advocates and researchers highlight autistic strengths such as capacity to focus on details, maintain interest in specific topics, and organize information in different ways than other people do [17]. A strengths-based approach to service delivery and treatment involves helping clients embrace their diversity and wholeness while striving to attain goals and greater quality of life [18].
Following the NIH’s Research Domain Criteria (RDoC) [19], we focus on three clusters of risk: affective, cognitive, and social. Figure 1 shows an fMRI meta-analysis of neural systems involved in autism, which suggests that these three domains are of specific relevance to autism. The figure reflects an automated meta-analytic aggregation across 244 functional MRI studies in which autism was mentioned, conducted using public data from the Neurosynth [20] engine as of 2/1/2023. The blue “uniformity map” (regions significantly associated with the mention of autism) and red “association map” (regions more uniquely associated with autism) strongly represent networks subserving primarily affective (e.g., amygdala, including structures involved in motivation such as the basal ganglia), cognitive (e.g., dorsolateral prefrontal cortex), and social (temporo-parietal junction) features. As such, we focus on these three domains in the ensuing sections. Finally, for those risk factors thought to be mutable, information on targeted treatments as well as potentially useful social change is provided, using an experimental therapeutics approach to connect basic science to clinical application [19, 21].
Fig. 1.
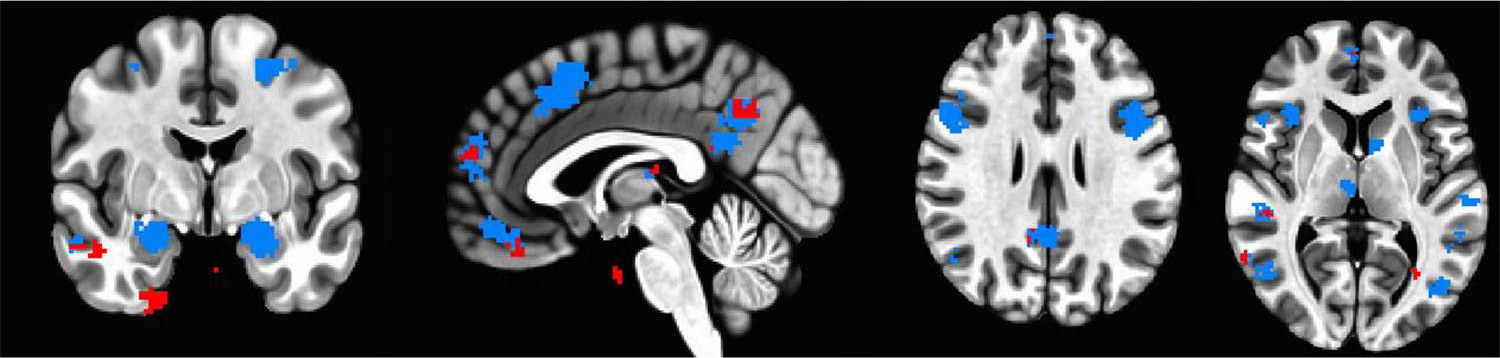
Automated fMRI meta-analysis depicting four different slices highlighting brain regions in which activity is associated with autism (from left to right: coronal, sagittal, dorsal axial, ventral axial view). Blue regions are nodes of activity reliably associated with autism in the literature, and red regions are uniquely associated with autism above and beyond other terms
Affective: Emotional Information Processing
There is tremendous heterogeneity in emotion processing patterns within the autism spectrum. Though emotional processing impairments are neither universally observed nor emblematic of the diagnosis, there is a fairly specific strength and profile pattern associated with ASD (see [22] for review). Challenges in emotional processing tend to be more pronounced in the context of social stimuli and when emotions or tasks are complex or cognitively demanding [22]. Alexithymia, or impaired ability to identify and report on, or describe, one’s own emotional state [23], is present in up to 50% of autistic adults [24] and is associated with a host of psychiatric conditions [25], including co-occurring conditions such as depression and social anxiety disorder in ASD [26–28]. Alexithymia, along with emotional acceptance, has been found to explain considerable variance in the association between ASD and anxiety among autistic adults [29].
Emotion dysregulation is a term used to describe diminished ability to manage one’s experienced or expressed emotion in the service of goal-directed behavior [30]. Dysregulation includes multiple sub-strategies such as heightened emotional reactivity, persistent negative affect, and reliance on ineffectual or maladaptive coping strategies [31–33]. Considerable research as shown that emotion dysregulation is common in ASD, and associated with the presence of psychiatric concerns including anxiety, depression, and suicidality [34–36].
Neural features of autism that could result in emotion dysregulation have been identified as early as infancy [37], with alterations in developmental trajectories of emotional regulatory function that are associated with neural changes observed within the first two years of life [38]. Features such as increased structural connectivity along pathways connecting brain regions involved in emotional processing (particularly cingulum, and superior longitudinal fasciculus [39]) have been found in young children. Other abnormalities in connectivity with temporal regions of the corpus callosum, subserving more complex emotional processing [39], have been observed in toddlers later diagnosed with ASD [40]. Thus, it is likely that alterations in neural processing of emotion begin early and continue through the lifespan; they may translate to frank symptomatology or be labeled as different from neurotypical processing for a given individual as a child, adolescent, or adult.
Autistic adults display characteristic patterns of brain activity across a wide variety of emotional information processing tasks including decreased reactivity in regions such as the striatum and dorsolateral prefrontal cortex in response to emotion regulation [41], decreased superior temporal and medial prefrontal activation during implicit emotion processing [42], and increased reactivity in structures associated with emotional information processing such as the amygdala, when viewing faces, which is further associated with gaze avoidance to those faces [43, 44] as well as symptomatology of psychiatric conditions associated with emotional avoidance such as social anxiety [45].
These data beg the question of why, if autistic individuals have increased reactivity to emotional information, they have been labeled as low in empathy. Recent findings suggest that, in actuality, autistic individuals have comparatively high levels of emotional reactivity to others’ emotions (affective empathy), but may have decreased differentiation of attribution for specific emotion categories (cognitive empathy). Practically speaking, it may be clear to the autistic adult that someone is in distress, and they experience empathic distress, but subtle distinctions regarding the nature of the distress (e.g., differentiating between another person’s anxious worry and sad rumination) may be less likely to occur [46].
Similarly, autistic adolescents and young adults have been found to show less frequent or less effective use of strategies to manage emotionality such as reappraisal, and potentially increased use of coping strategies that tend to be less potent, such as rumination [47, 48], which have been associated with increased amygdala reactivity in non-autistic depressed individuals [49]. Moreover, the brain’s salience network, of which the amygdala is a key component, has been associated with sustained negative information processing in adult autism [50]. Similarly, alterations in the functional connectivity (synchronization of brain activity across regions) between amygdala and prefrontal cortex (key pathway in regulatory processes in socioemotional processing) have been reported in autism [51]. Connectivity differences have also been reported in autistic individuals during task-free resting state, which may be indicative of pervasive alterations in emotional information processing that could increase vulnerability to other psychiatric conditions that contribute to broader problems with cognitive and socioemotional processing [52]. Yet, a growing body of data suggests that such observations may be a byproduct of comorbid depressive symptomatology or PTSD [53, 54] with psychophysiological reactivity characteristic of sustained rumination-like emotional information processing [55] being apparent only in autistic individuals who are depressed [56]. Thus, no differences are apparent in ecological observations of repetitive negative thinking between non-depressed autistic and non-autistic adults, and of note, repetitive negative thinking in autism is not related to the presence of other repetitive behaviors [57]. That said, commonly reported aspects of autistic symptomatology, such as “autistic inertia”, by which autistic individuals who have an internal experience like an intense emotion may feel “stuck” in that state and unable to mobilize coping resources to ask for help or otherwise regulate their reactions [58].
Another aspect of emotional functioning, which is affected in autism, regards motivation, particularly how reward and punishment are processed. There is a broad reward processing difficulty, reflected in differential neural reactivity, in ASD, which is not specific to social stimuli [59]. Specifically, the anticipation or ‘wanting’ of the stimulus, or reward [60], which is strongly associated with dopaminergic function [61], is diminished. Diminished anticipation of reward has been associated with stress and affective instability as well as cognitive difficulties in the executive function domain such as working memory and cognitive flexibility [62, 63]. For instance, one must be able to maintain information in memory related to a task and target outcome in order to anticipate reward [64], and reward cues indicate where to direct attention [65]. Aberrant reward processing has long been associated with anhedonia, or loss of pleasure, which is a hallmark of clinical depression. There are also known changes in reward processing linked to the onset of puberty [66, 67]. The research base on the role of motivation and reward processing more generally in relation to mental health in autism is not deep.
Thus, in contrast to previous models, which suggested concepts such as blunted affect, lack of awareness of affect, and low empathy in autism be addressed, neural data suggest that autistic individuals have increased affective reactivity, acute awareness of their heightened affective state, and normative affective empathy. Thus, helping autistic individuals accept and learn to work with their increased reactivity (e.g., via mindful acceptance strategies, and through using preserved capacities) can help prevent or ameliorate stress, anxiety, and depression [68]. Additionally, strategies such as redirecting sensory attention from interoception to external stimuli (e.g., via vibration or fidget toys) and, potentially, teaching cognitive empathy, could be useful. Similarly, increasing societal awareness of the lower threshold for affective reactivity in autism, and differences between affective and cognitive empathy could help to create pathways for autistic individuals to interact as themselves without having to continuously feel shame about, or mask their natural reactions.
Cognitive: Executive Function and Cognitive Load
Many differences in cognitive, sensory, and motor processing have been observed in autistic, compared to non-autistic, individuals (see [69] for a review), from frank learning disabilities and increased need for structure in some autistic individuals, to differences in how sensory information is processed [70]. Considerable work has been done to understand these features at the subjective, behavioral, neural, and molecular levels [71]. These features can, in some cases, lead to mental health issues.
Intellectual disability, in particular, is associated with certain types of psychopathology [72], though there is debate regarding the extent to which autism serves as a vulnerability factor for psychopathology above and beyond the intellectual disabilities themselves [73, 74]. There is more evidence that cognitive ability moderates the risk for psychopathology and perhaps influences symptom expression (e.g., anxiety and depression among those without cognitive impairment; aggression, ADHD, and pica among those with cognitive impairment).
Differences in executive function (EF), decision-making, and intolerance of uncertainty can lead to psychopathology. For example, severe EF deficits can be clinically impairing and disabling to daily functioning [75]. Autistic adults without cognitive impairment often struggle with cognitive flexibility, working memory, and phonemic fluency, along with relative strengths in planning, decision-making, and semantic verbal fluency [76]. ASD has been uniquely linked to cognitive inflexibility [77], or the ability to shift between different thoughts or tasks [78]. Decreased cognitive flexibility is associated with depression above and beyond ASD features or emotion regulation difficulty [79], potentially through the association of decreased flexibility with increased rumination in autism, which is a vulnerability factor for depression [53]. Alternatively, difficulty with cognitive flexibility and insistence on sameness can breed inflexible depressogenic cognitions (e.g., rigid or ‘black or white’ thinking) [80]. Similarly, autistic youth with reduced EF exhibit elevated symptoms of anxiety [4].
Consistent with the attentional control theory of anxiety, which suggests that top-down cognitive functioning is reduced during times of high anxiety in order to permit resources to be reallocated to addressing threat, it is possible that executive dysfunction may increase the risk for heightened reactivity and engagement of cognitive biases [81]. Likewise, executive dysfunction can also be associated with increased load on cognitive systems. Focus and cognitive energy are diverted to process stimuli that may be subconsciously disregarded by non-autistic individuals. The experienced cognitive load is only increased by the compensatory strategies that must be consciously applied to function despite these neurological deficits. This additional cognitive labor contributes to a state of chronic stress, well known to contribute to the development of other psychiatric disorders [82]. The accumulation of these effects over time needs more attention in adult outcome research. Alternately, executive control is mediated primarily by prefrontal resources that are implicated in emotion regulation [83] yielding strong relationships between emotion and basic cognitive function [84, 85]. Having low EF is associated with risk for and presence of disorders of decreased emotion regulation in people who are not autistic [86, 87]. Executive dysfunction can thus be associated with unmitigated emotion dysregulation. In autism, such dysregulation can present as anxiety, depression, meltdowns, or intense reactions to stimuli which might not be considered overtly emotional.
Although research evidence has not been uniformly conclusive [88], some autistic adolescents experience anxiety about decision-making, which may be partly due to increased attention to negative outcomes of previous decisions [89]. Emotional exhaustion and anxiety can result from a tendency to collect too much information, and feeling unable to reach a decision [90]. Intolerance of uncertainty, conceptualized as inability to tolerate the emotional and cognitive sequelae triggered by lack of sufficient information in a given situation [91], is commonly seen in autistic people, and contributes to anxiety, depression, and impaired coping [48, 92, 93]. Recent research supports intolerance of uncertainty as a transdiagnostic risk process for the experience of anxiety and depression. Emotion dysregulation has been found to mediate the relationship between intolerance of uncertainty and symptoms of both anxiety and depression [94]. Additionally, alexithymia can lead to confusion and intolerance of uncertainty [28]. There is support, based on cross-sectional data, for a model in which atypical sensory processing (e.g., sensory seeking and sensitivity), along with need for sameness and consistency, drive intolerance of uncertainty, which then partially mediates the experience of anxiety [95].
In light of the aforementioned cognitive-domain risk processes, it is plausible that intervention targeting specific EF processes (e.g., cognitive flexibility) may be helpful. A pilot study of a problem-solving program for autistic young adults showed promising findings with increased problem-solving ability and reduced subjective distress [96]. Likewise, approaches based on the principles of behavioral exposure that facilitate increasing a person’s tolerance of uncertainty might promote greater ability to ‘sit with’ unpredictability. Cognitive-behavioral approaches in this domain have demonstrated impact with autistic children and adolescents [97], but need upward translation to adults [98].
Social: Masking, Motivation, and Societal Factors
Social features common in autism, as well as societal factors broadly, are often strongly linked to mental health issues, including isolation [99], alexithymia, and their associated social consequences such as discrimination, stigma and ableism [100], and the resultant consequences in terms of access to housing, employment, healthcare, and wealth. Loneliness, in particular, may be a distal risk process for depression in this population. Specifically, both social communication impairment [8] and anhedonia, which are rooted in aberrant reward processing [101].
Social cognition, specifically processing of emotional stimuli and mental states, has been strongly linked to unipolar depression [102]. Among non-autistic adults experiencing a depressive episode, deficits have been documented in higher order social cognition (e.g., theory of mind, social perception, and metacognition) [103]. To date, little research has examined social cognition in relation to depression within autism though initial data suggests the links are not direct, and may, in fact, be mediated through executive control deficits [104]. Thus, diminished frontotemporal brain activity during social cognition tasks has been observed in autistic adults, an effect most pronounced among those with co-occurring depression [105].
There are other external and societal risk processes for depression and anxiety. Specifically, bullying and interpersonal victimization [106, 107], social rejection and social exclusion [108], child maltreatment [109], sexual victimization [110, 111], and other adverse interpersonal experiences during adolescence can result in long-term trauma and post-traumatic stress symptoms, difficulties interpreting social situations, depression and loneliness (e.g. [112]). These negative interpersonal experiences can fuel a feedback loop, whereby autistic people experience negative interpersonal interactions and thus grow less motivated to re-experience social contact due to the negative experience, and thus become more solitary, isolated, lonely, and at increased risk for further social rejection [107].
The historically pervasive but highly contested social motivation hypothesis [113] purports that autistic people find social stimuli less meaningful and less rewarding than do non-autistic people [114]. However, more recent research suggests that in fact any motivational impairments characteristic of ASD are not necessarily specific to the social domain [60]. Other aspects of stimuli, for instance perceptual factors, may play a significant role in motivation. Studies of face processing in autism have found perceptual differences contributing to motivation in unstructured tasks. With more explicit instructions, autistic individuals perform better, as well as show significant activity in fusiform face area [115]. Moreover, motivation for face processing can also be enhanced by familiar, familial, and friendly faces than random face stimuli [116]. For a detailed examination of the social motivation hypothesis and a critique of its assumptions, see [117]. Risk for depression may be higher among autistic people with intact social motivation, due to the mismatch between desire for social engagement and deficits in ability to form quality relationships or lack of self-confidence in one’s ability to do so [8].
Autistic burnout is similar to, yet distinct from, general psychological or occupational burnout [118–121]. Autistic burnout captures stress, intolerance, and chronic exhaustion that results from the compounding of cumulative stress, barriers to effective supports that could provide respite or relief, and resource depletion associated with masking autistic features while trying to perform other effortful tasks. Similarly, risk for psychopathology may be heightened through a confluence of high levels of negative social life events, lack of interpersonal reinforcement, and impoverished sense of mastery or competence. This model of depression etiology in ASD is consistent with the interpersonal model of depression [122], while identifying risk factors somewhat unique to autism.
There is specific evidence to suggest that for many autistic people, the strain of “masking” or attempting to camouflage autistic traits in order to increase social acceptance can lead to severe depletion of internal resources, anxiety, and depression [121, 123]. The cumulative stress of masking is often compounded by on-going experiences of interpersonal rejection, social isolation, societal-level stigma related to living with a disability, and barriers to receiving effective helping services.
Negative experiences with therapeutic and support services that are intended to help autistic people unfortunately can increase risk for depression and anxiety. For example, Applied Behavior Analysis (ABA) was founded on theories of operant conditioning, and based on the idea that clinicians should use reinforcement, punishment, extinction, and repetition to extinguish particular behaviors and increase communication in autistic youth [124, 125]. Evidence is now emerging to suggest that at least for some autistic youth, the experience of participating in ABA caused psychological distress and trauma (e.g., [126–128], methodological criticisms of this nascent body of research notwithstanding (e.g., [129–131].
Intervention often includes helping the person identify sustainable support networks outside one’s family [132]. Providers can help the person identify affinity groups, social networks or individuals, while also respecting that the autistic person may have variable desire and may need reprieve from social demands (i.e., wanting social discourse, but also finding it taxing). To some degree, to effectively address motivational processes therapeutically, we need to consider both individual targets and societal change. In other words, intervention that targets social motivation or social skills alone will likely be less impactful than an intervention that targets double empathy issues, interpersonal relationship health, and broader acceptance of differences in motivation and social wanting.
Some research suggests that autistic people who have a social identity as autistic may experience better self-esteem than autistic peers without that identity, and that this positive social identity buffers against depression and anxiety [133]. One study has found that autistic people who have experienced acceptance from external sources, and accept themselves as autistic, experience lower rates of depression [134]. Adults who receive an autism diagnosis in adulthood may experience self-compassion, feel more able to engage in self-care, and feel less self-critical for not conforming to societal expectations [135]. A recent study of 109 autistic adults found that those who adopted a neurodiversity-embracing attitude had higher self-esteem and better subjective well-being than autistic people who viewed autism as a disorder [136]. Finally, autistic people with mental health needs also face challenges identifying, getting access to and receiving counseling and psychotherapy [137]. Importantly, psychotherapists too rarely receive training in autism, lack general knowledge about autism, and may either refuse to treat autistic people or provide less than optimal care [138–140].
Conclusions
We have highlighted research underlying the interplay of autism with mental health conditions and have suggested that with this knowledge, there may be ways to interrupt the feedback loops which maintain them. We note that understanding of interactions between autism and mental health is in its infancy. Additionally, much of the extant research has focused on autistic people with lower service needs, and therapeutic mental health interventions have, for the most part, been explicitly targeted to this group (e.g., [141]). Our understanding of co-occurring psychiatric conditions, much less risk processes, in profoundly affected people and those with intellectual disability, as well as females, is considerably underdeveloped. It does appear, however, that degree of support need moderates the expression or type of mental health problem (e.g., mood, anxiety problems may be more common among autistic individuals without intellectual disability, whereas aggression and inattention are more problematic among those with higher needs).
Research on the processes that increase risk has begun to inform targeted prevention and intervention work. In this review, we summarized research across the broad domains of cognitive, affective, and social functioning. Consistent with an experimental therapeutics framework [21] to intervention design and evaluation, in which the proximal processes thought to be both malleable and responsible for development or perpetuation of the target behavior (e.g., aggression) are modified, we sought to identify the most viable risk processes within each domain. We assert that this approach holds promise in terms of cost, efficiency, and clinical impact, as clinicians and scientists address the mental health crisis in this population.
Footnotes
Declarations
Conflict of Interest Dr. White reports grants from the National Institutes of Health, the Department of Defense, the Patient Centered Outcomes Research Institute, and the Organization for Autism Research, during the conduct of this study. She is also a paid consultant to Mazzy Health LLC, inc., outside the submitted work. Dr. Siegle reports grants from the National Institutes of Health and receives royalty payments on a patent regarding vibroacoustic intervention technology, licensed to Apollo Neurosciences, which is being evaluated for applications to autism. Dr. Kana reports grants from National Institutes of Health. Dr. Rothman reports grants from National Institutes of Health, the Department of Defense, the Patient Centered Outcomes Research Institute, and the Organization for Autism Research.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR. 2022. [Google Scholar]
- 2.Lewis LF. Exploring the Experience of Self-Diagnosis of Autism Spectrum Disorder in Adults. Arch Psychiatr Nurs. 2016;30(5):575–80. 10.1016/j.apnu.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 3.Gotham K, Brunwasser SM, Lord C. Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. J Am Acad Child Adolesc Psychiatry. 2015;54(5):369–376. e3. 10.1016/j.jaac.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollocks MJ, Lerh JW, Magiati I, Meiser-Stedman R, Brugha TS. Anxiety and depression in adults with autism spectrum disorder: A systematic review and meta-analysis. Psychol Med. 2019;49(4). 10.1017/S0033291718002283. [DOI] [PubMed] [Google Scholar]
- 5.Benevides TW, et al. Listening to the autistic voice: Mental health priorities to guide research and practice in autism from a stakeholder-driven project. Autism. 2020;24(4):822–33. 10.1177/1362361320908410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cadman T et al. NEW RESEARCH Caregiver Burden as People With Autism Spectrum Disorder and Attention-Deficit/Hyper-activity Disorder Transition into Adolescence and Adulthood in the United Kingdom. [Online]. Available: www.jaacap.org [DOI] [PubMed] [Google Scholar]
- 7.Joshi G, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: A comparative study. J Autism Dev Disord. 2013;43(6):1314–25. 10.1007/s10803-012-1679-5. [DOI] [PubMed] [Google Scholar]
- 8.Smith IC, White SW. Socio-emotional determinants of depressive symptoms in adolescents and adults with autism spectrum disorder: A systematic review. Autism. 2020;24(4):995–1010. 10.1177/1362361320908101. [DOI] [PubMed] [Google Scholar]
- 9.Lugo-Marín J et al. Prevalence of psychiatric disorders in adults with autism spectrum disorder: A systematic review and meta-analysis. Res Autis Spect Dis. 2019;59. Elsevier Ltd, pp. 22–33. 10.1016/j.rasd.2018.12.004. [DOI] [Google Scholar]
- 10.Russell AJ, Mataix-Cols D, Anson M, Murphy DG. Obsessions and Compulsions in Asperger Syndrome and High-Functioning Autism. Brit J Psychiat J Ment Sci. 2005;186:525–528. [DOI] [PubMed] [Google Scholar]
- 11.Hofvander B et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiat. 2009;9. 10.1186/1471-244X-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tantam D Lifelong Eccentricity and Social Isolation. I. Psychiatric, Social, and Forensic Aspects. Br J Psychiatry. 1988;153:777–82. [DOI] [PubMed] [Google Scholar]
- 13.Vohra R, Madhavan S, Sambamoorthi U. Emergency Department Use Among Adults with Autism Spectrum Disorders (ASD). J Autism Dev Disord. 2016;46(4):1441–54. 10.1007/s10803-015-2692-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vohra R, Madhavan S, Sambamoorthi U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism. 2017;21(8):995–1009. 10.1177/1362361316665222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kõlves K, Fitzgerald C, Nordentoft M, Wood SJ, Erlangsen A. Assessment of Suicidal Behaviors Among Individuals With Autism Spectrum Disorder in Denmark. JAMA Netw Open. 2021;4(1):e2033565. 10.1001/jamanetworkopen.2020.33565. [DOI] [PubMed] [Google Scholar]
- 16.Anderson-Chavarria M The autism predicament: models of autism and their impact on autistic identity. Disabil Soc. 2022;37(8):1321–41. 10.1080/09687599.2021.1877117. [DOI] [Google Scholar]
- 17.Courchesne V, et al. Interests and Strengths in Autism, Useful but Misunderstood: A Pragmatic Case-Study. Front Psychol. 2020;11. 10.3389/fpsyg.2020.569339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White SW, Schall C, Santos JD, Maddox BB, Hillier A, Klinger L, Pugliese C. Promoting Quality of Life: Suggestions for Mental Health Care Providers Working with Young Autistic Adults. Aut Adult. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.“NIMH » A New Approach to Clinical Trials.” [Online]. Available: https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2014/a-new… [Google Scholar]
- 20.Yarkoni T, Poldrack RA, Nichols TE, Van Essen DC, Wager TD. Scale Automated Synthesis of Human Functional Neuroimaging Data. Nat Methods. 2011;8:665–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.White SW. Introduction to the Special Issue: Experimental Therapeutics in Clinical Child and Adolescent Psychology: Identifying Mechanisms and Moving the Needle. J Clin Child Adoles Psychol. 2022;51(3):261–263. 10.1080/15374416.2022.2051521. [DOI] [PubMed] [Google Scholar]
- 22.Nuske HJ, Vivanti G, Dissanayake C. Are emotion impairments unique to, universal, or specific in autism spectrum disorder? A comprehensive review. Cogn Emot. 2013;27(6):1042–61. 10.1080/02699931.2012.762900. [DOI] [PubMed] [Google Scholar]
- 23.Sivathasan S, Fernandes TP, Burack JA, Quintin EM. Emotion processing and autism spectrum disorder: A review of the relative contributions of alexithymia and verbal IQ. Research in Autism Spectrum Disorders 2020;77. Elsevier Ltd. 10.1016/j.rasd.2020.101608. [DOI] [Google Scholar]
- 24.Berthoz S, Hill EL. The validity of using self-reports to assess emotion regulation abilities in adults with autism spectrum disorder. Eur Psychiatry. 2005;20(3):291–8. 10.1016/j.eurpsy.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 25.Kinnaird E, Stewart C, Tchanturia K. Investigating alexithymia in autism: A systematic review and meta-analysis. Euro Psychiat. 2019;55. Elsevier Masson SAS, pp. 80–89. 10.1016/j.eurpsy.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Albantakis L, et al. Alexithymic and autistic traits: Relevance for comorbid depression and social phobia in adults with and without autism spectrum disorder. Autism. 2020;24(8):2046–56. 10.1177/1362361320936024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Costa AP, Loor C, Steffgen G. Suicidality in Adults with Autism Spectrum Disorder: The Role of Depressive Symptomatology, Alexithymia, and Antidepressants. J Autism Dev Disord. 2020;50(10):3585–97. 10.1007/s10803-020-04433-3. [DOI] [PubMed] [Google Scholar]
- 28.South M, Rodgers J. Sensory, emotional and cognitive contributions to anxiety in autism spectrum disorders. Front Human Neurosci. 2017;11. Frontiers Media S. A. 10.3389/fnhum.2017.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maisel ME, Stephenson KG, South M, Rodgers J, Freeston MH, Gaigg SB. Modeling the cognitive mechanisms Linking autism symptoms and Anxiety in adults. J Abnorm Psychol. 2016;125(5):692–703. 10.1037/abn0000168. [DOI] [PubMed] [Google Scholar]
- 30.Thompson RA. Emotion Regulation: A Theme in Search of Definition. Biol Behav Considerat. 1994. [PubMed] [Google Scholar]
- 31.Khor AS, Melvin GA, Reid SC, Gray KM. Coping, daily hassles and behavior and emotional problems in adolescents with high-functioning autism/Asperger’s disorder. J Autism Dev Disord. 2014;44(3):593–608. 10.1007/s10803-013-1912-x. [DOI] [PubMed] [Google Scholar]
- 32.Jahromi LB, Meek SE, Ober-Reynolds S. Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. J Child Psychol Psychiatry. 2012;53(12):1250–8. 10.1111/j.1469-7610.2012.02560.x. [DOI] [PubMed] [Google Scholar]
- 33.Mazefsky CA, Borue X, Day TN, Minshew NJ. Emotion Regulation Patterns in Adolescents With High-Functioning Autism Spectrum Disorder: Comparison to Typically Developing Adolescents and Association With Psychiatric Symptoms. Autism Res. 2014;7(3):344–54. 10.1002/aur.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Charlton AS, Smith IC, Mazefsky CA, White SW. The Role of Emotion Regulation on Co-occurring Psychopathology in Emerging Adults with ASD. J Autism Dev Disord. 2019. 10.1007/s10803-019-03983-5. [DOI] [PubMed] [Google Scholar]
- 35.Conner CM, White SW, Scahill L, Mazefsky CA. The role of emotion regulation and core autism symptoms in the experience of anxiety in autism. Autism. 2020;24(4):931–40. 10.1177/1362361320904217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brewe AM, Mazefsky CA. White SW. Autism Spectrum Disorder. in Encyclopedia of Autism Spectrum Disorders, Volkmar F, Ed., New York, NY: Springer, 2020. [Google Scholar]
- 37.Girault JB, Piven J. The Neurodevelopment of Autism from Infancy Through Toddlerhood. Neuroimaging Clin N Am. 2020;30(1):97–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piven J, Elison JT, Zylka MJ. Toward a conceptual framework for early brain and behavior development in Autism. Mole Psychiat. 2017;22(10)1385–1394. Nature Publishing Group. 10.1038/mp.2017.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weinstein M, et al. Abnormal white matter integrity in young children with autism. Hum Brain Mapp. 2011;32(4):534–43. 10.1002/hbm.21042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fingher N, et al. Toddlers later diagnosed with autism exhibit multiple structural abnormalities in temporal corpus callosum fibers. Cortex. 2017;97:291–305. 10.1016/j.cortex.2016.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richey JA, et al. Neural Mechanisms of Emotion Regulation in Autism Spectrum Disorder. J Autism Dev Disord. 2015;45(11):3409–23. 10.1007/s10803-015-2359-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kana RK, Patriquin MA, Black BS, Channell MM, Wicker B. Altered Medial Frontal and Superior Temporal Response to Implicit Processing of Emotions in Autism. Autism Res. 2016;9(1):55–66. 10.1002/aur.1496. [DOI] [PubMed] [Google Scholar]
- 43.Tottenham N, Hare TA, Casey BJ. Behavioral assessment of emotion discrimination, emotion regulation, and cognitive control in childhood, adolescence, and adulthood. Front Psychol. 2011;2;1–9. 10.3389/fpsyg.2011.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kliemann D, Dziobek I, Hatri A, Baudewig J, Heekeren HR. The role of the amygdala in atypical gaze on emotional faces in autism spectrum disorders. J Neurosci. 2012;32(28):9469–76. 10.1523/JNEUROSCI.5294-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kleinhans NM, et al. Association between amygdala response to emotional faces and social anxiety in autism spectrum disorders. Neuropsychologia. 2010;48(12):3665–70. 10.1016/j.neuropsychologia.2010.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shalev I, et al. Reexamining empathy in autism: Empathic disequilibrium as a novel predictor of autism diagnosis and autistic traits. Autism Res. 2022;15(10):1917–28. 10.1002/aur.2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Samson AC, Hardan AY, Podell RW, Phillips JM, Gross JJ. Emotion regulation in children and adolescents with autism spectrum disorder. Autism Res. 2015;8(1):9–18. 10.1002/aur.1387. [DOI] [PubMed] [Google Scholar]
- 48.Cai RY, Richdale AL, Uljarević M, Dissanayake C, Samson AC. Emotion regulation in autism spectrum disorder: Where we are and where we need to go. Aut Res. 2018;11(7):962–978. John Wiley and Sons Inc. 10.1002/aur.1968. [DOI] [PubMed] [Google Scholar]
- 49.Mandell D, Siegle GJ, Shutt L, Feldmiller J, Thase ME. Neural substrates of trait ruminations in depression. J Abnorm Psychol. 2014;123(1):35–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mazefsky CA, Collier A, Golt J, Siegle GJ. Neural features of sustained emotional information processing in autism spectrum disorder. Autism. 2020;24(4):941–53. 10.1177/1362361320903137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ibrahim K, et al. Reduced Amygdala-Prefrontal Functional Connectivity in Children With Autism Spectrum Disorder and Co-occurring Disruptive Behavior. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(12):1031–41. 10.1016/j.bpsc.2019.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Prater KE, Hosanagar A, Klumpp H, Angstadt M, Phan KL. Aberrant amygdala-frontal cortex connectivity during perception of fearful faces and at rest in generalized social anxiety disorder. Depress Anxiety. 2013;30(3):234–41. 10.1002/da.22014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Golan O, Haruvi-Lamdan N, Laor N, Horesh D. The comorbidity between autism spectrum disorder and post-traumatic stress disorder is mediated by brooding rumination. Autism. 2022;26(2):538–44. 10.1177/13623613211035240. [DOI] [PubMed] [Google Scholar]
- 54.Crane L, Goddard L, Pring L. Autobiographical memory in adults with autism spectrum disorder: The role of depressed mood, rumination, working memory and theory of mind. Autism. 2013;17(2):205–19. 10.1177/1362361311418690. [DOI] [PubMed] [Google Scholar]
- 55.Siegle GJ, Granholm E, Ingram RE, Matt GE. Pupillary and Reaction Time Measures of Sustained Processing of Negative Information in Depression. 2001. [DOI] [PubMed] [Google Scholar]
- 56.Gotham KO, et al. Pupil response to social-emotional material is associated with rumination and depressive symptoms in adults with autism spectrum disorder. PLoS One. 2018;13(8). 10.1371/journal.pone.0200340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cooper K, Russell A, Calley S, Chen H, Kramer J, Verplanken B. Cognitive processes in autism: Repetitive thinking in autistic versus non-autistic adults. Autism. 2022;26(4):849–58. 10.1177/13623613211034380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buckle KL, Leadbitter K, Poliakoff E, Gowen E. No Way Out Except From External Intervention’: First-Hand Accounts of Autistic Inertia. Front Psychol. 2021;12. 10.3389/fpsyg.2021.631596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Clements CC, Zoltowski AR, Yankowitz LD, Yerys BE, Schultz RT, Herrington JD. Evaluation of the social motivation hypothesis of autism a systematic review and meta-analysis, in JAMA Psychiatry. Am Med Assoc. 2018;797–808. 10.1001/jamapsychiatry.2018.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Keifer CM, Day TC, Hauschild KM, Lerner MD. Social and Nonsocial Reward Anticipation in Typical Development and Autism Spectrum Disorders: Current Status and Future Directions. 1920. 10.1007/s11920-021-01247-7/Published. [DOI] [PubMed] [Google Scholar]
- 61.Wise RA. Dopamine, Learning and Motivation. Nat Rev Neurosci. 2004;5(6):483–94. [DOI] [PubMed] [Google Scholar]
- 62.Schwarz K, et al. Transdiagnostic Prediction of Affective, Cognitive, and Social Function Through Brain Reward Anticipation in Schizophrenia, Bipolar Disorder, Major Depression, and Autism Spectrum Diagnoses. Schizophr Bull. 2020;46(3):592–602. 10.1093/schbul/sbz075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vidal-Ribas P, et al. Bidirectional Associations Between Stress and Reward Processing in Children and Adolescents: A Longitudinal Neuroimaging Study. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(10):893–901. 10.1016/j.bpsc.2019.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barch DM. The relationships among cognition, motivation, and emotion in schizophrenia: How much and how little we know, in Schizophrenia Bulletin. 2005;875–881. 10.1093/schbul/sbi040. [DOI] [PubMed] [Google Scholar]
- 65.Redgrave P, Gurney K. The short-latency dopamine signal: A role in discovering novel actions? Nat Rev Neurosci. 2006;7:967–75. [DOI] [PubMed] [Google Scholar]
- 66.Murty VP, Shah H, Montez D, Foran W, Calabro F, Luna B. Age-related trajectories of functional coupling between the VTA and nucleus accumbens depend on motivational state. J Neurosci. 2018;38(34):7420–7. 10.1523/JNEUROSCI.3508-17.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hallquist MN, Geier CF, Luna B. Incentives facilitate developmental improvement in inhibitory control by modulating control-related networks. Neuroimage. 2018;172:369–80. 10.1016/j.neuroimage.2018.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Conner CM, White SW. Brief Report: Feasibility and Preliminary Efficacy of Individual Mindfulness Therapy for Adults with Autism Spectrum Disorder. J Autism Dev Disord. 2018;48(1). 10.1007/s10803-017-3312-0. [DOI] [PubMed] [Google Scholar]
- 69.Schopler E, Mesibov GB. Learning and Cognition in Autism. New York, NY:. Springer Science & Business Media. 2013. [Google Scholar]
- 70.Tregay J Book Review: Sensory Perceptual Issues in Autism and Asperger Syndrome: Different Sensory Experiences - Different Perceptual Worlds. Autism. 2006;10(1):117–8. 10.1177/1362361306062016. [DOI] [Google Scholar]
- 71.Howell JW, Heck DH. Cognition, Motor Control and Other Aspects of Autism: A Pragmatic Review, in The Molecular Basis of Autism, Fatemi SH, Ed., New York, NY: Springer. 2015;393–406. [Google Scholar]
- 72.Gillberg C, Billstedt E. Autism and Asperger syndrome: Coexistence with other clinical disorders. Acta Psychiatr Scand. 2000;102(5):321–30. 10.1034/j.1600-0447.2000.102005321.x. [DOI] [PubMed] [Google Scholar]
- 73.Bradley EA, Summers JA, Wood HL, Bryson SE. Comparing Rates of Psychiatric and Behavior Disorders in Adolescents and Young Adults with Severe Intellectual Disability with and without Autism. 2004. [DOI] [PubMed] [Google Scholar]
- 74.Tsakanikos E, Bouras N, Sturmey P, Holt G. Psychiatric co-morbidity and gender differences in intellectual disability. J Intellect Disabil Res. 2006;50(8):582–7. 10.1111/j.1365-2788.2006.00832.x. [DOI] [PubMed] [Google Scholar]
- 75.Johnston K, Murray K, Spain D, Walker I, Russell A. Executive Function: Cognition and Behaviour in Adults with Autism Spectrum Disorders (ASD). J Autism Dev Disord. 2019;49(10):4181–92. 10.1007/s10803-019-04133-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.St. John T, Woods S, Bode T, Ritter C, Estes A. A review of executive functioning challenges and strengths in autistic adults. Clin Neuropsychol. 2022;36(5):1116–1147. Routledge. 10.1080/13854046.2021.1971767. [DOI] [PubMed] [Google Scholar]
- 77.Uddin LQ. Brain Mechanisms Supporting Flexible Cognition and Behavior in Adolescents With Autism Spectrum Disorder. Biol Psychiat. 2021;89(2):172–183. Elsevier Inc. 10.1016/j.biopsych.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Monsell S Task switching. Trends in Cognitive Sciences. 2003;7(3):134–140. Elsevier Ltd. 10.1016/S1364-6613(03)00028-7. [DOI] [PubMed] [Google Scholar]
- 79.Conner CM, Elias R, Smith IC, White SW. Emotion regulation and executive function: Associations with depression and anxiety in autism. Res Autism Spectr Disord. 2023;101. 10.1016/j.rasd.2023.102103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gotham K, Bishop SL, Brunwasser S, Lord C. Rumination and perceived impairment associated with depressive symptoms in a verbal adolescent-adult ASD sample. Autism Res. 2014;7(3):381–91. 10.1002/aur.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7(2):336. [DOI] [PubMed] [Google Scholar]
- 82.Tafet GE, Nemeroff CB. The links between stress and depression: Psychoneuroendocrinological, genetic, and environmental interactions. J Neuropsychiatry Clin Neurosci. 2016;28(2):77–88. 10.1176/appi.neuropsych.15030053. [DOI] [PubMed] [Google Scholar]
- 83.Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Ann N Y Acad Sci. 2012;1251:E1–24. 10.1111/j.1749-6632.2012.06751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McRae K, Zarolia P. Cognition and Emotion in Emotion Dysregulation, in The Oxford Handbook of Emotion Dysregulation, Beauchaine TP and Crowell SE, Eds., New York, NY: Oxford University Press, 2020;39–52. [Google Scholar]
- 85.Jazaieri H, Uusberg H, Uusberg A, Gross JJ. Cognitive Processes and Risk for Emotion Dysregulation, in Oxford Handbook of Emotion Dysregulation, Beauchaine TP and Crowell SE, Eds., New York, NY: Oxford University Press. 2020;127–140. [Google Scholar]
- 86.Zelazo PD. Executive function and psychopathology: A neurodevelopmental perspective. Annu Rev Clin Psychol. 2020;16:431–54. [DOI] [PubMed] [Google Scholar]
- 87.Romer AL, Pizzagalli DA. Is executive dysfunction a risk marker or consequence of psychopathology? A test of executive function as a prospective predictor and outcome of general psychopathology in the adolescent brain cognitive development study®. Dev Cogn Neurosci. 2021;51. 10.1016/j.dcn.2021.100994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vella L, Ring HA, Aitken MRF, Watson PC, Presland A, Clare ICH. Understanding self-reported difficulties in decision-making by people with autism spectrum disorders. Autism. 2018;22(5):549–59. 10.1177/1362361316687988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yechiam E, Busemeyer JR, Stout JC, Bechara A. Using Cognitive Models to Map Relations Between Neuropsychological Disorders and Human Decision-Making Deficits. 2005. [DOI] [PubMed] [Google Scholar]
- 90.Luke L, Clare ICH, Ring H, Redley M, Watson P. Decision-making difficulties experienced by adults with autism spectrum conditions. Autism. 2012;16(6):612–21. 10.1177/1362361311415876. [DOI] [PubMed] [Google Scholar]
- 91.Carleton RN. Into the unknown: A review and synthesis of contemporary models involving uncertainty. J Anxiet Dis. 2016;39:30–43. Elsevier Ltd. 10.1016/j.janxdis.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 92.Buhr K, Dugas MJ. The role of fear of anxiety and intolerance of uncertainty in worry: An experimental manipulation. Behav Res Ther. 2009;47(3):215–23. 10.1016/j.brat.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 93.Vasa RA, Keefer A, Reaven J, South M, White SW. Priorities for Advancing Research on Youth with Autism Spectrum Disorder and Co-occurring Anxiety. J Autism Dev Disord, vol. 48, no. 3, 2018, doi: 10.1007/s10803-017-3320-0. [DOI] [PubMed] [Google Scholar]
- 94.Conner CM, Kim PS, White SW, Mazefsky CA. The role of emotion dysregulation and intolerance of uncertainty in autism: Transdiagnostic factors influencing co-occurring conditions. Res Dev Disabil. 2022;130. 10.1016/j.ridd.2022.104332. [DOI] [PubMed] [Google Scholar]
- 95.Normansell-Mossa KM, Top DN, Russell N, Freeston M, Rodgers J, South M. Sensory Sensitivity and Intolerance of Uncertainty Influence Anxiety in Autistic Adults. Front Psychol. 2021;12. 10.3389/fpsyg.2021.731753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pugliese CE, White SW. Brief report: Problem solving therapy in college students with autism spectrum disorders: Feasibility and preliminary efficacy. J Autism Dev Disord. 2014;44(3). 10.1007/s10803-013-1914-8. [DOI] [PubMed] [Google Scholar]
- 97.Kenworthy L, et al. Randomized controlled effectiveness trial of executive function intervention for children on the autism spectrum. J Child Psychol Psychiatry. 2014;55(4):374–83. 10.1111/jcpp.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wallace GL, et al. Real-World Executive Functions in Adults with Autism Spectrum Disorder: Profiles of Impairment and Associations with Adaptive Functioning and Co-morbid Anxiety and Depression. J Autism Dev Disord. 2016;46(3):1071–83. 10.1007/s10803-015-2655-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Seifert N, Seddig D, Eckhard J. Does social isolation affect physical and mental health? A test of the social causation hypothesis using dynamic panel models with fixed effects. Aging Ment Health. 2022;26(7):1353–67. 10.1080/13607863.2021.1961125. [DOI] [PubMed] [Google Scholar]
- 100.Han E, Scior K, Avramides K, Crane L. A systematic review on autistic people’s experiences of stigma and coping strategies. Aut Res. 2022;15(1):12–26. John Wiley and Sons Inc. 10.1002/aur.2652. [DOI] [PubMed] [Google Scholar]
- 101.Han GT, Tomarken AJ, Gotham KO. Social and nonsocial reward moderate the relation between autism symptoms and loneliness in adults with ASD, depression, and controls. Autism Res. 2019;12(6):884–96. 10.1002/aur.2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Weightman MJ, Air TM, Baune BT. A review of the role of social cognition in major depressive disorder. Frontiers in Psychiatry. 2014;5. Frontiers Media S.A. 10.3389/fpsyt.2014.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ladegaard N, Larsen ER, Videbech P, Lysaker PH. Higher-order social cognition in first-episode major depression. Psychiatry Res. 2014;216(1):37–43. 10.1016/j.psychres.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 104.Hollocks MJ, et al. The Association Between Social Cognition and Executive Functioning and Symptoms of Anxiety and Depression in Adolescents With Autism Spectrum Disorders. Autism Res. 2014;7(2):216–28. 10.1002/aur.1361. [DOI] [PubMed] [Google Scholar]
- 105.Ohtani T, et al. Reduced brain activation in response to social cognition tasks in autism spectrum disorder with and without depression. Neuropsychiatr Dis Treat. 2021;17:3015–24. 10.2147/NDT.S327608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Van Roekel E, Scholte RHJ, Didden R. Bullying among adolescents with autism spectrum disorders: Prevalence and perception. J Autism Dev Disord. 2010;40(1):63–73. 10.1007/s10803-009-0832-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Maïano C, Normand CL, Salvas MC, Moullec G, Aimé A. Prevalence of School Bullying Among Youth with Autism Spectrum Disorders: A Systematic Review and Meta-Analysis. Aut Res. 2016;9(6):601–615. John Wiley and Sons Inc. 2016. 10.1002/aur.1568. [DOI] [PubMed] [Google Scholar]
- 108.Sebastian C, Blakemore SJ, Charman T. Reactions to ostracism in adolescents with autism spectrum conditions. J Autism Dev Disord. 2009;39(8):1122–30. 10.1007/s10803-009-0725-4. [DOI] [PubMed] [Google Scholar]
- 109.McDonnell CG, Boan AD, Bradley CC, Seay KD, Charles JM, Carpenter LA. Child maltreatment in autism spectrum disorder and intellectual disability: results from a population-based sample. J Child Psychol Psychiatry. 2019;60(5):576–84. 10.1111/jcpp.12993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mandell DS, Walrath CM, Manteuffel B, Sgro G, Pinto-Martin JA. The prevalence and correlates of abuse among children with autism served in comprehensive community-based mental health settings. Child Abuse Negl. 2005;29(12):1359–72. 10.1016/j.chiabu.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 111.Dike JE, DeLucia EA, Semones O, Andrzejewski T, McDonnell CG. A Systematic Review of Sexual Violence Among Autistic Individuals. Rev J Autism Dev Disord. 2022. [Google Scholar]
- 112.Taylor JL, Gotham KO. Cumulative life events, traumatic experiences, and psychiatric symptomatology in transition-aged youth with autism spectrum disorder. J Neurodev Disord. 2016;8(1). 10.1186/s11689-016-9160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bottini S Social reward processing in individuals with autism spectrum disorder: A systematic review of the social motivation hypothesis. Res Aut Spect Dis. 2018;45:9–26. Elsevier Ltd. 10.1016/j.rasd.2017.10.001. [DOI] [Google Scholar]
- 114.Dawson G et al. Neurocognitive and electrophysiological evidence of altered face processing in parents of children with autism: Implications for a model of abnormal development of social brain circuitry in autism. Dev Psychopathol. 2005;17(03). 10.1017/s0954579405050327. [DOI] [PubMed] [Google Scholar]
- 115.Hadjikhani N, et al. Activation of the fusiform gyrus when individuals with autism spectrum disorder view faces. Neuroimage. 2004;22(3):1141–50. 10.1016/j.neuroimage.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 116.Pierce K, Redcay E. Fusiform Function in Children with an Autism Spectrum Disorder Is a Matter of ‘Who.’ Biol Psychiatry. 2008;64(7):552–60. 10.1016/j.biopsych.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jaswal VK, Akhtar M. Being versus appearing socially uninterested: Challenging assumptions about social motivation in autism. Behav Brain Sci. 2018;42:e82. 10.1017/s0140525X18001826. [DOI] [PubMed] [Google Scholar]
- 118.Higgins JM, Arnold SRC, Weise J, Pellicano E, Trollor JN. Defining autistic burnout through experts by lived experience: Grounded Delphi method investigating #AutisticBurnout. Autism. 2021;25(8):2356–69. 10.1177/13623613211019858. [DOI] [PubMed] [Google Scholar]
- 119.Arnold SRC, Higgins JM, Weise J, Desai A, Pellicano E, Trollor JN. Confirming the nature of autistic burnout. Autism. 2023. 10.1177/13623613221147410. [DOI] [PubMed] [Google Scholar]
- 120.Mantzalas J, Richdale AL, Dissanayake C. A conceptual model of risk and protective factors for autistic burnout. Autism Research, 2022;15(6):976–987. John Wiley and Sons Inc. 10.1002/aur.2722. [DOI] [PubMed] [Google Scholar]
- 121.Raymaker DM, et al. ‘Having All of Your Internal Resources Exhausted Beyond Measure and Being Left with No Clean-Up Crew’: Defining Autistic Burnout. Autism in Adulthood. 2020;2(2):132–43. 10.1089/aut.2019.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Weissman MM, Markowitz JC, Klerman G. Comprehensive Guide to Interpersonal Psychotherapy. Basic Books. 2000. [Google Scholar]
- 123.Hull L, et al. Is social camouflaging associated with anxiety and depression in autistic adults? Mol Autism. 2021;12(1). 10.1186/s13229-021-00421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Morris EK, Smith NG, Altus DG. B.F. Skinner’s contributions to applied behavior analysis. Behav Anal. 2005;258:99–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Smith T, Eikeseth S. O. Ivar Lovaas: Pioneer of applied behavior analysis and intervention for children with autism. J Autism Dev Disord. 2011;41(3):375–8. 10.1007/s10803-010-1162-0. [DOI] [PubMed] [Google Scholar]
- 126.Sandoval-Norton AH, Shkedy G. How much compliance is too much compliance: Is long-term ABA therapy abuse? Cog Psychol. 2019;6(1). Cogent OA. 10.1080/2331908.2019.1641258. [DOI] [Google Scholar]
- 127.Kupferstein H Evidence of increased PTSD symptoms in autistics exposed to applied behavior-analysis. Advances in Autism. 2018;4(3):122–9. [Google Scholar]
- 128.Kirkham P ‘The line between intervention and abuse’ – autism and applied behaviour analysis. Hist Human Sci. 2017;30(2):107–26. 10.1177/0952695117702571. [DOI] [Google Scholar]
- 129.Gorycki KA, Ruppel PR, Zane T. Is long-term ABA therapy abusive: A response to Sandoval-Norton and Shkedy. Cogent Psychol. 2020;7(1). 10.1080/23311908.2020.1823615. [DOI] [Google Scholar]
- 130.Leaf JB, Ross RK, Cihon JH, Weiss MJ. Evaluating Kupferstein’s claims of the relationship of behavioral intervention to PTSS for individuals with autism. Advances in Autism. 2018;4(3):122–9. 10.1108/AIA-02-2018-0007. [DOI] [Google Scholar]
- 131.Chown N, Hughes E, Leatherland J, Davison S. Response to Leaf et al’s critique of Kupferstein’s finding of a possible link between applied behavior analysis and post-traumatic stress disorder. Adv Autism. 2019;5(4):318. 10.1108/AIA-01-2019-0002. [DOI] [Google Scholar]
- 132.Hussain M, Jones JM. Discrimination, diversity, and sense of belonging: Experiences of students of color. J Divers High Educ. 2021;14(1):63–71. [Google Scholar]
- 133.Cooper K, Smith LGE, Russell A. Social identity, self-esteem, and mental health in autism. Eur J Soc Psychol. 2017;47(7):844–54. 10.1002/ejsp.2297. [DOI] [Google Scholar]
- 134.Cage E, Di Monaco J, Newell V. Experiences of Autism Acceptance and Mental Health in Autistic Adults. J Autism Dev Disord. 2018;48(2):473–84. 10.1007/s10803-017-3342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wilson RB, Thompson AR, Rowse G, Smith R, Dugdale AS, Freeth M. Autistic women’s experiences of self-compassion after receiving their diagnosis in adulthood. Autism. 2022. 10.1177/13623613221136752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ferenc K, Płatos M, Byrka K, Król ME. Looking through rainbow-rimmed glasses: Taking neurodiversity perspective is related to subjective well-being of autistic adults. Autism. 2022. 10.1177/13623613221135818. [DOI] [PubMed] [Google Scholar]
- 137.Maddox BB, Dickson KS, Stadnick NA, Mandell DS, Brookman-Frazee L. Mental Health Services for Autistic Individuals Across the Lifespan: Recent Advances and Current Gaps. Curr Psychiat Rep. 2021;23(10). Springer. 10.1007/s11920-021-01278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Adams D, Young K. A Systematic Review of the Perceived Barriers and Facilitators to Accessing Psychological Treatment for Mental Health Problems in Individuals on the Autism Spectrum. Rev J Autism Dev Disord. 2021;8(4):436–53. 10.1007/s40489-020-00226-7. [DOI] [Google Scholar]
- 139.Lipinski S, Boegl K, Blanke ES, Suenkel U, Dziobek I. A blind spot in mental healthcare? Psychotherapists lack education and expertise for the support of adults on the autism spectrum. Autism. 2022;26(6):1509–21. 10.1177/13623613211057973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Darazsdi Z, Bialka CS. ‘Oh, you couldn’t be autistic’: Examining anti-autistic bias and self-esteem in the therapeutic alliance. Autism. 2023. 10.1177/13623613231154622. [DOI] [PubMed] [Google Scholar]
- 141.Cai RY, Brown L. Cultivating self-compassion to improve mental health in autistic adults. Autism in Adulthood. 2021;3(3):230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]


