Abstract
Lunotriquetral coalitions are the most common form of carpal coalition wherein the cartilage between the lunate and triquetrum ossification centers failed to undergo apoptosis. This technical case report examines the arthrokinematics of bilateral lunotriquetral coalitions with dissimilar Minnaar types in one participant with one asymptomatic wrist and one wrist with suspected distal radioulnar joint injury. Static and dynamic (four-dimensional) CT images during pronosupination were captured using a photon-counting detector CT scanner. Interosseous proximity distributions were calculated between the lunotriquetral coalition and adjacent bones in both wrists to quantify arthrokinematics. Interosseous proximity distributions at joints adjacent to the lunotriquetral coalition demonstrate differences in median and minimum interosseous proximities between the asymptomatic and injured wrists during resisted pronosupination. Altered kinematics from lunotriquetral coalitions may be a source of ulnar-sided wrist pain and discomfort, limiting functional range of motion. This case report highlights potential alterations to wrist arthrokinematics in the setting of lunotriquetral coalitions and possible associations with ulnar-sided wrist pain, highlighting anatomy to examine in radiographic follow-up. Further, this case report demonstrates the technical feasibility of four-dimensional CT using photon-counting detector technology in assessing arthrokinematics in the setting of variant wrist anatomy.
Keywords: carpal coalition, distal radioulnar joint, four-dimensional computed tomography, lunotriquetral joint, photon-counting detector computed tomography, wrist biomechanics
Introduction
Lunotriquetral (LT) coalitions are the most prevalent congenital carpal coalitions, with literature-reported prevalence ranging from 0.1% to 9% [1–5]. Females are twice as likely to demonstrate LT coalitions compared to males [2, 6]. Carpal coalitions occur when cartilage between ossification centers incompletely undergoes apoptosis during development from cartilaginous bone precursors. The persistent nonarticular cartilage zone between ossification centers then undergoes endochondral ossification and results in bony coalition [1, 6, 7].
LT coalitions are classified by the extent of ossification between bones. A complete coalition occurs if the structures in the non-articular cartilaginous zone are not replaced by synovium or intracapsular structures [1, 8]. The predominant classification system for LT coalitions is the Minnaar system, which describes LT coalitions as type 1: incomplete fibrocartilaginous coalition; type 2: partial osseous coalition; type 3: complete osseous coalition; and type 4: complete osseous coalition with associated abnormalities [3].
Clinically, LT coalitions are often incidental findings [3, 4]. However, recent case reports describe LT coalitions as a source of ulnar-sided wrist pain, either due to resulting mechanics or posttraumatically [5, 6, 9, 10]. Previous investigations have used two- and three-dimensional static imaging as well as dynamic fluoroscopy to examine incidental LT coalitions [1–4, 6, 10–13]. Dynamic four-dimensional computed tomography (4DCT) imaging offers quantitative assessments of carpal arthrokinematics not limited by anatomic overlap.
The objective of this case report is to examine arthrokinematics of bilateral LT coalitions—as quantified using interosseous proximity distributions at multiple wrist articulations—during pronosupination using 4DCT. This allows: (1) the exploration of arthrokinematics of an asymptomatic wrist with a type 3 LT coalition and (2) comparison with a type 2 LT coalition in a wrist with suspected distal radioulnar joint (DRUJ) injury. This case report offers insight into the kinematic effects of a LT coalition, which may have implications for evaluating other carpal coalitions or surgical LT arthrodesis. Examination of adjacent joint interactions describe potential sources of ulnar-sided wrist pain in this participant and demonstrates how 4DCT-derived arthrokinematics may be used to assess dynamic joint function.
Case Report
The participant was enrolled in an Institutional Review Board-approved prospective study exploring the implementation of 4DCT in aiding diagnosis of ulnar-sided wrist pain. This case report includes data from a 23-year-old white female participant with a suspected right-sided DRUJ injury (enrolled: October 2022). Written informed consent was obtained from the participant. Radiologist interpretation of posteroanterior radiographs reported incidental bilateral LT coalitions of different Minnaar classifications. The right (injured) hand demonstrates a type 2 LT coalition. The left (asymptomatic) hand demonstrates a type 3 LT coalition (Fig. 1).
Fig. 1.
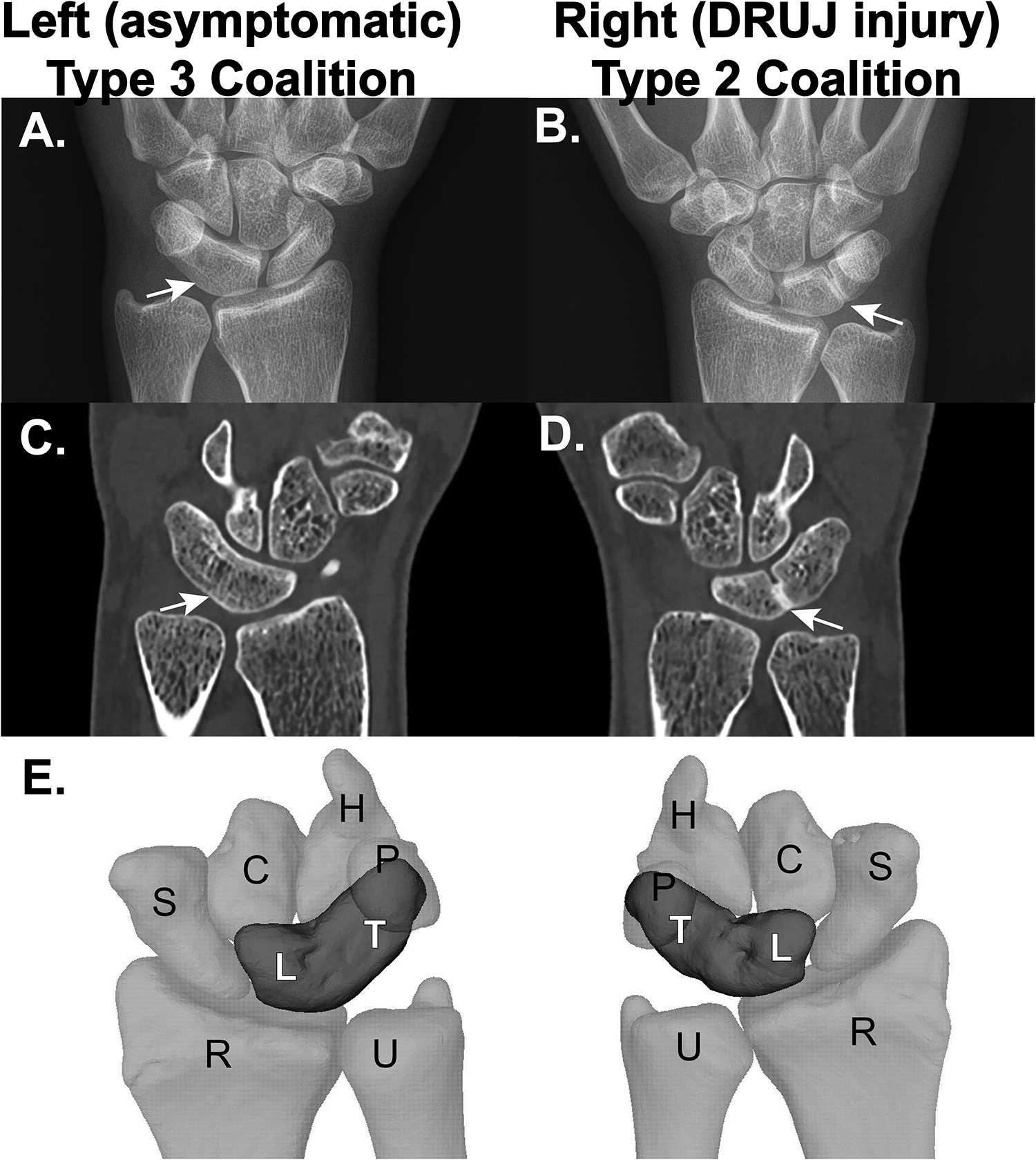
Imaging from a participant presenting with incidental bilateral lunotriquetral (LT) coalitions of dissimilar Minnaar types [3]. Arrows represent areas of osseous bridging. A. Posteroanterior radiograph of left, asymptomatic wrist demonstrating a type 3 LT coalition. B. Posteroanterior radiograph of right wrist with suspected DRUJ injury demonstrating a type 2 LT coalition. C. Coronal CT of left wrist. D. Coronal CT of right wrist. E. Three-dimensional mesh reconstructions of the bilateral LT coalitions (C = capitate, H = hamate, L = lunate, P = pisiform, R = radius, S = scaphoid, T = triquetrum, U = ulna).
Clinical examination of the injured/asymptomatic wrists revealed 70°/80° pronation, 70°/80° supination, 45°/60° dorsiflexion, 55°/65° palmar flexion, 10°/30° radial deviation, 20°/30° ulnar deviation, and grip strength 12 kg/22 kg. The participant was tender over the ulnar fovea with evidence of DRUJ instability. On the Patient-Rated Wrist Evaluation (PRWE) [14], which asks participants to rate levels of wrist pain on a 10-point scale—with higher scores corresponding to greater difficulty—during functional tasks, the participant reported always having wrist pain (10/10) with mild difficulty performing all activities (range: 2–5/10; mean: 3.9/10). Pain at rest was 4/10, with repeated motion 4/10, when lifting heavy objects 6/10, and at its severest intensity 7/10. Preoperative MRI of the right wrist demonstrated evidence of focal foveal triangular fibrocartilage complex (TFCC) perforation near its radial insertion as well as partial tearing near the ulnar foveal and styloid attachments. Arthroscopic examination of the right wrist revealed central and foveal TFCC tears and foveal detachment.
4DCT imaging protocol
The patient was imaged using a commercial dual-source photon-counting detector (PCD) CT system (NAEOTOM Alpha, Siemens Healthineers, Germany), acquiring static 3DCT and dynamic 4DCT scans of both wrists [15, 16]. Details on the scanning protocol, dose estimates, and image quality were similar to those presented previously [17–20]. The participant’s forearms were secured in a padded restraint device [21] (Fig. 2). During static acquisitions, the participant grasped the handles with wrists in a resting, functionally-neutral position. During dynamic acquisitions, the participant was asked to move through maximum comfortable pronosupination arcs at a rate of 35 cycles per minute as cued by an audible metronome set to 70 beats per minute. Pronosupination was performed with resistance applied via linear springs, which produced torsional resistance of 1.9 N∙m/rad. A resisted motion was chosen since most activities of daily living requiring pronosupination involve movement against resistance [22, 23]. This protocol was repeated for both hands. For dynamic acquisitions, fifteen CT volumes were collected over a period of 1.5 seconds (temporal resolution: 66 ms).
Fig. 2.

Images of the A. front and B. back of the resistance and restraint device used in the imaging of pronosupination motion [21]. Resistance was applied via the attachment of linear springs on the back of the device. Participant is positioned for static imaging and situated in a functional neutral position.
Static CT data were reconstructed with a sharp kernel (Br72) with resulting voxel dimensions of 0.234 mm × 0.234 mm × 0.400 mm. Dynamic CT volumes were reconstructed using a cardiac reconstruction algorithm. Dynamic CT volumes were reconstructed with a sharp kernel (Br64) with resulting voxel dimensions of 0.234 mm × 0.234 mm × 0.351 mm.
Image processing
The 4DCT image processing pipeline has been previously reported [17, 18, 24–26]. Briefly, image processing includes interpolation to isotropic voxel sizes using trilinear interpolation, semi-automated segmentation of the radius, ulna, and relevant carpal bones using Analyze 14.0 (Mayo Foundation for Medical Education and Research, Rochester, MN), registration of a segmented static bone to its corresponding bone in each dynamic image volume using Söderkvist’s method (singular value decomposition) on manually-selected point landmarks [27] followed by Nelder-Mead simplex optimization to maximize cross-correlations of surface intensity, computation of six degree-of-freedom osteokinematics, and calculation of interosseous proximities between bone pairs at each position in the pronosupination arc. Forearm pronosupination angle was estimated using the finite helical axis angle between the radius and ulna, relative to the ulna, at each position during pronosupination and reported relative to the forearm bone positions in the static-neutral image [28–32]. Pronation is represented as a positive angle and supination as a negative angle.
Interosseous proximity distributions quantify the distances from each mesh vertex on one bone to the nearest vertex on an adjacent bone. Intercarpal proximities are expected to be <2 mm [33, 34], and DRUJ proximities have been reported <5 mm [35]. A 5 mm distance threshold was applied to all joints for consistency. Interosseous proximity calculations are limited to mesh vertices within defined distance (5 mm) and surface-normal (60°) thresholds [17].
In this analysis, LT coalitions are treated as single bones due to the osseous connections between lunate and triquetrum. Six articulations were included in arthrokinematic analyses: ulna-LT, scaphoid-LT, capitate-LT, hamate-LT, pisiform-LT, and radius-LT. For each articulation, interosseous proximity distributions—which quantify separation between bones at each timepoint in the motion arc—were calculated. Qualitatively, interosseous proximity maps can be used to visualize changes in the location of closest proximity and alterations in the magnitude of the proximity; demonstrative interosseous proximity maps display the articulating areas being quantified (Fig. 3). From these distributions, median (25th – 75th percentile) and minimum interosseous proximities were calculated as summative metrics of interosseous proximity.
Fig. 3.
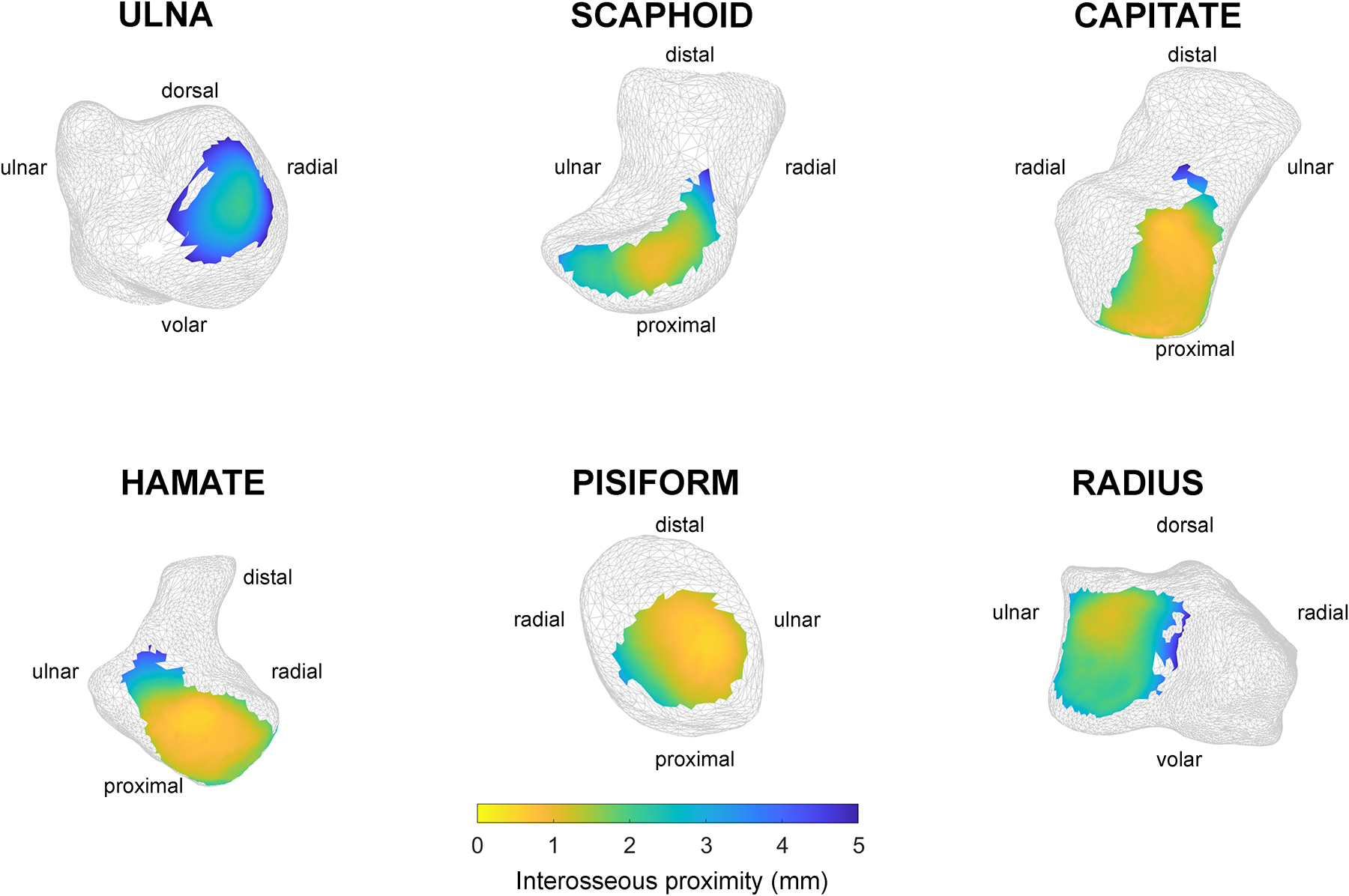
Demonstrative interosseous proximity maps, representing the distribution of interosseous proximities between the lunotriquetral coalition and the indicated bone, for each articulation adjacent to the lunotriquetral coalition from the injured (right) wrist in maximum supination. The medians of the colored proximity map patches at each position in the pronosupination arc were calculated as a summative metric for interosseous proximity during motion.
Results
Interosseous proximity maps at maximum supination and pronation are presented between the LT coalition and pisiform (pisotriquetral joint), projected onto the LT coalition (Fig. 4). Interosseous proximity distributions quantify LT-adjacent arthrokinematics as a function of pronosupination angle (Fig. 5).
Fig. 4.

Interosseous proximity maps between the pisiform and triquetrum, projected onto the LT coalition, at maximum pronation (asymptomatic: 42°; injured: 46°) and maximum supination (asymptomatic: 4°; injured: −4°) for both wrists.
Fig. 5.
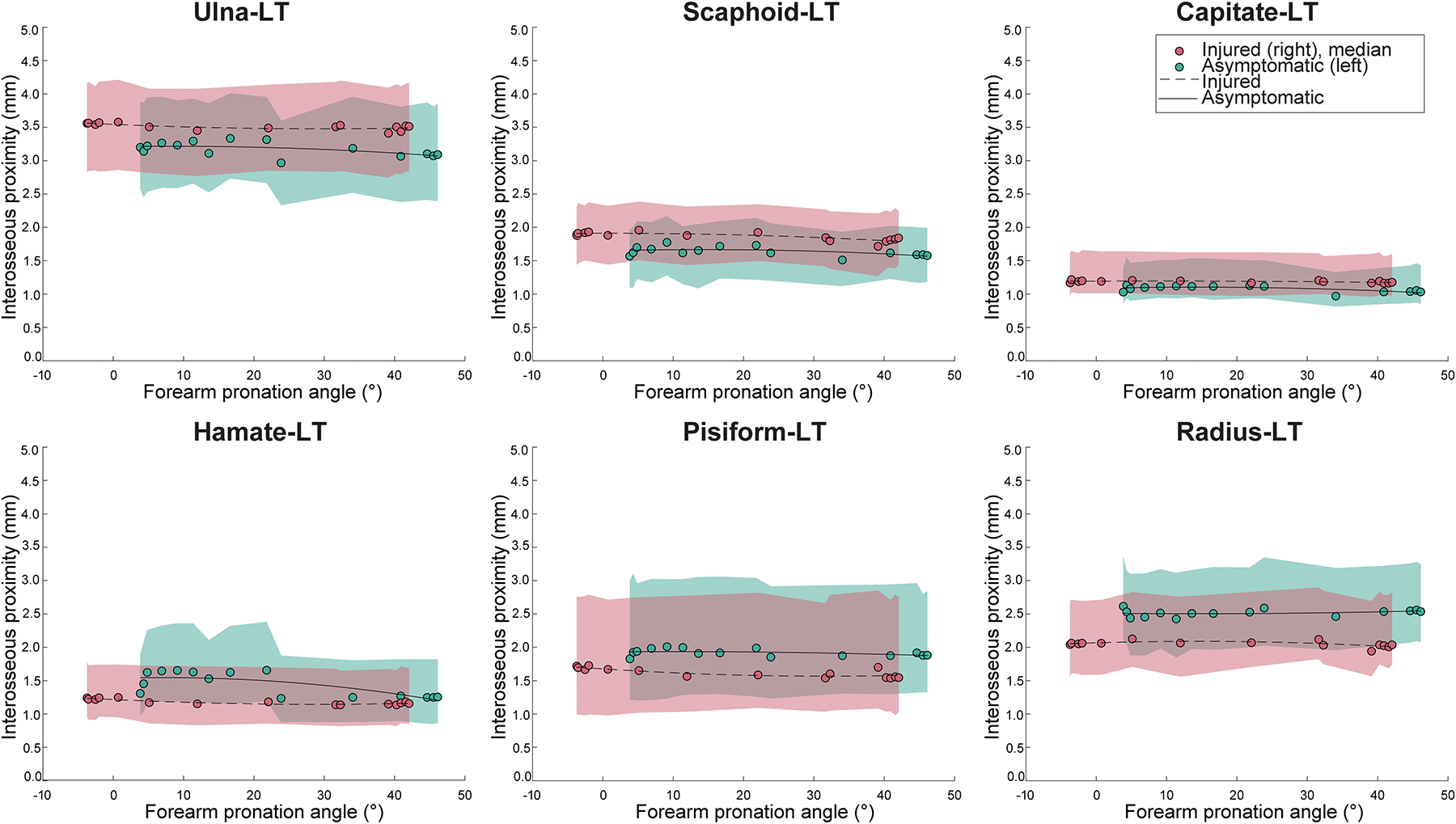
Median (25th – 75th percentile) interosseous proximities during pronosupination at joints adjacent to the LT coalition as a function of forearm pronation angle (pronation: positive angle; supination: negative angle). Second-order lines of best fit are presented for the asymptomatic (solid line) and injured (dashed line) wrists. Shaded areas represent the 25th – 75th percentile interosseous proximities during pronosupination as a function of forearm pronation angle.
At the ulna-LT joint, median (injured: 3.41 – 3.58 mm; asymptomatic: 2.97 – 3.33 mm) and minimum (injured: 1.96 – 2.11 mm; asymptomatic: 1.69 – 2.02 mm) interosseous proximities are increased in the injured versus asymptomatic wrists across the pronosupination arc. The change in the minimum interosseous proximity is most pronounced at maximum pronation (Δ 0.42 mm; injured: 42°, asymptomatic: 46°). At the scaphoid-LT joint, the median (injured: 1.71 – 1.95 mm; asymptomatic: 1.51 – 1.77 mm) and minimum (injured: 0.79 – 1.01 mm; asymptomatic: 0.57 – 0.73 mm) interosseous proximities are increased in the injured versus asymptomatic wrists across the pronosupination arc. At the capitate-LT articulation, there are minimal differences in median (injured: 1.16 – 1.22 mm; asymptomatic: 0.96 – 1.13 mm) and minimum (injured: 0.54 – 0.65 mm; asymptomatic: 0.35 – 0.73 mm) proximities between the two wrists. At the hamate-LT articulation, over wrist orientations of approximately 5° to 22° pronation, median (injured: 1.13 – 1.17 mm; asymptomatic: 1.52 – 1.65 mm) and minimum (injured: 0.38 – 0.43 mm; asymptomatic: 0.58 – 0.66 mm) interosseous proximities are closer (decreased) in the injured versus asymptomatic wrist. For the remainder of the motion cycle, there is minimal difference in the median (injured: 1.17 – 1.24 mm; asymptomatic: 1.23 – 1.26 mm) and minimum (injured: 0.37 – 0.44 mm; asymptomatic: 0.41 – 0.50 mm) hamate-LT interosseous proximities between the two wrists. At the pisiform-LT joint, median (injured: 1.54 – 1.73 mm; asymptomatic: 1.83 – 2.01 mm) and minimum (injured: 0.45 – 0.60 mm; asymptomatic: 0.73 – 0.92 mm) interosseous proximities are closer in the injured versus asymptomatic wrists across the pronosupination arc. At the radius-LT joint, median (injured: 1.93 – 2.12 mm; asymptomatic: 2.42 – 2.61 mm) and minimum (injured: 0.94 – 1.25 mm; asymptomatic: 0.95 – 1.33 mm) interosseous proximities are closer in the injured versus asymptomatic wrists across the pronosupination arc.
Discussion
This novel application of 4DCT to a case of bilateral LT coalitions revealed differences between injured and asymptomatic wrists at most joints adjacent to the osseous coalition during forearm pronosupination. The coalition modifies interosseous proximities at adjacent joints to compensate for limited motion, similar to what is seen after partial carpal arthrodeses [36]. A region of interest may be the pisotriquetral joint, as pisotriquetral osteoarthritis is a common pain generator and underdiagnosed contributor to ulnar-sided wrist pain [37–40]. In this participant, pisotriquetral interosseous proximities were closer in the injured versus asymptomatic wrist (Fig. 5); it is possible that LT coalitions may increase the likelihood of developing pisotriquetral osteoarthritis or that decreased pisotriquetral space is associated with ulnar-sided wrist pain. This is a known complication following surgical lunotriquetral arthrodesis [41, 42].
While this case report lacks a within-participant contralateral comparator or other comparator group without LT coalitions, comparison may be made to static-neutral interosseous proximities from ostensibly healthy wrists without osteoarthritis in the literature (Table 1) [37, 43]. LT coalition-induced rigidity may contribute to differences between the comparator datasets and wrists presented in this case report. The closer interosseous proximities in this case report, when compared to literature-reported values, may be related to ulnar-sided wrist pain. Although it has been conventionally thought that LT coalitions are asymptomatic incidental findings, pain has been reported in persons with LT coalitions [6–8, 10, 44]. As pisotriquetral, triquetrohamate, and lunatocapitate osteoarthritis are potential generators of wrist pain, the closer proximities at these joints in wrists with LT coalitions may be of clinical interest.
Table 1:
Comparison of the minimum interosseous distances reported in literature (Ten Berg et al. (2017), Patterson et al. (1998)) to the minimum interosseous proximities in the injured Minnaar type 2 wrist and uninjured Minnaar type 3 wrist.
| Literature-reported value (mm) | Asymptomatic: measured-LT (Δ), mm (mm) | Injured: measured-LT (Δ), mm (mm) | |
|---|---|---|---|
| Ulna a | 4.05 | 1.69 (2.36) | 1.96 (2.09) |
| Capitate a | 1.19 | 0.57 (0.62) | 0.79 (0.40) |
| Hamate a | 1.09 | 0.35 (0.74) | 0.54 (0.55) |
| Scaphoid a | 1.72 | 0.41 (1.31) | 0.37 (1.35) |
| Pisiform b | 0.80 | 0.73 (0.07) | 0.45 (0.35) |
| Radius a | 1.46 | 0.95 (0.51) | 0.94 (0.52) |
The values represent the minimum interosseous distances relative to the closer of the lunate or triquetrum. The difference (Δ) is the literature-reported value minus the measured value.
= Patterson et al.,
= Ten Berg et al.
Ulnar variance should be considered when interpreting ulnar-sided wrist arthrokinematics [31]. In addition to position-related ulnar variance, wherein the ulna is relatively longer in pronation, a potential concern is ulnar impaction or radioulnar length discrepancy-related ulnotriquetral and triquetrohamate joint motion [23, 44, 45]. Hamate-LT interosseous proximities remained relatively constant in the injured wrist across pronosupination but were closer in pronation than supination in the asymptomatic wrist; however, hamate-LT interosseous proximities were closer in the injured wrist at all positions. Hamate-LT articular interactions and motion constraints may be a therapeutic target for certain wrist disorders [46, 47].
This case report must be viewed in the context of its limitations. While including one participant limits generalizability of the findings, the techniques presented in this case report demonstrate how 4DCT imaging can reveal sources of symptom-provoking anatomy and positions within motion arcs when they occur. It is important to note that, for this participant, maximum supination was near functional neutral. Imaging in other positions, such as ulnar and radial deviation, may provide greater insight into activities impacted by LT coalitions [48]. Given the study design, a causal relationship between LT coalition and ulnar-sided wrist pain cannot be established. While the distinction between symptomatic versus asymptomatic wrists was based on subjective self-reported pain and function, the patient’s clinical MRI and arthroscopic examinations revealed TFCC injury consistent with patient-reported pain.
Understanding arthrokinematics in congenital LT coalition may inform understanding of chronic surgical lunotriquetral arthrodesis sequalae [49]. The procedure may result in nonunions, requiring revision in an average of 31% and up to 57% of cases [42, 50–52]. Using 4DCT, clinicians may identify regions of closer proximities throughout a motion cycle and counsel patients on postoperative rehabilitation and potential risk for adjacent joint osteoarthritis. Radiologists may use 4DCT to detect regions of abnormally close proximity to focus postoperative evaluation of arthrodesed wrists and assess adjacent joint OA progression.
Conclusion
Ulnar-sided wrist pain is prevalent and multifactorial, with a broad spectrum of disorders and structures contributing to functional impairment [23]. This exploratory investigation describes how quantifying arthrokinematics during functional tasks in a participant with bilateral lunotriquetral coalitions revealed articular interactions that could contribute to symptoms. Further, this case report demonstrates the application of 4DCT to nonstandard wrist anatomy, demonstrating how it can be used to investigate different partial wrist fusion techniques and other carpal coalitions.
Acknowledgements
This work was supported by NIH NIAMS R01 AR071338, NIH NIAMS T32 AR056950 (Mayo Clinic Musculoskeletal Research Training Program), NIH NIGMS T32 GM065841 (Medical Scientist Training Program at the Mayo Clinic), NIH NIAMS F31 AR082227, the Mayo Clinic Computed Tomography Clinical Innovation Center, and the generosity of W. Hall Wendel, Jr., to the Mayo Clinic W. Hall Wendel, Jr., Musculoskeletal Center. The authors would like to thank Daniel Hursh, Mayo Clinic Biomedical Imaging Resource Core Facility, for image transfers and Julie Block and Tyson Scrabeck, CCRP, for their contributions as study coordinators. The authors would like to thank the Division of Musculoskeletal Radiology at the Mayo Clinic for the clinical radiology reports and interpretations included in this case report.
Funding:
Multiple authors received funding from the Mayo Clinic Computed Tomography Clinical Innovation Center and the generosity of W. Hall Wendel, Jr., to the Mayo Clinic W. Hall Wendel, Jr., Musculoskeletal Center. Multiple authors received support from the National Institutes of Health (NIH) – NIAMS grant R01 AR071338: “4D CT Imaging for Improved Diagnosis and Treatment of Wrist Ligament Injuries” (Principal Investigator: Zhao KD). One author (TPT) received support from NIH –NIGMS grant T32 GM065841: “Medical Scientist Training Program at Mayo Clinic”, NIH NIGMS grant T32 GM145408: “MSTP at Mayo Clinic Rochester”, NIH – NIAMS grant T32 AR056950: “Mayo Clinic Musculoskeletal Research Training Program”, and NIH – NIAMS grant F31 AR082227.
Conflicts of interest:
RAF has no conflict of interest. TPT received support from NIH –NIGMS grant T32 GM065841: “Medical Scientist Training Program at Mayo Clinic”, NIH NIGMS grant T32 GM145408: “MSTP at Mayo Clinic Rochester”, NIH – NIAMS grant T32 AR056950: “Mayo Clinic Musculoskeletal Research Training Program”, and NIH – NIAMS grant F31 AR082227. CL has no conflict of interest.NMW holds a leadership position (Chair of Technologist and Nurse Educational Committee) in the Society of Cardiovascular Computed Tomography. ART has no conflict of interest. DRH has no conflict of interest. NSM has no conflict of interest. SL receives support from the National Institutes of Health – NIBIB Grant R01 EB028590: “Comprehensive characterization of coronary atherosclerotic disease using photon-counting-detector dual-source CT and its impact on patient management” (Principal Investigators: McCollough CH, Leng S). SK receives royalties or licenses and payment or honoraria for presentations and lectures from Arthrex and consulting fees for Arthrex – Restor 3D; holds stock or stock options in Sonex Health; has other financial or non-financial interests with the American Society for Surgery of the Hand, Journal of Bone and Joint Surgery, and The Bone & Joint Journal. KDZ receives support from the National Institutes of Health – NICHD Grant R01 HD102615: “Toward use of the synergy-based SoftHand Pro for activities of daily living by transradial amputees: A multi-site clinical trial” (Principal Investigators: Santello M, Zhao KD).
Footnotes
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Cockshott WP. Carpal fusions. Am J Roentgenol Radium Ther Nucl Med. 1963; 89:1260–1271. [PubMed] [Google Scholar]
- 2.Garn SM, Frisancho AR, Poznanski AK, Schweitzer J, McCann MB. Analysis of triquetral-lunate fusion. Am J Phys Anthropol. 1971; 34(3):431–433. [DOI] [PubMed] [Google Scholar]
- 3.Devilliers Minnaar AB. Congenital fusion of the lunate and triquetral bones in the South African Bantu. J Bone Joint Surg Br. 1952; 34-b(1):45–48. [DOI] [PubMed] [Google Scholar]
- 4.Delaney TJ, Eswar S. Carpal coalitions. J Hand Surg Am. 1992; 17(1):28–31. [DOI] [PubMed] [Google Scholar]
- 5.Mbaba AN, Ogolodom MP, Wekhe C, Maduka BU. Lunotriquetral coalition: an infrequent cause of wrist pain-a case report. Health Sci J. 2019; 13(4):0–0. [Google Scholar]
- 6.Ritt MJ, Maas M, Bos KE. Minnaar type 1 symptomatic lunotriquetral coalition: a report of nine patients. J Hand Surg Am. 2001; 26(2):261–270. [DOI] [PubMed] [Google Scholar]
- 7.Gross SC, Watson HK, Strickland JW, Palmer AK, Brenner LH, Fatti J. Triquetral-lunate arthritis secondary to synostosis. J Hand Surg Am. 1989; 14(1):95–102. [DOI] [PubMed] [Google Scholar]
- 8.Gottschalk MB, Danilevich M, Gottschalk HP. Carpal coalitions and metacarpal synostoses: a review. Hand (N Y). 2016; 11(3):271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lotter O, Amr A, Stahl S, Clasen S, Schraml C, Pfau M, et al. Pseudarthrosis after disruption of an incomplete luno-triquetral coalition: a case report. Ger Med Sci. 2010; 8:Doc34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simmons BP, McKenzie WD. Symptomatic carpal coalition. J Hand Surg Am. 1985; 10(2):190–193. [DOI] [PubMed] [Google Scholar]
- 11.Hughes PC, Tanner JM. The development of carpal bone fusion as seen in serial radiographs. Br J Radiol. 1966; 39(468):943–949. [DOI] [PubMed] [Google Scholar]
- 12.Metz VM, Schimmerl SM, Gilula LA, Viegas SF, Saffar P. Wide scapholunate joint space in lunotriquetral coalition: a normal variant? Radiology. 1993; 188(2):557–559. [DOI] [PubMed] [Google Scholar]
- 13.Mespreuve M, Vanhoenacker F, Verstraete K. Lunotriquetral coalition, a normal variant that may rarely cause ulnar sided wrist pain. Jbr-btr. 2015; 98(2):72–78. [DOI] [PubMed] [Google Scholar]
- 14.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998; 12(8):577–586. [DOI] [PubMed] [Google Scholar]
- 15.Rajendran K, Petersilka M, Henning A, Shanblatt E, Marsh J Jr., Thorne J, et al. Full field-of-view, high-resolution, photon-counting detector CT: technical assessment and initial patient experience. Phys Med Biol. 2021; 66(20). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajendran K, Petersilka M, Henning A, Shanblatt ER, Schmidt B, Flohr TG, et al. First clinical photon-counting detector CT system: technical evaluation. Radiology. 2022; 303(1):130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trentadue TP, Lopez C, Breighner RE, Fautsch K, Leng S, Holmes DR III, et al. Evaluation of scapholunate injury and repair with dynamic (4D) CT: a preliminary report of two cases. J Wrist Surg. 2023; 12(3):248–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leng S, Zhao K, Qu M, An KN, Berger R, McCollough CH. Dynamic CT technique for assessment of wrist joint instabilities. Med Phys. 2011; 38 Suppl 1(Suppl 1):S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baffour FI, Glazebrook KN, Ferrero A, Leng S, McCollough CH, Fletcher JG, et al. Photon-counting detector CT for musculoskeletal imaging: a clinical perspective. AJR Am J Roentgenol. 2023:1–10. [DOI] [PubMed] [Google Scholar]
- 20.Rajendran K, Baffour F, Powell G, Glazebrook K, Thorne J, Larson N, et al. Improved visualization of the wrist at lower radiation dose with photon-counting-detector CT. Skeletal Radiol. 2023; 52(1):23–29. [DOI] [PubMed] [Google Scholar]
- 21.Amrami KK, Moran SL, Berger RA, Ehman EC, Felmlee JP. Imaging the distal radioulnar joint. Hand Clin. 2010; 26(4):467–475. [DOI] [PubMed] [Google Scholar]
- 22.Chu E, Kim YS, Hill G, Kim YH, Kim CK, Shim JK. Wrist resistance training improves motor control and strength. J Strength Cond Res. 2018; 32(4):962–969. [DOI] [PubMed] [Google Scholar]
- 23.Kakar S, Garcia-Elias M. The “four-leaf clover” treatment algorithm: a practical approach to manage disorders of the distal radioulnar joint. J Hand Surg Am. 2016; 41(4):551–564. [DOI] [PubMed] [Google Scholar]
- 24.Kakar S, Breighner RE, Leng S, McCollough CH, Moran SL, Berger RA, et al. The role of dynamic (4D) CT in the detection of scapholunate ligament injury. J Wrist Surg. 2016; 5(4):306–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao K, Breighner R, Holmes D 3rd, Leng S, McCollough C, An KN. A technique for quantifying wrist motion using four-dimensional computed tomography: approach and validation. J Biomech Eng. 2015; 137(7):0745011–0745015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trentadue TP, Lopez C, Breighner RE, Akbari-Shandiz M, An KN, Leng S, et al. Assessing carpal kinematics following scapholunate interosseous ligament injury ex vivo using four-dimensional dynamic computed tomography. Clin Biomech (Bristol, Avon). 2023; 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Söderkvist I, Wedin PA. Determining the movements of the skeleton using well-configured markers. J Biomech. 1993; 26(12):1473–1477. [DOI] [PubMed] [Google Scholar]
- 28.Ancillao A The helical axis of anatomical joints: calculation methods, literature review, and software implementation. Med Biol Eng Comput. 2022; 60(7):1815–1825. [DOI] [PubMed] [Google Scholar]
- 29.Panjabi M, White AA 3rd. A mathematical approach for three-dimensional analysis of the mechanics of the spine. J Biomech. 1971; 4(3):203–211. [DOI] [PubMed] [Google Scholar]
- 30.Spoor CW, Veldpaus FE. Rigid body motion calculated from spatial co-ordinates of markers. J Biomech. 1980; 13(4):391–393. [DOI] [PubMed] [Google Scholar]
- 31.Akhbari B, Shah KN, Morton AM, Moore DC, Weiss AC, Wolfe SW, et al. Biomechanics of the distal radioulnar joint during in vivo forearm pronosupination. J Wrist Surg. 2021; 10(3):208–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oonk JGM, Dobbe JGG, Strijkers GJ, van Rijn SK, Streekstra GJ. Kinematic analysis of forearm rotation using four-dimensional computed tomography. J Hand Surg Eur Vol. 2022:17531934221142520. [DOI] [PubMed] [Google Scholar]
- 33.Ranota P, Zhang Y, Lalone EA, Suh N. Four-dimensional computed tomography to measure distal radial-ulnar and radio-carpal joint congruency following distal radius fractures. J Orthop. 2021; 25:31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robinson SM, Straatman L, Lee TY, Suh N, Lalone E. Evaluation of four-dimensional computed tomography as a technique for quantifying carpal motion. J Biomech Eng. 2021. [DOI] [PubMed] [Google Scholar]
- 35.Crowe MM, Martin JT, Grier AJ, Spritzer CE, Richard MJ, Ruch DS. In vivo mechanical function of the distal radial ulnar ligaments during rotation of the wrist. J Hand Surg Am. 2020; 45(11):1012–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bain GI, McGuire DT. Decision making for partial carpal fusions. J Wrist Surg. 2012; 1(2):103–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ten Berg PWL, Heeg E, Strackee SD, Streekstra GJ. Joint space narrowing in patients with pisotriquetral osteoarthritis. Hand (N Y). 2017; 12(5):490–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trail IA, Linscheid RL. Pisiformectomy in young patients. J Hand Surg Br. 1992; 17(3):346–348. [DOI] [PubMed] [Google Scholar]
- 39.Coggins CA. Imaging of ulnar-sided wrist pain. Clin Sports Med. 2006; 25(3):505–526, vii. [DOI] [PubMed] [Google Scholar]
- 40.Hayter CL, Gold SL, Potter HG. Magnetic resonance imaging of the wrist: Bone and cartilage injury. Journal of Magnetic Resonance Imaging. 2013; 37(5):1005–1019. [DOI] [PubMed] [Google Scholar]
- 41.Vandesande W, De Smet L, Van Ransbeeck H. Lunotriquetral arthrodesis, a procedure with a high failure rate. Acta Orthop Belg. 2001; 67(4):361–367. [PubMed] [Google Scholar]
- 42.Sennwald GR, Fischer M, Mondi P. Lunotriquetral arthrodesis. A controversial procedure. J Hand Surg Br. 1995; 20(6):755–760. [DOI] [PubMed] [Google Scholar]
- 43.Patterson RM, Elder KW, Viegas SF, Buford WL. Carpal bone anatomy measured by computer analysis of three-dimensional reconstructions of computed tomography images. J Hand Surg Am. 1995; 20(6):923–929. [DOI] [PubMed] [Google Scholar]
- 44.Davis DL. Lunotriquetral coalition and ulnar impaction syndrome: a pictorial essay. Radiol Bras. 2019; 52(2):112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kleinman WB. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am. 2007; 32(7):1086–1106. [DOI] [PubMed] [Google Scholar]
- 46.Kamal RN, Rainbow MJ, Akelman E, Crisco JJ. In vivo triquetrum-hamate kinematics through a simulated hammering task wrist motion. J Bone Joint Surg Am. 2012; 94(12):e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moritomo H, Goto A, Sato Y, Sugamoto K, Murase T, Yoshikawa H. The triquetrum-hamate joint: an anatomic and in vivo three-dimensional kinematic study. J Hand Surg Am. 2003; 28(5):797–805. [DOI] [PubMed] [Google Scholar]
- 48.Logli AL, Schueler BA, Littrell LA, Kakar S. Pronated grip view with wrist deviation: a pilot study on the effect on ulnocarpal relationships. Hand (N Y). 2021:15589447211028928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reagan DS, Linscheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg Am. 1984; 9(4):502–514. [DOI] [PubMed] [Google Scholar]
- 50.Nelson DL, Manske PR, Pruitt DL, Gilula LA, Martin RA. Lunotriquetral arthrodesis. J Hand Surg Am. 1993; 18(6):1113–1120. [DOI] [PubMed] [Google Scholar]
- 51.van de Grift TC, Ritt MJ. Management of lunotriquetral instability: a review of the literature. J Hand Surg Eur Vol. 2016; 41(1):72–85. [DOI] [PubMed] [Google Scholar]
- 52.Shin AY, Weinstein LP, Berger RA, Bishop AT. Treatment of isolated injuries of the lunotriquetral ligament. A comparison of arthrodesis, ligament reconstruction and ligament repair. J Bone Joint Surg Br. 2001; 83(7):1023–1028. [DOI] [PubMed] [Google Scholar]


