Abstract
Healthcare systems face significant challenges in meeting the unique needs of older adults, particularly in the acute setting. Age‐friendly healthcare is a comprehensive approach using the 4Ms framework—what matters, medications, mentation, and mobility—to ensure that healthcare settings are responsive to the needs of older patients. The Age‐Friendly Emergency Department (AFED) is a crucial component of a holistic age‐friendly health system. Our objective is to provide an overview of the AFED model, its core principles, and the benefits to older adults and healthcare clinicians. The AFED optimizes the delivery of emergency care by integrating age‐specific considerations into various aspects of (1) ED physical infrastructure, (2) clinical care policies, and (3) care transitions. Physical infrastructure incorporates environmental modifications to enhance patient safety, including adequate lighting, nonslip flooring, and devices for sensory and ambulatory impairment. Clinical care policies address the physiological, cognitive, and psychosocial needs of older adults while preserving focus on emergency issues. Care transitions include communication and involving community partners and case management services. The AFED prioritizes collaboration between interdisciplinary team members (ED clinicians, geriatric specialists, nurses, physical/occupational therapists, and social workers). By adopting an age‐friendly approach, EDs have the potential to improve patient‐centered outcomes, reduce adverse events and hospitalizations, and enhance functional recovery. Moreover, healthcare clinicians benefit from the AFED model through increased satisfaction, multidisciplinary support, and enhanced training in geriatric care. Policymakers, healthcare administrators, and clinicians must collaborate to standardize guidelines, address barriers to AFEDs, and promote the adoption of age‐friendly practices in the ED.
Keywords: age‐friendly, care transitions, emergency department, multidisciplinary collaboration
1. INTRODUCTION
The aging population of the United States is rapidly increasing, accounting for over 20% of annual emergency department (ED) visits. 1 As it relates to the ED, the current state of healthcare is characterized by the increasing number of older adults, which means an increase in the complexity of acute care, with more patients experiencing geriatric syndromes such as delirium, cognitive impairment, and falls. 2 Also, older adults visit EDs at higher rates than younger adults, and often present with multiple comorbidities, polypharmacy, complex physiologic changes, and multifaceted social and physical needs. 3 Finally, in general, the health systems are ill‐equipped to handle the increased volume and complexity of the vulnerable geriatric population.
The role of EDs in the care of older adults in particular is changing as ambulatory care interventions are becoming integrated into acute and inpatient care. It is now common for EDs to provide what was seen as preventative service, such as screening for chronic illnesses including Hepatitis C and HIV or offering vaccination for influenza and COVID‐19. For older adults, this can also include screening for geriatric specific problems such as cognitive impairment or fall risk.
As a result of these new demands, multiple national societies (American College of Emergency Physicians, American Geriatric Society, Society for Academic Emergency Medicine, and Emergency Nursing Association) developed the Geriatric ED Guidelines, 4 which provides a template for staffing, resources, policies, procedures, and protocols to improve the care of older adults in the ED setting. These guidelines became the basis of the Geriatric Emergency Department Accreditation Program. There are now more than 420 accredited geriatric EDs, mainly in the United States but also in other countries including Canada, Spain, Brazil, and Thailand. 5 GEDs are an important component of an age‐friendly health system (AFHS), which provides a set of four evidence‐based elements of high‐quality care to older adults. The GEDs are based on the geriatric ED guidelines, and accreditation is through the American College of Emergency Physicians (ACEP), while AFHS does not have an underlying guideline but a 4Ms framework within the larger health system. This review article describes the specific challenges and goals of the geriatric emergency department (GED) within the larger umbrella of healthcare within the 4M framework.
2. 4Ms FRAMEWORK
The 4Ms framework for an AFHS is a comprehensive approach focusing on crucial domains to ensure optimal care for older adults. 6 , 7 The origin of 4Ms framework is the key components for AFHS and it is designed to address the unique needs and challenges faced by older adults in healthcare settings comprehensively. In 2017, geriatric experts and health system professionals collaborated with the Institute for Healthcare Improvement to develop the framework. 8
The framework recognizes that addressing the specific needs of older adults requires attention to not only medical issues but also cognitive function, medication, mobility, and personal values. The first “M” stands for what matters to the individual, emphasizing the importance of understanding their unique goals, preferences, and values. The second “M” is for medication, ensuring appropriate prescribing, deprescribing, and medication management to minimize adverse effects and promote health. The third “M” is for mentation, addressing cognitive health and screening for dementia and depression. Finally, the fourth “M” is for mobility, recognizing the significance of maintaining physical function and preventing falls. Each component was evaluated in the non‐ED setting and showed benefits, for example, prevention of delirium, 9 , 10 , 11 risk of adverse event secondary to medications, 12 , 13 prediction of adverse event from mobility assessment, 14 , 15 and advanced care planning. 16 , 17 , 18 , 19 Together, these four dimensions provide a framework that promotes person‐centered care and enhances the overall health and well‐being of older adults within the healthcare system. As EDs are the entranceway into hospitals for over half of admitted patients, EDs can initiate age‐friendly hospital care similarly to how high‐quality sepsis bundles and other important quality measures are started from the ED (Figure 1).
FIGURE 1.
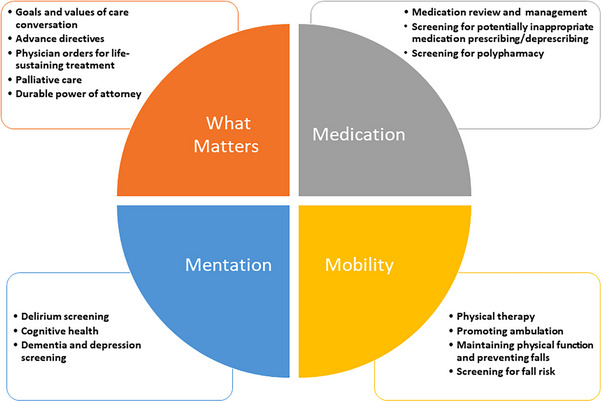
Specific ways in which the 4Ms framework applies to emergency department care.
As >90% of EDs experience inpatient boarding, where inpatient care is being provided in the ED for hours to days, EDs should be aware of age‐friendly practices and have access to the same inpatient resources needed to provide this care. 20 Some have argued that providing mobility, cognition, and other screening in the ED is superfluous because it should be done during primary care visits. Only 38% of older adults get annual exams so the ED visit may be the only opportunity to identify important geriatric syndromes. 21
GED and age‐friendly designation are two separate but overlapping certifications. All components for 4Ms must meet the required goals and a type of care implemented by a hospital or healthcare site to reach age‐friendly designation. In contrast, GED accreditation allows sites to choose from a variety of age‐friendly protocols. These protocols are very specific ways to implement the 4Ms (e.g., document a care process for medication reconciliation in the ED) while the 4Ms allow for broader interpretation and site‐specific adaptation (Supporting Information Appendix).
While we are still awaiting rigorous evaluations of the impact of the 4Ms in the ED on reducing return visits or avoidable admissions, evidence from similarly focused programs like GEDs has shown these types of improvements. As the 4Ms framework is becoming a common language within the healthcare system, coordination of care from clinic to ED, ED to clinic or hospital could improve with active use of 4Ms framework.
2.1. What matters
Aligning clinical care with a patient's goals and preferences can be challenging in the ED where patients are often approached unidimensionally, in the context of their chief complaint only, rather than holistically. In older adults, with complex medical, psychological, and social challenges, better understanding of the patient as a person is essential for thoughtful, high‐value, care delivery.
Understanding priorities of patients by healthcare professionals is perhaps more common in the ambulatory setting. 22 , 23 Reasons for this may include less clinical urgency, presence of family members, and established longitude rapport, all of which is frequently absent in the ED physician/patient relationship.
The literature showed that the successful goals of care conversation can have impact on physical and psychological health in the diverse clinical settings. 16 In the ED, clinicians have reported that discussions surrounding “what matters,” are time consuming and challenging to accomplish. 24 , 25 Moreover, although emergency medicine clinicians may recognize some recurring goals for many older adults, such as the importance of avoiding hospitalization, other priorities for these patients may not be appreciated including maintaining self‐care and independence. 26 In one study, the use of 4Ms showed contrast in acquiring the problem‐oriented goals but was limited on elucidating the underlying goals of care for older adults in the ED. 27 In an effort to increase awareness among physicians, beyond the Institute for Health Care Improvement's 4Ms framework, other subspecialty accreditation bodies, including emergency medicine and surgery, are emphasizing the importance of identifying goals and preferences for older adults. 5
Notwithstanding, the challenges of addressing “what matters” in the ED setting among older adult patients, efforts have been made to better recognize patient priorities. Many initiatives focus within the context of palliative and end of life care, especially among older adult patients in the ED. 28 , 29 , 30 Yet, routine consideration of what matters to older adults, outside of end of life care space, are not as prevalent in practice or the literature. Despite the paucity of routine practices, some initiatives do exist. These successful initiatives include screening for completion of advanced directives 31 or a living will on entry to the ED, routinely asking the “top three things you feel would make this a successful, useful or valuable visit,” 32 staff engagement of older adults during periods of ED waiting to inquire about personal priorities, 33 as well as successful prehospital initiatives by emergency medicine services simply asking “What matters to you today”? 34
The importance of identifying short‐ and long‐term goals of older adult patients and their caregivers or family members remains a challenge in the ED environment. However, with increased focus on this key domain by professional societies and accrediting bodies alike, new and innovative approaches to identifying what matters are certain to emerge.
2.2. Mentation
While delirium, depression, and dementia as the primary targets for the mentation element of the 4Ms, delirium screening is the most evidenced‐based and high‐yield screening in the ED and hospital. Due to constant noise, light, and exposure to crowds and new people, depression screening with a standardized form such as PHQ‐9 and dementia screening are not routine pathways, even when the ED has access to specialty service consultation. 35 As such, depression and dementia assessments are usually deferred to outpatient follow‐up after ED evaluations, and delirium assessment is the largest focus in the ED. That being said, the ED visit is an opportunity to connect patients with care and any patient with new cognitive impairment noted in the ED should be considered at risk and receive a referral for outpatient formal testing and diagnosis.
Delirium screening is a common mentation assessment in geriatric EDs in the United States. 36 Since the choice of delirium screening depends on who can administer it, it requires careful planning for establishing a workflow, training clinicians, and monitoring compliance. Generally, a screening test of choice lands on the workflow for nursing staff including geriatric EM‐trained nursing (for example, GENIE nurse). 37 The model where physicians/advanced practice providers (APPs) perform delirium screenings has yet to gain traction for various reasons, such as lack of time, lack of training, and relevance to the presenting problem.
Using a validated delirium assessment is vital to improving recognition of delirium in the ED. There are three kinds of delirium assessments: patient‐based, 38 proxy‐based, 39 and observational. 40 , 41 Patient‐based delirium assessments, such as confusion assessment method, require the evaluator to interact with the patient and employ bedside cognitive testing to assess the features of delirium. This approach has a potentially high ceiling for diagnostic accuracy. The disadvantages to this approach, however, are that to achieve high diagnostic accuracy, it may require significant training and a lengthier delirium assessment. 42 It also requires raters to conduct additional cognitive testing on the patient, which may be difficult in a setting with significant time constraints such as the ED. Machine learning may be a promising tool to reduce the testing time needed or identify those at higher risk for testing. 43 , 44 , 45 Once identified, there are many ways to manage delirium. AFED should have delirium pathways or toolkits that may utilize additional bedside volunteers or patient care technicians, mobilization with therapists, an evaluation of potential reversible causes of delirium, and reducing agitation from pain or tethering devices such as IVs and cardiac monitors. The rationale for (1) reorientation as a part of nonpharmacological prevention and treatment bundle, 46 , 47 (2) the use of physical therapy (PT) mobilization, 46 and (3) the adverse impact of tethering 47 are now available in the literature.
2.3. Medication
Both the 4Ms framework and the Geriatric ED Guidelines provide medication management recommendations to minimize the use of potentially inappropriate medications (PIMs) and implement ED order sets with geriatric‐appropriate dosing and management plans. Due to polypharmacy, comorbidities, and aging physiology, 48 , 49 , 50 , 51 , 52 older adults are at high‐risk for adverse health outcomes, particularly adverse drug events (ADEs). Importantly, ADEs due to PIMs represent a substantial proportion of ED visits and hospitalizations, leading to increased morbidity and mortality. 49 , 53 , 54 , 55 To improve geriatric medication safety, the American Geriatrics Society (AGS) Beers Criteria was developed to identify PIM use in older adults. 56 It is the policy of the Geriatric ED Guidelines to address the use of medications in the geriatric population presenting to the ED. 57
According to the Geriatric ED Guidelines, it is recommended that all geriatric patients presenting to the ED, regardless of chief complaint, have a medication list obtained and completed, either using pharmacy involvement, 58 , 59 , 60 , 61 , 62 multidisciplinary team, 63 or computer‐based resources. 64 , 65 , 66 The medication list should then be screened for polypharmacy and presence of high‐risk medications, using the AGS Beers Criteria or other established tool (e.g., STOPP/START). 56 , 67 Prior ED studies have shown that pharmacists and technicians reduced medication history errors and resultant medication order errors by over 80%. 68 , 69 Further, early pharmacist‐led medication review in the ED has been shown to decrease odds of admission, hospital length of stay, and unplanned rehospitalizations. 58 , 59 , 62 However, medication reconciliation takes ∼30 min per patient, and even longer for comprehensive medication reviews. 70 Further, early assessment of geriatric patients in the ED by telemedical consultation with a geriatrician significantly reduced the number of PIMs. 63 Computerized clinical decision support tools can also be effective for obtaining an accurate medication review, 64 in addition to supporting ED clinicians in reducing polypharmacy, the rate of PIM prescribing, and subsequent ADEs. 48 , 64 , 65 , 66 , 71 , 72
For older ED patients who screen positive for polypharmacy and/or high‐risk medications, (1) if admitted to the hospital, patients should be referred to the inpatient team for minimizing ADEs during hospitalization and upon discharge or (2) if discharged from the ED, patients should be referred to their primary care physician (PCP) for appropriate long‐term management. For medication management, tracking and trending of high‐risk medication lists for ADEs and pharmacist interventions on an annual basis by the inpatient team/PCP is advised. Due to the chronic and complex nature of geriatric syndromes in older adults, a multidisciplinary team approach is pivotal to providing tailored, high‐quality patient care, which can reduce ED revisits, mortality, and functional decline of older adults 73 , 74 (Figure 2).
FIGURE 2.
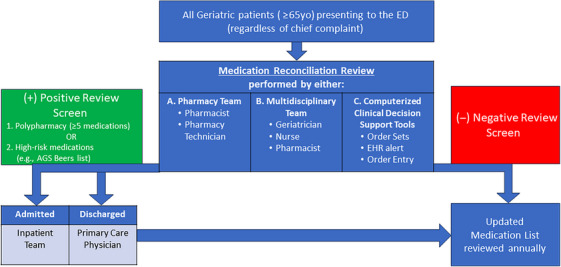
Medication management among older adults in the emergency department.
2.4. Mobility
The role of the mobility assessment in the ED ranges from fall risk assessment, sarcopenia measurement, PT, and whether an assist device is needed. Each ED has slightly different services available. For example, availability of PT service may not be available in all EDs at all times, so the scope of mobility assessments may be very heterogeneous. Furthermore, other EDs may formally evaluate sarcopenia status. One study found that sarcopenia predicted frailty and ED revisits and hospitalization. 75 Chary et al. 76 indicated that PT consultation potentially benefits older adults in the ED, but best practice recommendations are not yet available. Fareed et al. 77 reported that the use of assistive devices helps empower older ED patients engage in their care.
Unfortunately, most ED clinicians are not willing to spend more than a few minutes assessing mobility. 78 EDs are crowded and clinicians find it difficult to allocate sufficient time to determine a patient's fall risk a part of the mobility assessment. 78 Furthermore, with so many patients in hallway stretchers, it may even be difficult to find an area to do functional testing such as a timed up and go test. Finally, patients often present to the ED feeling unwell or in pain and may prefer to focus on management of their acute medical issue or injury. There has been work into using existing data in the electronic health records to target fall risk/mobility screening to those most likely to have needs, thereby reducing the burden on ED nurses. 79 Additional validated fall risk tools such as the 4‐Stage Balance test take under a minute to perform and many GEDs have integrated fall risk evaluation and reduction programs successfully into their standard care. 36
The mobility assessment is closely tied to the fall risk assessment and prevention. Older adults make nearly 3 million ED visits for falls each year. 4 The ED traditionally does not systemically assess patients’ multifactorial fall risks and misses unique opportunities to prevent future falls. 80 Within 6 months of their discharge from the ED, 14% of older nonfall patients experience a fall and up to 48% of older fall patients have a recurrent fall. 81 , 82 Nearly a quarter of older fall patients have a recurrent fall 6 months after their initial ED visit. 83 Since fall‐related emergencies are likely to increase as the population continues to age, and ED patients are a captive audience, the ED visit is the ideal site for a “teachable moment” and intervention. 81
Hence, it is vital the EDs partner with other clinicians, clinics, and/or create innovative fall programs such as telemedicine/mobile integrated health programs to reduce recurrent falls among ED fall patients. There have been several studies showing the benefit of PT and PT/pharmacy for fall patients in terms of decreased recurrent ED visits for falls. 84 , 85 Previous studies 86 , 87 show that multifactorial risk assessment and interventions can significantly decrease recurrent falls. However, other studies have found that ED patients rarely follow up in fall clinics, suggesting that a referral to a clinic may be insufficient to prevent falls. 88 , 89 Newer, more innovative programs that use home programs, community paramedics, and/or telemedicine for fall management are needed to decreased ED use, long ED stays, and recurrent falls. 90 , 91
3. TRANSITION OF CARE
EDs are by design very focused on identifying the optimal healthcare setting for the patient to go to next. Within the first few minutes of the patient/physician encounter, the physician is thinking about whether this patient needs the Intensive Care Unit, the hospital, or is safe to go home (Figure 3). “Safe discharge” can be considered the “s” in the 4Ms framework. 92 Case managers or social workers in the ED setting can be very helpful in teasing out what resources the patient has at home, what setting they currently live in (i.e., community alone, community with family or a caregiver, a senior living facility with some help with transportation and community meals). Understanding the person's current level of care needs and whether they will need more after the acute illness or injury that brought them to the ED is very important for discharge safety. Transitions of care programs from the ED to home or hospital to home have been shown to reduce the need for rehospitalization or sometimes ED revisits, 93 , 94 , 95 but there is no clear model that has significantly improved these outcomes. Most of these programs also evaluate short‐term outcomes (revisits within 30 days, for example), and the effects of having a case manager, improved medication reconciliation, or improved discharge communication may take longer to measure. We do note that current care does not result in good transitions. For example, 25% of older adults discharged from the ED after a fall will have a repeat ED visit within a year and 15% will die within the year. 96 Transitions of care programs that include rehabilitation assessment by physical and/or occupational therapy may be more successful at preventing functional decline and ED revisits. 84 , 97
FIGURE 3.
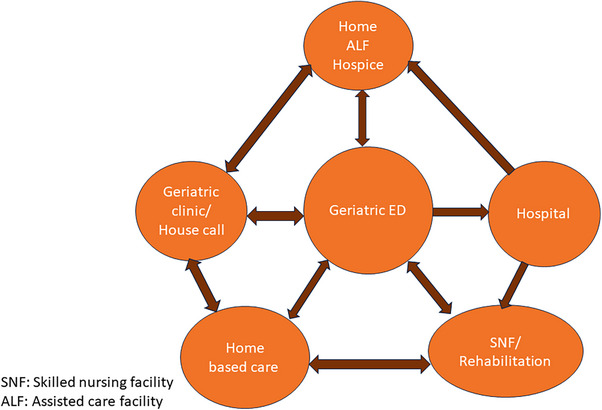
Care transitions within the age‐friendly health system.
Another area of consideration that falls under “safe discharge” or alternatively is sometimes called the “5th M” is mistreatment. Elder mistreatment is common and is experienced by one in six older adults worldwide. 98 , 99 Elder mistreatment comes in many forms, but the most commonly seen in the ED are self‐neglect and caregiver burden/caregiver neglect. Self‐neglect is when a person's medical issues, psychosocial circumstances, or cognitive impairment result in them being unable to or choosing not to care for themselves. This can be very difficult to detect. collateral information from people who witness the home (such as paramedics or home health personnel), family, and friends is very important. Self‐neglect is a high‐risk condition that increases the self‐harm and overall mortality. 100 , 101 , 102 Those with self‐neglect may be treatable by improving access to community services, such as meal delivery programs or home health aides after the underlying condition is treated in the hospital. Or it may require a higher level of care such as placement in a nursing facility or group home. Caregiver burden can be quickly assessed using informal questions (Do you have everything you need at home? Are you able to get enough sleep or take time for yourself?) or formal tools, such as the Caregiver Assessment Tool. 103 Prior studies have found about a third of caregivers of older adults in the EDs are experiencing a high caregiver burden. 104 If there is concern for intentional abuse or neglect, Adult Protective Services or a long‐term care ombudsman should be alerted by ED staff. Integration of a vulnerable elder team or validated screening tool for elder mistreatment increases identification and assists with getting services for these patients. 105 , 106 The transition of care to home and assessment of caregiver burden or elder mistreatment are very important areas of emergency care where the involvement of experienced social work, case management, and rehabilitation teams are critical.
4. CONCLUSION
EDs in the United States serve as the gateway to outpatient and inpatient care for older adults. With their specialized staff and resources, EDs provide immediate medical/surgical attention to older individuals needing emergent care, effectively addressing various health concerns. However, the complexities of healthcare delivery can challenge not only individual health systems but also front‐line nurses, APPs, and physicians. In approaching medically and socially complex patients within the context of multifaceted regulatory requirements and care settings, losing sight of the patient as a person and their immediate needs is common.
The 4Ms framework of what matters, mentation, medications, and mobility can help to create a more feasible approach to the care of complex older adults and ensure that healthcare clinicians continue to focus on patient‐centered, high‐value care practices. The approach using the 4Ms framework to the care of older adults is an approach that embodies the idea behind the phrase “first, do no harm,” attributed to the Greek physician Hippocrates. This sentiment is often overshadowed in the complex and heavily diagnostic/therapeutic based approach to the care of the ED patient. The 4Ms help to refocus the care for older adults on less invasive, patient and family centered, high‐value interventions.
But how can our frontline clinicians incorporate the principles of the 4Ms framework? Although institutional change often comes from senior leadership, the bedside nurse and physicians can adopt the 4Ms framework to the care of the geriatric ED patient. Applying the 4Ms framework throughout the healthcare system can bring consistency in the quality of care. For example, having a record of discussions on what matters in the ED can be reflected in the hospital stay and outpatients after hospital discharge. Another example could be a shared 4Ms individualized for older adults in the electronic health record so ED clinicians review them during the encounter and update them for the care coordination. Reimbursement for this additional work is also needed. The American College of Emergency Physicians passed a resolution at their 2023 council meeting devoted to improving reimbursement for evidence‐based age‐friendly care in the ED. The logistics of integrating 4Ms in the clinical flow can be overcome, but it requires a platform shared by clinicians from different clinical settings, not just in the ED. 107
Formally structuring routine documentation and handoff templates on the 4Ms framework can help remind those at the bedside of the importance of these domains. For EDs with observation units or those with high numbers of boarding older adults, daily rounding practices might follow a 4Ms framework for rounding rather than a more traditional problem or systems‐based approach. Additionally, outlining our discussions with patients and their families using the 4Ms can help with adoption and expectations among those who stand to benefit most from this approach. The 4Ms framework has the potential to enhance the care of older adults presenting to the ED to align with their preferences and improve outcomes while also guiding systematic improvements at the clinicians and health system levels. 108
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Supporting information
Supporting Information
ACKNOWLEDGMENTS
This work was possible as the author (S. L.) received grant from HRSA No. 2 U1QHP287310400 for Geriatric Workforce Enhancement Program. SL received research grants from AstraZeneca, Ceribell INC, honorarium from West Health and John A. Hartford Foundation (JAHF), JrSr Foundation, and University of Hawaii. RMS received research grant funding from the National Institute on Aging (NIA) (R33AG058926, R03AG082923, R21AG084218), the SAEM and Emergency Medicine Foundations (GEM2023‐0000000008), and a honorarium from West Health and JAHF. SWL received funding from the Stepping Strong Foundation, West Health and JAHF, and is GEDA Board Member.
Biography
Sangil Lee is a clinician scientist at the department of emergency medicine, University of Iowa Carver College of Medicine.
Lee S, Skains RM, Magidson PD, Qadoura N, Liu SW, Southerland LT. Enhancing healthcare access for an older population: The age‐friendly emergency department. JACEP Open. 2024;5:e13182. 10.1002/emp2.13182
Drs. Sangil Lee and Rachel M. Skains are first authors.
Supervising Editor: Alexander X. Lo, MD, PhD
REFERENCES
- 1. Cairns C, Kang K. National Hospital Ambulatory Medical Care Survey: 2020 Emergency Department Summary Tables. Centers for Disease Control and Prevention. 2022. doi: 10.15620/cdc:121911 [DOI] [Google Scholar]
- 2. Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780‐791. doi: 10.1111/j.1532-5415.2007.01156.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39(3):238‐247. doi: 10.1067/mem.2002.121523 [DOI] [PubMed] [Google Scholar]
- 4. Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society. Acad Emerg Med. 2014;21(7):806‐809. doi: 10.1111/acem.12415. Emergency Nurses Association, and Society for Academic Emergency Medicine. [DOI] [PubMed] [Google Scholar]
- 5. American College of Emergency Physicians . Home | Geriatric Emergency Department Accreditation. Geriatric Emergency Department Accreditation. Accessed July 20, 2023. https://www.acep.org/geda/
- 6. Cacchione PZ. Age‐friendly health systems: the 4Ms framework. Clin Nurs Res. 2020;29(3):139‐140. doi: 10.1177/1054773820906667 [DOI] [PubMed] [Google Scholar]
- 7. Emery‐Tiburcio EE, Mack L, Zonsius MC, Carbonell E, Newman M. The 4Ms of an age‐friendly health system. Am J Nurs. 2021;121(11):44‐49. doi: 10.1097/01.NAJ.0000799016.07144.0d [DOI] [PubMed] [Google Scholar]
- 8. Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33(7‐8):469‐481. doi: 10.1177/0898264321991658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669‐676. doi: 10.1056/NEJM199903043400901 [DOI] [PubMed] [Google Scholar]
- 10. Ghaeli P, Shahhatami F, Mojtahed Zade M, Mohammadi M, Arbabi M. Preventive intervention to prevent delirium in patients hospitalized in intensive care unit. Iran J Psychiatry. 2018;13(2):142‐147. [PMC free article] [PubMed] [Google Scholar]
- 11. Van Rompaey B, Elseviers MM, Van Drom W, Fromont V, Jorens PG. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care. 2012;16(3):R73. doi: 10.1186/cc11330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Levy HB, Marcus E‐L, Christen C. Beyond the beers criteria: a comparative overview of explicit criteria. Ann Pharmacother. 2010;44(12):1968‐1975. doi: 10.1345/aph.1P426 [DOI] [PubMed] [Google Scholar]
- 13. Hill‐Taylor B, Sketris I, Hayden J, Byrne S, O'Sullivan D, Christie R. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360‐372. doi: 10.1111/jcpt.12059 [DOI] [PubMed] [Google Scholar]
- 14. Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta‐analysis. BMC Geriatr. 2014;14(1):14. doi: 10.1186/1471-2318-14-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beauchet O, Fantino B, Allali G, Muir SW, Montero‐Odasso M, Annweiler C. Timed up and go test and risk of falls in older adults: a systematic review. J Nutr Health Aging. 2011;15(10):933‐938. doi: 10.1007/s12603-011-0062-0 [DOI] [PubMed] [Google Scholar]
- 16. Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long‐term health conditions. Cochrane Database Syst Rev. 2015;2015(3):CD010523. doi: 10.1002/14651858.CD010523.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Berlowitz DR, Foy CG, Kazis LE, et al. Effect of intensive blood‐pressure treatment on patient‐reported outcomes. N Engl J Med. 2017;377(8):733‐744. doi: 10.1056/NEJMoa1611179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Naik AD, McCullough LB. Health intuitions inform patient‐centered care. Am J Bioeth. 2014;14(6):1‐3. doi: 10.1080/15265161.2014.915650 [DOI] [PubMed] [Google Scholar]
- 19. Naik AD, Palmer N, Petersen NJ, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med. 2011;171(5):453‐459. doi: 10.1001/archinternmed.2011.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kelen G. Emergency Department Crowding: The Canary in the Health Care System | NEJM Catalyst. NEJM Catalyst Innovations in Care Delivery. 2021. [Google Scholar]
- 21. Chung S, Romanelli RJ, Stults CD, Luft HS. Preventive visit among older adults with medicare's introduction of annual wellness visit: closing gaps in underutilization. Prev Med. 2018;115:110‐118. doi: 10.1016/j.ypmed.2018.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tinetti ME, Costello DM, Naik AD, et al. Outcome goals and health care preferences of older adults with multiple chronic conditions. JAMA Netw Open. 2021;4(3):e211271. doi: 10.1001/jamanetworkopen.2021.1271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Blaum CS, Rosen J, Naik AD, et al. Feasibility of implementing patient priorities care for older adults with multiple chronic conditions. J Am Geriatr Soc. 2018;66(10):2009‐2016. doi: 10.1111/jgs.15465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bambach K, Southerland LT. Applying geriatric principles to transitions of care in the emergency department. Emerg Med Clin North Am. 2021;39(2):429‐442. doi: 10.1016/j.emc.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bright L, Marr B. Clinical relevance and considerations of palliative care in older adults. Emerg Med Clin North Am. 2021;39(2):443‐452. doi: 10.1016/j.emc.2021.01.007 [DOI] [PubMed] [Google Scholar]
- 26. Gettel CJ, Venkatesh AK, Dowd H, et al. A qualitative study of “what matters” to older adults in the emergency department. West J Emerg Med. 2022;23(4):579‐588. doi: 10.5811/westjem.2022.4.56115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sheber M, McKnight M, Liebzeit D, et al. Older adults’ goals of care in the emergency department setting: a qualitative study guided by the 4Ms framework. J Am Coll Emerg Physicians Open. 2023;4(4):e13012. doi: 10.1002/emp2.13012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Melady D, Perry A. Ten best practices for the older patient in the emergency department. Clin Geriatr Med. 2018;34(3):313‐326. doi: 10.1016/j.cger.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 29. Swenson A, Hyde R. Understanding patients’ end‐of‐life goals of care in the emergency department. J Am Coll Emerg Physicians Open. 2021;2(2):e12388. doi: 10.1002/emp2.12388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bigelow S, Medzon R, Siegel M, Jin R. Difficult conversations: outcomes of emergency department nurse‐directed goals‐of‐care discussions. J Palliat Care. 2024;39(1):3‐12. doi: 10.1177/08258597221149402 [DOI] [PubMed] [Google Scholar]
- 31. Megalla M, Avula R, Manners C, Chinnery P, Perrella L, Finefrock D. Using the 4 M model to screen geriatric patients in the emergency department. J Geriatr Emerg Med. 2021;2(9). doi: 10.17294/2694-4715.1013 [DOI] [Google Scholar]
- 32. Hunold KM, Pereira GF, Jones CW, et al. Priorities of care among older adults in the emergency department: a cross‐sectional study. Acad Emerg Med. 2016;23(3):362‐365. doi: 10.1111/acem.12885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jensen AN, Andersen O, Gamst‐Jensen H, Kristiansen M. Short communication: opportunities and challenges for early person‐centered care for older patients in emergency settings. Int J Environ Res Public Health. 2021;18(23):12526. doi: 10.3390/ijerph182312526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kate Taylor D FNP‐C, CPPS; Desiree Partain, CCP‐C, MHA; Brandon Pate, MPH, CPH, CP‐C, CCP‐C; Laura McEntire, LCSW, ACSW; Audrey Kwik; and Teresa Wagner, DrPH, MS, CPH, RD/LD, CPPS, CHWI, DipACLM, CHWC. Age‐Friendly EMS. EMSWorld . 2022.
- 35. Carpenter CR, Banerjee J, Keyes D, et al. Accuracy of dementia screening instruments in emergency medicine: a diagnostic meta‐analysis. Acad Emerg Med. 2019;26(2):226‐245. doi: 10.1111/acem.13573 [DOI] [PubMed] [Google Scholar]
- 36. Kennedy M, Lesser A, Israni J, et al. Reach and adoption of a geriatric emergency department accreditation program in the united states. Ann Emerg Med. 2022;79(4):367‐373. doi: 10.1016/j.annemergmed.2021.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Haynesworth A, Gilmer TP, Brennan JJ, et al. Clinical and financial outcome impacts of comprehensive geriatric assessment in a level 1 geriatric emergency department. J Am Geriatr Soc. 2023. doi: 10.1111/jgs.18468 [DOI] [PubMed] [Google Scholar]
- 38. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941‐948. [DOI] [PubMed] [Google Scholar]
- 39. Mailhot T, Darling C, Ela J, Malyuta Y, Inouye SK, Saczynski J. Family identification of delirium in the emergency department in patients with and without dementia: validity of the family confusion assessment method (FAM‐CAM). J Am Geriatr Soc. 2020;68(5):983‐990. doi: 10.1111/jgs.16438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lee S, Howard MA, Han JH. Delirium and delirium prevention in the emergency department. Clin Geriatr Med. 2023. doi: 10.1016/j.cger.2023.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gavinski K, Carnahan R, Weckmann M. Validation of the delirium observation screening scale in a hospitalized older population. J Hosp Med. 2016;11(7):494‐497. doi: 10.1002/jhm.2580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Minion SC, Obr BJ, Carnahan RM, Lee S. An educational module to improve knowledge of delirium screening in the emergency department. Am J Emerg Med. 2021;47:311‐312. doi: 10.1016/j.ajem.2021.01.031 [DOI] [PubMed] [Google Scholar]
- 43. Wang L, Laurentiev J, Yang J, et al. Development and validation of a deep learning model for earlier detection of cognitive decline from clinical notes in electronic health records. JAMA Netw Open. 2021;4(11):e2135174. doi: 10.1001/jamanetworkopen.2021.35174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gilmore‐Bykovskyi AL, Block LM, Walljasper L, Hill N, Gleason C, Shah MN. Unstructured clinical documentation reflecting cognitive and behavioral dysfunction: toward an EHR‐based phenotype for cognitive impairment. J Am Med Inform Assoc. 2018;25(9):1206‐1212. doi: 10.1093/jamia/ocy070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mueller B, Street WN, Carnahan RM, Lee S. Evaluating the performance of machine learning methods for risk estimation of delirium in patients hospitalized from the emergency department. Acta Psychiatr Scand. 2023;147(5):493‐505. doi: 10.1111/acps.13551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jordano JO, Vasilevskis EE, Duggan MC, et al. Effect of physical and occupational therapy on delirium duration in older emergency department patients who are hospitalized. J Am Coll Emerge Physicians Open. 2023;4(1):e12857. doi: 10.1002/emp2.12857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lee S, Chen H, Hibino S, et al. Can we improve delirium prevention and treatment in the emergency department? A systematic review. J Am Geriatr Soc. 2022;70(6):1838‐1849. doi: 10.1111/jgs.17740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stevens M, Hastings SN, Markland AD, et al. Enhancing quality of provider practices for older adults in the emergency department (equipped). J Am Geriatr Soc. 2017;65(7):1609‐1614. doi: 10.1111/jgs.14890 [DOI] [PubMed] [Google Scholar]
- 49. Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296(15):1858‐1866. doi: 10.1001/jama.296.15.1858 [DOI] [PubMed] [Google Scholar]
- 50. Xing XX, Zhu C, Liang HY, et al. Associations between potentially inappropriate medications and adverse health outcomes in the elderly: a systematic review and meta‐analysis. Ann Pharmacother. 2019;53(10):1005‐1019. doi: 10.1177/1060028019853069 [DOI] [PubMed] [Google Scholar]
- 51. Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug‐related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;38(6):666‐671. doi: 10.1067/mem.2001.119456 [DOI] [PubMed] [Google Scholar]
- 52. Hustey FM, Wallis N, Miller J. Inappropriate prescribing in an older ED population. Am J Emerg Med. 2007;25(7):804‐807. doi: 10.1016/j.ajem.2007.01.018 [DOI] [PubMed] [Google Scholar]
- 53. Laroche M‐L, Charmes J‐P, Nouaille Y, Picard N, Merle L. Is inappropriate medication use a major cause of adverse drug reactions in the elderly? Br J Clin Pharmacol. 2007;63(2):177‐186. doi: 10.1111/j.1365-2125.2006.02831.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Howard RL, Avery AJ, Slavenburg S, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol. 2007;63(2):136‐147. doi: 10.1111/j.1365-2125.2006.02698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Budnitz DS, Shehab N, Kegler SR, Richards CL. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. 2007;147(11):755‐765. doi: 10.7326/0003-4819-147-11-200712040-00006 [DOI] [PubMed] [Google Scholar]
- 56. By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel . American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052‐2081. doi: 10.1111/jgs.18372 [DOI] [PubMed] [Google Scholar]
- 57. American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, Society for Academic Emergency Medicine, Geriatric Emergency Department Guidelines Task Force . Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7‐e25. doi: 10.1016/j.annemergmed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 58. Briggs S, Pearce R, Dilworth S, Higgins I, Hullick C, Attia J. Clinical pharmacist review: a randomised controlled trial. Emerg Med Australas. 2015;27(5):419‐426. doi: 10.1111/1742-6723.12451 [DOI] [PubMed] [Google Scholar]
- 59. Hohl CM, Partovi N, Ghement I, et al. Impact of early in‐hospital medication review by clinical pharmacists on health services utilization. PLoS ONE. 2017;12(2):e0170495. doi: 10.1371/journal.pone.0170495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kitchen SA, McGrail K, Wickham ME, Law MR, Hohl CM. Emergency department‐based medication review on outpatient health services utilization: interrupted time series. BMC Health Serv Res. 2020;20(1):254. doi: 10.1186/s12913-020-05108-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Santolaya‐Perrín R, Calderón‐Hernanz B, Jiménez‐Díaz G, et al. The efficacy of a medication review programme conducted in an emergency department. Int J Clin Pharm. 2019;41(3):757‐766. doi: 10.1007/s11096-019-00836-0 [DOI] [PubMed] [Google Scholar]
- 62. Clementz A, Jost J, Lacour A, et al. Effect of clinical pharmacy services in an older adult emergency medicine unit on unplanned rehospitalization of older adults admitted for falls: MUPA‐PHARM Study. J Am Med Dir Assoc. 2019;20(8):947‐948. doi: 10.1016/j.jamda.2019.02.029 [DOI] [PubMed] [Google Scholar]
- 63. Matz O, Villa L, Lecce C, et al. Implementation of a telemedicine geriatric co‐evaluation in the emergency department: a prospective pilot study. Swiss Med Wkly. 2021;151:w20500. doi: 10.4414/smw.2021.20500 [DOI] [PubMed] [Google Scholar]
- 64. Liu Y‐L, Chu L‐L, Su H‐C, et al. Impact of computer‐based and pharmacist‐assisted medication review initiated in the emergency department. J Am Geriatr Soc. 2019;67(11):2298‐2304. doi: 10.1111/jgs.16078 [DOI] [PubMed] [Google Scholar]
- 65. Griffey RT, Lo HG, Burdick E, Keohane C, Bates DW. Guided medication dosing for elderly emergency patients using real‐time, computerized decision support. J Am Med Inform Assoc. 2012;19(1):86‐93. doi: 10.1136/amiajnl-2011-000124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Terrell KM, Perkins AJ, Dexter PR, Hui SL, Callahan CM, Miller DK. Computerized decision support to reduce potentially inappropriate prescribing to older emergency department patients: a randomized, controlled trial. J Am Geriatr Soc. 2009;57(8):1388‐1394. doi: 10.1111/j.1532-5415.2009.02352.x [DOI] [PubMed] [Google Scholar]
- 67. O'Mahony D. STOPP/START criteria for potentially inappropriate medications/potential prescribing omissions in older people: origin and progress. Expert Rev Clin Pharmacol. 2020;13(1):15‐22. doi: 10.1080/17512433.2020.1697676 [DOI] [PubMed] [Google Scholar]
- 68. Pevnick JM, Nguyen C, Jackevicius CA, et al. Improving admission medication reconciliation with pharmacists or pharmacy technicians in the emergency department: a randomised controlled trial. BMJ Qual Saf. 2018;27(7):512‐520. doi: 10.1136/bmjqs-2017-006761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Atey TM, Peterson GM, Salahudeen MS, Bereznicki LR, Wimmer BC. Impact of pharmacist interventions provided in the emergency department on quality use of medicines: a systematic review and meta‐analysis. Emerg Med J. 2023;40(2):120‐127. doi: 10.1136/emermed-2021-211660 [DOI] [PubMed] [Google Scholar]
- 70. Andersen TS, Gemmer MN, Sejberg HRC, et al. Medicines reconciliation in the emergency department: important prescribing discrepancies between the shared medication record and patients’ actual use of medication. Pharmaceuticals (Basel). 2022;15(2). doi: 10.3390/ph15020142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Vaughan CP, Hwang U, Vandenberg AE, et al. Early prescribing outcomes after exporting the EQUIPPED medication safety improvement programme. BMJ Open Qual. 2021;10(4). doi: 10.1136/bmjoq-2021-001369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Goldberg EM, Lin TR, Cunha CB, Mujahid N, Davoodi NM, Vaughan CP. Enhancing the quality of prescribing practices for older adults discharged from the emergency department in Rhode Island. J Am Geriatr Soc. 2022;70(10):2905‐2914. doi: 10.1111/jgs.17955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hickman LD, Phillips JL, Newton PJ, Halcomb EJ, Davidson PM. Multidisciplinary team interventions to optimise health outcomes for older people in acute care settings: a systematic review. Arch Gerontol Geriatr. 2015;61(3):322‐329. doi: 10.1016/j.archger.2015.06.021 [DOI] [PubMed] [Google Scholar]
- 74. Choi J‐Y, Rajaguru V, Shin J, Kim K‐I. Comprehensive geriatric assessment and multidisciplinary team interventions for hospitalized older adults: a scoping review. Arch Gerontol Geriatr. 2023;104:104831. doi: 10.1016/j.archger.2022.104831 [DOI] [PubMed] [Google Scholar]
- 75. Chong E, Bao M, Goh EF, Lim WS. SARC‐F at the emergency department: diagnostic performance for frailty and predictive performance for reattendances and acute hospitalizations. J Nutr Health Aging. 2021;25(9):1084‐1089. doi: 10.1007/s12603-021-1676-5 [DOI] [PubMed] [Google Scholar]
- 76. Chary A, Brickhouse E, Torres B, et al. Physical therapy consultation in the emergency department for older adults with falls: a qualitative study. J Am Coll Emerg Physicians Open. 2023;4(2):e12941. doi: 10.1002/emp2.12941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Fareed N, Southerland LT, Rao BM, Sieck CJ. Geriatric assistive devices improve older patient engagement and clinical care in an emergency department. Am J Emerg Med. 2021;46:656‐658. doi: 10.1016/j.ajem.2020.07.073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Davenport K, Cameron A, Samson M, Sri‐On J, Liu SW. Fall prevention knowledge, attitudes, and behaviors: a survey of emergency providers. West J Emerg Med. 2020;21(4):826‐830. doi: 10.5811/westjem.2020.4.43387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Haimovich AD, Shah MN, Southerland LT, Hwang U, Patterson BW. Automating risk stratification for geriatric syndromes in the emergency department. J Am Geriatr Soc. 2023. doi: 10.1111/jgs.18594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Paniagua MA, Malphurs JE, Phelan EA. Older patients presenting to a county hospital ED after a fall: missed opportunities for prevention. Am J Emerg Med. 2006;24(4):413‐417. doi: 10.1016/j.ajem.2005.12.005 [DOI] [PubMed] [Google Scholar]
- 81. Carpenter CR, Scheatzle MD, D'Antonio JA, Ricci PT, Coben JH. Identification of fall risk factors in older adult emergency department patients. Acad Emerg Med. 2009;16(3):211‐219. doi: 10.1111/j.1553-2712.2009.00351.x [DOI] [PubMed] [Google Scholar]
- 82. Whitehead C, Wundke R, Crotty M, Finucane P. Evidence‐based clinical practice in falls prevention: a randomised controlled trial of a falls prevention service. Aust Health Rev. 2003;26(3):88‐97. doi: 10.1071/ah030088 [DOI] [PubMed] [Google Scholar]
- 83. Tirrell G, Sri‐on J, Lipsitz LA, Camargo CA, Kabrhel C, Liu SW. Evaluation of older adult patients with falls in the emergency department: discordance with national guidelines. Acad Emerg Med. 2015;22(4):461‐467. doi: 10.1111/acem.12634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Lesser A, Israni J, Kent T, Ko KJ. Association between physical therapy in the emergency department and emergency department revisits for older adult fallers: a nationally representative analysis. J Am Geriatr Soc. 2018;66(11):2205‐2212. doi: 10.1111/jgs.15469 [DOI] [PubMed] [Google Scholar]
- 85. Goldberg EM, Marks SJ, Resnik LJ, Long S, Mellott H, Merchant RC. Can an emergency department‐initiated intervention prevent subsequent falls and health care use in older adults? Ann Emerg Med. 2020;76(6):739‐750. doi: 10.1016/j.annemergmed.2020.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending accident & emergency benefit from multifactorial intervention–a randomised controlled trial. Age Ageing. 2005;34(2):162‐168. doi: 10.1093/ageing/afi053 [DOI] [PubMed] [Google Scholar]
- 87. Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93‐97. doi: 10.1016/S0140-6736(98)06119-4 [DOI] [PubMed] [Google Scholar]
- 88. Shankar KN, Treadway NJ, Taylor AA, Breaud AH, Peterson EW, Howland J. Older adult falls prevention behaviors 60 days post‐discharge from an urban emergency department after treatment for a fall. Inj Epidemiol. 2017;4(1):18. doi: 10.1186/s40621-017-0114-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. van Wijck SFM, Rizzo C, Raybould T. Unexpected challenges to preventing falls in older adults: a mixed methods study of an emergency department‐based falls prevention referral pilot project. Health Edu Care. 2019;4(2). doi: 10.15761/HEC.1000158 [DOI] [Google Scholar]
- 90. Stark S, Keglovits M, Somerville E, et al. Home hazard removal to reduce falls among community‐dwelling older adults: a randomized clinical trial. JAMA Netw Open. 2021;4(8):e2122044. doi: 10.1001/jamanetworkopen.2021.22044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Xie F, Yan J, Agarwal G, Ferron R. Economic analysis of mobile integrated health care delivered by emergency medical services paramedic teams. JAMA Netw Open. 2021;4(2):e210055. doi: 10.1001/jamanetworkopen.2021.0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Southerland LT, Pearson S, Hullick C, Carpenter CR, Arendts G. Safe to send home? Discharge risk assessment in the emergency department. Emerg Med Australas. 2019;31(2):266‐270. doi: 10.1111/1742-6723.13250 [DOI] [PubMed] [Google Scholar]
- 93. Schumacher JR, Lutz BJ, Hall AG, et al. Impact of an emergency department‐to‐home transitional care intervention on health service use in medicare beneficiaries: a mixed methods study. Med Care. 2021;59(1):29‐37. doi: 10.1097/MLR.0000000000001452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department‐based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int. 2015;15(9):1107‐1117. doi: 10.1111/ggi.12538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Gettel CJ, Falvey JR, Gifford A, et al. Emergency department care transitions for patients with cognitive impairment: a scoping review. J Am Med Dir Assoc. 2022;23(8):1313.e1‐1313.e13. doi: 10.1016/j.jamda.2022.01.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Liu SW, Obermeyer Z, Chang Y, Shankar KN. Frequency of ED revisits and death among older adults after a fall. Am J Emerg Med. 2015;33(8):1012‐1018. doi: 10.1016/j.ajem.2015.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Cassarino M, Robinson K, Trépel D, et al. Impact of assessment and intervention by a health and social care professional team in the emergency department on the quality, safety, and clinical effectiveness of care for older adults: a randomised controlled trial. PLoS Med. 2021;18(7):e1003711. doi: 10.1371/journal.pmed.1003711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Yon Y, Mikton CR, Gassoumis ZD, Wilber KH. Elder abuse prevalence in community settings: a systematic review and meta‐analysis. Lancet Glob Health. 2017;5(2):e147‐e156. doi: 10.1016/S2214-109X(17)30006-2 [DOI] [PubMed] [Google Scholar]
- 99. Evans CS, Hunold KM, Rosen T, Platts‐Mills TF. Diagnosis of elder abuse in U.S. emergency departments. J Am Geriatr Soc. 2017;65(1):91‐97. doi: 10.1111/jgs.14480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Dong X, Simon M, Mendes de Leon C, et al. Elder self‐neglect and abuse and mortality risk in a community‐dwelling population. JAMA. 2009;302(5):517‐526. doi: 10.1001/jama.2009.1109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Jeong K, Jang D, Nam B, Kwon S, Seo E. The moderating effect of gender on the relationship between self‐neglect and suicidal ideation in older adults of Korea. J Prev Med Public Health. 2022;55(5):436‐443. doi: 10.3961/jpmph.22.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Dong X, Xu Y, Ding D. Elder self‐neglect and suicidal ideation in an u.s. chinese aging population: findings from the PINE study. J Gerontol A Biol Sci Med Sci. 2017;72(1):S76‐S81. doi: 10.1093/gerona/glw229. suppl_. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Epstein‐Lubow G, Gaudiano BA, Hinckley M, Salloway S, Miller IW. Evidence for the validity of the American Medical Association's caregiver self‐assessment questionnaire as a screening measure for depression. J Am Geriatr Soc. 2010;58(2):387‐388. doi: 10.1111/j.1532-5415.2009.02701.x [DOI] [PubMed] [Google Scholar]
- 104. Zaalberg T, Barten DG, van Heugten CM, et al. Prevalence and risk factors of burden among caregivers of older emergency department patients. Sci Rep. 2023;13(1):7250. doi: 10.1038/s41598-023-31750-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Rosen T, Mehta‐Naik N, Elman A, et al. Improving quality of care in hospitals for victims of elder mistreatment: development of the vulnerable elder protection team. Jt Comm J Qual Patient Saf. 2018;44(3):164‐171. doi: 10.1016/j.jcjq.2017.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Cannell B, Livingston M, Burnett J, Parayil M, Reingle Gonzalez JM. Evaluation of the detection of elder mistreatment through emergency care technicians project screening tool. JAMA Netw Open. 2020;3(5):e204099. doi: 10.1001/jamanetworkopen.2020.4099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Reed M, Huang J, Brand R, et al. Inpatient‐outpatient shared electronic health records: telemedicine and laboratory follow‐up after hospital discharge. Am J Manag Care. 2020;26(10):e327‐e332. doi: 10.37765/ajmc.2020.88506 [DOI] [PubMed] [Google Scholar]
- 108. Sheber M, McKnight M, Liebzeit D, et al. 335 “4ms” conversation in the emergency department: a qualitative study. Ann Emerg Med. 2022;80(4):S143. doi: 10.1016/j.annemergmed.2022.08.362 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


