Background
Straight-back syndrome is a rare congenital condition involving the loss of the normal dorsal curvature of the upper thoracic spine. This leads to flattening of the upper thoracic cavity, resulting in compression of the underlying vasculature and airways. In this case report, we discuss the management of an 18-year-old male with straight-back syndrome who was referred to our interventional pulmonary clinic for further management of his stridor and apneic events. A trial of airway stenting was done which resolved the patient's respiratory symptoms. Definitive surgical correction was not applicable due to other significant medical conditions, but tracheostomy provided a sustainable alternative treatment. Tracheostomy tube placement and airway stenting are reasonable alternatives to surgery for patients who experience airway obstruction due to straight-back syndrome. Stent placement may also relieve respiratory symptoms but is associated with a higher rate of complications.
Keywords: Straight-back syndrome, Tracheostomy, Airway stenting, Congenital condition
1. Introduction
Straight-back syndrome is a rare congenital condition characterized by a loss of the dorsal curvature of the thoracic spine, leading to a reduction of the anteroposterior diameter of the thorax. The diagnostic criteria require that the horizontal distance from the middle of the anterior border of T8 to a vertical line connecting T4 to T12 is less than 1.2 cm [1] and that the ratio of the anteroposterior to the transverse diameter is less than or equal to 1:3 [2]. Consequently, the heart and great vessels are compressed between the sternum and spine. This commonly presents with hypertension, cardiac murmurs (from mitral valve prolapse, mitral valve regurgitation, and/or pulmonic stenosis) [3,4], palpitations, or a “pancake-shaped” heart mimicking cardiomegaly [5]. Less frequently, it may result in tracheomalacia of the airways from several mechanisms-- external compression of the brachiocephalic artery as it crosses the trachea, compression between the sternum and vertebral body, or splaying of the lower trachea against the vertebral bodies. These anomalies exhibit a wide range of symptom severity. Some patients may experience significant dyspnea whereas others may be asymptomatic or have only mild symptoms such as back and chest pain [5]. As it is a rare condition with varying anatomic distinctions, there is no consensus on optimal management. One case report managed this conservatively with chiropractic therapy to increase the curvature of the upper thoracic spine [5]. Other successful case reports have been published of surgical techniques involving re-implantation of the offending brachiocephalic artery lower down on the aorta to relieve the compression, insertion of a reinforcing mesh, or resecting the sternum or manubrium to increase the anteroposterior space [6]. In this case report, we explore a more conservative approach to the treatment including a trial of airway stenting followed by long-term tracheostomy.
2. Case presentation
An eighteen-year-old male with a past medical history of cerebral palsy with spasticity, sleep apnea, gastroesophageal reflux disease (GERD) s/p Nissen fundoplication and G-tube placement, and recurrent aspiration pneumonia was referred to our interventional pulmonary clinic for further management of stridor and apneic episodes. At baseline, he is non-verbal and wheelchair-bound, and his family reported having to place him under constant observation to reposition his head during his stridor and apneic episodes. His initial imaging was consistent with “straight-back syndrome” with loss of dorsal kyphosis causing anteroposterior diameter narrowing to 2.3 cm between the top of the manubrium and the opposing thoracic vertebrae (normal range is 5.0–8.7 cm) (Fig. 1).
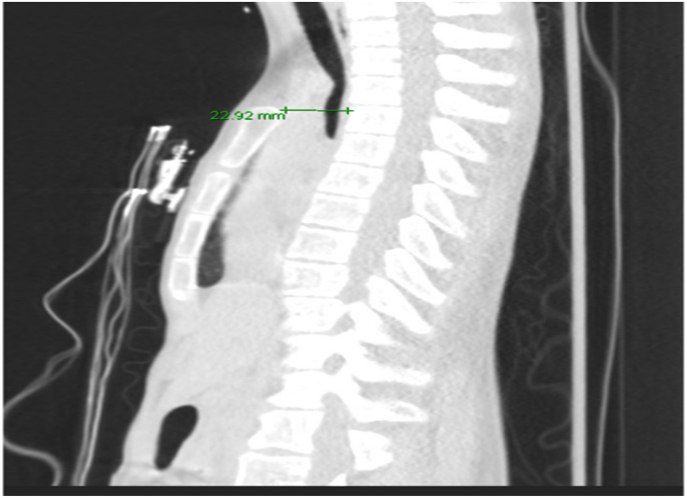
Fig. 1.
Chest CT sagittal view showing loss of dorsal kyphosis causing anteroposterior diameter narrowing to 2.3 cm between the top of the manubrium and the opposing thoracic vertebrae (normal range is 5.0–8.7 cm).
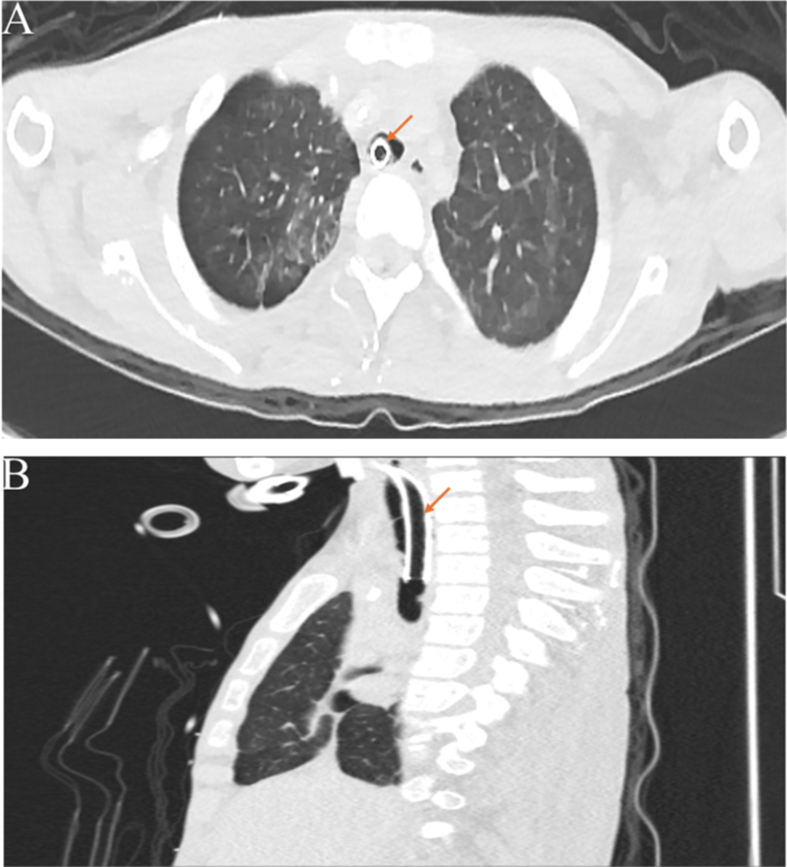
He had resultant crowding of his heart, great vessels, and most notably his airway. His tracheal diameter was significantly narrowed to 0.3 cm, likely because of extrinsic compression of the brachiocephalic artery crossing the midline (Fig. 2A). The CT scan also revealed critical narrowing of the left main stem airway (Fig. 2B).
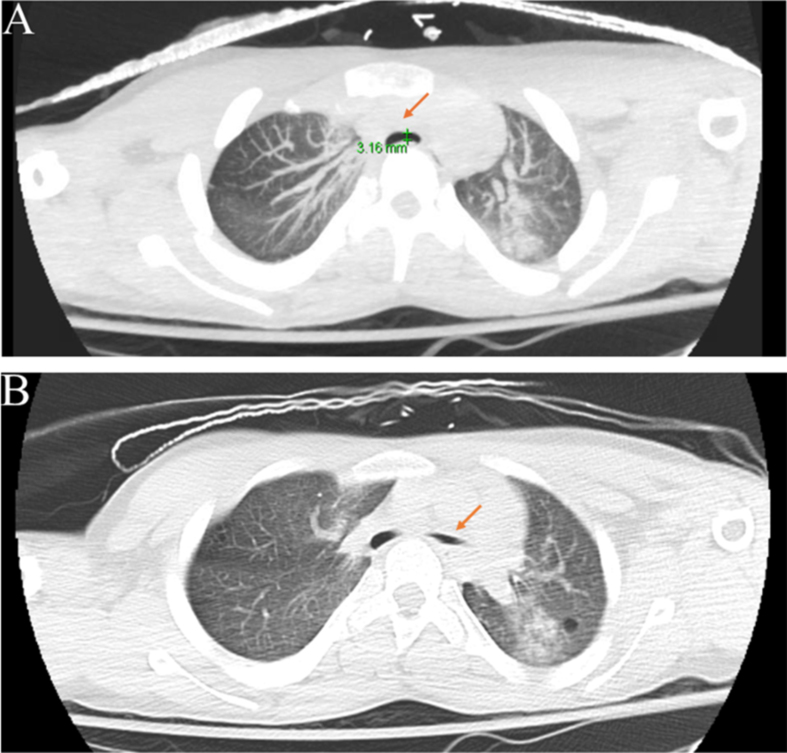
Fig. 2.
Chest CT transverse view showing crowding of his heart, great vessels, and most notably his airway. (A) His tracheal diameter was significantly narrowed to 0.3 cm. (B) The arrow points to a critical narrowing of the lumen of the left main stem airway.
A decision was made for a trial of airway stenting to evaluate for symptomatic improvement before proceeding to more definitive management. Airway stenting was not a long-term solution due to possible expected complications such as recurrent infections, granulation tissue formation, stent migration, and impaired mucus clearance. This was discussed with the patient's parents who agreed with the plan. He was subsequently admitted to the hospital for an elective bronchoscopy and stent placement. During the bronchoscopy severe narrowing of the mid tracheal lumen and proximal part of the left main stem was confirmed. Pulsations were also observed in the tracheal stenosis area likely from the brachiocephalic artery (Fig. 3).
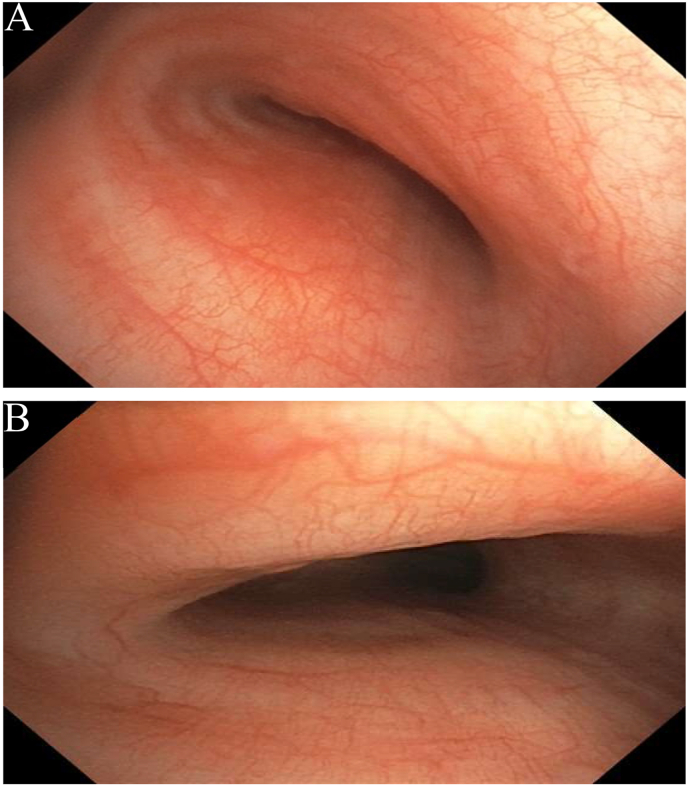
Fig. 3.
Bronchoscopic view of the mid tracheal lumen (A) and proximal part of the left main stem airway (B) showing severe airway lumen narrowing.
A 10 × 30 mm covered hybrid stent was placed in the left main stem bronchus and a 14 × 40 mm covered hybrid stent was placed in the trachea which effectively improved the patency of the airways (Fig. 4A&4B).
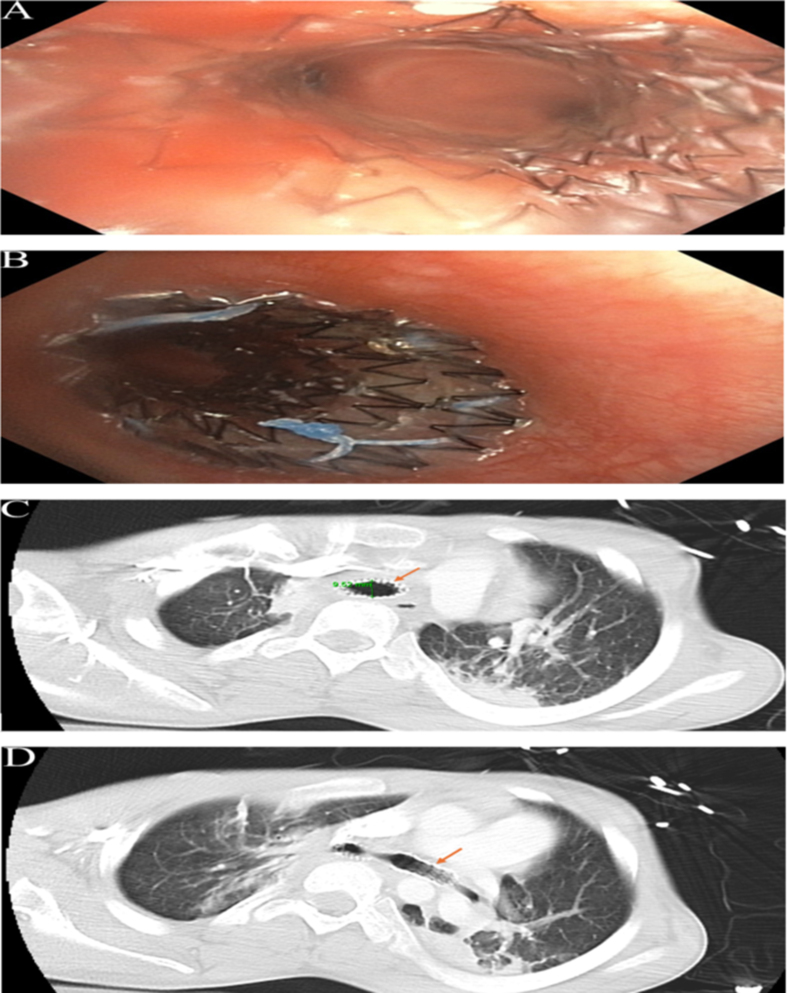
Fig. 4.
(A) Bronchoscopic view of the upper trachea showing a 14 × 40 mm covered hybrid stent placement. (B) Bronchoscopic view of the left main stem showing a 10 × 30 mm hybrid stent placement. CT scan of the chest showing improved airway lumen after airway stent placement in trachea (C) and left main stem (D).
On follow-up one week after bronchoscopy and airway stent placement, the patient's family reported complete resolution of respiratory symptoms. The plan was to remove the airway stents and arrange for a long-term solution. Unfortunately, two weeks later and immediately before the scheduled removal of the stents, the patient presented to the emergency room in respiratory distress secondary to left-sided pneumonia. He was subsequently intubated with bronchoscopic guidance and admitted to the pediatric intensive care unit. CT scan of the chest showed patent tracheal and left main stem airway stents with continued airway lumen improvement as shown in (Fig. 4C&D).
Rigid bronchoscopy was performed and the stents were removed. He was treated with a course of antibiotics for pneumonia. After extensive discussion in a multidisciplinary group of providers, surgical correction of the anatomic problems was deemed to be too risky due to his co-morbidities. Tracheostomy was felt to be the best treatment option with the least expected long-term complications. He underwent a tracheostomy on hospital admission day six. Post-tracheostomy bronchoscopy showed a successful bypass of the stenotic area by the tracheostomy tube. Four weeks later, he developed tracheal wall granulation tissue against the tip of the tracheostomy tube resulting in elevated peak pressures on the ventilator and significant respiratory distress. His tracheostomy tube was replaced with a custom 6.0 cuffed flextend Bivona (extra-long to bypass the most severe area of tracheomalacia). The new tube resolved his symptoms and he had no further significant respiratory problems for the remainder of his hospital course. However, he was not discharged until five months later due to other complications which were not directly related to the airway problems. Those included pneumoperitoneum requiring exploratory laparotomy, recurrent bowel obstructions, cardiac arrest secondary to sepsis of unknown source, renal failure requiring dialysis, and right ventricular thrombus. He was discharged home with outpatient follow-up and nocturnal ventilator support. He remained stable and was last seen in pulmonary and ENT office about eighteen months post hospital discharge. Repeat CT scan of chest in a few months showed stable central airway with patent lumen and the tracheostomy tube in good position (Fig. 5 A&B).
Fig. 5.
CT scan of the chest with representative axial (A) and sagittal (B) plane views showing the tracheostomy tube in an optimal position with patent central airways.
Discussion Due to its rarity, there are currently only case reports in the literature of straight-back syndrome causing airway compromise. The treatment of choice is usually surgical reconstruction [7]. However, our patient was very frail with significant medical comorbidities, so we opted for a less invasive intervention. Furthermore, we felt that a tracheostomy would not significantly affect his quality of life as he was nonverbal, wheelchair-bound, and required twenty-four-hour care at baseline. Fortunately, the outcome was satisfactory as observed in a follow-up exam several months post-discharge from the hospital. The patient's family also reported a resolution of his prior stridor and apneic events with the tracheostomy collar.
Another non-surgical intervention that could have been considered in this patient was long-term stenting. However, due to known long-term complications, they are not a favorable option. Metal stents (including bare and covered stents) are associated with complications such as the formation of granulation tissue, stent lumen occlusion, and difficulty of removal. Silicone stents are a better-tolerated option as they are easier to remove and replace but they also come with significant complications and require rigid bronchoscopy for placement and removal. For example, a study found that 10 out of 12 patients who had silicone-stents placed had twenty-six stent-related complications (twelve mucus plugs, eight migrations, and six granulation tissues) despite significantly improved functional status post-procedure [8]. The stent we initially placed in our patient was a fully covered tracheobronchial AERO stent (made with nitinol with polyurethane coating). This stent is a hybrid metallic stent with easy placement via flexible bronchoscopy and easier removal when compared to bare metal stents. However, as noted in our case presentation, our patient developed a stent-related complication only two weeks after placement and required intubation for left-sided pneumonia. In anticipation of higher complication rates, we did not plan for this route, as long-term stenting would likely subject our patient to repeated procedures and increase his discomfort and suffering.
After weighing the risks and benefits of stenting versus tracheostomy, tracheostomy was deemed to be the best option as agreed upon by all involved specialties. Nevertheless, tracheostomies are also not without complications. One case describing a patient with severe scoliosis causing airway obstruction requiring tracheostomy reported that the patient unexpectedly expired two weeks later due to massive bleeding from the tracheostomy site, probably due to a tracheo-brachiocephalic artery fistula [9]. This risk may be higher in patients with chest wall deformities [10]. Formation of granulation tissue is another concern that occurred in our patient and was treated with replacement with a custom-made tracheostomy tube to prevent further irritation of the tracheal wall. Given these known complications, effort should be made for routine surveillance with laryngoscopy and bronchoscopy [11].
3. Conclusions
Tracheostomy tube placement is a reasonable alternative to surgery for patients who are not a candidate for surgical correction of straight-back syndrome. Airway stent placement can successfully relieve respiratory symptoms in this condition but is associated with a higher rate of complications. Patients with chronic tracheostomies require regular monitoring, especially among those with thoracic deformities which have higher complication rates.
Ethics approval statement and patient consent statement
We obtained informed consent from the patient's father who is the patient's legal guardian.
Funding source
This study did not receive any financial support.
CRediT authorship contribution statement
Aham Okorozo: Writing – review & editing, Writing – original draft, Visualization, Data curation, Conceptualization. Vicky Chiang: Writing – review & editing, Writing – original draft, Visualization, Methodology, Data curation, Conceptualization. Hyun S. Kim: Writing – review & editing, Supervision, Conceptualization. Marc Vimolratana: Writing – review & editing, Supervision, Conceptualization. Ali Sadoughi: Writing – review & editing, Visualization, Supervision, Project administration, Methodology, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling Editor: DR AC Amit Chopra
Contributor Information
Aham Okorozo, Email: aok.research@gmail.com.
Vicky Chiang, Email: vickyyschiang@gmail.com.
Hyun S. Kim, Email: hkim.doc@gmail.com.
Marc Vimolratana, Email: mvimolrata@montefiore.org.
Ali Sadoughi, Email: sadoughia@gmail.com.
References
- 1.Davies M.K., Mackintosh P., Cayton R.M., Page A.J., Shiu M.F., Littler W.A. The straight back syndrome. Q. J. Med. 1980;49(196):443–460. [PubMed] [Google Scholar]
- 2.Deleon AC Jr, Perloff J.K., Twigg H., Majd M. The straight back syndrome: clinical cardiovascular manifestations. Circulation. 1965;32:193–203. doi: 10.1161/01.cir.32.2.193. [DOI] [PubMed] [Google Scholar]
- 3.Schiavone W. Straight back syndrome as a clue to diagnosing asymptomatic congenital valvular heart disease and limiting the risk of weightlifting. J. Osteopath. Med. 2020;121(2):135–140. doi: 10.1515/jom-2020-0046. [DOI] [PubMed] [Google Scholar]
- 4.Perez-Downes J., Leon A., Reddy P. Straight back syndrome. J. Osteopath. Med. 2020;120(7):485. doi: 10.7556/jaoa.2020.078. [DOI] [PubMed] [Google Scholar]
- 5.Shiba H., Kenzaka T. Straight back syndrome presented with chest and back pain: a case report. Int. Med. Case Rep. J. 2002;15:611–614. doi: 10.2147/IMCRJ.S385312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grillo H.C., Wright C.D., Dartevelle P.G., Wain J.C., Murakami S. Tracheal compression caused by straight back syndrome, chest wall deformity, and anterior spinal displacement: techniques for relief. Ann. Thorac. Surg. 2005;80(6):2057–2062. doi: 10.1016/j.athoracsur.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 7.Donnelly L.F., Bisset G.S., 3rd Airway compression in children with abnormal thoracic configuration. Radiology. 1998;206(2):323–326. doi: 10.1148/radiology.206.2.9457181. [DOI] [PubMed] [Google Scholar]
- 8.Murgu S.D., Colt H.G. Complications of silicone stent insertion in patients with expiratory central airway collapse. Ann. Thorac. Surg. 2007;84(6):1870–1877. doi: 10.1016/j.athoracsur.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Beck K.S., Lee B.Y., Kim H.S., et al. Extrinsic tracheal compression caused by scoliosis of the thoracic spine and chest wall deformity: a case report. Journal of the Korean Society of Radiology. 2014;70(5):343–346. doi: 10.3348/jksr.2014.70.5.343. [DOI] [Google Scholar]
- 10.Ogawa K., Nitta N., Sonoda A., et al. Tracheo-brachiocephalic artery fistula after tracheostomy associated with thoracic deformity: a case report. J. Med. Case Rep. 2011;5:595. doi: 10.1186/1752-1947-5-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Appachi S., Marcet-Gonzalez J., Brown J.N., Ongkasuwan J., Lambert E.M. An analysis of tracheostomy complications in pediatric patients with scoliosis. Laryngoscope. 2021;132(5):944–948. doi: 10.1002/lary.29747. [DOI] [PubMed] [Google Scholar]