Abstract
Objectives:To assess the immediate and six-month follow-up effects of medical education simultaneously provided by a practitioner and a science teacher on middle school students regarding self-medication and knowledge of the healthcare system.
Methods:Two groups were constituted: the learning group (L group), with students receiving an interactive medical education, and the control group (C group), which included students without medical education. Both groups were evaluated by using a six-multiple choice question (MCQ) evaluation form: three times for L group – just before the medical workshop (T0), immediately after the medical workshop (T1) and at six-month follow-up after the medical workshop (T2) – and only the evaluation at T0 for students in C group.
Results:In L group (n=219), medical education improved all results of the evaluations related to self-medication skills (p<0.001) and knowledge of the healthcare medical system (p<0.001). Students retained their knowledge over time as no significant gap has been identified between T1 and T2 evaluations. Age, gender, grade and students’ level did not have any impact on the results of L group. Students in L group had equivalent results to those in the C group (n=195) at T0 but the results increased at T1 (p<0.001) and T2 (p<0.001).
Conclusion:Interactive medical education in middle school co-animated by a medical practitioner and a natural science teacher improves long-term teenagers’ awareness of the current public health challenges.
Keywords:self-medication, drug overuse, analgesic, health school prevention, medical education, care pathways.
INTRODUCTION
Excessive reliance on in-office or emergency room consultations remains a real public health challenge with significant impact on healthcare system cost, drug overuse and care system saturation (1, 2). The overuse of the healthcare system is particularly prevalent in high income countries. In 2019, before the COVID-19 pandemic, France healthcare spending was 4,508 $ per capita and 11.1% of the gross domestic product (GDP). The healthcare system cost is constantly raising (3). Improving basic medical knowledge and better supervision of self-medication could reduce overuse of the healthcare system.
The practice of self-medication is wordily used but requires an extensive knowledge of medication and can lead to iatrogenic consequences (4). When it comes to self-medication for pain management, analgesics are the most commonly self-prescribed drugs without any physician advice globally (5). Easily accessible analgesic drugs are directly related to the important number of over-the-counter (OTC) analgesics such as non-steroidal anti-inflammatory drugs and paracetamol. These two analgesics have potential adverse drug reactions when misused and overdosed. Nevertheless, self-medication does not have only negative effects. Relevant self-medication could also have a positive effect by reducing overuse of medical service and involving the patient in his/her own healthcare as we can see it with asthmatic patients (4). Although the family environment plays a crucial role in shaping children's attitudes and behaviors, including their approach to self-medication, teaching self-medication practice, especially at school, could improve its use. In fact, young students are most likely to be receptive and could spread the adapted use of self-medication in their families (6, 7).
The present comparative prospective cohort study aimed to seek and evaluate the impact of medical learning on self-medication and healthcare system knowledge in middle school.
METHODS
Population setting
Two equivalent groups were prospectively constituted and each of them was composed of seventh to ninth grade students attending the same middle school. The first one, named “control group” (C group), comprised students who did not receive any medical education. The second one, named “learning group” (L group), included students who have received a medical education. The present study was accepted by the middle school management team.
Study design
All results have been anonymized. The medical education that has been provided to L group was done by a senior resident in general internal medicine along with a science middle school teacher. A practitioner in general internal medicine has been chosen because it is the specialty most confronted with the problem of self-medication misuse and the most included in the familial field and the closest to familial intimacy. The workshop duration was 40 minutes divided in both equivalent interactive sessions. Each session was attended by 10 to 15 students. The first session focused on self-medication with OTC analgesics. Recommendations regarding the duration of paracetamol use and its posology according to patient’s symptoms, disease and morphology were playfully exposed as clinical cases. Competition between groups has been used to engage the teenagers proactively. The teachers emphasized the temporary aspect of self-medication. During the clinical cases, fake patients suffering from different diseases were presented and some OTC drugs (tabs with notices and medicine boxes) with different posologies and treatment durations were proposed. The importance of temperature measurement has been highlighted. The second session focused on challenges related to the healthcare pathways used in France, with an explanation of the different circuits. Clinical cases were played and the care pathways were debated between students (Figures 1 and 2).
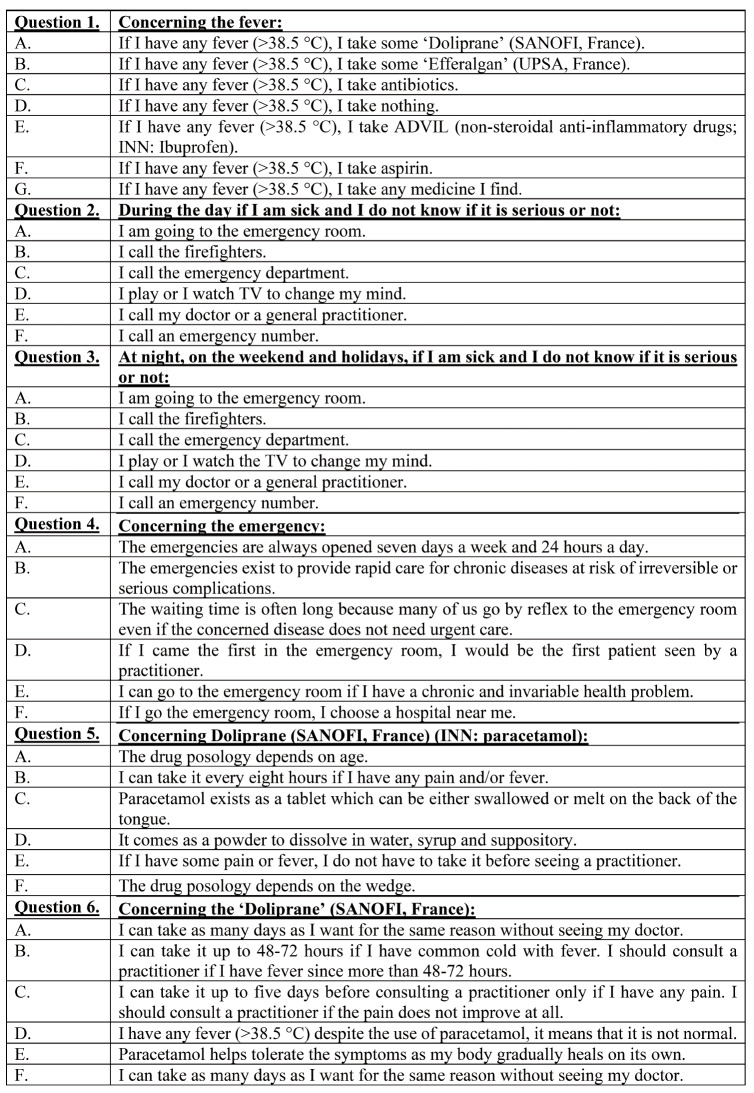
Three assessments of students’ knowledge on self-medication and care pathways before medical learning (T0), immediately after medical learning (short-term knowledge) (T1) and during the six-month follow-up (long-term knowledge) (T1) have been done. At each time, the same assessment based on six multiple choice questions (MCQ) (Table 1) has been used and anonymously corrected. Students included in L group have completed the assessment three times (T0, T1 and T2), while those in C group were only assessed one time (T0) to avoid the risk of contamination between groups. The results of C group students were compared with those of the three assessments for L group (T0, T1 and T2). The correction scale was as follows: each MCQ was weighted according to the number of items (Question 6: five points / Question 1: seven points / Questions 2, 3, 4 and 5: six points). Each question with the correct reply (which could be either true or false) was weighted as 1. For wrong replies, the weight was set to 0. If a student did not give any responses to a question, the assigned weight was 0. Students never had any correction of the evaluation. School level of each middle school student was a priori given by the referent teacher of each class. The school level was graded as follows: level A for very good students, level B for good students, level C for average students and level M for low education students.
Statistical analyses
Categorical data were expressed as percentage and were compared using Fisher test; continuous data were expressed as mean and 95% confidence interval (CI) and were compared using Student test. The normality of continuous variables has been previously assessed using Shapiro-Wilk test. To analyze the effect of medical education on students’ knowledge, three ways (age, sex, school level and school grade) repeated measures ANOVA have been performed. A priori post-hoc Bonferroni test has only been achieved if any difference using ANOVA test was present. All variables statistically significant were set at p-value <0.05. Data were anonymously recorded in Excel 2008 (Microsoft, Richmond, WA, USA). Statistical analysis was performed with SPSS Advanced Statistics 20.0 software (IBM, Armonk, NY, USA).
RESULTS
Groups' characteristics (Table 2)
A total of 414 school students divided into 20 different classes were included: 195 in C group and 219 in L group. Subjects’ mean age was 12.1 years (95% CI [12-12.3]) in C group and 11.9 years (95% CI [11.8-12]) in L group, with a statistical difference between groups being found (p=0.02). Regarding school grade distribution, there was no difference between groups (p=0.3). In L group, the school level was assessed by the referent teachers. Two school students were considered as level M (low level students) (0.9%), 57 (26%) as level C, 92 (42%) as level B and 68 (31.1%) as level A.
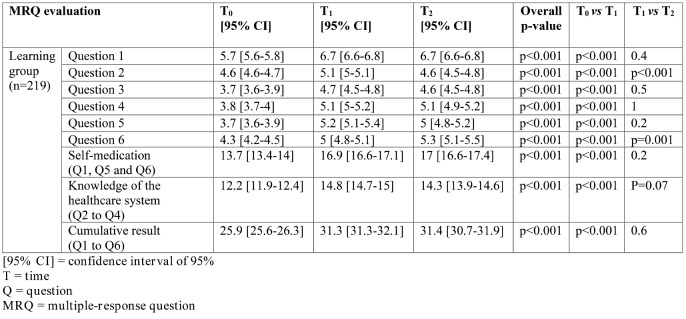
Effect of the medical education (Tables 3 and 4)
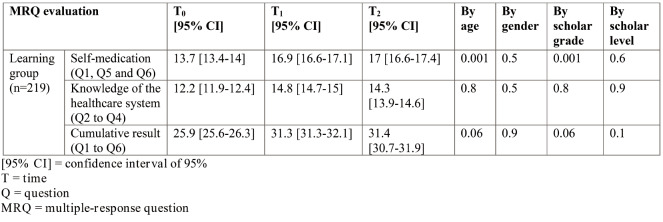
Among students included in L group, the medical education has statistically improved all results (overall p<0.001 for each question). Medical education allowed improving the self-medication skills (p<0.001) and knowledge of the healthcare system (p <0.001). Students have retained their knowledge over time as we did not identify any major differences between T1 (immediately after medical learning) and T2 (six-month follow-up) results. In fact, there was no significant difference on evaluations of either self-medication or knowledge of the healthcare system, or all results combined. Differences between T1 and T2 have only been identified for questions 2 and 6. In question 2, despite a significant increase of the result at T1 (5.1 95% CI [5-5.1]); p <0.001), the results have subsequently decreased at T2 (4.6 95% CI [4.5-4.8]; p <0.001) close to the initial result just before the medical learning T0 (4.6 95% CI [4.6-4.7]). In question 6, the school students constantly improved over time (4.3 CI 95% [4.2-4.5] at T0, thus 5 95% CI [4.8-5.1] at T1 (p <0.001) and 5.3 95% CI [5.1-5.5] at T2 (p=0.001)). Age, gender, scholar grade and scholar level did not have any influence on the results of L group regarding the cumulative results and knowledge of the healthcare system. Age (p=0.001) and scholar grade (p=0.001) statistically had a positive influence on self-medication skills. The results seemed to be better for older school students and those attending more advanced classes.
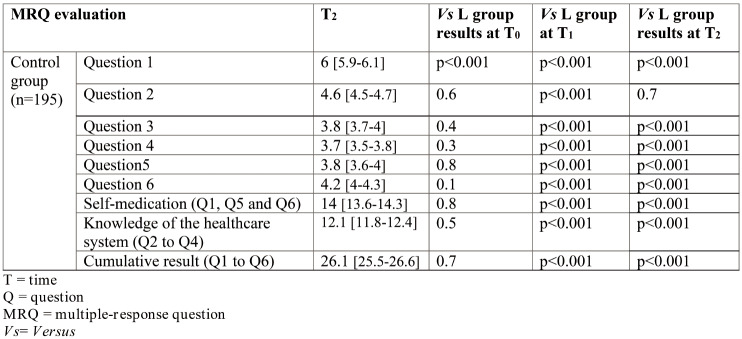
Comparison between the C group and the L group (Table 5)
School students included in C group (control group) had equivalent results to those in L group at T0, except for question 1 (p <0.001). After medical education at T1, students in L group had significantly better results than C group. Results of school students in L group at T2 differed from those of C group’s subjects, except for question 2.
DISCUSSION
As demonstrated by Tesfamariam et al (8), self-medication misuse is directly related to the lack of knowledge and a weak educational level. Likewise, Kelly et al (6) emphasized that baseline knowledge of OTC medications was low especially for middle school students. Moreover, some studies have argued the feasibility and positive interest of medical education achieved by a healthcare professional in middle school especially for improving chronic diseases such as asthma (9). In consequence, it was relevant to consider a medical education related to self-medication and healthcare system with a specific focus on middle school students. The present study has highlighted the positive impact of an interactive and short medical education, which helped middle school students improve self-medication use and knowledge of the healthcare system. Furthermore, the current study has shown that students’ knowledge related to medical education was sustainable over time. Possibly, additional appropriate education of self-medication for middle school students could have a real positive effect against further alcohol or tobacco addictions (10).
It is of paramount importance to underscore that teaching self-medication practices to young students not only fosters their understanding of basic healthcare principles but also directly impacts clinical practice by promoting responsible medication use and informed decision-making. By incorporating discussions, especially during scholarship, about potential medication interactions, adverse effects and the importance of medication adherence, students can develop critical thinking skills that are directly applicable to real-life clinical scenarios such as managing chronic illnesses or navigating complex treatment regimens Moreover, empowering students with the knowledge of recognizing common symptoms in long-lasting illness such as asthma, and understanding when self-medication is appropriate versus when professional medical attention is required can lead to earlier interventions for serious health conditions, ultimately improving patient outcomes and also reducing healthcare costs (9).
Furthermore, one approach to address concerns about children accessing emergency room (ER) services alone, regardless of age, is to emphasize the preventive role of self-education in schools. It is of note and clearly understood that children should ideally be accompanied by a responsible adult when seeking emergency medical care. Nevertheless, by equipping students with knowledge about self-medication practices, including understanding when to seek professional medical help, the likelihood of unnecessary visits to the ER may be reduced. For example, educating students about the appropriate use of OTC medications and common home remedies for minor ailments can empower them to manage simple health issues at home, thus decreasing the need for urgent medical care as parents may feel more confident in their children's ability to manage certain situations at home and assess situations more calmly and make informed decisions about whether a trip to the ER is necessary. Additionally, teaching students to recognize the signs and symptoms of serious health conditions and encouraging them to seek help from a trusted adult or healthcare professional, when necessary, can further reduce the risk of inappropriate ER visits.
It is worth to note that the family ambiance can influence self-medication practices in schools. Children often mimic the behaviors they observe at home. If family members practice responsible self-medication and prioritize seeking professional medical advice, when necessary, children are more likely to adopt similar attitudes and behaviors. In addition, the accessibility of medications at home can influence a child's likelihood of self-medicating. If parents store medications securely and emphasize the importance of using them only as directed, children are less likely to misuse or overuse them. Finally, open communication within the family about healthrelated topics fosters an environment where children feel comfortable discussing their symptoms and seeking or not advice. Families who encourage dialogue about health issues can help children make informed decisions about self-medication.
To the best to our knowledge, only few studies have prospectively assessed the interest of medical education for middle school students. The majority of them focused on medical education for a specific chronic disease and targeted school children suffering from that disease (9, 11). The six-MCQ (Table 1) have been created for this study. The evaluation form used by us was built in partnership with a middle school science teacher, a medical practitioner and a medical resident. An assessment only containing MCQ has been chosen as it was considered a relevant and reliable methodology of evaluation. It is admitted that MCQ is reproducible in time and prevents against inter-individual variations of the correction (12). Moreover, MCQ evaluation is a discriminant method of evaluation. We decided to employ MCQ with short questions as it was easier for teenagers to use. In our opinion, more sophistical MCQs as single best answer questions, clinical scenario or a progressive clinical case seems to be too tricky and challenging for middle school students. Single best answer questions and progressive clinical case-based MCQ are more adapted for undergraduate students (13).
Nevertheless, the present study has limits. In fact, we only performed a cross-sectional evaluation of the control group at T0. It might have been preferable to evaluate the control group at the same times as L group (T0, and T2). We decided to not assess the control group at T2 because we were concerned about the potential communication between school students of C and L groups, which might have led to an outcome bias. The potential risk of “contamination” between groups was incredibly increased because more than half of the middle school teenagers (n=800) were included in our study, which widely argued the risk of contamination between groups. Furthermore, organizing medical education is time-consuming for both the practitioner and middle school teacher. It requires a heavy involvement of healthcare professionals, who must feel comfortable with a younger audience. The family environment has not been considering in the present assessment. In fact, the family environment certainly influences the use of self-medication and knowledge of the healthcare system, which could be identified as a limit of this study. However, given the important population size in each group, family environment should not probably be considered as a confusion bias and therefore, its effect is evenly distributed.
CONCLUSION
Medical education in middle school involving both a healthcare professional and a science teacher is an efficient and relevant pedagogic method to educate teenage students and protect them against potential future public health issues, including self-medication misuse and ignorance of the healthcare system. This pedagogic method including two short interactive and playful sessions based on debates and short clinical case seems to bring durable knowledge for middle school students at all school grades, levels and ages. This educational format could be also performed for other public health problems which are frequently seen among teenagers such as alcohol, drug addictions or sexually transmitted infections.
Confilcts of interest: none declared.
Financial support: none declared.
FIGURE 1.
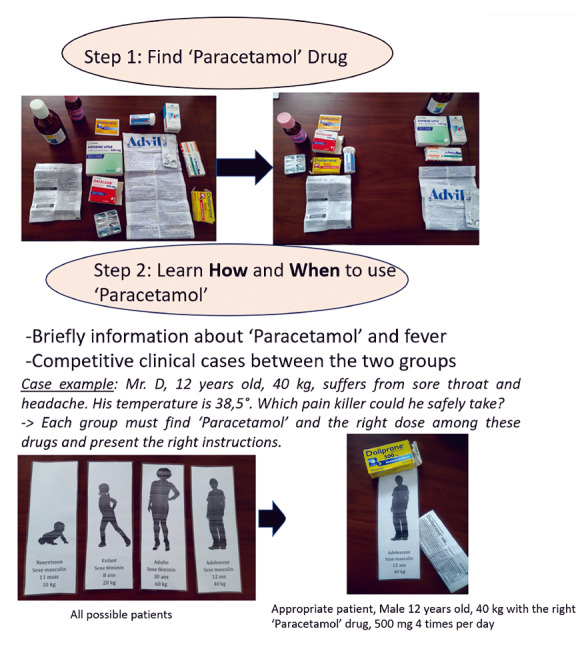
Self-medication workshop
FIGURE 2.
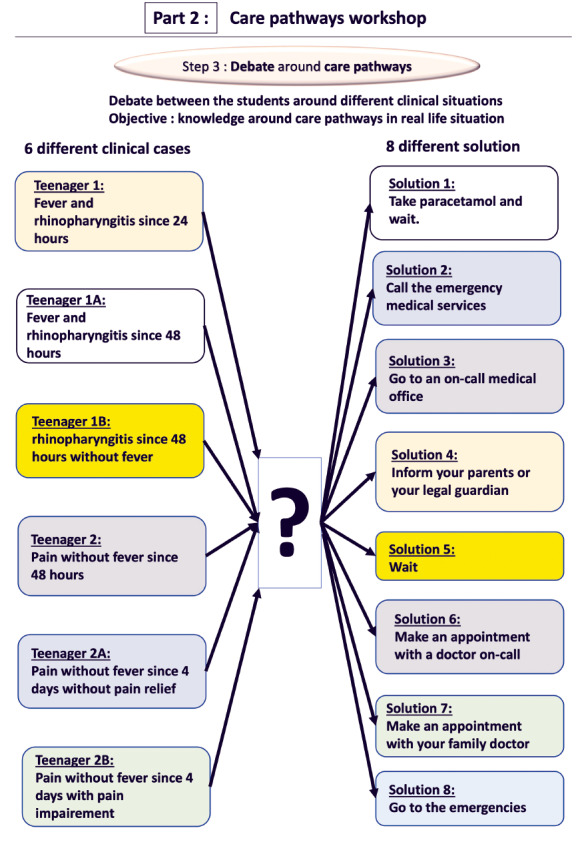
Care pathways workshop
TABLE 1.
The six-multiple choice questions (MCQs)
TABLE 2.
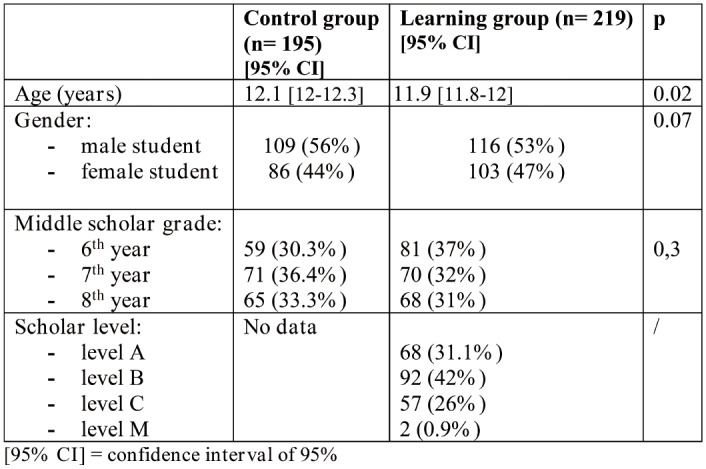
Characteristics of students in groups C and L
TABLE 3.
Characteristics of students in groups C and L
TABLE 4.
Evolution of L group evaluations by age, gender, scholar level and scholar grade
TABLE 5.
Results obtained in the control group at T2 and comparison with the learning (L) group
Contributor Information
Ghita DUBORY, Department of General Medicine, Paris Sorbonne University, France.
Victor HOUSSET, Department of Orthopaedic Surgery, Hôpital Henri Mondor, AP-HP, Université Paris Est Créteil (UPEC), 94010, Creteil, France; Cell and tissue engineering for musculoskeletal disorders (Group 5) / Biology of the NeuroMuscular System (INSERM Team 10) / Institut Mondor de Recherche Biomédicale, U955 INSERM-UPEC, Créteil, France.
Claire BASTARD, Department of Orthopaedic Surgery, Hôpital Henri Mondor, AP-HP, Université Paris Est Créteil (UPEC), 94010, Creteil, France; Cell and tissue engineering for musculoskeletal disorders (Group 5) / Biology of the NeuroMuscular System (INSERM Team 10) / Institut Mondor de Recherche Biomédicale, U955 INSERM-UPEC, Créteil, France.
Roxanne LIARD, Department of General Medicine, Paris Sorbonne University, France.
Marine JOULIN, Paul Vaillant Couturier Middle School. 20 Rue Paul Vaillant Couturier, 94500 Champigny-sur-Marne, France.
Arnaud DUBORY, Department of Orthopaedic Surgery, Hôpital Henri Mondor, AP-HP, Université Paris Est Créteil (UPEC), 94010, Creteil, France.
Angelo V. VASILIADIS, Orthopaedic Surgery and Sports Medicine Department, Croix-Rousse Hospital, University Hospital, 69004 Lyon, France
Vasileios GIOVANOULIS, Department of Orthopaedic Surgery, Hôpital Henri Mondor, AP-HP, Université Paris Est Créteil (UPEC), 94010, Creteil, France.
References
- 1.Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390:156–168. doi: 10.1016/S0140-6736(16)32585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA. 2019;322:1501–1509. doi: 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 3.McDonough JE. Our Greedy Health Care System. Am J Public Health. 2017;107:1744–1745. doi: 10.2105/AJPH.2017.304065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruiz ME. Risks of self-medication practices. Curr Drug Saf. 2010;5:315–323. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
- 5.Faqihi AHMA, Sayed SF. Self-medication practice with analgesics (NSAIDs and acetaminophen), and antibiotics among nursing undergraduates in University College Farasan Campus, Jazan University, KSA. Ann Pharm Fr. 2021;79:275–285. doi: 10.1016/j.pharma.2020.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly T, Conn KM, Zak M. Evaluation of Over-the-Counter Medication Knowledge and Literacy in Adolescent Students. Acad Pediatr. 2018;18:556–562. doi: 10.1016/j.acap.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Chang FC, Chi HY, Huang LJ, et al. Developing school-pharmacist partnerships to enhance correct medication use and pain medication literacy in Taiwan. J Am Pharm Assoc, 2003. [DOI] [PubMed]
- 8.Tesfamariam S, Anand IS, Kaleab G, et al. Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health. 2019;19:159. doi: 10.1186/s12889-019-6470-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buckner EB, Copeland DJ, Miller KS, Holt TO. School-Based Interprofessional Asthma Self-Management Education Program for Middle School Students: A Feasibility Trial. Prog Community Health Partnersh. 2018;12:45–59. doi: 10.1353/cpr.2018.0020. [DOI] [PubMed] [Google Scholar]
- 10.Lee CH, Chang FC, Hsu SD, et al. Inappropriate self-medication among adolescents and its association with lower medication literacy and substance use. PloS One. 2017;12:e0189199. doi: 10.1371/journal.pone.0189199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McClure N, Seibert M, Johnson T, et al. Improving Asthma Management in the Elementary School Setting: An Education and Self-management Pilot Project. J Pediatr Nurs. 2018;42:16–20. doi: 10.1016/j.pedn.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Coughlin PA, Featherstone CR. How to Write a High Quality Multiple Choice Question (MCQ): A Guide for Clinicians. Eur J Vasc Endovasc Surg. 2017;54:654–658. doi: 10.1016/j.ejvs.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Cohen Aubart F, Lhote R, et al. Progressive clinical case-based multiple-choice questions: An innovative way to evaluate and rank undergraduate medical students. Rev Med Interne. 2021;42:302–309. doi: 10.1016/j.revmed.2020.11.006. [DOI] [PubMed] [Google Scholar]