Abstract
Introduction and aim: Ovarian cancer is a prevalent neoplastic condition among females. Early diagnosis is essential in improving patient outcomes. This study aimed to determine the diagnostic value of magnetic resonance imaging (MRI) compared to histopathological diagnosis to distinguish between benign and malignant ovarian masses.
Methods:The present cross-sectional study, which was conducted between 2021 and 2022, included a cohort of women with ovarian mass. Gyneco-oncologists referred all patients to the MRI center. The imaging protocol encompassed T1 and T2 weighted images, T1 fat-suppressed sequence, post-contrast and diffusion-weighted images (DWI). After surgery, the histopathological results were compared to the MRI diagnosis. Statistical analysis was done by using SPSS v.25 software.
Results:A total of 67 women aged 15–82 years old were included in this study. Compared to histopathological diagnosis, MRI had a sensitivity of 96%, a specificity of 69%, a positive predictive value of 64.9% and a negative predictive value of 96.7%. Among patients under 40 years old, MRI showed a sensitivity of 100%, a specificity of 76.2%, a positive predictive value of 72.2% and a negative predictive value of 100%. Solid component and contrast enhancement within the solid component was significantly more frequent in patients with malignant diagnoses than those with benign masses (p<0.05).
Conclusion:According to the results of the study, MRI is valuable for discriminating between benign and malignant ovarian masses, especially in patients under 40.
Keywords:histopathology, ovarian neoplasm, magnetic resonance imaging, ovarian cancer.
INTRODUCTION
Ovarian cancer ranks as the second most prevalent form of malignancy among females and is the fifth principal contributor to cancer-related mortality in women (1). In 2019, the United States experienced an estimated 22,530 newly diagnosed cases, representing 1.3% of the total cancer cases, and witnessed approximately 13,980 deaths accounting for 2.3% of all cancer-related fatalities (2). Given the usual impracticability of conducting biopsies, the significance of the preoperative diagnosis of ovarian tumors through imaging techniques is underscored (3). Ultrasonography is the primary and preferred imaging modality for evaluating adnexal lesions, providing a valuable preoperative assessment to characterize simple cysts and noncomplex masses. However, in cases where ultrasound results are inconclusive or uncertain, a more detailed evaluation of morphologic characteristics and functional status of ovarian tumors is needed before any surgical procedure (4). Magnetic resonance imaging reveals structural characteristics and alterations in signal intensity in T1- and T2-weighted images to aid in assessing ovarian masses. Also, magnetic resonance images can readily identify papillary projections, mural nodules, thick septa and solid components, which may not consistently differentiate between malignant and non-malignant tumors (5).
Regarding the latest development in rapid MRI methods, abdominal and pelvic organs can now be evaluated using diffusion-weighted (DW) imaging, which allows for the analysis of unique cellular characteristics. Diffusion-weighted images are sensitive to alterations in water micro diffusion within both intracellular and extracellular space. However, proficient image interpretation skills are essential for the clinical utilization of this technique (6). In Farghaly Ali et al, adding DW images to routine MRI improved the diagnostic accuracy for detecting ovarian malignancies, exhibiting a sensitivity of 100%, a specificity of 71.4%, a negative predictive value of 100%, a positive predictive value of 74.2% and an efficiency of 84.3% (7). Furthermore, another study indicated the usefulness of dynamic contrast-enhanced MRI in characterizing complex ovarian tumors. Nonetheless, the efficacy of semi-quantitative parameters in distinguishing malignant tumors from borderline cases is significantly inadequate (8). According to Mansour et al (9), conventional MRI data utilizing DW imaging (DWI) can provide confirmation or exclusion of malignancy in cases of suspected ovarian masses.
Overall, the ability to distinguish between malignant and benign masses through non-invasive exams such as MRI can effectively decrease unnecessary treatments and patient stress. Hence, the primary objective of the present study was to evaluate the diagnostic efficacy of MRI in distinguishing between benign and malignant ovarian masses, compared to histopathological analysis.
METHODS
This cross-sectional study was conducted among patients with ovarian masses referred to the MRI department from several gynecological oncology clinics in 2021-2022. All women with ovarian masses had undergone preoperative MRI followed by surgery. The exclusion criteria were patients with uncomplicated endometrioma, those with no MRI before surgery such as persons with metal implants, people who were not allowed to receive contrast agents due to another comorbidity such as renal failure (elevated creatinine levels) or a known history of sensitivity to intravenous contrast agents, and patients whose postoperative histopathology results were unavailable. Based on prior research (7), a minimum sample size of 67 individuals was deemed appropriate. The sampling process was performed using an easy and readily accessible sampling approach.
Study participants (Ethical ID: IR.IAU.MSHD. REC.1400.010) underwent pelvic MRI scans using a Tesla Siemens 1.5 MRI scanner, intravenous contrast administration and non-contrast MRI imaging. Intramuscular hyoscine was administered to mitigate intestinal spasms in preparation for the imaging procedure. The procedural guidelines encompassed acquiring T1 and T2 weighted images and T1 fat saturated. Subsequently, intravenous contrast of 0.2 mmol/kg gadolinium was administered, followed by capturing T1 images in the axial, coronal and sagittal planes (10). Additionally, diffusion images were obtained using b values of 50, 500 and 1000. A radiologist analyzed all images and documented the observations within the research checklist. Finally, the preoperative MRI diagnosis was compared with the postoperative histopathology result following the surgical procedure. The histologically reported masses as borderline tumors were included in the group of malignant tumors in the statistical calculations. Statistical analysis was performed by utilizing SPSS statistical software version 25.
Data analysis
Quantitative data were described using relevant statistical tables and measures, including the mean and standard deviation. Qualitative data were described using frequency and percentage. Furthermore, the appropriate indicators were applied to determine the sensitivity, specificity as well as positive and negative predictive values based on the number of true positive and false positive and negative cases. For this study, IBMSPSS (version 25) and MedCalc 19.0 software were employed and a significance level below 5% was considered significant for the conducted tests.
RESULTS
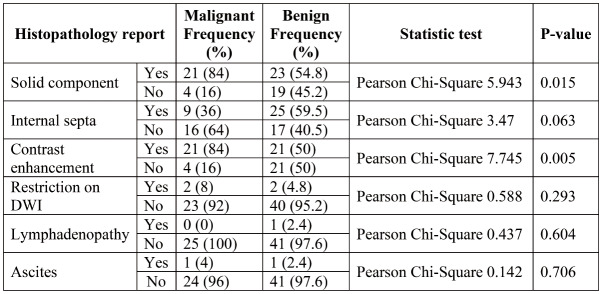
The present study included patients aged between 15 and 82 years, with an average age of 41. Table 1 shows the frequency distribution of different types of ovarian masses according to the histopathology results. Mucinous cystadenoma has the highest occurrence rate (16.1%).
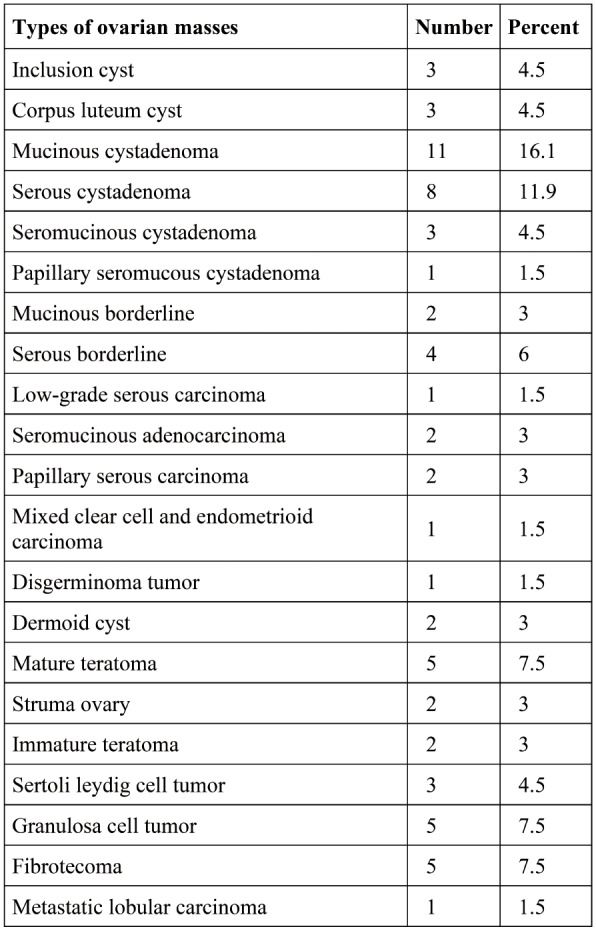
The sensitivity and specificity of MRI compared with histopathology results are shown in Table 2.
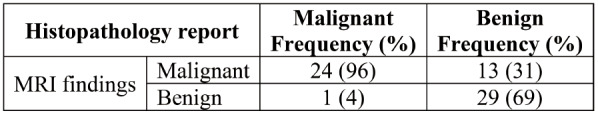
The positive and negative predictive values of MRI compared to histopathology results are presented in Table 3.
The study results indicated that, compared to histopathological examination, the sensitivity and specificity of MRI was 100% and 76.2%, respectively, for subjects under the age of 40, and 91.7% and 61.9%, respectively, for those aged 40 years or older; conversely, the positive and negative predictive value of MRI was 72.2% and 100%, respectively, for study participants under the age of 40, and 57.9% and 92.9% for subjects aged 40 years or older.
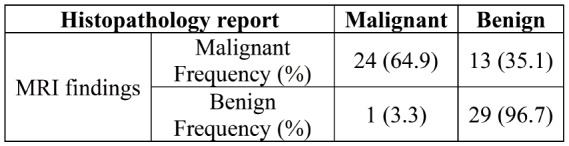
Various morphologic and functional parameters, including the presence of a solid component, internal septa as well as contrast enhancement and diffusion restriction in the solid tumors or solid component of the cystic masses, lymphadenopathy and ascites, were used to differentiate malignant tumors from benign masses for presurgical MRI diagnosis. Detailed information is summarized in Table 4.
According to the findings of the present study, there was a significant difference in the frequency of solid components between patients with malignant and those with benign histopathology results (P=0.15). Furthermore, the contrast enhancement frequency was significantly higher in malignant ovarian tumors than benign masses (P=0.05). The frequency of internal septa, lymphadenopathy and ascites on MRI did not differ significantly between the malignant and benign ovarian masses (P>0.05). The restriction frequency on diffusion sequences was not different between the two groups (P=0.293).
DISCUSSION
Ovarian cancer ranks as the second most prevalent form of cancer among women, which is frequently detected at an advanced stage and is characterized by extensive peritoneal metastases. The survival rate is reduced to 10% in patients with FIGO stage IV and ranges from 20% to 40% in those with FIGO stage IIIC (11). The process of cancer staging is a fundamental principle, which plays a vital role in forecasting patient prognosis and devising optimal treatment strategies (12). There is a universally accepted criterion for preoperative diagnosis, and distinguishing between benign and malignant ovarian tumors, especially when they exhibit both solid and cystic components, remains challenging. Several indicators are considered in utilizing MRI data to predict ovarian malignancies, such as the thickness of walls and septa (more than 3 mm) and the identification of internal structures such as papillary projection, nodularity, presence of solid component, necrosis, hemorrhage or regions that exhibit avid contrast enhancement. These imaging parameters overlap for benign and malignant ovarian lesions. According to Naggara et al, it is evident that the above-mentioned parameters may not consistently serve as the most precise predictors for ovarian malignancies (13). For example, a recent study including 168 ovarian masses showed that papillary projection or nodularity manifested in 37.5% of benign epithelial ovarian tumors. Further histological examination revealed that those projections were present in benign tumor samples at a rate of 20-26%, in borderline tumors at 62-78% and in ovarian cancers at 59-92% (14). Consequently, relying solely on the characteristics of the papillary ridge for diagnosis exhibited limited sensitivity and specificity.
Wenhua Li et al (15) found that ovarian surface epithelial cystadenocarcinoma was mainly associated with lower mean apparent diffusion coefficient (ADC) values. Hence, the inclusion of DW-MRI in standard pelvic MRI protocols has the potential to enhance the precision of differentiating between benign and malignant ovarian pathology. Studies have revealed that diffusion reflects the random movement of molecules caused by thermal energy (Brownian motion). In biological tissues, this microscopic motion encompasses the distribution of water molecules and blood circulation within capillary networks. Furthermore, research conducted under controlled laboratory conditions has demonstrated contrasting rates of water molecule diffusion between the extracellular and intracellular components of tissues (13). For example, the presence of the cell membrane can lead to a relatively slow-down diffusion process in the intracellular compartment. Similarly, ADC values quantitatively represent the diffusion characteristics of tissues and are primarily proportional to the extracellular intracellular ratio. As a result, ADC values decline as tissue cellularity or cell density increases. Hence, cell density in a tumor can serve as an indicator because it encompasses intracellular organelles along with matrix fibers and soluble macromolecules, all of which collectively contribute to the constraints on diffusion. The detection of diffusion limitations or low ADC values could suggest the existence of malignant tissue or the presence of tissue hypercellularity. Hence, using DW-MRI and the associated assessment of ADC values offers an ideal approach to employ imaging techniques in quantifying capillary perfusion and water diffusion.
This study was performed to determine the diagnostic value of MRI in distinguishing between benign and malignant ovarian masses in a group of 67 patients during 2021-2022 who were referred to the MRI department by gynecologists or oncologists during 2021-2022. The primary objective was to compare the MRI diagnosis with histopathological results to determine the relative diagnostic value of MRI. Based on the outcomes, 25 malignant and 42 benign tumors were reported; the sensitivity of MRI in discerning ovarian masses compared to histopathology results was 96%, while its specificity reached 69%. Furthermore, compared to histopathological diagnosis, MRI had a positive predictive value of 64.9% and a negative predictive value of 96.7% when examining patients with ovarian masses. Also, compared to histopathological examination, MRI had a sensitivity of 100% for subjects under the age of 40 years and a specificity of 76.2%. Additionally, in patients under 40 years old, MRI had a positive predictive value of 72.2% and a negative predictive value of 100% in distinguishing ovarian masses when compared to histopathological examination.
Magnetic resonance imaging showed a significant distinction in the frequency of solid component between malignant cases and those with benign histopathology results (p=0.015). These findings aligned with the outcomes reported in comparable studies (7, 9, 15). Furthermore, the occurrence rate of contrast enhancement by the solid component was more significant in patients with malignant histopathology than those with benign histopathology (p <0.005).
In a study conducted by Wenhua Li (15), the utilization of high b values (1000 s/mm2) in diffusion- weighted images exhibited a significant level of sensitivity (90.1%) and specificity (89.9%), which allowed the differentiation between benign and malignant ovarian tumors. However, the present study revealed no significant difference in the extent of diffusion restriction within the solid component between benign and malignant masses (P>0.05). These findings may be due to variations in the ADC values used as the standard in different studies, emphasizing the need for additional research and establishing a single standard to ensure a more precise comparison.
CONCLUSION
Magnetic resonance imaging is a valuable method for distinguishing benign ovarian tumors from malignant ones, particularly in patients under 40 years old. Due to its high sensitivity and favorable negative predictive value in this context, it is suggested that an MRI should be performed on suspicious ovarian masses for preoperative decision-making.
Financial support: none declared.
TABLE 1.
Frequency distribution of different types of ovarian masses
TABLE 2.
Sensitivity and specificity of magnetic resonance imaging compared to histopathology diagnosis
TABLE 3.
Positive and negative predictive values of MRI compared to histopathological result
TABLE 4.
Summary of results obtained in the present study
Contributor Information
Azamsadat JALILI, Faculty of Medicine, Mashhad Medical Sciences, Islamic Azad University, Mashhad, Iran.
Narges AFZALI, Faculty of Medicine, Department of Radiology, Mashhad Medical Sciences, Islamic Azad University, Mashhad, Iran.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Taylor EC, Irshaid L, Mathur M. Multimodality imaging approach to ovarian neoplasms with pathologic correlation. Radiographics. 2021;41:289–315. doi: 10.1148/rg.2021200086. [DOI] [PubMed] [Google Scholar]
- 3.Takeuchi M, Matsuzaki K, Nishitani H. Diffusion-weighted magnetic resonance imaging of ovarian tumors: differentiation of benign and malignant solid components of ovarian masses. J Comput Assist Tomogr. 2010;34:173–176. doi: 10.1097/RCT.0b013e3181c2f0a2. [DOI] [PubMed] [Google Scholar]
- 4.Zhang P, Cui Y, Li W, et al. Diagnostic accuracy of diffusion-weighted imaging with conventional MR imaging for differentiating complex solid and cystic ovarian tumors at 1.5 T. World J Surg Oncol. 2012;10:1–8. doi: 10.1186/1477-7819-10-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imaoka I, Wada A, Kaji Y, et al. Developing an MR Imaging Strategy for Diagnosis of Ovarian Masses. Radiographics. 2006;26:1431–1448. doi: 10.1148/rg.265045206. [DOI] [PubMed] [Google Scholar]
- 6.Kyriazi S, Collins DJ, Morgan VA, et al. Diffusion-weighted Imaging of Peritoneal Disease for Noninvasive Staging of Advanced Ovarian Cancer. Radiographics. 2010;30:1269–1285. doi: 10.1148/rg.305105073. [DOI] [PubMed] [Google Scholar]
- 7.Rahma Farghaly A, Nassef HH, Ibrahim AM, et al. The Role of Diffusion Weighted Imaging in suspected cases of ovarian cancer. The Egyptian Journal of Radiology and Nuclear Medicine. 2020;51:1–11. [Google Scholar]
- 8.Li H-M, Qiang J-W, Ma F-H, Zhao S-H. The value of dynamic contrast–enhanced MRI in characterizing complex ovarian tumors. J Ovarian Res. 2017;10:1–7. doi: 10.1186/s13048-017-0302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mansour S, Wessam R, Raafat M. Diffusion-weighted magnetic resonance imaging in the assessment of ovarian masses with suspicious features: strengths and challenges. The Egyptian Journal of Radiology and Nuclear Medicine. 2015;46:1279–1289. [Google Scholar]
- 10.Forstner R, Thomassin-Naggara I, Cunha TM, et al. ESUR recommendations for MR imaging of the sonographically indeterminate adnexal mass: an update. Eur Radiol. 2017;27:2248–2257. doi: 10.1007/s00330-016-4600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46:765–781. doi: 10.1016/j.ejca.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Prat J. FIGO's staging classification for cancer of the ovary, fallopian tube, and peritoneum: abridged republication. J Gynecol Oncol. 2015;26:87–89. doi: 10.3802/jgo.2015.26.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomassin-Naggara I, Daraï E, Cuenod CA, et al. Contribution of diffusion-weighted MR imaging for predicting benignity of complex adnexal masses. Eur Radiol. 2009;19:1544–1552. doi: 10.1007/s00330-009-1299-4. [DOI] [PubMed] [Google Scholar]
- 14.Bazot M, Nassar-Slaba J, Thomassin-Naggara I, et al. MR imaging compared with intraoperative frozen-section examination for the diagnosis of adnexal tumors; correlation with final histology. Eur Radiol. 2006;16:2687–2699. doi: 10.1007/s00330-006-0163-z. [DOI] [PubMed] [Google Scholar]
- 15.Li W, Chu C, Cui Y, et al. Diffusion-weighted MRI: a useful technique to discriminate benign versus malignant ovarian surface epithelial tumors with solid and cystic components. Abdom Radiol. 2012;37:897–903. doi: 10.1007/s00261-011-9814-x. [DOI] [PubMed] [Google Scholar]