Abstract
Objectives. To evaluate the effects of a comprehensive traffic safety policy—New York City’s (NYC’s) 2014 Vision Zero—on the health of Medicaid enrollees.
Methods. We conducted difference-in-differences analyses using individual-level New York Medicaid data to measure traffic injuries and expenditures from 2009 to 2021, comparing NYC to surrounding counties without traffic reforms (n = 65 585 568 person-years).
Results. After Vision Zero, injury rates among NYC Medicaid enrollees diverged from those of surrounding counties, with a net impact of 77.5 fewer injuries per 100 000 person-years annually (95% confidence interval = −97.4, −57.6). We observed marked reductions in severe injuries (brain injury, hospitalizations) and savings of $90.8 million in Medicaid expenditures over the first 5 years. Effects were largest among Black residents. Impacts were reversed during the COVID-19 period.
Conclusions. Vision Zero resulted in substantial protection for socioeconomically disadvantaged populations known to face heightened risk of injury, but the policy’s effectiveness decreased during the pandemic period.
Public Health Implications. Many cities have recently launched Vision Zero policies and others plan to do so. This research adds to the evidence on how and in what circumstances comprehensive traffic policies protect public health. (Am J Public Health. 2024;114(6):633–641. https://doi.org/10.2105/AJPH.2024.307617)
Numerous studies have shown persistent disparities in traffic-related injuries—and in unintentional injuries broadly—by income and race.1,2 Low-income people are more likely to experience and die from unintentional injuries and face long-term sequelae.3 They are also more likely to live in areas with roadways conducive to crashes,4 with low-income Black Americans being especially likely to live in high-crash areas.5 Despite this, little is known about how metropolitan-area-wide transportation policies affect these populations.
This study uses New York State (NYS) Medicaid data to evaluate the impact of New York City’s (NYC’s) Vision Zero traffic policy on low-income residents. Vision Zero included a package of over 100 interventions: speed limit reduction from 30 to 25 mph, physical modifications such as protected bike lanes, vehicle mandates such as trailer sideguards, educational campaigns, and traffic law enforcement.6 Mayor Bill de Blasio implemented the policy in early 2014 through 6 agencies. Modeled on a program established in Sweden in 1997,7 Vision Zero policies have since been adopted in dozens of US cities, including Boston, Massachusetts; Los Angeles, California; and Seattle, Washington. The majority of road safety professionals advocate Vision Zero strategies.8
Traffic-related injuries continue to be a major policy priority, as public concern grows.9,10 Two meta-analyses concluded that roadway design and traffic calming can reduce traffic-related risks,11,12 and several studies of stand-alone interventions, including speed humps,13 red light cameras,14 and signal timing,15 have also found positive impacts. However, not all Vision Zero packages have proven successful in practice.16–18 In NYC, reports by city agencies showed initial decreases in fatalities, with a 26% reduction through 2019, yet gains appeared greatest in the earlier years and have stagnated or been uneven for subpopulations such as cyclists since then.19,20 In the years since the COVID-19 outbreak in particular, reduced law enforcement and riskier driving have raised concerns that NYC may lose any gains from Vision Zero.21,22 In other US cities, commentators have questioned Vision Zero’s effectiveness, citing fundamental cultural and technological differences with the European cities that saw success.23
Even if Vision Zero is effective in US cities such as NYC as a whole, it is a nontargeted policy, so benefits may not accrue equitably. Some worry that Vision Zero may increase inequity if high-need, low-income areas are overlooked for interventions, and a 2017 analysis showed that interventions were less likely to be located in NYC’s low-income neighborhoods, despite having the highest fatality rates at baseline.24 Tracking injuries in Medicaid can shed light on how Vision Zero affects low-income New Yorkers and, by extension, whether citywide policies can address injury disparities. Medicaid data provide several other advantages. Most analyses have relied on police reports and Department of Transportation data to quantify changes in crashes,19 limiting our understanding of unreported injuries, injury severity or sequelae, and costs.25 Our data capture injuries of varying severity and longer-term consequences, including follow-up care such as physical therapy and medications. Medicaid data enable measurement of medical expenditures, offering an aggregated metric of impact.
Crucially, Medicaid data allow us to construct a compelling comparison group of similar low-income individuals living near NYC—a design that has not been implemented in evaluations to date. Although a recent article comparing NYC streets subjected to the speed limit reduction with those exempt from it found meaningful decreases in crashes, it could not estimate the broader impact of the Vision Zero package, given that even areas exempt from speed reduction still saw redesign, enforcement, and educational interventions.26 The period over which interventions were rolled out also coincided with other state and national safety initiatives, potentially confounding single-group time series analyses in prior studies. For instance, the public spotlight on traffic fatalities has put pressure on manufacturers to improve safety through backup cameras, collision alert systems, and safer phone integration. Using a comparison group of Medicaid enrollees in nearby areas allowed us to isolate Vision Zero’s influence from many confounding explanations.
METHODS
We used NYS Medicaid claims from 2009 to 2021. The sample encompassed individuals who were enrolled in Medicaid at least 1 month between 2009 and 2021 and had a home address in NYC or the 6 surrounding counties generally considered NYC’s suburbs (Appendix Exhibit A, available as a supplement to the online version of this article at http://www.ajph.org). Race/ethnicity, biological gender, and county were self-reported by enrollees.
Outcomes
International Classification of Disease (ICD) E-codes were used to identify crash-related claims.27 We included the E81 series under ICD-9 (Hyattsville, MD: National Center for Health Statistics; 1980), as well as several codes indicating traffic-related incidents of “unspecified” circumstances, and ICD-10 (Geneva, Switzerland: World Health Organization; 1994) equivalents. The codes encompass injuries involving cars, motorcycles, pedestrians, or bicyclists (online Appendix Exhibit B) and capture inpatient and outpatient visits. To measure traumatic brain injuries (TBI), we modified the Agency for Healthcare Research and Quality’s clinical classification category for “intracranial injury” by excluding “late effects” and “history of” head injury and including “head injury unspecified.”
Any given traffic injury claim does not necessarily indicate the crash happened that day, as the visit may be a follow-up. To reduce risk of false positives, we implemented a 45-day washout: if we found another traffic-related claim up to 45 days earlier, we counted only the first. Because Medicaid is the payer of last resort, traffic-related claims may be denied if an automobile insurer is responsible for payment. We therefore included denied claims to reduce false negatives.
To estimate financial impact, we calculated Medicaid expenditures associated with the crash and subsequent year of care. We calculated expenditures as the sum of all payments to providers, including fee-for-service payments made by the state and plan-reported payments to providers (for managed care enrollees). It is difficult to determine exactly which health system utilization is related to the injury and which would have occurred even in an injury’s absence; therefore, we included expenditures from all categories of care in the 12 months following the injury and leveraged the difference-in-differences methodology (described in the next section) to “wash out” unrelated expenditures (e.g., routine care).
Statistical Analyses
We analyzed the data set at the person-year level: every eligible enrollee had a row for each year, with variables indicating the injury count, injury details, demographics, and months enrolled. We tested for the policy’s effectiveness using difference-in-differences (DID) Poisson regression models, with an offset term to account for months enrolled.
We controlled for age, race/ethnicity, and gender to account for time-varying compositional differences between the areas. An interaction term between a location indicator (NYC vs suburbs) and a pre–post policy indicator provided the age-, race/ethnicity-, and gender-adjusted estimate of the policy’s impact. We then computed the marginal effects from the interaction coefficient to report absolute risk differences in the outcomes per 100 000 person-years due to Vision Zero, relative to the comparison areas. This DID effect estimate can be interpreted as the policy-induced change in injuries, net of any unrelated trend changes.28 Standard errors were clustered by zip code to account for varying exposure to different elements of the policy that may lead to nonindependence of errors. Given the pandemic’s influence on traffic patterns, enrollment, and utilization, we calculated an effect estimate excluding pandemic years (postpolicy period = 2014–2019), as well as one including pandemic years (postpolicy period = 2014–2021).
The DID design required the comparison group be on a similar trend prior to the intervention but did not require equivalent levels, although we controlled for age, race/ethnicity, and gender in the event that enrollee composition evolved differentially. To build the case that the suburbs are an appropriate counterfactual, we tested the coefficients for each year of the prepolicy period (2009–2013) in a model using dummy variables for each year (rather than a single pre–post indicator) interacted with the region indicator. Prepolicy coefficients close to 0 would demonstrate that the groups were on similar trajectories.
Because we did not have the crash location, we used home address as a proxy. Although some crashes occur outside one’s neighborhood, crashes are most likely to occur near home.2,29 This measurement error would only affect crashes occurring outside of NYC for NYC residents (and vice versa). If a Bronx resident was injured in Manhattan, it would not influence the estimate. To approximate the extent of this bias, we calculated the share of emergency injuries sent to a hospital within the enrollee’s county of residence (assuming that emergencies would be taken to a hospital near the crash).
We conducted several robustness checks. First, we focused on 2 NYC boroughs where cars are more common and compared them with the suburban counties closest to them: Queens was compared with Long Island, and the Bronx was compared with counties to the north (Westchester, Putnam, Orange, Rockland). Several other forces were at play around the time of Vision Zero. Most notably, Uber and Lyft rideshares grew in popularity within NYC, increasing the number of cars; rideshares remained illegal in the suburbs until 2017. Second, NYC established a bikeshare program (Citibike) in 2013 that increased the number of cyclists and changed streetscapes. To account for rideshares, we added the number of vehicles registered by county to our model. To account for Citibike, we ran a model excluding enrollees living in the areas where most Citibike stations existed during this period (south of 59th Street in Manhattan and western Brooklyn).
Finally, to address the fact that we could not perfectly identify new, unique injuries for people enrolled in Medicaid for brief stints, we reran the model limited to people enrolled 10 months or longer.
RESULTS
The number of unique enrollees totaled 10 999 419 (65 585 568 person-years). We identified 180 664 unique traffic-related injuries (168 715 individuals) from 2009 to 2021. NYC and its suburbs differed demographically: NYC enrollees were less likely to be White; were more likely to be Asian, Black, or Hispanic; and had a median age 2 years older than non-NYC enrollees (Table 1). Those involved in a crash (in either area) were more likely to be Black and less likely to be female. Subsequent models controlled for race/ethnicity, gender, and age to account for demographic differences that may have varied across the areas over time and been associated with injury risk. People were highly likely to be injured within their region of residence: of people with an emergency injury, 88.3% in NYC and 86.7% in the suburbs were sent to a hospital within their home region. This indicates that most crashes occurred close to home, and any attenuation bias from geographic misclassification was minimal.
TABLE 1—
Medicaid Enrollee Demographics in New York City (NYC) vs Suburbs (Comparison Counties): 2009–2021
| All Enrollees | Enrollees With a Traffic-Related Injury | |||
| NYC | Suburbs | NYC | Suburbs | |
| Total person-years | 51 866 126 | 13 719 442 | 140 486 | 40 178 |
| Unique enrollees, no. | 8 585 528 | 2 413 891 | 135 244 | 33 471 |
| Race/ethnicity, % | ||||
| Asian | 12.8 | 4.4 | 6.4 | 2.7 |
| Black | 18.5 | 12.7 | 26.1 | 19.6 |
| Hispanic | 18.0 | 10.6 | 17.8 | 8.7 |
| White | 13.8 | 30.6 | 11.5 | 28.8 |
| Other/unknown | 36.9 | 41.8 | 38.1 | 40.3 |
| Median age, y (IQR) | 30.5 (14.1–52.4) | 28.3 (12.2–49.2) | 30.9 (20.8–46.2) | 30.3 (20.5–45.3) |
| % Female | 53.9 | 54.6 | 44.4 | 49.1 |
| Median annual months enrolled (IQR) | 12 (10–12) | 12 (9–12) | 12 (12–12) | 12 (12–12) |
Note. IQR = interquartile range. Data come from New York State Medicaid claims and encounter data. Race/ethnicity and gender are self-reported on enrollment in Medicaid.
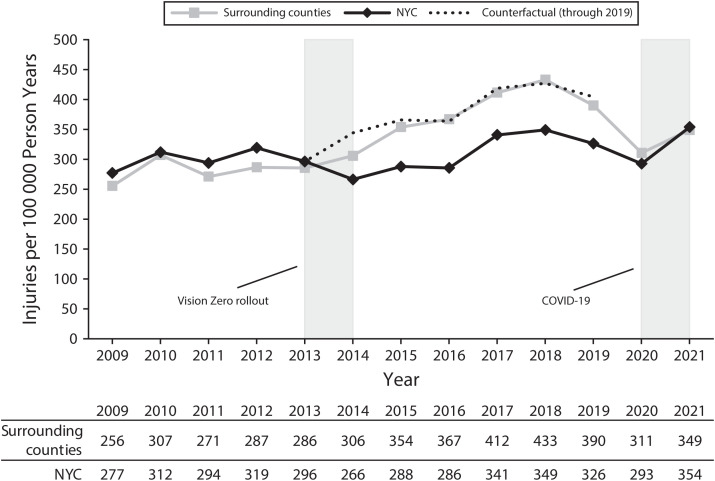
Figure 1 shows adjusted injury rates among Medicaid enrollees in NYC versus surrounding counties (unadjusted estimates showing similar results are in online Appendix Exhibit C). Rates in the 2 areas tracked one another very closely prior to Vision Zero, and the DID coefficients for these years (year × region coefficients) are effectively 0 (P > .05; online Appendix Exhibit D), suggesting that these counties are an appropriate comparison. Figure 1 shows that the yearly covariate-adjusted rates of traffic-related injuries among NYC Medicaid enrollees were slightly higher than those in nearby counties until 2014 (Vision Zero’s rollout), when NYC’s rate dropped significantly below the non-NYC rate. This difference persisted until the onset of COVID-19 in 2020, when NYC’s rate converged back to the suburbs’ rate, reversing the gains from the first 6 years of the policy.
FIGURE 1—
Adjusted Annual Traffic-Related Injury Rate Among Medicaid Enrollees in New York City (NYC) vs Surrounding Counties: 2009–2021
Note. Rates are adjusted for individual age, race/ethnicity, and gender in a Poisson model with an offset term for enrolled months. The counterfactual line is estimated from the difference-in-differences (DID) regression model described in the Statistical Analyses section: in the absence of Vision Zero, injury rates in NYC would be expected to be 77.5 (95% confidence interval [CI] = 57.6, 97.4) injuries per 100 000 person-years higher than the observed rate. If the pandemic period is included in the DID estimation model, the counterfactual rate would be 62.5 (95% CI = 42.2, 82.8) injuries per 100 000 person-years higher than the observed rate.
The DID estimate excluding the pandemic years (postpolicy period = 2014–2019) indicates that NYC had 77.5 fewer traffic-related injuries per 100 000 person-years than otherwise would have been expected in the years after Vision Zero’s launch (95% confidence interval [CI] = −97.4, −57.6; P < .001). This represents a 30% reduction from baseline. Including the pandemic years in the DID estimate (postpolicy period = 2014–2021) gives a total decrease of 62.5 fewer injuries per 100 000 person-years (95% CI = −82.8, −42.2; P < .001)—a lower effect estimate, which reflects the reversal of Vision Zero’s progress during the pandemic. Online Appendix Exhibit F shows full regression output.
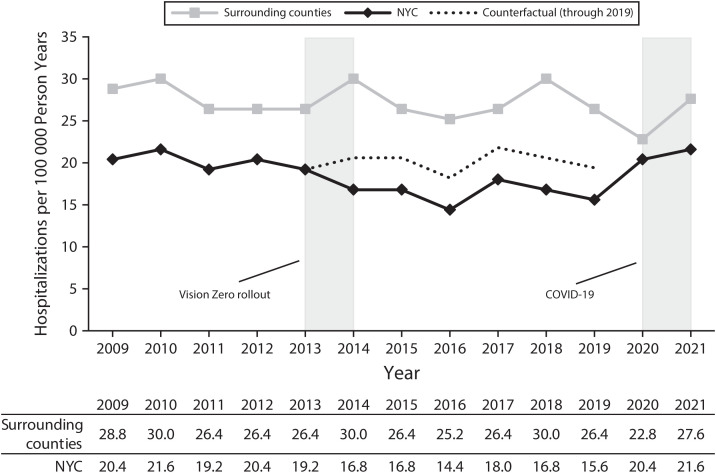
We examined several subtypes of traffic-related injuries to assess whether particularly severe crashes decreased. Figure 2 shows the adjusted trends for traffic-related hospitalization rates, and online Appendix Exhibit E shows the adjusted trends for TBI. Both outcomes show the same pattern as the overall rate: a parallel trend prior to Vision Zero, followed by a relative decrease in NYC after the policy until the COVID-19 outbreak. The impact for both outcomes also reversed during the pandemic. The DID model estimates a reduction of 3.8 hospitalizations per 100 000 person-years (95% CI = −6.3, −1.3; P < .001) and a reduction of 4.0 TBIs per 100 000 person-years (95% CI = −6.3, −1.7; P = .004) for the model excluding the pandemic (online Appendix Exhibit F). These impacts represent 18% and 34% decreases from baseline, respectively. In the model including the pandemic, we estimated a reduction of 1.8 hospitalizations per 100 000 person-years (95% CI = −4.4, 0.8; P = .05) and a reduction of 2.8 TBIs per 100 000 person-years (95% CI = −5.1, 0.5; P = .11).
FIGURE 2—
Adjusted Annual Traffic-Related Hospitalization Rate Among Medicaid Enrollees in New York City (NYC) vs Surrounding Counties: 2009–2021
Note. Rates are adjusted for individual age, race/ethnicity, and gender in a Poisson model with an offset term for enrolled months. The counterfactual line is estimated from the difference-in-differences (DID) regression model described in the Statistical Analyses section: in the absence of Vision Zero, hospitalization rates in NYC would be expected to be 3.8 (95% confidence interval [CI] = 1.3, 6.3) per 100 000 person-years higher than the observed rate. If the pandemic period is included in the DID estimation model, the counterfactual rate would be 1.8 (95% CI = −0.8, 4.4) injuries per 100 000 person-years higher than the observed rate.
Prior to Vision Zero, total care in the 12 months following crash injuries in NYC resulted in around $100 million to $125 million in expenditures annually, or around $30 per enrollee ([total spending in the 12 months after crashes for NYC enrollees]/[all NYC Medicaid enrollees]). Our DID model estimates that Vision Zero led to savings of $4.34 per enrollee in annual Medicaid expenditures (95% CI = −8.14, −0.53; P = .026; online Appendix Exhibit F), amounting to total savings of $90.8 million over the first 5 years (2014–2018). That is, had NYC continued to match the trend of the suburbs, total expenditures in the year following a crash would have been $762 million for crashes from 2014 to 2018; instead, actual postcrash expenditures over this window were $671 million.
Given prior evidence of racial/ethnic disparities,5 we stratified the model by race/ethnicity to obtain group-specific estimates (controlling for age and gender, and clustering errors by zip code). These race/ethnicity-specific estimates show a substantially larger reduction in injuries among Black enrollees (−195.6 person-years [95% CI = −237.0, −154.2]) than all other racial/ethnic groups (−59.4 [95% CI = −82.2, −36.5], −62.5 [95% CI = −87.4, −37.6], and −26.9 [95% CI = −57.6, 3.8] for White, Hispanic, and Asian enrollees, respectively).
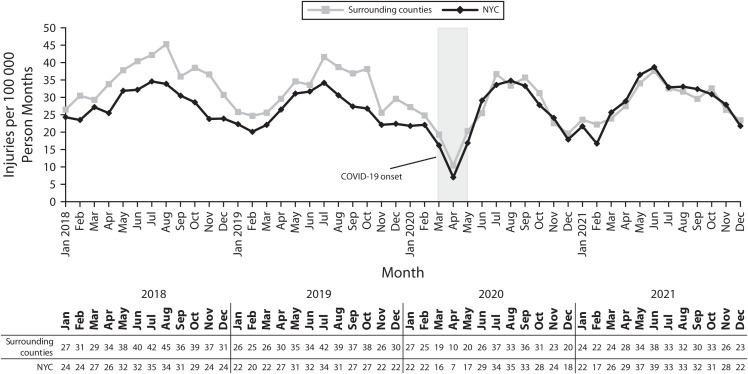
To understand the reversal of Vision Zero’s gains in 2020, we created a person-month version of the data set. If the gap between the regions was already closing before the pandemic, this would suggest the reversal was unrelated to the pandemic and may have been due to other factors, such as the launch of traffic policies in the suburbs or prepandemic decreases in the policy’s effectiveness in NYC. Figure 3 confirms that NYC’s reductions in injuries persisted up until February 2020 (15%–20% below the suburbs’ rate), at which point NYC’s rate immediately converged to the suburbs’ rate at the pandemic’s onset. NYC never regained its prepandemic achievements (through the latest data in 2021), suggesting that Vision Zero did not operate effectively during the pandemic. This is further confirmed by online Appendix Exhibit G, which uses ticketing data to show that, on average, NYC had 9771 more monthly tickets than the suburbs prior to the pandemic, but had 9715 fewer monthly tickets than the suburbs during the pandemic (DID estimate: −25.4% greater reduction in NYC; 95% CI = −25.7, −25.2).
FIGURE 3—
Adjusted Monthly Traffic-Related Injury Rate Among Medicaid Enrollees in New York City (NYC) vs Surrounding Counties: 2018–2021
Note. Rates are adjusted for individual age, race/ethnicity, and gender in a Poisson model.
In robustness checks focusing on Queens versus Long Island and the Bronx versus the northern suburbs, we observed effect sizes nearly identical to the main analysis (online Appendix Exhibit H). To account for rideshares, we added the number of vehicles registered by county to our model. The number of vehicles in NYC increased 12.2% between 2009 and 2017, whereas the number of vehicles in nearby counties increased by just 5.6% (online Appendix Exhibit I). However, after we controlled for vehicle registrations, our DID estimates remained nearly identical, suggesting that growth in vehicles was not confounding the estimate (online Appendix Exhibit H). We also obtained nearly identical estimates when we excluded areas with high Citibike participation, suggesting that Citibike infrastructure was not driving the effect. We also obtained a similar estimate when we limited the sample to those continuously enrolled (≥ 10 months/year; online Appendix Exhibit H).
DISCUSSION
Injuries are an important driver of socioeconomic and racial disparities. We found evidence that in the first 6 years of NYC’s citywide traffic safety policy, Vision Zero, the rate of traffic-related injuries among low-income New Yorkers, and low-income Black New Yorkers in particular, fell relative to trends in surrounding counties. Given that low-income and Black Americans are more likely to live and work in places with unsafe roadways and face injuries,4,5,30 these findings suggest that Vision Zero–style reforms are promising for reducing disparities. One concern with traffic policies is that they affect only the low-hanging fruit (e.g., fender-benders) while having little influence on severe crashes. Our data suggest that this was not the case; residents saw reductions in severe injuries, including TBI or hospitalization. These reductions may have contributed to decreases in Medicaid expenditures. We estimate that Vision Zero saved Medicaid a total of roughly $90.8 million over the first 5 years.
Our most striking finding is that the trend in NYC stayed persistently lower than the trend in nearby counties until the onset of the pandemic, despite growth in crash incidence in non-NYC areas. This finding persists even in the boroughs of NYC that are most like the suburbs, making Vision Zero the most plausible explanation. We explored other potential confounding explanations, including the introduction of rideshare and bikeshare services. Rideshares and bikeshares might increase crash risk, by increasing the number of vehicles and vulnerable riders,31 whereas other evidence suggests that these innovations might reduce risk because of “safety in numbers” or traffic slowing.32 However, our results persisted even after we included the number of vehicles registered as a covariate and when we omitted areas with high bikeshare penetration.
Notably, Vision Zero had positive impacts only in the period before COVID-19. In 2020 and 2021, gains from Vision Zero reversed, with NYC’s injury rate converging back toward that of surrounding counties. This is not especially surprising, given upheavals to NYC’s priorities and density during COVID-19. Two possible reasons include increases in unsafe driving behavior and decreases in traffic enforcement in NYC. Reckless driving during the pandemic—related to increases in driving under the influence or decline of “safety in numbers” in the less-dense pandemic-era city32—has been documented.21 Despite this, the NYC Police Department issued traffic violations at a lower rate than usual in 2020 and 2021, because of a shift in the department’s priorities during the pandemic and smaller workforce.22 Using ticketing data, we found a 25% greater reduction in traffic ticketing during the pandemic in NYC relative to the suburbs, lending credibility to this explanation. This is also consistent with prior research suggesting that speed limit reductions and traffic enforcement may be particularly critical pieces of Vision Zero.26 Our analyses demonstrate that Vision Zero was highly effective in the prepandemic world for which it was designed; whether it can be effectively adapted to the postpandemic era, and what changes are needed to recapture those gains, remain to be seen.
To our knowledge, the comparison counties did not undergo comprehensive reform, although the NYS Department of Transportation signed the Complete Streets Act in 2011, requiring projects involving state funds explicitly to “consider safe, convenient access” in the design of new roadways.33 Cities in 4 of the comparison counties made local-level “Complete Streets” pledges for construction involving municipal funds. However, these pledges do not change speed limits or require proactive redesign of roadways, as Vision Zero does. If anything, Complete Streets pledges in some comparison counties would bias our estimate toward the null, only understating Vision Zero’s impact.
Limitations
Although our data are comprehensive and the difference-in-differences approach is strong, this study has limitations. First, we did not know the exact location of crashes and relied on patients’ addresses. We found that 9 in 10 emergency injuries were sent to a hospital within their region of residence, indicating that bias from geographic misclassification was minimal. Still, future work should leverage better geographic information, both to minimize geographic misclassification and better understand relative contributions of each specific Vision Zero intervention (intersection modification, protected bike lanes, speed reduction) across neighborhoods. Second, we likely missed some injuries because of insurance laws in which automobile insurance is the sole payer. Third, although we adjusted for major demographic characteristics, it is possible that unmeasured time-varying differences in enrollees between NYC and the suburbs could still have biased our estimate. Finally, claims-based coding is subject to undercounting, as traffic injuries are only indicated if providers use “E-codes,” which not all providers consistently do.34
Public Health Implications
Our analyses provide evidence of a substantial impact of Vision Zero on traffic injuries among a disadvantaged population and imply health care savings. As a cornerstone piece of NYC’s recent agenda, Vision Zero generated considerable media attention, and dozens of US cities launched their own Vision Zero plans. NYS’s Governor Kathy Hochul recently signed statewide laws making it easier for cities to lower speed limits and increasing fines for hit-and-runs, building on momentum from NYC’s Vision Zero.35 NYC has also recently committed to increasing traffic enforcement to prepandemic levels, suggesting the potential for NYC to realize gains from Vision Zero once more.22
Although NYC and other cities continue to face challenges in reaching the goal of zero fatalities,9,23 our finding that Vision Zero policy bent an otherwise upward trend in injuries supports the idea that comprehensive traffic reform can make a meaningful dent in injury incidence, despite cultural and technological differences with European Vision Zero cities. This evaluation can guide efficient use of resources as the policy evolves and support conversations about why Vision Zero was less effective during the pandemic. Finally, it provides support for traffic reform as a strategy for enhancing health equity by reducing injuries among groups who are particularly vulnerable to the consequences and are at risk for being overlooked in citywide, nontargeted interventions.
ACKNOWLEDGMENTS
We gratefully acknowledge the funding for this research from the Robert Wood Johnson Foundation. K. L. Dragan was also supported by the Agency for Healthcare Research and Quality (T32HS000055) and the National Institute of Mental Health of the National Institutes of Health (T32MH019733) for a portion of the period over which this research was conducted.
We thank the NYU Health Evaluation and Analytics Lab and the New York State Department of Health for making the Medicaid claims data available.
Note. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the New York State Department of Health. Examples of analysis performed within this article are only examples. They should not be utilized in real-world analytic products.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
This study was approved by the New York University institutional review board.
See also Ehsani et al., p. 546.
REFERENCES
- 1.Cubbin C , Smith GS. Socioeconomic inequalities in injury: critical issues in design and analysis. Annu Rev Public Health. 2002;23(1):349–375. 10.1146/annurev.publhealth.23.100901.140548 [DOI] [PubMed] [Google Scholar]
- 2. Fung L , Conderino S. Pedestrian fatalities in New York City. New York City Dept of Health and Mental Hygiene. 2017. . Available at: https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief86.pdf . Accessed December 22, 2022.
- 3.Kruithof N , de Jongh MAC , de Munter L , Lansink KWW , Polinder S. The effect of socio-economic status on non-fatal outcome after injury: a systematic review. Injury. 2017;48(3):578–590. 10.1016/j.injury.2017.01.013 [DOI] [PubMed] [Google Scholar]
- 4.Morency P , Gauvin L , Plante C , Fournier M , Morency C. Neighborhood social inequalities in road traffic injuries: the influence of traffic volume and road design. Am J Public Health. 2012;102(6):1112–1119. 10.2105/AJPH.2011.300528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raifman MA , Choma EF. Disparities in activity and traffic fatalities by race/ethnicity. Am J Prev Med. 2022;63(2):160–167. 10.1016/j.amepre.2022.03.012 [DOI] [PubMed] [Google Scholar]
- 6. City of New York . Vision Zero initiatives. 2022. . Available at: https://www.nyc.gov/content/visionzero/pages/vision-zero-scorecard . Accessed December 16, 2022.
- 7.Kim E , Muennig P , Rosen Z. Vision Zero: a toolkit for road safety in the modern era. Inj Epidemiol. 2017;4(1):1. 10.1186/s40621-016-0098-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evenson KR , LaJeunesse S , Heiny S. Awareness of Vision Zero among United States’ road safety professionals. Inj Epidemiol. 2018;5(1):21. 10.1186/s40621-018-0151-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Staples JA , Yuan Y , Meddings L , Brubacher JR. Are we there yet? The American journey to safer city streets. Am J Public Health. 2021;111(9): 1586–1588. 10.2105/AJPH.2021.306405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Susaneck AP. American road deaths show an alarming racial gap. New York Times. April 26, 2023. . Available at: https://www.nytimes.com/interactive/2023/04/26/opinion/road-deaths-racial-gap.html . Accessed May 8, 2023.
- 11.Bunn F , Collier T , Frost C , Ker K , Roberts I , Wentz R. Area-wide traffic calming for preventing traffic related injuries. Cochrane Database Syst Rev. 2003; 2003(1):CD003110. 10.1002/14651858.CD003110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Retting RA , Ferguson SA , McCartt AT. A review of evidence-based traffic engineering measures designed to reduce pedestrian–motor vehicle crashes. Am J Public Health. 2003;93(9):1456–1463. 10.2105/AJPH.93.9.1456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tester JM , Rutherford GW , Wald Z , Rutherford MW. A matched case–control study evaluating the effectiveness of speed humps in reducing child pedestrian injuries. Am J Public Health. 2004;94(4):646–650. 10.2105/AJPH.94.4.646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mountain LJ , Hirst WM , Maher MJ. Are speed enforcement cameras more effective than other speed management measures? The impact of speed management schemes on 30 mph roads. Accid Anal Prev. 2005;37(4):742–754. 10.1016/j.aap.2005.03.017 [DOI] [PubMed] [Google Scholar]
- 15.Zegeer CV , Opiela KS , Cynecki MJ. Effect of pedestrian signals and signal timing on pedestrian accidents. Transp Res Rec. 1982;(847):62–72. [Google Scholar]
- 16. Nelson L. Pedestrian deaths in LA rise sharply but officials remain committed to traffic safety program. Los Angeles Times. March 1, 2018. . Available at: https://www.latimes.com/local/lanow/la-me-ln-vision-zero-20180228-story.html . Accessed January 16, 2023.
- 17. The Globe and Mail Editorial Board . 11. Globe editorial: Toronto’s road safety program, Vision Zero, is a failure. The Globe and Mail. June 13, 2018. . Available at: https://www.theglobeandmail.com/opinion/editorials/article-globe-editorial-torontos-road-safety-program-vision-zero-is-a . Accessed January 16, 2023.
- 18. Leber J. US cities want to totally end traffic deaths—but there have been a few speed bumps. Fast Company. August 2017. . Available at: https://www.fastcompany.com/3062492/us-cities-want-to-totally-end-traffic-deaths-but-there-have-been-a-few-speed-bumps . Accessed January 16, 2023.
- 19. Vision Zero Task Force . Vision Zero year 5 report. City of New York. 2019. . Available at: https://www1.nyc.gov/assets/visionzero/downloads/pdf/vision-zero-year-5-report.pdf . Accessed May 1, 2023.
- 20. Fitzsimmons EG. Traffic deaths in New York City drop to 200, a record low. New York Times. January 1, 2019. . Available at: https://www.nytimes.com/2019/01/01/nyregion/traffic-deaths-decrease-nyc.html . Accessed January 16, 2023.
- 21. US Government Accountability Office . During COVID-19, road fatalities increased and transit ridership dipped. GAO Blog. January 25, 2022. . Available at: https://www.gao.gov/blog/during-covid-19-road-fatalities-increased-and-transit-ridership-dipped . Accessed May 23, 2023.
- 22. Guse C. NYPD tickets to dangerous drivers down by nearly half from prepandemic year. New York Daily News. August 6, 2022. . Available at: https://www.nydailynews.com/new-york/ny-nypd-moving-motor-vehicle-violation-tickets-down-vision-zero-20220807-2pkrnnnt7fhmjdvntak3z74q3a-story.html . Accessed May 23, 2023.
- 23. Zipper D. Why “Vision Zero” hit a wall. Bloomberg.com. April 11, 2022. . Available at: https://www.bloomberg.com/news/features/2022-04-11/-vision-zero-at-a-crossroads-as-u-s-traffic-death-rise . Accessed January 16, 2023.
- 24. Armlovich A. Poverty and progress in New York XI: Vision Zero and traffic safety. The Manhattan Institute. 2017. . Available at: https://media4.manhattan-institute.org/sites/default/files/IB-AA-0517-v2.pdf . Accessed May 1, 2023.
- 25. Centers for Disease Control and Prevention . Motor vehicle crash injuries: costly but preventable. 2014. . Available at: https://www.cdc.gov/vitalsigns/pdf/2014-10-vitalsigns.pdf . Accessed May 1, 2023.
- 26.Mammen K , Shim HS , Weber BS. Vision Zero: speed limit reduction and traffic injury prevention in New York City. East Econ J. 2020;46(2): 282–300. 10.1057/s41302-019-00160-5 [DOI] [Google Scholar]
- 27.Ferdinand AO , Menachemi N , Blackburn JL , Sen B , Nelson L , Morrisey M. The impact of texting bans on motor vehicle crash–related hospitalizations. Am J Public Health. 2015;105(5):859–865. 10.2105/AJPH.2014.302537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wing C , Simon K , Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39(1):453–469. 10.1146/annurev-publhealth-040617-013507 [DOI] [PubMed] [Google Scholar]
- 29.Burdett BRD , Starkey NJ , Charlton SG. The close to home effect in road crashes. Saf Sci. 2017; 98:1–8. 10.1016/j.ssci.2017.04.009 [DOI] [Google Scholar]
- 30.Cottrill CD , Thakuriah P. Evaluating pedestrian crashes in areas with high low-income or minority populations. Accid Anal Prev. 2010;42(6): 1718–1728. 10.1016/j.aap.2010.04.012 [DOI] [PubMed] [Google Scholar]
- 31. Barrios J , Hochberg YV , Yi H. The cost of convenience: ridehailing and traffic fatalities. Becker Friedman Institute at University of Chicago. 2020. . Available at: https://bfi.uchicago.edu/working-paper/the-cost-of-convenience-ridesharing-and-traffic-fatalities . Accessed January 16, 2023.
- 32. Getman A , Gordon-Koven L , Hostetter S , Viola R. Safer cycling: bicycle ridership and safety in New York City. New York City Dept of Transportation. 2017. . Available at: https://www.nyc.gov/html/dot/downloads/pdf/bike-safety-study-frlandscapeformat2017.pdf . Accessed May 1, 2023.
- 33. New York State Dept of Transportation . Complete streets. 2022. . Available at: https://www.dot.ny.gov/programs/completestreets . Accessed January 17, 2023.
- 34.Conderino S , Fung L , Sedlar S , Norton JM. Linkage of traffic crash and hospitalization records with limited identifiers for enhanced public health surveillance. Accid Anal Prev. 2017;101:117–123. 10.1016/j.aap.2017.02.011 [DOI] [PubMed] [Google Scholar]
- 35. New York State Governor’s Office . Governor Hochul signs new laws to enhance street safety, prevent traffic deaths, and crack down on hit-and-run crashes. August 12, 2022. . Available at: https://www.governor.ny.gov/news/governor-hochul-signs-new-laws-enhance-street-safety-prevent-traffic-deaths-and-crack-down-hit . Accessed January 17, 2023.