Abstract
The purpose of this study was to determine the association between changes in physical activity and changes in body weight in a cluster-randomized weight loss trial conducted in an underserved population in Louisiana. This study reports analyses conducted in the intervention group only, which was a 24-month multi-component weight loss program delivered by health coaches embedded in primary care clinics. Physical activity was assessed at baseline and at 6, 12, and 24 months of follow-up and changes in body weight were expressed as percent weight change from baseline. Among the sample of 402 patients, percent changes in body weight (mean ± SE) across increasing tertiles of changes in walking between baseline and 24 months were −3.2 ± 1.0%, −5.5 ± 0.9%, and −7.3 ± 0.9%, respectively (p = 0.001). Changes in body weight across increasing tertiles of changes in moderate-to-vigorous-intensity activity between baseline and 24 months were −4.3 ± 1.0%, −5.0 ± 0.9%, and −7.0 ± 0.9%, respectively (p = 0.04). In conclusion, this multi-component intervention resulted in clinically significant weight loss, and greater increases in physical activity over the intervention period were associated with greater percent reductions in body weight. These results are consistent with those from other studies conducted primarily in non-underserved populations.
INTRODUCTION
Comprehensive lifestyle interventions are recommended for the treatment and management of obesity [1]. These interventions typically include a strong focus on behavioral strategies that result in changes in dietary intake and physical activity. The 2018 Physical Activity Guidelines Advisory Committee conducted systematic reviews of the scientific literature, and concluded that there was strong evidence for a relationship between greater amounts of physical activity and attenuated weight gain in adults [2]. Furthermore, the American College of Sports Medicine concluded that while moderate-intensity physical activity between 150 and 250 min/week is associated with only modest weight loss, greater amounts of physical activity (≥250 min/week) have been associated with clinically significant weight loss [3]. A recent metaanalysis of 16 randomized controlled trials of primary care initiated physical activity interventions resulted in significant reductions in BMI (−0.21 kg/m2; 95% confidence interval: −0.41 to −0.01) [4].
There is some evidence that physical activity is associated with weight loss within the context of multi-component lifestyle interventions. Participants in the Diabetes Prevention Program intervention had greater weight loss and a greater increase in leisure physical activity than did participants assigned to receive metformin or placebo [5]. The PROACTIVE intervention also reported that reductions in waist circumference were greater among men and women in the highest vs the lowest tertiles of change in physical activity [6]. However, the degree to which weight loss is associated with physical activity within the context of multi-component behavioral interventions delivered in primary care settings is not well understood. In addition, there is a lack of data on the effects of physical activity on health outcomes among underserved populations [2]. Thus, the purpose of this study was to determine the association between changes in physical activity and changes in body weight in a pragmatic weight loss trial conducted in an underserved population.
METHODS
This study reports secondary analyses from the Promoting Successful Weight Loss in Primary Care in Louisiana (PROPEL) trial [7, 8]. PROPEL was a cluster-randomized trial conducted in 18 primary care clinics serving primarily low-income patients in Louisiana (ClinicalTrials.gov, NCT02561221). The clinics were randomized to an intensive lifestyle intervention (ILI) or usual care. The primary inclusion criteria included age 20–75 years and BMI 30–50 kg/m2. The full list of inclusion and exclusion criteria have been reported previously [7]. This study reports analyses conducted in the ILI group only. The Institutional Review Board at Pennington Biomedical Research Center approved the protocol and all patients provided informed consent.
The intensive lifestyle intervention
The ILI was a multi-component program delivered by health coaches embedded in primary care clinics. Patients in the ILI attended weekly sessions (16 in-person and 6 telephone) in the first 6 months, followed by in-person and telephone sessions held at least monthly for the remainder of the trial [7]. Patients in the ILI were also provided an electronic scale and were encouraged to weigh themselves daily. Patients worked with coaches to develop action plans for eating and physical activity to reach a weight loss goal of 10% in the first 6 months, followed by weight maintenance. Within the context of the behavioral intervention, patients were counseled to undertake at least 175 min per week of moderate-to-vigorous physical activity. A major focus of the intervention was on increasing lifestyle activities, such as taking the stairs instead of the elevator, parking further away, actively commuting (walking or riding bicycle), and replacing sedentary behaviors with more active options.
Assessment of physical activity
Physical activity was assessed at baseline and at 6, 12, and 24 months of follow-up using the International Physical Activity Questionnaire – Short Form (IPAQ-SF). The IPAQ-SF has acceptable reliability [9] and has been shown to be sensitive to change within the context of a weight loss intervention [10]. For the current analysis, we used estimates of time spent walking (min/day) and time (min/day) in moderate-intensity physical activity (MPA), vigorous-intensity physical activity (VPA), and moderate-tovigorous physical activity (MVPA).
Changes in body weight
Body weight was measured with a digital scale to the nearest 0.1 kg at inclinic visits at baseline and at 6, 12, and 24 months of follow-up. Changes in body weight were expressed as percent weight change from baseline.
Statistical analysis
Changes in the physical activity variables from baseline were computed at each time point. These continuous measures of change were divided into sex-specific tertiles (1 = low, 2 = moderate, and 3 = high) at each time point. To avoid partitioning tie values into different tertiles, we assigned a patient having rank r to the tth tertile where t = ⌊ 1 +r × 3/(n − 1) ⌋ and n was the number of observations having no missing values of ranking variable within the subgroup. Data for men and women were combined after creation of the tertiles. Percent changes in body weight were analyzed for tertile differences at each time point using linear mixed effects multi-level ANOVA models, which included random cluster (clinic) effects and age, race, and sex (in combined analyses) as fixed covariates. Model-based least squares means and differences were estimated. Finally, we also performed subgroup analysis for men and women. All analyses were conducted using SAS version 9.4 (SAS Institute Inc.).
RESULTS
A total of 402 patients (354 women, 48 men) had data available for body weight and physical activity at baseline and at least one other time point. The sample was 73% Black, 32% of patients had low health literacy, and the mean (SD) age and BMI at baseline were 49.8 (12.4) y and 37.2 (4.6) kg/m2, respectively. At baseline, mean levels of walking, MPA, VPA, and MVPA were 33.4 (44.2), 15.6 (28.6), 8.7 (15.5), and 24.4 (36.4) min/day, respectively. Table 1 presents the mean changes in physical activity for each tertile of change in physical activity variables in addition to the corresponding changes in body weight. With the exception of MPA at 24 months and MVPA at 12 months, all associations were statistically significant (p < 0.05), indicating that greater increases in physical activity over the intervention period were associated with greater percent reductions in body weight. While the significant p values indicate significant differences across tertiles, the observed differences were not always strictly linear or stepwise across the groups. Figure 1 presents the results for the association between changes in walking and percent changes in body weight stratified by sex. In both women and men, there are trends for greater reductions in body weight being associated with greater increases in daily walking. While the results are qualitatively similar between men and women, the results were statistically significant in women (all p < 0.04) but not in men (p > 0.05), given the smaller sample size and larger standard errors in men.
Table 1.
Weight changes across changes in physical activity in the PROPEL intensive lifestyle intervention group.
| 6 Months | 12 Months | 24 Months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Changea (min/d) | Weight changeb (%) | N | Changea (min/d) | Weight changeb (%) | N | Changea (min/d) | Weight changeb (%) | |
| Walking | |||||||||
| Low | 100 | −37.6 (−129.9, −1.3) | −6.7 (0.8) | 95 | −48.0 (−130, −1.3) | −5.4 (1.0) | 90 | −44.1 (−130, −4.3) | −3.2 (1.0) |
| Moderate | 100 | 5.1 (−2.1, 17.1) | −7.3 (0.8) | 97 | 4.0 (−2.1, 17.1) | −7.1 (1.0) | 91 | 2.0 (−2.9, 10.7) | −5.5 (0.9) |
| High | 101 | 62.5 (17.1, 129.9) | −8.8 (0.7) | 93 | 60.9 (14.3, 130) | −8.1 (1.0) | 92 | 47.7 (10, 130) | −7.3 (0.9) |
| P | 0.017 | 0.02 | 0.001 | ||||||
| MPA | |||||||||
| Low | 79 | −34.8 (−107.1, −0.7) | −7.5 (0.8) | 72 | −34.0 (−107, −0.7) | −6.0 (1.0) | 85 | −38.3 (−107, −1.1) | −4.8 (1.0) |
| Moderate | 147 | 1.4 (0, 17.1) | −6.4 (0.7) | 145 | 0.8 (0, 11.4) | −6.3 (0.8) | 127 | 0.7 (0, 25.7) | −4.8 (0.9) |
| High | 113 | 43.0 (8.6, 107.1) | −8.7 (0.7) | 112 | 44.5 (8.6, 107) | −8.4 (0.9) | 106 | 41.6 (4.3, 107) | −6.5 (0.9) |
| P | 0.003 | 0.02 | 0.17 | ||||||
| VPA | |||||||||
| Low | 59 | −18.2 (−53.6, −2.1) | −7.8 (0.9) | 68 | −19.7 (−53.6, −1.4) | −6.3 (1.0) | 65 | −19.3 (−53.6, −1.4) | −4.2 (1.1) |
| Moderate | 181 | 0.3 (0, 8.6) | −6.9 (0.7) | 162 | 0.1 (0, 0) | −6.5 (0.8) | 170 | 0.0 (0, 0) | −5.1 (0.8) |
| High | 119 | 25.6 (5.7, 53.6) | −8.8 (0.7) | 115 | 25.6 (1.4, 53.6) | −8.7 (0.9) | 100 | 22.6 (1.4, 53.6) | −7.6 (0.9) |
| P | 0.01 | 0.01 | 0.006 | ||||||
| MVPA | |||||||||
| Low | 87 | −34.1 (−107, 0) | −7.4 (0.8) | 84 | −34.5 (−110, 0) | −6.1 (1.0) | 96 | −39.9 (−130, 1.4) | −4.3 (1.0) |
| Moderate | 135 | 4.3 (0, 34.3) | −6.5 (0.7) | 129 | 3.2 (0, 30) | −6.6 (0.8) | 112 | 1.8 (0, 34.3) | −5.0 (0.9) |
| High | 109 | 58.8 (17.1, 161) | −9.0 (0.7) | 108 | 61.6 (17.1, 161) | −8.1 (0.9) | 104 | 55.1 (7.1, 161) | −7.0 (0.9) |
| P | 0.001 | 0.09 | 0.04 | ||||||
Low, moderate and high represent tertiles of change in physical activity.
MPA moderate-intensity physical activity, VPA vigorous-intensityphysical activity, MVPA moderate-to-vigorous physical activity.
Change from baseline in physical activity [mean (range)]; note that the ranges overlap across some tertiles given that sex-specific tertiles were computed and combined for presentation.
Percent change from baseline in body weight [mean (SE)].
Fig. 1. Weight change from baseline in men and women across tertiles of change in daily walking.
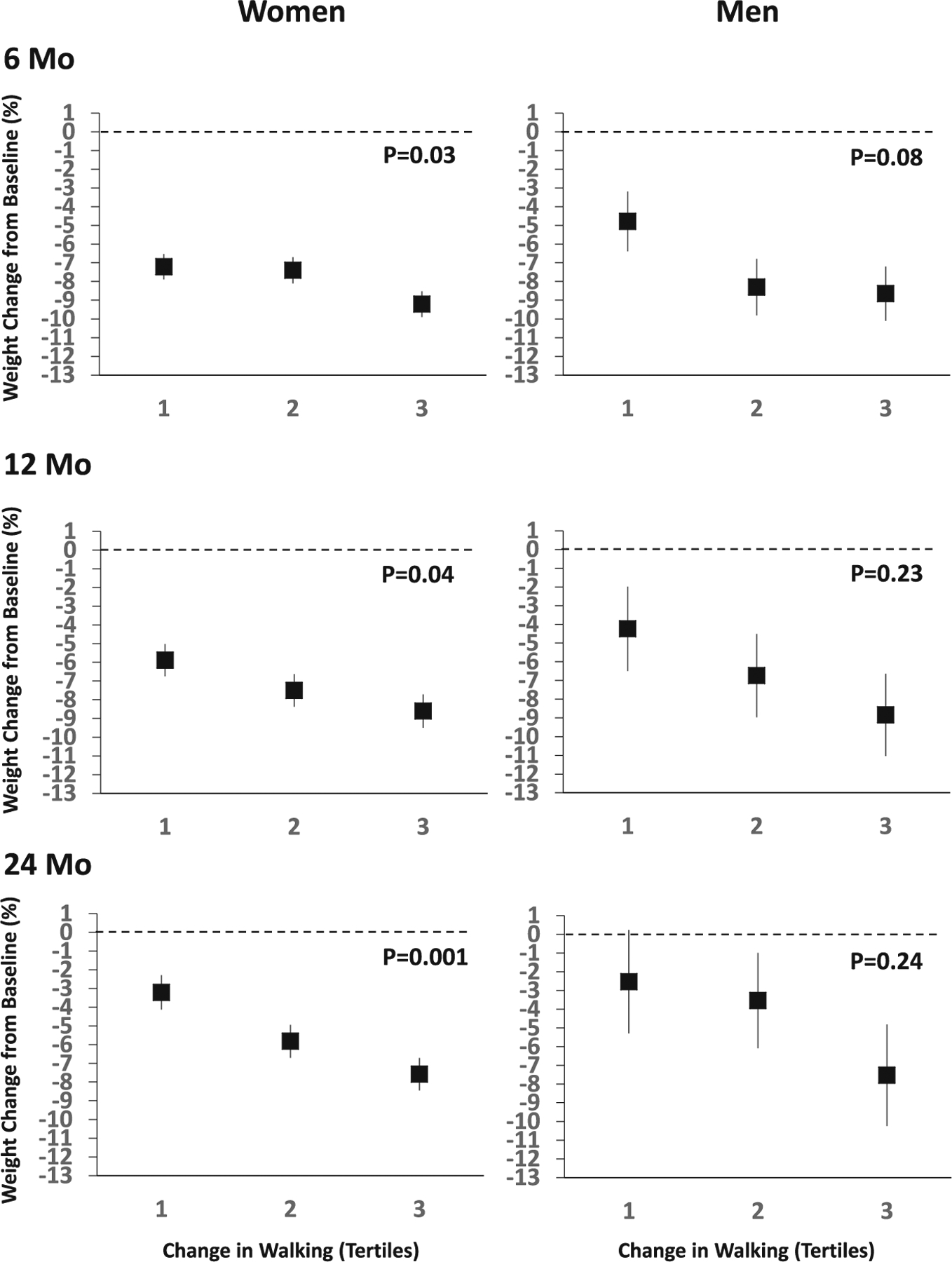
The sample included 354 women and 48 men. Estimates are adjusted for age and race, and error bars represent standard errors. The dotted lines represent zero weight change over the 24 months. The P values are for the comparison of weight loss across the three tertiles at each time point.
DISCUSSION
The results demonstrate an association between greater increases in physical activity and greater percent reductions in body weight within the context of a multi-component, behavioral intervention for obesity. While clinically significant weight loss was observed across all tertiles of change in physical activity, those that increased physical activity experienced greater weight loss. Exercise has been shown to induce weight loss within the context of randomized controlled trials where the focus has been on increasing physical activity as the primary intervention target [4, 11–13]. Our results provide evidence that physical activity may also be important within the context of multi-component lifestyle interventions delivered in underserved populations. In support of this contention, data from the PROACTIVE intervention showed the reduction in waist circumference was greater in the highest vs the lowest tertiles of change in physical activity over 24 months [6]. Our results also support those from a post-hoc analysis of data from the Step-up randomized trial, which showed that moderate-to-vigorous physical activity performed in bouts of at least 10 min was positively associated with achieving ≥10% weight loss at 18 months [14]. Similarly, the strongest correlate of 1-year weight loss in the Look AHEAD trial was greater physical activity [15], and participants who maintained ≥10% weight loss at years 1 and 4 of the intervention also had significantly higher levels of moderate-to-vigorous physical activity at years 1 and 4 [16].
The results of this study should be considered within the context of its limitations. The PROPEL trial was not designed to empirically examine the association between changes in physical activity and changes in body weight; thus, the study should be considered observational. Within that context, the observed associations do not necessarily represent independent effects; i.e., patients may have been performing different combinations of moderate and vigorous activity to enhance their weight loss experience. The IPAQ-SF does not provide estimates of physical activity in different domains (i.e., household, transportation, occupational, leisure-time), which could be important factors to consider. Finally, the majority (88%) of the participants were women; thus, the results reported for men should be interpreted with caution.
In conclusion, the PROPEL multi-component intervention resulted in clinically significant weight loss, and greater increases in physical activity were associated with greater reductions in body weight. These findings are consistent with those from studies conducted primarily in non-underserved populations, and the results should be confirmed using randomized trials designed to address the role of physical activity and weight loss within the context of multi-component behavioral interventions.
FUNDING
Supported by an award (OB-1402-10977) from PCORI, by a grant (U54 GM104940) from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center, and by a grant (“Nutrition and Metabolic Health through the Lifespan” [P30DK072476]) from the Nutrition and Obesity Research Center, sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
COMPETING INTERESTS
The intellectual property surrounding the mathematical code that creates the weight graph used in this study is owned by Louisiana State University/Pennington Biomedical and Montclair State University. CKM is an inventor of the IP, which is included in a US and European patent application. The code has also been licensed and Louisiana State University/Pennington Biomedical, Montclair State University, and CKM have received royalties. The other authors declare no competing interests.
DATA AVAILABILITY
The data generated and/or analyzed during the study are available from the corresponding author on reasonable request.
REFERENCES
- 1.Jensen MD, Ryan DH. New obesity guidelines: promise and potential. JAMA. 2014;311:23–4. [DOI] [PubMed] [Google Scholar]
- 2.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services; 2018. 779 p. [Google Scholar]
- 3.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459–71. [DOI] [PubMed] [Google Scholar]
- 4.Goryakin Y, Suhlrie L, Cecchini M. Impact of primary care-initiated interventions promoting physical activity on body mass index: systematic review and metaanalysis. Obes Rev. 2018;19:518–28. [DOI] [PubMed] [Google Scholar]
- 5.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross R, Lam M, Blair SN, Church TS, Godwin M, Hotz SB, et al. Trial of prevention and reduction of obesity through active living in clinical settings: a randomized controlled trial. Arch Intern Med. 2012;172:414–24. [DOI] [PubMed] [Google Scholar]
- 7.Katzmarzyk PT, Martin CK, Newton RL Jr., Apolzan JW, Arnold CL, Davis TC, et al. Promoting successful weight loss in primary care in Louisiana (PROPEL): rationale, design and baseline characteristics. Contemp Clin Trials. 2018;67:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katzmarzyk PT, Martin CK, Newton RL Jr., Apolzan JW, Arnold CL, Davis TC, et al. Weight loss in underserved patients - a cluster-randomized trial. N Engl J Med. 2020;383:909–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. [DOI] [PubMed] [Google Scholar]
- 10.Fuller NR, Williams K, Shrestha R, Ahern AL, Holzapfel C, Hauner H. et al. Changes in physical activity during a weight loss intervention and follow-up: a randomized controlled trial. Clin Obes. 2014;4:127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA. 1999;282:1554–60. [DOI] [PubMed] [Google Scholar]
- 12.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women: a randomized trial. JAMA. 2003;290:1323–30. [DOI] [PubMed] [Google Scholar]
- 13.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med. 2008;168:1550–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakicic JM, Tate DF, Lang W, Davis KK, Polzien K, Neiberg RH, et al. Objective physical activity and weight loss in adults: the step-up randomized clinical trial. Obesity. 2014;22:2284–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wadden TA, West DS, Neiberg RH, Wing RR, Ryan DH, Johnson KC, et al. One-year weight losses in the Look AHEAD study: factors associated with success. Obesity. 2009;17:713–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Unick JL, Gaussoin SA, Hill JO, Jakicic JM, Bond DS, Hellgren M, et al. Objectively assessed physical activity and weight loss maintenance among individuals enrolled in a lifestyle intervention. Obesity. 2017;25:1903–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated and/or analyzed during the study are available from the corresponding author on reasonable request.


