Abstract
Background
Post-operative pain is a major factor in surgical recovery. There is evidence that pain remains undermanaged. Complications related to the undermanagement of acute pain can increase length of stay and contribute to readmission and the development of chronic pain. It is well acknowledged that pain assessment is critical to pain management and that self-report of pain is the gold standard. As a result, patients play a central role in their own pain management. A preliminary review of the literature failed to provide a clear or consistent description of this key patient role.
Objective
A scoping review was conducted with the objective of reviewing literature that described adult patients’ perspectives or highlighted the adult patient's role in post-operative pain management, including assessment. Understanding patients’ attitudes toward their roles in pain management through a scoping review of the current literature is critical for informing research and improvements in post-operative pain management.
Design
Scoping review.
Methods
The databases searched for the review included CINAHL, MEDLINE, PubMed, and SCOPUS (ending May 2022). Thematic analysis, using the methodology of Arksey and O'Malley, was applied to the records identified
Results
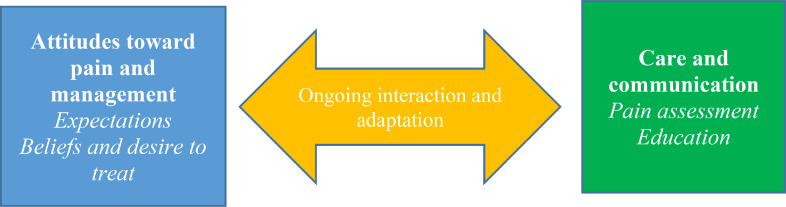
Of the 106 abstracts initially identified, 26 papers were included in the final analysis. Two major themes identified through thematic analysis were attitudes toward pain and pain management, with the subthemes of patient expectations and beliefs and desire to treat; and care and communication, with the subthemes of pain assessment and education.
Conclusions
This paper provides one of the first known comprehensive scoping reviews of surgical patients’ perspectives of their role in pain management, including assessment, and offers an important global awareness of this patient role. The findings suggest that improved understanding of patients’ perspectives of their roles in pain assessment and treatment is critical to improving post-operative pain management. Engaging patients as partners in their care can facilitate enhanced communication and improving congruence in pain assessment and treatment decisions. The complex nature of patients’ beliefs, expectations, and subjective experiences of pain present challenges for health care practitioners. These challenges can be met with enhanced education for patients, respect for patients’ beliefs and expectations, and the provision of dignified care.
Keywords: Acute pain, Chronic pain, Length of stay, Pain management, Pain measurement, Pain, Post-operative, Patient readmission, Self-report
What is already known
-
•
Post-operative pain remains undermanaged.
-
•
Self-report is the gold standard for pain assessment.
-
•
Patients’ perceptions of their roles in pain management are inadequately defined.
What this paper adds
-
•
Patients’ perspectives of their roles in pain management, including assessment, are influenced by their experiences and beliefs.
-
•
Patients and nurses benefit from a mutual understanding of pain management.
-
•
Patient education and nursing care contribute to patients’ overall satisfaction with pain control.
1. Background
Effective pain management has been regarded as a human right (Brennan et al., 2007; Tawil et al., 2018). Post-operative pain is one of the most common causes of pain (O'Donnell, 2018), with more than 80% of post-operative patients experiencing some degree of pain (Meissner et al., 2018) and up to 75% reporting moderate to severe intensity of pain (Gan et al., 2014b). It is widely acknowledged that undermanaged post-operative pain can lead to complications, such as decreased lung function, sleep disturbances, infection, delayed mobility, myocardial infarction, and increased morbidity and mortality (Bach et al., 2018; Eshete et al., 2019; Tawil et al., 2018). These pain-related complications can contribute to increased lengths of stay in the post-operative period and readmissions to hospital post-discharge (Belay Bizuneh et al., 2020; Ouellette et al., 2019).
Despite advances in anaesthetic approaches and pharmacological and adjunctive treatments, patients still experience unacceptably high levels of post-operative pain around the world (Gan et al., 2014a; Rawal, 2016; Scher et al., 2018; Wooldridge and Branney, 2020). Growing evidence has established a connection between high levels of acute post-operative pain and the development of persistent postoperative pain, considered a type of chronic pain (Baratta et al., 2014; Bokhari et al., 2012; Chapman et al., 2011). Therefore, management of acute pain in the post-operative period is of paramount importance to reduce the development of other complications, including chronic pain, and to improve post-operative patient outcomes (Gan, 2017).
It has been widely acknowledged that a foundational step in providing adequate pain management is to use a standardized and accurate pain assessment strategy (Wooldridge and Branney, 2020). This crucial first step in pain management has been explored in the literature, often independently of the treatment phase (Gélinas et al., 2021; Hirsh et al., 2009; Topham and Drew, 2017). This method of systematically gathering information has been variable in both experience and application by practitioners.
Patients’ self-reports of pain remain the gold standard for pain assessment (Van Dijk et al., 2012). Patients are expected to report their pain according to their own complex and subjective experiences of pain. Numerous validated pain assessment tools have been identified in the literature. These tools were developed with the goal of facilitating communication between patients and health care providers (Birkedal et al., 2021; Rijkenberg et al., 2017; Tong et al., 2018). The intent of pain assessment is to enable accurate documentation of pain and effective treatment choices by practitioners (Lapkin et al., 2021). While many health care professionals may play a role in pain assessment, nurses are the most frequent health care providers involved in pain assessment, based on their professional role and the time they spend providing patient care (Lauzon Clabo, 2008).
Patients’ involvement in care has been recognized as critical to improving outcomes and maximizing health care resources (Blumenthal-Barby, 2017; Mazer et al., 2020). In addition, understanding patients’ perspectives of pain management, including pain assessment, is crucial to maximizing the application of assessment tools and the effectiveness of treatment strategies (Kuperberg and Grubbs, 1997). Despite this, a preliminary review of the literature revealed a dearth of papers that examined the patients’ perspectives on their role in pain management. While it is acknowledged that post-operative pain is a factor across the spectrum of human development, the intent of this review was to explore the adult patient role. Therefore, the aim of this review was to assess current knowledge in the existing literature about adult patients’ perspectives of their role in post-operative pain management.
2. Methods
A scoping review is indicated when there is a substantive amount of information that is not homogenous and is very complex, as a precursor to a systematic review, or when there are barriers to conducting a systematic review (Duhn et al., 2020). The intent of a scoping review is to develop an understanding of the scope and depth of the available literature in order to identify gaps for future research (Arksey and O'Malley, 2005). Given the diverse state of the literature regarding patients’ perspectives of their role in pain management and the general aims of this study, the scoping review was an appropriate methodological approach for this research.
2.1. Search strategy
A structured search was conducted using the following databases: Cumulative Index of Nursing and Allied Heath Literature (CINAHL), Medline Complete, PubMed Complementary Index, and SCOPUS. The specific search terms used were: (surgery patient OR surgical patient) AND (attitude OR perspective OR belief OR patient role) AND (post-operative OR post-surgical) pain assessment AND management). The following filters were applied: adult population, English language, peer-reviewed, and published between January 2012 and May 2022. This time frame was selected to allow a broad search for seminal studies while ensuring the inclusion of more recent advancements and developments. The structured literature search yielded a total of 106 articles. After removing duplicates, 81 articles were screened for inclusion, and 51 of these articles were selected for manual review. Manual review was conducted and decisions for exclusion were made by the first author (LW), as part of the fulfillment of her master's thesis. Exclusion criteria were as follows: not pertaining to adult patients, not pertaining to post-operative pain, or not focused on patients’ perspectives of pain assessment or management. A total of 26 articles were identified (LW) and confirmed (DM) for inclusion. A variety of types of studies were accepted. In keeping with the methods of other scoping reviews, the quality of the studies was not assessed (Arksey and O'Malley, 2005; Fig. 1).
Fig. 1.
PRISMA-Sc-R flow diagram (Haddaway et al., 2022).
2.2. Data abstraction and collation
Arksey and O'Malley (2005) identified an “analytical descriptive” method of analysis, which involves reviewing articles for critical information, such as authors, country of study, aim, surgery type studied, methods, and results, and situating this information into a table to further scrutinize their ability to meet the aims of the scoping review. Articles were subjected to further review and were grouped thematically. The primary author (LW) completed the initial thematic analysis to identify patterns and trends, with subsequent validation by the second author (DM), who was the primary author's academic advisor. Proposed themes were reviewed and confirmed by the remaining authors (RA and ED).
3. Results
3.1. Study characteristics
Of the 26 articles included in the final review, 10 were qualitative (most of which employed a phenomenological approach), 10 were quantitative (most of which utilized a variety of questionnaires), four were mixed methods, and two were secondary analyses of existing data. Qualitative studies were well represented in the methodology of the included papers, which resonated with the goal of this research. The qualitative studies were focused on hearing patients’ voices and acknowledging their perspectives, attitudes, and roles. Multiple types of surgery were represented in the literature, with a focus on orthopaedic, general, spine, and cardiac (Table 1). The included literature was published between 2013 and 2021 and incorporated diverse global representations of countries with higher and lower levels of resources (Table 2).
Table 1.
Surgical focus of included literature: number of studies.
| Orthopaedic surgery | general surgery | obstetric surgery | cardiac surgery | neuro-surgery | urological surgery | mixed or not defined surgery | spine surgery | recon-structive surgery |
|---|---|---|---|---|---|---|---|---|
| 6 | 6 | 3 | 3 | 1 | 1 | 8 | 2 | 1 |
Table 2.
Summary of included studies and their core aspects related to patients’ perspectives of their role in pain management.
| Study, Country/Area | Aim of study | Population, Sample | Methods | Analysis/outcome measures | Core aspects related to patients’ perspectives of their role in pain management |
|---|---|---|---|---|---|
| Accardi-Rivard et al. (2020), USA1 | Describe patients’ pre- and post-operative pain experiences from their perspective | Individuals undergoing spine surgery, N = 14, (8 males, 6 females) |
Telephone interview with open ended questions developed by research team based on literature | Thematic analysis of interviews |
|
| Angelini et al. (2018), Sweden | Explore and describe patients’ experiences of pain and pain management | Individuals undergoing spine surgery, N = 12, (7 males, 5 females) | Focus group with semi structured interviews with patients to explore experiences following spine surgery (within a 5-week post-operative window) | Themes were determined through qualitative content analysis |
|
| Bjornnes et al. (2017), Norway | Examine patients’ pain characteristics and concerns about pain medications | Individuals undergoing cardiac surgery, N = 416, (322 males, 94 females) | Randomized control trial of an educational booklet on post-operative pain control. Telephone survey to complete Brief Pain Inventory |
Primary outcome was worst pain intensity, pain characteristics and medication usage |
|
| Bizuneh et al. (2020), Ethiopia | Assess level of patients’ satisfaction and identify factors that could impact postoperative pain management | Individuals undergoing thoracic, abdominal, genitourinary, and orthopaedic surgery, N = 418, (139 males, 279 females) | Retrospective chart review, interview, and semi-structured patient questionnaire | Patient satisfaction measured on a five-point Likert scale |
|
| Cogan et al. (2014), Canada | Describe the beliefs and attitudes of the cardiac surgery patient regarding pain management (medication) | Individuals undergoing cardiac surgery, N = 379, (250 males, 129 females) | Prospective questionnaire-based: Barriers Questionnaire and Screening Tool for Addiction Risk | Responses to barriers and Screening Tool and Addiction Risk tool were reviewed to determine belief and attitudes regarding addiction and side effect risk associated with pain treatments |
|
| Craig et al. (2015), USA | Understand the connection between pain management and patient satisfaction | Mixed surgical population, surgery not differentiated. N = 31,106, (11,199 males, 19,907 females) | Review of publicly reported patient experience surveys for aspects of satisfaction | Patient satisfaction regarding aspects of care such as degree to which pain was controlled and impact of care provided |
|
| Dagyaran et al. (2021), Denmark | Understand patient satisfaction with the erector spinae block for pain control | Individuals undergoing general surgery, not differentiated. N = 11, (4 males, 7 females) | Phenomenological semi- structured interviews, with thematic analysis | Themes identified from interviews |
|
| Egan et al. (2020), USA | Evaluate perception and experience of pain in patients undergoing mastectomy and reconstruction | Individuals undergoing reconstructive breast surgery. N = 100, (100 females) | A researcher developed prospective survey was administered pre-operatively and post-operatively | Relationship between attitudes to pain control as compared to opioid use |
|
| Erikson et al. (2016), Sweden | Describe patients’ experiences and actions when describing post-operative pain | Individuals undergoing general or orthopaedic surgery. N = 25 (12 males,13 females) | Semi-structured interviews days 1–7 post-operatively | Thematic analysis |
|
| Erikson et al. (2014), Sweden | Describe how patients perceive the use of the numeric rating scale in post-operative pain assessments | Individuals undergoing general and orthopaedic surgery, N = 25, (12 males, 13 females) | Semi-structured interviews on postoperative day 1 and 5 | Thematic analysis |
|
| Foust-Winton et al. (2021), USA | Describe experience of pain management while hospitalized | Individuals undergoing neurosurgery, N = 27, (11 males, 15 females) | Qualitative, descriptive semi-structured interviews | Thematic analysis |
|
| Henningsen et al. (2018), Denmark | Determine patient perspective of the acceptability of nerve blocks for pain control after surgery for ankle fracture | Individuals undergoing orthopaedic (ankle) surgery. N = 13, (4 males, 7 females) | Semi-structured interviews with thematic analysis | Thematic analysis |
|
| Kaptain et al. (2016), Denmark | Explore participation of spine surgery patients in post-operative pain assessment in a recovery unit | Individuals undergoing spine surgery. N = 15, (7 males, 8 females) | Semi -structured interviews with phenomenological analysis | Thematic analysis |
|
| Komann et al. (2021), European Union | Examine the indicator “desire to receive more pain treatment” in relation to pain intensity and quality of pain treatment programs | Mixed surgery population not differentiated. N = 79,996, (34,790 males, 45,206 females) | Secondary analysis of data from the Quality in Pain Service registry | Examination of the outcome “desire to receive more treatment” in relation to pain intensity |
|
| McTier et al. (2014), Australia | Explore patient participation in pain management during hospitalization | Individuals undergoing cardiac surgery, N = 98, (64 males, 34 females) | Pre-operative interview and post discharge interview as well as focus groups for nursing staff and naturalistic observations of pain assessment | Examination of patient outcomes such as intent to report pain, knowledge of treatments |
|
| Milosevic et al. (2021), United Kingdom | Determine if nerve catheter was an acceptable treatment of post-operative pain | Individuals undergoing orthopaedic (amputation) surgery, N = 14, (10 males, 4 females) | Qualitative interview with patients who received local anaesthetic through the catheter and those who received placebo | Acceptability of the pain management modality and the reasons for this indication |
|
| Mutiba et al. (2020), United Kingdom | Describe patient expectations related to pain and explore the meaning of satisfaction with pain management | Individuals undergoing general surgery, not differentiated. N = 10, (6 males, 4 females) | Semi-structured interviews exploring satisfaction with pain management | Thematically coded |
|
| Pius et al. (2020), USA | Describe the patient experience with pain control after discharge | Mixed surgery, population not differentiated. N = 1027, (441 males, 586 females) | Researcher developed questionnaire administered via telephone completed 1 week after discharge | Satisfaction scores and thematic coding to augment understanding of responses regarding pain control, satisfaction with pain control and satisfaction with prescription |
|
| Ramia et al. (2017), Lebanon | Describe patients’ perception toward pain management and determine overall satisfaction | Individuals undergoing orthopaedic or obstetrical surgery. Orthopaedic N = 177, (85 males, 92 females), Obstetric N = 119 (119 females) |
Two questionnaires developed for each surgical population to explore pain management perceptions. Questionnaires were tested in a pilot study before use in this study to ensure validity and clarity of the questions. | Satisfaction with pain treatment and assess patients pain intensity |
|
| Schwenkglenks et al. (2014), European Union | Improve understanding of factors influencing patient satisfaction with pain management | Mixed surgery population not differentiated. Records pulled from PAIN—OUT registry N = 18,009, (9178 males, 8831 females) |
Secondary analysis of data from PAIN—OUT registry to determine patient satisfaction. This registry uses the self- reported International Pain Outcome Questionnaire | Patient-reported satisfaction and influencing factors such as: interference with sleep and adverse effects of pain treatment |
|
| Tamer et al. (2020), Turkey | Investigate the Turkish surgical patients’ surgical experience | Individuals undergoing orthopaedic, urological, neurosurgical, or general surgery, N = 141, (79 males, 62 females) | Face to face completion of the Strategic and Clinical Quality Indicators Post-operative Pain Questionnaire | Pain intensity and patient related outcomes of pain management |
|
| Tawil et al. (2018), Lebanon | Evaluate patient satisfaction with pain management and identify barriers | Individuals undergoing obstetrical, gynaecological, orthopaedic or cardiac surgery, N = 183, (74 males, 109 females) | Face to face completion of a questionnaire developed by the researcher as a modification to the American Pain Society Outcomes Questionnaire and Barriers Questionnaire, and Numeric Rating Scale | Patient satisfaction and patient related outcomes such as pain intensity and pain interference |
|
| Van Boekel et al. (2017), Netherlands | Examine the relationship between the Numeric Rating Scale and other methods of assessment and acceptability of levels of intensity as compared to functional impact | Surgical population not differentiated. N = 9082, (4995 males, 4087 females) |
Comparing the acceptability of movement evoked Numeric Rating Scale and activity | Pain intensity and ability to complete activities necessary for post-operative recovery |
|
| Van Dijk et al. (2015), Netherlands | Describe the relationship between pain intensity and the patients desire for opioids | Surgical population not differentiated. N = 1084, (560 males, 524 females) | Pain intensity was assessed via Numeric Rating Scale, and patients were asked if they desired opioids | Numeric Rating Scale values and statements of desire for opioids or more opioids |
|
| Vu et al. (2021), Vietnam | Examine patient participation in pain management and its impact on the pain experience | Individuals undergoing otorhinolaryngological, oncological, trauma, orthopaedic, plastic, neurological, spine or general surgery. N = 245, (128 males, 117 females) |
Hospital based survey and interview | Satisfaction and themes from interview |
|
| Zoega et al. (2014), Iceland | Assess pain in hospitalized patients, their participation in pain management, and their satisfaction with care | Individuals undergoing urological, cardiac, vascular, plastic, orthopaedic or general surgery. N = 308, (152 males, 155 females) | Numeric Rating Scale and American Pain Society Outcome Questionnaire -Revised | Satisfaction and Numeric Rating Scores |
|
United States of America.
3.2. Synthesis of results
Of the 26 articles included in the final scoping review, only one paper explicitly used the term ‘patient role’. However, this study focused on the extent to which patients desired to be active in their pain control and did not explore the definition of the role nor the factors that influenced role development (McTier et al., 2014). Additionally, 25 articles offered implicit data on the patient's role. Measures of patient participation and patient satisfaction were the dominant outcome metrics reported in the reviewed studies. Core aspects of the literature that met the study aim are summarized in Table 2.
Summary of Articles
3.3. Thematic analysis
Despite the explicit gap in the reviewed literature in providing clearly defined patient pain roles, two main themes and four subthemes related to patients’ perspectives of their role in pain assessment and management emerged from the data: (1) Attitudes toward pain and pain management (subthemes: Patient expectations and Beliefs and desire to treat); and (2) Care and communication (subthemes: Pain assessment and Education). Findings from the thematic analysis of the literature are presented with respect to the identified themes and subthemes (See Fig. 2).
Fig. 2.
Interaction of themes identified related to patient perspectives.
3.4. Major theme: attitudes toward pain and pain management
A key theme that emerged from the data was related to patients’ attitudes toward pain and pain management. Attitude has been defined as “cognitive, affective, and behavioural and is a response to a stimulus” (Altmann, 2008, p.150). Direct measurement of attitude is not possible. Attitude can be observed only through an individual's behaviors and actions. Attitudes are influenced by experiences, circumstances, and situations and may be positive or negative, conscious or unconscious. In a similar way to the experience of pain, individuals may choose to display or hide their attitudes toward a given situation and may be unaware of how these attitudes influence their reaction to a specific circumstance (Altmann, 2008).
Aspects of pre-operative preparation, such as wait times for surgery, have been postulated to impact patients’ attitudes toward post-operative pain and its management (Angelini et al., 2018). Patients may experience social isolation while waiting for surgery, due to difficulty managing pain and symptoms, which may negatively impact their attitudes toward post-operative pain management and coping (Angelini et al., 2018). Patients’ beliefs regarding the safety and efficacy of treatment modalities can also influence their attitudes toward pain management (Cogan et al., 2014). The current literature review identified two subthemes associated with patients’ attitudes toward pain and pain management: (a) patient expectations and (b) beliefs and desire to treat.
3.4.1. Subtheme: patient expectations
Prior experience with post-operative pain has been shown to influence future reactions to painful stimuli (Accardi-Ravid et al., 2020; Angelini et al., 2018; Dagyaran et al., 2021; Egan et al., 2020; Henningsen et al., 2018). This association is concerning, as many surgical patients experience under-managed pain (Willingham et al., 2021). In one study of 247 surgical patients, more than half suffered with severe pain on the first post-operative day (Köse Tamer and Sucu Dağ, 2020). Reports of moderate to severe post-operative pain are supported throughout the literature (Öğüt and Sucu Dağ, 2019; Werner and Kongsgaard, 2014; Zoëga, 2017).
High levels of pain in post-operative patients have been reported to contribute to negative expectations and anxiety (Dagyaran et al., 2021; Henningsen et al., 2018; Köse Tamer and Sucu Dağ, 2020). For example, patients who had expectations of high pain intensity or inadequate relief due to prior pain experiences were five times more likely to report increased anxiety when compared to patients whose pain was previously well-managed (Egan et al., 2020). Another study of patients undergoing hemicolectomy surgery found that the expectation of a poor prognosis, in addition to anticipated post-operative pain, produced significant worry amongst patients (Dagyaran et al., 2021). Anxiety related to both realistic and unrealistic expectations could further complicate patients’ pain management. On the other hand, a paradoxical perspective of patients’ expectations and preoperative pain was identified in a study of patients undergoing spine surgery, a type of surgery associated with high levels of debilitating pain (Accardi-Ravid et al., 2020). Many patients undergoing spine surgery had the expectation that the surgery would improve their level of suffering, providing an expectation of relief (Accardi-Ravid et al., 2020; Angelini et al., 2018). This type of positive expectation can serve as justification for patients to proceed with surgery(Angelini et al., 2018).
In addition, research has shown that patients can develop expectations based on the experiences of their friends and family as well as their surgical care team (Accardi-Ravid et al., 2020; Henningsen et al., 2018; Mubita et al., 2020). Therefore, the development of expectations and their impact on patients’ pain experiences is a complex and multifactorial process. There is consensus in the existing literature that patients’ expectations of pain influence their levels of anxiety and quality of recovery. The following section reports the substantial variety of opinions in the literature regarding the impact of patients’ perceptions of pain, level of participation in their own care, and impressions of their overall care.
3.4.2. Subtheme: beliefs and desire to treat
The development of beliefs regarding treatment modalities for post-operative pain is a complex interaction of psychosocial aspects. Beliefs are “convictions based on truth or reality” that arise from a variety of sources and modulate or influence a person's expectations, attitudes, and decisions (Merriam-Webster, 2022). For instance, societal factors are known to contribute to patients’ understandings of the potential risks of opioid use (Pius et al., 2020). Cogan et al. (2014) conducted a study with 379 surgical patients and found that over one-quarter of the patients believed that addiction to pain medication could easily occur and that treatment with pain medication should be reserved for worst case circumstances. These findings highlighted the fact that misconceptions can develop through various mechanisms and serve as barriers to effective pain management (Cogan et al., 2017). Similar findings were noted in several studies that examined patients’ fears of addiction and other perceived opioid-related risks, such as nausea, vomiting, and drowsiness (Angelini et al., 2018; Bjørnnes et al., 2017; Egan et al., 2020; Milosevic et al., 2021; Ramia et al., 2017a; Tawil et al., 2018; van Dijk et al., 2015).
Patients’ beliefs influenced not only their desire for additional pain management, but also affected their perceptions of pain assessment. A study that examined the sociocultural influences of patients’ beliefs found that over 30% of patients expressed that “good people should avoid talking about pain” (Tawil et al., 2018, p.5). This was not a unique finding. In another study, over one-quarter of cardiac patients expressed that the primary reason they did not report pain was to avoid being viewed by care providers as ‘complaining’ (McTier et al., 2014). In addition, some patients expressed a desire to be viewed as having a high pain tolerance (Henningsen et al., 2018). Others indicated they were concerned that reporting a high level of pain on the numeric rating scale could lead clinicians to misperceive their intentions and suspect they were either attention- or medication-seeking (Eriksson et al., 2014).
3.5. Major theme: care and communication
The literature has supported that patients view empathetic delivery of care and good communication as critical factors for successful pain management (Craig et al., 2015; Mubita et al., 2020; Tawil et al., 2018). Nurses have been recognized as the clinicians most frequently involved in pain assessment and management (Eriksson et al., 2014; Kaptain et al., 2017a; McTier et al., 2014). Many of the studies included in this review demonstrated that nurses had a unique ability to establish rapport through communication, even in challenging settings like post-operative care, where patient contact is infrequent and brief (Foust Winton et al., 2021; Kaptain et al., 2017a). A sense of rapport with nurses was linked to feelings of calm and control amongst patients and was noted to influence patients’ overall levels of satisfaction (Angelini et al., 2018; Foust Winton et al., 2021; Kaptain et al., 2017b; Schwenkglenks et al., 2014; Tawil et al., 2018; Vu et al., 2021; Zoëga et al., 2014). The two subthemes that emerged from the major theme of care and communication were: (a) pain assessment and (b) education.
3.5.1. Subtheme: pain assessment
Pain assessment has been widely acknowledged as a crucial and foundational component of pain management (Bruckenthal and Simpson, 2016; Gordon et al., 2016; Wooldridge and Branney, 2020). Validated tools have been developed and widely used to assist patients to self-report pain, which is considered the gold standard methodology for pain assessment (Eriksson et al., 2014; Van Dijk et al., 2012). The Numeric Rating Scale is one of the most frequently used tools in post-operative assessments, as supported by the literature in this review. One study reported that patients found the Numeric Rating Scale challenging to use because of the novel pain sensations they experienced after spine surgery (Kaptain et al., 2017b). This was echoed in an interview-based study in which patients expressed that use of the Numeric Rating Scale was not sufficient to describe their pain; they indicated that more specific questions about the location and type of pain were required to obtain an accurate assessment (Eriksson et al., 2014).
Another study reported that the unidimensional nature of the numeric rating scale may limit its usefulness in guiding clinicians’ treatment decisions (Van Boekel et al., 2017). The study indicated that patients with higher Numeric Rating Scale scores did not always desire intervention and that lower scores were still associated with unacceptable levels of pain for some patients (Van Boekel et al., 2017). Despite inherent challenges with the Numeric Rating Scale, patients expressed that regular pain assessment provided a sense of security and personalized their care; as a result, they had an increased desire to participate in their own care and expressed higher levels of overall satisfaction (Angelini et al., 2018; Kaptain et al., 2017a; Tawil et al., 2018).
Researchers have indicated that interactions with clinicians may influence patient participation (Lindberg and Engström, 2011). One study determined that nurses’ interactions with patients during post-operative care were infrequent, brief, and focused on pain assessment (McTier et al., 2014). The authors explored the extent of desired participation using the Control Preference Scale, which was originally developed to assess individuals’ desired level of control during medical decision making (Degner et al., 1997). McTier et al. (2014) noted that, while nurses were responsible for initiating pain assessment, only 25% of patients independently and proactively sought out opportunities to report their pain to the nurses. As a result, it is critical that nurses encourage patients to actively participate in their own pain management. Patient participation in assessment has been widely accepted by clinicians and patients as a valid means of engagement in pain management, which may provide limitations by not extending to decision making (McTier et al., 2014; van Dijk et al., 2015). Patients have expressed that, while their engagement in pain assessment is attainable and expected, their participation in pain management can be restricted by their lack of knowledge or understanding of medications (McTier et al., 2014).
3.5.2. Subtheme: education
Patient education can significantly influence patients’ expectations, ability, and desire to participate in pain assessment and pain management (McDonall et al., 2020). Several studies have noted that the provision of clear and concise information can provide patients with an enhanced sense of control and reduce their anxiety, therefore contributing to increased participation in and overall satisfaction with pain management (Köse Tamer and Sucu Dağ, 2020; Milosevic et al., 2021; Mubita et al., 2020; Ramia et al., 2017a; Schwenkglenks et al., 2014). It can be challenging to navigate the appropriate timing and method of education for surgical populations (Henningsen et al., 2018).
One study examined the use of educational booklets and discovered that standardized information can be of benefit to patients but must be delivered by coordinated methods to ensure it is reviewed and understood (Bjørnnes et al., 2017). Another study utilized focus groups to examine patients’ perspectives and uncovered that patients viewed information as a “pain killer” (p.467) because it had a calming influence on them and made them feel that their care had been personalized (Angelini et al., 2018). The patients also expressed that having access to more information made them feel more comfortable asking questions about different aspects of pain management (Angelini et al., 2018).
Accardi-Ravid et al. (2020) conducted a qualitative study of spine patients in which many patients reported that increased preoperative information would have been beneficial. The patients noted that they would have felt more prepared for surgery if they had received information about post-operative pain expectations and the potential methods for pain management (Accardi-Ravid et al., 2020). The feeling of being underprepared was noted in another study in which patients were unsure if they had been prescribed appropriate pain medications post-discharge (Pius et al., 2020). Insufficient distribution of information was also identified in a study conducted in Lebanon, where almost one-quarter of patients did not receive satisfactory education about the relationship between self-reporting their pain and effective pain relief (Ramia et al., 2017b). Ramia et al. (2017b) also reported that decreased levels of patient education were associated with lower levels of satisfaction with pain management.
4. Discussion
The findings of this scoping review revealed a dearth of research on the patient's role in pain management, suggesting that this role is not well-elucidated. However, insights regarding patients’ perspectives of this role emerged indirectly from the data in the form of two major themes and four subthemes. The main themes revealed that the patient's role was shaped by their attitudes toward pain and pain management as well as the quality of care and communication they received. On a deeper level, the subthemes demonstrated that patients’ roles were also influenced by their own expectations and beliefs, as well as the type/quality of pain assessment and patient education.
Researchers have established that patients’ prior experiences with pain can influence their future expectations, as well as their desire and ability to take an active role in pain assessment and management (Accardi-Ravid et al., 2020; Dagyaran et al., 2021). The wider literature related to surgical outcomes also demonstrated that patients’ expectations played a critical role in shaping their outcomes, including their return to work after surgery (Hoorntje et al., 2018). In order to optimize patient participation, it is crucial that patients receive education regarding the importance of self-reporting their pain and its impact on pain management, in addition to the importance of having pain well-managed (Kuusniemi and Pöyhiä, 2016; McDonall et al., 2020). This information should be delivered throughout the perioperative period, using a variety of personalized methods (Avallin et al., 2018; Chudyk et al., 2021).
It is important to note that only one study included in this review directly examined the patient's role in pain management (McTier et al., 2014). The researchers did not specifically explore the meaning of the patient's role in the context of pain assessment and management (McTier et al., 2014). As a result, further research is required to gain a better understanding of the patient's role in this context.
Researchers have confirmed that the complexity of patients’ previous personal and vicarious experiences with pain can influence their future expectations of pain (Accardi-Ravid et al., 2020; Dagyaran et al., 2021; Eriksson et al., 2015; Henningsen et al., 2018). As demonstrated in the wider literature, the anticipation of pain can create anxiety and contribute to higher intensity of pain and may also lead to the development of chronic pain (Chang et al., 2021; Terry et al., 2007; Willingham et al., 2021). Research have also examined patients’ beliefs and attitudes toward their experiences of pain and the various methods used for pain relief, all of which contribute to the intricacy of the patients’ role in pain management (Doekhie et al., 2020; Forsberg et al., 2015; Kästner et al., 2021). Several studies have reported on patient engagement and noted that aspects of patients’ expectations and attitudes were found to influence their level of participation in pain management (Blumenthal-Barby, 2017; Davis et al., 2007; Jahandideh et al., 2019). Many patients were found to be misinformed about the risks associated with medications, the importance of self-reporting pain, and the potential complications of intense or unresolved pain (Bjørnnes et al., 2017; Cogan et al., 2014; Komann et al., 2021; Milosevic et al., 2021; Schwenkglenks et al., 2014; van Dijk et al., 2017; Vu et al., 2021). Patients’ ability and desire to participate in their own care and understand their role in pain assessment and management can be negatively affected by unrealistic expectations, high levels of anxiety, and misconceptions or misinformation (Mazer et al., 2020; McTier et al., 2014; Terry et al., 2007; Vu et al., 2021).
This scoping review also identified factors that facilitated patients’ participation and satisfaction with pain management, as well as the overall quality of their pain control. Patient education regarding expected post-operative pain, methods for pain management, the importance of self-reporting, and the benefits of effective pain management were found to facilitate feelings of control, decrease anxiety, improve participation, and enhance overall satisfaction with pain management (Angelini et al., 2018; Bjørnnes et al., 2017; Cogan et al., 2014; Dagyaran et al., 2021; Henningsen et al., 2018; Komann et al., 2021; McTier et al., 2014; Vu et al., 2021). Multiple studies noted that nurses were the clinicians most often involved in delivering pain-related information to patients (Craig et al., 2015; Eriksson et al., 2014; Foust Winton et al., 2021). Despite the typical time constraints and limited patient interaction in the post-operative period, patients reported that nurses used a caring and empathetic approach to promote questions and encourage patient participation (Craig et al., 2015; Mubita et al., 2020; Pius et al., 2020; Ramia et al., 2017b). Patients experienced a sense of reassurance when clinicians conducted thorough pain assessments and when nurses provided high-quality, empathetic care (Angelini et al., 2018; Craig et al., 2015; McTier et al., 2014; Mubita et al., 2020). Patients’ overall sense of reassurance was central to their desire and ability to participate in pain management and influenced subsequent reports of patient satisfaction (Ramia et al., 2017a; Schwenkglenks et al., 2014). Similar findings arose from literature that examined patients’ general satisfaction with hospital care (Magidy et al., 2016; Topham and Drew, 2017). The overall quality of nursing care and the time allotted to nurses to provide care were factors that deeply influenced patients’ perceptions of their post-operative care (Chen et al., 2022; Gishu et al., 2019).
There are inherent challenges associated with using the unidimensional measures of patient participation and patient satisfaction as a means of quantifying patients’ subjective experiences of pain and determining their role in pain management(Gordon, 2015a; Scher et al., 2018). Much of the research included in this scoping review relied on specific indicators, such as desire to receive additional treatment and higher levels of satisfaction. It is possible that, similarly to the limitations of unidimensional pain assessment tools, the context and complexity of patients’ perspectives can be lost through the use of such indicators (Gordon, 2015b; Gordon et al., 2016; Wooldridge and Branney, 2020).
Patients’ desires for more pain treatment, participation, and satisfaction may not be correlated with their experiences of pain and pain management nor with their perceived role in these actions. Measurable and repeatable metrics, such as patient satisfaction, are desirable for research because they allow comparison across settings and populations. In this review, we highlighted a possible area for further research; i.e., studies specifically focused on how patients define their role in this aspect of post-operative care. The primary challenge in this type of research is to select outcome measures that amplify patients’ voices. Research to enhance the patient voice may be improved by utilizing Patient Reported Outcomes (PROMS), which are developed in collaboration with patients (Castro et al., 2016; Rowland et al., 2017).
4.1. Limitations
The articles included in this review examined patients in a wide range of countries who underwent a variety of different surgeries. As a result, the findings of this review have a moderate degree of generalizability with regard to the role of the patient in post-operative pain assessment and management. The inclusion of qualitative and quantitative studies ensured a methodological balance and served to acknowledge the importance of patients’ voices. One limitation of this review is that some papers may have been missed during the search strategy, which focused on mainstream databases and English-language publications. In addition, the Arksey and O'Malley (2005) analytical framework, which served as the basis for this review, recommended that researchers discuss their findings with key stakeholders to enhance their depth of understanding of the results. Due to time and resource constraints, these discussions were not undertaken.
5. Conclusions
This scoping review aimed to determine post-operative patients’ perspectives of their role in pain management, including assessment. The review included a total of 26 papers that did not identify any clearly defined patient role with respect to post-operative pain management. Other findings of this review included: the need for improved patient education about the importance of self-reporting and effectively managing pain; an awareness of the complexity of patients’ pain experiences, which are influenced by their expectations, anxieties, and beliefs about pain; and the fact that nursing care is central to optimizing patients’ participation and satisfaction with pain management. This review also demonstrated the ongoing challenges associated with treating pain and understanding the complexity of the pain experience. Although this review explored many aspects of the pain experience from the patient's perspective, none of the articles included in this review specifically examined the patient's own perceptions or definitions of their role in pain management. This presents an opportunity for future research to build on the insights that emerged from this scoping review.
There are ongoing challenges with adequate post-operative pain control. The rising emphasis on patient-centred care and enhanced patient engagement in the healthcare system demands a shift toward personalized care, where patients can engage as partners in their care and contribute to assessments, treatment discussions, and the development of metrics. For this to be possible, clinicians and patients must develop a mutual understanding of their individual and collective roles in post-operative pain management. Therefore, further investigation into the surgical patient's role in pain management is warranted to narrow this gap in understanding and support optimal pain management for post-operative patients. Together with improved understanding of the patient's perspective, future investigation into the perspective of clinicians regarding post-operative pain management could enhance communication and outcomes.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
None.
Funding sources
University of Manitoba College of Nurses Endowment Fund & University of Manitoba Faculty Research Grant.
References
- Accardi-Ravid M., Eaton L., Meins A., Godfrey D., Gordon D., Lesnik I., Doorenbos A. A qualitative descriptive study of patient experiences of pain before and after spine surgery. Pain Med. 2020;21(3):604–612. doi: 10.1093/pm/pnz090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altmann T.K. Attitude: a concept analysis. Nurs. Forum. 2008;43(3):144–150. doi: 10.1111/j.1744-6198.2008.00106.x. [DOI] [PubMed] [Google Scholar]
- Angelini E., Wijk H., Brisby H., Baranto A. Patients’ experiences of pain have an impact on their pain management attitudes and strategies. Pain Manage. Nurs. 2018;19(5):464–473. doi: 10.1016/j.pmn.2018.02.067. [DOI] [PubMed] [Google Scholar]
- Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Avallin T., Muntlin Athlin Å., Elgaard Sørensen E., Kitson A., Björck M., Jangland E. Person-centred pain management for the patient with acute abdominal pain: an ethnography informed by the Fundamentals of Care framework. J. Adv. Nurs. 2018;74(11):2596–2609. doi: 10.1111/jan.13739. [DOI] [PubMed] [Google Scholar]
- Bach A.M., Forman A., Seibaek L. Postoperative pain management: a bedside perspective. Pain Manage. Nurs. 2018;19(6):608–618. doi: 10.1016/j.pmn.2018.05.005. [DOI] [PubMed] [Google Scholar]
- Baratta J.L., Schwenk E.S., Viscusi E.R. Clinical consequences of inadequate pain relief. Plast. Reconstr. Surg. 2014;134:15S–21S. doi: 10.1097/prs.0000000000000681. [DOI] [PubMed] [Google Scholar]
- Belay Bizuneh Y., Fitiwi Lema G., Yilkal Fentie D., Woldegerima Berhe Y., Enyew Ashagrie H. Assessment of patient's satisfaction and associated factors regarding postoperative pain management at the University of Gondar Compressive Specialized Hospital, Northwest Ethiopia. Pain Res. Manage. 2020;2020 doi: 10.1155/2020/8834807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkedal H.C., Larsen M.H., Steindal S.A., Solberg M.T. Comparison of two behavioural pain scales for the assessment of procedural pain: a systematic review. Nurs. Open. 2021;8(5):2050–2060. doi: 10.1002/nop2.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjørnnes A.K., Parry M., Lie I., Fagerland M.W., Watt-Watson J., Rustøen T., Stubhaug A., Leegaard M. The impact of an educational pain management booklet intervention on postoperative pain control after cardiac surgery. Eur. J. Cardiovasc. Nurs. 2017;16(1):18–27. doi: 10.1177/1474515116631680. [DOI] [PubMed] [Google Scholar]
- Blumenthal-Barby J.S. ‘That's the doctor's job’: overcoming patient reluctance to be involved in medical decision making. Patient Educ. Couns. 2017;100(1):14–17. doi: 10.1016/j.pec.2016.07.010. [DOI] [PubMed] [Google Scholar]
- Bokhari F.N., McMillan D.E., McClement S., Daeninck P.J. Pilot study of a survey to identify the prevalence of and risk factors for chronic neuropathic pain following breast cancer surgery. Oncol. Nurs. Forum. 2012;39(2):141–149. doi: 10.1188/12.ONF.E141-E149. [DOI] [PubMed] [Google Scholar]
- Brennan F., Carr D.B., Cousins M. Pain management: a fundamental human right. Anesth. Analg. 2007;105(1):205–221. doi: 10.1213/01.ane.0000268145.52345.55. [DOI] [PubMed] [Google Scholar]
- Bruckenthal P., Simpson M.H. The role of the perioperative nurse in improving surgical patients’ clinical outcomes and satisfaction: beyond medication. AORN J. 2016;104(6) doi: 10.1016/j.aorn.2016.10.013. [DOI] [PubMed] [Google Scholar]
- Castro E.M., Van Regenmortel T., Vanhaecht K., Sermeus W., Van Hecke A. Patient empowerment, patient participation and patient-centeredness in hospital care: a concept analysis based on a literature review. Patient Educ. Couns. 2016;99(12):1923–1939. doi: 10.1016/j.pec.2016.07.026. [DOI] [PubMed] [Google Scholar]
- Chang W.S., Hsieh Y.T., Chen M.C., Chang S.C., Chen T.S., Chang Y.C., Tsai Y.C., Lam C.F. Characterization of self-anticipated pain score prior to elective surgery - a prospective observational study. BMC Anesthesiol. 2021;21(1):1–9. doi: 10.1186/s12871-021-01303-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman C.R., Davis J., Donaldson G.W., Naylor J., Winchester D. Postoperative pain trajectories in chronic pain patients undergoing surgery: the effects of chronic opioid pharmacotherapy on acute pain. J. Pain. 2011;12(12):1240–1246. doi: 10.1016/j.jpain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- Chen X., Zhang Y., Qin W., Yu Z., Yu J., Lin Y., Li X., Zheng Z., Wang Y. How does overall hospital satisfaction relate to patient experience with nursing care? a cross-sectional study in China. BMJ Open. 2022;12(1):1–9. doi: 10.1136/bmjopen-2021-053899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chudyk, A.M., Ragheb, S., Kent, D., Duhamel, T.A., Hyra, C., Dave, M.G., Arora, R.C., & Schultz, A.S.H. (2021). Patient engagement in the design of a mobile health app that supports enhanced recovery protocols for cardiac surgery: development study corresponding author: 4. https://doi.org/10.2196/26597. [DOI] [PMC free article] [PubMed]
- Cogan J., Ouimette M.F., Vargas-Schaffer G., Yegin Z., Deschamps A., Denault A. Patient attitudes and beliefs regarding pain medication after cardiac surgery: barriers to adequate pain management. Pain Manage. Nurs. 2014;15(3):574–579. doi: 10.1016/j.pmn.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Cogan J., Ouimette M.F., Yegin Z., Ferland V., Vargas G., Lambert J., Rochon A.G., Belisle S. Perioperative pain management barriers in cardiac surgery: should we persevere? Appl. Nurs. Res. 2017;35(May 2013):6–12. doi: 10.1016/j.apnr.2017.02.007. [DOI] [PubMed] [Google Scholar]
- Craig A.R., Otani K., Herrmann P.A. Evaluating the influence of perceived pain control on patient satisfaction in a hospital setting. Hosp. Top. 2015;93(1):1–8. doi: 10.1080/00185868.2015.1012926. [DOI] [PubMed] [Google Scholar]
- Dagyaran Ii.I., Olesen C.M., Brix L.D. Patient-experienced quality during postoperative pain management - a phenomenological-hermeneutic study. J. Perianesth. Nurs. 2021;000:1–7. doi: 10.1016/j.jopan.2021.09.007. [DOI] [PubMed] [Google Scholar]
- Davis R.E., Jacklin R., Sevdalis N., Vincent C.A. Patient involvement in patient safety: what factors influence patient participation and engagement? Health Expect. 2007;10(3):259–267. doi: 10.1111/j.1369-7625.2007.00450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degner L.F., Sloan J.A., Venkatesh P. The control preferences scale. Can. J. Nurs. Res. 1997;29(3):21–43. [PubMed] [Google Scholar]
- Doekhie K.D., Buljac-Samardzic M., Strating M.M.H., Paauwe J. Elderly patients’ decision-making embedded in the social context: a mixed-method analysis of subjective norms and social support. BMC Geriatr. 2020;20(1):1–15. doi: 10.1186/s12877-020-1458-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhn L., Godfrey C., Medves J. Scoping review of patients’ attitudes about their role and behaviours to ensure safe care at the direct care level. Health Expect. 2020;23(5):979–991. doi: 10.1111/hex.13117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan K.G., De Souza M., Allen A.L., Muenks E., Nazir N., Korentager R. Perception of pain and influences on opioid use in implant-based breast reconstruction patients. Breast J. 2020;26(9):1712–1716. doi: 10.1111/tbj.13881. [DOI] [PubMed] [Google Scholar]
- Eriksson K., Wikström L., Årestedt K., Fridlund B., Broström A. Numeric rating scale: patients’ perceptions of its use in postoperative pain assessments. Appl. Nurs. Res. 2014;27(1) doi: 10.1016/j.apnr.2013.10.006. [DOI] [PubMed] [Google Scholar]
- Eriksson K., Wikström L., Fridlund B., Årestedt K., Broström A. Patients’ experiences and actions when describing pain after surgery – A critical incident technique analysis. Int. J. Nurs. Stud. 2015;56:27–36. doi: 10.1016/j.ijnurstu.2015.12.008. [DOI] [PubMed] [Google Scholar]
- Eshete M.T., Baeumler P.I., Siebeck M., Tesfaye M., Wonde D., Haileamlak A., Michael G.G., Ayele Y., Irnich D. The views of patients, healthcare professionals and hospital officials on barriers to and facilitators of quality pain management in Ethiopian hospitals: a qualitative study. PLoS One. 2019;14(3):1–20. doi: 10.1371/journal.pone.0213644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsberg A., Vikman I., Wälivaara B.M., Engström Å. Patients’ perceptions of their postoperative recovery for one month. J. Clin. Nurs. 2015;24(13–14):1825–1836. doi: 10.1111/jocn.12793. [DOI] [PubMed] [Google Scholar]
- Foust Winton R.E., Draucker C.B., Von Ah D. Pain management experiences among hospitalized postcraniotomy brain tumor patients. Cancer Nurs. 2021;44(3):E170–E180. doi: 10.1097/NCC.0000000000000851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan T.J. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J. Pain Res. 2017;10:2287–2298. doi: 10.2147/JPR.S144066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan T.J., Habib A.S., Miller T.E., White W., Apfelbaum J.L. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr. Med. Res. Opin. 2014;30(1) doi: 10.1185/03007995.2013.860019. [DOI] [PubMed] [Google Scholar]
- Gan T.J., Habib A.S., Miller T.E., White W., Apfelbaum J.L. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr. Med. Res. Opin. 2014;30(1):149–160. doi: 10.1185/03007995.2013.860019. [DOI] [PubMed] [Google Scholar]
- Gélinas C., Shiva Shahiri T., Richard-Lalonde M., Laporta D., Morin J.F., Boitor M., Ferland C.E., Bourgault P., Richebé P. Exploration of a multi-parameter technology for pain assessment in postoperative patients after cardiac surgery in the intensive care unit: the nociception level index (nol)tm. J. Pain Res. 2021;14(August):3723–3731. doi: 10.2147/JPR.S332845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gishu T., Weldetsadik A.Y., Tekleab A.M. Patients’ perception of quality of nursing care; a tertiary center experience from Ethiopia. BMC Nurs. 2019;18(1):1–6. doi: 10.1186/s12912-019-0361-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon D.B. Acute pain assessment tools: let us move beyond simple pain ratings. Curr. Opin. Anaesthesiol. 2015 doi: 10.1097/ACO.0000000000000225. [DOI] [PubMed] [Google Scholar]
- Gordon D.B. Acute pain assessment tools: let us move beyond simple pain ratings. Curr. Opin. Anaesthesiol. 2015;28(5):565–569. doi: 10.1097/ACO.0000000000000225. [DOI] [PubMed] [Google Scholar]
- Gordon D.B., De Leon-Casasola O.A., Wu C.L., Sluka K.A., Brennan T.J., Chou R. Research gaps in practice guidelines for acute postoperative pain management in adults: findings from a review of the evidence for an American pain society clinical practice guideline. J. Pain. 2016;17(2) doi: 10.1016/j.jpain.2015.10.023. [DOI] [PubMed] [Google Scholar]
- Haddaway N.R., Page M.J., Pritchard C.C., McGuinness L.A. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022;18(2):1–12. doi: 10.1002/cl2.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henningsen M.J., Sort R., Møller A.M., Herling S.F. Peripheral nerve block in ankle fracture surgery: a qualitative study of patients’ experiences. Anaesthesia. 2018;73(1):49–58. doi: 10.1111/anae.14088. [DOI] [PubMed] [Google Scholar]
- Hirsh A.T., George S.Z., Robinson M.E. Pain assessment and treatment disparities: a virtual human technology investigation. Pain. 2009 doi: 10.1016/j.pain.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoorntje A., Leichtenberg C.S., Koenraadt K.L.M., van Geenen R.C.I., Kerkhoffs G.M.M.J., Nelissen R.G.H.H., Vliet Vlieland T.P.M., Kuijer P.P.F.M. Not physical activity, but patient beliefs and expectations are associated with return to work after total knee arthroplasty. J. Arthroplasty. 2018;33(4):1094–1100. doi: 10.1016/j.arth.2017.11.032. [DOI] [PubMed] [Google Scholar]
- Jahandideh S., Kendall E., Low-Choy S., Donald K., Jayasinghe R., Barzegari E. The process of patient engagement in outpatient cardiac rehabilitation programs. Behav. Change. 2019;36(4):233–251. doi: 10.1017/bec.2019.14. [DOI] [Google Scholar]
- Kaptain K., Bregnballe V., Dreyer P. Patient participation in postoperative pain assessment after spine surgery in a recovery unit. J. Clin. Nurs. 2017;26(19–20):2986–2994. doi: 10.1111/jocn.13640. [DOI] [PubMed] [Google Scholar]
- Kaptain K., Bregnballe V., Dreyer P. Patient participation in postoperative pain assessment after spine surgery in a recovery unit. J. Clin. Nurs. 2017;26(19–20):2986–2994. doi: 10.1111/jocn.13640. [DOI] [PubMed] [Google Scholar]
- Kästner A., Ng Kuet Leong V.S.C., Petzke F., Budde S., Przemeck M., Müller M., Erlenwein J. The virtue of optimistic realism - expectation fulfillment predicts patient-rated global effectiveness of total hip arthroplasty. BMC Musculoskelet. Disord. 2021;22(1):1–14. doi: 10.1186/s12891-021-04040-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komann M., Baumbach P., Stamer U.M., Weinmann C., Arnold C., Pogatzki-Zahn E., Meißner W. Desire to receive more pain treatment – a relevant patient-reported outcome measure to assess quality of post-operative pain management? Results from 79,996 patients enrolled in the pain registry QUIPS from 2016 to 2019. J. Pain. 2021;22(6):730–738. doi: 10.1016/j.jpain.2021.01.002. [DOI] [PubMed] [Google Scholar]
- Köse Tamer L., Sucu Dağ G. The assessment of pain and the quality of postoperative pain management in surgical patients. Sage Open. 2020;10(2) doi: 10.1177/2158244020924377. [DOI] [Google Scholar]
- Kuperberg K.G., Grubbs L. Coronary artery bypass patients’ perceptions of acute postoperative pain. Clin. Nurse Spec. 1997;11(3):116–122. doi: 10.1097/00002800-199705000-00009. [DOI] [PubMed] [Google Scholar]
- Kuusniemi K., Pöyhiä R. Present-day challenges and future solutions in postoperative pain management: results from PainForum 2014. J. Pain Res. 2016 doi: 10.2147/JPR.S92502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapkin S., Ellwood L., Diwan A., Fernandez R. Reliability, validity, and responsiveness of multidimensional pain assessment tools used in postoperative adult patients: a systematic review of measurement properties. JBI Evidence Synthesis. 2021;19(2):284–307. doi: 10.11124/JBISRIR-D-19-00407. [DOI] [PubMed] [Google Scholar]
- Lauzon Clabo L.M. An ethnography of pain assessment and the role of social context on two postoperative units. J. Adv. Nurs. 2008;61(5):531–539. doi: 10.1111/j.1365-2648.2007.04550.x. [DOI] [PubMed] [Google Scholar]
- Lindberg J.O., Engström Å. Critical care nurses’ experiences: “a good relationship with the patient is a prerequisite for successful pain relief management. Pain Manage. Nurs. 2011;12(3):163–172. doi: 10.1016/j.pmn.2010.03.009. [DOI] [PubMed] [Google Scholar]
- Magidy M., Warrén-Stomberg M., Bjerså K. Assessment of post-operative pain management among acutely and electively admitted patients - A Swedish ward perspective. J. Eval. Clin. Pract. 2016;22(2):283–289. doi: 10.1111/jep.12475. [DOI] [PubMed] [Google Scholar]
- Mazer L.S., Lovett P.J., Miller J.M., Pitruzzello N.E., Boone M.K., Irizarry Alvarado J.M. Improving satisfaction with postoperative pain management for patients with persistent pain: a preoperative pain medicine consultation intervention. J. Perioper. Pract. 2020;30(11):345–351. doi: 10.1177/1750458919886720. [DOI] [PubMed] [Google Scholar]
- McDonall J., Heynsbergh N., Oxley S., Botti M., Hutchinson A. Opportunities for patients to engage in postoperative recovery following cardiac surgery: a systematic narrative review. Patient Educ. Couns. 2020;103(10):2095–2106. doi: 10.1016/j.pec.2020.04.004. [DOI] [PubMed] [Google Scholar]
- McTier L.J., Botti M., Duke M. Patient participation in quality pain management during an acute care admission. Clin. J. Pain. 2014;30(4):316–323. doi: 10.1097/AJP.0b013e318298ddc5. [DOI] [PubMed] [Google Scholar]
- Meissner W., Huygen F., Neugebauer E.A.M., Osterbrink J., Benhamou D., Betteridge N., Coluzzi F., De Andres J., Fawcett W., Fletcher D., Kalso E., Kehlet H., Morlion B., Montes Pérez A., Pergolizzi J., Schäfer M. Management of acute pain in the postoperative setting: the importance of quality indicators. Curr. Med. Res. Opin. 2018;34(1):187–196. doi: 10.1080/03007995.2017.1391081. [DOI] [PubMed] [Google Scholar]
- Merriam-Webster. (n.d.). Retrieved May 25, 2022, from https://www.merriam-webster.com/dictionary/belief#:∼:text=Definition%252.
- Milosevic S., Strange H., Morgan M., Ambler G.K., Bosanquet D.C., Waldron C.A., Thomas-Jones E., Harris D., Twine C.P., Brookes-Howell L. Exploring patients’ experiences of analgesia after major lower limb amputation: a qualitative study. BMJ Open. 2021;11(12):1–8. doi: 10.1136/bmjopen-2021-054618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mubita W.M., Richardson C., Briggs M. Patient satisfaction with pain relief following major abdominal surgery is influenced by good communication, pain relief and empathic caring: a qualitative interview study. Br. J. Pain. 2020;14(1):14–22. doi: 10.1177/2049463719854471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell K.F. Preoperative pain management education: an evidence-based practice project. J. Perianesth. Nurs. 2018;33(6):956–963. doi: 10.1016/j.jopan.2017.11.001. [DOI] [PubMed] [Google Scholar]
- Öğüt S., Sucu Dağ G. Pain characteristics and pain interference among patients undergoing open cardiac surgery. J. Perianesth. Nurs. 2019;34(4):757–766. doi: 10.1016/j.jopan.2018.10.009. [DOI] [PubMed] [Google Scholar]
- Ouellette C., Henry S., Turner A., Clyne W., Furze G., Bird M., Sanchez K., Watt-Watson J., Carroll S., Devereaux P.J., McGillion M. The need for novel strategies to address postoperative pain associated with cardiac surgery: a commentary and introduction to “SMArTVIEW. Canadian J. Pain. 2019;3(2):26–35. doi: 10.1080/24740527.2019.1603076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pius A.K., Jones E., Bonnell L.N., Fujii M.H., MacLean C.D. Patients’ experience with opioid pain medication after discharge from surgery: a mixed-methods study. J. Surg. Res. 2020;256:328–337. doi: 10.1016/j.jss.2020.06.026. [DOI] [PubMed] [Google Scholar]
- Ramia E., Nasser S.C., Salameh P., Saad A.H. Patient perception of acute pain management: data from three tertiary care hospitals. Pain Res. Manag. 2017;2017:1–12. doi: 10.1155/2017/7459360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramia E., Nasser S.C., Salameh P., Saad A.H. Patient perception of acute pain management: data from three tertiary care hospitals. Pain Res. Manage. 2017;2017 doi: 10.1155/2017/7459360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawal N. Current issues in postoperative pain management. Eur. J. Anaesthesiol. 2016;33(3):160–171. doi: 10.1097/EJA.0000000000000366. [DOI] [PubMed] [Google Scholar]
- Rijkenberg S., Stilma W., Bosman R.J., van der Meer N.J., van der Voort P.H.J. Pain measurement in mechanically ventilated patients after cardiac surgery: comparison of the behavioral pain scale (BPS) and the critical-care pain observation tool (CPOT) J. Cardiothorac. Vasc. Anesth. 2017;31(4):1227–1234. doi: 10.1053/j.jvca.2017.03.013. [DOI] [PubMed] [Google Scholar]
- Rowland P., McMillan S., McGillicuddy P., Richards J. What is “the patient perspective” in patient engagement programs? Implicit logics and parallels to feminist theories. Health (United Kingdom) 2017;21(1):76–92. doi: 10.1177/1363459316644494. [DOI] [PubMed] [Google Scholar]
- Scher C., Meador L., Van Cleave J.H., Reid M.C. Moving beyond pain as the fifth vital sign and patient satisfaction scores to improve pain care in the 21st century. Pain Manage. Nurs. 2018;19(2):125–129. doi: 10.1016/j.pmn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwenkglenks M., Gerbershagen H.J., Taylor R.S., Pogatzki-Zahn E., Komann M., Rothaug J., Volk T., Yahiaoui-Doktor M., Zaslansky R., Brill S., Ullrich K., Gordon D.B., Meissner W. Correlates of satisfaction with pain treatment in the acute postoperative period: results from the international PAIN OUT registry. Pain. 2014;155(7) doi: 10.1016/j.pain.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Tawil S., Iskandar K., Salameh P. Pain management in hospitals: patients’ satisfaction and related barriers. Pharm. Pract. 2018;16(3):1–9. doi: 10.18549/PharmPract.2018.03.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry R., Niven C., Brodie E., Jones R., Prowse M. An exploration of the relationship between anxiety, expectations and memory for postoperative pain. Acute Pain. 2007;9(3):135–143. doi: 10.1016/j.acpain.2007.04.041. [DOI] [Google Scholar]
- Tong Y.G., Konstantatos A.H., Cheng Y., Chai L. Improving pain management through addition of the functional activity score. Aust. J. Adv. Nurs. 2018;35(4):52–60. [Google Scholar]
- Topham D., Drew D. Quality improvement project: replacing the numeric rating scale with a clinically aligned pain assessment (CAPA) tool. Pain Manage. Nurs. 2017;18(6):363–371. doi: 10.1016/j.pmn.2017.07.001. [DOI] [PubMed] [Google Scholar]
- Van Boekel R.L.M., Vissers K.C.P., van der Sande R., Bronkhorst E., Lerou J.G.C., Steegers M.A.H. Más allá de los puntajes de dolor: la evaluación multidimensional del dolor es esencial para el manejo adecuado del dolor después de la cirugía. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0177345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dijk J.F.M., Kappen T.H., Schuurmans M.J., van Wijck A.J.M. The relation between patients’ NRS pain scores and their desire for additional opioids after surgery. Pain Pract. 2015;15(7):604–609. doi: 10.1111/papr.12217. [DOI] [PubMed] [Google Scholar]
- van Dijk J.F.M., Schuurmans M.J., Alblas E.E., Kalkman C.J., van Wijck A.J.M. Postoperative pain: knowledge and beliefs of patients and nurses. J. Clin. Nurs. 2017;26(21–22) doi: 10.1111/jocn.13714. [DOI] [PubMed] [Google Scholar]
- Van Dijk J.F.M., Van Wijck A.J.M., Kappen T.H., Peelen L.M., Kalkman C.J., Schuurmans M.J. Postoperative pain assessment based on numeric ratings is not the same for patients and professionals: a cross-sectional study. Int. J. Nurs. Stud. 2012;49(1):65–71. doi: 10.1016/j.ijnurstu.2011.07.009. [DOI] [PubMed] [Google Scholar]
- Vu P.H., Tran D.V., Dao T.T.H., Dong O.T., Nguyen T.T., Nguyen T.H. Patients’ active participation in postoperative pain management in an urban hospital of Vietnam: implications for patient empowerment. Hosp. Top. 2021;0(0):1–8. doi: 10.1080/00185868.2021.2014767. [DOI] [PubMed] [Google Scholar]
- Werner M.U., Kongsgaard U.E. Defining persistent post-surgical pain: is an update required? Br. J. Anaesth. 2014;113(1) doi: 10.1093/bja/aeu012. [DOI] [PubMed] [Google Scholar]
- Willingham M.D., Vila M.R., Ben Abdallah A., Avidan M.S., Haroutounian S. Factors contributing to lingering pain after surgery: the role of patient expectations. Anesthesiology. 2021;6:915–924. doi: 10.1097/ALN.0000000000003754. [DOI] [PubMed] [Google Scholar]
- Wooldridge S., Branney J. Congruence between nurses’ and patients’ assessment of postoperative pain: a literature review. Br. J. Nurs. 2020;29(4):212–220. doi: 10.12968/bjon.2020.29.4.212. [DOI] [PubMed] [Google Scholar]
- Zoëga S. Education and support strategies improve assessment and management of pain by nurses. Scand. J. Pain. 2017;16(2017):99–100. doi: 10.1016/j.sjpain.2017.04.004. [DOI] [PubMed] [Google Scholar]
- Zoëga S., Ward S., Gunnarsdottir S. Evaluating the quality of pain management in a hospital setting: testing the psychometric properties of the icelandic version of the revised American pain society patient outcome questionnaire. Pain Manage. Nurs. 2014;15(1):143–155. doi: 10.1016/j.pmn.2012.08.001. [DOI] [PubMed] [Google Scholar]