Abstract
Background
Nurse-patient communication in intensive care units is challenged by the fact that patients are voiceless due to intubation and mechanical ventilation. Difficult communication affects nurses negatively, and it requires knowledge and expertise to facilitate communication in this complex and technologically tense setting. Augmentative and alternative communication has been suggested as a way of optimising communication; several approaches can be combined in a multi-component intervention. Also, a communication algorithm has been proposed as a way of providing structure in patient communication. To enhance transparency and avoid poorly reported interventions, this paper describes the process, rationale and reflections behind developing a communication intervention called the ICU-COM.
Objectives
To present the development process of a communication intervention prototype that aims to support and strengthen nurses’ communication with mechanically ventilated patients in an intensive care unit.
Design
The Medical Research Council's framework for developing complex interventions in health was applied. The approach was target-population centred.
Settings
The intervention was developed and tailored to four intensive care unit departments at Aarhus University Hospital in Denmark.
Participants
Intensive care nurses and various experts, namely, speech-language pathologists, graphic designers, a software company, the local Centre for E-learning and nurse specialists were involved in its development.
Results
An intervention consisting of: 1) a multi-component communication bundle, 2) delivery of the bundle via a teaching session and 3) initial implementation via nurse communication guides was developed. The communication bundle contained: 1) a communication strategy with a BASIS framework and algorithm, 2) a nurse education programme and 3) low-tech and high-tech communication tools.
Conclusions
A systematic approach was applied in the development process. However, the acceptability and feasibility of the intervention is at present unknown.
Keywords: Augmentative and alternative communication, Complex interventions, Critical care, Intensive care unit, Intervention development, Mechanical ventilation, Nurse-patient communication
CONTRIBUTION OF THE PAPER.
What is already known about the topic:
-
•
Patients who are admitted to the intensive care unit and undergo mechanical ventilation can only express themselves nonverbally or via communication tools.
-
•
Communication is a challenge in this complex context, and the difficulties affect both nurses and patients negatively.
-
•
Nursing care faces the challenge of balancing patient-centred care with highly technical procedures; studies highlight the need to support nurses in this process.
What this paper adds:
-
•
The Medical Research Council's framework for developing complex interventions within health provides a systematic approach that can be applied in the critical care setting.
-
•
This paper demonstrates that it is possible to develop an intervention with a multi-component bundle whose aim is to support and strengthen nurses’ communication with mechanically ventilated patients; however, the intervention's feasibility and acceptability is at present unknown.
Alt-text: Unlabelled box
1. Introduction
Communication is an essential aspect of being a human. We communicate continuously in our interactions with the world and the people in it; it is part of what defines us as individuals. It is how we express our thoughts, needs, wishes and opinions. What if you woke up suddenly deprived of the possibility of expressing yourself verbally? How would you make yourself understood? This is the reality of many patients admitted to an intensive care unit (ICU) who undergo mechanical ventilation. During mechanical ventilation, patients temporarily lose speech function due to intubation causing communication difficulties, miscommunication or even non-communication between patients and healthcare professionals. Furthermore, ICU patients have characteristics that complicate communication further like paralysis, ICU-acquired weakness, delirium, fatigue and blurred consciousness. For healthcare professionals, it is not an easy task to establish communication that goes both ways, where their message is understood and mechanically ventilated patients also have the opportunity to express themselves. This article focuses on the development of a novel communication intervention prototype that aimed to strengthen and support nurses’ communication with mechanically ventilated patients in the ICU. The intervention consists of 1) a multi-component communication bundle, 2) delivery of the bundle via a teaching session and 3) initial implementation via nurse communication guides. We describe the process, rationale and reflections behind developing, modelling and designing the communication intervention, called the ICU-COM, within the framework of complex interventions (Craig et al., 2008, 2019).
2. Background
2.1. Nurse-patient communication in the ICU
The past decade has seen a paradigm shift in ICUs where using heavy sedation has been reduced in favour of analgosedation (Devabhakthuni et al., 2012), light sedation (Devlin et al., 2018; Hughes et al., 2013), daily sedation breaks (Kress et al., 2000) and no-sedation protocols (Strøm et al., 2010). Regardless of the choice of strategy, the rationale for avoiding deep sedation is the negative effects it might have on outcomes like time to extubation, tracheostomy rate and delirium (Devlin et al., 2018). This change in sedation practices means that patients are conscious for a longer period during their ICU stay. Conscious patients require more attention from nurses, and a nurse-patient ratio of 1:1 is ideal (Laerkner et al., 2016; Tsuyada et al., 2019). Nursing practice in contexts of light or no sedation faces the challenges of balancing care to comply with advanced technical devices and the many care and treatment procedures while establishing a close relationship with the patient (Everingham et al., 2014; Karlsson and Bergbom, 2014; Laerkner et al., 2015). This is a demanding task that requires knowledge and expertise, and communication is highlighted as a core component to achieving patient-centred care (Tingsvik et al., 2013; Vincent et al., 2016). Nurses are the main communication partners in the ICU as they are close to the patient 24 h a day. Also, nurses control the contents and duration of communication (Happ et al., 2011). It is complex and challenging communicating with voiceless patients, and even experienced nurses may encounter negative feelings like frustration and incompetence in their attempts to understand patients (IJssennagger et al., 2018; Rodriguez et al., 2015). These negative feelings associated with communication difficulties may even affect nurses’ job satisfaction (IJssennagger et al., 2018). In a recent study, nurses reported difficult communication in 35% of patient cases (Freeman-Sanderson et al., 2018), which underlines the need to support nurses during communication with mechanically ventilated patients. Failed communication not only affects nurses; it may also result in patients resigning and giving up on trying to communicate at all (Karlsen et al., 2018).
2.2. Communication interventions in the ICU
Voiceless, mechanically ventilated patients can only express themselves via nonverbal signs or different tools and devices. One of the most commonly used communication methods involves healthcare personnel asking a question and patient nodding or shaking their head to indicate a yes/no response (Happ et al., 2004; Karlsson et al., 2012; Khalaila et al., 2011). Augmentative and alternative communication (AAC) is, however, also a known method in the ICU where different strategies, tools and devices can support communication during patients’ voicelessness (Finke et al., 2008). A systematic review reports that the most effective AAC strategy in the ICU remains unknown, but that AAC can improve patient satisfaction and reduce communication difficulties (Carruthers et al., 2017). Another review concludes that communication interventions with mechanically ventilated patients are feasible, have utility and are safe (Zaga et al., 2019). Some studies have tested communication with single AAC interventions that may improve communication, e.g. low-tech tools (Hosseini et al., 2018; Otuzoğlu and Karahan, 2014), high-tech devices (Garry et al., 2016; Koszalinski et al., 2020; Rodriguez et al., 2016; Rose et al., 2018) and staff communication training (Dithole et al., 2017; Radtke et al., 2012). In the SPEACS trial, a multi-component intervention was designed that consisted of basic communication training and additional AAC training for nurses. This had a positive impact on the duration of communication exchanges, use of AAC and success in communication about ICU symptoms (Happ et al., 2014). However, to our knowledge, the SPEACS and SPEACS-2 are the only more recently conducted studies testing a multi-component intervention (Choi and Tate, 2021; Happ et al., 2015, 2010; Trotta et al., 2020). Furthermore, a study suggest applying an algorithm focusing on assessment and choice of methods to work towards a systematic approach in ICU patient communication (ten Hoorn et al., 2016). A similar algorithm can be seen in the SPEACS-2 website, which provides tangible tools for use in clinical practice (Happ, 2013).
2.3. The rationale of the study
We know from our previous study (Holm et al., 2020) that trying to optimise communication in the ICU requires a multi-component approach like the SPEACS trials. We also know that the local context plays a vital role when designing a communication intervention with respect to culture, treatment and care practices, and language (Holm et al., 2020). Therefore, we wanted to develop a novel communication intervention prototype designed for our Danish context that drew on the best available evidence.
Designing and setting up an intervention in the ICU setting is complex. It is complex at a relational level because patients’ voicelessness complicates nurse-patient interactions; it is also complex because of the patients’ critical condition. The acute technological ICU environment further intensifies complexity. This specific context particularly calls for a rigorous, systematic and thorough process for designing interventions. Richards and Borglin (2011) argue that nursing can be seen as the ‘quintessential complex interventions’. It involves a number of components that may interact when applied to clinical practice (Richards and Borglin, 2011). We therefore found it important to describe the evidence and rationale behind each component of the intervention that we set up. In that way, we could enhance transparency and avoid poorly reported interventions (Richards et al., 2014; Yamato et al., 2016). Furthermore, carefully developed complex interventions are more likely to prove effective during evaluation and be adopted in the real world (O'Cathain et al., 2019a). The essential processes and decision-making behind intervention development are rarely reported. However, intervention studies are entering a new era where the importance of methodological rigour in the early phase of development is gaining recognition (Hoddinott, 2015). Therefore, this article is dedicated to giving a detailed description of each step taken in the process of developing a communication intervention to support and strengthen nurses’ communication with mechanically ventilated patients.
2.4. AIM
The objective of this paper was to present the development of a communication intervention prototype targeted at ICU nurses. The intervention is called the ICU-COM and consists of:
-
•
A multi-component communication bundle
-
•
Delivery of the bundle via teaching session
-
•
Initial implementation via nurse communication guides
From a clinical perspective, the aim of the intervention was to support and strengthen nurses’ communication with mechanically ventilated patients in the ICU.
3. Development of the intervention
3.1. Methods
The Medical Research Council's (MRC) framework was used as the overall framework for developing the intervention (Craig et al., 2008, 2019). The MRC's framework supports the process of developing, pilot/feasibility testing, evaluating and implementing complex interventions in health care. It is an internationally acclaimed approach and the one most widely used for guiding development of interventions within nursing (Corry et al., 2013). Different methods are used for intervention development including co-creation, intervention mapping and implementation-based approaches (O'Cathain et al., 2019b). We used a target-population-centred approach (O'Cathain et al., 2019b) because we wanted to ensure that the target group – the ICU nurses – would find it meaningful and acceptable in their clinical practice.
To strengthen the development phase, the approach suggested by Bleijenberg et al. (2018) was applied. They combine the MRC framework with other existing development models to strengthen the design, increase value, reduce the risk of ineffective interventions, and enhance fit with clinical practice (Bleijenberg et al., 2018). Bleijenberg et al. (2018) add three new elements to the original MRC framework which thereby consists of six: 1) problem identification and definition, 2) systematic identification of evidence, 3) identification or development of theory, 4) determination of needs, 5) examination of current practice and context, and 6) modelling and process outcomes. These six steps guide the final phase, which is intervention design. The objective of this study was, however, to develop a prototype. Adjustment of the prototype will take place after feasibility testing, before setting up the final intervention for full implementation. The ‘problem identification’ and ‘results’ sections in the present paper are built up around the six steps. Table 1 summarises the development of the communication bundle, also based on Bleijenberg et al. (2018).
Table 1.
Summary of the development of the communication bundle, based on Bleijenberg et al. (2018).
| Strategy | Education of nurses | Communication tools | |
|---|---|---|---|
| Problem identification and definition | No national or international guidelines exist on the subject and the nurses have no guidance. | Nurses find communication with MV patients difficult. Implementation of AAC in ICUs is challenging. |
Communication tools have to be tailored to the local context in relation to contents and language. |
| Identification of evidence | An algorithm may support nurses’ assessment of patient communication, choice of communication strategies and documentation. Providing structure and building the relationship are two cornerstones in communication theory, also in the ICU. |
Communication training may improve nurses’ communication skills. Evidence detailing the contents and duration of nurse education programmes in ICUs is sparse. |
Communication tools can increase patient satisfaction and reduce communication difficulties. |
| Identification of theory | Augmentative and alternative communication (AAC) and the Calgary Cambridge Guide. | ||
| Needs determination | Nurses need support tools to help them assess patient communication and guide them in a systematic and structured approach. | Nurses need more knowledge about communicating with mechanically ventilated patients. | There is a need for updated, evidence-based communication tools in clinical practice. |
| Examination of current practice and context | Nurses describe communication as a ‘guessing game’, illustrating that communication can be random and unstructured. There is a lack of systematic communication assessment and documentation of patient communication and the methods applied. |
72% of nurses in our ICU report received teaching on communication with mechanically ventilated patients, but their contents and duration are unknown. | Communication tools in clinical practice are very different in design and contents; some departments have many different tools to choose from, while others have none. |
| Modelling process | The algorithm:
|
Teaching session:- Introduction of how to use the bundleE-learning:
|
A simple communication toolbox was chosen to make it easy for nurses to choose the right tool.
|
| People involved in the process |
|
|
|
During the entire process, we tried to comply with the key principles of intervention development making it a dynamic, iterative and creative process, adaptable for changes that made it more coherent with clinical practice while having future implementation in mind (O'Cathain et al., 2019a). As described by O'Cathain et al. (2019a), the essential outputs of the development phase are a document that describes the intervention and publication of the development process. This article encompasses both of these outputs as it focuses on describing the development process and will be combined with a detailed description of the intervention. Also, to strengthen the reporting, we applied the Guidance for reporting intervention development studies in health research (GUIDED) (Duncan et al., 2020), which can be seen in supplementary file A.
3.2. Intervention description
The quality of intervention descriptions in health is inadequate (Hoffmann et al., 2014; Hoffmann and Walker, 2015; Schumann et al., 2010). To ensure that the black box of this intervention is unravelled, we supplemented this article with the Template for Intervention Description and Replication (TIDieR) – see supplementary file B. Using this checklist ensures that the ‘why, what, who, how, when and where’ of the intervention are described so that it can be replicated in clinical practice and research (Hoffmann et al., 2014).
3.3. Problem identification
3.3.1. Examine current practices and context and needs determination
A key ingredient in determining the active components in an intervention is to understand usual care as well as the context and setting where the intervention is developed and subsequently delivered (Bleijenberg et al., 2018; O'Cathain et al., 2019a). To gain an in-depth understanding of the nurse-patient communication in our context, we undertook a comprehensive qualitative study encompassing participant observations, patient interviews and nurse focus group interviews (Holm and Dreyer, 2018a). Furthermore, we pilot-tested a tablet as a single intervention to examine whether this could support communication (Holm and Dreyer, 2018b). Together, these two studies provided a solid foundation for understanding our context, the implementation challenges, how each component of the bundle should be developed and designed, and the intervention delivered.
3.3.2. Setting
The ICU is situated in a university hospital in Denmark. Its capacity is 44 patients and it is divided into four smaller departments. Patients from all medical and surgical specialties are admitted. The ICUs perform the highly specialised treatment of patients with all types of organ failure and are equivalent to ‘high-dependency units’, even though this is not the term used in Denmark. All rooms are singe-bed rooms with the nurse observation station situated adjacently, separated by a window. The nurse-patient ratio is 1:1, and nurses are present 24 h a day, making them the main communication partners. Nurse-patient communication in the ICU is characterised by a process that is on-going throughout the day with focus on information about treatment, care and procedures as well as more relational communication where the nurse tries to understand the patient's needs, wishes and concerns. There is close interdisciplinary collaboration between the physicians, nurses and physiotherapists who constitute the permanent staff. Recommendations of the Danish Society of Anaesthesiology and Intensive Care guide the sedation practice, minimalising the use of sedatives, whenever possible. As in the rest of Denmark, patients are not physically restrained. There is no restriction on visiting hours – relatives are always welcome.
3.3.3. The target population
The goal of intervention development is to design an intervention that ‘solves’ or reduces the impact of the problem (Bleijenberg et al., 2018). In this study, we chose to target the ICU nurses, not the patients. This was based on the extremely vulnerable state of the acute and critically ill ICU patients who have no surplus energy to take the initiative or figure out how to handle the difficult communication. Instead, nurses have to take the initiative and responsibility for the success of the communication. The intervention will be targeted at nurses with all levels of experience and expertise. To get an overview of our target population, we did a cross-sectional survey (Table 2). The survey was undertaken in December 2019, and the response rate was 82% with 231 respondents. The data analysis was descriptive statistics. There were 281 employees at the given time, not counting nurses on maternity or long-term sick leave.
Table 2.
Demographic data of nurses working in our ICUs.
| Characteristics (n = 231) | Number/percentage |
|---|---|
| Gender | |
| Female | 221 (96%) |
| Male | 10 (4%) |
| Years with bachelor degree in nursing | |
| Less than 1 year | 18 (8%) |
| 1–2 years | 15 (6%) |
| 3–5 years | 26 (11%) |
| 6–10 years | 33 (14%) |
| 11–15 years | 40 (17%) |
| 16–25 years | 46 (20%) |
| More than 25 years | 53 (23%) |
| Total years of experience working in an ICU | |
| Less than 1 year | 34 (15%) |
| 1–2 years | 30 (13%) |
| 3–5 years | 21 (9%) |
| 6–10 years | 32 (14%) |
| 11–15 years | 40 (17%) |
| 16–25 years | 48 (21%) |
| More than 25 years | 26 (11%) |
| Degree in critical care nursing | |
| Yes | 147 (64%) |
| No | 74 (32%) |
| Trainee | 10 (4%) |
| Previous teaching on communication with mechanically ventilated patients | |
| Yes | 166 (72%) |
| No | 50 (22%) |
| Do not know | 15 (6%) |
3.3.4. Identify theory
The theoretical principle chosen to guide the ICU-COM was augmentative and alternative communication (AAC). AAC uses tools and strategies to facilitate communication when the patient is voiceless; and speech-language pathologists are experts within this area (Mirenda and Beukelman, 2013). The approach has been adopted in the ICU setting because it provides tangible methods that may support communication with the complex group of patients that temporarily lose their voice due to intubation (Hurtig and Downey, 2009). AAC systems are classified as either unaided or aided. Unaided approaches are those where the body is used as the means for communication, e.g. gestures; aided approaches include use of tools, equipment or devices to support communication, e.g. spelling boards. Aided AAC can furthermore be divided into low-tech and high-tech tools: low-tech are simple communication books or boards, whereas high-tech incorporate a diverse group of electronic tools or devices. AAC refers to an area of research, clinical and educational practice that can guide users to find the right strategies and tools to support communication with patients who have a temporary or permanent communication impairment (Mirenda and Beukelman, 2013). In the ICU-COM, AAC provided an overview and guidance as to which approaches and methods are useful in the ICU setting. Furthermore, it provided insight into the role and responsibilities of the communication partners – in this case, the nurses. To some degree, it also provided knowledge about how to structure a communication education and the training session or workshop. However, to strengthen this, we chose to supplement AAC with the Calgary-Cambridge guide (Silverman et al., 2013). This was originally designed to guide the curriculum of healthcare communication training with focus on dialogic conversation or a medical interview, e.g. at the general practitioner's office (Kurtz and Silverman, 1996). Even though dialogic conversation between nurses and patients in the ICU is very limited because the patient can give only nonverbal responses, we found it useful to include the two important perspectives of 1) building the relationship with the patient and 2) providing structure in communication, when developing the communication strategy and educating and training the nurses.
3.3.5. Identify evidence
To identify the current evidence base, we undertook a review of the literature. We found that several reviews already existed on the subject. Therefore, we chose the umbrella review to compare and contrast the findings of these research syntheses (Joanna Briggs Institute, 2014). Overall, we found that implementation of four key aspects may optimise communication in clinical practice: a) assessment and documentation, b) use of communication methods or approaches, c) training and education of nurses, and d) use of unaided AAC as well as low-tech and high-tech communication tools (Holm et al., 2020). Findings from this review will be included throughout the Results section, and additional references will be used when necessary.
3.3.6. Stakeholder and expert consultations
Throughout the study, we involved the main stakeholders – the clinical nurses working in our departments. It was of paramount importance for us to engage the end-users as recommended when designing interventions for healthcare professionals (Colquhoun et al., 2017; O'Cathain et al., 2019a). In the beginning of the study, we formed a group of clinical nurses to provide feedback on each component of the bundle, as they were designed and modelled. The nurses were contacted whenever the researchers needed feedback on their ideas and thoughts to increase the chance of the components being meaningful and useful in clinical practice. This meant that the development phase was an iterative process where the components were changed to comply with both the nurses’ perspectives and the evidence found in literature. The nurses also provided feedback on the best way of delivering the intervention.
During the whole process, experts were consulted for their opinions on each component of the communication bundle. Three speech-language pathologists provided feedback on the communication strategy and tools; graphic designers helped design the layout of the bundle; the Centre for E-learning in the Central Region Denmark assisted with the e-learning of the education programme; a software company provided assistance with the tools; IT experts supported the installation of the communication app; expert nurses supervised the e-learning programme; and a nurse with speciality in hygiene was contacted to ensure that the tools would live up to hospital hygienic requirements.
The experts were contacted during specific periods and their combined feedback provided priceless support to establish the evidence base of the contents and enhance the user friendliness and layout of the communication bundle.
4. Ethical issues and approval
We applied for ethical approval at our national research committee and the study did not require ethical approval to be conducted. Throughout the study, we followed the Declaration of Helsinki.
5. Results of intervention development
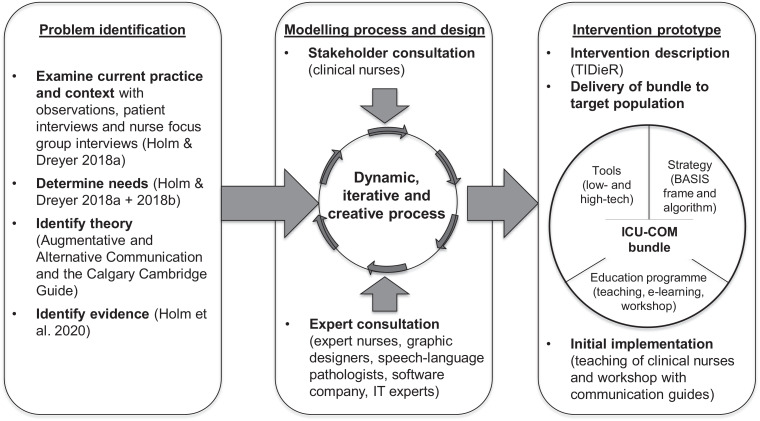
To illustrate the development process, we drew up Fig. 1.
Fig. 1.
Process model of the development of the ICU-COM intervention prototype with inspiration from Bleijenberg et al. (2018).
5.1. The communication bundle
Previous research shows that various intervention bundles may improve the outcome, treatment and care of ICU patients (Devlin et al., 2018;Knapp et al., 2013; Marra et al., 2017; Puntillo et al., 2014; Vincent et al., 2016). Therefore, the bundle perspective is not unfamiliar in the ICU context. The communication bundle that we designed consisted of three components as illustrated in Fig. 1. The rationale for choosing a multi-component bundle rather than just a single intervention was that the complexity of the subject required more active ingredients to have an impact (Holm et al., 2020). We found that a single intervention consisting of communication tools was not sufficient to support communication in all cases; a more comprehensive communication strategy had to be developed and tested (Holm and Dreyer, 2018b). Evidence of more complex communication interventions is sparse; however, the SPEACS study has shown a positive effect by combining training and AAC (Happ et al., 2014). Furthermore, we were inspired by the review of ten Hoorn et al. (2016) and found that the algorithm suggested could be a way of providing structure and a systematic approach to communication.
Because patients admitted to the ICU are a very heterogeneous group, the intervention must be patient-centred, allowing nurses to adapt their choices so that they fit each patient's unique needs and characteristics (Holm and Dreyer, 2018b, 2018a). This is reflected in the contents and design of each component of the bundle. Experts within AAC in the ICU setting acknowledge the challenges of implementing AAC in the complex and technologically intense ICU environment. However, they do suggest a formula for implementation of the AAC-ICU: referral/assessment + equipment availability + instruction + communication/teaming + simplicity (Beukelman et al., 2007). This formula contains some of the same components as our communication bundle and the ICU-COM intervention. Especially the aspect of simplicity was of vital importance to us, as our previous experience with setting up an AAC intervention in the ICU highlighted that this was necessary both in order for the patient to be able to use it, but also for the nurses to be willing to accept it in their daily work (Holm and Dreyer, 2018b). From the beginning, we considered how the intervention should be delivered and a future implementation strategy should be organised. Our study was a development/feasibility study, and focus was not on full-scale implementation. However, in agreement with the principles of the MRC framework, considerations concerning whether and how the intervention could be implemented were important (Craig et al., 2008, 2019). Each part of the bundle is described below.
5.2. Communication strategy
Research shows that clinical decision-support systems have proven effective in optimising healthcare processes (Bright et al., 2012; Kawamoto et al., 2005). We developed two support tools for clinical practice: 1) a communication assessment algorithm, and 2) an overall communication framework called BASIS. Together, the algorithm and framework constituted the ‘communication strategy’ of the bundle. It was designed as a support tool to guide nurses when communicating with patients, capturing all of the important aspects to incorporate in nurse-patient communication in the ICU. Furthermore, it provided nurses with a joint conceptual framework and terminology concerning communication with mechanically ventilated patients.
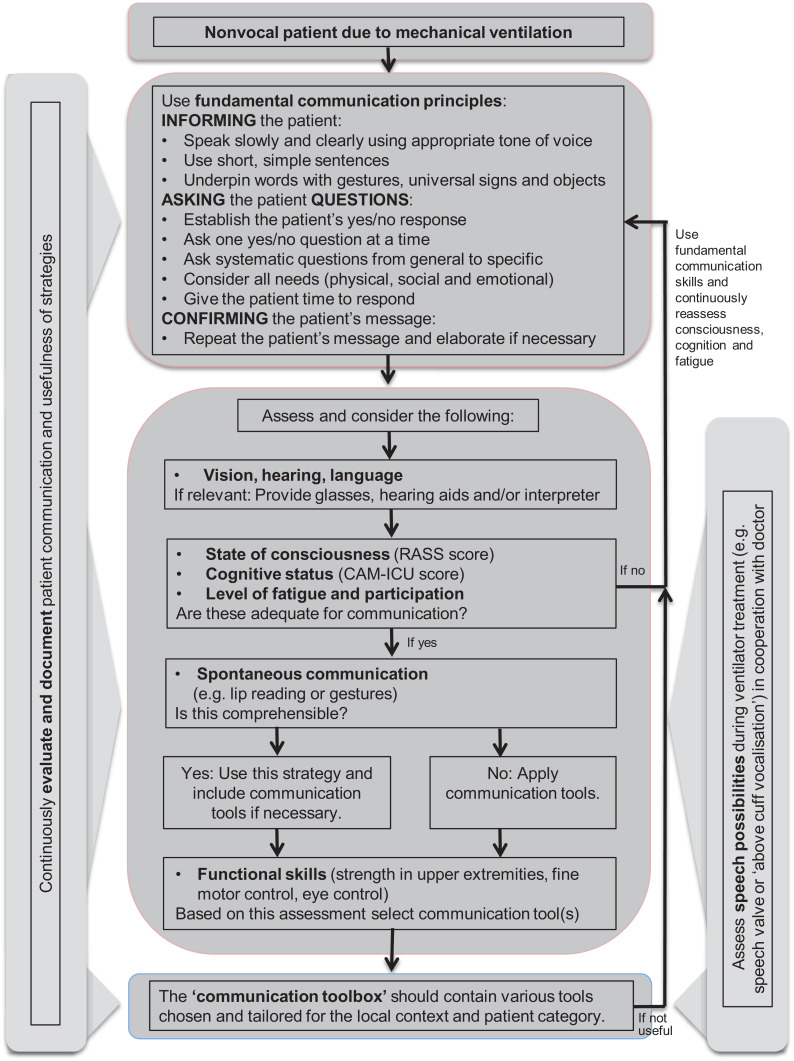
5.2.1. Algorithm
We know that communication is described as a ‘guessing game’ from the perspective of the nurses, illustrating that communication can be unstructured (Holm and Dreyer, 2018a). Furthermore, evidence highlights the importance of assessing, evaluating and documenting patient communication (Holm et al., 2020; Mirenda and Beukelman, 2013; Patak et al., 2009). A communication algorithm as suggested by ten Hoorn et al. (2016), Happ et al. (2013) and described by AAC experts (Mirenda and Beukelman, 2013) may support nurses in a systematic way. This was the rationale for designing the communication algorithm, which can be seen in Fig. 2. The algorithm was built up around five parts: 1) fundamental communication principles, 2) communication assessment 3) communication tools, 4) continuous evaluation and documentation, and 5) cooperation with a physician in the assessment of whether and when the patient was a candidate for a speech valve or ‘above cuff vocalisation’. Overall, a reader-friendly, logical and simple design was the goal during the design and modelling phase.
Fig. 2.
Communication algorithm: assessment and strategies.
Fundamental communication principles were the foundation of the algorithm. The rationale for this was that nurses should always start with this before considering using tools. We knew from our previous studies that tools and devices will not always facilitate communication, but that unaided AAC, e.g. a yes/no questioning technique is often useful (Holm et al., 2020; Holm and Dreyer, 2018b). Also, we hypothesised that these principles could be applied, no matter how acute or critically ill the patients were, in contrast with tools that require patients to have the cognitive and physical abilities and surplus energy to use them (Holm and Dreyer, 2018b). The principles were built on AAC theory (Garrett et al., 2007; Mirenda and Beukelman, 2013).
We chose a very simple toolbox that included 1) pen and paper on a solid surface, 2) a low-tech communication book with a spelling board and pictograms, and 3) a tablet with communication software (see details later).
We chose to separate what was purely nurse led and what was cooperation between nurses and physicians. This was in order to make clear which parts the nurse could work with independently and which parts had to be an interdisciplinary decision. Therefore, speech valves and ‘above cuff vocalisation’ were kept separate in the modelling phase and the final design of the algorithm. This was done not to belittle their importance, but merely to highlight that these were not exclusively nurse-led interventions.
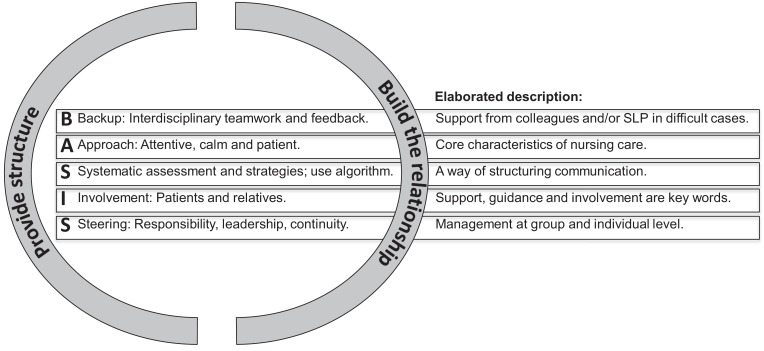
5.2.2. BASIS communication frame
Inspired by different acronyms or mnemonics (Blackstone, 2015; Burns et al., 2012), we designed the BASIS communication framework (Fig. 3). We brought together our knowledge from the problem identification phase to capture the most vital aspects of nurse-patient communication during mechanical ventilation. Furthermore, it captured organisational considerations like teamwork and leadership. Again, simplicity guided the modelling phase, and we tried to balance capturing the complex communication with a simple word that the nurses could remember and use in their daily work to support communication. We were inspired by the Calgary-Cambridge Guide where we chose to incorporate the two overall principles of providing structure and building the relationship (Silverman et al., 2013) as these are cornerstones in communicating with ICU patients. Instead of a linear process as in the Calgary-Cambridge guide, we encircled the BASIS word with the two components to highlight that they constitute an essential part of ‘every-day’ nurse-patient communication in the ICU.
Fig. 3.
The BASIS communication framework.
5.3. Education programme
We know little about the effect of communication training of healthcare personnel in the ICU setting. In other contexts, communication training has been shown to improve communication skills, particularly empathy (Moore et al., 2018; Selman et al., 2017). However, both in the ICU and cancer settings, for example, the optimal length and contents of an education programme remain unknown (Holm et al., 2020; Moore et al., 2018). Experts within AAC recommend that healthcare professionals obtain competencies in structuring the interaction, using appropriate strategies and enhancing personal communication (Blackstone, 2015). This is very much in line with the Calgary-Cambridge Guide (Silverman et al., 2013), and this supported us in building the curriculum of the education programme. Furthermore, we tried to incorporate persuasive arguments (Bartholomew Eldredge et al., 2016) in all of the components of the education programme to encourage and motivate the nurses to use the bundle. As shown in Table 2, 72% of nurses reported that they had previously received teaching on communication with mechanically ventilated patients. However, the contents and duration of such training are unknown.
The education programme was both a part of the communication bundle, a way of delivering the intervention and part of the initial implementation. It consisted of: 1) a teaching session (30 min) with introduction of how to use the communication bundle in clinical practice (power point presentation); 2) an e-learning course (approximately 25 min) providing basic knowledge about communication with mechanically ventilated patients which all nurses were asked to attend; and 3) a workshop (4 h) with communication guides with more in-depth knowledge of how to use the communication bundle and its underlying rationale to share with remaining nurse staff via bedside training and nurse conferences, for example.
A major challenge in organising the education programme was how to get almost 300 nurses through the education programme. This was the main reason for choosing the e-learning approach combined with the teaching session. However, the only way in which the teaching session could be organised was via already existing 30-minute educational sessions each Wednesday morning. Even though we completed 12 of these sessions, not all nurses were present because of the many evening and night shifts. An introductory video (PowerPoint with voiceover) was made, and this was emailed to all of the nurses who were unable to attend the teaching sessions to improve information uptake.
5.4. Tools
In the process of obtaining knowledge from international literature, we found that the contents of a communication toolbox is dependent on the local context because internationally ICUs are very differently organised (Egerod et al., 2015, 2013; Holm et al., 2020). All local differences influence the availability and usability of communication tools, and the communication toolbox must be developed accordingly.
We chose a ‘communication toolbox’ that included the most basic tools to ensure that nurses would find it easy to choose the right tool and not become overwhelmed by too many options. But this meant that more specialised or advanced tools were not readily available. Therefore, we entered into an agreement with the speech-language pathologists at our hospital that they could be contacted if there was need for more advanced tools and devices or if nurses needed support in assessing patient communication and choosing the best approaches to communication is the specific case. Previously, this had not been standard care (Holm and Dreyer, 2018a).
We had a meeting with each ICU department to establish which tools were available. It turned out that they all had very different options in relation to AAC tools. To standardise the selection of tools and ensure an evidence-based solution, we examined which tools and devices were available in our native language. We found that the app called Talk2Care by the software company BlueFragments was the best choice, and this was purchased for the project. The app was previously developed in cooperation with a Danish ICU, making it tailored for this particular setting. Therefore, both language and contents fitted our patient group. Furthermore, the graphic design was very simple and easy to understand.
However, the challenge was that Talk2Care only existed in an electronic version. From our previous study (Holm and Dreyer, 2018b), we knew that it was not sufficient with a high-tech tool; it needed to be supplemented with a low-tech version to make sure that more patients could use it. Therefore, we cooperated with BlueFragments to develop a low-tech version. We provided the contents and they undertook the graphical work, which meant that the pictograms were identical with the ones in the app. We knew from our examination of the context (Holm and Dreyer, 2018a) that ICU patients are a very heterogeneous group of patients with many different backgrounds and needs. Therefore, we had discussions with the clinical nurses and communication guides about the number of pictograms that were required. The tool should contain a sufficient number of expressions while not having too many, because this would make it difficult for the patient to get an overview. The final choice of pictograms was based on a pilot test and feedback from clinical nurses and communication guides. To make sure that the patient could always express if the contents of the tool was not sufficient, we added the option ‘I want to say something else’; this was an important aspect of making it patient-centred. Furthermore, we designed the first page so that the nurse could write down the special needs or expressions that were important for the patients as well as a box to tick off if the patient used glasses and/or hearing aid and the patient's yes/no signalling (Garrett et al., 2007). This was also an attempt to make it patient centred. Feedback from the pilot test in our ICU and another ICU in Denmark showed that the pictograms had to be bigger for the patients to see them. Therefore, we spread it out over more pages. None of the communication tools were discussed with patients or underwent a systematic validation process; as such, patient preferences as well as face validity and content validity are therefore unknown.
5.5. Initial implementation
In line with the MRC framework, implementation was considered from the beginning of the intervention development (Craig et al., 2008, 2019; O'Cathain et al., 2019a). Implementation of AAC in ICUs can be very challenging because the biomedical paradigm can be a barrier, where communication typically has low priority, and the ABCs of intensive care are given more attention (Garrett et al., 2007). However, healthcare professionals play a vital role in promoting the use of AAC, and the first step is to provide them with sufficient knowledge about it (Garrett et al., 2007; Handberg and Voss, 2018). Training special nurses as opinion leaders or role models is a way of strengthening implementation (Holleman et al., 2014). In the ICU setting, bottom-up initiatives may enhance implementation, which was an inspiration to the initial implementation during the test phase (Bjurling‐Sjöberg et al., 2015). When repeatedly exposed to an intervention, nurses may gradually adapt it (Bartholomew Eldredge et al., 2016), which supports the notion of bottom-up implementation and role models.
Therefore, we formed a group of communication guides (n = 15) who participated in a four-hour workshop and gained deeper knowledge about communication theory, the challenges of our particular setting, how to use the strategy and tools as well as their role as communication guides. The idea was that they could support bottom-up implementation as both role models and resource persons the nurses could consult for advice in difficult situations. Also, they functioned as a communication pathway between clinical practice and the research team, being bedside observers. Nurses at all levels of experience were enrolled as communication guides; the only requirement was that they were enthusiastic about patient-centred communication and read their e-mails regularly.
6. Discussion of strengths and weaknesses
The objective of this study was to describe the process of and rationale behind the development of the ICU-COM. We had some idea about which components the bundle should contain (Holm and Dreyer, 2018b); however, the final design was not clear. We made many subjective and pragmatic decisions along the way. Rationalising afterwards, we are, of course, left with some insecurity regarding whether “we did a good enough job”. However, the MRC framework gave excellent guidance and provided us with a systematic approach that supported the development phase. We strove to follow a systematic and transparent approach to avoid the so-called ‘research waste’ that occurs when researchers ask the wrong questions, do unnecessary studies, have poor designs, fail to publish promptly or write biased or unusable reports (Chalmers and Glasziou, 2009).
In the process of examining current practices and context, we used qualitative approaches. Even though qualitative methods are recognised as very valuable data sources in complex intervention studies (Griffiths and Norman, 2013; Hallberg and Richards, 2015; Liv Fegran et al., 2014), mixed methods could have provided further insights and perspectives that we did not include, such as the number of patients who are able to use low-tech and high-tech communication tools. Also, to strengthen the contents of the communication bundle, validation of each component should be conducted.
To increase ownership of the intervention, an approach with more co-creation rather than consultation with stakeholders could have been beneficial (Greenhalgh et al., 2016). We co-produced and co-designed with the software company BlueFragments and Centre for E-learning to optimise some of the components of the bundle. However, a framework with a higher degree of inclusion of end-users and stakeholders could been applied systematically (Leask et al., 2019).
Our choice of theory was unconventional within the MRC framework. However, our particular context called for this specific type of theory that guided us in strategies and tools to optimise communication with voiceless patients. In complex interventions, behaviour change theories that may explain the actions of the nurses are often recommended (Bartholomew Eldredge et al., 2016; Bleijenberg et al., 2018). We did not include this relevant perspective. We considered the initial implementation of the intervention, but do not know if we have taken the nurses’ attitudes towards the intervention carefully enough into account. Other studies (Lavallée et al., 2019; Loft et al., 2017) have, for example, used the Behaviour Change Wheel within nursing (Michie et al., 2014). This could also have guided our study to be more specific about how to adjust the intervention to accommodate the nurses’ attitudes and preferences. The National Institute for Health and Care Excellence have published a guideline with 17 recommendations on individual-level behaviour change interventions (NICE, 2014). Even though these recommendations are not directly targeted at behaviour change of healthcare professionals but rather patients or users of the health care system, they give tangible tools that could have guided the ICU-COM development. Furthermore, Bleijenberg et al. (2018) also recommend theories that explain the mechanisms and actions of an intervention within a casual chain. Process evaluation (Moore et al., 2015), normalisation process theory (May et al., 2009) or diffusion of innovations (Rogers, 2003), which can be used to guide evaluation and implementation, could, for example, have been useful. However, as our study was a feasibility study, we chose theories that could guide us in choosing the right contents and delivery of the intervention; ACC and the Calgary Cambridge Guide were adequate for this purpose.
The generalisability of the ICU-COM intervention is, of course, limited by the fact that the material was made in Danish. We have translated the two support tools (algorithm and BASIS frame) into English for this article, but the low-tech and high-tech communication tools and the education programme exist so far only in Danish. Other cultural aspects may also have affected transferability into other contexts, for example, care and treatment practices, nurse-patient ratios, patient characteristics and demographics, the organisational structure of the ICUs and interdisciplinary teamwork. These aspects may affect the feasibility and implementation of the intervention in other countries. Also, the intervention may be too complex to be applied in developing countries.
We did not perform a cost-effectiveness analysis as recommended (Bleijenberg et al., 2018; Craig et al., 2008). This is particularly relevant to get an overview of the cost of educating all of the nurses in a large department. In another Danish hospital, a comprehensive communication skills programme for all staff with patient contact has been implemented (Ammentorp et al., 2014). Even though this is resource intensive, a similar approach may be successful in the ICU setting. However, the cost of such would, of course, be an important perspective to consider.
7. Conclusions
By using a systematic approach guided by the MRC framework, we developed the ICU-COM intervention with the aim of strengthening and supporting ICU nurses in their communication with mechanically ventilated patients. One of the ideas behind the ICU-COM was that no single intervention will improve the nurse-patient communication in the ICU; we have to combine the methods, strategies and approaches already used with good effect in clinical practice with the best available evidence in an overall intervention and a multi-component bundle. The final design of the ICU-COM is an attempt to do so. However, we do not know yet if the nurses will find the bundle acceptable to use in clinical practice and if the intervention is feasible; that study will be published at a later point.
Declaration of Competing Interest
None.
Acknowledgments
Acknowledgements
We would like to thank all the participating intensive care units at Aarhus University Hospital for their support in the study.
Funding
Aarhus University and Aarhus University Hospital funded the project.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnsa.2021.100025.
Contributor Information
Anna Holm, Email: annasoe6@rm.dk.
Veronika Karlsson, Email: veronika.karlsson@hv.se.
Lone Nikolajsen, Email: lone.nikolajsen@clin.au.dk.
Pia Dreyer, Email: piadreye@rm.dk.
Appendix. Supplementary materials
References
- Ammentorp J., Graugaard L.T., Lau M.E., Andersen T.P., Waidtløw K., Kofoed P.-.E. Mandatory communication training of all employees with patient contact. Patient Educ. Couns. 2014 doi: 10.1016/j.pec.2014.03.005. [DOI] [PubMed] [Google Scholar]
- Bartholomew Eldredge L.K., Markham C.M., Ruiter R.A.C., Kok G., Parcel G.S., Fernández M.E. John Wiley & Sons; Hoboken: 2016. Planning Health Promotion Programs: An Intervention Mapping Approach. Incorporated. [Google Scholar]
- Beukelman D.R., Garrett K.L., Yorkston K.M., editors. Augmentative Communication Strategies for Adults with Acute or Chronic Medical Conditions. Paul H. Brookes Pub. Co.; Baltimore: 2007. [Google Scholar]
- Bjurling-Sjöberg P., Wadensten B., Pöder U., Nordgren L., Jansson I. Factors affecting the implementation process of clinical pathways: a mixed method study within the context of Swedish intensive care. J. Eval. Clin. Pract. 2015;21:255–261. doi: 10.1111/jep.12301. [DOI] [PubMed] [Google Scholar]
- Blackstone S.W. Plural Publishing; San Diego, California: 2015. Patient-Provider Communication : Roles for Speech-Language Pathologists and Other Health Care Professionals. [Google Scholar]
- Bleijenberg N., de Man-van Ginkel J.M., Trappenburg J.C.A., Ettema R.G.A., Sino C.G., Heim N., Hafsteindóttir T.B., Richards D.A., Schuurmans M.J. Increasing value and reducing waste by optimizing the development of complex interventions: enriching the development phase of the Medical Research Council (MRC) Framework. Int. J. Nurs. Stud. 2018;79:86–93. doi: 10.1016/j.ijnurstu.2017.12.001. [DOI] [PubMed] [Google Scholar]
- Bright T.J., Wong A., Dhurjati R., Bristow E., Bastian L., Coeytaux R.R., Samsa G., Hasselblad V., Williams J.W., Musty M.D., Wing L., Kendrick A.S., Sanders G.D., Lobach D. Effect of clinical decision-support systems: a systematic review. Ann. Intern. Med. 2012;157:29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- Burns M.I., Baylor C.R., Morris M.A., McNalley T.E., Yorkston K.M. Training healthcare providers in patient–provider communication: what speech-language pathology and medical education can learn from one another. Aphasiology. 2012;26:673–688. doi: 10.1080/02687038.2012.676864. [DOI] [Google Scholar]
- Carruthers H., Astin F., Munro W. Which alternative communication methods are effective for voiceless patients in Intensive Care Units? A systematic review. Intensiv. Crit. Care Nurs. 2017;42:88–96. doi: 10.1016/j.iccn.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Chalmers I., Glasziou P. Avoidable waste in the production and reporting of research evidence. The Lancet. 2009;374:86–89. doi: 10.1016/S0140-6736(09)60329-9. [DOI] [PubMed] [Google Scholar]
- Choi J., Tate J.A. Evidence-based communication with critically ill older adults. Crit. Care Clin. 2021;37:233–249. doi: 10.1016/j.ccc.2020.09.002. [DOI] [PubMed] [Google Scholar]
- Colquhoun H.L., Squires J.E., Kolehmainen N., Fraser C., Grimshaw J.M. Methods for designing interventions to change healthcare professionals’ behaviour: a systematic review. Implement. Sci. 2017;12:1–12. doi: 10.1186/s13012-017-0560-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corry M., Clarke M., While A.E., Lalor J. Developing complex interventions for nursing: a critical review of key guidelines. J. Clin. Nurs. 2013;22:2366–2386. doi: 10.1111/jocn.12173. [DOI] [PubMed] [Google Scholar]
- Craig P., Dieppe P., Macintyre S., Health P., Unit S., Michie S., Nazareth I., Petticrew M. Developing and evaluating complex interventions: following considerable development in the field since 2006, MRC and NIHR have jointly commisioned and update of this guidance to be published in 2019. Med. Res. Counc. 2019 [Google Scholar]
- Craig P., D. P., M. S., M. S., N. I., P. M. Developing and evaluating complex interventions: the new medical research council guidance. BMJ Br. Med. J. 2008;337:979–983. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devabhakthuni S., Armahizer M.J., Dasta J.F., Kane-Gill S.L. Analgosedation: a paradigm shift in intensive care unit sedation practice. Ann. Pharmacother. 2012;46:530–540. doi: 10.1345/aph.1Q525. [DOI] [PubMed] [Google Scholar]
- Devlin J.W., Skrobik Y., Gélinas C., Needham D.M., Slooter A.J.C., Pandharipande P.P., Watson P.L., Weinhouse G.L., Nunnally M.E., Rochwerg B., Balas M.C., van Den Boogaard M., Bosma K.J., Brummel N.E., Chanques G., Denehy L., Drouot X., Fraser G.L., Harris J.E., Joffe A.M., Kho M.E., Kress J.P., Lanphere J.A., Mckinley S., Neufeld K.J., Pisani M.A., Payen J.-.F., Pun B.T., Puntillo K.A., Riker R.R., Robinson B.R.H., Shehabi Y., Szumita P.M., Winkelman C., Centofanti J.E., Price C., Nikayin S., Misak C.J., Flood P.D., Kiedrowski K., Alhazzani W. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit. Care Med. 2018;46:e825–e873. doi: 10.1097/CCM.0000000000003299. [DOI] [PubMed] [Google Scholar]
- Dithole K.S., Thupayagale-Tshweneagae G., Akpor O.A., Moleki M.M. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs. 2017;16:74. doi: 10.1186/s12912-017-0268-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan E., O'Cathain A., Rousseau N., Croot L., Sworn K., Turner K.M., Yardley L., Hoddinott P. Guidance for reporting intervention development studies in health research (GUIDED): an evidence-based consensus study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2019-033516. e033516–e033516. Original research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egerod I., Albarran J.W., Ring M., Blackwood B. Sedation practice in Nordic and non-Nordic ICUs: a European survey. Nurs. Crit. Care. 2013;18:166–175. doi: 10.1111/nicc.12003. [DOI] [PubMed] [Google Scholar]
- Egerod I., Bergbom I., Lindahl B., Henricson M., Granberg-Axell A., Storli S.L. The patient experience of intensive care: a meta-synthesis of Nordic studies. Int. J. Nurs. Stud. 2015;52:1354–1361. doi: 10.1016/j.ijnurstu.2015.04.017. [DOI] [PubMed] [Google Scholar]
- Everingham K., Fawcett T., Walsh T. Targeting” sedation: the lived experience of the intensive care nurse. J. Clin. Nurs. 2014;23:694–703. doi: 10.1111/jocn.12058. [DOI] [PubMed] [Google Scholar]
- Finke E.H., Light J., Kitko L. A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. J. Clin. Nurs. 2008;17:2102–2115. doi: 10.1111/j.1365-2702.2008.02373.x. [DOI] [PubMed] [Google Scholar]
- Freeman-Sanderson A., Morris K., Elkins M. Characteristics of patient communication and prevalence of communication difficulty in the intensive care unit: an observational study. Aust. Crit. Care. 2018:1–5. doi: 10.1016/j.aucc.2018.09.002. [DOI] [PubMed] [Google Scholar]
- Garrett K.L., Happ M.B., Costello J.M., Fried-Oken M.B. In: Augmentative Communication Strategies for Adults with Acute or Chronic Medical Conditions. Beukelman D.R., Garrett K.L., Yorkston K.M., editors. Paul H. Brookes Pub. Co.; Maryland, Baltimore: 2007. AAC in the Intensive Care Unit. [Google Scholar]
- Garry J., Casey K., Cole T.K., Regensburg A., McElroy C., Schneider E., Efron D., Chi A. A pilot study of eye-tracking devices in intensive care. Surgery. 2016;159:938–944. doi: 10.1016/j.surg.2015.08.012. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T., Jackson C., Shaw S., Janamian T. Achieving research impact through co-creation in community-based health services: literature review and case study. Milbank Q. 2016;94:392–429. doi: 10.1111/1468-0009.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P., Norman I. Qualitative or quantitative? Developing and evaluating complex interventions: time to end the paradigm war. Int. J. Nurs. Stud. 2013;50:583–584. doi: 10.1016/j.ijnurstu.2012.09.008. [DOI] [PubMed] [Google Scholar]
- Hallberg I., Richards D.A. Routledge; Abingdon, Oxon: 2015. Complex Interventions in health : an Overview of Research Methods. [Google Scholar]
- Handberg C., Voss A.K. Implementing augmentative and alternative communication in critical care settings: perspectives of healthcare professionals. J. Clin. Nurs. 2018;27:102–114. doi: 10.1111/jocn.13851. [DOI] [PubMed] [Google Scholar]
- Happ, M.B., 2013. Speacs-2 Communication Training Program [WWW Document]. URL http://nucleus.con.ohio-state.edu/media/speacs2/howtouse.htm (accessed 8.12.19).
- Happ M.B., Baumann B.M., Sawicki J., Tate J.A., George E.L., Barnato A.E. SPEACS-2: intensive care unit “Communication Rounds” with speech language pathology. Geriatr. Nurs. 2010;31:170–177. doi: 10.1016/j.gerinurse.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Happ M.B., Garrett K., Thomas D.D., Tate J., George E., Houze M., Radtke J., Sereika S. Nurse-patient communication interactions in the intensive care unit. Am. J. Crit. Care. 2011;20:e28–e40. doi: 10.4037/ajcc2011433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happ M.B., Garrett K.L., Tate J.A., DiVirgilio D., Houze M.P., Demirci J.R., George E., Sereika S.M. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung. 2014;43:89–98. doi: 10.1016/j.hrtlng.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happ M.B., Sereika S.M., Houze M.P., Seaman J.B., Tate J.A., Nilsen M.L., van Panhuis J., Scuilli A., Paull B., George E., Angus D.C., Barnato A.E. Quality of care and resource use among mechanically ventilated patients before and after an intervention to assist nurse-nonvocal patient communication. Hear. Lung - J. Acute Crit. Care. 2015;44:408–415.e2. doi: 10.1016/j.hrtlng.2015.07.001. [DOI] [PubMed] [Google Scholar]
- Happ M.B., Tuite P., Dobbin K., DiVirgilio-Thomas D., Kitutu J. Communication ability, method, and content among nonspeaking nonsurviving patients treated with mechanical ventilation in the intensive care unit. Am. J. Crit. Care. 2004;13:210–220. [PubMed] [Google Scholar]
- Hoddinott P. A new era for intervention development studies. Pilot Feasibility Stud. 2015;1:36. doi: 10.1186/s40814-015-0032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann T.C., Glasziou P.P., Boutron I., Milne R., Perera R., Moher D., Altman D.G., Barbour V., Macdonald H., Johnston M., Lamb S.E., Dixon-Woods M., McCulloch P., Wyatt J.C., Chan A.-.W., Michie S. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348 doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- Hoffmann T.C., Walker M.F. TIDieR-ing up’ the reporting of interventions in stroke research: the importance of knowing what is in the ‘Black Box’. Int. J. Stroke. 2015;10:657–658. doi: 10.1111/ijs.12524. [DOI] [PubMed] [Google Scholar]
- Holleman G.J., Tol M.van, Schoonhoven L., Groot J., de, Achterberg T.van. Empowering nurses to handle the guideline implementation process: identification of implementation competencies. J. Nurs. Care Qual. 2014;29:E1–E6. doi: 10.1097/NCQ.0000000000000052. [DOI] [PubMed] [Google Scholar]
- Holm A., Dreyer P. Nurse-patient communication within the context of non-sedated mechanical ventilation: a hermeneutic-phenomenological study. Nurs. Crit. Care. 2018;23:88–94. doi: 10.1111/nicc.12297. [DOI] [PubMed] [Google Scholar]
- Holm A., Dreyer P. Use of communication tools for mechanically ventilated patients in the intensive care unit. CIN Comput. Inform. Nurs. 2018;36:398–405. doi: 10.1097/CIN.0000000000000449. [DOI] [PubMed] [Google Scholar]
- Holm A., Viftrup A., Karlsson V., Nikolajsen L., Dreyer P. Nurses’ communication with mechanically ventilated patients in the intensive care unit: umbrella review. J. Adv. Nurs. 2020;76:2909–2920. doi: 10.1111/jan.14524. [DOI] [PubMed] [Google Scholar]
- Hosseini S.-.R., Valizad-Hasanloei M.-.A., Feizi A. The effect of using communication boards on ease of communication and anxiety in mechanically ventilated conscious patients admitted to intensive care units. Iran. J. Nurs. Midwifery Res. 2018;23:358–362. doi: 10.4103/ijnmr.IJNMR_68_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes C.G., Girard T.D., Pandharipande P.P. Daily sedation interruption versus targeted light sedation strategies in ICU patients. Crit. Care Med. 2013;41:S39. doi: 10.1097/CCM.0b013e3182a168c5. [DOI] [PubMed] [Google Scholar]
- Hurtig R., Downey D. Plural Publishing; San Diego: 2009. Augmentative and Alternative Communication in Acute and Critical Care Settings. [Google Scholar]
- IJssennagger C.E., Ten Hoorn S., Van Wijk A., Van den Broek J.M., Girbes A.R., Tuinman P.R. Caregivers’ perceptions towards communication with mechanically ventilated patients: the results of a multicenter survey. J. Crit. Care. 2018;48:263–268. doi: 10.1016/j.jcrc.2018.08.036. [DOI] [PubMed] [Google Scholar]
- Joanna Briggs Institute, 2014. The Joanna Briggs Institute Reviewers’ Manual 2014 Methodology for JBI Umbrella Reviews.
- Karlsen M.M.W., Heggdal K., Finset A., Heyn L.G. Attention-seeking actions by patients on mechanical ventilation in intensive care units: a phenomenological-hermeneutical study. J. Clin. Nurs. 2018:66–79. doi: 10.1111/jocn.14633. [DOI] [PubMed] [Google Scholar]
- Karlsson V., Bergbom I. ICU Professionals’ experiences of caring for conscious patients receiving MVT. West. J. Nurs. Res. 2014 doi: 10.1177/0193945914523143. [DOI] [PubMed] [Google Scholar]
- Karlsson V., Bergbom I., Forsberg A. The lived experience of adult intensive care patients who were conscious during mechanical ventilation. A phenomenological-hermeneutic study. Intensive Crit. Care Nurs. 2012;28:6. doi: 10.1016/j.iccn.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Kawamoto K., Houlihan C.A., Balas E.A., Lobach D.F. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005 doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalaila R., Zbidat W., Anwar K., Bayya A., Linton D.M., Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. Am. J. Crit. Care. 2011;20:470. doi: 10.4037/ajcc2011989. [DOI] [PubMed] [Google Scholar]
- Knapp J., Sole Lou M., Byers Fowler J. The EPICS Family Bundle and its effects on stress and coping of families of critically Ill trauma patients. Appl. Nurs. Res. 2013;26:51–57. doi: 10.1016/j.apnr.2012.11.002. S. [DOI] [PubMed] [Google Scholar]
- Koszalinski R.S., Heidel R.E., Hutson S.P., Li X., Palmer T.G., McCarthy J., Hollibush T., Massoli J., Simmons A., Jagirdar N., Velur Rajashekaran P. The use of communication technology to affect patient outcomes in the intensive care unit. Comput. Inform. Nurs. 2020;38:183–189. doi: 10.1097/CIN.0000000000000597. [DOI] [PubMed] [Google Scholar]
- Kress J.P., Pohlman A.S., O'Connor M.F., Hall J.B. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N. Engl. J. Med. 2000;342:1471. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- Kurtz S.M., Silverman J.D. The Calgary—Cambridge Referenced Observation Guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Med. Educ. 1996;30:83–89. doi: 10.1111/j.1365-2923.1996.tb00724.x. [DOI] [PubMed] [Google Scholar]
- Laerkner E., Egerod I., Hansen H.P. Nurses’ experiences of caring for critically ill, non-sedated, mechanically ventilated patients in the Intensive Care Unit: a qualitative study. Intensive Crit. care Nurs. 2015;31:196–204. doi: 10.1016/j.iccn.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Laerkner E., Stroem T., Toft P. No-sedation during mechanical ventilation: impact on patient's consciousness, nursing workload and costs. Nurs. Crit. Care. 2016;21:28–35. doi: 10.1111/nicc.12161. [DOI] [PubMed] [Google Scholar]
- Lavallée J.F., Gray T.A., Dumville J.C., Cullum N. Preventing pressure injury in nursing homes: developing a care bundle using the Behaviour Change Wheel. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-026639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leask C.F., Sandlund M., Skelton D.A., Altenburg T.M., Cardon G., Chinapaw M.J.M., De Bourdeaudhuij I., Verloigne M., Chastin S.F.M. Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Res. Involv. Engagem. 2019;5 doi: 10.1186/s40900-018-0136-9. 2–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegran L., Meyer G., Aagaard H., Ludvigsen M.S., Uhrenfeldt L., Hall E.O.C. Development of clinically meaningful complex interventions – The contribution of qualitative research. Nord. sygeplejeforskning. 2014;1:3–14. doi: 10.1024/1012-5302/a000292. [DOI] [PubMed] [Google Scholar]
- Loft M.I., Martinsen B., Esbensen B.A., Mathiesen L.L., Iversen H.K., Poulsen I. Strengthening the role and functions of nursing staff in inpatient stroke rehabilitation: developing a complex intervention using the Behaviour Change Wheel. Int. J. Qual. Stud. Health Well-being. 2017;12 doi: 10.1080/17482631.2017.1392218. 1392218–1392215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marra A., Ely E.W., Pandharipande P.P., Patel M.B. The ABCDEF bundle in critical care. Crit. Care Clin. 2017;33:225–243. doi: 10.1016/j.ccc.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C.R., Mair F., Finch T., MacFarlane A., Dowrick C., Treweek S., Rapley T., Ballini L., Ong B.N., Rogers A., Murray E., Elwyn G., Légaré F., Gunn J., Montori V.M. Development of a theory of implementation and integration: normalization process theory. Implement. Sci. 2009;4 doi: 10.1186/1748-5908-4-29. 29–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Atkins L., West R. Silverback Publishing; UK: 2014. The Behaviour Change Wheel: a Guide to Designing Interventions. [Google Scholar]
- Mirenda P., Beukelman D.R., editors. Augmentative & Alternative communication : Supporting Children and Adults with Complex Communication Needs. 4. ed. Paul H. Brookes Pub.; Baltimore: 2013. [Google Scholar]
- Moore G.F., Audrey S., Barker M., Bond L., Bonell C., Hardeman W., Moore L., O'Cathain A., Tinati T., Wight D., Baird J. Process evaluation of complex interventions: medical Research Council guidance. BMJ. 2015;350 doi: 10.1136/bmj.h1258. h1258–h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore P.M., Rivera S., Bravo-Soto G.A., Olivares C., Lawrie T.A. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst. Rev. 2018;7 doi: 10.1002/14651858.CD003751.pub4. CD003751–CD003751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE, 2014. Behaviour change: individual approaches [WWW Document]. Guideline. URL https://www.nice.org.uk/guidance/ph49/resources/behaviour-change-individual-approaches-pdf-1996366337989 (accessed 10.21.20).
- O'Cathain A., Croot L., Duncan E., Rousseau N., Sworn K., Turner K.M., Yardley L., Hoddinott P. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cathain A., Croot L., Sworn K., Duncan E., Rousseau N., Turner K., Yardley L., Hoddinott P. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud. 2019;5:41. doi: 10.1186/s40814-019-0425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otuzoğlu M., Karahan A. Determining the effectiveness of illustrated communication material for communication with intubated patients at an intensive care unit. Int. J. Nurs. Pract. 2014;20:490–498. doi: 10.1111/ijn.12190. [DOI] [PubMed] [Google Scholar]
- Patak L., Wilson-Stronks A., Costello J., Kleinpell R.M., Henneman E.A., Person C., Happ M.B. Improving patient-provider communication: a call to action. J. Nurs. Adm. 2009 doi: 10.1097/NNA.0b013e3181b414ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puntillo K., Nelson J.E., Weissman D., Curtis R., Weiss S., Frontera J., Gabriel M., Hays R., Lustbader D., Mosenthal A., Mulkerin C., Ray D., Bassett R., Boss R., Brasel K., Campbell M. Palliative care in the ICU: relief of pain, dyspnea, and thirst - A report from the IPAL-ICU Advisory Board. Intensive Care Med. 2014;40:235–248. doi: 10.1007/s00134-013-3153-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radtke J.V., Tate J.A., Happ M.B. Nurses’ perceptions of communication training in the ICU. Intensive Crit. Care Nurs. 2012;28:16–25. doi: 10.1016/j.iccn.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards D.A., Borglin G. Complex interventions and nursing: looking through a new lens at nursing research. Int. J. Nurs. Stud. 2011;48:531–533. doi: 10.1016/j.ijnurstu.2011.02.013. [DOI] [PubMed] [Google Scholar]
- Richards D.A., Coulthard V., Borglin G. The state of European nursing research: dead, alive, or chronically diseased? A systematic literature review. Worldviews Evidence-Based Nurs. 2014;11:147–155. doi: 10.1111/wvn.12039. [DOI] [PubMed] [Google Scholar]
- Rodriguez C.S., Rowe M., Thomas L., Shuster J., Koeppel B., Cairns P. Enhancing the communication of suddenly speechless critical care patients. Am. J. Crit. Care. 2016;25:e40–e47. doi: 10.4037/ajcc2016217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez C.S., Spring H.J., Rowe M. Nurses’ experiences of communicating with hospitalized, Suddenly Speechless Patients. Qual. Health Res. 2015;25:168–178. doi: 10.1177/1049732314550206. [DOI] [PubMed] [Google Scholar]
- Rogers E.M. 5th ed. Free Press; New York: 2003. Diffusion of Innovations. [Google Scholar]
- Rose L., Istanboulian L., Smith O.M., Silencieux S., Cuthbertson B.H., Amaral A.C.K.-B., Fraser I., Grey J., Dale C. Feasibility of the electrolarynx for enabling communication in the chronically critically ill: the EECCHO study. J. Crit. Care. 2018;47:109–113. doi: 10.1016/j.jcrc.2018.06.013. [DOI] [PubMed] [Google Scholar]
- Schumann J., Zellweger M.J., Valentino M., Piazzalonga S., Hoffmann A. Sexual dysfunction before and after cardiac rehabilitation. Rehabil. Res. Pract. 2010:2010. doi: 10.1155/2010/823060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selman L.E., Brighton L.J., Hawkins A., McDonald C., O'Brien S., Robinson V., Khan S.A., George R., Ramsenthaler C., Higginson I.J., Koffman J. The effect of communication skills training for generalist palliative care providers on patient-reported outcomes and clinician behaviors: a systematic review and meta-analysis. J. Pain Symptom Manag. 2017;54:404–416. doi: 10.1016/j.jpainsymman.2017.04.007. e5. [DOI] [PubMed] [Google Scholar]
- Silverman J., Kurtz S.M., Draper J. 3. ed. Radcliffe Publishing; London: 2013. Skills for Communicating with Patients. n. ed. [Google Scholar]
- Strøm T., Martinussen T., Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet. 2010;375:475–480. doi: 10.1016/S0140-6736(09)62072-9. [DOI] [PubMed] [Google Scholar]
- ten Hoorn S., Elbers P.W., Girbes A.R., Tuinman P.R. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Crit. Care. 2016;20 doi: 10.1186/s13054-016-1483-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tingsvik C., Bexell E., Andersson A.C., Henricson M. Meeting the challenge: ICU-nurses’ experiences of lightly sedated patients. Aust. Crit. Care. 2013;26:124–129. doi: 10.1016/j.aucc.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Trotta R.L., Hermann R.M., Polomano R.C., Happ M.B. Improving nonvocal critical care patients’ ease of communication using a modified SPEACS-2 program. J. Healthc. Qual. 2020;42:E1–E9. doi: 10.1097/JHQ.0000000000000163. [DOI] [PubMed] [Google Scholar]
- Tsuyada H., Inoue S., Tsujimoto T., Ogawa T., Inada M., Kawaguchi M. Impact of nursing experience on cancellation of light sedation for mechanically ventilated patients in a setting of 1 : 2 nurse-patient ratio. Anaesthesiol. Intensive Ther. 2019;51:210–217. doi: 10.5114/ait.2019.87359. [DOI] [PubMed] [Google Scholar]
- Vincent J.L., Shehabi Y., Walsh T.S., Pandharipande P.P., Ball J.A., Spronk P., Longrois D., Strøm T., Conti G., Funk G.C., Badenes R., Mantz J., Spies C., Takala J. Comfort and patient-centred care without excessive sedation: the eCASH concept. Intensive Care Med. 2016;42:962–971. doi: 10.1007/s00134-016-4297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamato T., Maher C., Saragiotto B., Moseley A., Hoffmann T., Elkins M., Petersen S., Riley S., Brismée J.M. Improving completeness and transparency of reporting in clinical trials using the template for intervention description and replication (TIDieR) checklist will benefit the physiotherapy profession. J. Man. Manip. Ther. 2016;24:183–184. doi: 10.1080/10669817.2016.1210343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaga C.J., Berney S., Vogel A.P. The feasibility, utility, and safety of communication interventions with mechanically ventilated intensive care unit patients: a systematic review. Am. J. Speech-Language Pathol. 2019;28:1335–1355. doi: 10.1044/2019_AJSLP-19-0001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.