In a recent publication(1) Grandin et al reported that mechanical unloading of the left ventricle (LV) during peripheral veno-arterial extracorporeal membrane oxygenation (ECMO) is associated with lower mortality. The use of additional mechanical unloading devices to vent the LV inarguably increases the complexity and the rate of complications of ECMO support, as evidenced by higher complication rates. Hence, the benefits of this therapeutic choice should clearly outweigh its associated risks and indiscriminate utilization should be avoided. Rather than contemplating which device to use, the initial assessment should focus on whether mechanical unloading is needed at all after careful assessment of the patient’s acute shock hemodynamic state. Additionally, the use of mechanical LV unloading in the first 24–72h post ECMO should be limited to cases where increased risks of left-side thrombus formation or development of pulmonary edema have been identified and supported by the acute hemodynamic and clinical profile. At our institution, an Acute Shock ECMO Phenotype (ASEP) protocol is utilized to categorize which patients may benefit from LV venting with an intra-aortic balloon pump (IABP) or percutaneous ventricular assist device (pVAD) while on ECMO support (Figure 1). This assessment allows developing tailored strategy to prevent the clinical complications of reduced blood flow through the LV (formation of thrombi or development of pulmonary edema). In our protocol, we consider the first 12h post-ECMO insertion as a “blanking period” where we do not consider LV venting to give patients sufficient time to reach a steady state. During the following 12 to 72h, the decision to place a LV vent is based on the periodical (every 12h) assessment of the following conditions: A) absent aortic valve opening; B) arterial pulse pressure value <15 mmHg; and C) wedge pressure value >30 mmHg. If two or more of these criteria are present, a trial of low dose dobutamine infusion (2.5 – 5 μg/kg/min) is attempted and the patient is monitored for 2h: in case of lack of improvement, we eventually proceed to a device such as IABP or pVAD for LV venting.
Figure 1. Acute Shock ECMO Phenotype Protocol.
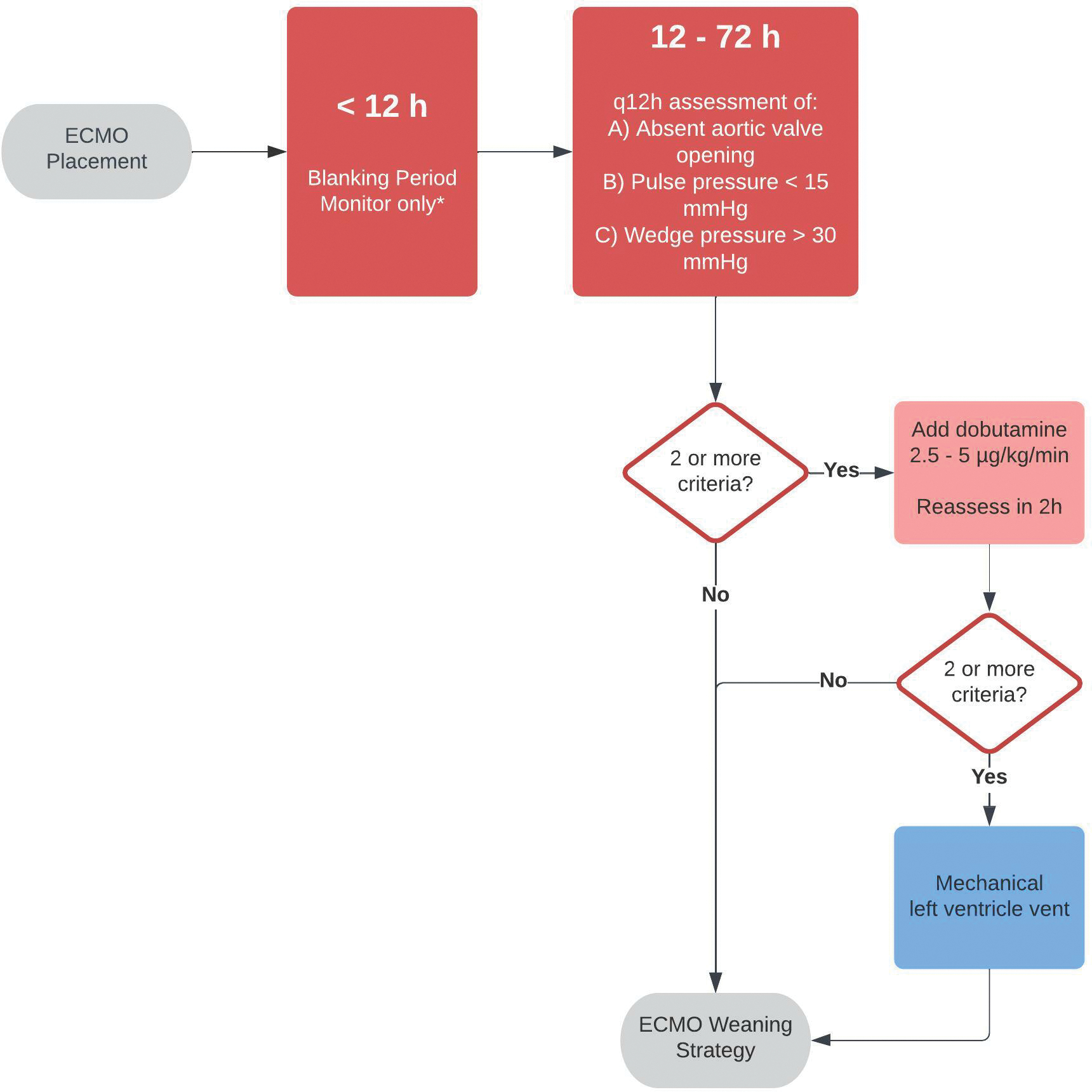
Left ventricle vent decision protocol. ECMO = extracorporeal membrane oxygenation. *= Exceptions if ECMO placed in cathlab and comprehensive assessment / ventricular standstill indicates need for immediate vent.
Figure 1: Left ventricle vent decision protocol
Funding:
Dr Jorde is supported by the McAdam Family Foundation. Dr Castagna is supported by a grant from the National Institute for Health (T32HL144456) and the National Center for Advancing Translational Science (NCATS) Clinical and Translational Science Award at Einstein-Montefiore (UL1TR001073). Dr Saeed is supported by grants from the National Institute for Health/National Heart, Lung and Blood Institute (K23HL145140) and the National Center for Advancing Translational Science (NCATS) Clinical and Translational Science Award at Einstein-Montefiore (UL1TR001073).
Footnotes
Disclosures: No conflicts of interest exist
Reference
- 1.Grandin EW, Nunez JI, Willar B et al. Mechanical Left Ventricular Unloading in Patients Undergoing Venoarterial Extracorporeal Membrane Oxygenation. Journal of the American College of Cardiology 2022;79:1239–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]


