Abstract
Background:
Individuals with limited English proficiency (LEP) have long faced barriers in navigating the health care system. More information is needed to understand whether their care was limited further during the early period of the COVID-19 pandemic.
Objective:
To assess the impact of English proficiency on delayed and forgone health care during the early COVID-19 pandemic.
Research Design:
Multivariate logistic regression analysis of National Health Interview Survey data (July–December 2020; n=16,941). Outcomes were self-reported delayed and forgone health care because of cost or the COVID-19 pandemic. Delayed health care included medical, dental, mental health, and pharmacy care. Forgone health care also included care at home from a health professional.
Results:
A greater percentage of LEP adults reported delayed (49%) and forgone (41%) health care than English-proficient adults (40% and 30%, respectively). However, English proficiency was not significantly associated with delayed or forgone health care, after adjusting for demographic, socioeconomic, and health factors. Among LEP adults, multivariate models showed that being uninsured, having a disability, and having chronic conditions increased the risk of delaying and forgoing health care. LEP adults of Asian race and Hispanic ethnicity were also more likely to forgo health care while those with 65+ years were less likely to forgo health care.
Conclusions:
Adults with LEP were more likely to experience challenges accessing health care early in the pandemic. Delayed and forgone health care were explained by low socioeconomic status and poor health. These findings highlight how during a period of limited health resources, deficiencies in the health care system resulted in an already disadvantaged group being at greater risk of inequitable access to care.
Key Words: delayed and forgone care, language, disparities, access to care
Over 25 million individuals in the United States (or 8% of the population) are described as having limited English proficiency (LEP), or as speaking English “less than very well.”1 These individuals have long encountered a unique set of challenges when accessing health care. Compared to individuals with English proficiency (EP), LEP individuals have significantly worse access and care, including greater difficulty gaining insurance coverage, being less likely to receive preventive care, and more likely to have preventable emergency department visits.2–4
The COVID-19 pandemic amplified the challenges that many individuals face in accessing health care. The percentage of US adults experiencing delayed or forgone medical care during early in the pandemic was estimated to be between 25% to 40%, compared with 8%–14% before the pandemic.5–13 Postponed or skipped care may increase the risk of morbidity and mortality, particularly among those with chronic health conditions; worsening health conditions can also limit the ability to work or perform other daily activities.9 Reductions in access to care were found to be worse among traditionally underserved populations such as people with disabilities and racial and ethnic minorities.6–8
Previous studies have largely focused on access to medical care, yet the pandemic disrupted all aspects of the health care system. Few studies have explored the extent of delayed and forgone health care across different types of health care services during the pandemic9,10 and none have examined the experiences among individuals with LEP. To address these gaps, we aimed to assess the impact of English language proficiency on delayed and forgone health care across several services (ie, medical, dental, mental health, pharmacy, and home care) during the early COVID-19 pandemic, using a nationally representative sample. Our primary research questions were whether there was an association between English proficiency and delayed and forgone health care; and what factors were associated with delayed and forgone health care among LEP adults. We hypothesized that during the early period of the COVID-19 pandemic, LEP adults had significantly more delayed and forgone health care than English proficiency adults. As a group that has long faced longstanding barriers in accessing care and subsequent disparities in health outcomes, it is important to understand health care access among LEP adults during the pandemic to better develop strategies to address their health care needs in future crises.
METHODS
Data and Sample
Data were from adult respondents to the 2020 National Health Interview Survey (NHIS) collected during July–December 2020. NHIS is a nationally representative, cross-sectional household survey of the civilian, noninstitutionalized US population.14 The COVID-19 pandemic necessitated changes to data collection.15 Interviews were typically conducted in person with a telephone follow-up visit; 2020 interviews were conducted over the telephone first with limited in-person follow-up visits. The 2020 response rate was 48.9% (compared to 59.1% in 2019).15,16 The analytic sample included 16,941 adult respondents aged 18 years and older who were interviewed in the third and fourth quarter of 2020 and had data on all measures of interest. All study variables had <5% missing. This study was determined to be not Human Subjects Research by the Advocate Aurora Health Institutional Review Board.
Measures
Our main outcomes were 2 dichotomous measures, self-reported delayed and forgone health care. Delayed health care was a composite measure constructed from respondents who answered yes to a delay in medical care, dental care, mental health care, or prescriptions due to cost in the past 12 months or the coronavirus pandemic. Similarly, forgone health care was constructed from respondents who answered yes to not getting medical care, dental care, mental health care, prescriptions, or home care due to cost in the past 12 months or the coronavirus pandemic. Questions related to the pandemic were added in July 2020.15 All questions were asked to all adults except delays in filling prescriptions due to cost was asked only from respondents who had taken prescription medication in the past 12 months. Full question texts can be found in Appendix A, Supplemental Digital Content 1, http://links.lww.com/MLR/C775.
The key independent variable was English proficiency (proficient vs. limited proficiency). Respondents were categorized as limited proficiency if their interview was conducted in Spanish, both English and Spanish, or some other language. Interview language has commonly been used as a proxy for English proficiency in the health care access and utilization literature.11,17
Covariates included demographic, socioeconomic, and health characteristics. Covariates included: race and ethnicity (non-Hispanic White, Hispanic, non-Hispanic Asian, non-Hispanic Other), age (18–44, 45–64, ≥65 years), sex (male, female), education (college degree or higher, some college, high school diploma, less than high school diploma), poverty status [family income <100% of federal poverty level (FPL), 100%–199% FPL, ≥200% FPL], insurance (private, public, uninsured), worked last week (yes, no), and having any one of 6 common chronic conditions (arthritis, cancer, congestive heart disease, diabetes, hypertension, high cholesterol). Respondents were considered to have a usual place of care if they responded to having one or more places. The presence of a disability (yes or no) was included using the Washington Group Short Set Composite Disability Indicator. We did not control for overall health status because the measure has been found to be susceptible to cultural bias among Asian and Latinx populations.18
Statistical Analysis
We conducted descriptive and multivariate analyses. Descriptive statistics were produced to understand differences in characteristics between LEP and English proficiency groups. We conducted bivariate analyses using χ2 tests to compare the distribution of the outcomes and other characteristics. We then performed 2 analyses using multivariate logistic regression models. The first analysis assessed the association between English proficiency and delayed and forgone health care. In the second analysis, we separately modeled characteristics associated with delayed and forgone health care in the LEP and English proficiency groups.
All analyses were conducted using Stata version 17.0 (Stata Corporation) and used statistical methods to account for the complex survey design (ie, weighting). Two-sided P<0.05 was considered statistically significant.
RESULTS
Descriptive Characteristics
The 16,941 respondents in our sample represented over 223 million adults nationally. Approximately 7% of respondents, representing over 16 million adults, were identified as LEP. A greater percentage of LEP adults were between 45 and 64 years, were Hispanic or Asian, had less education, were poorer, had public insurance or were uninsured, had not worked last week, and did not have a usual place of care (Table 1). We observed no differences by sex, having a disability, or having one or more chronic conditions.
TABLE 1.
Demographic, Socioeconomic, and Health Characteristics of Adult Respondents in the United States, by English Proficiency, National Health Interview Survey, July–December 2020
| Total (N=16,941) | English proficient (N=16,257) | Limited English proficient* (N=684) | ||
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | P | |
| Age | P=0.009 | |||
| 18–44 years | 45.7 (44.6, 46.9) | 45.7 (44.5, 46.9) | 45.7 (41.2, 50.2) | |
| 45–64 years | 32.5 (31.6, 33.4) | 32.1 (31.2, 33.1) | 37.4 (32.9, 42.1) | |
| 65+ years | 21.8 (21.0, 22.6) | 22.1 (21.3, 23.0) | 16.9 (14.0, 20.3) | |
| Male | 48.2 (47.2, 49.2) | 48.3 (47.2, 49.3) | 46.8 (42.4, 51.3) | P=0.54 |
| Race and ethnicity | P<0.001 | |||
| Non-Hispanic White | 63.5 (61.6, 65.4) | 68.1 (66.4, 69.7) | 1.7 (0.9, 3.1) | |
| Hispanic | 16.7 (15.1, 18.4) | 11.4 (10.3, 12.6) | 88.5 (84.6, 91.5) | |
| Non-Hispanic Asian | 5.9 (5.2, 6.6) | 5.6 (5.0, 6.4) | 9.0 (6.3, 12.8) | |
| Non-Hispanic Other† | 14.0 (12.9, 15.1) | 14.9 (13.8, 16.1) | 0.8 (0.3, 2.1) | |
| Education | P<0.001 | |||
| College degree or higher | 30.2 (29.1, 31.3) | 31.8 (30.7, 32.9) | 8.1 (5.9, 10.9) | |
| Some college | 29.8 (28.8, 30.8) | 31.1 (30.1, 32.1) | 12.1 (9.4, 15.5) | |
| High school diploma | 28.9 (27.9, 30.0) | 29.0 (27.9, 30.1) | 28.3 (24.1, 33.0) | |
| Less than high school diploma | 11.1 (10.2, 12.1) | 8.1 (7.4, 8.9) | 51.5 (46.4, 56.5) | |
| Poverty status | P<0.001 | |||
| ≥200% FPL | 71.5 (70.2, 72.7) | 74.3 (73.1, 75.5) | 33.5 (29.0, 38.3) | |
| 100%–199% FPL | 18.3 (17.4, 19.3) | 17.1 (16.2, 18.1) | 35.0 (30.9, 39.3) | |
| <100% FPL | 10.2 (9.4, 11.0) | 8.6 (7.9, 9.3) | 31.5 (27.0, 36.5) | |
| Insurance | P<0.001 | |||
| Private | 67.1 (65.9, 68.4) | 69.8 (68.6, 71.0) | 30.1 (25.8, 34.8) | |
| Public | 21.7 (20.7, 22.7) | 21.0 (20.0, 22.0) | 31.4 (27.4, 35.7) | |
| Uninsured | 11.2 (10.3, 12.1) | 9.2 (8.4, 10.0) | 38.5 (34.1, 43.0) | |
| Worked last week | P<0.001 | |||
| Yes | 61.3 (60.3, 62.4) | 61.9 (60.9, 63.0) | 53.2 (48.5, 57.8) | |
| No | 38.7 (37.6, 39.7) | 38.1 (37.0, 39.1) | 46.8 (42.2, 51.5) | |
| Has a disability | 8.2 (7.6, 8.7) | 8.1 (7.6, 8.7) | 8.6 (6.4, 11.5) | P=0.72 |
| Has ≥1 chronic condition | 51.5 (50.4, 52.6) | 51.7 (50.6, 52.8) | 49.2 (44.3, 54.1) | P=0.33 |
| Has a usual place of care | 89.9 (89.2, 90.6) | 90.4 (89.6, 91.1) | 84.0 (80.3, 87.2) | P<0.001 |
Respondents with limited English proficiency were identified using the language they used to respond to the survey.
Non-Hispanic Other includes respondents who self-identified as Black/African American, American Indian/Alaska Native, and other single and multiple races.
FPL indicates federal poverty level.
Data Source: National Center for Health Statistics, National Health Interview Survey, 2020.
LEP and English proficiency adults were markedly different in several demographic and socioeconomic characteristics. Almost all LEP adults were Hispanic (88.5%) or Asian (9.0%) while most English proficiency adults were White (68.1%). LEP adults also had much lower levels of educational attainment and income. More than half of LEP adults (51.5%) had less than a high school diploma, which is more than 6 times greater than English proficiency adults (8.1%). Almost one-third (31.5%) of LEP adults had an income below the FPL compared to only 8.6% of English proficiency adults. In addition, 38.5% of LEP adults were uninsured and 31.4% had public insurance compared to 9.2% and 21.0% of English proficiency adults, respectively. Finally, a smaller percentage of LEP adults reported a usual place of care (84.0%) compared to English proficiency adults (90.4%).
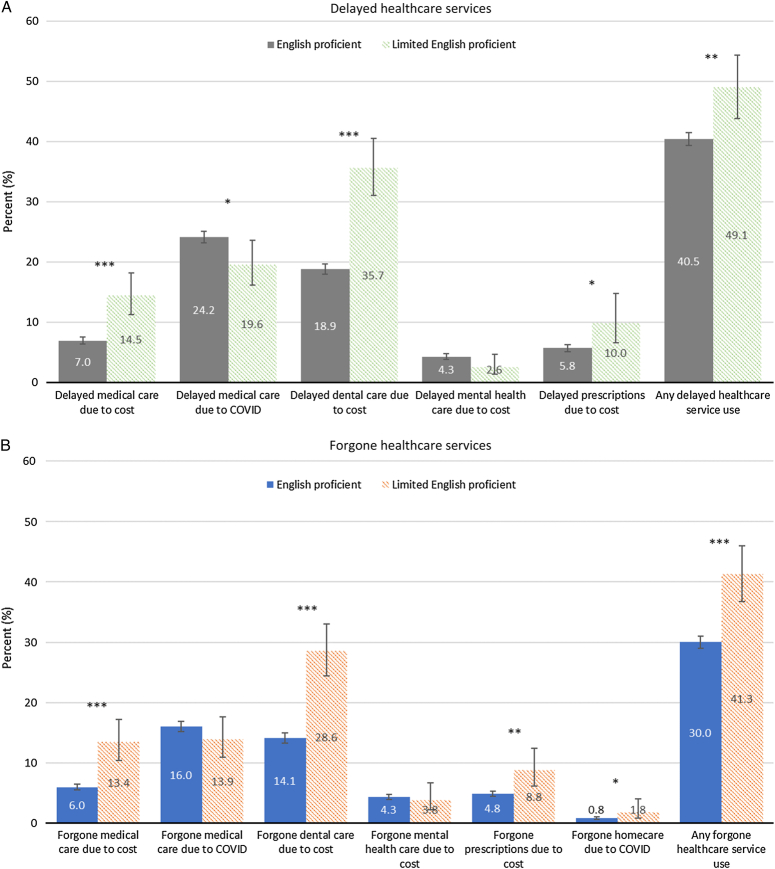
Differences in Delayed and Forgone Health Care
In aggregate, 44.9% of adults reported delaying or forgoing health care during the pandemic (41.1% reported delayed health care and 30.8% reported forgone health care). Descriptive analyses showed many statistically significant differences between LEP and English proficiency adults (54.1% of LEP adults and 44.2% of English proficiency adults reported delaying or forgoing health care, P<0.001). LEP adults reported a significantly higher proportion of both delayed and forgone health care compared to English proficiency adults (delayed: 49.1% and 40.5%, P<0.01; forgone: 41.3% and 30.0%, P<0.001) (Figs. 1A, B). Among specific measures of delayed health care (Fig. 1A), LEP adults were significantly more likely than English proficiency adults to report delays in medical care due to cost (14.5% vs. 7.0%), dental care due to cost (35.7% vs. 18.9%), and prescriptions due to cost (10.0% vs. 5.8%) while LEP adults were significantly less likely than English proficiency adults to report delays in medical care due to the pandemic (19.6% vs. 24.2%). Similarly, LEP adults were also significantly more likely than English proficiency adults to report forgone medical care due to cost, dental care due to cost, prescriptions due to cost, and home care due to the pandemic (Fig. 1B). There were no significant differences between LEP and English proficiency adults reports of forgone medical care due to the pandemic or delayed or forgone mental health care due to cost.
FIGURE 1.
Delayed and forgone health care services, by English proficiency, National Health Interview Survey, July–December 2020. (A) Delayed Health Care Services. (B) Foregone Health Care Services. *P<0.05, **P<0.01, ***P<0.001. Data Source: National Center for Health Statistics, National Health Interview Survey, 2020.
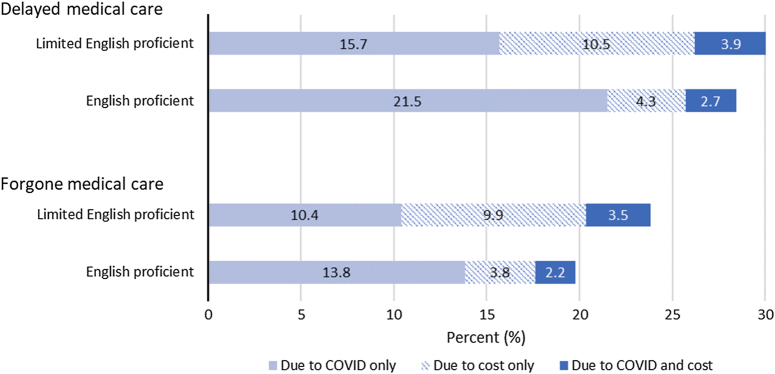
While similar percentages of LEP and English proficiency adults reported delayed medical care (due to costs or the pandemic; 30.1% and 28.5%, P=0.46), a greater percentage of LEP adults reported forgone medical care (23.8% and 19.8%, P=0.04). Reasons for delayed and forgone medical care also differed (Fig. 2). A greater percentage of LEP adults reported cost as the sole reason for delaying (10.5%) and forgoing (9.9%) medical care compared to English proficiency adults (4.3% and 3.8%, respectively). In contrast, a greater proportion of English proficiency adults reported the pandemic as the sole reason for both delaying (21.5% vs. 15.7% for LEP adults) and forgoing medical care (13.8% vs. 10.4%).
FIGURE 2.
Reasons for delayed and forgone medical care, by English proficiency, National Health Interview Survey, July–December 2020. Data Source: National Center for Health Statistics, National Health Interview Survey, 2020.
Unadjusted and Multivariate Associations With Delayed and Forgone Health Care Use for Adults With Limited English Proficiency
Table 2 presents the unadjusted and multivariate associations in delayed and forgone health care by English proficiency. Unadjusted logistic regression showed that compared to English proficiency adults, LEP adults had significantly greater odds of delaying prescriptions, medical care, and dental care because of costs and significantly lower odds of delaying medical care due to the pandemic. This resulted in LEP having greater odds of delaying health care in aggregate [odds ratio (OR)=1.42, 95% CI: 1.14, 1.77). Similar associations were seen in forgone health care; LEP adults had significantly greater odds of forgoing needed health care (OR: 1.64, 95% CI: 1.35, 1.99) due to their greater odds of forgoing medical care, dental care, prescriptions, and home care due to costs. After controlling for demographic, socioeconomic, and health characteristics, the relationships between English proficiency and delayed and forgone health care were no longer statistically significant.
TABLE 2.
Relationship Between Delay and Forgone Health Care Use Outcomes and English Proficiency (Reference English Proficient) Among Adult Respondents, National Health Interview Survey, July–December 2020
| Limited English proficient (reference: English proficient), OR (95% CI) | ||
|---|---|---|
| Outcome | Unadjusted odds ratio | Adjusted odds ratio |
| Delayed health care service use | 1.42 (1.14, 1.77)** | 1.17 (0.89, 1.55) |
| Delayed medical care due to costs | 2.26 (1.67, 3.05)*** | 1.05 (0.71, 1.55) |
| Delayed medical care due to COVID-19 | 0.77 (0.60, 0.97)* | 1.17 (0.87, 1.56) |
| Delayed dental care due to costs | 2.39 (1.92, 2.97)*** | 1.09 (0.82, 1.46) |
| Delayed mental health care due to costs | 0.59 (0.31, 1.12) | 0.65 (0.31, 1.35) |
| Delayed prescriptions due to costs | 1.71 (1.07, 2.74)* | 0.98 (0.56, 1.73) |
| Forgone health care service use | 1.64 (1.35, 1.99)*** | 1.16 (0.88, 1.52) |
| Forgone medical care due to costs | 2.45 (1.82, 3.31)*** | 1.25 (0.85, 1.83) |
| Forgone medical care due to COVID-19 | 0.85 (0.64, 1.12) | 0.91 (0.63, 1.32) |
| Forgone dental care due to costs | 2.43 (1.94, 3.05)*** | 1.06 (0.79, 1.43) |
| Forgone mental health care due to costs | 0.88 (0.48, 1.60) | 0.86 (0.43, 1.73) |
| Forgone prescriptions due to costs | 1.89 (1.26, 2.83)** | 1.12 (0.66, 1.89) |
| Forgone home care due to COVID-19 | 2.40 (1.02, 5.66)* | 1.52 (0.55, 4.24) |
P<0.05.
P<0.01.
P<0.001.
Adjusted models controlled for race and ethnicity, age, sex, education, poverty status, insurance, employment, disability status, chronic condition, and usual place of care.
OR indicates odds ratio.
English Proficiency-Specific Associations With Delayed and Forgone Health Care Service Use
Multivariate analyses showed that among LEP adults, insurance, having a disability, and chronic conditions were significantly associated with reports of both delayed and forgone health care (Table 3). Specifically, LEP adults without insurance had greater odds of reporting delayed health care [adjusted odds ratio (aOR): 4.32, 95% CI: 2.39, 7.84] and forgone health care (aOR: 2.98, 95% CI: 1.63, 5.46) than those with private insurance; LEP adults with public insurance also had greater odds of delayed health care (aOR: 2.02, 95% CI: 1.16, 3.53). Similarly, compared to LEP adults without a disability or chronic conditions, LEP adults with a disability and chronic conditions had greater odds of reporting delayed [disability (aOR: 1.92, 95% CI: 1.00, 3.66); chronic conditions (aOR: 2.42, 95% CI: 1.49, 3.93)] and forgone [disability (aOR: 1.85, 95% CI: 1.01, 3.39); chronic conditions (aOR: 3.15, 95% CI: 1.83, 5.41)] health care. In addition, race/ethnicity and age were also associated with reports of any forgone health care among LEP adults. Hispanic (aOR: 6.90, 95% CI: 1.71, 27.86) and Asian (aOR: 6.71; 95% CI: 1.36, 33.18) LEP adults had greater odds of forgoing any health care service use than White, non-Hispanic LEP adults, while adults 65+ years had lower odds than adults 18–44 years (aOR: 0.46; 95% CI: 0.23, 0.94).
TABLE 3.
Adjusted English Proficiency-Specific Associations With Delayed and Forgone Health Care Among Adults, National Health Interview Survey, July–December 2020
| Adjusted odds ratio (95% CI) | ||||
|---|---|---|---|---|
| Delay in health care services | Forgone health care services | |||
| Limited English proficient | English proficient | Limited English proficient | English proficient | |
| Race and ethnicity | ||||
| Non-Hispanic White | Reference | Reference | Reference | Reference |
| Hispanic | 0.95 (0.31, 2.90) | 0.97 (0.83, 1.13) | 6.90 (1.71, 27.86)** | 1.07 (0.89, 1.28) |
| Non-Hispanic Asian | 1.10 (0.31, 3.97) | 0.64 (0.52, 0.79)*** | 6.71 (1.36, 33.18)* | 0.64 (0.51, 0.80)*** |
| Non-Hispanic Other | 0.51 (0.04, 6.91) | 0.95 (0.83, 1.09) | 2.88 (0.21, 38.94) | 1.17 (1.01, 1.35)* |
| Age | ||||
| 18–44 years | Reference | Reference | Reference | Reference |
| 45–64 years | 1.10 (0.68, 1.79) | 1.06 (0.95, 1.18) | 1.05 (0.4, 1.74) | 0.97 (0.87, 1.09) |
| 65+ years | 0.56 (0.28, 1.12) | 0.62 (0.53, 0.72)*** | 0.46 (0.23, 0.94)* | 0.48 (0.41, 0.57)*** |
| Sex | ||||
| Male | Reference | Reference | Reference | Reference |
| Female | 1.28 (0.85, 1.93) | 1.59 (1.46, 1.74)*** | 1.31 (0.88, 1.93) | 1.54 (1.40, 1.69)*** |
| Education | ||||
| College degree or higher | Reference | Reference | Reference | Reference |
| Some college | 1.48 (0.63, 3.43) | 0.79 (0.71, 0.87)*** | 1.29 (0.49, 3.42) | 0.94 (0.83, 1.05) |
| High school diploma | 0.92 (0.39, 2.13) | 0.67 (0.60, 0.75)*** | 1.09 (0.45, 2.66) | 0.77 (0.67, 0.87)*** |
| Less than high school diploma | 0.77 (0.35, 1.67) | 0.58 (0.47, 0.71)*** | 0.89 (0.37, 2.13) | 0.65 (0.53, 0.81)*** |
| Poverty status | ||||
| ≥200% FPL | Reference | Reference | Reference | Reference |
| 100%–199% FPL | 0.93 (0.56, 1.56) | 1.37 (1.20, 1.56)*** | 1.06 (0.65, 1.72) | 1.64 (1.42, 1.89)*** |
| <100% FPL | 1.12 (0.65, 1.94) | 1.33 (1.10, 1.59)** | 1.54 (0.88, 2.68) | 1.51 (1.24, 1.82)*** |
| Insurance | ||||
| Private | Reference | Reference | Reference | Reference |
| Public | 2.02 (1.16, 3.53)* | 1.24 (1.09, 1.41)** | 1.22 (0.66, 2.26) | 1.34 (1.17, 1.54)*** |
| Not insured | 4.32 (2.39, 7.84)*** | 2.33 (1.92, 2.82)*** | 2.98 (1.63, 5.46)*** | 2.37 (1.95, 2.86)*** |
| Worked last week | ||||
| Yes | Reference | Reference | Reference | Reference |
| No | 0.80 (0.49, 1.28) | 0.92 (0.82, 1.03) | 0.72 (0.45, 1.16) | 0.98 (0.87, 1.11) |
| Disability | ||||
| No disability | Reference | Reference | Reference | Reference |
| Has a disability | 1.92 (1.00, 3.66)* | 1.93 (1.67, 2.22)*** | 1.85 (1.01, 3.39)* | 2.23 (1.92, 2.59)*** |
| Has ≥1 chronic condition | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 2.42 (1.49, 3.93)*** | 1.71 (1.53, 1.90)*** | 3.15 (1.83, 5.41)*** | 1.88 (1.67, 2.12)*** |
| Has a usual place of care | ||||
| Has a usual place of care | Reference | Reference | Reference | Reference |
| No usual place of care | 1.25 (0.73, 2.13) | 1.29 (1.08, 1.54)** | 0.97 (0.50, 1.88) | 1.25 (1.03, 1.53)* |
P<0.05.
P<0.01.
P<0.00.
FPL indicates federal poverty level.
Data Source: National Center for Health Statistics, National Health Interview Survey, 2020.
Among English proficiency adults, experiencing delayed health care varied across multiple factors. Like LEP adults, English proficiency adults who were uninsured (aOR: 2.33, 95% CI: 1.92, 2.82) or had public insurance (aOR: 1.24, 95% CI: 1.09, 1.41), had a disability (aOR: 1.93, 95% CI: 1.67, 2.22), and one or more chronic conditions (aOR: 1.71, 95% CI: 1.53, 1.90) had greater odds of delaying health care than English proficiency adults who had private insurance, no disabilities, and no chronic conditions, respectively. In addition, English proficiency adults who were Asian (aOR: 0.64, 95% CI: 0.52, 0.79), 65+ years (aOR: 0.62, 95% CI: 0.53, 0.72), and lower education levels had lower odds of delaying health care than their respective English proficiency adult counterparts. In contrast, English proficiency adults who were female (aOR: 1.59, 95% CI: 1.46, 1.74), had lower family income [less than 100% FPL (aOR: 1.33, 95% CI: 1.10, 1.59); between 100% and 199% FPL (aOR: 1.37, 95% CI: 1.20, 1.56)], and did not have a usual place of care (aOR: 1.29, 95% CI: 1.08, 1.54) had greater odds of delaying health care than their respective English proficiency adult counterparts.
The associations in delayed health care for English proficiency adults translated to similar associations in significance, magnitude, and direction to forgone health care for almost all characteristics (Table 3).
DISCUSSION
Using a nationally representative sample of US adults, this study examined differences in delayed and forgone health care services by English proficiency, early in the COVID-19 pandemic. We found that while 45% of all adults experienced delayed or forgone health care during the period, a significantly greater percentage of LEP adults experienced delayed or forgone health care (54%) compared to English proficiency adults (44%). The differences between the two groups were explained by differences in their health, socioeconomic status, and demographic characteristics. For LEP adults, insurance, health (ie, having a disability or a chronic condition), race and ethnicity, and age were significantly associated with delayed and forgone health care.
The study findings showed that almost half of all adults put off or missed health care during the early period of the COVID-19 pandemic and that the pandemic disproportionately affected LEP adults compared to English proficiency adults. Previous studies examining a range of health care services found that 36%–38% of adults had delayed or forgone health care in 2020.9,10 Our findings are higher than previous reports conducted during this period, likely because we included a greater range of health care services and reasons.
Consistent with earlier studies,9,10 dental care was the most frequently delayed or forgone service for LEP adults, while medical care was the most frequently delayed or forgone service for English proficiency adults. Access to dental care was particularly exacerbated among LEP adults during the pandemic; our study found 29% of LEP adults did not receive needed dental care compared to the previously reported 13% among nonelderly adults.13,19 Avoiding needed dental care can have adverse effects on general health and will contribute to future health care costs.19 Notably, the percentages of LEP and English proficiency adults who reported delayed and forgone mental health care were low and not significantly different; the percentages reported here are lower than the 6% previously reported by Gonzalez et al.9
Our inclusion of both cost-related and pandemic-related delayed or forgone health care is particularly important for LEP adults and other disadvantaged populations because the pandemic impacted all aspects of life, including the economy. Previous studies identified the financial repercussions of the pandemic as one of the main reasons why people forwent care.5 Similarly, our finding that 10% of LEP adults forwent medical care solely based on costs compared to 4% of English proficiency adults reinforces that cost continued to be a greater barrier to medical care for disadvantaged populations during the pandemic. LEP adults were primarily employed in low-paying jobs where high levels of English were not required.20 During the pandemic, many of the jobs employing a large percentage of LEP adults disappeared (eg, cleaning and maintenance, food preparation, and personal care and service).20,21 In addition, limited eligibility for health insurance, and sanctions imposed for the use of public programs early in the pandemic, further inhibited insurance coverage among immigrant adults.22,23 Understanding the dual reasons for delaying and forgoing health care is necessary for gaining a complete picture of how the pandemic impacted health care access.
Contrary to our hypothesis, after adjustment for potential confounding, there was no difference in delayed or forgone health care between LEP and English proficiency adults. While surprising given the large unadjusted differences, like Shi et al11, we hypothesize that LEP adults may have had other characteristics not accounted for in the study that may have led them to have a lower perceived need for health care services or to assess delays or forgone health care less severely than English proficiency adults. For example, accurate, translated public health information about COVID-19 was lacking during the early period of the pandemic; this may have limited LEP adults’ sense of risk of COVID-19 and their perceived need for health care services.24,25 Finally, LEP patients may access care differently based on their cultural habits or preferences from their home country.26,27 Since many of these cultural preferences are not captured in survey data, follow-up research is needed to understand how these differences may have influenced delayed and forgone health care during this time.
While factors associated with delayed and forgone care were mixed among previous studies assessing LEP populations,11,12 the proficiency-specific multivariate results suggested that delayed and forgone health care among LEP adults were driven by lack of insurance, poor health (ie, having a disability or a chronic condition), Asian race, and Hispanic ethnicity. Particularly, more research is needed to understand why while Asian English proficiency adults were less likely to forgo health care, Asian LEP adults were more likely to forgo health care than their White counterparts during the pandemic. While this finding likely partially reflects the differential levels of health care access and use between US-born and foreign-born Asian Americans,28,29 it is unclear whether this difference arises from differences in care-seeking behavior or perceived need or risk.
The high prevalence of delayed and forgone health care including medical, dental, and pharmacy care observed among LEP adults during the early period of the pandemic underscores the pressing need for policymakers, health care systems, payers, and other stakeholders to develop strategies now that would help protect against differences in access to health care for LEP individuals during future health crises. Postponing or missing needed services has long-term implications on the health and well-being of LEP individuals and the health care system. Having both health insurance and a regular primary care provider (or usual source of care) are essential for ensuring individuals have timely access to health care.30 This study found that almost 40% of LEP adults were uninsured and over 30% were on public insurance during the early pandemic period. Specifically, millions of LEP individuals are expected to lose insurance coverage with the ending of the Medicaid continuous enrollment provision on March 31, 2023, and policymakers to community organizations will need to help ensure eligible LEP individuals maintain Medicaid coverage or transition to other coverage.31 Crucial to the efforts to improve access will be providing culturally and linguistically appropriate public health outreach and education campaigns and direct language assistance.32
Stakeholders also need to work to improve the health care experience of LEP individuals. First, policymakers need to rescind a Trump-era administrative rule that removed protections for access to interpretation and translation services in Section 1557 of the Affordable Care Act.33 The rule removes video remote interpreting standards, provisions that require federally funded entities to notify individuals of the availability of language assistance, and requirements to provide language access services to all individuals.34 In addition, health care systems strategies for improving communication and fostering engagement of LEP patients recommended by The Joint Commission include integrating language services (ie, video and phone interpreters) into the workflow, integrating interpreters into the care team, promoting the use of patient portals, and involving families in patients’ care.35 Embedding bilingual providers into care teams would help provide both language and cultural representation. Finally, physician offices are expected to cover the cost of interpreters as the cost of doing business, but high costs of interpreters (from $45 to over $200 per hour) disincentivize their use.36 The clear evidence that medical interpreters reduce medical errors,37 suggests that all payers, including Medicaid, Medicare, and private payers, should reimburse clinicians for the cost of interpreter services.36
Our study has several limitations. First, our measure of English proficiency was based on the survey interview language. This may reflect respondents’ preferred language rather than their ability to communicate in English; in other words, our LEP sample may include bilingual individuals with high English proficiency. However, all respondents in the LEP sample were foreign-born, and previous research has found interview language to be a reliable proxy for acculturation among foreign-born respondents.38 This language choice by respondents may also be more appropriate for health care research than self-reported English proficiency because respondents who believe that they would have difficulty responding to a survey in English would likely need language-concordant providers or medical interpreters in health care settings.17,39 Relatedly, our study could not account for unobserved patient and provider health system factors such as patient-provider concordance that may contribute to health care access among LEP adults. Second, the NHIS only asked several pandemic-specific questions in the latter half of 2020. Given the timing of the questions and the changing circumstances of the pandemic, including the various policies implemented by states and cities and the rapidly changing social environment, our findings may not be generalizable beyond the last two quarters of 2020. We were also unable to include geographic indicators to assess how policies may have differentially impacted health care access in different areas. Finally, the recall period for some of the questions extended further back than the beginning of the pandemic so some respondents may have responded about delayed or forgone health care that occurred before the pandemic.
Our study found that over half of all LEP adults reported delaying or forgoing health care during the pandemic and LEP adults were more likely than English proficiency adults to delay or forgo service use because of cost. Although multivariate differences between the groups in delayed or forgone care were not explained by language proficiency but by low socioeconomic status and health-related characteristics, this is likely due to cultural differences in the perceived need for care and other unmeasured barriers. These findings highlight how pre-existing deficiencies in the health care system exacerbate inequitable access to care among LEP adults. Policymakers must continue to identify effective strategies for increasing accessibility and affordability of needed care.
Supplementary Material
Footnotes
A prior version of the findings was presented at the 2022 American Public Health Association Annual Meeting, Boston, MA, as well as the 2023 Health Care Systems Research Network Meeting, Denver, CO.
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Contributor Information
Eva Chang, Email: eva.chang@gmail.com.
Teaniese L. Davis, Email: Teaniese.L.Davis@kp.org.
Nancy D. Berkman, Email: nancyberkman@gmail.com.
REFERENCES
- 1. U.S. Census Bureau. Comparative Social Characteristics of the United States. 2016-2020 American Community Survey 5-Year Estimates (Table CP02). Accessed September 13, 2022. https://api.census.gov/data/2020/acs/acs5/profile
- 2. Ramirez N, Shi K, Yabroff KR, et al. Access to care among adults with limited english proficiency. J Gen Intern Med. 2023;38:592–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson TS, Karliner LS, Lin GA. Association of primary language and hospitalization for ambulatory care sensitive conditions. Med Care. 2020;58:45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Foiles Sifuentes AM, Robledo Cornejo M, Li NC, et al. The role of limited english proficiency and access to health insurance and health care in the Affordable Care Act era. Health Equity. 2020;4:509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anderson KE, McGinty EE, Presskreischer R, et al. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2034882 e2034882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Czeisler M, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee J. Delayed or forgone care and virtual care in a public health crisis using nationally representative population data. Telemed J E Health. 2023;29:222–234. [DOI] [PubMed] [Google Scholar]
- 8. Xie Z, Hong Y-R, Tanner R, et al. People with functional disability and access to health care during the COVID-19 pandemic: a US population-based study. Med Care. 2023;61:58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gonzalez D Karpman M Kenney GM, et al. Delayed and forgone health care for nonelderly adults during the COVID-19 pandemic: findings from the September 11–28 Coronavirus Tracking Survey. 2021. Accessed April 29, 2022. https://www.urban.org/research/publication/delayed-and-forgone-health-care-nonelderly-adults-during-covid-19-pandemic
- 10. Lei L, Maust DT. Delayed care related to COVID-19 in a nationally representative sample of older Americans. J Gen Intern Med. 2022;37:1337–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shi L, Lebrun LA, Tsai J. The influence of English proficiency on access to care. Ethn Health. 2009;14:625–642. [DOI] [PubMed] [Google Scholar]
- 12. Rodriguez JA, Saadi A, Schwamm LH, et al. Disparities in telehealth use among California patients with limited english proficiency. Health Aff (Millwood). 2021;40:487–495. [DOI] [PubMed] [Google Scholar]
- 13. Vujicic M, Buchmueller T, Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff (Millwood). 2016;35:2176–2182. [DOI] [PubMed] [Google Scholar]
- 14. National Center for Health Statistics. National Health Interview Survey, 2020. Public-use data file and documentation. Accessed April 20, 2022. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm; https://www.cdc.gov/nchs/products/citations.htm
- 15.https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2020/srvydesc-508.pdf National Center for Health Statistics. Survey description, National Health Interview Survey, 2020. 2021. Accessed April 20, 2022.
- 16.https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2019/srvydesc-508.pdf National Center for Health Statistics. Survey description, National Health Interview Survey, 2019. Accessed September 2020.
- 17. Weinick RM, Krauss NA. Racial/ethnic differences in children’s access to care. Am J Public Health. 2000;90:1771–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kandula NR, Lauderdale DS, Baker DW. Differences in self-reported health among Asians, Latinos, and non-Hispanic whites: the role of language and nativity. Ann Epidemiol. 2007;17:191–198. [DOI] [PubMed] [Google Scholar]
- 19. National Institutes of Health . Oral health in America: advances and challenges. 2021. Accessed September 16, 2022. https://www.nidcr.nih.gov/research/oralhealthinamerica
- 20. Wilson JH. Investing in English Skills: The Limited English Proficient Workforce in US Metropolitan Areas. Program MP; 2014. [Google Scholar]
- 21. Asfaw A. Racial and ethnic disparities in teleworking due to the COVID-19 pandemic in the United States: a mediation analysis. Int J Environ Res Publ Health. 2022;19:4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hill J, Rodriguez DX, McDaniel PN. Immigration status as a health care barrier in the USA during COVID-19. J Migr Health. 2021;4:100036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Touw S, McCormack G, Himmelstein DU, et al. Immigrant essential workers likely avoided Medicaid and SNAP because of a change to the public charge rule. Health Aff (Millwood). 2021;40:1090–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goodman B. Lost in translation: language barriers hinder vaccine access. WebMD. 2021. Accessed September 21, 2022. https://www.webmd.com/vaccines/covid-19-vaccine/news/20210426/lost-in-translation-language-barriers-hinder-vaccine-access
- 25. Chung C. NYC translation law often ignored, at high human cost in the COVID era. The City. 2021. Accessed September 21, 2022. https://www.thecity.nyc/services-safety-net/2021/6/2/22466019/nyc-translation-law-often-ignored-at-high-human-cost-in-the-covid-era
- 26. Chang E, Chan KS. Variations in Asian Americans: how neighborhood concordance is associated with health care access and utilization. Am J Public Health. 2015;105:66–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kandula NR, Wen M, Jacobs EA, et al. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites: cultural influences or access to care? Cancer. 2006;107:184–192. [DOI] [PubMed] [Google Scholar]
- 28. Kim EJ, Parker VA, Liebschutz JM, et al. Racial and ethnic differences in healthcare utilization among Medicare fee-for-service enrollees. J Gen Intern Med. 2019;34:2697–2699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen JY, Diamant A, Pourat N, et al. Racial/ethnic disparities in the use of preventive services among the elderly. Am J Prev Med. 2005;29:388–395. [DOI] [PubMed] [Google Scholar]
- 30. DeVoe JE, Tillotson CJ, Lesko SE, et al. The case for synergy between a usual source of care and health insurance coverage. J Gen Intern Med. 2011;26:1059–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haldar S, Pillai D, Artiga S. Overview of health coverage and care for individuals with limited English proficiency (LEP). KFF. 2023. Accessed July 11, 2023. https://www.kff.org/racial-equity-and-health-policy/issue-brief/overview-of-health-coverage-and-care-for-individuals-with-limited-english-proficiency/#
- 32. Ortega P, Martínez G, Diamond L. Language and health equity during COVID-19: lessons and opportunities. J Health Care Poor Underserved. 2020;31:1530–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nondiscrimination in Health and Health Education Programs or Activities, Delegation of Authority. In: Centers for Medicare & Medicaid Services, ed. 85 FR 371602020: 37160-37248. https://www.govinfo.gov/app/details/FR-2020-06-19/2020-11758
- 34. Musumeci M Kates J Dawson L, et al. Issue Brief: the Trump administration’s final rule on Section 1557 non-discrimination regulations under the ACA and current status. The Kaiser Commission on Medicaid and the Uninsured. 2022. Accessed September 27, 2022. https://www.kff.org/racial-equity-and-health-policy/issue-brief/the-trump-administrations-final-rule-on-section-1557-non-discrimination-regulations-under-the-aca-and-current-status/
- 35. The Joint Commission. Issue 13: overcoming the challenges of providing care to limited English proficient patients. 2021. Accessed September 27, 2022. https://www.jointcommission.org/-/media/tjc/newsletters/quick-safety-issue-13-lep-update-10-5-21.pdf
- 36. Jacobs B, Ryan AM, Henrichs KS, et al. Medical interpreters in outpatient practice. Ann Fam Med. 2018;16:70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Flores G, Abreu M, Barone CP, et al. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;60:545–553. [DOI] [PubMed] [Google Scholar]
- 38. Lee S, Nguyen HA, Tsui J. Interview language: a proxy measure for acculturation among Asian Americans in a population-based survey. J Immigr Minor Health. 2011;13:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ayers JW. Measuring English proficiency and language preference: are self-reports valid? Am J Public Health. 2010;100:1364–1366; author reply 1366-1367. [DOI] [PMC free article] [PubMed] [Google Scholar]