Abstract
Drug overdose deaths among adolescents are increasing in the United States, driven by illicitly manufactured fentanyl. Residential treatment facilities are one treatment option for adolescents with substance use disorders including opioid use disorder (OUD), yet little is known about their accessibility or cost. We sought to survey all identifiable US adolescent residential addiction treatment facilities and assess availability and cost of treatment for adolescents under age 18 seeking OUD care. We identified adolescent-serving facilities in the Substance Abuse and Mental Health Services Administration Treatment Locator and through proprietary search engine advertisement data. We called facilities posing as the aunt or uncle of a 16-year-old child with a recent non-fatal fentanyl overdose to inquire about admission and costs. We identified 160 facilities that provided adolescent residential addiction treatment. Eighty-seven facilities (54.7%) had a bed immediately available; 63 facilities (39.6%) had no availability or a waitlist. The mean wait time for a bed opening was 28.4 days (SD=29.2, median=21, IQR=[14, 30]). Among facilities, 57.1% (n=52/91) of those that accepted Medicaid reported a wait list, versus 18.8% (n=13/69) of facilities that do not accept Medicaid. Of facilities providing cost information (n=108), the mean cost-per-day of treatment was $878 (median=$513, IQR=[$333, $1875]). Daily costs among for-profit facilities (mean=$1,211, median=$1,200) were triple those of non-profit facilities (mean=$395, median=$350). Half of facilities (n=76, 47.5%) required partial or full upfront payment by self-pay patients. The mean upfront cost was $28,731 (median=$18,225, IQR=[$6,000, $58,500]). We were unable to identify residential treatment facilities for adolescents in ten states; an additional 13 states did not have a facility that accepted Medicaid. Access to adolescent residential addiction treatment centers is limited and costly in the United States.
Introduction
Drug overdose deaths among adolescents are increasing in the United States, driven by illicitly manufactured fentanyl1, 2. Residential treatment facilities are one treatment option for adolescents with substance use disorders including opioid use disorder (OUD), typically providing care for adolescents with more severe use disorders who are unable to access or unresponsive to outpatient treatment, have complex medical or psychiatric comorbidity, or have a challenging home environment3; the median length of stay at such facilities is typically around two months4. Identifying a residential treatment program can be difficult for families5, who are often tasked with finding and evaluating options in the midst of a crisis.
Previous research evaluating adolescent residential treatment settings found that facilities infrequently provide evidence-based care to adolescent patients, including buprenorphine, the only US Food and Drug Administration (FDA) approved medication for adolescents with OUD6, 7. Research among adult treatment facilities for OUD also found that facilities often require costly upfront payments, and that for-profit facilities charge twice as much as nonprofits, but often have greater bed availability. Additionally, adult facilities frequently use coercive recruitment techniques to encourage enrollment, and offer admission over the phone without additional screening8. However, little is known about the accessibility, cost, or recruitment practices of residential treatment facilities that offer treatment to adolescents with OUD9, 10. The goal of this study was to characterize treatment access and costs of US residential treatment facilities that treat patients with OUD under the age of 18.
Methods
Study design and setting
We conducted a “secret shopper” study, adapted from a prior survey of adult residential OUD treatment facilities8, 11, to capture the experience of families seeking treatment for an adolescent with OUD. Secret shopper methods approximate the “real-world” experiences of people seeking treatment and can help measure inequity in healthcare access12. We selected this method because we anticipated that responses to questions from academic researchers or physicians about treatment practices, costs and bed availability would be different than responses that families calling to ask about treatment would receive.
From October 24th, 2022, through December 20th, 2022, four callers (CK, NS, DB, PB) called adolescent residential treatment facilities in random order as the aunt or uncle of a 16-year-old child with a recent non-fatal fentanyl overdose to inquire about admission, treatment practices and costs7. We developed a structured calling script and data collection tool adapted from a survey of adult facilities11 to address questions specific to adolescent treatment7 (Supplemental Material 1±). All four callers are white; two are female and two are male. Previous research has shown that white patients seeking mental health care appointments have higher rates of being offered care than Black patients. We anticipated that any gaps of care elucidated in this project would underestimate real-world gaps experienced by callers who are Black13. Callers first practiced the script with each other, and then called adult, out-of-sample sites to trial the script. Weekly meetings were held among the four callers to re-review the script for consistency and troubleshoot problems on calls (for example, adjusting methods for female-only sites, as described below).
We called as the aunt or uncle instead of as a parent in case we were asked specific information about a child that it would be unusual for a parent not to know (e.g. child’s height and weight, name of high school). Because there were more sites that accepted male versus female children, we called all sites first with our case child identified as male; if sites only accepted females, we repeated calls with the case child as female with a different caller. At the end of each call, we emphasized that we were not able to make a decision on the phone about pursuing treatment and to not hold a bed or make an appointment for the case child.
The child in our case was uninsured but likely eligible for Medicaid. Using this framing, we were able to ask facilities if they accepted adolescents if they were uninsured and if so, how families typically covered the costs of treatment (e.g. cash pay); we were also able to ask if the facility accepted Medicaid. We asked about uninsured, cash-pay and Medicaid-covered adolescents to attempt to capture care availability for adolescents who could be excluded from care because of a lack of funds (versus adolescents on commercial insurance).
We identified facilities using the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Locator and SpyFu14, a website that provides access to Google advertising data15. The SAMHSA Treatment Locator is a commonly cited way to identify treatment options for substance use disorders, but previous research has found that the database may provide inaccurate information by overstating services that are available16, 17, in part because the database requires programs to self-report information. The Office of the Inspector General within the U.S. Department of Health and Human Services is currently auditing the SAMHSA Treatment Locator to assess accuracy18. SpyFu14 is a search analytics company that compiles data on search engine advertisements including comprehensive lists of keywords and ad variations website domains have purchased on Google Ads. This allowed for the identification of facilities advertising adolescent addiction treatment services through their purchase of relevant Google Ad keywords (see Supplemental Material 2± for further methodological details and keywords).
Study variables
Callers elicited information on bed availability (wait time and approval process), accepted payment methods (self-pay, Medicaid), and cost (cost-per-day, accepted self-pay payment forms, upfront costs). We assessed if facilities were for-profit, non-profit (including government-operated), and accredited (Joint Commission (JC) or Commission on Accreditation of Rehabilitation Facilities (CARF)) from the SAMHSA Treatment Locator, as families may consider accredited facilities to provide evidence-based care. For sites identified from Google Ads, we reviewed websites to ascertain accreditation and for-profit status.
Statistical analyses
We used descriptive statistics to report treatment admission availability and costs. Data were analyzed using StataIC Version 16.119.
This project was deemed non-human subject research by the Oregon Health & Science University (OHSU) Institutional Review Board (#13129). Study data were stored in REDCap electronic data capture tools hosted at OHSU20, 21.
Results
We enumerated 354 residential addiction treatment centers indicating that they provided services to adolescents (308 identified only through the SAMHSA Treatment Locator, 12 through Google Ads, and 34 through both). Of those, we were unable to reach 27 (n=27/354, 7.6%): 20 had non-working or incorrect phone numbers provided by SAMHSA and seven did not answer or return calls after five attempts. Of the 327 facilities reached (n=327/354, 92.4%), 160 (n=160/354, 45.2%) confirmed they currently provided residential addiction treatment to patients under 18 years of age 7. Of the original 308 sites identified that stated that they provided residential treatment to adolescents through the SAMHSA Treatment Locator online, 151 facilities reported in phone calls that they actually provided adolescent residential addiction treatment (49.0%).
Most facilities offered treatment to adolescents with OUD between the ages of 13 (mean minimum age) and 18 (mean maximum age): 106 facilities (n=106/160, 66.3%) treated only patients 18 and under, 44 (n=44/160, 27.5%) also treated adult patients but housed them separately, and 10 (n=10/160, 6.3%) treated adult patients and housed them with adolescents. Overall, 66 facilities (n=66/160, 41.3%) were for-profit, and 94 facilities (n=94/160, 58.8%) were non-profit; 53 facilities were CARF accredited (33.1%) and 66 were JC accredited (41.3%). Characteristics of centers stratified by for-profit and non-profit status are presented in Supplemental Material 3±.
Bed availability
Overall, 87 facilities (n=87/160, 54.4%) had a bed available immediately, 63 facilities (n=63/160, 39.4%) had no beds available or offered a waitlist, and nine (n=9/160, 5.6%) were unsure of bed availability. Fifty-one of 66 for-profit facilities (n=51/66, 77.3%) had a bed available that day, versus 36 of 93 non-profit facilities (n=36/93, 38.7%; p<0.001).
Sixty-five facilities estimated the number of days until a bed opened, with a mean wait of 28.4 (SD=29.2) days and a median of 21 (IQR=14, 30) days. Eleven of those sixty-five facilities anticipated having an open bed within the week (16.9%). Mean wait time for a for-profit bed was 18.9 (n= 14, SD=8.8) days, with a median of 14 (IQR=14, 28) days, versus a mean 31.0 (n=51, SD=32.2) days with a median of 21 (IQR=[14, 35) days for a non-profit bed (p=0.17). The longest wait time was 35 days at a for-profit facility vs. 180 days at a non-profit facility. Overall, 57.1% (n=52/91) of all facilities that accept Medicaid reported a wait list, versus 18.8% (n=13/69) of facilities that do not accept Medicaid (p<0.001).
Most facilities (n=132/160, 83.0%) required additional screening (financial, substance use, mental health, custody information) before offering admission. Twenty-five facilities (n=25/160, 15.6%) required only an intake interview, and two facilities (n=2/160, 1.3%) offered admission over the phone.
Treatment Payment
Acceptance of Medicaid
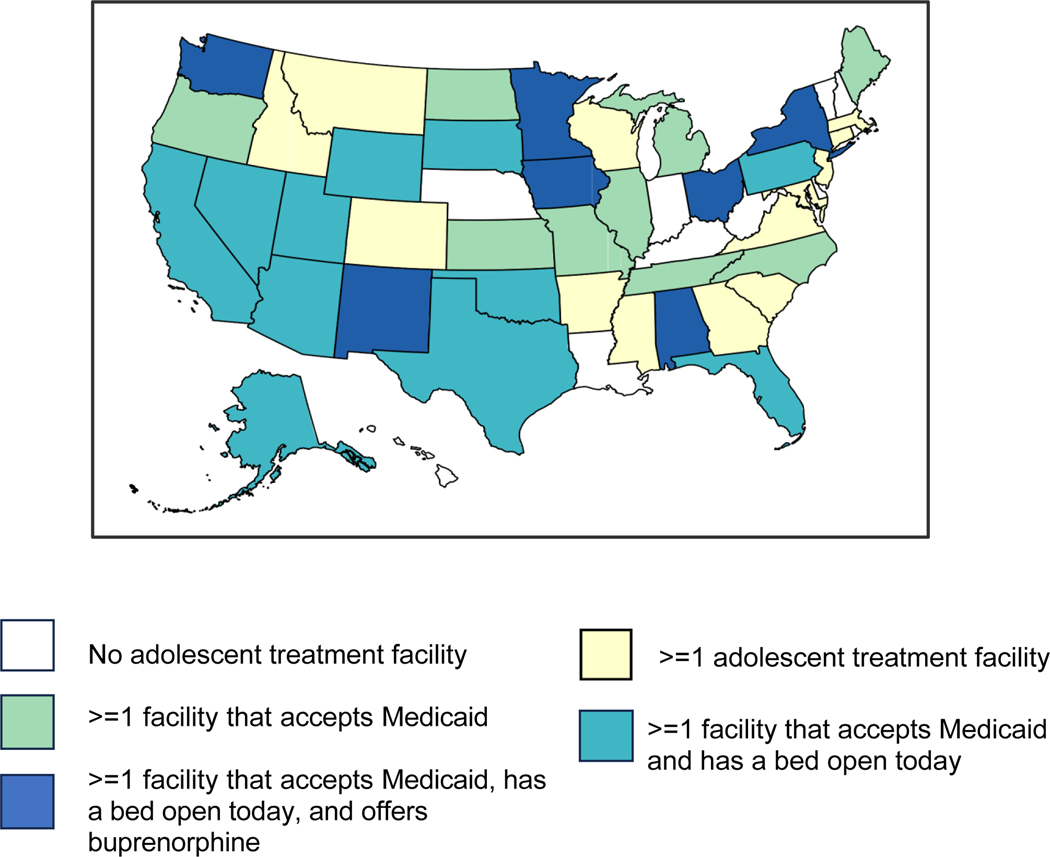
Ninety-one adolescent facilities (n=91/160, 56.9%) accepted Medicaid, including 19.7% of for-profits (n=13/66), and 83.0% of non-profits (n=78/94; p<0.001). Of the 69 sites that did not accept Medicaid, 11 (11/69, 15.9%) stated that most adolescents at their sites were privately insured. We were unable to identify any residential treatment facilities for adolescents in ten states, and none that accepted Medicaid in an additional 13 states. Eighteen states had a facility that accepted Medicaid and had a bed open today. Seven states had a facility that accepted Medicaid, had a bed open today and offered buprenorphine (Exhibit 1).
Exhibit 1. States that we identified have an adolescent residential treatment facility for OUD, and accept Medicaid, and have a bed open today, and offer buprenorphine.
Source: Authors’ analysis of data from phone survey of US adolescent residential addiction treatment facilities
Cash Pay
Of the 160 facilities, 126 (n=126/160, 78.8%) accepted cash-pay, including all 66 for-profit facilities. Twenty facilities (n=20/160, 12.5%) were reported as free or likely free in the setting of our simulated call (an adolescent likely eligible for Medicaid who did not yet have insurance), of which all were non-profits. Seven facilities (n=7/160, 4.4%) were unsure if they accepted cash-pay.
Of the 126 that accepted cash-pay, 108 provided estimated costs over the phone. The mean cost-per-day of treatment was $878 (SD=$721), with a median cost of $513 (IQR=$333, $1875). Among for-profit facilities (n=64), the mean cost-per-day of treatment was $1,211 (SD=732), with a median cost of $1,200 (IQR=$468, $1,950), versus non-profit facilities (n=44), with a mean cost-per-day of treatment of $395 (SD=323), and median cost of $350 (IQR=$200, $500; p<0.001).
Upfront costs
Nearly half of the 160 facilities (n=76/160, 47.5%) required some upfront payment if using self-pay. Facilities reported either a numeric value required on the first day, which could encompass more than one month of treatment, or provided the percent of the first month costs required upfront. The mean reported upfront cost was $28,731 (SD=$24,549), with a median cost of $18,225 (IQR=$6,000, $58,500). Among for-profit facilities that required an upfront payment (n=58), the mean upfront cost was $34,729 (SD=$24,681) with a median of $37,000 (IQR=$10,500, $58,500), versus for non-profit facilities that required an upfront payment (n=17), which reported a mean upfront cost of $9,897 (SD=$9,978) and median upfront cost of $6,000 (IQR=$4,500, $10,000; p<0.001, Supplemental Material 4±).
Discussion
Our study identified 160 adolescent residential addiction treatment facilities in the United States, with wide geographic variability in access to timely, evidence-based treatment. Just over half of facilities accepted Medicaid, with a stark contrast by facility profit orientation: one in five for-profits accepted Medicaid compared to four in five non-profits. For families paying out of pocket, the mean reported daily cost of treatment at for-profits was triple that of non-profits ($1,211 vs. $395). Close to half of all facilities required some upfront payment if using self-pay, including nearly all for-profit facilities; for-profit facilities had a mean upfront cost of $34,729. In 23 states, we did not identify an adolescent residential treatment center that accepted Medicaid. Only seven states had a facility that accepted Medicaid, had a bed open today, and offered buprenorphine.
Despite previous research demonstrating that few adolescent facilities provide evidence-based care for OUD7, the mean monthly reported cost of treatment in the current study was $26,353, which is twice the annual federal poverty level for a single-person household in the US ($13,590) 22. This is particularly striking as OUD disproportionately impacts people with low socioeconomic status23. Upfront costs were similarly expensive and required by nearly all for-profit facilities (with a mean of $34,729) versus only 17 non-profit facilities (with a mean of $9,897). Additionally, a higher percentage of for-profit facilities had beds available versus non-profit facilities. These disparities are similar to those identified among for-profit versus non-profit adult residential treatment sites, though the cost gap is greater among adolescent sites (adult for-profit site up-front costs were $17,434, versus non-profits at $5,712)8. Taken together, parents searching for treatment options amidst a crisis may be compelled to pursue the first available treatment, even at exorbitant costs and even though many facilities do not offer evidence-based treatment 7.
Physicians treating adolescents with OUD advocate for access to evidence-based treatment and overdose prevention in the least restrictive setting that is appropriate for the patient24. Residential treatment is one part of a broader treatment continuum, including outpatient addiction treatment programs and primary care, that is reckoning with the need for increased access to evidence-based care in the face of rising fentanyl-related overdoses among adolescents. While outside of the scope of the current study, primary care providers who treatment adolescents remain a key component for expanding treatment access, especially in rural areas, by maximizing screening for OUD during sports physicals and well-child visits. Technical support interventions to improve primary provider comfort prescribing buprenorphine for adolescents with OUD could increase access for those not requiring residential treatment, partner with adolescent treatment facilities to prescribe buprenorphine, and improve long-term recovery by offering ongoing buprenorphine treatment following completion of residential treatment.
Further compounding this challenge is the current mental health crisis among adolescents in the US; when an adolescent also has both an acute psychiatric crisis and substance use disorder, it may increase the need for residential treatment 3, 25. Previous research has shown that adolescent treatment interventions that integrate treatment of prevalent mental health conditions such as anxiety, depression, and ADHD are clearly needed26. Both residential and outpatient treatment settings must address the complex challenges that adolescents bring to SUD treatment, including further support for navigating family challenges, legal issues, and facilitating housing and school environments that support long-term recovery27. Successfully accomplishing this will mean not only expanding the services and care provided to adolescents at treatment facilities, but also likely the number of treatment beds. In 2021, the National Substance Use and Mental Health Services Survey estimated an age non-specific bed utilization rate of 96% in the US28. Same-day bed availability in our study was limited, particularly among non-profit facilities, and similar to adult facilities which had same-day bed availability in one out of every five non-profit facilities 8.
Further research is needed to identify which adolescents with OUD may benefit most from residential treatment, and to compare adolescent residential treatment outcomes with outpatient adolescent treatment approaches, which for adults achieve outcomes comparable to those of residential treatment, at lower cost 29. Economic analyses of adolescent treatment interventions, including treatment setting, should take into account externalities that affect adolescent treatment, such as level of Medicaid reimbursement to support staffing, legal system effects, school effects, and housing systems30. System-level reform that increases Medicaid reimbursement for adolescent treatment and supports providers and facilities with education and technical assistance may be required to improve access to evidence-based treatment in both outpatient and residential treatment settings, increase treatment options for adolescent patients using Medicaid or cash-pay, and decrease geographic disparities in access to treatment, as others have called for previously31.
Facilities with a waitlist were predominately non-profits and had, on average, approximately a month wait time until a bed opened or the adolescent could be admitted. This was longer than among adult addiction treatment facilities with a waitlist, which had a mean wait time of 16 days8. Additionally, nearly 60% of facilities that accepted Medicaid had a waitlist. The time between seeking and entering treatment is fraught with increased risk of overdose among adults32, and there is some evidence this is also true for adolescents33. Timely access to high quality residential and outpatient treatment services is critical to curb rising trends in adolescent overdose. Staffing challenges are a key driver of bed availability at residential treatment facilities, as facilities frequent have insufficient qualified staff to adequately open all available beds in a facility. For example, 54% of treatment facilities in the state of Oregon identified lack of staffing as the barrier to maximizing bed access34. Medicaid and other funders could develop financial reimbursement incentives that support hiring, retention, and adequate pay for qualified staff. The lack of affordable, evidence-based adolescent residential treatment capacity for large geographic areas of the US emphasizes the need to expand timely access to addiction treatment for adolescents, through both residential and outpatient programs.
Limitations
This study has several limitations. First, we used a fixed-script for simulated calls that focused on a 16-year-old uninsured patient who would likely qualify for Medicaid. Some cash-pay quotes provided may be lower than for higher income households because we used this scenario. Second, the treatment locator may have excluded some facilities that we did not recover from advertisements. However, we expect that we very nearly captured the full target population, and that our results likely represent those facilities that families searching for treatment would be able to identify and approach. Third, we did not explicitly highlight race, ethnicity, gender identity or sexual orientation in our survey; barriers to care for marginalized patients are likely greater than those described in this manuscript and should be evaluated in future research 35, 36. Fourth, in our analysis, we analyzed bed availability and practices at the state level; this may underestimate disparities in access in states with significant urban versus rural gaps (i.e. New York, Oregon) that have access to treatment predominately in urban areas. Fifth, our study likely underestimates burdens experienced by families seeking care, as there may be additional barriers to care related to insurance including Medicaid application, prior authorizations, or other burdens that we did not study. Finally, outpatient adolescent OUD treatment services, which have the potential to greatly expand OUD treatment access, were outside the scope of the current study. Primary care and outpatient specialty addiction treatment programs are an essential component of the adolescent treatment continuum and merit research.
Conclusions
Access to adolescent residential addiction treatment facilities is costly and unevenly distributed across the US. Findings suggest that systems-level interventions are needed to ensure adequate, equitable access to affordable treatment, including for Medicaid-paying patients, and through both residential and outpatient treatment. Future research is needed to identify how best to expand access to affordable, evidence-based treatment for adolescents with OUD.
Supplementary Material
References
- 1.Friedman J, Godvin M, Shover CL, Gone JP, Hansen H, Schriger DL. Trends in Drug Overdose Deaths Among US Adolescents, January 2010 to June 2021. JAMA. Apr 12 2022;327(14):1398–1400. doi: 10.1001/jama.2022.2847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanz LJ, Dinwiddie AT, Mattson CL, O’Donnell J, Davis NL. Drug Overdose Deaths Among Persons Aged 10–19 Years - United States, July 2019-December 2021. MMWR Morb Mortal Wkly Rep. Dec 16 2022;71(50):1576–1582. doi: 10.15585/mmwr.mm7150a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. J Addict Med. Sep-Oct 2015;9(5):358–67. doi: 10.1097/ADM.0000000000000166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Health and Human Services SAaMHSA. Treatment Episode Data Set (TEDS) 2019. 2019. https://www.samhsa.gov/data/sites/default/files/reports/rpt35314/2019_TEDS_Proof.pdf [Google Scholar]
- 5.American Academy of Child and Adolescent Psychiatry. Facts for Families: Residential Treatment Programs. 2017;97 [Google Scholar]
- 6.FDA. Drug Approval Package. Accessed December 24, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2002/20-732_20-733_subutex.cfm
- 7.King C, Beetham T, Smith N, et al. Treatments Used Among Adolescent Residential Addiction Treatment Facilities in the US, 2022. JAMA. 2023;329(22):1983–1985. doi: 10.1001/jama.2023.6266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beetham T, Saloner B, Gaye M, Wakeman SE, Frank RG, Barnett ML. Admission Practices And Cost Of Care For Opioid Use Disorder At Residential Addiction Treatment Programs In The US. Health Aff (Millwood). Feb 2021;40(2):317–325. doi: 10.1377/hlthaff.2020.00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hadland SE, Jent VA, Alinsky RH, Marshall BDL, Mauro PM, Cerda M. Opioid Use Disorder Treatment Facilities With Programs for Special Populations. Am J Prev Med. Sep 2020;59(3):e125–e133. doi: 10.1016/j.amepre.2020.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alinsky RH, Hadland SE, Matson PA, Cerda M, Saloner B. Adolescent-Serving Addiction Treatment Facilities in the United States and the Availability of Medications for Opioid Use Disorder. J Adolesc Health. Oct 2020;67(4):542–549. doi: 10.1016/j.jadohealth.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beetham T, Saloner B, Gaye M, Wakeman SE, Frank RG, Barnett ML. Therapies Offered at Residential Addiction Treatment Programs in the United States. JAMA. Aug 25 2020;324(8):804–806. doi: 10.1001/jama.2020.8969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rankin KA, Mosier-Mills A, Hsiang W, Wiznia DH. Secret shopper studies: an unorthodox design that measures inequities in healthcare access. Arch Public Health. Nov 4 2022;80(1):226. doi: 10.1186/s13690-022-00979-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kugelmass H. “Sorry, I’m Not Accepting New Patients”: An Audit Study of Access to Mental Health Care. J Health Soc Behav. Jun 2016;57(2):168–83. doi: 10.1177/0022146516647098 [DOI] [PubMed] [Google Scholar]
- 14.SpyFu. 2022. https://www.spyfu.com/ [Google Scholar]
- 15.SpyFu. 2022. www.spyfu.com [Google Scholar]
- 16.Flavin L, Malowney M, Patel NA, et al. Availability of Buprenorphine Treatment in the 10 States With the Highest Drug Overdose Death Rates in the United States. J Psychiatr Pract. Jan 2020;26(1):17–22. doi: 10.1097/PRA.0000000000000437 [DOI] [PubMed] [Google Scholar]
- 17.Pattani A. National addiction treatment locator has many flaws, critics say. Tampa Bay Times. May 17, 2022. https://www.tampabay.com/news/health/2022/05/17/national-addiction-treatment-locator-has-many-flaws-critics-say/ [Google Scholar]
- 18.HHS Office of Inspector General. Audit of Substance Abuse and Mental Health Services Administration’s Behavioral Health Treatment Services Locator. Accessed April 6, 2023. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000763.asp
- 19.Stata. 2023. www.stata.com [Google Scholar]
- 20.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. Jul 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. Apr 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HHS. HHS Poverty Guidelines for 2022. Accessed January 3rd, 2023. https://aspe.hhs.gov/topics/poverty-economic-mobility/poverty-guidelines [Google Scholar]
- 23.Ghertner R, & Groves L,. The Opioid Crisis and Economic Opportunity: Geographic and Economic Trends. 2018. ASPE Research Brief. https://aspe.hhs.gov/sites/default/files/private/pdf/259261/ASPEEconomicOpportunityOpioidCrisis.pdf [Google Scholar]
- 24.Levy SJ, Williams JF, Committee On Substance USE, Prevention. Substance Use Screening, Brief Intervention, and Referral to Treatment. Pediatrics. Jul 2016;138(1)doi: 10.1542/peds.2016-1211 [DOI] [PubMed] [Google Scholar]
- 25.Bommersbach TJ, McKean AJ, Olfson M, Rhee TG. National Trends in Mental Health-Related Emergency Department Visits Among Youth, 2011–2020. Jama. May 2 2023;329(17):1469–1477. doi: 10.1001/jama.2023.4809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sterling S, Weisner C, Hinman A, Parthasarathy S. Access to treatment for adolescents with substance use and co-occurring disorders: challenges and opportunities. J Am Acad Child Adolesc Psychiatry. Jul 2010;49(7):637–46; quiz 725–6. doi: 10.1016/j.jaac.2010.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silvers JA, Squeglia LM, Romer Thomsen K, Hudson KA, Feldstein Ewing SW. Hunting for What Works: Adolescents in Addiction Treatment. Alcohol Clin Exp Res. Apr 2019;43(4):578–592. doi: 10.1111/acer.13984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.SAMHSA. National Substance Use And Mental Health Services Survey. 2021. https://store.samhsa.gov/sites/default/files/pep23-07-00-001.pdf [Google Scholar]
- 29.Hartung DM, Markwardt S, Johnston K, et al. Association between treatment setting and outcomes among oregon medicaid patients with opioid use disorder: a retrospective cohort study. Addict Sci Clin Pract. Aug 19 2022;17(1):45. doi: 10.1186/s13722-022-00318-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Homer JF, Drummond MF, French MT. Economic evaluation of adolescent addiction programs: methodologic challenges and recommendations. J Adolesc Health. Dec 2008;43(6):529–39. doi: 10.1016/j.jadohealth.2008.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schubert K, Pond AN, Kraft MK, Aguirre-Molina M. The adolescent addiction treatment workforce: status, challenges, and strategies to address their particular needs. J Psychoactive Drugs. Dec 2004;36(4):483–8. doi: 10.1080/02791072.2004.10524431 [DOI] [PubMed] [Google Scholar]
- 32.Clausen T, Waal H, Thoresen M, Gossop M. Mortality among opiate users: opioid maintenance therapy, age and causes of death. Addiction. Aug 2009;104(8):1356–62. doi: 10.1111/j.1360-0443.2009.02570.x [DOI] [PubMed] [Google Scholar]
- 33.Alinsky RH, Zima BT, Rodean J, et al. Receipt of Addiction Treatment After Opioid Overdose Among Medicaid-Enrolled Adolescents and Young Adults. JAMA Pediatr. Mar 1 2020;174(3):e195183. doi: 10.1001/jamapediatrics.2019.5183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lenahan K RS, Baker R, Goren R, & Waddel EN. Oregon Substance Use Disorder Services Inventory and Gap Analysis. 2023. https://www.oregon.gov/adpc/SiteAssets/Pages/index/OHSU%20-%20Oregon%20Gap%20Analysis%20and%20Inventory%20Report.pdf [Google Scholar]
- 35.Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in Receipt of Buprenorphine and Naltrexone for Opioid Use Disorder Among Adolescents and Young Adults, 2001–2014. JAMA Pediatr. Aug 1 2017;171(8):747–755. doi: 10.1001/jamapediatrics.2017.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goedel WC, Shapiro A, Cerda M, Tsai JW, Hadland SE, Marshall BDL. Association of Racial/Ethnic Segregation With Treatment Capacity for Opioid Use Disorder in Counties in the United States. JAMA Netw Open. Apr 1 2020;3(4):e203711. doi: 10.1001/jamanetworkopen.2020.3711 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.