Abstract
Objective:
To assess the feasibility of implementation and customer perspectives of a sugar-sweetened beverage (SSB) reduction initiative across YMCA Victoria aquatic and recreation centres.
Design:
Two data sources were used to assess implementation and customer acceptability. Photo audits were used to assess the type of drinks available for purchase 6 months prior to initiative implementation and 6 months after, in thirty centres. Change in the range of SSB targeted for removal, non-targeted SSB, as well as drinks classified as ‘red’ (limit), ‘amber’ (choose carefully) and ‘green’ (best choice), was reported. Customer surveys were conducted in three centres to assess acceptability and awareness of the initiative. Inductive and deductive thematic analysis was used to analyse customers’ perspectives of the initiative.
Setting:
30 aquatic and recreation centres in Victoria, Australia.
Participants:
806 customers.
Results:
At post-implementation, 87 % of centres had removed targeted SSB. ‘Red’ drinks reduced by an average of 4·4 drink varieties compared to pre-implementation (11·9 varieties) and ‘green’ drinks increased by 1·4 varieties (3·2 varieties pre-implementation). Customers were largely unaware of the SSB-reduction initiative (90 %) but supported YMCA Victoria in continuing the initiative (89 %), with many believing it would support children in making healthier choices.
Conclusions:
Implementation of an initiative that limited SSB availability across a large number of aquatic and recreation centres was feasible and considered acceptable by customers. Customers frequently mentioned the importance of protecting children from consuming SSB.
Keywords: Process evaluation, Policy, Healthy food, Sports and recreation, Drink, Sugar-sweetened beverage
High consumption of sugar-sweetened beverages (SSB) contributes to a myriad of deleterious health outcomes, including dental caries(1), obesity(2) and type 2 diabetes(3). High-, middle- and low-income countries have demonstrated high consumption of SSB(4) leading to the enactment of public health policies at both government (e.g., taxes or levies)(5) and organisational levels (e.g., reduction or removal from schools and hospitals)(6,7).
Organisational-level policies have been popular in settings frequented by children and/or that have underlying interests in health promotion(8). Health-promoting settings such as health services, parks, local councils and sports, recreation and aquatic centres are optimal places to enact policies aimed at encouraging healthy eating, as they are already engaged in other health-related activities, have population reach and may have influence over food retailers in their purview(8). A common strategy employed in the pursuit of healthier food environments is addressing the availability of healthy and unhealthy options(9) by changing the range of products (i.e., the number of different varieties) and/or the number of units visible to customers (i.e., the number of slots filled in a vending machine)(10).
Evaluating public health initiatives on dimensions beyond effectiveness (i.e., reach, implementation) contributes a more holistic assessment of their population and/or community impact and provides valuable insights for further uptake or adaptation(11). There is some evidence demonstrating the successful implementation of availability-based interventions in individual centres with outdoor pools(12), on a short-term basis in pools(13), or in response to the release of government guidelines aimed at creating healthier sport and recreation centres(14). A 2015 evaluation of a policy that increased healthier food and drink offerings in forty-two Australian sports clubs found no impact on the availability of targeted beverages (including water and diet soft-drink) compared to forty-four control clubs, although measures of unhealthy option availability not reported(15). So far, there is yet to be an examination of implementation of an initiative targeting the reduction of unhealthy drink options across multiple centres.
While the potential public health nutrition benefits of availability changes have been demonstrated, there remain perceived risks in undertaking shifts to healthier food and drink offerings, including how feasible implementation of such a venture is(16,17), and a fear of customer dissatisfaction and drop in sales(17). Furthermore, there is currently insufficient evidence regarding the impact of policies focused on the removal of unhealthy drinks on the healthiness of the food environment across multiple sports centres. Filling this literature gap is particularly important when considering that many sports and recreation policies are adapted from existing government-produced guidelines that tend to focus on the removal and reduction of unhealthy options as well as an increase in healthier items(18,19).
Complementing evidence of extent of policy implementation with measures of customer acceptability aids the development of interventions that are acceptable to an organisation’s client base and contribute to overall understandings of the feasibility of policy implementation(20). Previous research has demonstrated high acceptability of healthy changes to menu(12) and high support for government restrictions of unhealthy options in children’s sports settings(21); however, this evidence is limited to measures in single recreation centres(12) or is over 10 years old(21).
In late 2014, YMCA Victoria (YMCA), an Australian aquatics and recreation provider, announced the introduction of a Healthy Food and Beverage Policy that would cover, among other settings, all food outlets and vending machines within its aquatic and recreation centres. YMCA aimed to implement the policy over a 3-year period from 2015 to 2017. Part of this policy was an SSB-reduction initiative that aimed to remove all SSB (excluding sports drinks) in the first year of implementation, by December 2015. While previous research has examined the impact of the initiative on customer purchasing behaviour(22), closer examination of elements of feasibility may guide other organisations on their approach and resourcing in implementing similar initiatives. In particular, conducting a nuanced assessment of implementation can inform future expectations and goal-setting, while evidence on customer acceptability can help allay organisational and staff fears of a negative reception and guide a communications strategy promoting the initiative.
Aim
To assess the extent of implementation and customer acceptability of implementing an SSB-reduction initiative in YMCA aquatic and recreation centres.
Methods
Organisation and initiative description
YMCA is a community not for profit organisation that operates aquatic and recreation centres on behalf of Local Government in Victoria, Australia. In 2015, YMCA managed seventy-five aquatic and recreation centres across Victoria. These centres provide a variety of amenities, including sports stadiums, pools, gymnastics studios and/or gym facilities. In addition, a number of centres have internally managed food outlets that range from full-service cafes with food preparation facilities, canteens that offer some hot, pre-made food, to kiosks which offer primarily packaged options. This paper focuses on an initiative to reduce the availability of SSB across all YMCA aquatic and recreation centres. YMCA head office adapted the SSB-reduction initiative from the state-government developed Healthy Choices Framework, which included policy guidelines and a food and beverage classification guide(18,23). Managers and staff at each centre were responsible for introducing and maintaining new drink options and fridge displays. YMCA head office supported centres in delivering the initiative through a toolkit that aimed to raise awareness and build capacity in staff based on the four P’s of marketing: including an approved product range, fridge display ‘planograms’ to guide drink placement, promotional material such as infographic posters, social media kits and factsheets for staff, and a recommendation that water was the lowest priced item. The SSB-reduction initiative was promoted as a ‘soft-drink free summer campaign’ to staff and customers by head office. While all SSB (excluding sports drinks) were expected to be removed from cafes and kiosks (including iced teas, large flavoured milks, fruit juices larger than 250 ml, fruit drinks with less 99 % fruit juice), there was a particular focus on ‘soft-drinks’, namely sugar-sweetened carbonated beverages. The focus on ‘soft-drinks’ was chosen by YMCA head office as these products contained the highest amount of sugar out of the existing product range and were one of the most popular products, particularly among children.
YMCA was one of the first aquatic and recreation providers to introduce a healthy food policy in the State of Victoria(24,25). Furthermore, YMCA operated in a complex business environment, wherein they were contracted to manage Local Government owned facilities, were bound by supplier contracts and in some centres food retail was outsourced to external café operators. Additionally, centres relied on the income from café and canteen sales to fund programmes and services and managers were concerned about the financial impact of the policy. Acknowledging these factors, YMCA head office adopted a phased approach to policy implementation, which began with a ‘small change, big impact’ strategy (the ‘soft drink free summer’ campaign) to counter any resistance to change among stakeholders. Sports drinks, the highest selling item in many centres, were excluded from the first phase and earmarked for removal the following year.
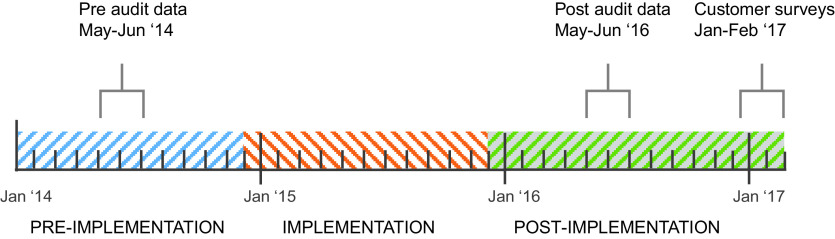
Implementation occurred over 1-year period from December 2014, to be completed by the beginning of December 2015 (Fig. 1). The initiative has been previously described in detail(22).
Fig. 1.
Timeline of initiative implementation and data collection.  ,
pre-implementation period;
,
pre-implementation period;  , implementation period;
, implementation period;
 , post-implementation period
, post-implementation period
Overview of methods
Two data sources were used to assess implementation and customer acceptability of the initiative. Implementation was assessed using a checklist audit from photographic information on the type of drinks available at one time point pre-implementation (May–June 2014) and at one time point post-implementation (May–June 2016; see Fig. 1). Customer acceptability was measured using exit surveys that were collected at 14 months following the initiative implementation (January–February 2017). This time point was chosen as it gave customers sufficient exposure to the changes in the availability of SSB and was the busiest time period for centres allowing for a large number of surveys to be collected.
Extent of initiative implementation
Centres were selected for inclusion in our study if they had a food outlet on the premise that sold pre-packaged beverages including soft-drinks and had an internal checklist audit (described in the following paragraph) conducted pre-implementation (during May–June 2014) and post-implementation (May–June 2016).
Photos of drink fridges were taken by head office, centre staff members or volunteers and uploaded to a central database, following instructions composed by YMCA head office. The photos were then assessed by YMCA head office and volunteers using a pre-existing data collection form (referred to as the ‘checklist audit’) where the name and variety of each drink available were recorded. From this, the research team assessed the Healthy Choices rating of ‘green’ (best choice), ‘amber’ (choose carefully) and ‘red’ (limit intake) for each item using the Healthy Choices classification guide criteria, which is based on the presence of added sugar, serving size, kilojoule and milk content(26). Products were identified as sports drinks when their product name included ‘sports drink’.
To ascertain the extent of implementation, centres were classified as either: (1) not soft-drink free, (2) soft-drinks removed but other SSB available (excluding sports drinks) or (3) all SSB removed (excluding sports drinks) at post-implementation.
We estimated the change in the number of different varieties of ‘red’, ‘amber’ and ‘green’ drinks available from the pre- to the post-implementation period using paired t tests and reported 95 % CI (Stata version 14.1). We conducted this additional analysis as measuring the extent of initiative implementation may not indicate the overall change in the healthiness of the food environment. For example, if the number of ‘red’ sports drinks varieties increased following the removal of all other SSB, this may mean that the initiative was successfully implemented but, in reality, did not create a healthier food environment for YMCA customers and staff. Furthermore, measuring the removal of SSB does not give an indication of how the availability of healthier beverages may have changed.
We conducted a number of sub-analyses to determine heterogeneity in the extent of initiative implementation and identify if any types of centres or food outlets experienced challenges in implementing the initiative and who may require additional support. Analyses were stratified by the following variables: the presence of a pool, stadium and recreation facilities (as these may be frequented by different patron groups, i.e., stadium patrons are likely to be older children/teenagers); socio-economic position (SEP) of the area in which the centre was located; type and revenue size of the food outlet.
Customer perspectives
Centres were chosen for customer surveys if they had large attendance numbers (as nominated by YMCA), full-service cafes on site, provided year-round children’s swimming lessons (to capture parents’ perspectives) and were located in metropolitan Melbourne. Centres located in areas of different SEP were chosen to capture a wide range of perspectives on the acceptability of the SSB-reduction initiative.
The survey used was an extension of a survey previously used by this research team(27). For the current study, four additional questions were added to the previously used survey. The first three of these added questions asked patrons to: (1) report on their awareness of the SSB-reduction initiative, (2) whether they thought it would affect soft-drink consumption and (3) whether YMCA should continue with the initiative. Question 1 answer options were yes or no. Questions 2 and 3 could be answered on a 5-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. Pearson chi-squared tests were used to assess whether responses differed according to a number of customer characteristics including the centre attended, customer age range, gender, SEP of customers home postcode and the presence of at least one child with them. SEP was assessed by postcode tertile, using Socio-Economic Index for Areas Index of Relative Socio-Economic Disadvantage(28). However, only 5 % of respondents fell into the lowest tertile. Postcodes were subsequently re-categorised into high (bottom half of Socio-Economic Index for Areas Index of Relative Socio-Economic Disadvantage) and low (highest measurers of Socio-Economic Index for Areas Index of Relative Socio-Economic Disadvantage) SEP. Note that customers surveyed may live in a postcode with a different SEP from the SEP of the centre they attend.
The fourth question was an open-ended question where customers were asked to report any perceptions, experiences or opinions they had regarding the SSB-reduction initiative. Comments were transcribed verbatim by data collectors and analysed by the lead author using a combination of deductive and inductive thematic coding where data were coded using a combination of pre-determined codes describing the overall reaction to the initiative (positive, neutral, negative), as well as codes emerging from the dataset (open-coding).
Surveys were conducted over 9 d in January and February 2017. Two data collectors were present on each day (AUTHORS BLINDED), using electronic tablets to collect survey responses through the QuickTapSurvey software application(29). Every third exiting patron estimated to be over the age of 17 was approached to participate, with data collectors confirming age as a first question for any patrons estimated to be below the age of 25.
Results
Results are presented in two sections. Firstly, the checklist audit which details the extent of initiative implementation measured by the change in soft-drink availability, and in ‘red’, ‘amber’ and ‘green’ drink availability in thirty centres. Secondly, the customer survey results from three centres which include the degree of acceptability and awareness of the initiative, as well as a thematic analysis of free-text responses from customers.
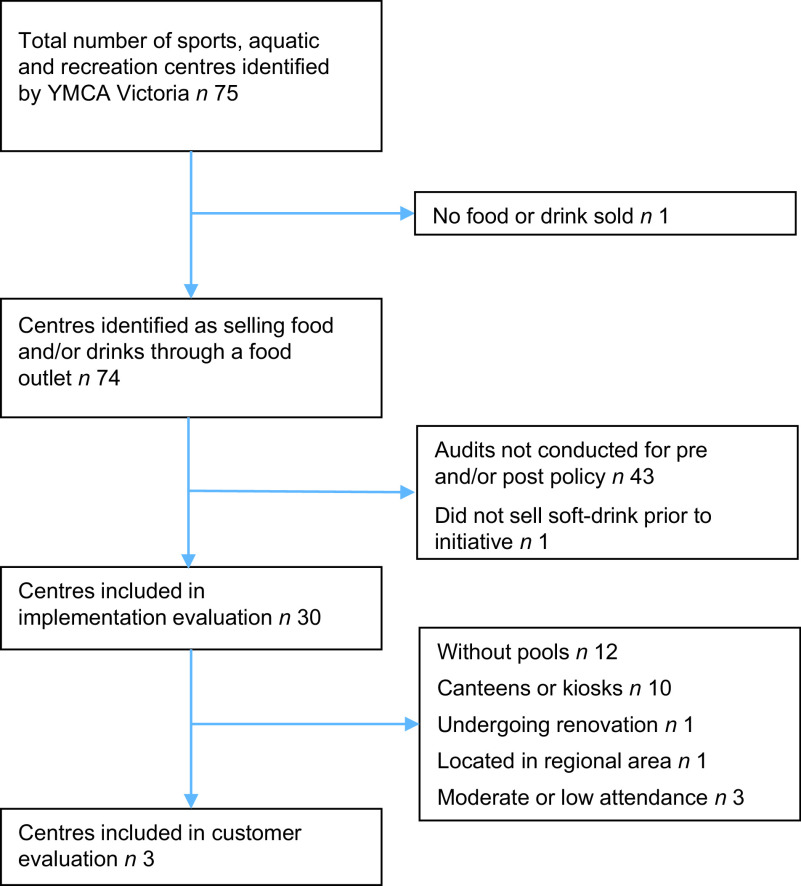
An overview of centre characteristics is available in the online supplementary material, Supplemental Table 1. Individual centre characteristics are not presented to maintain anonymity of centres. Thirty centres were included in this implementation evaluation (Fig. 2). The majority of the centres excluded for not having two time points were swimming pools (n 25), which are only open to the public during the hotter months (November–March) and therefore did not take part in the audits.
Fig. 2.
Centre selection for implementation and customer evaluation
Extent of initiative implementation: removal of soft-drinks
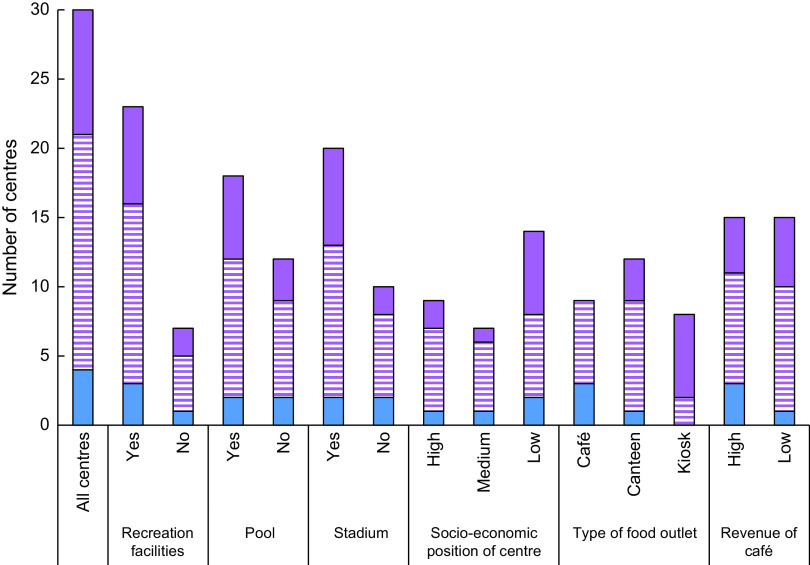
At post-implementation, ten of thirty centres had met the SSB-reduction initiative goal of removing all SSB (excluding sports drinks) (33 %; Fig. 3). A further sixteen centres had removed all soft-drinks, resulting in a total of twenty-six centres being soft-drink free (87 %). The proportion of centres that implemented the initiative was greater among centres that had a kiosk compared to centres with full-service cafes or canteens. There did not appear to be any difference in the proportion of centres that had fully implemented the initiative according to any other variable of interest. Figure 3 provides a descriptive measure of the results when examined by different variables of interest, including the presence of recreation facilities, pool and/or stadium; the SEP of the location of the centre; the type of food outlet in the centre and the revenue of the café.
Fig. 3.
Degree of initiative implementation by centre and food retail characteristics at
post-implementation.  , not soft-drink free;
, not soft-drink free;  ,
soft-drink free;
,
soft-drink free;  , sugar-sweetened beverage free
(excluding soft drinks)
, sugar-sweetened beverage free
(excluding soft drinks)
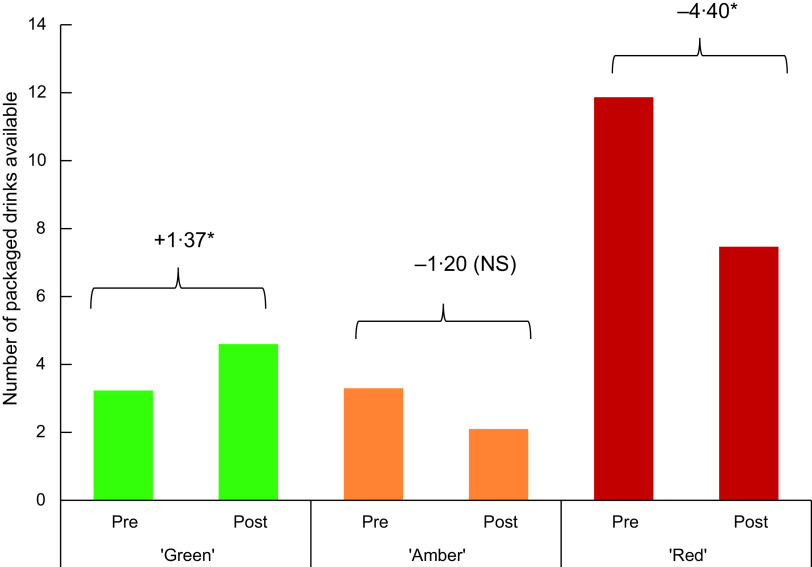
Extent of initiative implementation: change in drink varieties available
The variety of all packaged drinks per centre decreased by 4·5 over the study period (95 % CI −7·2, −1·8), from 18·4 drinks per centre at pre-implementation. The range of ‘red’ drink varieties available pre-implementation ranged from 2 to 22, with an average of 11·9 per centre. By post-implementation, centres had reduced the number of red drinks varieties on average by 4·4 (95 % CI −6·2, −2·6) (Fig. 4). Even centres that did not meet the initiative had reduced their availability of ‘red’ drink varieties (−3·8, 95 % CI −6·1, −1·5). Centres with full-service cafes had on average a greater variety of ‘red’ drinks available at the pre-implementation data point (15·1) compared to kiosks (10·9) and canteens (10·2). A description of pre-implementation availability of ‘green’, ‘amber’ and ‘red’ drinks is available in the online supplementary material, Supplemental Table 2).
Fig. 4.
Mean change in number of drink varieties available from pre- to post-implementation, by healthiness classification. *Significant P < 0·05, NS, non-significant
Stratification by variables of interest revealed that for centres with canteens, there was no change in the number of ‘red’ drink varieties available (n 13, −3·3, 95 % CI −6·7, 0·1), compared to centres with a cafe or kiosk. Five of the twelve centres that had canteens demonstrated either no change or an increase in the number of ‘red’ drink varieties available. Compared to the pre-implementation period, there was either no change or an increase in the total number of ‘red’ drinks available in the post-implementation in eight centres. Of these, seven had removed soft-drinks, but other ‘red’ drinks were stocked in their place. Examination of drinks in these centres showed that a number had added products marketed as ‘healthier’ alternatives, such as ones with natural added flavouring, that are classified as ‘red’ drinks. ‘Red’ drinks that remained included large juices or fruit drinks, large flavoured milks and iced tea.
The number of ‘amber’ drink varieties did not change pre- and post-initiative implementation (−1·20, 95 % CI −2·65, 0·25), which was consistent for all stratified sub-analyses.
At pre-implementation, availability of ‘green’ drink varieties ranged from 1 to 9, with the average being 3·1. Centres increased their stocking of ‘green’ drink varieties by an average 1·4 at post-implementation (95 % CI 0·3, 2·4). Fifteen centres did not change or decreased the variety of ‘green’ drinks over the period of the study. When stratifying analyses by the type of food outlet, the number of ‘green’ drink varieties significantly increased in centres with canteens (2·08, 95 % CI 0·29, 3·86) following implementation, but not in centres with cafes or kiosks. The change in number of ‘green’ drink varieties pre- and post-initiative implementation did not differ for any other stratified sub-analyses.
Customer perspectives
Surveys (n 806) were conducted at three different centres that encompassed centres located in areas of different SEP (Table 1). Two of the centres had removed soft-drinks at the time of data collection. Centre 2 had not removed all soft-drinks when surveys were conducted but had reduced the variety of soft-drinks available.
Table 1.
Recruited centres for customer surveys
| Centre | Type of centre | Type of food service | Removal of soft-drinks? | SEP of centre | Customer surveys completed |
|---|---|---|---|---|---|
| 1 | Recreation centre with pool | Café with full food preparation | Yes | High | 253 |
| 2 | Recreation centre with pool | Café with full food preparation | No | Medium | 400 |
| 3 | Recreation centre with pool and stadium | Café with full food preparation | Yes | Low | 153 |
SEP, socio-economic position.
At all three centres, customers were largely unaware of the existence of the SSB-reduction initiative (90 %). The proportion of customers who noticed the change was greater for those living in low SEP areas (14 %) compared to those living in high SEP areas (8 %).
Eighty-four percentage of those surveyed strongly agreed or agreed with the statement that the ‘soft-drink free initiative would reduce soft-drink consumption in the community’, with no observed differences between sub-groups.
Furthermore, 89 % strongly agreed or agreed that YMCA should continue with the initiative. A greater proportion of women compared to men were supportive of the initiative (92 %, 85 % respectively), with no other demographic differences observed. Centre 2 respondents were less likely to agree that the initiative should continue (87 %) compared to customers from Centre 1 (94 %) and Centre 3 (91 %).
Of the 806 customer responses, 227 (28 %) further commented on their perceptions, experiences and/or opinions of the SSB-reduction initiative. Fifty-three percentage of free-text comments were positive, 21 % neutral and 29 % negative (sum is more than 100 % as some participants made multiple comments). Thematic analysis of customer responses revealed four main themes: health, affirmation of initiative, efficacy of the initiative and responsibility and choice, with sub-themes under each of these (see Table 2).
Table 2.
Themes and sub-themes emerging from an open-ended survey question regarding customer perceptions, experiences and opinions of the SSB-reduction initiative (n 227)
| Theme | Sub-theme | Example quotes |
|---|---|---|
| Health-related messaging | Reduction of sugar is good for health | ‘Anything that reduces sugar is a good
idea’. Female, >65 years old |
| Soft-drinks are unhealthy for you | ‘Soft-drinks are evil, bad for your teeth,
bad for your weight, water’s where it’s at’. Female, 45–54 years old |
|
| Protective for children and easier for parents | ‘Kids see the unhealthy food at the counter
and want it’. Female, 35–44 years old |
|
| Affirmation of initiative | Initiative is in line with the heath-promoting nature of centres | ‘YMCA is promoting health so no soft-drinks
should be given’. Male, >65 years old |
| Commend YMCA on implementing initiative and taking a leadership role | ‘Lovely that YMCA is taking a leadership
role in this’. Female, 55–64 years old |
|
| Efficacy of the initiative | Will be effective as ‘out of sight out of mind’ mentality | ‘Makes it easier for parents if soft-drinks
and junk food aren’t in sight’. Female, 45–54 years old |
| Will not be effective as people will purchase elsewhere | ‘They’ll just get it somewhere
else’. Male, >65 years old |
|
| Soft-drinks should be limited in other settings as well | ‘Sports centres are a small portion of
people’s lives, changes need to be much broader to effect on a community
level’. Female, 35–44 years old, high SEP |
|
| Choices and responsibility | Adults should be allowed a choice | ‘I’m old fashioned and think people should
be able to choose for themselves, but I guess it’s a good
thing’. Female, >65 years old, high SEP |
| Need to have other choices to switch to | ‘As long as they don’t have other drinks
that have just as much sugar in them’. Male, 35–44 years old, low SEP |
Participants frequently commented on the deleterious health outcomes of soft-drinks and high sugar consumption, and that soft-drinks had high sugar content. In particular, many viewed the initiative as being protective for children, while allowing parents to avoid being pestered for it by their children. Respondents also noted that other drinks that remained had similar amounts of sugar (e.g., juice). A minority of surveyed customers believed that those visiting the centre were unlikely to drink soft-drink or were able to compensate the calories from SSB consumption with physical activity.
The initiative was viewed as being in line with the health-promoting ethos of the centres, and that it was inconsistent to sell soft-drinks in the first place. Some respondents believed further healthy changes could be made in the centre and in other settings. Many respondents commended YMCA for implementing the initiative.
There were divergent views as to the efficacy of the initiative. Participants noted that it was likely to be effective due to an ‘out of mind, out of sight’ mentality that often related to children asking for the soft-drinks. However, a large number held the view that visitors would engage in compensatory behaviour and purchase the unavailable soft-drinks at another location. Despite many participants not believing it would be effective, they nonetheless supported YMCA in implementing such an initiative.
Participants frequently commented on different elements around the notion of choice. Choice was closely entangled with the concept of responsibility, where participants stated that individuals had a responsibility to make the healthy choices for themselves, and the right to engage in unhealthy behaviours if they chose to. There were tensions between the desire for choice and the idea that removing soft-drink enabled them to live healthier lives.
Discussion
Our study is the first to assess the extent of implementation of an SSB-reduction initiative across a large number of Australian aquatic and recreation centres. One-third of the centres included in our analysis met the initiative’s aim of removing all SSB (excluding sports drinks) at post-implementation, with a further 54 % having removed all soft-drinks as well. The number of ‘red’ drink varieties decreased by an average of 4·4 drinks per centre, while ‘green’ varieties increased by 1·4 drinks on average from pre- to post-implementation periods. Combined with consistent high customer acceptability, the current study demonstrates that a healthy drink policy is likely to be feasible in a variety of sports and recreation centres.
Our findings that a healthy drink initiative resulted in the decrease of unhealthy drink varieties and an increase in healthy drink options are similar to that of a Canadian study where capacity-building support to implement a healthy food policy resulted in an increase in the number of healthy products (pre – 11 %, post – 15 %), and fewer unhealthy products (pre – 46 %, post – 56 %) within sport centre vending machines(30). However, the results from our study are in contrast to an Australian randomised control trial conducted in sports clubs that aimed to increase the availability of healthier beverages, which reported no change in the availability of healthy drinks (water and diet soft-drinks) in forty-two intervention clubs compared to forty-three control clubs(15). The divergence of results may be due to different levels of support offered. For example, while sports clubs in the study by Wolfenden et al. (15) were provided with a support officer for contact, there is no mention of support in identifying healthier options. In contrast, YMCA head office took a role in identifying healthy drink options and communicating these to centres.
Although centres received support in identifying healthier drink options, the magnitude of increase in ‘green’ drink variety was two-thirds less than the decrease in ‘red’ drink variety. The limited increase in variety of ‘green’ drinks may reflect minimal supply options of packaged healthy drink alternatives, which has been identified as a barrier to implementation in previous food retail interventions(31). Additionally, YMCA was bound by a beverage supply contract, which limited the variety of alternative healthier drink options available. Given the consumer concern with healthy drink availability, identifying and establishing supply of acceptable and varied healthy alternatives should be a key focus of organisations seeking to implement similar policies. For small organisations, finding suppliers who are willing to fill small orders(32) or exploring options to form co-operative buying groups may offer solutions to issues with limited buying power.
The type of centre food outlet appeared to influence implementation; centres with kiosks were more successful at implementing the initiative than other café types, in particular full-service cafes. Centres with canteens experienced on average no decline in the number of ‘red’ drinks available, despite eleven of twelve canteens removing soft-drinks. Examination of available options showed that a number of added beverages were ones with natural added flavouring that are however still SSB. The rapid pace of change in drink products, flavours and formulations that is occurring in the packaged beverage market(33,34) required frequent updates to approved product ranges and confusion between marketing messages from the drinks supplier and YMCA head office and centre staff. While traditional ‘soft-drinks’ may be easily identified as unhealthy, centres may require additional nutrition expertise support in identifying healthier drink alternatives as they emerge. Further studies may seek to conduct qualitative research into the difference in implementation between centres and different contexts to investigate why some settings are more successful than others. For example, interviews or focus groups with centre staff and managers may elucidate context-specific barriers or facilitators that may aid implementation in other settings, whether they be in sports and recreation or other contexts. Future research may also seek to examine supplier marketing and promotional strategies aimed at retailer to determine whether this is limiting the identification of healthy alternatives.
Our result of high customer acceptability of the SSB-reduction initiative echoes previous research examining sports and recreation patrons’ perspectives on healthy food and beverage policies. McGrath et al. (12) found that 86 % of surveyed outdoor pool visitors were supportive of changes to increase the availability of healthier menu offerings. The importance of protecting children from SSB found in our study supports previous research where restriction of unhealthy options is supported in settings heavily frequented by children, such as in children’s sporting venues(21) and schools(35). These results reveal that framing policies around the protection of children may resonate and be more acceptable than policies framed as being aimed at the general populace. The majority of attendees did not notice the policy (90 %). This may be due to the low use of the centre food outlets on average: less than 20 % of sport and recreation attendees purchased items from the centre food outlets in previous research conducted in the same setting(27). Customer surveys were conducted following the implementation of the initiative – however, they can also be conducted prior to implementation to gauge acceptability and engage organisations who are concerned about customer backlash.
The strengths of the current study include the measurement of implementation of the initiative across a large number of centres. This allowed us to explore the heterogeneity of key potential influences of implementation capacity. A limitation of the current study is that pre-implementation measures were conducted over a number of months, due to the large number of participating centres, rather than at one point in time. The baseline menu audits were completed by registered nutritionists or third year nutrition students on university placements. However, the post-implementation measures were reliant on YMCA centre staff taking drink fridge photos for the audit. This method may have limited the reliability of the measurement as staff may have an interest in meeting the initiative requirements. However, this is an example of working in the constraints of real-world research. Customer surveys were conducted at large centres in metropolitan areas and perspectives may not be generalisable to sports centres in different contexts or be representative of the broader Australian population. However, previous studies have indicated support across the population for healthier food environments in child-focused settings(35).
The low awareness, high acceptability and demonstrated feasibility of these policies indicate that they are likely to be easy wins for increasing the healthiness of community food environments, a fact reflected in the large number of local government initiatives aimed at this setting(18,19). These results build on evidence of this initiative’s effectiveness in reducing unhealthy drink purchases as explored previously(22).
Conclusion
Our study is the first to assess implementation of an SSB-reduction initiative in a large number of Australian aquatic and recreation centres. Strong compliance in removing soft-drinks and high customer acceptability indicates that a targeted policy is feasible and likely to create healthier community food and beverage environments. Implementation is likely to require support in identifying the nutrition content and healthiness of drinks and in sourcing a variety of healthy alternatives.
Acknowledgements
Acknowledgements: The authors would like to thank Stephen Bendle, Stella Cifone and the YMCA centre managers and staff. Financial support: The current study was funded in part by VicHealth. VicHealth has no role in the design, analysis or writing of this article. T.B.R. is supported by a National Health and Medical Research Council Centre for Research Excellence grant (APP1152968) and a grant from The Australian Prevention Partnership Centre. A.J. is supported by YMCA Victoria. A.K. is supported by the Alannah and Madeline Foundation. O.H. is supported by research funding from the Victorian Health Promotion Foundation (VicHealth). B.G. is supported by the Cancer Council Victoria. K.B. is supported by a National Heart Foundation of Australia Future Leader Fellowship (GN 102047). M.R.B. is supported by an Institute for Health Transformation Post-Doctoral Fellowship. A.C. is supported by an Australian Government Research Training Program Scholarship. A.P. is supported by a National Health and Medical Research Council fellowship (GNT1045456) and Deakin University. Conflict of interest: Professor Peeters has received funding from Melton and Wyndham city councils to conduct evaluations of healthy food policies. Ms Kurzeme was previously, and Ms Jerebine is currently, employed by YMCA Victoria. All other authors declare no competing interests. Authorship: T.B.R., A.P., K.B., A.J. and A.K. conceptualised the project. T.B.R., A.P. and K.B. designed the methodology. A.K. and A.J. provided information for centre selection and facilitated data collection. T.B.R., B.G., O.H., M.R.B. and A.C. conducted data collection and investigation. T.B.R., B.G. and A.C. conducted data curation. T.B.R. conducted formal analysis and managed the project. A.P. supervised the project. A.J., B.G. and A.C. validated the data. T.B.R. drafted the original manuscript. All authors contributed to reviewing and editing the final manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Monash University Human Research Ethics Committee (CF16/691–2016000340). Verbal informed consent was obtained from all participants. Verbal consent was witnessed and formally recorded.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021002421.
click here to view supplementary material
References
- 1. Bleich SN & Vercammen KA (2018) The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obes 5, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Malik VS, Schulze MB & Hu FB (2006) Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 84, 274–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Malik VS, Popkin BM, Bray GA et al. (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. Diabetes Care 33, 2477–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Singh GM, Micha R, Khatibzadeh S et al. (2015) Global, regional, and national consumption of sugar-sweetened beverages, fruit juices, and milk: a systematic assessment of beverage intake in 187 countries. PLoS One 10, e0124845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Backholer K, Vandevijvere S, Blake M et al. (2018) Sugar-sweetened beverage taxes in 2018: a year of reflections and consolidation. Public Health Nutr 21, 3291–3295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Taber DR, Chriqui JF, Powell LM et al. (2012) Banning all sugar-sweetened beverages in middle schools: reduction of in-school access and purchasing but not overall consumption. Arch Pediatr Adolesc Med 166, 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Niebylski ML, Lu T, Campbell NRC et al. (2014) Healthy food procurement policies and their impact. Int J Environ Res Public Health 11, 2608–2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crisp BR & Swerissen H (2003) Critical processes for creating health-promoting sporting environments in Australia. Health Promot Int 18, 145–152. [DOI] [PubMed] [Google Scholar]
- 9. Caspi CE, Sorensen G, Subramanian SV et al. (2012) The local food environment and diet: a systematic review. Health Place 18, 1172–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hollands GJ, Carter P, Shemilt I et al. (2017) Altering the availability or proximity of food, alcohol and tobacco products to change their selection and consumption. Cochrane Database Syst Rev issue 9, CD012573. [DOI] [PMC free article] [PubMed]
- 11. Glasgow RE, Vogt TM & Boles SM (1999) Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 89, 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGrath G & Tinney M (2014) Case Study: Healthy Choices at Lara Pool. Geelong: State Government of Victoria. [Google Scholar]
- 13. Olstad DL, Goonewardene LA, McCargar LJ et al. (2015) If we offer it, will children buy it? Sales of healthy foods mirrored their availability in a community sport, commercial setting in Alberta, Canada. Child Obes 11, 156–164. [DOI] [PubMed] [Google Scholar]
- 14. Olstad DL, Downs SM, Raine KD et al. (2011) Improving children’s nutrition environments: a survey of adoption and implementation of nutrition guidelines in recreational facilities. BMC Public Health 11, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wolfenden L, Kingsland M, Rowland BC et al. (2015) Improving availability, promotion and purchase of fruit and vegetable and non sugar-sweetened drink products at community sporting clubs: a randomised trial. Int J Behav Nutr Phys Act 12, 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kelly B, King L, Bauman AE et al. (2014) Identifying important and feasible policies and actions for health at community sports clubs: a consensus-generating approach. J Sci Med Sport 17, 61–66. [DOI] [PubMed] [Google Scholar]
- 17. Thomas HM & Irwin JD (2010) Food choices in recreation facilities: operators’ and patrons’ perspectives. Can J Diet Pract Res 71, 180–185. [DOI] [PubMed] [Google Scholar]
- 18. State of Victoria (2014) Healthy Choices: Policy Guidelines for Sport and Recreation Centres. Melbourne: Department of Health. [Google Scholar]
- 19. Alberta Health and Wellness (2010) The Alberta Nutrition Guidelines for Children and Youth. Edmonton, Alberta: Alberta Health and Wellness. [Google Scholar]
- 20. Eckert TL & Hintze JM (2000) Behavioral conceptions and applications of acceptability: issues related to service delivery and research methodology. Sch Psychol Q 15, 123. [Google Scholar]
- 21. Kelly B, Chapman K, King L et al. (2008) Double standards for community sports: promoting active lifestyles but unhealthy diets. Health Promot J Aust 19, 226–228. [DOI] [PubMed] [Google Scholar]
- 22. Boelsen-Robinson T, Orellana L, Backholer K et al. (2020) Change in drink purchases in 16 Australian recreation centres following a sugar-sweetened beverage reduction initiative: an observational study. BMJ Open 10, e029492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. State of Victoria (2010) Healthy Choices: Food and Drink Classification Guide, 2nd ed. Melbourne: Department of Health. [Google Scholar]
- 24. YMCA Victoria (2014) YMCA Victoria bans sugary drinks. http://victoria.ymca.org.au/news-events/news/ymca-victoria-bans-sugary-drinks.html (accessed October 2020).
- 25. McArthur G (2014) Soft drink to be banned from all Victorian YMCA centres. Herald Sun. https://www.heraldsun.com.au/news/victoria/soft-drink-to-be-banned-from-all-victorian-ymca-centres/news-story/a34216022c52a1b86c7ca6c8db8d5729 (accessed October 2020).
- 26. Department of Health (2014) Healthy Choices: Food and Drink Classification Guide. Melbourne: State of Victoria. [Google Scholar]
- 27. Boelsen-Robinson T, Chung A, Khalil M et al. (2017) Examining the nutritional quality of food and beverage consumed at Melbourne aquatic and recreation centres. Aust N Z J Public Health 41, 184–186. [DOI] [PubMed] [Google Scholar]
- 28. Australian Bureau of Statistics (2018) Socio-Economic Indexes for Areas. http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa (accessed July 2020).
- 29. TabbleDabble Inc. QuickTapSurvey 2019. https://www.quicktapsurvey.com/ (accessed February 2019).
- 30. Naylor P-J, Olstad DL & Therrien S (2015) An intervention to enhance the food environment in public recreation and sport settings: a natural experiment in British Columbia, Canada. Child Obes 11, 364–374. [DOI] [PubMed] [Google Scholar]
- 31. Andreyeva T, Middleton AE, Long MW et al. (2011) Food retailer practices, attitudes and beliefs about the supply of healthy foods. Public Health Nutr 14, 1024–1031. [DOI] [PubMed] [Google Scholar]
- 32. Gittelsohn J, Laska MN, Karpyn A et al. (2014) Lessons learned from small store programs to increase healthy food access. Am J Health Behav 38, 307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Euromonitor International (2018) Voice of the industry: soft drink. Euromonitor International. https://www.portal.euromonitor.com/ (accessed August 2018).
- 34. Euromonitor International (2018) The world market for health and wellness packaged food. Passport. https://www.portal.euromonitor.com/ (accessed August 2018).
- 35. Pescud M, Donovan RJ & Pettigrew S (2012) Stakeholder support for school food policy expansions. Health Educ Res 27, 996–1004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021002421.
click here to view supplementary material