Abstract
The role of the intestinal microbiota in the diagnosis and treatment of pancreatic diseases is increasingly significant. Consequently, fecal microbiota transplantation (FMT) is emerging as a promising therapeutic avenue for various pancreatic disorders, including cancer, pancreatitis, and type 1 diabetes (T1D). This innovative procedure entails transferring gut microbiota from healthy donors to individuals affected by pancreatic ailments with the potential to restore intestinal balance and alleviate associated symptoms. FMT represents a pioneering approach to improve patient outcomes in pancreatic diseases, offering tailored treatments customized to individual microbiomes and specific conditions. Recent research highlights the therapeutic benefits of targeting the gut microbiota for personalized interventions in pancreatic disorders. However, a comprehensive understanding of the intricate interplay between gut microbiota and pancreatic physiology warrants further investigation. The necessity for additional studies and research endeavors remains crucial, especially in elucidating both adult and pediatric cases affected by pathological pancreatic conditions.
Keywords: microbiota, fecal microbiota transplantation, pancreatitis, pancreatic cancer, T1D
1. Introduction
The medical community is increasingly focusing on the intestinal microbiota, especially due to its discovered links to the functioning of various organs in the human body [1]. Microbiota alterations seem to be especially beneficial for diagnosing certain pancreatic pathologies and it is possible that the future of non-invasive diagnosis may emerge from this realm [2]. Certainly, influencing the microbiota through fecal microbiota transplantation (FMT) is gaining recognition as a promising treatment strategy for a range of conditions, including pancreatic diseases like cancer, pancreatitis, and diabetes. FMT involves transferring gut microbiota and their byproducts from an individual in good health to one who is ailing. This procedure is drawing attention for its effectiveness and the ease of use, presently considered the most effective method for restoring intestinal flora and addressing both intestinal and potentially non-intestinal illnesses [3,4,5]. This technique involves altering the composition of the gut microbiota to normalize it, thereby obtaining therapeutic benefits [6,7].
As Antushevich outlines, the selection of donors for fecal material is subject to very stringent criteria to mitigate the risk of disease transmission from a nominally healthy donor to the recipient [8]. Before undergoing FMT, donors are subjected to thorough screening to rule out conditions such as HIV, syphilis, hepatitis A, B, C, or autoimmune diseases. Similarly, donors must not be overweight and they must be free of any tumors, inflammation, diabetes, infectious diseases, or metabolic syndromes [8,9,10,11].
Up until 2020, the only established application for FMT was in treating the persistent and difficult cases of the Clostridioides difficile infection (CDI), where it has been shown to be highly effective, achieving success rates of over 80–85% [12,13,14]. Recent studies, however, indicate that disorders specific to the pancreas might be influenced by the microbiota, whether through the direct effects of the pancreatic microbiota or indirectly via the intestinal microbiota [15,16,17].
The link between such microbial modulation and the emergence of pancreatic diseases, including pancreatic ductal adenocarcinoma, acute and chronic pancreatitis, and type 1 diabetes mellitus, will be explored. This insight opens up the potential use of the FMT in the treatment of these pancreatic conditions. This review aims to collate and discuss recent research on how gut microbiota can be utilized in diagnosing pancreatic pathologies through distinctive changes and particularly how modulating the microbiota via FMT can impact treatments for various pancreatic disorders, highlighting its potential benefits.
2. Microbiota Changes in Pancreatic Disorders
Analyzing microbiota is increasingly widespread in the study of digestive tract disorders, including those affecting the pancreas. Several authors have started identifying specific microbiota patterns for each disease. This approach could markedly enhance the diagnosis of future patients, especially in the cases of pancreatic cancer, by relying exclusively on the analysis of the microbiota [18,19]. Microbiota analysis is non-invasive, which could increase patient compliance with this type of testing and consequently increase the number of diagnoses at an earlier stage. Ren et al. not only showed that certain bacterial species are found in higher quantities in patients suffering from a certain pathology, but also observed notable differences in the quantity of Streptococcus in stool between those with pancreatic head cancer and those with pancreatic body cancer. The interaction between the intrapancreatic microbiome and gut microbiota has been recognized as a factor affecting the progression of patients with pancreatic tumor diseases [20]. Lu et al. have even demonstrated that the pattern of oral microbiota alterations can be correlated with the diagnosis of pancreatic cancer [21]. Both oral and rectal microbiota were utilized in a multicentric study involving over 400 patients, which identified that the composition of the microbiota can predict the course of acute pancreatitis. In the future, this kind of analysis could play a role in diagnosing pancreatitis and in directing treatment strategies [22].
3. Fecal Microbiota Transplantation (FMT) and Its Role in Pancreatic Illness
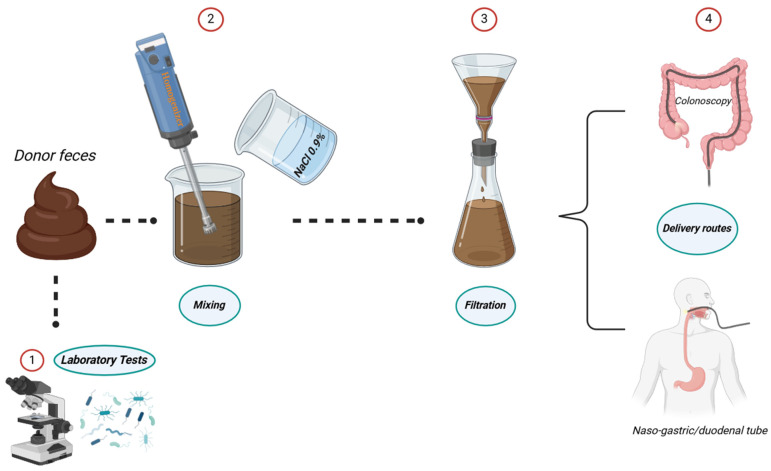
It is important to understand the foundational techniques involved in preparing the FMT, which may differ depending on the illness being addressed. The approach to donor selection, screening, and fecal material processing must be customized to suit the condition at hand [23].
A procedure for FMT, particularly aimed at treating CDI, is detailed by Perez et al. [24]. It involves mixing 50–60 g of stool with 200–300 mL of a diluent until it becomes a liquid suspension [24]. After allowing the mixture to settle for 5 min, it is filtered through gauze. The resulting liquid can be used immediately, refrigerated for up to 24 h at 2–8 °C, or frozen for up to 30 days at −20 °C. If glycerin is added, the fecal material can be preserved at −80 °C without losing its effectiveness. The method of FMT administration can vary, including oral (via the upper gastrointestinal tract), nasal, or rectal (via colonoscopy) routes [25,26,27]. Rectal administration is often preferred due to the fecal substrate’s location deep within the cecum, minimizing the risk of its removal (Figure 1). However, administering FMT through a nasogastric or nasoduodenal tube may lead to complications from the high levels of pathogenic bacteria in the upper digestive and respiratory tracts, potentially causing pulmonary or gastrointestinal issues [24]. Important studies in the literature have underscored the feasibility of culturing the microbiota to manipulate its content, aiming to stimulate the growth of specific bacterial strains, thus leading to the enhanced efficacy of the FMT [28,29].
Figure 1.
Necessary steps for preparing the stool for microbiota transfer.
In addition to its role in combatting recurrent CDI, FMT has shown promise in the field of oncology, especially in mitigating the side effects of tumor radiotherapy [30,31,32]. Radiation therapy often leads to damage and has negative effects on the gut microbiota’s composition [33]. Research by Cui et al. highlighted that animals subjected to radiation exhibited a higher survival rate following FMT [34]. Furthermore, both male and female mice that received the transplant showed an increase in peripheral white blood cell counts, along with enhancements in gastrointestinal function and the integrity of the intestinal epithelium [34]. Consequently, the researchers proposed that FMT could serve as a radioprotective agent, potentially improving outcomes in cancer treatment involving radiotherapy [34,35].
In addition to the discoveries concerning radiotherapy, a groundbreaking development in oncology involving the gut microbiota is the realization that the pancreas possesses its own unique microbial makeup. This challenges the previous belief that the pancreas was a sterile organ [15,36]. Numerous studies have confirmed the presence of micro-organisms within the pancreas under non-diseased conditions, referred to as the inherent pancreatic microbiota [16]. Although research in this area is still in its early stages and thus limited, this revelation introduces new avenues for exploring oncogenesis and identifying novel treatment targets for pancreatic tumors.
Additionally, a novel concept known as the “microbiota-pancreas axis” has been introduced, detailing a bidirectional communication system that illustrates the influence of pancreatic physiological functions on the intestinal microbiota and how the intestinal microbiota, in turn, affects the pancreas [37,38,39]. The FMT induces a notable response, particularly involving regulatory T cells, iNKT cells, and Antigen Presenting Cells (among others), which diminish the inflammatory response. This has been evidenced not only in patients with Clostridioides difficile infection but also in those with other pathologies. Reducing the activity of the inflammatory system could offer substantial advantages in pancreatic conditions, a significant number of which are inflammation-driven [40,41,42]. Building on this, the discussion will extend to the effects of both the inherent pancreatic and intestinal microbiota on the progression of intrinsic pancreatic diseases, whether malignant or benign.
The bacteria identified in the transplanted fecal matter that showed the most significant beneficial effects for patients with various pathologies are listed in Table 1, but the table also highlights the dominant microbiotas in humans and mice. These are particularly important because they can be stimulated to enhance the desired effect of the FMT.
Table 1.
Predominant beneficial bacteria in fecal microbiota transplantation and dominant microbiota in humans and mice.
| Dominant Microbiota in Humans and Mice | |||
|---|---|---|---|
| Authors | Dominant microbiota | Host | |
| Li et al. [43] | Lactobacillus reuteri, Enterococcus faecium, Escherichia coli, Bacteroides ovatus, Fusobacterium gastrosuis | Mice | |
| Rinninella et al. [44] | Fecalibacterium prausnitzii, Clostridium spp., Lactobacillus reuteri, Enterococcus faecium, Bacteroides vulgatus, Bacteroides uniformis Prevotella spp., Parabacteroides distasonis | Human | |
| Predominantly Beneficial Microbiota in Various Pathologies | |||
| Authors | Micro-organism | Pathology | Main Findings |
| Lima et al. [45] | Odoribacter splanchnicus | Ulcerative Colitis | Odoribacter splanchnicus plays a crucial role in enhancing both metabolic functions and immune cell resilience against colitis. |
| Yang et al. [46] | Lactobacillus acidophilus, coleohominis, gallinarum; Selenomonas artemidis | Constipation, depression, and anxiety | Psychiatric symptoms were improved after the FMT. |
| Aggarwala et al. [47] | Bacteroides vulgatus, uniformis ovatus, cellulosilyticus; Parabacteroides distasonis, merdae |
Clostridioides difficile infection |
Significantly predicted the clinical outcomes of the transplantation for up to five years. |
| Lee et al. [48] | Bacteroidales | Non specific intestinal disorders | The study effectively used genome-resolved metagenomics to track and identify bacterial strains that persist in FMT recipients, deepening insights into microbiota dynamics post-transplant. |
| Zhang et al. [49] | Faecalibacterium; Eubacterium; Roseburia | Inflammatory Bowel Disease | Symptoms were improved after FMT but outcomes are linked to gut microbiota and methodology variations, emphasizing the need for standardized research to improve FMT effectiveness through microbial and metabolite adjustments. |
4. The Intestinal-Pancreatic Axis
The gut–pancreatic axis, modulated by the microbiome, plays a pivotal role in pancreatic immunity and disease pathogenesis. This axis is defined by critical interactions: gut-derived short-chain fatty acids (SCFAs) regulate immune responses in the pancreas by controlling the production of the cathelicidin-related antimicrobial peptide in beta-cells [50]. Furthermore, pancreatic acinar cells affect gut microbiota and intestinal immunity through the secretion of specific antimicrobials [50]. These findings refute the traditional view of the pancreas as a sterile environment, illustrating instead a dynamic pancreatic microbiome of migratory bacteria and fungi from the gut, which may impact diseases like pancreatic ductal adenocarcinoma (PDAC) [50].
5. Pancreatic Cancer
Pancreatic cancer (PC) ranks among the deadliest diseases globally. In the United States, pancreatic ductal adenocarcinoma (PDAC), a particular type of pancreatic tumor, is recognized as the third highest cause of cancer death and accounts for 85% of all malignant pancreatic conditions [51].
The combination of ineffective treatments and late diagnosis contributes to the extremely low survival rates in pancreatic cancer, further hampered by the slim prospects for successful tumor removal. Although the complex interactions between pancreatic cancer and the gut microbiota are recognized, it is still unclear whether a causal relationship exists. Modifying the gut microbiota presents a promising approach for influencing tumorigenesis and the management of pancreatic cancer in the future, with ongoing research exploring antibiotics, probiotics, and FMT as potential treatments [52,53,54].
Studies have indicated that individuals with periodontal disease exhibit a higher incidence of PDAC compared to those without periodontal issues [55]. In light of this, Farrell and colleagues’ study was conducted to profile the oral microbiome of patients to explore its potential link with pancreatic cancer [56]. The researchers identified significant microbiome differences using bacterial microarrays and qPCR validation. Specifically, PDAC patients showed alterations in 31 species and reductions in 25, notably within the Firmicutes, Proteobacteria, and Actinobacteria groups. Further validation highlighted Neisseria elongata and Streptococcus mitis as significantly reduced in PDAC patients, suggesting their potential as biomarkers for the disease [56].
Pushalkar et al. undertook a study to investigate if gut bacteria could move to the pancreas, employing Enterococcus faecalis marked with fluorescent labels and Escherichia coli tagged with GFP, administered to mice [57]. The study confirmed bacterial migration to the pancreas, suggesting a direct impact of the gut bacteria on the pancreatic environment. Further, using 16S rRNA FISH and qPCR, a higher bacterial abundance was found in PDAC in both mice and humans compared to normal pancreas. The sequencing of 16S rRNA genes in human PDAC tumors identified 13 bacterial phyla with Proteobacteria, Bacteroidetes, and Firmicutes being predominant. Significant differences in bacterial composition between PDAC and normal pancreas were highlighted and oral antibiotics were found to slow oncogenesis, while transferring specific bacteria or fecal material from PDAC mice accelerated tumorigenesis. These results underline the microbiome’s role in disease progression and suggest that targeting the microbiota could potentially reduce PDAC risk [57].
FMT is being recognized as a promising strategy that could hinder the progression of pancreatic cancer. This process might be enabled by adjusting the gut microbiota, which includes decreasing the production of the inflammatory agents and cytotoxic byproducts, as well as correcting dysbiosis in the gut flora [58].
Another research focused on FMT related to pancreatic cancer involved transferring fecal matter from subjects with advanced stages of PC, those who have survived PC for more than five years, and healthy participants into mice. Thirty-five days after the transplantation, mice that received the FMT from the group with advanced pancreatic cancer showed markedly larger tumors compared to those receiving FMT from long-term PC survivors or healthy controls [20].
In addition to the previous studies about the connection between periodontal disease and a higher risk of PC, Castillo et al. explored the link between oral bacteria and pancreatic cancer progression by examining tissue samples from 50 pancreatic cancer patients at Rhode Island Hospital and 34 organs from the National Disease Research Interchange [59]. Using 16S rRNA gene sequencing on 189 tissue samples and 57 swabs, along with 12 stool samples, the study found diverse bacterial DNA in pancreatic tissues [59]. Bacterial DNA varied highly among individuals and sites within the pancreas and duodenum, regardless of cancer presence. Non-cancer subjects had higher levels of Lactobacillus, while cancer subjects showed an increased abundance of the Fusobacterium spp., known to be associated with colorectal cancer [59]. This study suggests bacteria may migrate from the gut to the pancreas, highlighting the need for further research on their potential causal role in pancreatic cancer [59].
Mitsuhashi et al. found that individuals with PC exhibit a higher abundance of Fusobacterium compared to healthy individuals. Their research further indicated that the increased occurrence of the Fusobacterium species in tissues affected by pancreatic cancer independently correlates with a worse outcome. This suggests that Fusobacterium species might serve as a promising prognostic marker for pancreatic cancer [60].
These studies collectively suggest that both intra- and extra-pancreatic microbiota play roles in the development, progression, and severity of pancreatic cancer, paving the way for potential new treatments centered around microbiota. FMT, known for its effectiveness and safety in conditions like Clostridioides difficile, emerges as a promising option. However, research on FMT’s use in pancreatic cancer treatment is sparse. Upcoming studies on animals are essential to verify the effectiveness and safety of the FMT and to investigate its potential for clinical application. There is also a need for tailored therapeutic strategies that target specific gut microbiota functions, improve transplant compatibility, and refine personalized FMT treatments for pancreatic cancer [3].
6. Acute and Chronic Pancreatitis
In addition to PC, other pancreatic disorders like pancreatitis, which can be either acute or chronic, also exhibit changes in gut microbiota composition, highlighting them as potential targets for FMT treatments.
Acute pancreatitis (AP) is a medical emergency characterized by the rapid-onset inflammation of the pancreas that can escalate into a systemic illness, presenting symptoms such as intense abdominal pain, vomiting, and nausea and may result in serious complications like infection and organ failure [61,62,63]. Given the critical nature of AP and its potential to endanger life, understanding the microbiome’s influence on the disease’s progression and severity has become a key research focus. This includes investigating how dysbiosis or microbial imbalance in the gut flora may contribute to the breakdown of the intestinal barrier function [61].
Patients with AP have been found to show changes in the diversity and composition of their intestinal microbiota [64,65,66,67,68]. Research indicates that acute inflammation can heighten intestinal permeability, possibly by altering the expression of claudin-4, a protein vital for tight junction integrity in intestinal epithelia [69]. Reduced claudin-4 levels weaken the connections between epithelial cells, impairing the epithelial barrier and resulting in an increased permeability. This allows substances to pass through more easily, potentially causing systemic and pancreatic bacterial translocation and perpetuating inflammation [69].
In addition to the increased permeability caused by inflammation, other contributing pathological mechanisms, such as microcirculation changes and ischemia–reperfusion injury also induce similar effects [37]. These changes compromise intestinal permeability, resulting in a condition referred to as leaky gut. When coupled with bacterial overgrowth, this leaky gut condition further facilitates the movement of bacteria and toxins towards the pancreas, aggravating pancreatic inflammation. This escalation of the inflammation can lead to further damage, potentially resulting in fibrosis or, in more severe instances, necrosis [37].
Furthermore, recent research has observed a rise in pathogenic bacteria during acute inflammatory states, alongside a reduction in short-chain fatty acids (SCFAs) such as propionate, acetate, and butyrate, which are metabolites generated by the gut bacteria via the fermentation of dietary fibers [20]. They play a vital role in maintaining gut homeostasis by restoring its flora, strengthening the intestinal epithelial barrier, and modulating inflammation [61]. They can also reduce systemic inflammatory responses, aid in the repair of the damaged pancreas and prevent dysfunction in other organs. Given these multiple benefits, increasing SCFA levels could represent a novel protective strategy for treating AP. Such treatments could be directly applied through butyrate administration or indirectly through fiber and probiotic supplementation via FMT. These approaches offer promising additions to conventional enteral nutrition support in AP therapy.
A stratified study analyzing patients with AP found that microbiota alterations vary with the disease’s severity, notably including a decrease in SCFA-producing bacteria which correlates with increased severity due to compromised intestinal barrier integrity [70]. Zhu et al. collected clinical data and fecal samples from 165 adults, revealing that severe AP is marked by a reduction in commensal bacteria like Bacteroides, Alloprevotella, and Blautia [70]. Further investigation in male mice with AP showed significant differences in intestinal microbiota compared to healthy controls, linking altered microbiota with systemic inflammation and intestinal barrier dysfunction.
Tan et al.’s findings align with Zhu et al.’s research, highlighting that microbial composition changes as AP progresses [71]. Specifically, they observed a significant rise in potentially pathogenic bacteria like Enterobacteriaceae and Enterococcus in severe AP (SAP) compared to milder forms (MAP or MSAP) [71]. Both studies conclude that the intestinal microbiota significantly influences AP as a mediator, with its imbalance associated with the disease’s severity [71].
Yang et al. documented a case where FMT was applied to a patient with moderately severe acute pancreatitis (MSAP) complicated by a severe CDI, a condition for which FMT is a common treatment [72]. The treatment led to the resolution of diarrhea within five days, with no adverse events reported and a colonoscopy 40 days after discharge showed complete recovery. However, the impact of the FMT on MSAP itself was not evaluated and while some studies have explored FMT in AP within mice models, showing increased bacteria translocation and mortality in AP mice receiving FMT from healthy ones, the effects and safety of the FMT for AP in humans remain unclear, indicating a need for further research [72].
Chronic pancreatitis (CP) is defined by the persistent inflammation of the gland, marked by distinctive features including the dilation of the Wirsung duct, calcifications, atrophy, and fibrosis [73]. Chronic pancreatitis results in the progressive dysfunction of both the endocrine and exocrine systems, with studies showing that individuals with CP undergo dysbiosis characterized by a rise in pathogenic bacteria [74,75].
Pan et al. highlight that intestinal dysbiosis, especially the reduction in SCFA-producing bacteria, accelerates the advancement of CP, similar to what is observed in AP [70,76]. Reduced SCFA levels undermine intestinal barrier integrity, leading to worsened pancreatic fibrosis, increased monocyte recruitment, and enhanced M2 macrophage polarization [77]. Supplementation with SCFAs has been shown to bolster intestinal barrier function and decrease monocyte recruitment, thereby offering greater protection against CP development. This highlights the therapeutic potential of dietary SCFAs and the targeting of SCFA-producing Gram-positive bacteria in CP’s prevention and management [77]. Additionally, studies indicate that pancreatic enzyme replacement therapy (PERT) effectively manages exocrine pancreatic insufficiency (PEI) symptoms by improving patients’ nutritional status [77,78].
Nishiyama et al. analyzed fecal samples from mice receiving pancreatic enzyme replacement therapy (PERT) compared to control mice to investigate changes in the intestinal microbiota. Their results bolstered the theory that PERT alleviates symptoms associated with exocrine pancreatic insufficiency (PEI), observing modifications in the gut microbiota composition of the treated mice. In particular, mice treated with PERT exhibited a notable rise in Akkermansia muciniphila and Lactobacillus reuteri populations [79].
In a double-blind, controlled, randomized trial, Dos Santos and colleagues examined the impact of synbiotics on the gut microenvironment in patients with CP [80]. The intervention group was administered a synbiotic combination that included 12 g daily of Lactobacillus casei, Lactobacillus rhamnosus, Lactobacillus acidophilus, and Bifidobacterium bifidum, whereas the control group was given 12 g daily of a medium absorption complex carbohydrate [80]. The research concluded that synbiotics resulted in better clinical and laboratory results for patients with CP, highlighting the potential of strategies aimed at manipulating the intestinal microbiome as viable treatments for this chronic condition [80].
These studies collectively hint at microbiota manipulation, with its affordability and ease of implementation, as not only a novel therapeutic avenue for CP but also as a preventive strategy to mitigate its symptoms and complications.
7. Type 1 Diabetes
Type 1 diabetes (T1D) is an autoimmune disorder characterized by the autoimmune destruction of the β cells in the pancreas, which are responsible for insulin production, and is another disorder likely linked to the dysregulation of our microbiota. Consequently, T1D may also stand to benefit from FMT treatments [74,81,82,83]. The development of T1D is shaped by environmental and genetic influences that affect immune regulation, with factors like viral infections, diet, and vitamin D deficiency linked to its onset.
Research, including a 2018 longitudinal study, has explored how gut microbiota may predispose individuals to T1D [84]. This study tracked the gut microbiomes of infants at genetic risk for T1D, collecting fecal samples from 3 months old until T1D diagnosis. Although the overall microbial composition was similar between T1D cases and controls, children without T1D showed a higher abundance of SCFA-producing bacteria in their gut microbiomes.
The research suggests that SCFAs may play a protective role in preventing T1D, as a lower presence of SCFA-producing bacteria is noted in T1D cases [74]. Zheng et al. also found a link between T1D and an increased Bacteroidetes/Firmicutes ratio, along with a reduced α-diversity in fecal microbiota [85]. T1D individuals showed higher levels of certain bacteria like Clostridium and Bacteroides, while beneficial bacteria such as Lactobacillus and Bifidobacterium were less common. This imbalance in gut microbiota is associated with an increased intestinal permeability seen in T1D children. Although no current treatments directly target gut microbiome alterations to delay or prevent T1D, emerging data point towards potential strategies, including microbiome modulation and enhancing diversity, perhaps by using Escherichia coli Nissle (EcN) to reduce pathogenic bacteria colonization [86].
8. Therapeutic Prospects in Pancreatic Disorders
8.1. Pancreatic Cancer
The role of micro-organisms like HCV, HBV, Helicobacter pylori, and HPV in cancer development highlights a complex interplay between environmental factors and host genetics, suggesting micro-organisms may synergistically contribute to tumorigenesis. The microbiota, a community of such micro-organisms, has been recognized as a crucial element in cancer biology. Although not fully understood, the interaction between the microbiota and cancer may involve bacterial metabolites that offer protective benefits against tumors [81]. For instance, acetate not only mitigates pancreatitis and reduces PDAC risk factors but also influences epigenetic changes in mesenchymal stem cells, promoting their transformation into cancer-associated fibroblasts that increase PDAC cell invasiveness. The link between the microbiota and pancreatic cancer was initially proposed following the detection of H. pylori (HP) in pancreatitis patients, leading to further research on the connections between fecal, pancreatic, intestinal, and oral microbiota and pancreatic cancer [81].
Xu’s study finds a significant link between HP infection and pancreatic cancer, especially in economically underdeveloped regions. However, no positive association is observed between specific H. pylori strains (CagA+ or VacA-positive) and pancreatic cancer [87]. While HP infection overall may raise pancreatic cancer risk, further research is needed to understand this relationship fully [87].
As the literature also underscores, the potential of the FMT as a novel therapeutic avenue is gaining attention. Research suggests a link between gut dysbiosis and pancreatic cancer, potentially due to bacterial translocation [88]. The role of both the oral and endogenous pancreatic microbiota further highlights the intricate microbial interactions involved in pancreatic cancer, underscoring FMT’s potential to address these imbalances. Yet, the efficacy and safety of the FMT in this context require further investigation [53,89].
8.2. Acute and Chronic Pancreatitis
AP leads to an imbalance in the intestinal microbiota, exacerbating pancreatic harm and systemic inflammatory reactions. In this context, FMT offers a promising approach to diminish tissue damage and inflammation and to mitigate the dysbiosis [50,90].
In their study, Li Wei Liu and colleagues investigated how the gut microbiota and their metabolites affect AP to understand the related pancreatic damage and inflammation better [91]. They discovered that normobiotic FMT corrects gut dysbiosis caused by AP, reducing its severity, including mitochondrial dysfunction, oxidative stress, and inflammation [91]. This improvement was linked to the increased levels of the NAD+-related metabolites, notably NMN, which mitigated the adverse effects of AP by enhancing pancreatic NAD+ levels. Furthermore, the study highlighted that activating the SIRT3-PRDX5 pathway through normobiotic FMT and NMN metabolism played a crucial role in exerting antioxidant and anti-inflammatory actions, suggesting normobiotic FMT as a viable treatment for PsA [91].
In Ding and his team’s study, they assessed FMT’s role in managing AP, focusing on its effect on intra-abdominal pressure, gastrointestinal function and infection rates [92]. Sixty patients were randomly assigned to receive either FMT or saline, showing no significant difference in gastrointestinal recovery between the two groups [92]. Although FMT led to increased levels of D-lactate and IL-6, suggesting potential adverse effects on the gastrointestinal barrier, it did not significantly benefit PAH or reduce infectious complications [92]. The findings indicate a need for further research to understand FMT’s effects and suggest using changes in gut microbiota as biomarkers for pancreatic fibrosis evaluation.
In the realm of pancreatic inflammation, including acute and chronic pancreatitis, FMT emerges as a promising treatment for addressing dysbiosis and its consequent effects. While its potential to alleviate the severity of acute pancreatitis through the modulation of the gut microbiota and the enhancement of the anti-inflammatory and antioxidative processes is recognized, the therapeutic impact on chronic pancreatitis and the prevention of fibrosis through microbiota modification also warrants further exploration [93,94].
These insights pave the way for new therapeutic strategies for acute, chronic, and autoimmune pancreatitis, with FMT offering a potential means to alter disease progression.
A study conducted by Li et al. explores how saikosaponin A affects the gut microbiota and SAP [95]. Through 16S rRNA gene sequencing and analyzing inflammatory and antioxidant markers, it was found that saikosaponin A promotes a healthier gut, increasing Lactobacillus and Prevotella, and reduces SAP symptoms [95]. This includes lower serum amylase, lipase, oxidative stress, and inflammation, with a boost in antioxidant signaling (Keap1-Nrf2-ARE) [95]. Similar outcomes from FMT suggest saikosaponin A‘s beneficial effects might be through microbiota improvement, highlighting the need for further investigation [95].
8.3. Type 1 Diabetes
T1D often leads to vascular and neurological complications, with current effective treatments being limited to lifestyle changes and pharmacological methods like insulin injections. However, chronic insulin use can result in obesity, hypoglycemia, hyperinsulinemia, as well as psychological and financial burdens. Given that T1D usually affects individuals at a young age and taking into account the significance of the gut microbiota in the disease’s development and progression, FMT presents a promising alternative.
In a 2022 experimental study, He et al. administered one to three cycles of FMT to two adolescent T1D patients, monitoring clinical outcomes, biochemical indices, and adjustments in therapeutic regimen and dosage [81]. The study, supported by the metagenomic sequencing of the fecal microbiota post-transplant, suggests that FMT protocols could be optimized for more effective outcomes, highlighting FMT’s potential as a viable treatment for autoimmune T1D, with implications for improving patient quality of life [81].
De Groot and colleagues found that FMT can preserve endogenous insulin production in patients with T1D diagnosed within the last 12 months [96]. The study divided participants aged 18 to 30, with recent T1D onset, into groups receiving either autologous or allogeneic FMTs for four months [96]. Results showed significant preservation of beta-cell function in the autologous FMT group over 12 months, linked to specific plasma metabolites and inversely related to Prevotella in the small intestine [96]. This preservation was evident regardless of the donor type, indicating FMT’s potential role in early T1D management [96].
Table 2 summarizes the main articles in the literature analyzing fecal microbiota transplantation in pancreatic disorders.
Table 2.
Key Studies in the literature on fecal microbiota transplantation in pancreatic pathology.
| Authors | Study Objective | Methodology | Main Findings |
|---|---|---|---|
| Yang et al. [72] | Examined the efficacy of fecal microbiota transplantation (FMT) in treating moderately severe acute pancreatitis complicated by severe Clostridioides difficile infection (CDI). | A case study of FMT application in patient with moderately severe acute pancreatitis and severe CDI. | FMT led to the resolution of diarrhea within five days with no adverse events reported. |
| He et al. [81] | Investigated the efficacy of the FMT in adolescent patients with type 1 diabetes (T1D). | The administration of one to three cycles of the FMT to adolescent T1D patients with the monitoring of clinical outcomes and adjustments in therapeutic regimen. | FMT protocols showed potential as a viable treatment for autoimmune T1D, with implications for improving patient quality of life. |
| Li Liu et al. [91] | Explored the impact of the gut microbiota and their metabolites on acute pancreatitis (AP). | The investigation of gut dysbiosis correction through normobiotic FMT in AP patients. | Normobiotic FMT corrected gut dysbiosis caused by AP, reducing its severity including mitochondrial dysfunction, oxidative stress, and inflammation. |
| Ding et al. [92] | Assessed the role of the FMT in managing acute pancreatitis. | Randomized controlled trial comparing FMT versus saline administration in AP patients. | No significant difference in gastrointestinal recovery observed between FMT and saline groups. Increased levels of D-lactate and IL-6 were noted with FMT, suggesting potential adverse effects on the gastrointestinal barrier. |
| De Groot et al. [96] | Explored the effect of the FMT on preserving endogenous insulin production in patients with recently diagnosed T1D. | The division of participants with recent T1D onset into groups receiving autologous or allogeneic FMTs. | A significant preservation of beta-cell function observed in the autologous FMT group over 12 months, linked to specific plasma metabolites. |
For T1D, the gut microbiome’s role in immune modulation suggests that FMT could offer therapeutic benefits by restoring gut microbiome balance, potentially slowing disease progression and reducing inflammation. While preliminary findings are promising, further studies are essential to validate FMT’s safety and efficacy in T1D management and its broader implications on patient quality of life and disease management [97,98].
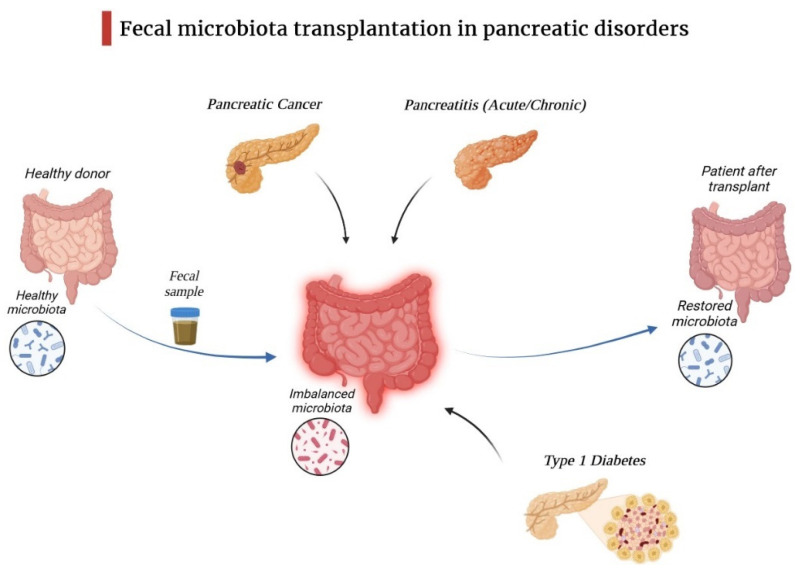
Figure 2 highlights the ability of fecal matter transfer to restore microbiota balance in pancreatic pathologies.
Figure 2.
Fecal microbiota transplantation in pancreatic disorders.
Although FMT is generally regarded as safe with few adverse effects, its long-term implications are yet to be thoroughly investigated. Future considerations include determining the frequency and duration of follow-ups post-FMT to monitor for long-term adverse events. The goal moving forward is to tailor FMT treatments to individual patients and specific conditions, considering the diversity of hosts and diseases [99].
9. Conclusions
The gut microbiota, a vast and intricate ecosystem, has been identified as a key player in diagnosing pancreatic disorders, but especially in influencing the onset and progression of pancreatic cancer, as well as acute and chronic pancreatitis and type 1 diabetes mellitus. Research into the gut microbiota has unveiled mechanisms underlying these pancreatic conditions, offering insights into their risk, severity, and the potential for new diagnostic and prognostic strategies.
The role of the intestinal microecology in the pancreas and broader physiological processes holds substantial scientific interest, warranting further investigation. The pursuit of novel therapeutic avenues to enhance patient outcomes for pancreatic disorders is crucial, with the microbiota presenting a vast potential for personalized treatments tailored to each individual’s microbiome and specific condition.
Abbreviations
FMT—fecal microbiota transplantation, CDI—Clostridioides difficile infection, PC—pancreatic cancer, PDAC—pancreatic ductal adenocarcinoma, AP—acute pancreatitis, SCFAs—short-chain fatty acids, MSAP—moderately severe acute pancreatitis, CP—chronic pancreatitis, PERT—pancreatic enzyme replacement therapy, PEI—exocrine pancreatic insufficiency, T1D—type 1 diabetes, EcN—Escherichia coli Nissle.
Author Contributions
Conceptualization and design: A.B., C.I. and S.B.T. Methodology: M.L.P. investigation: S.B.T., C.I. and P.A. resources: A.B. and M.L.P. Supervision: A.B., M.L.P. and P.A. Validation: A.B., C.I. and S.B.T. Writing—original draft: A.B., C.I., S.B.T., M.L.P. and P.A. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Guo Y., Chen X., Gong P., Li G., Yao W., Yang W. The Gut–Organ-Axis Concept: Advances the Application of Gut-on-Chip Technology. Int. J. Mol. Sci. 2023;24:4089. doi: 10.3390/ijms24044089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akshintala V.S., Talukdar R., Singh V.K., Goggins M. The Gut Microbiome in Pancreatic Disease. Clin. Gastroenterol. Hepatol. 2019;17:290–295. doi: 10.1016/j.cgh.2018.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Q., Zhang J., Zhu Y. Potential Roles of the Gut Microbiota in Pancreatic Carcinogenesis and Therapeutics. Front. Cell. Infect. Microbiol. 2022;12:872019. doi: 10.3389/fcimb.2022.872019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Su L., Hong Z., Zhou T., Jian Y., Xu M., Zhang X., Zhu X., Wang J. Health Improvements of Type 2 Diabetic Patients through Diet and Diet plus Fecal Microbiota Transplantation. Sci. Rep. 2022;12:1152. doi: 10.1038/s41598-022-05127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim K.O., Gluck M. Fecal Microbiota Transplantation: An Update on Clinical Practice. Clin. Endosc. 2019;52:137–143. doi: 10.5946/ce.2019.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J.-W., Kuo C.-H., Kuo F.-C., Wang Y.-K., Hsu W.-H., Yu F.-J., Hu H.-M., Hsu P.-I., Wang J.-Y., Wu D.-C. Fecal Microbiota Transplantation: Review and Update. J. Formos. Med. Assoc. 2019;118:S23–S31. doi: 10.1016/j.jfma.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Khoruts A., Sadowsky M.J. Understanding the Mechanisms of Faecal Microbiota Transplantation. Nat. Rev. Gastroenterol. Hepatol. 2016;13:508–516. doi: 10.1038/nrgastro.2016.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Antushevich H. Fecal Microbiota Transplantation in Disease Therapy. Clin. Chim. Acta. 2020;503:90–98. doi: 10.1016/j.cca.2019.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Seo H.S., Chin H.S., Kim Y.-H., Moon H.S., Kim K., Nguyen L.P., Yong D. Laboratory Aspects of Donor Screening for Fecal Microbiota Transplantation at a Korean Fecal Microbiota Bank. Ann. Lab. Med. 2021;41:424–428. doi: 10.3343/alm.2021.41.4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aira A., Arajol C., Casals-Pascual C., González-Suárez B., Martí S., Domínguez M.Á., Guardiola J., Soriano Á. Recommendations for Stool Donor Selection for Fecal Microbiota Transplant. Consensus Document Endorsed by the Catalan Society of Digestology, Catalan Society of Infectious Diseases and Clinical Microbiology and the GEMBIOTA Group from Spanish Society of Infectious Diseases and Clinical Microbiology. Enfermedades Infecc. Microbiol. Clin. Engl. Ed. 2022;40:142–146. doi: 10.1016/j.eimce.2021.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Bénard M.V., De Bruijn C.M.A., Fenneman A.C., Wortelboer K., Zeevenhoven J., Rethans B., Herrema H.J., Van Gool T., Nieuwdorp M., Benninga M.A., et al. Challenges and Costs of Donor Screening for Fecal Microbiota Transplantations. PLoS ONE. 2022;17:e0276323. doi: 10.1371/journal.pone.0276323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cammarota G., Ianiro G., Kelly C.R., Mullish B.H., Allegretti J.R., Kassam Z., Putignani L., Fischer M., Keller J.J., Costello S.P., et al. International Consensus Conference on Stool Banking for Faecal Microbiota Transplantation in Clinical Practice. Gut. 2019;68:2111–2121. doi: 10.1136/gutjnl-2019-319548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boicean A., Birlutiu V., Ichim C., Anderco P., Birsan S. Fecal Microbiota Transplantation in Inflammatory Bowel Disease. Biomedicines. 2023;11:1016. doi: 10.3390/biomedicines11041016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Porcari S., Severino A., Rondinella D., Bibbò S., Quaranta G., Masucci L., Maida M., Scaldaferri F., Sanguinetti M., Gasbarrini A., et al. Fecal Microbiota Transplantation for Recurrent Clostridioides difficile Infection in Patients with Concurrent Ulcerative Colitis. J. Autoimmun. 2023;141:103033. doi: 10.1016/j.jaut.2023.103033. [DOI] [PubMed] [Google Scholar]
- 15.Thomas R.M., Jobin C. Microbiota in Pancreatic Health and Disease: The next Frontier in Microbiome Research. Nat. Rev. Gastroenterol. Hepatol. 2020;17:53–64. doi: 10.1038/s41575-019-0242-7. [DOI] [PubMed] [Google Scholar]
- 16.Thomas R.M., Gharaibeh R.Z., Gauthier J., Beveridge M., Pope J.L., Guijarro M.V., Yu Q., He Z., Ohland C., Newsome R., et al. Intestinal Microbiota Enhances Pancreatic Carcinogenesis in Preclinical Models. Carcinogenesis. 2018;39:1068–1078. doi: 10.1093/carcin/bgy073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun J., Furio L., Mecheri R., van der Does A.M., Lundeberg E., Saveanu L., Chen Y., van Endert P., Agerberth B., Diana J. Pancreatic β-Cells Limit Autoimmune Diabetes via an Immunoregulatory Antimicrobial Peptide Expressed under the Influence of the Gut Microbiota. Immunity. 2015;43:304–317. doi: 10.1016/j.immuni.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 18.Ren Z., Jiang J., Xie H., Li A., Lu H., Xu S., Zhou L., Zhang H., Cui G., Chen X., et al. Gut Microbial Profile Analysis by MiSeq Sequencing of Pancreatic Carcinoma Patients in China. Oncotarget. 2017;8:95176–95191. doi: 10.18632/oncotarget.18820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kartal E., Schmidt T.S.B., Molina-Montes E., Rodríguez-Perales S., Wirbel J., Maistrenko O.M., Akanni W.A., Alashkar Alhamwe B., Alves R.J., Carrato A., et al. A Faecal Microbiota Signature with High Specificity for Pancreatic Cancer. Gut. 2022;71:1359–1372. doi: 10.1136/gutjnl-2021-324755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riquelme E., Zhang Y., Zhang L., Montiel M., Zoltan M., Dong W., Quesada P., Sahin I., Chandra V., San Lucas A., et al. Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes. Cell. 2019;178:795–806.e12. doi: 10.1016/j.cell.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu H., Ren Z., Li A., Li J., Xu S., Zhang H., Jiang J., Yang J., Luo Q., Zhou K., et al. Tongue Coating Microbiome Data Distinguish Patients with Pancreatic Head Cancer from Healthy Controls. J. Oral Microbiol. 2019;11:1563409. doi: 10.1080/20002297.2018.1563409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ammer-Herrmenau C., Antweiler K.L., Asendorf T., Beyer G., Buchholz S.M., Cameron S., Capurso G., Damm M., Dang L., Frost F., et al. Gut Microbiota Predicts Severity and Reveals Novel Metabolic Signatures in Acute Pancreatitis. Gut. 2023;73:485–495. doi: 10.1136/gutjnl-2023-330987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boicean A., Birlutiu V., Ichim C., Brusnic O., Onișor D.M. Fecal Microbiota Transplantation in Liver Cirrhosis. Biomedicines. 2023;11:2930. doi: 10.3390/biomedicines11112930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perez E., Lee C.H., Petrof E.O. A Practical Method for Preparation of Fecal Microbiota Transplantation. In: Roberts A.P., Mullany P., editors. Clostridium difficile. Volume 1476. Springer; New York, NY, USA: 2016. pp. 259–267. Methods in Molecular Biology. [DOI] [PubMed] [Google Scholar]
- 25.Gulati M., Singh S.K., Corrie L., Kaur I.P., Chandwani L. Delivery Routes for Faecal Microbiota Transplants: Available, Anticipated and Aspired. Pharmacol. Res. 2020;159:104954. doi: 10.1016/j.phrs.2020.104954. [DOI] [PubMed] [Google Scholar]
- 26.Brunse A., Martin L., Rasmussen T.S., Christensen L., Skovsted Cilieborg M., Wiese M., Khakimov B., Pieper R., Nielsen D.S., Sangild P.T., et al. Effect of Fecal Microbiota Transplantation Route of Administration on Gut Colonization and Host Response in Preterm Pigs. ISME J. 2019;13:720–733. doi: 10.1038/s41396-018-0301-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bakken J.S. Feces Transplantation for Recurrent Clostridium difficile Infection: US Experience and Recommendations. Microb. Ecol. Health Dis. 2015;26:27657. doi: 10.3402/mehd.v26.27657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goodman A.L., Kallstrom G., Faith J.J., Reyes A., Moore A., Dantas G., Gordon J.I. Extensive Personal Human Gut Microbiota Culture Collections Characterized and Manipulated in Gnotobiotic Mice. Proc. Natl. Acad. Sci. USA. 2011;108:6252–6257. doi: 10.1073/pnas.1102938108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Średnicka P., Roszko M.Ł., Popowski D., Kowalczyk M., Wójcicki M., Emanowicz P., Szczepańska M., Kotyrba D., Juszczuk-Kubiak E. Effect of in Vitro Cultivation on Human Gut Microbiota Composition Using 16S RDNA Amplicon Sequencing and Metabolomics Approach. Sci. Rep. 2023;13:3026. doi: 10.1038/s41598-023-29637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ding X., Li Q., Li P., Chen X., Xiang L., Bi L., Zhu J., Huang X., Cui B., Zhang F. Fecal Microbiota Transplantation: A Promising Treatment for Radiation Enteritis? Radiother. Oncol. 2020;143:12–18. doi: 10.1016/j.radonc.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 31.Yi Y., Lu W., Shen L., Wu Y., Zhang Z. The Gut Microbiota as a Booster for Radiotherapy: Novel Insights into Radio-Protection and Radiation Injury. Exp. Hematol. Oncol. 2023;12:48. doi: 10.1186/s40164-023-00410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang W., Cui B., Nie Y., Sun L., Zhang F. Radiation Injury and Gut Microbiota-Based Treatment. Protein Cell. 2024;15:83–97. doi: 10.1093/procel/pwad044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu J., Liu C., Yue J. Radiotherapy and the Gut Microbiome: Facts and Fiction. Radiat. Oncol. 2021;16:9. doi: 10.1186/s13014-020-01735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cui M., Xiao H., Li Y., Zhou L., Zhao S., Luo D., Zheng Q., Dong J., Zhao Y., Zhang X., et al. Faecal Microbiota Transplantation Protects against Radiation-induced Toxicity. EMBO Mol. Med. 2017;9:448–461. doi: 10.15252/emmm.201606932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao L.-Y., Mei J.-X., Yu G., Lei L., Zhang W.-H., Liu K., Chen X.-L., Kołat D., Yang K., Hu J.-K. Role of the Gut Microbiota in Anticancer Therapy: From Molecular Mechanisms to Clinical Applications. Signal Transduct. Target. Ther. 2023;8:201. doi: 10.1038/s41392-023-01406-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Halimi A., Gabarrini G., Sobkowiak M.J., Ateeb Z., Davanian H., Gaiser R.A., Arnelo U., Valente R., Wong A.Y.W., Moro C.F., et al. Isolation of Pancreatic Microbiota from Cystic Precursors of Pancreatic Cancer with Intracellular Growth and DNA Damaging Properties. Gut Microbes. 2021;13:1983101. doi: 10.1080/19490976.2021.1983101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pagliari D., Saviano A., Newton E.E., Serricchio M.L., Dal Lago A.A., Gasbarrini A., Cianci R. Gut Microbiota-Immune System Crosstalk and Pancreatic Disorders. Mediat. Inflamm. 2018;2018:7946431. doi: 10.1155/2018/7946431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang Z., Tanaka I., Pan Z., Ernst P.B., Kiyono H., Kurashima Y. Intestinal Homeostasis and Inflammation: Gut Microbiota at the Crossroads of Pancreas–Intestinal Barrier Axis. Eur. J. Immunol. 2022;52:1035–1046. doi: 10.1002/eji.202149532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ryu S.H., Stappenbeck T.S. Gut-Pancreatic Axis AMPlified in Islets of Langerhans. Immunity. 2015;43:216–218. doi: 10.1016/j.immuni.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Soveral L.F., Korczaguin G.G., Schmidt P.S., Nunes I.S., Fernandes C., Zárate-Bladés C.R. Immunological Mechanisms of Fecal Microbiota Transplantation in Recurrent Clostridioides difficile Infection. World J. Gastroenterol. 2022;28:4762–4772. doi: 10.3748/wjg.v28.i33.4762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li D., Cui L., Gao Y., Li Y., Tan X., Xu H. Fecal Microbiota Transplantation Improves Intestinal Inflammation in Mice with Ulcerative Colitis by Modulating Intestinal Flora Composition and Down-Regulating NF-KB Signaling Pathway. Microb. Pathog. 2022;173:105803. doi: 10.1016/j.micpath.2022.105803. [DOI] [PubMed] [Google Scholar]
- 42.Burrello C., Garavaglia F., Cribiù F.M., Ercoli G., Lopez G., Troisi J., Colucci A., Guglietta S., Carloni S., Guglielmetti S., et al. Therapeutic Faecal Microbiota Transplantation Controls Intestinal Inflammation through IL10 Secretion by Immune Cells. Nat. Commun. 2018;9:5184. doi: 10.1038/s41467-018-07359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li M., Yang H., Shao C., Liu Y., Wen S., Tang L. Application of Dominant Gut Microbiota Promises to Replace Fecal Microbiota Transplantation as a New Treatment for Alzheimer’s Disease. Microorganisms. 2023;11:2854. doi: 10.3390/microorganisms11122854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rinninella E., Raoul P., Cintoni M., Franceschi F., Miggiano G., Gasbarrini A., Mele M. What Is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. 2019;7:14. doi: 10.3390/microorganisms7010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lima S.F., Gogokhia L., Viladomiu M., Chou L., Putzel G., Jin W.-B., Pires S., Guo C.-J., Gerardin Y., Crawford C.V., et al. Transferable Immunoglobulin A–Coated Odoribacter Splanchnicus in Responders to Fecal Microbiota Transplantation for Ulcerative Colitis Limits Colonic Inflammation. Gastroenterology. 2022;162:166–178. doi: 10.1053/j.gastro.2021.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang C., Hu T., Xue X., Su X., Zhang X., Fan Y., Shen X., Dong X. Multi-Omics Analysis of Fecal Microbiota Transplantation’s Impact on Functional Constipation and Comorbid Depression and Anxiety. BMC Microbiol. 2023;23:389. doi: 10.1186/s12866-023-03123-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aggarwala V., Mogno I., Li Z., Yang C., Britton G.J., Chen-Liaw A., Mitcham J., Bongers G., Gevers D., Clemente J.C., et al. Precise Quantification of Bacterial Strains after Fecal Microbiota Transplantation Delineates Long-Term Engraftment and Explains Outcomes. Nat. Microbiol. 2021;6:1309–1318. doi: 10.1038/s41564-021-00966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee S.T.M., Kahn S.A., Delmont T.O., Shaiber A., Esen Ö.C., Hubert N.A., Morrison H.G., Antonopoulos D.A., Rubin D.T., Eren A.M. Tracking Microbial Colonization in Fecal Microbiota Transplantation Experiments via Genome-Resolved Metagenomics. Microbiome. 2017;5:50. doi: 10.1186/s40168-017-0270-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang J., Guo Y., Duan L. Features of Gut Microbiome Associated with Responses to Fecal Microbiota Transplantation for Inflammatory Bowel Disease: A Systematic Review. Front. Med. 2022;9:773105. doi: 10.3389/fmed.2022.773105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang T., Gao G., Sakandar H.A., Kwok L.-Y., Sun Z. Gut Dysbiosis in Pancreatic Diseases: A Causative Factor and a Novel Therapeutic Target. Front. Nutr. 2022;9:814269. doi: 10.3389/fnut.2022.814269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siegel R.L., Miller K.D., Jemal A. Cancer Statistics, 2016. CA Cancer J. Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 52.Li Q., Jin M., Liu Y., Jin L. Gut Microbiota: Its Potential Roles in Pancreatic Cancer. Front. Cell. Infect. Microbiol. 2020;10:572492. doi: 10.3389/fcimb.2020.572492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen D., Wu J., Jin D., Wang B., Cao H. Fecal Microbiota Transplantation in Cancer Management: Current Status and Perspectives. Int. J. Cancer. 2019;145:2021–2031. doi: 10.1002/ijc.32003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stoff R., Wolf Y., Boursi B. Fecal Microbiota Transplantation as a Cancer Therapeutic. Cancer J. 2023;29:102–108. doi: 10.1097/PPO.0000000000000651. [DOI] [PubMed] [Google Scholar]
- 55.Hujoel P.P., Drangsholt M., Spiekerman C., Weiss N.S. An Exploration of the Periodontitis–Cancer Association. Ann. Epidemiol. 2003;13:312–316. doi: 10.1016/S1047-2797(02)00425-8. [DOI] [PubMed] [Google Scholar]
- 56.Farrell J.J., Zhang L., Zhou H., Chia D., Elashoff D., Akin D., Paster B.J., Joshipura K., Wong D.T.W. Variations of Oral Microbiota Are Associated with Pancreatic Diseases Including Pancreatic Cancer. Gut. 2012;61:582–588. doi: 10.1136/gutjnl-2011-300784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pushalkar S., Hundeyin M., Daley D., Zambirinis C.P., Kurz E., Mishra A., Mohan N., Aykut B., Usyk M., Torres L.E., et al. The Pancreatic Cancer Microbiome Promotes Oncogenesis by Induction of Innate and Adaptive Immune Suppression. Cancer Discov. 2018;8:403–416. doi: 10.1158/2159-8290.CD-17-1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bibbò S., Ianiro G., Gasbarrini A., Cammarota G. Fecal Microbiota Transplantation: Past, Present and Future Perspectives. Minerva Gastroenterol. 2017;63:420–430. doi: 10.23736/S1121-421X.17.02374-1. [DOI] [PubMed] [Google Scholar]
- 59.Del Castillo E., Meier R., Chung M., Koestler D.C., Chen T., Paster B.J., Charpentier K.P., Kelsey K.T., Izard J., Michaud D.S. The Microbiomes of Pancreatic and Duodenum Tissue Overlap and Are Highly Subject Specific but Differ between Pancreatic Cancer and Noncancer Subjects. Cancer Epidemiol. Biomark. Prev. 2019;28:370–383. doi: 10.1158/1055-9965.EPI-18-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mitsuhashi K., Nosho K., Sukawa Y., Matsunaga Y., Ito M., Kurihara H., Kanno S., Igarashi H., Naito T., Adachi Y., et al. Association of Fusobacterium Species in Pancreatic Cancer Tissues with Molecular Features and Prognosis. Oncotarget. 2015;6:7209–7220. doi: 10.18632/oncotarget.3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li X.-Y., He C., Zhu Y., Lu N.-H. Role of Gut Microbiota on Intestinal Barrier Function in Acute Pancreatitis. World J. Gastroenterol. 2020;26:2187–2193. doi: 10.3748/wjg.v26.i18.2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Szatmary P., Grammatikopoulos T., Cai W., Huang W., Mukherjee R., Halloran C., Beyer G., Sutton R. Acute Pancreatitis: Diagnosis and Treatment. Drugs. 2022;82:1251–1276. doi: 10.1007/s40265-022-01766-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Boicean A., Birlutiu V., Ichim C., Todor S.B., Hasegan A., Bacila C., Solomon A., Cristian A., Dura H. Predictors of Post-ERCP Pancreatitis (P.E.P.) in Choledochal Lithiasis Extraction. J. Pers. Med. 2023;13:1356. doi: 10.3390/jpm13091356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yan X., Li J., Wu D. The Role of Short-Chain Fatty Acids in Acute Pancreatitis. Molecules. 2023;28:4985. doi: 10.3390/molecules28134985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patel B.K., Patel K.H., Bhatia M., Iyer S.G., Madhavan K., Moochhala S.M. Gut Microbiome in Acute Pancreatitis: A Review Based on Current Literature. World J. Gastroenterol. 2021;27:5019–5036. doi: 10.3748/wjg.v27.i30.5019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhu Y., Mei Q., Fu Y., Zeng Y. Alteration of Gut Microbiota in Acute Pancreatitis and Associated Therapeutic Strategies. Biomed. Pharmacother. 2021;141:111850. doi: 10.1016/j.biopha.2021.111850. [DOI] [PubMed] [Google Scholar]
- 67.Brubaker L., Luu S., Hoffman K., Wood A., Navarro Cagigas M., Yao Q., Petrosino J., Fisher W., Van Buren G. Microbiome Changes Associated with Acute and Chronic Pancreatitis: A Systematic Review. Pancreatology. 2021;21:1–14. doi: 10.1016/j.pan.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wu L., Hu J., Yi X., Lv J., Yao J., Tang W., Zhang S., Wan M. Gut Microbiota Interacts with Inflammatory Responses in Acute Pancreatitis. Ther. Adv. Gastroenterol. 2023;16:17562848231202132. doi: 10.1177/17562848231202133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Le Gall M., Gallois M., Sève B., Louveau I., Holst J.J., Oswald I.P., Lallès J.-P., Guilloteau P. Comparative Effect of Orally Administered Sodium Butyrate before or after Weaning on Growth and Several Indices of Gastrointestinal Biology of Piglets. Br. J. Nutr. 2009;102:1285–1296. doi: 10.1017/S0007114509990213. [DOI] [PubMed] [Google Scholar]
- 70.Zhu Y., He C., Li X., Cai Y., Hu J., Liao Y., Zhao J., Xia L., He W., Liu L., et al. Gut Microbiota Dysbiosis Worsens the Severity of Acute Pancreatitis in Patients and Mice. J. Gastroenterol. 2019;54:347–358. doi: 10.1007/s00535-018-1529-0. [DOI] [PubMed] [Google Scholar]
- 71.Tan C., Ling Z., Huang Y., Cao Y., Liu Q., Cai T., Yuan H., Liu C., Li Y., Xu K. Dysbiosis of Intestinal Microbiota Associated With Inflammation Involved in the Progression of Acute Pancreatitis. Pancreas. 2015;44:868–875. doi: 10.1097/MPA.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 72.Hu Y., Xiao H.-Y., He C., Lv N.-H., Zhu L. Fecal Microbiota Transplantation as an Effective Initial Therapy for Pancreatitis Complicated with Severe Clostridium difficile Infection: A Case Report. World J. Clin. Cases. 2019;7:2597–2604. doi: 10.12998/wjcc.v7.i17.2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dumonceau J.-M., Delhaye M., Tringali A., Arvanitakis M., Sanchez-Yague A., Vaysse T., Aithal G., Anderloni A., Bruno M., Cantú P., et al. Endoscopic Treatment of Chronic Pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline–Updated August 2018. Endoscopy. 2019;51:179–193. doi: 10.1055/a-0822-0832. [DOI] [PubMed] [Google Scholar]
- 74.Gesualdo M., Rizzi F., Bonetto S., Rizza S., Cravero F., Saracco G.M., De Angelis C.G. Pancreatic Diseases and Microbiota: A Literature Review and Future Perspectives. J. Clin. Med. 2020;9:3535. doi: 10.3390/jcm9113535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Duggan S.N. Negotiating the Complexities of Exocrine and Endocrine Dysfunction in Chronic Pancreatitis. Proc. Nutr. Soc. 2017;76:484–494. doi: 10.1017/S0029665117001045. [DOI] [PubMed] [Google Scholar]
- 76.Pan L.-L., Ren Z.-N., Yang J., Li B.-B., Huang Y.-W., Song D.-X., Li X., Xu J.-J., Bhatia M., Zou D.-W., et al. Gut Microbiota Controls the Development of Chronic Pancreatitis: A Critical Role of Short-Chain Fatty Acids-Producing Gram-Positive Bacteria. Acta Pharm. Sin. B. 2023;13:4202–4216. doi: 10.1016/j.apsb.2023.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.D’Haese J.G., Ceyhan G.O., Demir I.E., Layer P., Uhl W., Löhr M., Rychlik R., Pirilis K., Zöllner Y., Gradl B., et al. Pancreatic Enzyme Replacement Therapy in Patients With Exocrine Pancreatic Insufficiency Due to Chronic Pancreatitis: A 1-Year Disease Management Study on Symptom Control and Quality of Life. Pancreas. 2014;43:834–841. doi: 10.1097/MPA.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 78.Barkin J.A., Harb D., Kort J., Barkin J.S. Real-World Patient Experience with Pancreatic Enzyme Replacement Therapy in the Treatment of Exocrine Pancreatic Insufficiency. Pancreas. 2024;53:e16–e21. doi: 10.1097/MPA.0000000000002273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nishiyama H., Nagai T., Kudo M., Okazaki Y., Azuma Y., Watanabe T., Goto S., Ogata H., Sakurai T. Supplementation of Pancreatic Digestive Enzymes Alters the Composition of Intestinal Microbiota in Mice. Biochem. Biophys. Res. Commun. 2018;495:273–279. doi: 10.1016/j.bbrc.2017.10.130. [DOI] [PubMed] [Google Scholar]
- 80.Dos Santos P.Q., Guedes J.C., De Jesus R.P., Santos R.R.D., Fiaconne R.L. Effects of Using Symbiotics in the Clinical Nutritional Evolution of Patients with Chronic Pancreatitis: Study Prospective, Randomized, Controlled, Double Blind. Clin. Nutr. ESPEN. 2017;18:9–15. doi: 10.1016/j.clnesp.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 81.He L., Chen R., Zhang B., Zhang S., Khan B.A., Zhu D., Wu Z., Xiao C., Chen B., Chen F., et al. Fecal Microbiota Transplantation Treatment of Autoimmune-Mediated Type 1 Diabetes Mellitus. Front. Immunol. 2022;13:930872. doi: 10.3389/fimmu.2022.930872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kasti A. Fecal Microbiota Transplantation for The Early-Onset Type 1 Diabetes. Could It Be a Promising Solution? Kompass Nutr. Diet. 2022;2:36–38. doi: 10.1159/000522521. [DOI] [Google Scholar]
- 83.Fuhri Snethlage C.M., Nieuwdorp M., Van Raalte D.H., Rampanelli E., Verchere B.C., Hanssen N.M.J. Auto-Immunity and the Gut Microbiome in Type 1 Diabetes: Lessons from Rodent and Human Studies. Best Pract. Res. Clin. Endocrinol. Metab. 2021;35:101544. doi: 10.1016/j.beem.2021.101544. [DOI] [PubMed] [Google Scholar]
- 84.Vatanen T., Franzosa E.A., Schwager R., Tripathi S., Arthur T.D., Vehik K., Lernmark Å., Hagopian W.A., Rewers M.J., She J.-X., et al. The Human Gut Microbiome in Early-Onset Type 1 Diabetes from the TEDDY Study. Nature. 2018;562:589–594. doi: 10.1038/s41586-018-0620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zheng P., Li Z., Zhou Z. Gut Microbiome in Type 1 Diabetes: A Comprehensive Review. Diabetes Metab. Res. Rev. 2018;34:e3043. doi: 10.1002/dmrr.3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Knip M., Honkanen J. Modulation of Type 1 Diabetes Risk by the Intestinal Microbiome. Curr. Diab. Rep. 2017;17:105. doi: 10.1007/s11892-017-0933-9. [DOI] [PubMed] [Google Scholar]
- 87.Xu W., Zhou X., Yin M., Gao J., Weng Z., Xu C. The Relationship between Helicobacter Pylori and Pancreatic Cancer: A Meta-Analysis. Transl. Cancer Res. 2022;11:2810–2822. doi: 10.21037/tcr-21-2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kouzu K., Tsujimoto H., Kishi Y., Ueno H., Shinomiya N. Bacterial Translocation in Gastrointestinal Cancers and Cancer Treatment. Biomedicines. 2022;10:380. doi: 10.3390/biomedicines10020380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Merali N., Chouari T., Kayani K., Rayner C.J., Jiménez J.I., Krell J., Giovannetti E., Bagwan I., Relph K., Rockall T.A., et al. A Comprehensive Review of the Current and Future Role of the Microbiome in Pancreatic Ductal Adenocarcinoma. Cancers. 2022;14:1020. doi: 10.3390/cancers14041020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhang C., Li G., Lu T., Liu L., Sui Y., Bai R., Li L., Sun B. The Interaction of Microbiome and Pancreas in Acute Pancreatitis. Biomolecules. 2023;14:59. doi: 10.3390/biom14010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu L., Xie Y., Li G., Zhang T., Sui Y., Zhao Z., Zhang Y., Yang W., Geng X., Xue D., et al. Gut Microbiota-derived Nicotinamide Mononucleotide Alleviates Acute Pancreatitis by Activating Pancreatic SIRT3 Signalling. Br. J. Pharmacol. 2023;180:647–666. doi: 10.1111/bph.15980. [DOI] [PubMed] [Google Scholar]
- 92.Ding L., He C., Li X., Huang X., Lei Y., Ke H., Chen H., Yang Q., Cai Y., Liao Y., et al. Efficacy and Safety of Faecal Microbiota Transplantation for Acute Pancreatitis: A Randomised, Controlled Study. Front. Med. 2022;8:772454. doi: 10.3389/fmed.2021.772454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tan P., Li X., Shen J., Feng Q. Fecal Microbiota Transplantation for the Treatment of Inflammatory Bowel Disease: An Update. Front. Pharmacol. 2020;11:574533. doi: 10.3389/fphar.2020.574533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chechushkov A., Desyukevich P., Yakovlev T., Al Allaf L., Shrainer E., Morozov V., Tikunova N. Sterile Fecal Microbiota Transplantation Boosts Anti-Inflammatory T-Cell Response in Ulcerative Colitis Patients. Int. J. Mol. Sci. 2024;25:1886. doi: 10.3390/ijms25031886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Li J., Han J., Lv J., Wang S., Qu L., Jiang Y. Saikosaponin A-Induced Gut Microbiota Changes Attenuate Severe Acute Pancreatitis through the Activation of Keap1/Nrf2-ARE Antioxidant Signaling. Oxid. Med. Cell. Longev. 2020;2020:9217219. doi: 10.1155/2020/9217219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.De Groot P., Nikolic T., Pellegrini S., Sordi V., Imangaliyev S., Rampanelli E., Hanssen N., Attaye I., Bakker G., Duinkerken G., et al. Faecal Microbiota Transplantation Halts Progression of Human New-Onset Type 1 Diabetes in a Randomised Controlled Trial. Gut. 2021;70:92–105. doi: 10.1136/gutjnl-2020-322630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xie Y.-C., Jing X.-B., Chen X., Chen L.-Z., Zhang S.-H., Cai X.-B. Fecal Microbiota Transplantation Treatment for Type 1 Diabetes Mellitus with Malnutrition: A Case Report. Ther. Adv. Chronic Dis. 2022;13:204062232211174. doi: 10.1177/20406223221117449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Crudele L., Gadaleta R.M., Cariello M., Moschetta A. Gut Microbiota in the Pathogenesis and Therapeutic Approaches of Diabetes. eBioMedicine. 2023;97:104821. doi: 10.1016/j.ebiom.2023.104821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Park S.-Y., Seo G.S. Fecal Microbiota Transplantation: Is It Safe? Clin. Endosc. 2021;54:157–160. doi: 10.5946/ce.2021.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.