Abstract
Introduction
Mediastinal neuroendocrine tumors are rare malignancies with aggressive behavior and a grim prognosis. These malignancies often go undetected until they are diagnosed at advanced stages.
Case report
We present the case of 74 -years old man who was hospitalized because of non-ST elevation myocardial infarction and in case of three vessels coronary artery disease, coronary bypass surgery was planned. During preoperative investigation, computer tomography revealed a huge tumor (20 cm × 11 cm × 21 cm in size) in the anterior mediastinum. Successful simultaneous operation coronary bypass surgery and removal of the mediastinal tumor was performed.
Discussion
Surgery is the treatment of choice for neuroendocrine tumors but the relapse rate ranges between 5% and 30% and is higher (65%) in atypical neuroendocrine tumors and patients with mediastinal node involvement. Despite the poor prognosis of neuroendocrine tumors, the spread to the lymph nodes, the patient continues chemotherapy treatment 49 months after the operation.
Keywords: neuroendocrine mediastinum tumor, dyspnea, acute coronary syndrome, chest pain, carcinoid tumor
Introduction
Primary neuroendocrine tumors (NETs) of the mediastinum are rare and account from 2% to 4% of all mediastinal tumors.1–3 Atypical NETs are defined as tumors with 2–10 mitoses/2 mm2. 4 We present the case of an atypical NETs in 74-year-old man hospitalized because of non-ST elevation myocardial infarction (MI). Simultaneous operation of coronary bypass surgery (CABG) and removal of the mediastinal tumor (3 kg) were performed successfully. 49 months after operation, he continues treatment by oncologists. Written informed consent was obtained from the patient for publication of this case report and photos associated with this case report.
Case report
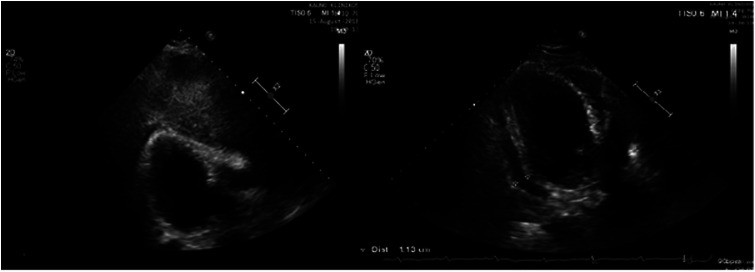
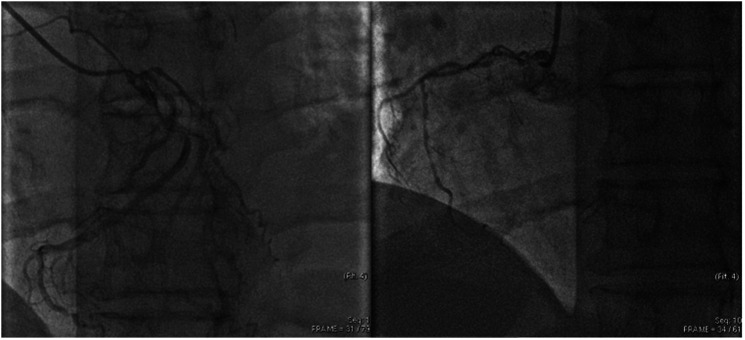
74-years old man was hospitalized because of non-ST elevation MI. He complained of chest pain and dyspnea even at rest. Dyspnea have been progressing during the past 3 months, while chest pain appeared 4 days before. Transthoracic echocardiography (TTE) (Figure 1) revealed mildly reduced left ventricle (LV) systolic function (LV EF 48%) with hypokinesis in inferior-posterior LV walls and mild pericardial effusion. Invasive coronary artery angiography (Figure 2) revealed three vessels disease: right coronary artery (RCA) - S2 – 95%, left anterior descending (LAD): S6 – 90%, S8 – 90%, S9 – 75%; left circumflex: S11 – 75%, S12 – 20%, S13 – 65%. Chest X-ray (Figure 3) showed homogeneous consolidation of the lower lobe of the left lung. Contrast-enhanced computed tomography (CT) (Figure 4) of the chest revealed a huge tumor (size 21 cm × 11 cm × 21 cm × 3 cm) in the anterior mediastinum with pronounced vascular network, displacing the surrounding organs. CT guided needle biopsy was performed. Histologically signs of a moderately-differentiated NETs were observed. Chromogranin A and 5-hydroxyindole-acetic acid were normal.
Figure 1.
2D echocardiography: parasternal long axis view and subcostal view. The heart was dislocated, large undefined masses were “covered” the heart in the chest.
Figure 2.
Left coronary artery angiogram: stenoses of left anterior descending artery (segments S6 – 90%, S8 –90%, S9 – 75%.) and left circumflex artery (segments S11 – 75%., S12 – 20%, S13 – 65%) Right coronary artery angiogram: segment S2 – 95%. stenosis.
Figure 3.
Chest X-ray – huge consolidated area in the left lung.
Figure 4.
Chest CT: tumor in anterior mediastinum with pathological vessel involvement.
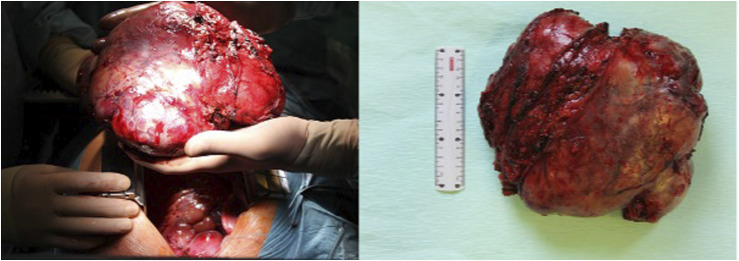
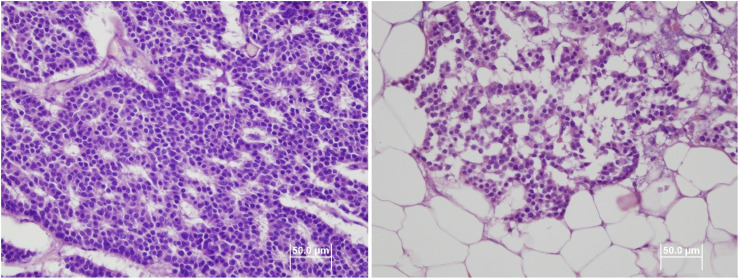
Heart team together with oncologists decision was simultaneous operation - CABG and removal of the mediastinal tumor. Tumor (Figure 5) with a capsule was removed radically. It started from the root of the right lung to the left, partially grown with the right pulmonary vein and aorta. The pericardium was restored with a synthetic patch and CABG (venous grafts) were performed. Histological examination showed moderately differentiated NETs (Figure 6). Tumor mitoses were found (2/10 mitoses/2 mm2), proliferation index was 2%. It was an infiltratively growing tumor formed by pseudo-rosette-like solid structures with a rim of relatively monomorphic, mitotically inactive cells with a chromatic nucleus and an average amount of light cytoplasm. Areas of necrosis were covering up to 20% of the tumor area. In two lymph nodes moderately differentiated NETs, G2 was also confirmed.
Figure 5.
Mediastinal tumor masses.
Figure 6.
Moderately differentiated neuroendocrine tumor.
Postoperative period was smooth. TTE after surgery showed preserved LV function and mild pericardial effusion. Somatostatin receptor scintigraphy showed no pathology, therefore control was planned after 3 months. Chest CT (6 months after operation) revealed the progression of the disease. Treatment with everolimus was started, but after 2 months life-threatening infectious complications were observed. The condition was assessed as pneumonitis or non-identified infection, therefore everolimus was stopped. The patient was observed and condition remained stable for 2 years.
Two years later somatostatin receptor scintigraphy showed multiple tumors containing somatostatin receptors in the mediastinum, left lung, liver, and left peritoneum. Treatment with octeotride was started and gave positive dynamics observed on chest CT and decreased chromogranin A level. During next control chest CT, 6 months later, negative dynamics of the disease was observed, that is why capecitabine and temozolamide was added. 49 months after operation, he continues treatment by oncologists.
Discussion
We describe a case of a primary NETs in the patient who was hospitalized because of acute MI. NETs may originate from neuroendocrine elements within the thymus (most frequently), from misplaced embryonal structures and even from parathyroid glands.5–7 Thymic NETs as in our presented case are the least common of all NETs. 8
Clinically patients with NETs may be asymptomatic or manifest local symptoms due to the compression of mediastinal structures, or systemic symptoms due to the tumor capacity to produce hormones or cytokines. 8 Our patient complained of chest pain and dyspnea which are typical symptoms in case of MI. CT-scan is important to define the tumor, its relationships with surrounding structures, but definitive diagnosis is based on histological examination and immunophenotypic markers. Tumor cell morphology, mitotic count and/or necrosis are crucial. 9 In our case, NETs was suspected based on chest X-ray and TTE data and CT revealed a huge tumor.
Surgery is the treatment of choice for NETs 10 but the relapse rate ranges between 5% and 30% and is higher (65%) in atypical NETs and patients with mediastinal node involvement.11,12 In our case, NETs were detected in two lymph nodes taken during surgery. Primary NETs are characterized by a poor prognosis due to their high propensity for local recurrence and earlier distant metastases. 13
Everolimus has been approved for the treatment of patients with advanced, progressive, well‐differentiated, non‐functional NETs.12,14 Somatostatin-analogue therapy is a good option in non-operable patients or in case of systemic recurrence. In our case postoperatively, in the absence of pathology during somatostatin scintigraphy and normal chromogranin A level, the patient was left for further observation. After CT scan, disease progression was detected and everolimus was started. Two months later, life-threatening infectious complications developed, due to which everolimus was discontinued. The patient remained in remission for 2 years. Repeated somatostatin receptor scintigraphy showed uptake of the disease that’s why octreotide was started, however, positive dynamics were observed only for 3 months. Capecitabine an temozolamide was added when the progress of the disease was confirmed. This treatment is used until now. Despite the poor prognosis of NETs, the spread to the lymph nodes, the patient continues treatment after 49 months after the operation.
Conclusions
Primary NETs express an aggressive behavior and poor prognosis due to local recurrence and earlier distant metastases. Early and accurate diagnosis are very important and surgery remains the mainstay of treatment, but long term disease control can be achieved with medical treatment.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was taken from the patient.
ORCID iDs
Eglė Rumbinaitė https://orcid.org/0000-0003-2657-5745
Šarūnė Stankevičienė https://orcid.org/0000-0001-9130-3709
References
- 1.Suster S, Moran CA. Neuroendocrine neoplasms of the mediastinum. Am J Clin Pathol 2001; 115 Suppl: S17–S27. [DOI] [PubMed] [Google Scholar]
- 2.Kan X, Wang P, Gong Z, et al. Investigation on computed tomography features of primary thymic atypical carcinoid tumors. J Comput Assist Tomogr 2017; 41(6): 990–994. [DOI] [PubMed] [Google Scholar]
- 3.Ventura L, Gnetti L, Silini EM, et al. Primary atypical carcinoid tumor of the mediastinum: A very rare finding. J Thorac Dis 2017; 9(4): E367–E372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bohnenberger H, Dinter H, König A, et al. Neuroendocrine tumors of the thymus and mediastinum. J Thorac Dis 2017; 9(Suppl 15): S1448–S1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maeda A, Nakata M, Yasuda K, et al. Unknown primary large cell neuroendocrine carcinoma (LCNEC) in the mediastinum. Gen Thorac Cardiovasc Surg 2013; 61: 542–545. [DOI] [PubMed] [Google Scholar]
- 6.Kacar F, Meteoglu I, Sen S, et al. Primary neuroendocrine carcinoma of the mediastinum. Pathol Oncol Res 2002; 8: 200–201. [DOI] [PubMed] [Google Scholar]
- 7.Madrid OA, Fatima S. Mediastinal carcinoid tumors. Treasure island (FL): StatPearls Publishing; 2022. PMID: 32809638. [PubMed] [Google Scholar]
- 8.Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005; 128: 2893–2909. [DOI] [PubMed] [Google Scholar]
- 9.Brcic L, Heidinger M, Popper H. Neuroendocrine Neoplasien des Mediastinums [Neuroendocrine neoplasms of the mediastinum]. Pathologe 2016; 37(5): 434–440. [DOI] [PubMed] [Google Scholar]
- 10.Caplin ME, Baudin E, Ferolla P, et al. ENETS consensus conference participants . Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol 2015; 26: 1604–1620. [DOI] [PubMed] [Google Scholar]
- 11.Sánchez de Cos Escuín J. Diagnosis and treatment of neuroendocrine lung tumors. Arch Bronconeumol 2014; 50: 392–396. [DOI] [PubMed] [Google Scholar]
- 12.Pusceddu S, Catena L, Valente M, et al. Long-term follow up of patients affected by pulmonary carcinoid at the Istituto Nazionale Tumori of Milan: a retrospective analysis. J Thorac Dis 2010; 2: 16–20. [PMC free article] [PubMed] [Google Scholar]
- 13.Gal AA, Kornstein MJ, Cohen C, et al. Neuroendocrine tumors of the thymus: a clinicopathological and prognostic study. Ann Thorac Surg 2001; 72: 1179–1182. [DOI] [PubMed] [Google Scholar]
- 14.Yao JC, Fazio N, Singh S, et al. RAD001 in Advanced Neuroendocrine Tumours, Fourth Trial RADIANT-4 Study Group . Everolimus for the treatment of advanced, non‐functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT‐4): A randomised, placebo‐controlled, phase 3 study. Lancet 2016; 387: 968–977. [DOI] [PMC free article] [PubMed] [Google Scholar]