Abstract
Introduction
There are very few scholastic studies applying a theory-driven methodology to analyse the employment of teledentistry in clinical practice by the Saudi dental community. The objective of this research was to predict the employment of teledentistry in clinical practice by the Saudi dental community using the UTAUT (Unified Theory of Acceptance and Use of Technology) model.
Methods
A countrywide survey was executed from November 2022 to April 2023 among the dental community (pre-graduate students, graduates, post-graduate students, general dentists, and specialist dentists) involved in clinical practice. The survey employed the UTAUT model, which has four fundamental constructs: performance expectancy (PE), effort expectancy (EE), social influence (SI) and facilitating conditions (FC). These constructs are known to impact the user's behavioural intention (BI). The four fundamental constructs were independent, and BI was the dependent variable. A Likert scale with five scores was used to record each variable. Descriptive statistics were used to describe all the constructs. Cronbach's alpha scores were used to measure the inner consistency of the Likert scale. Simple linear regression and multiple linear regression were used to determine the correlation between all the constructs and the overall model's prediction. The Statistical Package for the Social Sciences was applied for analysis. The study had 80% power and an alpha threshold of .05.
Results
The electronic survey was sent to 3000 participants, out of whom 2143 responded (response rate = 71.43%). PE (R2= 26%, p < .01) was the most significant predictor of the Saudi dental community BI to employ teledentistry in clinical practice, followed by SI (R2= 24%, p < .01), EE (R2= 19%, p < .01) and FC (R2= 6%, p < .01). With statistically significant predictive power, the UTAUT model explained 32% of the variance in the BI (R2= 0.32, p < .01).
Conclusions
Each UTAUT construct and the entire model were significantly correlated with the employment of teledentistry in clinical practice by the Saudi dental community. PE had the most salient correlation, followed by SI, EE and FC. The participants have perceived the benefits of teledentistry, increasing the future likelihood of its utilisation. The Saudi government could consider the UTAUT constructs to promote teledentistry in tandem with Vision 2030.
Keywords: telemedicine, teledentistry, dentistry, virtual medicine, remote consultation, COVID-19, theoretical model
Introduction
Teledentistry, a subset of telemedicine and telehealth, is an advanced digital health technology in dentistry. 1 The field of teledentistry combines dentistry and telecommunications to provide dental consultations and treatment planning via the remote exchange of clinical data and photographs. 2 Real-time patient consultations, patient data storage and forwarding to other dental professionals for consultations are the two teledentistry modes. The major applications of teledentistry in clinical practice include teleconsultation, telediagnosis, telecounseling, teletriage and telemonitoring. 3 Teledentistry can be used for tele-education as a distance learning modality for imparting dental education to students. 4 A few examples of teledentistry applications include dental emergency management, dental screening, the identification of dental caries, the detection of oral lesions, and the treatment of dental and temporomandibular problems.5–9 Teledentistry in clinical practice minimises costs, improves time efficiency, and provides convenient treatment options for patients and dentists.10,11 It has also improved access to and delivery of remote dental care.12,13
In alignment with the Kingdom's Vision 2030, the Saudi government has launched digital health projects and made large investments in the healthcare industry in recent years. 5 The Ministry of Health (MOH) has developed electronic strategies and also established the ‘Seha or Health’ application to offer telehealth consultations to the population. The MOH is also collaborating with the private sector to provide teledentistry consultations to patients. 14 During the Corona virus disease 2019 (COVID-19) outbreak, web-based teledentistry was widely used to transmit information to citizens and residents in Saudi Arabia. 15 However, the dental community in Saudi Arabia has not extensively employed teledentistry in mainstream clinical practice. A few surveys concluded that only 25–50% of Saudi dentists used teledentistry in clinical practice, and only 8.09% of the population used teledentistry during the pandemic.16–19
The successful implementation of teledentistry depends heavily on users acceptance of technology. The Unified Theory of Acceptance and Use of Technology (UTAUT) is a widely accepted and valid theoretical model for analysing users behavioural intentions (BI) towards accepting and utilising technology. 20 The UTAUT demonstrated strong predictive power (69% of the variance of BI) compared to the other technology acceptance models. 21
There are very few scholastic studies applying the UTAUT theory-driven methodology to analyse the employment of teledentistry in clinical practice by the Saudi dental community. Few studies have been reported to predict teledentistry adoption among pre-graduate dental students and adults in the United States.22–24 This model has also been used in a recent study to analyse the BI of the pre-graduate dental students in Saudi Arabia to utilise teledentistry. 25 Hence, the objective of this research was to predict the employment of teledentistry in clinical practice by the Saudi dental community using the UTAUT model. The research hypothesised that each UTAUT construct and the entire model would significantly correlate with the employment of teledentistry in clinical practice by the Saudi dental community.
Methods
Ethical considerations
This research was conducted after receiving ethical clearance (No. MUREC-HA-01-R-088) as per the World Medical Association Declaration of Helsinki and revision in 2013.
Sample size
GPower sample size software calculated the sample size using the following parameters:
F tests: linear multiple regression: fixed model, R2 deviation from zero
Analysis: A priori: compute the required sample size
Input:
α err prob = .05
Power (1-β err prob)= .80
Number of predictors = 4 (obtained from the key article)22,23
Squared multiple correlation coefficient = .40 (obtained from the key article)22,23
Effect size f2= .66
Output:
Noncentrality parameter λ = 16
Critical F = 2.89
Numerator df = 4
Denominator df = 19
Total sample size = 24 (minimum)
Actual power = .82
A minimum of 24 participants were suggested based on the calculation. However, we chose to contact all available participants as the study was planned as a nationwide survey.
Study design
This research was designed as descriptive, cross-sectional, and observational, with convenience sampling. A countrywide survey was executed from November 2022 to April 2023 among the Saudi dental community. The electronic survey was sent to 3000 prospective participants.
Inclusion criteria
Pre-graduate dental students (only third-, fourth-, and fifth-year were included as they had clinical postings).
Graduates and post-graduate dental students involved in clinical practice.
All dental professionals with a valid SCHFS (Saudi Commission for Health Specialties) licence in Saudi Arabia.
Exclusion criteria
Pre-graduate dental students (the first- and second-year were excluded as they were pre-clinical students).
Dental professionals involved in academia only.
All allied dental professionals.
The theoretical model and hypothesis testing
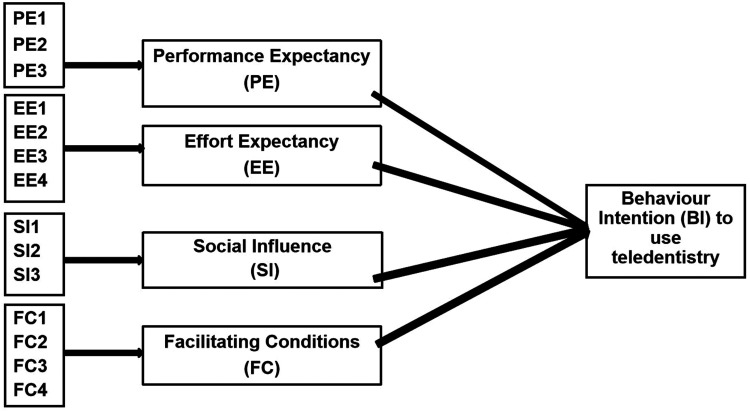
The UTAUT theoretical model was adapted with minimal modification from the original model. 26 The only modification done was alternating the word ‘system’ with ‘teledentistry’. The UTAUT model predicted the employment of teledentistry in clinical practice by the Saudi dental community (Figure 1). The UTAUT model, which has four fundamental constructs: performance expectancy (PE), effort expectancy (EE), social influence (SI) and facilitating conditions (FC). These constructs are known to impact the user's behavioural intention (BI). 26 PE reflects the participant's opinions on the benefits and productivity of teledentistry. EE reflects the participant's perceptions regarding the simplicity and complexity of employing teledentistry. SI reflects the participant's viewpoint about the impact of the employment of teledentistry on significant individuals, such as co-workers or employers. FC reflect the participant's perceptions of the existence of sufficient infrastructure to support the employment of teledentistry. The BI reflects the participant's intention to employ teledentistry in clinical practice. The four fundamental constructs were independent, and BI was the dependent variable. Since there is no commercialisation or legal regulation regarding the employment of teledentistry in clinical practice in Saudi Arabia, the BI was used as an outcome rather than actual utilisation. 14
Figure 1.
The UTAUT model (Copyright: Elsevier Inc. 2020; American Dental Education Association Wiley 2020; Cureus 2023).22,23,25
The theoretical model served as the foundation for examining five hypotheses.22,23,25
Hypothesis 1: PE is positively correlated with BI to employ teledentistry.
Hypothesis 2: EE is positively correlated with BI to employ teledentistry.
Hypothesis 3: SI is positively correlated with BI to employ teledentistry.
Hypothesis 4: FC is positively correlated with BI to employ teledentistry.
Hypothesis 5: The UTAUT model significantly predicts the BI to employ teledentistry in clinical practice as a whole.
Questionnaire and survey
The questionnaire used for the survey was adopted from previous studies with minor modifications to confirm the aim of our study (Copyright: Elsevier Inc. 2020; Wiley 2020 American Dental Education Association; Cureus 2023).22,23,25 It was administered in English and Arabic (Supplemental file 1). It consisted of three sections: the first section was comprised of general information and consent; the second section included demographic characteristics and professional profiles; and the third section included the UTAUT model. The demographic characteristics (age, sex and nationality) and professional profiles (location of clinical practice, qualification and work experience) were collected to get the background characteristics of the participants as they could possibly influence the study results. 27 In the UTAUT model, the participant's perceptions about each variable were recorded using statement items on a Likert scale with five scores. A higher score would indicate a greater intention to employ teledentistry in clinical practice. 28
Prior to the distribution of the survey, a team of four research experts from our institution with adequate language proficiency and prior experience in teledentistry and dental public health reviewed the questionnaire in both languages. Further, a piloting phase was conducted for both surveys, involving 50 dental students each, to review and assess the clarity, validity and reliability of the survey before it was disseminated.
The prospective participants in various dental colleges, hospitals and clinics were invited through emails and social media platforms. The link for the electronic survey (created in Google Forms) was sent to them along with the invitation. The non-respondents received two periodic reminders every week. Participant anonymity was ensured, and informed written consent was received.
Statistical analysis
Descriptive statistics were used to describe all the constructs. Cronbach's alpha (α) scores were used to measure the inner consistency of the Likert scale. Simple linear regression was used to test the correlation between each construct and the outcome. Multiple linear regression was used to examine the linear relationship between the set of constructs and the outcome as well as the overall model's prediction. The Statistical Package for the Social Sciences (version 24; SPSS Inc., Chicago, USA) was applied for analysis. The study had 80% power and an alpha threshold of .05.
Results
Sample characteristics
A total of 2143 participants (response rate = 71.43%) responded to the survey. The demographic characteristics showed that most of the participants were 21–30 years old (68.6%), males (68.7%) and Saudi citizens (94%). The professional profile indicated that the majority were from the central region (51.1%), nearly half were pre-graduate dental students (47.5%), and they had a minimum work experience of up to 5 years (70.3%) (Table 1).
Table 1.
Sample characteristics.
| Characteristics | Category | Frequency | % |
|---|---|---|---|
| Age (in years) | 21–30 | 1470 | 68.59 |
| 31–40 | 627 | 29.26 | |
| 41–50 | 31 | 1.45 | |
| ≥ 51 | 15 | 0.70 | |
| Gender | Male | 1473 | 68.73 |
| Female | 670 | 31.27 | |
| Nationality | Saudi | 2014 | 93.98 |
| Non-Saudi | 129 | 6.02 | |
| Location of clinical practice in the country | Central | 1096 | 51.14 |
| West | 61 | 2.85 | |
| North | 218 | 10.17 | |
| East | 426 | 19.88 | |
| South | 342 | 15.96 | |
| Qualification | Pre-graduate dental students | 1018 | 47.50 |
| Graduates | 334 | 15.59 | |
| Post-graduate dental students | 43 | 2.01 | |
| General dentists | 225 | 10.50 | |
| Specialist dentists | 523 | 24.40 | |
| Work experience (in years) | 0–5 | 1506 | 70.27 |
| 6–10 | 419 | 19.55 | |
| 11–15 | 182 | 8.68 | |
| ≥ 16 | 36 | 1.68 |
Descriptive statistics
The mean for all the fundamental constructs was greater than three. However, the mean BI was 2.84, which indicates a moderately fair intention to employ teledentistry in clinical practice by the Saudi dental community (Table 2).
Table 2.
The UTAUT constructs and its measuring scale items.
| Constructs | Items | Mean | Standard deviation | Cronbach's alpha (α) |
|---|---|---|---|---|
| Performance expectancy | PE1: Useful in clinical practice | 4.06 | 0.64 | 0.97 |
| PE2: Increasing productivity | ||||
| PE3: Time-saving | ||||
| Effort expectancy | EE1: Clear and understandable | 3.72 | 0.57 | 0.95 |
| EE2: Easy to learn | ||||
| EE3: Easy to use | ||||
| EE4: Easy to operate | ||||
| Social influence | SI1: Individuals recommend teledentistry | 3.76 | 0.58 | 0.94 |
| SI2: Co-workers recommend teledentistry | ||||
| SI3: Institution recommend teledentistry | ||||
| Facilitating conditions | FC1: Have resources to use teledentistry | 3.22 | 0.47 | 0.84 |
| FC2: Have knowledge to use teledentistry | ||||
| FC3: Compatible with other systems | ||||
| FC4: Assistance from a specific person (or group) | ||||
| Behavioral intention | BI1: Employ teledentistry in future | 2.84 | 0.49 | 0.97 |
| BI2: Anticipate the use of teledentistry in future | ||||
| BI3: Planning to use teledentistry in future |
UTAUT: Unified Theory of Acceptance and Use of Technology.
Reliability assessment
The reliability scores of all constructs ranged from .84 to .97, which indicated good to excellent reliability scores for the UTAUT constructs. Among the independent variables, FC (α = .84) had the lowest reliability score. The dependent variable, BI (α = .97), had the highest reliability score (Table 2).
Hypothesis testing
The first four hypotheses were tested using simple linear regression. The findings validated each UTAUT construct's correlation with the employment of teledentistry in clinical practice by the Saudi dental community.
There was a significant salient correlation between PE and BI. PE had the highest correlation efficiency (r = .51, p < .01). PE accounted for 26% of the variance in BI to employ teledentistry (F(1770)= 134.83, R2= .26, p < .01), hence supporting hypothesis 1 (Table 3).
Table 3.
Correlation analysis and hypothesis testing.
| Hypothesis | Construct | r | R2 | p | Hypothesis results |
|---|---|---|---|---|---|
| 1 | Performance expectancy | 0.51 | 26% | <.001 | Supported |
| 2 | Effort expectancy | 0.44 | 19% | <.001 | Supported |
| 3 | Social influence | 0.49 | 24% | <.001 | Supported |
| 4 | Facilitating conditions | 0.25 | 6% | <.001 | Supported |
| 5 | The UTAUT model | 0.56 | 32% | <.001 | Supported |
UTAUT: Unified Theory of Acceptance and Use of Technology.
There was a significantly moderate positive correlation (r = .44, p < .01) between EE and BI to employ teledentistry in clinical practice. EE accounted for 19% of the variance in BI to employ teledentistry (F(1518) = 99.43, R2= .19, p < .01), hence supporting hypothesis 2 (Table 3).
The SI also had a significantly moderate positive correlation (r = .49, p < .01) with BI to employ teledentistry in clinical practice. SI accounted for 24% of the variance in BI to employ teledentistry (F(1696) = 125.13, R2= .24, p < .01), hence supporting hypothesis 3 (Table 3).
There was a significantly low positive correlation (r = .25, p < .01) between FC and BI to employ teledentistry in clinical practice. FC accounted for 6% of the variance in the BI to employ teledentistry (F(1150) = 33.44, p < .01, R2= .06), hence supporting hypothesis 4 (Table 3).
Multiple regression tests were used to examine the fifth hypothesis. The UTAUT model, as a whole, could significantly predict the BI to employ teledentistry in clinical practice by the Saudi dental community (F(4256)= 41.28, R2= .32, p < .01) and supported hypothesis 5. The regression analysis showed that the combined independent variables could account for 32% of the variance in the BI (Table 3).
Discussion
The current research was effective in predicting the employment of teledentistry in clinical practice by the Saudi dental community. Our findings provided empirical support for every study hypothesis.
The Saudi dental community's BI was best forecasted by PE, being the salient correlation among all the UTAUT constructs. Hence, it can be inferred that the participants have perceived the favourable effects of teledentistry in resolving problems and drawing logical conclusions in their daily clinical practice. This outcome is consistent with similar studies done among dental students and graduates utilising the same theoretical model.22,23,25 Similar observations were proposed while determining professionals acceptance and use of tele-rehabilitation technology and telehealth records.28–33 However, PE did not yield meaningful interpretations about the acceptance of information systems among healthcare professionals in Canada. 34
Our results revealed a direct correlation between EE and BI. This implies that the dentists were ready to employ teledentistry in their practices if they were convinced that it could be implemented quickly and easily. To enable this, dentists should be proficient in computer science and have sufficient knowledge of information technology. 35 The knowledge and expertise of the dental practitioners in teledentistry should be continually improved through conferences, workshops and training programmes. 18 In congruence with our study results, EE was the most influential factor affecting physicians perceptions of using mobile health applications. 36 However, some studies agree on an insignificant correlation between EE and the actual use of telehealth technology.30,37,38
Furthermore, the results revealed a significant correlation between SI and BI. This suggests that external validation and support from organisations, employers or colleagues will play a critical role in developing clinicians decisions to employ teledentistry. According to research, 70% of Saudi dentists are in favour of utilising teledentistry for Vision 2030. 17 Moreover, public perceptions of teledentistry were positive. 14 This suggests a positive social influence supporting the implementation of teledentistry in the country. Concurrent with the results of our study, SI was an important factor influencing physician perspectives on practicing telemedicine in the Philippines and the adoption of teledentistry by US adults.24,39 SI was the only predictor influencing the adoption of telehealth applications by diabetic patients.40,41
The FC was the least significant correlating factor affecting the BI. Therefore, it can be assumed that the Saudi dental community's perception of the infrastructure's availability and technical support has no discernible impact on their decision to employ teledentistry in clinical practice. However, FC still has a major influence on a professional's BI in the dental care sector. In agreement with our results, FC was an influencing factor in predicting the users intentions to adopt cloud-based mobile health services for primary care. 41 Another study proposed this factor as the most prominent construct influencing physicians utilisation of telemedicine among health care professionals in Ethiopia. 42
The entire UTAUT model could predict the Saudi dental community's BI to employ teledentistry. Similar results were obtained when predicting the BI regarding the adoption of teledentistry, telemedicine, telepsychology, health technology systems, health software, medical education and other applications in telehealth.22,23,28,31,39,40,43–48
In our research, all the UTAUT constructs accounted for only 32% of the variance in the BI to employ teledentistry in clinical practice. This variance percentage was less than 70% of the participants BI, as predicted by the original model. 26 Contrary to our results, the UTAUT model demonstrated 60% of the variance in BI of pre-graduate students and graduates in Saudi Arabia to adopt teledentistry. 25 Similarly, in several studies, the UTAUT model had an explanatory capability ranging from 40% to 64% variation of BI to use teledentistry and telemedicine among healthcare professionals.22,23,39,42,49,50 In our research, the lower prediction value of BI may be attributed to the heterogeneous sample and convenience sampling. Most of the participants were in the age range of 21 to 30, were pre-graduate dental students, and had minimal experience up to 5 years in dentistry. There could be a possible lack of awareness, knowledge and sophistication required to use teledentistry among them. Dental universities and programme directors can consider the inclusion of teledentistry in the curriculum of dental schools. This may encourage pre-graduate dental students, graduates, and post-graduate dental students to promote the utilisation of teledentistry in their future clinical practice. 18 A focused campaign is required to educate dentists and the public regarding the true potential of this technology. 51 The MOH, SCHFS, and the Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) could enforce legal regulations, health policies, and healthcare practices when implementing teledentistry in the country. 15 Structured and sustainable business models and marketing strategies should be developed to commercialise the benefits of teledentistry usage in Saudi Arabia. 52
Limitations
This is a predictive study with theoretical support that measures behavioural intention rather than actual employment, which might not fully capture the complexities of teledentistry adoption in real-world settings.53,54 Moreover, the participants involved only a cross-section of the Saudi dental community, with a heterogeneous sample and convenient sampling comprising different ages, skills and experiences. These may act as confounding factors and limit the external validity and generalizability of the study. The selection of a homogeneous sample and census sampling would have produced more accurate and reliable results. It would have been feasible to determine the actual employment of teledentistry within the faculty and students of our university, but the application would be limited due to the absence of commercialisation or legal regulations in Saudi Arabia. 14
Future research
Being an advanced technology, this study opens the door to further research possibilities. A cohort study can be conducted in the same population to examine the actual employment of teledentistry in clinical practice and understand the success of this theoretical model. An assessment of the employment of teledentistry in academia among dental universities, programme leaders and academicians is required. The adoption of teledentistry by allied dental professionals needs to be researched. The utilisation of teledentistry by the general population requires further investigation. The factors affecting the dentist's and patient's resistance to teledentistry and strategies to overcome it should be explored.
Conclusions
Each UTAUT construct and the entire model were significantly correlated with the employment of teledentistry in clinical practice by the Saudi dental community. PE had the most salient correlation, followed by SI, EE and FC. The participants have perceived the benefits of teledentistry, increasing the future likelihood of its utilisation. The Saudi government could consider the UTAUT constructs to promote teledentistry in tandem with Vision 2030.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241253739 for Predicting the employment of teledentistry in clinical practice by the Saudi dental community using a theoretical model by Angel M Joseph, Rasha A Alsalman, Wjoud A Almasoud, Reem Almutairi, Rawan B Alammari, Yahya AM Deeban, Mohammed Z Mustafa and Amar A Thakare in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241253739 for Predicting the employment of teledentistry in clinical practice by the Saudi dental community using a theoretical model by Angel M Joseph, Rasha A Alsalman, Wjoud A Almasoud, Reem Almutairi, Rawan B Alammari, Yahya AM Deeban, Mohammed Z Mustafa and Amar A Thakare in DIGITAL HEALTH
Acknowledgements
The authors would like to thank the participants for their time and willingness to participate in the study. The authors also thank Dr Pooja Latti of the COHORT Research Group for helping with the statistical analysis for the study.
Footnotes
Contributorship: AMJ, RAA and WAA researched literature and conceived the study. RA, RBA, YAMD, MZM and AAT were involved in protocol development, gaining ethical approval, patient recruitment and data analysis. AMJ, RAA and WAA wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval: The ethics committee of Majmaah University approved this study (REC number: MUREC-HA-01-R-088).
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Deanship of Scientific Research, Majmaah University, Al-Majmaah 11952, Saudi Arabia (grant number R-2024-1064).
Guarantor: AMJ.
ORCID iD: Angel M Joseph https://orcid.org/0000-0003-2402-9011
Supplemental material: Supplemental material for this article is available online.
References
- 1.Ghai S. Teledentistry during COVID-19 pandemic. Diabetes Metab Syndr 2020; 14: 933–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jampani ND, Nutalapati R, Dontula BSet al. et al. Applications of teledentistry: a literature review and update. J Int Soc Prev Community Dent 2011; 1: 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golsanamloo O, Iranizadeh S, Jamei Khosroshahi AR, et al. Accuracy of teledentistry for diagnosis and treatment planning of pediatric patients during COVID-19 pandemic. Int J Telemed Appl 2022; 2022: 4147720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farooq I, Ali S, Moheet IAet al. et al. COVID-19 outbreak, disruption of dental education, and the role of teledentistry. Pak J Med Sci 2020; 36: 1726–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharka R, Abed H, Dziedzic A. Can undergraduate dental education be online and virtual during the COVID-19 era? Clinical training as a crucial element of practical competencies [version 1]. MedEdPublish 2020; 9: 215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joseph A, Joseph AM, James JP, et al. Evaluation of age, chief complaint, diagnosis, and treatment done during the first dental visit among children in an academic dental institution in southern Kerala, India. J Pharmacy Bioallied Sci 2023; 15: S641–S645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minervini G, Franco R, Marrapodi MM, et al. Correlation between temporomandibular disorders (TMD) and posture evaluated trough the diagnostic criteria for temporomandibular disorders (DC/TMD): a systematic review with meta-analysis. J Clin Med 2023; 12: 2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minervini G, Franco R, Marrapodi MM, et al. Prevalence of temporomandibular disorders in subjects affected by Parkinson disease: a systematic review and metanalysis. J Oral Rehabil 2023; 50: 877–885. [DOI] [PubMed] [Google Scholar]
- 9.Uhrin E, Domokos Z, Czumbel LM, et al. Teledentistry: a future solution in the diagnosis of oral lesions: diagnostic meta-analysis and systematic review. Telemed J E Health 2023; 29: 1591–1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Islam MRR, Islam R, Ferdous S, et al. Teledentistry as an effective tool for the communication improvement between dentists and patients: an overview. Healthcare (Basel) 2022; 10: 1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nemeth O, Simon F, Benhamida A, et al. Ehealth, teledentistry and health workforce challenges: results of a pilot project. BMC Oral Health 2022; 22: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiwari T, Diep V, Tranby E, et al. Dentist perceptions about the value of teledentistry. BMC Oral Health 2022; 22: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maqsood A, Sadiq MSK, Mirza D, et al. The teledentistry, impact, current trends, and application in dentistry: a global study. Biomed Res Int 2021; 2021: 5437237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El Tantawi M, Lam WYH, Giraudeau N, et al. Teledentistry from research to practice: a tale of nineteen countries. Front Oral Health 2023; 4: 1188557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdul NS. Teledentistry application during COVID-19 pandemic in Saudi Arabia: an overview. Ann Dental Specialty 2021; 9: 13–15. [Google Scholar]
- 16.Almazrooa SA, Mansour GA, Alhamed SA, et al. The application of teledentistry for Saudi patients care: a national survey study. J Dent Sci 2021; 16: 280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aboalshamat KT. Awareness of, beliefs about, practices of, and barriers to teledentistry among dental students and the implications for Saudi Arabia vision 2030 and corona virus pandemic. J Int Soc Prevent Communit Dent 2020; 10: 431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nassani MZ, Al-Maweri SA, AlSheddi A, et al. Teledentistry – knowledge, practice and attitudes of dental practitioners in Saudi Arabia: a nationwide web-based survey. Healthcare 2021; 9: 1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bugis BA. Patients self-reporting of utilizing teledental services during the COVID-19 pandemic in Saudi Arabia. J Patient Exp 2022; 9: 23743735221112209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rouidi M, Elmajid EA, Hamdoune A, et al. TAM-UTAUT and the acceptance of remote healthcare technologies by healthcare professionals: a systematic review. Inform Med Unlocked 2022; 32: 101008. [Google Scholar]
- 21.Momani AM. The unified theory of acceptance and use of technology: a new approach in technology acceptance. Int J Sociotechnol Knowledge Dev 2020; 12: 79–98. [Google Scholar]
- 22.Alabdullah JH. Predictors of dental students behavioral intention use of teledentistry: an application of the Unified Theory of Acceptance and Use of Technology (UTAUT) Model. Doctor of Philosophy (PhD) Dissertation 2020; Health Services Research: Old Dominion University. DOI: 10.25777/xqhg-yt76.
- 23.Alabdullah JH, Van Lunen BL, Claiborne DM, et al. Application of the unified theory of acceptance and use of technology model to predict dental students behavioural intention to use teledentistry. J Dent Educ 2020; 84: 1262–1269. [DOI] [PubMed] [Google Scholar]
- 24.VanDeWiele MD, Hastings AM, Evans MD, et al. Using the unified theory of acceptance and use of technology (UTAUT) to predict the behavioural intent of teledentistry utilisation amongst United States adults. J Telemed Telecare 2023: 1357633X231182405. DOI: 10.1177/1357633X231182405. [DOI] [PubMed] [Google Scholar]
- 25.Sharka R, Sedayo L, Aldahwani S, et al. Factors affecting the adoption of teledentistry based on the unified theory of acceptance and use of technology model. Cureus 2023; 15: e46016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Venkatesh V, Morris MG, Davis GBet al. et al. User acceptance of information technology: toward a unified view. MIS Q 2003; 27: 425–478. [Google Scholar]
- 27.Bahanan L, Alsharif M. Factors affecting the acceptance of teledentistry determined using the technology acceptance model: a cross-sectional study. Digit Health 2023; 9: 20552076231158034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharifian R, Askarian F, Nematolahi Met al. et al. Factors influencing nurse’s acceptance of hospital information systems in Iran: application of the unified theory of acceptance and use of technology. Health Inf Manage J 2014; 43: 23–28. [DOI] [PubMed] [Google Scholar]
- 29.Liu L, Miguel Cruz A, Rios Rincon A, et al. What factors determine therapists acceptance of new technologies for rehabilitation – a study using the unified theory of acceptance and use of technology (UTAUT). Disabil Rehabil 2015; 37: 447–455. [DOI] [PubMed] [Google Scholar]
- 30.Maillet E, Mathieu L, Sicotte C. Modeling factors explaining the acceptance, actual use and satisfaction of nurses using an electronic patient record in acute care settings: an extension of the UTAUT. Int J Med Inform 2015; 84: 36–47. [DOI] [PubMed] [Google Scholar]
- 31.Ahmadi M, Mehrabi N, Sheikhtaheri Aet al. et al. Acceptability of picture archiving and communication system (PACS) among hospital healthcare personnel based on a unified theory of acceptance and use of technology. Electron Physician 2017; 9: 5325–5330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jahanbakhsh M, Peikari HR, Hazhir Fet al. et al. An investigation into the effective factors on the acceptance and use of integrated health system in the primary health-care centers. J Edu Health Promot 2018; 7: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu D, Maimaitijiang R, Gu J, et al. Using the unified theory of acceptance and use of technology (UTAUT) to investigate the intention to use physical activity apps: cross-sectional survey. JMIR Mhealth Uhealth 2019; 7: e13127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ifinedo P. Technology acceptance by health professionals in Canada: an analysis with a modified UTAUT model. Proc Ann Hawaii Int Conf System Sci 2012: 2937–2946. DOI: 10.1109/HICSS.2012.556. [DOI] [Google Scholar]
- 35.Chaudhary FA, Ahmad B, Javed MQ, et al. Teledentistry awareness, its usefulness, and challenges among dental professionals in Pakistan and Saudi Arabia. Digit Health 2022; 8: 20552076221089776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Emre S, Sevgi O-Y, Soner Y. Understanding the perception towards using mHealth applications in practice: physician’s perspective. Inf Dev 2018; 34: 182–200. [Google Scholar]
- 37.Ibrahim S, Donelle L, Regan Set al. et al. Predicting registered nurses behavioural intention to use electronic documentation system in home care: application of an adapted unified theory of acceptance and use of technology model. Nurs Leadersh (Tor Ont) 2019; 32: 48–70. [DOI] [PubMed] [Google Scholar]
- 38.Woo K, Dowding DW. Decision-making factors associated with telehealth adoption by patients with heart failure at home: a qualitative study. Comput Inform Nurs 2020; 38: 204–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pasco PM. Physician user perspectives in the practice of telemedicine in the Philippines. J Int Soc Telemed eHealth 2016; 4: e26. [Google Scholar]
- 40.Zhang Y, Liu C, Luo S, et al. Factors influencing patients intentions to use diabetes management apps based on an extended unified theory of acceptance and use of technology model: web-based survey. J Med Internet Res 2019; 21: e15023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khatun F, Palas MU, Ray PK. Using the unified theory of acceptance and use of technology model to analyse cloud-based mHealth service for primary care. Digit Med 2017; 3: 69–75. [Google Scholar]
- 42.Mengesha G, Garfield MJ. A contextualized IT adoption and use model for telemedicine in Ethiopia. Inf Technol Dev 2019; 25: 184–203. [Google Scholar]
- 43.Idoga PE, Toycan M, Nadiri Het al. et al. Assessing factors militating against the acceptance and successful implementation of a cloud based health center from the healthcare professionals perspective: a survey of hospitals in Benue state, north central Nigeria. BMC Med Inform Decis Mak 2019; 19: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Azizi SM, Roozbahani N, Khatony A. Factors affecting the acceptance of blended learning in medical education: application of UTAUT2 model. BMC Med Educ 2020; 20: 367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barzegari S, Ghazisaeedi M, Askarian F, et al. Hospital information system acceptance among the educational hospitals. J Nurs Midwifery Sci 2020; 7: 186–193. [Google Scholar]
- 46.Farhady S, Sepehri MM, Pourfathollah AA. Evaluation of effective factors in the acceptance of mobile health technology using the unified theory of acceptance and use of technology (UTAUT), case study: blood transfusion complications in thalassemia patients. Med J Islam Repub Iran 2020; 34: 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van der Waal NE, de Wit J, Bol N, et al. Predictors of contact tracing app adoption: integrating the UTAUT, HBM and contextual factors. Technol Soc 2022; 71: 102101. [Google Scholar]
- 48.Mohammed R, Elmajid EA, Amine Het al. et al. Acceptance factors of telemedicine technology during COVID-19 pandemic among health professionals: a qualitative study. Healthc Technol Lett 2023; 10: 23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adenuga KI, Iahad NA, Miskon S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int J Med Inf 2017; 104: 84–96. [DOI] [PubMed] [Google Scholar]
- 50.Shiferaw KB, Mengiste SA, Gullslett MK, et al. Healthcare providers’ acceptance of telemedicine and preference of modalities during COVID-19 pandemics in a low resource setting: an extended UTAUT model. PLoS ONE 2021; 16: e0250220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Al-Khalifa KS, AlSheikh R. Teledentistry awareness among dental professionals in Saudi Arabia. PLoS ONE 2020; 15: e0240825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Al-Shaya M, Farsi D, Farsi Net al. et al. Perception, awareness, and knowledge of dental professionals about teledentistry in Saudi Arabia – a literature review. Biosci Biotechnol Res Commun 2021; 14: 1393–1397. [Google Scholar]
- 53.Eccles MP, Hrisos S, Francis J, et al. Do self- reported intentions predict clinician’s behaviour: a systematic review. Implement Sci 2006; 1: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zahed K, Fields S, Sasangohar F. Investigating the efficacy of behavioural models to predict use of health technology: a scoping review. Proc Human Factors Ergonom Soc Ann Meeting 2022; 66: 2172–2176. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241253739 for Predicting the employment of teledentistry in clinical practice by the Saudi dental community using a theoretical model by Angel M Joseph, Rasha A Alsalman, Wjoud A Almasoud, Reem Almutairi, Rawan B Alammari, Yahya AM Deeban, Mohammed Z Mustafa and Amar A Thakare in DIGITAL HEALTH
Supplemental material, sj-docx-2-dhj-10.1177_20552076241253739 for Predicting the employment of teledentistry in clinical practice by the Saudi dental community using a theoretical model by Angel M Joseph, Rasha A Alsalman, Wjoud A Almasoud, Reem Almutairi, Rawan B Alammari, Yahya AM Deeban, Mohammed Z Mustafa and Amar A Thakare in DIGITAL HEALTH