Abstract
Through cognate interaction between antigen-specific B-cell and CD4+ αβ T cells, the CD4+ αβ T cells secrete cytokines that initiate immunoglobulin (Ig) class switching from IgM to IgG. In this study, we show that formalin-inactivated influenza PR8 virus induces virus-specific IgM and IgG responses in the absence of CD4+ T cells and that all four subclasses of IgG are produced. The immunized CD4-deficient mice were also found to be completely protected against lethal infection with live, pathogenic influenza virus. The ability of CD4+ T-cell-deficient mice to generate these IgG responses was not found to be impaired when these mice were depleted of CD8+ T cells with an anti-CD8 monoclonal antibody. In contrast, αβ T-cell-deficient mice (TCRβ−/−) were not found to produce significant amounts of IgG upon immunization with formalin-inactivated PR8 virus. These results suggest that CD4− CD8− double-negative αβ T cells are playing a role in regulating Ig class switching in the absence of CD4+ T cells.
T-cell-independent (TI) antigens are antigens that stimulate antibody responses in the absence of major histocompatibility (MHC) class II-restricted T-cell help. TI antigens fall into two major categories, TI type 1 (TI-1) and TI type 2 (TI-2). TI-1 antigens are characterized by being mitogenic and inducing polyclonal B-cell proliferation. TI-2 antigens, which are represented by polysaccharides, have the properties of high molecular weight, repeating antigenic epitopes, and inability to stimulate MHC class II-dependent T-cell help (21–23). TI antigens induce only immunoglobulin M (IgM) responses. In contrast, protein antigens are thought to induce only T-cell-dependent antibody responses, which include both IgM and IgG responses (21, 22).
CD4+ T helper cells are believed to be essential for induction of a high-affinity antibody response and for efficient isotype switching from IgM to IgG production (25, 26). Through cognate interaction between antigen-specific B cells and CD4+ αβ T cells, the CD4+ αβ T cells secrete cytokines that initiate the Ig class switching process from IgM to IgG (9, 26, 32). These T-cell-dependent antibody responses are accompanied by the formation of germinal centers of B cells in the lymphoid organs such as the spleen and lymph nodes (14, 16). Recent studies have shown that Ig class switching can also be induced in T-cell-deficient mice when infected with live viruses (17, 33, 34). When αβ T-cell-deficient mice (T-cell receptor β chain knockout [TCRβ−/−] or T-cell receptor α chain knockout [TCRα−/−]) were infected with live polyomavirus, a protective virus-specific IgG response was reported in the absence of helper T cells. However, polyomavirus-like particles and soluble capsid antigens (VP1) were reported not to induce detectable IgG responses. In studies with vesicular stomatitis virus (VSV), TCRα−/− mice were found to produce neutralizing IgG antibodies when infected with live VSV or with a recombinant vaccinia virus expressing the VSV glycoprotein (17). These results suggest that there may be alternative mechanisms for antibody class switching and induction of IgG responses.
Formalin inactivation of VSV was reported to have no effect on the early IgM response after immunization, but class switching from IgM to IgG was significantly reduced in BALB/c mice (1, 2, 11). Low doses (2 × 104 PFU) of inactivated VSV did not induce any measurable neutralizing IgG responses, while high IgG titers were produced after immunization with the same dose of live virus. A higher dose (2 × 106 PFU and 1 × 108 PFU) of inactivated VSV induced almost normal levels of neutralizing IgG titers. However, when nude mice or mice depleted of CD4+ T cells with an anti-CD4 monoclonal antibody (MAb) were immunized with inactivated virus, no detectable virus-specific IgG was produced (2). It was therefore concluded that CD4+ T cells are required for the generation of class switching from IgM to IgG when inactivated virus vaccines are used.
In this study, we have investigated whether formalin-inactivated influenza A/PR8 virus can induce Ig class switching and generate virus-specific IgG responses in the absence of CD4+ T cells.
MATERIALS AND METHODS
Animals.
C57BL/6J mice, C57BL/6-Cd4tm1Mak mice, which had a targeted disruption in their CD4 gene and therefore lacked functional CD4+ T cells (28); C57BL/6J-Tcratm1Mom mice, which had a targeted disruption in their TCRα gene and lacked functional αβ T cells (19); and C57BL/6J-Tcrbtm1Mom mice, which had a targeted disruption in their TCRβ gene and also lacked functional αβ T cells (19) were obtained from the Jackson Laboratory (Bar Harbor, Maine). Some of the mice were bred in the Department of Animal Resources at Emory University from purchased breeding pairs. Two age groups of mice were used in this study; one age group was 16 to 24 weeks old, and the other age group was 6 weeks old.
Virus, immunization, and sampling.
Influenza virus strain A/PR/8/34 was grown in the allantoic cavity of embryonated hen's eggs (9 to 11 days old) and purified from allantoic fluid by sucrose gradient centrifugation at 100,000 × g. For inactivation, purified virus was mixed with formalin at a final concentration of 1:4,000 (vol/vol), incubated at 37°C for 72 h, and then dialyzed against phosphate-buffered saline (PBS) with three changes. The virus stock was stored in aliquots at −80°C before use. Inactivation of the virus was confirmed by both plaque assay on confluent monolayer MDCK cells and inoculation of the virus into 9- to 11-day-old embryonated hen's eggs. For immunization, mice were immunized with 10 μg of virus protein intramuscularly (i.m.) or intraperitoneally (i.p.) per 100 μl of PBS at day 0 and day 15. Blood samples were collected 15 days after priming and 10 days after boosting. Anesthetized mice were bled from retroorbital veins to obtain blood samples. Samples were centrifuged at 14,000 rpm, and sera were stored at −20°C.
In vitro virus neutralization assay.
A standard plaque reduction assay was performed to determine the PR8 virus-specific neutralizing titer of the sera as previously described (31). From 80 to 120 PFU of influenza A/PR8 virus was mixed with serum at 50-, 200-, 1,000-, and 5,000-fold dilutions and incubated at room temperature for 1 h. Aliquots of 200 μl were added to confluent MDCK cell monolayers in six-well plates and incubated at 37°C for 1 h, and the plates were shaken gently every 15 min. After washing, 1.95% white agar in 1× Dulbecco's modified Eagle's medium containing 1 μg of trypsin was overlaid on the wells. After incubation at 37°C for 4 days, plates were stained with neutral red. The numbers of plaques in each well were counted. The neutralizing antibody titer was expressed as the highest dilution of serum that was found to reduce the number of plaques by at least 50%.
Antibody responses.
Influenza virus-specific antibodies were measured by enzyme-linked immunosorbent assay (ELISA) as previously described (27). Briefly, the assays were performed in 96-well plates (Dynatech, Alexandria, Va.) coated with purified PR8 virus at a concentration of 2 μg/ml in borate-buffered saline buffer. Dilutions of serum were incubated overnight on coated and blocked ELISA plates, and the plates were then incubated with horseradish peroxidase-labeled goat anti-mouse IgG (Southern Biotechnology Associates, Birmingham, Ala.). After washing with PBS plus 0.05% Tween 20, the substrate ABTS (2,2′-azino-bis-[3-ethylbenzthiazoline sulfonic acid]; Sigma, St. Louis, Mo.) in phosphate citrate buffer (3 mg/10 ml) (pH 4.2) containing 0.03% H2O2 was added. After 30 min of incubation, the color was measured with an ELISA reader at 405 nm. Each sample was measured in duplicate. For determination of the relative levels of PR8-specific IgG subtype responses, a quantitative assay was performed. Standard curves were obtained by adding purified mouse IgG1, IgG2a, IgG2b, and IgG3 to plates captured with a precoated goat anti-mouse Ig antibody, and colors were developed with ABTS substrate and horseradish peroxidase-conjugated goat antibodies against each IgG subtype. Concentrations of IgG1, IgG2a, IgG2b, and IgG3 were determined by comparing the reading for the experimental samples with the standard curves.
In vivo CD8+ T-cell depletion.
CD8+ T cells were depleted in vivo by i.p. injection of purified rat anti-mouse IgG CD8 MAb (clone 2.43) (40). Antibodies were purified with a HiTrap protein G column (Pharmacia Biotech) from the supernatant of hybridoma 2.43 cultures. A total of 100 μg of antibody was injected i.p. in mice at days −3, −2, −1, and +1 of immunization, and the injections were repeated every 5 days thereafter. The effectiveness of depletion was confirmed by fluorescence-activated cell sorting (FACS) (anti-mouse IgG CD8 MAb clone 53-6.7; Becton Dickinson Co., Mountain View, Calif.) analysis of staining of peripheral blood leukocytes from killed mice, and these samples were found to be 98 to 99% free of CD8+ T cells.
Flow cytometry analysis.
Single-cell suspension from spleens of mice were made, and 106 cells were stained with anti-TCRβ, anti-CD8, and anti-CD4 MAbs (H57-FITC, 53-6.7-PerCP, and GK1.5-PE, respectively) (PharMingen, Beckton-Dickinson) for 30 min at 4°C in 100 μl of FACS buffer (PBS containing 0.3% bovine serum albumin and 0.1% sodium azide). Cells were washed with FACS buffer and fixed with 2% paraformaldehyde and then analyzed for single-, double-, and three-color flow cytometry analysis on a FACScan (Becton-Dickinson). From 10,000 to 20,000 events were counted for each sample. Forward and side-scattered characteristics were used to distinguish the lymphocyte population. CELLQuest software (Becton Dickinson) was used for the analysis.
Challenge studies.
For procedures requiring a lethal challenge of influenza virus, a mouse-adapted antigenically identical strain of A/PR/8/34 (provided by Jiri Mestecky, University of Alabama, Birmingham) was used for intranasal inoculation. Virus (10 times the 50% lethal dose [10 × LD50, 500 PFU]) was administered by instillation into the nostrils of anesthetized mice in a volume of 50 μl. The LD50 in CD4+ T-cell-deficient mice was comparable to the LD50 in normal C57BL/6 mice. Mice were observed daily for 16 days, and all deaths were recorded.
RESULTS
Inactivated PR/8/34 influenza virus induces CD4+ T-cell-independent IgG responses.
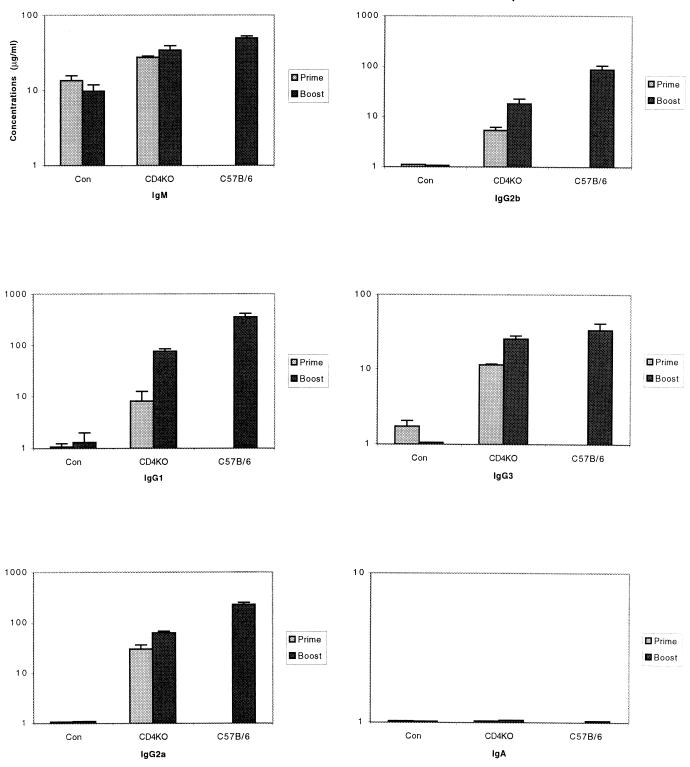
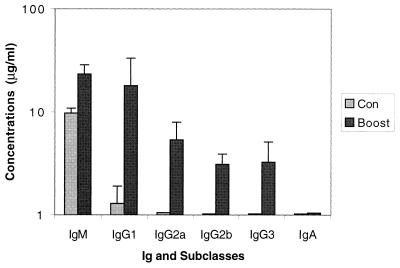
To investigate the potential of inactivated PR8 virus to induce IgG responses in the absence of CD4+ T cells, the magnitude of virus-specific IgG responses to i.m. immunization with inactivated PR8 virus in normal C57BL/6 mice and CD4+ T-cell-deficient mice in a C57BL/6 background were evaluated by measuring PR8-specific IgG concentrations by ELISA. Mice from 16 to 24 weeks old were used in this experiment. Formalin-inactivated influenza PR8 virus was found to induce virus-specific IgM and IgG antibodies in normal C57BL/6 mice. Analysis of the isotype distribution of the virus-specific IgG indicated that all four IgG subclasses were induced by the inactivated virus, with IgG1 and IgG2a being predominant (Fig. 1). In the CD4+ T-cell-deficient mice, an IgM response was induced in the absence of functional T helper cells. Furthermore, we also detected the presence of virus-specific IgG in the CD4+ T-cell-deficient mice, indicating that CD4+ T-cell-independent antibody class switching from IgM to IgG took place after the immunization. All four IgG subclasses were induced, with IgG1 and IgG2a being the predominant virus-specific subclasses. The magnitude of the responses was on the average about fivefold lower than that observed in the normal C57B/6 mice. Interestingly, IgA responses were not detected after immunization in either CD4+ T-cell knockout mice or normal C57B/6 mice, indicating the lack of class switching to IgA after i.m. immunization with inactivated PR8 virus. These data suggest that IgG but not IgA responses can be induced by inactivated virus independent of CD4+ T helper cells.
FIG. 1.
Magnitude and isotype profiles of serum antibody responses to i.m. immunization with inactivated PR8 virus in CD4+ T-cell-deficient and immunocompetent mice. CD4+ T-cell-deficient mice or C57BL/6 mice (16 weeks old) were immunized i.m. with 10 μg of inactivated PR8 virus per mouse. The mice were boosted with the same dose after 15 days. Con, unimmunized CD4+ T-cell-deficient mice (n = 5). CD4KO, CD4+ T-cell-deficient mice received inactivated PR8 virus (n = 5). C57B/6: C57BL/6 immunocompetent mice received inactivated PR8 virus (n = 5). Prime, samples were measured 15 days after first immunization. Boost, samples were measured 10 days after boost. Serum samples were assayed in 1:400 and 1:1,600 dilutions. Error bars in this and subsequent figures represent standard error.
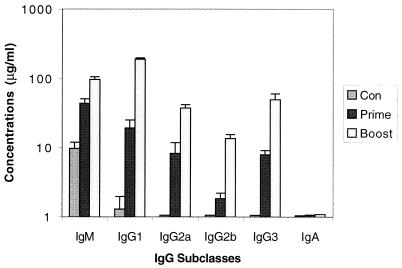
To examine whether or not the CD4+ T-cell-independent IgG responses in these experiments are specific to the i.m. route, we immunized CD4+ T-cell knockout C57BL/6 mice i.p. with formalin-inactivated PR8 virus. Analysis of the serum antibody levels indicated that both IgM and IgG were also induced by this route of immunization. All four subclasses of antibodies were detected, with IgG1 being the dominant response. The magnitude of these antibody responses was similar to those observed after i.m. immunization (Fig. 2). These data suggest that the CD4+ T-cell-independent Ig class switching elicited by inactivated virus can be induced by multiple routes and is not specific to the i.m. route.
FIG. 2.
Antibody responses and isotype distribution of virus-specific IgG in mice immunized intraperitoneally. CD4+ T-cell-deficient mice (n = 5) were immunized i.p. with formalin-inactivated PR8 virus (10 μg/mouse) on day 0 and boosted on day 15. Serum samples were collected 15 days after priming and 10 days after boosting. Con, control, unimmunized CD4+ T-cell-deficient mice. Prime, after first immunization. Boost, after boost.
CD8+ T cells are not required for induction of CD4+ T-cell-independent IgG responses.
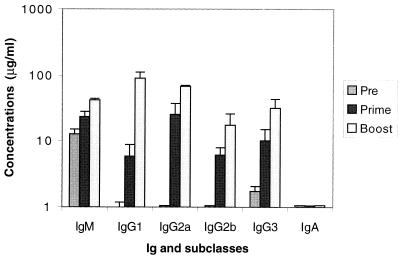
It is generally believed that Ig isotype switching requires the interaction between B cells and CD4+ T cells, the latter secreting cytokines that regulate isotype switching. Recent studies have shown that CD8+ T cells may also produce cytokines, and like CD4+ T cells, they can be divided into two subsets, Tc1 and Tc2 (4, 10, 24, 29, 30). Other studies suggested that CD8+ T cells may help B cells by the cytokines they produce (5, 8). To investigate whether CD8+ T cells play a role in the induction of IgG responses in CD4+ T-cell-deficient C57BL/6 mice, we depleted the CD8+ T cells in these mice by injection of 2.43 antibody. CD8+ T cells were found to be depleted by approximately 99% in peripheral blood when analyzed by FACS. When CD4+ T-cell-deficient mice were immunized i.m. with inactivated PR8 virus, depletion of CD8+ T cells did not abrogate the observed IgG responses (Fig. 3). The magnitude and subclass profile of the IgG responses were found to be similar to those observed in the CD4+ T-cell knockout mice without CD8+ T-cell depletion. These results provide evidence that CD8+ T cells are not required for the inactivated virus-induced CD4+ T-cell-independent IgG responses.
FIG. 3.
Antibody responses and IgG isotype profile in CD8-depleted CD4+ T-cell-deficient C57BL/6 mice after immunization with inactivated PR8 virus. CD4+ T-cell-deficient mice (n = 5) were depleted of CD8 T cells by i.p. injection of MAb. 2.43. These mice were then i.m. immunized with formalin-inactivated PR8 virus (10 μg/mouse) at day 0 and boosted at day 15 with the same dose. Pre, serum samples before immunization. Prime, serum samples taken at day 15 after first immunization. Boost, serum samples taken at day 10 after boost.
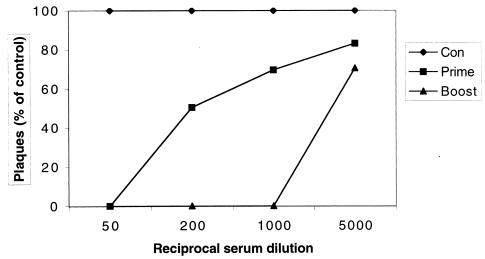
Immunization with inactivated PR8 virus in CD4+ T-cell-deficient mice induces neutralizing activity.
To explore whether immunization with formalin-inactivated PR8 virus in CD4+ T-cell-deficient mice induces virus-neutralizing activity in vitro, approximately 100 PFU of PR8 virus were incubated with serum at different dilutions, and a standard plaque reduction assay was performed on MDCK cells. The neutralizing titer of the sera from the CD4+ T-cell-deficient mice after the initial immunization was 1:200, and the titer was higher than 1:1,000 after boosting (Fig. 4). This result shows that the immune responses induced in the absence of CD4+ T cells have virus-neutralizing activity in vitro.
FIG. 4.
Serum virus-neutralizing antibody titers in CD4+ T-cell-deficient C57BL/6 mice i.m. immunized with formalin-inactivated PR8 virus. CD4+ T-cell-deficient mice were immunized i.m. with formalin-inactivated PR8 virus (10 μg/mouse) at day 0 and boosted at day 15 with the same dose. Different dilutions of serum samples from immunized mice were mixed with approximately 100 PFU of PR8 virus and incubated for 1 h at room temperature. The mixtures were then used to infect a monolayer of MDCK cells, and a standard plaque reduction assay was performed. The neutralizing-antibody titer of the serum is considered the highest dilution that was found to reduce the number of plaques by 50% or more. ⧫, control, serum from unimmunized CD4+ T-cell-deficient mice; ■, serum from CD4+ T-cell-deficient C57BL/6 mice 15 days after priming; ▴, serum from CD4+ T-cell-deficient C57BL/6 mice 10 days after boosting.
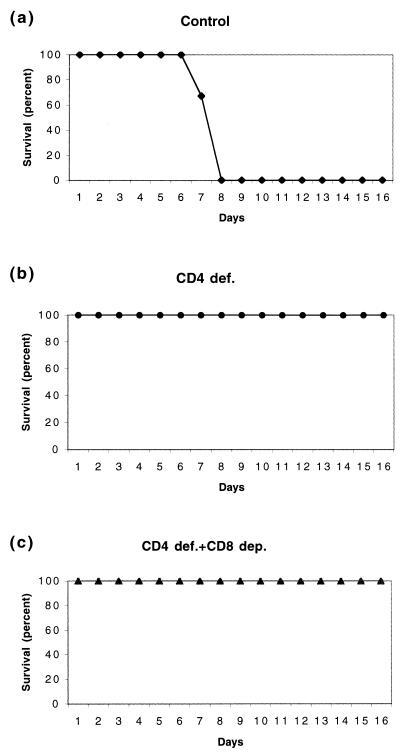
CD4+ T-cell-deficient mice are protected from lethal challenge with live virus after immunization with inactivated virus.
To investigate whether the observed immune responses can protect against lethal challenge, the immunized CD4+ T-cell-deficient mice were challenged with 10× the LD50 intranasally under anesthesia. One hundred percent of CD4+ T-cell-deficient mice immunized with inactivated PR8 virus were found to be protected from lethal infection. In addition, all the CD8+ T-cell-depleted mice were also protected. In contrast, unimmunized CD4+ T-cell knockout mice all died on days 6 to 8 after the challenge (Fig. 5). This result indicates that inactivated virus could induce fully protective immune responses without the participation of CD4+ T helper cells.
FIG. 5.
Protection of immunized CD4+ T-cell-deficient mice against lethal PR8 virus challenge. CD4+ T-cell-deficient C57BL/6 mice i.m. immunized with inactivated PR8 virus were challenged intranasally with 10 times the LD50 of live PR8 virus under anesthesia 4 weeks after boost. (a) Control, unimmunized CD4+ T-cell-deficient C57BL/6 mice. (b) CD4+ T-cell-deficient C57BL/6 mice immunized with inactivated PR8 virus. (c) CD8 T-cell-depleted CD4+ T-cell-deficient C57BL/6 mice immunized with inactivated PR8 virus.
TCRαβ+ T-cell-deficient mice are unable to produce IgG responses after immunization with inactivated PR8 virus.
To investigate whether mice deficient in total TCRαβ+ T cells were capable of mounting antiviral IgG responses after immunization with inactivated influenza virus, we examined the virus-specific antibody responses of TCRβ−/− mice after immunization with formalin-inactivated PR8 virus. We observed that the TCRβ−/− mice produced IgM responses after immunization with inactivated virus; the levels of IgM observed after priming and boosting were similar. However, the TCRβ−/− mice did not develop significant virus-specific IgG responses after immunization with the inactivated PR8 virus. No IgG1, IgG2a, or IgG2b responses could be detected, and only very low levels of IgG3 were produced (Fig. 6). These results indicate that although CD4+ and CD8+ T cells are not required, a population of αβ+ T cells is indispensable for IgG production after immunization with inactivated PR8 virus.
FIG. 6.
Isotype profile of PR8 virus-specific antibody responses of T-cell-deficient mice. TCRβ−/− mice were i.m. immunized with formalin-inactivated PR8 virus (10 μg/mouse) at day 0 and boosted at day 15. Serum samples were obtained 15 days after priming and 10 days after boosting. Con, control, unimmunized TCRβ−/− mice; PR8, TCRβ−/− mice immunized with formalin-inactivated PR8 virus. Prime and Boost are defined in the legend to Fig. 1.
Magnitude of IgG responses to inactivated PR8 virus is age dependent.
During these experiments, we observed that younger CD4+ T-cell knockout mice produced lower levels of IgG responses than older mice. In this experiment, 6-week-old CD4+ T-cell-deficient C57BL/6 mice were immunized i.m. with formalin-inactivated PR8 virus. A significant amount of IgM and all four subclasses of IgG were produced, but their levels on the average were five- to six-fold lower than those of the 16-week-old mice. IgG1 was predominant among the four subclasses of IgG, similar to the pattern observed in old mice (Fig. 7). These data indicate that younger CD4+ T-cell knockout mice produce lower levels of IgG responses than older mice.
FIG. 7.
Antibody responses and isotype distribution of virus-specific IgG in 6-week-old mice i.m. immunized with inactivated PR8 virus. Six-week-old mice (n = 4) were immunized intramuscularly with formalin-inactivated PR8 virus (10 μg/mouse) on day 0 and boosted on day 15. Serum samples were collected 10 days after boosting. Con, control, unimmunized CD4+ T-cell-deficient mice. Boost, serum samples after boost.
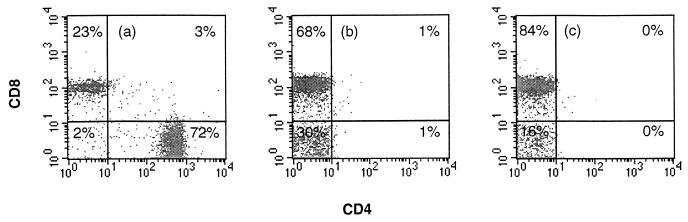
CD4+ T-cell-deficient mice contain higher levels of CD4− CD8− DN T cells in the spleen than normal C57BL/6 mice.
To investigate whether CD4+ T-cell-deficient mice have the same double-negative (DN) T-cell population as normal C57BL/6 mice, we analyzed different T-cell populations in these mice by flow cytometry after staining the T cells with anti-TCRβ, anti-CD8, and anti-CD4 MAbs. In normal 6-month-old C57BL/6 mice, DN T cells account for about 2% of the T-cell population. In contrast, DN T cells were found to constitute about 30% of the total T-cell population in 6-month-old CD4+ T-cell-deficient mice and about 15% in younger (6 week old) CD4+ T-cell-deficient mice (Fig. 8). These results demonstrate that higher levels of DN T cells are produced in CD4+ T-cell-deficient mice than in normal mice.
FIG. 8.
Flow cytometry analysis of αβ T cells in CD4+ T-cell-deficient mice. Spleen cells from C57BL/6 mice or CD4+ T-cell-deficient mice were stained with anti-TCRβ, anti-CD8, and anti-CD4 MAbs (H57-FITC, 53-6.7-PerCP, and GK1.5-PE, respectively, from PharMingen and Beckton-Dickinson). Plots show TCRβ-gated cells. Samples were from (a) a 16-week-old C57BL/6 mouse, (b) a 6-month-old CD4+ T-cell-deficient mouse, and (c) a 6-week-old CD4+ T-cell-deficient mouse.
DISCUSSION
We show in this study that formalin-inactivated influenza PR8 virus induces IgM and IgG responses in the absence of CD4+ T cells. All four subclasses of IgG were produced, with IgG1 and IgG2a being predominant. The sera from the immunized mice were also found to have neutralizing activity against influenza virus in vitro. The immunized CD4+ T-cell-deficient mice were also shown to be protected from intranasal challenge with lethal doses of live PR8 virus. To our knowledge, this is the first report that an inactivated virus can induce B-cell differentiation and isotype switching from IgM to IgG that is completely independent of CD4+ T helper cells.
The ability of CD4+ T-cell-deficient mice to generate IgG responses after immunization with inactivated PR8 virus was also not found to be impaired when these mice were depleted of CD8+ T cells with an anti-CD8 MAb. In contrast, αβ+ T-cell-deficient mice (TCRα−/− and TCRβ−/−) were not observed to produce significant amounts of IgG upon immunization with formalin-inactivated PR8 virus. These results suggested that CD4− CD8− DN T cells are playing a role in regulating Ig class switching in the absence of CD4+ T cells. To our knowledge, this is also the first evidence that CD4− CD8− DN αβ T cells play a role in Ig class switching and generation of IgG antibody in the immune response against viral pathogens.
The magnitude of virus-specific IgM responses in αβ+ T-cell-deficient mice is comparable to that in CD4+ T-cell-deficient mice after immunization with inactivated PR8 virus. However, CD4+ T-cell-deficient mice were protected from the lethal dose challenge with live PR8 virus, but αβ+ T-cell-deficient mice were not protected (data not shown). These observations suggest that the protective effect is mainly a result of IgG responses and not IgM responses.
The presence of CD4− CD8− DN T helper cells in the CD4+ T-cell-deficient mice is consistent with recent results from CD4+-deficient mice infected with Leishmania major (6, 15). T-cell-deficient nude mice and severe combined immunodeficient (SCID) mice cannot control L. major infection and the fatal dissemination of the parasite (12, 18). In contrast, CD4−/− mice were reported to be resistant to the infection, and resolution of the infection occurs within 6 weeks. The DN TCRαβ+ T cells purified from infected CD4−/− mice were found to have gamma interferon (IFN-γ) transcripts comparable in amount to that in the CD4+ population purified from infected CD4+/− animals (26). The IFN-γ production was also found to be comparable in these purified populations. MAb to IFN-γ abrogated the ability of CD4−/− mice to recover from L. major infection. Although CD4− CD8− DN αβ T cells are present in normal C57BL/6 mice, they account for only 2% of the T cells in the spleen. It is unlikely that this population plays a major role in Ig class switching in the presence of CD4+ T cells. In contrast, we observed that DN T cells constitute of almost 30% of the T-cell population in 6-month-old CD4+ T-cell-deficient mice. We suggest that these DN T cells may compensate for the functions of the CD4+ T cells which are absent in those mice. The quantitative difference in DN T cell levels between older and younger mice may reflect the different amounts of antibodies produced in these CD4+ T-cell-deficient mice.
Formalin-inactivated VSV was not observed to induce Ig class switching and IgG production in normal mice depleted of CD4+ T cells, which differs from the results obtained with influenza virus in our study. There are several possible explanations for this difference. First, influenza virus may have unique properties as an antigen. Influenza virions bind efficiently to any cell surfaces that contain sialic acid because of the receptor-binding activity of the hemagglutinin glycoprotein (37), and such binding may promote cell-to-cell contacts that could be involved in antibody induction. In contrast to VSV, influenza virions lack sialic acid on their surface (13) and can therefore bind to asialoglycoprotein receptors. There may also be differences between the effects of acute depletion of CD4+ T cells in normal mice versus the development of the immune system in congenital CD4+ T-cell-deficient mice, in which a compensatory mechanism may develop. This is supported by our result that a large number of DN T cells exist in the spleens of the CD4+ T-cell-deficient mice. Other studies with TCR mutant mice also support this hypothesis (20, 36).
The available data suggest that different antigens may use different mechanisms and cells to induce Ig class switching in mice when conventional αβ T cells are absent (7, 17, 33, 38, 39). In the case of VSV, the neutralizing IgG responses were crucially dependent on IFN-γ and were predominantly of the IgG2a subtype. This class-switching effect was reported to be abolished when γδ T cells are absent, indicating that γδ T cells are playing a role in Ig class switching when αβ T cells are absent (17). Studies with a mouse model of human systemic lupus erythematosus had also revealed that γδ T cells can induce Ig class switching (38). This type of B-T interaction sustains the production of germinal centers that are usually the result of αβ T-cell and B-cell collaboration. In contrast, polyomavirus was reported to induce IgG responses in both TCRβ−/− mice and TCRβxδ−/− mice, with similar virus-specific IgG titers, suggesting that TCRγδ+ T cells do not seem to play a role in helping the Ig class-switching process for this virus antigen (33–35).
Our results indicate that the CD4− CD8− DN T cells will trigger B-cell proliferation, differentiation, and isotype switching from IgM to IgG even in the complete absence of CD4+ T helper cells. These finding may have important practical implications. Usually, live attenuated virus vaccines are not administered to immunocompromised patients because of their potential to cause life-threatening infections. Inactivated virus vaccines would be the choice for use in these situations. In these patients, especially AIDS patients whose CD4 counts are extremely low, the “help” from CD4− CD8− DN T cells may allow the generation of long-lasting protective IgG immune responses against viral pathogens by vaccination with inactivated viral vaccines even with an impaired CD4+ T helper cell function. This notion is supported by the finding that antibodies directed against the gp120 Env protein persisted even at advanced stages of this disease, when the CD4+ T-cell count is very low (3).
REFERENCES
- 1.Bachmann M F, Hengartner H, Zinkernagel R M. T helper cell-independent neutralizing B cell response against vesicular stomatitis virus: role of antigen patterns in B cell induction? Eur J Immunol. 1995;25:3445–3451. doi: 10.1002/eji.1830251236. [DOI] [PubMed] [Google Scholar]
- 2.Bachmann M F, Kundig T M, Kalberer C P, Hengartner H, Zinkernagel R M. Formalin inactivation of vesicular stomatitis virus impairs T-cell- but not T-help-independent B-cell responses. J Virol. 1993;67:3917–3922. doi: 10.1128/jvi.67.7.3917-3922.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binley J M, Klasse P J, Cao Y, Jones I, Markowitz M, Ho D D, Moore J P. Differential regulation of the antibody responses to Gag and Env proteins of human immunodeficiency virus type 1. J Virol. 1997;71:2799–2809. doi: 10.1128/jvi.71.4.2799-2809.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Croft M, Carter L, Swain S L, Dutton R W. Generation of polarized antigen-specific CD8 effector populations: reciprocal action of interleukin (IL)-4 and IL-12 in promoting type 2 versus type 1 cytokine profiles. J Exp Med. 1994;180:1715–1728. doi: 10.1084/jem.180.5.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cronin D C, 2nd, Stack R, Fitch F W. IL-4-producing CD8+ T cell clones can provide B cell help. J Immunol. 1995;154:3118–3127. [PubMed] [Google Scholar]
- 6.Davis C B, Killeen N, Crooks M E, Raulet D, Littman D R. Evidence for a stochastic mechanism in the differentiation of mature subsets of T lymphocytes. Cell. 1993;73:237–247. doi: 10.1016/0092-8674(93)90226-g. [DOI] [PubMed] [Google Scholar]
- 7.Dianda L, Gulbranson-Judge A, Pao W, Hayday A C, MacLennan I C, Owen M J. Germinal center formation in mice lacking alpha beta T cells. Eur J Immunol. 1996;26:1603–1607. doi: 10.1002/eji.1830260729. [DOI] [PubMed] [Google Scholar]
- 8.Erard F, Wild M T, Garcia-Sanz J A, Le Gros G. Switch of CD8 T cells to noncytolytic CD8-CD4- cells that make TH2 cytokines and help B cells. Science. 1993;260:1802–1805. doi: 10.1126/science.8511588. [DOI] [PubMed] [Google Scholar]
- 9.Finkelman F D, Holmes J, Katona I M, Urban J F, Jr, Beckmann M P, Park L S, Schooley K A, Coffman R L, Mosmann T R, Paul W E. Lymphokine control of in vivo immunoglobulin isotype selection. Annu Rev Immunol. 1990;8:303–333. doi: 10.1146/annurev.iy.08.040190.001511. [DOI] [PubMed] [Google Scholar]
- 10.Fong T A, Mosmann T R. Alloreactive murine CD8+ T cell clones secrete the Th1 pattern of cytokines. J Immunol. 1990;144:1744–1752. [PubMed] [Google Scholar]
- 11.Freer G, Burkhart C, Ciernik I, Bachmann M F, Hengartner H, Zinkernagel R M. Vesicular stomatitis virus Indiana glycoprotein as a T-cell-dependent and -independent antigen. J Virol. 1994;68:3650–3655. doi: 10.1128/jvi.68.6.3650-3655.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holaday B J, Sadick M D, Wang Z E, Reiner S L, Heinzel F P, Parslow T G, Locksley R M. Reconstitution of Leishmania immunity in severe combined immunodeficient mice using Th1- and Th2-like cell lines. J Immunol. 1991;147:1653–1658. [PubMed] [Google Scholar]
- 13.Klenk H D, Keil W, Niemann H, Geyer R, Schwarz R T. The characterization of influenza A viruses by carbohydrate analysis. Curr Top Microbiol Immunol. 1983;104:247–257. doi: 10.1007/978-3-642-68949-9_15. [DOI] [PubMed] [Google Scholar]
- 14.Liu Y J, Johnson G D, Gordon J, MacLennan I C. Germinal centres in T-cell-dependent antibody responses. Immunol Today. 1992;13:17–21. doi: 10.1016/0167-5699(92)90199-H. [DOI] [PubMed] [Google Scholar]
- 15.Locksley R M, Reiner S L, Hatam F, Littman D R, Killeen N. Helper T cells without CD4: control of leishmaniasis in CD4-deficient mice. Science. 1993;261:1448–1451. doi: 10.1126/science.8367726. [DOI] [PubMed] [Google Scholar]
- 16.MacLennan I C. Germinal centers. Annu Rev Immunol. 1994;12:117–139. doi: 10.1146/annurev.iy.12.040194.001001. [DOI] [PubMed] [Google Scholar]
- 17.Maloy K J, Odermatt B, Hengartner H, Zinkernagel R M. Interferon gamma-producing gammadelta T cell-dependent antibody isotype switching in the absence of germinal center formation during virus infection. Proc Natl Acad Sci USA. 1998;95:1160–1165. doi: 10.1073/pnas.95.3.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell G F. Murine cutaneous leishmaniasis: resistance in reconstituted nude mice and several F1 hybrids infected with Leishmania tropica major. J Immunogenet. 1983;10:395–412. doi: 10.1111/j.1744-313x.1983.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 19.Mombaerts P, Clarke A R, Rudnicki M A, Iacomini J, Itohara S, Lafaille J J, Wang L, Ichikawa Y, Jaenisch R, Hooper M L, et al. Mutations in T-cell antigen receptor genes alpha and beta block thymocyte development at different stages. Nature. 1992;360:225–231. doi: 10.1038/360225a0. . (Erratum, 360:491.) [DOI] [PubMed] [Google Scholar]
- 20.Mombaerts P, Mizoguchi E, Ljunggren H G, Iacomini J, Ishikawa H, Wang L, Grusby M J, Glimcher L H, Winn H J, Bhan A K, et al. Peripheral lymphoid development and function in TCR mutant mice. Int Immunol. 1994;6:1061–1070. doi: 10.1093/intimm/6.7.1061. [DOI] [PubMed] [Google Scholar]
- 21.Mond J J, Lees A, Snapper C M. T cell-independent antigens type 2. Annu Rev Immunol. 1995;13:655–692. doi: 10.1146/annurev.iy.13.040195.003255. [DOI] [PubMed] [Google Scholar]
- 22.Mond J J, Vos Q, Lees A, Snapper C M. T cell independent antigens. Curr Opin Immunol. 1995;7:349–354. doi: 10.1016/0952-7915(95)80109-x. [DOI] [PubMed] [Google Scholar]
- 23.Mosier D E, Mond J J, Goldings E A. The ontogeny of thymic independent antibody responses in vitro in normal mice and mice with an X-linked B cell defect. J Immunol. 1977;119:1874–1878. [PubMed] [Google Scholar]
- 24.Mosmann T R, Li L, Sad S. Functions of CD8 T-cell subsets secreting different cytokine patterns. Semin Immunol. 1997;9:87–92. doi: 10.1006/smim.1997.0065. [DOI] [PubMed] [Google Scholar]
- 25.Oxenius A, Zinkernagel R M, Hengartner H. CD4+ T-cell induction and effector functions: a comparison of immunity against soluble antigens and viral infections. Adv Immunol. 1998;70:313–367. doi: 10.1016/s0065-2776(08)60390-9. [DOI] [PubMed] [Google Scholar]
- 26.Parker D C. T cell-dependent B cell activation. Annu Rev Immunol. 1993;11:331–360. doi: 10.1146/annurev.iy.11.040193.001555. [DOI] [PubMed] [Google Scholar]
- 27.Pertmer T M, Roberts T R, Haynes J R. Influenza virus nucleoprotein-specific immunoglobulin G subclass and cytokine responses elicited by DNA vaccination are dependent on the route of vector DNA delivery. J Virol. 1996;70:6119–6125. doi: 10.1128/jvi.70.9.6119-6125.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rahemtulla A, Fung-Leung W P, Schilham M W, Kundig T M, Sambhara S R, Narendran A, Arabian A, Wakeham A, Paige C J, Zinkernagel R M, et al. Normal development and function of CD8+ cells but markedly decreased helper cell activity in mice lacking CD4. Nature. 1991;353:180–184. doi: 10.1038/353180a0. [DOI] [PubMed] [Google Scholar]
- 29.Sad S, Marcotte R, Mosmann T R. Cytokine-induced differentiation of precursor mouse CD8+ T cells into cytotoxic CD8+ T cells secreting Th1 or Th2 cytokines. Immunity. 1995;2:271–279. doi: 10.1016/1074-7613(95)90051-9. [DOI] [PubMed] [Google Scholar]
- 30.Salgame P, Abrams J S, Clayberger C, Goldstein H, Convit J, Modlin R L, Bloom B R. Differing lymphokine profiles of functional subsets of human CD4 and CD8 T cell clones. Science. 1991;254:279–282. doi: 10.1126/science.254.5029.279. [DOI] [PubMed] [Google Scholar]
- 31.Sha Z, Vincent M J, Compans R W. Enhancement of mucosal immune responses to the influenza virus HA protein by alternative approaches to DNA immunization. Immunobiology. 1999;200:21–30. doi: 10.1016/S0171-2985(99)80030-8. [DOI] [PubMed] [Google Scholar]
- 32.Snapper C M, Mond J J. Towards a comprehensive view of immunoglobulin class switching. Immunol Today. 1993;14:15–17. doi: 10.1016/0167-5699(93)90318-F. [DOI] [PubMed] [Google Scholar]
- 33.Szomolanyi-Tsuda E, Le Q P, Garcea R L, Welsh R M. T-cell-independent immunoglobulin G responses in vivo are elicited by live-virus infection but not by immunization with viral proteins or virus-like particles. J Virol. 1998;72:6665–6670. doi: 10.1128/jvi.72.8.6665-6670.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Szomolanyi-Tsuda E, Welsh R M. T cell-independent antibody-mediated clearance of polyoma virus in T cell-deficient mice. J Exp Med. 1996;183:403–411. doi: 10.1084/jem.183.2.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Szomolanyi-Tsuda E, Welsh R M. T-cell-independent antiviral antibody responses. Curr Opin Immunol. 1998;10:431–435. doi: 10.1016/s0952-7915(98)80117-9. [DOI] [PubMed] [Google Scholar]
- 36.Viney J L, Dianda L, Roberts S J, Wen L, Mallick C A, Hayday A C, Owen M J. Lymphocyte proliferation in mice congenitally deficient in T-cell receptor alpha beta + cells. Proc Natl Acad Sci USA. 1994;91:11948–11952. doi: 10.1073/pnas.91.25.11948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weis W, Brown J H, Cusack S, Paulson J C, Skehel J J, Wiley D C. Structure of the influenza virus haemagglutinin complexed with its receptor, sialic acid. Nature. 1988;333:426–431. doi: 10.1038/333426a0. [DOI] [PubMed] [Google Scholar]
- 38.Wen L, Pao W, Wong F S, Peng Q, Craft J, Zheng B, Kelsoe G, Dianda L, Owen M J, Hayday A C. Germinal center formation, immunoglobulin class switching, and autoantibody production driven by “non alpha/beta” T cells. J Exp Med. 1996;183:2271–2282. doi: 10.1084/jem.183.5.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wen L, Roberts S J, Viney J L, Wong F S, Mallick C, Findly R C, Peng Q, Craft J E, Owen M J, Hayday A C. Immunoglobulin synthesis and generalized autoimmunity in mice congenitally deficient in alpha beta(+) T cells. Nature. 1994;369:654–658. doi: 10.1038/369654a0. [DOI] [PubMed] [Google Scholar]
- 40.Wilde D B, Marrack P, Kappler J, Dialynas D P, Fitch F W. Evidence implicating L3T4 in class II MHC antigen reactivity; monoclonal antibody GK1.5 (anti-L3T4a) blocks class II MHC antigen-specific proliferation, release of lymphokines, and binding by cloned murine helper T lymphocyte lines. J Immunol. 1983;131:2178–2183. [PubMed] [Google Scholar]