RFP01: Surgical Complications
1761
RF001: Analysis of factors influencing tether breakage following non fusion anterior scoliosis correction (NFASC) in adolescent idiopathic scoliosis (AIS) - A single center experience
Vigneshwara Badikkilaya 1 , Sharan Achar T 1 , Akshya Raj A 1 , Harith Reddy 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Orthopaedics, Apollo Hospitals Chennai India, Chennai, India
Introduction: NFASC is a fusion less correction technique of AIS which has gained popularity in recent times. Tether breakage is the most common mechanical complication after NFASC surgery. Unlike posterior fusion rod breakage, tether break doesn’t cause significant clinical curve progression or symptoms in majority of cases. But there has been no data on characteristics of tether breakage, its risk factors, loss of correction, criteria of revision. Aim of this study is to identify the risk factors of tether breakage, relationship with Apex/UIV/LIV, formulate a protocol for its management based on review of literature. Material and Methods: 75 patients who underwent NFASC with a mean follow up of 26 ± 12.2 months (12-60 months) were included. Pertinent clinical and radiological data collected regarding skeletal maturity, curve type, cobb angle, surgery details and SRS-22r questionnaire were documented. Patients were divided in two groups according to the presence or absence of a breakage and the outcomes of interest were compared. Results: Lumbar curves (Lenke 5CN) showed higher propensity of tether breakage than thoracic curves (80% vs 20%, p < 0.0001). Risk factors for tether breakage (incidence rate - 6.67%) found to be significant are: pre operative higher curve magnitude (MD, Mean Difference - 10.2, p = 0.04), limited correction with a large residual curve (MD - 14, p < 0.005), post operative increase in BMI (MD- 3.23, p = 0.0005). Most of the cord breakage was documented at 1 year follow (74%), at 1 or 2 levels below the apex of the curve (64%). No relationship with LIV/UIV was noted. Usage of double tether and thicker cord data has to be analysed (< 2 year follow up). 1 case of 3 level breakage with clinical decompensation is planned for revision of tether at a later date. Conclusion: Increase in post operative BMI, high magnitude curve with less correction and large residual curve were the significant risk factors noted. Meticulous tether handling and the care during torquing the top nut- to prevent de-rotation avoids stress raisers in cord during sequential tensioning. Further large volume multi centric studies are required to formulate a protocol regarding management of tether breakage cases.
2034
RF002: How to manage a ureteral injury after anterior lumbar spine interbody fusion surgery
Henri-Arthur Leroy 1, , Pierre De Buck 3 , Gautier Marcq 4,5 , Richard Assaker 1
1 Department of Neurosurgery, CHU Lille, Lille, France
2 Chairman for France, AO Spine, Davos, Switzerland
3 Faculty of Medecine, Lille Catholic Hospitals and Lille Catholic University, Lille, France
4 Department of Urology, CHU Lille, Claude Huriez Hospital, Lille, France
5 Cancer Heterogeneity Plasticity and Resistance to Therapies, CHU Lille, Institut Pasteur de Lille, UMR9020-U1277 - CANTHER - University Lille, CNRS, Inserm, Lille, France
Background: Anterior lumbosacral interbody fusion (ALIF) surgery is a predominant approach used in various indications such as treating discogenic back pain, spondylolisthesis, degenerative lumbar scoliosis, intervertebral foraminal stenosis, or spondylolysis. In comparison with posterior conventional approach, ALIF surgery has several advantages: direct access to the spine without muscle dissection, reduced blood loss, decreased postoperative pain, and improved fusion rates. Rare complications following ALIF surgery need to be reported, therefore the authors present an uncommon case of a ureteral injury diagnosed early after surgery and its management. Management of a urinoma: Herein, we present a case of a 35-year-old man who presented with abnormal abdominal pains 4 days after ALIF surgery. He was diagnosed with a distal left iatrogenic ureteral fistula on a contrast enhanced CT. After the initial endoscopic approach with double J stent and urinary catheter drainage insertion had failed, the injury was finally treated with ureterovesical reimplantation. At the last follow-up, the patient did well without any clinical or biological urinary sequelae after this grade IIIb complication on the Clavien Dindo Scale. Conclusion: Although ureteral lesions during ALIF surgery are extremely uncommon, surgeons must be cautious when dissecting the retroperitoneal area. A methodical identification of the ureter might guarantee the security of each surgery, especially for patients who have undergone previous abdominal interventions. Introduction of the Technical Note: Nowadays, anterior lumbosacral interbody fusion (ALIF) surgery is a predominant approach used in various indications, such as treating discogenic back pain, spondylolisthesis, degenerative lumbar scoliosis, or intervertebral foraminal stenosis. It is particularly popular due to its multiple advantages: direct access to the spine without muscle dissection, reduced blood loss, decreased postoperative pain, and improved fusion rates. However, anterior approaches are associated with surgical complications, such as vascular injuries, retroperitoneal hematoma, or hypogastric plexus lesions. Migliorini et al. reported a case-series of urological complications after anterior approach to the spine. The authors emphasized that, despite their rarity, spine surgeons should be more aware of their occurrence. Such injuries may be diagnosed in a delayed fashion after an anterolateral approach. In this case, the authors report an uncommon presentation of a left ureteral iatrogenic injury diagnosed during the first postoperative week following ALIF surgery.
951
RF003: How does the vertical expandable prosthetic titanium rib interval lengthening affect the clinical outcome in early onset scoliosis patients with a minimum of five years of follow up?
Norman Ramirez Lluch 1 , Alexandra Claudio-Marcano 2 , John Smith 3 , John Emans 4 , Amer Samdani 5 , Mark Erickson 6 , John Flynn 7 , Norberto Torres-Lugo 2 , Gerardo Olivella 2
1 Pediatric Orthopedic Surgery, Mayaguez Medical Center, Mayaguez, Puerto Rico
2 Orthopedic Surgery, University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
3 Orthopedic Surgery, Primary Children’s Medical Center, University of Utah, Utah, Puerto Rico
4 Orthopedic Surgery, Boston Children Hospital, Harvard Medical School, Boston, USA
5 Pediatric Orthopedic Surgery, Shriners Hospitals for Children - Philadelphia, Philadelphia, USA
6 Pediatric Orthopedic Surgery, Spine Center, Children's Hospital Colorado, Colorado, USA
7 Orthopedic Surgery, Children's Hospital of Philadelphia, Philadelphia, USA
Introduction: The Vertical Expandable Prosthetic Titanium Rib (VEPTR) was initially developed to stabilize chest malformations and correct Early Onset Scoliosis (EOS) deformities. This device required adjustment surgery every six months until patients reached sufficient maturity to undergo final fusion or to stop lengthening. However, there are no evidence-based guidelines for optimal VEPTR lengthening intervals. Due to limited information about how lengthening intervals affected VEPTR clinical outcomes and complications, our study aimed to evaluate the clinical outcomes and complications in relation to the lengthening intervals of all patients registered at the Pediatric Spine Study Group (PSSG) that underwent VEPTR treatment with a minimum of five years of follow-up. Method: All patients registered at the PSSG database without a history of prior spinal surgical procedures who underwent traditional VEPTR instrumentation surgery with a minimum of five years of follow-up were reviewed. Sample data were divided into two groups: group one: patients who underwent lengthening procedures in intervals of less than eight months throughout a five-year period; and group two: those who were lengthened in inconsistent intervals during the same time frame. We compared demographic variables, radiographic parameters, pulmonary function tests (PFT), 24-Items Early Onset Scoliosis Questionnaire (EOSQ-24) findings, and complication rates between both groups. Results: A total of 447 patients were included in the study. Group one comprised 158 patients, and Group one comprised 289 patients. Both groups were similar in sex distribution, race, and EOS etiology. No clinical differences were observed between groups regarding preoperative coronal Cobb angle, sagittal Cobb angle, and spine height. No clinical differences were observed regarding preoperative PFTs and EOSQ-24 findings between both groups. Five-year post-index surgery parameters showed no clinical difference in coronal Cobb angle, sagittal Cobb angle, PFTs, and EOSQ-24 findings. However, an increase in postoperative spine height in group two was noted. Furthermore, group one had a markedly increased percentage of postoperative complications (p = 0.034). Conclusions: Lengthening intervals of less than eight months was not associated with improvement in PFT measurements, EOSQ-24 findings, overall spinal height gain, or Cobb angle decrease. Yet, it was found to have a significant increase in postoperative complication rates. Our data supports shows that repetitive lengthening increases the treatment burden and introduces unexpected surgical complications. Furthermore, our findings question the standard practice for rib-based growth instrumentation lengthening every six months as proposed in the past.
2001
RF004: Association of late operative start time with surgical site infection in elective spinal surgery
Jessica Ryvlin 1 , Seung Kim 1 , Isabella Pecorari 1 , Kurt Widmaier 1 , Mousa Hamad 1 , Rose Fluss 1 , Rafael De la Garza Ramos 1 , Saikiran Murthy 1 , Reza Yassari 1 , Yaroslav Gelfand 1
1 Montefiore Medical Center/Albert Einstein College of Medicine, New York, USA
Introduction: Surgical site infection (SSI) following spinal intervention can cause significant morbidity. Several quality improvement measures, including case scheduling, have previously been shown to increase costs and prolong inpatients stays. The objective of this study was to determine if late operative start time impacts 30-day postoperative SSI following spinal surgery. Methods: This was a single institution retrospective study including 559 adult patients who underwent elective spinal surgery between 2021 and 2022. Our primary outcome was SSI diagnosed within 30 days postoperatively. Patients who had a late operative start time, defined as on or after 3:00 PM, were compared to patients who had an early operative start time, defined as before 3:00 PM. Statistical analyses were completed using univariable and multivariable logistic regression. Results: Fifteen percent of patients had a late operative start time and 86% had an early start time. The overall 30-day SII incidence was 4%. In univariable logistic regression, late start time was associated with increased odds of SSI (odds ratio [OR] 3.16; 95% confidence interval [CI] 1.31-7.66; p < 0.011). After controlling for American Society of Anesthesiologists class, diabetes, hypertension, and surgical approach, late start time was associated with increased odds of postoperative SSI (OR 3.39; 95% CI 1.23-9.33; p = 0.018). Conclusion: In this study, start time after 3:00PM was independently associated with 30-day postoperative SSI in adults undergoing elective spinal surgery. While several patient and case-specific factors have been shown to impact SSI, our results suggest that operative scheduling may be equally important in continued efforts to improve patient safety.
1545
RF005: Internal spinal marking for intraoperative localisation: current methods and future directions
Darius Tan 1 , Ameen Farsakh 1 , Fidel Toomey 1 , Frederick Mariajoseph 1 , Jeremy Kam 1 , Tony Goldschlager 1
1 Department of Neurosurgery, Monash Health, Melbourne, Australia
Introduction: Incorrect level spinal surgery is an avoidable complication, with significant ramifications. Several pre-operative spinal marking techniques have been described to aid intraoperative localisation. Material and Methods: A systematic search of Ovid MEDLINE, and EMBASE was performed from inception to July 2022. All publications describing cases of internal spinal marking were included for further analysis. 22 articles describing 503 patients satisfied our eligibility criteria. Results: A number of localisation techniques, including endovascular coiling (n = 16), fiducials (n = 177), dye (n = 109), needle/fixed wire (n = 199), cement (n = 4), and gadolinium tubes (n = 1) were described. The highest rates of technical success were observed with endovascular coiling, fiducials, cement and dye (100%), and complication rates were lowest with endovascular coiling, fiducials and cement (0 %). Conclusion: Overall, internal spinal marking was effective and safe. When considering practicality and efficacy, fiducial marking appears the optimal technique, as it can be performed in the outpatient setting under local anaesthesia. This review demonstrates the need for more targeted investigation into localisation methods in spinal surgery.
Keywords: spine; correct level; preoperative localization; intraoperative localization; marking
Disclaimer: full manuscript previously published in Journal of Clinical Neuroscience 111 (2023), 78-85.
915
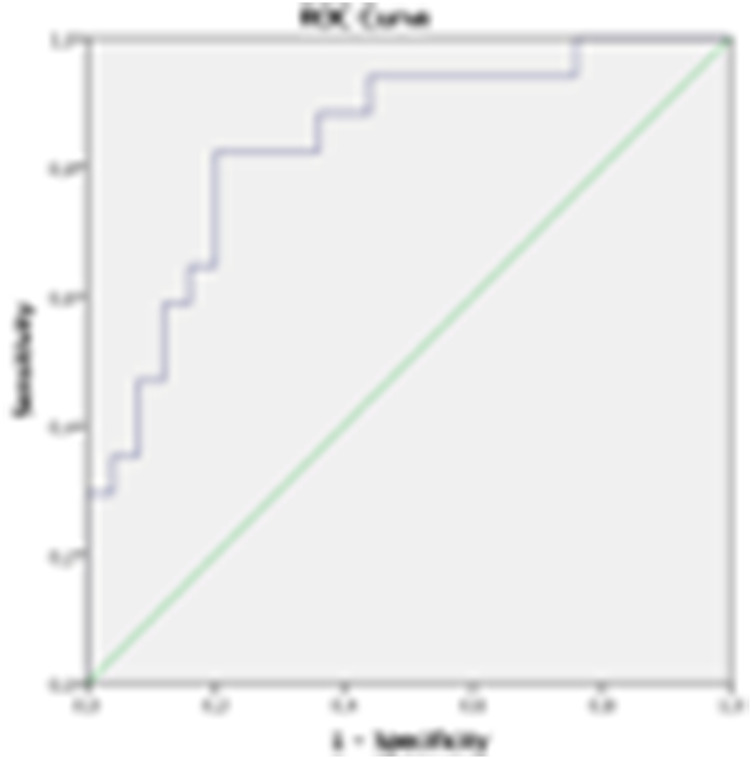
RF006: Predicting postoperative mechanical complications with the ethnicity-adjusted GAP score in degenerative scoliosis: does paraspinal muscle degeneration matter?
Zhen Liu 1 , Peiyu Li 1
1 Department of Spine Surgery, Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing University Medical School, Nanjing, China
Introduction: The global alignment and proportional (GAP) Score was developed to predict mechanical complications (MCs) after adult spinal deformity (ASD) surgery but showed limited sensitivity in the Asian population. Considering variations in sagittal parameters among different ethnic groups, our team developed an ethnicity-adjusted GAP(A-GAP) Score according to spinopelvic parameters of 566 asymptomatic Chinese volunteers. Notably, DS patients with MCs following DS surgery have more severe paraspinal muscle (PSM) degeneration. The uneven degeneration of PSM may largely affect the accuracy of A-GAP in clinical assessment. Besides, for DS patients with various sagittal alignments, PSM degeneration may exert different effects on the occurrence of MCs. Therefore, incorporating PSM degeneration indices within the A-GAP Score may improve its accuracy in predicting mechanical complications. Material and Methods: A total of 97 DS patients undergoing posterior spinal fusion surgery (≥ 4 vertebrae) with a minimum of 2 years follow-up were retrospectively reviewed. Their A-GAP scores were calculated based on our previous study and patients were divided into 3 A-GAP categories, “proportional” (P), “moderately disproportional” (M), and “severely disproportional” (S). Relative cross-sectional area (cross-sectional area of muscle–disc ratio×100) and the fatty infiltration rate, (FI %) at L1-L2, L2-L3, L3-L4, and L4-L5 discs were quantitatively evaluated using MRI. In each A-GAP category, patients were additionally divided into the MC group and the non-MC group. A multivariable logistic regression model consisting of the CSA-weighted average FI% (total FI%) and the A-GAP score (A-GAPM) was constructed. The AUC of the ROC curve was used to evaluate the predictability of the GAP score, the A-GAP score, the FI%, and the A -GAPM. Results: For all 97 patients, FI% at L1/2, L2/3, L3/4, and L4/5 disc and the total FI% of the MC group (n = 32) were significantly higher than that of the non-MC group (n = 65). The MC rates of 3 original GAP categories, P category, M category, and S category were 28.57% (6/21), 31.25% (10/32), and 36.36% (16/44) (χ2 = 0.456, p = 0.796). Based on the A-GAP score, the MC rates of the P, M, and S groups were 14.71% (5/34), 35.41% (17/48), and 66.67% (10/15), with significant differences (χ2 = 12.679, p < 0.001). In the A-GAP M category, compared with the non-MC group (n = 31), the MC group (n = 17) has a higher total FI% rate (29.37 ± 10.48 vs 22.63 ± 8.17, p = 0.017). A similar trend was identified in the A-GAP S category (34.68 ± 11.59 vs 19.85 ± 5.27, p = 0.019), but not in the A-GAP P category (27.21 ± 6.48 vs 24.48 ± 8.04, p = 0.480). The AUC of the GAP score, the A-GAP score, the FI%, and the A-GAPM were respectively 0.591, 0.703, 0.719, and 0.768. Conclusion: Compared with the GAP score, the A-GAP score shows better accuracy for the prediction of postoperative mechanical complications of Chinese DS patients. For DS patients in the A-GAP M and S category, the PSM degeneration exerts a significant effect on the occurrence of MCs after the corrective surgery. The integration of PSM fatty infiltration with the A-GAP score enables a more accurate prediction of MCs following ASD surgery.
1382
RF007: Sagittal alignment of diverse mechanical complications following adult spinal deformity surgery
Changyu PAN 1 , Guohua Lv 1
1 Spinal Surgery, The Second Xiangya Hospital of Central South University, Changsha, China
Introduction: Sagittal malalignment has been proved to be strongly related to the occurrence and progression of mechanical complications (MCs). Prior studies usually viewed MCs as a single entity and overlooked the differences among different subtypes; to our knowledge, a study that has comprehensively investigated the sagittal characteristics of each MC subtype has not yet been performed. The main objectives of this paper were to explore the sagittal alignment associated with different subtypes of MCs at different time points following adult spinal deformity (ASD) surgery and to assess the correlations of each MC subtype with the Global Alignment and Proportion (GAP) score, in order to understand the pathological alignment and evolution process of various MCs, which could provide a more adapted revision scheme. Material and Methods: A total of 371 patients who underwent ASD surgery were enrolled. The sagittal spinopelvic parameters were measured preoperatively and at the 6-month and last follow-up, and the Global Alignment and Proportion (GAP) score was calculated. The subjects were divided into normal and MCs groups, and the MCs group was further divided into rod fracture (RF), screw breakage (SB), screw dislodgement (SD), and proximal junctional kyphosis (PJK) subgroups. Results: In this cohort, a total of 252 MCs occurred in the 187 patients (50.4% of all patients), including 118 patients (63.1% of total MCs patients) with RF, 24 (12.8%) with SB, 36 (19.3%) with SD, and 74 (39.6%) with PJK; and 96 patients (51.3%) presented more than one MCs. Regarding the fusion levels, the mean UIV was higher in the RF (approximately T8) groups than in the normal group (approximately T10), and there was no significant difference in the LIV between the normal and MCs groups. Furthermore, the average number of fusion levels was larger in the RF (11.6 ± 3.5) groups than in the normal group (10.3 ± 3.6). Preoperatively, the RF group had marked kyphosis in the upper lumbar spine (6.1 ± 18.8°); the SB group had the largest pelvic incidence (PI, 63.6 ± 16.8°) and lumbar lordosis (LL, -42.1 ± 18.0°); the SD group had the greatest lower LL (-35.8 ± 14.9°); and the PJK group had the highest thoracic kyphosis (TK, 41.0 ± 18.0°). At the last follow-up, the RF and SB groups featured a small LL (-43.6 ± 13.7° and -42.5 ± 14.0°), while the PJK group featured a large TK (63.2 ± 17.6°); all the MCs subgroups had sagittal malalignment and a higher GAP score, and the SB group had the most severe cases. Logistic regressions showed that the relative spinopelvic alignment (RSA) score was correlated with RF (OR = 1.710) and SB (OR = 2.929), while the RSA (OR = 2.353), lordosis distribution index (LDI, OR = 0.656) and age (OR = 4.901) scores were associated with PJK. The reoperation rate of the total MCs group was 59.4%, which was comparatively higher in the RF (71.2%) and SB (70.8%) groups, followed by the SD (66.7%) and PJK (55.4%) groups. Conclusion: Each patient with MCs had individual characteristics in the sagittal plane at different time points following ASD surgery, which may be helpful to understand the pathophysiology of poor sagittal alignment with its subsequent MCs and guide an eventual revision strategy.
51
RF008: Outcomes and complications of surgery for symptomatic spinal metastases; a comparison between patients aged ≥70 and <70
Qinxiang Shant Sin 1 , Jiong Hao Tan 2 , Denni Hey 2 , Naresh Kumar 2 , James Hallinan 3 , Gabriel Ka Po Liu 2 , Isaac Le Tian Tan 4 , Joelle Hwee Inn Tan 4 , Shi Wei Ang 4 , Tuan Hao Tan 4
1 Orthopaedic Surgery, MOHH Singapore, Singapore, Singapore
2 Orthopaedic Surgery
3 Diagnostic Imaging, National University Hospital, Singapore, Singapore
4 Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Introduction: Advances in oncological treatment have resulted in increased life expectancies for cancer patients. This combined with an aging population has led to more elderly patients presenting with spinal metastases. Physicians may be deterred from operating on these elderly patients due to fears of poorer outcomes and increased complications. In this study we aim to compare the outcomes of surgical treatment of spinal metastases in patients aged ≥ 70 years old and patients aged < 70. Material and Methods: This is a retrospective study of patients who underwent surgical treatment for spinal metastases between January-2005 to December-2021. Inclusion criteria included surgical treatment for spinal metastases with metastatic spinal cord compression or spinal instability. Patients were followed up till death or minimum 1 year post surgery. Follow up was till death or a minimum 1 year post surgery. Data was collected from operative records and patient electronic medical records. This included demographic, clinical, oncological and operative data. These patients were divided into two groups age < 70 years and ≥ 70 years. Outcomes studied included post-operative neurological status, ambulatory status, medical and surgical complications and the need for readmission after surgery. Two Sample t-test/Mann Whitney U test were used to compare the differences for numerical variables between the two groups. Pearson Chi-Squared or Fishers Exact test were used for categorical variables. Overall survival between the two groups was presented with a Kaplan-Meier analysis. p value of < 0.05 was taken to be significant. Results: 412 patients were identified of which 383 (92.9%) were included for analysis, 29 (7.1%) patients were excluded due to loss to follow up and previous surgical treatment.” 79 (20.6%) were ≥ 70-yrs. Age ≥ 70-yrs patients had significantly poorer ECOG scores 3-4 (p = 0.0017) and, CCI Charlson Comorbidity Index (p < 0.001). There was no significant difference in modified Tokuhashi score (p = 0.393), but there were significantly more ≥ 70-yrs patients with prostate (p < 0.001) and liver (p = 0.029) cancer. Post-operative neurological function (Improved or maintained normal neurological function (≥ 7 0 vs < 70) (71.4% vs 73.4%) (p = 0.934), ambulatory status (Independent (≥ 70 vs < 70) (52.0% vs 41.8%) (p = 0.171), and survival was similar.at 6 months (p = 0.119) and 12 months (p = 0.659) was not significantly different. There was no significant difference in in medical (p = 0.528) or surgical (p = 0.466) complication rates and readmission (p = 0.800) rates. Conclusion: ≥ 70-yrs patients have comparable improvement in neurological function & ambulatory status to younger < 70 patients with no significant difference in complication rates. Age should not be a factor in deciding surgical management of spinal metastases.
2511
RF009: Saving spinal cord function by using intraoperative monitoring and rapid response during spinal deformity surgery
Munish Gupta 1 , Zeeshan Sardar 2 , Lawrence Lenke 2 , Saumyajit Basu 3 , Kenny Yat Hong Kwan 4 , Stephen Lewis 5 , Miranda van Hoff 6 , So Kato 7 , Alekos Theologis 8 , Anastasios Charalampidis 9 , Christopher Ames 8 , Kristen Jones 10 , Ferran Pellise 11
1 Orthopaedic Surgery, Washington University School of Medicine, St. Louis, USA
2 Columbia University
3 Kothari Medical, Kolkata, India
4 University of Hong Kong, Hong Kong
5 Toronto Western Hospital, Toronto, Canada
6 Radboud University, Nijmegen, The Netherlands
7 University of Tokyo, Tokyo, Japan
8 University of California, San Francisco, USA
9 Karolinska University, Solna, Sweden
10 University of Minnesota, Minneapolis, USA
11 Hospital Vall d'Hebron, Barcelona, Spain
Introduction: Intra-operative neuromonitoring (IONM) is used in spinal deformity operations to detect changes in neural function with the goal that such changes can be reversed to prevent neural injury. The purpose of this study is to assess use of IONM in preventing neurologic deficits during complex cord-level deformity operations. Material and Methods: 20 international centers prospectively documented IONM, demographics, radiographic findings, and surgical events of patients undergoing spinal deformity correction based on a standardized data collection form. Inclusion criteria included ages 10-80 years, neurologically intact, major Cobb > 80° or undergoing any spinal osteotomy with EMG, SSEP, and MEP monitoring. Detailed neurological examination was performed at baseline, immediately post-op and prior to hospital discharge. IONM change was defined as amplitude loss of > 50% in SSEP or MEP from baseline or sustained EMG activity that lasts > 10 seconds. Types and rates of IONM alerts as well as intra-operative responses to each alert during cord-level operations were assessed. Results: Of 349 patients who had cord-level operations, 16% had at least one IONM alert. These patients had a mean age of 23.4 ± 17.2 years and were primarily female (77.2%) who underwent primary operations (82.5%) for scoliosis (77.2%) or kyphosis (24.6%) through a posterior-only approach (99.4%; mean levels 12.2 ± 3.3) and utilized any osteotomy in 93% cases [PCO (type 2)-43; PSO (type 3/4)-5; VCR (type 5/6)-10]. While these patient characteristics and operative strategies were similar to non-alert patients, they had significantly larger coronal Cobb angles (73.4° v. 61.3°; p = 0.008) and coronal deformity angular ratios (DAR) (11.0 vs. 8.3; p < 0.001). There were 81 total IONM alerts. A single IONM alert was most common (71.2%) followed by 2-alerts (19.3%) and 3-alerts (19.3%). MEP changes were most common (76.5%; unilateral-53.2%; bilateral-46.8%). Combined MEP+SSEP alerts occurred in 17.5% of cases. Events preceding the alert were surgical in 67% of operations and included release/osteotomy (57.9%), correction/rod placement (21.1%), and instrumentation placement (18.4%). Osteotomy/release was the most common cause of unilateral IONM alerts whereas rod placement/correction was the most common cause of bilateral IONM alerts. Rapid corrective actions (i.e elevating blood pressure, transfusion, anesthesia adjustments, rod and/or implant removal, steroid administration, lessen correction, decompression) reversed 80% of the IONM changes. In patients with any IONM alert, 25.0% had new neurological deficits, 21.4% had motor dysfunction (LEMS decrease), and 5.8% had sensory dysfunction. New neurological deficits occurred in 4.9% of patients who did not have IONM alerts (i.e. false negatives). No spinal cord syndrome occurred without alerts (cord-level false negative). Conclusion: In complex, cord-level spinal deformity operations, IONM alerts occur more commonly in patients with larger coronal Cobb angles and DARs and are manifested most frequently in MEP changes. That the majority (80%) of alerts can be reversed with rapid responses resulting in preserved spinal cord function makes IONM an extremely valuable tool for spinal cord monitoring in these high-risk patients. However, its 4.9% false negative rate speaks to its limitations and highlights the need for more sensitive detection modalities for detecting LEMS decreases. There were no false negatives in detecting a spinal cord syndrome.
1879
RF010: Evidence-based risk mitigation protocol for patients undergoing scoliosis surgery
Fernando Alvarado Gómez 1 , Leslye Yadira Borrero Carabali 1 , Roberto Diaz Sanchez 1 , Nahala Aborashed-Amador 1 , Carlos Montero 1 , Mario Herrera Méndez 1 , Maria Camila Giraldo Bernal 1 , Ricardo León Restrepo Vallejo 1
1 Cirugia de Columna, Instituto Roosevelt, Bogota, Colombia
Introduction: Scoliosis encompasses a spectrum of complex and multifactorial deformities, posing challenges for the medical team, patients, and caregivers alike. On the other hand, surgical management of this condition carries elevated risks, as patients may present with poor nutritional status and involvement of multiple systems, including the cardiopulmonary system. These underlying conditions, in turn, increase the risk of postoperative complications. Therefore, the decision was made to establish a protocol to preoperatively mitigate these risks in these patients and improve outcomes. Materials and Methods: A systematic literature review was conducted using search queries in PubMed, Scopus, and Embase databases. Risks were categorized into nine risk domains: Hematological, Cardiopulmonary, Nutritional, Medication-related, Allergic, Adverse Transfusion Reactions (ATR), Infectious, Opioid Abuse, and Vision Loss. A specific question was formulated for each domain, followed by the identification of literature that met inclusion criteria. The search was performed, taking into account articles involving patients diagnosed with scoliosis undergoing surgical correction. Results: Articles were selected, and the following risk mitigation criteria were established for each domain. For hematological risk, taking a complete blood count, evaluating coagulopathies, and initiating replenishment and stimulants for suboptimal hemoglobin levels are considered appropriate. Concerning cardiopulmonary risk, the severity of the curve, medical history, and cardiopulmonary involvement should be assessed through extension tests and surgical approach (including the number of surgical stages and surgeons involved). Nutritional risk should involve an evaluation of alterations in the Body Mass Index (BMI), levels of albumin, total proteins, lymphocytes, and prealbumin, with referrals to specialized nutritional consultation as necessary. Medication-related risks require medication reconciliation to identify drugs that increase the risk of bleeding. Allergenic risks, both food and drug-related, should be taken into account. For ATR risks, it is advisable to inquire about previous transfusion reactions and alcohol and cigarette consumption. Infection risks depend on the number of surgical stages, surgical approaches, instrumented levels, and a history of urinary tract infection (UTI) and urinary incontinence. To mitigate these risks, additional measures should be taken before the procedure. Regarding the risk of vision loss, it is suggested to keep surgical durations under 6.5 hours, maintain optimal tension, hemoglobin, and hematocrit levels during the procedure. Finally, the risk of opioid dependence can be identified using the (SOAPP-R) tool, and alternative analgesia options should be explored. Conclusions: The adoption of evidence-based preoperative approaches significantly benefits the quality of life of patients undergoing surgery by reducing the risk of postoperative complications. In summary, the evaluation and mitigation of preoperative risks are essential tools for improving postoperative outcomes and enhancing healthcare, ultimately contributing to a more efficient and secure healthcare system.
1747
RF011: Anaphylaxis in spine surgery
Joseph Gutbrod 1 , Matthew Goodwin 1 , Kya Vaughn 1
1 Orthopedic Surgery, Washington University School of Medicine, St. Louis, USA
Introduction: Perioperative anaphylaxis is an acute, life-threatening condition that can affect patients undergoing anesthetic surgery. This condition is classically a type I hypersensitivity reaction that presents with several common cardiovascular and respiratory complications, all of which may have dire consequences on surgical outcomes. There is a scarcity of literature on anaphylaxis in spine surgery. This study seeks to determine the major causal agents of anaphylaxis in surgery of the spine, as well as the common presenting anaphylactic symptoms in spine surgery patients. This study also presents two case reports that portray the clinical context of perioperative anaphylaxis during spine surgery. Methods: A PubMed database search was performed using the following search terms: “anaphylaxis” AND (“spine” OR “spinal”). Articles were selected that documented cases of anaphylaxis during spine surgery. From these cases, relevant variables were collected, including the causal agent, presenting symptoms, outcome of the complication, medical history of the patient, and subsequent allergy testing results. Descriptive statistics and graphing were performed using Microsoft Excel and R Studio. Results: The search yielded 24 articles that reported cases of anaphylaxis in spine surgery. From these articles, 36 patient cases were documented and analyzed in this review. Gelatin, antibiotic agents, and neuromuscular blocking agents (NBMAs) were found to be the three most frequent causal agents of anaphylaxis in spine surgery, making up 43%, 27%, and 8% of cases respectively. Cement (6%), tranexamic acid (6%), albumin (3%), atropine (3%), and sugammadex (3%) were also found to be causal agents in our search. The most frequent symptoms during these anaphylactic events were hypotension (97%), tachycardia (72%), respiratory complications (44%), decreased oxygen saturation (41%), and cutaneous symptoms (38%). Of the 37 cases, 35 patients (94%) were stabilized without severe complication, while 2 cases (6%) resulted in fatal complications. Our first case report presents an anaphylactic reaction to roconurium (a common NMBA agent) during a T10-S2 posterior exposure for a patient with spinal stenosis. This patient presented with hypotension, hemodynamic instability, and a cutaneous rash during his reaction. Our second case report describes an anaphylactic reaction to sugammadex during a C4-C7 posterior instrumented fusion. This second case presented with hypotension and swelling of the face and hands. Both patients were emergently treated with epinephrine and stabilized thereafter. Conclusion: This study provides a valuable reference for spine surgeons hoping to understand potential etiologies of anaphylactic reactions as well as its significant presenting symptoms in the operating room. Our results suggest a linkage between spine surgery and risk of anaphylaxis to gelatin, which is not considered a common cause of general perioperative anaphylaxis. This finding warrants further investigation with higher powered studies and appropriate comparison groups. Although rare, perioperative anaphylaxis is a possibility that should be considered in the planning and execution of spine surgery. Spine surgeons should always take a detailed history of patient allergies and, if warranted, consider prophylactic allergy testing to prevent anaphylaxis in future cases.
Keywords: spine; anaphylaxis; surgery
2500
RF012: Incidental durotomy in spine surgery: an underestimate complication?
Maria Ilaria Borruto 1 , Calogero Velluto 1 , Andrea Perna 2 , Maria Concetta Meluzio 1 , Francesco Ciro Tamburrelli 1 , Maurizio Genitiempo 1 , Luca Proietti 1
1 Policlinico Universitario A Gemelli IRCSS, Rome, Italy
2 Fondazione Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy
Introduction: Incidental durotomy is a common complication in spine surgery, still it is underestimate. In order to reduce the incidence is important to understand potential risk factors. In literature most of scientific works are represented by small case-series or retrospective studies analyzing few cohorts of patients.This article aim to study the incidence, clinical consequence, treatment, risk factor of incidental durotomy during spine surgery. Material and Methods: We conducted a comprehensive review of medical records and surgical reports for patients who underwent spinal surgery at our institution between 1-01-2021 and 31-12-2022. Patients with documented accidental durotomies were included in the study, while those with dural injuries not directly related to the surgical procedure were excluded (i.e. traumatic injuries, intradural tumors). Demographic data, surgical details, intraoperative findings, postoperative complications, and follow-up outcomes were analyzed. Results: A total of 72 patients with accidental durotomies were identified within the study period. The overall durotomy rate was 8.15%, with the most common surgical procedures associated with durotomies being lumbar decompression, with a major incidence in MISS procedures comparing open-approach, but without a statistically significant difference. Risk factors such as ASA, previous spinal procedures (including steroids injections), diabetes, smoking were identified as significant predictors of durotomies (p < 0.05). In 39 patients a dural suture were performed, in the remaining part was used a graft. 18 patients showed complications such as: wound infection, pseudomeningoceles, CSF leak. 15 of these underwent revision surgery. Conclusion: Dural leakage is still a challenging complication to manage, so understand risk factors represent an important instrument for a spinal surgeon.
89
RF013: Gender disparities in postoperative outcomes following elective spine surgery: a systematic review and meta-analysis stratified by database source
Neerav Kumar 1 , Izzet Akosman 1 , Richard Mortenson 2 , Abhinav Kumar 3 , Grace Xu 4 , Kylie Bakhmat 5 , Cooper Lathrop 6 , Troy Amen 7 , Ibrahim Hussain 8
1 Weill Cornell Medical College, New York, USA
2 Duke University, Durham, USA
3 Stanford University, Palo Alto, USA
4 Princeton University, Princeton, USA
5 Boston University, Boston, USA
6 Neurological Surgery, Robert Wood Johnson Medical School, New Brunswick, USA
7 Hospital for Special Surgery, New York, USA
8 Neurological Surgery, Weill Cornell Medicine, New York, USA
Introduction: With several studies documenting disparities between male and female patients following spine surgery, the differential care for male and female patients is a growing concern. However, no pooled analyses have performed a robust review characterizing differences in post-operative outcomes based on gender. We sought to use an AI-assisted review platform to broadly assess the effects of gender on postoperative outcomes following elective spine surgery. Material and Methods: A comprehensive literature search of PUBMED, MEDLINE(R), ERIC, and EMBASE was performed using a semi-automated review software. 42 total meta-analyses were performed to calculate pooled odds ratios or standardized mean differences for each outcome: readmission, non-routine discharge (NRD), length of stay (LOS), extended LOS, reoperation, mortality, all medical complications (individual analyses for cardiovascular, DVT/PE, genitourinary, neurologic, respiratory, and systemic infection complications), and wound-related complications. For each outcome, two sub-analyses were performed with studies that use either center-based (single- or multi-institution) or high-volume (national or state-wide) databases. Results: 124 studies (13,790,096 total patients) were included. Across all included studies, male patients had increased incidence of mortality (OR 0.54, p < 0.0001) and all medical complications (OR 0.80, p = 0.0114) -specifically cardiovascular (OR 0.68, p < 0.0001) and respiratory (OR 0.76, p = 0.0008). Female patients were more likely to experience a wound-related surgical complication (OR 1.16, p = 0.0183). These findings persisted in the high-volume database sub-analyses. Only center-based sub-analyses showed that female patients were at greater odds of experiencing a NRD (OR 1.18, p = 0.0476), longer LOS (SMD 0.23, p = 0.0036), and extended LOS (OR 1.28, p < 0.0001). Conclusion: Males are more likely to experience death and medical complications, while females are more likely to face wound-related surgical complications. At the institution level, females more often experience NRD and longer hospital stays. These findings may better inform expectation management preoperatively, and provide a more accurate and tailored risk assessment for postoperative complications based on the patient’s gender.
967
RF014: Intra-abdominal content movement in prone versus lateral decubitus position lateral lumbar interbody fusion (LLIF)
Cristiano Menezes 1,2 , Luciene Andrade 3 , Gabriel Lacerda 4 , Marlus Salomão 4 , Mark Freeborn 5 , J. Alex Thomas 6
1 DALO (Departamento do Aparelho Locomotor), Federal University of Minas Gerais (UFMG), Belo Horizonte, Brazil
2 Spine, Biocor Rede D'Or - Vila da Serra Hospital, Nova Lima, Brazil
3 Radiology, Hermes Pardini, Belo Horizonte, Brazil
4 Spine, Biocor Rede D'Or - Vila da Serra Hospital, Nova Lima, Brazil
5 Spine, Evergreen Health, Kirkland, USA
6 Spine,Atlantic Brain and Spine Institute, Wilmington, USA
Hypothesis / Study Design: There is change in position of the peritoneal contents in individuals in lateral decubitus (LD) versus prone. Introduction: Radiographic study of 34 healthy volunteers using magnetic resonance imaging (MRI) obtained in right lateral decubitus and prone positions. Studies have validated the safety of LLIF with regards to visceral, vascular and neurological injury. While LLIF has historically been studied and performed in the lateral decubitus (LD) position, recently the technique has been performed in the prone position. There is still lack of clarity regarding the movement of peritoneal contents between the LD and prone position during LLIF. Methods: Anatomical measurements were performed on axial MRI images at the L3/4 and L4/5 disc spaces by two independent observers. For the prone scans, the subjects were positioned on a carbon fiber positioner such that the abdomen could hang freely. Results: Mean age was 44.4 years (24-67) and BMI was 27.5 ± 10.5 kg/m2. 56% of the cohort were males and 44% female. Distance between skin and lateral disc surface was increased in the prone position: L-SD = 118.7 mm versus P-SD = 134.9 mm, p < 0.0001. Distance between the posterior annulus and the colon was significantly decreased in the prone position: L-PVBC = 41.1 mm (-4.5 mm – 123 mm) versus P-PVBC = 20.3 mm (-10.4 mm – 75.5 mm), p < 0.0001. The colon moved more posteriorly in relation to the anterior margin of the psoas in the prone position: L-APC = -5.46 mm (-40 to 50.5 mm) versus P-APC = -21.67 mm (-47.3 mm to 21.3 mm), p < 0.0001 Lastly, distance between the QL and colon was decreased, though not significantly, in the prone position: L-QLC = 44.7 mm (2.2 mm - 94.5 mm) versus P-QLC = 20.50 mm (1.5 mm - 67.0 mm), p < 0.0001. Conclusion: The study demonstrates increased distance between the skin and disc space as well as a more posterior location of the colon in relation to the spine and psoas muscle in prone versus LD position. The presence of the colon within the intended LLIF access corridor was almost invariable. Surgeons should be alerted to the potential increased risks of this surgical approach in the prone position.
2520
RF015: Post surgery tool for prediction of upper airway compromise following anterior cervical spine surgery
Neel Patel 1 , Alexander von Glinski 1 , Christopher Elia 1 , Clifford Pierre 1 , Basem Ishak 1 , periklis godolias 1 , Ronen Blecher 1 , Joseph R. Dettori 2 , Daniel Norvell 2 , Steven Deem 1 , Blake Golden 3 , Thomas A. Schildhauer 4 , Rod Oskouian 1 , Jens Chapman 1
1 Swedish Neuroscience Institute, Seattle, USA
2 Spectrum Research Inc, Steilacoom, USA
3 Swedish Cancer Institute, Sweden
4 General and Trauma Surgery, Bochum, Germany
Objective: Acute upper respiratory tract compromise is a rare but catastrophic complication after anterior cervical discectomy and fusion (ACDF). This study aims to develop a score to identify patients at risk for acute post-operative airway compromise (PAC). Methods: Potential risk factors for acute PAC were selected through a modified Delphi process. Patients with acute PAC were identified out of 1,466 patients who underwent elective ACDF between July 2014 - May 2019. A comparison group was created by a randomized selection process (Non-PAC group). We compared presence or absence of potential risk factors for both groups using bivariate analysis retaining factors that showed a p-value ≤ 0.10. Results: We identified 18 potential risk factors from our Delphi process, of which 5 factors demonstrated a significant association with airway compromise. Age > 65 years, current smoking status, ASA > 2, history of a bleeding disorder, and duration of surgery > 179 min. We used the coefficients generated from the 5-item prediction model to create a score for each predictor relative to its coefficients weight. This has led to a 100 point total score. PACS to balance sensitivity (80.0%) and specificity (88%). Conclusions: We introduce a tool termed the acute Post-operative Airway Compromise Scoring system (PACS) to help patients at risk for upper airway compromise caused by surgical site abnormalities.
2037
RF016: Venous thromboembelism chemoprophylaxis follow spine surgery: a meta-analysis of randomized controlled trials
Aditya Muralidharan 1 , Anthony Baumann 2 , Joshua Piche 3 , Yasser Abusabha 1 , Davin Gong 1 , Kempland Walley 1 , Osama Kashlan 4 , Rakesh Patel 1 , Ilyas Aleem 1
1 Orthopedic Surgery, University of Michigan, Ann Arbor, USA
2 Rehab Services, College of Medicine, Northeast Ohio Medical University, Rootstwon, USA
3 Orthopedic Spine, USC Keck, LA, USA
4 Neurosurgery, University of Michigan, Ann Arbor, USA
Background: Postoperative venous thromboembolism (VTE) is an overall rare complication following spine surgery. Pharmacologic VTE prophylaxis remains controversial in this patient population, as potential risks associated with anticoagulants, namely epidural hematoma, must be considered. Methods: We conducted a systematic search of trusted electronic databases to identify randomized controlled trials (RCTs) that evaluated pharmacologic versus mechanical VTE prophylaxis following spine surgery. Two independent reviewers used the Grades of Recommendation Assessment, Development and Evaluation (GRADE) criteria to assess eligibility and risk of bias, perform data extraction, and rate the quality of evidence. The outcomes of interest were total VTE and bleeding. We conducted meta-analyses of total VTE, deep vein thrombosis (DVT), severe bleeding, and significant bleeding. Results: After screening 927 articles, a total of 7 studies were eligible for final inclusion. These included 1509 patients, of whom 1,151 received pharmacologic VTE prophylaxis and 358 received mechanical VTE prophylaxis. Moderate-quality evidence demonstrated there was no significant difference between groups in rates of VTE (p = 0.639; RR: 1.01; 95% CI: 0.96, 1.06) or DVT (p = 0.064; RR: 1.03; 95% CI: 1.00, 1.07). There was also no significant difference between groups in risk of severe bleeding (p = 0.377; RR: 1.04, 95% CI: 0.95, 1.14) or significant bleeding (p = 0.517; RR: 1.02; 95% CI: 0.96, 1.08). Conclusion: Moderate-quality evidence does not support the routine use of pharmacologic DVT prophylaxis following elective spine surgery. Future high-quality randomized comparative-effectiveness trials with sufficient power to evaluate safety and efficacy given the rarity of complications are warranted.
2563
RF017: Pedicle screw loosening: a proposed clinical grading system
James Hicks 1 , Gerrit Lewik 1 , Rod Oskouian 1 , Jens Chapman 1
1 Neurosurgery, Swedish Neuroscience Institue, Seattle, USA
Introduction: Pedicle screw loosening represents a challenging problem in fusion surgeries. Rates of loosening range from 1% up to 60%, and this varies by definition of loosening, which currently are vague. As of now, there is no grading system for screw loosening, and therefore, its clinical significance remains elusive. A grading scale is most useful when it possesses content validity, reliability, and predictive validity to help direct the best treatment strategy for the pathology and having a grading scale for screw loosening could also impact outcomes and treatment. Therefore, our goal is to create a valid and reliable grading system to classify screw radiographic loosening in a clinically useful way. Material and Methods: We used an IRB approved retrospective study format utilizing the electronic medical records of our Radiology and Clinical Departments searching for the phrase ‘screw loosening’ in all post operative instrumented patients with CT Thoracic and Lumbar scans from 2010 to 2022. These scans were viewed by fellowship trained spine surgeons for radiographic evidence of loosening. The patients were then scrutinized statistically for demographics and risk factors significant for loosening. A grading scale for pedicle screw loosening was created using the Delphi Method. This method utilizes survey/ questionnaire to qualify expert opinion. Five fellowship trained spine surgeons answered the survey in 2 rounds approximately 1 month apart. Over 900 responses were recorded through the survey.
The proposed grading process is as follows:
Grade A: inconclusive evidence of loosening Grade B: radiographic evidence of loosening Grade C: severe pedicle erosion or screw pullout Grade D: complete obliteration of pedicle/unsalvageable pedicle Grade E: Screw fracture
Statistical significance tests were performed to determine if certain grades of loosening correlated with particular survey answers using formal inter- and intra-observer testing. No cervical spine cases were used in this study. Results: Our results results confirmed reliability of the proposed grading system for screw loosening. We found a 0.87 correlation regarding the grade and a 0.86 correlation on how to manage the case surgically between the evaluators, which shows a high inter-surgeon reliability. The intra-surgeon reliability also confirmed satisfactory correlation. Risk factors associated with loosening were not determined within this study. Treatment impact, however, could be confirmed with this study. Conclusion: Using a simple 5-part grading system for screw loosening, created from a formal Delphi process conducted with spine survey content experts could prove a high degree of inter-surgeon and intra-surgeon reliability applying common statistical accepted terms. Our statistical validation did identify a meaningful differentiation that can have helpful applications in determining quality of fusion, detect possible correlation with patient pain and may influence treatment and salvage options. With our detected kappa correlation coefficient of 0.87 for screw loosening and treatment implications, we hope to have provided a helpful basis for further prospective studies to address fusion and outcome.
656
RF018: Investigating the use of peri-operative systemic steroid administration in anterior cervical discectomy and fusion (ACDF) - A systematic review
Hania Shahzad 1 , Muhammad Talal Ibrahim 2 , Cole Veliky 1 , Paul Alvarez 1 , Varun Singh 1 , Frank Epitropoulos 1
1 Orthopedics, The Ohio State University, Columbus, USA
2 Orthopedics, The Aga Khan University, Karachi, Pakistan
Introduction: Steroids have been employed in mitigating dysphagia, a common complication of anterior cervical discectomy and fusion (ACDF) surgery. A recurring debate revolves around the choice between local and systemic steroids. While systemic steroids may offer greater efficacy, concerns regarding non-union and an increased risk of infection limit their application. Conversely, local steroids can alleviate dysphagia without affecting surgical duration or increasing blood loss. However, their use carries a potential risk of esophageal perforation. A comprehensive assessment of the impact and side effects of systemic steroids is necessary to establish their effectiveness and risk profile for mitigating dysphagia. This review investigates the utility of systemic intravenous (IV) steroids in mitigating postoperative complications and clinical outcomes following ACDF surgery. Material and Methods: A comprehensive search of PubMed, Scopus, Cochrane, Web of Science, and Embase databases was conducted for studies that explored the role of systemic steroids in ACDF surgery. Studies with accessible manuscripts published in the English language were included in the review whereas studies involving patients receiving systemic steroids for chronic or metabolic diseases were excluded. Data extraction and risk of bias (RoB) assessment was performed by two independent reviewers using Covidence, and a third reviewer finalized the data. The risk of Bias 2.0 (RoB 2.0) tool was used for clinical trials and the Newcastle-Ottawa Scale (NOS) was used for retrospective studies. Results: Six studies met the eligibility criteria, comprising five clinical trials and one retrospective database study. These studies investigated the use of methylprednisolone or dexamethasone compared to normal saline or no treatment in ACDF surgery. Two of the clinical trials were deemed high quality, two had some concerns, and one had a high risk of bias. The included retrospective study was rated as poor quality. In terms of dysphagia assessment, five studies evaluated its severity using various scales. Earlier studies, including Nam 2013, Song 2014, and Jeyamohan 2015, showed significant improvements in dysphagia within the IV steroid group, particularly during the early postoperative period up to one month. More recent studies, like Jenkins 2018, indicated sustained improvements for up to one year compared to placebo, with superior outcomes to oral steroids initially. Siribumrungwong 2022 demonstrated short-term improvement up to 72 hours. Paravertebral swelling assessment, performed in three studies, yielded mixed results, with Song 2014 showing limited improvement. Dysphonia assessment indicated higher dysphonia on postoperative day 1 in the IV steroid group, while airway compromise improved temporarily. Pain assessment showed varying results, with local steroids providing short-term relief and IV steroids offering longer-term benefits. Fusion rates did not show significant differences, and opioid usage reduction was inconclusive. Notably, non-union cases were reported with local steroids but not IV steroids. Conclusion: IV steroids are beneficial in mitigating dysphagia, with multiple dosing sessions showing long-term effectiveness compared to transient effects of local steroids. Patients may experience anecdotal benefits in terms of airway compromise, pain, and dysphonia without significant systemic complications or lack of fusion. However, there is limited evidence regarding the ideal steroid dosing, frequency, and formulation.
RFP02: Infections
847
RF019: Surgical site infection (SSI) in posterior open spine surgery managed by negative pressure wound therapy: our experience in 25 cases
Nilesh Barwar 1
1 Orthopedics, All India Institute of Medical Sciences, Bathinda, India
Introduction: Post operative spine surgical site infection (SSI) is a serious problem as it entails repeated debridement of the wound with voluminous and expensive implant in-situ. There is a danger of persistent infection of the surgical site on account of extensive metal work in the body. Repeated debridement takes its toll on the patient’s body in form of adverse effects of anesthetic agents and surgical handling of the body tissue. The infection may be converted into a chronic one and the whole purpose of the spine surgery may be defeated if it is not eradicated. Here we report 25 cases of posterior spine surgery in which surgical site infections were successfully delt with repeated debridement along with negative pressure wound therapy (NPWT). Material and Methods: From 2017 to 2022 we performed 543 cases of posterior spine surgery and out of them 25 cases (4.5%) caught surgical site infection, which were managed by repeated debridement along with negative pressure wound therapy. The debridement consisted of copious amount of saline with 3% of H2O2 solution. The average age was 60.4 years (range: 42 to 87) with predominance of female Pts (F:17, M:8). Most common surgery was in lumbar area (≈50%) with the frequent diagnosis of adult degenerative scoliosis (36 % cases) and 3 levels of average instrumentation. Spino-pelvic fixations were also there in around 20% of the cases. 4 cases also had repaired dural tear from the index surgery. Results: First sign of SSI was serosanguinous discharge from the wound most commonly (in 20% of cases) on the day of 4 (range: 2 to 20 days) of the procedure. Temperature rise was recorded only in 40% of cases with a mean of 100.6 degree Celsius. One important thing is that in 11 cases (44 %) excessive increase in bloody discharge from the surgical sites was noted before the diagnosis of SSI was made. E-coli and klebsiella pneumoniae were the most common organisms grown with resistance to most of the antibiotics except intermediate sensitivity to colistin and tigecycline. The mean frequency of debridement with NPWT was 2.4 times (range: 2 to 5) with the delayed wound closure in the mean of 13 days (range:10-25). No Pt had chronic infection, though we needed to remove implant in two cases. No Pt reported recurrent infection in the follow of more than 1 year. Conclusion: SSI in posterior spine surgery with instrumentation can be successfully treated with repeated early debridement with the use of NPWT therapy. It acts as a sterile barrier for the wound and promotes wound healing by continuous static or dynamic suction with eradication of infection, however in persistent infection one might also need to remove the implant assembly.
1088
RF020: Peripherally inserted central venous catheter in outpatient antibiotic spinal infection treatment is safe, effective and leads to significant reduction in healthcare expenses
Maximilian-Niklas Bonk 1 , Krauss Philipp 1
1 Department of Neurosurgery, University Hospital Augsburg, Augsburg, Germany
Introduction: Prolonged antibiotic therapy is often recommended for the treatment of spinal infections. This study aimed to evaluate the efficacy and safety of outpatient intravenous (IV) antibiotic therapy for spinal neurosurgery patients with spondylodiscitis. Methods: We conducted a retrospective study including 67 patients who received peripherally inserted central catheter (PICC) for IV antibiotic therapy between January 2020 and December 2022. Patient data related to infectious and neurosurgical issues were evaluated. All patients received a minimum of 6 weeks of IV antibiotics as inpatients and outpatients. Results: 84 patients were analyzed. Median age of 63 years (SD ± 14.18 years), of whom approximately 46% were female. The average duration of inpatient treatment was approximately 20 days (SD ± 8.8 days). Subsequent outpatient antibiotic therapy had a mean duration of 70.14 days (SD ± 19.37 days), with the outpatient IV treatment accounting for 41.33 days (SD ± 10.03 days). The most frequently identified pathogens were Staphylococcus epidermis and methicillin-sensitive Staphylococcus aureus. No pathogens were detected in 14% of patients through microbiological processing. Radiographic and biochemical evidence of spondylodiscitis was absent in all patients during the final assessment. This approach led to a total cost savings of 3.1 million euros. Moreover, no significant complications were encountered during the treatment. Conclusion: Outpatient intravenous antibiotic therapy via a PICC line is a safe and effective treatment strategy for spinal infections, notably in elderly populations, offering both clinical benefits and significant financial savings.
144
RF021: Spondylodiscitis following non-spine surgery, another definition need attension
Ghazwan Hassan 1
1 Orthopedic & Spine Dept., Al-Kindy Teaching Hospital, Baghdad, Iraq
Background: The literature is lacking on the incidence and management of pyogenic spondylodiscitis (PS) following routine elective surgical procedures. This study aimed to analyze the presentation and treatment outcome in patients with PS following nonspinal surgeries at a tertiary care center with a minimum follow-up of 12 months. Methods: The demographic, clinical-radiologic features, and treatment outcomes in 100 patients with a diagnosis of PS following nonspinal surgical procedures were retrospectively reviewed and analyzed. Results: The common surgical procedures associated with PS were cesarean delivery (37%), gastric sleeve surgery (17.5%), and dilatation and curettage (11.5%). The tissue biopsy culture was positive in 82.5% of patients. A total of 64 patients (64%) were treated with conservative management and 36 patients (36%) were treated surgically. The mean pretreatment Core Outcome Measure Index score significantly decreased at 12 months (p = .0001) after treatment. The mean pretreatment erythrocyte sedimentation rate (p = .0001) and C-reactive protein (p = .0001) levels significantly decreased at 12 months after treatment. Conclusions: With most patients with PS following nonspinal surgeries treated with conservative management, excellent clinical outcomes were achieved in all patients at 12 months after treatment. The diagnosis of PS should be considered in patients presenting with low back pain (LBP) with a recent history of undergoing a nonspinal surgical procedure. Patients who undergo surgical procedures are an important ‘‘at-risk’’ patient population, and early diagnosis and treatment can help achieve excellent clinical outcomes. Further studies are required to determine risk factors and possible perioperative precautions that can be taken to prevent PS in patients who undergo nonspine surgeries. Early diagnosis and treatment offer excellent outcome, aggressive surgeries with debatable outcome in delayed missed presented cases.
223
RF022: Differentiating features of tuberculous and pyogenic spondylodiscitis: function of anterior meningovertebral ligament in the presence of anterior epidural abscess
Nirdesh Hiremaglur Jagadeesh 1
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
Introduction: Tuberculosis (TB) and pyogenic spondylodiscitis stand as the most prevalent forms of spine infections. In the context of an escalating population with compromised immune states, particularly in developing nations, the incidences of both TB and pyogenic spondylodiscitis are on the rise. This surge underscores the significance of promptly distinguishing between these infections, as they can present with similar clinical and radiological features. The present study is motivated by the imperative to differentiate between TB and pyogenic spondylodiscitis. The exploration revolves around the potential utility of identifying the ventral meningovertebral ligament through magnetic resonance (MR) imaging as a means of differentiation. A defining characteristic of TB spondylodiscitis is its early-stage sparing of the intervertebral disc and its associated ligament. This sparing can be attributed to deficiency in proteolytic enzymes. On the other hand, pyogenic spondylodiscitis destroys the ligaments. The central hypothesis of this study posits that TB spondylodiscitis, particularly in the presence of an anterior epidural abscess, will leave the anterior meningovertebral ligament unharmed. In contrast, pyogenic spondylodiscitis is expected to affect this ligament. Material and Methods: This retrospective study was conducted at the Indian Spinal Injuries Centre in New Delhi, covering the data span from 2012 to 2022. Hospital records, specifically from the Pacx system, along with laboratory reports were collected. Patients aged 12 to 90 years were considered eligible for the study. Inclusion criteria required the presence of an epidural abscess on the MRI report. Certain cases were excluded from the study, namely those having only ventral epidural abscess. Postoperative or post-traumatic infections were excluded, as were cases without a definitive diagnosis. Cases with unidentified organisms on culture and those demonstrating a non-infectious final pathology were also excluded. For each patient, a meticulous analysis of MR imaging sequences was undertaken. This encompassed axial and sagittal T2-weighted images (T2WI) as well as T1-weighted images (T1WI) without contrast. A proficient team of reviewers conducted the imaging evaluation. This team comprised two Board-certified Spine Surgeons, each having 5 and 4 years of experience, respectively, alongside two Spine Fellows. The assessment was the result of a collaborative process, culminating in a consensus. To ensure impartiality, all reviewers were blind to the final diagnosis. The reviewers collectively and unequivocally determined whether the anterior meningovertebral ligament remained intact or had been compromised. Results: The study comprised 97 patients (Mean Age: 48.31 ± 16.7; Male/Female: 53/44; Cervical/Dorsal/Lumbar: 8/48/41). Ligament status was assessed with 70 cases having a present ligament and 27 with an absent ligament. Among ligament-present cases, 69 were TB PCR positive and 1 was TB PCR negative. In ligament-absent cases, 10 were TB PCR positive, and 17 (all positive in aerobic cultures) were TB PCR negative. Following was the diagnostic performance metrics Sensitivity: 87.34%, Specificity: 94.44%, Positive Predictive Value (PPV): 80.23%, Negative Predictive Value (NPV): 9%, Accuracy: 88.66%. Conclusion: The presence of an intact anterior meningovertebral ligament serves as an indirect indicator of tubercular spondylodiscitis in cases involving epidural abscesses. This observation yields a Positive Predictive Value (PPV) of 80.2% and a specificity of 94.4%.
272
RF023: Time to positivity of culture - A valuable predictor for staphylococcus related recurrent infectious spondylodiscitis and mortality
Cheng-Min Hsu 1 , Yung-Hsueh Hu 1 , Yu-Cheng Yeh 1 , Tsung-Ting Tsai 1
1 Department of Orthopaedic Surgery, Division of Spine Surgery, Chang Gung Medical Center, Taoyuan City, Taiwan
Introduction: Time to positivity culture (TTP) could be a proxy for infectious burden in patients with infections. TTP on blood cultures has shown its ability to predict clinical outcomes, but there remains a paucity of data on the TTP of spondylodiscitis. This study aimed to determine the association between TTP and the prognosis of infectious spondylodiscitis. Material and Methods: This retrospective cohort study reviewed 582 consecutive patients with spondylodiscitis and receiving surgical management in Chang Gung Medical Hospital during 2017 - 2021. The bacterial, fungus and tuberculosis cultures were routinely taken intraoperatively on each patient, where 111 patients with intraoperative culture of Staphylococcus were analyzed. Cox regression models were used to study the association between TTP and primary outcomes, including survival and recurrence-free survival, where the recurrence was defined as requiring a revision operation for the recurrent spondylodiscitis. Results: The 2-year survival and recurrence-free survival in our cohort was 90 and 71 percent, and the average time to event was 48.0 ± 67.3 and 65.9 ± 83.9 weeks, respectively. The average TTP was 64.9 ± 21.5 hours. In our cohort, longer TTP and shorter ABO (antibiotic duration before operation) were independent predictors of better outcomes. Specifically, TTP ≥ 48 hours and ABO ≤ 1 week were significantly associated with both lower mortality (HR 0.30, p < 0.005; HR 0.35, p < 0.005) and lower recurrence of spondylodiscitis (HR 0.27, p = 0.02; HR 0.30, p = 0.04). Conclusion: TTP provides reliable information in patients with spondylodiscitis, on the survival and recurrence-free survival, with longer TTP and shorter ABO being independent predictors. These data, readily available at no cost, may be used to identify patients who require specific attention, leading to better management and improved outcomes for this challenging disease.
1440
RF024: Vacuum assisted closure and local drug delivery systems in spinal infections: a review of current evidence
Si Jian Hui 1 , Naresh Kumar 1 , Shahid Ali 1 , Renick Lee 1 , Sahil Athia 1 , Praveen Jeyachandran 1 , Jiong Hao Tan 1
1 Orthopaedic Surgery, National University Health System, Singapore, Singapore
Introduction: Spinal infections are still showing increased incidence throughout the years as our surgical capabilities increase, coupled with an overall aging population with greater number of chronic comorbidities. The management of spinal infection is of utmost importance, due to high rates of morbidity and mortality, on top of the general difficulty in eradicating spinal infection due to the ease of hematogenous spread in the spine. We aim to summarise the utility of Vacuum Assisted Closure (VAC) and Local Drug Delivery Systems (LDDS) in the management of spinal infections. Material and Methods: A narrative review was conducted for this paper using PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), The Cochrane Library and Scopus databases through 14 June 2023. The keywords used were “Spine” AND “Infect*” AND (“VAC” OR “drug delivery”). Inclusion criteria for the review were studies with discussion on the use of VAC or LDDS in spinal infection. All studies that had no description regarding the surgical procedure performed, no use of VAC or LDDS and not in English were excluded. The concept of our treatment algorithm for the use of VAC and/or LDDS in spinal infections was done as an expert opinion by the two senior spine surgeons in this manuscript, with experiences from treating and observing patients with spinal infection. Results: A total of 62 studies were included in this review. We discussed the utility of VAC as a tool for management of wounds requiring secondary closure, as well as how it is increasingly being used after primary closure as prophylaxis for surgical site infections (SSIs) in high-risk wounds of patients undergoing spinal surgery. Studies have shown that VAC is versatile in various aspects of spinal surgery, especially in cases where SSI wounds are large and not amenable to primary closure. VAC after primary closure may also be a valuable asset for higher risk procedures such as those with instrumentation, but clear evidence is yet to appear to support the blanket use in spine surgery. The role of LDDS in spinal infections was also discussed, with preliminary studies showing good outcomes when patients were treated with various novel LDDS. We discuss the role of various LDDS such as antibiotic bone cement (ABC), vancomycin powder and closed suction irrigation systems (CSIS). However, the current literature for LDDS are limited to small case series and there is still a lack of prospective comparative studies to establish the role of LDDS in wound healing. The article clearly shows that there is a definite place for VAC and LDDS in wound closure for complex spinal procedures. Conclusion: We have summarized and given our recommendations for the use of VAC and LDDS for spinal infections. A treatment algorithm has also been established, to act as a guide for spine surgeons to follow when tackling various spinal infections.
1460
RF025: Diagnostic accuracy of line probe assay for rapid detection of mycobacterium tuberculosis in spinal tuberculosis samples
Murahari Penkulinti 1 , Vishnu Manyam 1
1 Spine Surgery, Sunshine Bone and Joint Institute Kims Hospital, Hyderabad, India
Background: Among skeletal TB cases, the spine is the most common location, limited presence and difficulty in accessing infected regions for biopsy pose challenges in detecting Mycobacterium tuberculosis complex. Molecular diagnostic tests have shown promise in rapidly and accurately detecting MTBC. Objective: This study aimed to assess the diagnostic accuracy of a line probe assay for the rapid detection of MTBC and drug-resistant strains in samples from spinal TB patients. Methods: A prospective study was conducted at Sunshine Hospital India, between November 2017 and October 2022. Patients with suspected spinal TB based on clinical and radiological findings were included. Samples were collected from pus, tissues, and bones and subjected to Ziehl-Neelsen staining, culture on liquid and solid media, and GenoType MTBDRplus LPA. Results: A total of 72 patients were enrolled, with 53% being male and 50% belonging to the age group of 30-50 years. The majority of samples were obtained from pus (n = 47), followed by tissues (n = 13) and bones (n = 12). Out of these, 59 samples tested positive for MTBC, while 13 samples were negative across all diagnostic methods. Smear microscopy, culture, and LPA yielded positive results in 46 (63.9%), 43 (59.7%), and 56 (77.8%) samples, respectively. Using culture as the reference standard, LPA demonstrated a sensitivity of 93% and specificity of 44.83%. The positive and negative predictive values of LPA were 71.43% and 81.25%, respectively. Among the 59 positive samples, 53 were susceptible to both rifampicin and isoniazid, three samples showed rifampicin mono-resistance, one sample displayed isoniazid mono-resistance, and two samples exhibited multidrug resistance. Conclusion: This study underscores the rapid and sensitive nature of LPA in detecting M. tuberculosis. The results highlight the potential role of LPA in national control programs, particularly in high TB burden countries like India where isoniazid mono-resistance is prevalent.
30
RF026: Iodophor-impregnated adhesive incision draping reduces the rate of surgical side infection in spine surgery: study in 2279 patients
Aylin Gencer 1 , Christian Schichor 1 , Joerg-Christian Tonn 1 , Sebastian Siller 1
1 Department of Neurosurgery, LMU Hospital, Munich, Germany
Introduction: Surgical site infection (SSI) is a potentially devastating complication of spine surgery. While iodine-impregnated adhesive incise drapes are widely used during surgeries for reducing surgical site contamination, evidence is still scarce if this can reduce the rate of SSI in spine surgery. Material and Methods: All patients who had been surgically treated in our high-volume tertiary-care neurosurgical university spine center between January 2018 and December 2021 were retrospectively evaluated and devided into a cohort treated before (‘control cohort’) and after (‘study cohort’) introduction of iodophor-impregnated adhesive incision drapes in our institute. Epidemiological aspects, baseline characteristics, operative records and rate/characteristics of postoperative SSI were analyzed and compared between both cohorts. Results: A total of 2279 patients were included with a mean age of 60 years and a slight predomination of the male gender (male/female: 1.2/1). Baseline patients’ findings as well as surgical characteristics including indication, localization, procedure and duration of surgery did not significantly differ between the 1125 patients of the ‘control cohort’ and the 1154 patients of the ‘study cohort’. The rate for SSI was 0.5% (11/2279) in the overall cohort with a predomination of early postoperative SSI involving the deeper wound layers. Uni- and multivariate analysis showed that the use of a iodophor-impregnated adhesive incision drape (compared to no adhesive drape) was the only factor significantly associated with a lower risk of postoperative SSI. The rate of SSI was indeeded significantly lower in the “study cohort” with use of iodophor-impregnated adhesive incision drapes compared to the “control cohort” without use of incision drapes (0.2% vs. 0.8%; p = 0.036). While germs of the skin microbiome (like Staphylococcus epidermidis or aureus) were predominantly prevalent in both cohorts, faecal germs (like Enterococcus species or Enterobacter cloacae) were only found in the “control cohort” and not in the ‘study cohort’ using iodophor-impregnated adhesive incision drapes. Conclusion: The use of iodophor-impregnated adhesive incision drapes in spine surgery can help to lower the rate of postoperative SSI and aid to reduce the risk for faecal germ infections.
1269
RF027: Unmasking the menace: TB spine & the journey to recovery
Shah Alam 1 , Sarwar Jahan 2
1 Orthopedics & Spine Surgery, Bangladesh Spine & Orthopedic Hospital (BSOH), Dhaka, Bangladesh
2 Orthopedics & Spine Surgery, National Institute of Traumatology & Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
Introduction: TB spine is a common form of TB infection for 50% to 60% of osseous tuberculosis. The diagnosis of TB Spine is difficult and it commonly presents at an advanced stage. Delays in establishing diagnosis and management result in complications such as spinal cord compression and spinal deformity. Material and Methods: Total of 878 patients with tuberculosis of the cervical, thoracic and lumbar spine with moderate to severe cord compression were studied. Variable degrees of neurological deficit with deformity were treated from January 2003 to June 2023. Thoracotomy with fixation were done in 87 cases. Posterior decompression with stabilization by transpedicular screws and rods were done in 693 cases, whereas 98 cases of cervical tuberculosis were operated by either anterior approach or both anterior and posterior approaches. Appropriate anti TB drugs were given to all patients for 12-18 months. The follow-up period was 3 months to 10 years. Results: The average age was 47 (9-85) years. Superficial infections rate was 1.3% whilst 0.65% of deep infections. Revision surgery was performed in 1.94% patients. Implant failure occurred 2.7% whilst malposition of screws occurred in 3.4%. Perioperative excessive bleeding complications were reported for 0.6%. Neurological improvement occurred in all patients except for 2.5%. Conclusion: For patients with spinal tuberculosis anterior debridement, autograft bone fusion, anterior or posterior fixation appears to be effective in arresting disease, correcting kyphotic deformity and maintaining correction until solid spinal fusion.
1287
RF028: Instrumentation in children up to 5 years of age with spinal tuberculosis
Rajesh Kumar Chaudhary 1 , Deepak Kaucha 1 , Ram Barakoti 1 , Babu Shrestha 1
1 Orthopedics, Hospital and Rehabilitation Center for Disabled Children (HRDC), Banepa, Nepal
Introduction: Spinal Tuberculosis is still a common pathology encountered in developing countries. It is considered as medical disease which can be cured with antitubercular therapy (ATT). The risk of development and progression of deformity is higher in children due to several reasons. So, instrumentation may be required for stabilization and prevention of progression of deformity. The instrumentation in children is challenging because of poor bone stock, narrow pedicles, cartilaginous vertebra and poor soft tissue mass. So, patients may come with implant backout, breakage and prominence. This study aims to study the outcome of instrumentation in children up to 5 years of age with spinal tuberculosis. Materials/Methods: This is a retrospective study of all cases with spinal tuberculosis in children aged up to 5 years of age managed with ATT and instrumentation in Hospital and Rehabilitation Center for Disabled Children (HRDC) from December 2015 to August 2022. Medical records and X rays were reviewed. Level involved, deformity, neurological status, level of instrumentation, implants used and complications were recorded. Results: Total of 10 children aged up to 5 years with spinal tuberculosis were managed with spinal instrumentation during the specified duration. The mean age was 4.25 (ranged from 2-5 years). Four were boys and 6 were girls. Average follow up after surgery is 41.25 months (range 10-84 months). Dorsal spine was involved in 3 case, lumbar Spine in 2 cases and Dorso-lumbar spine in 5 cases. Posterior instrumentation only was done in 3 cases. Posterior instrumentation with anterior reconstruction with cage was done in 6 cases. Anterior reconstruction via anterior approach followed by short segment posterior instrumentation was done in 1 case. 4.5mm pedicle screws were used in 4 cases and 3.5 mm lateral mass screws were used as pedicle screws in 6 cases. All cases were treated with ATT for 12 months duration. 8 cases had excellent deformity correction and no progression of deformity. One case developed proximal junctional kyphosis which was revised later. One case developed mild progression of kyphosis. 3 cases out of four in which pedicle screws were used developed hardware prominence. Conclusion: Posterior instrumentation using pedicle screws in children aged up to 5 years is an effective armamentarium for prevention of deformity due to tubercular spondylitis. 3.5 mm lateral mass can be used as pedicle screws to avoid implant prominence.
311
RF029: A comparative factor analysis and new MRI scoring system for differentiating pyogenic vs tuberculosis spondylodiscitis
Kongtush Choovongkomol 1 , Terdpong Tanaviriyachai 1 , Patchara Pornsopanakorn 1
1 Department of Orthopedic Surgery, Maharat Nakhon Ratchasima Hospital, Nakhon Ratchasima, Thailand
Introduction: The differential diagnosis between Pyogenic and Tuberculous spondylodiscitis is crucial. Accurate diagnosis and early treatment are important to prevent further progression of disease and decrease patient morbidity. This study aims to compare and analyze the difference of clinical and magnetic resonance image (MRI) findings between pyogenic spondylodiscitis (PyS) and tuberculous spondylodiscitis (TbS). To develop and validate a simplified multi-parameter MRI-based scoring system for differentiating TbS from PyS. Material and Methods: We compared the predisposing factors of 190 patients (67 PyS patients and 123 TbS patients) whose confirmed diagnosis by laboratory, culture or pathology. The demographics, clinical characteristics, laboratory results, and MRI findings of the patients were collected between 2015 and 2020. The data were analyzed using logistic regression methods. The selected logistic coefficients were transformed into MRI-based scoring system. Internal validation was done with bootstrapping procedure. Results: In the univariable analysis, the significant risk factors associated with TbS were thoracic lesion, destroyed vertebral endplate and vertebral destruction > 50%, heterogeneous enhancement, vertebral intraosseous abscess, thin wall abscess and well-defined paravertebral abscess, subligamentous spreading, and epidural abscess. The multivariable analysis revealed that only thoracic lesion (OR = 819.81; 95%CI, 6.84-98313.95; p=0.006), no epidural phlegmon (OR = 900.86; 95%CI, 31.39 - 25857.73; p < 0.001), subligamentous spreading (OR = 185.78; 95%CI, 7.92 - 4360.64; p = 0.001), vertebral intraosseous abscess (OR = 19.59; 95%CI, 1.75 - 219.70; p = 0.016), well-defined paravertebral abscess (OR = 10.79; 95%CI, 1.28 - 90.80; p=0.029), epidural abscess (OR = 9.69; 95%CI, 0.78 - 121.06; p = 0.038) and no facet joint arthritis (OR = 7.25; 95%CI, 0.91 - 57.94; p = 0.042) were independent predictive factors for TbS. The potential predictors were used for derivation of the MRI scoring system. The total scores greater than or equal to 14 points can predict significantly probability of TbS with sensitivity 97.58% and specificity 92.54%. Conclusion: This simplified MRI-based scoring system for differentiating TbS from PyS were helpful to guide the appropriate treatment when the causative organism is not identified.
918
RF030: In-hospital mortality of spondylodiscitis - A single center experience
Ann Kathrin Joerger 1 , Carolin Albrecht 1 , Nicole Lange 1 , Bernhard Meyer 1 , Maria Wostrack 1
1 Neurosurgery, Technical University Munich, Munich, Germany
Introduction: Spondylodiscitis is a serious condition associated with high morbidity and mortality. Apart from patients with relatively mild course, there is a marked proportion of those who decease during the early stage of the disease despite the applied therapy. There is only sparse literature data on these severe cases. This study describes clinical data of patients with spondylodiscitis-related early mortality and attempts to identify risk factors. Material and Methods: We conducted a retrospective analysis comprising of consecutive patients’ data with spondylodiscitis treated between 01/01/2018 and 12/31/2022 at our high-volume Level I surgical spine center. We used simple logistic regression and multiple logistic regression analysis to identify risk factors for in-hospital mortality. Results: In total, 430 patients were included. 32 (7.4%) patients died during the same hospital stay after a median time of 28.5 days (2.0 – 84.0 days). Six out of these 32 (18.75%) patients were not treated surgically because they were in poor condition at admission or died prior to scheduled surgery. Five (16%) patients with early mortality were admitted in poor clinical condition requiring intensive care therapy. Identified causes for in-hospital death were multiorgan failure (n = 15), acute bone marrow failure (2), cardiac failure (4), liver failure due to cirrhosis (2), acute respiratory failure (2), acute renal failure (1) and concomitant oncological disease (1), respectively. In five cases a single reason could not be identified. Among patients with early mortality, the most prevalent sources of infection were joint empyema (21.9%), urosepsis (18.8%), and leg ulcers (15.6%). In contrast, the main focus in surviving patients was prior spinal surgery (29.4%). In a simple logistic regression analysis advanced age (p = 0.0006), diabetes mellitus (p = 0.0002), previous steroid medication (p = 0.0279), Charlson Comorbidity Index (p < 0.0001) and glomerular filtration rate (GFR) level at admission (p = 0.0008) were significant risk factors for in-hospital death. A multiple logistic regression analysis identified advanced age (p = 0.0038), diabetes mellitus (p = 0.0002) and previous steroid medication (p=0.0281) as significant risk factors, while BMI, CRP level at admission, history of malignant disease, substance abuse, hepatopathy, endocarditis, paraspinal abscess and intraspinal empyema were not significant. Conclusion: Even if admitted in a moderate clinical condition and if maximum medical treatment is applied immediately, a certain proportion of patients with spondylodiscitis deceases during the hospital stay. Special attention should be paid to the old patients and to patients with diabetes or steroid medication who harbor an elevated risk for a fulminant disease with fatal consequences.
1021
RF031: Single-stage debridement and reconstruction with trabecular metal cage for active infectious spondylodiscitis: a retrospective cohort study
Mingchi Kuo 1 , Fon-Yih Tsuang 2
1 Surgery, National Taiwan University Hospital Yun Lin Branch, Yunlin County, Taiwan
2 Neurosurgery Division, Department of Surgery, National Taiwan University Hospital, Taipei, Taiwan
Introduction: Early debridement and stabilization for pyogenic spondylodiscitis allow early mobilization of the patient and prevent subsequent spinal deformity. Tantalum (Ta) trabecular metal (TM) components have several potential advantages over conventional implant materials, such as its uniformity and structural continuity, and enhancing the host defense mechanism by increasing leukocyte chemotaxis, phagocytosis, and the bacterial killing rate. A single-stage surgery with a tantalum trabecular metal cage combining two different approaches is sufficient to maintain vertebral stability. Material and Methods: This was a retrospective study of spondylodiscitis patients who underwent surgery between January 2018 and March 2021 in our tertiary academic teaching hospital. We examined patient demographic data, including age and sex, as well as symptoms, laboratory results, neurological examination, radiographic images, operative reports, postoperative complications, and data from clinical and radiological follow-up. We evaluated the CRP data during therapy. In all patients, blood tests for CRP levels were obtained 3 days before surgery as baseline data. Further blood chemistry controls in all patients were performed after surgery. Results: We included 7 spondylodiscitis patients who underwent surgery. Out of 57 patients, 31 (54%) patients were treated with single-stage debridement and reconstruction with trabecular metal cages, and 26 (45.6%) patients received spine surgery without trabecular metal cages. All 31 cases were reconstructed with a Zimmer Biomet Trabecular Metal™ cage, and thoracolumbar spine cases were all combined with posterior pedicular screw fixation. At the latest follow-up, spinal deformity had been averted, and preexisting spinal deformities were partially rectified in all instances. Among the cases, five patients initially exhibited neurological deficits that ameliorated post-surgery. In the remaining 26 patients, spinal pain demonstrated greater responsiveness to analgesic treatment after vertebral stabilization, resulting in improved back pain or radicular pain during the follow-up period. Two patients experienced progression of spondylodiscitis necessitating intervention subsequent to the initial surgery. The follow-up duration ranged from 5–33 months with an average of 15 months. Notably, none of the patient developed new-onset neurological deficits after surgical procedure. The level of CRP data was lower in the TM cage group at three different times (before surgery, postoperation Days 0-3, postoperation Days 22-28). The CRP values dropped borderline significantly in the TM cage group compared with the non-TM cage group postoperatively. Conclusion: In patients with spondylodiscitis, it is advisable to perform single-stage debridement and reconstruction with a trabecular metal cage, which allows abscess drainage and rapid mobilization, prevents deformity.
1669
RF032: New silver-coated instrumentation for spinal procedures to counteract surgical infection: preliminary clinical outcomes
Silvia Terzi 1 , Lucrezia Leggi 1 , Maria Sartori 2 , Francesca Salamanna 2 , Luca Boriani 1 , Emanuela Asunis 1 , Giovanni Barbanti Bròdano 1 , Gianluca Giavaresi 2 , Alessandro Gasbarrini 1
1 Spine Surgery
2 Surgical and Technological Sciences, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Infection is one of the most concerning complication following spinal surgery, with instrumented procedures carrying infection rates ranging from 2% to 20%. This retrospective study aimed to assess the efficacy of newly developed titanium instrumentations coated with silver ion nanoparticles in treating and preventing the recurrence of spinal infections following instrumented surgery. Material and Methods: To evaluate the effectiveness of these new instruments in preventing infection recurrence, we conducted a retrospective observational study (Ethical Committee under Authorization n°232/2021/Oss/IOR). The study included patients who underwent thoraco-lumbo-sacral arthrodesis and received silver-coated instrumentation during revision surgery for post-operative surgical site infection (SSI) between 2018 to 2021, excluding those patients treated for primary infection (spondylodiscitis). We retrospectively evaluated patients who received silver-coated instrumentation. We examined pre-operative, intra-operative and post-operative variables focusing on SSI-related outcomes, and the efficacy of silver instrumentation in preventing late SSI recurrence. Results: Thirty-seven patients met the study's inclusion criteria with a mean age of 61.27 ± 11.67, (20 males and 17 females). Among these patients, 2 experienced infection recurrence within 30 days, with one case requiring the instrumentation revision. Of the remaining 35 patients, 2/35 (6%) required silver instrumentation revisions due to mechanical issues, specifically screw mobilization and bars breakage. In 2/35 (6%) cases, instruments revision became necessary due to wound dehiscence and a significant resurgence of infection around the implanted devices, ultimately leading to their removal. In 3/35 cases (8%), wound dehiscence occurred but was successfully managed with surgical site debridement without instrumentation revision. Therefore, when combined with appropriate antibiotic therapy targeting the pathogenic strains responsible for the infections, the use of silver instrumentation effectively controlled late infection recurrence in the analyzed case series. Conclusion: SSI remains a significant concern in spine surgery causing distress for both patient and surgeons. Based on our findings, the use of silver instrumentation appears to offer promising results in terms of infection control, with a revision rate consistent with the existing literature on similar surgical techniques.
533
RF033: A clinical prediction model to differentiate tuberculous spondylodiscitis from pyogenic spontaneous spondylodiscitis
Thamrong Lertudomphonwanit 1 , Chirtwut Somboonprasert 1 , Kittiphon Lilakhunakon 2 , Sasivimol Rattanasiri 1 , Siriorn Watcharananan 1 , Pongsathorn Chanplakorn 1
1 Orthopedic, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok
2 Orthopedic, Roi et Hospital, Roi et, Thailand
Introduction: Microbiological diagnosis of tuberculous spondylodiscitis (TS) and pyogenic spontaneous spondylodiscitis (PS) is sometime difficult. This study aimed to identify the predictive factors for differentiating TS from PS using clinical characteristics, radiologic findings, and biomarkers, and to develop scoring system by using predictive factors to stratify the probability of TS. Material and Methods: A retrospective single-center study. Demographics, clinical characteristics, laboratory findings and radiographic findings of patients, confirmed causative pathogens of PS or TS, were assessed for independent factors that associated with TS. The coefficients and odds ratio (OR) of the final model were estimated and used to construct the scoring scheme to identify patients with TS. Results: There were 73 patients (51.8%) with TS and 68 patients (48.2%) with PS. TS was more frequently associated with younger age, history of tuberculous infection, longer duration of symptoms, no fever, thoracic spine involvement, 3 vertebrae involvement, presence of paraspinal abscess in magnetic-resonance-image (MRI), well-defined thin wall abscess, anterior subligamentous abscess, and lower biomarker levels included white blood cell (WBC) counts, erythrocyte-sedimentation-rate (ESR), neutrophil fraction, and C-reactive protein (all p < 0.05). Multivariate logistic regression analysis revealed significant predictors of TS included WBC 9,700/mm3 (odds ratio [OR] 13.11, 95% confidence interval [CI] 4.23-40.61), neutrophil fraction 78% (OR 4.93, 95% CI 1.59-15.30), ESR 92 mm/hr (OR 4.07, 95% CI 1.24-13.36) and presence of paraspinal abscess in MRI (OR 10.25, 95% CI 3.17-33.13), with an area under the curve of 0.921. The scoring system stratified the probability of TS into three categories: low, moderate, and high with a TS prevalence of 8.1%, 29.6%, and 82.2%, respectively. Conclusion: This prediction model incorporating WBC, neutrophil fraction counts, ESR and presence of paraspinal abscess accurately predicted the causative pathogens. The scoring scheme with combination of these biomarkers and radiologic features can be useful to differentiate TS from PS.
1171
RF034: Spinal brucellosis - A diagnostic enigma with our institutional protocol
Vishnu Senthil Kumar 1
1 Orthopaedics, Government Royapettah Hospital, Chennai, India
Introduction: In developing countries, Spinal brucella is often neglected and is a diagnosis of exclusion. Importance of our study is to establish an algorithm for management of spinal brucellosis. Materials and Methods: Study performed in the Dept of Orthopaedics of a Tertiary care hospital. Sample size of 25 confirmed cases with a minimal follow up of 24 months. Inclusion criteria included patients with osteo-articular brucellosis, culture positive or positive agglutination test. Non brucella spondylodiscitis were excluded from the study. Treatment algorithm included antibiotics for 10-12 weeks, injectable aminoglycosides streptomycin or gentamycin for 2 weeks along with oral rifampicin 600 mg BD for 8-10 weeks and oral doxycycline 100mg bd for 10-12 weeks. All patients were serially followed up to ensure clearance of disease with relevant investigations. Stabilization and fusion was performed in 9 cases involving bone destruction with sensory/motor deficit. Results: Mean age was 52.16 ± 12.53 yrs, SSC grading of patients showed 4 patients in grade 1, 12 patients in grade 2 and 9 patients belonged in grade 3 at presentation. NRS for back pain (Pre- 6.55, post -2.14, p < 0.001) ESR (Pre -38.5, post -24.25, p = 0.017), CRP (Pre -39.99, Post -7.78, p = 0.004). Brucella agglutination titres (p < 0.001) and radiological outcomes improved statistically by 6 months. Treatment duration was individualized with mean duration of 11.42 ± 2.66 weeks. Mean follow up was 14.42 ± 8 months. Limitation: Small sample size, long term follow-up needed. Our study concentrated more on the spinal manifestations of the brucellosis taking into severity grading. We recommend validation of our treatment algorithm with high volume studies with sufficient follow up for widespread acceptance. Conclusion: High index of suspicion of patients from endemic regions, proper clinical assessment, serological evaluation, radiological assessment, appropriate decision making and regular follow up of patients is the key in comprehensive management of spinal brucellosis.
2043
RF035: Percutaneous pedicle screw fixation for patients with tuberculosis spondylitis of the thoracolumbar spine: a comparative study
Benjeddou Wassim 1 , Khalil Habboubi 1 , Amine Chabchoub 1 , Meddeb Mehdi 1 , Hassen Makhlouf 1 , Mondher Mestiri 1
1 Adults, Med Taieb Kassab Institute, Mannouba, Tunisia
Introduction: The primary approach to treating tuberculosis spondylitis traditionally involves conservative care. However, prolonged bed rest, inadequate pain management, and worsening infection have led to various complications in many cases, prompting the need for surgical interventions when conservative treatments fail. Recent research has highlighted percutaneous pedicle screw fixation as a promising technique to alleviate immediate pain, reduce the morbidity associated with extended bed rest, and improve pain control. In this study, we conducted a comparative analysis between a conservative treatment group and a percutaneous pedicle screw fixation group for patients who initially exhibited resistance to treatment, aiming to assess the impact of percutaneous pedicle screw fixation in managing tuberculosis spondylitis cases unresponsive to initial treatment. Material and Methods: We retrospectively reviewed 54 consecutive patients treated for tuberculosis spondylitis at our hospital between 2005 and 2022, with follow-up periods of at least 12 months. Patients who responded effectively to initial treatment (defined as experiencing fever relief and a C-reactive protein (CRP) decrease within three weeks of intravenous antibiotics) were excluded from the study. As a result, our retrospective analysis focused on 29 cases demonstrating initial treatment resistance. To assess the effects of percutaneous pedicle screw fixation, these cases were divided into two groups: the conservative group (17 cases) and the percutaneous pedicle screw group (12 cases). Since 2016, percutaneous pedicle screw fixation has been increasingly favored, although patients with compromised general health have typically received conservative treatment. Results: We examined the time interval between the initial hospital visit and the achievement of fever relief, CRP normalization, ambulation, discharge, or transfer. While no statistically significant differences were observed in terms of fever relief (p = 0.051) or CRP normalization (p = 0.208), the percutaneous pedicle screw group experienced significantly shorter periods to ambulation (p = 0.020) and discharge or transfer (p = 0.031). Outcomes were assessed at the 12-month mark following treatment initiation, discharge, transfer, or death. In the percutaneous pedicle screw group, one patient succumbed to intestinal obstruction, resulting in a 92% one-year survival rate. In the conservative group, five patients passed away due to various reasons, including infarction-sepsis (3 cases), acute myocardial infarction (1 case), and unknown causes (1 case), resulting in a 71% one-year survival rate. Although the percutaneous pedicle screw group exhibited a relatively higher one-year survival rate, no statistically significant difference was observed between the two groups (p = 0.354). The discharge rate to home or care facilities was 58% in the percutaneous pedicle screw group and 47% in the conservative group, while the transfer rate was 33% in the percutaneous pedicle screw group and 35% in the conservative group. Conclusion: Our study demonstrates that percutaneous pedicle screw fixation effectively reduces the time required for ambulation and discharge or transfer in patients with tuberculosis spondylitis who initially demonstrated treatment resistance. However, it did not significantly impact infection control indicators such as fever relief and CRP normalization. These findings suggest that percutaneous pedicle screw fixation should be considered as an aggressive treatment option for patients who can anticipate pain relief and early ambulation, particularly in cases of tuberculosis spondylitis resistant to initial treatments.
498
RF036: Can X-rays justify going under the knife? A study of functional outcomes of conservatively managed lumbar spine tuberculosis in a tertiary care centre
Arjit Vashishtha 1 , Tushar Rathod 1
1 Orthopaedics, Seth G.S.M.C. and K.E.M. Hospital, Mumbai, India
Introduction: Lumbar spine tolerates tuberculosis relatively better than dorsal spine as the weight bearing axis passes posterior to it preventing collapse and the wider diameter of spinal canal as compared to dorsal spine prevents neurological deficit. Considering the above-mentioned statements, conservative management of lumbar spine tuberculosis is warranted except in cases presenting with dense neurological deficits like Conus medullaris or Cauda Equina syndrome. This study aims to evaluate co-relation between radiological parameters of lumbar spine in sagittal plane such as segmental kyphosis and lumbar lordosis and the functional outcome in the patients treated conservatively with anti-tubercular drugs. Material and Methods: 34 patients of lumbar spine tuberculosis presenting without any neurological deficits, which were conservatively managed by anti-tubercular drugs after microbiological diagnosis of tuberculosis were evaluated clinico-radiologically at serial intervals from the beginning of treatment till the time the disease is healed. Functional outcomes were assessed by Oswestry Disability Index and radiologically by roentgenograms of lumbar spine in lateral views and sagittal spinal parameters, i.e., Segmental kyphosis and Lumbar Lordosis were calculated. Results: All 34 patients responded to the conservative management both clinically and radiologically. Oswestry disability index at the time of initial presentation ranges from 96% to 10% with a mean value of 66.9% which significantly improved to a mean value of 9.1% after the disease is healed. Similarly, mean values of segmental kyphosis at the initial presentation were 8.6° which progresses to 13.0° till the disease gets healed and bony ankylosis takes place between adjacent vertebrae. Mean lumbar lordosis at initial presentation is 25.9° as compared to 24.0° at the time of healed disease. Conclusion: There seems to be no co-relation between the degree of residual kyphosis and the functional outcome in conservatively managed lumbar spine tuberculosis. Due to the normal functioning adjacent motion segments, the segmental kyphosis is thought to be well compensated, thus lumbar lordosis in not significantly affected. This study highlights that the conservative management of lumbar spinal tuberculosis has an optimal functional outcome in-spite of segmental kyphosis. Thus, it warrants the need for review of the general application of sagittal parameters designed for degenerative spine pathologies while deciding conservative or operative treatment.
RFP03: Thoracolumbar Trauma
1365
RF037: Inter-observational analysis of computed tomography parameters to predict posterior ligament complex injury in thoracolumbar trauma
Joana Araújo de Azevedo 1 , Carolina Martins 2 , Tiago Barbosa 1 , André Santos Moreira 1 , Nuno Oliveira 1 , Pedro Varanda 1 , Bruno Direito Santos 1
1 Ortopedia e Traumatologia, Hospital de Braga, Portugal
2 Escola de Medicina, Universidade do Minho, Portugal
Introduction: Posterior ligamentous complex (PLC) is one of the most important predictors of instability in thoracolumbar fractures (TLF) and Magnetic Resonance Imaging (MRI) is the gold standard to evaluate it. Therefore, improving the accuracy of computed tomography (CT) in the diagnosis of PLC injury is essential to expedite the clinical decision regarding TLFs. The purpose of this study is to assess computed tomography diagnostic accuracy in detecting PLC injury in patients with acute TLF using combined parameters, comparing with MRI and generate a reproducible score to predict PLC injury. Material and Methods: Retrospective, observational and analytical study, including all consecutive patients with acute traumatic TLF without exclusion criteria and submitted to CT and MRI within 72 hours. 12 CT parameters were analyzed independently by four investigators and PLC integrity was observed in MRI. We measured interrater reliability of all 12 parameters and compared between patients with or without PLC injury on MRI. Using the coefficients (ß) of the multivariate logistic regression we created two risk scores to predict PC injury in CT. Results: 154 patients were included, of which 62 with PLC injury. PLC injury was detected in 40.3%. Interrater reliability was excellent in almost all parameters. Horizontal Fracture of the lamina or pedicle (HLPF), Spinous process fracture (SPF) and Interspinous Distance Widening (IDW) positive are associated with PLC injury. Risk scores to estimate PLC injury detected in the MRI had a total of 75.9% of correct classifications (p < .001). Risk score 2 included only statistically significant variables and has sensitivity of 71.0% and specificity of 78.3%. Conclusion: Standardized measurement procedure with well-defined definitions in CT images’ evaluation is effective. Close attention should be given to HLPF, SPF and IDW when analyzing CT images of TLF. Risk score 2 is easy to apply and can be helpful in treatment decision in facilities without available MRI.
602
RF038: Early versus late surgical fusion for gunshot-related spinal fractures: a propensity-score matched analysis
Dario Marotta 1 , Sam Jiang 1 , Zayed Almadidy 1 , Mounika Bhaskara 1 , Morteza Sadeh 1 , Ankit Mehta 1
1 UI Health Department of Neurosurgery, The University of Illinois at Chicago, Chicago, USA
Introduction: Gunshot wounds (GSW) are a common cause of injury in the USA that cause life-threatening complications such as hemorrhage, pneumothorax, and sepsis. Unstable spinal fractures can occur, however, definitive treatment is often deferred until after the life-threatening injuries are addressed. There currently lack definitive guidelines for the optimal timing of surgical fusion in this setting. As such, this study aims to compare the short-term outcomes of early vs. late surgical fusion for adult spinal fractures following GSW. Methods: The American College of Surgeons National Trauma Data Bank was queried from 2017-2019 for all patients with a spinal fracture at any level with GSW as the primary cause. Patients < 18, who died in the emergency department, had missing surgical timing data, or had lengths of stay greater than 12 days were excluded. Early surgery was defined as surgery within 48 hours upon arrival and late surgery was defined as surgery after 48 hours. This threshold was determined using the median cohort value rounded to the nearest day. The cohort was sampled to ensure equal match and propensity-score matching was performed between patients who received early vs. late fusion based on patient characteristics, injury severity, and fracture level. A sampling ratio of 0.8 was chosen iteratively to maximize the cohort size while eliminating post-match baseline group differences. Differences between the two groups in treatments and outcomes were compared using Student’s t-tests and Pearson’s chi-square tests. Result: A total of 360 patients matching the inclusion and exclusion criteria identified with 182 undergoing early fusion and 178 undergoing late fusion. At baseline, the early surgery group had a higher rate of diabetes (4.95% vs. 1.12%, p = 0.04) and was more likely to have unspecified insurance (1.10% vs. 4.49%, p = 0.05). The groups also differed significantly in the spinal levels involved and subsequent levels fused. Following sampling and propensity score matching, 142 patients in each group were identified and all baseline differences were eliminated. Compared to the late fusion group, the matched early fusion group had a shorter length of stay (LOS; 20.09 days vs. 26.66 days, p = 0.02) and lower rate of pressure ulcers (2.82% vs. 14.08%, p < 0.001). Otherwise, there were no significant differences in mortality, intensive care unit LOS, other hospital complications, or discharge disposition. Conclusion: This is the first study to date to evaluate early vs. late fusion for spine fractures associated with GSW. Fusion within 48 hours was associated with reduced LOS with no increase in in-hospital complications or worse discharge disposition. The reduced LOS of nearly one week associated with early surgery may expedite the recovery process as well as reduce costs to the healthcare system due to unnecessary hospitalization. These results represent a step towards developing comprehensive guidelines for neurosurgical spine care in GSW-related spinal fractures.
980
RF039: Surgical outcomes of balloon kyphoplasty combined with posterior spinal fixation for osteoporotic vertebral fracture concomitant with posterior wall injury - Time course of spontaneous canal remodeling with posterior wall injury
Masaaki Chazono 1 , Naomu Sawada 1
1 Orthopaedic Surgery, NHO Utsunomiya Hospital, Utsuonomiya, Tochigi, Japan
Introduction: Japan currently has the most aged population amongst the industrial countries because the elderly population more than 65 years of age accounts for 30% of the population in 2022. Balloon kyphoplasty (BKP) is widely used for a popular surgical treatment for osteoporotic vertebral fractures (OVFs), but in our department, BKP combined with posterior spinal fixation is generally performed for OVF pseudoarthrosis of burst fracture type with spinal cord and/or nerve root compression while vertebral body height is maintained. There have been little detailed studies on the change in the bone fragment remodeling in the spinal canal in this technique. In this study, we report on the surgical outcomes mainly in cases of intraspinal canal remodeling of bone fragments with posterior vertebral wall injury. Material and Methods: The subjects were 20 patients (5 males and 15 females) who underwent BKP + posterior spinal fixation without decompression at our department, with a mean age at the time of surgery of 79 years (72-86), and the injured vertebrae were T10: 1 case, T11: 2 cases, T12: 3 cases, L1: 7 cases, L2: 2 cases, L3: 3 cases, L4: 2 cases, with a mean postoperative follow-up period was 1 year and 11 months. The following items were examined: operative time, intraoperative blood loss, perioperative complications, and improved Frankel classification before and after surgery; radiological examination included preoperative, immediate postoperative, and final follow-up measurements of the collapsed rate of the injured vertebra and the local kyphosis angle in the thoracolumbar spine OVF excluding L3 and L4. The relationship between the number of fixed vertebrae and PS loosening was also investigated. Upon CT evaluation, the area of bone fragments in the spinal canal (A) and the relevant area of the spinal canal (B) were measured from PACS images based on axial images at the level that protruded most into the spinal canal in sagittal images, and the occupancy rate of bone fragments in the spinal canal (C) was calculated as A/B X 100 (%). The remodeling rate (immediate postoperative C- final follow-up C) / (immediate postoperative C) X 100 (%) was also evaluated. Results: The mean operative time was 199 minutes, the mean intraoperative blood loss was 309 ml, and superficial SSI occurred in only one case. All but one patient had Frankel E paralysis at the final follow-up period. The mean number of fixed vertebrae was 4.2, and PS loosening was not significantly correlated with the lowest instrumented vertebra (LIV) in all 9 cases. The mean intraspinal canal fragment occupancy improved to 26%, 20.3%, and 14.4% at preoperatively, immediately postoperatively, and final follow-up period, continuing the remodeling progression over time. The average intraspinal canal remodeling rate was 36.7%, but it varied from case to case. Conclusion: BKP combined with posterior spinal fixation for OVF pseudarthrosis with burst fracture is a less invasive procedure that can be applied to late-onset elderly patients with the expectation of spontaneous canal remodeling over time.
2524
RF040: Reliability and validity of the Arabic version of the AO Spine PROST (Patient Reported Outcome Spine Trauma)
Mohamed Hassanien 1 , Mirette Aziz 2 , Mohammad El-Sharkawi 1
1 Department of Orthopaedic and Trauma Surgery
2 Department of Public Health and Community Medicine, Faculty of Medicine, Assiut University, Assiut, Egypt
Background: Assessment of the quality of life and measurement of the outcome of the management options after injuries are important issues nowadays. It is difficult to quantify the effect size of various treatment choices in the absence of an outcome instrument particularly established and validated for traumatic spinal column injury patients. The AO Spine Knowledge Forum Trauma supported a project that resulted in the development of the AO Spine PROST (Patient Reported Outcome Spine Trauma), which consists of 19 items. The Arabic language, the official language in more than 25 countries over the world, is spoken by more than 475 million people globally, which makes it the 5th most commonly used language in the world after the English, Mandarin, Hindi, and Spanish. The aim of this work is to translate and adapt the AO Spine PROST into Arabic and test its psychometric properties among Egyptian and Arabic-speaking spine trauma patients. Materials and Methods: This validation study was performed on 245 spine trauma patients presenting for follow up in the outpatient clinic of the Orthopeadic and Trauma Surgery Department, Assiut University between May 2020 and June 2021. The criterion validity was assessed by comparing the responses of 149 patients to the Arabic version of the AO spine PROST with the Arabic version of the Oswestry disability index. The construct validity was assessed using known-groups comparison to test for hypothesized differences concerning sociodemographic variables. Patient characteristics were analyzed using descriptive statistics. Content validity was determined by looking at floor and ceiling effects. Internal consistency was measured using Cronbach's alpha and item-total correlation coefficients (ITCC). AO Spine PROST items were subjected to Spearman correlation tests, which were compared to the Oswestry disability index. Test-retest reliability was assessed by another 80 patients. Results: Using established principles, the AO Spine PROST was translated and adapted into Arabic. Two hundred twenty-nine patients (93.4%) of the 245 patients enrolled satisfied the inclusion criteria and supplied sufficient data, and 16 patients were excluded (due to missing data). Content validity showed good results, and no floor and ceiling effects were seen. The internal consistency was excellent (Cronbach’s α = 0.99; ITCC 0.50-0.90) as well as test-retest reliability (ICC = 0.994). Spearman correlations were good (0.59-0.95). The strongest correlations of AO Spine PROST with ODI were seen with the physical components (0.69-0.95; p < 0.001). However, the sleeping pattern and pain showed poor correlation (-0.083 and 0.192). This may be explained as sleeping and pain have many other factors that may affect it. Conclusions: The validity and reliability of the Arabic version of the AO Spine PROST were satisfactory. It is thought to be a useful tool that has the ability to help resolve existing debates in the field of spine trauma management.
Keywords: validity; spine trauma; AO Spine PROST; health-related quality of life
RF041 (2437 FYI: This abstract is in the program but due to copyright issue, cannot be published)
2542
RF042: Incidence of hidden injuries in patients with thoracic spine fractures: a descriptive observational study
Oscar Bravo 1 , Guillermo Izquierdo 1 , Jose Varas 1 , Ignacio Acuña 1
1 Traumatologia Columna, Hospital Clnico Mutual de Seguridad de Santiago, Santiago, Chile
Introduction: Thoracic spine fractures are defined as any fracture of the T1 to T10 vertebrae (inclusive). These fractures are complex due to the rigidity, narrow spinal canal, and the presence of the spinal cord. The gold standard for their evaluation is Computed Tomography (CT) due to its high sensitivity and specificity in detecting fractures and their classification. The complementary use of Magnetic Resonance Imaging (MRI) is justified by its high sensitivity and specificity in studying the spinal cord, posterior ligament complex injuries, and soft tissue lesions. Additionally, MRI can detect associated injuries, which has been the focus of a limited number of studies. Achieving a cost-effective study would help prevent the overuse of imaging and facilitate timely treatment optimization of resources. Therefore, a descriptive observational study of patients with thoracic fractures is proposed to measure the incidence of hidden fractures and/or posterior ligament complex injuries using MRI. Materials and Methods: Retrospective descriptive observational design. We evaluated 113 patients diagnosed with thoracic fractures between 2015 and 2023. Patients with a complete imaging study and preoperative neurological evaluation were included. Patients with previous spinal surgery, fractures in pathological bone, and delayed consultation exceeding 3 weeks were excluded. One observer analyzed the images, and the data were recorded in a database. A descriptive analysis of demographic variables, injury mechanisms, fracture characteristics, and findings from both CT and MRI was performed. Results: Of the patients, 91.15% were male and 8.84% were female, with an average age of 44.2 years (range 21-81, SD 15.32 years). The mechanism was primarily high-energy (90.26%), with motorcycle accidents being the most common (30.35%), followed by car accidents at 23.21%. The frequencies of type A, B, and C fractures were 69.91%, 28.31%, and 1.76%, respectively, and the time between CT and MRI was 4.62 days (range 0-46, SD 7.42 days). Ligament injury was suspected in CT in 38.05% of cases and was confirmed by MRI in 83.72% compared to 27.14% where there was no suspicion. Hidden injuries were found in 74.33% of cases on MRI, mainly consisting of bone edema (52.21%), with 46.90% being contiguous, and interspinous edema (48.67%). Additionally, vertebral fractures were found in 9.73%, yellow ligament injury in 5.30%, and supraspinous ligament injury in 7.07%. MRI resulted in a change in fracture classification in 4.42% of cases. Conclusions: While MRI is a valuable tool for a better understanding of the involvement of soft tissues in thoracic spine fractures, given the characteristics of this segment and the findings that can be obtained from CT, it does not provide additional information for classifying and determining injuries that might warrant a change in treatment approach. However, further studies are needed to better understand the limitations of these images and their true indications.
1641
RF043: The use of percutaneous stent-kyphoplasty (SpineJack®) in thoracolumbar fractures: A retrospective analysis of 331 implants from a Level-1 Trauma center in Switzerland
Magdalena Karner 1 , Osterhoff Georg 2 , Kai Sprengel 1,3 , Hans Christoph Pape 1 , Julian Scherer 1,4
1 Traumatology, University Hospital of Zurich, Zurich, Switzerland
2 Department of Orthopedics, Trauma Surgery and Plastic Surgery, University Hospital of Leipzig, Leipzig, Germany
3 Hirslanden Clinic St Anna, University of Lucerne, Lucerne, Switzerland
4 University of Cape Town, Cape Town, South Africa
Introduction: Vertebral compression fractures (VCFs) are common fractures, most often caused by low-energy trauma due to osteoporotic changes and high-energy trauma in adolescents. There is no international consensus on the treatment algorithm in VCFs. However, rapid pain-relief and mobilization should be achieved to decrease associated morbidities and mortality. The newly introduced SpineJack®-system has been advocated to be a suitable treatment option in osteoporotic (OVFs) and traumatic VCFs (tVCF). Thus, the aim of this study was to analyze the safety and efficacy of the SpineJack®-system regarding clinical outcomes and peri- and postoperative complications. Material and Methods: All patients with vertebral fractures who were treated with the SpineJack®-system from November 2014 to December 2022 were assessed. In total, 331 implants were analyzed. Demographics, fracture characteristics (AOSpine and OF-classification), clinical parameters such as pVAS and Lenghts of Stay (LoS), surgical procedures and complications were analyzed. Sub-group analysis was performed for tVCF versus osteoporotic vertebral fractures (OVFs). Results: Most of the assessed implants were from male patients (54.7%) and the mean age was 61.6 years (range 16 to 93 years, SD 17.8). Most fractures were seen in the lumbar region (56.8%). Most of the fractures were OVFs (n = 157), followed by tVCFs (n = 153) and malignant (primary tumor, metastasis or spondylodiscitis) fractures (n = 21). Most fractures were due to low-energy trauma (54.7%) predominantly assessed in female patients (66.0%), (p ≤ 0.001). One third (31.7%) underwent additional dorsal instrumentation, with a significant higher rate in patients with high-energy trauma (54.7%, p ≤ 0.001). The most often seen OVFs were OF 4 (35.7%) and OF 2 (35.0%). In the traumatic fracture group, we assessed A3 (41.2%) and A4 (27.5%) predominantly. The mean age was significantly lower in the tVCF group (49.6 y, SD 16.4 versus 73.3 y, SD 10.5, p ≤ 0.01) and more high-energy trauma occurred in the tVCF group (96.7% versus 0.6%, p ≤ 0.01). There was no difference in the affected spinal level between the groups and only five patients in each group showed neurological impairment at admission. More tVCFs were treated with additional instrumentation (n = 81, 27.2% B-type injury vs. n = 21, 61.9% OF 4 and OF 5, p < 0-001), whereas more OVFs were treated with additional vertebroplasty or balloon-kyphoplasty (n = 59, vs. n = 21, p < 0-001). The mean surgery duration of stand-alone SpineJack® procedures was 33.76 minutes (SD 22.77), (SpineJack® + Instrumentation: 131.40, SD 72.59). Higher pain reduction was detected in OVFs (mean 4.16, SD 2.58) compared to traumatic VCFs (mean 3.34, SD 2.73) between admission and first postoperative day. (p = 0.039) In 8.8%, intraoperative cement leakage was detected. Surgical site infection was assessed in four fractures (1.2%) of which 50% occurred in patients with additional instrumentation. OVFs showed shorter LoS (4.97 vs. 7.02 days, p = 0.012). There was no difference regarding mean opioid intake duration between the subgroups (p = 0.095, tVCFs 5.32 days vs. OVFs 3.93 days). Conclusion: The SpineJack®-system seems to be a viable option for treating OVFs and tVCFs with short (stand-alone) procedure durations, low complication rates and sufficient pain reduction. Further assessments regarding height-restoration, kyphotic angulation and clinical long-term follow-up shall be conducted from this cohort.
1314
RF044: Association of various types of facet diastasis with thoracolumbar posterior ligamentous complex injury
Mohamed Ali 1
1 Neurosurgery, Prince Mohamed Bin Abdelaziz Hospital, Riyadh, Saudi Arabia
Background: The association of various morphological features of facet diastasis with (posterior ligamentous complex) PLC injury has not been described. Objective: To determine the diagnostic value of facet diastasis subtypes for diagnosing thoracolumbar PLC injury. Methods: We retrospectively reviewed 337 consecutive patients with acute thoracolumbar fractures. Three and five reviewers evaluated MRI and CT images, respectively. Facet diastasis was subclassified as follows: Dislocated - no articular surface apposition, subluxed - incomplete articular surface apposition; Facet fracture - articular-process fractures which may be displaced > 2 mm vs. non-displaced, Facet joint widening > 3 mm (FJW). We examined the diagnostic accuracy and the multivariate associations of facet diastasis subtypes with PLC injury in MRI. Results: Facet dislocation, subluxation, and displaced facet fracture yielded a high PPV for PLC injury (96%, 89%, and 93%, respectively). In contrast, undisplaced facet fracture and FJW yielded a moderately high PPV for PLC injury (78%, and 45%, respectively). Facet dislocation, subluxation, and displaced facet fracture showed independent associations with PLC injury (AOR = 34.5, 16.8, 11.8, respectively; p < 0.05) wheras undisplaced facet fracture and FJW were not (OR = 4.5, p = .62 and OR = 1.0, p = .96, respectively). Conclusions: Facet dislocation, subluxation, and displaced facet fracture, but not undisplaced facet fracture or FJW, were independently associated with PLC injury. Therefore, we propose to define facet diastasis as a surrogate marker of PLC injury in MRI based on these morphologies.
Keywords: posterior ligamentous complex; fact diastasis; computed tomography; thoracolumbar fractures; AOSpine Classification
2186
RF045: Risk factors for insufficient reduction of intracanal fragment after short-segment posterior fixation for thoracolumbar burst fractures
Hiroyuki Aono 1 , Okuda Akinori 2 , Shota Takenaka 3 , Takeshi Kikuchi 4 , Hiroshi Takeshita 5 , Keiji Nagata 6 , Yasuo Ito 4
1 Orthopedic Surgery, Osaka National Hospital, Osaka
2 Orthopedic Surgery, Nara Medical University Hospital, Kashihara, Japan
3 Orthopedic Surgery, JCHO Osaka Hospital, Osaka, Japan
4 Orthopedic Surgery, Kobe Red Cross Hospital, Kobe, Japan
5 Orthopedic Surgery, Saiseikai Shiga Hospital, Ritto, Japan
6 Orthopedic Surgery, Wakayama Medical University Hospital, Wakayama, Japan
Introduction: Many surgeons have encountered patients who could not immediately undergo surgery to treat spinal fractures because they had associated injuries. For such patients, practitioners might assume that delays could mean that the eventual reduction would be insufficient. However, no report covered risk factors for insufficient reduction of intracanal fragment in the treatment for thoracolumbar burst fracture. Materials and Methods: The purpose of this study is to investigate the risk factors for insufficient reduction of intracanal fragment after short-segment fixation for thoracolumbar burst fractures. Our multicenter study included 241 patients who sustained a single traumatic acute thoracolumbar burst fracture and underwent short-segment fixation. We measured canal compromise ratio (CCR) of intracanal fragment on CT before and after surgery, and then calculated the reduction rate of the fragment by using the following formula: (Preoperative CCR − Postoperative CCR)/Preoperative CCR × 100. A multiple logistical regression analysis was performed to identify risk factors for insufficient reduction of intracanal fragment. The factors that we evaluated were age, gender, affected spine level, time elapsed from injury to surgery, inclusion of vertebroplasty with surgery, load-sharing score (LSS), AO classification (type A3.A4 or B1.B2), and preoperative CCR. Results: There were 132 male and 109 female patients, with an average age of 44 years, and the mean time elapsed between injury and surgery was 3.8 days. For fixation, we used Schanz pedicle screw system in 84% of the patients. Combination of vertebroplasty was performed in 114 patients. Mean preoperative CCR was 42% and improved to 24% after surgery. The mean LSS was 6.4 points. Multiple linear regression analysis revealed that T12 and L1 fracture and AO type B fracture had better reduction rate compared to L2 and L3 fracture and AO type A fracture. The time elapsed from injury to surgery had no relation to the quality of fracture reduction. Conclusions: Patients with T12 and L1 fracture and AO type B fracture had better reduction of intracanal fragment for treatment of thoracolumbar burst fracture by short-segment fixation. Because the timing of surgery did not affect the results of fragment reduction, few delays are acceptable, and we might not need to hurry surgical reduction of intracanal fragment in the acute phase, unless there was neurologic deficit.
1754
RF046: The role of AO spine-DGOU osteoporotic fracture classification system in therapeutic decision making: our experience
Meriem Souissi 1,2 , Adnene Benammou 1,2 , Firas Belatra 1,2 , Ahmed Ben Abid 1,2 , Mondher Kooli 1,2 , Mehdi Bellil 1,2 , Mohamed Ben Salah 1,2
1 Faculty of Medecine of Tunis, University Tunis el Manar, Tunis, Tunisia
2 Orthopedic Surgery Department, Charles Nicolle Hospital, Tunis, Tunisia
Introduction: Osteoporotic vertebral fractures represent an entity of an increasing occcurence in a particularly frail, multi-diseased and constantly aging population. The absence of a universal definition and uncodified management of this underdiagnosed entity motivated the establishment of a new classification system by AO spine-DGOU. The aim of this study was to report the value of this classification system in the management of osteoporotic fractures in our experience. Material and Methods: We conducted a retrospective study, including patients with thoraco-lumbar osteoporotic fractures treated surgically. The judgement criteria were based on the neurological status, the classification of the fracture, the pain intensity according to the Visual Analogic Scale in the pre and postoperative periods, the type of treatment, the deformity correction and the postoperative outcomes. Results: 36 patients with a mean age of 65 years old were included in this study that spanned over 4 years. The mean follow-up period was 17 months. All patients were free of neurological symptoms. We had zero patients with OF1 fracture, four had OF2 and were treated with vertebroplasty, five had OF3 of which 2 were managed with kyphoplasty and 3 with vertebroplasty, twelve had OF4 managed with kyphoplasty (10) and vertebroplasty (2) and fifteen had OF5 treated using kyphoplasty (10) and vertebroplasty (5). The day after the surgery, 34 patients were able to walk and 31 patients were discharged. The mean VAS dropped from 5.82 in preoperative to 2.92 in postoperative. The drop of vertebral kyphosis was of 2.1°, regional kyphosis of 2.3° and Beck's index of 0.04. Conclusion: The AO spine-DGOU classification system allowed in our experience a universal assessment and treatment algorithm. A larger prospective study should be realized to confirm the interest of this classification in decision making in vertebral osteoporotic fractures.
2163
RF047: Evaluation of risk factors for dural tear in thoraco-lumbar burst fracture with vertical laminar fracture
Mayukh Guha 1 , Atul Sareen 2 , Tankeshwar Boruah 2
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
2 Central Institute of Orthopaedics, VMMC and Safdarjung Hospital, New Delhi, India
Introduction: Thoracic and lumbar burst fractures are commonly associated with vertical laminar fractures and there is known association between laminar fractures and dural tears. It is still very difficult to accurately predict dural tears in patients with vertical laminar fractures. Magnetic resonance imaging (MRI) has been applied in diagnosis of dural tear, but might play a limited role in detecting small dural injury. We aim to do this study to evaluate the risk factors for the presence of dural tears associated with laminar fractures in thoracolumbar burst fractures. Material and Methods: From 2020 to 2022, total 104 patients who had thoracic or lumbar burst fracture with vertical laminar fractures who were surgically managed were included in the study. The various demographic parameters, site, type, AO classification, mechanisms of trauma, presence of dural tear during surgery etc were documented. Plain radiography was used to measure loss of anterior vertebral body height and local kyphotic angle at fracture site. Axial plane computed tomography scan was used for identifying laminar fracture and labelling it’s type as “complete” or “incomplete”. Interpedicular distance and canal compromise percentage were assessed. MRI helped to identify PLC injury and formulate TLICS score. Neurological impairment was classified according to American Spinal Cord Injury Association (ASIA) classification. Different clinico-radiological risk factors of burst fractures with laminar fracrures to cause dural tear were noted by statistical analysis. Results: Dural tear was found in 27 out of 104 patients (25.96%). Age (p = 0.343), sex (p = 0.737), mode of injury (p = 0.265), level of burst fracture (p = 0.298) and AO type (p = 0.552) were not a significant risk factor. Laminar fracture gap was found to be significantly associated dural tear (p = 0.0002). Dural tear was present in 60% of cases where the gap was found to be > 3 mm. Morphology of laminar fracture whether complete or incomplete was not significant risk factor (p = 0.267). Dural tear was associated in 33.85% cases where the interpedicular distance was ≥ 125% and was significant (p = 0.018). When the canal compression was ≥ 50%, 32.84% had dural tear which is found to be significant (p = 0.031). 33.33% dural tear was there in presence of PLC injury and was significant (p = 0.045). When neurological impairment was considered, there was no significant association found with dural tear (p = 0.315). However, it was found that there was no dural tear when the neurology was intact. The association of TLICS score with dural tear was significant (p = 0.002). Multivariate regression model couldn’t find an independent predictor of dural tear. The highest Odd’s Ratio (OR) 5.128 for lamina fracture gap > 3 mm was found in this analysis. Conclusion: Risk factors for dural tear in TL burst fracture with vertical lamina fracture are wider lamina fracture gap, canal encroachment ratio more than 50%, interpedicular distance more than 125%, PLC injury and high TLICS score. A high index of suspicion should be there if these risk factors are present as there is no definitive MRI or other imaging evidence of dural tear in these fractures. Pre operative preparation and on table logistics arrangements should be done to tackle the dural tear if found intra operatively.
1799
RF048: Is medullar canal invasion as a predictor for posterior ligamentous complex injury in thoracolumbar burst fractures?
Murat Korkmaz 1 , Yekta Furkan Altin 1 , Taha Furkan Yağci 1 , Turgut Akgul 1
1 Orthopedics, Istanbul Faculty of Medicine, Fatih, Turkey
Objective: The large part of spinal fractures occur in thoracolumbar zone and burst fractures constitute for 10%–20% of these injuries. Posterior ligamentous complex (PLC) acts a major role in spinal stability and injury of this structure leads to spinal instability and neurological compromise. In this study, correlation of medullar canal invasion and PLC injury were evaluated. Methods: A total of 58 patients with thoracolumbar fractures were retrospectively evaluated between January 2013 and December 2022. Exclusion criteria include flexion distraction and fracture dislocation injuries and pathological fractures. Computed tomography (CT) was performed to asses the medullar canal invasion and magnetic resonance imaging (MRI) was performed to assess the PLC injury. The compromise of the spinal canal defined as the ratio of the amount of the canal compromise to total spinal canal diameter at the cross-sectional area of injured level. Loss of vertebral body height (LOVBH), local kyphosis (LK), vertebral body translation, interlaminar distance (ILD), supraspinous distance (SSD), and interspinous distance (ISD) were also evaluated radiographically. Results: 42 patients were included in the study. There were 25 males (59.5 %) and 17 females (40.5 %), and the average age was 38.2 (15.3) years. The mean follow-up time was 19.9 (21.9) months (Table 1). Preoperative STIR-weighted MRI showed that 17 patients had posterior ligamentous injury. Based on the comparison of the radiographic parameters according to presence of the PLC injury, a significant difference was found between the two groups only in canal compromise (p<0.001) (Table 2). The results of ROC curve analysis indicate that medullar canal compromise rate greater than %27.99 is a predictive factor for posterior ligamentous injury. [area under the curve (AUC) 0.838; 95% CI 0.714-0.961; p<0.001; 82.4% sensitivity; 80% specifity] (Table 3, Figure 1). Conclusion: The results of our study indicate that LOVBH, LK, vertebral body translation, ILD, ISD, and SSD were not associated with the presence of a PLC injury, while medullar canal compromise percentage greater than 28% was associated with PLC injury. Our data demonstrate that canal compromise rate measured with CT at the cross-sectional area of injured level is a reliable indicator for PLC injury.
Table 1.
Demographic, Clinical and Radiographic Characteristics.
| w PLC injury (n = 17) | w/o PLC injury (n = 25) | Total (n = 42) | p | |
|---|---|---|---|---|
| Gender (n(%)) female male |
6 (35.3%) 11 (64.7%) |
11 (44%) 14 (56%) |
17 (40.5%) 25 (59.5%) |
0.228 |
| Age (year) | 38.8 (15.6) | 37.8 (15.4) | 38.2 (15.3) | 0.964 |
| Follow-up (months) | 24.2 (25.2) | 17.0 (19.5) | 19.9 (21.9) | 0.090 |
| Canal compromise (%) | 44.9 (19.8) | 22.2 (15.3) | 31.4 (20.4) | 0.044* |
| Loss of vertebral body height (mm) | 65.2 (15.5) | 71.3 (14.9) | 68.8 (15.3) | 0.925 |
| Local kyphosis (degree) | 15.9 (8.3) | 13.3 (7.5) | 14.4 (7.8) | 0.790 |
| Translation (mm) | 4.5 (1.4) | 3.7 (2.0) | 4.1 (1.8) | 0.345 |
| ILD | 15.8 (4.7) | 16.2 (3.6) | 16.0 (4.1) | 0.400 |
| ISD | 9.0 (2.9) | 9.4 (4.2) | 9.2 (3.7) | 0.727 |
| SSD | 21.5 (9.7) | 20.7 (8.3) | 21.0 (8.8) | 0.380 |
w: with, w/o: without, PLC: posterior ligament complex, mm: millimeter, ILD: interlaminar distance, ISD: interspinous distance, SSD: supraspinous distance. p<0.05 is significant for homogeneity test.
Table 2.
Comparison of the Variables According to Presence of Posterior Ligament Complex Injury.
| w PLC injury (n=17) | w/o PLC injury (n=25) | p | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Canal compromise (%) | 44.9 (19.8) | 22.2 (15.3) | <0.001* | -33.69 | -13.02 |
| Loss of vertebral body height (mm) | 65.2 (15.5) | 71.3 (14.9) | 0.228 | -3.77 | 14.79 |
| Local kyphosis (degree) ≥20 degrees(n(%)) ≥15 degrees (n(%)) |
15.9 (8.3) 4 (44.4%) 9 (56.3%) |
13.3 (7.5) 5 (55.6%) 7 (43.8%) |
0.218 0.784 0.102 |
-7.44 | 2.29 |
| Translation (mm) ≥3.5 mm (n(%)) |
4.5 (1.4) 11 (45.8%) |
3.7 (2.0) 13 (54.2%) |
0.191 0.414 |
-1.88 | 0.22 |
| ILD | 15.8 (4.7) | 16.2 (3.6) | 0.939 | -2.23 | 2.99 |
| ISD | 9.0 (2.9) | 9.4 (4.2) | 0.778 | -1.63 | 2.89 |
| SSD | 21.5 (9.7) | 20.7 (8.3) | 0.798 | -6.37 | 4.91 |
w: with, w/o: without, PLC: posterior ligament complex, mm: millimeter, ILD: interlaminar distance, ISD: interspinous distance, SSD: supraspinous distance. p<0.05 is significant for Mann-Whitney U test and chi-square test.
Table 3.
Optimal Cut-Off Value for Area Under the Curve and Preoperative Canal Stenosis Percentage According to ROC Analysis.
| AUC (95%) | Cut off | p | Sensitivity (%) | Specifity (%) |
|---|---|---|---|---|
| 0.838 (0.714-0.961) | 27,9926 | <0.001 | 82.4% | 80% |
AUC: area under the curve.
Figure 1.
Area under the curve according to the ROC analysis result.
Keywords: thoracolumbar fracture, burst fracture, posterior ligamentous complex, ligament injury, medullar canal compromise.
2079
RF049: Optimal timing of percutaneous vertebroplasty based on bone marrow cytokine concentrations
Yasuhiro Nakajima 1 , Sho Akahori 1 , Ayako Motomura 1 , Takato Ohno 1 , Takashi Tsujiuchi 1 , Koji Osuka 2
1 Neurosurgery, Daido Hospital, Nagoya, Japan
2 Neurosurgery, Aichi Medical University, Nagakute, Japan
Purpose: Recently, consensus for early phase percutaneous vertebroplasty for osteoporotic vertebral fractures (OVF) has been forming. However, if early surgery is recommended too much, there is a risk that even cases that might have improved with conservative treatment alone will undergo surgery. In this study, to clarify which vertebral fractures should be operated on early, we measured the concentration of inflammatory cytokines distributed in the bone marrow fluid in the fractured vertebral body, examined the relationship between the concentration and various preoperative parameters and MRI imaging findings. Subjects/Methods: The fracture group included only patients admitted to the ER by ambulance due to severe difficulty in movement. 39 patients in the fracture group (average age 80.6 years, male-female ratio 9:30), 16 patients in the non-fracture group (average age 70.1 years, male-female ratio 9:7). The bone marrow fluid in the fractured vertebral body that can be collected during vertebroplasty and the bone marrow fluid in the non-fractured vertebral body that can be collected during posterior spinal fixation are used for samples, containing concentrations of IL-6, IL-8, and adiponectin. We investigated the relationship between cytokine concentrations and patient pain scores, various radiological parameters, MRI image findings, etc. Results: IL-6, IL-8, and adiponectin were significantly elevated in the fracture group. IL-8 and adiponectin were markedly elevated especially in the patients who have confined T2WI high intensity lesions in fractured vertebrae. [Conclusion] It has been reported that there is a correlation between the IL-8 concentration in bone marrow fluid and that in serum. Early vertebroplasty may be preferable in patients with confined T2WI high intensity lesions in fractured vertebrae and high serum IL-8 levels.
1817
RF050: Predicting kyphotic deformity progression in type A1 traumatic thoracolumbar junction injuries: a nomogram-based approach
Oleksii Nekhlopochyn 1 , Vadim Verbov 2 , Ievgen Cheshuk 2 , Milan Vorodi 2
1 Spine Neurosurgery
2 Restorative Neurosurgery Department, Romodanov Neurosurgery Institute, Kyiv, Ukraine
Introduction: Traumatic injuries to the thoracolumbar junction of the spine, comprising over 60% of spinal injuries, often result in compression fractures. Among these, Type A1 injuries exhibit less osteo-destructive changes and have traditionally been managed conservatively. However, recent studies have shown a high failure rate in conservative treatments, leading to progressive kyphotic deformity. Most of this research has focused on osteoporotic lesions in older patients, leaving a gap in understanding the outcomes in working-age patients with normal bone density. This study aimed to evaluate factors influencing the risk of kyphotic deformity progression in working-age patients with Type A1 traumatic thoracolumbar junction injuries. Material and Methods: Clinical cases from patients at our institution between 2019 and 2022 were analyzed. Forty-seven eligible patients were selected based on specific criteria. Predictors considered included gender, age, body mass index, injury level, damaged endplate location (caudal or cranial), bone tissue radiodensity, angular kyphotic deformity, and pain intensity. Patients were categorized into two groups based on kyphotic deformity progression status two months post-injury. The most clinically significant predictors were identified through the LASSO (Least Absolute Shrinkage and Selection Operator) regression method. Results: Five potential predictors were identified through LASSO screening. The final logistic regression model, following regularization, exhibited strong predictive performance with an area under the ROC curve (AUC) of 0.907 and an 85% prediction accuracy. Age, bone density, angular kyphotic deformity, and pain intensity showed a direct proportional relationship and were found to be of utmost importance in assessing the risk of kyphotic deformity progression in Type A1 thoracolumbar junction injuries. Additionally, a compressed caudal endplate was associated with an increased risk of post-traumatic kyphosis progression. A nomogram was developed using these factors, facilitating quantification of risk levels when selecting an appropriate therapeutic strategy. Conclusion: This analysis resulted in the creation of a nomogram for predicting kyphotic deformity progression in Type A1 thoracolumbar junction fractures. The proposed model provides a rational means of assessing risk levels when determining optimal treatment approaches for affected individuals.
1930
RF051: Predicting early complications in patients with spinal gunshot wounds: a multicenter study
Guillermo Ricciardi 1 , Juan P. Cabrera Cousiño 2 , Oscar Martinez 3 , Javier Matta 4 , Hugo Vilchis Samano 5 , Jeasson Perez 6 , Charles Carazzo 7 , Michael Dittmar 8 , Ratko Yurac 9
1 Spine team - Orthopaedics and Traumatology, Centro Médico Fitz Roy, Ciudad de Buenos Aires, Argentina
2 Hospital Clínico Regional de Concepción, Chile
3 Hospital Universitario Dr. José E. González, Mexico
4 Hospital Militar Central, Colombia
5 Unidad Médica de Alta Especialidad Hospital de Traumatología y Ortopedia Lomas Verdes IMSS, México, Mexico
6 Clínica de columna "Dr. Manuel Dufoo Olvera", Mexico
7 São Vicente de Paulo Hospital - Passo Fundo - RS, Brazil, Brazil
8 Centro Médico Puerta de Hierro, Zapopan, México, Mexico
9 Clínica Alemana de Santiago, University del Desarrollo, Chile
Introduction: There is a wide variation in the clinical presentation of spinal gunshot wounds ranging from isolated minor stable fractures to extremely severe injuries with catastrophic neurological damage. We aim to analyze the risk factors for early complications and impact of surgical treatment in patients with spinal gunshot wounds. Material and Methods: Multicenter retrospective case-control study. Comparison between patients with postoperative complications and those without complications was made using the following matched criteria: gender (1:1), injury level (1:1), and age (±5 years). A univariate and multivariate analyses using logistic regression method were performed. Results: Among 387 patients, 36.9% registered early complications, being persistent pain (n = 32; 15%), sepsis/septic shock (n = 28; 13%), pneumonia (n = 27; 13%) and neurogenic bladder (n = 27; 12%) the most frequently reported. After case-control matched analysis, we obtained 133 patients who suffered early complications (cases) and 133 patients who did not as control group, not differing significantly in sex (p = 1.000), age (p = 0.535) and injury level (p = 1.000), while the 35% of complications group required surgical treatment versus 15% of the non-complication group (p < 0.001). On multivariable analysis, significant predictors of complications were surgical treatment for spinal injury (OR = 3.50, 95% CI = 1.68-7.30), dirty wound (3.32, 1.50-7.34), GCS ≤ 8 (3.56, 1.17-10.79), hemodynamic instability (2.29, 1.07-4.88), and multiple bullets (1.97, 1.05-3.67). Conclusion: Spinal gunshot wounds are associated with a high risk of early complications, especially when spinal surgery is required, and among patients with dirty wound, low level of consciousness, hemodynamic instability, and multiple bullets.
1143
RF052: Percutaneous posterior fixation with endoscopic decompression in patients with thoracolumbar fractures with incomplete neurologic deficit. Our initial experience
Chetan Chaudhary 1
1 Department of Trauma Surgery, AIIMS, Rishikesh, India
Introduction: Fractures of thoracolumbar junction are the most common injuries of the spine and are often accompanied by neurological deficit. Mechanical stabilization and neurological decompression is the standard of care in such cases, however the approach differs at the discretion of surgeon. In this study we are reporting on the clinico-radiologic outcome of thoracolumbar fractures (TLFs) with incomplete neurologic deficits treated by percutaneous posterior fixation (PPF) and bi-portal endoscopic decompression (ED). Material and Methods: Ours is a retrospective study of 12 cases operated between December 2021 and June 2023. Patients with thoraco-lumbar fractures (T10-L2) with incomplete neuro-deficit treated with aforesaid method were included. Clinical outcome was assessed by VAS and ASIA scoring, whereas radiologic outcome was assessed with segmental kyphosis (X-ray) and space available for the cord (MRI). The SAC was used to determine the adequacy of decompression while the deformity correction was assessed by sagittal cobb’s angle, segmental kyphosis sagittal index and the anterior vertebral height gain. While the functional assessment was done by ODI and ASIA score. Results: The mean follow up of the patients was 12 months. Our study showed that the mean intraoperative time was 165.5 minutes, the mean intra operative blood loss was 40.24 ml. The sagittal cobb’s angle decreased from 20.42° to 6.38°, while the percentage of anterior vertebral height increased from 48.76% to 80.43%. MRI showed an adequate increase in space available for cord in the operated cases. Dural injury was seen in one case. Conclusion: Minimally invasive surgical decompression and stabilization (PPF+ED) in selected cases of Thoracolumbar fractures (TLFs)with incomplete neurological deficits appears to be a safe technique with low complication rate and higher patient satisfaction. MIS reduces hospitalization and allows fast functional recovery.
69
RF053: Short segment posterior fixation with pedicle screws at the level of the fracture (short same segment fixation - SSSF) for unstable thoracolumbar burst fractures - Do they do better?
Surath Sanjaya Kumara Munasinghe Arachchige 1
1 Neurosurgery, Teaching Hospital Ratnapura, Ratnapura, Sri Lanka
Objectives: The primary objective of this study was to evaluate the efficacy of Short Same Segment Fixation in the treatment of unstable Thoraco-Lumbar Fractures (TLF) and the secondary objective was to study any difference in outcome whether single pedicle versus both pedicles included for fixation at the fractured level. Methods: Retrospective analysis of 81 patients who underwent SSSF for unstable TLF over 4 years operated by a single surgeon at a tertiary care centre and completed follow up for at least 12 months were included. Patients with Kyphotic Angle (KA) of more than 25 degrees, AO type C fractures, muti-level fractures and patients with severe osteoporosis were excluded. All injuries were categorised according to AO spine classification system, TLICS score and ASIA scale. All surgeries were performed within 72 hours of admission. Radiological evaluation with Cobb angle, functional outcome with Oswestry Disability Index (ODI) and Visual Analog Scale (VAS) for pain were evaluated as primary outcome measures and intra-operative blood loss, length of hospital-stay, post-op complications were assessed as secondary outcomes. Results: Study included 64 males and 17 females. Injury segment distribution was T10-L2 and most common fracture site was L1 and most common mechanism of injury was fall from height. 36 patients had single pedicle screw inserted at the injury level (out of which 30 patients could only afford 5 screws and 6 had one pedicle disrupted) and 45 patients had both pedicles fixed at the index level. Mean hospital stay was 5.12 days. Mean number of days before ambulation was 6.63 days. Mean pre-operative kyphosis was 16.48 degrees. Mean immediate post-operative kyphosis was 6.183. Mean kyphosis at 12 months follow up was 11.05. Mean kyphosis correction at immediate post op was 10.298 (p < 0.001). Mean kyphosis correction at 12 months follow up was 5.43 (p < 0.001). Mean loss of kyphosis correction at 12 months was 4.83. Pre-op mean VAS score was 7.86, and 3.04 at 1 month, 1.60 at 6 months and 0.86 at 12 months (p < 0.001). Mean pre-op ODI was 69.68 and 14.84 at 6 months and 9.41 at 12 months. There was a significant difference between pre-op ODI and follow up ODI at both 6 and 12 months (p < 0.001). Mean operative blood loss was 111.6 ml. Mean operative time was 84.89 minutes. There was no difference in VAS scores, ODI scores, hospital stay, blood loss, operative time, time before ambulation; between single pedicle vs both pedicles fixed groups at the fractured level. Only difference noted between above groups was kyphosis correction at immediate post-op period. No significance between the groups for other KA parameters noted. Number of failures at 12 months were 4 with 2 Pseudoarthrosis and 2 hardware failures (screw pull out). Conclusion: SSSF shows significant improvement in pain scores, functional outcomes and kyphotic angles but there is significant loss of kyphosis correction over time. No significant difference in outcome whether one pedicle or both pedicles were included at the fractured level.
2532
RF054: Early versus late stabilization in unstable thoracolumbar fractures: a systematic review
Stanley Masunda 1 , Alexander Montgomery 2 , Sebastian Ndlovu 3 , Emmanuel Oladeji 1 , Ahmed Lashin 1 , Ahmed Kaddah 1 , Mohammad Alhashash 1 , Matthias Wusu 1
1 Trauma and Orthopaedics, St Richard's Hospital Chichester, United Kingdom
2 Spine Surgery, Royal London Hospital, United Kingdom
3 Trauma and Orthopaedics, Dartford and Gravesham NHS Trust, United Kingdom
Background: Spinal injuries occur usually as a result of high energy injury mechanisms and are associated with debilitating consequences for patients. Controversy still exists regarding timing of surgical stabilization of thoracolumbar fractures. We conducted a systematic review of the literature comparing early versus late thoracolumbar stabilization, focusing on length of hospital stay (LOS), length of stay in the intensive care unit (ICULOS) and days on ventilator (VENT days), as the primary outcomes. Methods: An electronic database search was carried out on PubMed, Cochrane CENTRAL, and Embase spanning 1999 to 2020, using a developed search strategy. The time cut off used to distinguish early and late stabilization was 72 hours from injury. Results: Of the 2082 articles retrieved, 80 were screened by full text and a final 14 studies comprising data from 4576 patients were eligible for inclusion in this review. The overall level of evidence of included studies was low with only one quasi-randomised control trial. Most of the reviewed articles favoured early stabilization for the main outcome measures of hospital length of stay, and intensive care unit length of stay. This benefit was particularly significant in patients with higher injury severity scores (ISS). Conclusion: This review demonstrated favourable outcomes in patients who received early stabilization of thoracolumbar injuries. However, caution is advised when interpreting these results given the level of evidence of studies included. Further high-quality studies are required to better answer the question of timing of surgical stabilization of thoracolumbar fractures.
RFP04: Degenerative Cervical
2331
RF055: Facet resection in posterior cervical foraminotomy: is more than 50% resection really incompatible?
Ji Uk Choi 1 , Dong-Ho Lee 1 , Hyung Rae Lee 2
1 Orthopaedics, Asan Medical Center, Songpa-gu, South Korea
2 Orthopaedics, Uijeongbu Eulji Hospital, Uijeongbu-si, South Korea
Introduction: Since the implementation of biomechanical experiments using an in vitro model, previous research has suggested that facet resection during posterior cervical foraminotomy (PCF) should not exceed 50% to maintain postoperative stability. However, to date, there has been no investigation regarding the potential increase in instability associated with facet resection beyond 50%. Furthermore, recent data have cast doubt on whether resection of more than 50% of the facet can still be considered unstable. This study aimed to investigate the effects of facet resection exceeding 50% during PCF. Material and Methods: We conducted a retrospective review of 65 patients who had undergone unilateral posterior cervical foraminotomy (PCF) for cervical radiculopathy and were followed up for more than 2 years. The patients were categorized into two groups based on the amount of resection: group O (over-resection group, resection > 50%) and group C (control group, resection ≤ 50%). A chi-square test was employed to compare the bone bridge formation between the two groups. In addition, a regression analysis was conducted on 162 segments to assess the relationship between the amount of facet resection and four outcome variables: segmental instability, range of motion, disc height, and foraminal restenosis. Results: Group O demonstrated a significantly lower segmental ROM compared to group C (p = .005), while there were no significant differences between the groups in terms of clinical outcomes, cervical ROM, or alignment. The chi-square test did not show a significant difference in bone bridge formation between groups O and C; however, the former exhibited a notably higher number of fully formed bone bridges than the latter (p = .350). The regression analysis results revealed a significant negative correlation between the degree of facet resection and postoperative disc height (β = -.196, p = .013), indicating that greater facet resection was associated with a greater reduction in disc height after the surgery. Conclusion: The group O did not exhibit any adverse clinical or radiological outcomes, except for a decrease in segmental range of motion. In addition, there was no significant difference in radiographic changes according to the extent of resection for each segment, except for disc height change at 2-year follow-up. Contrary to the conventional understanding, facet resection of more than 50% does not seem to cause significant issues, but rather may induce spontaneous fusion, leading to a potential decrease in range of motion.
1598
RF056: Are patients with cervical OPLL more prone to neuromonitoring signal changes? A study of 100 patients of degenerative cervical myelopathy undergoing posterior decompression surgery
Shanmuganathan Rajasekaran 1 , Dinesh Iyer R 1 , Ajoy P Shetty 1 , Sri Vijay Anand KS 1 , Karthik Ramachandran 1 , Rishi Kanna 1
1 Department of Spine Surgery, Ganga Hospital, Coimbatore, India
Introduction: Degenerative cervical myelopathy (DCM) is the most common cause of non-traumatic spinal cord dysfunction. Intraoperative neuromonitoring (IONM) has become a useful adjunct during surgeries to predict post-operative neurological deficits. However, there is a lacuna in the literature about the risk factors for neuromonitoring signal changes and their prognostic significance. The aim of this study was to analyze the clinical and neuromonitoring data of patients of DCM undergoing posterior instrumented laminectomy and assess the incidence of signal changes, identify risk factors and their clinical correlation. Materials and Methods: A retrospective review of 100 patients of DCM who underwent posterior instrumented laminectomy with Intraoperative neuromonitoring (IONM) between July 2018 to March 2023 at our hospital. We analyzed the signal changes for any correlation with the diagnosis of Ossified posterior longitudinal ligament (OPLL) vs. cervical spondylotic myelopathy (CSM), type of OPLL, level of involvement, clinical parameters (Nurick grade and mJOA scores) and radiological parameters (C7 slope, C2-C7 kyphosis, length of intramedullary cord signal changes, number of levels of bidirectional compression, K-line). Patients were divided into false positives, false negatives, transient signal drops, and post-operative neurological deficits for further subgroup analysis and identifying the risk factors neuro deficits. Results: Out of the 100 cases, 55 were diagnosed with ossified posterior longitudinal ligament (OPLL) and 45 with cervical spondylotic myelopathy (CSM). The incidence of signal drops after decompression (both false positive and transient drop) was significantly higher in the OPLL group compared to the CSM group. 85% of the false positives and 75% of the transient drop cases belonged to the OPLL group. However, there was no difference in the incidence of post-operative neurological deterioration. Continuous OPLL, Hill-type lesion on axial CT, Negative K-line, high-grade myelopathy (Nurick 4 and 5), and length of intramedullary cord signal changes were correlated to a higher incidence of intra-operative signal alerts and postoperative neurological deficits. Overall we found a good negative predictive value (97%) of IONM although it had a poor positive predictive value (15.4%), especially in cases of OPLL. Conclusion: The presence of OPLL is a risk factor for a higher incidence of intraoperative signal alerts and false positive outcomes after cervical decompression. There is a higher incidence of post-operative neuro deficits if it is associated with hill type lesion, negative K-line, and continuous type of OPLL and can be used to prognosticate the patient about the potential complications.
878
RF057: Comparison of the postoperative motion stabilization between anterior cervical decompression and fusion with zero-profile implant system and a plate - Cage construct
Haimiti Abudouaini 1 , Hao Liu 2
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China, Xi 'an, China
2 Department of Orthopedics, West China Hospital, Sichuan University, West China Hospital, Sichuan University, Chengdu, China
Objective: Due to the lack of an additional anterior plate, the motion stability of a zero-profile device with an anchored cage (AC) may be inferior to that of a traditional plate-cage construct (PCC). However, the impact of this difference in motion stability on various outcomes has not been fully explored. Therefore, the aim of this study was to compare the motion stabilization features of an AC and a PCC and analyze their impact on postoperative outcomes and complications. Methods: A retrospective study of patients treated with single-level anterior cervical discectomy and fusion from January 2008 to May 2016 was performed. First, clinical and radiological outcomes, postoperative complications and time to achieve motion stabilization were compared between the AC and PCC groups. Then, based on the time to achieve motion stabilization, all patients were divided into group A (time to achieve motion stabilization < 3 months), group B (time to achieve motion stabilization from 3-6 months), and group C (time to achieve motion stabilization > 6 months). The early postoperative complications were compared across the 3 groups. Motion stabilization was measured on dynamic cervical radiographs using the interspinous process method and Cobb angle method according to previously published methods. Results: A total of 160 patients met the inclusion criteria, including 90 patients in the AC group and 70 patients in the PCC group. There were no significant differences between the AC and PCC groups in the clinical outcomes, C2-7 angle change, segmental angle change, final fusion rate or adjacent-level degeneration (p > 0.05). The disc height loss was 2.26 ± 1.00 mm in the AC group and 1.76 ± 1.13 mm in the PCC group (p = 0.004), and the incidence of implant subsidence was 24.44% in the AC group and 11.43% in the PCC group (p = 0.036). In addition, the PCC was more dynamically stable than the AC at 3 months post-surgery (p < 0.001), and at this time, the disc height loss and implant subsidence in motion-stable patients were significantly lower than those in motion-unstable patients (p < 0.05). Furthermore, our results also showed that when the arrival time of motion stabilization was prolonged, the loss of disc height and occurrence of subsidence gradually increased. Conclusions: More attention should be given to minimizing the adverse impact of poor motion stability in the design and development of future zero-profile cervical implants, although this has little impact on clinical efficacy.
Keywords: anterior cervical discectomy and fusion; cage subsidence; disc height; motion stabilization; zero profile
994
RF058: What predicts perioperative complications and 90-day readmission after cervical laminoplasty? Is it Frailty, ASA grade, Smoking, and/or Depression?
Michael Tawil 1 , Timothy Chryssikos 1 , Mohamed Macki 1 , Vardhaan Ambati 1 , Alexander Aabedi 1 , Vijay Letchuman 1 , Nishanth Krishnan 1 , Alysha Jamieson 1 , Joshua Rivera 1 , Andrew Chan 2 , Vivian Le 1 , Valli Mummaneni 1 , Lee Tan 1 , Dean Chou 2 , Praveen Mummaneni 1
1 Neurological Surgery, UCSF, San Francisco, USA
2 Neurological Surgery, Columbia University, New York, USA
Introduction: The modified Frailty Index-5 (mFI-5) is a simple assessment tool used in the preoperative setting to assess patient health and has been correlated to clinical outcomes after surgery. We aimed to determine if the mFI-5 predicts perioperative complications and readmission within 90 days following posterior cervical laminoplasty. Material and Methods: 302 patients who underwent open-door laminoplasty for cervical spondylitic myelopathy at a single quaternary center were retrospectively reviewed. Demographic, patient-reported (mJOA, EQ5D), and surgical data were collected. The mFI-5 was used to quantify patient frailty. Univariate and multivariate logistic regression analyses were used to evaluate mFI-5 and other clinically relevant variables and to compare frailty with other measures (ASA grade, smoking, and depression). Results: Mean age and BMI were 63.5 and 28.6, respectively. There were 188 males and 114 females. Rate of readmission within 90 days was 9.9%. Univariate logistic regression showed a significant association between 90-day readmission and depression (OR 3.27, p = 0.03). mFI-5 was more predictive than ASA grade for 90-day readmission (OR 1.40, p = 0.06 vs. OR 0.57, p = 0.16) on univariate analysis. Multivariate logistic regression including age, ASA grade, mFI-5, and depression showed that only depression was significantly associated with 90-day readmission (OR 2.60, p = 0.04). The overall rate of complications was 14.6%. Univariate logistic regression showed significant associations between complications and smoking (OR 2.41, p = 0.05) and mFI-5 (OR 1.64, p = 0.001). Multivariate logistic regression including age, ASA grade, mFI-5, and smoking showed that both mFI-5 (OR 1.56, p < 0.01) and smoking (OR 4.79, p < 0.01) were significantly associated with complication after cervical laminoplasty. Conclusion: Smoking status and patient frailty (mFI-5) outperformed ASA grade and depression for predicting perioperative complications following cervical laminoplasty. However, for 90-day readmission depression was the only significant predictor of 90-day readmission after cervical laminoplasty.
2108
RF059: C1-C2 subluxation causing refractory occipital neuralgia and option of treatments
Devatathan Arulkanesh 1 , Kumaran Thinesh 1 , Azmi Alias 1
1 Neurosurgery, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Introduction: Refractory occipital neuralgia has been under diagnosed and most patients will be on long term analgesia without good relief for many years. This refractory occipital neuralgia has severe impact on patient’s daily activities and productivities. Commonest cause of refractory occipital neuralgia has been C1-C2 subluxation which also less investigated. Prompt investigations to diagnose refractory occipital neuralgia is paramount when medical therapy failed to relief the symptoms. For interventional nerve block at C2 nerve root to relief pain and subsequently offer surgical intervention for patient with refractory or recurrent occipital headache despite underwent nerve block. Material and Methods: 81 patients with occipital neuralgia who has poor medical control underwent MRI Brain and Cervical to exclude other causes of headache. Subsequently, 64 patients underwent dynamic CT Cervical to look for evidence of C1-C2 subluxation. 49 patients who have C1-C2 subluxation subjected to interventional nerve block injection of C2 nerve root. 24 patients who failed interventional treatment were diagnosed as Refractory Occipital Neuralgia and subjected to C1-C2 posterior screw fixation. Bilateral C1 lateral mass and C2 pedicle screws inserted and fixed with rods while preserving the bilateral C2 nerve roots. Results: About 25% patients diagnosed as refractory occipital neuralgia after failed interventional C2 nerve root injection which documented as VAS score of 6 and more or reduction of pain less than 50%. These patients who underwent posterior fixation reported VAS score of less than 3 or pain reduction of more than 80% immediately after surgery. Post operation, almost 90% patient are medication free. Conclusion: Occipital neuralgia is a common presentation of C1-C2 subluxation. Patients with refractory occipital neuralgia achieved an excellent pain control with C1-C2 posterior fixation surgery and have a good outcome.
2495
RF060: Reoperations for adjacent segment disease in a cohort of patients operated for degenerative cervical myelopathy
Michele Da Broi 1 , Aria Nouri 1 , Granit Molliqaj 1 , Enrico Tessitore 1
1 Department of Neurosurgery, Geneva University Hospital, Geneva, Switzerland
Introduction: To analyze reoperation rate for adjacent segment disease (ASD) in a cohort of patients operated for degenerative cervical myelopathy (DCM). Material and Methods: A total of 175 consecutive patients who underwent surgery for DCM at Geneva University Hospital between 2008 and 2023 were analyzed regarding reintervention rate for ASD. Results: The overall reoperation rate was 19.4% (34/175) with 5 patients (2.9%, 5/175) reoperated for a proximal or distal ASD. The median age at first surgery was 41.0 years [range: 34-55 years]. The mean time to develop a symptomatic ASD which required surgery was 5 years (SD: 3.5 years, range: 1-9.5 years). All patients but 1 (N = 4, 80%) had an anterior cervical discectomy and fusion (ACDF) as first intervention, the other patient had two-level corpectomy. Among patients who had ACDF in the first place, 3 (60%) had one-level ACDF and only 1 (20%) had a two-level procedure. No patient had postoperative hematoma or infection. Every patient but 1 (N = 4, 80%) had a one-level ACDF as second surgery. Only 1 (20%) presented with a proximal and distal ASD associated to pseudoarthrosis. Therefore, he underwent implant revision and two-level ACDF. Only 1 patient (20%) underwent a third surgery for a second ASD. After 5.7 years he developed a second proximal ASD and underwent one-level ACDF. Conclusion: In our cohort 2.9% of patients were reoperated for an ASD. This long-term complication may be more related to anterior procedures, and it was treated with an extension of the anterior approach.
315
RF061: Open-door cervical laminoplasty with skip-fixation is not inferior to that with all-fixation: a multicenter non-blinded randomized controlled study
Koji Tamai 1 , Hidetomi Terai 2 , Akinobu Suzuki 2 , Minori Kato 2 , Hiromitsu Toyoda 2 , Shinji Takahashi 2 , Yuta Sawada 2 , Masayoshi Iwamae 2 , Yuki Okamura 2 , Yuto Kobayashi 2 , Hiroaki Nakamura 1
1 Osaka Metropolitan University, Osaka, Japan
2 Orthopedic Surgery, Osaka Metropolitan University, Osaka, Japan
Introduction: Degenerative cervical myelopathy (DCM) is the leading cause of spinal cord impairment (1). Surgical decompression, including cervical laminoplasty, is the standard treatment to improve the neurological function and quality of life (QOL) of most patients (2). In patients with DCM undergoing cervical laminoplasty, it is well-accepted that a multilevel laminar should be expanded to attain adequate spinal cord decompression (3). However, whether all the expanded lamina should be fixed or not have not been validated enough. We postulated that the surgical outcomes of open-door laminoplasty with every other expanded laminar fixation (skip-fixation) may not be inferior to those of surgery with an all-expanded laminar fixation (all-fixation) (figure). Therefore, this study aimed to test the non-inferiority of myelopathy improvement one year after open-door cervical laminoplasty with skip-fixation compared to all-fixation in patients with DCM. Additionally, in the sub-analysis, we compared other 1-year surgical outcomes, including patient-reported outcomes, between the two types of surgeries. Material and Methods: This prospective, multicenter, non-blinded randomized controlled trial was performed in four sites in Japan. Patients at least 60 years old and who underwent C3-C6 open-door cervical laminoplasty for DCM were included in this study. In total, consecutive 217 patients were assessed for eligibility, and 213 were randomized to undergo laminoplasty with skip-fixation (n = 112) or all-fixation (n = 101) using the permuted block strategy. The primary outcome was the difference in the one-year Japanese Orthopaedic Association (JOA) score between the groups. The non-inferiority margin was set as 2.0, the minimum clinically significant difference in the JOA score. Secondary outcomes included surgical data, surgical complications, one-year changes in the Neck Disability Index, EuroQol 5 Dimensions (EQ5D) score, and visual analog scale (VAS) score for neck pain, arm pain, arm numbness, and radiographic outcomes. Results: Among the 213 patients, 178 completed the trial after one year (skip-fixation, n = 92; all-fixation, n = 86; follow-up rate, 83.6%). The difference in the JOA score after one year was -0.101 (95% confidence interval: -0.799-0.596), which was significantly within the non-inferiority margin (p < 0.0001, non-inferior test). In the sub-analysis, laminoplasty with skip-fixation demonstrated a significantly shorter surgical time (p = 0.019), better improvement in neck pain VAS (p = 0.007), and better improvement in EQ5D score (p = 0.048) than laminoplasty with all-fixation. There were no significant differences in radiographic outcomes, including C2-7 angle and range of motion, between the surgical types. Conclusion: Because skip fixation requires half the number of implants compared to all-fixation, laminoplasty with skip-fixation can reduce medical costs. Current results indicates that among patients with DCM who underwent C3-C6 open-door cervical laminoplasty, skip-fixation was not inferior to all-fixation in terms of myelopathy improvement. Additionally, laminoplasty with skip-fixation can potentially improve neck pain and QOL more than that with all-fixation. As the incremental cost-effectiveness ratio was calculated by “medical cost/gained QOL”, cervical laminoplasty with skip-fixation can be considered a cost-effective procedure.
2222
RF062: Comparsion of hybrid anterior cervical corpectomy and fusion combined with total disc replacement or cage fusion for multilevel cervical spondylotic myelopathy
Bo Yuan 1 , Shengyuan Zhou 1 , Xiongsheng Chen 1
1 Orthopedics, Shanghai Changzheng Hospital, Shanghai, China
Introduction: The treatment for multilevel cervical spondylotic myelopathy (CSM) remains controversial. As widely used surgical techniques, anterior cervical corpectomy and fusion (ACCF) and anterior cervical discectomy and fusion (ACDF) possess definitive clinical efficacy and excellent fusion rate. However, the loss of range of motion and stress on adjacent segment may accelerate the incidence of adjacent segment degeneration (ASD). Total disc replacement (TDR) was designed and used in clinical practice in recent years. It can effectively maintain the motion function, restore the intervertebral disc height and prevent ASD, but its indication is relatively narrow. The outcomes of ACCF combined with TDR have not been evaluated. The aim of this retrospective comparative study is to compare the clinical and radiological outcomes of ACCF combined with TDR or ACDF for multilevel CSM. Material and Methods: Patients who underwent multilevel ACCF combined with TDR or ACDF from May 2008 to March 2019 were identified and propensity scores matching was preformed based on patient characteristic. The clinical data with follow-up more than two years were retrospectively analyzed. Finally, 110 patients (43 in TDR group and 67 in ACDF group) were enrolled in this study. Based on the treated segments were continuous or not, the patients could also be divided into continuous subgroup and noncontinuous subgroup. The clinical efficacy of the two procedures was evaluated by comparing the modified Japanese Orthopaedic Association (JOA) scores, Neck Dysfunction Index (NDI) and visual analogue scale (VAS) at timepoint of pre-operation and final follow-up. The radiological outcomes were assessed by using range of motion (ROM) of C2-C7 and the ASD was evaluated by Pfirrmann grading standard. Results: All the patients got significant increase in modified JOA scores, and decreases in NDI and VAS scores (p<0.001). But there was no statistically difference in modified JOA scores, NDI scores and VAS scores between the TDR group and the ACDF group at pre-operation and final follow-up (42.8 ± 16.1 months). For radiological parameters, the ROM of C2-C7 significantly decreased in ACDF group (p<0.001), and the TDR excellently maintained the motion function of index segment (Pre 6.47° ± 1.0° vs Po 6.84° ± 0.9°, p>0.05) at final follow-up. No matter in continuous or noncontinuous subgroup, ASD was successful postponed around the TDR segment at final follow-up (p<0.001). Conclusion: ACCF combined with TDR or ACDF could achieve favorable clinical and radiological outcomes in the treatment of multilevel CSM. Compared with ACCF combined with ACDF, ACCF combined with TDR could retain the motion function of non-fused segment, and did not significantly aggravate ASD. Hybrid surgery is suitable for multi-level degeneration of cervical spine, especially for obvious degeneration of adjacent segments of decompression area.
1253
RF063: Comparative study between decompressive laminectomy versus laminoplasty for multilevel cervical spondylotic myelopathy
Anowarul Islam 1 , Suvradev Saha 1
1 Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Introduction: Cervical laminoplasty is a standard surgical method for the decompression of multilevel cervical spondylotic myelopathy (CSM) without creating spinal instability and kyphosis. Cervical laminectomy with lateral mass screw fixation is also used for CSM in many centres. Our aim is to assess the axial pain, quality of life, sagittal alignment, and extent of decompression after standard cervical laminectomy or laminoplasty. Methods and Materials: We reviewed 45 patients with cervical spondylotic myelopathy who underwent cervical laminectomy (25) or laminoplasty (20) between January 2015 and January 2023. The clinical outcome was analyzed by visual analog scale for neck pain. The quality of life was analyzed by modified Japanese Orthopaedic Association (mJOA). Results: Laminoplasty was associated with more neck pain and worse quality of life when 4 or more levels were decompressed compared with the laminectomy group. For operations of 3 or fewer levels, there was no difference. Decompression effectivity was greater in the laminoplasty group. In laminoplasty group, the maintenance of cervical curvature is more than laminectomy with lateral mass fixation group. Conclusion: Laminoplasty is a better surgical option for 3 level CSM with preserving neck motion, better pain relief and cervical alignment, but when treated 4 or more level CSM laminectomy with lateral mass fixation should be considered.
1032
RF064: Prevalence, characteristics, and postoperative impact of hand atrophy in patients with degenerative cervical myelopathy
Wonyoung Lee 1 , Kyung-Chung Kang 1 , Jung-Hee Lee 1 , Ki-Young Lee 1 , Seong Jin Cho 1 , Hong-sik Park 1 , Se-Hwan Park 1
1 Orthopaedic Surgery, Kyung-hee University Medical Center, Seoul, South Korea
Introduction: Hand clumsiness is a presentative symptom of patients with degenerative cervical myelopathy (DCM). Some patients reveal significant hand dysfunction and atrophy of intrinsic muscles in hands. However, there is a lack of evidence for hand atrophy (HA) in patients with DCM. The aim of this study is to evaluate prevalence, characteristics, and postoperative impact of HA in patients with DCM. Material and Methods: Total 101 (male: 77, mean age: 58.8 yrs) patients with 1 year or more follow-up are enrolled in this study. According to the presence of HA, patients were sub-grouped into Group A (Atrophy) and Group N(Non-atrophy). Patients’ characteristics (age, sex, BMI, underlying diseases, hand grip strength (HGR) and so on), and radiographic (presence of ossification of posterior longitudinal ligament (OPLL) and high signal change in T2-weighted MR image) and clinical (neck/arm Visual Analog Scale (VAS), Japanese Orthopedic Association (JOA), and Neck Disability Index (NDI)) parameters were compared among the two groups. Results: Preoperatively, 44 patients (43.6%) demonstrated HA in their hands. Mean age of Group A (62.6 ± 10.9) was higher than Group N (55.9 ± 12.4). Although pre- and post-operative HGR were significantly lower in Group A than in Group N, both groups revealed significant increments of HGR postoperatively. The rate of cord high signal change was significantly higher in Group A (59.1%) than in Group N (36.8%) (p = 0.026). The rate of OPLL and postoperative neck/arm VAS, JOA, and NDI demonstrated no significant differences, but increments of JOA score in Group A was significantly higher than in Group N. Conclusion: The prevalence of HA in patients with DCM is high, particularly in elderly patients. These patients had significantly higher incidence of high signal change in MRI. Postoperative clinical scores significantly increased after surgeries in both groups, but the increment of JOA score was significantly higher in Group A than in Group N. These means surgical treatment would improve hand function, even in patients with HA.
1589
RF065: Spinal dural defect repair is effective in the management of superficial siderosis: a case series and systematic review
Frederick Mariajoseph 1 , Fidel Toomey 1 , Ameen Farsakh 1 , Darius Tan 1 , Jeremy Kam 1 , Tony Goldschlager 1
1 Department of Neurosurgery, Monash Health, Melbourne, Australia
Introduction: Superficial siderosis is a rare, disabling neurodegenerative condition that may be caused by spinal dural defects. Surgical repair is increasingly performed however an optimal treatment strategy and its clinical efficacy remains unclear. Currently only case reports and limited case series exist. Here we present five novel cases with a previously unreported cause of superficial siderosis and the only systematic review of existing literature. Material and Methods: A systematic search of PubMed, MEDLINE, and EMBASE was conducted (inception to February 2020). Studies reporting cases of (i) superficial siderosis, (ii) spinal dural defect, (iii) and surgical closure of the spinal defect were included. Demographic characteristics, clinical presentation, operative technique, and clinical outcome were extracted for patient-level analysis. All patients from our institution who underwent surgical management of superficial siderosis from 2021 to 2023 were included. Results: A total of 26 publications were included, which reported 38 patients with a median age of 58 years, and a male predominance (78.9%). Ataxia (85.7%) and hearing loss (80.0%) were the most common presenting symptoms. The causative dural defect was most commonly ventral in location (91.7 %) and most commonly identified by CT myelography (48.6%). Operative technique was highly variable and included primary suture, fibrin glue, dural substitute, or tissue (fat or muscle) graft. Clinical improvement was reported in 21% of patients, with stabilisation of symptoms in the majority (66%) and clinical deterioration in 13.2%. Surgical complications were observed in 7.9%. An additional five patients from our institution had undergone surgical repair and recovered without complications. Conclusion: In patients with superficial siderosis and spinal dural defect, operative closure leads to improvement or stabilisation of symptoms in the vast majority (88%) of patients.
Keywords: superficial siderosis; dural defect; dural closure; pseudomeningocele
Disclaimer: systematic review manuscript previously published in Journal of Clinical Neuroscience 109 (2023), 44-49.
898
RF066: Pharmacological therapy of degenerative cervical myelopathy: a critical review of the literature
Miltiadis Georgiopoulos 1,2 , Jordan Levett 3 , Simon Martel 4 , Nikolaos Foroglou 5 , Carlo Santaguida 2 , Michael Weber 4 , Jeff Golan 2 , Ahmed Aoude 4 , Peter Jarzem 4 , Jean Ouellet 4 , Andreas Demetriades 6
1 Spinal Surgical Unit, Trauma and Orthopaedics, Swansea Bay University Health Board, Swansea, United Kingdom
2 Department of Neurology and Neurosurgery
3 Faculty of Medicine, University of Montreal, Montreal, Canada
4 Division of Orthopaedic Surgery, Department of Surgery, Spine Surgery Program, McGill University Montreal, Canada
5 Division of Neurosurgery, Medical School, Aristotle University of Thessaloniki, AHEPA University Hospital, Thessaloniki, Greece
6 Department of Neurosurgery, Royal Infirmary, Edinburgh, United Kingdom
Introduction: Although degenerative cervical myelopathy (DCM) is the most frequent spinal cord disorder in adults, resulting in significant morbidity and healthcare and societal burdens, there is not any established pharmacotherapy. Unfortunately, patients suffering from DCM will eventually undergo surgical treatment sooner or later. However, the literature on pharmacological treatment of DCM remains limited. Health professionals would be interested in pharmacological agents that may benefit mildly myelopathic patients or improve surgical outcomes. We aim to present a comprehensive and critical review of clinical and experimental studies on the pharmacological therapy of DCM. Material and Methods: We present a narrative review of all pharmacological agents that have been investigated so far for the treatment of DCM, either in patients or animal models. Results: Although Riluzole showed effectiveness in rat models, those results were not reproduced in patients with mild DCM. It has also been suggested that Cerebrolysin is a neuroprotective agent for myelopathy in animals, but the results of clinical trials were contradictory. Limaprost alfadex resulted in improvement of the motor function of myelopathic animal models and showed promising results in a small clinical trial. Glucocorticoids not only failed to demonstrate clinical benefits, but also resulted in adverse events. Furthermore, Cilostazol, anti-Fas ligand antibody, and Jingshu Keli showed promise in animal models, while erythropoietin, granulocyte colony-stimulating factor and limaprost alfadex displayed potential in both animal and human studies. All existing studies have presented weak clinical or experimental evidence. Conclusion: The abovementioned research on the pharmacotherapy of DCM targets ion channels, stem cell differentiation, inflammatory, vascular, and apoptotic pathways. Unfortunately, some pharmacological substances failed to exhibit good outcomes in clinical studies. What is more, promising but weak evidence presented by studies on patients should be reproduced by new clinical studies of sound methodology. The inherent nature and pathogenesis of DCM offer attractive prospects for developing neurodegenerative or neuroprotective agents that may hinder disease progression, delay surgical intervention, or improve surgical outcomes.
2200
RF067: Are postoperative neck pain and kyphotic change after laminoplasty affected by degree of facet joint degeneration?
Gumin Jeong 1 , Sehan Park 1 , Dong-Ho Lee 1
1 Department of Orthopedic Surgery, Asan Medical Center, Seoul, South Korea
Introduction: Laminoplasty performed for cervical myelopathy inevitably injures neck musculature which increases possibility of neck pain and postoperative kyphosis. Previous studies have demonstrated association between laminoplasty and postoperative neck pain, and suggest preoperative severe neck pain as a relative contraindication for laminoplasty. Facet joint degeneration (FJD) could cause medial branch irritation which could lead to neck pain and is another factor that could contribute to postoperative neck pain. Furthermore, cervical lordosis is a prerequisite for laminoplasty since it achieves cord decompression by posterior shifting. However, relationship between postoperative neck pain or kyphosis after laminoplasty and FJD have not been clarified. Therefore, the present study was conducted to elucidate whether FJD affects postoperative neck pain or kyphotic change after laminoplasty. Material and Methods: One-hundred and twenty-six consecutive patients who underwent laminoplasty and were follow-up for more than 2-year were retrospectively reviewed. Degree of FJD was assessed on preoperative CT images with 1-4 scale using previously reported grading system. The independent variables included patient characteristics, baseline/final radiological cervical sagittal parameters and baseline/final clinical scores(JOA score, NDI). Patients with moderate to severe neck pain at postoperative 2-year (neck pain VAS ≥ 4, severe neck pain group) were compared with patients with mild neck pain at postoperative 2-year (neck pain VAS < 4, mild neck pain group). Furthermore, patients who experienced kyphotic change more than 10 degrees of C2-C7 lordosis (kyphotic change group) after laminoplasty were compared with patients who did not suffer postoperative kyphotic change (non-kyphotic change group). Regression analyzes were performed to elucidate factors associated with postoperative neck pain and kyphotic change. Results: Ninety-nine patients (78.6%) were included in the mild neck pain group, while remaining 27 patients (21.4%) were included in the severe neck pain group. Preoperative degree of FJD was significantly greater in the severe neck pain group (p = 0.040), while cervical sagittal parameters and demographics did not demonstrate significant intergroup difference. Correlation analysis demonstrated that FJD grade was significantly associated with neck pain VAS at postoperative 2-years (r = 0.179, p = 0.045). Furthermore, Multivariate logistic regression analysis showed that FJD grade associated with postoperative severe neck pain (p = 0.046). Patient demographics, cervical sagittal parameter, and FJD grade did not demonstrate significant results when comparing non-kyphotic change group with kyphotic change group. Moreover, FJD grade was not associated with postoperative cervical kyphosis in logistic regression analysis (p = 0.769). Conclusion: Patients with pre-established FJD would be more likely to experience postoperative severe neck pain as demonstrated in this study. However, FJD was not associated with postoperative kyphosis after laminoplasty, and does not seem to affect cervical alignment aggravation. In conclusion, preoperative FJD was associated with postoperative neck pain after laminoplasty while it did not aggravate kyphotic change. Therefore, in cases when anterior approach and posterior approach could be both indicated, performing anterior approach would be preferred when preoperative severe FJD exists, since performing laminoplasty could aggravate postoperative neck pain.
1209
RF068: Radiographic and clinical outcomes in cervical degenerative spine conditions utilizing titanium coated PEEK interbody fusion devices
Jillian Mohn 1 , Madilyn Riegel 1 , Joseph Lee 2 , Leo Spector 3 , Benjamin Chen 4 , Bruce Darden 3 , Anthony Kwon 3 , Eric Laxer 3 , Alden Milam 3 , Alfred Rhyne 3 , Paul Bradley Segebarth 3 , Hallie Murray 1
1 Clinical Research, Tyber Medical, LLC, Bethlehem, USA
2 Rothman Orthopaedic Institute, Tarrytown, USA
3 Spine, OrthoCarolina, Charlotte, USA
4 Orthopedic Surgery, Spine Surgery, MultiCare, Puyallup, USA
Introduction: Next generation interbody fusion devices made with polyetheretherketone (PEEK), an organic thermoplastic polymer, and porous titanium coating (ProTi) to treat patients with cervical degenerative spine conditions have been FDA cleared and CE marked for use. Preclinical research has shown significantly accelerated bony deposition on ProTi devices compared to titanium or PEEK alone1. However, clinical research on these devices is limited. Therefore, the objective of this study was to assess clinical and radiographic outcomes for subjects who received the ProTi interbody fusion devices in the treatment of degenerative spine conditions to evaluate safety and performance. Material and Methods: Institutional Review Board approval was obtained to perform a retrospective and prospective registry gathering data on subjects treated with ProTi interbody fusion devices to correct degenerative spine conditions. Subjects were evaluated for clinical healing and radiographic fusion. Patient reported outcome measurements (PROMs), including the Neck Disability Index (NDI) and Visual Analog Scale (VAS), assessed patient functionality and pain before and after treatment in a subset of subjects. Statistical significance was calculated between pre-operative and final post-operative measurements using a two-tailed, paired T-test with significance set at p < 0.05. Results: Included in the analysis were 54 patients who underwent a 1-level, 2-level, or 3-level fusion. Results showed 98.14% (53/54) of subjects achieved radiographic fusion, with 1 subject undergoing a 3-level fusion achieving fusion at 2-levels and pseudarthrosis at the third level. Additionally, 3 subjects (5.5%) had subsidence, 2 subjects (3.7%) had adjacent level disc disease (1 subject required revision surgery), and 1 subject had dysphagia that resolved by 3.5 months post-operative. No other adverse events were reported. Radiographically, patients achieved a mean time to fusion of 11.71 ± 6.73 months. A subset of subjects completed PROMs at pre-operative and final clinic visits (N = 25). Subjects demonstrated significant (p < 0.05) improvement in NDI scores (p = 0.002), VAS neck pain (p = 0.001), and VAS left upper extremity pain (p = 0.049) at their final visit; VAS right arm pain improved but was not statistically significant (p = 0.134). Clinical outcomes supported the radiographic findings with pain improvement and/or resolution and alleviation of extremity motor, sensory and reflex deficits. Conclusion: This early analysis in an on-going study was the first to show significant improvement in patient functionality and pain following treatment with ProTi interbody fusion devices for degenerative cervical spine conditions. While additional research is required to fully evaluate the ProTi interbody fusion devices, early evidence supports the ability of these devices to obtain solid cervical fusion.
References
1. Hickey et al. Colloids and Surfaces B: Biointerfaces 2019; 175: 509-516.
1228
RF069: Prospective randomized control trial to compare the role of injection cerebrolysin for 10 days duration against placebo in operated cases of degenerative cervical myelopathy
Atif Naseem 1 , Ayush Sharma 1 , Harsh Agrawal 1
1 Orthopaedics and Spine Surgery, Dr. Babasaheb Ambedkar Memorial Hospital, Byculla, Mumbai, Maharashtra, Mumbai, India
Introduction: Cerebrolysin has been extensively researched with variable success in neurodegenerative pathologies. There has been only one study in published literature till date that has studied role of cerebrolysin in Degenerative Cervical Myelopathy (DCM) in conservatively managed patients but none in the patients treated surgically Previous research has concluded that superior functional outcomes are achieved with the use of cerebrolysin in surgically treated patients of DCM for 21 days. Our study has been conducted to analyze the use of this drug for a shorter duration (10 days) and compare its clinical efficacy. Material and Methods: Ninety operated cases of mild to severe DCM were randomized into two groups. Sixty patients received the injection Cerebrolysin for 10 days postoperatively. The remaining 30 patients received a placebo. Functional outcomes were measured using modified Japanese Orthopaedic Association (mJOA) scores and visual analogue scale (VAS). The American Spinal Injury Association (ASIA) scale was used to document neurological recovery. Hand function was assessed by measuring the grip strength and the upper limb function score the upper extremity motor mJOA plus upper extremity sensory mJOA score. Assessments were performed and preoperatively and postoperatively and at one-month, three-month, six-month, and one-year following surgery. Results: Preoperative mJOA and VAS scores were comparable in both groups (p > 0.05). Both groups experienced an improvement in mJOA and VAS scores at all time-points during follow-up as compared with preoperative scores. However, the cerebrolysin group demonstrated significantly greater mJOA scores (16.37 ± 1) when compared with the placebo (15.2 ± 1.8) at one-year followup (p < 0.0001). Neurological improvement with cerebrolysin therapy was also superior (p = 0.04). No significant adverse reactions were documented. Conclusion: Injection cerebrolysin, when administered for 10 days postoperatively, can result in significantly greater neurological improvement and hand function in patients with DCM who also receive surgery.
1866
RF070: Comparative analysis of the Three Cervical Vertebral Bone Quality Score (C-VBQ) Methodologies and their Correlations to the Lumbar Vertebral Bone Quality Score (VBQ)
Mohamed Soliman 1 , Alexander Aguirre 1 , Cathleen Kuo 1 , Esteban Quiceno Restrepo 1 , Asham Khan 1 , John Pollina 1 , Jeffrey Mullin 1
1 Neurosurgery, University at Buffalo Neurosurgery, Buffalo, USA
Introduction: Common complications after spinal fusion, such as pseudoarthrosis, cage subsidence, or instrumentation failure, are affected by the patients’ bone quality. The cervical vertebral bone quality (C-VBQ) score, a magnetic resonance imaging-based adaption of the lumbar vertebral bone quality (VBQ) score, was developed by three separate research groups simultaneously to evaluate bone quality in cervical spinal fusion patients. We present the first analysis comparing these scoring methods to the well validated VBQ score. Materials and Methods: A retrospective analysis of data for consecutive patients who underwent spine surgery at a single institution was completed. The VBQ score was calculated using the Ehresman et al. method. The C-VBQ scores, named according to placement of the region of interest within the cerebral spinal fluid, were calculated separately using the methods of Soliman et al. (C2-VBQ), Razzouk et al. (C5-VBQ), and Huang et al. (T1-VBQ). Linear regression models were utilized to evaluate correlations to the VBQ score. Results: A total of 105 patients were identified (mean age, 57.0 ± 11.9 years; women, 50.5%). Mean scores were C2-VBQ, 2.37 ± 0.55; C5-VBQ, 2.36 ± 0.61; and T1-VBQ, 2.64 ± 0.68. The C-VBQ scores for the C2 level were significantly higher than those for the C3-C6 levels (3.18 ± 0.96 vs. 2.63 ± 0.77, p < .001), whereas the C7 level was found to have significantly lower C-VBQ scores (2.42 ± 0.78 vs. 2.63 ± 0.77, p = .04). The C2-VBQ (r = 0.63) score had the strongest correlation to the VBQ score, compared to the C5-VBQ (r = 0.41) and T1-VBQ (r = 0.43) (p < .001). Conclusions: This study demonstrates that the C2-VBQ had the strongest correlation to the lumbar VBQ score among all the C-VBQ scores.
2435
RF071: Single-door laminoplasty and internal fixation for the treatment of multi-level cervical spondylotic myelopathy with poor cervical physiological curvature
Long Tang 1,2 , Jiazhuang Zheng 1
1 Spine Surgery, Suining Central Hospital, Suining, China
2 Neurosurgery, Technical University of Munich, Klinikum rechts der Isar, Munich, Germany
Introduction: Multi-level cervical spondylotic myelopathy (CSM) is a multi-segmental spinal cord compressive lesion caused by cervical spine degeneration, ossification of the posterior longitudinal ligament (OPLL), and cervical spinal stenosis (CSS) that can lead to spinal cord compression leading to disability and paralysis. Anterior surgery is safe and classic that can improve cervical curvature, but with a high incidence of complications. Posterior surgery can improve neurological function through indirect decompression of the spinal cord. However, some studies have reported that there is a risk of increased cervical lordosis curvature after posterior surgery with the results that are often unsatisfactory for patients with poor cervical physiological curvature. So we have studied the early clinical efficacy of posterior cervical internal fixation combined with single-door laminoplasty in the treatment of multi-level CSM with poor cervical physiological curvature. Material and Methods: From January 2015 to January 2019, there were 33 patients with multi-segmental CSM with poor cervical physiological curvature were treated. There were 9 cases of multi-segmental disc herniation, 3 cases with ossification of the ligamentum flavum, 9 cases with OPLL, 10 cases with developmental CSS, and 2 cases with cervical spine instability. The duration of the disease is 12-48 months. All cases underwent posterior internal fixation with single-door laminoplasty. Among them, 28 cases had titanium plates fixed on the door-opening side, and 5 cases had silk thread suspension. The visual analogue scale (VAS) was used to evaluate the pain improvement, and the Japanese Orthopedic Association (JOA) score was used to evaluate the neurological function before and 1 week, 3 months, the last follow-up after surgery. The cervical CT was used to measure the sagittal diameter and area of the spinal canal at the surgical segment, and the MRI was used to measure the spinal cord retrograde distance to evaluate the decompression situation. also, the cervical spine X-rays was used to measure the C2-C7 Cobb angle to evaluate the cervical physiological curvature. In addition, the complications were recorded. Results: All patients successfully completed the operation and were followed up for 6-24 months. There was no case with door shaft breakage or re-closing of the door. There were 1 case of vertebral artery injury without obvious sequelae, 3 cases with C5 nerve root symptoms, and 2 cases with axial symptoms which disappeared with rehabilitation exercises at 6 months after surgery. At the last follow-up, the VAS (2.1 ± 0.9) was significantly lower than that before surgery (5.6 ± 1.6) (p < 0.05), the JOA (13.6 ± 1.3) was significantly higher than that before surgery (7.6 ± 1.2) (p < 0.05), the postoperative C2-C7 Cobb angle (14.6° ± 5.4°) was significantly increased compared with the preoperative (7.2° ± 3.5°) (p<0.05). The postoperative cervical CT and MRI showed that the spinal cord obtained adequate decompression. Conclusion: The single-door laminoplasty with posterior internal fixation to treat multi-level CSM with poor cervical physiological curvature is a safe and reliable operation that can effectively improve the symptoms and signs caused by spinal cord compression and the cervical physiological curvature of the cervical spine.
2374
RF072: Comparison of clinical outcomes of muscle-preserving expansive open-door laminoplasty and conventional expansive open-door laminoplasty in the treatment of multilevel cervical spondylotic myelopathy: a retrospective cohort study
Hao-Wen Chen 1,2 , Kuang-Ting Yeh 1 , Wen-Tien Wu 1 , Ing-Ho Chen 1 , Tzai-Chu Yu 1
1 Orthopaedic, Hualien Tzu Chi Hospital, Hualien City, Taiwan
2 Institute of Medical Sciences, Tzu Chi University, Hualien City, Taiwan
Introduction: Expansive open-door laminoplasty (EODL) has made an appropriate solution for multilevel cervical spondylotic myelopathy (MCSM) with non-kyphotic alignment. However, axial neck pain remains an unsolved issue. This study aimed to evaluate the efficacy and the clinical outcome between the conventional EODL via midline approach and the EODL with muscle-preserving osteotomy in patients with MCSM. Material and Methods: From 2017 to 2022, 100 patients who underwent EODL for three or more levels of spinal cord compression between C2 to C7 vertebral levels were enrolled. Fifty received EODL with a conventional midline approach, while a para-midline muscle-preserving osteotomy approach was applied to another 50 cases to achieve the EODL. The primary outcome was the Japanese Orthopedic Association (JOA) score change from the baseline to 5-year post-operation. The secondary outcome included changes in the Visual Analog Score (VAS), Neck Disability Index (NDI), and radiographic parameters. Results: The demographic data were comparable between groups. The change in JOA scores revealed no significant difference between groups at three times point postoperatively. At the same time, the improvement of VAS and NDI was more remarkable in the muscle-reserving EODL group. The sagittal range of motion and cervical lordosis decreased gradually in both groups, but only those in the conventional EODL groups reached a significant level of difference. Conclusion: Benefiting from the muscle-preserving osteotomy approach of EODL, the remaining intact unilateral Capitus muscle guarantees a comparative functional improvement with better sagittal balance. The muscle-preserving EODL could provide a comparable functional outcome with a better alignment for patients with MCSM in a midterm 5-year follow-up.
RFP05: Thoracolumbar & Other Trauma
2490
RF073: Health economic analysis of neurologically intact thoracolumbar A3 and A4 fractures reveals surgery to be the dominant strategy over non-surgical treatment
Marcel F. Dvorak 1 , Cumhur Oner 2 , Alexander Joeris 3 , Alex Vaccaro 4 , Lorin Benneker 5 , Shanmuganathan Rajasekaran 6 , Mohammad El-Sharkawi 7 , Eugen Cezar Popescu 8 , Jin Tee 9 , Jerome Paquet 10 , John France 11 , Richard Allen 12 , William Lavalle 13 , Klaus Schnake 14
1 Department of Orthopaedic Surgery, University of British Columbia, Vancouver, Canada
2 University Medical Center, Utrecht, The Netherlands
3 AO Foundation, AO Innovation Translation Center, Davos, Switzerland
4 Department of Orthopaedic Surgery, Thomas Jefferson University Hospital, Philadelphia, USA
5 University of Bern, Sonnenhof Spital, Bern, Switzerland
6 Department of Orthopaedics and Spine Surgery,Ganga Hospital, Coimbatore, India
7 Department of Orthopaedic and Trauma Surgery, Assiut University Medical School, Assuit, Egypt
8 Department of Orthopaedic Surgery, Prof. Dr. N. Oblu” Emergency Hospital, Iasi, Romania
9 Department of Neurosurgery, National Trauma Research Institute (NTRI), Melbourne, Australia
10 Department of Surgery, CHU de Quebec, Université Laval, Montreal, Canada
11 Department of Orthopaedic Surgery, West Virginia University, Morgantown, USA
12 Department of Orthopaedic Surgery, University of California, San Diego, USA
13 Department of Orthopedics, SUNY Upstate Medical University, Syracuse, USA
14 Center for Spinal and Scoliosis Surgery, Malteser Waldkrankenhaus St. Marien, Erlangen, Germany
Introduction: Investigators have failed to demonstrate a clinical outcome benefit of surgical treatment compared to non-surgical care for patients with thoracolumbar A3/4 neurologically intact fractures. A detailed health economic analysis has not previously been performed on these cohorts. Material and Methods: Our objective was to determine the cost-utility of surgical treatment versus non-surgical treatment of thoracolumbar (TL) burst fractures in neurologically intact patients from the AO Spine: Thoracolumbar (TL) burst fracture Study (AO Spine A3, A4) from a societal perspective with a one, two-year and working lifetime time horizon (65 years of age was considered as retirement age), including all regions/hospitals. Utility scores were obtained from the EQ-5D-3L from discharge, 6 weeks, 3-, 6-, 12-, and 24-months post-treatment. Quality Adjusted Life Years (QALYs) were derived from the EQ-5D-3L utility score and life expectancy. Direct and indirect costs were assessed from resource utilization data and patient diaries collected every 2 weeks that contained the Indirect Cost Questionnaire to document any productivity losses, caregiver burden and days of work lost. Incremental Cost-Effectiveness Ratio (ICER) was calculated by dividing total difference in costs by the difference in QALYs between the two treatment groups. A discounting of 3% was applied for costs as well as utilities over time. Results: Surgical patients were more likely to come from Europe, the Middle East and India while non-surgical treatment was more common in North America and Australia. At 1-year the non-surgical patients were twice as likely to be using opioids and had more days lost from work (95.82 surgical vs 115.52 non-surgical) and more caregiver days (2.19 surgical vs 14.53 non-surgical) than the surgical patients. The difference in QALY between surgical and non-surgical was only 0.02 and the costs in USD were $33,026.18 (surgical) and $29,193.22 (non-surgical). The ICER for surgical treatment was $191,648.00 US$ per QALY. At 2 years, indirect costs for non-surgical patients had increased to over $10,000 more than for surgical ($20,903.66 surgical and $31,560.46 non-surgical). These indirect costs (lost work days and caregiver burden) led to the total cost for non-surgical care ($37,056.19) being higher than that for surgical care ($36,476.62) and led to an ICER of -$28,978.50, i.e. surgery was the dominant treatment modality. Looking at the working lifetime time horizon and only considering work-days projected to be lost and not caregiver days, the cost of surgical care (direct and indirect) was $112,497.50 while the cost of non-surgical care increased to $121,177.76. Over the working lifetime, the ICER was -$25,530.18, i.e. surgery was the dominant treatment modality again. Conclusion: While surgical and non-surgical treatment of AO A3 and A4 thoracolumbar burst fractures with normal neurology appear to have similar clinical outcomes after two years following treatment, a cost-utility analysis revealed surgery to be the dominant strategy after two years and over a working lifetime time horizon from a societal perspective, mainly driven by caregiver burden in the first two years after injury and lost days from work over the working lifetime for non-surgical patients.
2419
RF074: Comparison of clinical effect between vertebroplasty and vertebroplasty combined with cortical bone tract screws for the treatment of osteoporotic thoractlumbar compression fracture
Der Cherng Chen 1
1 Neurosurgery, China Medical University Hospital, Taichung, Taiwan
Introduction: Cortical bone trajectory (CBT) is an alternative for pedicle screw fixation, especially in osteoporotic patients. We present the clinical effects between vertebroplasty (VP) and VP combined with CBT screw fixation for the treatment of osteoporotic thoracolumbar junction compression fractures. To compare the clinical effects between VP and VP combined with CBT screw fixation for the treatment of osteoporotic thoracolumbar junction compression fractures. Material and Methods: In the previous study, 12 consecutive patients with osteoporotic thoracolumbar junction fracture who underwent VP with CBT (VP+CBT group) were reviewed. Results were compared with 17 consecutive patients who underwent VP alone (VP group) in this study. All patients were enrolled from 2015 to 2018. Patients’ demographics were recorded. Results: Cobb’s angle of the VP+CBT group was significantly higher than that of the VP group (VP; 27.12 ± 10.90 vs. VP+CBT; 18.83 ± 9.99, p = 0.0134*). Changes in Cobb’s angle of the VP group were slightly higher than those of the VP+CBT group, although the two groups had no significant differences (p = 0.0795). Moreover, significant changes in body height were observed in both groups (VP; p < 0.0046** and VP+CBT; p = 0.0073**). However, a decrease in body height was observed in the VP group in the final follow-up (p < 0.0001****). Conclusion: Data supported the evidence that CBT instrumentation combined with percutaneous VP efficiently maintained the fractured vertebral body height and kyphotic sagittal Cobb’s angle for the treatment of osteoporotic thoracolumbar junction fractures. Moreover, it could prevent subsequently adjacent fractures during follow-up periods.
904
RF075: Evaluation of dynamic fracture mobility ofsub acute osteoporotic vertebral fractures through combination of prone cross-table lateral radiographs and standing lateral radiographs
Ashish Jain 1,2
1 Orthopaedics, Hind Institute of Medical Sciences, Barabanki, India
2 Spine Surgery, Globe Medicare, Lucknow, India
Introduction: Osteoporotic Vertebral column fractures constitute a major health problem in post menopausal and geriatric population. On presentation, the duration of such fractures is often unknown even though they present with significant pain in Spine. This makes it difficult to formulate a standard treatment plan. Use of Prone cross lateral radiographs is an established diagnostic tool. We intend to use this radiograph and compare it with standing radiographs to asses nature and extent of dynamic fracture mobility and establishing its role in understanding Kyphoplasty as a suitable modality in cases of dynamic fracture mobility in non acute cases. Material and Methods: We inducted 80 patients of non acute neurologically intact Osteoporotic vertebral column fractures in our study over a period of 2 years. It was a prospective study of consecutive patients of Osteoporotic Vertebral column fractures which were subjected to Prone cross lateral and Straight standing lateral radiographs. Any patients with pre-existing neurological deficits were excluded from study. We evaluated demography, bone densitometry, Vertebral wedge angles (VWA), Anterior vertebral height, pain on VAS scale on standing and supine positions. Patients with established dynamic fracture mobility were treated with Kyphoplasty. After 6 weeks all patients were again subjected to above radiographic assessments. Results: The patients were aged between 61 years and 92 years. Dynamic fracture mobility was demonstrated in 44% of patients. Average pain was 4.98 ± 1.34 in standing radiographs compared to 4.18 ± 1.18 in prone radiographs. The average vertebral height in standing radiographs (15.6 mm ± 6.8 mm) was found to be 28% less than the lateral radiographs in prone lateral radiographs (20.01 mm ± 6.13 mm). The increase in post operative restoration of vertebral height was found to be higher in prone lateral radiographs (5.32 mm ± 2.52 mm) than Standing radiographs (4.12 mm ± 2.98 mm). Conclusion: Prone lateral radiographs provide for a more accurate assessment of the nature of dynamic fracture mobility when combined with standing lateral radiographs in sub acute osteoporotic vertebral compression fractures and provoke less pain during evaluation. They also provide a better estimate of restoration of vertebral height after Kyphoplasty as compared to standing radiographs.
253
RF076: Kyphoplasty versus vertebroplasty in the treatment of vertebral compression fractures in the treatment of vertebral compression fractures in patients with osteoporosis: a meta-analysis
Robert Meves 1
1 Orthopedic and Traumathology, Santa Casa of Sao Paulo, Sao Paulo, Brazil
Introduction: Vertebral fracture is the main complication of osteoporosis and occurs frequently in the elderly. Conservative treatment is the first choice for osteoporotic vertebral compression fractures (OVCF) but for persisting painful cases, vertebral cemented percutaneous augmentation techniques such as vertebroplasty and kyphoplasty are indicated. We performed a systematic review to compare clinical and radiological outcomes of both methods. Materials & Methods: A systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Cochrane Handbook of Systematic Reviews. The PICO search strategy was: Population- Patients with OVCFs; Intervention- Kyphoplasty; Control- Vertebroplasty; Outcomes- Pain, Cement Leakage, Vertebral Body Height, Adjacent level fractures, Oswestry (ODI) and SF36. Results: Seven articles were included in qualitative analysis, only randomized controlled trials. 450 patients were treated with vertebroplasty (VP) and 469 with kyphoplasty (KP). The leakage rate of the VP group was 63% versus 14% of the KP. However, it did not reach 5% level of statistical significance to differ Cement Leakage rate between KP and VP. The Visual Analogue Scale (VAS), ODI and SF-36 outcomes were evaluated considering 6-months and 1-year follow-up results and we could not point out differences between treatments at a significance level of 5%. Finally KP presents average 0.71 cm higher values than VP for vertebral body height restoration, with 95% CI. Conclusions: In this systematic review kyphoplasty was superior to vertebroplasty for vertebral body height gain. There was no statistically significant superiority between the two methods for cement leakage and other clinical outcomes.
References
1. Gaitanis IN, Hadjipavlou AG, Katonis PG, Tzermiadianos MN, Pasku DS, Patwardhan AG. Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J 2005; 14: 250-260.
2. Ensrud KE, Schousboe JT. Clinical practice - Vertebral Fractures 2011.
3. Voormolen MHJ. Kyphoplasty. In: Adv. COURSES ESNR Meet. 2011 - Neuroradiol. Cambridge University Press 2011; S203-S205.
4. Sambrook P, Cooper C. Osteoporosis 2006.
5. Chandra RV, Mmed F, Yoo AJ, Hirsch JA. Vertebral augmentation: Update on safety, efficacy, cost effectiveness and increased survival? Pain Physician 2013; 16: 309-320.
6. Nanes MS, Kallen CB. Osteoporosis. In: Semin. Nucl. Med. Springer International Publishing 2014; 1-13.
7. McConnell CT, Wippold FJ, Ray CE, et al. ACR appropriateness criteria management of vertebral compression fractures. J Am Coll Radiol 2014; 11: 757-763.
8. Chandra RV, Meyers PM, Hirsch JA, et al. Vertebral augmentation: Report of the Standards and Guidelines Committee of the Society of NeuroInterventional Surgery. J Neurointerv Surg 2014; 6: 7-15.
9. Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): Conservative treatment versus balloon kyphoplasty. Spine J 2012; 12: 998-1005.
10. Wang H, Sribastav S Sen, et al. Systematic review comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: a meta-analysis of the literature. 2015.
11. Gu CN, Brinjikji W, Evans AJ, Murad MH, Kallmes DF. Outcomes of vertebroplasty compared with kyphoplasty: A systematic review and meta-analysis. J Neurointerv Surg 2015; 8:636-642.
12. Xiao H, Yang J, Feng X, et al. Comparing complications of vertebroplasty and kyphoplasty for treating osteoporotic vertebral compression fractures: a meta-analysis of the randomized and non-randomized controlled studies. Eur J Orthop Surg Traumatol 2014; 25: 77-85.
13. Zhao S, Xu CY, Zhu AR, et al. Comparison of the efficacy and safety of 3 treatments for patients with osteoporotic vertebral compression fractures: A network meta-analysis. Med (USA) 2017. https://doi.org/10.1097/MD.0000000000007328
14. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: 1006-1012.
15. Higgins J, Green Sally. Cochrane Handbook for Systematic Reviews of Interventions. 2008.
16. Vogl TJ, Pflugmacher R, Hierholzer J, et al. Cement directed kyphoplasty reduces cement leakage as compared with vertebroplasty: Results of a controlled, randomized trial. Spine (Phila Pa 1976) 2013; 38: 1730-1736.
17. Endres S, Badura A. Shield kyphoplasty through a unipedicular approach compared to vertebroplasty and balloon kyphoplasty in osteoporotic thoracolumbar fracture: A prospective randomized study. Orthop Traumatol Surg Res 2012; 98: 334-340.
18. Omidi-Kashani F, Samini F, Hasankhani EG, Kachooei AR, Toosi KZ, Golhasani-Keshtan F. Does percutaneous kyphoplasty have better functional outcome than vertebroplasty in single level osteoporotic compression fractures? A comparative prospective study. J Osteoporos 2013; 1-5
19. Wang CH, Ma JZ, Zhang CC, Nie L. Comparison of high-viscosity cement vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Pain Physician 2015; 18: E187–E194
20. Dohm M, Black CM, Dacre A, et al. A randomized trial comparing balloon kyphoplasty and vertebroplasty for vertebral compression fractures due to osteoporosis. Am J Neuroradiol 2014; 35: 2227-2236.
21. Liu JT, Li CS, Chang CS, Liao WJ. Long-term follow-up study of osteoporotic vertebral compression fracture treated using balloon kyphoplasty and vertebroplasty. J Neurosurg Spine 2015; 23: 94-98.
22. Liu JT, Liao WJ, Tan WC, et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: A prospective, comparative, and randomized clinical study. Osteoporos Int 2010; 21: 359-364.
23. Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 Statement : updated guidelines for reporting parallel group randomised trials. 2010.
24. Otten LA, Bornemnn R, Jansen TR, et al. Comparison of balloon kyphoplasty with the new Kiva(R) VCF system for the treatment of vertebral compression fractures. Pain Physician 2013; 16: E505-512.
25. Kruger A, Oberkircher L, Figiel J, et al. Height restoration of osteoporotic vertebral compression fractures using different intravertebral reduction devices : a cadaveric study. Spine J 2013; https://doi.org/10.1016/j.spinee.2013.06.094
26. Zhang L, Wang J, Feng X, et al. A comparison of high viscosity bone cement and low viscosity bone cement vertebroplasty for severe osteoporotic vertebral compression fractures. Clin Neurol Neurosurg 2015; 129: 10-16.
27. Meirhaeghe J Van, Bastian L, Boonen S, Ranstam J, Tillman JB, Wardlaw D. A randomized trial of balloon kyphoplasty and nonsurgical management for treating acute vertebral compression fractures vertebral body kyphosis correction and surgical parameters. Spine (Phila Pa 1976) 38: 971-983.
28. Boonen S, Van Meirhaeghe J, Bastian L, et al. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 2011; 26: 1627-1637.
29. Movrin I. Adjacent level fracture after osteoporotic vertebral compression fracture: A nonrandomized prospective study comparing balloon kyphoplasty with conservative therapy. Wiener Klin Wochenschr 2012; 124: 304-311.
30. Borgström F, Olafsson G, Ström O, Tillman JB, Wardlaw D, Boonen S, et al. The impact of different health dimensions on overall quality of life related to kyphoplasty and non-surgical management. Osteoporos Int 2013; 24: 1991-1999.
448
RF077: Correlation of clinical outcome and spinopelvic sagittal alignment after pedicle screw fixation of a thoracolumbar traumatic fractures
Saurabh Singh 1 , Himanshu Chaudhary 1 , Rahul Patel 1 , Rohit Saroj 1 , Prashant Kumar 1 , Sushit Sonu 1
1 Orthopedics, Institute of Medical Sciences, BHU, Varansi, India
Introduction: Thoracolumbar traumatic fractures manifest as pain and deformity of the spine, which are usually complicated by injury to the spinal cord. Spinal restoration and sagittal alignment of the spinopelvic area are increasingly valued as significant indicators of prognosis, determining improvement in clinical outcomes after surgical intervention. The present study was conducted to assess the sagittal alignment of the spine and pelvis before and after surgical treatment of a thoracolumbar traumatic fracture while providing an analysis of the functional outcome. Materials and Method: The present study was conducted on 50 patients, 31 males and 19 females, aged 18-70 years, who had thoraco-lumber vertebrae fractures. All patients were operated on using a posterior procedure involving transforaminal lumbar interbody fusion and pedicular fixation. Pre- and post-operative clinical and radiographic parameters were measured. The data obtained was subjected to statistical analysis using IBM SPSS version 20.0 at a significance level of p-value 0.05. Results: In the present study, the mean age of patients was 33.7 years, with a male predominance. L1 fractures were the most common. A significant change (p-value < 0.05) from pre-operative to post-operative periods was observed in relation to both regional kyphotic (RKA) and thoracolumbar (TLA) angles. A significant change in mean VAS and Oswestry disability index scores was recorded from day 1 to the 6th month. A significant difference (p-value < 0.05) was observed between VAS score with PI and RKA and between ODI score with PI, RKA, and TKA. Conclusion: The present study showed success with pedicle screw treatment in attaining good postoperative pain control and improvement in functional outcome of patients. Future studies are required to analyse various risk factors affecting the spine's sagittal balance.
1185
RF078: Thoracolumbar fractures with compromised neurology: Is direct decompression beneficial along with posterior spine stabilization
Shahrukhkhan Pathan 1 , Pratik Sidhdhapuria 1
1 Orthopaedics, Surat Municipal institute for Medical Education and Research, Surat, India
Introduction: There is a lack of standard treatment of care for traumatic thoracolumbar injury with compromised neurology. Posterior spinal stabilization is well studied and accepted by surgeons but to add direct decompression or laminectomy to it, is always a matter of debate. Indirect decompression with ligamentotaxis by posterior pedicle screws is enough for normal neurology, but in neurological deficit direct decompression can give full potential for spinal cord to recover. Material and Methods: Retrospective analysis of data collected from January 2021 to May 2023 at tertiary care hospital was done and all the patients with thoracolumbar fracture with compromised neurology with atleast 6 months of follow-up were included. Patients were divided in two groups; one group were operated with pedical screw fixation only (indirect decompression) and another group operated with pedical screw fixation with laminectomy (direct decompression). All patients were analysed preoperatively and post operatively at 1 month and at 6 months by ASIA grading for neurological involvement and Xrays and MRI for radiological outcomes. Results: 26 patients were included in the study, 16 patients were treated with posterior screw fixation and 10 were treated with fixation with direct decompression. Mean age of the patients were 40.4 years and 15 (57.7%) were males. 19 (73.1%) patients were burst fracture and 16 (61.5%) fractures were at dorso-lumbar junction. 10 (38.5%) patients had ASIA grade C preoperatively. Both groups have similar improvement in clinical and radiological outcome at 6 months (p < 0.05). Conclusion: Radiological and clinical outcome of both the group were found comparable at the end of 6 months. However, large randomized controlled study is needed to establish posterior screw fixation with indirect decompression as standard of treatment.
2039
RF079: Delayed fixation of unstable thoraco lumbar burst fracture incuding fractured vertebra: Does it always results worse outcome? Our experience in NITOR, Dhaka
Provash Chandra Saha 1 , Rezaul Karim 1
1 Spine, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
Introduction: There is little consensus regarding the optimal timing of traumatic spine fracture fixation. Neurological outcome after thoraco lumbar spine fracture is a subject of debate. The optimum efficacy is observed when performed within 12 hours of the injury. There is little number of studies showing outcome of delayed fixation. A randomized controlled trial to evaluate early versus late stabilization is difficult to perform especially in the heavily loaded setting of National Institute of Traumatology and Orthopaedic Rehabilitation, NITOR, Dhaka as early fixation is difficult to schedule. Short segment fixation of the fracture level gradually replacing the traditional long segment instrumentation. It decreases the number of motion segments sacrificed in the fusion process. Materials and Methods: Study Periods was December 2016 to June 2021. Study place was NITOR. Study design Prospective observational study. Among 36 patients, 21 are male and female 15. Inclusions criteria were Magerl Type A, Local kyphosis of more than 25°, ASIA Grade B, C and D neurology, fracture level limited to D10–L2, duration of injury - 3 weeks or less. Exclusion criteria were, Magerl Type B, C fractures, ASIA A neurology, duration of injury less than 3 days and more than 3 weeks. Patients were evaluated according to their age, gender, mode of injury, fracture level, fracture type according to the Magerl classification, duration between injury and surgery, neurologic status according to the ASIA grading system, Beck index, ODI Index, Denis work scale, and follow-up. Results: Among all patients 30 patients showed neurological improvements except 6 cases. Pain was improved according to VAS scale in most of the patients. All patients showed radiological sign of bony union in all cases at follow up till date. All patients gained improved scoring of ODI index except 7cases with ASIA C neurology. All patients gained improved Dennis working scale except 6 cases of ASIA C neurology. Conclusion: Results of delayed fixation (within 3 weeks) of thoraco lumbar Burst fracture including fractured vertebra showed satisfactory outcome regarding kyphosis correction, neurological improvement and functional recovery.
1929
RF080: Minimally invasive surgery for traumatic thoracolumbar fractures: a cross-sectional study of spine surgeons
Guillermo Ricciardi 1 , Ignacio Cirillo 2 , Juan P. Cabrera Cousiño 3 , Alfredo Guiroy 4 , Charles Carazzo 5 , Ratko Yurac 6
1 Centro Médico Fitz Roy, Ciudad de Buenos Aires, Argentina
2 Hospital del Trabajador, Chile
3 Hospital Clínico Regional de Concepción, Chile
4 Elite Spine Health and Wellness Center, Florida, USA
5 São Vicente de Paulo Hospital, Brazil
6 Clinica Alemana, Santiago, Chile
Introduction: To describe the perceived feasibility of minimally invasive surgical treatment of thoracolumbar fractures among spine surgeons in Latin American centers. Material and Methods: This is a cross-sectional study on minimally invasive surgical treatment for unstable thoracolumbar fractures. We conducted an online survey of spine surgeons working in Latin American centers, administered between December 16, 2022 and January 15, 2023. A non-probabilistic sample was selected (snowball sampling). A questionnaire was sent by email and other messaging applications. Results: Data were extracted from 134 surgeons. The majority of the respondents were from Brazil (n = 30, 22.4%), Mexico (n = 24, 17.9%), Argentina (n = 22, 16.4%), and Chile (n = 15, 11.2%). Their mean age was 46.53 years (SD, 9.7; range 31-67) and almost all were male (n = 128, 95.5%). Most respondents were orthopedists (n = 85, 63.4%) or neurosurgeons (n = 49, 36.9%). Most of the respondents (n = 110, 82.1%) reported at least some difficulty using minimally invasive techniques for thoracolumbar fractures. It should be noted that there were significant regional differences between the surgeons’ responses (p = 0.017). Chilean surgeons reported better outcomes than others. Conclusion: Spinal surgeons from Latin American centers have identified challenges and obstacles to performing minimally invasive surgery for thoracolumbar trauma. The survey found that a majority of respondents experienced some level of difficulty, with regional variations. The most frequently reported difficulties were the high cost of the procedure, patient insurance restrictions and long insurance approval times.
2441
RF081: Falls in the elderly have 50% higher 30-day mortality: an underestimated lethal cause of spine trauma
Zion Hwang 1,2,3 , Tesfaladet Kurban 2 , Bisola Ajayi 2 , Emily Tsang 2 , Priyanshu Saha 4 , Jason Bernard 2 , Timothy Bishop 2 , Darren Lui 2,4
1 Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust, United Kingdom
2 St. George's University Hospital, London, United Kingdom
3 University of Sheffield, United Kingdom
4 St. George's University of London, United Kingdom
Introduction: Spine trauma are a significant presentation to trauma centres. This cohort of patients often present with polytrauma from high energy mechanisms of injury, and these can result in poorer outcomes. It is important for centres to know the common mechanisms of these type of injuries to inform their resources and management decisions. Methods: A review of all trauma patients admitted to a level 1 major trauma centre between 2018-2022 period was conducted using electronic patient database. Subsequently, patients with spinal injuries, their demographics and the characteristics of the trauma were identified from this dataset. Results: A total of 862 patients with traumatic spinal injuries were found. 559 (65%) were male, the average age was 57 years old, and 581 (67%) had poly-injuries. 220 (26%) patients were admitted to intensive care unit (ICU), and 30-day mortality was at 10% (83/862). We assessed the mechanisms of injury. 500 (58%) were from falls: 20% from < 5 feet, 30% from 5-15 feet, and 8% from > 15 feet height. 265 (31%) were from road traffic collisions: these were 6% cyclist, 11% car, 8% motorbike/moped, and 6% pedestrian. 97 (11%) had injuries relating to ‘other’ or unknown mechanisms of injury. Out of the 500 patients with spinal injuries from falls, 271 (54%) were elderly (> 65 years). Out of the 271 elderly spine trauma patients, 188 (69%) had poly-injury including: 112 (41%) head injury, 69 (25%) limb, 133 (49%) thorax, 24 (9%) abdomen, 35 (13%) pelvis. We found 53 (20%) had ITU admissions, with an average length of 6 days stay in ITU, and 30-day mortality in elderly patient with spine trauma was at 15% (42/271). Conclusion: 7 out of 10 spine trauma patients present with poly-injuries, and more than one quarter go onto have adverse outcomes. Falls from heights under 15 feet are the main cause of these injuries, and over half of these patients are elderly. Many of these patients present with accompanying head and thoracic injuries so there should be a high index of suspicion for intracerebral injury and underlying respiratory disease respectively. These patients have a 50% higher chance of dying, suggesting that these are risk factors for poorer outcomes. Therefore, early investigation and treatment for these complications is paramount.
2074
RF082: Spotlight on drain or no drain after lumbar discectomy? A comparative study on surgical outcome
Sandesh Agarawal 1 , Manoj Ramachandriah 1
1 Department of Orthopaedics, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, India
Background: A major issue in spinal surgery is avoiding complications. Hematomas in the surgical wound are a complication that can occasionally necessitate revision surgery and affect 0.2% to 2.9% of patients. Hematomas may be asymptomatic or symptomatic depending on the presence of spinal cord or nerve root compression, increased wound tension, delayed healing, wound infection, or any combination of these factors. Aims and Objectives: To assess the incidence of wound infections after single level lumbar discectomy in patients with or without post-operative wound drainage.To compare functional outcome in terms of VAS score and ODI score between the two groups. Methodology: A Hospital based retrospective study was conducted among 84 patients who underwent elective lumbar spine surgery at Department of Orthopedics, R.L. Jalappa Hospital, Tamaka, and Kolar from May 2022 - April 2023. Results: The mean age among group A was 59.76 + 10.8 years and among group B was 62.24 + 9.7 years. The mean hospital stay duration among group A was 10.6 + 3.4 days and among group B was 12.8 + 4.1 days. Out of total, in group A 25 were males and 17 were females, while in group B 23 were males and 19 were females. Conclusion: Although many surgeons are concerned about postoperative infection by surgical drainage, no difference in wound healing or postoperative neurological deficiency has been detected. Nor has there been any rise in infection rate. Surgical drains, on the other hand, have a positive impact in lowering infection rates by hematoma. Surgery drain tip cultures can be used as an efficient a technique for postoperative infection detection.
Keywords: drain; epidural hematoma; lumbar discectomy; VAS Score, ODS score.
1667
RF083: The triangular osteosynthesis for traumatic spinopelvic instability. A consecutive series
Lương Quang 1
1 Spine Unit, Department of Neuro-spine Surgery, Saint Paul General Hospital, Hà Nội, Vietnam
Traumatic spinopelvic instabilities are rare and hard to diagnose and treat. Sacropelvic fractures with an H- or U-shaped line are severely unstable due to a dissociation of the spine and the upper body of the sacrum from the pelvis. They are commonly due to high-energy trauma events, with severe injuries in 80% of cases.
Objective: To evaluate the clinical outcomes of traumatic spinopelvic instability (TSI) treated with triangular osteosynthesis. Materials and Methods: 25 consecutive patients of TSI were admitted to our hospital and included in the study from July 2018 to April 2022, and the medical records of patients were reviewed retrospectively. Patients were followed up for at least 03 months. Fracture lines were evaluated using the Denis, Isler, and Roy-Camille classification. Neuro-impairment was scored using Gibbon's type, and the clinical outcome of fracture was assessed with Majeed function assessment at the last follow-up. The following data were also ascertained from the patient's medical records: gender, age, etiology, associated injuries, level of surgery, type of surgery, complications, and trauma mechanism. Results: There were 19 men and six women with an average age of 41.2 ± 15.7 years (range, 16 - 73 years). A total of 7 cases were caused by falling, and traffic accidents caused 18 patients. All sacral fractures had associated injuries. According to Denis's classification, there were 11 cases of Zone I, 7 cases of Zone II, and 7 of Zone III. According to Isler's classification, there were 2 cases of type I, 3 cases of type II, and 2 cases of type III. According to Roy-Camille classification, there were 2 cases of type I, 3 cases of type II, and 2 cases of type III. Sacro-iliac joint dissociation: There were 6 cases of injured bilaterally and 11 unilaterally injured. Triangular osteosynthesis was applied for all patients, with 14 cases bilaterally and 11 cases unilaterally. All patients were followed up continuously within an average of 23.1 ± 14.3 months (3 - 47 months). According to the Majeed function evaluation, 15 cases were classified as excellent, six as good, three as fair, and one as bad. The average Gibbons score changed from 1.2 ± 0.2 preoperatively to 0.5 ± 0.1 postoperatively, with a significant difference (t = 2.19, p < 0.05). Three of the 25 cases needed internal pelvic arterial preop-embolization. 5 points suffered from surgical site infection, but only one patient required debridement re-operatively. Conclusion: Triangular osteosynthesis showed satisfactory outcomes in treating TSI, which is recommended as a practical surgical choice.
288
RF084: Classification of thoracic spine fracture-the four column theory
Dakheel A. Aldakheel 1
1 Orthopaedic Surgery, King Fahd Hospital of the University, Khobar, Saudi Arabia
Introduction: Thoracic spine fractures have been overlooked in the literature, and the surgical indications are still unclear. In the last century, spine fracture classifications have evolved. It is safe to say that no classification has been developed to accommodate the anatomical and biomechanical characteristics of the thoracic spine. The rib cage is a distinctive feature and has been advocated as the fourth column of the thoracic spine. Several studies have indicated its importance to thoracic spine stability. In addition, others discussed the importance of the posterior column in ensuring the stability of the thoracic spine. Therefore, a classification that embraces recent evidence will contribute significantly to the existing literature gap. The purpose of this paper is to present a classification of thoracic spine features that is based on both anatomical and biomechanical characteristics. Material and Methods: A mechanistic concept is incorporated into the classification, which considers both movements and the application of forces, leading to pathomorphological characteristics. A hierarchical ranking determines the severity of fractures within the thoracic spine, and treatment recommendations are presented in each category. The fourth column of the spine is incorporated into the classification through direct and indirect mechanisms. Results: The classification is based on the relationship between movement and common forces. The primary deforming factor is movement, whereas common forces, which include compression, distraction, and torsion forces, are considered the main categories. Type A injuries occur due to axial compression, which commonly affects one or two vertebral columns. Type A compression injury is furtherly divided based on movement, which will determine where and how the vertebral columns are affected. Type B represents a dynamic relationship between the primarily tensile force acting posteriorly and a simultaneous secondary compression force acting on the anterior vertebral column. Type C result from torsional injury acting axially either in flexion or extension. The hierarchy arrangement within the subcategories is devised to reflect ongoing events of force and movement. Conclusion: The proposed classification accommodates several advantages, such as simplicity and practicality, that make this classification helpful in daily practice. The dynamic relationship between movement and force provides a better understanding of the fracture mechanism. Finally, incorporating the fourth column will strengthen the indication for surgical management. To the best of our knowledge, this classification is the first classification developed uniquely for the thoracic spine fractures and will help to address a critical gap in the literature.
Keywords: thoracic spine; fractures; spine instability; rib cage; sternum; the fourth column
940
RF085: Specificity of blunt spinal injury of thoracolumbar junction
Oleksii Nekhlopochyn 1 , Vadim Verbov 2 , Iaroslav Tsymbaliuk 2 , Ievgen Cheshuk 2 , Milan Vorodi 2
1 Spine Neurosurgery
2 Restorative Neurosurgery Department, Romodanov Neurosurgery Institute, Kyiv, Ukraine
Introduction: Blunt spinal injury resulting from direct traumatic mechanisms that lead to spinal cord lesion are relatively rare during peacetime. The specific characteristics of such injuries are not extensively covered in contemporary literature. The need to optimize treatment methods for military personnel engaged in active combat operations on the territory of Ukraine necessitates an examination of this specific type of injury. Material and Methods: We conducted an analysis of patient data from those admitted for inpatient treatment to our institution, as well as patients referred to other healthcare institutions in Kyiv, from February 2022 to May 2023. Results: We analyzed the treatment outcomes of 5 patients, aged 27 to 53 years (mean age: 37.6 years), presenting with initial neurological deficits classified as ASIA A. Surgery was performed in 3 patients. All cases underwent wide laminectomy with facetectomy at the level of injury. Large arachnoid cysts were drained, and in one case, a subdural hematoma was removed. Posterior spinal fusion using an 8-screw transpedicular system was performed in all patients, utilizing a minimally invasive percutaneous approach. At the 2-month follow-up positive dynamics were observed in all patients. Neurological status improved to ASIA B in 2 cases and ASIA C in 1. Recovery of proprioceptive sensitivity was noted, as well as an increase in the intensity of neuropathic pain (up to 5-7 points at 2 months). In 2 patients undergoing conservative therapy, the neurological impairment level remained ASIA A, with pain intensity not exceeding 2 points. Conclusion: The findings emphasize the need for more comprehensive instrumental assessment in patients with suspected blunt spinal cord injuries. Active use of surgical treatment methods in this type of injury contributes to achieving better clinical outcomes.
1565
RF086: S1/S2 traumatic spondyloptosis in teenage: two case report
Phaik Shan Khoh 1 , Han Sim Lim 2
1 Orthopaedics, Hospital Sultanah Bahiyah, Alor Setar Kedah, Malaysia
2 Orthopaedics, Hospital Pulau Pinang, Georgetown Penang, Malaysia
Introduction: Sacral fracture involving S1/S2 spondyloptosis is a type of transverse sacral fracture. This sacral fracture is a rare injury among the teenage and commonly associated with high energy trauma. Neurological deficit involving the sacral roots are common, which bowel and bladder dysfunction and saddle anesthesia are the typical manifestation. We report two on two teenage patients presenting with S1/S2 traumatic spondyloptosis associated with neurological deficits. Material and Methods: Case 1: A fifteen-year-old boy was involved in motor vehicle accident and was fall from motorbike. He presented with severe low back pain and abdominal pain. Neurological examination revealed bilateral lower extremity paraparesis with muscle strength grade 3-4 at right lower limb and grade 0 at left lower limb. Sensation in both lower extremities had decreased with bowel and bladder dysfunction. Radiographs and computed tomography (CT) scans showed fracture dislocation of S1 over S2 with retroperitoneal hematoma and bilateral kidney injury. Magnetic resonance imaging (MRI) showed anterior displacement of S1 over S2 with stenosis of spinal canal and compression of sacral nerve root at the level. Spinopelvic fixation with pedicle screws from L4 to S2 alar iliac was performed for fracture reduction, stabilization and neural decompression. Case 2: A fourteen-year-old boy fall from motorbike in a road traffic accident. He presented with severe low back pain and saddle anesthesia. Both his lower limb power and sensation was intact. He had perianal numbness with bowel and bladder incontinence. CT scans showed anterior displacement of S1 over S2 with right iliac wing fracture. MRI showed impingement of caudal equina at S1/S2 level with presacral hematoma. This patient underwent operation spinopelvic fixation with pedicle screws from L4 to S2 alar iliac fracture reduction, stabilization and neural decompression. Results: Both patients had good postoperative neurological recovery and able to ambulate without assistant. Conclusion: Open reduction and surgical stabilization of S1/S2 spondyloptosis allow anatomical fracture reduction, stable sacral fixation, sacral neural decompression, and facilitation of return of neurologic function. Therefore, operative management is recommended for teenage patient who presented with S1/S2 traumatic spondyloptosis with good postoperative orthopedic and neurological outcomes.
629
RF087: Outcome analysis of alternate level pedicle screw fixation in thoraco-lumber spinal fractures
Saurabh Singh 1 , Rohit Saroj 1 1 , Prashant Kumar 1 , Rahul Patel 1 , Himanshu Chaudhary 1 , Sushit Sonu 1
1 Orthopaedics, IMS BHU Varanasi, Varanasi, India
Introduction: The optimal treatment of junctional thoracolumbar fractures is still a controversial topic. The goal of treatment is to stabilize the spine, to maintain sagittal balance, to prevent short-term or long-term deformity and neurological recovery along with improving the other clinico-radiological outcome. The purpose of this study was to evaluate the effectiveness of alternate level pedicular screw fixation technique in junctional thoracolumbar fractures in terms of clinical and radiological outcomes. Material and Methods: We prospectively analyzed 80{56 males and 24 females} patients with thoracolumbar fractures, treated with alternate level pedicular screw fixation technique. Preoperative and postoperative clinical and radiological outcomes evaluated, operative time, blood loss, and implant failure also measured. Results: All surgeries were conducted uneventfully within 133+ 14min with mean operative blood loss 422 ± 55m and mean duration of hospitalization was 10 ± 3 days. The mean pre-operative VWA was 17.6° ± 5.5°, and postoperatively corrected to 5.5° ± 3.2° (p < 0.05). The mean preoperative LKA was 15.0° ± 3.4°, which was significantly corrected to 4.2° ± 1.0° (p < 0.05) after surgery and the preoperative AVH was 14.5 ± 4.1 mm and postoperative restored AVH was 26.3 ± 3.2 mm. VAS score significantly reduces from 8.5 ± 1 to 4.5 ± 0.5. Conclusions: Alternate level pedicular screw fixation technique in junctional thoracolumbar fractures is a novel technique which significantly improves postoperative clinical and radiological outcomes as well as decreases duration of surgery, blood loss, decreases intraoperative spinal cord injury and decreases economic burden on patients.
319
RF088: Feasibility of electronic patient - Reported outcome measures following spine injuries in Tanzania
Romani Roman Sabas 1,2 , Julie Woodfield 1,3 , Chibuikem Ikwuegbuenyi 3 , Laurent Mchome 1 , Zarina Shabhay 1 , Magalie Cadieux 1 3 , Abel Makubi 1 , Halinder Mangat 4 , Roger Härtl 3 , Hamisi Shabani 1
1 Division of Neurosurgery, Muhimbili Orthopedic and Neurosurgery Institute, Dar Es Salaam, Tanzania
2 Plastic and Reconstructive Surgery, Muhimbili National Hospital, Surgery, Dar ES Salaam, Tanzania
3 Department of Neurological Surgery, Weill Cornell Medicine, New York, USA
4 Department of Neurology, Division of Neurocritical Care, University of Kansas Medical Center, Kansas City, USA
Introduction: Traumatic spinal injuries cause severe consequences such as pain, weakness, numbness, impaired bladder, bowel and sexual function, financial burdens, and psychological issues. They are common in resource-limited environments, but follow up is challenging due to financial constraints, physical disability, and limited transportation. Given difficulties associated with in-person follow-up, and the rapid expansion of mobile and internet access, we explored the feasibility of using electronic patient-reported outcome measures (PROMs) at home following spinal injuries in Tanzania. We aimed to assess whether patients with spinal injuries have a method of receiving electronic invitations, are able to complete electronic PROMs, any reasons for being unable to complete electronic PROMs and whether questionnaires completed electronically match in person results. Secondarily, we assessed the QoL after spinal injuries. Material and Methods: From March to June 2023, we prospectively recruited consecutive inpatients with traumatic spinal injuries at Muhimbili Orthopedic Institute in Tanzania. We recorded mobile phone and internet access and administered the Kiswahili-validated SF-8 quality- of- life (QoL) questionnaire. This was chosen for its brevity and ease of completion. We compared completion rates between in-person and electronic versions in hospital and assessed post-discharge electronic PROM completion. Results: A total of 50 participants were included (mean age:33 years (SD:14), 43/50 (86%) male). Most had access to a mobile phone (47/50, 94%), and 27/50 (54%) had access to a smartphone. Only 10 participants (20%) completed at least one electronic PROM, either in-hospital (7/50, 14%) or after discharge (6/50, 12%). 3/50 (6%) participants completed both the in-hospital and post-discharge electronic QoL PROM. Reasons reported for not being able to complete the electronic PROM were: limited internet access (9/50, 18%), unfamiliarity with electronic questionnaires (5/50, 10%), and lack of motivation to respond due to illness (3/50, 6%). The in-person SF-8 results for the 50 participants showed a significant decline in both the physical (37 (SD:14) vs 95 (SD:8)) and mental (52 (SD:19) vs 98 (SD:4)) components of QoL compared to the reported pre-injury levels. Intraclass correlation between in-person and electronic completion was high (0.84) for the physical but low (-0.32) for the mental component score. Conclusion: This is the first study to assess the feasibility of electronic PROMs after spinal injuries in a low-middle income country. It is not currently feasible to use electronic PROMs in Tanzania. Internet access was the main barrier due to lack of smartphone or lack of connectivity on a smartphone. Comprehensive telephone, text message, and in-person follow-up strategies with cost-free transportation to clinic are needed to ensure representative capture of QoL outcomes after spinal injuries in Tanzania. In-person QoL questionnaire responses highlighted the significant impact of spinal injuries emphasizing the importance of its assessment. As QoL may be differentially affected by location-specific factors, findings from high income countries cannot be applied to other settings. The difference in mental component scores between in-person and electronic questionnaires highlights that completion method can affect responses so methods of completion should be considered when comparing QoL results from different settings.
569
RF089: My surgical strategy of late-onset osteoporotic vertebral collapse
Hitoshi Hayase 1
1 Neurospinal Surgery, Sapporo Kojinkai Memorial Hospital, Sapporo, Japan
Introduction: Japan is in the midst of a super-aging society. In particular, the number of patients with osteoporosis, which rapidly increases with age, is said to be 13 million at present, and has become a social problem. Among them, the incidence of osteoporotic vertebral body fractures is increasing, and the number of patients with decreased ADL due to this is increasing. Early Balloon Kyphoplasty (BKP) for osteoporotic vertebral compression fractures can reduce pain, early ambulation, and progressive mal- alignment. However, when encountering cases of osteoporotic vertebral body collapse (OVC), it is a problem that troubles spine surgeons. The pathology of late-onset OVC is non-union or pseudoarthrosis after weakened vertebral body fracture, and the pathological condition to be treated is the anterior element of the spine. There are concerns about the perioperative risk and its invasiveness for weakened elderly people, and there are cases in which it is not always easy. Material and Methods: I will present my surgical strategy for 16 cases of the late-onset osteoporotic vertebral collapse that I operated on, and minimally invasive spinal stabilization of vertebroplasty using calcium phosphate cement (CPC-VP) under negative pressure control with short-segment cement-augmented fenestrated percutaneous posterior pedicle screw for elderly perioperative high-risk patients. Results: (1) First, anterior column reconstruction should be considered for 7 cases of OVC with severe posterior wall protrusion. (2) 8 cases of stabilization using OLIF is useful for instability with mild posterior protrusion. (3) 1 case of percutaneous vertebroplasty with Calcium Phosphate Cement combined negative pressure technique is useful for high instability due to severe wedge deformity with extra-vertebral fluid cyst. The advantage of this procedure is that even if there is a crack in the wall of the vertebral body, the pressure inside the vertebral body is controlled by suction from the contralateral pedicle to create a negative pressure, and the vertebral body is checked through lateral fluoroscopy to avoid CPC injection. It is possible to fill as much as possible while preventing it from leaking out of the body. Combination of posterior percutaneous cement-augmented fenestrated pedicle screw recently introduced in Japan is useful for osteoporotic cases, too. Conclusion: The widespread adoption of minimally invasive devices has made the surgical technique for anterior vertebral replacement surgery relatively accessible. It emphasizes the importance of acquiring this skill for spine and spinal cord surgeons. Additionally, with the development of various augmentation methods and the diversification of techniques, it is essential to be flexible in addressing the risk of systemic complications associated with aging and tailoring the approach to individual cases.
528
RF090: Single-stage posterior circumferential stabilization using double small cages for the treatment of thoracic and lumbar spine fractures
Jung-Kil Lee 1 , Seong-Chan Jung 1
1 Neurosurgery, Chonnam National University Hospital, Gwang-ju, South Korea
Objective: Controversy remains regarding the optimal methods for resection of the vertebral body, reconstruction of the anterior column, and decompression of the spinal cord in patients who have severe vertebral body destruction of the thoracic or lumbar spine with associated neurologic impairment. We report an alternative technique for primary treatment and salvage involving single-stage corpectomy followed by reconstruction of the anterior column using double small mesh cages via the posterior-only approach. Methods: Plain radiographs and computed tomography scans, taken at different intervals, were used to measure local kyphosis, segmental height, and fusion grade. Pain was evaluated using visual analogue scale (VAS) and neurological symptoms were classified according to Frankel grade. Results: The mean kyphotic deformity improved by 14.47 ± 9.06o (p < 0.001) and the mean segmental height improved by 7.17 ± 6.11 mm (p < 0.001) after surgery. Fusion was achieved at 84% of patients, within a median interval of 12 months. Kyphotic recurrence was observed in 2 patients (11%), segmental height loss (SHL) occurred in 1 patient (5%), and both kyphotic recurrence and SHL occurred in 1 patient (5%). None of the patients reported worsening pain or neurologic symptoms after surgery, and there were no surgery-related complications such as neural injury, cerebrospinal fluid leakage, cage dislocation, surgical site infection, or cardiopulmonary complications. Conclusion: Single-stage corpectomy followed by reconstruction of the anterior column using double small mesh cages via the posterior-only approach is a reliable and less invasive single-stage treatment and salvage option in selected cases.
Keywords: Corpectomy, vertebral body resection, small cage, expandable cage, posterior approa
RFP06: Minimally Invasive Spine Surgery & Novel Technology
2336
RF091: Treatment of claudication in lumbar canal stenosis with listhesis: minimally invasive TLIF and microscopic over the top decompression. Analysis of 50 cases
Siddhartha Shankar Sahoo 1
1 Neurosurgery, Utkal Institute of Medical Sciences, Bhubaneswar, India
Introduction: Lumbar canal stenosis (LCS) accompanied by listhesis often leads to debilitating symptoms of claudication, significantly impacting patients' daily lives. While TLIF directly decompresses the symptomatic side foramen, Over the top Decompression addresses central canal and contralateral foramen stenosis This study outlines the outcomes of an approach utilising Minimally Invasive Trans-foraminal Lumbar Inter-body Fusion (MIS TLIF) combined with microscopic Over-the-Top Decompression (OTT-D) in the management of claudication associated with LCS and listhesis. Methods: A retrospective analysis was conducted on a cohort of 50 patients with LCS and listhesis who underwent MIS TLIF and OTT-D between 2021-2023 with a minimum follow-up of 3 months. MIS TLIF was performed on the more symptomatic side under 2D C arm guidance. The surgical table was turned to the contralateral side to bring the central canal and contralateral foramen in the line of sight which exposed itself more with sequential decompression. Demographic information, preoperative symptomatology, radiological findings, and surgical details were recorded. Postoperative outcomes were assessed using validated scales, including the Zurich Claudication Questionnaire (ZCQ), Visual Analog Scale (VAS) for pain, and Oswestry Disability Index (ODI). Results: A total of 58 procedures were performed in 50 patients. M: F ratio was 2:3. Average Age was 62. The majority of patients underwent surgery at one level, the commonest being L4-5. The Listhesis was mostly grade 1. The Duration of surgery was 4 ± 1.5 hrs, the blood loss was 150 ± 50 ml. The Hospital stay was 4 ± 1 day. Dural Injury was seen in 2 patients without any new neurological deficits and was repaired with dural supplements. Conversion to open TLIF was required in one case and Screw revision was required in two cases. Surgery resulted in significant improvement in claudication symptoms, with 85% of patients reporting relief within three months. ZCQ scores showed increased walking capacity and reduced symptom severity. Postoperative VAS scores showed a significant reduction in back and leg pain, with an average decrease of 6.2 points and 5.8 points, respectively. The ODI scores showed significant improvement in overall function, resulting in reduced disability and better daily activity performance for patients. Radiographic evaluation showed correction of listhesis and partial fusion in most cases, ensuring long-term spinal stability. Conclusion: A promising treatment option for patients suffering from claudication caused by LCS with listhesis is MIS TLIF combined with OTT-D. This minimally invasive approach effectively alleviates symptoms while providing radiological stability and improved functionality. The combination of direct and indirect decompression of central and foramina stenosis may be the reason for the excellent relief of claudication. Further prospective studies are needed to validate these outcomes.
889
RF092: Is stand-alone percutaneous endoscopic lumbar interbody fusion superior to instrumented percutaneous endoscopic lumbar interbody fusion for the treatment of singe-level, low-grade, lumbar spondylolisthesis?
Jun-Song Yang 1 , Jian-Min Wei 2
1 Department of Spine Surgery, Honghui Hospital of Xi'an Jiaotong University, Xi'an, China
2 Department of Minimally Invasive Spine Surgery, Xi'an International Medical Center, Xi'an, China
Background: The aim of this study was to compare clinical and radiographic outcomes of stand-alone and instrumented percutaneous endoscopic lumbar interbody fusion (PELIF) in the treatment of single-level low-grade lumbar spondylolisthesis. Methods: Fifty-five patients with single-level low-grade lumbar spondylolisthesis, who underwent stand-alone PELIF (stand-alone group, [n = 24]) or PELIF plus percutaneous posterior fixation (instrumented group, [n = 31]) were enrolled in this study. Operative time, intraoperative blood loss, serum C-reactive protein (CRP) and creatine kinase (CK) levels, the length of postoperative bed rest time, and hospital stay were compared between the 2 groups. Disc height, segment lordosis, lumbar lordosis, the visual analog scale score, the Oswestry Disability Index and complications were also compared. Results: Operative and bed rest time were shorter, intraoperative blood loss was less, and postoperative CRP and CK levels were lower in the stand-alone group. During the follow-up period, no patients in stand-alone group received secondary posterior fixation due to the aggravation of lumbocrural pain caused by cage subsidence. Although satisfactory radiographic results were achieved in both groups, the maintenance of increased disc heights and segment lordosis was inferior in the stand-alone group at the final follow-up. Greater improvement in postoperative VAS scores and ODI were observed in the stand-alone group, although the rates of cage subsidence was higher. Conclusion: Stand-alone PELIF was superior to instrumented PELIF in terms of tissue trauma for the treatment of single-level low-grade lumbar spondylolisthesis. However, stand-alone PELIF was inferior in the maintenance of disc height and segment lordosis, and the occurrence of cage subsidence.
Keywords: percutaneous endoscopic lumbar interbody fusion; stand-alone; instrumentation; lumbar spondylolisthesis; minimally invasive; endoscopy
1041
RF093: Transfacet full-endoscopic lumbar interbody fusion: a novel approach
Akarawit Asawasaksakul 1 , Abhirat Suebsing 2 , Siravich Suvithayasiri 3 , Warayos Trathitephun 3
1 Department of Orthopedics, Ramkhamhaeng Hospital, Bangkok, Thailand
2 Department of Orthopedics, Warinchamrab Hospital, Ubon Ratchathani, Thailand
3 Department of Orthopedics, Chulabhorn Hospital, Chulabhorn Royal Academy, Bangkok, Thailand
Introduction: Since 1986, when Kambin first introduced full-endoscopic spinal procedures, there have been significant changes in how we treat spinal issues. These endoscopic techniques have provided benefits like smaller incisions, less damage to tissues, and quicker recovery times. However, there are still challenges. One of the main ones is how to achieve spinal fusion using endoscopic methods. As more tools and technologies are developed for spinal endoscopes, the range of spinal problems they can address grows. Yet, fusion surgery through these methods remains tricky. Material and Methods: To address this, we developed a new "transfacet" method for endoscopic spinal fusion. This technique is guided by the A-Area approach, which offers a clear and effective way to perform the procedure. We tested this method with a patient who had degenerative spinal disease. During the procedure, we also used a tool called a cage glider. Its purpose was to protect an important nerve root while we worked. This combination allowed us to avoid areas that are risky to operate on and could be problematic with other methods. Results: Our findings from using the transfacet Full-Endoscopic Lumbar Interbody Fusion (FE-LIF) technique were encouraging. When we looked at how the patient recovered, the results were positive and suggested that this method could work well for lumbar spine fusions. There were some challenges, like limited space to work in and a bit of a learning curve for surgeons new to the method. But overall, there were no complications, and the fusion was successful. Conclusion: The transfacet technique looks promising for the future of spine surgery. While it's different from more traditional methods like MIS-TLIF, it shows a lot of potential. It could be a big step forward for minimally invasive spine surgeries. However, we need more long-term studies to understand fully how effective and safe this method is. As we gather more data, this technique could change how surgeons approach spinal fusion procedures.
1052
RF094: Evaluation of safety and efficacy of CT navigated minimally invasive transforaminal lumbar inter body fusion (MIS-TLIF): a retrospective study
Mirant Dave 1 , Shivanand Mayi 1 , Bharat Dave 1 , Ajay Krishnan 1 , Devanand Deglumadi 1 , Raviranjan Rai 1
1 Stavya Spine Hospital and Research Institute, Ahmedabad, India
Introduction: Minimally Invasive Surgery Transforaminal Lumbar Interbody Fusion (MIS TLIF) has garnered significant attention in recent years as a less invasive alternative to traditional open procedures for treating various lumbar spinal disorders such as degenerative disc disease and spondylolisthesis. The technique promises reduced tissue damage, lower rates of infection, and quicker postoperative recovery. This study aims to further validate the safety and effectiveness of CT Navigated MIS TLIF in a clinical setting. Materials and Methods: A retrospective study was conducted on 155 patients who underwent CT Navigated MIS TLIF at a leading institute for spine care between June 2022 and December 2022. Patients ranged in age from 30 to 70 and had been diagnosed with lumbar spinal disorders requiring surgical intervention. Metrics recorded included operative time and volume of blood loss. Patient outcomes were gauged using the Visual Analog Scale (VAS) for pain and the Oswestry Disability Index (ODI) at follow-up intervals of 1, 3, and 6 months post-surgery. Complications were also documented. Results: The average operative time was 92.5 minutes with a mean blood loss of 50 ml. A statistically significant reduction in both VAS and ODI scores was noted at the 1-month (VAS: 2.0 ± 0.7, ODI: 20 ± 4), 3-month (VAS: 1.5 ± 0.5, ODI: 16 ± 3), and 6-month (VAS: 1.0 ± 0.4, ODI: 12 ± 2) follow-up periods. These metrics demonstrate substantial improvements in postoperative pain and functionality. The incidence of complications was low, comprising 3 cases of minor dural tears and 2 cases of superficial wound infection, which were successfully managed without any long-term consequences. Conclusion: The study concludes that CT Navigated MIS TLIF is a safe and effective surgical technique for treating lumbar spinal disorders, offering benefits in terms of reduced postoperative pain and improved functionality. Furthermore, the procedure was executed with an optimized operative time and demonstrated low complication rates. These findings provide robust evidence supporting the advantages of adopting CT Navigated MIS TLIF in the surgical management of lumbar spinal conditions. However, future studies with larger sample sizes and extended follow-up are encouraged to substantiate these promising results.
1132
RF095: Is minimally invasive arthrodesis a safe choice in selected cases of neuromuscolar scoliosis?
Chiara Cini 1 , Francesco Vommaro 1 , Giovanni Ciani 1 , Antonio Parciante 1 , Bruna Maccaferri 1 , Alessandro Gasbarrini 1
1 Chirurgia Vertebrale, Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Neuromuscular scoliosis (NMS) is rapidly progressive and often leads to an imbalance in musculoskeletal mechanics that extends to the pelvis causing pelvic obliquity (PO). Segmental instrumentation systems, especially the use of pedicle screws, are reported to be safe and effective in the posterior surgical correction of NMS. However, surgical correction of NMS is still associated with high complication rates. Nowadays, most complications are pulmonary in nature (23%), followed by implant (13%), and infection (11%) related complications. NMS patients tend to experience higher blood loss during surgery as well. The aim of this study was to report the results of an alternative technique to the posterior standard fusion (PSF) for NMS using a minimally invasive surgery (MIS) with a minimum of 1 year follow-up. This approach is original in that it corrects deformities by proximal and distal arthrodesis, with steady pelvic fixation using iliosacral screws. Material and Methods: 15 NMS patients requiring correction surgery were enrolled prospectively between 2021 and 2022. All patients underwent X-ray imaging, before surgery, after surgery, and during follow-up. The surgical technique involved the use of a double-rod construct fixed proximally by polyaxial screws and distally by iliosacral screws, in a minimally invasive approach. MISS technique was performed through two small midline skin incisions (5-6 cm). Two rods contoured were placed from proximal to distal incision passing below the fascia in the not exposed tract. All patients underwent Smith-Petersen osteotomy (SPO) exclusively at the levels instrumented. Inclusion criteria were Age 9-25 years, preoperative Cobb Angle > 45°, PO > 10°, a reduction of at least 25% in Cobb degrees of the primary curve assessed in the supine X-ray compared with that in the sitting position, non-ambulatory patients. Complications were classified into two main categories: surgery-related complications (neurological, site infections, mechanical) and clinical complications (cardiopulmonary, thromboembolic, infectious, iatrogenic). Results: The mean age was 15 years (10 ± 19). Mean BMI was 19,3. The mean operating time was 243 minutes (210 ± 260). Mean preoperative Cobb angle was 96° (85 ± 123°) and it was reduced to 45,8° (38 ± 52,3°) after surgery, corresponding to a mean correction of 52,3%. Mean preoperative pelvic obliquity was 29° (0 ± 42°). It was reduced to 5,8° (4,9-9°) after surgery, corresponding to a mean improvement of 80%. The mean Blood loss (cc/level) was 41,00. Overall, there were no major medical complications. Among the 15 consecutive patients who completed follow-up, no mechanical or infective complication occurred. No patient needed a revision surgery. Conclusion: This new technique enables significant correction of NMS and PO with reduced complication rates. The result of MIS technique is a solid and strong proximal and distal fixation to correct the deformity under the effect of the permanent force maintained between the two extremities of the construct. As the disharmonious control of trunk musculature, progressively worsening due to a lack of effective muscular compensation mechanisms, predominantly affects the transitional zones of the curves, by stabilizing those areas the resultant forces in action are neutralized at the apex of the curve.
2271
RF096: A completely new approach to image guidenace in minimally invasive spine surgery - Results of a first in human trial
Ory Keynan 1 , Shay Menachem 1 , Elias Haddad 1
1 Division of Spine Surgey, Department of Orthopedics, Rambam Healthcare Center, Haifa, Israel
Introduction: With the gaining popularity of MIS procedures in spine surgery, thoracolumbar instrumentation using a percutaneous technic has become one of the key steps using either fluoroscopy or navigation. “VUZE System” is a novel intra-operative image guidance system that consists of software only. Utilizing a preloaded CT scan and real-time image processing, the software incorporates intra-operative fluoroscopic images and generates simulated axial and sagittal views of the of the instruments used in the procedure. The system does not require any special tools or add-ons, nor optical tracking. In this study we evaluated the safety and performance of the “VUZE System” in the first in-human prospective study. Material and Methods: Eligible patients were identified, and enrolled, pre-operative planning was performed using the planning software of the system based on the preoperative CT scan. The planned surgery was performed according to routine practice for MIS implant insertion, utilizing standard tools and fluoroscopy in the AP view only. Concurrently, the system grabbed the fluoroscopic images and the software converted each image to a 3D image simulating the position of the tool (guide wire, Jamshidi needle, or screw). Verification of implant position was performed utilizing intraoperative 3D scans at the end of the procedure. Results: Twenty patients were enrolled. No adverse events were encountered in any patient. Comparison of simulated implant position as projected by the system, to actual position shown on 3D imaging, showed an excellent match in all implants. Conclusion: The results of this first-in-human prospective study show the system is safe and accurate. Further study, to ensure safety and accuracy of the system on a larger cohort is underway.
2065
RF097: Importance of medial facetectomy including superior articular process in a patient with lumbar spinal stenosis associated with spondylolisthesis: pinched root at lateral recess area
Changwook Kim 1 , Jisoo Ha 1 , Dohyoung Kim 1
1 Neurosurgery, YSOK Hospital, Gyeonggi-do, South Korea
Introduction: Several studies report that biportal endoscopic unilateral laminectomy for bilateral decompression (ULBD) has the advantages of less postoperative back pain and shorter hospital stays compared to open lumbar surgery. Because the field of view that can be seen at once is narrow, endoscopic surgery may feel like enough decompression is done even though it is not sufficient. The medial portion of facet should be removed to decompress the lateral recess area and traversing root in ULBD. In this procedure, we recommend sufficient removal of medial facetectomy including the superior articular process (SAP) especially in patients with lumbar spinal stenosis and spondylolisthesis. The traversing root or thecal sac may move ventrally and get pinched in the lateral recess area if the medial facetectomy is insufficiently performed after surgery. We will introduce the patients cases and goal of lateral recess area decompression in endoscopic ULBD. Material and Methods: A 44-year-old female presented to the department with a 12-month history of left radiating pain. The MR images showed severe central and lateral recess stenosis with grade 1 spondylolisthesis at the L4-5 levels. Biportal endoscopic ULBD by Left L4 partial laminectomy performed under general anesthesia. After surgery, a right foot drop with severe right leg radiating pain occurred. The postoperative MR images showed no specific lesions for the symptoms. We did revision surgery with biportal endoscopy at postoperative 1 day. We found that the lateral recess area at the L4-5 level was pinching the right L5 traversing root. Additional medial facetectomy including SAP removal was performed until enough root decompression and L5 pedicle was seen. Results: The medial portion of the SAP should be removed to decompress the lateral recess area and traversing root. Because the field of view that can be seen at once is narrow, endoscopic surgery may feel like enough decompression is done even though it is not sufficient. Ideal decompression should be performed on the medial margin of the lower vertebra pedicle. The same procedure should be performed at contralateral sublaminar decompression. The authors try to decompress until the medial border of the contralateral pedicle is seen. Enough SAP removal using osteotome is important, especially in patients with spinal stenosis associated with spondylolisthesis. After decompression of the lateral recess area, the traversing root moves to ventral freely, and the recess area can be pinch the root. Severe radiating pain or motor weakness including foot drop can be occurred. A pinched root or thecal sac can be seen on postoperative MRI. This problem can be seen more often in spondylolisthesis patients. Some surgeons worry about facet violation or instability. However, many cases showed that 50% and 75% of facetectomies exhibited motion similar to those of the intact model at all loadings. The facetectomy during biportal endoscopic decompression is limited to the tip of the SAP, this technique may not be associated with postoperative instability. Conclusion: To prevent the pinched root, enough medial facetectomy including SAP removal is very important, especially in patients with lumbar spinal stenosis associated with spondylolisthesis.
1980
RF098: Danish experience of minimal invasive extraforaminal lumbar interbody fusion
Sasa Randelovic 1 , Aleksandar Visnjic 2
1 Spinal Surgery, Center for Planlagt Kirurgi, Silkeborg, Denmark
2 Public Health, Faculty of Medicine, University of Niš, Serbia, Nis, Serbia
Objectives: The aim of this work was to evaluate radiological and clinical results in patients operated on by the MIS (Minimally Invasive) ELIF (extraforaminal interbody fusion) method, as well as to evaluate the safety of the method itself. Methods: In this clinical study, conducted from February to May 2023, 58 patients who underwent minimally invasive ELIF were included. Clinical outcomes were assessed using the visual analogue scale (VAS). Imaging and clinical findings, as far as related complications were depicted and analyzed. Results: The mean age of all the 58 treated patients (39 women, 29 men) was 59.22 (SD 10.12) years. There was no difference between gender, nor age (Student T test, p = ns). Paired-Samples T Test was used to evaluate the influence of ELIF on the results related to the VAS scales related to both the pain in back and pain in the legs of the patients after 3 months of the intervention. In the case of back pain, a statistically significant decrease in the value on the VAS scale was found from the moment the patients were admitted (M = 6.42, SD = 1.91) to the monitored moment 3 months after the intervention (M = 2.61, SD = 1.75), t = 9.44, p < 0.001. The mean reduction in VAS score in these patients was 3.95 (SD 2.38) (95% CI: 08-4.58). In the case of leg pain, a statistically significant decrease in the value on the VAS scale was found from the time of admission (M = 6.77, SD = 1.52) to the monitored time 3 months after the intervention (M = 1.55, SD = 2.18), t = 13.01, p < 0.001. The mean reduction in VAS score in these patients was 5.25 (SD 2.56); (95% CI: 4.53-6.02). The condition of the implants after 3 months was without any complications in any of the treated patients. Body max index did not play any significant role (Pearson’s correlation test, p < 0.001). Conclusion: MIS ELIF has been proven as a safe operative method that provides stable spinal fusion with good clinical results in terms of reduced pain in the spine and legs.
Keywords: ELIF; VAS; spine
1373
RF099: Does the use of porous printed titanium cages in lateral lumbar interbody fusion surgery lead to less cage subsidence? A retrospective age-, gender- and levels-of-surgery-matched case control analysis from a single surgeon's series
Bing Howe Lee 1 , Reuben Soh 1
1 Orthopaedic Surgery, Singapore General Hospital, Singapore, Singapore
Introduction: Lateral lumbar interbody fusion (LLIF) facilitates the restoration of disc height and the indirect decompression of neural elements. These benefits are partially lost when the cage subsides into the adjacent endplates. The novel 3D-printed intervertebral porous titanium cage (TI) maximises bone to implant contact and decreases stress shielding and subsidence risk. No study has compared its subsidence rate and functional outcomes to a matched control sample of Polyetheretherketone (PEEK) cages. This study aims to compare the early subsidence rate and patient reported functional outcomes in an age-, gender- and levels-of-surgery-matched sample of TI vs PEEK cages from a single surgeon’s series. We hypothesise that TI cages lead to less cage subsidence and comparable functional outcomes, as compared to PEEK cages. Material and Methods: A retrospective review of a consecutive, prospectively collected, single-surgeon database of patients who underwent LLIF was performed. There were 15 consecutive cases of TI cage matched with previous cases of PEEK cage. Patients were matched for age, gender and levels-of-surgery. There was a minimum of 6 months follow-up. Cage subsidence was assessed on post-operative radiographs according to Marchi grading. Validated patient reported outcome scores (Oswestry Disability Index [ODI]) were compared. Post-op complications were also recorded. Results: There were 7 males and 8 females in each group, with an average age of 69.1 in the TI group and 69.2 in the PEEK group. In each group, there were 8 of cases of 1-level fusion, 6 cases of 2-level fusion and 1 case of 3-level fusion. VAS back pain score for TI and PEEK group improved from mean 6.4 to 1.9 and 7.5 to 2.1 respectively after surgery. VAS leg pain score for TI and PEEK group improved from mean 5.8 to 0.3 and 6.2 to 0.5 respectively after surgery. ODI for TI group improved from mean of 50.1 to 28.1 after surgery. ODI for PEEK group improved from mean 54.7 to 23.8. There were no statistically significant difference between pre- and post-op VAS back and leg pain, pre and post-op ODI between both groups. There were 2 cases of subsidence in the TI group and 3 cases in the PEEK group. In the TI group, 1 patient had Grade 2 subsidence due to infection. The other patient had stable Grade 1 subsidence. In the PEEK group, 1 patient with Grade 2 subsidence had persistence of leg numbness and weakness. Another patient had eventual non-union with loosening of the posterior pedicle screws. No patients required revision surgery. All patients in the TI group rated the surgery “good”, “very good” and “excellent”. Conclusion: The use of Ti cages in LLIF leads to less cage subsidence and comparable functional outcomes, as compared to PEEK cages. This will certainly be key in long term maintenance of sagittal parameters. There are various risk factors for cage subsidence. This study matched the samples by age, gender levels-of-surgery and surgeon. Early results are promising but larger study size and longer follow-up is required for multi-variate analysis of risk factors.
2453
RF100: What is the prevalence and prognosis of coronal malalignment following LLIF for adult spinal deformity with Qiu Type A coronal alignment?
Timothy Yee 1 , Andrew Chan 2 , Praveen Mummaneni 1 , Paul Park 3 , Juan Uribe 4 , Jay Turner 4 , Vivian Le 2 , Robert Eastlack 5 , Richard Fessler 6 , Kai-Ming Fu 7 , Michael Wang 8 , Adam Kanter 9 , David Okonkwo 10 , Pierce Nunley 11 , Neel Anand 12 , Gregory Mundis 5 , Peter Passias 13 , Shay Bess 14 , Christopher Shaffrey 15 , Dean Chou 2
1 UCSF, University of California, San Francisco, USA
2 Och Spine Hospital at NewYork, Presbyterian Columbia University, NewYork, USA
3 Semmes Murphey Clinic, Memphis, USA
4 Barrow Neurological Institute, Phoenix, USA
5 Scripps Institute, San Diego, USA
6 Rush Medical College, Chicago, USA
7 Weill Cornell Medicine, New York, USA
8 University of Miami, USA
9 Hong Neurosciences Institute
10 UPMC Neurological Institute – Presbyterian, Pittsburgh, USA
11 Louisiana Spine Institute, Shreveport, USA
12 Cedars-Sinai, Los Angeles, USA
13 NYU Langone, NewYork, USA
14 Denver International Spine Center, Denver, USA
15 Duke University, Durham, USA
Introduction: Qiu Type A (QTA) coronal alignment is defined as coronal vertical axis (CVA) less than 30 mm. In adult spinal deformity (ASD) with QTA, it is unclear how circumferential minimally invasive surgery (cMIS) with lateral lumbar interbody fusion (LLIF) associates with postoperative coronal malalignment (CM) and clinical outcomes. Material and Methods: This was a retrospective analysis of a prospective multicenter adult spinal deformity (ASD) database. Patients undergoing cMIS with LLIF for ASD with CM < 30 mm were included. Clinical outcomes were compared for QTA with 2-year (2Y) CVA ≥ 30 mm (MAL) versus < 30 mm (ALIGN) and were adjusted for factors reaching p < 0.05 on univariate comparisons (age, BMI, and ODI). Results: Eighty-five patients reached 2-year follow-up - 43 met prespecified inclusion criteria. Overall, 12 (27.9%) patients developed CM at 2Y. MAL were older (73.0 vs. 69.0, p = 0.045) and had lower BMI (26.1 vs. 29.5, p = 0.047). MAL were less disabled at baseline (ODI 42.8 vs. 51.7, p = 0.016). Otherwise, the groups were well matched, including SVA, CVA, and surgical characteristics. At 2Y, MAL had greater mean CVA (43.2 vs. 11.5 mm, adj-p < 0.001) and worsening in CVA (ΔCVA: +26.1 vs. -1.0 mm, adj-p < 0.001) compared to ALIGN, respectively. Clinically, MAL was associated with inferior 2Y SF-36 PCS (34.8 vs. 37.4, adj-p = 0.043) and 2Y SRS-22r function/activity domain (3.0 vs. 3.4, adj-p = 0.040), but otherwise similar 2Y ODI, NRS Back Pain, NRS Leg Pain, EQ-5D, EQ-5D VAS, SF-36 MCS, and SRS-22r total score (adj-p > 0.05 for all). 2Y complications were similar between MAL and ALIGN, including for reoperations and both major and minor complications (adj-p > 0.05 for all). Conclusion: In patients undergoing cMIS with LLIF for ASD who are coronally aligned at baseline (Qiu Type A), approximately 27.9% develop CM. CM was associated with worse SF-36 PCS and SRS-22r function/activity. Despite malalignment, MAL was not associated with worse 2-year complication rates.
697
RF101: Full-endoscopic retroperitoneal approach for the devastating spondylodiscitis with psoas abscess
Siravich Suvithayasiri 1,2 , Chan-Woong Park 2 , Yanting Liu 2 , Khanathip Jitpakdee 3 , Akaworn Mahatthanatrakul 4 , Jin-Sung Kim 2
1 Department of Orthopedics, Chulabhorn Royal Academy, Bangkok, Thailand
2 Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea
3 Department of Orthopedics, Queen Savang Vadhana Memorial Hospital, Chonburi, Thailand
4 Department of Orthopedics, Naresuan University Hospital, Phitsanulok, Thailand
Introduction: Spondylodiscitis and psoas abscess pose a formidable clinical challenge, necessitating extensive antibiotic regimens and potentially surgical intervention. This is more pronounced in cases displaying resistance or those implicating adjacent vertebral or disc space, inducing spondylodiscitis, systemic instability, or neurological sequelae. While the traditional retroperitoneal approach for open drainage and debridement is efficacious, it is linked with significant morbidity and mortality, particularly in frail patients with multiple co-morbidities. The novel full-endoscopic spine approach, an evolution in minimally invasive surgery, offers a promising alternative, reducing surgical trauma, providing better visualization, and enhancing overall outcomes. Our study undertakes a retrospective analysis of patients treated with this novel approach, seeking to illuminate its outcomes and feasibility. Material and Methods: A comprehensive review of a case series was conducted involving patients diagnosed with psoas abscess who underwent a full-endoscopic retroperitoneal approach for irrigation and debridement between 2013-2023 at our institution. Systematic data collection encompassed patient demographics, radiographical information, signs of vertebral infection, cultured organisms, antibiotic regimen details, and surgery-related data. Clinical outcomes were assessed using the numeric pain rating scale (NRS), American Spinal Injury Association (ASIA) Impairment Scale, time to normalization of lab markers (ESR and CRP), and the Modified Macnab Criteria at 6-months postoperatively, reflecting patient satisfaction. Results: Nine patients (6 male and 3 female; mean age 65.67 ± 10.6 years) with varying underlying conditions were included. Most patients had a high Age-adjusted Charlson Comorbidity Index (ACCI) (mean 4.67 ± 3.39, range 1-12), with Staphylococcus aureus being the most common cultured organism. Spinal stabilization was performed in six cases (66.67%), with overall mean operative time and blood loss of 149.44 ± 63.05 minutes and 88.89 ± 117.59 mL, respectively. Significant pain reduction after the surgery was observed, with 88.89% of cases reporting ASIA Impairment Scale of E improvement or maintenance one year post-surgery. Laboratory markers normalized within a week to a month postoperatively for most patients. At six months, 77.78% of cases reported good to excellent scores on the Modified Macnab Criteria without a report of any perioperative complications. Conclusion: This full-endoscopic retroperitoneal approach demonstrates promise for managing spondylodiscitis associated with psoas abscess, with encouraging patient outcomes and experiences reported in our series. This minimally invasive technique, offering reduced tissue damage and potential for quicker recovery, may particularly benefit frail patients with multiple co-morbidities.
1726
RF102: Can pre-operative traction imaging predict the success of indirect decompression? Results of a novel pre-operative traction and weight bearing MRI study
J Naresh-Babu 1 , Gajendra Dr 1 , Prajwal G S 1
1 Mallika Spine Centre, Spine Surgery, Mallika Hospital, Guntur, India
Introduction: Indirect decompression of spinal canal by restoring disc height, foraminal height, unbuckling of ligamentum flavum and correction of sagittal and coronal deformities is gaining popularity recently. The information obtained in the supine MRI and dynamic load bearing radiographs are of value while performing direct neural decompression but may not provide the necessary information required for decision making for indirect decompression which works entirely on the principle of distraction. The present study aims to evaluate the utility of pre-operative traction radiographs and MRI in predicting the success of indirect decompression and correlates with clinical symptoms. Material and Methods: This prospective clinico-radiological study and included 20 patients with degenerative lumbar spondylolisthesis planning to undergo single level indirect decompression procedure. All patients underwent through clinical examination and radiological evaluation by pre-operative radiographs and MRI in traction as well as in supine and standing positions. Radiological parameters and cross sectional area of the thecal sac measured in all three positions. Results: In the supine position, the lumbar lordosis measures 44.9 degrees, with an intervertebral listhesis index of 1.5 mm, an intervertebral translation of 0.6 mm, an intervertebral angle of 2.4 degrees, and a spine curvature (L1-3-5 Angle) of 166 degrees. The foraminal area on the right and left sides is 6 mm and 8 mm, respectively, and the axial CSA of thecal sac is 5.5 mm, with a mid-sagittal thecal sac area of 5 mm. In the standing position, the lumbar lordosis measures 45.8 degrees, with an intervertebral listhesis index of 2.0 mm, an intervertebral translation of 1.0 mm, an intervertebral angle of 1.5 degrees, and a spine curvature (L1-3-5 Angle) of 165 degrees. The foraminal area on the right and left sides is 4 mm and 6 mm, respectively, and the axial CSA of thecal sac is 4.3 mm, with a mid-sagittal thecal sac area of 3 mm. During traction, the lumbar lordosis measures 43.4 degrees, with an intervertebral listhesis index of 0.9 mm, an intervertebral translation of 0.4 mm, an intervertebral angle of 3.3 degrees, and a spine curvature (L1-3-5 Angle) of 169 degrees. The foraminal area on the right and left sides is 8 mm and 9 mm, respectively, and the axial CSA of thecal sac is 7 mm, with a mid-sagittal thecal sac area of 6.5 mm. By applying traction, the cross sectional area of the thecal sac, mid sagittal thecal sac area and foraminal height was found to increase by 50% compared to those in standing position. By applying traction, there was also nearly 50% reduction in intervertebral listhesis index and translation compared to standing in both plain radiographs and load bearing MRI. Conclusion: Present study evaluates the utility of pre-operative traction imaging which in principle mimics the surgical indirect decompression in selecting ideal candidates for indirect decompression. For the first time, present study documented that a 50% reduction in spondylolisthesis index or translation (measured on both radiographs and MRI) could result in 50% increases in the cross sectional area and foraminal area of the lumbar spine on MRI. This data has huge clinical implications as traction and standing radiographs can be readily obtained pre-operatively.
646
RF103: Improved productivity using deep learning assisted Cobb angle measurement on scoliosis radiographs
Xi Zhen Low 1 , Shaheryar Mohammad Furqan 2 , Andrew Makmur 3 , Noah Lim 4 , Hien Anh Tran 4 , Desmond Shi Wei Lim 1 , Kian Wei Ng 5 , Tricia Kuah 1 , Aric Lee 3 , You Jun Lee 3 , Ren Wei Liu 3 , Natalie Hui Wen Tan 6 , Si Jian Hui 6 , Xin Yi Lim 6 , Dexter Seow 6 , Yiong Huak Chan 7 , Premila Hirubalan 8 , Lakshmi Kumar 8 , Jiong Hao Tan 6 , Leok Lim Lau 6 , James Hallinan 1 3
1 Diagnostic Imaging, National University Hospital, Singapore, Singapore
2 Division of Biomedical Informatics, YLL school of Medicine NUS, Surgery, Singapore, Singapore
3 Department of Diagnostic Radiology,Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
4 Lee Kong Chian School of MedicineSingapore, Singapore
5 AIO Innovation Office
6 Orthopaedic Surgery, National University Health System, Singapore, Singapore
7 Biostatistics Unit, Yong Loo Lin School of Medicine, Singapore, Singapore
8 Youth Preventive Health Service Division, Singapore, Singapore
Introduction: Background: Radiographic analysis of scoliosis using the Cobb's angle is time-consuming and repetitive. Deep learning (DL) could provide more consistent and faster interpretation. Purpose: Assess the interpretation time and accuracy of clinicians for Cobb’s angle assessment with and without DL-assistance. Material and Methods: A DL model was developed to assist Cobb’s angle interpretation on spine radiographs. Consecutive radiographs in patients 10-18 years with scoliosis and no instrumentation from January 2018-January 2019 were included. Eight clinicians, four radiologists in-training (R1-R4, no experience) and four orthopedists in-training (O1-4, 6-months-experience) performed retrospective assessment with and without DL-assistance with a 6-week washout. Interpretation time and mean angle differences were assessed with and without DL-assistance with a spine surgeon (6-years-experience) as the reference standard. Results: Overall, 640 patients (mean ± SD, 12.6 years ± 2; 465 girls) were split into 580 patients for training (73%) and validation (18%), and 60 (9%) for testing. DL-assisted clinicians had reduced or equivalent mean angle differences versus unassisted reads; Radiologist-R4 showed the largest reduction in mean-angle difference from -3.20° (95%CI: -4.21- -2.12°) unassisted to 1.03° (95%CI: -0.5 - 2.57°) with DL-assistance. Despite different prior experience in-training radiologists and orthopedists showed equivalent mean angle differences with and without DLmodel assistance. For DL-assisted reads, radiologists had a mean time saving of 13.25 seconds (95%CI: -19.6 - -6.91) versus a time increase of 3.85 seconds (95%CI: -2.94 - 10.63) for orthopedists in-training (p = 0.005). Conclusion: DL assistance for Cobb’s angle on spine radiographs provided superior or equivalent mean angle differences. There was a reduction in interpretation time for radiologists in-training (novices), with no reduction in time for orthopedists in-training (experienced). Clinical Relevance Statement: Radiologists in-training assisted by deep learning for Cobb angle measurement on scoliosis radiographs showed marked reduction in interpretation time and reduced or equivalent mean angle differences.
214
RF104: NeuroReach - Making surgery in neurosurgery accessible - An intradural spinal catheter device
Uri Hadelsberg 1 , Andres Vargas 1
1 Neurosurgery, Hadassah University Medical Center, Jerusalem, Israel
Introduction: At present, there are no medical devices to aid in providing a minimally approach into the spinal canal or into the intracranial vault. The only way to access a spinal intramedullary/intradural tumor or to perform a microvascular deompcression, endoscopic third ventriculostomy, or the insertion of intrathecal/intratumor/spine neurotrauma protective drug administration, among other procedures, is via surgery. In addition, neural foramen decompression via a complete spinal intradual approach might be feasible using this device as well as radiofrequency techniques. This requires general anesthesia and admission to the intensive care unit for a lengthy hospital stay. We propose a novel device which will address these pathologies and other patgoloties by the use of a camera-equipped catheter and a working channel inserted via a lumbar puncture and insertion of a catheter, thus eliminating the need for craniotomy or spinal canal exploration. Material and Methods: We have developed and patented a device which comprises of a mini-camera and a working channel through which micro-tools (a knife, forceps and other devices) can travel up to the brainstem and cerebrum and perform the above mentioned and other neurosurgical procedures. We have received $250K USDs funding from the Israeli innovation authority and our institution to pursue this idea. Results: In August 2022 we used grant money from our hospital and developed and tested a catheter prototype equipped with a mini camera and working channel. Three (3) prototype catheters were produced and were tested in an animal (swine). Helsinki approval and the hospital ethics comittee approved the experiment using our device, approval for developing the device and testing it on the animal were obtained prior to the trial. During the procedure we inserted our catheter in the lumbar spinal sac of a male swine. We managed to progress the catheter all the way up the spinal canal and harbor it infront of the brainstem with visualization of the brainstem structures itself. We recorded our results of which some are attached in this absatrat (Figures 1–6). A second in-vivo experiment is planned to take place this September (after the submission date) and videos and our progress will be readily available towards the end of September. Conclusion: To the best of our knowledge this is the first time a camera recording of the brainstem and intracrnial anatomy as well as the spinal canal were visualized in a living animal. We are developing our device and hope to apply this as a standard of care in future.
Figure 1.
Distal catheter tip.
Figure 2.
Insertion of the catheter into the swine’s back.
Figure 3.
Intracanal navigation to the brainstem. Nerve roots and the spinal cord can be appreciated.
Figure 4.
Above on left hand side is the brainstem.
Figure 5.
Inferior view of the brainstem and its supplying arteries from a lumbar puncture approach, here upon entrance through the foramen magnum.
Figure 6.
The brainstem and choroid plexus can be appreciated.
353
RF105: Unilateral biportal endoscopy (UBE) in patients with lumbar canal stenosis: early results of a prospective study of 31 patients
Ashwinkumar Khandge 1
1 Clinical Associate Professor in Orthopedics, Dr D Y Patil Medical College and University Hospital, Pune, India
Introduction: Lumbar canal stenosis (LCS) requires surgical management in cases that are unresponsive to conservative treatment. Spine surgery for LCS has evolved from open spine surgery to microscopic lumbar decompressions and most recently to spine endoscopy. Unilateral Biportal endoscopy (UBE) is the most recent advance in spine endoscopy and utilizes an arthroscope and routine spine instruments. The aim of this study was to analyze the early results of UBE spine surgery in patients with LCS. Material and Methods: The inclusion criteria were patients aged 20-70 years old with LCS at one level not responding to conservative management pain radiating to the lower extremity. The senior author consecutively performed UBE surgeries for 45 patients of LCS. We included in the study only patients who were followed up for more than six months after surgery. Clinical outcomes were evaluated using modified Macnab criteria, the visual analogue scale (VAS) for legs, and the Oswestry Disability Index (ODI). Results: A total of 45 patients were selected after applying the inclusion and exclusion criteria. 31 patients were followed up for 6 months and their outcomes evaluated. The VAS improved from mean 4 (range 2-5) to 2 (range 1-4) for back pain and 8 (range 4-9) to 2 (range 1-5) for leg pain at 6 months follow-up. While the ODI improved from a mean 46.6 (range 32-68) to 22.4 (range 16-42) at 6 months follow-up. The average satisfied outcome based on the Macnab criteria was excellent to good. Conclusion: A marked early improvement was seen in the perception of pain and symptoms after undergoing UBE surgery in cases of single level LCS. We need further randomized controlled studies to establish long term efficacy of UBE in LCS as compared to gold-standard surgical modalities.
1429
RF106: Novel 3D printable PEEK-HA-Mg2SiO4 composite material for spine implants: biocompatibility & imaging compatibility assessments
Naresh Kumar 1 , Renick Lee 1 , Sahil Athia 1 , Praveen Jeyachandran 1 , Jagadeesh Babu Veluru 1
1 Orthopaedic Surgery, National University Health System, Singapore, Singapore
Purpose: The current ‘gold standard’ (Titanium) for manufacturing spine implants have high young’s modulus which causes stress shielding and generate imaging artifacts. Standard PEEK material is bioinert with low tensile strength and Young’s modulus. We aim to develop a novel 3D printable polyether ether ketone (PEEK)-hydroxyapatite (HA)-magnesium orthosilicate (Mg2SiO4) composite material with enhanced properties for potential use in tumour, osteoporosis and other spinal conditions. We also aim to evaluate biocompatibility and imaging compatibility of the material. Methods: Materials were prepared in three different compositions, namely, composite A: 75 weight % PEEK, 20 weight % HA, 5 weight % Mg2SiO4; composite B: 70 weight% PEEK, 25 weight % HA, 5 weight % Mg2SiO4; and composite C: 65 weight % PEEK, 30 weight % HA, 5 weight % Mg2SiO4. The materials were processed to obtain 3D printable filament. Biomechanical properties were analyzed as per ASTM standards and biocompatibility of the novel material was evaluated using indirect and direct cell cytotoxicity tests. A three-point bending to evaluate the flexural properties of biocomposites was conducted. Cell viability of the novel material was compared to PEEK and PEEK-HA materials. The novel material was used to 3D print a standard spine cage by Fused deposition modelling. Furthermore, the CT & MR imaging compatibility of the novel material cage vs PEEK and PEEK HA cages were evaluated using a phantom setup. Results: Composite A resulted in optimal material processing to obtain a 3D printable filament, while composite B & C resulted in non-optimal processing. Our biocomposites exhibited linear elastic characteristic under bending load. Our composite material showed flexural strength of 2.89 ± 0.2 GPa which is significantly higher than the flexural strength of individual components. The linear flexural strain was observed with increasing flexural stress but it did not affect the elastic characteristics of the PEEK biocomposite. Composite A enhanced cell viability up to ∼20% compared to PEEK and PEEK-HA materials. Enhancement in cell viability displayed could possibly be due to the favourable mechanism of magnesium and silicate ion release that enhances cell growth. Our material induces bioactivity thus avoiding the risk of delamination. Our material is hypothesized to have Young’s modulus closer to that of cortical bone that results in optimal load sharing between bone and implant. Composite A cage generated minimal/no artefacts on CT & MR imaging and the images were comparable to that of PEEK and PEEK-HA cages. This facilitates improved RT planning and delivery. Conclusion: Composite A demonstrated superior bioactivity vs PEEK and PEEK-HA materials and comparable imaging compatibility vs PEEK and PEEK-HA. Our biocomposite has Young’s modulus comparable to that of cortical bone, facilitating reduction in stress shielding. Therefore, our material displays an excellent potential to manufacture spine implants with enhanced mechanical and bioactive property. This novel material is predicted to improve osseointegration and reduce the chances of construct loosening/implant failure in spinal conditions, especially MSTS and osteoporotic fixations.
Keywords: spine; PEEK, 3D printing; implants; magnesium orthosilicate
1172
RF107: Manipulative reduction combined with concave-side percutaneous kyphoplasty for the treatment of kyphoscoliosis caused by acute thoracolumbar osteoporotic vertebral compression fractures
Chao-Yuan Ge 1 , Ding-Jun Hao 1
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
Introduction: There are no studies on the management of local kyphoscoliosis caused by acute thoracolumbar osteoporotic vertebral compression fractures (ATLOVCFS). The aim of this study is to evaluate the safety and efficacy of manipulative reduction combined with concave-side percutaneous kyphoplasty (PKP) in the treatment of local kyphoscoliosis caused by ATLOVCFs. Material and Methods: A total of 56 ATLOVCFs patients with coronal asymmetric compression fractures treated with manipulative reduction combined with concave-side PKP were retrospectively reviewed. The patients were followed-up regularly and were assessed with clinical and radiological outcomes. The clinical outcomes were assessed with visual analogue scale (VAS) for back pain and oswestry disability index (ODI) for functional status. The radiological outcomes were evaluated with cobb angle of local scoliosis and kyphosis. The cases of leakage of bone cement during surgery and new vertebral fractures during follow-up were also reviewed. Results: Manipulative reduction combined with concave-side PKP was successfully completed in all 56 patients. All patients had significantly improvement on VAS and ODI scores compared with their preoperative values and these improvements remained significant during the follow-up period (p < 0.05). Meanwhile, patients had significantly improved cobb angles of local scoliosis and kyphosis postoperatively and the local spine alignments were maintained well during the follow-up period (p < 0.05). There were four cases of cement leakage during surgery, but none of them developed clinical symptoms and there was no new vertebral fractures during follow-up. Conclusion: Manipulative reduction combined with concave-side PKP is a safe and effective approach for the treatment of kyphoscoliosis caused by ATLOVCFs. It can effectively relieve pain, improve quality of life, and improve spinal local kyphoscoliosis.
987
RF108: Estimation of bone mineral density from computed tomography hounsfield unit using artificial intelligence: a working model based on free and open-source software
Leo Shaw 1 , Han-Ting Shih 1 , Kao-Chang Tu 1 , Cheng-Hung Lee 1 , Kun-Hui Chen 1
1 Taichung Veterans General Hospital, Taiwan
Introduction: HU obtained from the ROI in the spine on CT scans have been established to correlate with BMD. However, the conventional manual approach for ROI acquisition is time-consuming. This study aimed to develop an AI model capable of accurately acquiring HU values from the desired ROI in the lumbar spine on CT scans. Material and Methods: A total of 164 patients with both dual-energy X-ray absorptiometry (DXA) and lumbar spine CT scans were included in this study. Lumbar spines with implants were excluded. Using free and open-source software, custom-coded algorithms were developed to accurately acquire the ROI in the lumbar spine on CT images. HU values were then calculated using established methods. The calculated HU values were subsequently compared with BMD measurements obtained from DXA scans. Results: The study assessed a total of 414 lumbar spines. Significant differences in HU values were observed among the three patient groups (Normal bone density, osteopenia, osteoporosis) categorized based on their BMD status (p ≤ 0.01). The Spearman rank coefficient between BMD and HU values yielded an R2 value of 0.74, indicating a strong correlation. Conclusion: This method may be an auxiliary tool for BMD estimation in clinical practice for patients without DXA.
RFP07: Cervical Trauma
536
RF109: Factor associated with non-contiguous spine fracture in patients with traumatic cervical spine fracture: a 10-year retrospective study
Anuchit Chaiamporn 1 , Torphong Bunmaprasert 1
1 Orthopaedic, Chiang Mai University, Chiang Mai, Thailand
Objective: To identify factors associated with non-contiguous spine fracture in patients with traumatic cervical spine fracture. Method: The 10-year retrospective observational study included 588 patients with traumatic cervical spine fractures who be admitted at Maharaj Nakorn Chiang Mai Hospital between January 2011 to December 2022. Patients were categorized into two groups: those with non-contiguous spine fractures and those without non-contiguous spine fractures. Outcomes were analyzed using multivariable logistic regression. Results are presented as odd ratio (OR) and 95% confidence interval (95% CI). Results: Among 588 patients, the incidence of non-contiguous spine fractures was 17.01% (100 of 588 patients). Independent factors associated with non-contiguous spine fracture were ASIA grade A-D (OR 2.00, 95% CI (1.25-3.22), p = 0.004), Glasgow Coma Score (GCS) < 13 (OR 2.64, 95% CI (1.63-4.27), p = 0.000), and intrathoracic injuries diagnosed by E-FAST and chest radiograph (OR 2.60, 95% CI (1.58-4.29), p = 0.000). Conclusion: The risk of non-contiguous spine fracture in patients with a traumatic cervical spine fracture will increase if patients have motor weakness (ASIA score A-D), Glasgow Coma Score < 13 and presence of intrathoracic injury. Whole spine CT or MRI imaging is beneficial in these patients to avoid missing the remote spinal injury.
306
RF110: Application of modest hypothermia in patients with acute traumatic cervical spine injury: a pilot study
Sarvdeep Dhatt 1
1 Orthopaedics, PGIMER, Chandigarh, India
Introduction: This prospective randomized controlled study aimed to examine the role of modest systemic hypothermia in individuals with acute cervical spinal cord injury (SCI) regarding neurological improvement. Studies have shown that the application of hypothermia is safe and that it improves neurological outcomes in patients with traumatic spine injury. Hypothermia helps in decreasing a secondary damage to the cord. Methods: Twenty cases of acute post-traumatic cervical SCI with AISA were selected and randomly divided into two treatment groups: Group A-Hypothermia with surgical decompression and stabilization; and Group B-Normothermia with surgical decompression and stabilization. American Spinal Injury Association (ASIA) motor and sensory scores were evaluated at presentation; post-surgery; and at a 2-week, 6-week, and 12-week follow-up. Results: At the final follow-up, the change in ASIA motor scores of Group A was 46 (11.5-70.5) and Group B 13 (4.5- 58.0), whereas ASIA sensory scores were 118 (24.75-186.5) and 29 (15.25-124.0) in Group A and Group B, respectively. ASIA scores between the two groups were statistically significantly different at a 2-week follow-up (ASIA motor p = 0.04, ASIA sensory p = 0.006), showing early improvement in the hypothermia group. There was no significant difference between the two groups on further follow-up. Conclusions: Hypothermia can be applied safely to subjects with acute SCI. Our study showed that hypothermia was beneficial in the early improvement of functional outcomes in acute cervical SCI.
Keywords: hypothermia; cervical; spinal cord injury; hypothermia; improvement; American Spinal Injury Association score
1582
RF111: C1-2 fixation with C1 lateral mass and C2 laminar screws: a case series, technique note and outcomes
Chang Kai-Chieh 1 , Chih-Ju Chang 1
1 Neurosurgery, Cathay General Hospital, Taipei City, Taiwan
Introduction: Transarticular screw fixation (Margel’s technique) and C1 lateral mass and C2 pedicle screw fixation (Goel-Harms technique) is an ideal technique for correcting atlantoaxial instability (AAI). However, the inevitable situation for vertebral artery injury, especially narrow pedicle and high-riding vertebral arteries (HRVAs) may endanger the artery. Recent technical reports described posterior C2 fixation using bilateral, crossing C2 laminar screws. The translaminar screw technique has the advantages of producing little risk of VA injury and the unconstrained screw placement. In addition, biomechanical studies have demonstrated the potential of the translaminar screw technique to provide a firmer construct that is equivalent to methods currently used. Material and Methods: We retrospectively reviewed 22 patients with atlantoaxial subluxation treated in our institution from 2016 to 2022. Among them, 5 patients had narrow C2 pedicles and HRVAs treated with C2 laminar screws were analyzed in this study. The internal height(C2InH), isthmus height(C2IsH), laminar width(C2Lw) and pedicle width(C2Pw) of C2 vertebra were measures using preoperative thin-slice computed tomography (CT). The position and length of the screws were observed using postoperative CT. The subjects were followed up for pain, neurological status and radiographic outcomes. Results: In total, 9 C2 laminar screw were placed in 5 patients. One patient treated with a customized guiding-block and one patient used dyna-CT assisted intraoperatively. The mean C2InH was 3.67 mm, C2IsH was 3.6 mm, C2 Lw was 6.2 mm and C2Pw was 4.16 mm. Only one screw had breached the C2 lamina and reposition immediately with dyna-CT. By 1 year postoperatively, no case of C2 lamina screw required reoperation or screw pullout or pseudoarthrosis. The accuracy of the screws is good in comparison with preoperative and postoperative CT findings, and no vascular injury occurred. Conclusion: C2 laminar screws can be a useful alternative technique for the treatment of C1-C2 instability in the presence of anatomic constraints. The variations of C2 morphology hold important clinical implications for the technical reporting of C2 operations. Thorough preoperative anatomical studies, along with image evaluation provide satisfactory reliability and accuracy.
2247
RF112: Clinico-radiological study of traumatic facet joint injuries according to the AOSpine subaxial injury classification. Is there a better way to differentiate Type-F1 and Type-F2 injuries?
Maximilian Reinhold 1 , Driesen Tobias 1 , Ecker Carolin 1 , Jaeckle Katharina 1 , Lehmann Wolfgang 1 , Weiser Lukas 1 , Kuczera Tim Niklas 1
1 Department of Trauma, Orthopaedic, and Plastic Surgery, Goettingen University, Germany
Introduction: The AOSpine classification for the subaxial cervical spine (2016) is based on morphopathological criteria and for the first time includes different entities of facet joint injuries (F1-F4), in particular the classification and differentiation of subtype F1 (stable) and F2 (potentially unstable) is controversial in clinical practice. The aim of this study was to evaluate the extent to which the new classification allows unambiguous assignment of each facet joint injury. Material and Methods: Clinical and available images (X-ray, CT, and MRI) of the own patient population with traumatic subaxial spinal injuries (2013 to 2021) were reviewed. A detailed radiographic facet fracture analysis, clinical parameters (age, sex, ISS score) and treatment (non-operative vs. surgical) was carried out. Injuries were classified according to the AOSpine classification and the White and Panjabi criteria (1990) (stable vs. unstable). Results: A total of 54 patients with 74 facet injuries were included in the study. With few exceptions (n = 4), nearly all injuries (> 94%) could be assigned to an AO subtype (F1-F4). We identified 29 type F2 injuries that were either treated non-operative (n = 14) or surgically (n = 15). The most common level of injury was C6/7 (n = 38, 51.4%). Extension of the fracture lines into the pedicle (n = 19, p = 0.002) and involvement of both articular surfaces (n = 23, p = 0.003) occurred statistically more often in type F2 facet fractures. According to White and Panjabi, almost equal proportions of F1 (57% “AO stable”) and F2 (55%, AO “potentially unstable”) injuries were considered "unstable". The following three pathomorphologic features showed statistically differences within the stable White & Panjabi group: a) cranial joint surface (p = 0.032), b) loosened bone fragment (p < 0.001), and c) joint space width (stable: on average 1.3 mm vs. unstable 2.3 mm). Conclusion: Most subaxial facet fracture injuries can be classified into one the 4 subgroups. The implication of F1 vs. F2 in terms of clinical decision making remains controversial and somewhat ambiguous. This study highlights thee characteristic pathomorphological features that allow for a better differentiation between radiological stable or unstable injuries according to White and Panjabi.
152
RF113: How MRI changes treatment decisions in cervical spine trauma
Niklas Rutsch 1 , Florian Schmaranzer 2 , Pascale Amrein 1 , Martin Müller 3 , Christoph Albers 1 , Sebastian Bigdon 1
1 Department of Orthopedic Surgery and Traumatology
2 Department of Diagnostic, Interventional, and Pediatric Radiology
3 Department of Emergency Medicine, Inselspital, Bern, Switzerland
Introduction: Cervical spine (c-spine) injuries are common. Computed tomography (CT) is the gold standard for evaluating c-spine injuries in the emergency department (ED). However, with the increasing availability and the advantage of reduced radiation exposure, magnetic resonance imaging (MRI) has emerged as a potent alternative diagnostic tool. Nonetheless, the cost and time implications of MRI raise concerns regarding its role in the ED, particularly in patients with already diagnosed c-spine injuries, leading to ongoing debates over its utility. The objective of this study was to assess the value of incorporating an additional MRI in the evaluation of patients with c-spine injuries in the ED. Materials and Methods: We conducted a retrospective monocenter cohort study between January 1st, 2012, and December 31st, 2017, at Inselspital, University Hospital Bern, Switzerland. Participants included all ED patients presenting with trauma and neck pain requiring radiographic c-spine evaluation based on the NEXUS criteria. Pediatric ED cases and those with incomplete medical records were excluded from the study. Imaging modalities used were categorized as CT, MRI, or a combination of both. Spine surgeons performed a full-case review to classify each case into "c-spine injured" and "c-spine uninjured". Injuries were classified according to the AO Spine. We then further narrowed down to patients with a c-spine injury initially detected by CT, who received a subsequent MRI. In this subset, injuries were classified separately in both imaging modalities. We monitored treatment changes after the additional MRI and performed a regression analysis to investigate the predictive power of the AO Spine Classification Neurology/Modifier variables on therapy change. After data extraction, the statistical analysis was performed in RStudio. Results: A total of 4,496 subjects were identified, with 2,321 meeting the inclusion criteria and 186 patients diagnosed with c-spine injuries. The incorporation of an additional MRI significantly prolonged the patients' ED stay (geometric mean ratio 1.32, p < 0.001). Among 56 patients initially identified with c-spine injury via CT, 25% experienced a change in treatment strategy after the additional MRI. Of patients with neurological symptoms (AO N ≥ 1), 45.8% experienced treatment changes based on the MRI findings. Patients testing positive for neurological deficits (N-positive) had 12.4 times higher odds (95% CI 2.7-90.7, p < 0.01) of treatment alteration after an additional MRI compared to neurologically intact patients. Conclusion: In conclusion, our findings underscore the importance of considering MRI in the evaluation of c-spine injuries, particularly when neurological symptoms are present, as it can significantly impact treatment decisions. A judicious approach should be taken when utilizing MRI, considering its impact on ED resources and patient management. This study contributes valuable insights to inform clinical practice and optimize patient care in the ED setting.
1403
RF114: Vertebral artery injuries in patients with cervical trauma: a retrospective descriptive study
Ignacio Cirillo 1,2,3 , José Via Dorado 1,3 , Marcos Gimbernat 1,4 , Juan Jose Zamorano 1,5,6 , Alejandro Urzúa 1 , Carlos Tapia 1,7 , Valentina Herrera Bascuñan 1
1 Hospital del Trabajador, Santiago, Chile
2 Clínica Universidad de los Andes, Santiago, Chile
3 Universidad Nacional Andres Bello, Facultad de Medicina, Santiago, Chile
4 Clínica Davila Vespucio, Santiago, Chile
5 Clínica Alemana, Santiago, Chile
6 Universidad del Desarrollo, Santiago, Chile
7 Instituto Traumatológico Dr. Teodoro Gebauer, Santiago, Chile
Introduction: 2% of closed cervical traumas present with carotid dissection or vertebral artery injury (VAI). 70% are associated with cervical fractures: transverse processes, C1-C3 bodies and subluxations. The areas at highest risk of VAI are V2 (26%) and V3 (55%). The clinical picture is variable (generally vertebrobasilar symptoms) and early diagnosis is difficult (70% asymptomatic in the first 24 hours). The mortality rate is 8-38% and 14-54% develop a cerebrovascular accident (CVA). The modified Denver criteria are used for screening and angio-CT is considered the best method of investigation. Treatment is controversial: anticoagulants and antiplatelet drugs would not make a difference in the development of stroke and endovascular therapy would not be justified because of its high risk. The purpose of the present study was to report the demographics, treatment, clinical and imaging outcomes of patients with VAI associated with cervical fracture. Material and Methods: Retrospective observational study. Cases of cervical spine fracture with angio-CT of the neck vessels between January 2015 and December 2021 were analysed. Radiological reports were evaluated for the diagnosis of VAI, classifying lesions according to Denver. The medical evolution of the traumatology and neurology teams was reviewed. Data analysis was performed using Excel. Results: 42 cases of cervical fracture were identified by angio-CT, 11 with LAV (26%), 72.7% males. Most common mechanism: fall from height (27.3%) and motorcycle accident (27.3%). 36.3% had vertebrobasilar symptoms and 81.8% had a brain injury or ECT. The most frequent vertebral segment C0-C1 (27.3%) and C6-C7 (27.3%), in no case did the VAI change the surgical plan. 72.7% were in zone V2 and 27.3% in zone V3, with 25.3 days at diagnosis. 8 patients were treated with aspirin (for 354.7 days), 2 cases developed sequelae. In 3 patients without antiplatelet treatment, 1 patient developed sequelae. Only one patient required invasive treatment for an arteriovenous fistula, but developed no sequelae. Mean imaging follow-up was 478 days: 45.4% with complete regression, 36.3% with no evidence of recanalization and 18.1% lost to follow-up. Conclusion: VAI associated with cervical fractures generally do not alter the surgical plan of the fracture and are most often diagnosed late. Furthermore, neurological outcome is favourable in most cases with conservative management.
302
RF115: Surgical outcome of Mingsheng Tan technique for C2 odontoid fracture
Phuc Diep 1
1 Department of Spine Surgery B, Hospital for Traumatology and Orthopaedics, Ho Chi Minh, Viet Nam
Introduction: Regarded as the gold standard of surgery for C2 odontoid fracture, Goel-Harms technique had several drawbacks including but not limited to the necessity of dealing with the venous plexus and C2 nerve roots. To overcome those obstacles, several modifications have been proposed and Mingsheng Tan technique was one of alternative solutions that we used since 2014 for C1-2 fixation. Material and Methods: Mingsheng Tan technique differed from conventional Goel-Harms technique only on the entry points of C1, which located at the posterior arch of C1 rather than C1 lateral mass only. We retrospectively assessed C2 odontoid fracture patients surgically treated with Mingsheng Tan technique from January 2014 to June 2022. Clinical parameters (including neck pain, range of motion and neurological complications if any) and radiographic findings (including sign of implant failure and fusion rate) were assessed. Results: There were forty-four recruited patients with mean age of 34.67 years. The mean operation time and blood loss were 126.67 ± 25.34 minutes and 125 ± 3.12 milliliters, respectively. No intraoperative neurovascular complications were documented in our group. In terms of postop clinical findings, restriction of cervical rotation was the most common chief complain, with minimal to moderate impact on the patient’s quality of life. The mean rate of odontoid union and posterior fusion were 87.93% and 100%, respectively. Conclusion: Given the preliminary results of our study, Mingsheng Tan technique could be considered as a safe and reliable alternative option apart from Goel-Harms procedure for C2 odontoid fracture. The avoidance of dealing with the C1-2 venous plexus might help to minimize the blood loss as well as surgical duration. Further studies with larger sample size and longer duration are required in order to make more definitive conclusions.
970
RF116: A novel interlocking technique for enhancing anterior spinal fixation in pediatric spinal instrumentation
Senol Jadik 1
1 Neurosurgery, Kuwait Hospital, Kuwait City, Kuwait
Introduction: Pediatric spinal instrumentation has historically borrowed from adult techniques, leaving a gap in pediatric-specific solutions for complex spine disorders. Traditional screw-based fixation methods may fall short in addressing the unique challenges presented by the pediatric spine. This study introduces a pioneering interlocking technique for anterior spinal fixation, designed to substantially enhance screw pull-out strength in pediatric spinal instrumentation. Material and Methods: We present a case study involving a 1.5-year-old infant undergoing extensive spinal surgery from C7 to T3. Detailed patient demographics, operative data, and perioperative complications were meticulously documented. In parallel, a comprehensive literature review was conducted to assess existing spinal instrumentation techniques employed in the pediatric population. Results: The surgical procedure involved corpectomy at T1 and T2, spinal cord decompression, anterior cervical discectomy and fusion (ACDF) employing the smallest cervical PEEK cage (5 x 12 mm), and specialized plates from an orthopedic finger plating system. Screws ranging from 6 to 8mm in length were utilized to secure vertebral bodies. Notably, an innovative interlocking mechanism was introduced by affixing an anterior plate to a posterior plate configured as a hook, positioning the posterior end behind T3 and interlocking with the anterior plate. The implementation of this technique eliminated the need for an external Halo fixator, ensuring stability during follow-up assessments. Conclusion: Pediatric spine surgeons, particularly those addressing complex spine disorders in infants, require secure and reliable instrumentation techniques with minimal complications and enhanced perioperative comfort. Our novel interlocking technique for anterior spinal fixation demonstrates a substantial reduction in screw pull-out strength, a critical factor in infants with fragile bones, while also improving postoperative patient comfort. This technique represents a unique advancement in anterior cervical discectomy and fusion (ACDF) stability, contributing to the growing body of knowledge in pediatric spinal instrumentation.
2044
RF117: Intra operative manual reduction of post traumatic cervical sublaxation and stabilization: tertiary care center experience
Suresh Jayabalan 1
1 Department of Neurosurgery, Kovai Medical Center Hospital, Coimbatore, India
Introduction: Traumatic cervical dislocation or subluxation is a serious important entity of traumatic sub axial spine injuries. severity of injury varies depends on degree of subluxation, Fracture of the vertebrae, Facetal lock either unilateral or bilateral and Traumatic spinal cord injury. Patients present with minimal cervical pain to complete quadriplegia. Material and Methods: This study has been don at Kovai Medical center Hospital, Coimbatore, India which is a tertiary care center, dealing major Head and spinal injury in this region. We have analyzed all cases of spinal cord injury for last 10 years from 2010 to 2021. Degree of Subluxation, MRI findings, Clinical signs and Degree of Reduction along with fixation techniques assessed. Results: We have analyzed 495 cervical spine injuries, among which 53 patients with different degree of Cervical Subluxation / Dislocation, reduction carried out intra operatively under anaesthesia. 40 patients underwent closed manual reduction successfully and 6 patient underwent anterior intra procedural reduction following failure of closed manual reduction. Cervical traction used in 7 patients who were not willing for surgery and subsequently underwent stabilisation. All patient underwent anterior cervical discectomy and stabilization. No patient underwent Posterior reduction or combined reduction in this series. We will discuss in detail about the procedure, timing of intervention along with influence on success rate and clinical outcome. Conclusion: Closed manual reduction under anesthesia followed by Anterior cervical stabilization is a reliable option in majority of the patients. This procedure if done early gives higher success rate in reduction of subluxation. Clinical improvement mainly depends on extent of cervical cord injury and initial neurological state.
2541
RF118: Validating spinal cord decompression following cervical sci using real-time intraoperative ultrasound
Bizhan Aarabi 1 , Jesse Stokum 1 , Timothy Chryssikos 1
1 University of Maryland, Baltimore, USA
Early surgical decompression in traumatic cervical spinal cord injury (tCSCI) is neuroprotective and the extent of decompression further improves outcome. In a pilot study, real-time intraoperative ultrasound (IOUS) proved to be a valuable diagnostic technique in defining the extent of decompression. Additionally intramedullary lesion length (IMLL) was important in preoperative planning defining the levels of laminectomy. Over a 9-month period 50 consecutive patients with tCSCI were enrolled in this decompressive study. Each patient had a defined algorithm of decompression based on preoperative IMLL and canal stenosis. Decompression was judged by real-time IOUS and postoperative MRI or CT myelogram. Mean age was 59.3 (SD 16.6) years and 42 patients were male. Thirty-one patients had falls, 17 motor vehicle accidents and two were involved in sport injuries. Fracture dislocations were apparent in 28 patients. ASIA motor score (AMS) was 50.2 (SD 36.6) and 17 patients had motor complete tCSCI (AIS grades A in 7 and B in 10). Admission IMLL was 29.9 millimeters (SD 20.4) and postoperative IMLL 42.7 (SD 32.4). All patients had laminectomy and 15 had discectomy and/or corpectomy. Length of laminectomy ranged from 2-6 levels and expansion duraplasty was needed in two patients. Complete decompression was noted in 49 patients with one patient having persistent extrinsic pressure in axial postoperative MRI cuts around C7 lamina. Two patients who needed expansion duraplasty suffered from AIS grade A injuries with an admission IMLL of 83.3 (SD 1.9) millimeters and postoperative IMLL of 161.3 (SD 8.6). Preoperative and postoperative IMLL (p = 0.0001), age (p = 0.003), AIS grade (p = 0.01), and presence of fracture dislocations (p = 0.04) were significant determinants of the need for expansion duraplasty.
2353
RF119: ISCoS Spine Trauma Study Group grading system of spinal cord injury unit
Harvinder Singh Chhabra 1
1 Spine and Rehabilitation Centre, Sri Balaji Action Medical Institute, New Delhi, India
Introduction: The year 1944 witnessed game changing philosophy of Sir Ludwig Guttmann for patients with spinal cord injury (SCI) wherein he advocated comprehensive management for SCI. From “ailment not to be treated” today persons with SCI have “almost same life span as able-bodied individuals”. Management of SCI involves pre-hospital, acute care, comprehensive rehabilitation, mental and social care, community inclusion, and lifelong follow-up. It is well established that specialized SCI units reduce length of stay and complications and facilitate better neurological recovery. Centres in spinal service pyramid cater to all or some elements of SCI care. Hence it is important to identify facilities and manpower available in defining the level/grading of SCI unit. Grading would help in standardization of SCI unit i.e. consistent outcomes, labor savings, improved quality of care, better documentation, reduced waste, improved efficiency, improved patient safety and reduced costs. Recognizing the need, Spinal Trauma Study Group (STSG) of ISCOS worked on grading system of Spinal Unit with global relevance. Materials and Methods: Review of existing literature was done including levels of Trauma Centres proposed by American College of Surgeons (ACS), service description and structural characteristic components of Paraplegic Centre defined by DMGP and Praxis SCI Standards of Care. A draft grading system was prepared and recommendations were presented to group of experts in ISCoS 2020. Inputs were also taken through survey conducted amongst professionals from across the globe and affiliated Societies before finalizing the Grading System. Results: The Grading System incorporates:
• Level wise grading based on available elements of care,
• Resources required
• Quality Metrics
SCI Unit is graded from Level 1 to 5:
Level 1: provides highest tertiary level of acute and rehabilitation care. It would be identifiable as National/Regional centre of excellence.
Level 2: provides comprehensive acute and rehabilitation care. They should work with Level 1 Unit in providing regional support to training, research and prevention activities.
Level 3: provides acute and rehabilitation care. It has been sub-divided into Level 3 ‘S’ and Level 3 ‘R’, based on type of specialization, ‘surgical’ or ‘rehabilitation’.
Level 4: able to provide initial acute management in SCI.
Level 5: caters to basic rehabilitation, community outreach and home care services.
The grading system foresees levels which could perform as a network such that SCI patients would be able to re-integrate within community. Level 3-5 SCI Unit should be attached to Level 1 or 2 SCI Unit.
Quality Metrics: Measures have been defined to assess quality of services provided by SCI Unit.
Conclusion: STSG Grading System is an attempt to provide a system for standardization and grading of spinal services with global relevance, in both emerging and developed countries. It foresees a five level grading system of SCI unit based on available resources and elements of SCI care. Level wise manpower and capabilities/other resource requirements of SCI unit have been defined along with quality metrics. Grading System will need to go through validation process and is expected to gradually evolve as practical issues get obvious with implementation.
663
RF120: Outcome of subaxial cervical spine facet dislocations after short segment fixation with lateral mass screws and wide central laminectomy
Latif Khan 1 , Atiq Zaman 1 , Rizwan Akram 1
1 Orthopaedic and Spine Surgery, Ghurki Trust Teaching Hospital, Lahore, Pakistan
Introduction: Subaxial cervical spine trauma accounts for 65% of cervical spine injures. Road traffic accidents are most common cause of such injuries followed by fall from height or sports injuries. Sub-axial cervical facet dislocation ranges from unilateral to bilateral facet dislocation. Such injuries are commonly associated with neurological injuries ranging from transient neurological loss to complete neurological loss in the form of paraplegia or quadriplegia. Such patients need immediate assessment following strict ATLS protocol to treat life and limb threatening injuries followed by detailed evaluation of spinal injuries. Subaxial facet dislocation need immediate reduction either closed or open followed by fusion. Open reduction can be done from anterior or posterior approach. One believes that reduction by posterior approach followed by lateral mass screw fixation in the absence of traumatic disc herniation is safe and effective in emergency setting. Material and Methods: It is retrospective review of total 48 patients who presented to emergency department of Ghurki Trust Teaching Hospital, Lahore form to with subaxial facet dislocation. Pre operative evaluation included detailed evaluation according to ATLS protocol followed by neurological and radiological evaluation. Patients of either age group and gender having subaxial cervical spine facet dislocation with partial neurology available for follow up who underwent lateral mass screw fixation and wide laminectomy were included. Those patients who have complete neurological loss, neck surgery, unfit for surgery, traumatic anterior disc herniation and now available for follow up were excluded. Postoperative evaluation includes neck disability index and improvement in neurological status according to ASIA score. Results: Total patients were 48, of which 40 (83.30%) were male and 8 (16.6 %) were female. Mean age at the time of surgery was 39.83 ± 15.1 (16-70) years. Mean follow up was 43.34 ± 27.94 (12-95) months. 30 (62.5%) patients have unilateral facet dislocation and 18 (37.5%) have bilateral facet dislocation. Regarding level of dislocation, most common level was C5-6 which was involved in 24 (50%) patients, followed by C6-C7 which was involved in 12 (25%) patients and C4-5 which was involved in 10 (20.83%) patients. C3-4 was involved only in 2 (4.16%) patients. Pre-operatively ASIA impairment scale neurology was Grade E in 20(41.7%) patients, D in 8 (16.7%) patients, C in 6 (12.5%) patients, B in 14 (29.16%) patients. Postoperatively at last follow up mean Neck Disability Index (NDI) was 8.54 ± 6.89 (0-29). There were 13 (27%), 26 (54.160%), 7 (14.6%) and 2 (4.16%) patients in no disability, mild, moderate and severe disability group respectively. Post-operatively, neurology according to ASIA impairment scale there were 34 (70.8%) in grade E, followed by 7 (14.5 %) in group C and 7 (14.5%) in group B. All patient having ASIA grade D and C neurology at presentation gained complete neurological recovery at last follow up. Only 7 patients having ASIA grade B neurology have partial recovery at last follow up. Conclusion: Lateral mass screw fixation for subaxial cervical spine facet dislocation is a safe and effective procedure in emergency setting with reproducible results.
1888
RF121: Use of a novel Ilizarov assembly in cervical traumatic fractures: its results and associated complications
Atiq Uz Zaman 1 , Usama Muhammad 1 , Jawad Haq 1
1 Orthopedics, Ghurki Trust Teaching Hospital, Lahore, Pakistan
Background: At Ghurki Trust Teaching Hospital Lahore a modified assembly of Ilizarov was invented and named as Halo-pelvic traction. It is in use that has its one end fixed to the skull and the other end is fixed to the pelvis via supraacetabular and iliac crest Schanz. This assembly spans the spine and thus can be used for stabilization as well as distraction of the spine. It has been used in correction of scoliotic spine for last few years. The aforementioned assembly has been used for reduction and then stabilization of cervical traumatic fractures as well. Aim: the objective is to summarize the few results and complications associated with the use of this novel assembly in cervical traumatic fractures. Case descriptions: First case was a Jefferson’s fracture (C1 fracture) sustained by a 15-year-old male on falling from stairs while bearing weight on his head. On presentation he had cervical tenderness but neurological examination was unremarkable. Thus, with the aforementioned assembly the fracture dislocation was reduced and stabilized. At 3 months the neurology was static and radiology showed healing thus assembly was removed. At 6 months patient had achieved full pain-free range of motion of cervical spine, had attained radiologic union and had no associated complaints. Second cased was a C3-4 fracture dislocation in a 30 yrs. old male who sustained trauma in an RTA. On examination he demonstrated weakness on the left side with power of 3/5 in both upper and lower limb and had associated numbness. Rest of the neurology was intact. Cervico-pelvic assembly was applied and reduction of the fracture dislocation was achieved, the patient’s neurology improved to 5/5 power and no residual numbness in 3 months. During the 6th postoperative week patient presented with pain at right iliac crest schanz with discharge. The schanz was lose and thus was re-sited. Third case treated with the same assembly was a 38 yrs. old lady whole had a road traffic accident and sustained fracture dislocation of C2 vertebra. On examination the only deficit was motor weakness on the right upper limb (power 4/5). After application of the assembly fracture and dislocation was reduced by applying traction through assemble and at 3 months follow-up the assembly was successfully removed. At 6 months patient still had the aforementioned neurological deficit but had attained pain-free cervical range of motion and radiologic union of the fracture. Fourth case was also C2 fracture in a 20yrs. old male, who had intact neurology and was treated by the aforementioned halo-pelvic traction and achieved union. He developed superficial skin infection at site of pelvic schanz that was successfully managed conservatively. Conclusion: Thus, it can be concluded that the Ilizarov assembly is effective in reduction and stabilization of traumatic cervical fractures but has limitations that of an external fixation device.
1881
RF122: A propensity score match comparative study of standalone vs anterior cervical plating for one to two level anterior cervical discectomy and fusion
Ammad Baig 1 , Mohamed Soliman 1 , Alexander Aguirre 1 , Asham Khan 1 , Esteban Quiceno Restrepo 1 , John Pollina 1 , Jeffrey Mullin 1
1 Neurosurgery, University at Buffalo Neurosurgery, Buffalo, USA
Introduction: Anterior Cervical Discectomy and Fusion (ACDF) can be performed with and without the use of a supportive anterior cervical plating. Fusion rates, incidence of dysphagia, and repeat surgery are a concern when performing ACDF either with or without plating. We aim to compare procedure success, and outcomes between patient groups treated with and without cervical plating for 1-2 level ACDF. Materials and Methods: A prospectively maintained database was retrospectively searched for patients eligible for 1-2 level ACDF. Patients were divided into two cohorts; those treated with anterior cervical plating and those treated without (standalone). Propensity score matching (PSM) was performed to eliminate selection bias and control for baseline comorbidities and disease severity. Patient baseline demographics (age, BMI, smoking status, diabetes, osteoporosis, etc.), disease presentation (cervical stenosis, disk herniation, and trauma), and operative details (no. of levels treated, level of surgery, cage type used, intra- and post-operative complications) were recorded. Outcomes were assessed as fusion observed at 3, 6 and 12 months, patient reported post-operative pain, and any repeat surgeries. Student t-test and chi-square test were performed according to data normality and variables. Results: A total of 365 patients were identified (plating = 288, standalone = 77). After PSM, 130 patients (65 in each group) were included for final analysis. In terms of procedural outcomes, similar mean operative time was noted (101.3 ± 26.5 [standalone] vs. 104.8 ± 32.2 [plating]; p = 0.5), as well as mean duration of hospital stay (1.2 ± 1.8 [standalone] vs. 0.7 ± 0.7 [plating]; p = 0.1). Overall fusion rates were also similar between the two groups (84.6% standalone vs. 89.3% plating; p = 0.5), along with equivalent rates for repeat surgery (13.8% standalone vs. 12.3% plating; p = 0.8). Conclusions: In this propensity score-matched case-control study, we report comparable efficacy and outcomes of performing 1-2 level ACDF with and without cervical plating.
1462
RF123: A challenging case of cervico-thoraco-lumbar tendem spinal stenosis manifested with severe spastic paraplegia : a surgical dilemma and outcome
Mohd Hafizuddin Ahmad Sabri 1
1 Orthopedic Department, University Science Malaysia, Kubang Kerian, Malaysia
Introduction: Tandem spinal stenosis (TSS) is the occurrence of stenosis in at least two or more different regions of the spine. TSS generally manifests as a combination of upper and lower motor neuron deficiency symptoms and signs. This case will describe the clinical presentation of an individual with cervico-thoraco-lumbar TSS (CTLTSS). This case is unique due to the severity of the lesion and the significant neurologic compromise and also demonstrates a dilemma in surgical strategy with regard to the patient factor and condition. Case report: A 53 years old lady with underlying of type 2 diabetes melitus and hypertension presented with a history of bilateral lower limb weakness for the past 6 month. It was gradually began with intermittent back discomfort, an unsteady gait, and frequent falls. One month Later, her bilateral lower limb become spasm and stiff with hip and knee in flexion position. It associated with numbness over the bilateral lower limb. However, there was no bladder and bowel dysfunction. On examination, Her bilateral lower limb, muscle was hypertonia with hip and knee in flex position. Unable to scale the muscle strength in view of her bilateral lower limb was in severely hypertonia and spasm. Best sensory level at the T10 area and Babinski was upgoing. Bilateral upper limb muscle strength was good. However myelopathic sign was positive. Whole-spine magnetic resonance imaging (MRI) was done and showed extensive multi regional spinal stenosis at the cervical, thoracic and lumbar region. At cervical region there was extensive mixed type OPLL from C2 till C7 causing mild spinal canal stenosis. Two compression site at the thoracic area, first at T2/T3 there degenerative disc with impigement over the posterolateral aspect. Multilevel posterior spinal canal lesion from T7 until T11 causing spinal canal stenosis and spinal cord oedema. And at the lumbar area there was degenerative disc disease from L2 until S1, causing multilevel spinal canal stenosis and impingement worse at L4/L5 and L5/S1. She went for surgical decompression and instrumentation of the thoracic level from T1 until T12. Post-operatively, the muslce spasm started to diminished and she able to straighten her bilateral lower limb within 2 week. Further follow-up are needed, as the most recent was at less than one year post-surgery. Conclusion: Surgery that is performed in stages is less difficult and more acceptable to both surgeons and patients. By decompressing several adjacent lesions together in separate stages or resolving one region per stage, patients significantly improve the attenuated risk. In this patient with CTLTSS, our surgical strategies intended to identify the single spinal location with the most severe canal stenosis and match the patient's signs and symptoms to the site of spinal canal stenosis. In conclusion, identification of tandem spinal stenosis is critical as the initial step in therapy, and while there is no preferred technique, both staged and simultaneous operations have been demonstrated to be beneficial.
1648
RF124: Coin test: a novel facile examination for assessing upper extremity function in cervical myelopathy
Xudong Li 1 , Li Jin 1
1 Orthopaedic Surgery, University of Virginia, Charllottesville, USA
Introduction: Cervical myelopathy is a complex neurological condition that often presents with a range of motor and sensory deficits. Common diagnostic tests for myelopathy include the tandem gait, Hoffmann's sign, and various reflex assessments. While the tandem gait test is commonly used to evaluate lower extremity function, there is a gap in assessing upper extremity function. This study introduces a novel facile examination, the "Coin Test," designed to fill this void and evaluate hand dexterity in patients with cervical myelopathy. Methods: A pilot study was conducted, involving 28 patients who were unable to perform the tandem gait due to balance problems. These patients were evaluated using traditional myelopathy exams, including the tandem gait, Hoffmann's sign, and reflex assessments, in addition to the newly introduced Coin Test. The Coin Test involved the placement of a stack of five coins on a table, with patients instructed to move one coin at a time to create another stack. Magnetic resonance imaging (MRI) of the cervical and lumbar spine was performed for each patient, and their medical histories were recorded. For patients with neuropathic symptoms, consultations with neurologists were sought to explore underlying causes. Reasons for the inability to perform the tandem gait were evaluated. The Institutional Review Board approved this study. Results: Among 28 patients, 12 (43%) exhibited both lumbar pathology (5 with lumbar stenosis and 7 with lumbar radiculopathy) and cervical stenosis, rendering them unable to perform both the tandem gait and the Coin Test, except for one patient (8%) who passed the Coin Test. However, their performance in Coin Test was significantly improved after surgical interventions (anterior cervical discectomy and fusion or laminoplasty). Nine (32%) patients with lumbar stenosis failed the tandem gait but they successfully completed the Coin Test. The remaining 7 patients (25%) passed the Coin Test but failed the tandem gait due to various factors, including old age, diabetes, peripheral neuropathy, minor stroke, obesity, thoracic stenosis, and multiple sclerosis. Discussion: The Coin Test proves to be a valuable supplementary tool to assess hand dexterity in patients with cervical myelopathy. Several advantages make it a promising addition to clinical assessments: 1) High specificity, approaching 100%. 2) No specialized training is required for examiners and can be performed by specialists, primary care physicians, or even patients themselves. 3) Easy implementation, as coins are readily available. 4) Potential utility as an outcome measure to assess surgical interventions in cervical myelopathy patients. Altogether, this study underscores the clinical utility of the Coin Test, offering a reliable and accessible means of evaluating upper extremity function in cervical myelopathy patients, which may assist in diagnosis and post-surgical assessment.
804
RF125: How to confirm the operative level in spine surgery: the study using the questionnaire from the Japanese Society for Spine Surgery and related research
Yoshiharu Kawaguchi 1 , Shiro Imagama 2 , Hiroshi Takahashi 3
1 Department of Orthopaedic Surgery, University of Toyama, Toyama
2 Department of Orthopaedic Surgery, Nagoya University, Nagoya, Japan
3 Department of Orthopaedic Surgery, Toho University, Tokyo, Japan
Introduction: In spinal surgery, there are some cases in which it is difficult to confirm the operative spinal levels. In this study, we conducted an anonymous questionnaire survey regarding the experiences and the reasons of wrong site spine surgery (WSSS). We also investigated measures for accurate operation level confirmation through the questionnaire. The purpose of this study was to analyze the factors for WSSS, and to seek the measures for the prevention. Material and Methods: We conducted a questionnaire survey targeting spine surgeons belonging to The Japanese Society for Spine Surgery and Related Research (JSSR) regarding accurate operation level confirmation. The specific questionnaire items were: 1) Years of experience, availability of a specialist, estimated annual and total number of surgeries, 2) How to confirm the operative spinal level, 3) Incidence of WSSS and causes, 4) Current confirming method, 5) Ideal preventive measures for WSSS. Results: 1. Responses were received from 1,275 JSSR members. 3/4 were senior spine surgeons. 2. The method of level confirmation was to place a marker on the spinous process and check it with an X-ray, 68%, put a marker on the skin and check it with an X-ray, 9%, grasp the spinous process with bone grasping forceps during surgery and confirm it with fluoroscopy or X-ray, 15%, and 7% had markings in two places. 3. Approximately 80% had an incidence of WSSS. Operators with more years of experience tended to have more experience. Causes included severe deformity of the patient’s spine and transitional vertebrae. 4. Many answered that they are currently dealing with multiple people, and they answered that the preventive measures were effective. 5) There was an answer that the ideal preventive measure was to confirm the conventional method with multiple people. Conclusion: The causes of WSSS were divided into the surgeon’s and patient’s oriented factors. Several preventive measures are considered, as follows. 1) To confirm the surgical level by multiple surgeons, 2) to avoid a hierarchical environment, 3) to put a marker at the spinous process and take an X-ray, 4) to use fluoroscopy in cases with unclear X-ray, and 5) additionally, to check the spinal level before the patient is awakened from general anesthesia.
213
RF126: Machine learning in predicting cauda equina outcomes
Rosa Sun 1 , Abdel Mageed Rahman 2 , Amin Andalib 1 , Ghayur Abbas 1 , Ahamed Thaaqib Nazar 1 , Marcin Czyz 1
1 Neurosurgery, Queen Elizabeth Hospital, Birmingham, United Kingdom
2 Medical Education, University of Birmingham, Birmingham, United Kingdom
Introduction: Cauda equina syndrome (CES) is a very rare neurosurgical emergency, when missed they have serious disabling consequences for patients and high implications for medicolegal compensation. In the UK, a national increase in emergency MRI scanning has occurred in response. This has flooded scanning capacities at tertiary centres; with low pick-up rates, high cost and clinical burden for neurosurgical departments. We hypothesized the use of machine learning in developing algorithms as an adjunct to screen patients who present with possible CES. Material and Methods: Combined retrospective and prospective analysis of 499 patients who underwent an emergency MRI scan presenting with signs/symptoms of CES. All cases of possible CES were screened between time periods (1/11/21 – 30/11/21, 18/01/23 – 20/02/23). Age, sex, presence of the ‘red flag’ symptoms, total number of the ‘red flags’ as well as diagnosis based on the emergency MRI (CES/no CES) were recorded. Data was fed into WEKA data mining environment. Different classifiers were tested with subgroups for risk-stratification of patients, positive and negative predictive values. Independent variables were tested against each algorithm for their predictive values. Results: Random Forrest classifier was the most accurate in predicting outcomes, achieving 98.96% accuracy in 10 fold cross-validation. IBk and J48 allowed to achieve 98.92% and 98.23% accuracy respectively. No false negatives were generated and all (476/499) 0-20% risk group patients had negative scans for CES. Conclusion: Even with a limited dataset, we demonstrate that machine learning can be useful and safe in identifying true CES among all patients presenting with the ‘red flag’ symptoms of CES. Further data input and training will improve positive predictive algorithms. Machine learning has great potential to dramatically reconfigure our existing knowledge, pathways and investigative protocols of CES.
RFP08: Non-Operative Patient Care
1489
RF127: On-site clinician-led bracing algorithm with short clinical feedback loops lead to significant improvements in bracing outcomes
Anna Courtney 1 , Sam Walmsley 1 , Darren Lui 2 , Jack Choong 1 , Jason Bernard 2 , Tim Bishop 2
1 Orthotics, The London Orthotic Consultancy, United Kingdom 2 Orthopaedics & Trauma, St George's University Hospital, London, United Kingdom
Introduction: Despite the increasing evidence-base for spinal bracing as a key treatment for adolescent idiopathic scoliosis (AIS), efficacious and widespread implementation remains limited. Common barriers include financial restrictions, brace design exclusivity, blocking patents and induced dependence on off-site involvement. This results in lengthy and incomplete clinical feedback loops which impair clinical outcomes such as immediate in-brace correction – a documented primary predictor of overall brace treatment outcomes. Therefore, a clinical algorithm was designed with rapid and complete feedback loops to optimise the initial in-brace correction and fine tune the brace at the fitting stage. This study examined 10 months of clinical data with the new clinical algorithm (LOCBrace) and compared them to 12 months of bracing data with a Chêneau-derivate to assess if it led to improved clinical outcomes. Patients and Methods: AIS patients were treated according to the LOCBrace algorithm. Braces were modelled and manufactured on-site applying Chêneau principles. Baseline x-rays were obtained prior to treatment. Braces were fitted and immediate increase in standing height was used as an indicator for fine tuning. A further x-ray was taken within 72 hours of brace provision measuring Cobb angle in-brace. In-brace correction was measured by Cobb angle as a percentage improvement from baseline. As part of the algorithm, low dose full spinal EOS scans were recommended for the rapid and safe turnaround. Over the course of 10 months, each patient’s pre-treatment and immediate in-brace correction was measured (n = 61) and compared to preceding 12-month data from the Chêneau-derivate (n = 44) to determine the effects of the LOCBrace algorithm on in-brace Cobb Angle correction. For consistency, only patients treated by the same clinician were evaluated in both cohorts. Patients were classified using the Scoliosis Research Society (SRS) inclusion/exclusion criteria. Results: For patients treated within the SRS inclusion criteria, the average correction was 86.04% in LOCBrace compared to 68.42% in the Chêneau-derivate – a 25.76% greater brace efficacy compared to the Chêneau-derivate. For patients treated outside of the SRS inclusion criteria, the average correction was 75.95% in LOCBrace compared to 55.08% in the Chêneau-derivate - a 37.89% greater brace efficacy compared to the Chêneau-derivate. Overall, the average correction was 76.58% for the LOCBrace and 60.13% in the Chêneau-derivate. Conclusions: This study suggests that the use of short clinical feedback loops led by on-site clinicians can improve initial in-brace correction results, which is predictive of enhanced bracing outcomes. In-brace correction rates improved over the course of the study due to immediate feedback into the modelling techniques secondary to rapid data collection using x-rays. The LOCBrace algorithm characterised by clinician driven, in-house manufacturing and rapid feedback loops resulted in improved in-brace correction in AIS patients compared to the preceding Chêneau-derivate brace algorithm.
834
RF128: Pain evaluation a week after sacroiliac joint block is useful for diagnosis of sacroiliac joint dysfunction
Ryota Kimura 1 , Yuji Kasukawa 1 , Daisuke Kudo 1 , Yuichi Ono 1 , Michio Hongo 1 , Naohisa Miyakoshi 1
1 Department of Orthopedic Surgery, Akita University Graduate School of Medicine, Akita, Japan
Introduction: Sacroiliac joint (SIJ) dysfunction is 15 % of the cause of lower back and buttock pain. However, there have been many times when I have treated patients with what I thought was SIJ dysfunction, when in fact it was other diseases. The purpose of this study is to examine the types and incidence of diseases that cause SIJ dysfunction and to compare the effects of SIJ block immediately after and one week after, and to examine its diagnostic utility. Material and Methods: The study design was a retrospective cohort study. The subjects had buttock pain in an orthopedic outpatient clinic and 141 cases had SIJ score 4 or more and we performed SIJ block. Exclusion criteria were Straight Leg Raise Test or Femoral Nerve Strech Test positive cases, motor paralysis cases, and dementia cases. The outcomes are history of disease or surgery around the buttock, such as lumbar disease or hip disease. The block effect was evaluated twice; immediately and one week later. The Pain Relief Scale was used for this evaluation. The block was performed under ultrasound guidance, and 10 mL of lidocaine was injected intra-articularly or intra-ligamentously. If the block was not effective, CT and MRI imaging studies were performed to search for the cause of the pain in combination with other joint/nerve blocks. Results: The immediate effect of the block was observed in 95% of cases and a diagnosis of SIJ dysfunction was made. After one week of the block, 75% of the patients showed efficacy. SIJ dysfunction was the final diagnosis in 77% and others in 23%. Lumbar disc herniation was the most common other, followed by lumbar canal stenosis, discogenic pain, and sacral insufficiency fracture. Twenty-two of the 33 patients, or 67%, also met the diagnostic criteria for SIJ dysfunction and were diagnosed with concurrent SIJ dysfunction. The past medical history included 21 cases after lumbar fusion, 12 cases after lumbar decompression, and 9 cases of lumbar disc herniation for another symptom complaint. A total of 37% had a history of peri-buttock disease. The sensitivity and negative likelihood ratio were comparable, however the specificity (30.3/93.9, respectively) and positive likelihood ratio (1.4/15.8, respectively) were higher for the 1-week effect. Conclusion: SIJ pain can occur with conditions other than SIJ dysfunction. Pain assessment one week after SIJ block is useful in diagnosing SIJ dysfunction. Even if the block is effective immediately after the block, but there is no block effect after 1 week, other conditions should be suspected and further evaluation is needed.
948
RF129: Impact of timing of post-surgical rehabilitation on outcomes after surgery for degenerative cervical myelopathy
Mahmudur Rahman 1 , Anjishu Banerjee 2 , Yushan Yang 2 , Evanka Anyappu 1 , Andrew DeGroot 1 , Benjamin Best 1 , Marjorie C. Wang 1 , Aditya Vedantam 1
1 Neurosurgery, Medical College of Wisconsin, Milwaukee, USA
2 Biostatistics, Medical College of Wisconsin, Milwaukee, USA
Introduction: Despite widespread use, there is no evidence to support the use of post-surgical rehabilitation to improve neurological recovery after surgery for degenerative cervical myelopathy (DCM). Surgical outcome studies for DCM seldom account for the effect of post-surgical outpatient rehabilitation. It is unclear if post-surgical rehabilitation impacts neurological and functional outcomes after surgery for DCM. The aim of this study was to quantify the impact of post-surgical outpatient rehabilitation on outcomes after surgery for DCM. Material and Methods: This study is a retrospective analysis of prospectively collected data from a single center. Consecutive DCM patients who were undergoing surgery from 2011-2015 were enrolled and demographics, imaging, and surgical data were collected prospectively. For this study, additional chart review was performed to record details on post-surgical rehabilitation- timing, type of therapy, duration of therapy and outcomes of therapy. Outcomes were collected prospectively for the modified Japanese Orthopedic Association score (mJOA), Neck Disability Index (NDI), and Short Form 36- Physical Component Summary (SF36-PCS) score at 3, 6 and 12 months after surgery. Linear multivariate regression models were created to determine the effect of type and timing of post-surgical rehabilitation on functional outcomes for DCM, while controlling for age, gender and baseline disability. Results: Sixty-six DCM patients (mean age 55 ± 11, 56% female (n = 37)) were included in the study. Mean duration of symptoms was 46 months. Anterior surgery was performed in 27 patients (41%), posterior surgery in 36 patients (55%) and antero-posterior surgery in 3 patients (4%). The mean preop mJOA was 13.1 ± 2.3, SF36 PCS 36 ± 10 and NDI was 35 ± 19. At 12 months follow-up, the mean mJOA was 14.2 ± 2.4, SF36 PCS 42.3 ± 11.1 and NDI was 24.9 ± 18.5. Eighteen patients (27.2%) underwent post-surgical outpatient occupational therapy (OT), while 49 patients (74.2%) underwent post-surgical outpatient physical therapy (PT). The time interval between surgery and start of outpatient therapy was < 42 days for 31.1% and > 42 days for 68.9%. The most common type of PT was cervical range of motion/neck stabilization (75%), while PT that focused on gait training and upper extremity mobility/strength (11%) were less common. The median number of PT sessions that a patient attended was 6 (range 2-22). Patients who underwent post-surgical outpatient OT had significantly greater improvement in 12-month SF 36PCS scores (p = 0.007) and mJOA scores (p = 0.019). Greater co-morbidities were associated with significantly smaller improvement in mJOA (p = 0.003) and SF36-PCS (p = 0.04) at 12 months. Delaying therapy > 42 days after surgery (compared to < 42 days after surgery) was associated with smaller improvements in SF 36 PCS scores (p = 0.032). Conclusion: Post-surgical rehabilitation is independently associated with sustained improved post-surgical outcomes at 12 months after surgery for DCM and early post-surgical outpatient therapy (< 42 days) was associated with superior outcomes compared to delayed therapy. This study supports the need to control for the effect of post-surgical rehabilitation on surgical outcomes for DCM, as well as the need for prospective comparative studies for post-surgical rehabilitation strategies in DCM.
147
RF130: Cooled radiofrequency treatment for sacroiliac joint dysfunction: clinical outcome from a minimum 2 year retrospective study
Chih-ying Wu 1,2,3
1 Neurosurgery, China Medical University Hsinchu Hospital, Zhubei, Taiwan
2 Neurosurgery, China Medical University Hospital, Taichung, Taiwan
3 Graduate Institute of Integrated Medicine, China Medical University, Taichung, Taiwan
Introduction: The Sacroiliac Joint (SIJ) is a complex structure comprising bone and ligaments, mainly innervated by the dorsal rami of L5 and the lateral branches of S1 to S3. SIJ dysfunction is responsible for 10% to 25% of mechanical low back pain cases. The dysfunction can result from various intra- and peri-articular factors, including trauma, infection, inflammatory diseases, post-spinal fusion, scoliosis, and leg length discrepancy. However, diagnosing SIJ dysfunction remains challenging. The 2009 criteria from the International Association for the Study of Pain (IASP) are still used for diagnosis. Initially, conservative treatments are employed, but if they fail, patients may consider surgery or pain interventions. Pain interventions have advantages such as minimal invasiveness and early ambulation. In our study, we aim to analyze the clinical efficacy of cooled radiofrequency denervation for treating SIJ dysfunction. Material and Methods: Between June 2019 and July 2021, we enrolled 38 patients meeting the IASP criteria for SIJ dysfunction at China Medical University Hsinchu Hospital. Cooled radiofrequency denervation was performed under fluoroscopy guidance, targeting the L5 dorsal ramus and lateral branches from S1 to S3, approximately 5mm from the respective neural foramens. Pain levels were assessed using the Visual Analog Scale (VAS) at baseline, two weeks post-procedure, and during the latest follow-up visit. Additionally, we evaluated the Global Perceived Effect (GPE) during the latest follow-up. Results: The mean age of the 38 patients was 62.1 ± 9.4 years, with 9 males and 29 females. Post lumbar-sacral spine fusion surgery was the leading cause of SIJ dysfunction (57.9%), followed by trauma (28.9%). The mean follow-up time was 35.3 ± 7.8 months. Baseline VAS scores were 7.8 ± 0.9, significantly decreasing to 2.6 ± 2.1 at two weeks and 2.9 ± 2.2 at the latest follow-up visit after treatment (p value < 0.001). During the follow-up, four patients experienced SIJ dysfunction relapse, with an average recurrence time of seven months after cooled radiofrequency treatment. Additionally, six patients did not respond favorably to the procedure. The GPE assessment revealed an 80% positive outcome in terms of perceived treatment effectiveness. Importantly, no major complications, such as nerve root injuries, pelvic organ trauma, or internal bleeding, were reported, indicating the safety of the cooled radiofrequency procedure. Conclusion: In conclusion, our study suggests that cooled radiofrequency denervation can be an effective and safe option for managing SIJ dysfunction, particularly in cases where conservative treatments have failed. However, further research with larger sample sizes and longer follow-up periods may be needed to validate these findings.
1120
RF131: Thoracic spine extramedullary haematopoiesis in two patients with transfusion dependent beta-thalassaemia major
Anderson Yong Zae Szen 1 , Choong Hoon Foo 1 , Sook Kwan Chan 1
1 Orthopaedic and Traumatology, Hospital Queen Elizabeth, Kota Kinabalu, Malaysia
Introduction: Beta-thalassaemia major is the most common inherited blood disorder in Malaysia. One of the common complications of beta-thalassaemia major secondary to chronic anaemic state is extramedullary haematopoiesis (EMH) which refers to haematopoiesis outside of the medulla of the bone. We herein report two transfusion dependent beta-thalassaemia major patients with magnetic resonance imaging (MRI) confirmed thoracic spine extramedullary haematopoiesis presenting with neurological deficits. Material and Methods: Both cases are male patients at age of 17 and 21 years old respectively with underlying transfusion dependent beta-thalassemia major with chronic anaemia presented with complaints of neurological deficit which were objectively assessed with American Spinal Injury Association (ASIA) chart. With alternative causes ruled out and confirmation of extramedullary haematopoiesis through MRI scan. Both subjects were treated with radiotherapy and blood hypertransfusion. Results: Both patient at 1 month follow-up showed significant improvements in neurology to pre-morbid state which were objectively assessed with American Spinal Injury Association (ASIA) chart. Both patients also saw an increase in haemoglobin levels during follow-up. Conclusion: The case series aims to highlight the occurrence of spinal cord compression secondary to thoracic spine extramedullary haematopoiesis (EMH) in transfusion dependent beta-thalassaemia major patients and the positive clinical outcome from radiotherapy and blood hypertransfusion as current management remains controversial. We hope to improve recognition of EMH to avoid irreversible neurological deficits, supplement current practice in the treatment of EMH and provide a starting point for further study on spine extramedullary haematopoiesis in patients with transfusion dependent beta-thalassaemia major.
1768
RF132: Casting for Early Onset Scoliosis - Can it be done without a casting table?
Arjun Dhawale 1 , Shubhanshu Bhaladhare 1 , Akshay Gadia 1 , Munjal Shah 1 , Abhay Nene 1 , Ashok Johari 1
1 Orthopaedics, Bai Jerbai Wadia Hospital for Children, Mumbai, India
Introduction: Casting is an effective and cost-effective treatment for early onset scoliosis (EOS). Early surgery for EOS with growth rods has a high rate of complications. Mehta and Risser have described the use of casting with special casting tables bearing their names. The lack of availability of these special frames and training in casting techniques precludes the use of casting as a popular method of treatment at many centres. There is no literature on the casting method and results without the use of a casting table. The aim of our study is to evaluate the efficacy of a simple and reproducible casting technique with universally available equipment without the use of a special casting table for EOS. Methods: A retrospective study of 27 consecutive EOS children who underwent serial casting under general anaesthesia with a simple technique with two standing stools, a Cervical Sayre traction kit and a metal plate at a children's hospital by one surgeon. Casts were changed every 3-4 months. The pre and post procedure Cobb angle and any complications due to the casting procedure were recorded. At follow-up the Cobb angle was recorded and the treatment plan which was being followed, that is casting, bracing or growth rod surgery. Patient were grouped into congenital and non-congenital EOS and compared. Descriptive statistics and paired t test were used for analysis. Results: 27 children with mean age 4.15 years (range 1 to 9 years) with EOS (15 congenital, 10 idiopathic and 2 syndromic) underwent 116 casting procedures, mean 4.29 casts/ patient. The mean pre-procedure Cobb angle was 63.85 degrees and post procedure Cobb angle was 33.8 degrees, and a significant change was noted (p < 0.05). % Curve correction in Non Congenital scoliosis (31.83%) was better as compared to congenital scoliosis (17.83%) post First Cast (p < 0.05). There were 4 complications noted-three episodes of dermatitis which needed a temporary cast holiday and re-application after an interval and one episode of mild respiratory distress needing cast removal. At mean follow-up of 21.11 months, 16 patients were continuing casting, 2 patient had undergone growth rod surgery, 9 patient was being treated in a brace. Conclusion: The casting technique without a casting table, is well tolerated by children and their families and can be an effective method of treatment of EOS for curve correction, arresting progression and delaying surgery. Also this technique is eminently suitable for under resourced environment. Longer follow-up is necessary.
1918
RF133: Incidence and risk factors for complications following cervical epidural steroid injections
John Kleimeyer 1
1 Orthopaedic Surgery, Stanford University, Stanford, USA
Introduction: Cervical epidural steroid injections (CESIs) are commonly used in diagnosis and treatment of cervical pathology. Rare and severe complications have been reported, but incidence and risk factors have not been well characterized due to the paucity of cases. The purpose of this study was to determine the incidence of complications 7, 30, and 90 days after CESI. Material and Methods: A retrospective cohort study of a large, national administrative claims database was completed. The study included 448,209 patients (age 52.2 ± 11.3 years, 57.1% female) who underwent a CESI from 2008-2015. Outcomes included complication rates following CESI, and risk factors for complication. Adults undergoing a CESI with active enrollment for one year prior to and 90 days after CESI were included. Patients with neoplasm, fracture, infection, inflammatory spondyloarthropathy or cervical surgery within one year preceding CESI were excluded. Multivariable repeated measures logistic regression models were used to identify risk factors for complication at 7, 30, and 90 days. The patient was treated as the repeated factor to adjust for patients having multiple CESIs, and a complication that occurred after multiple CESIs was attributed to the most recent CESI to avoid double-counting. Complications were stratified into procedural and medical complications. Each time point was modeled separately, and level of significance was Bonferroni-adjusted for 3 time points (α = 0.05/3 = 0.017). Results: Complications increased from 1.7% to 4.1% to 8.0% at 7, 30, and 90 days, respectively. Procedural complications occurred in 0.6%, 1.0%, and 1.9%, at 7, 30, and 90 days, respectively. Among procedural complications, neurological injury (0.5%, 0.8%, and 1.3%, respectively) was most common. All other procedural complications occurred in 0.1% of cases or less. After multivariable risk adjustment, a transforaminal approach was associated with greater odds of overall procedural, and neurological complications relative to the interlaminar approach at all time points (all p < 0.001), with odds (95% confidence intervals) at 7 days of 1.23 (1.14, 1.34), 1.55 (1.35, 1.77), and 1.69 (1.45, 1.95), respectively. A myelopathy diagnosis was not associated with risk of overall, procedural, medical, or neurological complications. The most influential factors associated with greater odds of complication at 30 days included anticoagulant use [5.40 (4.55, 6.41); p < 0.001] and diagnosis of venous thromboembolism [3.01 (2.40, 3.77); p < 0.001]. The factors most strongly associated with procedural complications at 30 days included diagnosis of neurologic deficit [3.52 (3.19, 3.88); p < 0.001] and antiplatelet use [2.10 (1.6, 2.68); p < 0.001]. Conclusion: Complications following CESIs are rare, occurring at rates of 0.6%, 1.0%, and 1.9%, at 7, 30, and 90 days respectively. Neurologic injuries were the most common procedural complications and were most strongly associated with anticoagulant use. A transforaminal approach was associated with more frequent complications. A myelopathy diagnosis was not associated with complication risk. Multiple risk and protective factors for severe complications after CESI were identified.
1615
RF134: Robotic assisted surgery in posterior pelvic ring fractures: our experience
Francesco Ciccolo 1 , Sigismondo Mauro 1 , Cesare Vitale 2 , Ilaria Sanzarello 2 , Danilo Leonetti 2 , Daniele Pontoriero 1
1 Ortopaedic Department, Azienda Ospedaliera Papardo, Messina, Italy
2 rtopaedic Department, University of Messina - Policlinico G Martino, Messina, Italy
Introduction: Several techniques are reported in literature to treat posterior pelvic ring fracture with sacral involvement. We report our experience about sacral fracture and posterior pelvic ring fracture. Material and Methods: Retrospective analysis including 18 patient treated, for sacro-iliac fracture/dislocation from September 2018 to September 2022, by Spino-pelvic fixation or trans ileo-sacral screw fixation by Navigated Tc and robotic assisted surgery. In 6 cases we perform a surgical decompression of neurological structure. All patients are analyzed by clinical and radiological follow up at 1, 3, 6, 12 months after surgical treatment. In all cases the patients are preoperative evaluated by X-Ray and Tomography scan and postoperative by clinical Oswestry ODI disability score evaluation and imaging. Results: We report medium follow up 27 months (Max 48-min 6); 16 cases presented an unilateral compromising of posterior pelvic ring, 2 cases bilateral. In 8 cases osteosynthesis hardware are removed at 10 months postoperative. In all cases every systemic traumatic injury are recorded (thoracic, abdominal, cranic and appendicular skeleton). Spino pelvic fixation are performed in 10 patients and in 8 patients we choose trans ileo-sacral screw fixation. Clinical outcome showed good to intermediate results (ODI). ODI score showed worst result in patient with preoperative neurological status compromising. Conclusion: Robotic assisted surgery with navigation and intraoperative TC allows total accuracy in screws insertion. That permits exact alignment of the final construct, reduction of intra operative bleeding and reduction of surgical times. Robotic assisted Spinopelvic fixation represent a good option to treat posterior pelvic ring fracture associated to sacral fracture.
1655
RF135: Combined intraoperative real-time colour Doppler and fluorescein assisted videoangiography guided surgical ligation of spinal dural arterio-venous fistula
Razmeender Singh Kelly 1 , Devatathan Arulkanesh 1 , Kumaran Thinesh 1
1 Neurosurgery, Tunku Abdul Rahman Institute of Neurosciences, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Introduction: Surgical ligation remains the gold standard treatment for spinal dural arteriovenous fistulas (DAVFs). These pathologies are considered rare and during surgical ligation of spinal dural arteriovenous fistulas, all vessels may be dilated and easily mixed-up. Given the rarity and technicalities of spinal DAVFs surgeries, the use of adjuncts when performing surgical ligation is of paramount importance. We describe a series of symptomatic patients with spinal DAVF who underwent laminectomy and surgical ligation of the spinal DAVF using intra-operative colour doppler ultrasound and fluorescein video-angiography (FVA) as adjuncts. Material and Methods: Intra-operative colour Doppler ultrasound and fluorescein video-angiography was utilized during the surgical ligation of a series of patients with spinal dural arteriovenous fistulas. The intra-operative colour Doppler ultrasound was performed using a BK5000 ultrasound machine with a 9062 craniotomy transducer. Intravenous bolus of fluorescein was given to map the vascular angioarchitecture under direct visualization of using the Carl Zeiss Kinevo 900 microscope installed with the Carl Ziess Flow 800 software. Results: The utilization of these adjuncts was effective in identification and proper ligation of the fistula. As the location of the fistulous connection was identified prior to dural opening, only minimally invasive surgery was required. No significant addition in surgical time was seen in patients using these adjuncts. The results were similarly reproduced in all samples within our series. Conclusion: During surgical ligation of spinal DAVFs, all vessels may be dilated and easily mixed-up. Intra-operative colour doppler ultrasound is a readily available, non-invasive, cost-effective tool with a simple learning curve that helps in localization of the fistulous point in the surgical management of spinal dural arterio-venous fistulas prior to dural opening. Fluorescein video-angiography is a reliable method to accurately identify the fistulous point and ensure proper ligation of fistulous points in spinal dural arteriovenous fistulas surgeries.
1946
RF136: Accuracy of pedicle screws trajectories using neuronavigation and 3D-CT in adult spinal deformity: A comparative analysis of predicted angles and pedicle screws in a Colombian cohort
Pablo Sanchez Quinones 1 , Leonardo Laverde 1
1 Neurosurgery Department, Hospital Universitario Mayor Méderi, Bogotá, Colombia
Introduction: Intraoperative imaging acquisition with real-time and three-dimensional reconstruction is now considered a standard in complex spinal pathology healthcare due to its accuracy in predicting transpedicular trajectories. We assess the accuracy of pedicle trajectories in adult spinal deformity correction comparing the coincidence between the pedicle trajectory angle using neuronavigation (anatomical pedicle axis) and the angles obtained from 3D tomography for each surgically treated patient (transpedicular screw axis), in a Latin-American (Colombia) cohort. Materials and Methods: We evaluated retrospectively collected data from 2017 to 2022. Thoracic and lumbosacral pedicle screws analyzed were placed using intraoperative O-arm navigation system. Axial angles were measured using the midline of the vertebral body whereas the sagittal angles were compared using the superior vertebral endplate as a reference. The degrees were described using means, standard deviations (SD), and 95% confidence intervals. Values were presented globally and stratified by vertebral level. To assess the agreement of angles before and after the measurements, a mixed linear regression model was developed. Results: Twenty-six patients were included, for a total of 273 pedicle screws in 142 vertebral segments. Globally, the mean axial angle of the anatomical pedicle axis (without screws) was 13.9º (95% CI: 13.2-14.6), and the sagittal angle 5.8º (95% CI: 5.2-6.4). The planned angle before screw placement was on average 1.8º degrees greater than the angle of the final trajectory (95% CI: 0.9 to 2.7) in the axial angle and 0.9 degrees greater in the sagittal angle (95% CI: 0.1 to 1.7). A total of 4 pedicular screw trajectories were replaced, accounting for 1.46% of the total screws analyzed, all of them in L5 segment. The correlation between the screw positioning angle and the predicted angle by neuronavigation in the axial plane was statistically significant (p: 0.001). For every 1-degree increase in the angle calculated by neuronavigation, the final trajectory increased by 0.19° (95% CI: 0.07-0.31). This relationship was also observed by levels, especially in screws placed at dorsal level (p: 0.047). In the sagittal plane, there was a 0.24° increase in the final angle for every 1-degree increase in the angle predicted by neuronavigation at the lumbar level (95% CI: 0.089-0.406). Interestingly, greater angular variability in the sagittal plane was demonstrated in the thoracic spine without clinical representation. Similarly, greater axial angular variability was demonstrated in the lumbosacral spine compared to thoracic axial angles. Conclusions: This is the first study to assess the accuracy of pedicle screws trajectories in adult scoliosis using neuronavigation and 3D CT in Colombia. Overall, pedicle height in the thoracic segment and pedicle thickness in the lumbosacral segment allow for angular variations without clinical representation, so future research should establish the degrees of pedicle safety margins in our population. We have found that the pedicle screw placement technique for adult scoliosis correction using neuronavigation and 3D CT provides high accuracy for pedicle screw trajectories. This technique has been established as routine practice in our surgical procedures.
1103
RF137: Risk factors of screw misplacement by using intraoperative computed tomography image guided navigation: a series of 1471 screws
Bastian Stemmer 1 , Baptist Pia 1 , Ertl Sebastian 1 , Ehab Shiban 1
1 University hospital Augsburg, Department of Neurosurgery, Augsburg, Germany
Introduction: The aim of this study was to identify potential risk factors for screw misplacement after using an intraoperative computed tomography (iCT) guided navigation for Screw insertion. Methods: A retrospective analysis of all patients following iCT navigated spinal pedicle screw placement between October 2015 and March 2022 was performed. Navigated drilling of the pedicle was followed by screw placement (with and without via K-wire). Screw position was checked by a further iCT scan. Screw position was assessed according to the Gertzbein-Robbins classification and the rates of screws actually revised intraoperatively were calculated. Results: 256 consecutive patients were identified (50.39% male, 49.61% female). A total of 1471 Screws were implanted. Median age was 67 years. The all-over revision rate was 4.49%. Screws were placed in all spinal regions. Degenerative spine disease was the most common diagnosis (43.44%). No significant differences in revision rates were found for gender and age. Lumbar spine (6.25%), thoracic spine (5.86%), tumor (6.40%) and infection (7.98%) diagnosis were associated with highest revision rate. We also found significantly increased revision rates for overweight (BMI 25 to 30) and obesity (BMI > 30) at 4.17% and 7.38%. Conclusion: The all-over revision rate was 4.49%. The highest revision rates were observed for tumor (6.40%), infection patients (7.98%), lumbar spine (6.25%) and thoracic spine (5.86%). Overweight and obesity also seems to be a significant risk factor for screw misplacement (BMI < 25: 0.46%; BMI 25 to 30: 4.17%; BMI > 30: 7.38%). None of the patients suffered from any neurovascular damage. No secondary operation to revise the misplaced screws was required.
323
RF138: Computer-assisted navigation for T2 pedicle subtraction osteotomy in ankylosing spondylitis with cervico-thoracic kyphotic deformity
Urawit Piyapromdee 1
1 Orthopedics, Maharat Nakhon Ratchasima Hospital, Nakhon Ratchasima, Thailand
Introduction: Managing Ankylosing Spondylitis with cervicothoracic kyphotic deformity (CTKD) poses significant challenges. Osteotomy corrections, which aim to address both deformity and neck pain, are considered high-risk procedures. However, the use of T2 pedicle subtraction osteotomy (T2PSO) helps reduce the risk of vascular and nerve injuries. Additionally, incorporating Computer-Assisted Navigation surgery enhances the precision of osteotomy planning and pedicle screw placement, leading to improved overall outcomes. The objective of this study is to describe the application of computed tomographic (CT)-based image navigation for planning pedicle screw placement and executing T2PSO in Ankylosing Spondylitis with CKTD. Material and Methods: Preoperative planning aimed to correct the global sagittal alignment and chin-brow vertical angle using a specific program called ASkyphoplan for deformity planning in ankylosing spondylitis. The surgical planning for screw and osteotomy positions was developed based on preoperative CT data. Intraoperative registration and verification of anatomic landmarks were performed using CT-based navigation across the cervicothoracic junction. The navigation probe was utilized to identify the targeted pedicle and rehearse and save the intended trajectories on the navigational computer. During the T2PSO procedure, the navigation probe was used to ensure the depth, accuracy, and trajectory on each side. Preoperative and postoperative sagittal plane radiographic measurements were compared, while the chin-brow vertical angle (CBVA) was measured using clinical photographs. The operative technique and perioperative complications were thoroughly documented. Results: The author reports on a 60-year-old male who presented with Ankylosing Spondylitis with CKTD and underwent T2PSO. The correction of C2-C7 SVA was 4.5 cm, and the CBVA correction was 25 degrees. No neurologic complications were observed. Conclusion: The application of Computer-Assisted Navigation T2PSO offers a safe and effective method for managing cervicothoracic kyphotic deformity. This procedure demonstrates outstanding correction of cervical kyphosis and delivers favorable results in terms of restoring the chin-brow vertical angle (CBVA).
2049
RF139: Robot-assisted pedicle screw insertion: an UK Tertiary spine centre experience
Fabian Wong 1 , Priyanka Jani 1 , Michael Mokaem 1
1 Spinal Surgery Unit, Royal National Orthopaedic Hospital, London, United Kingdom
Introduction: We are the first NHS hospital to adopt robot-assisted (RA) pedicle screw insertion in adult thoracolumbar spine. The aim of this study is to assess the placement accuracy and cortical breach rate of RA-pedicle screws and to compare with published data in current literature. Material and Methods: Ours is a single centre prospective study. Patients who had RA-pedicle screw insertion between January 2019 and August 2023 by single surgeon in UK tertiary spinal unit, were included. Data on the screw positioning was assessed on routine post-operative scans either by O-arm in theatre or CT. Data was collected on patient demographics, radiological evidence of cortical breach, accuracy of screw placement, and any peri- and post-operative complication. The Gertzbein and Robbins (G&R) classification was used to report the accuracy of screw placement. Results: A total of 20 patients were identified and included. There were 127 RA screws inserted. There were 4 screws with cortical breaches (medial = 1, lateral = 2, anterior = 1), with an overall breach rate of 3.1%. All screws were deemed Grade A based on the G&R classification, giving 100% accuracy. None of the patient with cortical breach suffered from neurological or vascular deficit. One patient required return to theatre for rod revision for disengagement from the locking mechanism. Conclusion: Our study is the first NHS single centre, single surgeon experience with over a hundred robot-assisted pedicle screws inserted. Our result is comparable to a similar international series of over a thousand RA screws using the same robotic system, with an accuracy (G&R Grade A) of 94%, although their actual cortical breach rate was not known. Further studies including comparison and cost-analysis of robotic systems are required to strengthen the current body of evidence to help inform clinical decision-making and surgical planning.
1572
RF140: First MRI navigated spinal fusion in the USA
David Zurita 1 , Jacob Rumley 1
1 Orthopedic Surgery - Spine, Scientific Education and Research Foundation AO Spine Fellowship, Thornton, USA
Background: Image guidance navigation has become a widely used aid in spine surgery to place accurate and safe pedicle screws. However, many navigation systems are reliant on Computed Tomography imaging, either acquired pre-operatively, intra-operatively or both. This causes a large radiation burden on the patient. However, recent advances in technology have allowed the option to use multiple MRI sequences to provide the bony anatomy needed for intraoperative navigation, thus reducing the amount of radiation the patient receives dramatically. Case: Patient is a 60-year-old male with a complex spine history, significant for tandem stenosis at the cervical and lumbar regions. He had prior anterior cervical discectomy and fusion at C4-C7 due to myelopathy. He was indicated for a T12-Pelvis posterior spinal fusion with transforaminal lumbar interbody fusion from L3-S1. Due to being the first case utilizing MRI for navigation, the patient obtained both the MRI as well as CT for both diagnostic and navigation purposes. Intra-operatively, the MRI navigation sequences were correlated with the CT sequences as well as fluoroscopy to confirm accurate screw placement. Conclusion: MRI proved to provide accurate sequences needed to place safe and precise pedicle screw via navigation. This was continuously confirmed with well-established CT and fluoroscopy techniques. Post-operative radiographs again confirmed accurate placement of the screws. The ability to provide patient’s the option of navigated spine surgery without the risk of radiation and cost of CT scans is an exciting advance in the field of spine surgery.
1855
RF141: Utilization and reimbursement of the top ten most common spine procedures: a retrospective analysis using a large national insurance claims database
Hannah Shelby 1 , Michael Kim 1 , Tara Shelby 1 , Jacob Ball 1 , Andy Ton 1 , Sagar Telang 1 , Raymond Hah 1 , R. Kiran Alluri 1
1 Orthopaedics, University of Southern California, Los Angeles, USA
Introduction: There has been limited investigation into reimbursement trends in spine surgery. The objective of the present study is to query a large, national insurance claims database to assess how utilization and reimbursement has changed for the top ten most common spinal procedures from 2010 to 2021. Material and Methods: PearlDiver, a large, national insurance claims database, was queried for data from 2010 to 2021 for common spine procedures using Current Procedural Terminology (CPT) codes. For the ten most common spinal procedures, annual reimbursement rates by payor (commercial, Medicare, Medicaid, Government, cash, other) and demographic data including gender, age, region, payor type, and service location were extracted. Dollar values have been adjusted using the Consumer Price Index and are reported in 2023 US dollars. Trend analysis was performed for the larger cohort, with subsequent subanalysis separated by payor and by type of procedure. Results: 1,819,635 patients underwent the top ten spinal procedures from 2010 to 2021. From greatest population to least, the top ten spinal codes broadly covered fusion, laminectomy, and laminotomy (included codes: CPT-63047, CPT-63030, CPT-63048, CPT-22551, CPT-22612, CPT-22614, CPT-22552, CPT-22633, CPT-22558, CPT-22585). All procedures, combined and individually, demonstrated a significantly positive linear trend in use over the included time period (combined: +24%, p < 0.001; fusion: +46.32 %, p < 0.001; laminectomy: +24.2%, p < 0.001; laminotomy: +3.5 %, p = 0.02). Medicare beneficiary utilization also significantly increased by +1.68% (p < 0.001) during this time. On the other hand, Medicare reimbursement demonstrated a significant decline across fusion alone (all time: -12.47%, avg annual: -2.57%), laminectomy alone (all time: -25.20%; avg annual: -1.09%), laminotomy alone (all time: -12.70%, avg annual: -0.63%), and the three procedures combined (all time: -13.19%, avg annual: -2.06%). Conclusion: Despite the growing number of Medicare beneficiaries and utilization of all included procedures, the present data has demonstrated a decrease in Medicare reimbursement across all subgroups. Knowledge of such trends is important for the orthopedic field in order to advocate for sustainable reimbursement that supports the consistent delivery of high-quality patient care. Further analysis will include analyzing trends of other reimbursement modalities across all three procedure groups.
848
RF142: Enhanced recovery after spine surgery (ERASS), time to change traditional outlook and protocols?
Kedar Parelkar 1
1 Spine, We are Spine, Mumbai, India
Background: There is limited published research regarding implementation of enhanced recovery after surgery (ERAS) for spine surgery. ERAS was popularized by Henrik Kehlet originally called “fast track surgery” which included pre-operative care, multimodal optimization of patient pathway, improved patient experience and reduction in length of stay. Aim: This study is aimed to change traditional outlooks and protocols in all spine surgery and improve patient outcome, reduce length of stay as well as reduce patient expenditure in spine surgery. Materials and Methods: All cases between the age group of 18 years to 98 years who were operated for spine surgery and post operatively managed with traditional post-operative protocols and ERAS protocol were considered for this study. This group included 300 patients managed by traditional post-operative protocols post spine surgery and 300 patients managed by ERAS protocol. Traditional management constituted of longer pre-operative stay, delayed post-operative mobilization, ERAS bundle included elements such as multimodal analgesia, early post-operative mobilization and physiotherapy etc. Traditional and ERAS data was compared to evaluate the benefits and check the complications in both groups. Results: A total of 600 patients were included from the July 2018 to June 2021. Patients in the group managed post operatively with ERAS showed a better functional outcome, patient satisfaction scores were higher, patients scored lower on the pain scale and showed early recovery. Conclusions: We implemented an ERAS protocol for all spine surgeries in our limited 600 patient study group and identified the various benefits from perioperative intervention, intra operative measures and post-operative protocols. Within our limited study group of 600 patients, it was noted that the ERAS protocol helped to improve patient experience, surgical outcomes, reduced length of stay along with reduced complications associated with delayed mobilization and prolonged hospital stay.
Keywords: Spine surgery, ERAS, mobilization, recovery
1476
RF143: Investigation into the patient reported outcomes of patients receiving perioperative services prior to surgery compared to those who do not
Alana Celenza 1 , Jessica Gaff 1 , Gregory Cunningham 1 , Michael Kern 1 , Andrew Miles 1 , Paul Taylor 1
1 Research, NeuroSpine Institute, Perth, Australia
Introduction: Perioperative care provides a means of mitigating complications particularly in high-risk patients, improving communication between healthcare professionals. These services are uncommon in neurosurgical and orthopedic practices. This study aims to assess the effectiveness of a perioperative services by comparing the rates of morbidity, complications, revision, and patient reported outcome measures (PROMs) between patients who received perioperative consultations prior to surgery with those who did not. Methods: Here, a retrospective analysis of prospectively collected demographic, perioperative and pre- and post-operative PROMs data was performed. PROMs included the EQ-5D-5L, VAS to assess back, leg, neck and arm pain intensity, the Oswestry Disability Index (ODI) and Neck Disability Index (NDI) to assess back and neck-pain related disability. Outcomes between those who received perioperative services prior to surgery (PO) and those who did not (NPO) were analysed. Results: A total of 989 participants with a median age of 58 years, a body mass index (BMI) of 27.8 and 45% female underwent lumbar surgery and 304 participants with a median age of 53 years, a BMI of 27.8 and 41% female underwent cervical surgery. Of these, 201 (20%) lumbar and 59 (19%) cervicothoracic patients received perioperative services prior to surgery. The PO group was significantly older (54 vs 66 years; < 0.001) and had a relatively higher BMI compared to the NPO group (27.8 vs 28.4; p = 0.24). A total of 6 (1%) cases for the PO group and 11 (2%) cases for the NPO group were considered complex. Three participants in the PO group required revision surgery after their primary lumbar procedure compared to 14 participants in the NPO group (p = 0.8). The post-operative complication rate for the PO group was 10% compared to 12% for the NPO group (p = 0.44). For lumbar procedures, the PO group reported better pre-operative ODI (p = 0.016) and VAS for leg pain scores (p = 0.055) than NPO group. At follow up the PO group also demonstrated better VAS Back and Leg scores at 12, 24 and 52-weeks post-operative. This was only significant for VAS Leg at 12-weeks (p = 0.009). Scores were similar at each timepoint for EQ-5D-5L VAS and Index and ODI measures. No differences were observed in pre-operative cervical PROMs (p > 0.05) and the NPO group demonstrated better VAS Neck and NDI scores at 12, and 52-weeks and in VAS Arm scores at 24 and 52-weeks post-operative compared to the PO group. This was not significant at any timepoint. Scores were similar at each timepoint for EQ-5D-5L VAS and Index, but significantly worse in EQ-5D-5L scores for the PO group at 24-weeks (p = 0.047). Conclusion: Here, patients receiving perioperative services prior to surgery were significantly older, generally had a higher BMI, and a similar number of complex cases. The complication rate was generally lower in the PO group and less revision procedures were required and both groups reported improvements in PROMs. Investigation in a larger cohort and with a prolonged follow-up period may identify greater distinctions in outcomes. Overall, this study demonstrates perioperative services may be beneficial to patients at high-risk of post-operative complications.
2430
RF144: What is the impact of socioeconomic status on the mental and physical health, functional recovery, and risk of post operative complications in spine surgery?
James Hall 1 , Alex Coffman 1 , Brandon Marshall 1 , Sarah Ryan 1 , Natalie Glass 1 , Cassim Igram 1 , Andrew Pugely 1 , Catherine Olinger 1
1 Orthopedics and Rehabilitation, University of Iowa Hospitals and Clinics, Iowa City, USA
Introduction: Socioeconomic status (SES) has been recognized as a domain outside the individual’s control that may influence other health domains. Within the field of Orthopaedic Surgery, low SES is associated with decreased survival in sarcoma patients, increased musculoskeletal symptoms, and associated functional impairment. The impact of SES on patients undergoing spine surgery, however, is not completely understood. Area Deprivation Index (ADI) is a composite measure of income, education, employment, housing quality, and access to social services that encompasses SES. Our primary aim was to evaluate the association between ADI and patient-reported physical and mental health in patients undergoing thoracolumbar spine surgery. Our secondary aim was to evaluate the association between ADI and the risk for post-operative complication following spine surgery. Material and Methods: A single-center retrospective cohort analysis using electronic medical record (EMR) data from patients undergoing spine surgery between Jan 1, 2019 and Dec 31, 2020. IRB approval was obtained. Patients aged 18 years and older who underwent thoracolumbar spine surgery with greater than 3 levels addressed were identified. Demographic information including age, sex, race, body mass index (BMI), primary residential address, smoking status, American Society of Anesthesiologists (ASA) classification were collected. Review of the medical record was completed to determine 90-day re-operation and post-operative medical complications. The Charlson Comorbidity Inex (CCI) was calculated for each patient at the time of surgery. Patient reported outcomes measures (PROM) scores including Oswestry Disability Index (ODI), Modified Japanese Orthopaedic Association (mJOA), and Patient-Reported Outcomes Measurement (PROMIS) physical and mental health were assessed. ADI was used to define SES. Participants were stratified into ADI tertiles with the highest tertile having the lowest SES and greatest amount of socioeconomic deprivation. Mean baseline, postoperative, and baseline to postoperative changes in PROM scores were compared among tertiles using generalized linear models. Logistic regression was used to model the association between ADI tertiles and odds of postoperative complication or 90-day reoperation. Results: 283 patients (mean age = 61.3 ± 14.3 years, 45% women) were included in analyses. Groups did not differ regarding age, sex, tobacco use, ASA or CCI. Patients in the highest ADI group had a higher BMI when compared to the middle group, but not compared to the lowest group. Race approached significance with those in the highest ADI group having a higher proportion of non-white participants, however all groups were predominantly White. Preoperative PROMs did not significantly differ among tertiles (p = 0.549). 3-month and 12-month follow-up PROMs showed significant differences in 3-month ODI with the middle deprivation group having less disability than the lowest and highest deprivation groups (p = 0.03 and p = 0.04). Change in PROMs from baseline was only significant in the 12-month post-operative ODI with the middle deprivation outperforming the highest deprivation group (p = 0.03). There was no significant difference between groups regarding 90-day re-operations or post-operative complications. Conclusion: Socioeconomic deprivation does not appear to affect preoperative or postoperative PROMs of patients undergoing thoracolumbar spine surgery greater than 3 levels. ADI does not impact changes in postoperative PROMs when compared to preoperative baseline.
RFP09: Novel Technologies
2004
RF145: Optical-kinematic measurement of spinal alignment: a radiation-free technique using light field navigation
Sigurd Berven 1 , Erica Bisson 2 , Steven Glassman 3 , Charles Fisher 4 , Kosei Nagata 3 , Catherine Olinger 5 , Rafid Kasir 6 , Timothy Chryssikos 7 , Rob Grupp 8 , Thomas Carls 8 , Sarah McGray 8
1 University of California, San Francisco, USA
2 Neurosurgery, University of Utah, Salt Lake City, USA
3 Norton Leatherman Spine Center, Louisville, USA
4 Vancouver Spine Surgery Institute, Blusson Spinal Cord Center, Vancouver, Canada
5 University of Iowa, Iowa City, USA
6 Orthopedic Spine Surgery, San Diego Orthopedic Associates Medical Group, San Diego, USA
7 Department of Neurosurgery, University of Maryland, Baltimore, USA
8 Preclinical Research, Proprio, Seattle, USA
Introduction: Achieving patient-specific spinal alignment goals is an important determinant of clinical outcomes and surgical complications. The conventional method for intraoperative assessment of spinal alignment can be difficult to assess, has inherent variability, and requires use of ionizing radiation, adding operative time and radiation exposure. Volumetric Intelligence (VI) is a radiation-free, real-time optical tracking tool that reports spinal alignment measures, enabling intraoperative confirmation that preoperative goals have been achieved. The purpose of this study is to demonstrate the accuracy of VI compared with manual measurement in the assessment of spinal alignment. Materials and Methods: This study compared novel and conventional methods for alignment measurement in a cadaveric specimen using data captured intraoperatively. Novel method: Data was collected with a navigation system powered by light-field and optical sensing technologies. A virtual 3D model of the spine was created from a preoperative CT. The navigation system was then used to instrument T10-S1 and to save the vertebral coordinates of the spine in a pre-correction state. Lateral fluoro shots were also taken at this pre-correction timepoint. The pedicle screws were compressed to increase segmental lordosis, creating a “corrected” construct. The light-field navigation system was again used to save post-correction vertebral coordinates and a second set of lateral fluoro shots was taken. The saved intraoperative vertebral coordinates were then processed with VI to calculate regional and segmental sagittal angles for each of the pre- and post-correction timepoints. Conventional method: The companion fluoro shots were individually reviewed by spine surgeons who defined vertebral endplates for assessing manual measurements. For regional measures, multiple fluoro shots were stitched together. Manual measures were calculated from the surgeon-defined endplates and compared with the VI calculations. Results: Seven spine surgeons each annotated 28 scans from a single cadaveric specimen. Across all data, the mean absolute difference between automated 3-D measurements and manual measurements was 1.96° (SD = 1.30) and 95% of all data were within ±2.53° of the manual measurements. The mean absolute difference of manual measurements from manual mean was within ±3.38° (RMSE). In measures of lumbar lordosis (L1-S1, L4-S1) the mean absolute difference of the 3-D and manual measurements was 1.60° (SD = 1.10). There was a strong correlation between the automated and the manual measures (r = 0.98, p < 0.0001). For the manual measures, inter-rater and intra-rater reliability was also good (ICC = 0.94 and 0.90, respectively). Conclusion: There is a strong correlation between Volumetric Intelligence and manual measurements for intraoperative assessment of alignment. VI enables intraoperative confirmation that alignment goals have been achieved without use of radiation and in a fraction of the time needed to obtain intraoperative XR and complete manual measurements. VI could potentially be used to assess other parameters, such as disc height, foraminal height, and pelvic tilt.
1155
RF146: Three-dimensional reduction technique with a modified C2 isthmus screw in irreducble atlantoaxial dislocation: a technique note
Xiongsheng Chen 1
1 Orthopeadics, Shanghai General Hospital, Shanghai, China
Background: Reduction technique plays a decisive role in the operation of irreducible atlantoaxial dislocation (IAAD). At present, the most commonly used techniques include C1 pedicle screw (PS) or lateral mass screw (LMS), and C2 pedicle screw or short isthmus screw. These techniques lack sufficient reduction space due to the short anteroposterior and vertical distance between the screw heads, resulting in difficult reduction. It is often impossible to obtain a satisfactory reduction at one time. The aim of this study was to describe a 3D reduction technique of a modified C2 isthmus screw and evaluate its safety and efficacy in the treatment of IAAD. Methods: Twelve patients with IAAD received surgery with modified C2 isthmus screw combined with C1 PS or LMS and bone graft fusion. The entry point was located on the lateral side of the intersection between the caudal edge of the C2 lamina and the lateral mass, and the C2 isthmus was the entry point through the lateral mass. 3D reduction was achieved by pulling C1 posteriorly and distracting between C1 and C2. The C1-C2 angle was corrected by pre-bending of connecting rods. Imaging evaluation included the distances between the entry points of C1 and C2 screws, occipital-axial Angle (O-C2A), clivus canal Angle (CCA) and cervical spinal cord Angle (CMA). Japanese Orthopedics Association (JOA) score, Visual analogue scale (VAS) and Neck Disability Index (NDI) were used to evaluate the clinical outcomes. Results: All patients maintained effective reduction during follow-up. The average length of C2 screws used in all the patients was 22 mm. No matter combined with C1 screw or combined with LMS screws, the anteroposterior distance and direct distance of the modified C2 isthmus screw were greater than those of the C2 PS screw, and the differences were statistically significant (p<0.05). The O-C2A, CCA, CMA, JOA score, NDI and VAS were significantly improved after operation (p<0.05). Conclusion: The modified C2 isthmus screw three-dimensional reduction technique is safe and effective in the treatment of IAAD. It can increase the anteroposterior and vertical distance between the C1 and C2 screws, which is beneficial to the three-dimensional reduction of IAAD.
1009
RF147: The Kiva system versus balloon kyphoplasty for vertebral compression fractures: a meta-analysis of randomized controlled trials
Humaid Al Farii 1 , Nikhil Gattu 2 , Caleb Yeung 3 , Christopher Alvarez-Breckenridge 4 , Rob North 4 , Claudio Tatsui 4 , Laurence Rhines 4 , Valerae Lewis 5 , Justin Bird 5 , Shalin Patel 5
1 Orthopaedic Surgery, Sultan Qaboos University Hospital, Seeb, Oman
2 The University of Texas Health Science Center at Houston, Houston, USA
3 OrthoVirginia, Alexandria, USA
4 Neurosurgery
5 Orthopaedic Oncology, The University of Texas MD Anderson Cancer Center, Houston, USA
Introduction: Vertebral compression fractures (VCFs) commonly occur in patients with osteoporosis and can also arise due to trauma and metastasis. The Kiva VCF Treatment System is a relatively new and novel technique to manage VCFs. The aim of this study is to examine the efficacy of the Kiva system versus existing balloon kyphoplasty (BK) in the surgical treatment of VCFs through evaluation of published randomized controlled trials (RCTs). Materials and Methods: This study was performed following PRISMA guidelines. We performed a systematic literature search using the PubMed and MEDLINE databases in June 2023. The search keywords used were “Kiva” and “Kyphoplasty”, which yielded a total of 112 articles from both databases. Studies were excluded if they were not RCTs, included patients < 16 years of age, were commentary or editorial pieces, or did not compare clinical variables. Outcome measures included pain, measured through the Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI), and cement leakage rates. Risk of bias was assessed according to the Cochrane Handbook for Systematic Reviews of Interventions. Combined data from the included studies was utilized to perform a meta-analysis. Data was analyzed using IBM SPSS Statistics Version 28.0. Results: Three RCTs were included in this meta-analysis. A total of 468 patients (232 treated with Kiva and 236 treated with BK) and 694 VCFs (351 treated with Kiva and 343 treated with BK) were included after fulfilling the inclusion and exclusion criteria. The mean age of the patients was 73.5 years and the patient cohort consisted of 356 females (76.1%). The revised Cochrane risk-of-bias tool indicated that all of the included RCTs were free of bias. The VAS pain score in both the Kiva and BK groups improved significantly. However, there was no difference in VAS improvement between the two groups (95% CI [-0.19, 0.23], p-value = 0.84). VAS score reduction was compared between patients who were receiving treatment for osteoporotic VCFs and VCFs caused by osteolytic metastases. In this subgroup analysis, there was no significant difference in the VAS improvement between the two groups (95% CI [-0.17, 0.22], p-value = 0.78). Of the 694 fractures that were treated procedurally, the Kiva system had significantly less cement leakage than BK (95% CI [-0.89, -0.22], p-value < 0.001). Conclusions: This meta-analysis demonstrates that the Kiva system and balloon kyphoplasty are both reasonable surgical options for the purpose of reducing pain associated with VCFs, whether osteoporotic or metastatic in etiology. However, the Kiva system demonstrated lower rates of cement leakage compared to BK, and may be a more favorable treatment strategy from this standpoint.
1295
RF148: Initial experience with novel system for robotic-assisted pedicle screw placement in thoracic and lumbar spine: first 425 screws
Mirza Pojskic 1 , Miriam Bopp 1 , Christopher Nimsky 1 , Benjamin Saß 1
1 Department of Neurosurgery, University Hospital Marburg, Marburg, Germany
Introduction: The aim of this study is to present thoracolumbar pedicle screw placement using Brainlab’s Cirq® surgeon-controlled robotic arm (BrainLab, Munich, Germany) and its robotic alignment module. Material and Methods: All patients who underwent robotic-assisted implantation of pedicle screws in the thoracolumbar spine at our Department in period January 2020 – September 2023 were included in the study. Pedicle screw accuracy was assessed using Gertzbein-Robbins scale (GRS). Results: A team of two surgeons conducted 66 surgeries in 65 patients (29 male, median age 70.35 ± 9.9 years) with robot-assisted pedicle screw placement. Indications included degenerative spine disease (n = 19 patients), spondylodiscitis (n = 16), metastases (n = 18), primary spinal tumors (n = 2) and fracture (n = 10). 19 surgeries were performed in thoracic spine, 27 in lumbar and lumbosacral spine and 19 in thoracic and lumbar spine. Workflow included intraoperative computed tomography (iCT) imaging with automatic registration, fusion with preoperative imaging and review of the preplanned screw trajectories, robotic-assisted insertion of K-wires, followed by a fluoroscopy-assisted insertion of pedicle screws (first 12 surgeries) or insertion of navigated screws (latter 23 surgeries), with control iCT scan. A total of 425 screws were placed, 45 in open cases and 21 minimally invasive. The mean surgery time was 243.11 ± 111.42 minutes and mean robotic time was 31.74 ± 12.72 minutes. Mean time per screw for fluoroscopy-assisted robotic screws was 08.27 ± 06.54 minutes and for navigated robotic screws was 4.59 ± 1.80 minutes, the difference which was statistically significant (p < 0.05). 417 screws were clinically acceptable (GRS A, B and C). A total of 8 screws (2.1%) were GRS D and E screws, from this number two screws were removed. For 2 screws, robot was abandoned and iCT-based navigation was used. All revised screws were GRS A screws. A total of two screws experienced loosening during follow up, which prompted revision and extension of the spinal construct. Complications included wound healing deficits, cerebrospinal fluid fistula and postoperative bleeding. Conclusion: Brainlab’s Cirq® Robotic Alignment module feature enables safe and accurate placement of pedicle screws in thoracolumbar spine with low rate of screw misplacement.
1730
RF149: Outcomes of robotic revision spine surgery in failed back syndromes
Akshya Raj 1 , Harith Reddy 1 , Vignesh Badikillaya 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Apollo Hospital, Chenai, India
Introduction: Contemporary literature shows that robotic guided pedicle screw placement is highly accurate. This makes it effective in revision spine surgeries, where screw trajectories have to redrilled and anatomical landmarks are lost due to fusion mass from previous operations. However, current literature is sparse as regards the clinical outcomes of such revision surgeries performed with robotic guided instrumentation. Hence it is as yet unestablished as to whether robotic revisions translate to improvement in clinical outcome. Material and Methods: Objective:To study the patient reported outcomes of robotic assisted revision for failed back surgeries. Methods: Patients diagnosed with failed back surgery, who underwent revision surgery with robotic assisted instrumentation in the authors’ institute were prospectively assessed clinically and radiologically. Complications during surgery and in postop period were noted. They were followed up at 3 months, 6 months and 1 year post revision surgery. Radiological outcomes were assessed by means of standard radiographs. Patient reported outcome measures (PROMs) utilized were VAS scores for grading leg and back pain, the MODI (modified Owestry Disability Index) scores and the Short Form (SF-36) Physical Component Summary. Results: A total of 18 patients with failed back surgery, who underwent robotic assisted revision surgery, at our institute from 2022-2023 were included in the current study. A total of 102 pedicle screws were robotically placed. Mean follow-up was 15+2 months. Length of hospital stay was 2.5 ± 1.2 days and operating time was 120.55 ± 30.5 minutes. No case had inadvertent durotomy. No patient required a screw revision postoperatively. There were no cases of surgical site infection. The VAS score for back pain improved significantly from 67 ± 15.6 preoperatively to 21.6 ± 15.4 at the final follow-up, as did the VAS score for leg pain (from 70.6 ± 20.2 to 10.4 ± 5.5) and MODI (from 45.8 ± 15.2 to 15.3 ± 5.6; all p < 0.001). There was improvement in SF-36 PCS at final follow-up (20 vs 45, p < 0.001). In 4 patients, there was neurological recovery postoperatively, following removal and robotic revision of malpositioned screws causing impingement of nerve roots with neurological deficits. Conclusion: Robotic revision surgery leads to significant improvement in PROMs in treating failed back surgery. In revision spine surgery with previously traversed paths, with screw malpositioning, robotic revision surgery is not only highly safe and effective in correcting the screw trajectory, producing good radiological outcomes, but also translates to significantly improved patient reported outcomes.
770
RF150: Initial experience and learning curve during the first 150 cases in robotic spine instrumentation
Pablo de la Fuente 1 , Pablo Clavel 1 , Maria Dolores Varela 1
1 Neurosurgery, Clavel, Barcelona, Spain
Introduction: To report the initial experience of a high-volume spine surgery centre during its learning curve in robotic spinal surgery, exposing the difficulties encountered and the changes introduced to reduce clinical complications. Material and Methods: Retrospectively, the first 150 patients in whom a posterior robotic instrumentation was performed were collected. Type of surgery performed, materials used, robot usage time, set up and registration drawbacks, and revision rate were all collected. Results: Patients were divided in 3 groups as experience evolved and part of the data specifically concerning the precision and revision rate is as follows:
First 50 cases:
11 cases (22%) were aborted.:
9 cases there were registration or merge problems.
2 cases were aborted for other reasons.
In 6 cases (15%) incorrect placement of the instrumentation was recorded.
In four patients screws were intraoperatively repositioned,
In one patient was not modified and another patient required a revision surgery.
The most frequent surgery was 1-level TLIF.
Cases 50 to 100:
7 cases (14%) were aborted due to registration issues.
In 11 of 43 patients (25%), intraoperative correction of screw placement was recorded.
In 6 of the cases trajectories executed with navigation seemed outside the pedicle and screw placement was performed in another fashion.
In 5 of the cases, a malposition was identified with intraoperative x-ray and screws were repositioned intraoperatively
None of the 43 patients underwent a revision surgery in relation to the malposition.
In this second set of patients, the medial cortical trajectory (MidLIF) was incorporated to better deal with skin disturbing the screw trajectory and placement.
Cases 100 to 150:
3 cases (6%) were cancelled due to registration issues.
In 3 of 43 patients (6.9%) minor issues were recorded during screw placement. This corresponds to 5 screws out of 213 placed (2%). They were all repositioned intraoperatively.
Only one patient underwent a revision surgery.
The most frequent surgery in this group was a combined ALIF with posterior robot guided screw placement.
Conclusion: Registration related issues progressively decreased as experience increased.The abandonment rate decreased from an initial 22% to 6%. It was possible to identify potential erroneous trajectories thanks to navigation. The MLIF trajectory was introduced. Only two revision surgeries (1.3%) were performed due to screw placement.
2421
RF151: Radiation-free assessment of the 3D morphology of the adolescent scoliotic spine: a feasibility study in synthetic CT
Lorenzo Costa 1 , Tijl van der Velden 1 , Tom Schlosser 1 , René Castelein 1 , Peter Seevinck 1
1 Orthopedics, UMCU, Utrecht, The Netherlands
Introduction: A variety of imaging techniques are used in the diagnosis and management of adolescent idiopathic scoliosis (AIS). X-rays provide 2D images with low ionising radiation (IR), while CT scans, often used for navigation for complex cases, provide 3D information but with higher radiation doses. Innovative echography such as Scolioscan detects 3D deformities without IR, but has limitations. None of these methods can visualize intervertebral discs (IVDs), which are critical in the development of AIS. Recently, synthetic CTs (sCTs) from MRI images show promise for visualizing osseous spinal structures in adults, but their efficacy in adolescent and curved spines remains unclear. This study investigates the feasibility of sCTs in visualizing scoliotic spines in adolescents. Methods: The study included 10 MRI scans of adolescent female patients, with a mean age of 14 years (13-15 years). These patients presented with significant thoracic or thoracolumbar curves, characterized by a Cobb angle exceeding 40° on standing radiographs, as determined by the Cobb method. As part of the MRI examination, a 4-minute 3D spoiled gradient echo sequence was incorporated and subsequently processed into a sCT (BoneMRI V1.7, MRIguidance BV, Utrecht, NL). The focus during the MRI examination was directed towards the scoliotic region of the spine. Analysis of Cobb angle, thoracic kyphosis (TK), axial rotation, anterior-posterior ratio (A-P%), and left-right ratio (L-R%) was conducted using ScoliosisAnalysis 7.2 from UMCU, Utrecht, NL. For axial rotation, the vertebrae involved in the spinal deformity and the first distal neutrally rotated vertebra were analyzed. Axial rotation per endplate was defined as the angle between each vertebral endplate's antero-posterior (AP) axis and the AP axis of the first distal neutrally rotated vertebra. For A-P% and L-R%, the most anterior, posterior, left, and right points of each endplate of each vertebra involved in the deformity were identified and thus analyzed. Results and Discussion: The sCTs provided high resolution 3D CT-like images clearly visualizing the entire spine, effectively highlighting each vertebra and intervertebral joints. While the overall image quality provided high precision for measurement identification, minor artifacts were observed within the intervertebral discs (IVD) and in proximity to the respiratory tract, which did not impact the analysis of the images. The obtained results showed a remarkable alignment with existing literature. Notably, the findings demonstrated a substantial reduction in Cobb angle (from 51° to 40°) and TK magnitude (from 28° to 21°) in the supine position as compared to the standing X-ray (in line with Brink et a. 2017). At the apex, vertebral rotation measured 16° ± 5.2°, and 10° ± 3.3° at the overall curve. In the A-P%, the analysis showed a relevant anterior lengthening, mainly prominent within the IVDs (13.5% ± 7.2%). These findings align well with current literature, both in terms of the observed trends and the magnitude of the detected changes (in line with Brink et a. 2017). Conclusion: This study demonstrates that sCT provides realistic CT-like images derived from MRI which can be used for the quantification of 3D deformity of the scoliotic spine in AIS patients, without the need for ionizing radiation.
2264
RF152: The use of artificial neural networks in idiopathic scoliosis screening - Pilot study
Anna Danielewicz 1 , Michał Latalski 1 , Marek Kamiński 2 , Róża Czabak-Garbacz 3 , Marek Fatyga 4
1 Childrens' Orthopedic Department, Medical University in Lublin, Lublin, Poland
2 Computer Science, Lublin University of Technology, Lublin, Poland
3 Lipinski University in Kielce, Kielce, Poland
4 Childrens' Orthopeadic Department, Childrens' University Hospital in Lublin, Lublin, Poland
Aim of the Study: The aim of the study was to find an algorithm allowing early detection of scoliosis based on optical data obtained using the Kinect II device. Introduction: Scoliosis is defined as a curvature in the frontal plane exceeding 10° according to Cobb measurment. The growing number of children and adolescents with spinal deformities necessitates the introduction of an effective and non-invasive screening method in order to detect the defect early and start treatment in its initial phase. Material and Method: The described method for detecting spinal scoliosis is based on the analysis of a heat map generated by the Kinect depth sensor (Microsoft). From a distance of 70 cm, the device is able to cover the back with a grid of points 2 mm apart. A single frame is represented by a grid of 512 by 424 points. Frame points converted to heatmap. The image of the patient's back was then divided into 15 equal rectangles. Our areas of interest included the entire spine from the cervical spine to the border of the lumbar spine and sacrum. For this purpose, 70 children (mean age 13,5 yo) were examined at the Orthopedic Clinic, in whom radiological images of the spine were taken and their bodies were scanned using a Kinect device. Two independent orthopedists measured the angular values of curvatures and divided the patients into two groups: healthy (Cobb angle 0-10°) and patients with scoliosis (Cobb angle over 10°). The obtained data were divided into two groups - the first one (n = 34; 23F:11M) was used to train the neural network, and the next one (n = 36; 31F:6M) - to verify it. Results: The network training error was 8.2%. 89% of patients (n = 32) from the test group were correctly identified, three had a false positive result and one had a false negative result. Conclusions: The obtained results seem promising for the proposed method, which allows for quick, simple and non-invasive detection of scoliosis at an early stage of deformation and can also be used by non-medical workers in general examinations of children and adolescents. This method certainly requires further prospective studies on a larger population and with use of the new generation of device (Kinect Azure).
703
RF153: C2 anatomical pedicle screw: a novel alternative technique for C2 fixation under the concept of atlantoaxial joint distraction and fusion with intra-articular cages
Yue-Qi Du 1 , Wanru Duan 1 , Zan Chen 1
1 Department of Neurosurgery, Xuanwu Hospital, Capital Medical University, Beijing, China
Introduction: To describe a novel alternative technique for C2 fixation under the concept of atlantoaxial joint distraction and fusion with intra-articular Cages, and to report its preliminary clinical outcomes with a minimum 8-month follow-up. Material and Methods: Eighteen patients with basilar invagination and atlantoaxial dislocation underwent atlantoaxial joint distraction and fusion with intra-articular Cages. All patients had hypoplasia of the C2 isthmus prohibiting insertion of the pedicle screw. A new method, the C2 anatomical pedicle screw (C2APS) was used as an alternative. In this technique, we directly inserted screw into the C2 anatomical pedicle after facet joint distraction and Cage implementation. The trajectory mostly went through the anatomical pedicle, which completely bypasses the variated VA and eliminates the risk of VA harm. The dense anatomical pedicle could provide robust and secure screw purchase. Results: Satisfactory C2APS placement and reduction were achieved in all 18 patients. No instance of vertebral artery injury was observed. There were no cases of implant failure, and all patients demonstrated solid fusion. Conclusion: This novel technique can provide rigid fixation of the axis while eliminating VA injury. Favorable clinical outcomes with low complication rates were achieved with this technique. When placement of a C2 pedicle screw is not possible due to anatomical constraints under the concept of atlantoaxial joint distraction and fusion with intra-articular Cages, the C2APS can be considered as an efficient alternative.
81
RF154: Analysis of efficiency outpatient halo-gravity with severe scoliosis with a monitoring device
Sofía Frank 1 , Leandro Peryera 1 , Carlos Tello 1 , Eduardo Galaretto 1 , Rodrigo Remondino 1 , Mariano Noël 1 , Lucas Piantoni 1
1 Spine Disease Unit, Hospital de Pediatría Juan P. Garrahan, Ciudad Autónoma de Buenos Aires, Argentina
Introduction: Patients with severe spinal deformities represent a major clinical and surgical challenge. Halo-gravity traction (HGT) is a traditional method to correct the deformity prior to surgery. Typically, children undergoing HGT remain in the hospital until surgery. Therefore, it has been suggested to treat these children at lower level healthcare centers or even at home. The aim of this study was to assess the efficiency and the adherence to HGT with a monitoring device and a program to analyze traction results. Materials and Methods: The recording system was designed with an Arduino Nano®. The data were analyzed with the MatLab R2018a MathWorks®. The patient's weight and the weight placed on the bed and chair traction system were analyzed. Target weight was defined as 50% of the patient's body weight. The measured actual average weight was analyzed and compared to the weight placed on the system. The time with more than 80% of the weight placed was also analyzed, denominating this as the effective time of use. The percentage of the traction weight was evaluated in comparison with the weight of the patient. Individual daytime traction efficiency evaluations were then made. Results: Six patients receiving HGT were analyzed. The average evaluation time was 158 hours. The mean of effective time of use was 35.48%. The percentage of the patient weight actually loaded was 20.75%. The patient with the best result loaded 32.82% of his body weight on average. In a one-day evaluation of a patient with the best results in effective time load, it was found that the effective time of use was 30.8%, being 41.27% during the day and 7.74% at night. Conclusions: The efficiency of the use of home HTG systems could be evaluated. It was discovered that the weight carried by the patients did not achieve the desired weight in relation to their body weight. A difference in efficiency could be found during the day compared to night.
349
RF155: Awake micro-endoscopic lumbar spine decompressions and fusions performed in lateral decubitus position under regional anaesthesia in 29 patients with at-least 6 month follow-up: case series, technical note and literature review
Saurabh Kapoor 1 , Mohanjeet Juneja 2 , Sunil Gupta 2 , Shekhar Srivastav 3
1 Spine Surgery
2 Anaesthesia
3 Orthopaedic Surgery, Sant Parmanand Hospital, New Delhi, India
Introduction: Awake spine surgery under regional anesthesia has been restricted to predominantly decompressions and limited fusions owing to poor tolerance of prone positioning in surgical patients. This has made it difficult to utilize the better safety profile, early rehabilitation and other benefits of awake spine surgeries in lumbar spinal procedures. We describe a novel technique of performing single and multilevel micro-endoscopic decompressions and interbody fusions in lateral decubitus position in an awake patient. Material and Methods: The records 29 patients who underwent awake micro-endoscopic spinal procedures in lateral decubitus position performed by a single surgeon, from August 2021 to February 2023 were retrospectively reviewed. All included patients were followed up for at least 6 months. Results: 4 unilateral discectomies, 3 lateral recess and over the top decompressions, 4 postero-lateral fusions (one multilevel) and 17 trans-foraminal interbody fusions (2 multilevel) were performed using micro-endoscopic approach in lateral decubitus position in awake patients. American society of anesthesiologists (ASA) grade was 1 in 14 patients, 2 in 9 patients, 3 in 5 patients and 4 in1 patient. Average age of patients was 49 years (range - 18 to 75). Average duration of surgery was 122 minutes (range- 55 to 175 minutes) and average blood loss was 73 ml (range- 30 to 150 ml). Except for 1 patient with ASA grade 4 who required precautionary cardiac critical care stay, none of the patients needed critical care. 2 patients (7%) had intra-operative dural tears which were managed with fat graft patch and gradual mobilization. Early (< 4 weeks) complications included one case of wound dehiscence, one posterior cage migration and one cage subsidence (8%), all managed conservatively. One patient (3%) suffered right S1 screw pullout after 3 months which required re-operation. All patients except for those with dural tears were mobilized 12 hours after surgery and discharged after an average of 2 days (range - 1 to 4) of in-hospital stay. Average follow-up was 17 months (range- 6 to 24 months). The pre-operative visual analog scale (VAS) for leg pain and modified Oswestry disability index score improved from 8.7 and 78% to 2.3 and 16%, respectively, after 6 months of follow-up. 2 known cardiac patients died of cardiac arrest in the follow-up period 3 months and 18 months post-surgery. Conclusion: Awake spine surgery in lateral decubitus position using micro-endoscopic equipment is a novel technique which can be used to perform diverse and longer lumbar spinal procedures effectively. Acquaintance of spine surgeon to micro-endoscopic procedures in prone position is a must before attempting it in lateral decubitus position.
1775
RF156: Outcome of expansion duraplasty in transverse myelitis
Muhammad Jawad Saleem 1
1 Orthopedic Spine Surgery, Orthopedic Spine Institute, Lahore, Pakistan
Introduction: Transverse Myelitis is currently treated by neurologist with medication and plasmapheresis with some success. For patients in whom the medical treatment is unsuccessful, no treatment option is available. We performed expansion duraplasty in this subset of patients. Material and Methods: A pilot study was carried out after IRB approval on compassionate grounds. 15 patients (12 male, 3 females) with mean age 34 years (26-42 years) underwent expansion duraplasty at the effected spinal cord levels. We are presenting 6 months data on this subset of patients. Outcome was determined in improvement in neurological status, sphincter control and dysesthatic pain control. Results: Pre-operatively 11 patients had grade 1 motor power in both lower extremities, 4 patients had grade 2 motor power in both lower extremities. Post-operatively no patient had worsening in pre-operative neurological status. 11 patients showed improvement in neurological function (Motor Power 4+/5) with return of sphincter control. 4 Patients showed no improvement in neurological function at 6 months follow up. The only statistically significant difference between 2 groups was the time interval between the onset of symptoms and surgical intervention, with shorter time interval showing better outcomes. Conclusion: Expansion duraplasty shows promising results in our pilot study in patients with transverse myelitis who had unsuccessful medical management. A larger study and long term follow up is required to establish efficacy of this treatment modality.
576
RF157: A deep learning approach for spine cervical injury severity determination through axial and sagittal magnetic resonance imaging segmentation and classification
I Gusti Lanang Ngurah Agung Artha Wiguna 1 , Maria Florencia Deslivia 1 , Ivan Alexander Liando 1 , Hendra Aryudi Hamzah 1 , Kevin Kusuman 1 , Dominicus Dimitri 1 , Maria Anastasia 1 , I Ketut Suyasa 1 , Yosi Kristian 2 , Rudi Limantara 2 , David Cahyado 2
1 Orthopaedic Surgery, Udayana University, Prof I G N G Ngoerah Hospital, Denpasar, Bali, Indonesia
2 Institut Sains dan Teknologi Terpadu Surabaya, Surabaya, Indonesia
Introduction: Spinal cord injuries (SCI) require extensive efforts to predict the outcome of patients. While the ASIA Impairment Scale is the gold standard to assess patients with SCI, it has some limitations due to the subjectivity and impracticality in certain cases. Recent advances in machine learning (ML) and image recognition have prompted research into using these tools to predict outcomes. The aim of this cross-sectional database study is to present a comprehensive analysis that uses deep learning techniques to identify, evaluate, and predict cervical spine injuries from MRI scans. Material and Methods: Patients admitted with traumatic and nontraumatic cervical SCI from 2019 to 2022 were included in our study. MRI images were labelled by four senior resident physicians. We trained a deep convolutional neural network using axial and sagittal cervical MRI images from our dataset and assessed model performance. Results: In the axial spinal cord segmentation, we achieved a dice score of 0.94 for and IoU score of 0.89. In the sagittal spinal cord segmentation, we obtained a dice scores up to 0.9201 and IoU scores up to 0.8541. The model for axial image score classification gave a satisfactory result with an f1 score of 0.72 and AUC of 0.79. Conclusion: Deep learning has been used in automated diagnostic tools, showing promise for significant future advancement. Our models were effectively able to identify cervical spinal cord injury on T2-weighted MR images with satisfactory performance. Further research is necessary to create an even more advanced model for predicting patient outcomes in spinal cord injury cases.
2113
RF158: Establishment and clinical evaluation of a deep learning approach for automated estimation of 3D vertebral orientation in dual fluoroscopic images of the lumbar spine
Nanfang Xu 1 , Shanshan Liu 1 , Yuepeng Chen 2 , Kailai Zhang 3 , Chenyi Guo 4 , Cheng Zhang 1 , Fei Xu 1 , Wanyi Fu 4 , Xiangling Fu 2 , Ji Wu 4 , Weishi Li 1
1 Department of Orthopaedics, Peking University Third Hospital, Beijing, China
2 School of Computer Science, Beijing University of Posts and Telecommunications, Beijing, China
3 Department of Networks, China Mobile Communications Group Co., Ltd., Beijing, China
4 Department of Electronic Engineering, Tsinghua University, Beijing, China
Introduction: Lumbar degenerative disc diseases constitute a major contributor to lower back pain. In pursuit of an enhanced understanding of lumbar degenerative pathology and development of more effective treatment modalities, the application of precise measurement techniques for lumbar segment kinematics is imperative. This study aims to pioneer a novel automated lumbar spine orientation estimation method using deep learning techniques, facilitate the automatic 2D-3D pre-registration of the lumbar spine during physiological movements, in order to enhance the efficiency of image registration and the accuracy of spinal segment kinematic measurements. Material and Methods: A total of 12 asymptomatic volunteers were enrolled and captured in two oblique views with seven different postures. Images were used for deep learning model development training and evaluation. The model was composed of segmentation module using Mask R-CNN and estimation module using ResNet50 architecture with Squeeze-and-Excitation module. Cosine value of the angle between the prediction vector and the vector of ground truth was used to quantify the model performance. Data from another 2 prospective recruited asymptomatic volunteers were used to compare time cost between model-assisted registration and totally manual registration without model. Results: The cosine values of vector deviation angles at three axes in cartesian coordinate system were 0.9647 ± 0.0069, 0.9823 ± 0.0059, 0.9532 ± 0.0060, respectively. The value of angular deviation of between intermediate vector obtained by utilizing the three direction vectors and ground truth was 11.0434 ± 1.1053. Time consumption for model-assisted registration was 3.47 ± 0.90 minutes while manual registration without model cost 8.10 ± 1.60 minutes, which showed the significant difference between two methods (p < 0.001). Conclusion: The automatic estimation method enabling 2D-3D automatic pre-registration of the lumbar spine under distinct functional postures, reduces the time required for image registration and enhances the efficiency of clinical research pertaining to kinematic measurements, ultimately contributes to the advancement of clinical practice.
1631
RF159: Optimizing neurosurgery operative note-writing using Artificial Intelligence
Abdullah Ali 1 , Rohit Prem Kumar 1 , Raj Lavadi 1 , Andrew Legarreta 1 , Joseph Hudson 1 , Manan Shah 1 , David Paul 1 , James Mooney 2 , Nicholas Dietz 3 , Hanish Polavarapu 4 , Michael Cloney 1 , Daryl Fields 1 , Kojo Hamilton 1,5 , Nitin Agarwal 1,5
1 Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, USA
2 Neurosurgery, The University of Alabama at Birmingham, Birmingham, USA
3 Neurosurgery, University of Louisville, Louisville, USA
4 Neurosurgery, SUNY Upstate Medical University, Syracuse, USA
5 Neurological Surgery, University of Pittsburgh School of Medicine, Pittsburgh, USA
Introduction: Accurate and complete surgical operative notes play an important role in medical documentation and postoperative patient care; they are necessary for audits and medico-legal reasons in the case of disputes. Any shortcoming in operative note-writing has the potential to compromise patient care. Large language models (LLMs) such as OpenAI’s ChatGPT can write operative notes efficiently and accurately, potentially allowing surgeons to optimize their responsibilities. This study endeavors to explore how artificial intelligence can help improve operative note-writing in the field of neurosurgery. Material and Methods: Eighteen operative notes, written by two attending surgeons, were used for the study. These notes were anonymized of patient-centric and surgeon-centric information. Data from these notes were extracted, such as perioperative details, diagnosis, and demographics. ChatGPT 4.0 was trained to use the template of each surgeon’s operative note (surgeon note) to create its version of the operative note (AI note) when prompted with a sample surgical vignette. Seventy-two surveys accompanying a surgeon or AI note were distributed among three fellowship-trained surgeons. The criteria evaluated included accuracy, content, and organization on a five-point Likert scale. Two participants independently evaluated each note. The readability of each note was assessed based on the Flesch-Kincaid Grade Level (FKGL). Results: All surveys were completed. The mean AI note accuracy (3.81) was significantly different from the mean surgeon note accuracy (4.51, p < 0.01). The mean AI note content (2.92) was significantly different from the mean surgeon note content (4.37, p < 0.01). The mean AI note organization (4.06) was not significantly different from the mean surgeon note organization (4.06, p = 0.99). The mean AI note FKGL (13.59) was significantly different from the mean surgeon note FKGL (11.75, p < 0.01). Conclusion: Given the significantly poorer ratings of the AI notes than the surgeon notes, AI may not optimize the workflow for time-restricted trainees and attending neurosurgeons at its current capacity.
1309
RF160: The modulable Halo-Brace: the present of Halo-Vest
Timothée de Saint-Denis 1 , David Karoubi 2 , Elie Saghbiny 1 , Mathilde Gaume 1 , Laura Marie-Hardy 1 , Raphael Vialle 1
1 Pediatric Orthopaedics, University Institute for Spine Surgery, Sorbonne University, Paris, France
2 EOS, Paris, France
Introduction: Cranio-cervical spine deformities are challenging situations that need a multidisciplinary management. Halo gravity traction is widely used to reduce deformity and prepare correction-fusion surgery. Halo-Vest or halo-cast are used to immobilize during and after surgery of craniovertebral junction and neck spine surgery or trauma. Halo-Ilizarov distraction cast has been used for ambulatory correction in the past and other devices such as Lerman Halo have proposed improvement for non-invasive strategy. We intend to develop an adaptable orthosis that can be used all along the patient journey. Materials and Methods: The Modulable Halo Brace is a bivalve thoraco-lumbar orthosis that can be converted either in an adjustable halo-vest or in a Milwaukee brace (TLSO). After a laser skin scanning a polyurethane 3D shape of the chest is modeled before bivalve brace is applied. Chin and occipital holders in thermoformed propylene also are adjustable in height. Cranial Halo is connected to the brace through four aluminum profiles, with perforated extremities to adjust height. Cranial extremities are directly screwed in the perforated halo, lower extremities are screwed in the pre-drilled thickness of the brace. Results: 20 Modulable Halo Braces have been made for a total of 18 patients. All patients have been braced for a minimum duration of 3 months. Mean age at treatment was 103.8 months (min 21; max 176; med 109.5). 5/20 braces have been used exclusively as TLSO. 15/20 braces have been used both as TLSO and Halo-vest. Mean duration of Halo-vest immobilization was 29.2 days (min 2; max 124; med 16). 7/15 halo-vest have been used perioperatively for spine fusion. Two adverse events were encountered: one head pin mobilization directly related to the halo brace treatment ending at day-33 progressive step reduction of cervical deformity and one pin penetrating craniocerebral injury following an unofficial highspeed wheelchair race accident. No neurological impairment, no intra-operative complications encountered. Conclusion: This historical device optimized with modern materials and processes offers safety for intra-operative management of complex cranio-cervical deformities without worsening significantly the ergonomy of the surgical field thanks to the low-profile conception. Constraints applied on cranial bone by halo pins may be reduced thanks to aluminum profile elasticity and may decrease bone resorption around the pins. Small weight device and versatility between traction, halo-vest and TLSO can be helpful for pediatric patients with complex diseases who need constant rehabilitation care.
2218
RF161: Midterm result of a novel un-instrumented suspension bridge cervical laminoplasty for compressive cervical myelopathy
Charanjit Singh Dhillon 1 , Mukhesh Thangavel 1
1 Spine Surgery, MIOT International, Chennai, India
Introduction: This is a retrospective study to evaluate the mid-term outcomes of a novel self-developed technique of performing un-instrumented open-door suspension bridge laminoplasty (ODCL) in compressive cervical myelopathy. Materials and Methods: Retrospective data were collected from 109 patients who underwent un-instrumented ODCL for compressive cervical myelopathy at a single institution from January 2010 to May 2019. The preoperative and postoperative Modified Japanese Orthopaedic Association score (mJOA) and Nurick grading were documented. Cervical lordotic angle (C2–C7) and range of motion (ROM) were obtained from the preoperative and postoperative radiographs. Results: The average age was 57.2 ± 7.8 years. The average time of presentation was 5.6 ± 3 months. In this study, majority had segmental OPLL; remaining were continuous & mixed OPLL and multiple-level spondylotic myelopathy. C3-C6 was the most commonly operated level (50.43%). The mean operating time was 115 ± 31 min with a mean blood loss of 152.7 ± 75 ml. There was a significant improvement in the mJOA scores (8.8 ± 1.1–14.4 ± 1.0, p < 0.0001) and Nurick grading (4.2 ± 0.8–1.8 ± 0.5, p < 0.0001) at 36-month follow-up. Preoperative C2-C7 angle had an average decrease of 4.60 at 36-month follow-up (22.4 ± 7.3–17.8 ± 8.6, p < 0.0001). There was a mean reduction of 5.70 ± 3.78° noted in the C2-C7 ROM between the preoperative and final follow-up. Conclusion: The suspension bridge technique for un-instrumented ODCL represents a cost-effective and readily replicable alternative to traditional instrumented laminoplasty, offering comparable mid-term results.
2149
RF162: Novel technique of PA limited laminectomy for Cervical-spine to prevent C5 nerve root palsy in the post-operative period who underwent cervical laminectomy for cervical myelopathy due to multi-level compression
Prasanna Gunasena 1 , Anil Weerasinghe 1 , Eranga Ganewatte 2 , Anupa Walgamage 1
1 Neurosurgery
2 Radiology, Lanka Hospital, Colombo, Sri Lanka
Summary: This retrospective study analyzed C5 Nerve root function 3 months after doing modified limited posterior cervical decompression and lateral mass fusion to treat multilevel cervical cord compression with moderate to severe myelopathy. The results were compared with a similar number of patients who underwent standard cervical laminectomy and lateral mass fusion for the same indication. Primary Objective: C5 nerve root failure following posterior cervical decompression is a challenging problem. The incidence of C5 palsy associated with deferent technique of posterior decompression vary from 4% to 12% [1,2]. C5 nerve root traction following decompression is the Probable mechanism. Many etiological factors identified but no successful preventive measure has been described in literature [1,2,3]. C5 root failure is diagnosed when patients show a deterioration in muscle power of the deltoid or biceps brachi by at least one grade in the manual muscle test without aggravation of lower extremity function [2,3,4]. Deferent techniques of posterior decompression have been attempted with no major success. With attention to the probable cause of root failure which is traction to the C5 roots [1], we modified our laminectomy technique. Instead of removing the whole lamina from one lateral mass to the opposite lateral mass we removed only 70% of lamina leaving 15% ridge of lamina on either side attached to the lateral mass. Rest of the surgery was performed in the standard manner. All patients had per-operative neuro monitoring and posterior cervical fusion with lateral mass screws. Per-operative monitoring revealed no abnormality in EMGs. Standard post-operative care was given and all patients were reviewed after 3 months. 3.1% of 96 patients who underwent standard laminectomy and lateral mass fusion had C5 root failure, whereas 23 patients who had modified PA laminectomy had no root failure. It is too early to compare the functional outcome in both groups. However, a satisfactory decompression has been confirmed by MRI of the cervical spine which was reported by an independent board-certified specialist radiologist. Conclusion: PA cervical limited laminectomy is a satisfactory alternate surgical technique to prevent C5 root failure when performing cervical decompression for multilevel posterior cord compression with moderate to severe myelopathy.
References
1. Epstein NE, Hollingsworth R. C5 Nerve root palsies following cervical spine surgery: surgical Neurology Int 2015; v. 6 (Supplement 4).
2. Pan F-M, Wang S-J, Ma B, Wu D-S. C5 nerve root palsy after posterior cervical spine surgry, Journal of Orthopaedic Surgery 2017.
3. Katsumi K, Yamazaki A, Watanabe K, et al. Analysis of C5 palsy after cervical open-door laminoplasty: relationship between C5 palsy and foraminal stenosis. 2013
4. Minoda Y, Nakamura H, Konishi S, et al. Palsy of the C5 nerve root after midsagittal-splitting laminoplasty of the cervical spine. Spine (Phila Pa 1976) 2003.
FRP10: Cervical Arthroplasty & Deformity
1637
RF163: Risk factors for delayed discharge after ambulatory cervical spine surgery
Austin Kaidi 1 , Tejas Subramanian 1 , Pratyush Shahi 1 , Gregory Kazarian 1 , Kasra Araghi 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Tomoyuki Asada 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Avani Vaishnav 1,2 , Sheeraz Qureshi 1,3 , Sravisht Iyer 1,3
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, Boston, USA
3 Weill Cornell Medical College, New York, USA
Introduction: Ambulatory cervical spine surgery is growing in popularity worldwide. As surgeons begin to shift practices to the ambulatory setting, it is critical to understand factors that can prognosticate a successful outcome. In this study we aimed to identify risk factors for delayed discharge after ambulatory cervical spine surgery. We hypothesized that patients undergoing multilevel surgery and those with worse pre-operative patient reported outcome measures (PROMs) would be more likely to have a delayed discharge. Material and Methods: This was a retrospective review of a prospectively collected cohort. Patients were included if they were scheduled for ambulatory cervical spine fusion or cervical disc replacement (CDR). Patient information including age, American Society of Anesthesiologist (ASA) class, and pre-operative PROMs were recorded. Surgical factors including surgical start time, surgical approach, operation, and vertebral levels were also collected. Patients were stratified into two cohorts: those discharged on post-operative day 0 and those with a delayed discharge (defined as > 24 hours inpatient). Multivariable logistic regression was performed to determine risk factors for delayed discharge. p-values < 0.05 were considered significant. Results: 424 patients were included in our cohort. 214 (50.5%) underwent cervical fusion and 210 (49.5%) underwent CDR. 278 (65.6%) underwent single level surgery, 135 (31.2%) underwent 2 level surgery, and 11 (2.5%) underwent 3+ level surgery. Among the 424 patients, 54 (12.7%) required delayed discharge. The mean post-operative length of stay for these patients was 62.6 hours. The only factors associated with delayed discharge were increased age and increased neck-disability index (NDI). Age > 65 was associated with 3.27 times increased odds of delayed discharge (p = 0.01; 95%CI:1.32-6.13). Higher pre-operative NDI was protective with 0.32 times decreased odds of delayed discharge (p < 0.01, 95%CI:0.12-0.87). All other factors were not significant. Conclusion: When indicated appropriately, cervical spine surgery can be successfully performed in the ambulatory setting. This held true among patients undergoing cervical fusion, CDR, and even multilevel operations. Of note, when patients did require a delayed discharge, they often required a prolonged hospitalization. In this study, age >65 was the most significant factor in delayed discharge. Contrary to our hypothesis, however, patients with worse PROMs were less likely to have a delayed discharge.
1656
RF164: Commonly used patient-reported outcomes measures (PROMS) do not adequately reflect patient-perceived changes in health status following cervical disc arthroplasty
Avani Vaishnav 1,2 , Jung Kee Mok 2 , Kasra Araghi 2 , Yeo Eun Kim 2 , Olivia Tuma 2 , Eric Kim 2 , Chad Simon 2 , Nishtha Singh 2 , Tomoyuki Asada 2 , Joshua Zhang 2 , Myles Allen 2 , Maximillian Korsun 2 , Eric Mai 2 , Cole Kwas 2 , Sravisht Iyer 2 , Sheeraz Qureshi 2
1 Boston Medical Center, Boston, USA
2 Hospital for Special Surgery, New York, USA
Introduction: In recent years there has been a growing focus on patient-reported outcome measures (PROMs) as important metrics in spine surgery. As a result, they are increasingly being utilized to assess healthcare expenditure, determine compensation and evaluate cost-effectiveness. However, there is little data on whether changes in PROMs correlate with patients’ perceptions of improvement. Thus, the purpose of this study was to assess the correlation between patient perceived changes in health and commonly utilized PROMs in patients undergoing cervical disc arthroplasty. Material and Methods: We performed a retrospective review of prospectively collected data on consecutive patients who underwent cervical disc arthroplasty at s single academic institution between May 2017 and February 2023. PROMs including Neck Disability Index (NDI), Numeric Rating Scale (NRS) for Neck pain and Arm pain, Short-Form 12 (SF-12) and PROMIS Physical Function were prospectively completed by patients pre-operatively and at 6 weeks, 12 weeks, 6 months and 1 year after surgery. In addition, at each post-operative visit patients completed a ‘Global Rating Change’ question, which assessed how the patient’s spine condition compared to before surgery and to their previous visit. This was assessed using a 5-item Likert Scale (Much better, slightly better, about the same, slightly worse, much worse). Spearman correlation coefficient (Rho) was used to assess the correlation between change in PROMs and Global Rating Change. Results: 109 patients with a mean age of 43 years, mean BMI of 27 and comprised of 67 (61.5%) males. A majority of patients underwent single-level surgery (1-level: 61.5%; 2-level: 38.5%) and were discharged on post-operative day 1 (0 days: 30.3%, 1 day: 61.5%, 2 days 8.3%). Percentage of patients feeling ‘Much better’ compared to pre-operatively was 65% at 6 weeks, 75% at 12 weeks and 80% at 6 months and 1 year. At all time-points, less than 5% of patients reported feeling ‘slightly worse’ or ‘much worse’ compared to pre-operatively. Change in PROMs from pre-operatively demonstrated a statistically significant correlation with Global Rating Change at all time-points for NDI, NRS neck pain and PROMIS physical function, and at 3 out of the 4 timepoints for NRS arm and SF-12 physical component. However, the strength of the correlation was weak-to-moderate with Spearman’s Rho ranging from 0.311 to 0.604. Change in PROMs compared to the previous visit did not show a statistically significant correlation with Global Rating Change. Conclusion: The results of this study show that a majority of patients undergoing cervical disc arthroplasty experienced a notable improvement in the early post-operative period (6-12 weeks). Despite this early improvement, patients continue to have improvements at longer follow-up, with approximately 50% of patients reporting feeling better at 1 year compared to 6 months. In addition, commonly used PROMs demonstrated moderate-to-poor correlation with patient-perceived changes in health status from pre- to post-operatively, and showed no correlation with post-operative changes. These findings suggest that currently used PROMs may not be as sensitive at detecting these changes, or may not be adequately assessing changes in health condition that are meaningful to patients.
1101
RF165: Analysis of influence factors of anterior bone loss after cervical disc arthroplasty and its effect on postoperative outcomes
Junbo He 1 , Tingkui Wu 1 , Hao Liu 1
1 Orthopedic Surgery, West China Hospital, Sichuan University, Chengdu, China
Introduction: Cervical disc arthroplasty (CDA) has become an alternative procedure for the treatment of refractory cervical degenerative disc disease with satisfactory outcomes. However, some adverse outcomes have recently emerged, such as anterior bone loss (ABL). ABL was defined as non-progressive early peri-prosthetic vertebral bone loss commencing within 6 months after surgery. The primary aim of the present study was to explore the influence factors of ABL after CDA and effects of ABL on the clinical and radiographic outcomes. Material and Methods: One hundred and fifty-five patients who underwent single-level Prestige-LP CDA between January 2008 and December 2017 were enrolled in the study. The Japanese Orthopaedic Association (JOA) score, Neck Disability Index (NDI), and the visual analogue scale (VAS) score were used for clinical outcomes evaluation. Radiographic parameters including cervical lordosis, C2-7 range of motion (ROM), disc angle, segmental ROM, and the lengths of the upper and lower endplates were assessed on the X-ray films. Device-related complications, including ABL, subsidence, radiographic adjacent segment pathology, and heterotopic ossification, were recorded. Univariate analysis and logistic regression analysis was used to screen the influence factors. Patients were grouped according to whether ABL occurred after operation, and the differences in clinical and imaging evaluation parameters were compared. Results: There were 94 cases (60.6%) in the ABL group and 61 cases (39.4%) in the non-ABL group. Multivariate analysis showed that the age and BMI were influence factors for ABL after CDA (p < 0.05). The JOA score, NDI, and VAS score significantly improved in both groups at 3 months after operation (p < 0.05), and the scores were further improved at last follow-up (p < 0.05). There was no significant difference in JOA score, NDI, and VAS score between the two groups before and after operation (p > 0.05). The preoperative cervical lordosis was significantly smaller in the ABL group than in the non-ABL group (t = -2.402, p = 0.018). At last follow-up, the segmental ROM was significantly greater in the ABL group than in the non-ABL group (p < 0.05), and the lengths of the upper and lower endplates were less in the ABL group than in the non-ABL group (p < 0.05). Heterotopic ossification occurred in 67 cases (43.2%), including 32 cases in the ABL group and 35 cases in the non-ABL group; the difference between the two groups was significant (χ2 = 8.208, p = 0.004). High-grade heterotopic ossification was detected in 26 cases (13 cases in the ABL group and 13 cases in the non-ABL group). Twenty-nine cases (18.7%) had radiographic adjacent segment pathology, including 15 cases in the ABL group and 14 cases in non-ABL group; the difference between the two groups was not significant (χ2 = 1.190, p = 0.276). Conclusion: The incidence of ABL after CDA was relatively high, which mainly occurred within 3 months after operation, and no longer progressing with stable radiographic features after the first 12 months. Age and BMI were independent influence factors for ABL. ABL does not affect the clinical outcomes but may preserve more ROM of prostheses.
57
RF166: Th antero-posterior positioning of visco-elastic cervical disc prosthesis does not alter the outcomes
Marc-Antoine Rousseau, Lorenzo Serfaty, Mohamed Zoghlami, Haroun Bouhali, Bilal El Hachache, Zied Chenguel, Baptiste Boukebous
Introduction: Second-generation visco-elastic disc prostheses are of most interest today for cervical reconstruction after discectomy. The biomechanical concept of one-piece implants combines intervertebral cohesion, elastic return, full-6 degrees of freedom, and free center of rotation. While first generation articulated disc prostheses had an ideal positioning schematically as posterior as possible because of their geometrically determined center of rotation, the dogma may change for visco-elastic implants, whose center of rotation is free. Since the center of rotation in visco-elastic cervical disc prostheses is free, our hypothesis was to check if the antero-posterior positioning of the implants may influence the clinical outcomes at follow-up. Material and Methods: Data have been compiled from 30 consecutive patients with single-level cervical total disc replacement of second generation (i.e. viscoelastic implant). There were 16 women and 14 men, aged 28 to 73 years-old. The average follow-up was 25.9 months (15 to 38). The population was retrospectively divided in two groups : the most anterior placement / the most posterior placement depending on the relative position of the middle of the prosthesis to the middle of the inferior endplate on the lateral radiograph. Recorded outcomes were clinical and radiological: Neck Disability Index (NDI), visual analog scale for neck and radicular pain (VASn and VASr), flexion-extension range of motion (ROM) and McAfee’s classification for heterotopic ossifications (HO).All outcomes at last follow-up (LFU) were correlated to the groups. Results: The average NDI was 63.3% preop, dropping to 25.3% at LFU. The average VASn and VASr were 8.6 and 7.3 preop, dropping to 3.2 and 2.5 at LFU. At LFU, the average flexion / extension ROM was 14°. The relative position of the prosthesis to the endplate was in mean 44%. Using a 50% cut-off (middle of the endplate) the two groups were 15/15. No significant difference in any outcome between the anterior group (n = 15) and the posterior group (n = 15). Conclusion: The antero-posterior positioning of viscoelastic dis arthroplasty do not significantly influence the clinical or radiological outcomes at follow up. The comparison of the clinical and radiological outcomes regarding the antero-posterior positioning of a visco-elastic cervical disc prosthesis in a series of 30 consecutive patients suggests this generation of implants tolerate greater variability in its technique of implantation.
751
RF167: Correlation between intervertebral disc degeneration degree and heterotopic ossification after artificial cervical disc replacement
Yin Zhao 1 , Xiongsheng Chen 1
1 Spine Center, Department of Orthopedics, Shanghai Changzheng Hospital, Naval Medical University, Shanghai, China
Introduction: There were kinds of factors influencing the incidence of heterotopic ossification (HO) after artificial cervical disc replacement (ACDR), while not including reports about the effects of intervertebral disc degeneration on the occurrence of HO. In view of this, the current research retrospectively analyzed the data of 120 patients having accepted ACDR, to investigate the correlation between the degeneration degree of cervical intervertebral disc and the HO after ACDR. Material and Methods: From January 2009 to June 2016, 120 patients who had undergone ACDR were included into this study. There were 87 males and 33 females with an average age of 43.83 ± 8.76 years old (range, 27-67 years old). There were 100 patients who had undergone single level implant, and 20 patients double level implant. Cervical spine flexion-extension X-rays were taken to assess the range of motion (ROM) of the surgical level. HO situation was evaluated by McAfee classification through cervical lateral X-rays. Degeneration degree of patients’ cervical intervertebral discs were evaluated by Pfirrmann grading standards with the preoperative cervical magnetic resonance imagings (MRIs). The occurrence and McAfee classification of HO in the replacement segment at the last follow-up were concerned. According to whether HO occurred, the patients were divided into HO group and non-HO group. ROM and preoperative Pfirrmann score were compared between the two groups of patients. Results: All 120 patients were followed up. The average follow-up time was 52.29 months (13 to 102 months). The VAS score, JOA score, and NDI index all improved at the last follow-up. At the last follow-up, a total of 27 patients developed HO, and the incidence of HO was 22.5%. ROM of the HO group (7.40 ± 1.75)° was significantly lower than that of the non-HO group (9.79 ± 1.40)°. Pfirrmann score of preoperative disc degeneration (3.31 ± 1.11) was significantly higher in HO group than which in non-HO group (2.40 ± 0.96). The correlation analysis showed that the Pfirrmann degeneration score of the preoperative replacement segment of the HO group was positively correlated with the postoperative HO McAfee classification (R = 0.765, p < 0.01), and negative correlated with ROM of the replacement segment (R = -0.866, p < 0.01). Conclusion: The occurrence of HO after ACDR was correlated with the degree of preoperative degeneration of intervertebral disc. The degree of degeneration of cervical disc in HO group was significantly higher than that of non-HO group. In the HO group, the higher the degree of Pfirrmann degeneration of the intervertebral disc preoperatively was, the higher the McAfee grade at the last follow-up was and the lower ROM of the replacement segment was.
1630
RF168: Ultrasound assessment of the anterior neck and hematoma before and after anterior cervical spine surgery
Lauren Barber 1 , Chad Simon 2 , Sumedha Singh 2 , Daniel Shinn 2 , Philip Louie 2 , Jung Kee Mok 2 , Ogonna Nwawka 2 , Theodore Miller 2 , Han Jo Kim 2 , Russel Huang 2 , Todd Albert 2 , Harvinder Sandhu 2 , Sravisht Iyer 2 , Sheeraz Qureshi 2
1 Department of Orthopaedic Surgery, Emory University
2 Hospital for Special Surgery, Atlanta, USA
Introduction: With more anterior cervical surgeries (ACS) being performed in outpatient settings, the evaluation of postoperative hematoma and soft tissue swelling are crucial. Magnetic resonance imaging is the most common imaging modality to evaluate these postoperative features but can be costly or unavailable. Ultrasonography (US) is a cheaper, mobile, and more widespread imaging modality that has shown efficacy in evaluating fluid collections and soft-tissue morphology. Our primary goal was to assess the reliability of US as a method to evaluate hematoma volume and the surrounding structures of the neck before and after anterior cervical spine surgery. Our secondary goal was to develop a range of baseline hematoma formation and soft-tissue morphologic changes following ACS. Material and Methods: This is an IRB-approved, prospective, single-center study. All patients scheduled to undergo 1-3 level anterior cervical discectomy fusion (ACDF) or cervical disc replacement (CDR) by six fellowship-trained spine surgeons with no post-operative drain placement were recruited. Preoperatively and on the morning after surgery (POD1), patients obtained a neck US and a lateral cervical radiograph. The neck US was evaluated by an orthopaedic resident and a radiology resident for the following parameters: hematoma presence and dimensions, longus colli dimensions, and visualized vertebral bodies, esophagus, and trachea. Plain radiographs were evaluated for retropharyngeal soft-tissue swelling at C2-C7. Additionally, a fellowship-trained radiology attending evaluated the postoperative neck US for presence of hematoma to serve as the ‘gold standard’. Inter-rater reliability was calculated for all measurements. Results: From 2019-2022, 45 patients were enrolled in this study. The mean age was 50.9 ± 10.9 years with 53.3% females. Nineteen patients underwent 1-level and 25 patients underwent 2-level procedures. One patient had a 2-level CDR with a single-level ACDF. Thirteen (28.9%) hematomas were observed on POD1 US; none were clinically significant. There were significant differences in the thickness of the longus colli pre- and postoperatively. Baseline dimensions of soft-tissue morphologic changes and hematoma formation following ACS were also established. The intraclass correlation coefficient (ICC) was 0.685 (good reliability) for visualization of a postoperative hematoma and 0.970 (excellent reliability) for measurement of the hematoma long axis. When the two primary evaluators were compared to an attending radiologist, the ICC reliability was 0.921 (excellent reliability) for visualization of a postoperative hematoma and 0.867 (good reliability) for measurement of the hematoma long axis. Mean measurements for the hematoma long and short axes of all three evaluators were compared and found to not be significantly different. Conclusion: After ACS without drain placement, nearly one third of patients developed a hematoma observed on US, though none developed airway compromise. Even for a non-radiologist trainee, neck ultrasound appears to be an effective method to evaluate hematoma and soft-tissue structures in the neck before and after ACS. With good to excellent inter-observer reliability, ultrasound after anterior cervical surgery may be an additional tool to allow for a quick, bedside hematoma evaluation without needing advanced imaging or radiologist interpretation.
1245
RF169: Cervical disc arthroplasty versus anterior cervical discectomy and fusion for the treatment of single-level disc degenerative disease with preoperative reversible kyphosis
Beiyu Wang 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Objective: The purpose of the study was to compare the clinical and radiological outcomes of single level CDA and single-level anterior cervical discectomy and fusion (ACDF) in the patient with preoperative reversible kyphosis. Methods: From 2014-2018, patients who underwent single-level CDA and single-level ACDF were consecutively reviewed. The Japanese Orthopedic Association score, Neck Disability Index and VAS were used to evaluate clinical outcomes. Range of motion (ROM), C2-7 Cobb angle, functional spinal unit (FSU) angle, and heterotopic ossification (HO) were assessed. Results: Thirty-eight CDA patients (a mean follow-up of 39.8 months) and 42 ACDF patients (37.6 months) with preoperative reversible kyphosis were included. Both groups had significant improvements in clinical outcomes, without statistically significant differences. After surgery, both groups had a significant increase in C2-7 angle and FSU without significant inter-group differences. At the last follow-up, the C2-7 ROM was preserved in both groups. The segmental ROM of CDA group decreased mildly from 8.3° preoperatively to 5.1° finally, whereas the segmental ROM of ACDF group decreased significantly to nearly zero. 60.5% (23/38) patients in CDA group developed HO with 9 levels of grade III and 3 levels of grade Ⅳ. Conclusion: For the patients with single-level disc degenerative disease and preoperative reversible kyphosis, both CDA and ACDF achieved satisfactory and comparable clinical results. CDA was non-inferior to ACDF regarding the radiological outcomes of cervical alignment.Patients in CDA group had a relatively high incidence of HO formation.
Figure 1.
Case presentation. a, b, c: preoperative neutral, extension and flexion X-rays; d, e, f: neutral, extension and flexion X-rays at 5-year follow-up; red circle indicated the grade III HO foramtion.
1467
RF170: Analysis of patient reported outcomes in patients who underwent CTDR with the M6-C artificial disc and developed fusion as a result of heterotrophic ossification, compared to patients who underwent ACDF
Juan Amaya 1 , Jessica Gaff 1 , Gregory Cunningham 1 , Alana Celenza 1 , Paul Taylor 1 , Michael Kern 1 , Andrew Miles 1
1 Research, NeuroSpine Institute, Perth, Australia
Introduction: Spinal heterotopic ossification (HO) occurs when calcification or ossification occurs in the soft tissues and is a known complication of cervical disc replacements (CTDR) resulting in reduced motion at the CTDR level. Various devices have reported incidence of HO including the M6-CTM artificial disc. Unlike CTDR which aims to preserve motion, anterior cervical disc fusions (ACDF) aim to eliminate motion for bone growth between adjacent segments. Comparisons between patient reported outcome measures (PROMs) of ACDF and CTDR with HO have been limitedly investigated and not assessed in reference to the M6-CTM artificial disc, despite various reports of HO in this device after more than 12-months follow-up. This study aims to investigate the difference in outcomes between ACDF and fused CTDR as a result of HO with the M6-CTM artificial disc. Methods: For the CTDR group, radiographic and clinical outcomes data were collected during routine follow-up of patients who underwent CTDR with the M6-CTM implant at a multi-center between 2011 and 2022 and retrospectively assessed. Conventional X-Ray and CT scans of the cervical spine were used to identify HO and categorised as fused by an intersegment process motion measure of ≤ 1 mm. For the ACDF group, demographic and perioperative data were retrospectively analysed for participants who underwent single level ACDF procedures between July 2019 and August 2023 in a prospective, multi-centre, multi-surgeon database called the SPINE Registry. PROMs were completed post-operatively at 2 years at a mean 107 weeks and 105 weeks for CTDR and ACDF participants. PROMs assessed included EQ-5D-5L, VAS for neck and arm pain and the Neck Disability Index (NDI). Results: A total of 37/140 (26%) participants who underwent CTDR with the M6-CTM were categorised as fused at a mean follow-up of 5.4 years. The CTDR participants had a mean age of 47 years, a body mass index (BMI) of 29.0 and 38% female. A total of 54 participants with a mean age of 57 years, a BMI of 29.4 and 41% female underwent single level ACDF. The post-operative complication rate in the CTDR group was 6.3% compared to 7.4% in the ACDF group (p = 0.33) with 1 requiring return to theatre for implant failure. The mean scores for the CTDR group at 2 years post-operative were 80.1, 0.79, 15.3, 1.8 and 2.2 and 71.4, 0.73, 20.3, 2.1 and 1.8 in the ACDF group for EQ-5D VAS, EQ-5D Index, NDI and VAS neck and arm measures respectively indicating low pain and pain-related disability in both groups. The PROMs scores were generally better in the CTDR group but were not statistically significant. Long-term follow-up PROMs will be presented. Conclusion: Fused CTDR as a result of HO with the M6-CTM implant is common soon after CTDR. However, given the low complication rate of CTDR and good patient-reported outcomes, comparable to ACDF, fusion as a result of HO following CTDR with the M6-CTM implant may be a satisfactory outcome. Comparison of the radiographic outcomes at the fused and adjacent levels between CTDR with the M6-CTM and ACDF is warranted.
1044
RF171: The influences of endplate coverage and intervertebral height change on heterotopic ossification after cervical disc replacement
Yi-Wei Shen 1 , Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: Heterotopic ossification (HO) is a common complication after cervical disc replacement (CDR). Biomechanical factors including endplate coverage and intervertebral disc height change may be related to HO formation. However, there is a dearth of quantitative analysis for endplate coverage, intervertebral height change and their combined effects on HO. Material and Methods: Patients who underwent single-level or two-level CDR with Prestige-LP were retrospectively reviewed. Clinical outcomes were evaluated through Japanese Orthopaedic Association (JOA) score, Neck Disability Index (NDI) score, and visual analogue scale (VAS) score. Radiological data, including the prosthesis-endplate depth ratio, intervertebral height change, posterior heterotopic ossification (PHO) and angular parameters, were collected. Logistic regression analysis was used to identify the potential risk factors. Receiver operating characteristic curves were plotted and the cut-off values of each potential factors were calculated. Results: A total of 138 patients with 174 surgical segments were evaluated. Both the prosthesis-endplate depth ratio (p < 0.001) and post-operative disc height change (p < 0.001) were predictive factors for PHO formation. The area under the curve (AUC) of the prosthesis-endplate depth ratio, disc height change and their combined effects represented by the combined parameter (CP) were 0.728, 0.712 and 0.793, respectively. The risk of PHO significantly increased when the prosthesis-endplate depth ratio < 93.77% (p < 0.001, OR = 6.909, 95% CI 3.521-13.557), the intervertebral height change ≥ 1.8 mm (p < 0.001, OR = 5.303, 95% CI 2.592-10.849), or the CP representing the combined effect < 84.88 (p < 0.001, OR = 10.879, 95% CI 5.142-23.019). Conclusion: Inadequate endplate coverage and excessive change of intervertebral height are both potential risk factors for the PHO after CDR. Endplate coverage less than 93.8% or intervertebral height change more than 1.8 mm would increase the risk of PHO. The combination of these two factors may exacerbate the non-uniform distribution of stress in the bone-implant interface and promote HO development.
2062
RF172: Cervical sagittal balance after consecutive three-level hybrid surgery versus anterior cervical discectomy and fusion: radiological results from a single-center experience
Shihao Chen 1
1 Sichuan University, West China Hospital, Chengdu, China
Introduction: According to the different numbers and relative locations of cervical disc replacement (CDR) and anterior cervical discectomy and fusion (ACDF), three-level hybrid surgery (HS) has many constructs. The purpose of this retrospective study was to compare the sagittal alignment parameters of HS and ACDF for cervical degenerative disc disease (CDDD) and the association of the respective parameters. Methods: This study involved patients with three-level CDDD who underwent ACDF or HS at our institution between June 2012 and August 2021. This follow-up included one-level CDR and two-level ACDF (type I group), two-level CDR and one-level ACDF (type II group) and three-level ACDF. Cervical sagittal alignment parameters included cervical lordosis (CL), segment alignment (SA), T1 slope (T1S), C2-C7 sagittal vertical axis (SVA), T1S-CL, C2 slope (C2S), occipital to C2 angle (O-C2A) and segment range of motion (ROM). Postoperative complications included adjacent segment degeneration (ASD), imbalance, prosthetic subsidence and heterotopic ossification (HO). Results: The three groups with a total of 106 patients were better matched in terms of demographics. Patients who underwent HS had significantly higher CL than those who underwent ACDF at 1 week, 6 months, 12 months and the final follow-up after surgery, as well as significantly better SA at 12 months and the final follow-up. There was no significant difference in T1S, SVA, T1S-CL, C2S, O-C2A or segment ROM among the three groups after surgery. The T1S-CL was significantly associated with C2S in the type I and type II groups at the preoperative and final follow-up. There was no significant difference in postoperative complications among the three groups. Conclusions: Most improvements in cervical sagittal alignment (CL, SA, T1S, SVA, T1S-CL, C2S, O-C2A, and segmental ROM) were observed in all three groups postoperatively. HS was more advantageous than ACDF in the maintenance of postoperative CL and SA. Thus, three-level HS may be better for maintaining cervical curvature. The number of replacement segments differed in those who underwent HS but did not affect the correlation between T1S-CL and C2S, both of which are well balanced.
Keywords: cervical sagittal balance; radiological outcomes; hybrid surgery; anterior cervical discectomy and fusion; three-level surgery
1144
RF173: Impact of bone-implant gap size on the interfacial osseointegration: an in vivo study
Kangkang Huang 1 , Rongguo Yu 1 , Beiyu Wang 1 , Hao Liu 1
1 Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Objective: To evaluate the impact of bone-implant gap size on the interfacial osseointegration of cervical disc arthroplasty (CDA) in a rabbit animal model. Methods: A cylindrical (8 mm in diameter with different depth) calvarial bone-implant gap model was established to assess the impact of bone-implant gap size on interfacial osseointegration. A series of round-plate implants with different teeth depth (0.5 mm, 1.0 mm, 1.5 mm and 2.0 mm) was specifically designed. A total of 48 New Zealand white rabbits were randomly categorized into four groups by the implants they received (0.5 mm: group A, 1.0 mm: group B, 1.5 mm: group C, 2.0 mm: group D). At 4th and 12th week after surgery, animals were sacrificed. Micro-CT, acid fuchsin and methylene blue staining and hematoxylin and eosin (HE) staining were conducted. Results: At 4th week and 12th week after surgery, both micro-CT and HE staining showed more new bone formation and larger bone coverage in group A and group B than that in group C and group D. At 12th week, the bone biometric parameters were significantly superior in group C when compared with group D (p < 0.05). At 12th week, hard tissue slicing demonstrated larger portion of direct contact of new bone to the HA coating in group A and group B. Conclusions: Bone-implant gap size larger than 1.0 mm negatively affected bone-implant osseointegration between compact bone and HA coated implant surface.
1690
RF174: Incidence of bone loss after Prestige-LP cervical disc arthroplasty: a single-center retrospective study of 396 cases
Tingkui Wu 1 , Hao Liu 1 , Junbo He 1
1 Orthopedics, West China Hospital of Sichuan University, Chengdu, China
Introduction: The development of bone loss (BL) at the operated level after cervical disc arthroplasty (CDA) has not been well recognized. The incidence of bone loss (BL) may be correlated with the prosthesis type. Currently, no study has reported the incidence of BL after CDA with the Prestige-LP disc, and this remains an active area of research. To determine the incidence of BL after Prestige-LP CDA and evaluate the impact of BL on clinical and radiological outcomes. Material and Methods: We retrospectively reviewed patients who underwent Prestige-LP disc from January 2008 to October 2018 at our institution. Clinical outcomes were evaluated using Japanese Orthopedics Association (JOA), Visual Analogue Scale (VAS), and Neck Disability Index (NDI) scores. Radiological variables, including cervical lordosis, disc angle, global and segmental range of motion (ROM), heterotopic ossification (HO), and BL, were retrieved. Results: A total of 396 patients and 483 CDAs were evaluated. BL occurred in 56.6% of patients and 52.8% of CDA segments. Mild BL occurred in 30.2%, moderate BL in 37.3%, and severe BL in 32.5% of CDA segments. Notably, 88.2% of CDA segments developed BL within the first 3 months, and 19.1% of them progressed at 6 months. However, no progressive BL after 12 months was seen. 50.2% of CDAs showed superior and inferior endplates involvement. The incidence of BL was associated with age, surgery type, level distribution, and incidence and grade of HO. Patients with BL had a better segmental ROM, but no relationships between patients with or without BL were found in clinical outcomes. Conclusion: This study showed that BL was a common but self-limited phenomenon after CDA at the early postoperative stage. BL occurred starting from 3 months to 6 months after CDA, but it did not affect the clinical outcomes. It was prevalent in relatively young age patients, and those underwent 2-level CDA and involved C5/6 segment. Notably, patients with BL have larger ROM at the arthroplasty level, and this may be explained by the lower incidence and lower grade of HO. Future, a long-term follow-up study with more detailed radiographic data is mandatory to evaluate the long-term effects of BL.
2395
RF175: Refining criteria and classification of cervical kyphosis considering compensation mechanism based on 'neck tilt': A separate 'cone of economy' for cervical spine balance
Wesley Durand 1 , Yesha Parekh 1 , Jae-Koo Lee 2 , Seung-Jae Hyun 2 , Sang Hun Lee 1
1 Orthopaedic Surgery, Johns Hopkins Hospital, Baltimore, USA
2 Department of Neurosurgery,Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, South Korea
Introduction: Several criteria and classifications for cervical kyphosis (CK) have been proposed, though the majority are based on morphological grouping and do not directly address compensatory mechanisms. This study evaluated CK using ‘neck tilt’ (NT)—a constant parameter originating in prior studies—and proposes the ‘NT- T1 slope (C2/T1S) classification’, which classifies both morphology as well as the presence or failure of compensatory mechanisms. Material and Methods: This was a two-center, retrospective review of consecutive patients undergoing surgical management of CK. Preoperative and postoperative radiographic parameters were measured in cervical and full-length entire spine lateral radiographs. We defined cervical decompensation as C2S > T1S, and thoracolumbar (TL) decompensation as C2-SVA anterior to NT. Patients were grouped according to the NT- T1S classification, 1: focal CK, C2S < T1S, C2-SVA was posterior to NT, both cervical and TL compensation of CK; 2: global CK, C2S>T1S, C2-SVA was posterior to NT, no cervical compensation but intact TL compensation; 3: C2S < T1S, focal CK, C2-SVA anterior to NT, intact cervical compensation but no TL compensation; 4: C2S > T1S, global CK, C2-SVA anterior to NT, no cervical or TL compensation. Group 2, 3, and 4 were considered cervical deformity. Parameters were compared between the groups and previous criteria of CK; C2-C7 kyphosis ≥ 10°, C2-C7 SVA ≥ 4 cm, T1S-CL ≥ 2 5°, and classifications by Kim-ISSG and European-CSRS. Statistical significance was considered p < 0.05. Results: In total, 106 patients were included (mean age 57.9 ± 14.4years, female 57.6%, prior cervical fusion 33.0%). Pre-operatively, the distribution of patients based on the NT- T1S classification was: group 1 44.3% (n = 47), group 2 27.4% (n = 29), group 3 13.2% (n = 14), group 4 15.1% (n = 16). Group 1 showed normal range of C2-C7 angle, C2-7 SVA, C2S, T1S and showed normal cervical and TL compensation. Group 2 showed mean 11.9° T1S, 29.8° C2S, and a significant increase in T1S and decrease in C2S postoperatively (both p < 0.05). Group 3 showed mean 34.5° C2S and 47.9° T1S. Group 4 showed 74.9° C2S, 49.8° T1S, and a significant decrease in C2S post-operatively (p < 0.05). Overall, NT did not significantly change post-operatively among any group (all p > 0.05). Among all patients in groups 2, 3, and 4 combined, 81.4% met previous CK criteria. Conclusion: This study presented the NT- T1S classification, a refined classification for cervical kyphosis both based on morphology and compensatory mechanisms. This classification implies a separate cone of economy for the cervical spine, based around NT, which was reasonably constant at ∼45° both pre- and post-operatively. The NT- T1S classification is intuitive and comprehensive, and integrates cervical kyphosis with compensation mechanisms within and outside of the cervical spine. Futures studies will focus on clinical outcomes and implications for surgical decision-making.
1304
RF176: C7 extension crosswise osteotomy. A novel osteotomy for correction of chin-on-chest deformity in ankylosing spondylitis and method of planning of restoration of horizontal gaze
Andrzej Maciejczak 1
1 Neurosurgery, University of Rzeszow, St Lucas Hospital Tarnow, Poland
Introduction: Cervicothoracic C7 and T1 pedicle subtraction osteotomies (C/T PSO) are the surgical techniques most frequently implemented for the correction of chin-on-chest deformity in ankylosing spondylitis (AS). An alternative procedure is cervicothoracic extension osteoclasis (C/T EO), which involves osteotomy of posterior elements followed by osteoclasis of the ankylosed cervicothoracic intervertebral disk through head extension. The osteoclasis is poorly controlled and carries the risk of unintended dislocation of the cervical spine with consequent neurological injuries. It is believed that chin-brow angle between 10o-20o is the good compromise between downward and upward gaze is correction of rigid cervical kyphosis. This angle can be personalized for every individual patient and we present our method to do so. Materials and Methods: To eliminate this risk, we modified C/T EO by replacing osteoclasis with a crosswise cut of the C7 vertebral body, which we call C7 extension crosswise osteotomy (C7 ECO). This crosswise cut also eliminated the risks and disadvantages of C/T PSO; posteriorly based wedge excision may lead to stretching injuries of the lower cervical roots and/or failure to achieve the exact angle of excision, and therefore, sagittal correction. Furthermore, opening the osteotomy anteriorly, as in our method, instead of closing it posteriorly, as in PSO, eliminates the risks related to shortening of the posterior column, such as buckling dura, kinking of the spinal cord, and stretching of the lower cervical nerve roots within the newly formed neuroforamen. Results: We report the case of a 69-year-old male chin-on-chest deformity in the course of ankylosing spondylitis who underwent successful correction of froward gaze with the use of our novel osteotomy after preoperative personalized planning of chin-brow angle. Conclusions: The C7 ECO seems a viable alternative to C/T EO and C/T PSO for correction of fixed chin-on-chest deformity and cervical kyphosis.
414
RF177: Posterior two-step distraction and reduction for basilar invagination with atlantoaxial dislocation: a novel technique for precise control of reduction degree without traction
Xiaqing Sheng 1 , Yang Meng 1 , Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: The pathological changes of basilar invagination (BI) and atlantoaxial dislocation (AAD) include vertical and horizontal dislocations. Current surgical techniques have difficulty accurately controlling the degree of reduction in these two directions and often require preoperative traction, which increases patients’ pain, hospital stay, and medical cost. This study aimed to introduce a novel technique for accurately reducing horizontal and vertical dislocation without preoperative traction and report the radiological and clinical outcomes. Methods: From 2010 to 2020, patients with BI and AAD underwent posterior two-step distraction and reduction (TSDR) and occipitocervical fixation. Radiological examination was used to evaluate the reduction degree (RD) and compression. Japanese Orthopedic Association (JOA) score was used to evaluate clinical outcome. Results: A total of 55 patients with BI and AAD underwent TSDR and occipitocervical fusion. The clinical symptoms of 98.2% of them improved. JOA score increased significantly after the operation. Appropriate (50% ≤ RD < 80%) or satisfactory (RD ≥ 80%) horizontal reduction was achieved in 92.7% of patients, and 90.9% obtained appropriate or satisfactory vertical reduction. Thirty-one patients did not undergo preoperative skull traction. There was no significant difference in radiological outcomes or JOA scores between the traction- and non-traction groups. However, the length of hospital stay in the traction group was longer than that in the non-traction group. Conclusion: TSDR enables horizontal and vertical reduction. It is a safe, simple, and effective technique for patients with BI and AAD. Despite the absence of preoperative skull traction, the degree of reduction and clinical outcomes were satisfactory.
596
RF178: Practical answers to frequently asked questions in cervical spine surgery
Austin Kaidi 1 , Pratyush Shahi 1 , Tejas Subramanian 1 , Kasra Araghi 1 , Troy Amen 1 , Tomoyuki Asada 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Evan Sheha 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Surgical counseling enables shared decision-making (SDM) by improving patients' understanding. Here we aimed to provide answers to frequently asked questions (FAQs) in minimally invasive cervical spine surgery. Material and Methods: This is a retrospective review of prospectively collected data. Patients who underwent primary one- or two-level cervical spine surgery in form of cervical disc replacement (CDR) or anterior cervical discectomy and fusion (ACDF) and had a minimum of 1-year follow-up. Outcome measures included (1) Surgical (radiation exposure and intraoperative complications) (2) Immediate postoperative (length of stay [LOS] and complications) (3) Clinical outcomes (Visual Analog Scale [VAS] neck and arm, VAS; Neck Disability Index [NDI], 12-Item Short Form Survey Physical Component Score [SF-12 PCS], Global Rating Change [GRC], return to activities; complications/reoperations). The outcome measures were analyzed to provide answers to nine FAQs that were compiled based on the authors' experience and a review of literature. Changes in VAS neck, VAS arm, NDI, and SF-12 PCS from preoperative values to the early (< 6 months) and late (> 6 months) postoperative time points were analyzed with Wilcoxon Signed Rank Tests. % of patients achieving minimal clinically important difference (MCID) for these patient-reported outcome measures (PROMs) at the two time points was evaluated. Changes in PROMs from preoperative values too early (<6 months) and late (≥ 6 months) postoperative time points were analyzed within each of the two groups. Percentage of patients achieving MCID was also evaluated. Results: 197 (116 ACDF, 81 CDR) were included. The following FAQs were answered: (1) Will my neck pain improve? Most patients report improvement by > 50%. 64% of patients achieved MCID for VAS-Neck at ≥ 6 months for CDR and 55% did for ACDF. (2) Will my arm pain improve? Most patients report improvement by > 50%. 62% of patients achieved MCID for VAS-Arm at ≥ 6 months for CDR and 56% did for ACDF. (3) Will my activity level improve? Most patients report significant improvement. 55% of patients achieved MCID for SF 12-PCS at ≥ 6 months for CDR and 66% did for ACDF. (4) Is there a chance I will get worse? 9% after ACDF, 5% after CDR. (5) What is the likelihood that I will have a complication? 10% (6.5% minor, 3.5% major) for ACDF, 5% (3.8% minor and 1.2% major) for CDR. (6) Will I need another surgery? 1.5% after ACDF, 3.7% after CDR. (7) How long will I stay in the hospital? Most patients get discharged on postoperative day one after both ACDF and CDR. 16% and 35% get discharged on postoperative day zero for ACDF and CDR respectively. (8) When will I be able to return to work? > 80% of patients return to work (average: 2 weeks after ACDF, 10 days after ACDF). (9) Will I be able to drive again? > 80% of patients return to driving (average: 2 weeks after ACDF, 10 days after ACDF). Conclusion: These concise answers to the FAQs in cervical spine surgery can be used by physicians as a reference to enable patient education.
828
RF179: Challenges and innovative techniques in the surgical management of pediatric cervical spine deformities
Kandarpkumar Patel 1,2 , Sandip Chatterjee 1
1 Department of Neurosurgery, Park Clinic, Kolkata, India
2 Department of Spine Surgery, New Sheth P.T. Multispeciality Hospital, Surat, India
Introduction: Cervical spine deformities in pediatric age group are difficult to treat as limited options are available. The main challenges are abnormal anatomy, cartilaginous bone, and growing spine. To address these challenges, depending upon the conditions we may need to use innovative techniques for conservative as well as surgical management. Material and Methods: This was a retrospective single-center case series. We reviewed pediatric patients who underwent surgical intervention between 2005-2020 in our institute. Data collected included demographic details, detailed surgical interventional procedures, Preoperative and postoperative radiological as well as clinical findings. PROCESS guidelines were followed. Results: We identified 175 pediatric patients who underwent surgery for cervical spine deformity. The majority had craniovertebral junctional abnormalities. 112 patients had atlantoaxial joint deformity and 63 patients had subaxial cervical spine deformities. In subaxial group, we identified 36 congenital, 5 post-traumatic and 22 post-infective patients. Anterior, posterior, or anterior with posterior fixation techniques were used as per patients’ condition and bone quality. In very young patients in which cage, plate and large diameter spine screws were not suitable, we used cannulated lag screws, modified implants with wires and in some case, we used molded cervical braces and skeletal traction to buy out some time for growing spine for fixation. Intraoperative neuromonitoring was used during manipulation of cervical spine. All interesting cases are discussed in detail in this study. Conclusion: Pediatric cervical spine deformities are difficult to treat surgically because of limited available options for this age group. Understanding anatomy, evaluation of bone quality and identifying optimum length for stable fixation is vital in treating such deformities. If conventional surgical options are not suitable for some patients, then innovative techniques can be used if they serve the basic principles of decompression and stable fixation in the treatment of pediatric cervical spine deformity.
756
RF180: Clinical features and outcomes of basilar invagination
Maoyang Qi 1,2 , Zan Chen 1,2,3 , Wanru Duan 1,2,3
1 Neurosurgery
2 Spine Center, China International Neuroscience Institute (CHINA-INI), Beijing, China
3 Lab of Spinal Cord Injury and Functional Reconstruction, Xuanwu Hospital, Beijing, China
Background: Currently, there is inadequate reporting regarding the progression of basilar invagination, and the inseparable association between radiological features and symptomatology. Objective: This study endeavors to investigate the general patterns of symptom progression and prognosis in two types of basilar invagination, as well as the underlying mechanisms linking symptomatology and radiological findings. This will provide theoretical guidance for clinical intervention. Methods: A retrospective analysis was conducted on a total of 141 patients diagnosed with basilar invagination who underwent surgical treatment at Xuanwu Hospital from January 2016 to December 2020. The patients' neurological function was assessed preoperatively, postoperatively, and during follow-up using the Japanese Orthopedic Association (JOA) scale and Short-Form 12 (SF-12). The primary outcome measures were the JOA score, JOA improvement rate, and SF-12 score. Secondary outcome measures included reduction loss and postoperative adverse events. Logistic univariate and multivariate analyses were performed to predict prognostic risk factors. Results: The average age of the patients with basilar invagination in the cohort of 141 cases was 45.4 ± 13.1 years, and the mean onset age was 40.7 ± 13.2 years. Type A (21/101, 20.8%) had a higher likelihood of experiencing dizziness compared to type B (2/40, 5%) (p = 0.022). Preoperative JOA and SF-12 PCS scores indicated a greater degree of neurological impairment in type A as compared to type B (JOA, 13.0 vs 13.9, p = 0.042; SF-12 PCS, 37.48 vs 38.42, p = 0.034). Lateral cervical triangle area (251.2 ± 8.2 mm2) was more severe in type A than in type B (207.1 ± 13.2 mm2) (p = 0.001). Type B (22/40, 55%) had a higher likelihood of associated ataxia than type A (35/101, 34.7%) (p = 0.026), and exhibited a higher proportion of Chiari malformation (70% versus 45.6%; p = 0.006) and syringomyelia (72.5% versus 41.6%; p = 0.001), as well as a lower posterior fossa height (32.2 ± 1.8 mm versus 33.6 ± 2.5 mm; p = 0.017). Among patients with complete reduction, type B demonstrated a significantly higher improvement rate in SF-12 PCS than type A (22.5 ± 35.0% vs 40.4 ± 26.7%, p = 0.018). Patients with severe neurological impairment (JOA < 14) had smaller lateral mass and condylar heights (13.7 ± 2.6 mm vs 12.5 ± 3.3 mm, p = 0.023) and a smaller clivus-axial angle (135.3 ± 11.1° vs 131.0 ± 12.6°, p = 0.035). Further logistic regression revealed that onset age ≥ 45 years (OR 4.654, 95% CI 1.645-13.165; p = 0.004) and basal angle ≥ 125° (OR 28.139, 95% CI 1.090-726.239; p = 0.044) were independent risk factors for postoperative early neurological without improvement in type A and type B basilar invagination, respectively. Additionally, a preoperative atlantodental interval (ADI) ≥ 6 mm (OR 5.358, 95% CI 1.146-20.278; p = 0.013) was an independent risk factor for deteriorating neurological function without improvement in type A. Conclusion: Patients with type A basilar invagination present more severe lateral compression on radiological findings, resulting in significant neurological impairment and specific dizziness. Therefore, early clinical intervention is recommended for these patients. On the other hand, type B basilar invagination patients has milder neurological impairment, with more cases of ataxia, who can achieve better long-term prognosis following clinical intervention. However, the intervention time for type B should be based on the severity of actual symptoms and radiological characteristics.
RFP11: Minimally Invasive Spine Surgery
1105
RF181: Platelet rich plasma in lumbar facet join pain: a systematic review
Robert Meves 1
1 Santa Casa de São Paulo, Orthopedics-Spine Surgery, São Paulo, Brazil
Introduction: To evaluate the efficacy and safety of the use of Platelet Rich Plasma (PRP) in low back pain of facet origin. Material and Methods: The research was carried out according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), searching the following Databases: Pubmed, Scopus and Web of Science. A manual search was also performed. Randomized clinical trials, non-randomized trials and case series with more than 10 patients were included. The quality assessment and risk of bias of the works were analyzed using the RoB II tools and the Joanna Briggs Institute (JBI) Case Series checklist. Results: Nine articles that met the criteria were selected, being two randomized clinical trials with 190 patients and seven case series with 370 patients. The randomized clinical trials showed a low risk of bias, according to the RoB II instrument, while the case series showed heterogeneity, according to the checklist proposed by the JBI. All studies showed favorable conclusions to the use of PRP in facet joints. There were no reports of serious adverse effects. Conclusion: The results of the present studies demonstrate that the use of PRP can be a viable option for the management of low back pain in facet degenerative disease, with evidence level IV, according to the researched articles. Larger multicenter studies are needed.
1666
RF182: The effect of topical steroid on postoperative pain in patients undergoing stand-alone lateral lumbar interbody fusion
Soji Tani 1,2 , David Dalton 1 , Gaston Camino-Willhuber 1 , George Gorgy 1 , Thomas Caffard 1 , Lukas Schönnagel 1 , Erika Chiapparelli 1 , Ali Guven 1 , Jiaqi Zhu 1 , Jennifer Shue 1 , Darren Lebl 1 , Frank Cammisa 1 , Federico Girardi 1 , Alexander Hughes 1 , Gbolabo Sokunbi 1 , Andrew Sama 1 , William Zelenty 1
1 Hospital for Special Surgery, New York, USA
2 Department of Orthopaedic Surgery, Showa University, Shinagawa-ku, Japan
Introduction: Postoperative pain in the psoas and femoral nerve distribution is common following lateral lumbar interbody fusion (LLIF) surgery. Topical steroids have shown beneficial effects in spinal surgery. However, the effect of topical steroids applied directly to the psoas and the traversing nerve complexes in patients undergoing stand-alone LLIF (SA-LLIF) is unclear. We aimed to investigate the efficacy of topical steroids applied to the psoas muscle in patients who underwent SA-LLIF. Material and Methods: Patients who underwent SA-LLIF were included. Patient demographics, perioperative factors, length of stay (LOS), opioid consumption measured in oral morphine equivalents (OME), and pain scores on the numeric rating scale (NRS) were recorded and analyzed. Uni- and multi-variable regression analyses were performed to assess the impact of topical steroid use on OME, NRS, and LOS. A subgroup analysis was conducted on patients who did not receive transversus abdominal plane (TAP) blocks. Results: There was no significant difference between patients who received topical steroids and those who did not. In the subgroup analysis, NRS in the first 24 hours post-surgery was significantly lower in the topical steroid group (p = 0.03), while there was no significant difference in OME and LOS. In multivariable analysis, topical steroid use was an independent factor associated with decreased NRS in the first 24 hours post-surgery (p < 0.01). Conclusion: Topical steroids did not significantly improve pain measures during the postoperative period for patients undergoing SA-LLIF. However, topical steroids were associated with a lower NRS score in patients who did not receive a TAP block.
1604
RF183: Perception of intraoperative robotics and navigation by spine fellows and early attendings: a survey-based study
Pratyush Shahi 1 , Tejas Subramanian 1 , Sumedha Singh 1 , Evan Sheha 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: The utilization of navigation and robotics in spine surgery has been increasing; however, its impact on training and practice has still not been assessed. The objective of this study was to help address the deficiency in the literature by conducting a survey of current trainees and recent spine fellowship graduates (early-career spine surgeons) to determine their perspective of robotics and navigation in training and their experiences in practice. Material and Methods: The survey was administered in April 2022 to the young surgeon members of Society of Minimally Invasive Spine Surgery (SMISS) and orthopedic spine fellowship applicants from past 6 years. For analyses, only respondents who were trainees (residents or fellows) or early attendings ( < 5 years of practice) were included. The survey gathered information regarding: 1) Demographics, 2) Training - imaging modalities exposed to during training, perceived impact of navigation and robotics on training and reasons behind a positive or negative impact, 3) Practice - imaging modalities used in practice, reasons why or why not navigation and robotics were incorporated into practice, and anticipated utilization of navigation and robotics in 5 years’ time, 4) Confidence - confidence in placing screws using different imaging modalities, and 5) Teaching - perceived impact of navigation and robotics on teaching. Results: 51 surveys were analyzed. 71% were attendings (average practice years: 2), 29% were trainees. During training, 22% of respondents were exposed to only fluoroscopy, 75% were exposed to navigation, 51% were exposed to robotics, and 40% were exposed to both navigation and robotics. 87% and 61% of respondents who had exposure to navigation and robotics, respectively, felt that it had a positive impact on their training. In practice, 28% reported utilizing only fluoroscopy, 69% reported utilizing navigation, 30% reported utilizing robotics, and 28% reported utilizing both navigation and robotics. The top 3 reasons behind positive impact on training and incorporation into practice were: 1) increased pedicle screw accuracy, 2) exposure to upcoming technology, and 3) less radiation exposure. The top 3 reasons behind negative impact on training were: 1) compromises training to independently place screws, 2) time and personnel requirements for setup, and 3) concerns about being able to avail it in practice. The top 3 reasons behind not incorporating navigation and robotics in practice were: 1) difficulty to obtain, 2) time and personnel requirements for setup, and 3) technical complexity. > 65% of attendings reported that navigation and robotics had a positive impact on their ability to teach trainees. The confidence level was reported higher when placing screws with navigation and robotics than fluoroscopy. 76% of attendings felt that they will be utilizing more navigation and robotics in 5 years’ time. Conclusion: Navigation and robotics have a largely positive impact on spine surgery training, practice, and teaching. Most attendings believe they will be using more navigation and robotics in the coming years. However, the concerns of negative impact, too much exposure, and high cost voiced by some respondents demand spine surgeons to be thoughtful about how they integrate these technologies moving forward.
2136
RF184: Unilateral biportal endoscopic decompression (UBE) alone in degenerative spondylolistheis with lumbar canal stenosis : a clinical case series
Rajeesh George 1 , Rohit Kawishwar 1 , Panghung Wu 2 , Gamaliel Tan Yu Heng 1
1 Orthopedics, Ng Teng Fong General Hospital, Singapore, Singapore
2 Achieve Spine and Orthopedic Centre, Singapore, Singapore
Introduction: Unilateral biportal endoscopy (UBE) is an effective and safe surgery for complete decompression in patients of lumbar canal stenosis with advantages like minimal soft tissue damage, early mobilization, decreased length of hospital stays and decreased postoperative back pain. However, there is paucity of literature regarding treatment modality of UBE decompression alone in stable low grade spondylolisthesis patients. Aim: To analyse clinical outcomes of UBE decompression in patients of stable low-grade spondylolisthesis with lumbar canal stenosis. Methods: We retrospectively analysed patients who underwent UBE decompression alone in 9 patients of stable low-grade spondylolisthesis with lumbar canal stenosis from January 2022 to September 2022. The clinical outcomes were quantified in terms of visual analogue scale (VAS) for back pain and leg pain and Oswestry disability index (ODI). The radiological outcomes were measured by comparing the disc height, slip percentage and vertebral slip angle in lateral view at all the follow-ups. Results: For all the patients VAS for leg pain and ODI scores significantly improved at post-operative 2 weeks, 3 months, 6 months and final follow-up (p < 0.05). VAS for back pain did not increase statistically at final follow-up. In terms of radiological outcomes ratio of disc height, slip percentage and vertebral slippage did not worsen at final follow-up and this showed maintenance of stability of facet joints. Conclusion: UBE decompression alone is safe and effective modality of treatment for low grade stable spondylolisthesis. Along with its efficacy in decompression, this technique has capability of preserving stability of the facet joints. In selected patients with less preoperative back pain and more of claudication features with stable spondylolisthesis on dynamic x-rays, UBE decompression alone is effective way of treatment.
2585
RF185: Spinal cord tumor excision with tubular retractor system: a minimally invasive approach for improved patient outcomes
Naveen Ma 1
1 Neurosurgery, BGS Gleneagles Global Hospital, Bangalore, India
Introduction: Spinal cord tumors present complex challenges due to their delicate location and potential impact on neurological function. Traditional open surgery for spinal cord tumor excision often involves large skin incision and significant tissue disruption. The tubular retractor system has emerged as a promising minimally invasive alternative, offering potential benefits such as reduced tissue trauma, shorter hospital stays and improved patient outcomes. Methods: Eleven patients with spinal cord tumors were operated in a period of two years with age ranging from 27 to 55 years. Ten patients had intradural extramedullary tumor at various levels from D11 to L4 and one being extradural lesion at L1. Results: All the patients underwent complete tumor excision using 18 to 22 mm tubular retractor system with no postoperative deficits. The location of the tumor being D11-12 in three patients, L1-L2 in two cases and L3-4 in seven patients. The most common tumor encountered in our series is schwannoma (82%) in 09 cases and meningioma (18%) in 02 cases. Conclusion: Spinal cord tumor excision with the tubular retractor system offers a valuable alternative to traditional open surgical approach in terms of reduced tissue trauma, less postoperative pain and shorter hospital stay.
2359
RF186: Socioeconomic factors affecting length of stay (LOS) and post operative rehabilitation in lumbar fusion
Ramkumar Mohan 1 , Andrew Wu Guan Ru 2 , Chen Siyu 3 , Douglas Choi 3 , Dinesh Shree Kumar 2 , Reuben Soh 1
1 Orthopaedic Surgery Department, Singapore General Hospital, Singapore, Singapore
2 Changi General Hospital, Simei, Singapore
3 National University of Singapore, Singapore, Singapore
Introduction: Patients undergoing spine surgery have a fair amount of information presented to them in terms of expected procedure risk, post operative treatment plans and rehabilitation targets. Different patients of varied backgrounds can have different levels of understanding that affect their post operative outcomes. This study investigates the effects of socioeconomic indicators on Length Of Stay (LOS) as well as rehabilitation targets following Minimally invasive Transforaminal Lumbar Interbody Fusion (MIS-TLIF). Material and Methods: We use Socioeconomic Disadvantage Index1 (SEDI) and Socioeconomic Advantage Index1 (SAI) to compare socioeconomic status (SES) at various locations in Singapore. A recruitment of consecutive patients that underwent single and double level MIS-TLIF procedures from August 2015 to August 2022 across two institutions were included into the study. We used a national database to derive at individual room index for our patients. (Equation for room index: Sum total[number of rooms in an apartment × number of such apartments per block] / total number of apartments in a block). SEDI and SAI indices were obtained from a public policy paper by Earnest et al1. After comparative analysis, at individual and neighbourhood levels, the analysis was repeated with propensity score matching at 1:1 ratio. Results: A total of 221 patients were analysed. 115 (52.0%) of our total cohort were female patients and overall median LOS was 4 days (Interquartile range: [2.00, 6.00]). When Room index values were compared, no significant differences were noted in terms of LOS, intra-operative variables, post-operative complications and follow up compliance. Similarly, when unmatched cohorts stratified by neighbourhood based SES indicators were compared, no significant differences were noted. However, in these unmatched cohorts, there were numerical trends towards shorted LOS in individuals from neighbourhoods with higher SAI (4.00 [3.00, 7.00] vs 3.00 [2.00, 5.00], p = 0.092). Congruent numerical trends were noted in individuals in neighbourhoods with higher disadvantage scores having longer LOS (4.00 [3.00, 6.00] vs 3.00 [2.00, 6.00], p = 0.156]. After matching cohorts, there was a significantly shorter LOS noted amongst patients living in neighbourhood with higher advantage scores (n = 73:73), (4.00 [3.00, 6.25] vs 3.00 [2.00, 5.00], p = 0.035). There was also a non-significant trend towards patients with higher neighbourhood advantage scores having lower number of Physiotherapy (PT) sessions needed prior to being discharged (3.83[2.41] vs 2.82 [1.44], p = 0.071). We noted a complementary non-significant trend towards patients with higher disadvantage scores having longer LOS after matching (4.00 [3.00, 6.00] vs 3.50 [2.00, 5.70], p = 0.297). Conclusion: Patients with high advantage scores had shorter LOS and less physiotherapy sessions before discharge. These findings were supported by trends towards patients with higher disadvantage scores having longer LOS. This paper provides information for surgeons when consenting patients for Spine surgery, that secondary effort in pre operative counselling and physiotherapy will be beneficial to provide adequate understanding for Spine surgery.
References
1. Earnest A, Ong MEH, Shahidah N, et al. Derivation of indices of socioeconomic status for health services research in Asia. Preventive Medicine Reports 2015; 2: 326-32.
2406
RF187: Percutaneous spine fusion: an experience overview in a tertiary cancer center
Romulo Augusto Andrade de Almeida 1 , Christopher Alvarez-Breckenridge 1 , Franco Rubino 1 , Laurence Rhines 1 , Rob North 1 , Claudio Tatsui 1
1 Department of Neurosurgery, MD Anderson Cancer Center, Houston, USA
Introduction: advances in diagnosis and treatment have led to an increase in the prevalence of patients with cancer and, consequently, metastases. Distant spread to the spine is relatively common and an important cause of morbidity (pain and neurological deficits), often requiring spine stabilization through fusion. However, the hold on chemotherapy during surgery recovery probably negatively impacts systemic disease control, and therefore efficient minimally invasive procedures would benefit these frequently frail patients. There is evidence that percutaneous implantation of pedicle screws-rod hardware is safe and may provide a durable stabilization, while reducing pain. Here, we report our experience with percutaneous fusion in a tertiary cancer center. The frequency of spontaneous facet fusion and hardware failure were investigated. Local control rates and time to resume chemotherapy were also reported for metastatic cases. Material and Methods: a retrospective, single-arm, single-institution study was conduct. IRB approval was obtained for data collection. Consecutive patients that had surgery from April 2014 to September 2023 were identified, and all who had percutaneous fusion were included. Patients’ medical charts were reviewed and demographic, histopathological, surgical, and evolutive/outcome data were collected. Pain was evaluated by the visual analogic scale (VAS). Results: 119 patients (68 males, 51 females), corresponding to 125 constructs implanted, were found. Six cases had two spinal segments fused. Mean age was 59 years (±11.8). Metastatic etiology was found in 101 patients (85%), followed by multiple myeloma/plasmocytoma (N = 16, 13%), primary tumor (N = 1, 1%), and fracture not related to tumor (N = 1, 1%). Between metastatic disease, the first three more frequent primary sites were renal, lung, and breast, in decrescent order. Titanium screws were used in 121 cases (97%), and carbon fiber-reinforced PEEK screws were used in 4 (3%). Median construct length was 3 vertebral levels. The most frequent construct design was bilateral screws on the immediate upper and lower vertebrae to the affected level. Cement augmentation was used in 120 (96%). Intraoperative complications were seen in three cases, all cement extravasation. Median length of stay was 5 days (range 2–36 days). Overall, postoperative VAS was reduced by a median of three points compared to pain at hospital admission. Any sign of spontaneous facet fusion was seen in 48(38%) after a median time of 11 months (range 0-71). Eight cases (6%) presented hardware failure, requiring open surgery to fix: 3 screw fractures, 1 rod fracture, 3 peri-screw haloing, 1 construct disassemble. The median interval between surgery and resuming/initiating chemotherapy for those receiving chemotherapy up to 90 days after surgery (N = 80) was 20 days (range 1-86). Conclusion: percutaneous fusion has shown low rates of hardware failure and complications. Surgery promoted spinal stability and reduced pain in short/medium-term. Its smaller incisions and less disruption of the paraspinal musculature attachment may relate to lower length of in-hospital stay, quicker recovery and resume of chemotherapy. Further studies comparing open versus minimally invasive surgery are necessary.
1465
RF188: A novel minimally invasive sacroiliac joint fusion technique - Surgical technique and case series
Andrew Berg 1 , Jessica Gaff 1 , Gregory Cunningham 1 , Paul Taylor 1 , Michael Kern 1 , Andrew Miles 1 , Alana Celenza 1
1 Research, NeuroSpine Institute, Perth, Australia
Introduction: The sacroiliac joint (SIJ) is considered the primary source of low back pain in approximately 10-38% of patients. It may be more common in those with pain after lumbar fusion because of increased stress transfer. Traditional open surgical fusion of the SIJ is associated with significant morbidity and poor outcomes but a growing body of evidence supports treatment with minimally invasive surgical (MIS) techniques, when conservative measures fail. These MIS techniques neglect many principles of traditional fusion surgery. MIS implants inserted via a lateral or posterolateral approach provide only a small surface area for fusion at the interface between the implant and SIJ. Those utilizing a posterior approach rely on distraction between the generally weak sacral and alar bones and grafting of the sacroiliac recess rather than the true SIJ itself. While these techniques show good clinical and radiographic outcomes in the short term few results have been published beyond 5 years follow-up. Without solid SIJ fusion the mechanical longevity of the implants and maintenance of clinical outcomes is a concern. We report a novel SIJ fusion technique which maintains MIS principles but enables the introduction of bone graft directly into the SIJ, providing greater surface area for fusion and facilitates grafting of the sacroiliac recess. Material and Methods: Patients who had undergone SIJ fusion utilizing the described technique were identified from the institutions database. A review of prospectively collected data has been performed. Surgical Technique: The patient is positioned prone. A posterior approach to the sacroiliac recess is made utilizing a longitudinal paramedian or midline incision. The lateral recess is cleared of soft tissue, decorticated and iliac crest bone harvested for autograft. A navigation frame is attached to the pelvis and 3D imaging obtained following which screw trajectories are planned. A corresponding lateral incision and muscle splitting approach to the ilium is made. RIALTO (Medtronic) system guidewires are navigated into place using a Brainlab drill-guide. Guidewires and later screws packed with bone graft, are placed posteriorly from posterosuperior to anteroinferior directed “down” the SIJ principally for the purpose of graft bed preparation and graft delivery and from the ilium into S1 or S2 segments “crossing” the SIJ principally for the purpose of enhancing stability of the now weakened and grafted SIJ. Implant position is confirmed with imaging. Bone graft is packed into the sacroiliac recess. Layered closure is performed. Results: Seven (4 right, 3 left) procedures have been performed on 6 patients. Mean age was 63.4 years (range 36-77) at surgery. Post-operative CT imaging was available for 5 procedures (4 patients) at a mean of 65 weeks follow-up, of which all confirmed fusion across the SIJ external to the implant. No implant-related complications or requirement for revision surgery have been identified. Conclusion: A novel SIJ fusion technique that enables introduction of bone graft directly to the SIJ and sacroiliac recess and enhanced stability using combined lateral and posterolateral approaches is described. Early results suggest that solid fusion within the SIJ can be obtained while maintaining MIS principles.
1609
RF189: High accuracy of 3D navigated K-wire-less single step pedicle screw system (SSPSS) in MIS-TLIF surgery: comparison of intraoperatively planned vs. actual screw placement
Mateusz Bielecki 1 , Yizhou Xie 1 , Jessica Berger 1 , Catherine Mykolajtchuk 1 , Blake Boadi 1 , Ji Tu 1 , Pravesh Gadjradj 1 , Ibrahim Hussain 1 , Roger Härtl 1
1 Och Spine, Weill Cornell Medicine, New York, USA
Introduction: Our group previously described the Single Step Pedicle Screw System (SSPSS), which does not incorporate K-wires, as a safe and effective workflow for lumbar fusions. K-wires pose a risk of visceral or vascular injury and unintended migration. For navigation, many instruments including a drill guide and awl are also needed which can cause disruption in surgical workflow. With the SSPSS, we were able to completely eliminate the use of K-wires and combine docking, tapping, and screw placement into one step with one device registered for intraoperative navigation in lumbar fusions. Concerns remain, however, about the reliability and accuracy of screw placement in MIS surgery when using a system without K-wires. We sought to address concerns about the reliability of our SSPSS system by assessing placement accuracy of 3D navigated screws. This was done by comparing intra-operatively planned screw trajectories to final screw placement. Materials and Methods: A retrospective study was conducted of patients undergoing MIS TLIF for lumbar degenerative disease at a tertiary referral center. Screws were placed using intraoperative 3D navigation. Together with surgical parameters, intra-operatively planned screw trajectories stored within a navigation system and actual screw placement were scored with the Gertzbein-Robbins classification by two spine surgeons. Scoring between each planned trajectory and its corresponding implanted screw was then compared to assess accuracy. Results: A total of 47 consecutive patients were included in this study. Most patients underwent a one level MIS TLIF (80.9%). In total, 206 screws were placed. Most screws were placed at L4 and L5. According to the Gertzbein-Robbins classification 197/206 (96%) of screws were placed as intra-operatively planned. No revisions or complications were recorded. Conclusion: Our study demonstrates that 96% of pedicle screws were implanted as intra-operatively planned. This favorable result demonstrates that the SSPSS workflow with 3D navigation allows for accurate and reliable placement of MIS pedicle screws despite the elimination of K-wires in the surgical workflow.
1976
RF190: Correlation of clinical outcomes to intraoperative transcranial motor evoked potential during L4-L5 lateral lumbar interbody fusion
Andrew Legarreta 1 , Joseph Hudson 1 , Raj Lavadi 1 , Rohit Prem Kumar 1 , Gregory Adams 1 , Nitin Agarwal 1 , Kojo Hamilton 1 , David Okonkwo 1 , Adam Kanter 2 , Nima Alan 3
1 Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, USA
2 Hoag Neurosciences Institute, Hoag Specialty Clinic, Newport Beach, USA
3 Neurological Surgery, University of California, San Francisco, USA
Introduction: Transpsoas lateral lumbar interbody fusion (LLIF) at the L4-5 level has historically been associated with the risk of femoral nerve injury. Spontaneous and triggered electromyography are routinely employed, but these neuromonitoring modalities do not provide data about the health of the femoral nerve during retraction of the lumbar plexus. This study aimed to assess the utility of intraoperative transcranial motor evoked potentials (tcMEP) in detecting postoperative femoral nerve injury following L4-L5 LLIF. Material and Methods: This study is a consecutive series of patients undergoing L4-L5 LLIF with tcMEP. A decrease in amplitude by 50% was defined as significant, and surgeons were alerted. Information about patient demographic variables, neuromonitoring data, and postoperative neurologic examinations were collected. The sensitivity, specificity, and area under the curve (AUC) for the receiver operating characteristics (ROC) curve were calculated. A simple logistic regression analyzed the relationship between a significant reduction in tcMEP and the presence of postoperative femoral nerve injury, defined as concurrent knee extension and hip flexion weakness. Results: Sixty-two patients (69% female) were included with a mean age and follow-up of 62.8 ± 10.0 years and 13.7 ± 14.6 months, respectively. Seven patients had motor weakness at the time of the last follow-up. In an analysis of tcMEP, 24 of 62 patients (38.7%) had a significant decrease in tcMEP amplitude, as defined above. The sensitivity of tcMEP to detect persistent neurologic deficit was 29% (95% CI 3.7% to 71%), and the specificity was 60% (95% CI 46% to 73%). The AUC for the ROC curve of tcMEP amplitude reduction was 0.54. Logistic regression demonstrated no association with postoperative neurologic deficit with an odds ratio of 1.0 (95% CI 0.98 to 1.02). Conclusion: Reduction in tcMEP amplitude by 50% during L4-L5 LLIF has poor accuracy in detecting persistent neurologic deficits.
1211
RF191: Comparative efficacy of clinical interventions for sacroiliac joint pain: systematic review and network meta-analysis with preliminary design of treatment algorithm
Yanting Liu 1 , Siravich Suvithayasiri 1,2 , Jin-Sung Kim 1
1 Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea
2 Department of Orthopedics, Chulabhorn Hospital, Chulabhorn Royal Academy, Bangkok, Thailand
Introduction: Sacroiliac joint (SIJ) pain is a major contributor to chronic low back pain, a condition that plagues approximately 10-33% of individuals worldwide. While commonly misdiagnosed or overlooked, SIJ pain can significantly impair an individual's quality of life, limiting mobility and daily function. The SIJ is a complex anatomical structure coupled with a range of potential etiological factors, makes diagnosing and treating SIJ pain a clinical challenge. Over the past few years, a range of clinical interventions have been developed to address SIJ pain, but their comparative effectiveness remains an open question. This study aims to synthesize existing evidence through a systematic review and network meta-analysis (NMA) to evaluate the comparative effectiveness of various clinical interventions in treating SIJ pain, focusing on pain intensity and quality of life as primary outcomes. Material and Methods: This study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and was registered with PROSPERO prior to commencement. A comprehensive literature search was conducted across multiple databases. The inclusion criteria encompassed randomized controlled trials (RCTs) that compared at least two different clinical interventions for treating SIJ pain in adult populations. Extracted data included study design, sample size, interventions compared, follow-up periods, and primary and secondary outcomes (pain intensity and quality of life). Discrepancies between the two reviewers were resolved through discussion or by involving a third reviewer. The quality of the included studies was assessed using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2). The NMA was performed using Stata software, utilizing a frequentist framework. Both direct and indirect evidence were combined to assess the comparative effectiveness of interventions. Primary outcomes included pain intensity (PI), measured using the Visual Analog Scale (VAS) or Numeric Rating Scale (NRS), and quality of life (QoL), assessed through validated instruments like the SF-36 or EQ-5D. Network geometry was created to visualize the connections between the different treatments, and the Surface Under the Cumulative Ranking Curve (SUCRA) was utilized to rank the interventions. Results: Nine RCTs involving 652 patients met the inclusion criteria, reporting six different clinical interventions: conservative therapy, cooled radiofrequency (CRF), thermal radiofrequency (TRF), pulsed radiofrequency (PRF), intraarticular injection (IJ), and SIJ fusion. Pairwise meta-analysis showed CRF and TRF to be superior to conservative therapy and IJ, respectively, in relieving PI. CRF also outperformed conservative therapy in improving QoL. In the NMA, SIJ fusion emerged as the most effective intervention for both PI and QoL, followed by CRF and TRF. IJ was the least effective compared to conservative therapy. The Surface Under the Cumulative Ranking Curve (SUCRA) revealed SIJ fusion as the most efficacious treatment, ranking highest in both PI (92.2%) and QoL (95%). Conclusion: fusion appears to be the most effective treatment for SIJ pain, significantly improving both pain intensity and quality of life. CRF and TRF also show promising results. However, the evidence is still limited, and further RCTs are needed to substantiate these findings.
1218
RF192: Mini-open retropleural approach based on microneurospinal surgical anatomy
Takashi Moriwaki 1 , Sho Fujiwara 1 , Koichi Iwatsuki 1
1 Department of Neuro Spinal Surgery, Osaka Gyoumeikan Hospital, Osaka, Japan
Introduction: Thoracic to thoracolumbar junction have anatomical complexity which consist of not only organs, but also membranes and layers. Mini-Open Retropleural approach is getting available for Adult Spinal Deformity correction by LIF, OVFs by LIF corpectomy. To purpose is to report Mini-Open Retropleural approach based on Microneurospinal Surgical Anatomy focusing on membranes and layers. Material and Methods: From 2020 to 2022, 17 cases by using Mini-Open Retropleural approach with one lung ventilation performed. They consisted of 10 cases; vertebral collapse/LIF corpectomy from T10 to L1, male 4/female 6, mean age 73.1y, blood loss 171.1 cc, Op. time 278.8cc and 6 cases; cMIS including Thoracic LIF for ASD from T10 to L1, male 2/female 4, mean age 76y, blood loss 108.3cc, Op. time 346min and 1 case; Thoracic disc herniation of T10, male, 60y, blood loss 50cc, Op. time 227min. All patients underwent surgery under a microscope, we retrospectively confirmed the Microneurospinal Surgical Anatomy of Mini-Open Retropleural approach, and examined the presence or absence of organ damage, nerve damage, and membrane damage during surgery. After partial costal bone resection just above the target vertebral body, you can enter the extrapleural compartment between the endothoracic fascia and the parietal pleura, and beyond the intervertebral foramen, using the communicating branch as a landmark, you can return to the subendothoracic compartment and reach the anterior lateral side of the target vertebral body. Results: There was no lung or Aorta, vena cava injury. There was 1 case of postoperative transient intercostal neuralgia and 6 cases of partial parietal pleural injury. There were no pneumothorax or organ injuries requiring treatment. There was no spinal cord injury due to unilateral segmental artery dissection. Conclusion: Mini-Open Retropleural approach can safely reach the anterolateral side of the vertebral body through a layer (extrapleural compartment) that is different from the layer passing the intercostal nerves and intercostal arteries and veins.
1217
RF193: Navigation guided endoscopic decompression for ossified ligamentum flavum in thoracic spine
Phattareeya Pholprajug 1,2 , JinSung Luke 1
1 Neurosurgery, Catholic University of Korea, Seoul St. Mary's Hospital, Seoul, South Korea
2 Rayong Hospital, Orthopedics, Rayong, Thailand
Objective: Surgically addressing thoracic Ossification of the ligamentum flavum (OLF) presents a complex challenge, given the need to achieve adequate decompression while preserving the integrity of the facet joint. This study seeks to underscore the advantages of a minimally invasive spine surgery technique, further enhanced by a highly precise and safe visualization system. This approach combines endoscopic decompression with a Navigation-guided system for the benefit of patients dealing with thoracic Ossification of the ligamentum flavum (OLF). Methods: Patients who underwent navigation-guided endoscopic decompression, using either a uniportal or biportal technique, within the time frame of 2019 to 2022 were subject to review. Inclusion criteria encompassed patients with a minimum of one year of follow-up. The study gathered data on various clinical outcomes, including VAS scores for back and leg pain, ODI scores, EQ5D scores, and satisfaction scores. Additionally, postoperative Computerized Tomography (CT) scans were utilized to assess the adequacy of decompression. Results: All surgical procedures were successfully carried out without encountering any complications. Furthermore, all 6 patients exhibited favorable clinical outcomes, showing significant improvement postoperatively. CT scans also confirmed adequate decompression, with minimal facet resection, and no remnants of OLF were detected throughout the entire follow-up period. Conclusion: Endoscopic decompression combined with Navigation-guided system can achieve successful decompression and ensure favorable postoperative outcomes for patients with thoracic Ossification of the ligamentum flavum (OLF).
1708
RF194: Characteristics of post-operative infective spondylodiscitis following full endoscopic lumbar disc surgery - A retrospective analysis of eight years
Phani Kiran Surapuraju 1
1 Spine Surgery, Gleneagles Global Health City, Chennai, India
Introduction: Infective spondylodiscitis following a lumbar discectomy is a rare complication. Full endoscopic lumbar discectomy is a minimally invasive technique emerging as a favoured technique for lumbar disc surgery in the last couple of decades. The use of irrigation fluid and radiofrequency ablators add to the possible sources of intraoperative contamination. There is a paucity of information on post-operative discitis after endoscopic disc surgery in the literature. The purpose of this study is to analyse the incidence, clinical characteristics and results of infective spondylodiscitis after endscopic lumbar discectomy at our centre. Material and Methods: A retrospective analysis of all the full endoscopic lumbar discetomy surgeries performed at our centre over the past 8 years was done. Incidence, risk factors, co-morbidities, clinical presentation, laboratory parameters and radiological features of the cases which developed post-operative infective spodylodiscitis were analysed. The parameters were compared to the published literature on discitis after microdiscectomy. Results: The study found that there were six cases of infectious discitis in over 550 cased of endoscopic discectomy surgeries performed in the past eight years. Five of the six patients had medical conditions that compromised their immunity. Five cases had undergone endoscopic interlaminar approach while one had transforaminal approach. Five patients were diagnosed within initial eight weeks after index surgery while one patient developed symptoms after 6 months. All the six patients underwent a fusion surgery. Four cases had no growth on aerobic cultures, two cases had pseudomonas growth. Two cases were diagnosed as tuberculosis based on histopathology and were treated with anti-tubecular therapy. Conclusion: The incidence of post-operative infective spondylodiscitis after full endoscopic discectomy is around one percent, similar to the known incidence after microdiscectomy. There doesn't seem to be any apparent benefit of continuous irrigation in terms of reducing risk of disc infection. Diabetes mellitus and long term steroid medication have been found to be risk factors for post-operative spondylodiscitis. Improved reporting of complications and larger studies will help characterise the risk factors and microbiological nature of the infective spondylodiscitis after endoscopic discectomy.
1543
RF195: Third generation vertebral body augmentation for osteoporotic compression fracture
Aditya Thakur 1 , Sudhir G 1 , Karthik Kailash 1
1 Spine Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, India
Introduction: Osteoporotic fracture incidence typically ranged between 500 and 1000 per 100,000 person- years among adults aged 50 and older. Osteoporosis spine fracture is endemic implications are fracture are far reaching. In older population the treatment options tends to limited. In view of it we need the modalities which avoids Anaesthetic complications as well as it should provide complete solution to the problem of osteoporotic fracture. Aim: To Study the Vertebral body augmentation in form of Vertebral body Stenting for osteoporotic fracture. Material and Methods: Prospective study with 32 sample size all osteoporotic compression fracture after 3 weeks of conservative trial. Inclusion criteria: -OF 1, 2, 3 without neurological deficits. Exclusion criteria: - OF 4, 5, OF 1, 2, 3 with neurological deficits. Results: Male: 12, Female: 20. Most common level involved: D-12 (15/32). Most common type: OVCF Type - OF 3. Average Pre-op Height: 12 mm increased to 26 mm. Average Pre-op Focal segmental kyphosis: 17.3 degrees decreased to 8.5 degrees. Average Pre-op vertebral angle: 12.6 degrees decreased to 6.0 degrees. Average Pre-op Beck Index: 0.67 increased to 0.80. Average Pre-op VAS: 7.3 decreased to 2.1. High Viscosity Cement in Low pressure Area. Conclusion: Reduction of Pain with adequate amount and equal spread of cement. Restoration of Height with Mechanical Stability. Sustained maintenance of Correction of height preventing further collapse. Maintenance of Global Sagittal balance. Minimal invasive procedure under Local Anaesthetia. The Stent allow reconstruction of the anterior column with reduced subsequent loss of correction / maintenance of correction Prevents complications: Immediate - Cement Leakage / Extravasation. Late - Global Sagittal Imbalance i.e. Progressive kyphotic deformity.
775
RF196: Radiological and clinical adjacent segment degeneration of midline lumbar inter-body fusion (MIDLF) surgery with cortical bone trajectory (CBT) screw insertion: a minimum 2 year retrospective study
Chih-ying Wu 1,2,3
1 Neurosurgery, China Medical University Hsinchu Hospital, Zhubei, Taiwan
2 Neurosurgery, China Medical University Hospital, Taichung, Taiwan
3 Graduate Institute of Integrated Medicine, China Medical University, Taichung, Taiwan
Introduction: Treatment for lumbar degenerative spondylolisthesis (LDS) remains a topic of debate. However, instrumented fusion surgery has demonstrated superior long-term outcomes. One meta-analysis review indicates that the rate of developing adjacent segment degeneration (ASDeg) after lumbar instrumented fusion surgery is as high as 26.6%, with nearly 1/3 of cases progressing to adjacent segment disease (ASDis). Risk factors for ASDeg include age, genetic factors, high body mass index, and surgical techniques. The MIDLF surgery with CBT screw insertion, introduced by Mizuno in 2014, offers several advantages over traditional pedicle screw fixation, such as less blood loss, early ambulation, and improved pain scores on postoperative assessments. Therefore, in this study, we will investigate whether MIDLF decreases the probability of ASDeg or ASDis, associated risk factors and re-operation rate. Material and Methods: This is a single-hospital retrospective study. ASDeg was defined as meeting at least one of the following criteria: 1. Disc height decreased ≥ 3 mm, 2. Vertebral body sagittal anteroposterior translation ≥ 3 mm, 3. Segmental angulation > 10º on flexion and extension. Inclusion criteria: Patients who underwent MID-LIF with CBT screw fixation, followed for more than 2 years, met the criteria for ASDeg. Exclusion criteria: Patients with a history of lumbar spine fusion, tumor, infection, or trauma. Assessment included age, gender, BMI, segments of fusion, sacrum involvement, pre- and post-operative back and leg visual analog scale (VAS), post-operative Macnab criteria, radiological evaluation, and reoperation after MIDLF. Results: We collected 31 patients who met the inclusion criteria between 2019 and 2021. Age was 60.703 ± 9.6 years. Male and female was 12 (38.7%) and 19 (61.3%). BMI was 25.503 ± 1.4. Preoperative VAS of back was 903 ± 1.1 and leg was 8.303 ± 2.5. Among the patients, 20 (64.5%) underwent one level fusion, 6 (19.4%) had two levels fusion, 4 (13.0%) had three levels fusion, and 1 (3.2%) had more than four levels fusion. The follow-up period was 37.503 ± 10.3 months. Clinical outcome revealed that the postoperative VAS of back was 203 ± 1.5 and leg was 1.803 ± 1.4. Macnab criteria excellent: 6 (19.4%); Good: 24 (77.4%); Fair: 1 (3.2%). Radiological evaluation revealed four patients got ASDeg. The first patient, five levels fusion with sacrum involvement, was decreased upper-level disc height (5.7 mm) and increased lower-level segmental angulation (14.8o). The second, two levels fusion with sacrum involvement, was decreased upper-level disc height (4.2 mm) and increased upper-level segmental angulation (10.5o). The third, three levels fusion with sacrum involvement, was increased upper-level segmental angulation (10.8o). The fourth patient, two levels fusion, increased upper-level segmental angulation (11.7o) and development with ASDis (low back pain, bilateral leg paresthesia). Furthermore, he received upper-level decompression due to stenosis on post-operative MRI. Overall, in our study, the rate of ASDeg and ASDis were 12.9% and 3.2% respectively after MIDLIF with CBT screw fixation. The rate of reoperation due to ASDis is 3.2%. Conclusion: According to our initial data, MIDLIF with CBT screw fixation appears to be an effective spinal fusion surgery for preventing ASD. Further research involving a larger patient cohort and longer follow-up periods is necessary to validate these findings.
1160
RF197: First clinical results after cement-augmented Ringosteosynthesis for osteoporotic Pincer fractures of the spine - a new percutaneous minimally invasive surgical procedure - as an alternative to long segment instrumentations
Tabea Miron 1 , Ina Moritz 1 , Charalampos Christoforou 1 , Yu-Mi Ryang 1
1 Helios Klinikum Berlin Buch, Clinic for Neurosurgery and Spinal Surgery, Berlin, Germany
Introduction: The treatment of osteoporotic vertebral body fractures is a major challenge due to their prevalence and impact on quality of life, especially in frail patients. The management of OF-Pincer fractures is particularly complex as long-segment instrumentation with or without vertebral body replacement is usually recommended. Such invasive procedures are associated with significant perioperative risk. This paper presents first clinical results of a new surgical procedure, minimally invasive percutaneous PMMA-augmented pedicle screw Ringosteosynthesis, with special attention to complication rate, revision surgery and pain reduction. Methods: A cohort of 46 patients with osteoporotic OF4-Pincer fractures between thoracal vertebrae 8 and lumbar vertebrae 5 was treated with Ringosteosynthesis. Pre- and postoperative pain intensity (NRS) was assessed. In addition intra- and postoperative complications, incidence of subsequent fractures, need for follow-up surgery and long-term pain intensity and quality of life during follow-up were investigated. Data were collected and analysed retrospectively. Results: There were 31F and 15M (mean age 77.7 ± 6.5 (52-91) years), with mBMI: 25.2 ± 4.95 (18.4-40) and ASA score: 2.5 ± 0.65 (1-4) operated. After treatment with Ringosteosynthesis there was a significant reduction in pain by an average of 4.43 ± 1.58 (1-9) points on the NRS pre- to postoperatively (mNRS preop 7.88 ± 1.51 (2-10); postop 3.44 ± 1.55 (0-6); p < 0.05). 69% of patients were followed up at an average of 27.7 ± 11.07 (3-72) weeks, showing a pain reduction of 5.6 ± 1.58 (0-7) points on the NRS compared to preoperatively. One intraoperative complication (2.2%) occurred with pedicle screw avulsion during rod placement. One patient had a subsequent fracture (2.2%), 5 patients (10.9%) showed asymptomatic post-sintering in the fractured vertebral body on CT after 27.7 ± 11.07 (3-72) weeks. None of these post-sinterings required revision surgery. Discussion: This paper presents the clinical application of Ringosteosynthesis as a new minimally invasive surgical procedure as a promising alternative to long-segment stabilisation for thoracolumbar OF4-Pincer fractures. Potential advantages of this minimally invasive technique include a reduced rate of union fractures, proximal junctional failure when instrumenting the fractured vertebral body alone, shorter operating time, less blood loss, faster recovery, shortened hospital stay and higher cost-efficiency. The significant reduction in pain intensity and the low rate of subsequent fractures and interventions indicate sufficient stability and effectiveness of Ringosteosynthesis in geriatric patients. Further long-term studies with a larger cohort of patients are required.
858
RF198: How to avoid dural tear in UBE surgery? The "no Kerrison punch" decompression technique
Jwo-Luen Pao 1
1 Department of Orthopedic Surgery, Far Eastern Memorial Hospital, New Taipei City, Taiwan
Introduction: Unilateral biportal endoscopic (UBE) spine surgery has gained a worldwide popularity and extended indications in recent years. To avoid the most frequently encountered complication, the dural tear, we propose the “no Kerrison punch” technique. Material and Methods: From July 2018 to July 2023, we have performed 921 UBE surgeries. These patients were divided into Group A comprising the first 666 patients receiving the conventional decompression technique, and Group B comprising the later 255 patients receiving the new technique. The operation notes and medical charts were reviewed to evaluate the incidence of incidental dural tear. Results: There were 27 dural tears in Group A with an overall incidence of 4.1%. The highest incidence occurred in the subgroup of revision cases (11 in 115 patients, 9.6%), followed by decompression (14 in 405 patients, 3.5%), spinal fusion (2 in 134 patients, 1.5%), and no dural tear for posterior cervical foraminotomy (12 patients). Most of the dural tears were less than 2 mm, which were treated conservatively. Only one dural tear of 6 mm was treated by direct repair under the endoscope. In contrast, there was no dural tear in Group B, which was comprised by 132 decompression, 87 spinal fusion, 26 revision, and 10 cervical cases. Conclusion: Dural tear occurs most frequently in the revision surgery and in the early learning curve. Although most of the dural tears in UBE surgeries are very small with no need for open repair, the post-operative course was prolonged due to this complication. The new “no Kerrison punch” UBE decompression technique effectively avoid the dural tear and makes the spine surgery much safer.
RFP12: Tumors
672
RF199: Clinical outcomes of total en bloc spondylectomy for previously irradiated spinal metastases
Noriaki Yokogawa 1 , Satoshi Kato 1 , Takaki Shimizu 1 , Satoshi Nagatani 1 , Masafumi Kawai 1 , Takaaki Uto 1 , Yuji Ishino 1 , Kazuhiro Nanpo 1 , Satoru Demura 1
1 Department of Orthopaedic Surgery, Kanazawa University, Kanazawa, Japan
Introduction: With the recent improvement in the prognosis of cancer patients, long-term local control of spinal metastases have become highly important. Total en bloc spondylectomy (TES) is expected not only to provide long-term local control of spinal metastases but also to prolong the prognosis of some carcinomas. Meanwhile, radiotherapy (RT) is widely used as the standard treatment for spinal metastases, and its effectiveness is indisputable. However, since the duration of its efficacy is often limited, patients with irradiated spinal metastases with potentially long-term prognoses increasingly require further treatments including TES. Perioperative complications are generally more likely to occur during spinal surgery at irradiated sites. Furthermore, TES at the irradiated sites reportedly increases local recurrence in the peridural region. Thus, there is a concern that TES for irradiated spinal metastases may not only increase postoperative complications, but also increase local recurrence with a potential effect on survival. This study aimed to compare the postoperative complications, local recurrence, and overall survival rates after TES in patients with spinal metastases with and without an RT history, after background adjustment with propensity score matching. Material and Methods: A total of 154 patients underwent total en bloc spondylectomy as spinal metastasectomy at our institution between 2005 and 2018; 142 patients were followed up and retrospectively examined for at least 2 years after surgery. Patients were divided into two groups based on having a history of RT. The postoperative complication rate, local recurrence-free survival, and overall survival were compared between the groups after background adjustment using propensity scores. Postoperative local recurrence-free survival and overall survival were determined using Kaplan–Meier curves. In addition, for all patients, independent factors associated with overall survival were detected using Cox proportional hazards model. Results: Of the 142 patients, 46 (32%) had a history of RT and 96 (68%) had no such history. Forty-two pairs of patients were selected by propensity score matching. There were no significant differences among the groups in patients and surgical characteristics. The incidence of postoperative complications was significantly higher in the group with RT history than in the group without RT history (57.1% vs. 35.7%, respectively). The group with RT history had a higher local recurrence rate than the group without RT history (2-year: 20.8% vs. 2.9%; 5-year: 24.4% vs. 6.9%). The overall postoperative survival tended to be lower in the group with RT history; however, there was no significant difference between the two groups (2-year: 64.3% vs. 66.7%; 5-year: 47.3% vs. 57.1%). The Cox proportional hazards model revealed that only the revised Tokuhashi score was a significant prognostic factor and that a history of RT and prognosis were not significantly associated. Conclusion: TES for spinal metastases in patients with RT history significantly increases the postoperative complication and local recurrence rates than in those without RT history. Although there was no significant difference in overall survival after TES between patients with and without RT history, the risk of postoperative complications and local recurrence should be fully considered when planning TES for irradiated spinal metastases.
2485
RF200: Performance assessment of four predictive scoring systems regarding perioperative morbidity following metastatic spinal surgery
Sorasek Asawathavornvanich 1 , Thamrong Lertudomphonwanit 1 , Wuttichai Sutantavibu 1 , Pongsathorn Chanplakorn 1 , Sukanya Siriyotha 2
1 Orthopedics
2 Clinical Epidemiology and Biostatistics, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Introduction: Despite advances in spinal oncology, there has been reported high perioperative complication rate in spinal metastasis surgery. Evaluation of postoperative morbidity is a key determinant of selection for surgical candidacy. Given the high rate of perioperative morbidity and paramount impact on the surgical outcomes, it is essential to evaluate scoring system capable of predicting morbidity following metastatic spinal surgery. Over the past few years, a few models have been developed in an attempt to address this issue including The spine oncology morbidity assessment score (SOMA), Metastatic spinal tumor frailty index (MSTFI), Modified 5-item frailty index (mFI-5), and New England Spinal Metastasis Score (NESMS). The purpose of this study was to evaluate the accuracy of these scores and to compare their ability to predict perioperative morbidity for patients undergoing spine metastatic surgery. Material and Methods: A retrospective cross-sectional study of patients who underwent spinal surgery for spinal metastasis from January 2007 to December 2021 were included. The inclusion criteria were the patients who had spinal metastasis and received operative treatment. The patient demographics, laboratory data, surgical data and medical comorbidities were collected. These parameters were selected given that they are component of the studied scoring systems. The postoperative complications within 30 days and 90 days were collected. Each patient was scored using the SOMA, MSTFI, mFI-5, and NESMS. The predictive ability for each score was assessed using receiver operating characteristic (ROC) analysis and calculations of the area under the curve (AUC) to evaluate predictive accuracy. Results: Two hundred forty-eight patients were included in the analysis. The average age was 57 ± 13.11 years; 52% of patients were female. The most common primary tumor origins were Lung (22.2%), breast (19.4%) and prostate (11.3%). The overall 30-day and 90-day complication rates were 19.4% and 23.8%, respectively. MFTSI and mFI-5 were significantly associated with major in-hospital complications (p < 0.001and p < 0.001, respectively) and length of stay (p = 0.002 and p < 0.05). NESMS was significantly associated with failure to rescue (p < 0.05) and prolonged length of stay (p < 0.05) but there was no significant association with major complications and morbidities (all p > 0.05). SOMA was not significantly associated with 30-day morbidity (p = 0.061). Among all patients surgically treated for metastatic spine disease, MFTSI demonstrated the highest accuracy of 30-day major (AUC 0.743; 95% CI, 0.65-0.79) and overall morbidity (AUC 0.765; 95% CI, 0.696-0.834). Furthermore, MFTSI also demonstrated the highest accuracy of 90-day major (AUC 0.772; 95% CI, 0.698-0.846) and overall morbidity (AUC 0.770; 95% CI, 0.709-0.831). Conclusion: Among the four scoring systems, MFTSI demonstrated the highest accuracy in predicting overall and major morbidity for short-term (30-day) and intermediate-term (90-day) following metastatic spinal surgery in our study population. The finding of the present study may be useful for the surgeons to select the appropriate scoring system to stratify risk of perioperative morbidity and patient counseling.
566
RF201: Anterior vertebroplasty as treatment for aggressive and symptomatic cervical hemangioma
Chao-Yuan Ge 1 , Ding-Jun Hao 1
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
Introduction: At present, there is no literature on the treatment of aggressive and symptomatic cervical hemangioma (ASCH). Material and Methods: Clinical data of patients of ASCH who underwent anterior cervical vertebroplasty in our hospital from January 2018 to January 2022 were retrospectively analyzed. A total of 20 patients (20 vertebrae) were included in this study, including 12 males and 8 females, with an average age of 48.2 ± 5.3 years. In all patients, anterior cervical incision was performed under general anesthesia, the target vertebra was identified by fluoroscopy, and the working channel was inserted under fluoroscopy guidance to slowly inject bone cement. The injection process was stopped immediately If bone cement dispersed to the posterior margin of the vertebra or bone cement leakage in the paravertebral vessels. The VAS scores and NDI index of patients were compared before and 24 hours after surgery, 3 months, 6 months, 12 months after surgery and at the last follow-up, to evaluate the therapeutic effect. And the amount of intraoperative bone cement injection, diffusion and leakage of bone cement were also recorded. Results: All of the 20 patients with ASCH underwent surgery successfully, including 4 cases of C3, 6 cases of C4, 7 cases of C5 and 3 cases of C6. The average injection volume of bone cement was 2.8 ± 0.6 ml, and the average follow-up was 42.5 ± 5.6 months. The VAS scores of patients before surgery, 24 hours after surgery, 3 months, 6 months, 12 months and the last follow-up were (8.2 ± 1.2), (4.3 ± 0.7), (3.7 ± 0.6), (2.2 ± 0.6), (1.8 ± 0.2) and (1.0 ± 0.3), respectively, and the NDI index was (62.5 ± 5.8) %, (15.8 ± 2.2) %, (13.2 ± 3.1) %, (10.2 ± 2.2) % and (8.7 ± 1.8) %, respectively. The VAS score and NDI index were significantly improved after surgery and follow-up period compared with that before surgery (p < 0.05). Intraoperative bone cement was observed to spread to both sides of the injured vertebra, and no bone cement leakage occurred. Conclusion: Anterior vertebroplasty is a safe and effective surgical method for patients with ASCH.
963
RF202: Pediatric spinal tumours and mimics - An institutional case series
Chandan Mohanty 1 , Chandrashekhar Deopujari 1 , Uday Andar 2
1 Neurosurgery, Bombay Hospital & Wadia Children's Hospital, Mumbai, India
2 Neurosurgery, Wadia Children's Hospital, Mumbai, India
Introduction: Pediatric spinal tumours are an uncommon disease comprise 0.5-1% of all central nervous system tumours. Pediatric primary spinal osseous tumours constitute only 0.5% of spinal and spinal cord tumours. The tumours can be benign and can also be frankly malignant and the treatment needs to be tailored as per the patient since clear guidelines in management of these tumours are lacking. Material and Methods: An institutional retrospective review of all patients, from the year 2015 to 2022, aged under 18 years, undergoing surgery for spinal tumours was performed. Clinical, radiological, and histopathological features of all the patients and their management and overall outcome were analysed and our data was compared with the pertinent literature. Results: A total of 32 patients were identified who met the inclusion criteria. A total of 33 tumours were identified (one child had a concomitant benign and malignant tumour). The youngest child identified with a spinal tumour (intramedullary) was 2 days old. Out of the 33 tumours, 19 tumours were malignant and 14 tumours were benign. All patients underwent surgery for tumour excision. Intraoperative monitoring was used in 20 patients. Seven out of 32 patients required spinal instrumentation in addition to tumour excision due to the associated deformity or instability. A wide variety of surgical strategies were employed based on the clinical and radiological features. Our analysis also revealed 5 tumour mimics which was correctly identified with additional radiological imaging, percutaneous biopsy and open surgical biopsy. Multi-disciplinary tumour boards were especially useful in children less than 3-5 years of age. Conclusion: We report one of the largest series of pediatric spinal tumours in the last 15 years. We also encountered tumor mimics in approximately 13% of cases and discussed the nuances in the correct identification and management of the same. Multi-disciplinary boards were useful to minimize surgical morbidity and helped in the management of malignant spinal tumours in infants and toddlers where the use of radiotherapy is limited.
1265
RF203: Evaluation of computed tomography artefacts of carbon-fiber and titanium implants in patients with spinal oligometastatic disease undergoing stereotactic ablative radiotherapy
Zeger Rijs 1 , Khandkar Kawsar 2 , Priyanshu Saha 3 , Michiel van de Sande 1 , Darren Lui 4
1 Department of Orthopedic Surgery, Leiden University Medical Center, Leiden, The Netherlands
2 Department of Neurosurgery, Queen Elizabeth Hospital, Birmingham, United Kingdom
3 School of Medicine, St George's University of London, London, United Kingdom
4 Department of Orthopedic and Spinal Surgery,St George's University Hospitals NHS Foundation Trust, London, United Kingdom
Introduction: A possible improvement for spinal oligometastatic disease treatment with stereotactic ablative body radiotherapy (SBRT) is to change traditional titanium (or other metallic) implants to innovative carbon-fiber (CF) implants. CF materials have good biocompatibility, chemical stability, good mechanical properties, and a modulus of elasticity which is like human bone and theoretically leads to better bone quality. CF implants could improve SBRT planning and lead to more accurate delivery of the calculated dose compared to traditional implants. Several CF spine implants have shown promising results with regards to reducing artefacts, better radiation planning, and potentially greater safety and quality of radiotherapy. Material and Methods: This retrospective observational study evaluated artefacts on computed tomography (CT) images using Hounsfield units (HU) in patients with spinal oligometastatic disease that received carbon-fiber or titanium spine implants and underwent post operative SBRT. Pre- and postoperative HU were measured at the vertebral body, pedicle, and spinal cord at three different levels: the lower instrumented vertebra, the level of metastatic spinal cord compression, and an uninvolved level. Areas measured at each level were delicately matched pre- and postoperatively. Results: In total, 22 patients were included. Six males and five females (n = 11) were included in the CF implant group, with a mean age of 54 years (range 20 - 70 years). The titanium group consisted of five males and six females (n = 11), with a mean age of 56 years (range 36 - 66 years). Significant differences in HU were observed at the vertebral body, the pedicle, and the spinal cord at the lowest instrumented vertebra level for both CF and titanium (average increase 1.54-fold and 5.11-fold respectively). At the metastatic spinal cord compression level, a trend towards a higher HU-increase was observed in titanium compared with CF (average increase 2.51-fold and 1.43-fold respectively). The relatively high postoperative HU-increase after insertion of titanium implants indicated CT artefacts, while the relatively low HU-increase of CF implants was not associated with artefacts. In general, no screws are inserted at this level, which means the HU-increase comes from the scatter of a cage or rods posteriorly. As expected, no postoperative HU-increase was observed at the uninvolved level for both CF and titanium. Based on our observations, the HU-increase indicates an increase in CT artefacts. Conclusion: This study utilized a quantitative technique to compare pre- and postoperative CT artifacts produced by CF and titanium implants in patients with spinal oligometastatic disease undergoing stereotactic ablative radiotherapy (SABR). A greater increase in Hounsfield units (HU) was observed in the group treated with titanium spine implants than in the group treated with CF spine implants. This relatively high postoperative HU-increase after insertion of titanium implants indicated CT artefacts, while the relatively low HU-increase of CF implants was not associated with artefacts. Therefore, we propose a CT artefact grading system based on postoperative HU-increase. This could be used in future studies to assess if less CT artefacts lead to better tumoricidal effects and decreased adverse effects after SBRT.
1398
RF204: Predicting bone metastasis risk in patients with lung cancer: a pilot study
Wang Leong So 1
1 Department of Orthopaedic and Traumatology, The University of Hong Kong, Hong Kong
Introduction: Bone is the most frequent site of metastasis [1], and bone metastasis (BM) is a leading cause of mortality in lung cancer (LC) patient, one of the commonest cancers in Hong Kong and worldwide [2, 3]. Identifying LC patients at high risk of BM is crucial for effective prevention and surveillance. This retrospective study aimed at constructing a Machine learning (ML) model to predict risk of BM in LC patients. Materials and Methods: Patients diagnosed with LC in 2021 were included in the study. A total of 25 demographic, clinical, pathological, surgical, and non-surgical treatment based variables obtained at diagnosis and during follow-up were used to construct ML-based models with the primary outcome being BM. Pathological variables encompassed histopathological type, resection margin, lympho-vascular invasion, T staging, differentiation grade, and AJCC cancer staging. Treatment based variables were defined as any treatment modalities for primary lung cancer, including lobectomy, wedge resection, chemotherapy, radiotherapy, targeted therapy, and immunotherapy. BM detection utilized various imaging methods, such as Bone scan, X-ray, MRI, CT, or PET-CT. All patients’ data were obtained from discharge summary, clinician coding of diagnosis and procedures codes, pathology reports and radiology results. Nine different ML classifiers, including logistic regression, linear support vector machines (SVM), radial basis function kernel SVM, random forest, decision tree, gradient boosting, k-nearest neighbour, linear discriminant analysis, and multilayer perceptron with backpropagation, were compared. Due to the rarity of BM events, three techniques for handling imbalanced data – Synthetic Minority Oversampling Technique, Adaptive Synthetic Sampling Approach, and class weight assignment – were employed. A total of 23 ML-based models were compared. The best model was selected according to accuracy, sensitivity, and specificity. The Shapley additive explanations (SHAP) framework was utilized to interpret the rationale behind the best-performing model. Results: 340 LC patients, among which 37 of them developed BM during follow up, were included in the study. 15 patients (40%) developed more than two sites of BM (most commonly spine). The best ML-based risk prediction model was logistic regression with class weight assignment, which achieved a sensitivity, specificity, and accuracy of 0.86, 0.90, and 0.90. SHAP showed the top five positive predictors of BM are advanced AJCC cancer staging (Stage III and IV), poor differentiation grade, the use of chemotherapy or radiotherapy for primary lung tumor, and not having surgical resection of primary lung tumor. Conclusion: These findings suggest that ML-based models could be useful to stratify LC patients according to their risk of BM using basic patient variables which are available from a standard tertiary hospital. Risk of BM is higher in patients who received surgical resection of lung tumor than in patients treated with chemotherapy or radiotherapy alone. Both poor differentiation grade and stage III or IV LC are also highly predictive of BM. Clinicians should be alert to the risk of BM if above risk factors are found in LC patients. ML-based model can be used to determine the necessity of further radiological investigations or therapeutic interventions for early identification or prevention of BM.
References
1. Wu S, Pan Y, Mao Y, Chen Y, He Y. Current progress and mechanisms of bone metastasis in lung cancer: a narrative review. Transl Lung Cancer Res 2021; 10(1): 439-51.
2. Thandra KC, Barsouk A, Saginala K, Aluru JS, Barsouk A. Epidemiology of lung cancer. Contemp Oncol (Pozn) 2021; 25(1): 45-52.
3. Tse LA, Wang F, Wong MC, Au JS, Yu IT. Risk assessment and prediction for lung cancer among Hong Kong Chinese men. BMC Cancer 2022; 22(1): 585.
1238
RF205: Unlocking success: a single-center retrospective analysis comparing laminoplasty, laminectomy, and laminotomy for microsurgical resection of intradural, extramedullary spinal tumors
Felix Stengel 1 , Martin Stienen 1 , Oliver Bozinov 1 , Nader Hejrati 1
1 Department of Neurosurgery, Cantonal Hospital St.Gallen & Medical School of St.Gallen, St. Gallen, Switzerland
Introduction: Intradural, extramedullary spine tumors are usually benign lesions that may become symptomatic with myelopathy and/or radiculopathy due to neurocompression. The choice of surgical approach - laminotomy, laminectomy or laminoplasty - has been poorly studied. However, the choice of the approach is crucial to achieve complete resection under the premise of optimal functional outcome. Our study assesses functional outcomes and cerebrospinal fluid (CSF) leakage risk based on surgical approach, considering spinal segment, tumor type, and size. Material and Methods: In an IRB-approved retrospective cohort study, we included consecutive patients who underwent microsurgical resection of intradural, extramedullary spinal tumors at our center from 2012 to 2023. Excluded were patients with intraspinal metastases, non-neoplastic conditions, or intramedullary tumors. Data management utilized REDCap, and statistical analysis was conducted using STATA (significance level: p < 0.05). Primary outcomes assessed neurological status via the McCormick scale and surgical results via the McNab scale at discharge and 90 days post-surgery. Additional analysis encompassed demographic, radiological, tumor entity, surgical technique, and complication data. Results: Among 99 patients (mean age: 57 years, female:male ratio 64:35), 90% underwent planned surgery, 10% as emergencies. Most patients (72%) had symptoms for over 90 days before diagnosis; common symptoms included radiculopathy (44%), sensory deficits (43%), motor deficits (35%), ataxia (34%), spasticity (8%), and caudal symptoms (5%). Eight percent were asymptomatic. Tumors were frequently thoracic (40%), lumbar (32%), cervical (18%), or junctional (9%). The extent of the lesions and resections were two levels (55%), followed by one level (29%) and three levels (13%), with a median tumor volume of 3.8 ml and with spinal cord/cauda compression in 78%. Surgical approaches were laminoplasty (42%), laminectomy (39%), hemilaminectomy (12%), and laminotomy (9%), without instrumentation or corpectomy. Common histologies were meningioma (39%), schwannoma (35%), and ependymoma (12%). Neurological status improved significantly at discharge (mean: -0.18, p = 0.0039, SD 0.61) and 90 days (mean: -0.54, p < 0.0001, SD 0.75, missing: n = 2) per the McCormick scale. Surgical outcomes per the McNab scale were good/excellent in 85% at discharge and poor/very poor in 2%. At 90 days, 92% had good/excellent outcomes, 2% poor/very poor (change in time: mean: -0.46, p < 0.0001, SD 0.07, missing n = 2). Six patients had CSF leakage within 90 days, one requiring re-operation. Other complications that did not require invasive treatment included new sensory deficits (n = 5), motor deficits (n = 2), radiculopathy (n = 1), and superficial wound infection (n = 2). Multivariate analysis found tumor volume, histology, and extent of surgery had no influence on McCormick, McNab scores, or CSF leakage. Surgical approach (hemilaminectomy, laminectomy, laminoplasty, laminotomy) also showed no significant impact by ordered logistic regression on postoperative outcomes (McCormick, McNab, CSF leak) based on the level of surgery. Conclusion: In this single-center series, microsurgical resection significantly improved the patient’s neurological status, with 85% achieving good or excellent results at discharge and 92% at 90 days follow-up with a reasonably low complication rate. The surgical approach was not significantly associated with functional/neurological outcome or complications in this cohort. A future multicenter study would be needed to provide sufficient power for a more in-depth analysis.
190
RF206: Longitudinal changes in outcomes of transcranial motor evoked potential monitoring during intra- and extra medullary spinal cord tumor surgeries
Hiroki Ushirozako 1,2 , Go Yoshida 1 , Kenta Kurosu 1 , Hiroaki Nakashima 3 , Naoki Segi 3 , Muneharu Ando 4 , Shinichirou Taniguchi 4 , Shigenori Kawabata 5 , Jun Hashimoto 5 , Kei Yamada 6 , Shinji Morito 6 , Tsukasa Kanchiku 7 , Yasushi Fujiwara 8 , Hiroshi Iwasaki 9 , Hideki Shigematsu 10 , Nobuaki Tadokoro 11 , Masahito Takahashi 12 , Kanichiro Wada 13 , Naoya Yamamoto 14 , Masahiro Funaba 15 , Akimasa Yasuda 16 , Tsunenori Takatani 17 , Kazuyoshi Kobayashi 18 , Kazuyoshi Nakanishi 19 , Shiro Imagama 3 , Yukihiro Matsuyama 1
1 Department of Orthopaedic Surgery, Hamamatsu University School of Medicine, Hamamatsu, Japan
2 Department of Orthopaedic Surgery, Morimachi Public Hospital, Mori, Japan
3 Department of Orthopaedic Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan
4 Department of Orthopaedic Surgery, Kansai Medical University, Osaka, Japan
5 Department of Orthopaedic Surgery, Tokyo Medical and Dental University, Tokyo, Japan
6 Department of Orthopaedic Surgery, Kurume University School of Medicine, Kurume, Japan
7 Department of Orthopaedic Surgery, Yamaguchi Rosai Hospital, Yamaguchi, Japan
8 Department of Orthopaedic Surgery, Hiroshima City North Medical Center Asa Citizens Hospital, Hiroshima, Japan
9 Department of Orthopaedic Surgery, Wakayama Medical University, Wakayama, Japan
10 Department of Orthopaedic Surgery, Nara Medical University, Nara, Japan
11 Department of Orthopaedic Surgery, Kochi University, Kochi, Japan
12 Department of Orthopaedic Surgery, Kyorin University, Tokyo, Japan
13 Hirosaki University Graduate School of Medicine, Hirosaki, Japan
14 Department of Orthopaedic Surgery, Tokyo Women's Medical University Medical Center East, Tokyo, Japan
15 Department of Orthopaedic Surgery, Yamaguchi University, Yamaguchi, Japan
16 Department of Orthopaedic Surgery, National Defense Medical College Hospital, Saitama, Japan
17 Division of Central Clinical Laboratory, Nara Medical University, Nara, Japan
18 Department of Orthopaedic Surgery, Nagoya Red Cross Hospital, Nagoya, Japan
19 Department of Orthopaedic Surgery, Nihon Universit, Tokyo, Japan
Introduction: The use of transcranial motor evoked potential (Tc-MEP) has been recognized as an indispensable tool in high-risk spine surgeries, particularly in cases involving spinal tumors, ossification of the posterior longitudinal ligament, and spinal deformities. These surgeries have an increased likelihood of intraoperative spinal cord and nerve root injuries. Given the significance of Tc-MEP in mitigating these risks, this research undertakes a comprehensive analysis of the annual changes in the precision of Tc-MEP monitoring, the incidence of postoperative paralysis, and the success rate of rescue interventions during surgeries for intramedullary spinal cord tumors (IMSCT) and extramedullary spinal cord tumors (EMSCT). Material and Methods: We examined data spanning five years, from 2017-2022, covering 163 IMSCT patients (92 male, 71 female, average age 48, BMI 23.2) and 754 EMSCT patients (325 male, 429 female, average age 58, BMI 23.2). These patients were treated in 17 prominent domestic institutions, all affiliated with the Monitoring Committee of the Japanese Society for Spine Surgery and Related Research. We established an alarm threshold when the Tc-MEP waveform in one or more limbs exhibited a decrease of 70% or more from the baseline. A postoperative disability was determined as a one-grade decline in muscle strength immediately after the procedure. From 2010, the committee convened regular meetings to assess and enhance waveform judgment protocols, with a focus on evaluating true-positive and rescue cases. The rescue case was defined as a patient with recovered TcMEP amplitudes after certain procedures and without a de novo paralysis. We assessed the Tc-MEP monitoring results, postoperative incidence of a de novo paralysis, and the rescue rate (number of rescue cases / number of true-positive + rescue cases). Results: For IMSCT resection surgeries, Tc-MEP monitoring results were: Sensitivity/Specificity/Positive predictive value/Negative predictive value: 95%/83%/75%/97% (2017-18, n = 58), 89%/73%/42%/97% (2019-20, n = 52), and 64%/67%/35%/87% (2021-22, n = 53). Postoperative paralysis incidence/rescue cases/rescue rate were: 33%/3 cases/14% (2017-18), 17%/2 cases/20% (2019-20), and 21%/2 cases/22% (2021-22), indicating a gradual decline in postoperative paralysis over the years. For EMSCT resection surgeries, Tc-MEP monitoring results were: Sensitivity/Specificity/Positive predictive value/Negative predictive value: 88%/91%/47%/99% (2017-18, n = 205), 87%/85%/27%/99% (2019-20, n = 261), and 67%/93%/37%/98% (2021-22, n = 288). Postoperative paralysis incidence/rescue cases/rescue rate were: 8%/7 cases/33% (2017-18), 6%/15 cases/54% (2019-20), and 5%/11 cases/52% (2021-22), showcasing an annual increase in the rescue rate and a decline in the incidence of postoperative paralysis. Conclusion: The study underscores the importance of proactive interventions and accurate judgments concerning Tc-MEP waveform alterations. By adopting a rigorous and standardized approach across multiple institutions, we've seen not just an uptick in the success of rescue procedures but also a substantial reduction in incidences of postoperative paralysis. This inter-institutional collaboration and commitment to refining practices have yielded encouraging results in safeguarding patient well-being during high-risk spinal surgeries.
620
RF207: Malnutrition in spine oncology: where are we and what are we measuring?
Rafael De la Garza Ramos 1 , Raphaële Charest-Morin 2 , C. Rory Goodwin 3 , Scott Lawrence Zuckerman 4 , Ilya Laufer 5 , Nicolas Dea 2 , Arjun Sahgal 6 , Laurence Rhines 7 , Ziya Gokaslan 8 , Chetan Bettegowda 9 , Anne Versteeg 10 , Hanbo Chen 6 , Cordula Netzer 11 , Daniel Sciubba 12 , John O'Toole 13 , Michael Fehlings 14 , Naresh Kumar 15 , Disch Alexander C. 16 , Byron Stephens 17 , Tony Goldschlager 18 , Michael Weber 19 , John Shin 20
1 Neurosurgery, Brown University, Providence, USA
2 Orthopedic Surgery, Combined Neurosurgical and Orthopedic Spine Program, Vancouver, Canada
3 Neurosurgery, Duke University, Durham, USA
4 Neurosurgery
5 Neurosurgery, NYU, New York, USA
6 Radiation Oncology, Sunnybrook Health Sciences Centre, Toronto, Canada
7 Neurosurgery, The University of Texas MD Anderson Cancer Center, Houston, USA
8 Neurosurgery, Brown University, Providence, USA
9 Neurosurgery, Johns Hopkins University, Baltimora, USA
10 Orthopedics, University of Toronto, Canada
11 Spine Surgery, University Hospital of Basel, Switzerland
12 Neurosurgery, Northwell Health, USA
13 Neurosurgery, Rush University Medical Center, Chicago, USA
14 Neurosurgery, University of Toronto, Canada
15 Orthopedic Surgery, National University Health System, Singapore
16 Orthopedic Surgery, University Hospital Carl Gustav Carus, Dresden, Germany
17 Orthopedic Surgery, Vanderbilt, USA
18 Neurosurgery, Monash Health, Australia
19 Surgery, Montreal General Hospital, Canada
20 Neurosurgery, Massachusetts General Hospital, Boston, USA
Introduction: Malnutrition is common in cancer patients. Patients with metastatic spine disease represent a unique and challenging sub-population of cancer patients given the predisposition to back pain, limited mobility, neurological deficits, and overall lower activity levels. The real prevalence of malnutrition in this population is unknown but has been reported to be as high as 90%. While studies have found significant associations between a malnourished state and higher risk of complications and decreased survival, there remains a need for a consensus agreement on how best to define this condition in this population and how it uniquely affects metastatic spine tumor patients. The purpose of this scoping review was to: 1) Identify which markers are most used as surrogates for malnutrition in metastatic spine disease, and 2) describe the most studied outcomes associated with poor nutritional intake. Material and Methods: A scoping review was performed by searching the PubMed/Medline, EMBASE, and Web of Science databases up to July 2022. We searched for articles exploring markers of malnutrition in spine oncology patients including but not limited to albumin, body weight, weight loss, nutrition indices, and others. A narrative synthesis was performed. Results: A total of 61 articles reporting on 31,385 patients met inclusion criteria. There were 13 different surrogate markers of nutrition, with the most common being albumin in 67% of studies (n = 41), body weight/BMI in 34% (n = 19), and muscle mass in 28% (n = 17). Among the 13 surrogate markers, there were two biochemical markers, two anthropometric measurements, two measures of body composition assessed by imaging, five nutrition indices, one study examining preoperative nutrition consults, and one study examining “malnutrition” (including nutritional marasmus and severe protein-calorie malnutrition). The most common studied outcomes were survival in 82% (n = 50), complications in 28% (n = 17), and length of stay in 10% (n = 6). Quality of life outcome measures and functional outcome were assessed in 2% (n = 1) and 3% (n = 2) of studies, respectively. Out of 61 studies, 18% (n = 11) found no association between the examined markers and outcome. Conclusion: Assessment of nutritional status in patients with spinal metastases is of paramount importance. However, there is lack of a comprehensive and consistent way of assessing malnutrition in oncologic spine patients and therefore inconsistency in its relationship with outcomes. A consensus agreement on the assessment and definition of malnutrition in spine tumor patients is needed.
1117
RF208: Spinal chordoma and chondrosarcoma treatment experiences: a 22-year retrospective study from databases of two medical centers in Taiwan
Pin-Lin Kuo 1 , Yu-Cheng Yeh 1 , Fon-Yih Tsuang 2 , Po-Liang Lai 1
1 Department of Orthopedic Surgery, Chang Gung Memorial Hospital Linkou, Taoyuan City, Taiwan
2 Division of Neurosurgery, Department of Surgery, National Taiwan University Hospital, Taipei City, Taiwan
Introduction: Low-grade primary spinal malignancies such as chordoma and chondrosarcoma are generally resistant to conventional radiotherapy (RT) or chemotherapy. Although wide-margin en bloc resection of the tumor is considered the appropriate treatment based on the Enneking classification, the extent of surgical resection sometimes has to be weighed against survivorship and long-term comorbidities. The purpose of this study is to review the disease prognosis and outcomes of patients with primary low-grade spinal malignancies, specifically chordoma and chondrosarcoma, treated in two medical centers in Taiwan. Material and Methods: Patients with spinal chordoma and chondrosarcoma treated in two medical centers in Taiwan were retrospectively reviewed from 2001 to 2022. Patients presenting with recurrent tumors or distant metastases at the time of the initial visit were excluded. Overall survival (OS) and progression-free survival (PFS) were compared between patients who received wide-margin/marginal-margin (R0/R1) resection and those who underwent intralesional (R2) resection. Subgroup analyses were conducted to evaluate the impact of adjuvant RT. Patients who received only RT without operative treatment were also compared to the R0/R1 and R2 groups. The Kaplan-Meier Method and log-rank tests were used for statistical analysis. A p value < 0.05 was considered statistically significant. Results: A total of 48 patients (34 males, 14 females) were enrolled. Of these, 15 were in the R0/R1 group, 28 in the R2 group, and 5 in the RT-only group. The mean follow-up length was 4.8 ± 3.7 years; the cohort included 39 chordomas and 9 chondrosarcomas. Tumor locations were as follows: cervical: 3, thoracic: 5, lumbar: 4, and sacrum: 36. The R0/R1 group had significantly higher OS (12.1 vs. 6.8 years, p = 0.031) and PFS (9.1 vs. 2.2 years, p < 0.001) than the R2 group. In subgroup analyses, OS and PFS were comparable, whether adjuvant RT was added or not, in both the R0/R1 and R2 groups. When the RT-only group was compared to the R0/R1 and R2 groups, its OS was similar to that of the R2 group (6.3 vs. 12.1 vs. 6.8 years, p = 0.091). However, the RT-only group had significantly better PFS than the R2 group (6.1 vs. 9.1 vs. 2.2 years, p = 0.001). Conclusion: The resection margin is the most critical indicator for the prognosis of spinal chordoma and chondrosarcoma. Wide-margin or marginal-margin en bloc resection significantly improves overall survival and progression-free survival compared to intralesional resection. Radiotherapy alone may be considered an alternative if en bloc resection is unachievable.
1135
RF209: A comparative study of different prosthesis for reconstruction after total spondylectomy of upper cervical tumors
Feng Li 1
1 Orthopedics, Tongji Hospital of Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
Introduction: Although upper cervical tumor is rare, total spondylectomy is recommended for most primary invasive, malignant or solitary metastatic tumors to reduce local recurrence. However, due to the local anatomy, biomechanical reconstruction after spondylectomy is technically challenging. Currently, various reconstruction methods are applied without consensus. This study aims to evaluate the clinical efficacy of 3D-printed artificial prosthesis and atypical titanium mesh for reconstruction after total spondylectomy of upper cervical tumors. Material and Methods: A retrospective analysis was conducted on 25 patients who underwent total spondylectomy of upper cervical tumors in Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology from March 2015 to March 2022, and they were divided into two groups:9 patients with 3D printed artificial prosthesis in group 1 and 16 patients with atypical titanium mesh in group 2.In group 1, through the patient's 3D-Space MRI and CT data modeling, the 3-Matic software was imported for prosthesis design, adjustment, and finally printed out using a 3D printer. The atypical titanium mesh was manufactured by the surgeon with unique anchoring structure from route mesh. All patients underwent one-stage total spondylectomy by combined anterior-posterior approach,while anterior reconstruction was gained by 3D printed prosthesis or atypical titanium mesh. The clinical outcome was evaluated by Visual analog scale (VAS) and neurological function score (JOA). And the length of hospital stays, operation time, and intraoperative blood loss were also recorded and compared between the two groups. Perioperative complications, such as dysphagia and hardware failure were recorded. Results: The mean followed-up duration was 19.4 months. Postoperative pain disappeared or relieved in all patients, including 18 patients with complete relief of pain and 7 patients with obvious relief of pain. The VAS score significantly decreased from 7.5 ± 2.2 pre-operation to1.8 ± 0.6 post-operation (p < 0.05). Neurological function was improved in all patients, with JOA scores statistically increase from 12.4 ± 1.7 to 16.1 ± 1.2 statistically (p < 0.05). Between the 2 groups, length of hospital stay, operation time and intraoperative blood loss in group 1 were less than those in group 2 significantly. The JOA improvement rate in group 1 were higher than that in group 2 at last follow-up with significant differences (p < 0.05). There was no hardware failure in either group at last follow-up. Additionally, the incidence of dysphagia in group 1 (11.1%) was lower than in group 2 (25.0%). Conclusion: Two types of prostheses, the 3D-printed artificial prostheses and atypical titanium mesh, both are effective methods for reconstruction after total spondylectomy for upper cervical tumors, can significantly relieve pain and improve neurological symptoms. However, compared to the atypical titanium mesh, 3D printed artificial prostheses can reduce operation time, reduce intraoperative blood loss and promote the recovery of neurological function with minor complications.
1084
RF210: Carbon-fiber reinforced PEEK instrumentation in the spinal metastasis: a retrospective series of 92 patients
Maximilian-Niklas Bonk 1 , Krauss Philipp 1
1 Department for Neurosurgery, University Hospital Augsburg, Augsburg, Germany
Background: This study examines the efficacy and safety of Carbon-PEEK stabilization for the treatment of spinal metastases. Methods: A retrospective single center analysis of all Patients following spinal instrumentation with carbon fiber-reinforced PEEK instrumentation between January 2021 and December 2022 was done. SIN-Score, ASIA Motor Score and Karnofsky Performance Index were evaluation with a minimal follow up of 12 months Results: 92 Patients (56 males, 36 females) with an average age of 67 years were identified. The most common primary tumors were Bronchial-Ca (23%), Plasmacytoma (23%), and Breast Cancer (13%). The average SIN-Score was 10.77. Patients were followed up for an average of 411 days. Preoperatively, 11 patients were unable to walk, reducing to only 2 postoperatively. The Karnofsky Performance Index improved by an average of 3 points. Complications occurred in 8% of cases, half of which were wound healing disturbances during radiation therapy, and the other half were operation-independent complications such as pulmonary embolism. There were no implant related complications. Conclusions: Carbon-PEEK stabilization appears to be a safe and efficient procedure for the treatment of metastatic spinal lesions.
628
RF211: Risk factors for the development of neurological deficits in metastatic spinal disease: an international, multicenter Delphi study
Eline Huele 1 , Roxanne Gal 1 , Wietse Eppinga 2 , Lenny Verkooijen 1 , John O'Toole 3 , Ilya Laufer 4 , Daniel Sciubba 5 , Cordula Netzer 6 , Wouter Foppen 7 , Arjun Sahgal 8 , Michael Fehlings 9 , Sheng-Fu Larry Lo 5 , Charles Fisher 10 , Laurence Rhines 11 , Jeremy Reynolds 12 , Aron Lazary 13 , Alessandro Gasbarrini 14 , Nicolas Dea 10 , Michael Weber 15 , Jorrit-Jan Verlaan 16
1 Division of Imaging and Oncology
2 Department of Radiotherapy, Division of Imaging and Oncology, University Medical Center Utrecht, Utrecht, The Netherlands
3 Department of Neurosurgery, Rush University Medical Center, Chicago, USA
4 Department of Neurosurgery, Division of Spinal Neurosurgery, NYU Langone Health, New York, USA
5 Department of Neurosurgery, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Great Neck, USA
6 Department of Spine Surgery, University Hospital Basel, Basel, Switzerland
7 Department of Radiology and Nuclear Medicine, Division of Imaging and Oncology, University Medical Center Utrecht, Utrecht, The Netherlands
8 Department of Radiation Oncology, Odette Cancer Centre, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Canada
9 Division of Neurosurgery and Spine Program, University of Toronto and Toronto Western Hospital, Toronto, Canada
10 Division of Spine Surgery, Vancouver General Hospital and University of British Columbia, Vancouver, Canada
11 Department of Neurosurgery, Division of Surgery,The University of Texas MD Anderson Cancer Center, Houston, USA
12 Spinal Division,Oxford University Hospital NHS Trust, Oxford, United Kingdom
13 National Center for Spinal Disorders and Buda Health Center, Budapest, Hungary
14 Department of Spine Surgery, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
15 Department of Surgery, McGill University, Montreal, Canada
16 Department of Orthopaedic Surgery, University Medical Center Utrecht, Utrecht, The Netherlands
Introduction: Timely identification of patients with metastatic spinal disease who are at increased risk of developing neurological deficits can facilitate prevention of the development and/or progression of neurological deficits, thereby greatly improving patient outcomes. However, recognizing patients at increased risk of neurological deficits, preferably before the onset of neurological deficits, is challenging. Evidence on factors that are predictive for the development of neurological deficits in metastatic spinal disease is scarce. This Delphi study was conducted to use expert knowledge and opinion to identify factors perceived (or thought) to be associated with the development and/or progression of neurological deficits in patients with metastatic spinal disease. Material and Methods: A three-round Delphi study was conducted between January-May 2023 including AO Spine members, comprising mainly neurosurgeons and orthopedic surgeons. In round 1, participants listed radiological factors, patient characteristics, tumor characteristics, previous cancer-related treatment factors and additional factors. In round 2, participants ranked the factors on importance per category and selected a top 9 from all factors. Kendall’s W coefficient of concordance was calculated as a measure of consensus. In the final round, participants provided feedback on the top-half rankings resulting from round 2. Lastly, the highest-ranking factors were more clearly defined and operationalized by an expert panel. Results: Over two hundred physicians and researchers participated in each round. The factors listed in the first round were collapsed into 12 radiological factors, 14 patient characteristics, 6 tumor characteristics and 12 previous cancer-related treatment factors. High agreement was found in round 3 on the top-half lists in each category and the overall top 9, originating from round 2. Kendall’s W indicated strong agreement between the participants. ‘Epidural spinal cord compression’, ‘aggressive tumor behavior’ and ‘mechanical instability’ were deemed most influential for the development of neurological deficits in patients with metastatic spinal disease. Conclusion: This Delphi study provides a comprehensive and widely supported list of factors that may be related to the development and/or progression of neurological deficits in patients with metastatic spinal disease. This list can serve as a basis for future directions in prognostication research.
1636
RF212: Review on racial disparities in the reporting and recruitment for clinical trials involving metastatic spinal tumors
Anne Schlumprecht 1,2 , Rafael De la Garza Ramos 1 , Jessica Ryvlin 1 , Mousa Hamad 1 , Lucas Dziesinski 1 , Mitchell Fourman 2 , Yaroslav Gelfand 1 , Saikiran Murthy 1 , Reza Yassari 1
1 Department of Neurological Surgery
2 Department of Orthopaedic Surgery, Montefiore Medical Center, New York City, USA
Introduction: Total en bloc spondylectomy (TES) poses unique biomechanical challenges when attempting to reconstruct the spinal column. In the lumbar spine, this is even more challenging given the unique anatomy of this region and the high rate of instrumentation failure. The purpose of our study was to conduct a systematic review of the incidence and risk factors of instrumentation failure after lumbar TES. Material and Methods: We conducted a systematic review using the PRISMA guidelines and screened for studies between April 2000 and August 2023 that reported individual patient data on lumbar spondylectomy. Our primary endpoint was instrumentation failure (IF). The data was pooled and provided an overall instrumentation failure rate. The timing of instrumentation failure and risk factors were ascertained from individual studies. Levels of evidence were also reported. Results: A total of 16 studies conducted between April 2000 and August 2023 that met our eligibility criteria were included in our study, with a total of 153 patients undergoing lumbar TES. The mean patient age was 42 years (standard deviation 16), and the mean follow-up time was 52 months. Out of 153 patients, 129 included data on IF, with 36% (46 of 129) having metastatic tumors, 64% (82 of 129) having primary tumors, and one case (0.8%) where the origin of the tumor was unclear. The total reported failure rate was 21% (27 of 129), with 63% (17 of 27) experiencing late failure (> 12 months after surgery), 4% (1 of 27) experiencing early failure (< 12 months after surgery), and 33% (9 of 27) at an unspecified time. There was a statistically significant correlation between radiotherapy and IF (p < 0.001). The posterior surgical approach was associated with a reduced incidence of IF (p = 0.011). The use of autografts and the use of a titanium cage were significantly associated with a greater incidence of IF (p < 0.001 and p < 0.001, respectively). Instrumentation failure was not correlated with age (p = 0.686), gender (p = 0.739) or multilevel surgery (p = 0.963). Conclusion: Our data indicates that the posterior approach in patients with TES is associated with a lower incidence of instrumentation failure, whereas identified risk factors for instrumentation failure were autografts, titanium cages, and radiotherapy. In regards to the high rate of IF, continued research on more robust construction designs is needed.
109
RF213: Utility of surgical invasiveness score for assessing operative course and early post-operative outcome in spinal en bloc surgery
Thomas Land 1 , Yan Woo 1 , Melvin Grainger 1 , Marcin Czyz 1
1 Neurosurgery and Spinal Surgery, Queen Elizabeth Hospital Birmingham, United Kingdom
Introduction: En bloc resection (EBR) is a rare procedure reserved for select spinal tumours. Necessary expanded surgical approaches allow for specimen removal with intact margins optimising oncological results however, high morbidity is often the trade off for these benefits and complications are frequent. EBR procedures are lengthy and may need to be performed in stages, hence judicious bespoke surgical planning and patient counseling is required. Standard surgical factors such as tumour size, number of spinal levels, approach and reconstruction technique influence operative course. We use a spinal surgical invasiveness score (SSIS), previously described by Mirza et al, to summate and apply these factors against early surgical outcomes and complications. Material and Methods: We present a case series of all en bloc procedures performed in our unit between January 2019 and August 2022. Retrospective search of our database for all “en bloc” spinal tumour procedures over this 3.5 year period was conducted with subsequent review of the case notes and imaging of the 30 patients identified. Subgroup analysis based on SSIS was completed. Low invasiveness grade (LIG; SSIS ≤ 20) and high invasiveness grade (HIG; SSIS > 20) groups were compared for complication rate and severity, deterioration in Eastern co-operative group oncology grade (ECOG) performance status, operative time, length of intensive care (ITU) stay and total length of admission. Results: 30 EBR procedures were identified. Pathologies included 23 primary bone tumours and 7 metastases. Our total moderate-severe complication rate, i.e. life threatening or requiring invasive intervention, was 20% (LIG and HIG groups 14% and 25% respectively demonstrated no significant difference). Difference in median deterioration in ECOG score of 1 for the LIG group and 2 for the HIG group was significant (p = 0.01). Difference in mean ITU stay of 2.6 days vs 7.9 days for LIG and HIG groups respectively demonstrated statistical significance (p = 0.002) as did difference in mean total length of stay for LIG group, 16.3 days, and HIG group, 35.7 days (p = 0.04). Mean operative time for LIG group was 451 minutes and for HIG group was 712 minutes showing significant difference (p < 0.001). Marked correlation was seen between SSIS and operative length Rs = 0.76 (p = 0.001). Conclusion: Our rates of complication are similar to published literature. Although SSIS is not specific for en bloc surgery it does have utility in assessing complexity of surgery, showing strong correlation with operative length as expected and a relationship with post op performance status, ITU requirement and length of stay. SISS can be added as a tool for operative planning of en bloc spinal surgery but other simple to calculate variables such as tumour volume and surgical approach may be of similar efficacy.
2256
RF214: Results of a biphasic calcium phosphate bone graft with submicron-sized needle-shaped surface topography as standalone alternative to autograft are favorable in a prospective, multi-center, randomized, intra-patient controlled trial
Moyo Kruyt 1 , Diyar Delawi 2 , Eric Hoebink 3 , Diederik Kempen 4 , Job van Susante 5 , Katherine Sage 6
1 UMC Utrecht, The Netherlands
2 Antonius Ziekenhuis, The Netherlands
3 Amphia Ziekenhuis, The Netherlands
4 OLVG, Amsterdam, Thr Netherlands
5 Rijnstate, The Netherlands
6 Kuros
Introduction: Pseudoarthrosis after spinal fusion is an important complication leading to an estimated 92,000 revision spine surgeries in the USA each year. Iliac Crest Bone Graft is considered the gold standard, but with limited availability and an extra procedure for harvesting, spine surgeons often utilize alternatives. We initiated a large multicenter trial to determine non-inferiority of a submicron-sized needle-shaped surface biphasic calcium phosphate (BCP < µm) as compared to autograft in instrumented posterolateral spinal fusion. For registration purposes we analyzed the safety and fusion rate in the first 50 patients. Material and Methods: Adult patients indicated for instrumented posterolateral spinal fusion of one to six levels from T10-S2 were enrolled at five participating centers. After instrumentation and preparation of the bone bed, the randomized allocation side of the graft type was disclosed. One side was grafted with 10 cc of autograft per level containing a minimum of 50% iliac crest bone. The other side was grafted with 10 cc of BCP < µm granules standalone (without autograft or bone marrow aspirate). In total, 71 levels were treated (average 1.4 per patient). Prospective follow-up included adverse events, the Oswestry Disability Index (ODI), and a fine-cut (< 1 mm) Computerized Tomography (CT) at one year. Fusion was systematically scored as fused or not fused per level per side by two spine surgeons blinded for the procedure. Disagreements were resolved by panel discussion Results: The inclusion period spanned two years and follow up of these patients is one year. Average age was 57 years old (27-79 years), with 60% female and 40% male. The diagnoses included deformity (56%), structural instability (28%), and instability from decompression (20%). The fusion rate determined by fine-cut (< 1 mm) CT for BCP < μm was 76.1% (54/71 levels), which compared favorably to the autograft fusion rate of 43.7% (31/71 levels). Fusion of the BCP < μm side was not contingent upon fusion of the autograft side, as 36.6% (26/71) of levels fused on the BCP < μm side but did not fuse on the autograft side. In contrast, 4.2% (3/71) of levels fused on the autograft side but not on the BCP < μm side. 39.4% (28/71) of levels had complete fusion of both sides, while 19.7%% (14/71) did not have fusion on either side. BCP < μm performed better than autograft in single-level fusions, achieving a 73.5% (25/34 levels) fusion rate, compared to 47.1% (16/34 levels) for autograft. In two-level fusions, the fusion rate for BCP < μm was 73.1% (19/26 levels), compared to 38.5% (10/26 levels) for autograft. Fourteen percent of patients experienced a procedure or possible device-related severe adverse event and there were four reoperations. Oswestry Disability Index (ODI) score decreased from a mean of 46.0 (±15.0) to a mean of 31.7 (±16.9), and 52.4% of patients improved with at least 15-point decrease. Conclusion: This data, aiming to determine non-inferiority of standalone BCP < μm as compared to autograft for posterior spinal fusions, is promising. Ongoing studies to increase the power of the statistics with more patients is forthcoming.
896
RF215: Does i-factor™ bone graft enhances fusion rate after anterior cervical disectomy and fusion?: propensity matched cohort study from single institution case series
Jungwoo Hur 1 , Jae-Taek Hong 1
1 Neurosurgery, Eunpyeong St. Mary's Hospital, The Catholic University of Korea, Seoul, South Korea
Introduction: The efficacy and safety of traditional anterior cervical discectomy and fusion (ACDF) surgery has improved with the introduction of new implants and compounds. i-Factor™ bone Graft (Cerapedics Inc, Westminster, Colorado, USA) is a composite bone substitute material consisting of P-15 synthetic collagen fragment adsorbed onto anorganic bone mineral suspended in an inert biocompatible hydrogel carrier. A pivotal, noninferiority, US FDA Investigational Device Exemption study demonstrated the benefits of i-Factor™ compared to local autograft bone in single-level ACDF at 1-yr postoperative. Objective of this study is to compare the fusion rate of single-level anterior cervical discectomy and fusion (ACDF) using i-Factor™ Bone Graft versus conventional demineralized bone matrix (DBM) in minimum 12-month follow-up. Material and Methods: A retrospective matched cohort study was performed at a single tertiary care hospital. ACDF surgery using stand-alone 3D-printed porous titanium cage filled with i-Factor™ was performed and followed for at least 12 month. Using propensity score matching, a cohort of cases with conventional DMB(DBX, West Chester, PA, USA) was matched 1:1 with study cohort after controlling for patient demographics to reduce bias. The clinical outcomes were evaluated using the Visual analogue scales (VAS) scores for neck and arm pain, neck disability index (NDI) scores. The radiologic results were evaluated with serial plain film and 3D-CT to assess fusion status and device-related complications Results: Eighteen patients who underwent single-level ACDF surgery using i-Factor™ were matched paired with control group according to age, sex and operation level. Mean follow-up period was 18.1 month. Mean operation time, fluoroscopic time, intraoperative blood loss, and postoperative surgical drainage were similar between the two groups. Clinical outcome was significantly improved in both groups and well maintained until final follow-up. The fusion rate of DBM group at 3, 6, 12 month postoperatively were 72.7%, 81.8% and 95.4%, respectively. All patients in i-Factor™ group achieved solid fusion at 3 month postoperatively. Subsidence rate were similar in both group and no device related complications were observed in all patients. Furthermore, there were no allergic or adverse reactions associated with i-Factor™. Conclusion: ACDF surgery using i-Factor™ demonstrated favorable clinical and radiographic outcomes compared to conventional DBM in minimum of 12-month follow-up. The final fusion rate was similar but time to achieve solid fusion might be superior with i-Factor™. However, more long-term follow-up results and more cases should be investigated to prove the superiority.
1201
RF216: Calcium-phospho-silicate ceramic augmented autograft for inter-transverse fusion in the lumbar spine - A prospective controlled study of 100 patients
K Venugopal Menon 1 , Mandar Borde 1 , Umesh Kanade P 1 , Akash Mane 1 , Sangram Rajale 1 , Tanmay Datey 1
1 Spine Surgery, Bharati Vidyapeeth Medical College Hospital, Pune, India
Introduction: Synthetic bio-degradeable ceramics have been used extensively as bone graft augmenters in general Orthopaedics and to a limited extent in the spine. The authors explore the use of local bone graft from the laminae, spinous process and facets augmented with bio-degradeable Calcium-Phospho-Silicate ceramics to achieve inter-transverse fusion in the spine. Materials and Methods: The patient cohort is 100 patients who underwent laminectomy and inter-transverse fusion for their spinal condition. All patients had degenerative disorders of the spine and infections, tumours and fractures were excluded. Only Adults were included in the study. The patients received autologous bone graft on the left inter-transverse bed (Control) and synthetic ceramic (Calcium Phospho-Silicate) mixed with local graft in a 50:50 ratio, on the right side (Test). Preparation of the graft beds were similar on both sides. The follow up protocol was 6 weeks, 3,6 and 12 months, and the outcome measures were clinical- VAS, ODI and radiological- Lenke and Bridwell score. The autograft side was compared with the ceramic side as well and the grade of fusion mass recorded. Results: Ninety-four patients had complete documents required for the evaluation. 64.9% (61) patients revealed good fusion on the ceramic side while 71.3% (67) were good on the autograft side. There were 6.4% (6 each) definite nonunions in both groups but all of them were asymptomatic. The remaining patients were classified as indeterminate in term of fusion but the clinical results were good or excellent. Radiologically, the fusion mass seemed to transition through stages of “granular”, “amorphous” and “diffuse” coinciding with the resorption of the ceramic materials. Conclusion: Ceramic augmentation with Calcium-Phospho silicate granules produces a safe and effective alternative to autograft harvesting. The product also has the advantage of added radio-opacity that helps delineate fusion status more effectively than autograft.
RFP13: Degenerative Lumbar
1350
RF217: Cost-analysis of single-position versus conventional dual positioning for lumbar interbody fusions
Jacob Ball 1 , Andy Ton 1 , Benjamin Hopkins 1 , Fergui Hernandez 1 , Nicole Hang 1 , Edward Shontz 1 , Zabiullah Bajouri 1 , Emily Mills 1 1 , Jeffrey Wang 1 , R. Kiran Alluri 1 , Raymond Hah 1
1 Orthopaedic Department, Keck School of Medicine of USC, Los Angeles, USA
Introduction: Single-position (SP) techniques for lumbar fusion have gained considerable interest in attribution to their improved operative efficiency and reduced complication risks relative to conventional dual-positioning (DP), wherein patients are repositioned from either supine or lateral decubitus positioning to prone for subsequent pedicle screw fixation. The SP lateral approach offers the advantages associated with traditional lateral lumbar interbody fusions (LLIF), such as improved disc space access and disc height restoration while enabling simultaneous access to the posterior column. Additionally, SP allows surgeons to circumvent the logistical inefficiencies associated with patient repositioning. As value-based care becomes a central paradigm in determining treatment indications, cost utility becomes an increasingly important consideration. As such, this study aims to compare the cost-effectiveness of SP versus DP approaches for lumbar interbody fusion. Material and Methods: A retrospective cohort study of patients who underwent lateral-based (LLIF/OLIF) or anterior lumbar interbody fusion (ALIF) with posterior pedicle screw fixation between 2019-2022 at a single institution was conducted. Surgeries were performed among seven spine surgeons, of which two performed SP procedures in addition to customary DP approaches. Cost data (operating room costs, variable costs, total cost of admission), demographic data, complications, operative variables, and surgical details were compared between SP and DP cohorts. Univariate and multivariate analyses, and subgroup analysis were performed to identify independent predictors for increased costs. All costs were adjusted accordingly to 2023 U.S. consumer price index (CPI) data. Results: Overall, 66 patients were included; 41 (63%) underwent DP and 24 (37%) underwent SP. On average, the SP group had shorter mean operative times (354 ± 141 vs. 493 ± 135 minutes; p < 0.001) and length of stay (3.3 ± 2.6 vs 4.9 ± 3.1 days; p = 0.008) relative to the DP cohort while demonstrating comparable complication rates. Operating room costs ($9,659 ± 2544 vs $14,407 ± 4741; < 0.001), variable costs ($29,013 ± 8,932 vs $39,755 ± 19,347; p = 0.002), and total costs ($38,673 ± 10,477 vs $54,162 ± 23,269; p < 0.001) were significantly lower in the SP group. Subgroup analysis for only single-level fusions (n = 35) reaffirmed significant reduction in OR costs (β = -1,406.9; p = 0.043) and total admission costs (β = -6,871.6; p = 0.005) for patients who underwent SP. Conclusion: Our results suggest that SP surgery significantly reduces operative time, length of stay, and costs in comparison with traditional DP surgery without increasing complications. While individual surgeon preferences and unaccounted factors may impact cost variations, our study supports that SP surgery may present a cost-effective approach with a comparable safety profile. As more surgeons adopt this technique, tracking potential savings compared to DP surgery will be crucial, thereby providing pragmatic insights to improve outcomes across economic, clinical, and patient-centered domains. This study establishes that there are significantly lower costs associated with SP technique for lumbar fusion when compared to DP while offering similar safety profiles. These findings introduce a cost-effective strategy that emphasizes patient-centered care and reduces the burden on the healthcare system by reducing OR time and utilization of additional intraoperative resources.
375
RF218: Does the combination of intrathecal fentanyl and morphine improve clinical outcomes in patients undergoing lumbar fusions?
Alan Villavicencio 1 , Hash Taha 1 , Kara Beasley 1 , Sigita Burneikiene 1
1 Neurosurgery, Justin Parker Neurological Institute, Boulder, USA
Introduction: Intrathecal morphine (ITM) has been effective in improving postoperative outcomes in patients undergoing a multitude of surgeries, including lumbar spine fusion. A major limitation of ITM administration is the increase in the incidence of respiratory depression in a dose-dependent manner. One way to bypass this is to use a more potent opioid with a shorter half-life, such as fentanyl. The study aims to investigate potential differences in postoperative outcomes in three groups of patients: ITM, ITM + fentanyl, and control. Material and Methods: This is a retrospective analysis of patients who underwent one- or two-level transforaminal lumbar interbody fusions. The patients received one of two interventions: 0.2mg intrathecal duramorph/morphine (ITM group; n = 70), 0.2 mg duramorph + 50 mcg fentanyl (ITM + fentanyl group; n = 68) and the control group (n = 102). Primary outcomes included postoperative pain (Visual Analog Scale) and opioid intake (MED – morphine equivalent dosage, mg) for postoperative days (POD) 1- 4. Secondary outcomes included opioid-related side effects. One-way analyses of variance and follow-up post-hoc Tukey’s honest significant difference statistical tests were used to measure treatment effects. Results: Significantly lower POD1 pain scores for both the ITM and ITM + fentanyl groups vs. control were detected, with no difference between the ITM vs. ITM + fentanyl groups. Similar results were found for POD1 MED intake. A multivariate regression analysis controlling for confounding variables did not attenuate the differences seen in POD1 pain scores while revealing that only the ITM + fentanyl predicted a decrease in POD1 MED intake. No differences were seen for postoperative opioid-related side effects. Conclusion: Our study provides support for supplementing a low dose of intrathecal morphine with a low dose of fentanyl to improve postoperative outcomes. The results demonstrate that ITM + fentanyl administration may be superior to ITM in reducing POD 1 opioid intake and other means of postoperative pain management.
1712
RF219: Outcome PredicTIon following lumbar Disc surgery (OPtiDisc): a Canadian longitudinal study of outcome trajectories, prognostic factors, and risk models
Jeffrey Hebert 1 , Erin Bigney 2,3,4 , Najmedden Attabib 5,6 , Chris Small 2,7,8 , Edward Abraham 2,7,9 , Neil Manson 2,7,9
1 Faculty of Kinesiology, University of New Brunswick, Fredericton, Canada
2 Canada East Spine Centre, Research, Saint John, Canada
3 University of New Brunswick, Interdisciplinary Studies, Fredericton, Canada
4 Research, Horizon Health Network, Saint John
5 Neurosurgery, Horizon Health Network, Saint John, Canada
6 Neurosurgery, Dalhousie University, Saint John, Canada
7 Orthopaedic Surgery, Dalhousie University, Saint John, Canada
8 Surgery, Saint John Orthopaedics, Saint John, Canada
9 Orthopaedic Surgery, Saint John Orthopaedics, Saint John, Canada
Introduction: Although lumbar discectomy for radiculopathy effectively reduces pain and disability for most patients, many report continued or relapsing pain following surgery. Information to predict patient outcomes following discectomy could assist surgeons with patient selection. Therefore, this study aimed to i) describe the perioperative trajectories of leg pain and overall clinical outcome following lumbar disc surgery for radiculopathy, ii) identify the preoperative prognostic factors that predict trajectories representing poor clinical outcomes, and iii) develop and internally validate multivariable prognostic models to assist with clinical decision-making. Material and Methods: This retrospective cohort study included patients enrolled in the Canadian Spine Outcomes and Research Network and diagnosed with lumbar disc pathology and radiculopathy, who underwent lumbar discectomy, at one of 18 spine centers. Potential outcome predictors included preoperative demographic, health-related, and clinical prognostic factors. Clinical outcomes were univariable latent-class trajectories of leg pain intensity (numeric pain rating scale) and overall outcomes modelled with multivariable trajectories of leg and back pain intensity and pain-related disability (Oswestry index). Multivariable risk model performance and internal validity were evaluated with discrimination and calibration statistics based on bootstrap shrinkage with 500 resamplings. Results: We included data from 1,142 patients (47.6% female) cared for by one of 66 surgeons. The trajectory models identified 3 subgroups, with 11.4% of patients in the leg pain model and 28.2% in the overall outcome model experiencing a poor clinical outcome. Eleven demographic, health, and clinical factors predicted patients’ leg pain and overall outcomes. The performance of the leg pain risk model was inadequate. The overall outcome model had acceptable discrimination, calibration, and evidence of internal validity in its ability to predict patients at risk of experiencing a poor outcome following discectomy. Conclusion: Patients experience heterogeneous outcomes following lumbar discectomy that were predicted by numerous preoperative prognostic factors. Multivariable risk models adequately predicted the overall outcomes experienced by patients but not leg pain intensity as a solitary measure. These results can help to inform clinical practice but require additional replication and validation before confident clinical implementation.
1722
RF220: Titanium coated PEEK interbody fusion devices support successful lumbar fusion outcomes regardless of the type of bone graft used
Madilyn Riegel 1 , Jillian Mohn 1 , Matthew Gary 2 , Joseph Lee 3 , Benjamin Chen 4 , Safdar Khan 5 , Elizabeth Yu 6 , Hallie Murray 1
1 Clinical Affairs, Tyber Medical, Bethlehem, USA
2 Emory University, The Emory Spine Center, Atlanta, USA
3 Orthopaedic Surgery, Rothman Orthopaedic Institute, Harrison, USA
4 Orthopaedic Surgery, Multicare Institute of Research and Innovation, Puyallup, USA
5 Orthopaedic Surgery, The Ohio State University, Dublin, USA
6 Orthopaedic Surgery, The Ohio State University, Columbus, USA
Introduction: Bone graft extenders and substitutes are an integral part of supporting successful spine fusion outcomes. While many different types of bone grafting substitutes are available to support spine fusion, there is a disparity of data supporting different types of bone grafting options. Moreover, in interbody spine fusion, the combination of bone grafts with various interbody fusion devices has not been fully evaluated. Therefore, the objective of this research was to evaluate the radiographic and clinical outcomes of patients treated with polyetheretherketone (PEEK) interbody fusion devices with a porous titanium coating (ProTi) when different bone grafting options, both simple (local autograft with or without allograft), and complex (cellular allografts or recombinant proteins) are used. Material and Methods: Institutional Review Board approval was obtained to gather healing outcomes data on patients treated with ProTi interbody fusion devices with pedicle screw fixation to treat degenerative lumbar spine conditions. Patients underwent 1-level (15 patients), 2-level (6 patients) or 3-level (1 patient) spine fusion procedures and were stratified by the type of bone grafting material used (recombinant bone morphogenetic protein 2 (rhBMP-2) (11 patients), cellular bone matrix (CBM) (5 patients) or local autograft with and without demineralized bone matrix and/or cancellous bone chips (simple) (6 patients)). Patients were evaluated for time to fusion, adverse events, and a subset of patients completed the Oswestry Disability Index (ODI) (N = 13) and the Visual Analog Scale (VAS) back pain scores (N = 10). Results: Patients treated with ProTi interbody fusion devices demonstrated good osteo-integration with the vertebral endplates and bridging bone across the interbody space at final follow-up in all three bone grafting groups. Patients treated with rhBMP-2 fused in an average time of 10.3 ± 1.3 months compared to 11.4 ± 5.9 months for patients treated with CBM and 12.8 ± 7.1 months for patients treated with simple bone grafts. Treatment groups had similar demographics including age, comorbidities (all patients had at least one risk factor for impaired bone healing), and levels of fusion. All bone grafting treatment groups demonstrated improved ODI and VAS back pain following treatment, however only the rhBMP-2 group had statistically significant (p < 0.05) improvements. Complications were similar amongst the different bone grafting treatment groups with one patient with adjacent segment disease (ASD) in the rhBMP-2 group, one patient with ASD and one patient with infection requiring debridement surgery and pedicle screw replacement (interbody fusion device not involved) in the CBM group, and two patients with subsidence in the simple bone graft group. Conclusion: This early analysis in an on-going study was the first to evaluate the performance of different bone grafting materials when used with ProTi interbody fusion devices. Study results found that rhBMP-2, CBM and simple bone grafts supported successful fusion outcomes with improved patient functionality and alleviation of pain when used with ProTi interbody fusion devices. While additional research is required to fully evaluate whether different bone grafts can lead to better fusion outcomes, this study demonstrates ProTi interbody fusion devices support lumbar fusion regardless of the bone graft used.
1296
RF221: Comparing the quality of CT guidet steroid injections and manuel injections, for Coccydynia. A retrospective cohort study
Marie Petersen 1 , Stine Zwisler 1 , Kristian Mortensen 2 , Ane Simony 3
1 Department of Anestesia, Odense University Hospital, Odense, Denmark
2 Department of Orthopedics, Hvidovre Hospital, Hvidovre, Denmark
3 Department for Spine Surgery, Spinecenter Middelfart, Middelfart, Denmark
Introduction: Coccydynia is a painful condition, with a prevalence < 1 % of patients suffering from low back pain. Previous studies has proven good outcomes after treatment with steroid injection or surgery. The aim of this study was to evaluate the outcome after steroid injections in a cohort treated with CT-guided injections and a cohort treated by manual steroid injections. To the knowledge of the authors, no study has previously compared the efficacy of CT-guided steroid injections versus manually injected steroids, and reported the efficacy of treatment in a large patient cohort. Material and Methods: 315 patients from two hospitals, treated between 2017-2021 were included. All data were retrospectively collected, from the medical records. All patients were examined by the same surgeon (AS), and the indication for treatment was VAS > 4 while sitting, and no relief from conservative treatment, > 6 months. Consumption of pain medication was also recorded. All patients was treated by steroid injections; 123 patients had the procedure done by manually techniques using anatomic landmarks, and 192 patients had CT-guided steroid injections. A treatment plan of three injections were recommended, in order to evaluate its efficacy, with an interval of 8-12 weeks. 10-12 weeks after the last steroid injection, patients were asked about their satisfaction, and divided into 4 categories: "no pain”, “some relief/some limitations”, “brief relief” and “no relief”. The association between injection method and proportions of patients with a positive effect of treatment, was examined by Fisher’s exact test. Results: Patient demographic from the two groups of patients, did not show any difference. 82% were females. Mean age 44 years (15-88), and mean BMI 29 (14-48). The aetiology of the chronic coccydynia (trauma, birth-related, or spontaneous) was also equal between the cohorts. Trauma was 48% in one centre vs. 43.9% in the other, birth-related was 22% vs. 13.5% and spontaneous was 30% vs. 42.6%. A total of 257 (81,6%) patients with a minimum follow-up of 10 weeks were available for analysis. Overall, 130 (50,6%) of the patients reported having a positive effect (“no pain” or “some relief/some limitations”) from the steroid injections 3 months after the last treatment. Of the 257 patients, 66 patients reported no pain relief, and 53 out of the 66 patients underwent surgery afterwards. 58 of 101 (57,4%) patients who received the manual technique had a positive effect, and 72 of 156 (46,2%) patients who underwent CT-guided steroid injections had a positive effect. No statistical difference was observed between the two groups. Conclusion: 130 of 257 (50.6%) patients with chronic coccydynia had satisfactory pain relief after os coccygis steroid injection. No statistical significant effect was found using CT-guided injections. CT-guided injections are time consuming and exposes the patients for radiation, and this study does not support the benefit of this technique.
2281
RF222: Outcome results after 200 consecutive single portal full endoscopic unilateral laminotomy for bilateral decompression for lumbar spinal stenosis in Hong Kong
Sze Hung Wong 1
1 Medigrove Orthopaedic and Spine Centre, Hong Kong, Hong Kong
Introduction: Lumbar spinal stenosis is a common aetiology of neurogenic claudication, radiculopathy and back pain in elderly. Traditional open or minimal invasive laminotomy is commonly performed in Hong Kong, but with more soft tissue trauma, blood loss and postoperative length of stay. Single portal Full endoscopic unilateral laminotomy for bilateral decompression LE-ULBD was used with aim to provide comparable results with less tissue trauma. Material and Methods: This study retrospectively reviewed 200 consecutive patients who underwent LE-ULBD. The preoperative and postoperative VAS, blood loss and complication was analyzed. Results: There is a definite learning curve in endoscopic spine surgery. The initial average operation time for the first 50 cases was 50% longer than the subsequent 150 cases. The mean length of stay after surgery was 1 day, with mean blood loss of less than 20 ml, and drain output of less than 50 mL. No mortality and major morbidities encountered. Conclusion: Single portal full endoscopic unilateral laminotomy for bilateral decompression for lumbar spinal stenosis is a safe approach that minimize tissue trauma. The advantage includes reduce blood loss and shorten length of stay. Since lumbar spinal stenosis is common in elderly population. Use of endoscopic technique can benefit the healthcare system by reducing the length of stay, reduce blood transfusion requirement. Elderly who receives the surgery can be discharge the next day and save a lot of precious hospital bed in public Hospital.
714
RF223: A radiological parametric comparison of low-grade lytic spondylolisthesis to degenerative spondylolisthesis: a retrospective approach to establish its dysplastic origin
Aayush Aryal 1 , Pratap K. R. 1 , Vikas Tandon 1 , Aditya Goparaju 1
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
Introduction: Although a significant proportion of patients with lytic and degenerative spondylolisthesis are treated conservatively, patients with failed conservative management or neurological deficit need surgical interventions. Fusion with pedicle screw fixation is a commonly performed procedure, and this requires a proper insight into vertebral anatomy. Therefore, understanding the difference in the morphology of lumbar vertebrae and pedicles in these two situations is of utmost significance as an element of preoperative workup. This study aims to compare low-grade lytic and degenerative spondylolisthesis radiologically. Additionally, it seeks to identify underlying similarities between lytic and dysplastic spondylolisthesis. Material and Methods: We retrospectively included patients with low-grade single-level spondylolisthesis at L4-L5 or L5-S1 surgically treated at our institution between April 2021 and July 2023. They were categorized into lytic and degenerative spondylolisthesis. Radiological features, including pedicle height, width, transverse and sagittal pedicle angle, as well as anterior and posterior vertebral heights, were measured on T1-weighted MRI. Results: The study included a total of 88 patients: 46 in the degenerative spondylolisthesis group (DS) and 42 in the lytic spondylolisthesis (LS) group. In the LS group, the anterior vertebral height (AVH) was significantly higher than the posterior vertebral height (PVH) at L4 and L5 [L4 PVH/AVH ratio 0.93 in LS vs 0.96 in DS; L5 PVH/AVH ratio 0.84 in LS vs 0.92 in DS] and the pedicles were more medially oriented [L4: 19.62° in LS vs 17.7° in DS; L5: 28.92° in LS vs 26.47° in DS]. Additionally, at L5, the pedicle height [10.67mm in LS vs 11.48mm in DS] and width [13.56mm in LS vs 14.37 mm in DS] were smaller compared to the DS group. Conclusion: Low-grade lytic spondylolisthesis shows distinct radiological vertebral and pedicle anatomy compared to degenerative spondylolisthesis. Short and thin pedicles and wedge-shaped vertebrae in lytic spondylolisthesis resemble dysplastic spondylolisthesis, indicating its dysplastic origin.
956
RF224: Findings from a pilot randomised trial of spinal decompression alone or spinal decompression plus instrumented fusion
Nicolas Beresford-Cleary 1 , Alan Silman 2 , Chrishan Thakar 1 , Adrian Gardner 3 , Ian Harding 4 , Cushla Cooper 2 , Jonathan Cook 2 , Dominique Rothenfluh 5
1 Spine Surgery, Oxford University Hospitals, Oxford, United Kingdom
2 Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Oxford, United Kingdom
3 Spine Surgery, Royal Orthopaedic Hospital, Birmingham, United Kingdom
4 Spine Surgery, North Bristol NHS Trust, Bristol, United Kingdom
5 Spine Surgery, CHUV, Lausanne, United Kingdom
Introduction: Symptomatic spinal stenosis is a very common problem, and decompression surgery has been shown to be superior to nonoperative treatment in selected patient groups. However, performing an instrumented fusion in addition to decompression may avoid revision and improve outcomes. The aim of the SpInOuT feasibility study was to establish whether a definitive randomized controlled trial (RCT) that accounted for the spectrum of pathology contributing to spinal stenosis, including pelvic incidence-lumbar lordosis (PI-LL) mismatch and mobile spondylolisthesis, could be conducted. Material and Methods: As part of the SpInOuT-F study, a pilot randomized trial was carried out across five NHS hospitals. Patients were randomized to either spinal decompression alone or spinal decompression plus instrumented fusion. Patient-reported outcome measures were collected at baseline and three months. The intended sample size was 60 patients. Results: Of the 90 patients screened, 77 passed the initial screening criteria. A total of 27 patients had a PI-LL mismatch and 23 had a dynamic spondylolisthesis. Following secondary inclusion and exclusion criteria, 31 patients were eligible for the study. Six patients were randomized and one underwent surgery during the study period. Given the low number of patients recruited and randomized, it was not possible to assess completion rates, quality of life, imaging, or health economic outcomes as intended. Conclusion: This study provides a unique insight into the prevalence of dynamic spondylolisthesis and PI-LL mismatch in patients with symptomatic spinal stenosis, and demonstrates that there is a need for a definitive RCT which stratifies for these groups in order to inform surgical decision-making. Nonetheless a definitive study would need further refinement in design and implementation in order to be feasible.
500
RF225: Study to compare functional and radiological outcomes following open TLIF using PEEK versus Titanium cages in low grade spondylolisthesis
Taarini Johri 1 , Rohan Gala 1 , Sanjay Dhar 1 , Shashwat Anand 1
1 Orthopaedics, Dr. D Y Patil Medical College, Hospital & Research Centre, Navi Mumbai, India
Introduction: Degenerative spinal disorders, particularly spondylolisthesis, present complex challenges in management due to their impact on spinal structures and the variability in patient profiles. Spondylolisthesis, characterized by vertebral body slippage, manifests in various forms, including degenerative, isthmic, traumatic, dysplastic, and pathologic. While often seen in the lower lumbar spine, cases in the cervical and thoracic regions are not unheard of. Surgical interventions have evolved over the years, with transforaminal lumbar interbody fusion (TLIF) emerging as a popular choice. However, the choice between implant materials, such as titanium and polyetheretherketone (PEEK) cages, remains a subject of debate. Material and Methods: This study, conducted on 50 patients with low-grade spondylolisthesis who underwent single-level TLIF, aimed to compare the functional and radiological outcomes of PEEK cages and titanium cages with transpedicular instrumentation. Patient data, including demographics, medical comorbidities, surgical level, and surgical indications, were collected and analysed over a one-year follow-up period at 3, 6 and 12 months. Simple randomization divided the patients into two groups: Group 1 (PEEK cage) and Group 2 (titanium cage). Subsidence rates were assessed using CT scans and cage positioning via lateral X-rays at 12 months. Results: The study found that postoperative VAS scores were numerically lower in the titanium cage group at 3 months, 6 months, and 12 months' follow-up, although this difference was not statistically significant (p > 0.05). Similarly, postoperative ODI scores showed a numerical advantage in the titanium cage group at all assessment time points, but this was not statistically significant (p > 0.05). Notably, the PEEK cage group exhibited a significantly lower mean subsidence rate compared to the titanium cage group at 12 months (p < 0.05). Regarding demographics, the majority of patients in both study groups were female. In the PEEK cage group, 32% of patients were between 51-60 years of age, and 24% were in the 61-70 age group. In contrast, the titanium cage group had 40% of patients in the 51-60 age group and 36% in the 41-50 age group. Conclusion: Both PEEK and titanium cages demonstrated similar outcomes. However, radiologically PEEK cages exhibited an advantage by having a lower subsidence rate when compared to titanium cages. Drawbacks of this study are smaller sample size and a single centre study. This research contributes essential insights to guide clinical decision-making in managing this challenging condition.
2594
RF226: Clinical comparison of microscopic minimally invasive transforaminal interbody fusion (MIS-TLIF) with enhanced recovery after surgery (ERAS) approach versus unilateral biportal transforaminal lumbar interbody fusion (BE-TLIF)
Rohit Kavishkar 1
1 Dept of Orthopaedics, Clinical Fellow in Spine Surgey, Ng Teng Fong General Hospital, Singapore, Singapore
Introduction: Unilateral biportal endoscopy has become a procedure of choice for lumbar discectomies and decompressions at our center replacing the microscopic techniques. Lumbar fusion is performed either by Unilateral biportal endoscopic transforaminal lumbar interbody fusion(BE-TLIF) or Minimally invasive transforaminal lumbar interbody fusion by microscopic tubular technique(MT-TLIF). Our aim was to compare these two techniques. Material and Methods: This is a retrospective study in which 59 patients underwent lumbar fusion between November 2020 and November 2022. 28 patients underwent BE-TLIF for 34 levels of fusion and 31 patients underwent MT-TLIF for 36 levels of fusion. All the patients were followed up for more than 12 months. Clinical outcome was measured by Visual Analogue Score(VAS) for back pain and leg pain, pre-operatively and at subsequent follow-up’s. Functional outcome was measured by Oswestery Disability Index (ODI) and McNab’s criteria. The Bridwell grading system was used for assessing fusion on Xrays at follow-up. Results: Both the cohorts (BE-TLIF and MT-TLIF) showed significant improvement of back pain and leg pain post-operatively and all the follow-ups. There was statistically significant improvement of VAS for back pain at immediate post-operative, 6 weeks post-operative, 6 months post-operative and final follow-up in BE-TLIF group as compared to MT-TLIF. At final follow-up BE-TLIF cohort had better ODI scores (p = 0.04). Fusion rates were better in BE-TLIF group at 6 months but eventually they were similar in both the groups at final follow-up but BE-TLIF cohort showed less subsidence than MT-TLIF group at final follow-up (p = 0.02). Conclusion: UBE fusion offers promising option of lumbar fusion with fusion rates similar to MIS-TLIF and added benefits of better clinical outcome scores, early ambulation, shorter hospital stay, less blood loss, less subsidence rate and very less incidence of surgical site infection.
99
RF227: The relationship between range of motion in the lumbar spine and paralumbar muscle health
Basel Sheikh Alshabab 1 , Joshua Mathew 1 , Bongseok Jung 2 , Jonathan Elysee 1 , Priya Duvvuri 2 , John Fallon 2 , Austen Katz 2 , Junho Song 2 , Adam Strigenz 2 , Luke Zappia 2 , Renaud Lafage 1 , Virginie Lafage 1 , Sohrab Virk 2
1 Orthopedic Surgery, Lenox Hill Hosptial, New York, USA
2 Orthopedic Surgery, North Shore University Hospital-Long Island Jewish Medical Center, Zucker School of Medicine at Hofstra University, New Hyde Park, USA
Introduction: Lumbar spine range of motion (ROM) and reserve of extension (ROE) have been associated with physical function and quality of life. While the association between posterior spine muscle characteristics and motion ability has been previously theorized, it has not yet been investigated in the setting of simple lumbar degenerative conditions. Therefore, the purpose of this study is to investigate the association between lumbar spine ROM and ROE and posterior muscle health. Materials and Methods: A retrospective single center review was performed on patients with degenerative lumbar spine pathology and complete MRI and x-ray imaging. After describing the cohort’s demographic, neutral and dynamic alignment, and posterior muscle characteristics, associations between neutral alignment, ROM, ROE, and muscle health were investigated using bivariate correlations. Multivariate analysis, controlling for regional alignment and demographics, was performed separately for male and female subjects. A sub-analysis focusing on patients with limited distal motion (< 50th%) was conducted to identify independent predictors of maintained regional lumbar motion (ROM L1-S1 > 20°). Results: 400 patients were included (55.4 ± 15.4 yo, 60.8% female, BMI 29.5 ± 6.2 kg/m2). Median ROM of the lumbar spine was 19° (IQR 12 to 30), with 9° (IQR 5 to 14) coming from L4-S1, representing 48.1% of total ROM (IQR 32.3% to 63.7%). Median ROE of the lumbar spine was 4° (IQR 1 to 8), with 144 patients (36.0%) having a reserve of extension smaller than 2.5°. Bivariate correlation revealed a weak association between CSA/BMI and both L1-S1 ROM and ROE (r = 0.21, r = 0.14, resp. p < 0.05). Results revealed a significant difference in L1-S1 ROM (24.1 vs 19.4, p = 0.001) and ROE (5.3 vs 3.7, p = 0.004) between Goutallier 0-1 vs > 2 (more fat infiltration). After stratifying by sex and controlling for age and L1-S1 neutral alignment, no significant association was found between dynamic motion and muscle health in males. Conversely, in females, CSA/BMI was significantly correlated with L1-S1 ROM (r = 0.24), L4-S1 ROM (r = 0.15), and L1-S1 ROE (r = 0.15), all p < 0.05. Smaller ROM at L1-S1 (B = -0.06, p < 0.001) and larger L1-S1 (B = 0.02, p = 0.013) were independent predictors of absent ROE, versus some ROE. Among patients with a stiff distal lordosis, those maintaining a L1-S1 ROM > 20° had larger posterior muscles (CSA = 4745 vs 4093 mm2, and CSA/BMI = 169 vs 138, p < 0.001) and less fat infiltration (35.6% with Goutallier > 2 vs. 60% p = 0.003). Multivariate analysis conducted on males and females separately and controlling for regional alignment and age demonstrated that CSA/BMI for females and fat infiltration for males were independent predictors of general mobility despite stiff distal spine. Conclusion: The association between muscle parameters and dynamic alignment does depend on demographics and overall alignment. For female patients, CSA/BMI was an independent predictor of motion and reserve of extension, while fat infiltration was an independent predictor of motion in male subjects. Understanding these differences in muscle role and motion may help explain the variability in pathophysiology of the degenerative lumbar spine.
1705
RF228: Commonly used patient-reported outcome measures (PROMs) do not adequately reflect patient-perceived changes in health status following lumbar fusion
Avani Vaishnav 1,2 , Jung Kee Mok 2 , Chad Simon 2 , Joshua Zhang 2 , Cole Kwas 2 , Eric Kim 2 , Tomoyuki Asada 2 , Nishtha Singh 2 , Yeo Eun Kim 2 , Olivia Tuma 2 , Eric Mai 2 , Kasra Araghi 2 , Maximillian Korsun 2 , Sravisht Iyer 2,3 , Sheeraz Qureshi 2,3
1 Boston Medical Center, USA
2 Hospital for Special Surgery, New York, USA
3 Weill Cornell Medical College, New York, USA
Introduction: In recent years there has been a growing focus on patient-reported outcome measures (PROMs) as important metrics in spine surgery. As a result, they are increasingly being utilized to assess healthcare expenditure, determine compensation and evaluate cost-effectiveness. However, there is little data on whether changes in PROMs correlate with patients’ perceptions of improvement. Thus, the purpose of this study was to assess the correlation between patient perceived changes in health and commonly utilized PROMs in patients undergoing lumbar fusion surgery. Material and Methods: We performed a retrospective review of prospectively collected data on consecutive patients who underwent 1-3 level lumbar fusion at a single academic institution between April 2017 and February 2023. PROMs, including Oswestry Disability Index (ODI), Visual Analogue Scale (VAS), Short-Form 12 (SF-12 PCS/MCS), and PROMIS physical function (PROMIS-PF), were prospectively completed pre-operatively and at 6 weeks, 12 weeks, 6 months and 1 year postoperatively. In addition, at each post-operative visit patients completed a ‘Global Rating Change (GRC)’ question, which assessed how the patient’s spine condition compared to before surgery and to their previous visit. This was assessed using a 5-item Likert Scale (‘much better’, ‘slightly better’, ‘about the same’, ‘slightly worse’, ‘much worse’). Spearman correlation coefficient (Rho) was used to assess the correlation between change in PROMs and GRC. Results: This study included 509 patients with a mean age of 59.5 years, mean BMI of 28.1 kg/m2, and comprised of 50.3% females and 49.7% males. Most patients underwent one-level surgery (74.5%) and were discharged on postoperative day 1 (50.6%). The percentage of patients feeling ‘much better’ compared to pre-operatively was 59.5% at 6 weeks, 69.1% at 12 weeks, 73.2% at 6 months, and 71.8% at 1 year. Less than 4% of patients reported feeling ‘much worse’ compared to pre-operatively at all time points. Changes in PROMs from pre-operatively demonstrated a statistically significant correlation with GRC at all time-points for all collected PROMs. The strengths of the correlations were very weak-to-moderate (Spearman’s Rho range: 0.156 to 0.562). Changes in PROMs compared to the previous visit demonstrated statistically significant correlation with GRC at all time points for ODI, VAS Back, SF-12 PCS, and PROMIS-PF, and one out of three time-points for SF12-MCS. No significant correlation with GRC was seen for VAS Leg. The strengths of the correlations were very weak-to-weak (Spearman’s Rho range: 0.133 to 0.344). Conclusion: The results of this study showed that a majority of patients undergoing lumbar fusion experienced notable improvement in the early post-operative period. However, commonly utilized PROMS demonstrated very weak-to-moderate correlation with perceived changes in overall spine-related health status from preoperatively to postoperatively, and very weak-to-weak correlation with postoperative changes. These findings suggest that currently used PROMs may not be as sensitive at detecting these changes, or may not be adequately reflecting changes in health condition that are meaningful to patients.
1739
RF229: Surgical site infections following lumbar fusion
Kasra Araghi 1 , Tejas Subramanian 1 , Tomoyuki Asada 1 , Yusef Jordan 1 , Chad Simon 1 , Eric Mai 1 , Yeo Eun Kim 1 , Eric Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Olivia Tuma 1 , Nishtha Singh 1 , Maximillian Korsun 1 , Avani Vaishnav 1,2 , Francis Lovecchio 1 , Sravisht Iyer 1 , Sheeraz Qureshi 1
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, USA
Introduction: Surgeons and patients have long known that surgical site infections are a potential risk associated with undergoing spinal surgery. Although we are aware of this risk, prioritizing their consideration may not occur as frequently as it should. An intensified examination of this complication is both appropriate and warranted in light of the current medical landscape, which includes increasing antimicrobial resistance, significant SSI-associated economic implications, and the increasing proportion of elderly or complex patients undergoing spine surgery. A considerably limited amount of focused data exists studying the difference in SSI rates depending on the technique utilized in a cohort of lumbar fusion patients. Therefore, it remains unclear if minimally invasive surgical techniques ultimately produce significantly decreased SSI rates in lumbar fusion surgery as compared to open or mini-open approaches. Therefore, the primary goal of this study was to investigate the difference in surgical site infection rates for different surgical techniques in patients undergoing instrumented lumbar fusion. Material and Methods: This study is a retrospective review of all patients who underwent instrumented lumbar fusion between January 2019 and June 2022. Three cohorts (Mini, MIS, and Open) were created to divide patients based on the surgical technique utilized. Surgical Site Infections were identified according to the Centers for Disease Control and Prevention’s National Healthcare Safety Network (CDC/NHSN) criteria. Superficial SSIs involved only skin and subcutaneous tissue of the incision, deep involved deep soft tissues of the skin (i.e., fascial and muscle layers), and organ/space involved surgeries in which a body part was opened or manipulated deeper than the fascial/muscle layers. Results: A total of 2,147 lumbar fusion surgeries performed in 2,044 patients were included. The mean age was 61.5 ± 12.8 years, and the mean BMI was 28.5 ± 5.74 kg/m2. Of the 2,044 patients, 1,948 (95.3%) had one lumbar fusion surgery, 89 (4.4%) patients had 2, and 7 (0.3%) patients had 3 surgeries within the time period analyzed. The traditional open surgical technique was utilized in most of the surgeries (45.9%, 985), followed by MIS (29.2%, 626), and Mini (25.0%, 536). The overall SSI rate following lumbar fusion surgery was 1.3%. MIS cases had the lowest infection rate (0.5%, 3) followed by Mini (1.1%, 6) and Open (1.9%, 19). There were 27 patients with a surgical site infection, of which, 26 had 1 SSI, and 1 patient had 2 SSI events. Of the 27 patients with a surgical site infection, 4 patients experienced a superficial incisional SSI, and 23 patients experienced a deep incisional SSI. Conclusion: In our cohort, cases performed using MIS techniques had the lowest infection rate, followed by Mini-open techniques and the traditional open technique.
1676
RF230: Ultrasound guidance in lumbar unilateral biportal endoscopy
Ishant Gunadala 1,2
1 Orthopaedic Spine, Apollo Hospital, Ahmedabad, India
2 Orthopaedic Spine, METAS Hospital, Surat, India
Study Design: Experimental study. Objective: This study aims to establish a novel method to identify the landmarks for Unilateral biportal endoscopy using ultrasound guidance (US) and compare that with Fluoroscopy imaging for the surgical procedure. Background: The role of ultrasound in spine endoscopy has been underappreciated, partly because of the unfamiliarity and partly because of the perceived difficulty in imaging through the narrow acoustic windows produced by the bony framework of the spine. However, this is also the basis for the utility of ultrasound: the major bony landmarks for spine endoscopy have a signature ultrasound appearance, thereby permitting identification and targeting of the needle. Methods: Nineteen patients with Lumbar disc herniation or Lumbar canal stenosis were enrolled prospectively in this study and randomly divided into ultrasound and X-ray (C-arm) guidance groups. The time to puncture, cannulation, total duration of the surgery and the number of fluoroscopy shots were recorded in both groups. Results: The puncture, cannulation and operation times in the US group were comparable to those in the X-ray group. The patients in the US group had received about 4 fluoroscopy shots, significantly lower than the values in the X-ray (C-arm) group (9.9 shots). The time duration taken to targeting and cannulation in the US group was about 6.32 minutes, similar to the X-ray group (5.59 minutes). The overall duration of the surgery was longer in L5/S1 level in the ultrasound group when compared to the X-ray group. No complications were observed in either group. Conclusion: US guidance is a new method that reduces the number of fluoroscopy shots and time duration to puncture and cannulation in Unilateral Biportal endoscopy.
2052
RF231: The durability of decompression alone in eligible candidates for spinal fusion
Phattareeya Pholprajug 1,2 , JinSung Luke 2
1 Orthopedics, Rayong Hospital, Rayong, Thailand
2 Catholic University of Korea, Seoul St. Mary's Hospital, Orthopedics, Seoul, South Korea
Introduction: The ongoing debate surrounding fusion versus non-fusion spinal surgery has persisted for years, particularly in the context of decompression alone for conditions like deformity, low-grade spondylolisthesis, and extensive spinal canal decompression. However, patients with high morbidity and advanced age pose unique considerations that may preclude them from being suitable candidates for fusion surgery. In these instances, decompression alone emerges as a viable option, even for those exhibiting radiographic signs of mild instability or a predisposition toward post-surgical instability. This study endeavors to assess the long-term durability and efficacy of decompression as an independent procedure for patients deemed eligible for spinal fusion, with a particular focus on its potential sustainability as a viable alternative. Material and Methods: We conducted a study involving patients who underwent 1-2 level decompression procedures utilizing tubular microscopic or endoscopic techniques. Our inclusion criteria included individuals with low-grade degenerative spondylolisthesis, isthmic spondylolisthesis, degenerative scoliosis, and spinal stenosis, while excluding patients with a history of previous surgery. All participants were tracked for a minimum of one year. We retrospectively evaluated clinical scores, including Visual Analog Scale scores (VAS) for back and leg pain, Oswestry Disability Index (ODI) scores, EQ-5D scores, and satisfaction scores. Radiographic parameters, such as translational or angular instability, spino-pelvic parameters, and Cobb's angle, were analyzed both pre-operatively and at the final follow-up. Furthermore, we assessed cases requiring subsequent fusion revision and measured the time interval between the initial and subsequent surgeries to determine longevity. Results: Our study comprised 109 patients covering 133 levels of decompression alone. Patients universally reported a significant reduction in both back and leg pain, as evidenced by VAS scores. Functional outcomes, as evaluated by the Oswestry Disability Index, demonstrated substantial improvement. Quality of life, assessed through EQ-5D scores, exhibited remarkable enhancements, in line with the high levels of patient satisfaction. In terms of radiographic outcomes, the majority of patients maintained spinal stability, with no significant deterioration in translational or angular instability, spino-pelvic parameters, or Cobb's angle. A small subset of patients from the cohort required subsequent fusion surgeries at the decompressed level, with varying time intervals, ranging from months to years following the initial decompression. Conclusion: Decompression alone emerges as a viable option for patients necessitating extensive decompression, even in cases where spinal segments appear stable or non-obviously unstable, irrespective of underlying spinal conditions. The results demonstrate durability, with few patients requiring fusion procedures within three years.
1635
RF232: Review of intraoperative management and outcomes of incidental durotomy in minimally invasive spine surgery
Chad Simon 1 , Jung Kee Mok 1 , Tomoyuki Asada 1 , Kasra Araghi 1 , Eric Mai 1 , Yeo Eun Kim 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Joshua Zhang 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Avani Vaishnav 1,2 , Sheeraz Qureshi 1,3 , Sravisht Iyer 1,3
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, USA
3 Weill Cornell Medical College, New York, USA
Introduction: Incidental durotomy (ID) is a well-recognized complication of lumbar minimally invasive spine surgery (MISS). Due to inherent limitations in visualization, ID is often managed without primary suture repair in MISS. Prior studies have hypothesized that the smaller incisions and muscle sparing approach of MISS lead to decreased dead space and subsequently lessen the risk of persistent CSF leaks, pseudomeningocele, or other perioperative complications. However, there still remains a relative lack of data on the optimal management of IDs in MISS and their effects on short- to long-term outcomes. Thus, the purpose of this study was to review the authors’ experiences in managing IDs without primary suture repair and to describe various outcome measures in patients who sustained an ID during lumbar MISS. Material and Methods: This was a retrospective review of prospectively collected data of consecutive patients who underwent primary/revision lumbar MISS from 2017-2023 at a single academic institution for degenerative lumbar pathology and had experienced an ID. Repair of IDs was performed with dural patch and/or sealant. Descriptive statistics included age, BMI, sex, age-adjusted Charlson comorbidity index (CCI age), ASA, and operative characteristics. Hospital course, postoperative complications, and PROMs at 2, 6, and 12 weeks, 6 months, 1 and 2 years were analyzed. Results: Of 3,361 patients, 43 (1.3%) experienced IDs repaired without suture. Mean age was 66.4 ± 14.0 years, mean BMI was 26.4 ± 3.8, and mean CCI age was 2.9 ± 1.6. Most patients were males (60.5%) and were ASA II (95.3%). Surgical procedures included 31 (72.1%) decompressions, 4 (9.3%) fusions, and 8 (18.6%) microdiscectomies. Thirty-eight (88.4%) were primary procedures. Thirty (69.8%) durotomies were repaired with patch and sealant, 6 (14.0%) with patch only, and 7 (16.3%) with sealant only. Mean length of stay was 33.7 ± 48.3 hours with 31 (72.1%) patients discharged same day or the first postoperative day. In-hospital complications included one headache, one new-onset foot drop, and one case of recurrent stenosis and radiculopathy due to CSF leak, which returned to the OR for primary suture repair. At 2 weeks, four patients had new-onset radiculopathy, two of which were unrelated to CSF leak. There were three reoperations: one at 6 weeks for new-onset radiculopathy, which returned to the OR for exploration of rootlet clumping and was repaired primarily with suture; one at 12 weeks for ganglion cyst removal; and one at 6 months for recurrent stenosis. Compared to preoperatively, significant improvement was seen at 1 year and later for ODI (p = 0.03), VAS-back (p = 0.005), VAS-leg (p = 0.021), and SF-12 PCS (p = 0.034). PROMIS-PF was significantly improved at 6 months (p = 0.029) but not afterwards. Conclusion: The results of this study suggest that patients who underwent ID repair without suture in MISS experienced early discharge and significant improvement in certain PROMs. Complications related to the ID were transient with no permanent deficits, except for two reoperations that required primary repair. Ultimately, ID repair without suture in MISS appears to be effective and warrants further comparative investigation.
2294
RF233: Analysis of post-operative outcome in patients with lumbar spinal stenosis: a prospective study
Kartik Soni 1 , Navin Singh 1 , Venkatesh Dasari 1 , Vrushabh Kumbhare 2
1 Department of Orthopaedics, Raipur Institute of Medical Sciences, Raipur, India
2 Department of Orthopaedics, Jawaharlal Nehru Medical College Datta Meghe Institute of Medical Sciences, Sawangi, India
Introduction: Lumbar spinal stenosis is a common degenerative disorder that can lead to clinical syndromes such like neurogenic claudication, low back pain, impairment of urination-defecation, radiating pain, decreasing sensation and fatigue in lower limb and increasing pain in both buttocks or lower limbs, which may worsen when walking or standing for a long time when the space surrounding the neurovascular tissue becomes narrower. Lumbar spinal stenosis is of 3 types: central stenosis, foraminal stenosis, and lateral recess stenosis. Due to hypertrophied ligamentaum flavum anteriorly and bulging disc posteriorly with consequent thecal sac compression causes central stenosis. There is compression of descending nerve roots due to lateral recess stenosis which is due to facet joint arthropathy, osteophyte formation, overgrowth of superior articular facet, herniation of the intervertebral disc and hypertrophy of the ligamentum flavum. Chronic pain and functional impairment caused by this progressive disease results in limitation in both mobility and inability to perform activities of daily living. Likewise, there are many different terminologies used by spinal surgeons to describe methods to surgically decompress the lateral spinal canal stenosis: foraminectomy, foraminotomy, partial facetectomy, total facetectomy, and total laminectomy. There are different terminologies often used by clinicians that mean the same thing. Preservation of spinal stability and adequate decompression are the two main prerequisites for successful neural decompression. Before decompression preservation of spinal stability and the exact location of the nerve root compression must be confirmed. Posterior decompression and spinal fusion procedures are the standard treatment for LSS. In view of inadequate data regarding surgical outcome of patients with Lumbar Spinal Stenosis with respect to improvement in pain, function and quality of life, this study was pursued. Methods: In this prospective study, 224 patients above 18 years of age were enrolled willing to participate in the study and clinico-radiologically suffered from LSS. Patients were assessed using through history taking and clinical examination (Inspection, palpation, kinematics and neurology). Special care was given to note down the VAS score (Visual Analogue Score), ODI (Oswestry Disability Index) and Quality of life index (SF-36 Questionnaire). Post-operative assessment was done at interval of 3 months. These values were then further tabulated to establish the change in pain, function and quality of life in patients with LSS by surgical intervention. Results: The mean VAS score was 7.5 (4-9) and 2.9 (0-4) pre op and 3 month short term follow up simultaneously, mean ODI was 58.7 ± 11.22 and 17.22 ± 4.70 pre op and 3 month short term follow up simultaneously, mean changes in dimension specific 36-item short form health survey scores was 28 (50-58) and 82 (80-88) pre op and 3 month short term follow up simultaneously which was found significant. Conclusions: Using the result of this study it was established that evidence based surgical treatment for patients with LSS had change the pain, function and quality of life. This will help practicing spine surgeons to make better management plans, pre determine and accordingly counsel LSS patients regarding surgical outcomes.
2526
RF234: Lumbar spinal stenosis - surgical outcome and the odds of revision surgery - is it all due to the surgeon?
Carolin Melcher 1 , Bernd Wegener 2 , Christof Birkenmaier 3
1 Department of Spine Surgery and Scoliosis Center, Schön Klinik Neustadt, Neustadt in Holstein, Germany
2 Orthopedic and Trauma Surgery (MUM), LMU Munich, Munich, Germany
3 Department of Spine Surgery and Scoliosis Center, Artemed Klinik München Süd, Munich, Germany
Background: Surgical decompression is the intervention of choice for lumbar spinal stenosis (LSS) when non-operative treatment has failed. Apart from acute complications such as hematoma and infections, same-level recurrent lumbar stenosis and adjacent-segment disease (ASD) are factors that can occur after index lumbar spine surgery. The aim of this retrospective case series was to evaluate the outcome of surgery and the odds of necessary revisions. Methods: Patients who had undergone either decompressive lumbar laminotomy or laminotomy and spinal fusion due to lumbar spinal stenosis (LSS) between 2000 and 2011 were included in this analysis. Demographic, perioperative and radiographic data were collected. Clinical outcome was evaluated using numeric rating scale (NRS), the symptom subscale of the adapted version of the german Spinal Stenosis Measure (SSM) and patient- reported ability to walk. Results: Within the LSS- cohort of 438 patients, 338 patients underwent decompression surgery only, while instrumentation in addition to decompression was performed in 100 cases (22.3%). 38 patients had prior spinal operations (decompression, disc herniation, fusion) either at our hospital or elsewhere. Thirty-five intraoperative complications were documented with dural tear with CSF leak being the most common (33/35; 94.3%). Postoperative complications were defined as complications that needed surgery and differentiated between immediate postoperative complications (≤ 3 weeks post operation) and complications that needed revisions surgery at a later date. Within all patients 51 revisions were classified as immediate complications of the index operation with infections, neurological deficits and hematoma being the most common. Within this group only 22 patients had fusion surgery in the first place, while 29 were treated by decompression. Revision surgery was indicated by 53 patients at a later date. While 4 patients decided against surgery, 49 revision surgeries were planned. 28 were performed at the same level, 10 at the same level plus an adjacent level, and 10 were executed at index level with indications of adjacent level spinal stenosis, adjacent level spinal stenosis plus instability and stand-alone instability. Pre- operative VAS score and ability to walk improved significantly in all patients. Conclusions: While looking for predictors of revision surgery due to re-stenosis, instability or same/adjacent segment disease none of these were found. Within our cohort no significant differences concerning demographic, peri-operative and radiographic data of patients with or without revision wer noted. Patients, who needed revision surgery were older but slightly healthier while more likely to be male and smoking. Surprisingly, significant differences were noted regarding the distribution of intraoperative and early postoperative complications among the 6 main surgeons while these weren´t obious within the intial index group of late revisions.
RFP14: Adolescent Deformity
47
RF235: Bilateral vertebral body tethering for lenke 6 curves
Stephanie Da Paz 1 , Per Trobisch 1
1 Spine Surgery, Eifelklinik St. Brigida, Simmerath, Germany
Introduction: Spinal fusion is the standard treatment for severe forms of adolescent idiopathic scoliosis that usually exceed > 45°. Lenke 6 curves typically require posterior spinal fusion down to L3 or L4 with a high risk for the development of adjacent level disc degeneration. VBT has become an alternative for selected adolescent idiopathic scoliosis patients while preserving motion. Various studies have shown successful outcome after VBT but the majority of these studies focus on Lenke 1 curves and few studies have analyzed bilateral VBT for double curves. Additionally, no study has specifically analyzed the outcome after VBT for Lenke 6 curves. Material and Methods: This is a retrospective analysis of a prospectively collected database. All consecutive patients who underwent a bilateral VBT from 1/2019 to 4/2021 with a Lenke type 6 curve were considered and consequently met the following inclusion criteria: Sanders 7 or below, whole spine xrays at 2 years postoperatively. VBT was performed during a single stage by using a mini-open retroperitoneal lumbar and a thoracoscopically assisted thoracic approach with the use of a double-tether for thoracolumbar curves. Coronal and sagittal radiographic analysis was performed pre-operatively and six weeks as well as 24 months postoperatively. Results: 18 patients met the inclusion criteria. The average age at surgery was 14 years with an average Sanders stage of 6. The average thoracic Cobb was 56 degrees and the average lumbar Cobb was 61 degrees. The immediate postoperative results showed an average reduction of 57% for the thoracic curve and 70% for the lumbar curve. At the 2 year follow up the thoracic Cobb demonstrated a significant reduction of 52% and the lumbar Cobb a decrease of 51% compared to the preoperative measurements. The thoracic curves showed an average loss of correction from the 6 weeks results to the 2 year measurement of 13% and the lumbar curve showed a significant loss of correction of 66 % after 2 years. Perioperative complications were observed in 4 patients and one patient underwent a revision VBT with a 2 level fusion. Conclusion: VBT is a motion preserving alternative for AIS and shows an overall correction of the lumbar curve of 51 % for Lenke 6 curves after 2 years. The significant loss of correction for the lumbar curve suggests a higher rate of tether breakages for thoracolumbar and lumbar curves, which may be of limited clinical significance as the majority of patients have reached skeletal maturity 2 years post-operatively.
1361
RF236: Pelvic fixation using ilio-sacral screws in neuromuscular scoliosis: results in a retrospective series of 173 patients
Mathilde Gaume 1,2 , Raphael Vialle 1 , Lotfi Miladi 2
1 Pediatric Orthopaedics, University Institute for Spine Surgery, Sorbonne University, Paris, France
2 Pediatric Orthopaedics, Hôpital Necker Enfants Malades, Paris, France
Introduction: The surgical goal in patients with neuromuscular scoliosis is to obtain a stable, compensated spine with the torso balanced over a leveled pelvis. Pelvic fixation using iliac screws is recommended to obtain coronal and sagittal alignment of the spine in cases where pelvic obliquity is greater than 15º. Extending the fusion to the pelvis in frail neuromuscular patients increases the technical difficulty of the procedure, pseudoarthrosis, and risk of skin ulcerations. Therefore, pelvic fixation using iliac screws remains one of main challenging issues between clinical effectiveness in the non-ambulatory NMS patients and high complication rates. The wide variety of pelvic fixation techniques described in the literature reflects the difficulty in finding the best option. The aim of this work was to evaluate complications and radiological results of ilio-sacral screw pelvic fixation in this population. Materials and Methods: 173 patients with neuromuscular scoliosis who underwent a spinopelvic fixation with ilio-sacral screw were retrospectively reviewed. The screws were inserted from outside the iliac bone toward the center of the S1 body. The entry point was on the posterior sacral cortex, between the S1 facet joint and the first dorsal sacral foramen. Age, neuromuscular etiology, functional outcomes, radiographic measurements (angle of the major coronal curve and pelvic obliquity) and complications were reported. Pelvic obliquity was measured with the pelvic obliquity angle. The minimal follow-up was two years. Results: Mean operative age was 13.7 ± 7 years (6 to 19.2 years). Neuromuscular disease was cerebral palsy in 102 cases (59.0%), spinal muscular atrophy in 19 cases (11.0%), muscular dystrophy in 14 cases (8.1%), flaccid paraplegia (traumatic or tumoral) in 11 cases (6.4%), myelomeningocele in 9 cases (5.2%) and Rett syndrome in 7 cases (4.0%). After surgical correction the mean angle of the main coronal curve was 63.8° and improved by a mean of - 39.5° postoperatively. Mean preoperative pelvic obliquity was 23.0° and improved by a mean of -14° postoperatively. No loss of frontal or sagittal correction was observed at last follow-up. Sitting posture and comfort improved in all cases. 29 patients (17%) had early post operative infection treated by local wound debridement and antibiotics in 26 cases. In three cases, hardware removal was required due to persistent chronic infection. 14 mechanical complications (8%) occurred: early mobilization of one ilio-sacral screw made it necessary to change the screw for a longer one percutaneously (n = 6), screw malposition with S1 root irritation (n = 6), screw skin prominence (n = 1) and connector failure (n = 1). Conclusion: Despite a high rate of postoperative infection, the pelvic fixation using ilio-sacral screws is a reliable and powerful technique to correct pelvic obliquity in neuromuscular patients. In our series ilio-sacral screws permitted stable radiographic outcomes in frontal and sagittal planes, with a reduced rate of mechanical complications. The introduction of intraoperative navigation should minimize the risk of nerve root injury and facilitate revision or primary fixation for patients with disturbed sacropelvic anatomy. Pelvic fixation using ilio-sacral screws deserves to be better known, especially for neuromuscular scoliosis.
823
RF237: Effectiveness and safety of pre-operative distraction using modified halo pelvic distraction assembly in severe kyphoscoliosis patients
Muhammad Saad Ilyas 1 , Amer Aziz 1 , Uruj Zehra 2 , Abdullah Shah 1
1 Orthopedics and Spine Surgery, Ghurki Trust Teachingn Hospital, Lahore, Pakistan
2 Anatomy Department, University of Health Sciences, Lahore, Pakistan
Introduction: The management of severe kyphoscoliosis is challenging despite the fast-developing modern techniques & instrumentation. It becomes more crucial if the curve magnitude is greater than 100° with significant kyphosis and or a history of intraspinal pathology. These difficult curves require prolonged surgeries with complex osteotomies and are usually accompanied by tissue releases creating a likelihood of several problems. Pulmonary complications are most reported followed by implant related complications, infection, neurological complications and pseudoarthrosis. Methods like pre-operative halo-femoral, halo-tibial and halo-gravity traction have been seen to provide significant corrective forces but compliance is a big issue. Keeping in view the halo-pelvic distraction as an effective and affordable means of treatment for severe kyphoscoliosis, halo-pelvic apparatus has been modified using standard Ilizarov set. The constructed assembly was used for severe curves before definitive surgeries to reduce complications. Material and Methods: Kyphoscoliotic patients having coronal Cobb angle > 100 were applied modified halopelvic Ilizarov distraction assembly pre-operatively. Complete clinical assessment along with pulmonary function tests was done and scoliosis series x rays were assessed for coronal & sagittal Cobb angle and other spinopelvic parameters before applying assembly and during follow-up of one year. Modified assembly consisted of a pelvic component and halo ring, and distraction was given at the rate of 2-3 mm/day for 6-12 weeks. Cobb angles and spinopelvic parameters were compared before and after distraction and after surgery. Results: Thirty-four patients (age range 9-27years 18M/16F) included were having mean (SD) coronal and sagittal Cobb angle of116 (16.2) & 84 (28.3) respectively. Correction obtained through modified halopelvic assembly was almost 52% (p < 0.001) in coronal and 40% (p < 0.001) in sagittal Cobb angle respectively with improvement in height (p < 0.001). Apical vertebral translation and coronal balance were also improved significantly (p < 0.001). Further improvement in all the parameters were obtained after definitive surgery with improvement in FEV1 (p = 0.002) & FVC (p = 0.001). Conclusion: The results of this study reveal that our modified halo-pelvic Ilizarov distraction assembly is a device with unlimited potential, which can achieve good correction in severe spinal deformities without significant risk to neurology, fewer complications and good patient compliance.
6
RF238: Posterior pediatric scoliosis surgery method using intravertebral interpedicle constructs for fusion within the major curve(s) and posterolateral vertebral tethering can decrease the number of levels fused and preserve lumbar spine range of motion, min. 2-year follow-up
Saechin Kim 1 , Philip Hanna 1 , Hao-Hua Wu 1
1 Orthopaedic Surgery, Mass General Brighaml/Harvard Medical School, Boston, USA
Introduction: The surgical goals for pediatric scoliosis surgery are to create a balanced, stable spine, to preserve range of motion (ROM) especially in the lumbar spine, and to avoid complications such as revision surgery (RS) or adding on phenomenon (AO). We describe a posterior scoliosis surgical method with coronal and rotational control of each vertebra and each disc angle for fusion within the major structural curve(s) and correction of the deformity above or below the fusion with posterolateral vertebral tethering (PVT). Our hypothesis is that this method is safe and results in fewer levels fused and in the preservation of lumbar ROM in patients who are at or near skeletal maturity. Methods: Manipulation of constructs placed transversely into the pedicle screw tulips of the same vertebra, intravertebral interpedicle (IVIP), at two adjacent vertebrae can directly change the adjoining disc angle and the rotation between the vertebrae. In the IVIP method, IVIP constructs with open lateral extenders are used for fusion and closed lateral extenders with polyethylene terephthalate bands placed through the closed heads are used for PVT of disc levels in the compensatory curve or that correct fully with side bending (SB). This IRB approved prospective study presents minimum 2-year results of the first 10 patients treated with the IVIP method. The number of levels fused is compared to matched historical standard posterior fusion controls (MHSPFC). Radiographic measurements from xrays at 3-month and final follow up (f/u) assess for AO and from bending xrays at pre-op and 1- and 2-year f/u determine the ROM as the difference between the right and left SB lumbar (LCSBROM) or T12L5 (T12L5SBROM), or flexion and extension T12L5 (FEROM) Cobb angles. Three independent observers determined the Cobb angles, ROM calculated, and the results averaged. SRS 22r Questionnaire was scored pre-op and at each f/u. Results: Average (avg) age was 16.4 ± 2.2 years, pre-op main curve was 56o ± 8o, and post-op main curve was 25o ± 8o for avg correction of 55 ± 13%. Female to male ratio was 9:1. Risser stages were 3 (n = 2), 4 (n = 2) and 5 (n = 6). The number of levels fused (avg 4.6 ± 1.3) with the IVIP method was less than the number of levels fused in the MHSPFC (avg 10.8 ± 1.8) and the difference was statistically significant (p <.0001). At avg of 27-month f/u (min. 24), no PVT failure, AO, or RS was seen. Eight patients (1 Lenke1B, 2 1C, 2 3C, 1 4C, 1 5C, 1 6C) had complete pre- and post-op SB xrays and had avg 3.3+/-0.9 levels (1.4 ± 0.9 in the lumbar spine) of PVT. LCSBROM at pre-op (avg 22o ± 10o) and at f/u (avg 25o ± 10o) (p =.29), and T12L5SBROM at pre-op (avg 28o ± 12o) and at f/u (avg 30o ± 10o) (p =.64) were not statistically different. Post-op FEROM was 41o ± 13o. SRS-22r scores (n = 9) at final f/u was 4.5/5 and pre-op was 4.0/5 and the increase was statistically significant (p <.001). Discussion: The IVIP method of posterior spinal fusion and PVT results in significantly fewer levels fused compared to MHSPFC and preserved lumbar ROM, both SB and FE, in patients who are at or near skeletal maturity.
231
RF239: Comparison of radiologic outcomes and assessment of the degeneration of unfused segments with MRI and core muscle strengths and quality of life in Lenke Type 5 AIS patients treated with either anterior or posterior spinal fusion; mean 13 years follow up
Hamisi Mraja 1 , Ayhan Mutlu 1 , Onur Levent Ulusoy 1 , Halil Gok 1 , Cem Sever 1 , Enas Daadour 1 , Tunay Sanli 1 , Selhan Karadereler 1 , Meric Enercan 1 , Azmi Hamzaoglu 1
1 Orthopedics and Traumatology, Scoliosis-Spine Center Istanbul, İstanbul, Turkey
Introduction: Selective lumbar fusion (Cobb to Cobb) was accepted as standard treatment for AIS with Lenke Type 5 curves, but the choice of surgical approach is still controversial. Aim of the study is to compare the long-term functional, clinical, radiological outcomes and assess disc degeneration (DD) and facet joint degeneration (FJD) in the unfused lumbosacral spine with MRI in patients. Material and Methods: 43 Lenke type 5 AIS patients treated with Anterior Spinal Fusion (ASF) or Posterior Spinal Fusion (PSF) between Cobb levels with > 10 years f/up were included. Preop, postop, f/up coronal and sagittal parameters were analyzed. Lumbar core muscle strengths were evaluated with computer-assisted 3D spatial rotation device (SRD). DD and FJD at unfused lumbar segments were assessed with MRIs and clinical outcomes were evaluated with SRS22r at f/up. Results: The anterior spinal fusion group included 15 patients with 18,7 (12-23) years f/up. The posterior spinal fusion group included 28 patients with 13(10-17) years f/up. The mean age at the time of surgery was 15 for both. LIV levels were similar for both (L3; 80% ASF vs 78% PSF). Mean TL/L curve correction was 76% in ASF and 85% in PSF without any correction loss at f/up. Residual lumbar curve magnitudes were similar and stable over time (ASF: 6.4° vs PSF: 5.8°). DD and FJD grades of distal unfused segments were similar for both despite the longer f/up period and higher mean age at f/up (ASF; 18 years f/up and mean age was 34yo vs PSF; 13 years f/up and mean age was 28yo). Posterior lumbar core muscle strengths measured with SRD were significantly higher in ASF (p < 0.05; U = 21). SRS22r domains including pain, self-image, function, and satisfaction scores were higher in the Anterior spinal fusion group. Revision surgery was performed only in 1 patient (1.9%) for pseudoarthrosis in PSF. Conclusion: Anterior spinal fusion and Posterior spinal fusion provided satisfactory functional, clinical, and radiologic outcomes in long-term f/up. The anterior spinal fusion group demonstrated better functional outcomes in terms of lumbar core muscle strengths. Although the mean f/up length and the mean age were at least 5 years greater in the Anterior spinal fusion group compared to the Posterior spinal fusion group, in the unfused lumbosacral spine below the fusion level, both groups had similar grades of disc degeneration and facet joint degeneration. SRS22r pain, self-image, function, and satisfaction scores are higher in the Anterior spinal fusion group than the Posterior spinal fusion group at f/up.
1837
RF240: Modification of spinopelvic parameters in the surgical treatment of high grade pediatric spondylolisthesis
Antonio Parciante 1 , Chiara Cini 1 , Francesco Vommaro 1 , Giovanni Ciani 1 , Bruna Maccaferri 1 , Alessandro Gasbarrini 1
1 Spine Surgery, Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Pediatric spondylolisthesis [SL] presents with a wide spectrum of clinical and pathological manifestations. Unlike low-grade SLs, high-grade SLs predominantly require surgical treatment. There is growing interest in the literature in the relationship between sagittal malignment and SL grade, particularly in the assessment of pelvic parameters (pelvic incidence [PI], sacral slope [SS] and pelvic tilt [PT]) in relation to clinical and treatment. Aim: The aim of our study is to evaluate the relationship between the surgical treatment of reduction by arthrodesis of pediatric high-grade SL and the modifications in pelvic parameters. Materials and Methods: We conducted a single-center retrospective observational study. We included a total of 35 patients diagnosed with ontogenic spondylolisthesis [SL] grade III or IV according to Meyerding who were treated surgically in a period from January 2016 to December 2020. We included patients aged between 10 and 18 years. We divided our study population into two groups according to the calculation of preoperative pelvic parameters in balanced (Group 1) and unbalanced (Group 2). All included patients had a clinical and radiographic follow-up period of at least two years. The following parameters were calculated for each patient: preoperative gliding percentage, Lumbosacral Angle [LSA], Lumbar Lordosis [LL], PI, SS, and preoperative and postoperative PT. Complications collected throughout the FU period included temporary or permanent nerve injury, surgical wound dehiscence or infection, and mechanical complications. Results: We included a total of 35 patients, 21 females and 14 males, in our study. The mean age of the study population was 13.6 years (8-17 years). Group 1 consisted of 17 patients, group 2 consisted of 18 patients. The mean slip magnitude was 78% (62% ± 85%), 65% in group 1 and 81% in group 2. The mean follow-up time was 15 months (13 ± 18 months). Slip reduction was statistically significant (from 78% to 36%) with a mean percentage reduction of 54.7% in group 1 and 59.3% in group 2. A statistically significant improvement was observed in both groups in the LSA parameter, from -19.8% to -5.9% in group 1 and from -23.1% to -7.8% in group 2. We did not find a statistically significant improvement in LL, PI, SS, PT parameters in both groups. In group 1 there were no complications, in group 2 there was a single mechanical complication that was successfully treated surgically. Conclusions: We found a significant improvement in both groups in the degree of listhesis and LSA, without obtaining a statistically significant improvement in spino-pelvic parameters. In our experience, surgical reduction treatment is the main parameter for achieving good arthrodesis and stabilization. However, further investigation is needed to define the relationship between type, amount of listhesis and pelvic orientation.
1779
RF241: Comparison of selective anterior fusion versus vertebral body tethering for the treatment of adolescent idiopathic scoliosis
Jack Williams 1 , Edward King 1 , Mathew Gallagher 1 , Sarah Abbott 1 , Tesfaladet Kurban 1 , Emily Tsang 1 , Vaseharan Suntharan 1 , Libby Gooda 1 , Timothy Bishop 1 , Jason Bernard 1 , Sebastian Siller 1 , Darren Lui 1
1 St George's Hospital, London, United Kingdom
Introduction: A comparative analysis of Selective Anterior Fusion (SAF) and Vertebral Body Tethering (VBT) was conducted to assess efficacy, impact on sagittal balance and perioperative outcomes. Material and methods: A retrospective analysis between 2014-2022 of patients with Adolescent Idiopathic Scoliosis (AIS) undergoing SAF and VBT was performed. Data was collected from British Spine Registry (BSR) and local records for a 1 year minimum follow up. Cobb angles for standing and bending radiographs (XR) pre-operatively and post-operatively were measured. Thoracic (T4-T12) and maximum kyphosis angles were recorded pre-operatively and post-operatively. Results: 64 patients were assessed, SAF (n = 44) and VBT (n = 20), with a mean age of 15.6y, F:M ratio of 9.7. In the SAF group there were 31 single major curves and in the VBT group there were 14. Mean pre-operative Cobb was 53.6° (SAF) and 51.5° (VBT). Mean post-operative Cobb was 17.7° (SAF) and 19.7° (PSF). Mean Correction Rate (CR) was greater for SAF: 67.0% (SAF) vs 61.7% (VBT). Mean Fulcrum Flexibility was higher in the SAF group: 67.3% (SAF) vs 53.4% (VBT). FBCI was greater in the VBT group: 115.6% (VBT) vs 99.5% (SAF). SAF showed a greater preservation sagittal balance. Percentage change of thoracic kyphosis angle was +4.6% (SAF) vs +33.5% (VBT). Percentage change of maximum kyphosis angle was +2.5% (SAF) vs +46.0% (VBT). VBT had lower mean blood loss 396.0 mL (VBT) vs 431.2 mL (SAF). VBT had lower occurrence of intra-operative adverse events: 0% (VBT) vs 2.3% (SAF). VBT had shorter mean operation length: 188.9 minutes vs 350.3 minutes. Conclusion: SAF is shown to have a greater Correction Rate than VBT; however, FBCI is greater in VBT due SAF being selected on patients with a greater Fulcrum Flexibility. SAF is shown to have a greater preservation of sagittal balance. VBT showed favourable perioperative outcomes when compared to SAF.
200
RF242: Functional outcome and sagittal balance in adolescent idiopathic scoliosis corrective surgery utilizing unid and conventional rods
Kuok Thong Foo 1,2 , Phaik Shan Khoh 3,4 , Han Sim Lim 2,4 , Zairul Anuar Kamarul Bahrin 2,4
1 Orthopaedic, Traumatology and Rehabilitation Department, International Islamic University Malaysia, Kuantan, Malaysia
2 Orthopaedic and Traumatology Department, Penang General Hospital, Georgetown, Malaysia
3 Orthopaedic and Traumatology Department, Hospital Sultanah Bahiyah, Alor Setar, Malaysia
4 Northern Spine Unit, Orthopaedic and Traumatology Department, Georgetown, Malaysia
Introduction: Adolescent Idiopathic Scoliosis (AIS) corrective surgery commonly utilizes pedicle screws and rods to correct the deformity. Conventionally the rod contoured was performed intraoperatively prior to rod placement. Patient-specific rods allow preoperative rod bending with personalized preoperative plan and execute patient specific sagittal alignment. This study analyzed patient’s functional outcome and sagittal balance correction utilizing either UNiD or conventional rods (CR). Material and Methods: A retrospective cohort study, where AIS patients who underwent posterior corrective surgery from 2019 until 2020 in 2 state hospitals were recruited. They were divided into two groups based on the rods utilized: UNiD rod and conventional rod. Radiographic evaluation of sagittal vertical axis (SVA), pelvic tilt (PT), and pelvic incidence-lumbar lordosis mismatch (PI-LL) parameters were recorded before and three months after operation. Surgeries were performed with the aim of achieving SVA < 40 mm, PT < 200, and PI-LL < 100. Patients were interviewed using SRS-30 questionnaires after six months post-operation to compare the functional outcome. Results: 33 patients were recruited, 18 were UNiD group and 15 were CR group. Pre- and post-operative PI-LL change in the CR group is significant (p < 0.05). Comparison of mean difference showed only the PI-LL difference is significant between UNiD and CR (p < 0.05). UNiD group showed a higher percentage of achieving planned correction in all three parameters, with 72.22% in PI-LL, 94.44% in PT, and 94.44% in SVA. In the CR group, only SVA has a higher percentage of patients able to achieve planned sagittal parameters (93.33%). Both the groups produce comparable functional outcomes scores, with a total average of 4.36 for UNiD and 4.47 for CR, out of a maximum of 5. Conclusion: UNiD rod can achieve better planned sagittal parameters compared to CR. Both UNiD and CR groups have comparable functional outcomes.
1468
RF243: Efficacy and outcomes of deformity correction in patients with healed post-tubercular kyphosis - Retrospective analysis of 45 patients managed in a single centre
Vikas Hanasoge 1 , Saumyajit Basu 1
1 Spine Surgery, Kothari Medical Centre, Kolkata, India
Introduction: Sequalae of spinal tuberculosis manifest after eradication of tuberculosis eventually leading to kyphotic deformity. The risk is higher in children compared to adults due to the destruction of the cartilaginous vertebral body with the continued growth of the unaffected posterior column. The Kyphotic deformity will eventually cause cord stretching/compression leading to paraparesis/paraplegia. The aim of surgery in these patients is to correct/prevent spinal deformity progression and to relieve cord/canal compression. We present our efficacy and outcomes of surgical management of old healed post-tubercular kyphosis patients treated in our institute. Materials and Methods: A total of 45 patients diagnosed with healed post-tubercular kyphosis who underwent deformity correction surgery in our center during the period 2007 to 2018 were retrospectively analyzed – including Demographic data, Neurological status, Radiological evaluation (Apex and Level of deformity, Pre & Post Operative Sagittal Cobb’s angle, Functional outcome (SRS-22r), and complications. Results: The mean age of the study group was 22.9 years (2-68). The mean follow-up period was 3.2 years (1.2 – 11). The apex of the deformity was in the thoracic, Thoraco-dorsal, or lumbar spine in 26, 13, and 6 cases respectively. The mean thoracic kyphosis significantly improved from pre-op Cobb’s angle of 66.48 degrees (40-120) to post-op Cobb’s angle of 21.9 degrees (8-45). All patients underwent deformity correction by PSO (19 cases), Trans-pedicular Decancellation osteotomy (17 cases), VCR (9 cases) with pedicle fixation cranial and caudal to the osteotomy site. Pre-operatively 71.1% of patients had neurological deficits of which ASIA D (24%) had complete recovery, ASIA C (35%) had either complete or improvement in one grade of neurology but ASIA A patients (6.6%) had no neurological recovery at the end of follow up. The overall complication rate was 20% including 2 neurological (intra-op drop in Neuromonitoring signals) and 7 non-neurological (PJK, Rod Breakage, Implant prominence). The functional score measured with SRS-22r questionnaire improved post-correction (preoperative: 2.2 ± 0.3 and at last follow-up: 4 ± 0.3). Conclusion: Post-tubercular kyphosis corrections are safe and effective offering good clinic-radiological and functional outcomes. Neurological recovery can be expected of at least one grade from ASIA C, ASIA D and in some cases of ASIA B but no Neurological recovery occurred in patients of ASIA A. Complications are anticipated in these cases due to the severity of the deformity.
1501
RF244: Robotic assisted minimal invasive surgery for neuromuscular scoliosis in children: a minimum 2 year follow up study
Josh Schroeder 1 , Leon Kaplan 1 , Ohad Einav 1
1 Orthopedic Surgery , Hebrew University Hadassah Medical Center, Jerusalem, Israel
Introduction: Neuromuscular scoliosis (NMS), a complex spinal deformity often arising from neurological or neuromuscular disorders, presents unique surgical challenges in pediatric patients. Traditional open surgical approaches have historically been associated with increased morbidity due to the extent of the surgery. Robotic-assisted minimal invasive surgery (RAMIS) allows precise instrument placement in spinal surgeries with a reduced exposure. In pediatric neuromuscular scoliosis, RAMIS offers a minimally invasive alternative to conventional open procedures. This approach utilizes smaller incisions, reduces muscle dissection, and employs robotic precision to achieve spinal realignment while minimizing tissue trauma. The indications for RAMIS are long C type curves with a apex at the lumbar or thoracolumbar junction. Materials and Methods: During the years 2018-2022, children with NMS who needed spine surgery in a referral center were collected. Indications for surgery, curve shape and magnitude, type of surgery performed, length of surgery and blood loss were collected. The two year outcome of these procedures was assessed. All the surgeries were performed with the assistance of a Mazor robot (Medtronic). In these patients an open surgery was performed form D11- Sacrum that included, screw placement, releases and osteotomies. Screw placement in the thoracic spine was performed via RAMIS, the rods were placed from caudal to cephalad correcting the deformity. Results: During the years 2018 – 2022 130 children with NMS were operated for scoliosis. Of them 35 were allegeable for RAMIS surgery. Surgery was planned for all children on the robotic platform from T3/4 to the Sacrum. A standard exposure was performed between T11 and the sacrum in all cases and screws were placed. Release osteotomies were performed in the lumbar area. In the thoracic spine in 28 of the 35 children screws were placed percutaneously, in 7 of the children registration of the thoracic vertebrae failed and the surgery was converted to open standard deformity correction surgery. Time of surgery was 5 hours (range 4-7 hours). Blood loss was 600 CCs. All patients were transferred to the PICU after surgery and sent to a rehabilitation hospital on POD 4-5. There were three infections in the RAMIS group, one needing a washout surgery and two others treated with antibiotics. There were no hardware related complications in the RAMIS group. Conclusion: RAMIS surgery is advantageous NM pediatric population. including reduced blood loss, shorter hospital stays, and reduced complications. Importantly, the minimally invasive nature of RAMIS preserved spinal muscle integrity in the upper spine, critical for the growing bodies of pediatric patients with compromised musculature. Additionally, the robotic platform allowed for accuracy in screw placement and spinal deformity correction, leading to minimal hardware complications.
1688
RF245: Effect of enhance recovery pathway (ERP) resulting in reduced length of stay (LOS) and opioid consumption after non fusion anterior scoliosis correction (NFASC) surgery for adolescent idiopathic scoliosis (AIS) - A single center experience
Harith Reddy 1 , Sharan Achar Thala 1 , Akshya Raj 1 , Umesh Kanade 1 , Keyur Akbari 1 , Vignesh Badikillaya 1 , Appaji Krishnan 1 , Vasantha Roopan C 1 , Sajan Hegde 1
1 Spine Surgery, Apollo Hospitals, Chennai, India
Introduction: There have been several reports on enhanced recovery pathway (ERP) in patients undergoing posterior spinal fusion (PSF) for AIS resulting in early recovery and mobilization, decreased usage of opioids, and reduced LOS. However, there is a paucity of literature emphasizing its role in AIS patients undergoing NFASC. Material and Methods: Pertinent data of consecutive 35 AIS patients who underwent NFASC with Lenke 1 and Lenke 5 curves with a minimum of 1 year of follow-up were analyzed. Patient demographics, post-op analgesia, mobilization, patient satisfaction survey score with respect to information and care, and 90 days complications were collected. Results: Pertinent demographic and operative data of 35 AIS patients were analyzed. The average time to commencing solid food was 6.5 ± 1.5 hrs. The average time to mobilization following surgery was 15.5 ± 4.3 hrs. 20 patients had a urinary catheter and the average time to removal of the catheter was 17.5 ± 1.4 hrs. 25 patients had a chest tube and the average time to removal of chest tube was 25.5 ± 3.2 hrs. The average duration to the stopping of the epidural was 42.5 ± 3.5 hrs. Average opioid usage was much lower. The average duration to transition to oral analgesia was 55.5 ± 8.5 hrs. The post-op pain VAS scores declined gradually with the ERP pathway. The mean LOS was 3.1 ± 0.5 days. No patient had a blood transfusion or any other complications. No correlation was found between LOS and initial cobb angle. The average patient satisfaction score for both information and care were 8.9 ± 0.5 and 9.1 ± 0.4 respectively. Conclusion: ERP in AIS patients undergoing NFASC results in reduced LOS and indirectly the cost, post-op opioid use, early mobilization, enhance patient recovery, and overall improve patient satisfaction score.
256
RF246: Scoliosis and kyphosis prevalence in Turner syndrome: a retrospective review at a pediatric tertiary care medical center
Manasa Pagadala 1 , Jeremy Marx 1 , John Carney 1 , Erik Gerlach 1 , Peter Swiatek 1 , Jennifer Zabinsky 1 , John Sarwark 1 , Wendy Brickman 1 , Reema Habiby 1
1 Department of Orthopaedic Surgery, Northwestern University Feinberg School of Medicine, Chicago, USA
Introduction: The prevalence of major coronal and sagittal spinal curves (scoliosis and kyphosis) in Turner syndrome (TS) is not well established due to limited reporting. The relationship between growth hormone (GH) therapy and its effect on TS spinal curve incidence is also not well established. Material and Methods: A retrospective chart review of 306 TS patients from 2007 to 2021 evaluated major coronal and sagittal spinal curves, progression of the curve, and treatment with GH. Statistical significance (defined as p < 0.05) between curvature rates and curve progression was compared between GH-treated patients and non-GH-treated patients using a χ 2 or Fisher exact test when appropriate. Results: Thirty-seven of 306 (12%) TS patients had a radiographically relevant spinal deformity. Twenty-seven of 37 (73%) had mild; 4 of 37 (11%) had moderate, and 6 of 37 (16%) had severe curves. Of those with severe, 4 underwent spinal fusion, 1 was treated with bracing, and 1 was braced before a cardiovascular-related death. Regarding GH use among TS patients, 190 of 306 (62%) used GH versus 116 of 306 (38%) who did not. Of those with a spinal curve, 24 of 37 (65%) used GH compared with 13 of 37 (35%) who did not. On univariate analysis, GH therapy was not a risk factor for the diagnosis of a major spinal curve, a more severe degree of the curve at the time of diagnosis, or spinal curve progression (p > 0.05 for all). Conclusion: This is the largest single institution retrospective review of a TS cohort known to the authors assessing spinal curve prevalence and relation to GH treatment and demonstrates a TS spinal curve rate of 12% (37/306). Four of six (11%) TS patients with a severe curve underwent corrective spine fusion. There was no relationship between the use of GH and the presence of a spinal curve or curve progression. Further study is warranted to determine risk factors for curve progression.
67
RF247: Can the apex in early onset scoliosis (EOS) be controlled through posterior tethering with non-fusion instrumentation? A single center experience
Alexander Schupper 1 , Majid Dawik 2 , Farah Shahin 2 , Mohammad Awad 2 , Haya Warasna 2 , Mohamad Banat 2 , Bashar Awad 2 , Alaa Azmi Ahmad 2
1 Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, USA
2 School of Medicine, Orthopedic Surgery, Palestine Polytechnic University, Hebron, Palestine
Introduction: Both growth-guided and compression-based interventions have been assessed for Early Onset Scoliosis, each with its own merits and shortcomings. Active Apex Correction (APC), a hybrid strategy featuring replacing a traditional SHILLA with apex growth modulation through unilateral compression on the convex side, has been shown to be safe and effective for Early Onset Scoliosis. Decreasing the rate of arthrodesis at the apex has been shown to decrease the incidence of the crankshaft phenomena. However, the rate of facet fusion in the APC technique has not been well described. Aims/Objectives: To determine the rate of Apex arthrodesis in children with Early Onset Scoliosis receiving treatment with the APC technique. Methods: Patients with Early Onset Scoliosis treated with the APC technique as the index surgery at a single institution were retrospectively enrolled. Patient demographic data and preoperative radiographic data was collected. Postoperative CT imaging was collected with minimum 1-year follow up to determine rates of bony facet fusion at the apical levels. Apical levels where the instrumentation prohibited measurement of facet fusion were excluded from analysis. Patients without at least 1-year follow up, any surgery before APC were excluded. Postoperative complications were recorded. Univariate statistics were performed with Student’s t-test, with significance level at p = 0.05. Results: Nine patients received APC as the index surgery for Early Onset Scoliosis with at least 1-year follow up. The average age of surgery was 5.2 years, and 78% of cases were congenital, with the remaining juvenile idiopathic or neuromuscular. Mean patient follow up was 30 months. The most common facet levels assessed were L2-3 (7 patients), L1-2 and L3-4 (6 patients) and T12-L1 (5 patients). In total 80 facets in the tethered apex were evaluated, with 62 (77.5%) facets demonstrating clear radiological evidence of no fusion, while the remaining 18 facets could not clearly be determined due to instrumentation artifact. The mean intra-facet distance was 1.11 ± 0.57 mm on the convex side, compared to 1.17 ± 0.61 mm on the concave side (p = 0.466). Conclusions: APC for Early Onset Scoliosis offers patients a modulatory correction, without creating facet fusion at the apical levels, limiting the crankshaft phenomena seen in cases resulting in arthrodesis at apical levels.
1910
RF248: Vascular complications in anterior scoliosis tether surgery
Evan Davies 1
1 Southampton Childrens Hospital, Southampton, United Kingdom
Introduction: Anterior Tether surgery in the management of adolescent idiopathic scoliosis is increasing in incidence. Anterior spinal vascular anatomy can be compromised by prominent and malpositioned metalwork. Material and Methods: We present two cases of vascular complications in anterior tether surgery performed for adolescent idiopathic scoliosis. In the first case the patient presented with post operative haemothorax of 2 litres. Long sharp screws excoriated the descending aorta causing a mediastinal bleed. In a second patient renal and adrenal vascular anatomy was compressed and haemorrahge caused by prolonged screws. Results: Both patients required implant removal in order to improve curtail haemorrhage and persistent visceral bleeding. Each patient required vascular and cardiac surgical team involvement in order to have cardiac bypass and endovascular support. Both patients had removal of anterior spinal implants without requirement for vascular stenting or bypass. Both had delayed traditional posterior scoliosis surgery a year post tether removal without complication and return of scoliosis correction. Conclusion: Prominent malplaced anterior spinal metalwork has the potential to cause vascular injury in the anterior spine. Anatomical placement of screw heads and long screws with prominent sharp screws can lead to penetration and excoriation of vascular anatomy. Attention to surgical anatomy, use of dedicated anterior systems should reduce the incidence of these injuries. Prompt recognition of unanticipated blood loss and haemorrahge should lead to urgent assessment and prompt removal in a complex surgical environment. This requires multidisciplinary working with vascular and cardiac teams involved and available to support the surgery.
1833
RF249: Lights and shadows in the surgical treatment of early-onset scoliosis by conventional and magnetic growing rods
Antonio Parciante 1 , Chiara Cini 1 , Francesco Vommaro 1 , Giovanni Ciani 1 , Bruna Maccaferri 1 , Alessandro Gasbarrini 1
1 Spine Surgery, Istituto Ortopedico Rizzoli, Bologna, Italy
Objective: The implantation of lengthening systems now represents the Gold Standard for the treatment of infantile and juvenile scoliosis (early and late onset sec. Dickens), definitive arthrodesis being contraindicated in early onset scoliosis (EOS) before the age of 10 years. Traditional mechanical lengthening systems, "classic growing rods" (CGR), require multiple lengthening surgeries under general anesthesia about every 8-10 months with a high impact both psychologically for the patient and family and in terms of health care costs. Therefore, there has been increasing development of magnetic lengthening systems (MCGR-type systems) that, through bars that lengthen according to the physiological growth of children, avoid repeated surgeries. However, both systems have limitations: the former require numerous lengthening surgeries while, the latter, a high number of complications, mostly mechanical. This is the context of this study, the purpose of which was to compare the two surgical techniques CGR and MCGR to which patients with EOS underwent, highlighting the mechanical complications encountered such as proximal junctional kyphosis (PJK) or failure of the posterior fixation. Materials and Methods: A retrospective case-control review was conducted of a homogeneous group of 42 patients by extent of curve and age < 10 aa who underwent surgery at a single center (Rizzoli Insitute Bologna – Italy). Nineteen were treated with Magec-type MCGR system and 23 with CGR. Both growing rod systems were applied with standard surgical technique, i.e., under general anesthesia, patient prone, with antibiotic therapy induction. The surgical technique made use of standard posterior median incision and use of sublaminar hooks proximally and pedicle screws distally, connected by rods of Diameter = 5.5 mm. In the MCGR group, noninvasive magnetic lengthening was performed on average every 2 1/2 months while, in the CGR group, the patient underwent surgical distraction with an average of about 10 months. Results: From the authors' experience, there was a significant reduction in complications and a major curve correction in favor of the mechanical CGR system. In 7 of 23 patients undergoing surgery by CGR, failure of posterior fixation or PJK was found. Late surgical complication was found in 6 of 19 patients undergoing distraction surgery by MCGR system. Conclusion: Comparison of the two techniques showed that both have limitations but the CGR system allows better correction and curve management than the magnetic system. In fact, according to the authors, the most relevant difference between the two systems lies in the actuator that allows shaping the bars giving global kyphosis in the CGR, contrary to the MCGR where it is not modifiable. However, improvements of the present study may be its extension to a larger population and further technical insights on the parameters to be considered for the comparison between the mechanical and magnetic system.
2367
RF250: A survey of functional outcome of patients undergoing surgery for adolescent idiopathic scoliosis
Lucia Tavares 1
1 Orthopaedics, Barts, Health Trust, Royal London Hospital, London, United Kingdom
Introduction: Adolescent idiopathic scoliosis (AIS) can lead to significant physical and mental distress amongst children leading to surgical correction. The outcome of surgery is based on clinical, radiological measurements and patient reported outcome measures. We report the results of a qualitative survey on patients who underwent surgery for AIS with at least two years follow up. Material and Methods: Twenty nine patients undergoing deformity correction surgery were included in the survey questionnaire electronically at two years after spine surgery. All patients underwent posterior spinal thoracolumbar fusion. All questions were based on the Scoliosis research Society (SRS 22 questionnaire). Results: Severe to debilitating back pain was reported by 44.8% patients and pain even at rest was reported by 13.8 % although 24.1% responders confirmed taking regular opiate or non-opiate pain killers at 2 years. Forty eight percent of patients had little or no anxiety about surgery and 41.37% patients did not feel that their deformity or back pain had progressed after surgery. Ninety six percent reported going back to activities of daily living with normal sports being undertaken by 44.6 % patients. Finally 60.7 % percent patients reported significant improvement to their self-image and 69% reported feeling attractive again after surgery with 82.7 % denied any impact of surgery in their personal relationships. Satisfaction after surgery was reported by 65.5% subjects. Conclusion: This survey reflects patient’s attitude after deformity correction surgery at 2 years interval. This data can be sued to consent and counsel patients and help to manage patient expectations whilst planning corrective surgery for AIS.
1773
RF251: Selective hemivertebrae resection in adolescent and young adult congenital scoliosis with multiple hemivertebrae : a review of the management at a single center
Jie Zhou 1 , Yong Qiu 1 1 , Zezhang Zhu 1 , Saihu Mao 1
1 Division of Spine Surgery, Department of Orthopedic Surgery, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, China
Introduction: Treatment of congenital scoliosis caused by multiple hemivertebrae (MHV) is complicated and controversial. There has been a noticeable absence of in-depth guideline that convey effective coping strategies for this rare condition. This study is to conduct a retrospective review of the selective resection strategies, their immediate efficacy, as well as the progression of residual deformity associated with the unresected hemivertebra in adolescentsand young adult congenital scoliosis. Material and Methods: A total of 29 patients with MHV were enrolled from July 2009 to July 2022. They were categorized into complex MHV group (CMHV: ≥ 4 HVs, coronal imbalance, kyphosis > 70°, contralateral bone bridge/> 3 fused rids, sacral dysplasia/torticollis) and otherwise simple MHV group (SMHV). The selective resection strategies were reviewed. Data being recorded involved number and reason of selective HV resection, correction rate and curve progression of residual HV. Results: 29 MHV patients comprising 17 males and 12 females were recruited. The number of hemivertebrae averaged 2.7, and the main scoliosis reached 66.0°. 14 were classified into CMHV group. In the SMHV group, the number of HV resection were 0 in 6 patients and 1 in 9 patients. As to the CMHV group, the number of HV resection were 0 in 3 patients,1 in 7 patients and 2 in 4 patients. Conclusion: A sophisticated analysis analysis of the number, location, interrelationships of MHV and concomitant rib deformity to identify the driver of major deformity/imbalance was essentially important for design of tailored selective HV resection.
1772
RF252: 3D printed custom navigation jigs in posterior spinal fusion: a retrospective case series analysis of 55 patients
Libby Gooda 1 , Samuel Walters 2 , Bisola Ajayi 2 , Emily Tsang 1 , Jack Williams 2 , Sarah Abbott 2 , Mohamed Abdalla 2 , Mathew Gallagher 2 , Timothy Bishop 2 , Jason Bernard 2 , Darren Lui 2
1 St. George's University of London, London, United Kingdom
2 St. George's University Hospital, London, United Kingdom
Introduction: The use of 3D printing in spinal surgery is a recognized technique. Pedicle cannulation in a deformed spine with occasionally hypoplastic pedicles can be technically challenging and risky. For this reason, navigational techniques are often utilized. Current available techniques often require intra-operative CT scanning which can increase intra-operative time and disrupt the workflow. A whole spine, low dose, 1mm axial cut CT scan is used to create a life-size model of the spine, to which 3D printed custom navigation jigs (3DPCNJ) are created unique to each vertebra. This case series aims to elucidate the safety and efficacy of these jigs in the surgical treatment of adolescent idiopathic scoliosis. Material and Methods: 55 scoliosis patients with posterior spinal fusion using 3DPCNJ at a tertiary medical center had data collected prospectively for time and blood loss during screw insertion (and facet osteotomies). Our standard free hand technique is to perform a facet osteotomy prior to screw insertion and thus was studied in this manner to allow for comparison in future studies. Demographics, patient-reported outcomes (SRS-22), intra-operative parameters, and radiographic measurements were collected retrospectively. Results: The mean age was 15.9 and female patients comprised 80% of the cohort. The mean screw density 82.9%. Mean time for screw insertion was 83.1 minutes (average 4.1 minutes per screw/osteotomy). Total blood loss during screw insertion and all facet osteotomies was 167.8 ml (average 8.2 ml per screw/osteotomy). There were two spinal cord monitoring events in one case. They were both reversible. The average hospital length of stay was 5.9 days with one patient returning to theatre due to a loose implant. SRS-22 preoperatively was 3.43 vs. 4.38 postoperatively (12 months). The average improvement in SRS-22 scores at last available follow-up is 0.46. The preoperative Cobb angle was 63.9 vs. 28.8 postoperatively. Conclusion: The time taken for segmental facet osteotomies and pedicle screw insertion using 3DPCNJ has been shown to be efficient, rapid, effective, and safe with minimal blood loss. The average screw density was 82.76%, suggesting that the use of 3DPCNJ allows for high density screw constructs which may provide a better correction and mitigate screw pull out. Radiographic parameters and PROMS improve in line with other gold standards but 3DPCNJ has an advantage over other navigation techniques due to uninterrupted workflow with no intraoperative CT scanning or accidental loss of accuracy.
RFP15: Deformity-Adult and Adolescent
613
RF253: Modic changes in a large animal model of intervertebral disc degeneration
Andres Bonilla 1 , Brad Nelson 1 , Jeremiah Easley 1
1 Clinical Sciences, Colorado State University, Fort Collins, USA
Introduction: Modic changes (MCs) represent alterations in MRI signal intensity within the vertebral bone marrow, often seen adjacent to deteriorated Intervertebral discs. Over the years, their importance has grown as multiple studies have indicated a direct link between MCs and the diagnosis of Intervertebral Disc Degeneration (IDD), a primary contributor to low back pain. As obtaining human tissue samples is challenging, animal models become pivotal to comprehend the emergence and significance of MCs. Although research literature underscores the value of studying MCs, detailed analyses in large animal models remain sparse. This study's aim was to categorize the MCs observed on MRIs of mature sheep with IDD. As a significant large animal model for IDD, sheep can be instrumental in deepening our understanding of MCs' variability in relation to IDD progression. Material and Methods: Three sheep were utilized to study the progression of degeneration after inducing IDD via partial discectomy at the L2-L3, L3-L4, and L4-L5 levels. The Colorado State University Animal Care and Use Committee approved this study. MRI scans (3 Tesla) were taken pre-surgery and again at 8, 16, and 30 weeks after the procedure to track disc degeneration and monitor the emergence or alteration of MCs. The scans utilized T1W and T2W sequences in a sagittal view, capturing from the L1 caudal to the S1 cranial endplate (covering 36 endplates). A blinded observer analyzed the images using an imaging software (Horos). The collected data was subjected to a variance analysis between the different time points. Results: In the baseline MRI assessment of the 36 endplates (ranging from L1 Caudal to S1 Cranial), only two endplates exhibited type 2 MCs. With the passage of time, there was an evident surge in these changes. At the 8-week mark, type 2 MCs appeared on four endplates. This count rose to eight by the 16-week point. By 30 weeks, a total of 11 endplates showed MCs of type 2. This pattern indicates a steady increase in the endplates demonstrating MCs throughout the research duration. Notably, these shifts were not consistent across the entire spine but were majorly concentrated in the final lumbar segments, notably the L4-L5, L5-L6, and L6-S1 intervertebral spaces. The number of MCs over time revealed statistical differences, especially when comparing the baseline (0 weeks) to the study's conclusion (30 weeks). The rapid emergence of these MRI manifestations within a limited timeframe emphasizes the potential dynamic of MCs in this animal model of IDD. Conclusion: This study offers crucial understanding into the rapid progression of Modic changes type 2, emphasizing the evolving nature of spinal degenerative alterations. Additionally, the specific localization of these changes delivers essential direction, informing targeted therapeutic strategies for optimal patient outcomes.
1715
RF254: Should the pelvis be included? An analysis of Distal Junctional Failure risk factors in correcting Adult Spinal Deformity with fusion to L5
Domenico Compagnone 1 , Riccardo Cecchinato 1 , Andrea Pezzi 1 , Francesco Langella 1 , Marco Damilano 1 , Andrea Redaelli 1 , Daniele Vanni 1 , Claudio Lamartina 1 , Pedro Berjano 1
1 GSpine4, IRCCS Ospedale Galeazzi - Sant'Ambrogio, Milan, Italy
Introduction: The aim of the present study is to identify the risk factors for distal junctional failure (DJF) in patients treated for adult spine deformity with fusion to L5 and to highlight the significance of preoperative assessment, surgical decision-making, and postoperative care. Material and Methods: This is a retrospective study of data collected prospectively on the local institutional spine surgery registry (2016-2021). All patients older than 18 years, with a diagnosis of adult spine deformity who underwent long posterior instrumentation to L5 and had a minimum follow-up of 2 years were included in the study. Included patients were divided into two groups, according to whether or not they had developed a DJF. Demographic and radiographic data, corrective strategy, preoperative level of degeneration at L5/S1 and GAP score were compared between the two groups. Results: Forty-eight patients (n = 48) underwent adult deformity surgical correction and long fusion to L5 satisfied eligibility criteria. At two years follow-up, nine patients (18.7%) developed a DJF that required surgical revision. Thirty-nine patients did not present distal junctional complications. Patients with or without DJF showed significant differences in terms of preoperative spinopelvic parameters (PT: 28°± 6° vs. 23°± 9°, p-value 0.05; DJF group vs. not DJF) and degeneration of L5-S1 (Pfirmann grade L5-S1 disc 3.7 ± 1.0 vs. 2.6 ± 0.8, p-value 0.001; DJF group vs. not DJF) (L5-S1 Facet joint Osteoarthritis 3.1 ± 0.8 vs. 2.4 ± 0.8, p-value 0.023; DJF group vs. not DJF). Conclusion: DJF following spinal deformity correction surgery is influenced by a combination of patient-related, surgical and implant-related factors. Fusion construct length, preoperative and postoperative sagittal alignment and the grade of degeneration of the distal disc have been identified as significant risk factors. Surgeons should carefully evaluate these factors and employ appropriate strategies.
409
RF255: The role of function and morphology of paraspinal muscles on the cascade of sagittal imbalance
Gengyu Han 1 , Weishi Li 1
1 Department of Orthopaedics, Peking University Third Hosptial, Beijing, China
Introduction: The role of paraspinal muscle degeneration on the cascade of sagittal imbalance is still indistinct. This study aimed to compare paraspinal muscle degeneration in the four stages of sagittal imbalance including sagittal balance (SB), compensated sagittal balanced (CSB), decompensated sagittal imbalanced (DSI) and sagittal imbalance with failure of pelvic compensation (SI-FPC), and to explore whether the evaluations of paraspinal muscle function and morphology have different effects on the sagittal spinopelvic alignment in lumbar spinal stenosis (LSS) patients. Material and Methods: This is a cross-sectional study of 219 consecutive hospitalized LSS patients. The isometric paraspinal extensor endurance test and imaging evaluation of atrophy and fat infiltration of paraspinal extensor muscles (PEM) and psoas major (PS) on magnetic resonance imaging were performed at baseline. Spinopelvic measurements included lumbar lordosis, pelvic tilt, sacral slope, pelvic incidence (PI) and sagittal vertical axis (SVA). We also calculated the relative pelvic version (RPV) and relative lumbar lordosis (RLL) to eliminate the impact of discrepancy of PI. Results: The LSS patients were divided into four groups based on the combination of RPV and SVA: SB group (-7° ≤ RPV < 5° and SVA ≤ 5 cm, n = 67), CSB group (RPV < -7° and SVA ≤ 5 cm, n = 85), DSI group (RPV < -7° and SVA > 5 cm, n = 49) and SI-FPC group (RPV ≥ -7° and SVA > 5 cm, n = 17). No significant difference of PI was found among the four groups (p > 0.05). There were significant differences of paraspinal muscle endurance and morphology among the four groups (all p < 0.05). Besides, moving from the SB group to the DSI group, there was progressive deterioration in PEM atrophy, RPV and RLL (all adjusted p < 0.001). Moreover, the SI-FPC group exhibited poorer paraspinal muscle endurance than either the SB or the CSB groups, while no significant differences of paraspinal muscles were found between the SI-FPC and the DSI groups. In multiple linear regression analyses, paraspinal muscle endurance and relative functional cross-sectional area (rFCSA) of PEM were independent predictors for SVA, and rFCSA of PS was the one for RPV. Conclusion: We completed the new perspectives regarding different roles of paraspinal muscle degeneration that it is not only an initiating factor of pelvic retroversion, but a risk factor to aggravate patients from compensatory to decompensatory stage. Furthermore, the impairment of muscle function at the early stage might be the reason why patients occurred failure of pelvic compensation. In addition, the evaluations of paraspinal muscle function and rFCSA of PEM and PS had different clinical values on the sagittal balance.
2373
RF256: Risk factors of adjacent segment disease after short-segment fusion in patients with de novo degenerative lumbar scoliosis
Se-Jun Park 1 , Jin-Sung Park 1 , Dong-ho Kang 1 , Hyun-Jun Kim 1
1 Orthopedic Surgery, Samsung Medical Center, Seoul, South Korea
Introduction: Short-segment fusion (SSF) is an effective surgical option for appropriately selected patients with de novo degenerative lumbar scoliosis (DNDLS). Considering that DNDLS is frequently accompanied by multi-segment degeneration and potential instability across the entire lumbar segments, it is inevitable that unhealthy segments remain after SSF, thereby increasing the potential risk of adjacent segment disease (ASD) occurrence. Therefore, we aim to identify the risk factors for ASD in patients with DNDLS who underwent SSF. Material and Methods: This retrospective study included 80 patients with DNDLS (Cobb angle > 10°) who underwent SSF (1 or 2 levels) between December 2010 and July 2018 with a minimum follow-up duration of 5 years. The participants were divided into two groups: ASD and non-ASD. ASD was defined as clinical ASD rather than radiographic ASD. Various patient and operative variables were compared between the groups. Global and regional radiographic parameters (pre- and post-operatively) were also compared between the two groups using plain radiograph and MRI. Consequently, univariate and multivariate analyses were conducted to identify the risk factors for ASD occurrence. The receiver operating characteristic (ROC) curve was used to calculate the cutoff values. Results: The mean age was 67.7 ± 7.2 years at the time of SSF, and there were 62 women (77.5%) enrolled in the study. Thirty patients (37.5%) were in the ASD group and 50 patients (62.5%) were in the non-ASD group. Average time from the surgery to ASD diagnosis was 34.9 ± 28.2 months in ASD group. Thirteen patients required revision surgery at a mean time of 8.8 ± 7.0 months after ASD occurrence. A multivariate logistic regression analysis demonstrated that preoperative disc wedging angle (p = 0.001, odds ratio [OR] = 1.806, 95% CI = 1.255 - 2.598), presence of facet tropism [defined as ≥ 10° of facet joint angle between the right and left sides] (p = 0.009, OR = 5.534, 95% CI = 1.528 - 20.040), and foraminal stenosis ≥ grade 2 (p = 0.025, OR = 5.935, 95% confidence interval [CI]=1.253 - 28.117) were significant risk factors for ASD development. The cutoff value of the preoperative disc wedging angle was calculated to be 2.5° using the ROC curve. Conclusion: Preoperative disc wedging angle ≥ 2.5°, presence of facet tropism, and foraminal stenosis ≥ grade 2 were identified as significant risk factors for ASD development after SSF in patients with DNDLS.
1306
RF257: Return to activities of daily living after fusion to the pelvis for adult spinal deformity
Omri Maayan 1 , Bo Zhang 1 , Mitchell S. Fourman 1 , Anthony Pajak 1 , Hiroyuki Nakarai 1 , Leah Andrews 1 , John Clohisy 1 , Robert Merrill 1 , Jerry Du 1 , Francis Lovecchio 1 , Han Jo Kim 1
1 Hospital for Special Surgery, New York, USA
Introduction: No prior studies have assessed the extent and timing of return to employment, driving, and walking without a postoperative assistive device among a single cohort of adult spinal deformity patients. Therefore, the objective of the present study was to investigate return to activities among adult spinal deformity patients following long-segment fusion to the pelvis. Material and Methods: Patients who underwent thoracolumbar adult spinal deformity surgery between 2016-2021 with ≥ 1 year follow-up were included (posterior-only, ≥ 3 levels of fusion to pelvis). A cross-sectional survey was implemented to evaluate both preoperative and postoperative activity tolerance. Patients were categorized into two groups based on their postoperative activity tolerance: (1) Better/Unchanged or (2) Worse. Differences in demographics and perioperative variables between patients reporting better/unchanged and worse activity tolerance were assessed. Results: 95 patients were included (mean age: 64.3 ± 10.1 years; BMI: 27.3 ± 6.1 kg/m2; levels fused: 8 [range 3-16]; LL correction 17.8 ± 11.3°; follow-up: 43.5 months). Most patients endorsed improved capacity to walk (improved: 64.2%, unchanged: 17.9%, worse: 17.9%) and navigate stairs (improved: 52.6%, unchanged: 33.7%, worse: 13.7%) postoperatively. A total of 75 (97.4%) patients returned to driving (4.1 ± 10.8 months postoperatively) and 44 (88.0%) patients returned to work (5.4 ± 8.0 months postoperatively). Patients with decreased walking tolerance were more likely to have a greater LL correction (37.2 ± 10.5° vs. 18.6 ± 16.7°, p = 0.02) and exhibit worse patient-reported outcomes at long-term follow-up (40.2 ± 11.0 vs. 48.0 ± 9.6, p = 0.03). Patients with decreased ability to navigate stairs were more likely to have undergone revision fusion (69.2% vs. 28.0%, p = 0.003) and have a greater body mass index (30.7 ± 5.8 vs. 26.7 ± 6.0 kg/m2, p = 0.04). Patients requiring the use of a postoperative assistive walking device were also more likely to have undergone revision fusion (66.7% vs. 27.5%, p = 0.003), exhibit a greater body mass index (31.4 ± 7.2 vs. 26.5 ± 5.6 kg/m2, p = 0.004), longer operative times (285.1 ± 79.9 vs. 244.5 ± 63.4 minutes, p = 0.03), and worse patient reported outcomes at long-term follow-up (39.9 ± 5.1 vs. 47.7 ± 10.5, p = 0.04). Conclusion: Most patients experienced improvements in their capacity to walk and navigate stairs postoperatively, as well as successful return to both driving and work. Greater lumbar lordosis correction, higher body mass index, and revision fusion were the most commonly implicated factors among patients expressing reduced postoperative activity tolerance. These findings suggest that despite the reduced range of motion caused by fusion to the pelvis, deformity surgery is successful in improving patients’ daily functioning.
778
RF258: Does pedicle subtraction osteotomy at APEX+1 level affect the clinical and radiographic outcomes in patients with degenerative kyphosis?
Hui Xu 1 , Zhen Liu 1 , Zezhang Zhu 1 , Yong Qiu 1
1 Nanjing Drum Tower Hospital, Jiangsu Province, Nanjing, China
Introduction: Traditionally, in patients with DK, to restore optimal sagittal alignment, PSO was frequently performed at the apex level of the kyphotic curve. However, an osteotomy at apex+1 level was preferred by spine surgeons due to technical feasibility and safety. Tang et al reported that PSO level could affect the correction of kyphosis and sagittal imbalance. However, several studies reported that the degree of PSO resection correlated more with spinopelvic parameters than the PSO level. Therefore, the possibility exists that PSO at one level below the kyphotic apex (apex+1) in some selected DK patients could achieve similar correction effects. The purpose of this study was to compare the clinical and radiographic outcomes of patients with degenerative kyphosis (DK) who underwent pedicle subtraction osteotomy (PSO) at the apex vertebra versus those who received PSO at the apex+1 level. Methods: We retrospectively reviewed 49 DK patients with a minimum follow-up of 2 years who underwent single level PSO from January 2015 to November 2020. Patients were divided into two groups based on PSO level: PSO at the apex (APEX group) or PSO at one level below the apex (APEX+1 group). The following radiographic parameters, including global kyphosis (GK), thoracic junctional kyphosis (TJK), sagittal vertical axis (SVA), distance from sacrum to apex (DSA), lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), sacral slop (SS), and T1 pelvic angle (T1PA) were measured at pre-operation, post-operation and the final follow up. Clinical outcomes were evaluated by the Scoliosis Research Society-22 questionnaire (SRS-22), the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI), Lumbar Stiffness Disability Index (LSDI), Oswestry Disability Index (ODI), and Visual Analog Scale (VAS). Results: 37 patients of 1 male and 36 female, aged 57.2 ± 6.2 years old were enrolled in the present study. APEX+1 group showed significantly larger DSA than APEX group at post-operation (31.2 ± 28.6 vs. 15.8 ± 11.5, p = 0.04) and final follow-up (38.7 ± 21.0 vs. 24.4 ± 11.9, p = 0.015). APEX+1 had larger postoperative TJK than APEX group (16.9 ± 3.5 vs 11.8 ± 5.6, p = 0.002). This trend was also continued at the final follow up (18.8 ± 3.8 vs 14.3 ± 6.6, p = 0.015). In addition to DSA and TJK, global sagittal parameters were similar between the two groups (p > 0.05). Higher LSDI were observed in APEX+1 group at final follow up (21.9 ± 4.6 vs. 25.4 ± 4.3, p = 0.027). Comparison of the CPSQI between two groups showed that APEX+1 group is inclined to have poor sleep quality during follow-up period, presenting with impaired sleep duration (0.78 ± 0.43 vs. 1.21 ± 0.54, p = 0.010), daytime dysfunction (1.00 ± 0.00 vs. 1.21 ± 0.42, p = 0.042), and total PSQI (4.72 ± 1.45 vs. 6.16 ± 2.36, p = 0.033). Conclusions: Generally speaking, PSO at apex+1 could achieve satisfactory radiographic outcomes for patients with DK, indicating the feasibility of performing PSO and APEX+1. Although impaired sleep quality and increased lumbar stiffness were observed, most patients were satisfied with function and pain relief.
1987
RF259: Outcome of incidental durotomy repair in thoracolumbar spine surgery - An institutional experience with orthopaedic residents
Sandesh Agarawal 1 , Manoj Ramachandriah 1
1 Department of Orthopaedics, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, India
Background: The occurrence of incidental durotomies (IDs) following spinal operations is a widely recognized issue. Complications such as poor outcomes, extended hospitalization, prolonged immobilization, infections, and revision surgeries are all potential consequences of inadequate durotomy management during the initial surgery. This study aims to describe the outcomes of ID repair in thoracolumbar spine surgery in terms of the Oswestry Disability Index (ODI) score and visual analog scale (VAS) when performed with the active involvement of orthopaedic residents in the surgical procedure. Methodology: Between April 2021 and April 2023, a hospital-based observational study was conducted among 110 patients hospitalized in the orthopaedic ward at R.L. Jalappa Hospital and Research Centre in Kolar, Karnataka, who required IDs due to an accidental dural tear or a postoperative CSF fluid leak following thoracolumbar spine procedures. Patients with a previous history of thoracolumbar spine surgery, vertebral tumour’s, spinal metastasis, infections, e.g., spondylodisctis, or Pott's spine were excluded. The ODI score and VAS score were calculated on the postoperative day, one month, and three months following surgery. Results: The mean age of the study participants was 62.81 + 10.49 years, with a male preponderance of 67.2% among the study participants. The mean BMI of study participants was 23.77 kg/m2. Approximately 24.5% of participants had a prior history of spinal surgery. Among 110 patients, 32 had postoperative complications. Six patients reported experiencing urinary retention, followed by five with CSF leakage and one with a postural headache (five cases). Based on the ODI score, mild disability was seen in 32.7% of the study samples at three months of follow-up. Based on the VAS score, moderate pain was seen among all the study samples at three months of follow-up. The ANOVA test revealed statistically significant differences in ODI and VAS score reductions between the immediate postoperative period and the one-month and three-month follow-up periods (p = 0.001 and p = 0.0247, respectively). Conclusion: Less than one-third of the samples had postoperative complications. At three months, ODI scores showed mild disability in one-third of the study samples. At three months, all study samples had moderate VAS pain. The improvement in ODI and VAS scores from the day after surgery through the one-month and three-month follow-up periods was statistically significant.
2278
RF260: Recommendations for the surgical treatment of spinal stenosis in patients with achondroplasia: systematic review of the literature
Joab Olivo 1 , Miguel Farfan 1 , Baron Zarate-Kalfopulos 1 , Carla García-Ramos 1 , José Luis 1 , Fátima Soreim 1 , Alejandro Reyes-Sánchez 1
1 Spine Surgery, Instituto Nacional de Rehabilitacion, Mexico City, Mexico
Introduction: Spinal stenosis in patients with achondroplasia is due to the alteration in the osteogenic development of the spine and may be present in 20 to 50% of patients with achondroplasia. However, 20 to 78% of them will develop symptoms and one-third will require surgical management (1). This frequency of symptomatic spinal stenosis is higher than that of the general population (11%). Neurological impairment in patients can be significant and affect the quality of life of the patient and their family. Treatment of thoracic and lumbar spinal stenosis in patients with achondroplasia is controversial. Its presentation and prognosis may vary from patient to patient. The anatomical and spinal canal characteristics of these patients constitute a diagnostic and therapeutic challenge for specialists. Material and Methods: A systematic review of the literature was carried out following the PRISMA methodology of all studies published to date in relation to the presentation, treatment and/or prognosis of thoracic or lumbar stenosis in patients with achondroplasia. Articles were searched in the databases Pubmed, Embase and Google Scholar. No case reports were considered. There were no restrictions regarding the date of publication of studies for inclusion. According to the PRISMA methodology, at an initial stage the titles of the articles resulting from the systematic search were reviewed by the two main authors to select those that corresponded to the research topic. Results: A total of 499 studies for the initial review were found. After reviewing the titles and abstracts of these, a total of 461 were excluded as not being relevant to the objective of the study. Finally, 18 duplicate articles and 4 articles whose full text could not be found were eliminated. A total of 16 studies were included in the final analysis. 12 of the 16 studies (75%) reported clinical features of spinal stenosis presentation in patients with achondroplasia. The most frequent symptoms reported by the studies were neurogenic claudication, followed by functional impairment for walking or standing. 10 of the 16 studies (62.5%) reported alternatives, situations, or recommendations for the surgical management of these patients. The most used surgical procedures were laminotomies, laminectomies, with partial medial flavectomies and facetectomies, discectomies. 11 studies (69%) reported the presence of postoperative complications in the surgical management of spinal stenosis in patients with achondroplasia. Patient outcome results are variable, but most articles report more frequent total improvement (up to 54% of cases), partial improvement in 37%, and no improvement of up to 10%. Conclusion: Spinal stenosis in patients with achondroplasia requires early diagnosis and surgical management ideally before 6 months of symptoms. Patients and their families should be informed of the high risk of trans and postoperative complications such as dural sac puncture, infection, decompression level error, postoperative thoracolumbar kyphosis and need for reintervention. It is recommended the judicious study of magnetic resonance imaging and the clinical of patients, the use of bone cutting systems such as bone scalpel, in situ fixation of thoracolumbar kyphosis and having the necessary elements for the management of trans operative dural injuries.
1919
RF261: American College of Surgeons Risk Factor Calculator as a predictor of post operative outcomes after spinal deformity surgery
Justin Im 1 , Mohamed Soliman 1 , Alexander Aguirre 1 , Asham Khan 1 , Cathleen Kuo 1 , Esteban Quiceno Restrepo 1 , John Pollina 1 , Jeffrey Mullin 1
1 Neurosurgery, University at Buffalo, Buffalo, USA
Introduction: In recent years, there has been a large output of scoring systems that claim to be able to predict outcomes after various surgical procedures, however, research validating these studies is quite limited. In this study, we evaluate the predictability of the American College of Surgeons (ACS) Risk Calculator for various postoperative outcomes after spinal deformity surgery. Materials and Methods: A retrospective chart review of all patients who underwent spinal deformity surgery at a single institution between 2009 and 2022 was completed. All necessary demographic data to utilize the ACS risk calculator and postoperative outcomes were collected for all patients. Predictability was analyzed through the use of the area under the curve (AUC) for diagnostic accuracy. Results: A total of 156 patients were identified in this cohort, the mean age was 63.70 ± 9.73 years old and had 56 (35.9%) males. Preoperative diagnosis was a flat back deformity in 65 (41.7%) patients, degenerative scoliosis in 52 (33.3%) patients, and kyphosis in the remaining 39 (25.0%) patients. The mean number of operative levels was 7.23 ± 4.78 and patients had a mean length of stay of 4.99 ± 3.38 days. The ACS calculator had poor predictability for the occurrence of any complication after surgery (AUC = 0.64). Individually, it had good predictability for postoperative pneumonia (AUC = 0.81) but poor predictability for sepsis (AUC = 0.68), infection (AUC = 0.65), readmission to the hospital (AUC = 0.63), and discharge to rehab (AUC = 0.62). Conclusions: The ACS risk calculator could be utilized to identify patients at higher risk for postoperative pneumonia, although it is a poor predictor for outcomes after spinal deformity surgery.
2084
RF262: Analysis of personalized interbody implants in the surgical treatment of adult spinal deformity
Justin Smith 1 , Gregory Mundis 2 , Joseph Osorio 3 , Rodrigo Nicolau 4 , Michele Temple-Wong 4 , Renaud Lafage 5 , Shay Bess 6 , Christopher Ames 7
1 Department of Neurosurgery, University of Virginia, Charlottesville, USA
2 Department of Orthopedic Surgery, Scripps Clinic, La Jolla, USA
3 Department of Neurosurgery, University of California San Diego, San Diego, USA
4 Carlsmed, Carlsbad, USA
5 Department of Orthopedic Surgery, Lennox Hill Hospital, New York City, USA
6 Department of Orthopedic Surgery, Presbyterian St Lukes Medical Center, Denver, USA
7 Department of Neurosurgery, University of California San Francisco, San Francisco, USA
Introduction: Malalignment following adult spinal deformity (ASD) surgery can negatively impact outcomes and risk of mechanical complications. A recent report from the International Spine Study Group (ISSG; DOI: 10.1177/21925682231161304) noted that surgeons failed to achieve their sagittal alignment goals in nearly two-thirds of 266 complex adult deformity surgery (CADS) cases. We assess whether use of 3D-printed personalized interbody spacers is associated with improved rates of achieving goal alignment following ASD surgery. Material and Methods: 65 ASD patients surgically treated at 11 centers across the U.S. were assessed. Patients were included if their surgery included use of 3D-printed personalized interbody spacer(s) (aprevo, Carlsmed) and they met the same inclusion criteria as described for the ISSG CADS study. Planned PI-LL mismatch, intervertebral lordosis angle, intervertebral coronal angle, and posterior disc height, were prescribed in a personalized manner for each patient by the surgeon during personalized interbody planning. Planned versus achieved alignment was assessed and compared with the ISSG CADS series that utilized stock interbodies. Results: For 65 patients with personalized interbodies, 62% were women, mean age was 70.3 years (SD = 8.3), and mean baseline PI-LL mismatch was 19.6° (SD = 16.7°). The mean number of levels instrumented was 9.9 (SD = 4.1), and the mean number of personalized interbodies used per subject was 2.2 (SD = 0.8). Numbers of cases with ALIF, LLIF, and TLIF were 32 (49%), 25 (38%), and 13 (20%), respectively. Intervertebral segmental alignment was achieved close to plan for the levels treated with personalized interbodies, with mean (SD) difference between goal and achieved as follows: intervertebral lordosis = 0.9° (5.2°), intervertebral coronal angle = 0.1° (4.7°), and posterior disc height = -0.1 mm (2.3 mm). Achieved PI-LL correlated significantly with goal PI-LL (r = 0.668, p < 0.001). Compared with the ISSG CADS cohort that utilized stock interbodies, utilization of personalized interbodies resulted in significant improvement in achieving PI-LL alignment within 5° of the preoperative plan (p = 0.046). Furthermore, compared to ISSG cases, utilization of personalized interbodies led to a significant reduction in cases in which the PI-LL mismatch exceeded 15° (p = 0.012). Conclusion: Malalignment following ASD surgery can negatively impact outcomes and mechanical complications. Even among experienced deformity surgeons, it remains challenging to achieve preoperative goal alignment in ASD surgery. This study supports the use of 3D-printed personalized interbody spacers as a means of better achieving goal segmental sagittal and coronal intervertebral alignment and significantly improving achievement of goal PI-LL mismatch compared with stock devices.
1507
RF263: Proximal laminar hooks don't show a protective effect against PJF in long spinal fusions for adult deformities. A preliminary retrospective study
Riccardo Cecchinato 1 , Domenico Compagnone 1 , Andrea Redaelli 1 , Marco Damilano 1 , Francesco Langella 1 , Daniele Vanni 1 , Claudio Lamartina 1 , Pedro Berjano 1
1 GSpine4, IRCCS Galeazzi-Sant'Ambrogio Hospital, Milan, Italy
Background: Proximal junctional failure (PJF) is a relative frequent complication in adult deformity surgery after long instrumented fusions, with a rate up to 21% in some series and a high chance of undergoing revision surgery to solve the issue. The real causes of this disease are not perfectly clear, and different strategies have been proposed to reduce the rate of this complication. Among these, the use of a more flexible transition between the fused and unfused spine has the theoretical advantage of reducing the stiffness of the fused spine and thus the biomechanical stress at the junctional level. Laminar hooks could theoretically be a good way to obtain this mechanical advantage when used on the Upper Instrumented Vertebra (UIV). Our hypothesis was that the use of laminar hooks as the cranial end of the implant could reduce the incidence of PJF in adult deformity spine patients treated with long thoracolumbar fusion when compared to the use of pedicle screws in UIV. Materials and Methods: Retrospective observational study on patients treated with long thoracolumbar or thoracopelvic posterior fusions for adult spinal deformity, with at least 2 years of follow-up. Demographic data, spinopelvic parameters, type of instrumentation were collected and analyzed. Patients were pooled in different groups based on the type of implant that was used to instrument the UIV (pedicle screws, laminar hooks, sublaminar bands). Statistical analysis using the chi-square test has been performed. Results: After applying the inclusion and inclusion criteria 95 patients were collected in the study and divided in the different groups (group hooks or sublaminar bands, n = 21, group screws, n = 74). The statistical analysis showed no significative difference between the use of hooks and screws in the rate of PJF in these patients. All the patients that had sublaminar bands at UIV showed a PJF in the follow-up period. Conclusions: This retrospective study shows no protective effect of laminar hooks against PJF in long instrumented fusions for adult deformity surgery, when compared to pedicle screws. Conversely, all the instrumentations that had sublaminar bands at the UIV showed a PJF. While it seems that screws and hooks don’t differ much in terms of protection against PJF in long instrumented thoracolumbar fusions, the use of sublaminar bands at the UIV seems to produce a higher rate of PJF and should be discouraged. Further analysis on a larger pool of patients will be needed to confirm these results.
1321
RF264: Fetal scoliosis: natural history and outcomes
Samuel Walters 1 , Ben Barkham 1 , Mathew Gallagher 2 , Timothy Bishop 1 , Jason Bernard 1 , Christina Coroyannakis 3 , Baskaran Thilaganathan 3 , Darren Lui 1
1 Trauma & Orthopaedic Surgery
2 Neurosurgery
3 Fetal Medicine Unit, St George's Hospital, London, United Kingdom
Introduction: Scoliosis can be detected on prenatal ultrasound, and may be associated with other spinal abnormalities such as hemivertebrae, as well as structural and syndromic abnormalities. Associations and pregnancy outcomes related to the prenatal diagnosis of fetal scoliosis are poorly understood. Methods: A retrospective cohort study was undertaken at a busy tertiary referral centre in London. Referred cases between 1997-2021 were identified from the ultrasound database. Included patients had a finding of fetal scoliosis or spinal deformity on a prenatal ultrasound scan. Outcomes were ascertained from the database and electronic notes. Results: There were 123 cases of fetal spinal deformities from a referral population of 660,000 pregnancies, giving an incidence of approximately 0.2 per 1000 fetuses. There were 58 (47.2%) live births and 65 (52.8%) cases of fetal demise or termination. Most live births were isolated spinal deformities with a good postnatal outcome (n = 35, 60.3%). The commonest syndromic diagnosis in this group was VACTERL association (n = 7, 12.1%). Except in 2 (3.1%) patients, all the cases that resulted in fetal demise (termination, intrauterine or postnatal death) were associated with chromosomal abnormalities, multiple organ abnormalities, or developmental structural malformations, most commonly spina bifida, body stalk anomaly and amniotic band sequence. Conclusions: This study represents the largest database review to date of prenatal scans for spinal abnormalities. The incidence was approximately 1 in 5000 (0.2 in 1000), implying that fetal spinal deformity is commonly missed prenatally, given that the accepted incidence of congenital scoliosis in live births is approximately 0.5-1 in 1000. Approximately half of cases resulted in live birth, with the other half (fetal loss) strongly associated with concurrent severe malformations. Of the live birth group, the majority had a good postnatal outcome, with 3 in 5 (60.3%) having no other abnormalities, and 1 in 8 diagnosed with VACTERL association. This provides useful information for healthcare professionals and patients faced with a prenatal diagnosis of fetal scoliosis.
145
RF265: Scoliosis and tethered cord: tenets for concurrent management
Andrew Kobets 1 , Rose Fluss 2 , Jaime Gomez 2
1 Neurosurgery
2 Orthopedics, Montefiore Medical Center, Bronx, USA
Introduction: Tethered cord syndrome occurs in 12 to 17% of patients with scoliosis and has been demonstrated to worsen scoliotic curves over time if the tether is not released. Scoliosis associated with tethered cord syndrome is one of the most challenging spinal deformities to manage, as a tethered spinal cord may increase the chance of neurological injury when undergoing surgical correction of scoliosis due to excessive traction during reduction maneuvers. We present our experience managing patients with concurrent pathologies and offer some pearls during operative correction. Material and Methods: A series of cases with concurrent tethered cords and scoliosis were reviewed from our institution and a review of the literature was performed. Information regarding timing of surgery, optimal order of surgical procedures, and outcomes were collected. Results: An exemplary case is presented demonstrating a large scoliotic curve, kyphotic deformity at L1, and a tethered cord. Decision making regarding logistics of surgery are presented, demonstrating that tethered cord release prior to laminectomy at the kyphosis, and scoliotic correction prevents neurological injury that can result from decompression first with a still tethered cord. Concurrent procedures have become the standard of care as opposed to prior staged procedures, with lower complication rates and more robust clinical outcomes. Cobb angle less than 35 degrees and Risser grades > 3 allow for tethered procedures alone which may halt scoliosis progression in itself. Conclusion: For smaller scoliotic curves, it is feasible to perform a detethering surgery alone and observe the patient to demonstrate an arrested curve progression. Concurrent pathologies can be treated simultaneously, however the tether should be addressed first, as we demonstrate that decompression or scoliosis repair may induce neurological injury. If neurological injury occurs from detethering, a wake-up test may be performed, yet consideration to complete scoliosis correction should be entertained.
1459
RF266: MURST trial: a randomised controlled trial of a rail versus rod in adolescent idiopathic scoliosis surgery
Evan Davies 1 , Laura Mitchelson 2
1 Childrens Hospital, University Hospital Southampton, Southampton, United Kingdom
2 Southampton Medical School, Southampton, United Kingdom
Introduction: We present the first randomized controlled trial comparing the use of a standard rod (USS 2 DePuy Synthes) versus a rail (Mesa Stryker) system in the surgical correction of adolescent idiopathic scoliosis. Material and Methods: 60 patients were randomized to received surgical correction with either a standard rod or rail system. National ethics approval for gained for the trial all patients were blinded to the selection of surgery after informed consent from the patient and their parents or careers. Results: For the analysis of covariance, post-operative cobb angle was classed as the dependent variable subject to individual patients pre-operative cobb angles. Once controlling for other factors including age, gender and number of vertebrae fused, there was no statistical significance found between device groups in post-operative cobb angle (p = 0.096). However mean percentage correction was found to be statistically significant in favour of the MESA improving percentage of curvature correction over the USS group (p= 0.045). Conclusion: The Rail versus Rod Trial shows no statistical post operative difference between the two groups. The Rail device appears to have cause a statistically significant improvement in percentage curve correction.
1668
RF267: Convex instrumentation technique for correction of adolescent idiopathic scoliosis - Should this be the gold standard?
Anindya Basu 1 , Selvin Vijayan 1 , Christopher Gerber 1
Introduction: Deformity correction surgery in AIS requires extensive preoperative planning, challenging intraoperative execution and potentially devastating complications. Convex instrumentation technique reduces cost of surgery by reducing implant density, reduces risk of intraoperative damage to neural and vascular structures, operative me, blood loss and provides more surface area for bone grafting. Material and Methods: We present a series of 32 patients aged between 10 and 18 with AIS managed surgically with convex technique. The patients were of Lenke type 1, 5and 6. The preoperative and post operative Cobb angles, blood loss, operative me and complications were noted. Functional outcomes were noted at 6 months follow up. Results: Mean pre operative cobb was 66 and post operative cobb was 13, blood loss was 900 ml and mean surgical me was 210 minutes. There was no complication intraoperatively or in the immediate post operative period and at 6 months follow up. Conclusion: This novel method has shown lower patient morbidity, reduced surgical costs with satisfactory correction of deformity, equivalent patient satisfaction and functional outcomes compared to the traditional technique
636
RF268: Influence of traditional growing rod on quality of life of idiopathic scoliosis patients: comparison between traditional growing-rod graduates and adolescent idiopathic scoliosis patients treated by single posterior fusion surgery
Haruki Ueda 1 , Satoshi Inami 1 , Hiroshi Moridaira 1 , Tomoya Kanto 1 , Satoshi Takada 1 , Kazuo Doi 1 , Hiroshi Taneichi 1
1 Orthopaedic Surgery, Dokkyo Medical University, Shimotsuga, Japan
Introduction: Traditional Growing Rod (GR) surgery has been concerned to have negative social and psychological impact on young scoliosis children. Unlike the one-stage fusion technique for AIS, the GR method requires repetitive surgeries over a long period of time, although they are similar in that they fuse the pediatric spine over a long range. The aim of this study is to assess the influence of GR treatment on the quality of life of early onset idiopathic scoliosis patients by comparing the corrective fusion surgery for AIS. Material and Methods: We retrospectively compared the GR graduates for early onset idiopathic scoliosis (EOS) and the adolescent idiopathic scoliosis (AIS) patients after posterior fusion surgery. Their whole spine X-ray film and SRS-22 score at 2 years after fusion surgeries were assessed. In comparison, the cases were included using the criteria of the age at fusion (11-13 years old), UIV (T2 or T3), LIV (Lumbar spine), number of levels fused (10-13). Results: Seven EOS and twelve AIS cases met the criteria and were included in this comparison. On the X-ray at two years after final fusion, Proximal Thoracic Cobb (following numbers and scores described EOS/ AIS, respectively) (21/ 14mm, p = 0.025), TK (39/ 15 degrees, p = 0.001), Right Shoulder Height (3.2/ 16, p = 0.047) had statistically significant difference. On the SRS-22 score, there was statistically significant difference in function (4.4/ 4.7, p = 0.034), but not in pain (4.7/ 4.8), self-image (3.9/ 4.0), mental health (4.5/ 4.7) domains. Each question besides Q5 (activity level:3.3/ 4.3, p = 0.001) had no significant difference. Of note, in Q22 regarding the likelihood to choose the same management again, none of 12 AIS but three of 7 EOS chose never, although no statistical difference was detected (2.9/4.1, p = 0.12). Conclusion: At two years after the graduation fusion of GR its spinal alignment was comparable to AIS single-stage fixation. However, the GR graduates showed the feeling of limitations in daily activity. This suggests that this feeling in the GR graduates could be from the other reasons than spinal inflexibility, such as long restrictions on physical activity over the GR treatment from an early age. Nearly half of the GR graduates strongly refused to choose the same treatment, and this suggests that there may exist the psychological influences that is not reflected in the differences of SRS-22 score.
1914
RF269: What is the reality of pediatric scoliosis in Latin America?
Karen Weissmann 1,2 , Carlos Huaiquilaf 1,2 , Marcelo Costa 1,2 , Francoise Descazeaux 1,2
1 Spine Surgery, Patagonia Spine Foundation, Santiago, Chile 2 Spine Surgery, Clinica MEDS, Santiago, Chile
Introduction: Latin America comprises 21 countries. All of them under Organization for Economic Co-Operation and Development (OECD) standards. Access to healthcare, costs, infectious disease, maternal and infant mortality still constitute the main problems in the continent, thus leaving little resources for spinal deformity surgery. Our aim was to describe the situation of pediatric scoliosis in Latin America. Material and Methods: Prospective descriptive longitudinal study. We performed an online survey through the Sociedad Iberolatinoamericana de Columna (SILACO) trough google forms (Google corp, LA). Demographical data was collected regarding number of spine and deformity surgeons, age and sex geographical localization of those surgeons, time to patient evaluation and surgical resolution, number of deformity cases performed per year, techniques and implants used, national scoliosis surgery programs and financing. Per capita analysis was performed considering the population data published by the OCED. Statistical analysis was performed using Pearson correlation (p - value < 0.05). Results: 140 surgeons from 15 countries answered the survey. Cuba, El Salvador, Guatemala, Honduras, Puerto Rico and Haití did not respond. Surgeons mean age was 48.9 ± 10.6 (32 - 77 years old); 86% men. Mean number spine surgeons/country were 255.7 ± 352.4; number of deformity surgeons/country 73.2 ± 187.9; 98.6% of surgeons are centralized in big cities. The number of deformity cases per year is 27.92 ± 28.3; when analyzed by sex, there are 28,37 deformity cases per year performed by men and 20,89 by women. Mean spine surgeons/capita are 8/1.000.000 people (0.88 - 30/1.000.000p); deformity surgeons/capita: 2/10.000.000 people (1.79 - 6.85/10.000.000p). The most common used technique was posterior spinal fusion with a mean number of techniques performed per surgeon of 3.98 ± 3.2 (1 - 13 techniques, p = 0.439). Only Chile has a national program for scoliosis surgery. There are private initiatives in specific hospitals in Colombia, Mexico, and Nicaragua. Surgery is mainly financed by social security (40%), Private insurance (35%). National programs take up 12% of the financing followed by private foundations and Global outreach programs (10% and 3% respectively). 70% of the patients are seen by a spine surgeon before 6 months, and 84% before a year. 72.9% of surgical patients undergo the necessary procedure before 1 year. The number of surgeons positively correlates with shorter referral times (p = 0.030), but not with surgical resolution times (p = 0.281) or the use of different techniques (p = 0.024). Number of deformity surgeons do not correlate with the number of technologies used (p = 0.178), but it does correlate with shorter referral and surgical resolution times (p = 0.046, p = 0.006). Conclusion: There is a severe lack of data regarding scoliosis deformity in Latin America. Most countries have a deficient number of spine surgeons that are concentrated in larger city. The presence of more surgeons diminishes waiting times for resolution. National and governmental incentives are needed to train more deformity surgeons.
2240
RF270: Proposal for a treatment-oriented classification system for congenital kyphosis in children
Ziming Yao 1 , Xuejun Zhang 1 , Dong Guo 1
1 Orthopedics, Beijing Children's Hospital, Capital Medical University, Beijing, China
Introduction: The classification of congenital kyphosis described by Winter is the one most commonly used. However, this classification of congenital kyphosis cannot direct the surgical options and the treatment choices remain controversial. Our purpose is to propose a new treatment-oriented classification system for pediatric congenital kyphosis based on radiographic findings and evaluates the reliability of this new classification system. Material and Methods: For each type of congenital kyphosis, we propose a set of radiological criteria that are suggestive for diagnosis as well as the corresponding surgical options. To evaluate the reliability of this new classification system, 35 patients with congenital kyphosis were reviewed and classified by four attending spine surgeons and five spine fellows. Results: Our new classification system divides congenital kyphosis into five types. The overall Fleiss kappa coefficient (k) value for the new classification system was 0.755, which indicates significant agreement. The interobserver and intraob- server k values were 0.755 and 0.828, respectively, and there were no significant differences in the k values between the attending spine surgeons and spine fellows. Conclusion: The proposed classification system provides clear descriptions and surgical options for various types of pediatric congenital kyphotic deformities. The reliability study confirmed that the classification system is both simple and consistent.
202
RF271: Is 'Sarcopenia' a hype? Or does it really affect the outcome of lumbar spine surgeries?
Manojkumar Gaddikeri 1 , Abhay Nene 1
1 We are Spine, Lilavati Hospital, Mumbai, India
Introduction: Sarcopenia, defined as progressive impairment of muscle function secondary to loss of skeletal muscle mass has prevalence of 24%- 56% in patients > 60years. 44% of elderly patients undergoing orthopaedic surgery are found to be sarcopenic. It is a known risk factor for fall, fractures, disability, increased post-operative morbidity and mortality. If diagnosed pre-operatively, it can help prepare the patient and surgical team to foresee complications and thereby reduce morbidity and mortality. In the present study, we evaluated and correlated sarcopenia with the surgical outcome of operated patients with lumbar spine pathology. Materials and Methods: A prospective, observational study was conducted on 108 patients > 40 yrs undergoing lumbar spine surgeries, who were studied and followed up for 3-months. They were segregated into 5 groups based on age (40-49 yr, 50-59 yr, 60-69 yr, 70-79 yr, ≥ 80 yr) and were assessed separately. Data on demography, grip-strength analysis, 30s chair stand test, Psoas muscle index (calculated on pre-operative MRI), pre and post-operative ODI (Oswestry Disability Index) scores at 2weeks and 3months, Dindo-Clavien Classification of peri-operative complications, 90-day readmission rates and mortality (if any) were included. Patients were segregated into sarcopenic & non-sarcopenic groups based on the definition and set parameters as per the European Working Group on Sarcopenia in Older People (EWGSOP). A comparative analysis between these groups was performed. Results: Of 108 patients, there were 18 patients in 40-49 yrs, 24 in 50-59 yrs, 27 in 60-69 yrs, 30 in 70-79 yrs and 9 in > 80 yrs age group. Statistically significant difference in peri-operative ODI scores was seen in sarcopenic vs non-sarcopenic patients in all age groups (p < 0.05) except 40-49yrs. Results showed that sarcopenic group had higher rate of peri-operative complications, delayed mobilisation, longer stay and mortality compared to non-sarcopenic group. Conclusion: We conclude that sarcopenic patients have poor outcome in lumbar spine surgery compared to those without. So, by diagnosing sarcopenia using tests routinely done as pre-operative requirement, one can reduce radiation exposure and cost of treatment. The management can be revolutionized by predicting those who are at high risk of developing post-operative complications and poor surgical outcomes by mere diagnosis of sarcopenia. This knowledge will benefit both the patients and the surgeons.
Keywords: sarcopenia; EWGSOP; grip strength; chair stand test; Dindo-Clavien Classification; Oswestry Disability Index
2291
RF272: A finite element study of alternative laminectomy procedures
Craig Almeida 1 , Alexandra Seidenstein 2 , Amit Jain 2 , Jill Middendorf 1
1 Mechanical Engineering, Johns Hopkins University, Baltimore, USA
2 Orthopedic Surgery, Johns Hopkins Medical Institute, Baltimore, USA
Introduction: Laminectomy procedures are common treatments for lumbar stenosis. However, iatrogenic conditions like spondylolisthesis and pars interarticularis (PI) fracture can occur after laminectomies. Recently, unilateral procedures and laminotomy procedures, which remove less bone from the lamina than a full laminectomy, have been proposed as potential solutions to reduce the risk of PI fracture and prevent iatrogenic conditions. Finite element models can provide an excellent framework to understand the risk of PI fracture by identifying the PI stress due to multiple types of spinal motion. Existing finite element models of laminectomies focus on full lamina removals and present the range of motion (ROM) not PI stress. Therefore, to assess the risk associated with different laminectomy procedures, this study identified differences in the PI stress for clinical procedures associated with low bone removal (Unilateral laminotomy, Bilateral laminotomy) versus procedures with high bone removal (Hemi laminectomy, Full laminectomy). Material and Methods: A finite element model of a 49-year-old female L1 through L5 lumbar spine was analyzed by applying a follower load and moment in FEBio. Four variations of the surgical procedures were simulated: Unilateral Laminotomy (ULO), Bilateral Laminotomy (BLO), Hemilaminectomy (HL) and Full Laminectomy (FL) and compared with the intact model. Each surgical procedure removed approximately 50% of the L4-L5 facet joint and preserved at least 1 cm of the L4 pars interarticularis. After each model was created, a follower load was applied. Additionally, four different torsional loads were individually applied to put the lumbar spine into flexion, extension, lateral bending, and axial rotation. The PI stress and ROM for each of these four motions were compared to each other and the intact spine. Results: Increased removal of the bone within the lamina during ULO and BLO typically resulted in increased PI stress compared to HL and FL procedures, while the ROM of the spine remained unaffected. Under flexion motion, the FL procedure increased stress by at least 35% compared to all other procedures. During extension loading both the FL and HL procedures increased stress by at least 35% more than both the ULO and BLO procedures. Due to lateral bending and axial rotation the PI stress progressively increased with increased volume removal of the lamina with a maximum increase of 40% as compared to the conservative laminotomy procedures. Conclusion: By preserving the midline spinous process and reducing removal of the lamina during the ULO procedure, PI stress can be reduced when compared to the FL and HL procedures. PI stress increases in the FL and HL procedures over the ULO and BLO procedures may be attributed to increased removal of both lamina and ligaments. Although the PI stress does not reach the failure stress of bone (∼140 MPa), patient specific variables and disc degeneration could potentially cause much higher PI stresses. Because the ULO and BLO procedures both reduce the risk of PI fracture (by reducing PI stress) when compared to HL and FL, surgeons should consider performing either of these two procedures over HL and FL to treat spinal stenosis.
734
RF273: Do lordotic changes at L4-S1 following spinal fusion cause compensatory lordotic changes at L1-L3?
Parker Brush 1 , Rajkishen Narayanan 1 , Michael Carter 1 , Yunsoo Lee 1 , Nicholas Pohl 1 , Alexa Tomlak 1 , Sebastian Fras 1 , Emily Ducaji 1 , Abbey Glover 1 , Julian Takagi-Stewart 1 , Alan Hilibrand 1 , Gregory Schroeder 1 , Christopher Kepler 1 , Alex Vaccaro 1 , Jose Canseco 1 , Joseph Lee 1
1 Rothman Institute, Thomas Jefferson University, Philadelphia, USA
Introduction: Sagittal balance of the lumbar spine involves a distribution of lordosis favoring the lower segments. Patients with a normal lumbar lordosis distribution are well described as having favorable outcomes with regards to postoperative mechanical symptoms. However, the impact of altering lower lumbar segmental lordosis through fusion surgery on the sagittal alignment of the proximal lumbar segment has not been defined. The purpose of this study is to assess the relationship between changes in L4-S1 lordosis by fusion surgery on the change in L1-L3 lordosis. Material and Methods: We conducted a retrospective review of radiographic sagittal balance on patients with degenerative spine disease receiving a 1- to 2-level lower segment (L4-S1) lumbar fusion surgery. Patient demographics, comorbidities, surgical indications, and surgical procedures were obtained from review of the electronic medical record. Preoperative and one-year postoperative radiographs were reviewed for lumbar sagittal balance measurements. Delta values were calculated by subtracting the preoperative data from the postoperative data. Groups were formed based on delta L4-S1 values: <10°, -10° to -6°, -5° to -1°, 0 to 5°, 6° to 10°, and >10°. Bivariate analysis was performed to detect changes in L1-L3 segmental lordosis between groups. Multivariate analyses identified variables independently associated with changes in L1-L3 segmental lordosis and L1-S1 lordosis. Results: We identified 251 patients receiving a 1- to 2-level fusion between L4-S1. No differences were detected between the groups with regards to BMI (median: 30.6; p = 0.314), Elixhauser Comorbidity Index (median: 1.00; p = 0.323), or sex (54.2% female; p = 0.065). Patients in the >10° group were more likely to be younger (58 vs 66; p = 0.007) and patients in the -5° to -1° group were less likely to be current smokers (0% vs 9.2%; p = 0.036). Preoperative diagnosis was similar between groups with exception to the > 10° group having fewer patients with stenosis (72.0% vs 87.6%; p = 0.019). In addition, patients in the > 10° group were more likely to receive an anterior lumbar interbody fusion (ALIF) (52% vs 17.1%; p < 0.001). A similar number of levels were decompressed (median: 2, p = 0.416) and fused (one-level: 84.9%; p = 0.313) between the groups, however the > 10° group was more likely to have a 1-level L5-S1 fusion. Delta L1-L3 segmental lordosis was similar between the groups (median: 1; p = 0.963). Multivariate regression analysis identified former smoking status as an independent predictor of delta L1-L3, and receiving an ALIF as independently associated with an increased delta L1-S1. Conclusion: Regardless of the degree of change in L4-S1 segmental lordosis by the fusion operation, L1-L3 segmental lordosis was static. These data suggest that any change in lordosis that is achieved by surgery for lower lumbar fusions is likely to be realized as a change in overall lumbar lordosis without significant compensation by the proximal segment at one-year. In addition, there does not appear to be any factor reasonably associated with a change in L1-L3 lordosis from surgery below this segment. Consistent with previous literature, receiving an ALIF is associated with the greatest degree of change in total lumbar lordosis.
616
RF274: Detection of transthyretin amyloid protein in the ligamentum flavum of patients at risk of systemic amyloidosis
Sree Vemu 1 , Varan Haghshenas 1 , Takashi Hirase 2 , Brendan Holderread 1 , Andreana Rivera 3 , Jeffrey Ratuzsnik 1 , William Watters 1 , Barry Trachtenberg 4 , Bradley Weiner 1 , Shari Liberman 1
1 Orthopedics and Sports Medicine, Houston Methodist Hospital, Houston, USA
2 Department of Orthopedic Surgery, Hospital for Special Surgery, New York, USA
3 Department of Pathology and Genomic Medicine
4 Houston Methodist Hospital DeBakey Heart & Vascular Center, Houston Methodist Hospital, Houston, USA
Introduction: Systemic amyloidosis (SA) involves the buildup of misfolded proteins, causing organ failure. It mainly manifests as primary (AL) or secondary (ATTRwt and ATTRm) types. ATTR or AL deposition accounts for over 95% of cardiac amyloidosis cases, often leading to heart failure or atrial fibrillation. Diagnosis is confirmed via Congo Red stain. SA can also affect the neuromusculoskeletal system, causing conditions like spinal stenosis and peripheral neuropathy, often years before cardiac symptoms. Amyloid deposits in the ligamentum flavum (LF) exacerbate lumbar spinal stenosis. Though treatments exist for cardiac forms, there's no formal magnetic resonance imaging (MRI) screening for LF in lumbar decompression patients. This study aims to: 1) assess SA incidence in at-risk patients with lumbar spinal stenosis undergoing surgical decompression via LF evaluation; and 2) develop an evidence-based algorithm to guide surgeons in identifying patients for Congo Red stain evaluation of the LF, enabling early diagnosis and treatment. Material and Methods: This institutional review board-approved pilot study aims to enroll 120 patients, based on power analysis. Enrollment started in August 2021 and includes 17 patients to date (11M, 6F). Developed by the principal investigator, inclusion criteria are: M>50 or F>60 years old, undergoing lumbar decompression for spinal stenosis, and at least two qualifying orthopedic or cardiac conditions like average (LF) thickness >4.9 mm on MRI, carpal tunnel, rotator cuff tear, atrial fibrillation, or family history of amyloidosis. LF thickness is calculated by averaging left and right measurements. Exclusions are M<50, F<60, prior lumbar surgery, or spinal malignancy. Intraoperative LF samples undergo categorical Congo Red staining. Positive samples are sent to the Mayo Clinic for amyloid typing via mass spectrometry. Patients receive referrals to a cardiologist specializing in amyloid cardiomyopathy. Data on demographics and decompression levels are recorded. Descriptive statistics are applied to all variables, but statistical significance isn't yet assessed due to the current sample size. Results: The negative cohort had an average age of 73.3 ± 7.2 years and BMI of 32.1, compared to 79 ± 7.1 years and 31.5 BMI in the positive cohort. The study included 6 females (42.9%) and 8 males (57.1%). LF thickness was 6.38 ± 1.22 mm in the negative cohort and 6.45 ± 1.27 mm in the positive (Overall: 6.39 ± 1.18 mm). Two males (14.3%) tested positive for Congo Red stains, both ATTRwt. Overall, 82.6% had LF thickness > 4.9 mm. Both positive patients underwent multi-level decompression. Post-op, both ATTRwt positives experienced radicular symptoms, with one requiring revision (0/12 in the negative group). One amyloid-positive completed a negative nuclear scan; the other did not. Conclusion: Amyloid-positive patients were older males with ATTRwt, consistent with previously described risk factors. Patients undergoing multi-level decompression and exhibiting LF hypertrophy may show evidence of transthyretin deposits in the LF. Postoperatively, ATTRwt patients may face an increased risk of persistent symptoms. A larger cohort is needed to determine how these differences may influence surgical decision-making and the likelihood of a positive Congo Red stain in this patient population.
877
RF275: Treatment effect of poly(lactic-co-glycolic) magnesium hydroxide-ricinoleic acid loaded with luteolin and bupivacaine in peripheral nerve injuty
Joon Hyuk Jung 1 , So Yeon Park 1
1 Department of Life Science, CHA University School of Medicine, Gyeonggi-do, South Korea
Introduction: In this study peripheral nerve injury (PNI) and explore alternative treatments to mitigate its effects. PNI refers to damage or dysfunction of peripheral nerves, leading to pain and functional impairments. Currently, drugs like dexamethasone, a corticosteroid, are used for PNI treatment, but they can induce adverse side effects. In this study, we investigate the potential of luteolin, a flavonoid compound, as a replacement for dexamethasone. Luteolin exhibits anti-inflammatory and neuroprotective properties, making it a promising candidate. By utilizing luteolin-loaded PLGA microspheres, we aim to provide sustained drug release for PNI, offering a safer and more effective therapeutic option compared to dexamethasone. Material and Methods: PLGA/MH-RA loaded with luteolin and bupivacaine was directly injected. The animal model used was a 10-week-old female SD rat weighing 200-220g. Chronic constriction injury modeling was performed on the right sciatic nerve, involving four ligations at 1mm intervals using 04slik. Results: The results of the experiment revealed that both the von Frey and hot plate tests exhibited a significant anesthetic effect for up to seven days following the initial injury, gradually declining thereafter. Subsequent RT-PCR and immunofluorescence analyses identified reduced pain and inflammatory markers in the treatment group compared to the existing drug and damage model groups. These findings indicate improvements in pain and inflammation levels associated with the treatment using PLGA/MH-RA loaded with luteolin and bupivacaine. Conclusion: Our study demonstrates that PLGA/MH-RA loaded with luteolin and bupivacaine provides extended efficacy compared to conventional drugs in the treatment of peripheral nerve injury (PNI). luteolin exhibits anti-inflammatory and neuroprotective effects, offering a promising alternative to dexamethasone in treatmenting PNI. These findings shed light on a novel treatment approach for PNI and underscore the potential of luteolin as a viable substitute for dexamethasone. This research opens new avenues for therapeutic advancements in PNI and highlights the importance of exploring alternative medications for improved patient outcomes.
393
RF276: Lumbar vertebropexy after unilateral total facetectomy
Anna-Katharina Calek 1 , Jonas Widmer 1 , Marie-Rosa Fasser 1 , Mazda Farshad 1
1 Orthopedic Department, Balgrist University Hospital, Zurich, Switzerland
Background Context: Posterior spinal instrumentation and fusion is associated with well-known complications. A good surgical solution that includes decompression and restoration of native stability of the vertebral segment without fusion is still pending. Purpose: To aim of this study was to test two different synthetic lumbar vertebral stabilization techniques that can be used after unilateral total facetectomy. Study design: Biomechanical cadaveric study. Methods: Twelve spinal segments were biomechanically tested after unilateral total facetectomy and stabilized with a FiberTape cerclage. The cerclage was pulled through the superior and inferior spinous process (interspinous technique) or through the spinous process and around both laminae (spinolaminar technique). The specimens were tested after (1) unilateral total facetectomy, (2) interspinous vertebropexy and (3) spinolaminar vertebropexy. The segments were loaded in flexion-extension (FE), lateral shear (LS), lateral bending (LB), anterior shear (AS) and axial rotation (AR). Results: Unilateral facetectomy increased native ROM in FE by 10.6% (7.6-12.6%), in LS by 25.8% (18.7-28.4%), in LB 7.5% (4.6-12.7%), in AS 39.4% (22.6-49.2%), and in AR by 27.2% (15.8-38.6%). Interspinous vertebropexy significantly reduced ROM after unilateral facetectomy: in FE by 73% (p = 0.001), in LS by 23% (p = 0.001), in LB by 13% (p = 0.003), in AS by 16% (p = 0.007), and in AR by 20 % (p = 0.001). In FE and LS the ROM was lower than in the baseline/native condition. In AS and AR, the baseline ROM was not reached by 17% and 1%, respectively. Spinolaminar vertebropexy significantly reduced ROM after unilateral facetectomy: in FE by 74% (p = 0.001), in LS by 24% (p = 0.001), in LB by 13% (p = 0.003), in AS by 28% (p = 0.004), and in AR by 15 % (p = 0.001). Baseline ROM was not reached by 9% in AR. Conclusion: Interspinous vertebropexy seems to sufficiently counteract destabilization after unilateral total facetectomy, and limits range of motion in flexion and extension while avoiding full segmental immobilization. Spinolaminar vertebropexy additionally restores native anteroposterior stability, allowing satisfactory control of shear forces after facetectomy. Clinical significance: Lumbar vertebropexy seems promising to counteract the destabilizating effect of facetectomy by targeted stabilization.
Keywords: spinal stabilization; semi-rigid; vertebropexy; facetectomy; lumbar fusion; lumbar spine
1000
RF277: Can spinal cord biomechanics predict the risk of spinal cord injury due to pre-existing cervical stenosis after minor trauma?
Aditya Vedantam 1 , Balaji Harinathan 1 , Narayan Yoganandan 1
1 Neurosurgery, Medical College of Wisconsin, Milwaukee, USA
Introduction: Patients with asymptomatic cervical spinal stenosis are often referred to spine surgeons due to the potential increased risk of spinal cord injury from minor trauma such as rear impact whiplash injuries. Current clinical guidelines do not support prophylactic spinal cord decompression for asymptomatic cord compression, however, there is limited data to guide patient counseling on potential risks and activity restrictions. It is unclear how the degree of cervical stenosis or the rate of impact relates to the risk of cervical spinal cord injury from minor trauma. The aim of this study was to determine the risk of spinal cord injury with progressive pre-existing cervical stenosis during whiplash injury using a finite element approach. Material and Methods: A previously validated three-dimensional finite element model of the human head-neck complex with the spinal cord was used. Progressive spinal stenosis was simulated at the C5-C6 segment, reducing the anteroposterior spinal canal diameter from 14mm to 6 mm, at 2 mm intervals of ventral disk protrusion. Rear impact acceleration was applied to the constrained T1 vertebra at 1.8 m/s (4 miles/hour) and 2.6 m/s (5.8 miles/hour) with activated cervical musculature. The cervical range of motion, spinal canal diameter, intrinsic spinal cord von Mises stress and spinal cord strain were compared to known thresholds for spinal cord injury. We also investigated the impact of neck range of motion and dynamic spinal cord diameter on spinal cord biomechanics. Results: The mean segmental range of motion at C5-C6 was 7.9 degrees (at 1.8 m/s) and 9.3 degrees (at 2.6 m/s), and this was unaffected by the degree of stenosis. Canal diameter was the lowest at 150ms after impact in all models. A decrease in in canal diameter below the average spinal cord diameter (7.2 mm) was noted with when canal stenosis was ≤ 6 mm (at 1.8 m/s) and ≤ 8 mm (at 2.6 m/s). The maximum von Mises stress in the spinal cord increased linearly with increasing stenosis and rate of impact. Spinal cord and canal parameters did not reach the threshold for spinal cord injury for any degree of stenosis at 1.8 m/s. Spinal cord stress/strain as well as spinal canal narrowing approached the threshold for spinal cord injury with 8mm and 6mm stenosis at 2.6 m/s. Conclusion: Using a finite element approach, we show that anteroposterior spinal canal diameter <= 8mm at 2.6 m/s was associated with spinal cord stress/strain values near the threshold for spinal cord injury during whiplash injury. Both the rate of impact and degree of stenosis increased intrinsic spinal cord stress and the risk of spinal cord injury. Our method can be extended to patient-specific FE models to objectively define patient-specific spinal cord injury risk for cervical stenosis with varying degree of trauma. This personalized medicine approach can improve patient counseling and management of expectations for patients with asymptomatic cervical stenosis.
862
RF278: Determining the association between spinal pathology and gene expression within muscle below and adipose above the thoracolumbar soft tissue envelope
Timothy Foster 1 , Apratim Maity 1 , Pooja Swami 2 , Haixiang Liang Dr. 2 , Daniel Grande Dr. 2 , Sohrab Virk 1 3
1 Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, USA
2 Feinstein Institute for Medical Research, Manhasset, USA
3 Northwell Health Physician Partners Orthopaedic Institute at New Hyde Park, Orthopaedics, New Hyde Park, USA
Introduction: The thoracolumbar soft tissue envelope has been suggested as a potential origin of pathology in the back and spine. Histologic examinations have revealed the existence of pain-sensitive nerve endings within paralumbar soft tissue, but the exact way in which these findings contribute to pathophysiology related to the spine is unknown. This study sought to analyze gene expression within tissues in proximity to this fascia to uncover potential associations between spinal pathology and gene expression in muscle below this fascia (MBF) or adipose above this fascia (AAF). Materials and Methods: After receiving institutional review board approval #22-0630, MBF and AAF specimen from 25 patients undergoing spinal surgery were obtained, homogenized, and RNA samples were isolated. qPCR was performed to quantify gene expression. The genes analyzed were grouped by associated functions: Inflamation (TNF-α, IL-1B, and FOXO3); Vascular (VWF, CD31, and HIF1-α); Extracellular Matrix Remodeling (ADAMTS4 and COL-1); Muscle Development and Repair (PAX7 and Nestin); Lipid Metabolism (LPL); Neuronal (MAP2 and Nestin). Using K-means clustering, a machine learning algorithm that partitions datasets into “clusters” based on similarities amongst data points, each MBF/AAF sample was assigned to a cluster based on similarities in gene expression of the genes in each of the aforementioned gene groups. A chi-square test was then performed to determine if there was any significant relationship between each gene group’s expression and the spinal pathologies that the donor patients possessed such as radiculopathy, neurogenic claudication, spondylolisthesis, disc herniation, and degenerative disc disease (p value < 0.05 = significant). Additionally, the relationship between each gene group’s expression and the donor patient’s position on the Goutallier Classification scale and other measures (SF-12, Oswestry Disability Index, and PROMIS Physical Function) was determined. Statistical analyses were generated using python. Results: A total of 21 MBF samples and 19 AAF samples were analyzed. A significant relationship between gene expression involved in ECM remodeling in MBF and degenerative disc disease was found (p value = 0.0472). No significant relationships between any of the gene group’s expression and radiculopathy, neurogenic claudication, spondylolisthesis, or disc herniation were found (p value > 0.05). A significant relationship was also found for both the inflammation gene group’s expression in MBF and the donor patient’s position on the Goutallier Classification scale (p value = 0.0344). In AAF, a significant relationship between the muscle development and repair gene group’s expression and Goutallier Class was found (p value = 0.0175). No significant relationships between any of the gene groups and the SF-12, Oswestry Disability Index, and PROMIS Physical Function patient outcome measures were found (p value > 0.05). Conclusion: The relationship between gene expression involved in ECM remodeling in MBF and degenerative disc disease may indicate an interdependent relationship between disc degeneration and paralumbar muscle breakdown. Additionally, the association between muscle development and repair related gene expression in AAF and the donor patient’s position on the Goutallier Classification scale indicates that AAF may contribute to muscle breakdown below fascia.
222
RF279: Let's think beyond the pedicle: a biomechanical study of a new conceptual extra pedicular screw and hook construct
Vikas Tandon 1 , Nirdesh Hiremaglur Jagadeesh 1
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
Introduction: Transpedicular screws have proven the test of time, yet they are not devoid of complications which at times can be catastrophic. Many newer techniques such as 2 D and 3D fluoroscopy, O arm Navigation assisted surgery, robotic assisted surgery have come into existence to the increase precision in pedicle screw insertion. But complications do occur in their presence. We propose an Extra pedicular screw and hook system (EPSH) with similar biomechanical property, better safety profile and short learning curve compared to traditional pedicle screw. Material and Methods: Biomechanical testing was conducted according ASTM F543 guidelines to compare the pull-out strength of EPSH based construct and traditional pedicle screw construct. Six saw bone samples in each group considered. Screw of 5.5 mm diameter and length of 35 mm was used in both the groups. Rods connected to both the system secured to tensile load tester. Pull out strength assessed by giving 5 mm/min axial load. The axial load Vs displacement of the screw were recorded and plotted. The maximum load required for screw failure is noted in both the group. Statistical analysis was done. Results: The mean peak load of pedicle screw group was found to be 1670.9 ± 393.2 N with mean displacement at peak load was found to be 13.44 ± 1.7 mm and in EPSH group it was 1416.4 ± 341.4 N and 15.78 ± 3.9 mm respectively. A paired t test showed no statistical difference (p < 0.05) between 2 groups. Conclusion: EPSH has shown to have almost similar biomechanical property as that pedicle screw construct. With Addition of the hook, it provides an extra rotational stability as well. Being an extra-pedicular screw it has high safety profile and needs less expertise for insertion.
Keywords: biomechanical study; extra pedicular screw and hook system; traditional pedicle screw; safety profile
634
RF280: Association between serum interleukin-17 levels and ectopic bone formation in OPLL patients with DISH
Tran Canh Tung Nguyen 1 , Zhongyuan He 2 , Yasuhito Yahara 1 , Hiroto Makino 1 , Yoshiharu Kawaguchi 1
1 Department of Orthopaedic Surgery, University of Toyama, Toyama City, Japan
2 Department of Orthopaedic Surgery, The Seventh Affiliated Hospital of Sun Yat-sen University, Shenzhen, China
Introduction: This study aimed to investigate the relationship between the severity and morphology of heterotopic ossification in the spine and sacroiliac (SI) joints and serum interleukin-17 (IL-17) levels in patients with ossification of the posterior longitudinal ligament (OPLL) with or without diffuse idiopathic skeletal hyperostosis (DISH). Material and Methods: A total of 103 patients with OPLL (DISH (−), n = 50; DISH (+), n = 53) and 53 age- and gender-matched controls were included in this study. The serum levels of IL-17 were analyzed, and the severity of ectopic ossification and the morphology of ectopic bone formation was evaluated. The SI joint variations were categorized into four types. Results: No significant differences were found in serum IL-17 levels between the OPLL and control groups. However, the DISH (+) group showed higher IL-17 levels than the DISH (−) group, especially in female patients (p = 0.003). Additionally, IL-17 levels were positively correlated with the number of Flat vertebral units (VUs) (R2 = 0.199, p = 0.012). Type 2 was more common in the DISH (−) group, while type 4 was more common in the DISH (+) group. IL-17 levels in type 4 were significantly higher in the DISH (+) group than in the DISH (−) group. Conclusion: The degree and morphological features of spinal and SI joint ossification are more closely related to IL-17 levels in OPLL patients with DISH, providing pathological and serological evidence of local inflammation for spinal heterotopic ossification and SI joint variations.
1030
RF281: The impact of varying drilling angles on cutting torque with a robotic system designed for breach detection during pedicle screw placement
Elie Saghbiny 1 , Lylian Leblanc 2 , Christina Bobbio 1 , Brahim Tamadatze 2 , Raphael Vialle 1
1 Pediatric Orthopaedics, University Institute for Spine Surgery, Sorbonne University, Paris, France
2 Institut des Systèmes Intelligents et Robotique (ISIR) - CNRS - INSERM - Sorbonne Université, Paris, France
Introduction: Pedicle screws are currently used to provide stable and rigid fixation of the spine, especially to treat severe scoliosis. The insertion of pedicle screws is challenging with the risk of neurological complications. Several robotic solutions are proposed in combination with navigation systems to guide the surgeon during pedicle screw insertion. None of the robotic assistance systems currently allow to detect a breach in real-time and stop the drilling of the pedicle before the perforation. This study aims to investigate how the cutting torque varies with the drilling angle in relation to the cortical bone. Material and Methods: To make a collection of signals we have established an original robotic setup including:
1. A robotic arm pre-certified for medical applications.
2. A self-made velocity-controlled power drill enabling continuous measurement of the cutting torque during drillings.
3. A threaded cutting instrument.
4. A clamping device allowing the fixation of the vertebra.
5. A camera recording the interior of the vertebral foramen for further verification.
With this configuration, we can synchronously measure the displacement of the robot, and the cutting torque while recording a video of the instrument exiting the bone. All recorded videos are reviewed frame by frame to determine the exact time of the breach with a precision of 0.33 ms. By measuring the depth of the instrument, a safety zone of 2 mm around the timestamp is chosen to process the signals. We collected 81 fresh lumbar vertebrae of pigs and 100 lumbar vertebrae of lambs. The angular velocity drill is set to 30 rpm. Drillings within the spinous process are executed perpendicular to the cortical bone of the spinal canal, while pedicle drillings involve varying angles. We employed the Beast (Bayesian evolutionary analysis by sampling trees) to identify breaches. For each vertebra, we compared the timestamp of breach as recorded by video footage with the timestamp detected by the algorithm. Subsequently, we calculated the corresponding depth for each timestamp and determined the difference between these depths (Δ𝑑𝑒𝑝𝑡ℎ). The angles of drillings are measured on a post-experience CT scan. Results: The drilling angles exhibit an average of 80.43° with a standard deviation of 16.17°. Specifically, for drillings conducted at a 90° angle, i.e. through the spinous processes, the mean Δ𝑑𝑒𝑝𝑡ℎ is -0.14 ± 0.83 mm, whereas for drillings at angles other than 90°, i.e. through the pedicles, the mean Δ𝑑𝑒𝑝𝑡ℎ is -0.6 ± 2.41 mm. However, it is worth noting that this observed difference in mean Δ𝑑𝑒𝑝𝑡ℎ between the two groups is not statistically significant (p = 0.08). In the subset of cases involving drilling at a 90° angle, Δ𝑑𝑒𝑝𝑡ℎ consistently remains below 2 mm across all vertebrae. Conversely, in cases where drilling occurs at angles other than 90°, Δ𝑑𝑒𝑝𝑡ℎ exceeds 2 mm in 13 instances. Discussion: This study highlights the utility of cutting torque as a valuable signal for detecting breaches outside the pedicle. It's important to emphasize that the drilling angle plays a significant role in potentially introducing errors in the accurate detection of breaches.
824
RF282: Vitamin D receptor gene polymorphism with a novel SNP is associated with risk & severity of spinal TB phenotypes
Uruj Zehra 1 , Shamaila Ejaz 1 , Muhammad Saad Ilyas 2 , Ijaz Ahmad 2 , Amer Aziz 2
1 Anatomy, University of Health Sciences Lahore, Lahore, Pakistan
2 Ghurki Trust Teaching Hospital, Orthopedic & Spine Surgery, Lahore, Pakistan
Introduction: Spinal tuberculosis (STB) is one of the most common extrapulmonary manifestations of tuberculosis in developing countries. Few studies have demonstrated the role of genetic susceptibility to STB including Vitamin D receptor (VDR) gene polymorphism, but with controversial findings. Since vitamin D plays a crucial role in bone metabolism, its role in the susceptibility and clinical severity of spinal TB needs to be explored especially in the areas where there is a huge burden of the disease. Therefore, the current study was planned to investigate the genotype and allele frequency of VDR- Fok-1 & Apa-1 in local population of Pakistan, furthermore the association of polymorphism with clinical severity and histological features was also established. Patients & Methods: Forty-three spinal TB patients who underwent spine surgery within an age range of 18-70 years were recruited after informed consent. Demographic details and relevant clinical profile were collected. X-rays and T1-T2 W magnetic resonance images (MRI) were assessed for spinal changes. Post-surgical tissue samples were analyzed for histological parameters. Polymerase chain reaction (PCR) and sequencing was done to analyze Fok-1 and Apa-1 polymorphisms of VDR gene in spinal TB patients and healthy controls. An additional rs11574113 polymorphism was found while analyzing sequence chromatogram and evaluated. Statistical analyses were done using SPSS and P- value less than 0.05 was considered significant. Results: Results showed that STB patients had significant association with heterozygous (Ff) & homozygous (ff) genotype of Fok-1 (p = 0.003) and with heterozygous (Rr) genotype of rs11574113 (p = 0.02). Wild type (FF) Fok-1, homozygous (aa) Apa-1 and heterozygous (Rr) genotype of rs11574113 polymorphisms were significantly associated with severe spinal phenotypes on imaging such as higher number of vertebral involvement (p = 0.01), complete vertebral bodies (p = 0.001) & intervertebral disc collapse (p = 0.002) and higher Pfirrmann grades (p = 0.03). Apa-1 polymorphism was also found to be significantly associated with well-formed granuloma (p = 0.01) on histological analysis. Conclusion: The study suggests a statistically significant role of Fok-1 and rs11574113 polymorphisms of VDR gene in increasing the risk and severity of spinal TB phenotypes. In Pakistani population a novel SNP rs11574113 is strongly associated with STB which is not reported in any other population, further exploration is important to manage the disease with better prognosis.
308
RF283: Ex vivo protein distinguishers of symptomatic and asymptomatic lumbar discs along the spectrum of degeneration
Theodore Choma 1 , Jacob Kramer 1 , Aaron Stoker 1 , Abigail Baumann 1 , Chantelle Bozynski 1 , Emily Leary 1 , Jinpu Li 1 , Donald Moore 1 , James Cook 1
1 Orthopaedic Surgery, University of Missouri, Columbia, USA
Introduction: Low back pain (LBP) is highly prevalent. While pathomechanisms for the development of LBP may vary between individuals, intervertebral disc degeneration (IVDD) is often implicated. While IVDD is commonly observed in patients with chronic LBP, many patients with IVDD are not symptomatic for LBP. It is unclear why some patients develop symptoms, while others with similar degrees of disc degeneration remain asymptomatic. It is suspected that the development of symptomatic IVDD is a multifactorial process that is affected by patient, tissue, cellular, and molecular factors that result in pain. This study aims to determine if differences in the ex vivo release of inflammation-, degradation-, and growth factor-related proteins by IVD tissues recovered from symptomatic (SYM) clinical patients and asymptomatic (ASYM) tissue donors could be identified for a given IVDD severity grade. Material and Methods: IVD tissues were recovered from SYM patients undergoing surgery for degenerative conditions (n=184, mean age 55.8y, 105F). IVD tissues were recovered from qualified ASYM recently deceased tissue donors (n=20, mean age 51.8y, 10F) without a reported history of back pain. Morphologic IVDD was quantified using the Thompson grade gross assessment (ASYM) or Pfirrmann MRI grading system (SYM) using pre-surgical images (T/P-grade). Tissue explants for each were created and cultured. On day 3 the media were collected for biomarker analysis, tissues were weighed. Media samples were tested for an array of inflammatory and degradative cytokines using Luminex assays. Biomarker concentrations were standardized to the wet weight of each explant and natural log transformed. SYM tissues were compared to ASYM tissues with adjustment for patient age, sex, obesity status, and their interactions. Two-sided significance was set at p ≤ 0.05. Results: Inflammatory Cytokines: SYM tissues released significantly (p ≤ 0.037) higher levels of GRO-α (T/P-grade 5), IL-1Ra (T/P-grades 2/3), MCP-1 (T/P-grade 5) and RANTES (All T/P-grades) compared to ASYM tissues. Additionally, SYM NP tissues released significantly (p ≤ 0.039) higher levels of IL-1Ra (T/P-grade 5), IL-6, IL-8, MIP-1β (T/P-grades 2/3 & 5), MIP-1α (All T/P-grades), and TNF-α (T/P-grade 5) compared to ASYM NP tissues. Matrix Metalloproteinases: SYM tissues released significantly (p ≤ 0.019) higher levels of MMP-2 and MMP-13 (T/P-grades 2/3 & 4), and significantly (p ≤ 0.023) lower levels of MMP-3 (T/P-grade 2/3) and MMP-8 (all T/P-grades), compared to ASYM tissues. Tissue Inhibitors of Metalloproteinases and Growth Factors: ASYM tissues released significantly (p ≤ 0.050) higher levels of TIMP-2, TIMP-3, and TIMP-4 (all T/P-grades) and TIMP-1 (T/P-grades 2/3) compared to SYM tissues. Conclusion: Degenerative disc tissues from symptomatic patients are associated with significantly higher release of inflammatory proteins and specific MMPs, and significantly lower release of TIMPs, compared to degenerative disc tissues from asymptomatic individuals with similar morphologic degeneration. These findings suggest that pro-inflammatory signaling and degradative enzyme activity, especially in the earlier stages of disease, may be important distinguishing factors in the development of symptomatic IVDD in patients. Interestingly, the majority of significant differences in biomarkers noted for SYM versus ASYM IVDs involved the nucleus pulposus when compared to the annulus fibrosis, suggesting that pain-related processes may be driven primarily from the nucleus pulposus.
1133
RF284: Whole-exome sequencing of a cohort of 19 families with adolescent idiopathic scoliosis (AIS): new candidate pathways
Laura Marie-Hardy 1 , Thomas Courtin 2 , Raphael Vialle 3 , Serge Zakine 3 , Pascal-Moussellard Hugues 1 , Alexis Brice 1
1 Brain Institute of Paris, Paris, France
2 Necker Hospital, Genetics, Paris, France
3 University Institute for Spine Surgery, Hôpital Trousseau, Pediatric Orthopaedics, Paris, France
Introduction: A significant genetic involvement has been known for decades in adolescent idiopathic scoliosis (AIS), a spine deformity affecting 1-3% of the world population, but while biomechanical and endocrinological theories have emerged, to date there is no single pathophysiological explanation. Material and Methods: Data from whole exome sequencing performed in 103 individuals in 19 multi-generational families have been filtered and analyzed via interaction pathways and functional categories analysis (Varaft, Bingo and Panther). Results: A list of 2566 variants has been compared to the literature, with a 18% matching rate. The molecular functions of the corresponding genes correspond largely to binding activities, notably to nucleotides, nucleosides, proteins, and calmodulin, suggesting a highly connected pathway. The cellular component analysis revealed significant enrichment in myosin-related and neuronal activities related categories. Conclusion: All together, these results reinforce the suspected role of the neuronal and muscular systems and the calmodulin pathway and suggest a role for DNA-binding activities in AIS physiopathology that may have been underestimated.
1437
RF285: Are supine and prone radiographs similar in assessing curve flexibility?
Wing Ki Cheung 1 , Prudence Cheung 1 , Jason Cheung 1
1 Department of Orthopaedics and Traumatology, University of Hong Kong, Hong Kong
Introduction: Spinal flexibility plays a crucial role in brace treatment and surgery management of Adolescent Idiopathic Scoliosis (AIS). Supine radiograph is one of the commonly used methods to determine the spinal flexibility1 and supine Cobb angle had a significant correlation with immediate in-brace Cobb angle2 which was a strong predictor of brace outcome3. However, while correlation provides insight into the relationship between variables, it does not provide a prediction equation. Prone and supine postures are similar in that no axial loading is applied on the spine but the latter is rarely studied. This study aims to compare the spinal morphology between prone and supine postures and to determine which spinal flexibility method is more appropriate to be used in bracing using first in-brace major Cobb angle as the evaluation. Methods: This was a radiographic analysis of 59 patients treated with bracing. Prebrace standing, prone, supine and first in-brace posteroanterior and lateral radiographs were obtained. Paired t-test of major Cobb angle, spinal flexibility, sagittal and pelvic parameters, and apical vertebral rotation and wedging between prone and supine postures was performed. Correlation of the two postures and first in-brace major Cobb angle was determined. Multivariable regression analysis of supine and prone and immediate in-brace Cobb angles were studied and the equations derived were used to calculate the predicted immediate in-brace Cobb angles, which was then compared to the actual value. Results: There were significant differences in all parameters except spinal flexibility between prone and supine postures (all p < 0.05). These findings indicated that there were notable variations in spinal morphology between the two positions. This discrepancy may be explained by the contract surface location, which is the back during the supine posture and the chest and abdomen during the prone posture. The spine tends to be extended more in the prone posture than in the supine posture. Consequently, it is crucial for clinicians to acknowledge that the spine respond differently during both postures. The correlation of major Cobb angle between first in-brace and supine, and between first in-brace and prone were significant positive (r = 0.54, p < 0.05; r = 0.58, p < 0.05). 45.76% and 3.39% of the supine predicted and prone predicted first in-brace Cobb angle was more than 5 degrees different from the actual values. Thus, prone major Cobb angle exhibited a stronger positive correlation with the first in-brace major Cobb angle compared to the supine major Cobb angle. Additionally, the prone predicted first in-brace major Cobb angle showed greater accuracy compared to the one predicted by supine major Cobb angle. Conclusion: Result of this study suggested that the spinal flexibility may be similar between postures, but with notable differences in sagittal and pelvic parameters. When choosing the spinal flexibility methods in determining the brace outcomes, prone radiographs may be better than the supine radiographs since prone major Cobb angle had a better prediction result of first in-brace Cobb angle than the supine major Cobb angle. Clinicians should consider the sagittal and pelvic parameters when choosing the curve flexibility assessment in decision making.
1220
RF286: Automatic laminectomy cutting plane planning based on artificial intelligence in robot-assisted laminectomy surgery
Zhuofu Li 1 , Weishi Li 1
1 Orthopaedics, Peking University Third Hospital, China
Introduction: Laminectomy is the standard treatment for symptomatic lumbar spinal stenosis refractory to conservative management. How to choose the appropriate laminectomy range is a problem faced by surgeons. Especially with the advent of the robot era, a set of strategies for automatic laminectomy cutting plane planning is needed to simplify this procedure. In this study, we propose a new way to achieve automatic laminectomy cutting plane planning, which was based on a deep learning landmark detection technology. Material and Methods: 1302 vertebra CT images were included, including 782 CT images in the training set, 260 CT images in the verification set and 260 CT images in the test set. The 7 landmarks were manually annotated by an attending physician with 2 years of experience to ensure the reliability of the data. We used the Euclidean distance as the evaluation criterion. By identifying 7 landmarks for each vertebra, we can generate a spatial coordinate system and finally generate the laminectomy plane. Another 320 vertebra CT image data were used to test our cutting plane planning method. Results: The average positioning error of landmarks was 0.65 ± 0.70 mm. And 97.18% of the longitudinal planes, 99.38% of the transverse planes reached the excellent level. Conclusion: The results show that the effect of this strategy is satisfactory. More studies are needed in the future to confirm the reliability of this strategy.
2523
RF287: A novel 3D printed titanium cage, mirroring the mechanical characteristics of vertebral bone, reveals reduced subsidence and minimizes scatter on CT scans
Willems Karel 1 , Amélie Willems 2
1 Orthopaedic Surgery, AZ Delta Roeselare, Roeselare, Belgium
2 Orthopaedic Surgery, Cathololic University of Leuven, Leuven, Belgium
Introduction: Posterior interbody fusion is frequently used to treat degenerative low back pain. Titanium and PEEK are two of the most popular materials for fusion cages. PEEK is non-osteoinductive and leads to limited osteointegration because it is inert to the human body. Titanium cages potentially create more subsidence and more scattering images on CT scans, blurring the evaluation of formation and ingrowth of bone. This unique design of contact surface of the new 3D printed Titanium cage, creates optimal biomechanical conditions for bone settlement and ingrowth of bone and additionally mechanically stimulates bone remodeling. Materials and Methods: We analyzed the clinical and radiological results of 50 patients 3 months after surgery. We only included patients older than 50 years, who underwent one- or two-level lumbar fusion. To assess this, we employed the Visual Analog Scale (VAS) score, the Oswestry score, and performed a CT scan three months after surgery to evaluate bone formation at the endplate, the space between the cages and the presence of subsidence. Discussion: To avoid subsidence, we utilize the mechanical physical properties close to the bone by using a titanium mesh-like endplate surface. Additionally, we incorporate 3D printing topography, ensuring immediate stability while preserving the same elasticity as bone. Thanks to its hollow core, this design results in significantly reduced scattering on CT scans, enabling us to observe bone formation more effectively. Our initial findings at the three-month mark indicated minimal subsidence and showed bone formation at the contact surface of the endplate. Conclusions: The novel 3D-printed titanium cage is a secure implant that minimizes subsidence, fosters bone formation, and leads to reduced CT-scan artifacts.
216
RF288: Angle of obliquity of exiting nerve root on MRI, a test to replace dynamic X-Rays, “current gold stranded”, in detecting spondylolisthesis
Dattaprasanna Katikar 1
1 Neurosurgery, Balwant Institute of Neurosurgery and Intensive Trauma Care, Solapur, India
Objective: MRI has become investigation of choice for patients of low back pain with radiculopathy. On MRI in about 34 to 40% of patients, spondylolisthesis may be missed. We had published a retrospective study of 247 patients, in which we found very high correlation between oblique exiting nerve root on saggital MRI and spondylolisthesis, confirmed by dynamic radiographs. We have done a prospective study to validate these findings. Methods: We prospectively studied 1000 patients who attended Out Patients Department for lumbosacral radiculopathy and had undergone MRI. We did standing lateral flexion extension X-Rays in all these patients. We had described an angle to measure obliquity of the exiting nerve root. "Angle of obliquity of the exiting nerve root" to detect spondylolisthesis. We measured this angle on both right & left sides. If the angle was more than 105° there was spondylolisthesis and if it was less than 105° there was no spondylolisthesis. We compared our findings with findings on dynamic radiographs and statistically calculated the sensitivity and specificity of our test. Results: We present demographic data of the patients included in our study. We found that obliquity of the exiting nerve root (> 1050) very highly correlates with spondylolisthesis. We found that if angle of obliquity is more than 1200, the listhesis is very likely to be grade two. If one side angle is > 1050 and other side is < 1050 then the patient had mild slip < 3 mm. We present our analysis and finding, which prove that our test can detect spondylolisthesis with equal accuracy of dynamic X-ray's. “The current gold standard”. Conclusion: Obliquity of the exiting nerve root is very easy to detect on MRI. It has a very high sensitivity and Specificity for detecting spondylolisthesis. It has a potential to replace dynamic X-rays as ‘gold standard’ in detecting spondylolisthesis.
Disclosure: The author has no declaration or conflict of interest.