Arthroplasty-cervical
812
P001: Recovery kinetics following cervical spine surgery
Tejas Subramanian 1 , Daniel Shinn 1 , Maximillian Korsun 1 , Kasra Araghi 1 , Olivia Tuma 1 , Chad Simon 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Nishtha Singh 1 , Tomoyuki Asada 1 , Pratyush Shahi 1 , Evan Sheha 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Very few studies have described return to activities (driving, work, discontinuation of opioids) following cervical spine surgery. This is a big gap in the literature as preoperative counseling and expectations before surgery are important. Here we aimed to study recovery kinetics and the factors associated with them following cervical spine surgery. Material and Methods: Patients were queried from a prospectively maintained database. Patients that underwent either anterior cervical discectomy and fusion (ACDF) or cervical disc replacement (CDR) were included. Data collected included preoperative patient-reported outcome measures, return to driving, return to working, and discontinuation of opioids data. A multivariable regression was conducted to identify the preoperative characteristics and factors associated with return to driving by 15 days, return to working by 15 days, and for discontinuing opioids by 30 days. Results: In total, 70 ACDF patients and 70 CDR patients were included. Overall, 98.2% of ACDF patients and 98% of CDR patients returned to driving in 16 and 12 days, respectively; 85.7% of ACDF patients and 90.9% of CDR patients returned to work in 16 and 14 days; and 98.3% of ACDF patients and 98.3% of CDR patients discontinued opioids in a median of 7 and 6 days. Though not significant, minimal [odds ratio (OR)=1.65, p=0.085] and moderate [OR=1.79, p=0.072] disability was associated with greater odds of returning to driving by 15 days. Similarly, sedentary work [OR=0.8, p=0.08] and preoperative narcotics [OR=0.86, p=0.198] were associated with decreased odds of returning to driving by 15 days. Return to work by 15 days was associated with returning to drive by 15 days [OR=1.37, p=0.019]. Medium [OR=0.81, p=0.053] and heavy [OR=0.78, p=0.025] intensity occupations were associated with decreased odds of returning to work by 15 days. As was returning to drive by 15 days [OR=1.31, p=0.015] and discontinuing opioids by 10 days [OR=1.28, p=0.03]. High school as the highest level of education [OR=0.75, p=0.006], sedentary work [OR=0.79, p=0.03], retired/not working [OR=0.69, p=0.001] were all associated with decreased odds of discontinuing opioids by 30 days. Returning to drive by 30 days was associated with increased odds of discontinuing opioids by 30 days. Conclusion: Recovery kinetics for ACDF and CDR as comparable. Most patients return to activity following ACDF and CDR, within 16 days for all activities for both surgical procedures. These findings serve as an important compass for preoperative counseling.
965
P002: Severe obesity is an independent risk factor of early readmission and non-home discharge after cervical disc replacement
Tejas Subramanian 1 , Daniel Shinn 1 , Pratyush Shahi 1 , Troy Amen 1 , Kasra Araghi 1 , Eric Zhao 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Avani Vaishnav 1 , Tomoyuki Asada 1 , James Dowdell 1 , Evan Sheha 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Despite growing interest in cervical disc replacement (CDR) for conditions such as cervical radiculopathy, limited data exists describing the impact of obesity on early postoperative outcomes and complications. The goal of this study was to compare the demographics, perioperative variables, and complication rates following CDR. Material and Methods: The 2005-2020 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) datasets were queried for patients who underwent primary 1- or 2-level CDR. Three cohorts were created: Non-Obese (BMI:18.5-29.9), Obese Class-I (BMI:30-34.9), Obese Class-II/III (BMI ≥ 35). Morbidity was defined any complication within 30 days postoperatively. Rates of 30-day readmission, reoperation, morbidity, individual complications, length of stay, frequency of non-home discharge disposition were collected.
Results: A total of 5397 patients were included for analysis. 3130 were non-obese, 1348 were Obese-class-I, and 919 were Obese-Class-II/III. There were more 2-level CDRs performed in the Class-II/III cohort compared to the non-obese group (25.7% vs 21.5%, respectively; p < 0.05). Class-II/III had more non-home discharges than Class-I and non-obese (2.1% vs 0.5% vs 0.7%, respectively; p < 0.001). Readmission rates differed as well (non-obese: 0.5%, Class-I: 1.1%, Class-II/III: 2.1%; p < 0.001) with pairwise significance between class-II/II and non-obese. Class II/III obesity was an independent risk factor for both readmission (OR: 3.32, p = 0.002) and non-home discharge (OR 2.51, p = 0.02). Neither 30-day reoperation nor morbidity rates demonstrated significance. No mortalities were reported.
Conclusion: Although obese class-II/III were risk factors for 30-day readmission and non-home discharge, there was no difference in reoperation rates or morbidity. CDR procedures can be performed independent of obesity status.
1023
P003: Choice of the open side in unilateral open-door laminoplasty for cervical ossification of the posterior longitudinal ligament
Yifan Tang 1
1 Orthopeadics, Shanghai Changzheng Hospital, Shanghai, China
Background: No literature has reported which side of the vertebral arch should be chosen as the open side in open-door laminoplasty (UODL) for lateral cervical ossification of posterior longitudinal ligament (OPLL). This article retrospectively analyzed the included patients to determine the optimal open side in unilateral UODL for lateral cervical OPLL. Methods: Patients with lateral cervical OPLL who were treated with UODL between 2013 and 2018 were retrospectively analyzed in two groups: Group A, where the open side was contralateral to the ectopic bone, and Group B, where the open side was ipsilateral to the ectopic bone. The Japanese Orthopaedic Association (JOA) Score, JOA recovery rate, spinal canal enlargement rate, cervical range of motion (ROM), and spinal cord area (SCA) were measured to evaluate and compare the clinical outcomes between the two groups. Statistical analysis was performed by t test and Hotelling T2 test. Results: There was no significant difference in patient demographics and major complications between the two groups. The postoperative JOA Score and JOA recovery rate in Group A were significantly higher than those in Group B. There was no significant difference in cervical ROM within or between the two groups during the 2-year follow-up period, nor was there significant difference in spinal canal enlargement between the two groups. However, both postoperative SCA and increased SCA in Group A were significantly higher than those in Group B. Conclusion: The contralateral open side approach is preferable to the ipsilateral open side approach in UODL for lateral cervical OPLL.
Keywords: contralateral open side, laminoplasty, lateral ectopic bone, open door, open side, ossification of posterior longitudinal ligament, retrospective study, spinal canal enlargement, spine drift, unilateral open-door laminoplasty.
1037
P004: The relationship between craniocervical sagittal balance and clinical and radiographic outcomes of cervical disc replacement: a retrospective study
Yi-Wei Shen 1 , Ying Hong 2 , Hao Liu 1
1 Department of Orthopedics
2 Department of Operation Room and Anesthesia Center, West China Hospital, Sichuan University, Chengdu, China
Introduction: Cervical disc replacement (CDR) is an effective procedure for the treatment of cervical radiculopathy and myelopathy. As one of the most important functions of the cervical spine is to support the mass of the head, the cranial position in the sagittal plane may play an essential role in cervical sagittal balance and surgical outcomes. Previous studies have shown the significance of indices evaluating the balance of the gravity of the head in patients who underwent ACDF and laminoplasty. However, the effect of craniocervical sagittal balance on the patient-reported outcomes and radiological results of CDR has been poorly studied. This study aimed to evaluate the craniocervical sagittal alignment parameters in patients who underwent CDR to determine whether preoperative and postoperative craniocervical sagittal alignment affects the clinical and radiological outcomes after CDR. Material and Methods: Patients who underwent 1-level and 2-level CDR were retrospectively analyzed. Clinical outcomes were evaluated using scores on the Japanese Orthopaedic Association (JOA), Visual Analogue Scale (VAS), and Neck Disability Index (NDI). The craniocervical sagittal alignment parameters, including the C0-C2 Cobb angle, C2-C7 Cobb angle, C2 slope, T1 slope, C2- C7 sagittal vertical axis (SVA), C1-C7 SVA, the center of gravity of the head (CGH)-C7 SVA, and range of motion (ROM) at the surgical segments were measured. Results: A total of 169 patients were involved. Both the pre- and postoperative C2 slope were significantly higher in the less mobile group than in the more mobile group (preop: 13.63 ± 8.34° vs. 11.18 ± 7.02°, p = 0.035; postop: 12.15 ± 7.15° vs. 9.50 ± 6.45°, p = 0.011). Analogously, the CGH- C7 SVA before and after surgery was significantly larger in the less mobile group (preop: 18.38 ± 16.54 mm vs. 13.91 ± 13.33 mm, p = 0.036; postop: 17.40 ± 11.43 mm vs. 12.48 ± 11.98 mm, p = 0.009). Patients with a higher preoperative C2 slope and CGH-C7 SVA had lower cervical lordosis and ROM after surgery. There were no significant differences in the clinical outcomes between patients with different sagittal balance statuses. Patients with radiographic adjacent segment pathology (rASP) had significantly higher CGH-C7 SVA (19.57 ± 14.16 mm vs. 13.77 ± 13.83 mm, p = 0.014) and C2- C7 SVA (20.83 ± 9.62 mm vs. 17.06 ± 9.91 mm, p = 0.041) before surgery. Conclusion: Craniocervical sagittal balance is associated with cervical lordosis and ROM at the index level after CDR. A higher preoperative SVA is related to the presence and progression of rASP. A relationship between sagittal alignment and clinical outcomes was not observed.
1092
P005: Cervical disc arthroplasty for patients with osteopenia: a matched cohort study
Junbo He 1 , Hua Chen 1 , Hao Liu 1
1 Orthopedic Surgery, West China Hospital, Sichuan University, Chengdu, China
Introduction: Osteoporosis was unanimously listed as an exclusion criterion for cervical disc arthroplasty (CDA). However, there was a paucity of data on CDA patients with osteopenia. This study aims to evaluate postoperative outcomes of single-level CDA in patients with osteopenia and compare these results with a matched cohort of normal bone mineral density (BMD). Material and Methods: This study included 38 patients with osteopenia who underwent single-level CDA. A 1:1 match was utilized based on gender, follow-up time, and arthroplasty level. BMD was assessed with dual-energy x-ray absorptiometry. Clinical, radiographic data, and BMD-related complications were recorded. Results: The osteopenia group achieved satisfactory improvements in clinical outcomes, with no significant intergroup differences. Additionally, there were no significant differences between groups in any of the radiological parameters, either in cervical alignment or segmental height, or range of motion. In terms of BMD-related complications, the radiological incidence rate of adjacent segmental degeneration (ASD) and heterotopic ossification (HO) was comparable in both groups, respectively, with a similar composition of ROM-limiting HO. However, the osteopenia group had a tendency of more implant subsidence (2.7% vs. 15.2%). According to the logistic regression analysis, the osteopenia group had a significantly higher incidence rate of anterior bone loss (ABL) than the normal group (OR=5.37, 95% CI: 1.50 - 19.22). Conclusion: Single-level CDA for patients with osteopenia achieved similar improvements in clinical outcomes compared with the normal BMD group and maintained satisfactory sagittal balance and segmental height. However, the possibility of postoperative ABL and implant subsidence remains a source of concern. Single-level CDA should not be routinely recommended for patients with osteopenia.
Keywords: osteopenia; bone mineral density; cervical disc arthroplasty; anterior bone loss
1113
P006: Comparison of clinical and imaging outcomes of cervical disc replacement in patients wit different housfield units
Haimiti Abudouaini 1 , Hao Liu 2 , Beiyu Wang 2
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
2 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Objective: To compare clinical and imaging outcomes after cervical disc replacement (CDR) in patients with different Hounsfield units (HU). Methods: We performed a retrospective study of patients with cervical degenerative disc disease treated by 1-level and 2-level Prestige-LP arthroplasty. The patients were divided into group A (HU < 320), group B (HU 320-347), and group C (HU > 347) according to the results of cervical vertebral HU measurement in the literature, and the clinical and radiographic results were compared among the 3 groups. Results: A total of 127 patients were reviewed, comprising 13 patients in group A, 31 patients in group B, and 83 patients in group C. The clinical parameters were significantly improved postoperatively in the 3 groups (p < 0.05). However, no significant differences were found among the 3 groups at the final follow-up (p > 0.05). The mean postoperative intervertebral space height (ISH) was 4.76 ± 0.45 mm, 5.23 ± 0.81 mm, and 6.26 ± 1.12 mm in the 3 groups, respectively. The postoperative ISH in group C was significantly higher than those in the other groups at the final follow-up (p < 0.001). One patient in group A and 1 patient in group B had implant subsidence, and degeneration at the inferiorly adjacent level was radiographically identified in 30.77% patients in group A, 16.13% patients in group B, and 9.64% patients in group C. However, there were only significant differences between group A and group C in subsidence (p [ 0.011) and occurrence of adjacent level degeneration (p = 0.032). Conclusions: The HU value has a large variation range among the patients with T-score > -2.5. We found significantly increased rates of implant subsidence, loss of ISH, and adjacent segment degeneration in patients with lower HU value undergoing CDR. However, these radiographic complications did not predispose patients with lower HU value to worse clinical outcomes. Routine application of HU combined with dual-energy X-ray absorptiometry measurement to evaluate bone quality may help to screen the optimal candidates for CDR and reduce the implant-related complications.
Keywords: cervical degenerative disc disease; cervical disc replacement; computed tomography; hounsfield units; subsidence
1159
P007: Pit fall and fundamental skill for cross tightening in cervical laminoplasty
Takahiro Iizuka 1 , Tokuji Kashiro 1 , Hiroshige Debata 1 , Tetsuro Takai 1 , Toyohito Iwami 1
1 Orthopedic Spine Surgery, Kouseikai Takai Hospital, Nara, Japan
Introduction: We have reported Cross Tightening Technique for Cervical Laminoplasty which reduced the post-operative neck pain and preserved ROM of cervical spine in 2022 and 2023 GSC. We would like to show the technical problems surgeons have when they first try to Cross Tightening. Material and Method: We retrospectively review our surgical technique of Cross Tightening.
Original Cross Tightening
1. Skin incision was made in midline over C2-Th1
2. Multifidus Muscles (MM) attached C2 were ligated with 1-0 Ethbond before detachment.
3. MM attached C7 were also ligated with 1-0 Ethbond before detach. 4. Laminoplasty was performed with left open using spacers (Chanber: Nuvasive).
5. Muscles were reconstructed in an anatomical direction tightening to the opposite fascia.
Results and Counterplan: If you tighten MM to the fascia with strong tension, the ligated muscle will be easily torn off. So we recommend tightening the muscles to less than 40 degrees cranially with adequate tension. Once MM is torn off, it is quite difficult to re-ligate it to the original site in particular elder patients have very fragile muscles. We recommend #1 ligating MM and its aponeurosis and #2 tightening MM to less than 40 degrees with adequate tension. We also recommend #3 neck rest with a color for 2-4 weeks. Conclusion: Gentle procedure for MM will preserve the function of MM and other Muscles when cervical laminoplasty. Cross Tightening will reduce the postoperative neck pain and preserve neck ROM.
1236
P008: Cervical disc arthroplasty combined with two-level ACDF for the treatment of contiguous three-level cervical degenerative disc disease: a comparative study
Beiyu Wang 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Objective: To compare the differences among constructs with one-level cervical disc arthroplasty (CDA) and two-level anterior cervical discectomy and fusion (ACDF). Methods: A retrospective study was conducted involving patients who underwent one-level CDA and two-level ACDF between June 2012 and July 2020. According to the different locations of CDA and ACDF, we divided the constructs into three types: type Ⅰa: CDA-ACDF-ACDF; type Ⅰb: ACDF-CDA-ACDF; type Ⅰc: ACDF-ACDF-CDA. The differences of clinical and radiological outcomes were evaluated. Results: Fifty-three patients were included with 29 in type Ⅰa group, 11 in type Ⅰb group, and 13 in type Ⅰc group. After surgery, all groups showed significant improvement in Japanese Orthopedic Association, Neck Disability Index, and Visual Analog Scale scores (p < 0.001). Range of motion (ROM) of the total cervical spine in type Ⅰc group decreased significantly compared with those in type Ⅰa and type Ⅰb groups (p < 0.05). The fusion rates of the superior ACDF segments were significantly higher at 6 and 12 months postoperatively than those of the inferior ACDF segments (p < 0.05). Conclusions: The clinical outcomes were similar among constructs concerning different locations of CDA and ACDF in three-level hybrid surgery. ROM of the cervical spine in type Ⅰc group decreased significantly compared with that in type Ⅰa and type Ⅰb groups. The fusion rates of superior ACDF segments were higher at early time points after surgery than those of inferior ACDF segments.
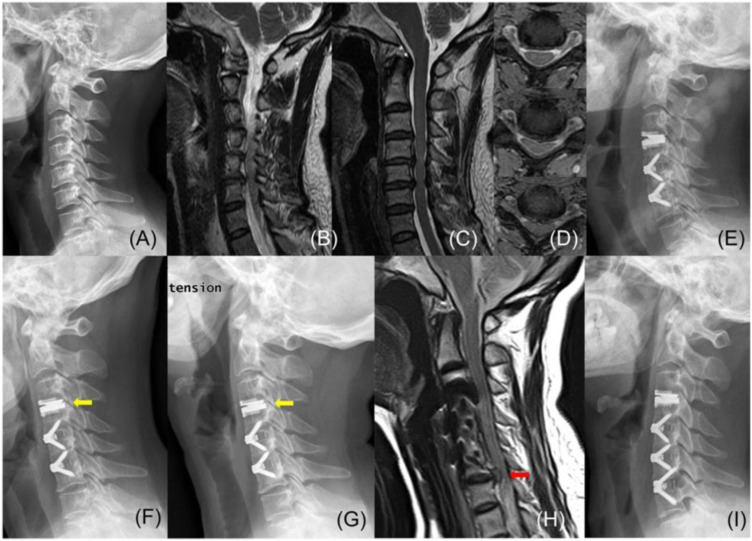
Figure 1. One case of ASD. A 41-year-old woman diagnosed with spondylotic radiculopathy at C3-4 and spondylotic myelopathy at C4-5 and C5-6 (A–D). Type Ⅰa HS was performed (E). At 3.5 years after surgery, the patient came back to our hospital with a severe symptom. A class Ⅳ HO was observed at the CDA segment with the absence of motion (F and G), and ASD was found at the inferior adjacent level (H). An addition ACDF was performed (I). ACDF, anterior cervical discectomy and fusion; ASD, adjacent segment disease; CDA, cervical disc arthroplasty; HS, hybrid surgery.
1250
P009: Cervical disc replacement shows similar outcome in clinical outcomes to anterior cervical discectomy and fusion in patients with significant neck pain
Tomoyuki Asada 1 , Tejas Subramanian 1,2 , Kasra Araghi 1 , Nishtha Singh 1 , Olivia Tuma 1 , Myles Allen 1 , Cole Kwas 1 , Joshua Zhang 1 , Yeo Eun Kim 1 , Eric Mai 1 , Avani Vaishnav 1,3 , Chad Simon 1 , Maximillian Korsun 1 , Sravisht Iyer 1,2 , Sheeraz Qureshi 1
1 Hospital for Special Surgery, New York, USA
2 Weill Cornell Medical, New York, USA
3 Boston Medical Center, Boston, USA
Introduction: While anterior cervical discectomy and fusion (ACDF) has historically been thought to better treatment for neck pain, recent studies suggested positive outcomes in these patients after cervical disc replacement (CDR). However, there is a lack of research comparing the clinical outcomes of ACDF and CDR specifically in patients with predominant neck pain. This study aimed to identify and compare the clinical outcomes between CDR and ACDF in patients who experience neck pain equal to or greater than arm pain preoperatively. Material and Methods: Patients with preoperative neck pain greater than or equal to arm pain in visual analog scale (VAS) who underwent CDR or ACDF from April 2017 to Oct 2021 were included in this study. Data collected were patients’ demographics and patient-reported outcome measures (PROMs) including VAS neck, VAS arm, Neck Disability Index (NDI), 12-item Short Form Survey Physical (SF-12 PCS) and Mental Component Score (SF-12 MCS), and Patient-Reported Outcomes Measurement Information System-Physical Function (PROMIS). Patients with predominant neck pain were defined as those with VAS neck ≥ VAS arm pre-operatively. Three post-operative time points for PROMs were defined namely preoperative, ≤ 3 months postoperative, and ≥ 1 year postoperative time point, and MCID achievement at ≥ 1 year postoperative time point. Results: One hundred and nineteen patients (40 CDR and 79 ACDF) were included in the study. Both groups showed significant improvement in NDI (p < 0.001) and VAS (p < 0.001) neck without significant differences between the groups (NDI: p = 0.098, VAS neck: p = 0.457). The clinical courses of SF-12 PCS (p = 0.751), SF-12 MCS (p = 0.242), and PROMIS (p = 0.515) were comparable between the ACDF and CDR groups. SF-12 PCS was worsened until the ≤ 3 months time point in both groups (p = 0.028). MCID achievement rate at the ≥ 1 year postoperative time point was similar between the groups for NDI (CDR:81.6% vs. ACDF: 77.6%, p = 0.626) and VAS neck (CDR: 60.0% vs. ACDF: 46.8%, p = 0.245). There was no significant difference in MCID achievement of VAS arm, SF-12 PCS, SF-12 MCS, and PROMIS (VAS arm: 14 (35.0%) vs. 31 (39.2%), p = 0.802; SF-12 PCS: 14 (35.9%) vs. 32 (45.7%), p = 0.428; SF-12 MCS: 18 (46.2%) vs. 33 (47.1%), p = 1.000; PROMIS: 22 (61.1%) vs. 50 (70.4%), p = 0.452). Conclusion: CDR demonstrated a significant clinical improvement in all PROMs comparable to ACDF. CDR can be a viable option as a treatment for cervical degenerative disease with prominent neck pain.
1252
P010: Does age affect the clinical outcomes of cervical disc replacement?
Tomoyuki Asada 1 , Tejas Subramanian 1 , Kasra Araghi 1 , Chad Simon 1 , Nishtha Singh 1 , Maximillian Korsun 1 , Myles Allen 1 , Cole Kwas 1 , Olivia Tuma 1 , Avani Vaishnav 1,2 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Eric Kim 1 , Russel Huang 1 , Todd Albert 1 , Sravisht Iyer 1 , Sheeraz Qureshi 1
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, Boston, USA
Introduction: Initially, cervical disc replacement (CDR) was indicated exclusively for soft disc herniation. Most studies analyzing clinical outcomes of CDR have focused on relatively young cohorts. There is limited data on the outcomes of CDR in older patients. Therefore, this study aims to investigate the clinical outcomes of CDR in older patients. Material and Methods: This study was a retrospective study for the patients who underwent 1- or 2- levels of CDR. The demographic data and cervical alignment were collected preoperatively. Patient-reported outcomes including the neck disability index (NDI), visual analog scale (VAS) arm, and VAS neck were collected as a primary outcome at 12 weeks, 6 months, or 1-year postoperative time points. Clinical courses were assessed with repeated measure two-way ANOVA and MCID achievement between ≥ 50 years old and < 50 years old patients. Results: Clinical improvement courses for NDI (p = 0.052), VAS arm (p = 0.682), and VAS neck (p = 0.338) were comparable between patients ≥ 50 and < 50 years old. Symptomatic improvement occurred in the first 12 weeks, with 58.6 % in the ≥ 50 group and 55.2% in the < 50 group achieving MCID of NDI at 12 weeks (p = 0.828) and continued through 6 months postoperatively. At the ≥ 1 year time point, 72.2% of the ≥ 50 group and 83.0% of the < 50 group achieved MCID in NDI, which was not significant different (p = 0.408). Conclusion: CDR can improve the symptoms effectively postoperatively in patients over 50 years old. These patients demonstrated similar outcomes to younger patients. Thus, even in older patients, CDR is a viable treatment option for various cervical spinal pathologies.
1254
P011: Pretic-I was a safe and effective artificial cervical disc prosthesis- a retrospective and comparative study with 5-year follow-up
Chengyi Huang 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: The newly designed cervical disc prosthesis, Pretic-I, had been finished its limited clinical use for over 5 years. At a short-term follow-up of 2 years, we obtained satisfactory clinical results. The long-term clinical efficacy and safety of Pretic-I will now be analyzed. Material and Methods: Peri-operative parameters included intra-operative blood loss, operation time, of-bed time. Clinical parameters included visual analogue scale (VAS) for arm and neck, neck disability index (NDI), and Japanese Orthopaedic Association (JOA) score. Radiological parameters included C2-7 Cobb angle, Shell angle, and the range of motion (ROM) of C2-7, functional segment unit (FSU), and adjacent FSU. The CDA-related complications included adjacent segment degeneration (ASDeg), adjacent segment disease (ASDis), heterotopic ossification (HO), prosthesis subsidence, prosthesis displacement, and dysphagia. Results: A total 64 patients from two independent centers received a single-level CDA with Discover (n = 32) and Pretic-I (n = 32), and all of patients finished a 5-year follow-up. There are no significant differences between two groups in peri-operative parameters. The clinical parameters improved greatly in Pretic-I group (p < 0.0001), and there’s no statistical difference from Discover group. Furthermore, Pretic-I could slightly improve the cervical curvature (15.08 ± 11.75 to 18.00 ± 10.61, p = 0.3079) and perfectly maintain the Shell angle (3.03 ± 3.68 to 2.23 ± 4.10, p = 0.1988), cervical ROM (52.48 ± 14.31 to 53.30 ± 11.71, p = 0.8062) and FSU ROM (12.20 ± 4.52 to 10.73 ± 4.45, p = 0.2002). The incidence of high-grade HO (Grade III-IV) at the final follow-up was significantly lower in Pretic-I group than in Discover group (12.50% vs. 34.38%, p = 0.0389, Statistical Power = 95.36%). The incidences of other CDArelated complications in Pretic-I group were also well-accepted, comparable to the Discover group, without significant differences. Conclusion: CDA with Pretic-I demonstrated a well-accepted and sustained clinical outcome, with a significantly lower incidence of high-grade HO. This newly designed prosthesis is expected to become an alternative choice for cervical disc prosthesis in the future.
Keywords: cervical disc arthroplasty, Pretic-I, Discover, adjacent segment disease, heterotopic ossification
1278
P012: Early outcomes of cervical disc arthroplasty in patients with autoimmune arthritis: a case series
Nishtha Singh 1 , Avani Vaishnav 1 , Chad Simon 1 , Tomoyuki Asada 1 , Cole Kwas 1 , Kasra Araghi 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Myles Allen 1 , Eric Kim 1 , Evan Sheha 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Cervical disc arthroplasty (CDA) is a motion-sparing solution primarily indicated for a cervical disk herniation causing radiculopathy or myelopathy. An exclusion criterion for the initial CDA trials was autoimmune arthritis. As better clinical outcomes following CDA were reported, suggesting its superiority to fusion surgery for disc herniation, indications for CDA have begun to expand to include a wider range of patient comorbidities. However, due to the historical exclusion criteria, the clinical outcomes following CDA in patients with autoimmune arthritis are limited and are not well reported in the literature. The purpose of this study is to investigate the clinical outcomes following CDA in patients with autoimmune arthritis. Material and Methods: A single-center case series of 12 patients with a pre-operative diagnosis of autoimmune arthritis undergoing CDA from July 2016 to April 2022 was conducted. Patient-reported outcome measures (PROMs) were utilized, namely, the NDI (Neck Disability Index), SF-12 PHS (Short Form 12-Item Physical Health Score), SF-12 MHS (Short Form 12-Item Mental Health Score), VAS (Visual Analog Scale), and PROMIS-PF (Patient-Reported Outcomes Measurement Information System-Physical Function) were utilized at 2 weeks, 6 weeks, and 12 weeks. Descriptive analysis was performed on the PROMs data and compared with a Mann-Whitney Test. Results: Out of 12 patients, 9 were male, and 3 were female. The average age was 41 ± 10 years. Five patients had psoriasis, two had rheumatoid arthritis, one had sarcoidosis, one had systemic lupus erythematosus, and three had unclassified arthritis. Eight patients underwent a one-level CDA, and four patients underwent a two-level CDA. In all cases, there were no perioperative complications. The post-op PROMs at 2 weeks were as follows: NDI 23.0 ± 19.2, SF-12 PHS 36.3 ± 13.1, SF-12 MHS 51.6 ± 10.0, VAS neck 2.7 ± 2.1, VAS arm 0.9 ± 1.5, and PROMIS-PF 43.8 ± 8.8. At 6 weeks post-operation, NDI improved significantly (20.8 ± 16.9, p < 0.05). At 12 weeks post-operation, there was a reduction in mean NDI (20.6 ± 16.5), VAS neck (2.1 ± 1.2), and VAS arm (1.0 ± 2.2) (p > 0.05). Conclusion: The clinical outcome of CDA in patients with autoimmune arthritis was found to be safe and comparably effective to non-autoimmune patients with original indications. Looking forward, a larger cohort with consistent follow-up will be essential to provide evidence for the long-term clinical success of CDA in the autoimmune arthritic population.
1281
P013: Clinical outcomes of cervical disc arthroplasty (CDA) in keel vs keel-less implants: early results
Nishtha Singh 1 , Tomoyuki Asada 1 , Chad Simon 1 , Eric Mai 1 , Kasra Araghi 1 , Maximillian Korsun 1 , Olivia Tuma 1 , Avani Vaishnav 1 , Cole Kwas 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Myles Allen 1 , Eric Kim 1 , James Dowdell 1 , Evan Sheha 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Cervical Disc Arthroplasty (CDA) has proven to be comparable to Anterior Cervical Discectomy and Fusion (ACDF) for treating various cervical pathologies. CDA has also shown a much greater potential in preserving the cervical range of motion. Keel and Keel- less implants have been utilized for CDA but the clinical outcomes for the patients for the respective implants have yet to be explored in detail. We aim to compare the patient-reported outcome measures (PROMs) for the CDA for keel vs keel-less groups. We aim to compare the patient-reported outcome measures (PROMs) for the CDA for keel vs keel-less groups. Material and Methods: 37 patients with keeled implants CDA and 122 with keel-less implant CDA were retrospectively analyzed with a minimum follow-up for 6 months from 2017 to 2021. Patient-reported outcomes (PROMS) - Neck Disability Index (NDI), Short Form 12-Item Physical Health Score (SF12-PHS), Short Form 12-Item Mental Health Score (SF12-MHS), Visual Analog Scale (VAS), PROMIS Physical Function (PROMIS PF), PROMIS Physical Health (PROMIS PH) and PROMIS Mental Health (PROMIS MH) were utilized. Descriptive statistics were utilized to compare early and late PROMs. Changes in PROMs from preoperative values to early (< 6 months) and late (≥ 6 months) time points and percentage of people achieving minimally clinically important difference (MCID) were compared between different groups. Results: A total of 159 patients (37 keeled and 122 keel-less implants) were included in the study. A more significant proportion of patients undergoing primary CDA had keel-less implants (94.3%, p = 0.042). The keeled implant group demonstrated lesser preoperative VAS arm and neck scores as compared to the keel-less implant group (p < 0.05). Both keeled and keel-less implant cohorts showed significant improvement in early and late NDI, VAS arm and neck, PROMIS-PF, and PROMIS PH scores. Patients with keel-less implants showed more significant improvement in VAS-neck as compared to the keeled implant group (p < 0.05). 56.5% of patients with keel-less implants achieved MCID as compared to 32% of patients with keeled implants for PROMIS-PH outcome at an early time point (p < 0.05). In both cohorts, no statistically significant difference was found in the MCID achievement rates for NDI, VAS- arm and neck, SF-12PHS, SF-12MHS, and PROMIS PF. Conclusion: Keeled and keel-less implants show comparable clinical outcomes at early and late time points in patients undergoing CDA. While the early results are comparable between both groups, long-term outcomes are awaited.
1612
P014: Cervical disc arthroplasty for the treatment of noncontiguous cervical degenerative disc disease: results of mid- to long-term follow-up
Tingkui Wu 1 , Hao Liu 1 , Beiyu Wang 1
1 Orthopedics, West China Hospital of Sichuan University, Chengdu, China
Objectives: The long-term results of cervical disc arthroplasty (CDA) for noncontiguous cervical degenerative disc disease (CDDD) are still uncertain. Moreover, it is unclear whether CDA delays or avoids the degeneration of the intermediate segment (IS), leading to controversy in the field. Therefore, this study aimed to investigate the mid- to long-term clinical and radiographic outcomes of CDA in treating noncontiguous CDDD and to explore whether the IS degenerated faster after CDA than other non-surgically treated adjacent segments. Methods: We retrospectively analyzed patients with noncontiguous CDDD who underwent CDA in our department between January 2008 and July 2018. The patients were divided into the CDA and hybrid surgery (HS) groups, and clinical and radiographic outcomes were evaluated at routine postoperative intervals. Clinical outcomes were assessed using the Japanese Orthopaedic Association (JOA), Neck Disability Index (NDI), and Visual Analogue Scale (VAS), while radiographic outcomes included cervical lordosis (CL), C2-C7 range of motion (ROM), segmental ROM, and disc angle (DA) at the arthroplasty level. Complications were also evaluated. Results: 64 patients with noncontiguous CDDD, with 31 in the CDA group and 33 in the HS group, were evaluated. The most frequently involved levels were C4/5 and C5/6. Both groups showed significant improvements in JOA, NDI, and VAS values after surgery. Although CL was maintained, the CL in the CDA group was consistently lower than that in the HS group (p < 0.05). There was a significant decrease in C2-C7 ROM (p < 0.05), but at the last follow-up, the C2-C7 ROM in the CDA group was greater than that in the HS group (p < 0.05). At the last follow-up, 44.3% of arthroplasty levels had developed HO, and 48.45% had developed ABL. In addition, ASDeg was observed in the IS (22.7%), superior adjacent segment (20.6%) and inferior adjacent segment (21.9%). Conclusions: CDA or CDA combined with fusion are viable treatments for noncontiguous CDDD, with satisfactory outcomes after mid-to-long-term follow-up. ASDeg is similar in non-surgical segments after 70 months of follow-up. ROM of the IS is similar to preoperative levels, indicating CDA does not increase the risk of IS degeneration.
Keywords: cervical disc arthroplasty; hybrid surgery; noncontiguous cervical degenerative disc disease; skip level; intermediate segment; adjacent segment degeneration
1663
P015: Investigating the utility of the osteolysis grading scale for assessing implant outcomes following cervical total disc replacement with the M6-C implant
Jessica Gaff 1 , Alana Celenza 1 , Andrew Berg 1 , Juan Amaya 1 , Sonja Häckel 2 , Michael Kern 1 , Paul Taylor 1 , Andrew Miles 1 , Gregory Cunningham 1
1 NeuroSpine Institute, Perth, Australia
2 University Hospital Bern, Switzerland
Introduction: Periprosthetic osteolysis is associated with inflammatory processes and increased wear, typically manifesting in the long-term post-operative period. Periprosthetic osteolysis is common in patients with cervical total disc replacement (CTDR) with the M6-CTM implant and therefore requires regular and routine monitoring to allow for early detection and intervention. Current osteolysis grading systems distinguish between mild, moderate, and severe inflammatory osteolysis but do not include explicit thresholds which are necessary for easy and replicable grading. Conventional CT is the optimal radiologic technique for detection of osteolysis however, to minimize radiation exposure, accurate detection by Xray alone would prove beneficial. Here we describe the ‘Osteolysis Grading Scale’ a simple and coherent method to categorise CTDR implants and assess the utility of the using Xray scans alone and CT and Xray scans. Material and Methods: The Osteolysis Grading Scale includes four grades of osteolysis based on the severity of osteolysis at the endplates: Grade 0, no osteolysis; Grade 1, < 50% of 1 endplate; Grade 2, <5 0%of both endplates; Grade 3, > 50% of 1 endplate; Grade 4, > 50% of both endplates. Conventional CT and Xray scans collected during routine follow-up of the M6-CTM implant following CTDR were reviewed and graded using the Osteolysis Grading Scale by a single spine surgeon. A random, deidentified subset of the CT scans and Xray images including a mix of no osteolysis and Grades 1-4 were graded by an additional 3 raters (a spine surgeon and 2 spine surgical fellows) who were blinded to the original grading. The accuracy of the grades were reviewed and the strength of inter-rater agreements were assessed using two-way random effects intraclass correlation coefficients (ICC). Results: Xray images for 28 M6-CTM discs from 20 patients were graded. Osteolysis grades 1-4 were poorly graded by Xray alone (< 20% accuracy). No osteolysis was accurately reported for 67% of discs without osteolysis and 19% of discs were incorrectly reported as having no osteolysis. The ICC was 0.49 (p < 0.0001) indicating poor interrater reliability when graded by X-ray only. CT and Xray images for an additional 29 discs from 20 patients were graded. Correct grades were recorded for 68% of the discs and no discs were incorrectly reported as having no osteolysis. The ICC for grading using CT and Xray was 0.80 indicating strong interrater reliability. Conclusion: The Osteolysis Grading Scale using CT and Xray can reliably grade osteolysis and implant outcomes and provides a beneficial and practical tool to spine surgeons. While it is important to limit exposure to CT in the cervical spine, Xray images alone are inadequate to accurately grade implant outcomes following CTDR with the M6-CTM implant. A follow-up protocol to detect adverse implant outcomes as early as possible while minimizing the frequency of cervical spine CT is required.
1683
P016: Investigating osteolysis following cervical total disc replacement with the M6-C: Analyses of retrieved implants and periprosthetic tissue
Jessica Gaff 1 , Alana Celenza 1 , Andrew Berg 1 , Juan Amaya 1 , Moreica Pabbruwe 2 , Paul Taylor 1 , Michael Kern 1 , Andrew Miles 1 , Gregory Cunningham 1
1 NeuroSpine Institute, Perth, Australia
2 East Metropolitan Health Service, Perth, Australia
Introduction: Periprosthetic osteolysis is one of the leading causes of cervical total disc replacement (CTDR) failure. Periprosthetic osteolysis results from chronic inflammation triggered by implant-derived particulate debris. A recent study reported 34% of patients with the M6-CTM implant required revision surgery due to wear-induced osteolysis evidenced by macroscopic disc failure, disrupted polyethylene and polycarbonate urethane implant polymers and histologic evidence of wear-induced osteolysis. However, the cause of implant failure and release of implant fibres into periprosthetic tissue was not reported. We recently reported that 44% of patients had periprosthetic osteolysis of their M6-CTM implant at a mean follow-up of 8 years and 10% of patients required revision surgery to remove their failed implant as a consequence of osteolysis. The aim of this study is to investigate the causes and mechanisms of failure contributing to the development of periprosthetic osteolysis. Material and Methods: Five patients underwent revision surgery to remove their M6-CTM implant due to severe periprosthetic osteolysis. An additional two M6-CTM implants from 2 of the patients that had not yet failed were removed during the revision procedure. The M6-CTM devices and periprosthetic tissues were removed during the revision procedure and fixed in formalin or no fixative and tested by external laboratories for histopathological analyses, extended microscopy, culture and sensitivity (MCS), metal ion analyses and physical examination of the M6-CTM devices. Results: Microbiology results were available for 4 patients and were MCS negative except for 1 sample for which Cutibacterium acnes was identified in the extended culture media for one specimen however is likely due to contamination. In all cases, periprosthetic tissue demonstrated a florid foreign-body type granulomatous reaction to refractile and birefringent fibres including giant cells and histiocytes with lightly pigmented cytoplasm indicating foreign-body inflammatory response. Trace amounts of titanium, aluminium and vanadium evident in all periprosthetic tissue samples however was likely due implant removal indicated by localised damage to the titanium endplates but no obvious signs of endplate contact. The endplates were covered with bone indicating good osseointegration with vertebral bodies. The polyurethane sheath was ruptured in all cases and the woven polyethylene annulus were frayed. Frayed fibres were evident in periprosthetic tissue and bone tissue indicating failure of the implant and migration of debris occurred a long time prior the revision surgery. Conclusion: Periprosthetic osteolysis is not due to poor vertebral body integration, infection, or metal ions sheared by endplate contact but is likely due to rupture of the polyurethane sheath and nucleus resulting in migration of fibres into the surrounding tissue a long time prior to the revision surgery causing a foreign-body inflammatory response and the development of osteolysis. The cause of implant failure leading to the rupture of the sheath remains unknown and biomechanical mechanisms warrant investigation.
1725
P017: Impact of pre-operative disc height loss on outcomes following cervical disc replacement
Avani Vaishnav 1,2 , Jung Kee Mok 1 , Kasra Araghi 1 , Eric Mai 1 , Olivia Tuma 1 , Chad Simon 1 , Cole Kwas 1 , Maximillian Korsun 1 , Yeo Eun Kim 1 , Myles Allen 1 , Eric Kim 1 , Nishtha Singh 1 , Joshua Zhang 1 , Tomoyuki Asada 1 , Russel Huang 1,3 , Todd Albert 1,3 , Sravisht Iyer 1,3 , Sheeraz Qureshi 1,3
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, Boston, USA
3 Weill Cornell Medical College, New York, USA
Introduction: Cervical disc replacement (CDR) is increasingly being utilized as a safe and effective motion-sparing alternative to ACDF. Recent studies have identified numerous predictors of outcomes in CDR, including patient-related factors and radiographic parameters. Preoperative disc height loss has been discussed as a potential risk factor for poorer outcomes, but there remains a paucity of literature on this topic. Thus, the purpose of this study was to assess whether preoperative disc height loss at the operative level is associated with outcomes following CDR. Material and Methods: We performed a retrospective review of prospectively collected data on patients who underwent primary CDR at a single academic institution between February 2016 and February 2023. Disc height was assessed pre-operatively on standard lateral spine radiographs and graded as follows:
• 0 = no disc height loss;
• 1 = < 50% disc height loss compared to adjacent levels
• 2 = ≥ 50% disc height loss compared to adjacent levels
In patients undergoing two-level surgery, the more severe grade was utilized for analysis. The three cohorts were compared for the following outcomes: operative time, blood loss (EBL), post-operative length of stay (LoS), in-hospital complications, reoperations and patient reported outcome measures (PROMs). PROMs, including Neck Disability Index (NDI), Visual Analogue Scale (VAS) for neck and arm pain, Short-Form 12 (SF-12 PCS/MCS) and PROMIS-Physical Function (PROMIS-PF), were collected pre- and postoperatively (within 90 days& ≥ 6 months postoperatively). Chi-square test was used for categorical variables. ANOVA and Kruskall-Wallis test were used for normally and non-normally distributed continuous variables. Wilcoxon signed-rank test was used to assess change in PROMs within each group. Results: 244 patients were identified of which 50 did not have both, pre- and post-operative PROMs, and 22 did not have a pre-operative x-ray in the system, resulting in 172 patients being included. 107 patients underwent single-level surgery and 65 underwent two-level surgery, resulting in 236 operative levels. Inter-rater agreement for disc height evaluation was 70.3%. 34.2% of surgical levels were graded as ‘0’, 49.6% as ‘1’ and 16.1% as ‘2’. One level was excluded due to inability to adequately visualize it on available x-ray. There were no significant difference in demographics, except age, with patients graded as ‘0’, being younger compared to grades ‘1’ and ‘2’ (mean 39.5yrs vs 43.9 and 45.1yrs respectively, p = 0.007). There were no significant difference in operative time (mean 83-97 mins; p = 0.353), EBL (median 25 ml, p = 0.229), Los (mean 22-23 hours; p = 0.704), or in-hospital complications (p = 0.791). Six re-operations were seen, all due to mechanical failure of the device. Reoperation rate did not differ amongst groups. There were no significant differences in pre- or post-operative PROMs, with all groups showing improvements from pre- to post-operatively. Conclusion: An inherent limitation is that only patients who were deemed appropriate candidates for CDR were included, thus the full spectrum of disc height loss was likely not seen in this cohort. With this in mind, the results of the current study show that pre-operative disc height loss was not associated with peri-operative outcomes, mid-term patient-reported outcomes or reoperations following CDR.
2021
P018: Translational and rotational response of a keeled total disc replacement after one-,two-, and three-level implantation
Antonio Valdevit 1 , Todd Lanman 2 , Jason Cuellar 2 , Michael Wernke 1 , Elizabeth Carruthers 1
1 SEA Ltd, Health Sciences, Columbus, USA
2 Cedars-Sinai Spine Center, Los Angeles, USA
Introduction: Motion associated with cervical disc replacement (CDR) has been studied, but few investigations report the physical separation between translational and rotational components associated with devices. Current literature is concentrated on angular motion of the spinal segment rather than the necessary translational motion within the intervertebral disc space required for total motion. This study examined effects of segment motion above, below, and at the surgical index level induced by a keeled CDR with distinction between translational and rotational motion. The investigators hypothesized that multi-level CDR offers similar or improved motion to intact specimens. Material and Methods: Seven cervical spines (C2-C7, age range: 38 to 66 years) were equipped with 3D motion sensors on the lateral aspect of C4, C5 and C6. Specimens were inserted into a fixture permitting flexion, extension, and lateral bending without disruption of specimen orientation. For each loading mode, specimens were subjected to application of a 3 mm deflection to the central (index) vertebra at a rate of 0.1 Hz for 20 cycles data collection at 60 frames/s. Testing conditions included the intact specimen with sequential implantation of a keeled CDR at the index (C5-C6), inferior (C6-C7), and superior (C4-C5) levels. The loading regimen was repeated between implantations. The resulting motion was calculated from the X, Y, and Z directional components of the three sensors relative to each other and expressed as fraction of intact specimens. Changes to the intact specimen within loading modes were computed using a 1 sample t-test (Intact = 1). Results: In flexion, compared to intact specimens, the vertebral levels displayed increased translation (p < 0.025) and rotation distal to the index surgery (p < 0.035). Continued implantations resulted in increased translations at (C5-C6) and increased rotations at (C5-C6) and (C6-C7), (p < 0.036). Superior implantation resulted in increased translation at the index level with increased but non-statistically significant rotations at all levels. Extension resulted in increased translations at index and distal segments (p < 0.022) for one- and two-level surgeries. A three-level surgery only increased translation distal to the index level. Rotation was not different from intact in extension. Lateral bending displayed increased translations for the index (p < 0.017, all segments) and two-level surgery (p < 0.025, (C5-C6), (C4-C5)). No statistical differences were detected for a three-level implantation in either translation or rotation as compared to the intact condition. Implantation of this keeled CDR device placed inferior, superior, and at index level increased, or retained the translation and rotation associated with the intact specimens. Conclusion: The study represents the physical separation of motion into the translational and rotational components as manifested by a keeled CDR. Up to three-levels of this keeled CDR device resulted in increased and/or retained specimen motion relative to intact specimens. The results demonstrated that multi-level prosthesis implantation does not lead to detrimental motion but can provide increased range of motion based on loading mode and insertion site.
2308
P019: Trends in patient selection for cervical disk arthroplasty (2015-2020): a retrospective analysis
Andrew Sauer 1 , Yichen Fan 1 , W.H. Andrew Ryu 2 , Jung Yoo 3 , Jonathan Kark 3
1 Oregon Health and Science University, Portland, USA
2 Neurological Surgery
3 Orthopaedics and Rehabilitation, Oregon Health and Science University, Portland, USA
Introduction: Cervical disk arthroplasty (CDA) is an evolving technology used to manage cervical pathologies and has shown both favorable short-term and medium-term outcomes. In comparison to anterior cervical discectomy and fusion (ACDF), CDA preserves the physiological flexion-extension motion, reduces the occurrence of adjacent segment disease, and expedites the healing process. Because CDA is a relatively new procedure, the surgical indications require refinement based on growing experience and data. In this retrospective analysis, we investigated how patient selection factors for CDA have evolved between 2015 and 2020. Material and Methods: We conducted a retrospective analysis using a comprehensive national insurance database, Pearldiver. This database contains data on 151 million individual patients followed longitudinally through most of private and government insurance products. We identified patients who underwent single- or two-level cervical disk arthroplasty (CDA) between 2015 and 2020, as indicated by the CPT codes 22856 and 22858. The data was categorized based on patient factors recorded prior to the index surgery, including obesity, tobacco use, fibromyalgia, osteoporosis, diabetes, preoperative opioid use, insurance status, and multi-level disease. To assess changes over time, we calculated the compound annual growth rate (CAGR) and overall surgical case changes for each patient factor group between 2015 and 2020. We performed a Chi-squared analysis to compare the frequency of patient factors between the two time periods and applied the Bonferroni correction to account for multiple comparisons and considered a significant statistical difference at p < 0.01. Results: 20,575 CDA cases were identified between 2015 and 2020, with a compound annual growth rate (CAGR) of 11.1% during this period. However, within the overall growth, there was a decrease in the proportion of cases among patient populations with tobacco use (CAGR -5.25%), fibromyalgia (CAGR -8.33%), osteoporosis (CAGR -6.95%), diabetes (CAGR -3.36%), and preoperative opioid use (CAGR -4.97%), resulting in an overall reduction of -23.60%, -35.60%, -30.20%, -15.70%, and -22.50%, respectively (all p < 0.001). Interestingly, the only patient factor that saw an increase in CDA utilization was obesity (CAGR 2.68%), with an overall growth of 14.10% during the study period (p < 0.001). Additionally, there was an increase in the proportion of patients undergoing two-level surgery (CAGR = 12.8%, p < 0.001) and Medicaid patients (CAGR = 11.1%, p < 0.001). Conclusion: Given the annual growth and purported advantages of CDA, we would expect to see a wider utilization of CDA across patient demographics, particularly as surgeons become more experienced with the procedure. Our data suggests the opposite trend-indicating a narrowing of indications for CDA despite the overall growth of this technology. The decrease in CDA utilization among patients with a history of tobacco use and osteoporosis is especially notable because these populations could potentially benefit the most from a minimally invasive procedure that does not rely on bone fusion. It is unclear if these patient populations were treated using more traditional methods due to perceived risk. Further research is needed to better understand these trends and guide the clinical decision-making in the management of cervical spine conditions.
2565
P020: Anterior cervical discectomy and fusion versus cervical disc arthroplasty for myelopathy: a propensity matched analysis of short-term outcomes in smokers
Stephen Barchick 1 , Sarthak Mohanty 2 , David Casper 1 , Amrit Khalsa 1
1 Department of Orthopaedic Surgery, University of Pennsylvania, Philadelphia, USA
2 Perelman School of Medicine at the University of Pennsylvania, Philadelphia, USA
Introduction: Smoking is associated with adverse post-operative complications in patient undergoing cervical fusion surgery, however data for single-level anterior cervical surgery is mixed. Single-level anterior cervical discectomy and fusion (ACDF) may not independently predict an adverse outcome in smokers, however large-scale studies continue to support smoking cessation to reduce overall patient risk. Data supports operative management of cervical myelopathy over non-operative management, with ACDF being the most common method of addressing pathology anteriorly.4 Cervical disc arthroplasty (CDA) has been utilized as a motion sparing method to address pathologies also treated with ACDF.5 Large database assessment comparing ACDF and CDA in patients with myelopathy who smoke may help to guide surgeon treatment selection. Methods: The American College of Surgeons National Surgical Quality Improvement (ACS-NSQIP) database was surveyed for all patients who were indicated for single-level ACDF or CDA for cervical myelopathy from the years 2011 to 2020. Only elective cases with selected pre-operative laboratory values and comorbidities were included. As patients were not randomized to treatment arms, propensity score matching was employed to minimize treatment selection bias when estimating causal treatment effects. A multivariable logistic regression was used to delineate factors significantly associated with a specific treatment group. Individual propensity scores per covariate were calculated in a logistic regression model. “Case” (ACDF) and “control” (CDA) patients were paired 4:1 on these propensity scores via exact matching based on factors that were found to be significantly associated with the decision to perform ACDF versus CDA. 819 patients were assessed in the CDA group and 3,276 in the ACDF group after matching. Standardized differences are estimated before and after matching to evaluate the balance of covariates; small absolute values (∼0.2) indicate balance between treatment groups. The PSM matched cohort was evaluated using 2-sided t-tests with Welch’s correction. Analyses of binary variables with Fisher mid-P value. Following PS matching, the incidence of a non-binary event was evaluated using the McNemar test. Results: After propensity score matching, patients who underwent CDA had greater length of surgical case compared to those who underwent ACDF (102 minutes v. 95 minutes p < 0.0009). No other factors were found to be statistically significant in the difference between the two surgical techniques among smokers to address cervical myelopathy. The overall rate of complications was low with additional patients having surgical site infections, pneumonia, reintubation, pulmonary embolism, urinary tract infection, DVT, and sepsis, none of which were found to have statistical significance between matched groups. Additionally, there was no statistical difference in reoperation or readmission between groups within 30 days. Conclusion: There is no difference in 30-day outcomes in patients who undergo ACDF or CDA to address cervical myelopathy when active smokers are matched. Surgeons can utilize this information to counsel patients who use tobacco that both surgical techniques are safe and effective. Further studies are needed to assess if longer term outcomes are different between motion preservation techniques and fusion in a cohort of patients known to have risk factors for pseudoarthrosis and other complications.
Arthroplasty-lumbar
718
P021: Outcome of unilateral osteoplastic recapping hemi-laminoplasty for lumbar interforaminal stenosis
Takashi Chikawa 1 , Daiki Nakajima 1 , Keisuke Nishidono 1
1 Orthopedic Surgery, Tokushima Prefecture Naruto Hospital, Naruto, Japan,
Introduction: Lumbar intervertebral foraminal stenosis are reported to account for 8-11% of all degenerative diseases of the lumbar spine. Although Posterior lumbar intervertebral fusion (PLIF) and full endoscopic lumbar foraminotomy (FELF) have been performed as surgical procedures, we performed the recapping hemi-laminoplasty (RHL) in our department. Objective: The purpose of this study is to discuss the surgical technique, short-term results, and usefulness of RHL in patients with single lumbar intervertebral foraminal stenosis due to lumbar spinal canal stenosis in elderly patients. Subjects: The mean age of the patients was 63.0 years and the mean number of patients who underwent RHL from October 2018 to December 2022. The mean age was 63.0 years (40 to 87 years), 20 were male and 10 were female. Methods: After opening the cephalocaudal intervertebral window, the spinous process was divided medially and longitudinally using a T-saw, the intervertebral joint process was osteotomized with a chisel, the intervertebral joint capsule was separated, the inferior joint process and the back surface of the vertebral arch were separated with a bump, and the unilateral vertebral arch was removed temporarily. Osteophytes, lateral hernias, and other lesions of the intervertebral foramen are removed, and the affected nerve roots are circumferentially decompressed. The extracted vertebral arch is then returned to its original position, and the osteotomized spinous process is fixed with an absorbable screw. The clinical outcomes (preoperative and postoperative JOA BPEQ VAS) and perioperative complications were investigated. Results: The results showed a slight improvement in JOABPEQ and a significant improvement in VAS in comparison with the preoperative and postoperative JOA BPEQ and VAS. Discussion: RHL was less invasive and more cost-effective than PLIF. On the other hand, FELF is a good indication for patients with intervertebral foramen stenosis with single root symptoms, but FELF is not indicated for patients with multiple intervertebral foramen stenosis, and the short-term results of RHL, which can simultaneously perform lumbar partial laminectomy and RHL, were excellent. Since the long-term results are unknown, it is necessary to consider the possibility that this procedure may be a time-saving alternative to PLIF, and to examine the rate of bony fusion and the occurrence of spinal instability over the long term.
1798
P022: Patients undergoing multilevel thoracolumbar fusions with prior total hip arthroplasty are at higher risk for prosthetic dislocations
Khoa Tran 1 , Olivia Opara 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Michael Megphara 1 , Tristan Fried 1 , Michael Carter 1 , Michael McCurdy 1 , Johnathan Ledesma 2 , Hamd Mahmood 2 , Luke Kowal 2 , Sandy Li 1 , Ashley Wong 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Orthopaedics, Rothman Orthopaedic Institute, Philadelphia, USA
2 Thomas Jefferson University, Philadelphia, USA
Introduction: As the number of patients undergoing total hip arthroplasty (THA) and lumbar spinal fusion rises, clinicians must better understand the biomechanical and clinical associations between these two procedures. Therefore, the aim of this study was to evaluate the effect of single versus multilevel spinal fusion on spinopelvic parameters, clinical outcomes, and THA dislocation rates in patients with an existing THA. Material and Methods: A retrospective cohort study was conducted on patients who received surgery at a single urban, tertiary academic medical center. Patients over 18 years of age with a history of THA who then underwent elective spinal fusion between 2004 and 2021 were included. Cohorts were stratified by spinal fusion construct length (single or multilevel) and the THA approach (anterior, anterolateral, lateral, or posterior). Patients were excluded from the study if they underwent revision THA before spinal fusion or received operative intervention for malignancy, infection, trauma, or revision spinal surgery. Standing AP and lateral lumbar spine radiographs were evaluated at 150% magnification to assess lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), pelvic incidence (PI), pelvic incidence – lumbar lordosis mismatch (PI-LL), and L1 axis S1 distance (LASD) preoperatively, 6-months postoperatively, and 1-year postoperatively. Femoroacetabular measurements, including acetabular anteversion (AA) and acetabular inclination (AI) were also evaluated at these time points. All statistical analyses were performed using R Studio Version 4.1.2 (Boston, MA), with P values <0.05 considered statistically significant. Results: A total of 440 patients (254 single-level, 76 two-level, and 110 long-level) were included. A significant difference was noted in patient's age, sex, race, and smoking (p < 0.05). Patients who underwent longer level fusion had significantly greater hospital length of stay (long 6.16 ± 4.16 vs. two 3.72 ± 1.94 vs. single 3.63 ± 3.88 days, p < 0.001) and lower rates of discharge home (long 45.7% vs. two 70.9% vs. single 81.1%, p < 0.001). Patients in the multilevel group had significantly higher dislocation rates (long 3.64% vs. single 0.39% vs. two 1.32%, p = 0.039), spinal revision (long 25.5% vs. two 17.1% vs single 13.4%, p = 0.019), complication rates (long 26.4% vs. two 17.1% vs single 7.87%, p < 0.001) and 90-day readmission rates (long 10.9% vs. two 5.26% vs. single 3.54%, p = 0.029). Radiographically, patients with multilevel constructs had significantly lower 1-year lumbar lordosis (long 45.7 ± 15.2 vs. two 43.1 ± 16.0 vs. single 51.4 ± 12.9, p = 0.022). Regression analysis shows that patients in the single level group have lesser dislocation risk (odds ratio:0.10, CI: 0.01 - 0.72, p = 0.045) compared to the multilevel group (odds ratio:0.35,CI: 0.02 – 2.45, p = 0.356). Conclusion: Patients with prior THA undergoing multilevel fusions experienced more dislocations, higher spinal revision rates, less frequent discharge home, longer hospital length of stay, and higher 90-day readmission rates. Patients with multilevel fusions had lower LL, higher PI-LL mismatch, and greater anteversion. This study suggests that patients with existing THA who undergo multilevel fusion have more abnormal spinal sagittal balance and have higher risk of dislocation despite higher baseline and postoperative acetabular anteversion.
Basic science
327
P023: Protein biomarkers can distinguish histologically degenerative symptomatic from asymptomatic lumbar discs
Theodore Choma 1 , Jacob Kramer 1 , Aaron Stoker 1 , Abigail Baumann 1 , Chantelle Bozynski 1 , Emily Leary 1 , Jinpu Li 1 , Donald Moore 1 , James Cook 1
1 Orthopaedic Surgery, University of Missouri, Columbia, USA
Introduction: Low back pain (LBP) is the most common cause of pain and disability, and its pathomechanisms may vary between individuals. While intervertebral disc degeneration (IVDD) is frequently noted in cases of chronic LBP, IVDD is also seen in patients who are not symptomatic for LBP. This study was designed to determine if differences in the ex vivo release of inflammation-, degradation-, and growth factor-related proteins by IVD tissues recovered from symptomatic (SYM) clinical patients and asymptomatic (ASYM) tissue donors could be identified for a given IVD histologic degenerative (HD) score. Material and Methods: IVD tissues were recovered from SYM patients undergoing surgery for IVDD (n = 184 patients, mean age 55.8y, 105F) and ASYM tissue donors (n = 20 patients, mean age 51.8y, 10F) without a reported history of back pain. Tissue explants for each were created and cultured for 3 days. On day 3, the media were collected for biomarker analysis and tissues weighed. Histological Assessment: A modified IVD scoring system based on the scheme published by Boos et al was used to evaluate each tissue by one blinded pathologist. Media Analysis: Media samples were tested for inflammatory, degradative and growth cytokines using Luminex assays. Media biomarker concentrations were standardized to the wet weight of each explant and natural log transformed. Multivariable linear models (LMs) were then created with adjustment for patient age, sex, obesity status, and their interactions. Two-sided significance was set at p ≤ 0.05. Interaction plots of predicted biomarker values were used to interpret LM results. Results: SYM annulus fibrosis (AF) tissues released significantly (p ≤ 0.048) higher levels of IL-1RA, MCP-1, MIP-1α, RANTES, and TNF-α compared to ASYM AF tissues. SYM nucleus pulposis (NP) tissues released significantly (p ≤ 0.042) higher levels of GRO-α, IL-8, MCP-1, MCP-3, MIP-1α and MIP-1β, RANTES, and TNF-α compared to ASYM NP tissues. SYM AF tissues released significantly (p ≤ 0.044) higher levels of MMP-1, MMP-2, MMP-9, and MMP-13 compared to ASYM AF tissues. ASYM AF tissues released significantly (p ≤ 0.049) higher levels of MMP-3, MMP-7, and MMP-8 compared to SYM AF tissues. Similarly, SYM NP tissues released significantly (p ≤ 0.036) higher levels of MMP-1, MMP-2, MMP-7, MMP-13, and significantly (p ≤ 0.046) lower levels of MMP-3, MMP-7, and MMP-8 compared to ASYM NP tissues. ASYM AF tissues released significantly (p ≤ 0.045) higher levels of TIMP-2, TIMP-3, TIMP-4, and significantly (p ≤ 0.039) lower levels of PDGF-AA and VEGF compared to SYM AF tissues. Similarly, ASYM NP tissues released significantly (p ≤ 0.045) higher levels of TIMP-1, TIMP-2, TIMP-3, TIMP-4, and significantly (p ≤ 0.039) lower levels of PDGF-AA, VEGF, FGF2 compared to SYM NP tissues. Conclusion: Histologically degenerative, cultured disc tissues from symptomatic patients are associated with significantly higher release of inflammatory proteins and specific MMPs, and significantly lower release of TIMPs, compared to similarly histologically degenerative disc tissues from asymptomatic individuals. Specific proteins including RANTES, MMP-2, MMP-8, and TIMPs 2-4 are consistently upregulated by symptomatic or asymptomatic IVD tissues across a spectrum of histological degeneration, indicating potentially fundamental biochemical properties in the development of pain.
394
P024: Load distribution on intervertebral cages with and without posterior instrumentation
Anna-Katharina Calek 1 , Frédéric Cornaz 1 , Mauro Suter 1 , Marie-Rosa Fasser 1 , Sina Baumgartner 1 , Philipp Sager 1 , Mazda Farshad 1 , Jonas Widmer 1
1 Orthopedic Department, Balgrist University Hospital, Zurich, Switzerland
Background Context: Posterior and transforaminal lumbar interbody fusion (PLIF, TLIF) are well-established procedures for spinal fusion. However, little is known about load sharing between cage, dorsal construct, and biological tissue within the instrumented lumbar spine. Purpose: The aim of this study was to quantify the forces acting on cages under axial compression force with and without posterior instrumentation. Study Design: Biomechanical cadaveric study. Methods: Ten lumbar spinal segments were tested under uniaxial compression using load cell instrumented intervertebral cages. The force was increased in 100N increments to 1000N or a force greater than 500N on one load cell. Each specimen was tested after unilateral PLIF (uPLIF), bilateral PLIF (bPLIF) and TLIF each with/without posterior instrumentation. Dorsal instrumentation was performed with 55N of compression per side. Results: Cage insertion resulted in a median cage preload of 16N, 29N and 35N for uPLIF, bPLIF and TLIF. The addition of compressed dorsal instrumentation increased the median preload to 224N, 328N and 317N, respectively. With posterior instrumentation, the percentage of the external load acting on the intervertebral cage was less than 25% at 100N (uPLIF: 14.2%; bPLIF: 16%; TLIF: 11%), less than 45% at 500N (uPLIF: 31.8%; bPLIF: 41.1%; TLIF: 37.9%) and less than 50% at 1000N (uPLIF: 40.3%; bPLIF: 49.7%; TLIF: 43.4%). Without posterior instrumentation, the percentage of external load on the cages was significantly higher with values above 50% at 100N (uPLIF: 55.6%; bPLIF: 75.5%; TLIF: 66.8%), 500N (uPLIF: 71.7%; bPLIF: 79.2%; TLIF: 65.4%), and 1000N external load (uPLIF: 73%; bPLIF: 80.5%; TLIF: 66.1%). For absolute loads, preloads and external loads must be added together. Conclusion: Without posterior instrumentation, the intervertebral cages absorb more than 50% of the axial load and the load distribution is largely independent of the loading amplitude. With posterior instrumentation, the external load acting on the cages is significantly lower and the load sharing becomes dependent on the load amplitude, with a higher proportion of the load being transferred by the cages in high load situations. The bPLIF cages tend to absorb more force than the other two cage configurations. Clinical significance: Cage instrumentation allows some of the compression force to be transmitted through the cage to the screws below, better distributing and reducing the overall force on the pedicle screws at the end of the construct and on the rods.
Keywords: intervertebral cage; TLIF; PLIF; fusion
458
P025: The impact on high glucose-induced inflammation and fibrosis on intervertebral disc degeneration: a novel insight into the role of mTOR/PKC and NF-kB signaling pathways
Chun Tseng 1,2,3 , Yichin Fong 1,3
1 Department of Orthopedic Surgery
2 Graduate Institute of Biomedical Sciences, China Medical University, Taichung, Taiwan
3 Department of Orthopaedic Surgery, China Medical University Beigang Hospital, Beigang, Taiwan
Introduction: Low back pain majorly contributes to age-related disability, accounting for the highest disability-adjusted life years of any disease. IVDD-induced secondary spinal instability and spinal stenosis are primary causes of low back pain. Fibrosis, an exaggerated inflammatory response to injury, is implicated in IVDD progression. Increased CTGF expression, a fibrosis marker, is frequently observed in degenerated intervertebral disc (IVD) tissues. Although hyperglycemia-induced inflammation and fibrosis contribute to many diseases' pathogenesis, their involvement in IVDD remains unclear. Material and Methods: The study followed ethical standards and the Helsinki Declaration of 1975, revised in 2000. Ten human IVDs were dissected from patients with lumbar spinal intervertebral disc herniation and intervertebral degeneration disease. The Ingenuity Pathway Analysis of the GEO database (GSE219145) was used to identify several IVDD-involved pathways, particularly the mTOR and PKC pathways. Masson staining was employed to observe IVD fibrosis, while fibrosis markers (CTGF, COLa1, ATF4, and EIF2) were quantified by qPCR and western blot assay. Results: The study discovered a positive correlation between IVD fibrosis progression and the IVDD gradient. As the annulus fibrosus (AF) is crucial for IVD mechanical function, it was used for experiments. High-glucose (33 mM) treatment in AF cells elevated the expression of fibrosis markers at both mRNA and protein levels. Masson's staining revealed a positive association between tissue fibrosis and Pfirrman scores. Immunohistochemistry also displayed a positive expression of fibrosis markers in high-grade IVDD tissues. Interestingly, high glucose treatment promoted mTOR and PKC phosphorylation time-dependently, which was inhibited by mTOR and PKC inhibitors (Repamycin and GF109203x) or siRNA. Additionally, NF-κB, a vital fibrosis response transcription factor and a common PKC signaling downstream target, was inhibited by NF-κB inhibitors or p65 siRNA, reducing high glucose-induced fibrosis markers upregulation. Conclusion: The findings suggest that high glucose upregulates fibrosis marker expression via the mTOR/PKCδ and NF-κB signaling pathways in AF cells. This offers novel insights into hyperglycemia-induced IVDD mechanisms and potential therapeutic targets for low back pain treatment.
531
P026: mRNA expression of LBX1 in paraspinal muscles is associated with severity of curves in idiopathic scoliosis
Uruj Zehra 1 , Ayesha Ahmad 1 , Abdullah Shah 2 , Bushra Rauf 1 , Muhammad Saad Ilyas 2 , Amer Aziz 2
1 Anatomy, University of Health Sciences, Lahore, Pakistan
2 Orthopedic & Spine Surgery, Ghurki Trust Teaching Hospital, Lahore, Pakistan
Introduction: Idiopathic scoliosis is the leading cause of spinal deformity worldwide. Recently role of ladybird homeobox 1 (LBX1) gene has been explored by a couple of studies in the development of idiopathic scoliosis, however, the biological basis of LBX1 contribution to idiopathic scoliosis remains mostly unknown. It is critical to explore the potential role of LBX1 in the severity of curves (Coronal & sagittal Cobb angle) and other spinopelvic parameters. Materials & Methods: Complete demographic and clinical profile with radiographs (lateral & AP) of 22 patients (16F/6M) aged 10-18 years undergoing surgeries for idiopathic scoliosis were obtained after informed consent. Paraspinal biopsies were obtained from both convex & concave sides of the curves for mRNA analysis of LBX1. Radiological parameters such as coronal & sagittal Cobb angle, vertebral rotation, apical vertebral translation (AVT), Rissers sign & coronal balance were measured on radiographs using RADIANT DICOM viewer. Pain was graded by visual analogue scale (VAS) from 0 to 10. The data was analyzed using independent sample t test and regression analysis. Results: There wasn’t any significant difference of LBX1 expression on both sides of the curves. The expression did not have any correlation with age and sex. Mean ± SD of coronal & sagittal Cobb angle was 81.6 ± 17.7 & 40 ± 20.8 respectively. The convex side expression was in significant positive correlation with coronal Cobb angle (r = 0.44, p = 0.03) & AVT (r = 0.57, p = 0.006). Conclusions: The correlations of LBX1 with coronal Cobb suggest that LBX1 expression has a potential role in determining the severity of the curve. Hence, the molecular mechanism by which LBX 1 contributes to this severity needs to be further explored.
766
P027: Novel etiology of adolescent idiopathic scoliosis: SLC6A9 variant impairs glycine neurotransmission
Jason Cheung 1 , Xiaolu Wang 1 , Ming Yue 2 , Prudence Wing Hang Cheung 1 , Jianguo Zhang 3 , Nan Wu 3 , Carol Wise 4 , Keith Dip Kei Luk 1 , You-Qiang Song 2 , Bo Gao 2
1 Orthopaedics and Traumatology
2 School of Biomedical Sciences, The University of Hong Kong, Hong Kong, Hong Kong
3 Peking Union Medical College Hospital, Beijing, China
4 Texas Scottish Rite Hospital for Children, Dallas, USA
Introduction: AIS is the most common form of spinal deformity affecting millions of adolescents worldwide, but it lacks a defined theory of etiopathogenesis. The origin of some Adolescent Idiopathic Scoliosis (AIS) is neuropathic. Variants of SLC6A9, which encodes glycine transporter 1 (GLYT1), reduce glycine transportation, impaired glycine neurotransmission, and central pattern generators (CPGs) dysfunction leading to spinal deformity. Material and Methods: Clinical investigation, genetic analysis, and functional studies were conducted. Five multi-generation AIS families and 843 sporadic cases were identified, and along with 3219 controls, underwent genetic analyses including linkage analysis, genome sequencing, and targeted sequencing to identify pathogenic variants. Paraspinal muscle sEMG tests were performed on familial cases. Additionally, 858 patients from two additional AIS cohorts in China and US were used for validation. After identifying disease-associated variants, cellular mechanisms were studied and zebrafish models were generated to understand the underlying etiology of the spinal curvature and to test candidate treatments. Results: Disease-causing and predisposing variants of SLC6A9 in multiple families and many sporadic cases were identified via genetic analyses. SLC6A9 variants affected subcellular localization and stability of GLYT1, leading to reduced glycine uptake activity in cells. Slc6a9 mutant zebrafish exhibited discoordination of spinal neural activities and pronounced spinal curvatures which resembles the human patients carrying the SLC6A9 pathogenic variant. Administration of a glycine receptor antagonist or a clinically used glycine neutralizer sodium benzoate partially rescued the phenotype (scoliosis phenotype dropped from 70.2% to 30.3%). Aberrant EMG bursts were found in SLC6A9 pathogenic variants suggesting an impairment of paraspinal muscle balance control. Conclusion: Genetic variants affecting glycine transportation are strong causal risk factors of AIS. Results from patients and animal models suggest a neuropathic origin for “idiopathic” scoliosis, involving the dysfunction of CPGs, potentially a common cause of AIS. Our work suggests further avenues for early diagnosis and prevention of AIS.
829
P028: Expression of TGF Beta 1 & degenerative changes in the paraspinal muscles of scoliotic patients
Uruj Zehra 1 , Kinza Fatima 1 , Abdullah Shah 2 , Bushra Irum 1 , Muhammad Saad Ilyas 2 , Amer Aziz 2
1 Anatomy, University of Health Sciences Lahore, Lahore, Pakistan
2 Orthopedic & Spine Surgery, Ghurki Trust Teaching Hospital, Lahore, Pakistan
Introduction: Various studies advocate the genetic pathogenesis of idiopathic scoliosis, recently the role of paraspinal muscles in the initiation and progression of idiopathic scoliosis has been identified. However, the complex mechanism of the muscle tissue changes remains unclear. A couple of studies have found the asymmetric expression of various transcripts between the two sides of the muscles, it is plausible to hypothesize that the expression of certain proteins is responsible for muscular changes. The current study has been designed to elucidate the role of transforming growth factor β1(TGF-β1) in histological changes of paraspinal muscles of scoliotic patients. Material & Methods: Paraspinal muscle tissue samples were obtained from both sides of idiopathic scoliotic patients (n=22) and from degenerative disc disease patients (n = 21) as controls who were undergoing surgery after informed consent along with relevant demographic & clinical details. The obtained muscular tissue samples were processed for protein analysis of TGF-β1 and for histological changes like necrosis, atrophy, hypertrophy and fatty involution on H& E-stained sections. The data was analyzed using one way ANOVA & linear regression analysis. Result: Scoliotic patients (16F/6F) had mean coronal Cobb angle of 81.63 ± 17.7, with mean-age of about 14.1 ± 2.1 years. mRNA expression of TGFβ1 was more on concave side of the paraspinal muscles as compared to controls (p = 0.04). While both convex & concave sides of paraspinal muscles of scoliotic patients were having significantly increased necrosis, atrophy, hypertrophy and fatty involution (p < 0.001) as compared to controls. While comparing convex & concave side paraspinal muscles, fatty involution was more on concave side (p = 0.004) as compared to convex side. Female scoliotic patients had more atrophy (p = 0.01) as compared to males. Conclusion: TGF-β pathway is a known critical regulator of the degenerative muscle changes, current results suggest that TGF-β1 signaling may play an important role in the development of these muscle pathologies.
921
P029: Fundamental biophysics of wolff's law and molecular properties of bone that opposes the fracture force in the frame of orthopedics and neurosurgery
Nery Lamothe 1 , Mara Lamothe 1 , Alejandro Alonso-Altamirano 1 , Daniel Lamothe 2 , Jesus Hernandez-Coria 3 , Francisco Castillo-Vazquez 4 , Hugo Contreras-Blancas 3 , Pedro Mojica-Guerrero 3,5 , Eber Martinez-Joffre 3 , Armando Martinez-Aguilar 3 , Anna De la Pena 2 , Jose Talavera-Martinez 3 , Jose Hernandez-Ortiz 3 , Victor Renteria-Ferruzca 3 , Sharla Rivera-Baena 3 , Alejandro Bayo del Castillo 3 , Victor Perez-Aguilar 3 , Hair Galan-Rosalio 3
1 Division de Ciencias Biologicas y de la Salud, Universidad Autonoma Metropolitana, Mexico City, Mexico
2 Internal Medicine, Jersey City Medical Center, New Jersey, USA
3 Orthopedics, Hospital General de Xoco, Mexico City, Mexico
4 Orthopedics, Foot and Ankle, Prince of Wales Hospital, Sydney, Australia
5 Orthopedics, Hospital Angeles Mocel, Mexico City, Mexico
Introduction: Wolff’s law states that bones will adapt to the degree of mechanical loading, which is a matter of mechanical transduction of bone cells. Mechanotransduction is the conversion of mechanical stimuli in bone formation. Decreasing mechanical stimuli during immobilization, muscular debility, and the loss of gravity astronauts encounter, generates bone loss due to decreasing mechanical transduction. On the other hand, increasing mechanical stimuli promotes bone formation, as happens while walking after a fracture with bone loss occurs. This work constitutes the fundamental basis of what lies in Wolff’s law and the biophysical properties of bone that oppose the fracture force. We investigate the properties of the bone that oppose the forces that will break the bone, as the physics of Young and Bulk modulus. Material and Methods: The only method used was the logarithm base 2 of the number of choices, corresponding to information in the mathematical theory of communication of Shannon, to arrive at apodictic inferences, in terms of the electromagnetic interactions and what constitutes the molecular basis of the biomechanics; ascending to the different organizational levels: The cellular, subcellular and molecular fundamentals of the biomechanics, biochemistry, biophysics of the collagen, the fibers of Sharpey and the histology of the interstitial architecture, and also the mechanical transduction of the osteocyte. Results: The structure of hydroxyapatite is determined by the hysteresis that arises as an emergent property of Bertalanffy, starting from the dispositions of the space-time of the atoms. In compression strain, generated by the compression stress, it is the Bulk modulus of the Hydroxyapatite that opposes the compression strain. In tension strain, generated by the tension stress, it is the Yung modulus of collagen type-1 that opposes the tension strain of the bone. In torque strain, generated by tension stresses applied opposite in the transversal plane and tangential to the bone, the torque is the Young modulus, but of the collagen bundle. When this reaches the threshold of Sharpey fibers, the torsion strain of bone results; even though this corresponds to a helicoidal simple pattern of a fracture, it is the fracture pattern with greater stability, because of the contact area between the fragment's cortices, as a matter of electromagnetic interaction, among electrons and protons of their atoms. Mechanical forces applied to bone make liquid inside the canaliculi and lacunae get outside the interstitium in the compressed bone segment. The movement of liquid in the canalicular system, made up of a network of osteocytes dendritic cytoplasmatic processes inside canaliculi and connected through GAP junctions, generates a streaming potential at the moment the bone is under stress. This electrical potential opens voltage-gated Ca2+ channels, increasing Ca2+ intracellular levels, which together with Nitric Oxide and PGE2 alter c-fos and COX2 gene expression. The IGF-1 gene expression increases the production of IGF-1, which promotes the transformation of osteoprogenitor cells into osteoblasts, as such, the regions of bone under stress will have a greater amount of bone deposits. Conclusion: All the concepts of biomechanics are apodictically inferible in terms of electromagnetic interactions.
1470
P030: Role of endocannabinoids in pathogenesis of sub-clinical infection of intervertebral disc
Shanmuganathan Rajasekaran 1 , Gowdaman Vasudevan 2 , Chitraa Tangavel 3 , Karthik Ramachandran 1 , Sri Vijay Anand KS 1
1 Department of Spine Surgery, Ganga Hospital,Coimbatore, India 2 Department of Genomics, 3 Department of Proteomics, Ganga Research Centre,Coimbatore, India
Introduction: The microbiome in both control and degenerated IVD disc samples showed similar bacterial diversity at the genus level, however, control discs were devoid of infection-related immune responses. Our objective is to understand the role of the Endocannabinoid mediated signaling mechanism during the sub-clinical infection of IVD. Methods: This is an experimental case-control study. Bacterial diversity in IVD tissue of normal healthy disc from brain dead organ donors, Control (C) (n = 20) and degenerated disc (n = 40; (modic (M) = 20; non-modic (NM) = 20)), from patients undergoing discectomy were studied using 16S metagenome V3-V4 sequencing. Data analysis was performed using the Qiime2 pipeline followed by OTU clustering and taxonomic classification using Greengenes / SILVA reference databases. In addition, global metabolome profiling was performed in the same samples (n = 60) using uHPLC coupled to Q Exactive TM Plus Hybrid Quadrupole-Orbitrap TM mass spectrometer. Metabolic features were identified using compound discoverer vs 3.3 and further subjected to principal component analysis (PCA) and OPLS-DA using MetaboAnalyst 5.0. Results: A total of 14 bacterial genera were identified common in control, modic, and non-modic discs, with a high abundance of gram-negative bacteria. The bacterial genera identified were: Pseudomonas, Prevotella, Mycobacterium, Bacteroides, Faecalibacterium, Roseburia, Leifsonia, Acinetobacter, Cutibacterium, Corynebacterium, Clostridium, Achromobacter, Ruminococcus, Staphylococcus. The classified OTUs representing bacterial genera were higher in control (45397) followed by Non-modic (43552) and Modic (37319) respectively. Untargeted metabolomic analysis in the same samples revealed a total of 3187 metabolites, of which 1294 were fatty acids, lipids, and its derivatives which contribute to 40% of the total metabolites identified. Among the lipids identified, signaling lipids such as Endocannabinoids, play a major role in host immune response. The Endocannabinoid metabolites were significantly reduced in degenerated discs than in control discs with Log fold change of -0.78 for 2-Arachidonylglycerol (2-AG) and -0.89 for N-arachidonoylethanolamine (AEA). The role of 2-AG and AEA in the host were reported to be anti-inflammatory and attenuates bacterial infection, especially gram-negative bacteria. The two metabolites 2-AG and AEA bind to the Cannabinoid 1 (CB1) and Cannabinoid 2 (CB2) receptors and prevent the production of pro-inflammatory molecules such as IL-6 and IL-10. The metabolite 2-AG attenuates the type -3 secretion system (T3SS) of the pathogen which interacts with the host molecules. The CB2 receptor activation by agonists like 2-AG significantly reduces the infection and inflammation induced by Pseudomonas, thereby preventing or delaying disc degeneration. Conclusion: The bacterial diversity of the discs revealed the abundant gram-negative bacteria which includes opportunistic pathogens. Though all the discs had pathogenic bacteria, the control disc was devoid of any infection. The metabolome analysis revealed 2-AG and AEA, signaling lipid molecules play a major role in providing resistance towards bacterial infection in control intervertebral discs compared to low levels in degenerated discs.
1558
P031: The role of artificial intelligence language model in generating spine abstracts
Hong Jin Kim 1 , Jae Hyuk Yang 2 , Dong-Gune Chang 1 , LAWRENCE LENKE 3 , Javier Pizones 4 , René Castelein 5 , Per Trobisch 6 , Gregory Mundis 7 , Seung Woo Suh 8 , Se-Il Suk 1
1 Orthopedic Surgery, Inje University Sanggye Paik Hospital, Seoul, South Korea
2 Orthopedic Surgery, Korea University Anam Hospital, Seoul, South Korea
3 Orthopedic Surgery, The Daniel and Jane Och Spine Hospital, NY, USA
4 Orthopedic Surgery, Hospital Universitario La Paz, Madrid, Spain
5 Orthopedic Surgery, University Medical Centre Utrecht, Utrecht, The Netherlands
6 Spine Surgery, Eifelklinik St. Brigida, Simmerath, Germany
7 Orthopedics, Scripps Clinic, CA, USA
8 Orthopedic Surgery, Korea University Guro Hospital, Seoul, South Korea
Introduction: Due to recent advances in artificial intelligence (AI), language model applications can generate logical text output that is difficult to distinguish from human writing. The use of AI to write scientific abstracts in the field of spine surgery is the center of much debate and controversy. This study is to evaluate the reproducibility of scientific abstract generated by AI’s large language model in the field of spine surgery. Material and Methods: Sixty abstracts were randomly selected and used as ChatGPT and Bard input statements to generate abstracts based on supplied article titles. A total of 174 abstracts divided into human-written abstracts, ChatGPT-generated abstracts, and Bard-generated abstracts was evaluated. The likelihood of plagiarism and AI output were assessed using the iThenticate and zeroGPT programs, respectively. Eight reviewers in the spinal field evaluated 30 randomly extracted abstracts to determine whether they were produced by AI or human authors. Results: The plagiarism rate was significantly lower among ChatGPT-generated abstracts (20.7%) compared with Bard-generated abstracts (32.1%) (p < 0.001). The AI-detection program predicted that 21.7% of the human group, 63.3% of the ChatGPT group, and 87.0% of Bard group were possibly generated by AI, with an area under the curve value of 0.863 (p < 0.001). A sensitivity of 56.3% and a specificity of 48.4% were shown in assessing human-written abstracts by human reviewers. Conclusion: Writing abstracts in the field of spinal research, most abstracts generated by AI program showed high levels of plagiarism and AI detection that can be deemed unethical. As humans are unable to clearly distinguish between abstracts generated by AI and those written by humans, caution is advised regarding the ethical implications of using AI programs such as ChatGPT and Bard.
1569
P032: The diversity of transcriptome in lumbar degenerative disease and novel isoform of bone morphogenic protein-6 revealed by long-read RNA sequencing
Hong Jin Kim 1 , Jun Kim 2 , Dong-Gune Chang 1 , Chun-A Kim 3
1 Orthopedic Surgery, Inje University Sanggye Paik Hospital, Seoul, South Korea
2 Life Sciences, Chungnam National University, Daejeon, South Korea
3 Korea Research Institute of Bioscience and Biotechnology, Aging Convergence Research Center, Daejeon, South Korea
Introduction: The etiology and pathological mechanisms of degeneration in spine was not clearly established. The bone morphogenic proteins (BMPs) has an osteo-inductive potential and important role of bone graft substitute in spine fusion surgery. This study is aimed to assess the diversity of transcriptome in degenerative lumbar spinal stenosis and find the novel isoforms of BMPs from lamina, ligament flavum, pelvic bone using the long-read RNA sequencing. Material and Methods: Long-read RNA sequencing were performed based on samples including degenerative lamina, hypertrophied ligament flavum, and pelvic bone from the patients with degenerative lumbar spinal stenosis. The genes and isoforms specifically expressed in degenerative spine and normal pelvic bone were discovered and analyzed from the comparison of the extracted data with short-read RNA sequencing. Results: Our data discovered the 45,174 novel genes and 20,767 isoforms indicating the diversity of splicing pattern in degenerative spine. Reflecting these genes and isoforms, 2,492 differentially used isoforms (DIUs) and 887 differentially expressed genes (DEGs) were obtained and there was a total of 124 genes that possessed both DIUs and DEGs, which were found to be the factors in bone or ligament formation. Specifically, the total of 4 isoforms in BMP-6 were observed in normal pelvic bone and these isoforms indicates that they have a potent on bone formation process. Conclusion: The diversity of transcriptome including splicing patterns were revealed from the long-read RNA sequencing, which were found to be influential factors in pathological mechanism of degeneration. Especially, the four novel isoforms of BMP-6 in pelvic bone suggested that their important role in osteo-inductive potential.
1767
P033: Genetic study of patients with ossified posterior longitudinal ligament in Indian population
Anindya Basu 1 , Tosaddeque Hussain 1 , Christopher Gerber 1
1 Spine Surgery, Institute of Neurosciences Kolkata, Kolkata, India
Introduction: Ossification of Posterior Longitudinal Ligament (OPLL) is a pathological condition most commonly encountered in the cervical spine. It is most prevalent in South East Asian population and relatively rare in the West, with incidence being 2.4 % in the Asian population and 0.16% in the non-Asian population. While the pathogenesis of OPLL is multifactorial and not well understood, it is widely believed to have genetic associations as suggested by various studies in the past. While, various studies have been conducted in the past mostly in the Japanese to study pathological variants through genome sequencing, none have been performed in the Indian subcontinent despite it being fairly common in clinical practice. Material and Methods: It was a Cross sectional observational study with a Sample size 40. We received Ethical clearance by IRB and the cost was covered by research grant. Patients with Age >18 years and CT confirmed cases of Cervical OPLL were included in the study. Patients with dorsal and lumbar OPLL and history of trauma were excluded. Blood sample (3 ml) was collected in EDTA vial and we conducted next generation sequencing on 40 radiologically confirmed OPLL patients to identify deleterious genetic mutations. We noted gross motor power and mJOA scores and and Nurick grading at presentation. Relationship to K line, type of OPLL and Maximum Occupying ratio on sagittal CT was considered. Need for surgery was also noted. Results: Mutations were identified in RNF170 chr8, GIPC1 chr9, BMP4 chr14, MTHFR chr1, COL6A1 chr21, MICU1 chr10, ATL1 chr14, DHTKD1 chr10, KBTBD13 chr 15, DDHD1 chr14, LRRK2 chr12, GARS1 chr7, SCN11A chr3, HTRA1 chr10, MYH2 chr17, SLC5A7 chr2, GDAP1 chr8, RNASEH2B chr13, LRSAM1 chr9, CAMTA1 chr1, ALDH18A1 chr10, FAT2 chr5, SPG7 chr16 and COL2A1 chr12. Pathological variants were found in 7 of 12 patients having continuous, 3 of 6 in mixed, 6 of 16 segmental and only 1 of 6 circumscibed types of OPLL. Conclusion: Apart from providing insight into genetic pathobiology of OPLL and related skeletal disorders in Indian population, identification of these mutations might help in the development of molecular targeted therapy and a standardized genetic screening panel for family members of affected individuals in the future.
2019
P034: Contact loading response of 3D printed implants with additive surface features
Antonio Valdevit 1 1 , Nicole Mottole 1 , Robert Hirschl 2
1 SEA Ltd, Health Sciences, Columbus, USA
2 Orlando Health Neuroscience and Rehabilitation Institute, Orlando, USA
Introduction: 3D-printing creates structures to optimize fusion by including features such as surface roughness, teeth and/or outer framework to resist migration to increase structural integrity. While common, little is known how these features may alter the propensity for subsidence. It is recognized that clinical subsidence is a dynamic cyclic event and not due to a single overloading condition. The current study addresses static implant/substrate contact to elucidate effects of traditional surface features upon surface engagement. The investigators hypothesize that an open structure allows for increased surface engagement and load transfer via increased interdigitation with the underlying surface. Material and Methods: Randomized and equal allocation of 20 PCF bone blocks (N = 20) were assigned to one of four (same manufacturer, Xenix Medical, Orlando, FL) 3D-printed intervertebral implant groups possessing equal dimensions and matrix configuration but differing in surface geometry designated as; Base Matrix (BM), BM+Frame (BMF), BM+Teeth (BMT) and BM+Frame+Teeth (BMFT). Ultralow Fuji film was placed on the surface of the bone blocks. Static compression testing was performed using each implant type to a load of -350 N at a rate of 10 N/s and sustained for 15 seconds. The exposed film was analyzed using Topaq software that converted the film image to a quantitative contact pressure image. Mean pressure and surface engagement (Area) were normalized to the BM implant (BM = 1) and compared using a 1-way ANOVA with a Holm-Sidak post-hoc tests. Results: The BM and BM+Frame designs displayed decreased mean pressures (p < 0.0001) and were not different from each other. More specifically, designs incorporating Teeth upon the surface resulted in increased pressures. With respect to surface engagement, the BM design displayed statistically increased engagement compared to all other designs incorporating a Frame and/or Teeth (p < 0.03 for all). Designs incorporating a Frame and/or Teeth were not statistically different from each other. The BM and BM+Frame designs displayed a statistically decreased pressure as compared to all other designs. The interdigitation of the matrix without the presence of the Teeth feature likely permits increased surface engagement as the BM and surrounding frame allow for increased contact with the substrate and therefore results in decreased pressure as compared to point contact in the case of Teeth residing on the substrate. It should be noted that in addition to decreased pressure, the BM design also demonstrated statistically increased surface engagement compared to other designs. The combination of increased engagement and decreased pressure in the BM design is a favorable mechanical environment for subsequent fusion via load transfer without increasing subsidence propensity. Conclusion: Using implants of identical matrix with/without a circumferential Frame provided reduced pressures in comparison to inclusion of Teeth. With respect to surface engagement, it was determined that inclusion of a circumferential Frame with/without Teeth reduced the load transfer ability as evidenced by a significant reduction in engagement with the underlying substrate. The BM design without features likely allows for increased interdigitation with underlying surfaces, especially if one considers the non-uniform endplate surface under clinical applications.
2020
P035: Effects of interbody implant framework and anti-migration geometry on vertebral endplate subsidence resistance due to cyclic loading
Antonio Valdevit 1 1 , Nicole Mottole 1 , Robert Hirschl 2
1 SEA Ltd, Health Sciences, Columbus, USA
2 Orlando Health Neuroscience and Rehabilitation Institute, Health Sciences, Orlando, USA
Introduction: 3D-printing permits biomimetic structures to optimize fusion. Little is known how teeth and/or outer framework alter subsidence. Clinical subsidence is a multi-factorial cyclic process, not a catastrophic event. Standardized tests evaluate implant subsidence using blocks and static loading but are not clinically realistic. The investigators introduce the concept of subsidence resistance as a more clinically relevant scenario of cyclic penetration of a device into vertebra and that an open structure allowing for interdigitation with the endplate results in improved subsidence resistance. Material and Methods: Randomized and equal allocation of L4 (N = 3) and L5 (N = 3) porcine vertebra were assigned to four 3D-printed implant groups from the same manufacturer (Xenix Medical, Orlando, FL) possessing equal dimensions but differing in surface geometry: Base Matrix (BM) , BM+Frame (BMF), BM+Teeth (BMT) and BM+Frame+Teeth (BMFT). Implants were placed on superior endplates and subjected to 500 cycles of loading (-35N to -350N), with load and deformation data acquired at cycle 5 and at 25 cycles thereafter. Subsidence resistance was computed from the elastic region of the load/deformation curve and normalized to the initial resistance (cycle 5). For each implant, exponential analysis of subsidence resistance versus cycle number resulted in parameters of Span (Total Subsidence Resistance) and Rate (K). Span can be considered as the asymptotic limit of the subsidence resistance increase. The Rate parameter (K) is the resistance per cycle but is more clinically meaningful to report Half-Life or number of cycles to achieve a 50% change from initial values (Half-Life (HL) = (Ln (2))/K). Span and Half-Life were compared using a 1-way ANOVA with a Holm-Sidak post-hoc tests. Results: BM designs demonstrated dual exponential (i.e., dual Rate (K) values and hence dual Half-Lives) fits as compared to single K curves for other designs (F Test, p < 0.0001). The Slow Half-Life component of BM designs was greater than single components of other designs (P<0.0001 for all). Simultaneously, the Fast Half-Life component in BM designs was less than single components of other designs (P<0.045 for all). The combination of a rapid increase (Fast) and a gradual subsidence resistance increase (Slow) in BM designs was different from other designs. With respect to the Span, BM designs demonstrated a greater change or increased subsidence resistance as compared to the other designs (P<0.0001 for all). The addition of Teeth to BM designs increased subsidence resistance only as compared to Frame designs (P<0.0001 for both). The open matrix of BM designs permits increased opportunities for inter-digitation with the endplate surface for immediate engagement and subsequently only results in small micro-adjustment under load. Inclusion of a Frame forces a device to reside on surface features protruding from the endplate. The use of Teeth results in device penetration until sufficient engagement supports the load. Conclusion: Rapid initial subsidence resistance combined with gradual resistance in the open matrix BM design may be a clinically viable scenario as implant subsidence is likely to occur early during post-operative recovery.
2022
P036: Regional mapping of the vertebral endplate response under dynamic loading
Antonio Valdevit 1 , Nicole Mottole 1 , Joseph Turner 2 , Charles Forton 2
1 SEA Ltd, Health Sciences, Columbus, USA
2 Acuity Surgical, Irving, USA
Introduction: It has been reported that removal of the endplate decreases surface strength and thereby increases the likelihood of subsidence and is most notable in the posterior region. Such a practice could be viable provided the intervertebral device displays a footprint that takes advantage of the mechanically stronger endplate region in the vertebral periphery. Devices that reside upon the periphery and demonstrate a large contact area with the endplate should result in a reduced stress distribution pattern. Studies that have investigated endplate mechanics have involved static compression to failure for evaluation. The use of cyclic stress relaxation loading may be more fitting and clinically applicable. This suggests that a low frequency indentation fatigue evaluation may be appropriate and can be used to elucidate subsidence properties of the vertebral endplate. Material and Methods: The mechanical evaluation of the endplate consists of concentric regional boundaries of Inner, Middle, Outer and Periphery subdivided into angular positions identified as 0°, 30°, 45°, 60° and 90°. Each location was subjected to 500 cycles of continuous compression from -2.5 N to -25 N using a fixture permitting perpendicular orientation of the test location with the loading axis. The most posterior central location was identified as the origin and used to normalize the response for each vertebral body to pool the results. For each test site, a non-linear exponential regression was performed that provided clinically relevant parameters of Yo (Initial Deformation), Plateau (Asymptotic Deformation Limit), Span (Total Subsidence), and K (the deformation per unit cycle). Each of parameter was averaged over the concentric region for each vertebral body for all five spines. The fitted parameters were subjected to a 1-Way ANOVA with a Tukey post-hoc test for determination of statistical differences between concentric regions. Results: In the case of Yo, Plateau, Span (or subsidence) and K, statistically significant differences were observed between the Periphery and the Middle and Inner regions (p < 0.046 for all regions and parameters). The summary result is best exemplified by the Span data where the total change from the initial Yo deflection to the Plateau (Asymptotic Limit), considered as a measure of the subsidence in a region, illustrates a gradual increase in subsidence from the Periphery to the Middle (p = 0.0453) and Inner (p = 0.0116) regions and depicts a increase from the Outer region to the Inner region (p = 0.0287) as well. Proper placement of intervertebral spacers is generally an acquired feel gained through experience. Intuitively one may place the spacer in the posterior region to minimize expulsion risk. This study suggests the posterior inner radius region is most vulnerable to compressive fatigue failure which may be mitigated by ensuring contact with the posterior endplate rim. Conclusion: The cyclic loading employed in this study may be a more clinically relevant method for the evaluation of regional endplate integrity. Based upon fatigue loading from this study, the mechanical integrity of the endplate may be more limited than observed under static conditions.
2408
P037: Association between low back pain, overweight and muscle trophism
Luiz Claudio Rodrigues 1 , Fernanda Andrea Navarro 2 , Rodrigo Nakao 2 , Nathalia Adelina Pereira 1 , Victoria Americhi Stering do Nascimento 1 , Rodrigo Pinho de Araújo 2
1 Ortopedia Surgery, Santa Marcelina University of Medicine, São Paulo
2 Spine Surgery, Hospital Santa Marcelina, São Paulo
Introduction: Low back pain is a multifactorial condition, extremely prevalent in industrialized countries. Its occurrence may be related to psychosocial, organizational, physical, and sociological factors. Obesity and overweight are directly related to changes in the locomotor system, especially in body alignment. In this sense, this is a cross-sectional quantitative study, which aimed to relate low back pain with the degree of overweight and paravertebral hypotrophy. Material and Methods: For this, 100 patients from an orthopedics clinic in São Paulo were evaluated, 71 women and 29 men, with an average age of 52 years. The results were subjected to a descriptive and inferential statistical analysis, which showed that the average pain presented by women (7.1) is higher than that of men (7.1), with a standard deviation of 2.2. Results: Furthermore, it was found that physical exercise is a factor in improving low back pain, improving the average pain by 0.8 points. There was a relationship between pain, metabolic age, and abdominal circumference, while fat replacement was defined as a qualitative variable, without a linear character. Regarding time, it was found that the longer the time, the greater the average pain. Conclusion: There was an association between lipo substitution and pain, resulting in higher pain averages in Goutallier grades 2 and 3. However, fat replacement was not directly related to being overweight, but to a sedentary lifestyle. Thus, it is inferred that low back pain is closely related to muscle trophism.
Biomechanics
429
P038: The range of motion of atlantoaxial joints with the "sandwich" deformity: a human cadaveric biomechanical study
Yinglun Tian 1
1 Orthopedics, Peking University Third Hospital, Beijing, China
Introduction: Patients with “sandwich” deformity (concomitant atlas occipitalization and C2-3 fusion, a subtype of Klippel-Feil syndrome) are at particular risk of developing atlantoaxial dislocation (AAD). Those patients were characterized with earlier onset age, more severe dislocation, higher incidence of Chiari deformity and syringomyelia, and greater difficulty in surgery. But it is unknown if there is special biomechanical characteristics between atlantoaxial joints. To explore if the biomechanical characteristics between atlantoaxial joints in “sandwich” deformity patients is particular and if there is a relationship between the AAD and the malformations (Chiari malformation and the formation of syringomyelia). Material and Methods: We conducted a biomechanical study on the atlantoaxial joint by simulating “sandwich” deformity in cadaveric specimens. Five fresh frozen cadaver spinal specimens (from the occiput to C7) were selected from human donors with no history of spinal trauma and congenital malformations. The C0-1 and C2-3 (C1 pedicle screws combined with occipital titanium, C2 pedicle screws and C3 lateral mass screws) were fixed to develop congenital atlas occipitalization and C23 fusion deformities (“sandwich” deformity). Each specimen was tested two times, firstly under the normal condition and secondly under the “sandwich” condition. Then the range of motion (ROM) between C1 and C2 was measured under different conditions. Results: The results showed that the relative range of flexion-extension motion between C1-2 in the “Sandwich” specimens was significantly greater than that in the normal specimens (p < 0.05). No significant difference in the relative range of other two motion modes (lateral bending and axial rotation) between C1-2 was observed for the normal and “Sandwich” specimens. Conclusion: The ROM between C1-2 in “sandwich” deformity increased during flexion and extension compared with normal atlantoaxial joints. The “clamp” mechanism of “sandwich” deformity might be involved in the pathogenesis of AAD and secondary nervous system damage.
728
P039: Multilevel contribution of passive structures in the spine - a cadaveric stepwise reduction study on the torso
Moritz Jokeit 1,2 , Frédéric Cornaz 1 , Jana Schader 1,2 , Anna-Katharina Calek 1 , Cooper Harshbarger 1,2 , Jess G. Snedeker 1,2 , Mazda Farshad 1 , Jonas Widmer 2,3
1 Department of Orthopedics, Balgrist University Hospital, University of Zurich, Zürich, Switzerland
2 Institute for Biomechanics, ETH Zurich, Zürich, Switzerland
3 Spine Biomechanics, Department of Orthopedics, Balgrist University Hospital, University of Zurich, Zürich, Switzerland
Introduction: Multisegmental spinal structures such as the posterior ligamentous complex (composed of the spinous processes and the interspinous and supraspinous ligaments) and the paraspinal musculature could play an essential role in spinal stability. Due to their multisegmental nature, their effect might be underestimated in biomechanical analysis of single-level functional spine units. The aim of this study was to quantify the load distribution in intact cadaveric human torsi during full flexion. Materials and Methods: A stepwise reduction study was performed on three fresh frozen cadaveric torsi using a custom-built setup with a rigid 6-screw fixation of the pelvis. An external fixator at Th11, Th9, and Th7 combined with a transglenoidal bar was used to mount the torso on a mobile frame that allowed only sagittal plane motion. Preloading (dead load of trunk and frame, relaxation time: > 30 min) was followed by locking of the mobile frame in full flexion and gradual resection of the posterior lumbar structures. Load cells measured the increase in force on the frame after each resection step. The resection steps were performed on the lumbar spine and included: Skin, fascia, musculature, posterior ligamentous complex, facet joints, laminae, posterior longitudinal ligaments. Results: The posterior ligamentous complex contributed 74%, 71% and 69%, for torso #1, #2 and #3 respectively. The combined contribution of skin, fascia and muscles was 3%, 15% and 3%. The facet joints (including their capsules) contributed 2%, 10% and 15% and the ligamentum flavum (between the laminae) 18%, 3% and 2%. The posterior longitudinal ligament contributed 3%, 1% and 11%. Conclusion: In the cadaveric situation, the posterior ligamentous complex plays an essential role in the passive stability of the fully flexed position and analyzing isolated spinal segments might result in underestimation of its relevance. The contribution of skin, fascia and musculature was markedly smaller and appears to be less important.
Acknowledgments: The authors thank the Promedica Stiftung, Chur, for financial support.
748
P040: Radiological progression of scoliosis and spondylolisthesis following bilateral segmental microscopic decompression of the lumbar spine
Walter-Soon-Yaw Wong 1 , Ashton Kai Shun Tan 1 , Kenneth Zhi Kuan Loi 1 , Craigven Hao Sheng Sim 1 , Yilun Huang 1
1 Orthopaedic Surgery, Sengkang General Hospital, Singapore, Singapore
Background: Lumbar spine microscopic decompression is a common surgical procedure for treating various conditions, such as prolapsed intervertebral discs, degenerative disc disease, and spinal canal stenosis, among others. It is currently understood that more extensive decompression may lead to increased instability in the spinal column. However, there is no definitive evidence-based guideline specifying the extent of decompression before biomechanical instability occurs, necessitating instrumented fusion. Existing studies suggest that unilateral segmental decompression surgeries do not result in instability, but there is limited literature on the potential instability associated with bilateral segmental decompression, especially in patients with pre-existing degenerative lumbar scoliosis (SC) and degenerative lumbar spondylolisthesis (SL), who may be at a higher risk of degenerative deformity progression. This study aims to assess whether patients with pre-existing SC or SL are prone to progression following bilateral segmental microscopic decompression of the lumbar spine (BSM). Materials and Methods: A retrospective single-centre cohort study was conducted from August 2018 to October 2021, involving patients who underwent BSM without instrumented fusion. The patients were divided into two cohorts: the first group included patients with pre-existing SC (Cobbs Angle ≥ 10°) or SL (≥ 2 mm), and the second group consisted of patients with no pre-existing SC or SL. The primary outcome was the occurrence of new-onset or progression of scoliosis or spondylolisthesis, defined as a change in Cobbs Angle of ≥ 5° or spondylolisthesis of ≥ 2 mm. Secondary outcomes included revision rates, changes in Back and Leg Visual Analogue Scores (bVAS/lVAS), and changes in Oswestry Disability Index (ODI) scores. These outcomes were collected preoperatively and at 18 months postoperatively for all patients. Baseline characteristics, such as age, BMI, sex, number of levels operated, and whether a discectomy was performed were also collated. Results: A total of 31 patients were reviewed, with 16 patients having pre-existing SC or SL and the remaining 15 patients having no pre-existing SC/SL preoperatively. Patients with pre-existing SC/SL had a 31% incidence of SC/SL progression, which was significantly higher than the 0% incidence in patients without pre-existing SC/SL (p < 0.05). Revision rates, changes in visual analogue scores (VAS), and changes in Oswestry Disability Index (ODI) scores for patients with and without pre-existing SC/SL were as follows: Revision rates: 25% vs. 13.3% (p = 0.65), bVAS: 4.73 vs. 5.15 (p = 0.72), lVAS: 5.20 vs. 4.15 (p = 0.33), ODI: 13.7 vs. 19.0 (p = 0.11). Conclusion: In patients undergoing BSM, pre-existing SC or SL is associated with a higher likelihood of developing radiological progression of spondylolisthesis or scoliosis compared to patients without these pre-existing SC or SL. However, pre-operative SC or SL does not appear to be a strong predictor of revision rates, pain outcomes, or functional outcomes. We recommend close monitoring, especially in the follow-up period, for patients with pre-operative SC and SL, as they are predisposed to the progression.
1002
P041: Is there a difference in spinal cord biomechanics after anterior versus posterior fusion for degenerative cervical myelopathy?
Aditya Vedantam 1 , Balaji Harinathan 1 , Narayan Yoganandan 1
1 Neurosurgery, Medical College of Wisconsin, Milwaukee, USA
Introduction: Spinal cord stress/strain is increased during neck motion and contributes to spinal cord dysfunction in degenerative cervical myelopathy (DCM). It is not known how surgery for DCM changes spinal cord biomechanics but preliminary studies show a reduction in spinal cord stress/strain after surgery. It is expected that anterior and posterior surgical approaches will have distinct post-surgical spinal cord stress/strain profiles, and these may impact neurological recovery. In cases with clinical equipoise, incorporating spinal cord biomechanics into surgical decision-making may best optimize neurological outcomes. The aim of this study was to compare changes in spinal cord biomechanics after anterior cervical diskectomy and fusion (ACDF) versus laminectomy and fusion (LF) using a patient-specific finite element model for DCM. Materioal and Methods: Patient-specific finite element models (FEM) of the cervical spine and spinal cord were created. Clinical equipoise for either an anterior or posterior surgical approach was determined by the surgeon based on clinical and imaging data. Surgical simulation was performed for multi-level ACDF (C4-C5, C5–C6, C6–C7) and LF (C4-6 laminectomy and C3-C7 fusion). Spinal cord von Mises stress and maximum principal strain during neck flexion-extension, lateral bending and axial rotation were recorded. Segmental range of motion and capsular ligament strain were also measured. FEM outputs were calculated as a change with respect to the preoperative values and compared between the two models. Results: Across the surgical levels (C4-C7), neck flexion was associated with decreased spinal cord stress by 24% after ACDF but increased by 4% after LF. Neck extension and axial rotation were associated with similar decrease in spinal cord stress after ACDF and LF. Lateral bending was associated with greater decrease in spinal cord stress after ACDF (-45%) compared to LF (-28%). Decrease in spinal cord strain during neck flexion was greater for LF (-37.6%) compared to ACDF (-16.5%). Spinal cord strain decreased after ACDF (-37.8%) during neck extension but increased after LF (+25.4%). At the superior adjacent segment, spinal cord stress was greater after LF during neck flexion (+8%) and extension (+75%) as well as axial rotation (+28%). Spinal cord stress was higher in the adjacent segments after LF compared to ACDF, despite a decrease in global neck range of motion. Capsular ligament strain was similar between ACDF and LF across the fused levels. Conclusion: Anterior and posterior cervical approaches for DCM are associated with distinct effects on spinal cord stress/strain especially during neck flexion-extension. Despite decreased global neck range of motion, LF was associated with greater spinal cord stress during neck flexion and increased spinal cord strain during neck extension at both the decompressed levels and adjacent segments. The distinct effects on spinal cord biomechanics may play a role in neurological recovery after surgery and could be incorporated into surgical decision-making in DCM cases with clinical equipoise.
1046
P042: Anterior bone loss after anterior cervical discectomy and fusion and cervical disc replacement: analysis from the influence of cervical sagittal alignment
Yi-Wei Shen 1 , Tingkui Wu 1 , Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu
Introduction: Anterior bone loss (ABL) is a common phenomenon after cervical disc replacement (CDR), while it is also observed after anterior cervical discectomy and fusion (ACDF). This study aimed to investigate the incidence and severity of ABL in single-level CDR and ACDF and explore the association of cervical sagittal alignment with ABL. Material and Methods: This is a single-center retrospective cohort study. 113 patients treated with CDR and 99 patients treated with ACDF were retrospectively reviewed from January 2014 to January 2019 in West China Hospital. Radiological data were collocated at pre-operation, 1 week, 3 months postoperatively, and the last follow-up. Cervical sagittal alignment parameters, including C0-C2 angle, cervical lordosis (CL), C2-C7 sagittal vertical axis (cSVA), T1 slope, functional spinal unit angle, disc angle, and surgical level slope, were evaluated. Results: ABL was identified in 75 (66.4%) patients in the CDR group and 57 (57.6%) patients in the ACDF group. There were no significant differences in the incidence, severity, and location of ABL between the ACDF and CDR groups. For patients who underwent ACDF, the proportion of females was significantly higher in ABL group (p = 0.002), while the BMI was significantly lower in the ABL group compared to non-ABL group (22.72 ± 3.09 vs. 24.60 ± 3.04, p = 0.002). The effect of ABL on the short-term clinical outcomes of ACDF and CDR was not observed. In the ACDF group, patients with ABL had significantly smaller postoperative CL (11.83 ± 8.24° vs. 15.25 ± 8.32°, 95% CI 0.08-6.75, p = 0.045), T1 slope (24.06 ± 6.85° vs. 27.35 ± 8.19°, 95% CI 0.27-6.29, p = 0.033), cSVA (17.77 ± 10.08 mm vs. 23.35 ± 9.86 mm , 95% CI 0.15-0.96, p = 0.007), and surgical level slope (13.99 ± 6.43° vs. 16.97 ± 5.88°, 95% CI 0.48-5.49, p =0.020). ABL after CDR was less correlated to the cervical sagittal alignment. Conclusion: ABL is common after both CDR and ACDF. The incidence, severity, and location of ABL were all comparable between CDR and ACDF. Cervical sagittal alignment was closely related to ABL after ACDF while had less influence on ABL after CDR. Smaller postoperative cervical lordosis, T1 slope, sagittal vertical axis, and surgical level slope were observed in patients with the occurrence of ABL after ACDF.
1062
P043: The pelvic incidence (PI) is a dynamic parameter: preliminary results of a retrospective analysis on flexion and extension X-ray scan in patients operated for spinal fusion
Pasquale Donnarumma 1 , Luca Reale 2 , Gianluca Colella 3 , Armando Rapanà 1
1 Neurosurgery, Moscati Hospital, Avellino, Italy
2 University of Campania Luigi Vanvitelli, Naples, Italy
3 Orthopedics and Traumatology, Santobono Hospital, Naples, Italy
Introduction: Since they were described by Legaye et al, pelvic parameters have gained increasing interest in the scientific community and their measurement are nowadays routinely used by vertebral surgeons all over the world. Pelvic Incidence (PI) has been considered a fixed measurement for a long time, since it describes the morphology of the patient’s pelvis. It is recently shown PI is not necessarily a constant value since minimal changes in different positions have been described in normal individuals, but the implications of PI changing under pathological conditions have not yet fully investigated. The aim of the study is to evaluate PI in patients operated for spinal fusions, analyzing pre-operative X-ray scan in flexion-extension and comparing the value with postoperative X-ray scan. Material and Methods: Retrospective cross-sectional study. Participants included consecutive patients operated for spinal fusion due to degenerative spinal disorders. Inclusion criteria: 1) age > 18 years; 2) flexion and extension X-ray scan of the lumbar spine in standing position obtained in pre-operative period; 3) standing X-ray scan obtained 30 days after surgery; the images had to include both femoral heads. Exclusion criteria: 1) previous vertebral body or pelvic fracture; 2) tumor or infection involving the vertebral bone or spinal canal; 3) hip arthroplasty; 4) previous spinal surgery. Demographic and clinical data were extracted from the medical records. The PI, PT, SS and lumbar lordosis were measured using Radiant Viewer software analyzing the DICOM files. Results: The final sample included 33 patients (F = 20, 67%; M = 13, 33%) with a mean age of 63 years old. All the patients underwent spinal fusions using a posterior approach: 26 patients underwent TLIF or PLIF, 10 including sacrum, 4 including pelvis (bilateral S2-Alar screws). Careful review of the data revealed 27 of the 33 subjects (81%) had a change in their pelvic incidence from flexion to extension in pre-operative period; 12 of them (36%) showed a change in pelvic incidence ≥ 3°. The mean change was 2.67°. Three degrees was taken as a cutoff threshold because it was determined that the standard deviation for all of our measurements was 2°. A change of ˃ 5° was observed in 6 of the 33 subjects (18%). 7 of 33 subjects (21%) decreased their PI after surgery by a mean of 2,6° and 25 of 33 subjects (75%) increased their PI by a mean of 3.7°. In 4 patients undergoing S2AIar screws placement and sagittal cantilever correction, PI changed ≥ 6°. Conclusion: PI is a dynamic parameter that can change from flexion to extension and after spinal fusions including the sacrum and pelvis. These changes appear to be due to mobility of the sacrum relative to the pelvis through the sacroiliac joints and they can be relevant in sagittal cantilever correction techniques for adult deformity. A high preoperative PI were more associated to a significant PI change between flexion and extension. Regarding whole-spine lateral radiographs, errors in PI measurements may occur due to pelvic rotation or nonvertical projection of X-rays.
1102
P044: Does the gap matters? Finite element analysis of the biomechanical effect of bone-implant interface gap after cervical disc replacement
Yi-Wei Shen 1 , Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu
Introduction: The solid binding of the artificial cervical disc to the vertebral endplates is the key to achieve the stability of the prosthesis and good clinical outcomes after cervical disc replacement (CDR). Due to the irregularity of human cervical endplate morphology and the variances between different individuals and segments, it is difficult for current commercial artificial cervical disc prosthesis and the cervical endplate to match perfectly, and there are often different sizes of gap between the bone-implant interface after implantation. The existence of the gap may lead to uneven stress distribution at the bone-implant interface and decrease the immediate stability of the implant. This study aims to explore the influence of bone-implant interface gap on biomechanical environment after CDR through three-dimensional finite element study. Material and Methods: The DICOM data of CT images from a young male volunteer was used to construct the three-dimensional finite element model of intact cervical spine (C2-C7), then the intact model was validated. The finite element model of Prestige-LP cervical disc prosthesis was established, followed by the simulation of CDR at C5/6. Then we constructed the cervical spine model with bone-implant interface gap and model without gap, and defined the boundary conditions. The model was fixed at the inferior endplate of C7. Follower loads of 73.6N were applied to the odontoid of C2 vertebra to simulate head weight, accompanying with a 1.0 N·m moment to produce flexion, extension, lateral bending, and axial rotation of cervical spine. The stress distribution, micromotion, and subsidence displacement at the bone-implant interface between the gap and no-gap model were compared to clarify the biomechanical effects of the bone-implant interface gap after CDR. Results: For bone-implant interface stress, the maximum stress of the inferior endplate of C5 in the gap model was larger than those in no-gap model in all the 4 loading conditions. The presence of the gap increased the maximum stress of the endplate by 86.5%, 100.9%, 64.2%, 11.4% in flexion, extension, lateral bending, and axial rotation, respectively. The stress diagram suggested that there was an obvious stress concentration area at the posterior portion of the vertebral endplate in the gap model, while the stress distribution was more uniform in the endplate in the no-gap model. The micromotion in the gap model was smaller than that in the no-gap model in flexion and extension, while in the lateral bending and axial rotation, the gap model had larger micromotion than no-gap model. The micromotion mainly existed in the contact area between the prosthesis rails and the endplate. The subsidence was greater in the gap model in flexion and lateral bending than that in the no-gap model, which primarily occurred at the posterior junction between the prosthesis and the endplate. Conclusion: The bone-implant interface gap after CDR significantly increases the stress of the posterior area of the endplate. The existence of the gap may increase the risk of subsidence in the posterior bone-implant interface, while its effect on the micromotion is not significant.
1392
P045: Effect of decompressive surgical techniques on the biomechanics of the lumbar spine
Sara Montanari 1 , Elena Serchi 2 , Giovanni Barbanti Bròdano 3 , Alfredo Conti 2 , Luca Cristofolini 1
1 Department of Industrial Engineering, Alma Mater Studiorium - University of Bologna, Bologna, Italy
2 Ospedale Bellaria, IRCCS Istituto delle Scienze Neurologiche, Bologna, Italy
3 Spine Surgery Unit, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Lumbar spinal stenosis causes the compression of neurovascular structures. The different decompression techniques, such as the hemilaminectomy and laminectomy, partially or completely remove the posterior elements increasing the space in the spinal canal. Removal of these structures could aggravate or create spinal instability [1]. Therefore, these surgical techniques are often completed by a posterior fixation. In addition, the deriving changes of the load transmission could also alter the disc strains. The aim of this study was to investigate if and how the decompressive techniques, alone or with a posterior fixation, alter the mechanical stability and strains on the intervertebral discs in the lumbar spine. Material and Methods: Twelve L2-S1 human spine segments were prepared preserving all the ligaments and removing fat and muscles around the discs and the vertebral bodies. A white speckle pattern was sprayed on the surface of each specimen to measure the displacements and surface strains with Digital Image Correlation (DIC). All the specimens were mechanically tested in flexion, extension, right and left lateral bending under 2.5 Nm. Each specimen was sequentially tested in the intact condition, after L4-L5 hemilaminectomy, after full L4-L5 laminectomy, and after L4-S1 posterior fixation with pedicle screws and rods. The side of the hemilaminectomy was selected randomly. Surface images were acquired and analyzed by a 3D-DIC system with two sensors (GOM Aramis 12M) using optimized parameters [2]. The L2-S1 segment motion under load (RoM) was measured. Furthermore, the tensile (Ɛ1) and compressive (Ɛ2) principal strains distribution in the L4-L5 discs were assessed for each loading configuration. Results: Correlations and measurements were successfully performed for all the loading configuration and all conditions. Data were analyzed at the stage of the maximum moment of 2.5 Nm. No statistically significant changes (p > 0.05, Friedman test) were observed from intact to hemilaminectomy neither for the Rom nor for L4-L5 disc strains. A statistically significant (p < 0.05, Friedman test) increase in RoM was observed after laminectomy, indicating a loss of stability in flexion and in lateral bending on opposite side where the hemilaminectomy was performed (contralateral bending). Contralateral bending was the most challenging loading configuration also due to the significant increase in maximum tensile strain on L4-L5 disc surface after laminectomy (p < 0.05, Friedman test). Preliminary results after fixation showed the reduction of both RoM and tensile and compressive strains in the L4-L5 disc, with respect to the intact. Conclusion: This study aimed to assess the risk of instability and changes in the strain distribution after lumbar spinal decompression, performed by hemilaminectomy or laminectomy, and fixation. These results showed that the hemilaminectomy does not significantly alter the biomechanics of the lumbar spine. The increased RoM in flexion, after laminectomy, did not seem to significantly challenge the L4-L5 disc. Indeed, no significant increases in strain were observed. Conversely, in the contralateral bending both the maximum tensile strain and RoM increased.
References
1. Zaina et al, Cochrane Database Sys Rev, Jan 29, 2016
2. Palanca et al, MEP, 52: 76-83, 2018.
1463
P046: Investigation of the biomechanical properties of fixation constructs used in L5/S1 anterior lumbar fusion spine surgeries
Alana Celenza 1 , Jessica Gaff 1 , Gregory Cunningham 1 , Paul Taylor 1 , Michael Kern 1 , Andrew Miles 1
1 NeuroSpine Institute, Research, Perth, Australia
Introduction: In anterior lumbar interbody fusion (ALIF), the maintenance of stability and rigidity at the fusion site is fundamental in obtaining successful fusion and is often dependent on the instrumentation used and the use of supplementary fixation constructs. Fixation in ALIF may be performed using integrated cages, anterior plates, pedicle screws or a combination of these. Selection of fusion devices are currently determined by the surgeon’s preference with no investigation into the suitability of these supplementary fixation constructs to the lumbosacral (L5-S1) site, which distinctly receives a higher degree of mechanical load and stress compared to above segments. Here we compare surgical, patient-reported and in silico biomechanical properties of these supplementary fixation techniques for the L5-S1 site. Methods: Demographic, surgical and patient reported outcome measures (PROMs) were retrospectively analysed for participants who underwent single level ALIF-L5-S1 with an integrated cage and/or additional fixation constructs of anterior plate or pedicle screws between June 2019 and August 2023. PROMs were collected pre-operatively and at 12, 24, 52 and 104-weeks post-operative, including the EQ-5D-5L, Visual Analogue Scale (VAS) for back and leg pain intensity and the Oswestry Disability Index (ODI). Biomechanical properties were assessed computationally. A 3-dimensional finite element model for the L5-S1 segment was developed using computerised tomography scan data and physiological forces applied and assessed for each of the stand alone, integrated cage, anterior plate and pedicle screw fixation techniques. Results: A total of 130 patients (52% female, mean age 51.4 years) underwent ALIF-L5-S1 with additional fixation; Integrated cage n = 3; Anterior plate n = 80; Pedicle screw n = 36; Anterior plate with pedicle screw n=11. Blood loss and surgery duration were 50ml and 120minutes for the integrated cage, 50 ml and 120 minutes for anterior plate, 120 ml and 120 minutes for the pedicle screw and 150ml and 120 minutes for anterior plate with pedicle screws. The anterior plate with pedicle screw fixation group had the highest post-operative complication rate (18%) followed by anterior plate (14%) and pedicle screw (11%), with no complications in the integrated cage group. Three participants (anterior plate n = 2; pedicle screws n = 1) required return to theatre for pseudomeningocele and wound debridement. Improvements in PROMs were generally greatest for the integrated cage group. This was followed by the anterior plate and the pedicle screws fixation groups which demonstrated statistically significant improvements for most PROMs. At 104-week follow-up the mean improvement in ODI and VAS back were 41.5 and 5.6 for the integrated cage respectively, compared to 18.2 and 3.3 for the anterior plate, 20.6 and 3.8 for the pedicle screw and 12.9 and 0.9 for the anterior plate with pedicle screw. Finite element analyses data will be presented. Conclusions: Surgical outcomes were similar across all fixation techniques assessed and all techniques demonstrated improved post-operative PROMs. The integrated cage resulted in the best surgical and patient-reported outcomes however, increased sample size may improve comparability. Results of finite element analyses may highlight the biomechanical differences of each of these supplementary fixation techniques and aid in informing surgeon decision making.
1694
P047: Impact of lumbar degenerative change on vertebral bone strength: a finite element analysis
Soji Tani 1,2 , Koji Ishikawa 2 , Erika Chiapparelli 1 , Gaston Camino-Willhuber 1 , Lukas Schönnagel 1 , Thomas Caffard 1 , Krizia Amoroso 1 , Ali Guven 1 , John Carrino 1 , Federico Girardi 1 , Andrew Sama 1 , Frank Cammisa 1 , Alexander Hughes 1
1 Hospital for Special Surgery, New York, USA, 2 Showa University, Shinagawa-ku, Japan
Introduction: Assessing the bone condition in patients with spinal disease is clinically valuable. However, evaluating bone strength in the presence of spine degenerative changes can be challenging. To address this issue, quantitative computed tomography (QCT) and finite element analysis (FEA) have been proposed as potential methods for more accurate bone quality assessment. Nonetheless, the impact of degenerative changes on bone strength is not fully understood. Therefore, the aim of this study is to investigate the relationship between bone strength measured by FEA and other relevant biological parameters. Material and Methods: This retrospective cross-sectional study included 127 patients with spinal disease who underwent preoperative CT scans between 2014 and 2020. Baseline patient characteristics, volumetric bone mineral density (vBMD) measured by QCT, and vertebral bone strength measured by FEA were collected. The degree of degeneration was evaluated by classifying osteophyte formation, disc height narrowing, vertebral sclerosis, and spondylolisthesis into a grading scale ranging from 0 to 2. Multiple linear regression analysis was conducted to assess the effect of each factor on bone strength measured by FEA. Results: Of 127 patients, 120 patients (median age was 62 years) were included. The median vBMD and vertebral strength were 114.3 mg/cm3 and 7892.9 N, respectively. After adjusting for age, sex, body mass index, smoking status, diabetes mellitus, vBMD, and degenerative changes, multiple linear regression analysis revealed that sex, vBMD, and degree of degeneration independently increased the vertebral strength measured by FEA. Conclusion: The results of this study suggest that in patients with spinal disease, vertebral bone strength is affected not only by sex and bone mineral density but also by degenerative changes. FEA is a useful method that can comprehensively determine multiple bone strength factors. Thus, bone quality could be assessed more accurately considering degenerative changes in patients with spinal disease.
1703
P048: Biomechanics effect of a novel "tether pedicle screw" in long-segment spinal instrumentation
Raphael Gmeiner 1 , Heiko Koller 2 , Sara Lener 1 , Christoph Orban 1 , Anto Abramovic 1 , Marko Konschake 3 , Werner Schmoelz 4 , Claudius Thomé 1 , Sebastian Hartmann 5
1 Neurosurgery, Medical University of Innsbruck, Innsbruck, Austria
2 Department of Orthopedics and Traumatology, Asklepios Kliniken GmbH & Co, Bad Abbach, Germany
3 Department of Clinical and Functional Anatomy
4 Department of Orthopedics and Traumatology, Medical University of Innsbruck, Innsbruck, Austria
5 Spine Center/Neurosurgery, Sanatorium Kettenbrücke, Innsbruck, Austria
Introduction: Correcting adult spinal deformities with long thoracolumbar instrumentations bears a high failure incidence. A “soft landing” at the cranial construct end might reduce the risk of proximal junctional kyphosis and the corresponding failure. Therefore, a novel “tether pedicle screw” (TPS) was developed. This redesigned pedicle screw contains a tether between the thread and the screw head, allowing some residual motion. Objective of the study is the biomechanical comparison of the TPS at the proximal junction in thoracolumbar instrumentations of human spine specimen. Material and Methods: For the first flexibility test, ten human thoracolumbar (Th7-L1) spine specimen were tested in three instrumented states (each n = 10). The conventional instrumentation (Conv state) represented a standard thoracolumbar fixation from Th10-L1. In the TPS+1 instrumentation the novel screw with rod was implanted in Th9, in the TPS+2 instrumentation in Th9 and Th8. Flexibility tests (±5 Nm) for flexion/extension, axial rotation as well as lateral bending were performed in all states and after cyclic loading (250 cycles, +1 – 10 Nm). Cyclic loading was conducted with the standard instrumentation from Th10-L1 (standard group, n = 5) and TPS+2 instrumentation (TPS+2 group, n = 5). ROM changes and differences were expressed in %, normalized to the Conv state. Results: In the precyclic flexibility tests, the TPS+2 instrumentation demonstrated the largest ROM decrease in the first adjacent segment Th9-10, with a reduced effect in the second adjacent segment Th8-9. There was no change in the ROM observed in the upper most segment Th7-8 between the three instrumented states. Cyclic loading increased the ROM across all states and motion directions in standard and TPS+2 group. No ROM difference was observed in the first adjacent segment Th9-10. Conclusion: The novel “tether pedicle screw” demonstrated promising biomechanical results by effectively distributing the loads across three segments, representing a new semi-rigid junctional fixation technique.
2030
P049: In vivo segmental vertebral kinematics in patients with degenerative lumbar scoliosis
Fei Xu 1 , Weishi Li 1
1 Orthopaedic Department, Peking University Third Hospital, Beijing, China
Introduction: In clinical settings, previous studies [18, 19] explored the biomechanics of scoliotic spines using the finite element method (FE). However, this method did not accurately represent the real status of the human spine. To overcome these limitations, this study employed a combined dual fluoroscopic and magnetic resonance imaging (MRI) technique to determine the six degrees-of-freedom (DOF) vertebral motion of patients [20-22]. Material and Methods: Fifty-four patients were involved into this study with forty-two in DLS group and twelve in the control group. The three-dimensional (3D) vertebral models from L1 to S1 of each participant were reconstructed by computed tomography (CT). Dual-orthogonal fluoroscopic imaging, along with FluoMotion and Rhinoceros software, was used to record segmental vertebral kinematics during functional weight-bearing activities. The primary and coupled motions of each vertebra were analyzed in patients with DLS. Results: During flexion-extension of the trunk, anteroposterior (AP) translation and craniocaudal (CC) translation at L5-S1 were higher than those at L2-3 (9.3 ± 5.1 mm vs. 6.4 ± 3.5 mm; p < 0.05). The coupled mediolateral (ML) translation at L5-S1 in patients with DLS was approximately three times greater than that in the control group. During left-right bending of the trunk, the coupled ML rotation at L5-S1 was higher in patients with DLS than that in the control group (17.7 ± 10.3° vs. 8.4 ± 4.4°; p < 0.05). The AP and CC translations at L5-S1 were higher than those at L1-2, L2-3, and L3-4. During left-right torsion of the trunk, the AP translation at L5-S1 was higher as compared to other levels. Conclusion: The greatest coupled translation was observed at L5-S1 in patients with DLS. Coupled AP and ML translations at L5-S1 were higher than those in healthy participants. These data improved the understanding of DLS motion characteristics.
2534
P050: The impact of lumbar laminectomy and laminotomy on spinal stability and mobility using biomechanical evaluations: a systematic review
Alexandra Seidenstein 1 , Andrew Kim 1 , Gabriel Nazario-Ferrer 1 , Craig Almeida 2 , Jill Middendorf 2 , Amit Jain 1
1 Department of Orthopaedic Surgery, The Johns Hopkins Hospital, Baltimore, USA
2 Department of Mechanical Engineering, The Johns Hopkins Whiting School of Engineering, Baltimore, USA
Introduction: Lumbar laminectomy and laminotomy are well-established procedures that effectively alleviate neural compression and restore neurological function. Despite their efficacy, there is limited consensus on their impact on spinal mobility and stability. This study aims to analyze biomechanical studies assessing the range of motion outcomes following different laminectomy and laminotomy techniques to understand how each decompression procedure affects spinal mobility and segmental stability. Material and Methods: PubMed (NLM), Google Scholar, and Scopus databases were systematically searched in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines using Keywords including ‘laminectomy,’ laminotomy,’ spinal decompression,’ ‘spine biomechanics,’ ‘partial laminectomy,’ and ‘spinal stability.’ The search included articles published from 2000 to 2023 and were screened and evaluated by three independent reviewers. Data on study design, surgical techniques, biomechanical measurements, and reported outcomes were collected when available. Results: leven studies were included for analysis, seven modeling laminectomy, three on hemilaminectomy, two on unilateral laminotomy, one on bilateral laminotomy, and four on facetectomy procedures. Among studies modeling full laminectomy, post-procedure flexion and extension measurements had mean changes of 35.0% (range 12-53%) and 118.8% (range 10-400%) respectively. Studies modeling partial and hemilaminectomy procedures had mean changes of 4.4% (range 2-10%) and 2.0% (range 0-5%) in post-procedure flexion and extension. Mean changes in rotation were 41.0% (range 0.4-120%) and 8.3% (range 1-15%) for laminectomy and partial/hemilaminectomy procedures. Conclusion: Less invasive spinal decompression surgeries, such as laminotomy and hemilaminectomy, exhibit less post-procedure destabilization and instability concerning range of motion, compared to full laminectomy and facetectomy. These findings advocate for additional research and application of laminotomy techniques to preserve spinal biomechanical integrity. Understanding biomechanical differences associated with each surgical technique allows orthopaedic surgeons to tailor management strategies to patient specific needs and spinal pathologies, thereby optimizing functional outcomes.
Deformity-cervical
480
P051: Posterior intra-articular distraction technique to treat pediatric atlantoaxial instability
Wanru Duan 1 , Mading Zhou 1 , Zan Chen 1
1 Neurosurgery, Xuanwu Hospital, Capital Medical University, Beijing, China
Introduction: Besides trauma and growth of a neoplasm, atlantoaxial instability in pediatric patient can also be caused by inflammatory processes, Down’s syndrome, os odontoideum, rheumatologic disorders and etc. The relatively small-size underdeveloped cervical spine ossification centers and ligamentous structures, as well as the presence of congenital malformations with possible abnormal vertebral artery location have made the surgical treatment of these pediatric patients technically challenging. Historically, the choice of surgical treatments includes anterior transoral decompression or posterior occipito-cervical fusion. However, the anterior transoral decompression might be really limited in pediatric patients due to risks of wound infection, CSF leaks, difficulty swallowing and etc., while the traditional posterior-only approaches lack the ability to release the anterior soft tissue and may resulting in unsatisfactory reduction. Material and Methods: This is a retrospective descriptive study which included 15 patients of atlantoaxial instability whose age was less than 18 years at the time of clinical presentation. All had one or more radiologic markers of congenital atlantoaxial instability. C1-C2 subluxation secondary to traumatic or degenerative pathology was excluded. All patients underwent anterior soft tissue released through a posterior-only approach, followed by intra-facet cages implantation, cantilever correction, and instrumentation. Clinical results were measured using the Japanese Orthopedic Association (JOA) scale, and radiographic measurements including the atlantodental interval(ADI), posterior atlantodental interval(PADI), the distance of odontoid tip above Chamberlain’s line, clivuscanal angle (CCA), and triangular area(TA) of cranio-vertebral junction. Results: The follow-up time ranges from 18 to 72 months with an average of 41.4 months. JOA score increased from 12.50 to 14.56. The mean TA decreased from 253.73 mm2 preoperatively to 185.36 mm2 postoperatively. The mean CCA improved from 135° preoperatively to 145° postoperatively. There were no evidence of postoperative neurovascular complications or iatrogenic secondary cervical deformity during follow-up. Radiological evaluation showed satisfactory corrections and bony fusions of C1/2 facet joint in all cases. Conclusion: Posterior intra-articular distraction followed by cage implantation and cantilever correction can be one of the safe and effective way to solve this challenging pediatric spinal disorder.
690
P052: Cervicothoracic dislocation due to congenital and bony-anomaly-related vertebral malformations
Olga Sergeenko 1 , Alexandr Burtcev 2 , Alex Evsukov 1
1 Ilizarov Center, 9, Kurgan, Russian Federation, 2 Ilizarov Center, Director, Kurgan, Russian Federation
Objective: This study aims to assess treatment approaches for pediatric cervicothoracic dislocations related to congenital and bone dysplasia, with a focus on identifying the optimal treatment method. Methods: We conducted a comprehensive literature review using PubMed and Google Scholar databases, applying specific criteria including the pediatric age group, disease category, treatment details, and follow-up outcomes. Additionally, we present case descriptions of six pediatric patients with cervicothoracic dislocations and various vertebral malformations. Results: Our review identified only eight patients meeting the aforementioned selection criteria in the published literature. Among them, three had Klippel-Feil syndrome (KFS), two had single-level vertebral anomalies, one had neurofibromatosis type 1 (NF1), one had Larsen syndrome, and one presented with a variant of VACTERL association. Treatment for these patients was characterized by its complexity, requiring long-term and multi-stage interventions. Among our own cases, four patients also had KFS, one had a variant of VACTERL association, and one had NF1. All patients exhibited preoperative neurological disorders. Surgical procedures included posterior instrumental fixation with posterior vertebral body resection in four cases, while one patient underwent a combined surgery. The parents of one patient declined surgery, and they opted for observation and bracing treatment. Given the challenging and protracted nature of treatment, the average follow-up period extended to five years. Conclusions: Congenital cervicothoracic dislocations represent a highly uncommon pathology that typically emerges in early childhood, necessitating prompt surgical intervention to prevent disability. Individualized surgical strategies are required for these patients; however, both published data and our own experience suggest that early multi-stage combined treatment has shown the most promising outcomes thus far. Notably, cervicothoracic dislocations related to NF1 tend to manifest later and exhibit a more favorable prognosis.
1177
P053: Measurement of cervical range of motion by comprehensive musculoskeletal analysis system: repeatability and reliability analysis
Huajiang Chen 1
1 Orthopedics, Shanghai Changzheng Hospital, Shanghai, China
Objective: To propose a new method of measuring the cervical range of motion (ROM) by Comprehensive Musculoskeletal Analysis System (CMAS), and investigate the repeatability and reliability. Methods: The patients with neck or shoulder pain in the spine surgery clinic of our hospital were included. The ROM of the cervical spine was measured by CMAS and the dynamic image of DSA. 50 patients were measured with CMAS (Group A). There were 28 males and 22 females, aged from 20 to 68 years, with an average of 45.1 ±13.8 years old. 15 patients were also measured with dynamic x-ray (DSA, digital subtraction angiography) images (Group B). There were 8 males and 7 females, aged from 21 to 68 years, with an average age of 46.1 years old. The measurement results of the two groups were compared and correlation analyzed. Intra-observer and inter-observer consistency of Group A were analyzed. The two methods' reliability was analyzed using Standard error of measurement (SEM) and minimum detectable change (MDC). Results: There was no significant difference in demographic dates between the two groups (p > 0.05). And there was no significant difference between the two methods in different gender and age groups (p > 0.05). Intra-observer consistency analysis of Group A showed high degree, ICC = 0.947, 95% CI (0.763, 0.980), p < 0.01. Inter-observer consistency analysis also showed high degree, ICC = 0.899, 95% CI (0.799, 0.947), p < 0.01. For Group A, SEM and MDC were 3.0° and 6.9° respectively, and SEM and MDC were 1.8 ° and 4.1 ° respectively for Group B. Correlation analysis showed that the two methods had significant correlation (p < 0.01), and the correlation coefficient was 0.758. Bland Altman's analysis showed that the average difference between the two methods was 0.29°. The Bland-Altman plots demonstrated that most of the data were within the 95% consistency limit. Conclusion: The measurement of cervical ROM with CMAS has good repeatability and reliability and is an effective method for measuring cervical ROM.
1335
P054: Diffuse cervical idiopathic skeletal hyperostosis causing dysphagia: report of three cases
Hassan Hachicha 1 , Habboubi Khalil 1 , Amine Chabchoub 1 , Chaker Mohamed 1 , Hassen Makhlouf 1 , mondher mestiri 1
1 Adultes Department, Mohamed Kassab Institute, Mannouba, Tunisia
Introduction: Consultations in otolaryngology and gastroenterology are frequently requested due to dysphagia. This symptom may be brought on by mechanical compression of the pharyngo-oesophageal region brought on by an anterior cervical osteophyte. A diffuse idiopathic skeletal hyperostosis, commonly known as Forestier's illness, or ankylosing spondylitis can all cause anterior cervical osteophyte. In addition to compressing the pharyngo-oesophageal segment, cervical osteophytes can also obstruct the trachea, sympathetic chain, jugular foramen, and vertebral artery. Here, we discuss three examples with dysphagia that needed to be treated surgically in our orthopedic department. Cases Presentation: We represent three patients treated for progressive dysphagia brought on by anterior osteophytes. They were all males, with an average age of 64 years. Their main complaint was increasing dysphagia. Every patient expressed concern about the worsening dysphagia for solids than for liquids. One patient had a significant weight decrease of ten kilograms in six months. There was no prior history of odynophagia, shortness of breath, noisy breathing, or voice changes. All patients have seen other doctors before us. Anterior osteophytes were visible at various cervical levels on plain radiographs of the cervical spine (from C2 to C7 in one case and arising from the C4, C5, and C6 vertebra in the two other cases). All patients had a barium swallow that revealed indentations on the posterior esophageal wall had extrinsic mechanical compression confirmed. There was no requirement for discectomy, fusion, or internal fixation; they underwent an anterior cervical osteophytectomy instead. Within one month of follow-up, all patients reported complete symptom relief and immediate postoperative considerable improvement of dysphagia. The average patient follow-up time was 52 months, and no instability was noted in patients during this time. A patient consulted us at 6 years postoperatively for recurrence of dysphagia. He was explored by a barium swallow which showed an esophageal stenosis with recurrence of the anterior cervical osteophyte from C4 to C6 on CT. The patient is a candidate for a revision of the osteophytectomy. Conclusion: It is uncommon to experience dysphagia, airway obstruction, or both as a result of anterior osteophytes. Fortunately, a straightforward lateral radiograph of the neck confirms the diagnosis. Osteophytes are removed as part of treatment, usually without the requirement for spinal stabilization.
1563
P055: Physical and psychological impact of scar cosmesis after cervical spine fusion surgery
Parker Brush 1 , Olivia Opara 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Matthew Meade 2 , Omar Tarawneh 1 , Alexa Tomlak 1 , Abbey Glover 3 , Julian Takagi-Stewart 3 , Emily Ducaji 4 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Rothman Orthopaedic Insitute, Orthopaedics, Philadelphia, USA
2 Rowan University, Division of Orthopaedics, New Jersey, USA
3 Drexel University, Philadelphia, USA
4 Thomas Jefferson University, Philadelphia, USA
Introduction: The perception of cutaneous scarring between patients and surgeons can vary, causing unpleasant physical and psychological outcomes. It is of utmost importance that surgeons are aware of the effect of scarring on patients before and after surgery to encourage and enable communication between both parties. This study aims to bridge the current scientific literature gap and understand the impact of patient-perceived scar cosmesis after anterior and posterior cervical spine surgery. Material and Methods: Retrospective review of patients ≥18 years old who underwent anterior or posterior cervical spine surgery from 2017 to 2022 at a large, urban academic group. Surgical interventions for trauma, infection, or malignancy were excluded. To select patients with adequate time for surgical scar maturation, only patients who were greater than six months post-surgery were included. Electronic medical records for all included patients were retrospectively reviewed for demographics, comorbidities, psychiatric history, and operative information. The SCAR-Q survey, a surgical scar assessment tool, assessed scar symptomatology, appearance, and psychological impact. Scores range from 0 to 100, with 100 as the best outcome. A Kruskal-Wallis test was used to compare continuous data, and a Chi-Square test was used to compare categorical data. Linear regression analysis was utilized to identify factors independently associated with the three components of the Scar-Q survey, and a Poisson regression was utilized to identify factors associated with a more favorable outcome. Results: Of the 4696 patients sent the SCAR-Q survey, 854 completed the survey. All respondents were stratified into five groups based on surgical satisfaction: very unsatisfied, unsatisfied, neutral, satisfied, and very satisfied. Patient demographics between these groups were not significantly different. Patients who reported being “very satisfied” with their cervical spinal surgery demonstrated the greatest numerical outcome for all scar-related questions evaluated. Patients who were “unsatisfied” with their surgery had the lowest outcome scores for SCAR-Q appearance, symptom, and psychologic scores; the “unsatisfied” patient scores were significantly lower than those who were “very unsatisfied” for all scores (p < 0.001). Further comparison was carried out comparing males vs. females, with females having a significantly higher/“more favorable” SCAR-Q Appearance (77.5 vs. 82.8 p < 0.001) and Psychologic (87.4 vs. 94.3 p < 0.001) scores as compared to their male counterparts. Regression analysis performed for each component score showed that unsatisfied patients were associated with worse SCAR-Q component scores (Appearance Estimate:-16.47, p =< 0.001; Symptom Estimate: -4.67, p =< 0.001; Psychological Estimate:-16.48, p =< 0.001) and very satisfied Likert score was only associated with better SCAR-Q symptom score (Estimate: 1.21, p = 0.029). Additionally, posterior spine surgery was associated with better SCAR-Q appearance (Estimate: 4.73; p = 0.019) and symptom (Estimate: 1.53, p = 0.004) scores. Conclusion: Our study demonstrates that patients dissatisfied with their surgical outcome have lower scar-related scores, highlighting the impact of cosmetic closure and appearance. While surgical wound closure is a vital terminal step in cervical spine surgery to provide the decreased risk of wound complications, this study demonstrates that wound cosmesis is imperative to patient-reported outcome scores as well.
1789
P056: Posterior approach release and reduction followed by intra-articular interbody fusion cage implantation for basilar invagination with irreducible atlantoaxial dislocation
Xiaoyu Cai 1 , Tao Xu 1 , Maierdan Maimaiti 1 , Weibin Sheng 1
1 First Affiliated Hospital of Xinjiang Medical University, Ürümqi, China
Introduction: To evaluate the clinical outcomes for the treatment of basilar invagination (BI) with irreducible atlantoaxial dislocation (irAAD) by posterior approach release and reduction followed by intra-articular interbody fusion cage implantation. Material and Methods: Between January 2010 and January 2020, clinical data of patients who had BI-irAAD received surgery at our institution were retrospective analyzed. A total of 19 patients were enrolled, including 11 males and 8 females. The age of the cohort was 37.4 ± 13.9 years (range 13 - 69 years). Visual analogue scale (VAS) and Japanese Orthopaedic Association (JOA) scores were recorded to evaluate the relief of neck pain and the recovery of neurological functions, respectively. The atlantodental interval (ADI), apex distance of odontoid to Chamberlain’s line (DOCL), and cervico-medullary angle (CMA) were measured to evaluate the reduction of AAD and BI. The duration of bony fusion and complications were also recorded and analyzed. Results: The follow-up period was 54.7 ± 29.4 months (range 25 - 131 months). The duration of surgery was 136.1 ± 29.0 mins (range 95-210 mins), and the estimated blood loss was 189.7 ± 85.0 ml (range 100 - 455 ml). For functional scores, the VAS was 6.06 ± 1.21 pre-operation, 2.35 ± 0.76 post-operation, and 1.12 ± 0.90 at the latest follow-up (F = 97.59, p < 0.001). The JOA was 9.26 ± 2.24 pre-operation, 14.05 ± 2.01 post-operation, and 15.16 ± 1.42 at the latest follow-up (F = 41.27, p < 0.001). Regarding the dislocation, the ADI was 9.63 ± 1.93 mm pre-operation, 1.21 ± 1.10 mm post-operation, and 1.26 ± 1.02 mm at the latest follow-up (F = 174.88, p < 0.001). The DOCL was 11.47 ± 3.93 mm pre-operation, 2.53 ± 3.30 mm post-operation, and 2.26 ± 2.73 mm at the latest follow-up (F = 33.97, p < 0.001). The CMA was 114.31 ± 11.00° pre-operation, 144.16 ± 9.33° post-operation, and 143.42 ± 9.12° at the latest follow-up (F = 41.05, p < 0.001). Bony fusion was achieved in all patients, the fusion time was 10.3 ± 2.7 months (range 5 - 15 months). Of these patients, one developed wound infection and one developed cerebrospinal fluid leakage. The two patients were cured through corresponding management. No patient developed implant failure or re-dislocation. Conclusion: Posterior approach release and reduction followed by intra-articular interbody fusion cage implantation is a safe and efficient surgical strategy for the treatment of BI-irAAD.
1826
P057: Association between the severity of cervical spinal stenosis and paraspinal muscle parameters in patients undergoing anterior cervical discectomy and fusion
Thomas Caffard 1,2 , Artine Arzani 1 , Bruno Verna 1 , Vidushi Tripathi 1 , Erika Chiapparelli 1 , Samuel Medina 1 , Lukas Schönnagel 1,3 , Soji Tani 1 , Gaston Camino-Willhuber 1 , Ali Guven 1 , Krizia Amoroso 1 , Jiaqi Zhu 4 , Ek Tsoon Tan 5 , John Carrino 5 , Jennifer Shue 1 , Michael Kelly 4 , Marco Burkhard 1 , Hassan Malik 2 , Timo Zippelius 2 , David Dalton 1 , Andrew Sama 1 , Federico Girardi 1 , Frank Cammisa 1 , Alexander Hughes 1
1 Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, USA
2 Klinik Für Orthopädie, Universitätsklinikum Ulm, Ulm, Germany
3 Charité-Universitätsmedizin Berlin, Berlin, Germany
4 Biostatistics Core
5 Department of Radiology and Imaging, Hospital for Special Surgery, New York, USA
Introduction: Cervical central stenosis (CCS), resulting from degenerative changes leading to spinal cord compression, causes degenerative cervical myelopathy (DCM) which can result in sensory and motor dysfunction. Although recent studies have correlated DCM with atrophy of the cervical paraspinal muscles, the relation between CCS and cervical muscle quality remains underexplored. Therefore, we aimed to evaluate the association between CCS severity and fatty infiltration of the cervical multifidus and rotator muscles (CMR) across all subaxial levels in patients undergoing anterior cervical discectomy and fusion (ACDF). Material and Methods: Patients with preoperative cervical magnetic resonance imaging (MRI) who underwent ACDF between 2015 and 2018 were included. CMR were segmented on axial T2-weighted MRI scans at the C3 to C7 mid-vertebral levels. Percent fatty infiltration (FI) was calculated using a custom software. The severity of the CCS at each subaxial level was assessed using a previously published classification. Grade 3, representing a loss of cerebrospinal fluid space and deformation of the spinal cord > 25% was defined as significant spinal cord compression. Multivariable linear regression analyses were conducted and adjusted for age, sex, and body mass index. Results: 156 consecutive patients (37.2% females) with a mean age of 55.1 years were included in the analyses. After adjustment for cofounders, spinal cord compression at the C3-C4 and C4-C5 levels was significantly associated with the FI of the CMR from C3 to C6 and C5 to C7, respectively. Spinal cord compression at the C5/6 and C6/7 levels were also significant predictors of FI of the CMR at the C7 level. Conclusion: Our results demonstrated significant correlations between the severity of CCS and FI of the CMR. Moreover, significant level-specific correlations were found. A significant increase in FI of the CMR at the levels below the stenosis was observed in patients presenting with spinal cord compression. Given the segmental innervation of the CMR, increased FI might be attributed to neurogenic atrophy.
1831
P058: Dropped head syndrome: example of a three-stage surgery
Tuong Lu 1 , Leroy Henri Arthur 1 , Richard Assaker 1
1 CHU de Lille, Neurosurgery, Lille, France
Introduction: Cervical spine scoliosis is a rare pathology, and surgical treatment is often complex and carries a high risk of complications. There is currently no consensus on the best management strategy. Material and Methods: We present a clinical case report of a 57-year-old female patient with a two-year history of depression and nocturnal sleep in a seated position with her head in flexion. The patient gradually developed cervical deformity with kyphosis centered on C5 in the sagittal plane and with right-sided convexity in the coronal plane, partially reducible on dynamic radiographs. There was no focal neurological deficit or pain, but there was alteration of the horizontal gaze and quality of life. The patient underwent three-stage surgery under EMG monitoring, including:
- posterior laminectomy from C3 to C6 with piezoelectric scalpel and Smith-Peterson osteotomies, placement of screws in the lateral masses of C2 and C3 and pedicles of T1 to T4 under neuronavigation
- anterior triple discectomies from C4 to C7
- posterior placement of rods and autologous bone grafts.
Results: Follow-up at 2 years revealed no sensory-motor deficit, natural posture and head position, and restored horizontal gaze and quality of life. Conclusion: Cervical scoliosis surgery can be performed with either anterior, posterior, or combined approaches, and techniques range from simple posterior osteotomy to corporectomy. Various instrumentation is available for correction, stabilization, and arthrodesis, including anterior cervical plate, cage, screws, hooks, and rods. Here we report a severe cervical deformity managed surgically with low grade osteotomies.
Deformity-thoracolumbar (Adolescent)
32
P059: Vertebral body tethering and postoperative thoracic kyphosis in adolescent idiopathic scoliosis patients: preliminary long-term results and a comparison to posterior spinal fusion
Sebastian Siller 1 , Libby Gooda 1 , Timothy Bishop 1 , Jason Bernard 1 , Darren Lui 1
1 Department of Trauma and Orthopaedics, St. George's University Hospitals NHS Foundation Trust, London, United Kingdom
Introduction: Vertebral body tethering (VBT) is a novel alternative to posterior spinal fusion (PSF) surgery to treat skeletally immature patients with adolescent idiopathic scoliosis (AIS) and data on long-term outcome is still scarce. We aimed to evaluate the long-term outcome of VBT with regard to thoracic kyphosis and compare to a historical control group with PSF. Material and Methods: We reviewed surgical results and radiographic measurements of 20 VBT patients who were prospectively enrolled between 2014 and 2016 and long-term followed up (mean 63 ± 16 months post surgery) at our NHS university center. Data of a historical control group with PSF were used for comparison. Thoracic kyphosis was assessed with the Cobb angle at T4-T12. Results: There were no significant differences in terms of distribution of Lenke curve types (most often type 1), median age (14 vs 14 years) and gender distribution (f:m = 19:1 vs. 7:1) in our 20 VBT and 35 PSF patients; median preoperative Cobb angle of the major curve was 51 degree in the VBT and 64 degree in the PSF group. Number of surgical levels, operative time and blood loss were lower in the VBT group (median 8 vs. 12, p < 0.001, mean 199 vs. 292 minutes, p < 0.001; mean 400 vs. 550 ml, p = 0.001, respectively). In the VBT group, mean thoracic kyphosis was 22 degree preoperatively, 29 degree postoperatively and 27 degree at long-term follow-up, while it was 34 degree preoperatively and 24 degree at last follow-up in the PSF group. At last follow-up, mean change of thoracic kyphosis was +6 degree in the VBT group and, therefore, significantly differed from the change of kyphosis in the PSF group (-10 degree, p = 0.006). Conclusion: While PSF might have a tendency to produce a flatter thoracic sagittal alignment, VBT seems to be able to better preserve the thoracic kyphosis in the long-term outcome.
62
P060: Propofol sensitivity alone can cause alert level loss of TcMEP during corrective surgery for adolescent idiopathic scoliosis
Matthew Geck 1 , Devender Singh 1 , Brian Kaufman 1 , Ryan Murdock 1 , Ashley Duncan 1 , John Stokes 1 , Eeric Truumees 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
Introduction: Use of Transcranial motor evoked potential (TcMEP) in Adolescent Idiopathic Scoliosis (AIS) surgeries poses challenges. This study aims to investigate the safety and efficacy of a TcMEP protocol incorporating maintenance of MAP over 65 and HCT > 25; delaying incision until first TcMEP obtained, and progressive dosing of propofol. Materials and Methods: From 2009-2022, consecutive AIS patients undergoing deformity corrections using a TcMEP protocol were studied. Inclusion criteria: age (11-49 years), and ≥ 5 spinal fusion levels. Exclusion criteria: previous surgery, fusion to the pelvis, neurogenic scoliosis, and other deformity related diagnoses. Results: 510 patients met inclusion criteria with mean age 15.4 (±3.5) years. 86% were female. Mean spinal levels treated and OR time were 9.6 (±3.3) and 346.2 (±89.4) min, respectively. There were 21 TcMEP alerts (4.1%). Of these, 3 were hypotension related, 9 occurred during deformity correction, 7 were Propofol dose related and 2 indeterminate. None were related to screw placement. In 4 manipulation related alerts, any rod-based deformity correction triggered an alert, leading to placement of in situ contoured rods. These patients were staged, and successful correction achieved 3 weeks later. In all 7 of the Propofol dose related alerts, there were no concurrent confounding factors. Initiation, but not completion, of a wake-up test resolved the alert. Propofol was restarted at a lower dose. No post-op neurologic deficits were encountered. None of our patients reported intra-operative awareness. Conclusion: For reliable TcMEP monitoring during AIS surgery, our protocol incorporated hemodynamic support, no incision until TcMEPs achieved, and progressive Propofol titration. Successful monitoring was achieved in all 510 patients. There were no post-op neurologic deficits or episodes of intro-operative awareness. Of the 21 TcMEP alerts, in 7 cases, Propofol dose reduction leads to restoration of baseline potentials. Propofol was determined to be the sole cause of TcMEP loss, and initiation of the Wake-Up test but not completion, with lightening of the propofol dose, resolved the issue.
63
P061: Prospective analysis of tissue injury markers and radiographic comparisons after mini vs. open deformity corrections in adolescent idiopathic scoliosis patients
Matthew Geck 1 , Devender Singh 1 , Ashley Duncan 1 , John Stokes 1 , Eeric Truumees 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
Introduction: When compared to traditional open surgery, MIS technique may significantly reduce tissue injury reactions post-operatively. This study sought to compare the impact of minimally invasive surgery (MIS) and open complex spinal deformity corrections on the paraspinal musculature and soft tissues in adolescent idiopathic scoliosis (AIS) patients through analysis of early post-operative serum tissue injury markers and later radiographic evidence of muscle atrophy and within the paraspinal musculature at 1-year post-operative (postop) follow up. Materials and Methods: Data were collected at a single tertiary care center from 1st, January 2015 to 30th, November 2020. If a patient met the criteria for the study, the surgeon assigned the patient to either open or MIS cohort based on patient preference. Demographic, clinical, laboratory, and radiographic data, including post-operative MRIs, were collected at various intervals. Descriptive and inferential analyses was conducted. Results: 37 patients met the inclusion criteria. Mean patient age for the MIS and open groups were 16.6 years (±3years) and 15.8 years (±3.5 years), respectively. There was a significant difference between the groups with respect to mean estimated blood loss (MIS vs. open: 143.3 ± 104.4 ml. vs. 408.1 ±2 90.2 ml, p < 0.05). Mean operative time was significantly greater for the MIS cases as compared to their counterparts (349.5 ± 32.7 min vs. 318 ± 31.2 min, p < 0.05). On postop day 1, the open group had significantly higher serum aldolase concentrations than MIS group (18.2 ± 7.6 mU/mL vs. 12.9 ± 4.2 mU/mL, p < 0.05). Relatively higher values were also seen on days 2-4. On postop day 1, the mean CK value was significantly greater in the open group than their counterpart (3003.1 ± 60.1IU/L vs. 1649.4 ± 40.6IU/L, p < 0.05). These differences remained significant on postop days 2, 3 and 4 (p < 0.05). Eventually, both markers returned to the baseline values in both groups. Radiographically, the normalized difference (preop vs. postop) in the loss of paraspinal muscle mass was comparatively higher in the open group as compared to MIS (14.1% vs. 9.1%, respectively). Patient reported outcomes improved significantly in both the groups (preop vs. 24 months), but there were no significant differences between the groups. Both the groups reported similar complication rates. Conclusions: In patients with AIS, MIS is associated with decreased tissue injury markers and muscle atrophy than open surgical correction in the early post-operative period. While this difference may be associated with decreased blood loss and shorter hospital stays seen in MIS, it did not result in a significant difference in the clinical outcome when compared to open surgery for AIS.
64
P062: Comparative radiographic and clinical outcome analysis of custom vs. surgeon contoured rods for adult deformity correction at six months postoperative
Matthew Geck 1 , Devender Singh 1 , Ashley Duncan 1 , John Stokes 1 , Eeric Truumees 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
Introduction: We compared clinical and radiographic outcomes between matched cohorts of adult deformity patients with custom rods and surgeon contoured rods. Our hypothesis was that custom manufactured rods provide superior clinical and radiographic outcomes than surgeon contoured rods for adult deformity correction. Materials and Methods: Two cohorts of adult deformity patients undergoing surgical correction were created: standard rods that were hand bent intraoperatively vs. patient specific custom rods. The cohorts were matched based on number of levels treated, fusion to pelvis, age, and ASA score. Radiographic and clinical outcomes were compared preoperatively and at 6-months postoperatively. Results: 18 patients, 94.4% female, were included in the custom cohort and 22 patients, 100% female, were included in the surgeon contoured cohort. There were no significant differences between the two cohorts in terms of mean age, body mass index, and number of levels treated. Mean estimated blood loss (EBL) and operative time (OR) were significantly higher in the custom cohort (EBL: 1444 ± 757 mls, OR: 484 ± 68.9 minutes) than their counterpart (EBL: 1121.8 ± 502.2 mls, OR: 438.2 ± 66.6 minutes). Mean time per screw placement was 2.6 minutes per screw (range: 1.73-3.6 minutes) for the custom and 2.8 minutes per screw (range:1.94-4.1 minutes) for the other group. At 6 months postoperative, custom cohort demonstrated higher mean % correction in Cobb angle (custom manufactured vs. surgeon contoured: 77.4% vs. 74.3%). Mean %improvement in T1 pelvic angle, PI-LL (PI: pelvic incidence, LL: lumbar lordosis) mismatch and C7 plumb line at 6 months were higher for the custom group than their counterpart. Both groups had similar improvements in PRO scores (custom vs. surgeon contoured: visual analog scale: 46.5% vs. 43.2%; oswestry disability index: 61.6% vs. 60.4%; scoliosis research society-22r 22r: 59.8% vs. 57.6%). Postoperative complications were also similar between the two cohorts. Conclusion: Patients who had deformity correction using adaptive spine intelligence generated custom rods demonstrated better % correction and less screw time but similar PRO scores and complication rates as those patients who had standard rods. There was a significant increase in EBL and OR time in the custom manufactured cohort. These cohorts will continue to be followed for long-term analysis.
220
P063: Back pain in ankylosing 6
Mohamed Malabari 1
1 Orthopedic, Saudi German Hospital Jeddah, Jeddah, Saudi Arabia
Introduction: Sever back pain not resolved with basic medication analgesia and physiotherapy with abnormal signal radiological finding missed by many doctor. Results in diagnosis of ankylosing spondylitis. Material and Methods: Case series. Through clinic visiting. Results: Early diagnosis of ankylosing spondylitis. Proper reading of the x ray. X ray appearance of ankylosing spondylitis spine. Conclusion: Ankylosing spondylitis become common. Not specific to nationality. Radiological changes early appear in the thoracic region.
239
P064: Comparison of disc and facet degeneration and quality of life in stopping fusion al L3 versus L4 in AIS: An MRI study with mean 17 (15-21) years follow up
Hamisi Mraja 1 , Ayhan Mutlu 1 , Onur Levent Ulusoy 1 , Cem Sever 1 , Baris Peker 1 , Enas Daadour 1 , Tunay Sanli 1 , Selhan Karadereler 1 , Meric Enercan 1 , Azmi Hamzaoglu 1
1 Orthopedics and Traumatology, Scoliosis-Spine Center Istanbul, İstanbul, Turkey
Introduction: Selection of lowest instrumented vertebra (LIV) is often difficult when lumbar curve was included into the fusion (L3 vs L4). Saving L4 is believed to be beneficial for preserving motion and preventing degeneration of unfused lumbar spine. The aim of the study was to evaluate the disc degeneration (DD) and facet joint degeneration (FJD) of the caudal mobile lumbar spine and assess the clinical outcomes after min 15 years follow up and compare these results with healthy controls. Material and Methods: AIS patients treated with long posterior fusion (LIV; L3 and L4) having min 15 years f/up were included. Preop, postop, and final f/up radiographs were reviewed. All f/up lumbar MRIs were evaluated by two radiologists independently, and classified for each patient in terms of DD according to Phirmann classification and FJD Fujiwara classification. Clinical evaluation was done by using SRS22r and Numerical Rating Scale (NRS). Results: L3 group included 17 patients (14F, 3M) with mean age 31 (26-39). L4 group included 12 patients (8F,4M) with mean age 33 (28-39). Control group included (20F, 7M) age and gender-matched healthy individuals with no spinal deformities [mean age 33 (26-39)]. Mean f/up was 17.4 (15-21) years. Mean correction rates for lumbar curve were 78% in L3 and 79% in L4 group, with no significant correction loss at f/up. In terms of DD of L3 and control groups demonstrated similar and less degeneration rates than L4 group but this difference was not statistically significant. However, FJD was significantly greater in both L3 and L4 groups when compared to the controls. The grade of FJD was significantly higher in L4 than L3 group at the LIV+1 level (x2:8, 575; p < 0.05). SRS-22r and NRS scores were similar for all groups. Conclusion: AIS patients who underwent long fusion down to L4 demonstrated higher grades of disc degeneration than L3 and control groups but this was not statistically significant. L3 and L4 group showed greater FJD when compared to healthy controls. L4 group showed significantly greater facet joint degeneration at LIV+1 than when compared to L3 group. Despite the degenerative findings, clinical outcome scores were similar for all groups at a minimum 15 years follow-up.
242
P065: Core muscle strengths, lumbar flexibility and quality of life in AIS patients treated with either long fusion or hybrid technique compared to healthy individuals
Celaleddin Bildik 1 , Selmin Arsoy 1 , Selen Saygili 1 , Hamisi Mraja 1 , Cem Sever 1 , Tunay Sanli 1 , Enas Daadour 1 , Selhan Karadereler 1 , Meric Enercan 1 , Azmi Hamzaoglu 1
1 Orthopedics and Traumatology, Scoliosis-Spine Center Istanbul, İstanbul, Turkey
Introduction: We introduced a Hybrid technique including posterior pedicle screw fixation fusion for the thoracic curve and vertebral body tethering (VBT) for the thoracolumbar/lumbar (TL/L) curve in order to preserve lumbar flexibility and motion for the surgical treatment of AIS with double major curves. Unfortunately, there is very limited objective data showing the advantages of TL/L VBT technique over the posterior long fusions. The aim of this study was to compare the functional results in terms of lumbar core muscle strengths, lumbar flexibility, and HRQoL in AIS patients with double major curves treated with either long fusion or hybrid technique and compare these results with healthy individuals. Material and Methods: 30 patients treated with the Hybrid technique (Hybrid Group) and 36 patients treated with posterior long fusion stopped at L3 or L4 (Fusion Group) were included. The control group (Control Group) included age and gender matched 30 healthy individuals. Lumbar core muscle strengths were evaluated with an endurance test using a computer assisted 3D spatial rotation device. Schober test and lumbar ROM measurements were done by two physical therapists. SRS22r scores were used for clinical assessment. Results: The mean f/up was 3.7 years in the Hybrid Group and 13.6 years in the Fusion Group. According to the Schober test both the Hybrid Group and Fusion Group showed decreased flexibility compared to the Control Group (p < 0.05; U1 = 179 and U2 = 28), but the Fusion Group showed similar ROM values whereas the Fusion Group showed significant limitation (p < 0.05). Posterior Lumbar core muscle strengths were similar in the Hybrid Group and Control Group (p > 0.05) but significantly lower in the Fusion Group (p < 0.05; U1 = 201 and U2 = 369). SRS22r functions were significantly higher in the Hybrid Group and Control Group than the Fusion Group (p < 0.05; U1 = 296 and U2 = 190). Total SRS22r did not show any difference between groups. Conclusion: The hybrid technique showed similar lumbar core muscle strengths and lumbar ROM values in healthy individuals. Although the lumbar flexibility of the Hybrid Group was significantly higher than the Fusion Group, it was lower than the Control Group. SRS22r function was higher and similar in the Hybrid Group and Control Group, but there was no difference in the total SRS22r between groups.
243
P066: Core muscle strengths, lumbar flexibility and quality of life in Lenke Type 5 AIS patients treated with either Cobb to Cobb VBT versus fusion compared with healthy individuals
Celaleddin Bildik 1 , Selen Saygili 1 , Selmin Arsoy 1 , Hamisi Mraja 1 , Cem Sever 1 , Enas Daadour 1 , Tunay Sanli 1 , Selhan Karadereler 1 , Meric Enercan 1 , Azmi Hamzaoglu 1
1 Orthopedics and Traumatology, Scoliosis-Spine Center Istanbul, İstanbul, Turkey
Introduction: Cobb to Cobb posterior fusion is accepted as standard treatment for Lenke 5 curves. Recently vertebral body tethering (VBT) gained popularity as a non-fusion surgical alternative for these curves. Unfortunately there are no available objective data showing the superiority of VBT over post fusion. The aim of this study was to assess lumbar core muscle strengths (LCMS); flexibility and quality of life measures in Lenke 5 AIS patients treated with either VBT or post fusion between Cobb levels, and compare these results with healthy individuals. Material and Methods: 16 patients treated with VBT technique (VBT Group) and 26 patients treated with fusion (Fusion Group) were included. The control group (Control Group) included age and gender-matched 30 healthy individuals. LCMS were evaluated with endurance test using computer assisted 3D spatial rotation device (SRD). Schober test and lumbar ROM measurements were done by two experienced physical therapists. SRS22r scores were used for clinical assessment. Results: Mean follow up was 4,2 years in VBT Group and 9.9 years in Fusion Group. According to Schober test, lumbar flexibility of VBT Group was significantly higher than Fusion Group (p < 0.05; U = 25), but lower than Control Group (p > 0.05). In terms of lumbar ROM assessment including forward bending, lateral bending and rotation towards both sides, VBT Group and Control Group showed similar ROM values whereas Fusion Group showed significant limitation (p < 0.05). Posterior LCMS were similar in VBT Group and Control Group (p > 0.05), but significantly lower in Fusion Group (p < 0.05; U = 20). SRS22r function were significantly higher in VBT Group and Control Group than Fusion Group (p < 0.05; U = 8.0). Total SRS22r scores did not show any difference between groups. Conclusion: Cobb to Cobb VBT technique which preserves the posterior muscle structures showed similar lumbar core muscle strengths and lumbar ROM values with healthy individuals. Although the lumbar flexibility of the VBT group was significantly higher than the fusion group, it was lower than the control group. SRS22r function in the VBT group was higher than the fusion group, but there was no difference in total SRS22r scores between all groups.
265
P067: Three-staged correction of severe rigid kypho-scoliosis using halo-femoral or halo-gravity traction after surgical release - A systematic review and meta-analysis
Nigil Palliyil 1 , Jim Vellara 1
1 Orthopaedics (Spine Surgery), Amrita Institute of Medical Sciences, Cochin, India
Introduction: Management of severe rigid kyphoscoliosis is quite challenging despite the availability of advanced spinal instrumentation and osteotomy techniques. The incidence of postoperative neurological complication following complex osteotomies in severe deformity correction is 4.0% - 21.2%. Traction helps in obtaining gradual curve correction, especially when applied after surgical release. Use of traction after a spinal release procedure has not been described frequently in literature. We performed a systematic review on the use of traction after spinal release and prior to definitive scoliosis correction. Material and Methods: The systematic review was conducted as per PRISMA guidelines using the search phrase (Halo-femoral OR Halo-pelvic) AND Traction AND release AND (scoliosis OR kyphosis). Articles published in English between June2000-June2023 were included. Results: 4 articles that met the inclusion criteria were analysed. 168 patients with a mean age of 17.5years with rigid kyphoscoliosis (curve flexibility < 30% on side bending) were included. Mean follow up was 31.6 months (12-96). The aetiological diagnoses for the scoliosis were Idiopathic (43.4%), Congenital (35.2%), Neuromuscular (13%), Syndromic (8.4%). 67 patients underwent posterior release, while the remaining 101patients underwent anterior release followed by traction. Halo-femoral traction was applied in 147 patients while 21 patients had halo-gravity traction. All patients were put on traction immediately after the release. The mean traction weight used was 21.9 kg (49.7% of body weight). The mean traction duration was 17.1 (9-44) days. The mean preoperative cobb angle for the major curve was 101.50 for scoliosis and 76.70 for kyphosis. The overall correction rate achieved following the final posterior fusion was 59% for scoliosis and 46.5% for kyphosis. 48% of the overall curve correction was obtained following release and traction prior to final fusion. The final curve correction rate following anterior release traction and posterior fusion was 60.4% when compared to patients who had posterior release, traction and posterior fusion 55% (p value-0.307). 11.9% of the patients had complications related to traction. The incidence of complications was greater following posterior release and traction (15.9%) when compared to the patients who had anterior release and traction (9.52%). The most encountered complication was brachial plexus palsy (3.6%) followed by transient paraparesis (1.7%); Pleural injury (1.7%); Pin loosening (1.7%). Conclusion: Prior spinal surgical release helps to improve the curve flexibility and increases the efficacy of traction application. This approach helps to obtain satisfactory curve correction without the need for 3 column/complex osteotomies.
Keywords: rigid kypho-scolioisis, halo-femoral traction, halo-gravity traction, anterior release, posterior release
469
P068: Myelopathy associated with rapid progression of a dystrophic NF-1 curve - A case report
Sai Gautham Balasubramanian 1 , Sudarshan Munigangaiah 1
1 Spinal Unit - Trauma & Orthopaedics, AlderHey Children's NHS Foundation Trust, Liverpool, United Kingdom
Introduction: Thoracic myelopathy in NF-1 is most commonly due to intra-spinal neurofibromas / dumb-bell tumors/Intra-canal rib head penetration (RHP) causing cord compression. However, acute thoracic myelopathy due to rapid progression of the kyphoscoliotic curve alone in NF-1 without a significant spinal cord compression has never been reported in literature. This case report discusses our experience with one such patient and we also discuss intra-operative and post-operative challenges encountered with this patient and a rare complication of hemothorax post-operatively. Case Description: A 15 year old male presented to the clinic after being lost to follow-up for 4 years with a rapid acute deterioration of dystrophic curve and no myelopathic symptoms (Scoliosis – 65˚, Kyphosis – 77˚). His subsequent examination in 6 weeks showed acute development of myelopathic gait with right ankle and EHL weakness. He was admitted for halo gravity traction for 6 weeks and a single stage posterior instrumentation with excision of rib heads at the apex was planned. Post-operatively, the patient developed massive left hemothorax and loss of power in both lower limbs at Day 2. He subsequently regained full power and complete resolution of myelopathic symptoms at the end of 9 months follow-up with a satisfactory alignment of spine in the follow-up X-rays. Conclusion: Acute onset of myelopathy is a rare and uncommon finding with a rapid deterioration of dystrophic curve alone without any major spinal cord compromise. Early detection of dysplastic changes with early aggressive surgical management and deformity correction is necessary with dystrophic NF-1 curves to prevent pre-operative and post-operative morbidities.
599
P069: Risks of developing postoperative infection after correction of AIS in patient who are carriers Staphylococcus aureus
Ayrat Syundyukov 1 , Pavel Kornyakov 1 , Elena Preobrazhenskaya 2
1 Pediatric Orthopedic
2 Scientific Department, Federal State Budgetary Institution «Federal Center for Traumatology, Orthopedics and Arthroplasty» of the Ministry of Health of the Russian Federation (Cheboksary), Cheboksary, Russian Federation
Introduction and Objective: Postoperative infection after AIS correction is a very rare complication, but when it develops it becomes a disaster for the patient, doctor and clinic. The most common postoperative wound infection is caused by Staphylococcus aureus (St.aureus). A lot of people are asymptomatic carriers of St.aureus. Carriage of St.aureus contributes to the development of infectious complications after AIS surgery. Aim of study was to evaluate the impact of St.aureus carriage on the development of postoperative infection after AIS correction. Study design: Based on the data of the medical information system for 2017-2021 a retrospective continuous assessment of information about patients (n = 137) operated on for AIS surgery was performed. The results of microbiological examination of patients biomaterial, the number and types of complications were analyzed. The mean age of the patients was 14.8 ± 1.6. Materials and Methods: All patients took a swab from the nose and pharynx for St.aureus on the day of hospitalization, determined the carriage of St.aureus, concentration and sensitivity to antibiotics. A dorsal correction of AIS was performed by one team of surgeons, with standard antibiotic prophylaxis. Surgeons were examined for carriage of St.aureus quarterly. Results: In 57 (41.6%) patients out of 137, microbiological examination revealed the growth of St.aureus: from the nose 20, pharynx 24, nose and pharynx 13. In total we received 1 infectious complication - 0.73% of all patients studied. No infectious complications were detected in the group of patients with a negative result for St.aureus. In the group of patients with a positive test for St.aureus, the percentage of complications was 1.75. A patient with a complication received a positive test for St. aureus from the nose and pharynx, in high concentration, and the same type of pathogen with similar sensitivity to antibiotics was detected in the postoperative wound. Despite the presence of a complication in the group of St.aureus patients, the difference, according to the Fisher test, is considered not statistically significant (p = 0.4161). Conclusions: The risk of developing infectious complications during AIS correction is minimal, including in St.aureus carriers, however, in our opinion, carrying out a carrier test is mandatory in order to alibi the surgical team and the clinic in case of possible legal claims from the patient.
Keywords: AIS, St.aureus, carriage of St.aureus, postoperative infections
624
P070: Deformity correction with single rod technique on concavity side in adolescent idiopathic scoliosis: preliminary results on six cases
Giovanni Ciani 1 , Francesco Vommaro 1 , Chiara Cini 1 , Antonio Parciante 1 , Luca Boriani 1 , Alessandro Gasbarrini 1
1 Spine Surgery, Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Correction of thoracic scoliosis classically involves a selective arthrodesis with the exposure and fusion of concave and convex side of the curve. The correction and arthrodesis of non-severe thoracic scoliosis (lenke 1) only on the side of the concavity of the curve, with the use of pedicle screws and current derotation systems could be an alternative to classic technique, with same capacity of correction and less invasive surgery. Material and Methods: We collected retrospectively 6 cases (4 females 2 males) of AIS Lenke 1 treated with single rod technique on concavity side between February and September 2022. We only performed this technique on Lenke 1 scoliosis with ≤ 70° cobb angle (54-68°), and almost 50% reduction of the cobb angle on bending X-ray. In all cases we use single 6.5 mm Cr-Co rod on concavity side of the curve. Median age was 14 yy (12-16yy). We evaluated the correction rate of the curve, instrumented levels, operative time, intraoperative blood loss, days on ICU, days of stay, postoperative pain as a mean value of NRS score on stay days. We collected any possible intra and postoperative complications. All of patients attempted an outpatient follow-up consisting of clinical and radiological evaluation for at least 1 years (mean follow up 15 months). Results: Mean correction rates of the structural curve were 68% (59-80%) at postop and 64% at last follow up (55-77%). Mean operative time was 146 min (139-158min). Intraoperative blood loss was minimal (180 ml mean value). Mean value of stays was 4 days, and only one patient needed one day on ICU. Mean value of NRS score were 2.1 (1-4). No postoperative complications were recorded at last follow up. No adding on complications or progression of main curves were reported at last follow up. Conclusion: The use of single rod technique could be a safe and capable alternative to standard open approach for Lenke 1 AIS patients with curves ≤ 70°. The are no relevant difference in correction rate of the curve with standard open technique, but single rod technique showed short operative time, minimal intraoperative blood losses and low postop pain. One side posterior fusion of the curve seems to be sufficient to control deformity correction, since no significant radiological or clinical changes were reported at last follow up.
696
P071: Outcomes of surgical intervention for spinal deformities in neurofibromatosis type I: a comprehensive analysis of 48 cases
Olga Sergeenko 1 , Alexandr Burtcev 1 , Alex Evsukov 1
1 Spinal Department, Ilizarov Center, Kurgan, Russian Federation
Goal: This study aims to assess the treatment outcomes of 48 patients with spinal deformities associated with neurofibromatosis type 1 (NF1). The goal is to evaluate the effectiveness of surgical interventions and identify contributing factors for improved patient care. Methods: We will recruit a diverse group of 48 NF1 patients who have undergone surgical treatment for spinal deformities. Comprehensive data will be collected, including patient demographics, NF1-specific information, spinal deformity details, complications, and comorbidities. A standardized follow-up period will monitor spinal correction, complications, and patient-reported outcomes. Complications will be classified, and the long-term sustainability of deformity correction and patient well-being will be assessed. Results: Among the cohort of 48 patients diagnosed with NF 1, the gender distribution consisted of 28 females and 20 males. The onset of spinal deformities typically manifested at an average age of 8 years, spanning a wide range from 2 months to 56 years. Predominantly, these deformities presented as kyphoscoliosis in 19 cases and scoliosis in 22 cases. Two patients experienced non-traumatic vertebral dislocations. The investigation uncovered several distinctive anatomical features associated with the development of spinal deformities in NF 1 patients, including vertebral dystrophy with concurrent dural ectasia (35 cases), wedge-shaped apical vertebra (25 cases), vertebral spondylolisthesis or dislocation (8 cases), intracanal rib head dislocation (9 cases), and primary upper thoracic curvature (15 cases). Notably, 8 cases exhibited concomitant paravertebral plexiform neurofibromas, and two patients had intracanal small neuromas. Prior to undergoing surgery, 5 cases displayed mild chronic paresis in the arms and/or legs, three individuals presented with subacute lower paraplegia, one patient experienced urinary incontinence due to tumors affecting the sacral roots, and one patient had a slowly progressive tetraplegia. The median age at the time of surgery was 13.6 years, ranging from 4 to 56 years old. The primary surgical approaches employed included one-time correction with posterior screw fixation without vertebrotomy (26 cases), one-time correction with posterior screw fixation involving vertebrotomy (10 cases), and the implantation of growth-friendly constructs (12 cases). Short-term complications included 2 cases of tense hemothorax, 2 cases of persistent neurological deterioration, and 1 case of wound cerebrospinal fluid (CSF) leakage. The most prevalent long-term complications consisted of rod fractures (5 cases), upper screw loosening (4 cases), and deformity progression (7 cases). The median follow-up duration extended to 6 years, ranging from 0.6 to 13 years. In three cases, gradual neurological improvement was observed during the follow-up period, while in the remaining cases, the patients' conditions remained stable. Notably, 5 patients experienced significant chronic back pain. Conclusions: In conclusion, this study examined the treatment outcomes of 48 patients with spinal deformities associated with neurofibromatosis type 1 (NF1). The study identified various anatomical features contributing to these deformities and assessed the surgical approaches used, highlighting short-term and long-term complications. The median follow-up period revealed variability in patient outcomes, including neurological improvement and chronic back pain. Overall, this research underscores the complexity of managing NF1-related spinal deformities and the need for ongoing investigation to enhance patient care.
857
P072: Correction of congenital kyphoscoliosis by combination of different types of spinal osteotomies and cantilever or rod derotation technique
Anowarul Islam 1 , Suvradev Saha 1
1 Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Introduction: Congenital kypho-Scoliosis is a three-dimensional deformity recognized with lateral curvature with coronal tilt of the spine as well as axial vertebral rotation. Surgical interventions are recommended when patients with Scoliosis have severe/ progressive curvature (Cobb’s angle > 45°). Spinal flexibility is one of important parameters for surgeons to plan surgical treatment but here it is rigid curvature. So, spinal osteotomy with posterior instrumentation and combined cantilever, rod derotation technique are often needed for the triplannar correction of this deformity. Material and Methods: This prospective study was conducted from July 2015 to June 2023. A total number of 30 patients with Adolescent idiopathic scoliosis evaluated by X-ray(Scoliogram), MRI & CT- Scan was selected for the study who were non-responsive to conservative treatment. Clinical outcomes was assessed by using Scoliosis Research Society-22 and spinal appearance questionnaires, pain control was assessed by VAS Score. All the patientswere followed up at 1 month, 6 months, 12 months, 24 months and 36 months with a structured case record form. Results: Onset of the disease between 10 years of birth. Average age was 13.69 ± 02.06 when operated. Most of the patients were female. Most of the patients has Mid thoracic curve (12) and then thoracolumbar (10). Proximal thoracic (8) has the least number of involvement. Post-operatively VAS score was decreased significantly after 36 months of follow up (1.92 ± 0.48) compared to pre-operative status (p value < 0.001). Pre-operative & post-operative mean scoliosis correction, which was 73.3% in thoracic and 86.7% in lumbar spine. Overall mean scoliosis correction was statistically significant (p value < 0.001). Overall mean kyphosis correction was 25.46° ± 1.71° which was also statistically significant (p value < 0.001). Preoperative SRS-22 score has been improved significantly after 36 month of operation (p value < 0.001). Conclusion: This study shows, spinal osteotomy with posterior instrumentation and combined cantilever, rod derotation technique is a effective and safe surgical choice with excellent functional, clinical, radiological and cosmetic recovery with minimum perioperative complications.
999
P073: Progression of curve in patients with adolescent idiopathic scoliosis greater than 50 degrees after skeletal maturity: over 5-year follow-up
Yunjin Nam 1 , Jungwook Lim 1 , Sangmin Lee 1 , Young Bin Lee 1 , Seung Woo Suh 1
1 Department of Orthopaedics, Korea University Guro Hospital, Seoul, South Korea
Introduction: Surgical treatment is recommended if curvature is larger than 50 degrees even after skeletal maturity in adolescent idiopathic scoliosis (AIS). However, few articles have reported on progression rate or risk factors for progression of curve greater than 50 degrees in patients with AIS after skeletal maturation. Material and Methods: The inclusion criteria were as follows: (1) skeletally matured (Risser 4 or 5) patients with AIS, (2) curve greater than 50 degrees; followed up more than 5 years. Sex, age, magnitude of curve, location of apex, Risser stage, height and weight were measured at initial period and end of follow-up. More than 5 degrees of progression in curve was defined as significant curve progression. Results: A total of 79 curves were observed in 72 patients. Mean follow-up period was 79 months. The mean age was 15.2 and 23.3 years at initial and the end of follow-up. The mean magnitude of curve was 54.3 and 58.6 degrees at initial and the final follow-up. The mean change in curve was 4.1 degree and the annual change was 0.63 degrees. Significant curve progression was observed in 35 cases (44.3%). In cases with a significant curve progression, the mean change in curve was 9.6 degrees, and the annual change was 1.1 degrees. Thoracic curve and Risser stage 4 showed more curve progression, but there was no statistical difference. Conclusion: In patients with AIS whose curve is greater than 50 degrees, significant curve progression was observed at 44.3% even after skeletal maturation. The progression of curve averaged 1.1 degrees per year, and no distinct risk factors for curvature progression were identified.
1020
P074: Anterior approach to scoliosis - Reacquainting forgotten skill
Mukhesh Thangavel 1 , Charanjit Singh Dhillon 1
1 Spine Surgery, MIOT Internation Hospital, Chennai, India
Introduction: Scoliosis is a complex three-dimensional spinal deformity that often requires surgical intervention in cases where patients experience severe pain, curve progression, or progressive disability. The conventional approach to operative treatment has typically involved extensive posterior stabilization. However, in specific situations, anterior-only and combined approaches can play a valuable role in addressing this condition. Material and Methods: We had treated 241 patients for scoliosis. Of them 10 were addressed with anterior only approach, 53 with combined and 178 with all posterior approach. Results: Anterior-only approaches offer several advantages in the treatment of scoliosis, including superior corrective ability and a higher fusion rate, while requiring fewer motion segments to be involved in the instrumented construct. Additionally, these approaches inherently protect the posterior paraspinal musculature from denervation, which is a desirable outcome. We have had a rewarding experience with anterior only approach to adolescent idiopathic scoliosis. Nonetheless, it is important to acknowledge some disadvantages associated with anterior-only approaches, such as potential pulmonary complications resulting from thoracic cavity violation and the occurrence of chronic pain after thoracotomy. Furthermore, when anterior approaches combined with posterior helped us address rigid curves, tether and reduce fusion segments. Conclusion: Leveraging the enhanced corrective ability and biomechanical advantages offered by the anterior column can significantly contribute to the treatment of scoliosis. While the indications for anterior strategies in scoliosis remain limited, it is crucial to consider such operations in suitable scenarios when addressing spinal deformity.
1261
P075: Hope for the hunched: scoliosis surgery & embracing a brighter future
Shah Alam 1 , Sarwar Jahan 2
1 Orthopedics & Spine Surgery, Bangladesh Spine & Orthopedic Hospital (BSOH), Dhaka, Bangladesh
2 Orthopedics & Spine Surgery, National Institute of Traumatology & Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
Introduction: A significant number of Scoliosis needs surgical intervention. Revolutionary design & capability of spinal instruments have drastically changed the principle of scoliosis correction. Material and Methods: From February 2009-June 2023, 168 cases underwent surgery. 98 female and 70 male, age ranged 14-38 years. The pedicle is a power nucleus of the vertebra and offers a secure grip of all 3 columns. Pedicle screw instrumentation ensures rigid fixation with improved 3D correction. Accurate placement of screws is important to reduce possible irreversible complication. All cases were corrected by transpedicular screws and rods. 159 cases were managed by only posterior approach and 9 cases required both anterior releases, costoplasty, posterior stabilization as well. Fusion was done in selected segments. Total follow up time was about 10 years (6 months-7 yrs). All patients were assessed by deformity correction, cosmesis, and functional outcome. Use of Neuromonitor is an excellent & effective method for prevention of post operative neuro deficit. Results: 75% patients had average coronal plane cobb’s angle measuring about 700 pre-operatively and 17.120 immediate post-operative period. 8 patients developed neurodeficit. 3 regained completely but other regaining her neurological deficit very slowly. There were malposition of screws in 13.04%, painful prominence of screws in 10.56%, superficial infection in 4.35%. 80 % patients improved cosmetically. Conclusion: Overall outcome in surgical treatment of Scoliosis by transpedicular screws and rods system was satisfactory.
1275
P076: Changing trend in surgical management of pediatric scoliosis in low-and middle-income (LMIC): 15 years’ experience
Rajesh Kumar Chaudhary 1 , Deepak Kaucha 1 , Ram Barakoti 1 , Babu Shrestha 1
1 Orthopedics, Hospital and Rehabilitation Center for Disabled Children (HRDC), Banepa, Nepal
Introduction: Scoliosis is common cause of spinal deformity in children. There are different options of management available but patients may not be receiving proper treatment because of lack of resources, technologies, expertise, affordability etc. in low- and middle-income countries (LMIC) like Nepal. Despite several challenges, scoliosis surgery is being conducted for several years and all the effort is made to catch up with the recent advances. We want to share our 15 years’ experience in the surgical management of such deformities and study the change in trends. Materials and Method: This is a retrospective study conducted in Hospital and Rehabilitation Center for Disabled Children (HRDC). All the cases of pediatric scoliosis operated in HRDC from January 2008 to December 2022 were included. The data was collected from electronic medical record. Since HRDC is the only center in Nepal which is treating pediatric spinal deformities since 1985 and surgery is regularly being performed since 2008, it represents the changing trend and current situation of such treatment in LMIC like Nepal. The data collected were age, gender, etiology, surgical approach, procedure performed and technological advances. Based on this data, changing trends regarding the surgical approaches and surgical procedures were analyzed. Results: 725 cases were managed in HRDC during this period which includes 635 (87.8%) cases scoliosis of various etiologies. 395 (62.2%) cases were managed conservatively and 240 (37.8%) surgically. Average age of the children at the time of surgery was 12.3 years (range 4-18 years). 52% were male and 48% female. Among operated cases, 47% were idiopathic, 36% congenital and 17% neuromuscular or syndromic. Surgical procedures performed were deformity correction posterior instrumentation with or without osteotomies in 127 cases (52.91%) hemiepiphysiodesis in 28 (11.66%), hemivertebra excision and posterior instrumentation in 16 cases (6.66%%), growing rod application in 8 cases (3.33%%) and thoracotomy in 25 cases (10.41%%). Only anterior approach was performed till 2014, combined staged anterior and posterior approach was performed till 2012. Posterior approach is the main preferred approach since 2014. Hemiepiphysiodesis for early onset scoliosis (EOS) was performed via anterior approach till 2014. Hemivertebra excision and posterior instrumentation via posterior approach is being performed regularly since 2016. Traditional growing rod application for EOS has been regularly performed since 2017. Intraoperative neuromonitoring has been added as the new armamentarium for safe sine surgery since 2021 and is being used in all cases of deformity correction. 30 revision surgeries were performed during this period for various post-operative complications. Conclusion: Idiopathic scoliosis remains the common among various etiologies who were managed surgically. Surgical approach has been shifted from anterior or combined to posterior only since 2014. Non fusion surgery using traditional growing rod is being performed since 2017 for early onset scoliosis (EOS) and hemivertebra excision with limited level fusion has been performed since 2016 instead of fusion surgeries in EOS. Intraoperative neuromonitoring has been used in every case since 2021 for safe spine surgery.
1279
P077: Is a four-month radiographic follow-up sufficient to assess spinal balance after adolescent idiopathic scoliosis correction?
Elie Saghbiny 1 , Adnan Alkandari 1 , Raphael Vialle 1
1 Pediatric Orthopaedics, University Institute for Spine Surgery, Sorbonne University, Paris, France
Introduction: The primary objective of spinal fusion procedures in adolescent idiopathic scoliosis (AIS) patients is to obtain a harmoniously fused spine. Intraoperative radiographs are typically done for accurate placement of pedicular screws assessment. Early postoperative bi-planar low-dose standing radiographs may also be routinely done to confirm the correct screw placement. Due to postoperative pain and muscular contractures, early radiographic assessment does not provide comprehensive insight on trunk balance. This study aims to investigate the relevance of performing postoperative radiographs at four months, given that achieving optimal spinal balance often extends beyond the first year following surgery. Material and Methods: We conducted a retrospective analysis of a monocentric cohort of 37 consecutive adolescent idiopathic scoliosis patients operated on by a single operator (RV). All patients had the same all-screw construct following the same validated preoperative planning method. All standing X-rays were done using biplanar low-dose imaging. X-rays were done pre-operatively, immediate post-operative (Day 4), at four months, and one year post-operatively. The radiological parameters measured were frontal cobb angle, CVA (Horizontal distance between the center of C7 and a vertical line through the middle of S1), L1–L5 lumbar lordosis angle, T1–T12 thoracic kyphosis and T1 obliquity. Results: T1 obliquity exhibited a significant reduction from 2.04° to 1.22° at the four-month control (p = 0.01), further decreasing to 0.81° at the one-year control (p = 0.02). Concurrently, the CVA demonstrated a substantial decrease from 14.41 mm in the immediate post-operative X-ray to 8.01 mm at the four-month control (p = 0.009), with a continued reduction to 5.6 mm at the one-year follow-up (p = 0.01). The frontal Cobb angle remained stable between the four-month and one-year follow-up assessments, at 28.37° and 28.78°, respectively. The L1-L5 lordosis angle showed no significant change from the immediate postoperative evaluation to the four-month follow-up, at 47.69° and 47.85°, respectively (p = 0.8). However, L1L5 lordosis significantly increased to 49.60° at the one-year follow-up (p = 0.01). T1-T12 thoracic kyphosis showed no significant variation between the four-month and one-year follow-up, measuring 39.16° and 40.44°, respectively (p = 0.08). Conclusion: The balance of the trunk changes in a statistically significant way between the 4-months and the one-year control and these variations explain the modification and progressive improvement of the clinical and functional result. Achieving a satisfactory spinal balance may extend beyond the first postoperative year. This evolution must be explained to the patient as the as well as the low benefit of doing to many early x-rays after the surgery. In our daily practice, the only one-year x-ray assessment remains necessary to assess the quality of the correction of the balance of the trunk. This optimized protocol is an opportunity to reduce radiation exposure for patients.
1448
P078: Clinical effect of intraoperative use of tranexamic acid in minimal invasive scoliosis surgery (MISS) in patients with adolescent idiopathic scoliosis
Jungwook Lim 1 , Young Bin Lee 1 , Sangmin Lee 1 , Yunjin Nam 1 , Seung Woo Suh 1
1 Department of Orthopeadics, Korea University Guro Hospital, South Korea
Introduction: Minimally invasive surgery (MIS) has come quite far in spine and its benefits have found significance in AIS (Adolescent idiopathic scoliosis). MISS (Minimally invasive spine surgery) in AIS has shown to provide adequate deformity correction with good functional outcome and impeccable cosmetic outcome. Traditional open adolescent deformity surgeries are associated with blood loss, ranging from 800 to > 2700 ml and subsequent transfusion of blood products. It gained worldwide recognition in the 2010 Clinical Randomization of an Antifibrinolytic in Significant Haemorrhage (CRASH- 2) trial. Schouten et al. in their study demonstrated an almost two-fold decrease in blood loss by TXA for patients undergoing scoliosis surgery. TXA has been proven to reduce risk of adverse events associated with blood transfusions and healthcare costs due to use of blood products. MISS for AIS is fairly uncommon due to technical expertise involved and a long learning curve. To the best of our knowledge no study has by far evaluated the efficacy of TXA in MISS for AIS. MIS itself reduces blood loss in scoliosis surgery as compared to an open procedure. Our study aimed to explore the prospects of introducing TXA in scoliosis surgery as a routine protocol to further ameliorate overall outcomes by cutting down blood loss to the bare minimum. Material and Methods: Our center started using tranexamic acid intraoperatively in MISS from June, 2022. Consecutive data were collected from 104 patients who underwent surgery for AIS from 2021 to 2023. All patients underwent minimal invasive scoliosis surgery done by a single surgeon. Expected blood loss, hemo-vac drainage amount, complication (hemothorax, pelural effusion etc.) was compared between two groups. Results: 47 patients underwent surgery without intra-operative use of tranexamic acid (Group A), 57 underwent surgery with tranexamic acid (Group B). To confirm homogeneity between the two groups, age, gender, height, weight, BMI, Cobb’s angle, curve type, fusion extent, amout of correction, pre-operative hemoglobin level was compared. There was no difference between two groups. (All p-values > 0.50). An average of 2.03 pack of RBC transfusions were performed, Group A needed an average of 2.28 packes and Group B needed 1.82 packes, reducing the amount of transfusion, but there was no statistical significance (p = 0.158). An average of 0.5 pack of RBC transfusions were performed after operation was done, Group A needed an average of 0.81 packes and Group B needed 0.25 packs, and there was significant statistical difference (p = 0.001). 9 patient needed thoracentesis or chest tube insertion after MISS in group A but non needed these invasive procedure in Group B. Conclusion: In minimal invasive scoliosis surgery, intraoperative use of intravenous tranexamic acid can reduce the amount of bleeding during the surgery, also the need of blood transfusion during perioperative period. Also with the use of intravenous TXA the incidence and severity of hemothorax associated with thoracoplasty, which is commonly during deformity correction of the rib hump decreases.
1477
P079: Restoration of thoracic kyphosis after selective posterior fusion surgery in adolescent idiopathic scoliosis Lenke type 5C: A minimum 2 year follow up
Farid Yudoyono 1,2 , Yong Qiu 2
1 Neurosurgery, Universitas Padjadjaran, Faculty of Medicine, Hasan Sadikin Hospital, Bandung, Indonesia
2 Spine Surgery, Nanjing DrumTower Hospital, Nanjing University Medical School, Nanjing, China
Introduction: Adolescent idiopathic scoliosis (AIS) is a type of complex three dimensional structural deformity of the spine and is characterized by vertebral rotation in the transverse plane, lateral curvature in the frontal plane, and abnormal alignment in the sagittal plane. The retrospective study aimed to report the sagittal outcome measures in patients with Lenke type 5C adolescent idiopathic scoliosis (AIS) undergoing thoracolumbar/lumbar (TL/L) selective fusion surgery. Methods: Fifty patients with Lenke type 5C AIS underwent selective posterior TL/L curves fusion (mean age, 13.9 ± 2.0 yrs). Preoperative and postoperative radiographic and clinical parameters were analyzed at a minimum 2-year follow-up period. Results: The main TL/L Cobb angle was 40.3° ± 4.7° preoperatively and 18.7° ± 4.3° (p < 0.0001) at 2-year follow-up. Also, thoracic kyphosis (TK) (T1-12) angle was 22.0° ± 7.2° preoperatively and 29.4° ± 5.3° at follow-up (p < 0.001), and TK (T5-12) angle was 13.1° ± 9.0° preoperatively and 21.7° ± 6.4° at follow-up (p < 0.001). Thoracolumbar kyphosis (TLK) were significantly different from both the groups; and after the surgery, no significant differences in these parameters were observed between the two groups. Conclusion: After the selective TL/L posterior fusion surgery in patients with Lenke type 5C AIS, the sagittal alignment profile, including TK, TLK, cobb angle, was significantly restored.
Keywords: Adolescent idiopathic scoliosis, Abnormal Alignment, Correction of curves
1638
P080: Minimally invasive anterior spinal fusion comparing thoracic versus lumbar for scoliosis
Jack Williams 1 , Edward King 1 , Mathew Gallagher 1 , Sarah Abbott 1 , Tesfaladet Kurban 1 , Libby Gooda 1 , Vaseharan Suntharan 1 , Emily Tsang 1 , Timothy Bishop 1 , Jason Bernard 1 , Darren Lui 1
1 St George's Hospital, London, United Kingdom
Introduction: It is established that Anterior Spinal Fusion for scoliosis may result in shorter fusion levels. Recently there has been a trend towards Vertebral Body Tethering through an anterior approach. An analysis of minimally invasive (MIS) anterior fusion surgery was conducted to assess reliability and efficacy. Material and Methods: A retrospective analysis between 2017-2022 of patients undergoing selective anterior thoracic fusion (SATF) and thoracolumbar spinal fusion (TLSF) was performed. Data was collected from British Spine Registry (BSR) and local records for a 1 year minimum follow up. Cobb angles for standing and fulcrum bending radiographs (XR) pre-operatively and post-operatively were measured. Patient satisfaction reported with SRS22 questionnaires. Results: 45 patients with a mean age of 16.3y and a F:M ratio of 8:1. Group 1 SATF (n = 21) and Group 2 TLSF (n = 24). Overall Mean pre-operative Cobb was 53.9 ° and post-operative cobb 17.7 ° giving a Mean Correction Rate (CR) 67.2%. Fulcrum bending correction Index mean was 99.5%. Group 1 CR was 58.1% with a FBCI of 100.9% versus Group 2 CR of 75.2% with a FBCI of 106.9%. Overall SRS22 was 3.32 (pre-op), 3.90 (1-year postop) and 4.08 (2 years). Return to surgery within 30 days 4.4% (n = 2) for screw adjustment. Reinsertion of chest drain 2.2% (n = 1). Overall mean blood loss was recorded at 431 mL (Group 1- 426 ml and Group 2 -436ml). Mean operation length 350 minutes and mean length of stay 6 days. Conclusion: MIS Anterior spinal fusion surgery is found to be an effective and safe approach to the management of AIS. Fulcrum bending XR is predictive of final Cobb angle giving an FBCI of 99.5%. Correction rate and FBCI was greater in the TLSF group. The mean levels fused were 6.1 showing that selective fusion via a minimally invasive approach is possible.
1736
P081: Fusing half the levels: a comparison of the efficacy and fusion levels required between anterior fusion versus posterior spinal fusion for the treatment of adolescent idiopathic scoliosis
Jack Williams 1 , Libby Gooda 1 , Edward King 1 , Mathew Gallagher 1 , Sarah Abbott 1 , Tesfaladet Kurban 1 , Vaseharan Suntharan 1 , Emily Tsang 1 , Timothy Bishop 1 , Jason Bernard 1 , Darren Lui 1
1 St Georges Hospital, London, United Kingdom
Introduction: It is established that Anterior Spinal Fusion for scoliosis may result in shorter fusion levels. A comparative analysis of Selective Anterior Fusion (SAF) and Posterior Spinal Fusion (PSF) was conducted to assess reliability, efficacy and perioperative outcomes. Material and methods: A retrospective analysis between 2017-2022 of patients undergoing SAF and PSF was performed. Data was collected from British Spine Registry (BSR) and local records for a 1 year minimum follow up. Cobb angles for standing radiographs (XR) pre-operatively and post-operatively were measured. Patient satisfaction reported with SRS22 questionnaire. Results: 88 patients with a mean age of 15.9y, F:M ratio of 5.77. SAF (n = 44) and PSF (n = 44). Mean pre-operative Cobb was 53.6° (SAF) and 62.2° (PSF), mean post-operative Cobb was 17.7° (SAF) and 23.1° (PSF). Mean Correction Rate (CR) was greater for SAF- 67.0% vs 62.2% (PSF). SAF had lower mean levels fused - 6.1 (SAF) vs 11.7 (PSF). SRS22: preoperatively - 3.32 (SAF) and 3.34 (PSF); 1-year follow up - 3.87 (SAF) and 4.28 (PSF); SRS22-year follow up - 4.05 (SAF) and 4.13 (PSF). SAF had favourable perioperative outcomes with mean blood loss 431.2 mL (SAF) vs 547.1 mL (PSF), return to surgery 4.5% (SAF) vs 13.6% (PSF), and occurrence of intra-operative adverse events 2.3% (SAF) vs 4.6% (PSF). Conclusion: SAF is found to be an effective and safe approach to the management of AIS with superior CR and perioperative outcomes, and was found to require 52.1% of fused vertebral levels of its counterpart PSF.
1788
P082: Comparison of selective anterior fusion and posterior spinal fusion for the preservation of sagittal balance in adolescent idiopathic scoliosis
Libby Gooda 1 , Jack Williams 1 , Edward King 1 , Mathew Gallagher 1 , Sarah Abbott 1 , Tesfaladet Kurban 1 , Vaseharan Suntharan 1 , Emily Tsang 1 , Timothy Bishop 1 , Jason Bernard 1 , Darren Lui 1
1 St George's Hospital, London, United Kingdom
Introduction: It is established that Anterior Spinal Fusion for scoliosis may result in shorter fusion levels. A comparative analysis of Selective Anterior Fusion (SAF) and Posterior Spinal Fusion (PSF) was conducted to assess the preservation of sagittal balance. Material and methods: A retrospective analysis between 2017-2022 of patients undergoing SAF and PSF was performed. Data was collected from British Spine Registry (BSR) and local records for a 1 year minimum follow up. Kyphosis angles were measured from standing radiographs (XR) pre-operatively and post-operatively, with the maximum kyphotic angle and thoracic kyphotic angle (between T4-T12) being reported. Results: 88 patients with a mean age of 15.9y, F:M ratio of 5.77. SAF (n = 44) and PSF (n = 44). Mean pre-operative thoracic kyphosis angle was 26.3° (SAF) and 33.0° (PFS). Mean pre-operative maximum kyphosis angle was 36.2° (PFS) and 44.2° (PFS). Mean post-operative thoracic kyphosis angle was 27.5° (SAF) and 24.9° (PFS). Mean post-operative maximum kyphosis angle was 37.1° (SAF) and 43.1° (PFS). SAF was shown to be superior than PFS in the preservation of kyphosis, with a percentage change in thoracic kyphosis angle of +4.6% (SAF) vs -24.5% (PFS), and percentage change maximum kyphosis angle of +2.5% (SAF) vs -2.5% (PFS). SAF was also shown to require lower mean levels fused – 6.1 (SAF) vs 11.7 (PFS). SAF had favourable perioperative outcomes with mean blood loss 431.2 mL (SAF) vs 547.1 mL (PSF), return to surgery 4.5% (SAF) vs 13.6% (PSF), and occurrence of intra-operative adverse events 2.3% (SAF) vs 4.55% (PSF). Conclusion: SAF is found to be an effective and safe approach to the management of AIS with a greater preservation of natural sagittal balance and requiring 52.1% of fused vertebral levels of PSF.
1845
P083: What factors predict cervical sagittal alignment restoration after correction of thoracic adolescent idiopathic scoliosis with severe thoracic hypokyphosis? A multicenter retrospective study on 57 patients
Giovanni Viroli 1 , Mohammadreza Chehrassan 2 , Alberto Ruffilli 1 , matteo traversari 1 , Marco Manzetti 1 , Cesare Faldini 1
1 1 st Orthopaedic and Traumatologic Clinic, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
2 Iran University of Medical Sciences - Shafa Yahyaian Hospital, Teheran, Iran
Introduction: The sagittal alignment of Adolescent Idiopathic Scoliosis (AIS) has attracted growing interest in recent years. In particular, thoracic curves, due to the anterior overgrowth, are almost invariably characterized by thoracic hypokyphosis, which can be severe (T5-T12 thoracic kyphosis < 10°, i.e. Lenke - sagittal modifier). This has consequences that are not limited only to the thoracic region, but it rather results in a disruption of the entire sagittal alignment. In fact, thoracic hypokyphosis tends to shift the C7SVA backward and to decrease the T1 slope. As a compensation, this ultimately leads to the development of a cervical kyphosis to translate the head forward and maintain global sagittal balance. While the interplay between thoracic hypokyphosis and cervical kyphosis is well described, the results regarding the amount of spontaneous correction of cervical kyphosis achieved after AIS correction are conflicting. The aim of the work was to assess the changes in cervical sagittal alignment after correction of AIS with associated severe thoracic hypokyphosis (<10°). The second aim was to seek for any radiographical parameter able to predict the postoperative cervical sagittal alignment, via a multivariate regression analysis. Material and Methods: A multicenter retrospective study was conducted with this inclusion criteria: AIS patients with a Lenke 1, 2, 3 patterns, associated severe thoracic hypokyphosis (TK < 10°; Lenke - modifier), treated with posterior spinal fusion, high-density pedicle screws, Ponte osteotomies and differential rod contouring. Radiographic analysis was performed preoperatively and at minimum 2 years follow-up. Univariate analysis was performed; binomial logistic regression and linear logistic regression models were created adopting a backward stepwise approach. Results: 57 patients were included. At the last follow-up, T5-T12 TK showed a significant improvement (from 0.7° to 12.9°; p < .001). Cervical Lordosis (CL) significantly increased from 10.7° to 4.1 (p = 0.003; average change = -6.7° ± 16.7°). According to Staub et al formula (T1slope - 16.5°), ideal CL was calculated, and the mismatch between this value and the actual CL passed from 22.7° to 15.9° (p = 0.003). Postoperative T5-T12 TK (z = 2.551; p = 0.011) and preoperative T2-T5 TK (z = 2.112; p = 0.035) showed significant correlation with the chance to have a postoperative CL of at least -5°. Considering only patients with a preoperative neutral or kyphotic CL (CL > -5°), TK apex-SVA, C5-T2° Change and TK apex-scoliosis apex distance showed significant correlation with the chance to have a minimum detectable change (-6.2°) for CL. At linear logistic regression, preoperative CL, PI, UIV slope, postoperative PI-TK mismatch and preoperative main curve Nash-Moe showed significant correlation with the CL change. Conclusion: CL showed significant improvement after posterior only correction of hypokyphotic Lenke 1-2-3 AIS; despite that, a 15.9° mismatch between ideal and actual postoperative CL still remains. The degree of restoration of thoracic and cervithoracic alignment seem to correlate with a spontaneous CL restoration.
1861
P084: Ponte osteotomies in the surgical treatment of adolescent idiopathic scoliosis: better defomity correction or just extra blood loss? A systematic review of the literature and meta-analysis of comparative studies
Giovanni Viroli 1 , Alberto Ruffilli 1 , matteo traversari 1 , Francesca Barile 1 , Marco Manzetti 1 , Francesco Sartini 1 , Alessandro Cargeli 1 , Stefania Claudia Parisi 1 , Cesare Faldini 1
1 1 st Orthopaedic and Traumatologic Clinic, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Considering the tridimensional nature of adolescent idiopathic scoliosis (AIS), the results of surgical correction on the sagittal plane component of the deformity, typically characterized by a reduction of thoracic kyphosis (TK) due to anterior spinal overgrowth, have been inconsistent. Several studies have demonstrated not only a failure in the restoration of TK, but also a proper iatrogenic hypokyphotic effect, which has been ascribed to DVR at times and to all-pedicle-screws-based constructs. This aspect of AIS surgery has received growing attention, since thoracic hypokyphosis is related to long term consequences in the adjacent spinal regions, such as an increased risk of lumbar degenerative disc disease and of cervical spine kyphotic decompensation after AIS surgery. Many authors have therefore adopted ancillary procedures such as Ponte Osteotomies (POs), in order to restore the TK, or at least to avoid the risk of iatrogenic hypokyphosis as much as possible. Through a systematic literature research and a metanalysis of comparative studies, the first aim of the present paper is to assess whether the adoption of POs allows to restore the TK during AIS correction surgery. The second objective is to assess the influence of POs on the coronal correction rate. The final endpoint is to determine if the use of POs results in significantly increased blood loss, operative time and complication rate, such that their adoption for a better correction may not be justified by their safety profile. Material and Methods: A systematic search of electronic databases was conducted. Inclusion criteria: comparative studies that reported the outcomes of AIS patients who underwent surgical correction through posterior-only approach with and without POs. Clinical and radiographic outcomes were extracted and summarized. Meta-analyses were performed to estimate the differences between patients treated with and without POs. p < 0.05 was considered significant. Results: 9 studies were included. No significant difference in TK change between patients treated with and without POs resulted (+3.8°; p = 0.0603). Considering only hypokyphotic patients, a significant difference in TK change resulted with POs (+6.6°; p < 0.0001), while a non-significant TK change resulted in normokyphotic patients (+0.2°; p = 0.9569). No significant difference in coronal correction (2.5031°; p = 0.1037) was recorded. Significant EBL (142.5 mL; p = 0.0472) and surgical times (21.5 minutes; p = 0.0446) differences were found with POs. Regarding complications rate, meta-analysis showed a non-significant log odds ratio of 1.1 (p = 0.0801) with POs. Conclusion: POs allow to restore TK in hypokyphotic AIS, without a significantly greater TK change in normokyphotic patients, nor a significantly better coronal correction. Considering the significantly greater EBL and the trend toward a higher complications rate, the correct indication for POs is crucial.
1901
P085: A randomised controlled trial: comparison of the mesa spinal system with the universal spinal system for the treatment of adolescent paediatric spine deformity
Evan Davies 1 , Laura Mitchelson 2
1 Southampton Childrens Hospital, Southampton, United Kingdom
2 Southampton University, Medical School, Southampton, United Kingdom
Introduction: Adolescent idiopathic scoliosis (AIS) is a deformity causing an abnormal spinal curvature. Surgical treatment can be considered in patients with a curvature > 40 degrees. The Universal Spinal System (USS) was developed in 1990’s. The MESA™ rail was developed in 2012 with a unique design, for improved corrections. Quality of life is assessed in the scoliosis specific questionnaire, the SRS-22r. A new surgical device that improves curvature corrections and patient quality of life should be validated. Literature is limited for MESA™ rail efficacy. There are no studies prospectively comparing the MESA™ rail to other devices. Material and Methods: 60 patients aged 11-21 years who did not meet exclusion criteria were recruited. Patients and guardians signed assent and consent forms for study inclusion. The SRS-22r questionnaire were completed before surgery. These same assessments were completed at post-operative. Patients were randomly allocated a device and all patients and guardians were blinded to device pre-operatively. Analysis of covariance was used to establish statistical significance between groups. This allowed for control of pre-operative patient data and control of external factors which have been evidenced to affect AIS surgical outcomes including age, gender and number of fused vertebrae. Results: There were 26 patients from the USS group and 27 from the MESA group used within this part of the analysis due to missing questionnaire data for the remaining 7 participants. Mean overall score and all domain mean scores improved in both groups at post-operative follow-up compared to pre-operative. The greatest mean difference was seen in patient self-image scores for both the USS and MESA group. These differences were a mean score improvement of 1.55 and 1.51 respectively. Neither post-operative curvature nor scoring in any of the SRS-22r domains was found to be statistically significant between device groups. Conclusion: This study has validated the MESA™ rail as comparable to the USS. We have shown that randomised controlled trials are possible in surgery.
2006
P086: Non - opioid dependen post operativa analgesia in pediatric scoliosis
Karen Weissmann 1,2 , Francisca Castro 3 , agustin cavagnaro 3 , Andres Chain 2 , Juan Otto 2 , Hernan Arraño 4 , Alicia Olivares 4 , Ana Sanchez 3
1 Spine Surgery, Patagonia Spine Foundation, Santiago, Chile
2 Spine Surgery
3 Pediatry
4 Anesthesiology, Clinica MEDS, Santiago, Chile
Introduction: Post operative analgesia must be multimodal; opioids have historically constituted a mayor part of it but imply adding effects such as slower bowel movements, urinary retention and post operative nausea and vomiting (PONV) thus delaying ambulation and causing longer hospitalization times. Our aim was to evaluate the patient response to post operative analgesia in scoliosis surgery without opioids. Material and Methods: Retrospective descriptive study of two cohorts: with and without intrathecal morphine. 21 patients (76% women, mean age13.38 ± 2.2 years old) that underwent deformity surgery for scoliosis. Demographic data, surgical data (bleeding, transfusions, surgical technique, use of topical and iv tranexamic acid (TXA)(30mg/Kg)) and post operative parameters (Length of stay (LOS), post operative Ht/Hb, VAS, use of invasive and noninvasive ventilatory assistance, days with foley,) were analyzed. Post operative analgesia consisted of a continuous infusion of sodic metamizol (20mg/kg/dose) and ketorolac (0.5 mg/Kg), acetaminophen (15 mg/kg/dose) and parecoxib (40 mg/dose). Patients had a rescue patient-controlled analgesia (PCA) with morphine, the use and number of opioid shots was measured, along with (PONV), days to ambulation, urinary retention post retrieval of urinary catheter. Data was analyzed using SPSS (Statistical analysis, IBM, Chicago) was performed with spearman’s rank correlation coefficient (p < 0.05). Results: The most common diagnosis was Adolescent idiopathic scoliosis (85.7%) followed by neuromuscular, syndromic, and congenital (4.8% each), average BMI was 20.1 ± 4.4, mean number of comorbidities per patients was 0.38 ± 0.6, being the most common psychiatric pathology (depression/anxiety syndromes), followed by genetic syndromes. Mean pre op Ht/Hb was 41.4 ± 3.4%/13.8 ± 1.3grs/dl. The most common technique was vertebral body tethering (52.4%) followed by posterior spinal fusion (42.9%) and posterior dynamic distraction devices (4.8%). Mean bleeding was 288.1 ± 234.5, post operative Ht/Hb was 33.3 ± 4.3%, 11.3 ± 1.6 grs/dl. 14.3% of patients required transfusion, 47.6% of patient received iv TXA and 33% topical TXA. 19% of patient received topical vancomycin. When we analyzed analgesia, There was no difference in between both groups regarding postoperative VAS (p = 0.729) the number of days with continuous analgesia (p = 0.894), the use of celecoxib on the first and second post operative day (p = 0.612, 0.511)), pregabalin (p = 0.857), the anxiolytics (p = 0.511), dexamethasone (p = 0.857), high volume oxygen (p = 0.729), number of days with foley catheter (p = 0.364), days with a central venous catheter (p = 0.857), use of PCA (p = 0.165), number of shots of PCA (p = 0.579), use of other rescue opioids (p = 0.538), PONV (p = 0.614), time to ambulation (p = 0.233), urinary retention (p = 0.857) or other complications (p = 0.857), LOS in intensive care unit (ICU) (p = 0.641), LOS in medico surgical units (p = 0.147) or total length of stay (p = 0.524). Conclusion: Pediatric deformity patients can undergo surgery without the use of post operative opioids. There is no impact regarding LOS, the use of post operative rescue opioids or post operative complications.
2109
P087: Ponte's osteotomy for surgical treatment of adolescent idiopathic scoliosis
Pedro Torres 1 , Andre Castilho 1 , Henrique Dagostin de Arjona 2 , Rodrigo dos Santos Grandini 2 , André Luís Fernandes Andújar 2
1 Spine Surgery, Hospital Unimed
2 Spine Surgery, Hospital Joana Gusmão, Florianópolis, Brazil
Objective: to evaluate retrospectively the potential surgical correction in patients with idiopathic scoliosis of the adolescent submitted to posterior arthrodesis and pedicle screw instrumentation; and to compare a group in which the same procedure was realized with the addition of the Ponte osteotomy, attempting to show through preliminary results, the influence of this procedure in the surgical treatment of the idiopathic scoliosis of the adolescent. Methods: retrospective study of 30 patients operated on, at the Joana de Gusmão Hospital Children's in Florianópolis, evaluating their general characteristics and surgical effectiveness. The level of curvature correction in the post-operation period, as well as the descriptive and comparative analysis of the differences between the group of patients that received surgical treatment with pedicle screws, 17 patients, and the group of patients that in addition to the pedicle screw, received the Ponte osteotomy technique, 13 patients, was evaluated. The percentage of the curvature correction between pre- and immediate post-operation (up to two months after surgery) period for each group was evaluated and a comparative analysis was realized. Results: in the patients without Ponte osteotomy, the average deformity correction in the coronal plane in post-operation evaluation was 67.06% and, in the patients, submitted to osteotomy, 79.47%. When the average correction difference of both groups was evaluated, there was a significant correction in those submitted to osteotomy. There were no neurological complications. Conclusion: favorable to the use of the referred technique and higher effectiveness in the correction of the curvature with the use of pedicle screws associated with Ponte osteotomy.
2345
P088: Scoliosis in a patient with nemaline myopathy: a case report and narrative review
Pedro Torres 1 , Andre Castilho 1 , Anna Luiza Amancio 1 , Rodrigo Cruzeiro 1 , Daniel Araujo 1
1 Spine Surgery, Hospital Unimed, Brazil
Introduction: Nemaline myopathy (NM) was first identified in muscle biopsies from children with hypotonia in the 1950s. Microscopic examination revealed rod-like or ovoid structures in muscle fibers. NM comprises a heterogeneous group of congenital myopathies caused by mutations in the genes encoding skeletal muscle α-actin. Clinically, most patients present with muscle weakness and hypotonia, but the phenotypic spectrum is heterogeneous, ranging from severe neonatal presentations to childhood onset. Materials and Methods: We present a case of a 13-year-old patient admitted to our service with neuromuscular scoliosis secondary to NM. Family members reported the onset of the deformity in childhood, with a recent worsening of symptoms. Due to the underlying pathology, the patient required gastrostomy and tracheostomy support, was unable to walk, but could stand with the assistance of upper limbs. A panoramic radiograph revealed two curves, the largest being thoracolumbar with a Cobb angle of 65 degrees from T9 to L3, and a second proximal thoracic curve from T1 to T5 with a 45-degree angle. The thoracic segment between the curves (T5 to T8) was rectified. Consequently, this curve does not fit into the Lenke classification. A literature search was conducted on PubMed and the Google Academic database for review studies and case reports related to Nemaline myopathy and scoliosis. Results: The patient underwent surgery involving T2-L4 arthrodesis. During the procedure, difficulties arose in identifying anatomical structures due to multiple fusions of posterior elements. As a result of this challenge, cerebrospinal fluid leaked out during the passage of two screws. Furthermore, during the passage of the screw from T2 on the left, there was a decrease in potential in the left lower limbs, with partial recovery at the end of the procedure. Conclusion: Nemaline myopathy is a rare disease with limited research. There is scarce literature on the treatment of scoliosis in these patients. Despite the dearth of literature, prognosis seems to be influenced by scoliosis and restrictive lung disease secondary to deformity. Treatment requires a multidisciplinary approach focused on maintaining as much muscle power and function as possible, with a particular emphasis on scoliosis management. When opting for surgical treatment, attention must be given to other consequences of muscle weakness, such as respiratory disease. Surgeons should be prepared for multiple challenges arising from anatomical deformities during the procedure. Therefore, we recommend that the surgical team include an experienced surgeon due to the high likelihood of intraoperative complications.
2351
P089: Scoliosis and pectus excavatum deformities: what should be treated at first?
Nikita Khusainov 1 , Dmitry Kokushin 1 , Alexandra Filippova 1 , Sergey Beljanchikov 1 , Dmitry Ryzhikov 1 , Marat Asadulaev 1 , Vissarionov Sergey 1
1 Spine Pathology and Neurosurgery, National Medical Research Center for Pediatric Trauma and Orthopedics n.a. H.I.Turner, Saint-Petersburg, Russian Federation
Introduction: Reported association between pectus excavatum and scoliosis is up to 22.58%. Both disorders can be managed surgically but there is a lack of information about the influence of one procedure on the natural course of the second disease and/or further treatment process. As a result of derotation in the thoracic area during correction of scoliosis there is a potential threat of the mediastinal compression development. There is no consensus about which condition should be treated at first. Material and Methods: We analyzed data of 54 surgically treated patients with mean age of 15.3 y (12.1 y - 16.4 y) who were presented at our institution due to pectus excavatum deformity. 3 of them had pectus and spine deformity requiring surgery for both conditions. According to CT there was a lack of retrosternal space which could potentially lead to cardiac tamponade or compression of the trachea during scoliosis correction thus correction of pectus deformity using metal bar was decided to be performed as a first stage. Posterior instrumental fusion was performed 6 month later. CT-data, results and complications of this approach were evaluated. Results: As a result of the first stage significant increase of retrosternal space was observed: from mean 1.91 cm to mean 5.5 cm. Haller index improved from mean 9.4 to 3.9. There was no improvement of lung function according to PFTs at that time. Both first procedure and correction of the spine deformity went uneventfully. Mean pre-op Cobb angle was 67.9⁰, post-operatively it improved up to mean 34.5⁰. There was a slight decrease of the retrosternal space and signs of metal bar instability after second stage were observed but these were clinically insignificant. All patients were satisfied with final result. Conclusion: We consider that in patients with combination of pectus excavatum and spine scoliotic deformity retrosternal space should be restored as a first step to decrease a risk of potentially life threatening complications. The presence of metal bar does not produce difficulties for ventilation or correction maneuvers during anesthesia and surgery. Correction of scoliosis leads to trunk elongation and decrease of transverse diameter of the chest which may result in change of metal bar position in its fixation points which is usually asymptomatic.
2583
P090: Maintaining shoulder balance in Lenke 2 curves - novel surgical technique for UIV fixation
Nikita Khusainov 1 , Sergey Beljanchikov 1 , Dmitry Kokushin 1 , Alexandra Filippova 1 , Marat Asadulaev 1 , Vissarionov Sergey 1
1 Spine Pathology and Neurosurgery, National Medical Research Center for Pediatric Trauma and Orthopedics N.A. H.I.Turner, Saint-Petersburg, Russian Federation
Introduction: Maintaining of the shoulder girdle balance remains an important issue in treatment of AIS patients especially with Lenke 2 curves. A number of authors have proposed instrumental fixation of the T2 vertebra as an effective measure. However placing a pedicle screw on the concave side is not always possible whereas insertion of a supralaminar hook leads to aggravation of the existing curvature worsening the shoulder imbalance. The purpose of the study was to evaluate the effectiveness of a new technique for UIV instrumentation. Material and Methods: Preoperative examination and surgical treatment of our patients was carried out according to local protocol. Based on the results of panoramic and bending x-ray the deformities were classified as Lenke type 2. During the surgical intervention instrumentation was performed using a standard technique from the level of the T2 vertebrae. Due to the lack of technical ability to insert a transpedicular screw into the body of T2 vertebra a supralaminar hook was inserted at this level on the concave side of the deformity. Taking into account the worsening of the existing proximal thoracic curve after contraction maneuver to fix the hook at the lamina of the vertebra and in order to maintain the balance of the shoulder girdle a supralaminar hook was inserted at the level of the Th1 vertebra on the convex side of the deformity. Results: With contraction maneuver we achieved horizontalization of T1 vertebra and maintained shoulder balance. In the postoperative period, panoramic radiography of the spine was performed in a standing position which confirmed the preservation of the balance of the shoulder girdle without worsening the proximal thoracic curve, as well as sufficient correction and stabilization of the main thoracic curve. 1.5 years post-op there were no signs of implant loosening or development of PJK. Conclusion: In the absence of the technical possibility of installing a transpedicular screw at the level of the upper instrumented vertebra on the concave side of the proximal structural arch, an effective method of maintaining shoulder girdle balance in the postoperative period is an insertion of a supralaminar hook at the level of the overlying segment on the convex side of the arch. This method provides sufficient correction and stabilization of the deformity, eliminates the need for extensive dissection of soft tissues to install a pedicle screw, and helps to prevent the development of PJK.
Deformity-thoracolumbar (Adult)
170
P091: Post-operative shift in pain profile following fusion surgery for adult spinal deformity - a cluster analysis
So Kato 1 , Nozomu Ohtomo 1 , Yoshitaka Matsubayashi 1 , Yuki Taniguchi 1 , Yujiro Takeshita 2 , Hiroyasu Kodama 3 , Takashi Ono 4 , Masahito Oshina 5 , Akiro Higashikawa 2 , Nobuhiro Hara 3 , Shima Hirai 6 , Kazuhiro Masuda 7 , Sakae Tanaka 1 , Yasushi Oshima 1
1 Department of Orthopaedic Surgery, The University of Tokyo, Tokyo, Japan
2 Department of Orthopaedic Surgery, Japan Organization of Occupational Health and Safety Yokohama Rosai Hospital, Japan
3 Department of Spine and Orthopedic Surgery, Japanese Red Cross Medical Center, Japan
4 Department of Spinal Surgery, Japan Community Health-Care Organization Tokyo Shinjuku Medical Center, Japan
5 Department of Orthopaedic Surgery, NTT Medical Center Tokyo, Japan
6 Department of Orthopaedic Surgery, Sagamihara National Hospital, Japan
7 Department of Orthopaedic Surgery, Tokyo Metropolitan Tama Medical Center, Japan
Introduction: Adult spinal deformity (ASD) is associated with a combination of back and leg pain of various intensities. The reaction of pain profiles to the surgical management of ASD is also diverse, which complicates the interpretation of the effectiveness of ASD surgery. Material and Methods: Multicenter prospective surveillance collected data for patients ≥ 19 years old who underwent primary thoracolumbar fusion surgery at five or more spinal levels for ASD between 2017 and 2021. Demographic data and surgical details such as the number of spinal levels involved and fixation technique were collected. Pain profile was recorded using the numeric rating scale (NRS) for back pain (NRSback) and leg pain (NRSleg). Patient-reported outcome (PRO) scores (Short Form-12 physical component summary [PCS], EuroQOL 5-dimension, and Oswestry Disability Index) were also obtained. Two-step cluster analysis was performed utilizing pre-operative NRSback and NRSleg. One-year post-operative outcomes and satisfaction rates were compared among clusters, and influencing factors were analyzed. Results: Participants comprised 191 ASD patients. Mean age was 65.9 years and females comprised 81% of participants. Mean pain scores were 6.4 (standard deviation [SD]: 2.9) for NRSback and 3.1 (SD: 3.3) for NRSleg. Based on cluster analysis, patients were categorized into three groups: ClusterNP, mild pain only (n = 55); ClusterBP, back pain only (n = 68); and ClusterBLP, significant back and leg pain (n = 68). ClusterBLP showed the worst pain profile, with a mean NRSback of 7.6 and a mean NRSleg of 6.9. ClusterBLP was the oldest 73.4 years (p < 0.001) and underwent interbody fusion (88%, p < 0.001) and sacral/pelvic fixation (69%, p = 0.001) more commonly than the other groups. While NRSback, NRSleg and PRO scores were all improved postoperatively in ClustersBP and BLP, ClusterBLP showed the lowest satisfaction rate (80% vs 80% vs 63%, p = 0.11), which correlated with post-operative NRSback (rho = -0.357). Conclusion: Cluster analysis of pre-operative ASD patients revealed three clusters based on severity of back and leg pain. The cluster with the worst pain back and leg pain profile was associated with the most advanced disease and showed the lowest satisfaction rate, which was affected by post-operative back pain.
188
P092: Co-occurrence of Treacher Collins syndrome and scoliosis in monozygotic twins
Javier Grajeda 1 , Andrés Cobar 2 , Joshua Pahys 3 , Steven Hwang 3
1 Faculty of Medicine, Universidad Francisco Marroquín, Guatemala City, Guatemala
2 Orthopedic Surgery, Hospital Centro Médico, Guatemala City, Guatemala
3 Shriners Hospitals for Children-Philadelphia, Philadelphia, USA
Introduction: Treacher Collins Syndrome (TCS) is a rare congenital disorder primarily characterized by craniofacial malformations resulting from abnormal differentiation of the first and second pharyngeal arches during fetal development. It is uncommon for this syndrome to be associated with extracraniofacial malformations, such as spinal deformities, which adds a further layer of complexity to the management of this condition. While scoliosis is one such spinal deformity reported in TCS patients, its occurrence in monozygotic twins with the syndrome has not been previously documented. Therefore, the present study aims to describe the unusual presentation of scoliosis in monozygotic twins with TCS, while following their medical course over time to evaluate management outcomes. Material and Methods: A prospective evaluation was performed from May 2022 to July 2023 on two monozygotic female twins, both previously diagnosed with TCS. Data collected at the initial evaluation included patient demographics, as well as clinical and radiological findings that confirmed the diagnosis of scoliosis and guided future surgical decisions. Clinical and radiological variables were re-evaluated at 3 months preoperatively and 1 month postoperatively, enabling the recording of progression and postoperative data. Surgical variables were also collected. Results: At the initial assessment, the first twin reported an SRS-22r of 70, whereas the second twin reported a score of 42. Additionally, both patients complained of back pain and deformity. Each presented with a distinct three-curve configuration at radiographic assessment. The major curve in both patients involved the thoracolumbar portion, measuring 52° (T9-L2) in the first patient and 73.1° (T8-L2) in the second. Although surgery was indicated, waiting time till surgery (13 months for both) influenced the major curves, which had progressed to 61.6° and 80.4°, respectively, at the 3-month preoperative evaluation. The patients underwent posterior approach spinal fusion surgery, during which several variables were recorded, including operative time, estimated blood loss, levels of spinal fixation, and adjustments to the surgical plan. The first patient's surgery lasted 4.3 hours with an estimated blood loss of 200mL, while the second patient's surgery took 3.3 hours with an estimated blood loss of 250mL. Post-operative complications were minimal and transient, with only the first patient experiencing lower extremity hypoesthesia, which improved prior to discharge. One-month postoperative follow-up revealed improved posture and shoulder balance, as well as reduced curvature measurements in both patients by clinical and radiographic evaluation. Conclusion: Despite the predominance of craniofacial features in Treacher Collins syndrome, spinal deformities such as scoliosis should be recognized. This report highlights the potential occurrence of scoliosis in these patients, a finding not been well documented in the literature, particularly in monozygotic twins. Despite curve progression due to waiting time till surgery, our report demonstrates that timely surgical intervention can improve both clinical and radiographic outcomes in these patients. Therefore, increased awareness and surveillance of scoliosis in TCS is warranted for early detection and management.
258
P093: Same level fenestrated transpedicular screw fixation combined with vertebroplasty for the management of unstable osteoporotic vertebral fractures co-existing with pedicle fractures: a technical note
Hamisi Mraja 1 , Enas Daadour 1 , Cem Sever 1 , Halil Gok 1 , Tunay Sanli 1 , Selhan Karadereler 1 , Meric Enercan 1 , Azmi Hamzaoglu 1
1 Orthopedics and Traumatology, Scoliosis-Spine Center Istanbul, İstanbul, Turkey
Introduction: Osteoporotic vertebral fractures (OVF) co-existing with pedicle fractures may cause unstable fracture patterns associated with separation and displacement risk. Vertebroplasty is considered one of the surgical treatment options for osteoporotic vertebral fractures. The existence of pedicle fractures in OVF may cause a separation between the anterior column and posterior column which mainly leads to instability. This fracture pattern may have a risk of developing separation and displacement even after traditional vertebroplasty. We aim to introduce fenestrated transpedicular screw fixation technique of pedicle fracture at the same level co-existing with unstable Osteoporotic vertebral fractures. Material and Methods: Analysis of unstable Osteoporotic vertebral fractures co-existing with pedicle fractures who were surgically treated with vertebroplasty combined with a percutaneous fenestrated transpedicular screw fixation of pedicle at same level of the OVF was performed. Prophylactic vertebroplasty was performed one level above and below. All patients underwent MRI and CT scans during preoperative screening. Radiological and clinical evaluations were analyzed during the preop, early postop, and f/up. Results: 20 patients (5M, 15F) mean age 76 (61-91) years of OVF with a mean f/up of 2.5 (2-5) years. QCT analysis including BMD and T-score mean values was 61 mg/cm3 and -4.23 ± 1 respectively. Vertebroplasty was performed at 87 levels. Mean vertebral body angle, cobb angle, anterior vertebral height, and posterior vertebral height improved by 38%, 62%, 25%, and 14% respectively. None of patients developed osteoporotic vertebral fractures separation and displacement, nor did pedicle screw pull-out was observed. Conclusion: Vertebroplasty combined with a percutaneous fenestrated transpedicular screw fixation of pedicle fracture at the same level of osteoporotic vertebral fractures has managed to achieve a stable fixation to the unstable vertebral level. This surgical option may be used to prevent vertebral fracture separation and displacement in elderly patients with these unstable osteoporotic vertebral fractures. Preoperative evaluations to determine this osteoporotic vertebral fractures pattern should include CT scans in addition to MRI scans.
422
P094: Clinical application of personalized digital surgical planning and precise execution for severe and complex adult spinal deformity correction utilizing 3D printing techniques
Yong Hai 1 , Hongtao Ding 1,2
1 Orthopedic Surgery, Beijing Chao-Yang Hospital, Capital Medical University, Beijing
2 Orthopedic Surgery, Beijing Jishuitan Hospital, Capital Medical University, Beijing, China
Introduction: The three-dimensional printing (3DP) technique has been reported to be of great utility in spine surgery. The purpose of this study is to report the clinical application of personalized preoperative digital planning and a 3DP guidance template in the treatment of severe and complex adult spinal deformity. Material and Methods: Eight adult patients with severe rigid kyphoscoliosis were given personalized surgical simulation based on the preoperative radiological data. Guidance templates for screw insertion and osteotomy were designed and manufactured according to the planning protocol and used during the correction surgery. The perioperative, and radiological parameters and complications, including surgery duration, estimated blood loss, pre- and post-operative cobb angle, trunk balance, and precision of osteotomy operation with screw implantation were collected retrospectively and analyzed to evaluate the clinical efficacy and safety of this technique. Results: Of the eight patients, the primary pathology of scoliosis included two adult idiopathic scoliosis (ADIS), four congenital scoliosis (CS), one ankylosing spondylitis (AS), and one tuberculosis (TB). Two patients had a previous history of spinal surgery. Three pedicle subtraction osteotomies (PSOs) and five vertebral column resection (VCR) osteotomies were successfully performed with the application of the guide templates. The main cobb angle was corrected from 99.33° to 34.17°, and the kyphosis was corrected from 110.00° to 42.00°. The ratio of osteotomy execution and simulation was 97.02%. In the cohort, the average screw accuracy was 93.04%. Conclusion: The clinical application of personalized digital surgical planning and precise execution via 3D printing guidance templates in the treatment of severe adult rigid deformity is feasible, effective, and easily generalizable. The preoperative osteotomy simulation was executed with high precision, utilizing personalized designed guidance templates. This technique can be used to reduce the surgical risk and difficulty of screw placement and high-level osteotomy.
470
P095: Correction of severe & rigid kyphotic deformity by a single stage posterior vertebral column resection (PVCR) - An analysis of 28 cases
Sharif Ahmed Jonayed 1
1 Dept. of Orthopaedics & Spine Surgery, National Institute of Trarmatology & Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Introduction: Treatment of a severe & rigid kyphotic deformity due to any cause is always challenging to the treating Spine Surgeon. Nevertheless, Vertebral Column Resection (VCR) has evolved over the past century to become a viable last resort for correction of the most challenging spinal deformities through a single, posterior approach. Method: This is a prospective case series of 28 patients either with a severe (Cobb angle > 60) or rigid kyphotic deformity who underwent treated for correction of deformity by a single stage PVCR from July 2016 to June 2022. Results: Mean age of the patient was 30.2 years with a mean follow-up time 27 months. Average operating time was 420 minutes (range 320-760 minutes). Overall final postoperative kyphotic Cobb angles correction ranged from 30.4° to 55.9°. ODI improved from 58.6 ± 6.5 to 10.5 ± 3.2. VAS was improved from 6.7 ± 0.5 to 1.7 ± 0.8. Most frequent complications observed in our series were massive blood loss with a mean of 740 ml (range 560- 1380), dural tear (8%), thoracic root pain (4%) and neurological deterioration (4 cases -3 transient and 1 late onset). Mean recovery period for neurological recovery was 3months.Surgical site infection rates range from 2.9% to 3.7%. Conclusion: Although the PVCR is a highly technically demanding, exhaustingly lengthy, and associated with a variety of complications but can be performed safely with proper training and patience for correcting these deformities with a satisfactory outcome in a resource constrained environment like us.
Keywords: posterior vertebral column resection (PVCR); severe kyphotic deformity; rigid deformity
548
P096: The result of posterior vertebral column resection for correcting angular potts kyphosis in a long-term follow-up
Kai Cao 1 , Zhenhai Zhou 1 , Junlong Zhong 1 , Jiachao Xiong 1 , Honggui Yu 1
1 The First Affiliated Hospital of Nanchang University, The Orthopaedic Hospital, Nanchang, China
Introduction: It is reported that 10% of spinal tuberculosis children can develop an angular kyphosis greater than 90° when entering their adulthood. Angular Potts kyphosis not only leads to cosmetic concerns but can also result in persistent back pain, cardiorespiratory compromise, and neurological deficits, which dramatically affects patients’ quality and span of life. Posterior vertebral column resection (PVCR) has gained popularity in recent years by virtue of its powerful correction ability. Most relevant PVCR studies have reported the short- to medium-term outcomes in patients with moderate to severe PTK. In this study, we reviewed patients with angular Potts kyphosis who were treated by PVCR with a mean follow-up of 80.8 mons to evaluate the operation safety and medium- to long-term clinical efficacy. Material and Methods: This was a multicentric retrospective study. Seventy-five patients with angular Potts kyphosis, who underwent a PVCR surgery between September 2013 and August 2017, were reviewed. Surgery-related data, neurological function, and patients’ self-assessment of quality of life were evaluated. Spinal parameters, including focal scoliosis (FS), coronal balance (CB), focal kyphosis (FK), sagittal vertical axis (SVA), C2-7 lordosis (CL), thoracic kyphosis (TK), lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), and pelvic incidence (PI), were measured. Results: The operative time was 365.2 ± 86.5 minutes and the blood loss was 1371.9 ± 610.1 ml. The mean follow-up time was 80.8 months. All individual domain scores of SRS-22 were significantly improved at final follow-up. FS was improved from preoperative 20.8 ± 2.3° to 6.1 ± 2.8° at final follow-up (p < 0.05). FK was improved from preoperative 109.6 ± 16.5° to 28.6 ± 4.4° at final follow-up (p < 0.05). CL, TK, and LL were significantly changed postoperatively, respectively. Thirty-six patients suffered from neurological deficits preoperatively. Twenty-two patients got improved by one Frankel grade and eight patients got improved by two Frankel grades at final follow-up. Dural tear occurred in three patients. Four patients underwent transient neurological deficit. Seven patients had superficial wound infection. Pneumothorax was encountered in two patients. Implant failure was observed in eight patients. Bone fusion was observed in all patients at final follow-up. Conclusion: Severe angular Potts deformity can be effectively treated by PVCR. The kyphosis correction and improvement of neurological function can be favorably maintained in a long-term follow-up.
578
P097: The reliability of three-dimensional printing guided template based on computer-assisted three-dimensional reconstruction in the posterior osteotomies for the correction of severe kyphotic deformity secondary to ankylosing spondylitis
Nan Kang 1 , Yong Hai 1 , Yunsheng Wang 1 , Yiqi Zhang 1 , Honghao Yang 1
1 Orthopedic Surgery, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China
Objective: The aim of this study is to evaluate the reliability of three-dimensional printing (3DP) guided template based on computer-assisted three-dimensional reconstruction in the posterior osteotomies for the correction of severe kyphotic deformity secondary to ankylosing spondylitis. Methods: From June 2018 to June 2022, patients with severe kyphotic deformity secondary to ankylosing spondylitis undergoing posterior osteotomy were retrospectively included. Based on the data of preoperative whole spine CT, 3-Matic Medical software was applied to construct the spinal model. Guided template for posterior osteotomy according to the surgical planning was designed, manufactured, and applied to assist the osteotomy execution. The preoperative and postoperative radiographic parameters were measured to evaluate the reliability of 3DP guided template based on computer-assisted three-dimensional reconstruction through intraclass correlation coefficients (ICCs) and Bland-Altman analysis. Results: A total of 36 patients (male: female, 34:2; age 38.5 ± 7.8 years) were included in this study. Three cases underwent two-level pedicle subtraction osteotomy (PSO), 15 cases underwent single-level PSO, and 18 cases underwent single-level PSO combined with multi-level posterior column osteotomy (PCO). The spinal alignment was significantly restored: maximal kyphosis (93.4° ± 13.8° to 60.1° ± 8.1°), lumbar lordosis (4.7° ± 12.2° to 25.1° ± 10.1°), and sagittal vertical axis (7.1 ± 2.1 mm to 4.0 ± 1.2 mm). The osteotomy angles measured were 19.7° ± 4.3° per PSO level and 7.7° ± 1.5° per PCO level, which were consistent with the surgical planning. ICCs and Bland-Altman analysis indicated excellent reliability of 3DP guided template based on computer-assisted three-dimensional reconstruction. Conclusion: The application of 3DP guided template based on computer-assisted three-dimensional reconstruction could facilitate the identification of osteotomy sites and execution of surgical planning for the correction of severe kyphotic deformity secondary to ankylosing spondylitis.
755
P098: PI changes in patients with adult spinal deformity following S2AI fixation: is the hip joint coverage involved?
Dongyue Li 1 , Zhen Liu 1,2
1 Department of Orthopedic Surgery, Nanjing Drum Tower Hospital Clinical College of Nanjing Medical University, Division of Spine Surgery, Nanjing, China
2 Department of Orthopedic Surgery, Nanjing Drum Tower Hospital,The Affiliated Hospital of Nanjing University Medical School, Division of Spine Surgery, Nanjing, China
Introduction: PI has historically been recognized as a constant parameter of pelvic anatomy after skeletal maturity, and many important theories, such as the SRS classification, utilize this characteristic to determine the optimal sagittal alignment of adult spinal deformity (ASD) patients. However, recent studies suggest that PI is a variable parameter in which the hip joint may play a role, as some research has reported forces on the hip and the progression of hip joint narrowing to be associated with several spinopelvic parameters, including PI. Yet, there is still an ongoing debate regarding the specific causes of PI changes, and the relationship between PI changes and the hip joint is an area lacking in research. Given the importance of understanding the factors influencing PI changes for developing surgical strategies in ASD patients, as well as the close relationship between the hip joint and spine, our study aims to investigate the role of the hip joint in postoperative PI changes and explore the potential of preoperative radiographic hip parameters in predicting postoperative PI changes. Material and Methods: In this retrospective cohort study of ASD patients who underwent pelvic fixation with S2AI screws, patients were categorized into C (change, ∆PI ≥ 10°) and NC (not change, ∆PI < 10°) groups based on whether their postoperative PI changes exceeded 10° . The changes in hip parameters postoperatively were compared between group C and group NC. Additionally, we further included patients who had supine CT full-spine position from group C and group NC to compare the differences in hip parameter changes during positional changes. Finally, a correlation analysis was performed between changes in PI and changes in hip parameters. Spinopelvic parameters measured included pelvic incidence, pelvic tilt, sacral slope, Cobb angle, sagittal vertical axis, coronal vertical axis, thoracic kyphosis, lumbar lordosis, T1 pelvic angle, and PI-LL. Hip parameters measured included femoral head coverage, lateral center-edge angle, acetabular index, sharp angle, and extrusion index. Results: A total of 121 ASD patients (242 hips) were included with 28 patients (50 hips) had preoperative radiographs in supine position. In patients with greater postoperative changes in PI following S2AI fixation, there were also more significant alterations in hip parameters postoperative (∆FHC: 5.9 ± 5.1 vs. 2.0 ± 2.0, p = 0.021; ∆LCE angle: 3.1 ± 2.7 vs. 1.4 ± 1.4, p = 0.042; ∆AI: 4.4 ± 3.0 vs. 1.3 ± 1.5, p = 0.012; ∆SA: 2.6 ± 1.5 vs. 1.3 ± 1.7, p = 0.041; ∆EI: 4.1 ± 3.0 vs. 2.0 ± 1.4, p = 0.001). Furthermore, a significant, negative correlation was found between preoperative position-related ∆FHC (Left: r =- 0.317, p = 0.021; Right: r = -0.320, p = 0.031), ∆EI (Left: r = -0.753, p = 0.003; Right: r = -0.420, p = 0.021), ∆LCE angle (Left: r = -0.532, p = 0.021) and postoperative ∆PI. Based on the ROC curve, the optimal threshold of preoperative position-related ∆FHC, ∆LCE angle, ∆EI were 6.65%, 5.40° and 4.55%, respectively. Conclusion: The hip joint may play a role in postoperative PI changes in ASD patients following S2AI fixation. When the preoperative position-related ∆FHC, ∆LCE angle and ∆EI were higher than 6.65%, 5.40° and 4.55%, respectively, the possibility of the occurrence of postoperative changes in PI significantly increased.
767
P099: Inserting screw with a diameter larger than the pedicle width at the upper instrumented vertebra increase the risk of fracture
Shin Oe 1 , Yu Yamato 1 , Tomohiko Hasegawa 1 , Go Yoshida 1 , Tomohiro Banno 1 , Hideyuki Arima 1 , Koichiro Ide 1 , Tomohiro Yamada 1 , Kenta Kurosu 1 , Yukihiro Matsuyama 1
1 Orthopedic Surgery, Hamamatsu University School of Medicine, Hamatsu, Japan
Objective: There have been numerous reports on the causes of upper instrumented vertebra (UIV) fractures in adult spinal deformity (ASD) surgery. The width of the pedicle in the UIV varies among individuals. When the diameter of the screws inserted in the UIV exceeds the width of the pedicle, it may lead to UIV fractures (UIVF) due to pedicle screw insertion. The aim of this study is to investigate whether a screw diameter larger than the pedicle width in the UIV is a cause of UIVF. Methods: We studied 322 patients who underwent ASD surgery after March 2010, had a follow-up of more than 2 years, and had the UIV above the T10 vertebra with a screw diameter of 5.5 mm. Patients with a pedicle width in the UIV measuring less than 5.5 mm on preoperative CT scans were classified as the N group, while those with a width of 5.5 mm or more were classified as the W group. Results: The N group comprised 264 patients, and the W group comprised 58 patients, with both groups having an average age of 68 years. The average pedicle width on both sides was 4.0 mm in the N group and 6.2 mm in the W group. The incidence rate of UIVF was N group: W group = 69 patients (26%): 8 patients (14%) (P = 0.046). In the N group, UIV was at T2 (1 case), T3 (1 case), T4 (18 cases), T5 (22 cases), T6 (11 cases), T7 (11 cases), T8 (29 cases), T9 (92 cases), T10 (79 cases), while in the W group, it was at T5 (1 case), T8 (4 cases), T9 (13 cases), and T10 (40 cases). Particularly in the N group, for cases where the UIV was at T7-10, the incidence rate of UIVF was 22.7% (48/211 patients), while for cases at T2-6, it was 39.6% (21/53 patients). Conclusion: A smaller pedicle width than the screw diameter suggests a risk of UIVF. Paying attention is especially crucial when the UIV is located more cranially, as the pedicle width tends to be smaller. In cases where the pedicle width is smaller than the screw diameter, it is advisable to consider reducing the screw diameter or using alternative fixation methods, such as hooks.
879
P100: The role of thoracic tilt in identifying thoracic compensation and predicting proximal junctional kyphosis in degenerative lumbar scoliosis
Weishi Li 1 , Weipeng Qiu 1 , Zhuo Ran Sun 1
1 Department of Orthopaedics, Peking University Third Hospital, Beijing, China
Introduction: Thoracic compensation has been shown to be associated with the development of proximal junctional kyphosis (PJK), while thoracic shape and morphology in patients with degenerative lumbar scoliosis (DLS) remain understudied. This study aimed to investigate the clinical value of the thoracic tilt (TT) in characterizing thoracic compensation and predicting PJK in patients with DLS. Material and Methods: Patients with DLS who underwent long-segment fusion were divided into the PJK group and the non-PJK group. Asymptomatic elderly volunteers were recruited as healthy controls. Thoracic parameters were measured in both cohorts, including the TT (the angle between the line of the anterior edge of T1 upper endplate and T12 lower endplate and the plumb line), T1-L1 pelvic angle (TLPA), T12 slope, thoracic kyphosis (TK, T4-T12), global thoracic kyphosis (GTK, T1-T12), and thoracolumbar kyphosis (TLK, T10-L2). Multivariate logistic regression was used to assess the association between TT and the development of PJK, adjusting for confounders. Multivariate linear regression was used to establish the predictive formula for TT. Results: A total of 126 patients with DLS were enrolled, of which 37 (29.4%) patients developed PJK. Compared with 110 healthy controls, DLS patients had significantly greater TT, TLPA, T12 slope and TLK as well as smaller TK and GTK (all p < 0.001). Preoperatively, the PJK group showed significantly greater TT (p = 0.013), TLPA (p < 0.001) and TLK (p = 0.034) than the non-PJK group. No significant differences were found in TK and GTK before surgery. Postoperatively, the PJK group showed significantly greater TT (p < 0.001), TLPA (p < 0.001), TLK (p < 0.001) and proximal junctional angle (p < 0.001). Multivariate logistic regression analysis showed that greater postoperative TT was an independent risk factor of PJK. Multivariate linear regression analysis suggested that the regression formula was postoperative TT = 0.675×T12 slope + 0.412×TK + 0.158×TLK – 4.808 (R2 = 0.643, p < 0.001). Conclusion: Here we propose a novel sagittal spinal parameter, TT, which is proposed to describe thoracic morphology and inclination. TT can be applied in the evaluation of thoracic compensation. Compared with healthy subjects, patients with DLS have a more forward-leaning thoracic spine. Greater preoperative TT might represent a decompensated state of TK, which is more susceptible to the development of PJK. Rebalancing the TT in a sagittal neutral position during surgical correction may help prevent the postoperative development of PJK in patients with DLS.
936
P101: Comarison of the frequency of complication after complete and incomplete correcion of sagittal balance in adult patients with degenerative scoliosis
Dmitry Mikhaylov 1 , Dmitry Ptashnikov 2
1 Neurosurgery, Russian Railways Medicine Clinic, Saint Petersburg, Russian Federation
2 Neuro-Orthopedics with Bone Oncology, R.R. Vreden National Research Medical Center, Saint Petersburg, Russian Federation
Introduction: To date, the issues of treatment of elderly patients with ADS accompanied by instability, spinal stenosis, and decrease in the quality of life remain topical. The aim of this study was to compare the frequency of complications after complete and incomplete correction of sagittal balance in adult patients with degenerative scoliosis. Material and Methods: a prospective study of 60 patients (age 65-83 years) with rigid scoliotic deformity. The average follow-up period was 3 years (1-5 years). We evaluated the deformity in accordance with SRS-Schwab Based on the HQROL classification of deformities in adults, studying in all cases long cassette anteroposterior and lateral radiographs. A Thomas test was performed to detect the rigidity of the ilio-lumbar muscle. the main indications for surgery were static and biomechanical spinal disorders with pain syndrome (100%) and neurological syndrome (74.3%). All patients were divided into 2 groups depending on the degree of correction of the sagittal profile. The first group included 32 patients who underwent a complete correction of sagittal balance using transpedicular screw fixation Th4-S1-Pel, multilevel SPO, PSO and TLIF, SVA 0-1 cm. The second group included 28 patients with correction of deformation by multilevel fixation of Th4-S1-Pel, SPO, TLIF, SVA 4-8 cm. The data obtained (the number of complications) were used to calculate the relative risk of complications using four-fold tables and 95% ci. We used the Wilcoxon statistical test. There were no statistically significant differences between patients at the preoperative stage (p> 0.05). Results: In the first group, 9 patients in the postoperative period were found to have screw displacement - PJK, PJF. In 6 cases, the metal structure was broken. These complications led to the loss of correction, which required repeated surgery in all cases. In the second group, PJK was detected in 3 cases, and in 1 case, a fracture of the metal structure. In all cases with complications, SAV was in the range of 7-8 cm. The number of complications in the first group was statistically significantly higher than in the second group (p < 0.01). The assessment of the risk of complications after correction of the sagittal profile showed that the statistically significant risk of complications in SVA is 0-1 cm. The relative risk was RR = 3.281 at 95% CI 1.232-8.738. Conclusion: The study showed that correction of the sagittal profile in patients with rigid scoliotic deformity of the spine in the area of SVA 4-6 cm leads to fewer postoperative complications.
943
P102: Laminectomy in degenerative scoliosis as a risk factor for the progression of spinal deformity
Dmitry Mikhaylov 1 , Dmitry Ptashnikov 1,2
1 Neurosurgery, Russian Railways Medicine Clinic, Saint Petersburg, Russian Federation
2 Neuro-Orthopedics with Bone Oncology, R.R. Vreden National Research Medical Center, Saint Petersburg, Russian Federation
Introduction: To date, the issues of treatment of elderly patients with ADS accompanied by instability, spinal stenosis, and decrease in the quality of life remain topical. The main surgical techniques for treatment are laminectomy and foraminotomy. 1/3 of patients are not satisfied with the results. A prospective study of 100 patients with ADS. According to ODI, VAS after local spinal decompression by foraminotomy - different clinical and radiological outcomes. Foraminotomy is not a risk factor of spinal motion segment instability. Material and Methods: A prospective study. 100 patients with lumbar stenosis and ADS. The mean follow-up period was 3.8 y (6 m. to 4 y), 45 patients more than 3 y. Introduction The main complaint - is pain. The cause - degenerative stenosis of the spinal canal, which leads to the need for surgical intervention.The main surgical techniques for this - laminectomy and foraminotomy. Approximately one third of patients treated are not satisfied with the results of surgery. The objective - assess the risk of spinal motion segment instability after local foraminotomy. X-ray, teleradiography, MRI, CT, classical neurological and orthopedic examination. The conservative treatment had no effect. Local decompressive foraminotomy was in I group (n=50). II group (n= 50) treated conservatively - spinal motion segment stability was monitored in order to further assess the relative risk of instability after foraminotomy. The obtained data (spinal instability), were used to calculate the relative risk of instability using four-fold tables and a 95% ci. We used the Wilcoxon statistical test. There were no statistically significant differences among patients at the preoperative stage (p > 0.05). X-ray - 3, 6, 12, and 18 m and annually; MRI was carried out every 6 m. Patients completed VAS and ODI questionnaires. Results: Foraminotomy provides positive results within 1 y, with further deterioration in the quality of life and an increase in pain both. There was progression of degenerative changes, spinal stenosis and spinal motion segment instability. Assessment of the risk of spinal motion segment instability after foraminotomy showed that there was no statistically significant risk of instability development after local foraminotomy. The relative risk was RR = 0.857 at a 95% CI of 0.916-2.456. Conclusion: Foraminotomy is not a risk factor of spinal motion segment instability. Foraminotomy is indicated for the treatment patients with spinal stenosis with ADS. The treatment effect decreases over time, and another surgical intervention may be required with implants to stabilize the spinal motion segment.
1100
P103: Incidence,risk,and outcome of pedicle screw loosening in degenerative lumbar scoliosis patients undergoing long-segment fusion
Lei Yuan 1 , Yan Zeng 1 , Weishi Li 1
1 Orthopedic Department, Peking UniversityThird Hospital, Beijing, China
Introduction: The incidence, risk, and outcome of screw loosening in DLS patients undergoing multilevel posterior spinal segmental instrumented fusion were unclear. Material and Methods: 130 DLS patients undergoing posterior long instrumented spinal fusion were retrospectively studied. Screw loosening was defined as a halo sign larger than 1 mm around a screw. The patients were divided into loosening and non-loosening groups. Patient-related, surgical and radiographic risk factors were analyzed. Preoperative and follow-up Quality-of-Life scores were compared between loosening and non-loosening groups. Results: 1784 screws were placed in total, and radiologically evident loosening was found in 168 screws (9.42%) in 71 (54.62%) patients. The mean bone mineral density (BMD) and T-scores was significantly lower in loosening group. Compared with the non-loosening group, the loosening group had a significantly higher proportion of patients with osteoporosis or osteopenia, LIV in the sacrum, the maximal lateral listhesis of vertebrae > 8 mm preoperatively and preoperative SVA imbalance. Immediately postoperative TLK and SVA of the loosening group was significantly higher than that of the non-loosening group, and loosening group had a higher proportion of patients with TLK ≥ 10° and sagittal imbalance. Multiple logistic regression analysis indicated that the preoperative maximal lateral listhesis of vertebrae > 8 mm, osteopenia, osteoporosis, LIV at sacrum, postoperative TLK ≥ 10° and sagittal imbalance greatly affected the incidence of screw loosening. The loosening group had a significantly lower JOA score and SF-36 MCS score and improvement of JOA and SF-36 MCS score and improvement of JOA and SF-36 MCS score was not significant. Conclusion: Screw loosening in DLS underwent long-segment surgery is common and tends to occur in the LIV or UIV. Lateral subluxation > 8 mm, osteopenia, osteoporosis, fusion to the sacrum, postoperative TLK greater than 10°, and SVA imbalance were the independent influencing factors. Screw loosening can be asymptomatic, while longer-term follow-up is required.
1110
P104: Kappa: a novel technique for pelvic fixation in adult spinal deformity correction
Laura Marie-Hardy 1 , Clelia Thouement 1 , Raphael Pietton 1 , Pascal-Moussellard Hugues 1
1 Orthopaedic Surgery, University Institute for Spine Surgery, Sorbonne University, Paris, France
Introduction: Pelvic fixation in degenerative spinal deformation is as crucial as demanding. Several pelvic anchoring technics have been described, but loosening rates remain high for most solutions. Here is described the “Kappa” technic, combining ilio-sacral screws to S2A1 screws at two years of follow-up. Material and Methods: Thirteen patients that underwent a spinal deformity correction with “Kappa” fixation to the pelvis and with more than 2 years of follow-up were prospectively included in this study. The surgical technic is described, and clinical and radiographic data have been collected for all patients. Results: The population exhibited an important pre-operative sagittal imbalance (mean SVA of 104.4 mm, mean PI-LL mismatch of 22.8°) that had improved significatively after surgery (mean SVA of 75.5 mm and mean PI-LL mismatch of 4.9°). No loosening of pull-out of the implants was to deplore at two years of follow-up. Conclusion: The association of ilio-sacral screw, resistant to pull-out because of the traction axis perpendicular to the construct, to S2A1 screws, known to be effective in sagittal balance restoration seems to be an effective and safe option to pelvic fixation for adult spinal deformity correction.
1114
P105: Novel risk factors and a radiological predictor model for the progression of proximal junctional kyphosis in osteoporotic vertebral compression fracture following posterior corrective surgery
Junyu Li 1,2,3 , Yinghong Ma 1,2,3 , Junjie Ma 1,2,3 , Zhuo Ran Sun 1,2,3 , Yongqiang Wang 1,2,3 , Miao Yu 1,2,3 , Weishi Li 1,2,3 , Yan Zeng 1,2,3
1 Department of Orthopaedics, Peking University Third Hospital, Beijing, China
2 Engineering Research Center of Bone and Joint Precision Medicine, Beijing, China
3 Beijing Key Laboratory of Spinal Disease Research, China
Introduction: Osteoporotic vertebral compression fracture (OVCF) with spinal kyphosis, are compression fractures of the vertebral body of the spine with minor or no significant trauma due to primary osteoporosis. The high incidence of postoperative mechanical complications brings difficulty and challenge to the surgery treatment. One of the most common complications following surgical correction of OVCF patients is proximal junctional kyphosis (PJK). Two novel parameters, thoracolumbar slope (TLS) and the L1 plumb line (L1PL) can help evaluate the global sagittal alignment in patients as important additions to common sagittal parameters in adult spinal deformity (ASD) patients. Global Alignment and Proportion (GAP) Score has recently been introduced in 2017 to guild spinal correction surgery, but it is currently unclear whether the above conclusions can be applied to OVCF with kyphosis. This study aims to define the correlation of thoracolumbar slope (TLS) and L1 plumb line (L1PL) with the occurrence of proximal junctional kyphosis (PJK) and evaluate the Global Alignment and Proportion (GAP) Score’ effect for PJK following Osteoporotic vertebral compression fracture (OVCF) correction surgery. Based on our findings, we aimed to further provide clinical recommendations on the current operational strategy for preventing PJK. Material and Methods: A total of 74 OVCF patients undergoing posterior corrective surgery between January 2008 and June 2021 with a minimum 2-year follow-up were included. These patients were divided into PJK and non-PJK groups. Spinopelvic parameters, TLS and L1PL were measured preoperatively, postoperatively, and at follow-up. Multivariate logistic analysis was performed on various risk factors as well as GAP score. Associations between novel parameters and PJK were analyzed using receiver operating characteristic analysis. Results: PJK was identified radiographically in 28.4% of patients. The mean age and follow-up were 63.45 ± 7.47 years and 38.17 ± 7.92 months, respectively. There was no difference between the PJK and the non-PJK groups in baseline demographics, pre-operative and immediate post-operative pelvic incidence-lumbar lordosis mismatch. Multiple comparisons showed that the proportion of PJK in the severely disproportioned group (the group of the highest GAP scores) and that of other two groups of lower GAP scores was statistically different (p < 0.001). Potential risk factors for PJK included preoperative TK (p = 0.000), TLS (p = 0.016), and postoperative TLS (p = 0.000), L1PL (p = 0.000). Postoperative TLS and L1PL were respectively independent as risk factors for PJK, with the cut-off values set at 8.6° and 10.4 mm to predict the occurrence of PJK. Conclusion: TLS and L1PL can be used to predict the occurrence of PJK in patients undergoing surgery for OVCF and are crucial for preventing the progression of PJK. Achieving a proportionate GAP Score postoperatively seems to be a viable option as higher GAP scores were associated with higher rates of PJK.
1193
P106: Lumbar facet joint morphometric analysis in South Indian population - A cross sectional study
Vishnu Senthil Kumar 1
1 Orthopaedics, Government Royapettah Hospital, Chennai, India
Introduction: Facet orientation is the angle of the facet joint in the transverse plane relative to the sagittal plane. Facet tropism is defined as asymmetry of the left and right vertebral facet joint angles with one joint having a more sagittal orientation than the other. Improper orientation of the facet joints can alter the movements of lumbar spine leading to spinal instability, facet joint osteoarthrosis, degenerative spondylolisthesis, disc prolapse and non- specific back pain. Materials and Methods: Few studies have been done in south-indian population to evaluate facet joint orientation and incidence of facet tropism. In a prospective cross sectional study, CT scans done in 70 patients with spinal injuries were analysed. Orientation of the facet joint in lumbar spine were measured by the method described by Noren et al. The injured facet joints were excluded from the study. Facet orientation at L1-S1 were calculated on both sides and incidence of facet tropism at each level was assessed. Results: The average facet orientation at L1L2 was 27 deg, L2L3 was 29 deg, L3L4 was 30 deg, L4L5 was 34 deg and L5S1 was 40 deg. Prevalence of facet tropism (difference in facet angle more than 7 deg) was 0.1% at L1L2, 0.06% at L2L3, 0.11% at L3L4, 0.11% at L4L5 and 0.1% at L5S1. Conclusion: Incidence of facet tropism was most frequently seen at L4L5 and least at L2L3 level. Facet orientation was similar in males and females and more coronally oriented in lower spinal segments. Further studies need to be done to correlate these findings with different causes of back pain.
References
1. Kalichman L, Suri P, Guermazi A, Li L, Hunter DJ. Facet orientation and tropism: associations with facet joint osteoarthritis and degenerative spondylolisthesis. Spine (Phila Pa 1976) 2009; Jul15.
1207
P107: Thoracic to lumbar multilevel LIF by combined mini-open retropleural and retroperitoneal approach for adult spinal deformity
Takashi Moriwaki 1 , Sho Fujiwara 1 , Koichi Iwatsuki 1
1 Department of Neuro Spinal Surgery, Osaka Gyoumeikan Hospital, Osaka, Japan
Introduction: Multilevel cMIS from thoracic level for adult spinal deformity is effective for correction in coronal and sagittal planes. To perform LIF between multiple vertebrae from the thoracic level to lumbar level, it is necessary to capture each disc space in parallel. Therefore, we report on cMIS corrective fixation for ASD using multilevel LIF from the thoracic vertebrae by combined mini-open retropleural approach and the retroperitoneal approach. Material and Methods: We enrolled patients who underwent Multilevel cMIS from thoracic level for ASD From by combined mini-open retropleural and retroperitoneal approach, 11 cases (M/F; 4/7, 76.8age) (T-cMIS). We compared surgical and clinical results between Multilevel cMIS from lumbar level, 12 cases (M/F; 3/9, 76.25age) (L-cMIS) and Multilevel cMIS from thoracic level. Results: A total 23 patients underwent multilevel cMIS (T-cMIS, 11 patients; L-cMIS, 12 patients). Surgical and clinical results were F/U (T-cMIS 11.5 m, L-cMIS 15 m), op.time (T-cMIS 673.2 min, L-cMIS 411.1 min (p < 0.05)), blood loss (T-cMIS 547.6 cc, L-cMIS 260.1 cc), pre PI-LL (T-cMIS 40.5, L-cMIS 18.9 (p < 0.05)), post PI-LL (T-cMIS 6.26, L-cMIS 12.2), pre C7-SVA (T-cMIS 134.5 mm, L-cMIS 84.5 mm), post C7-SVA (T-cMIS 47mm, L-cMIS 59.5 mm), PJK (T-cMIS 1/10 case, L-cMIS 3/12 cases), rod breakage (T-cMIS 0, L-cMIS 1). Regarding mini-open retropleural approach, there was no lung or Aorta, vena cava injury. There was 1 case of postoperative transient intercostal neuralgia and 6 cases of partial parietal pleural injury. There were no pneumothorax or organ injuries requiring treatment. Conclusion: Multilevel cMIS from thoracic level for adult spinal deformity by combined mini-open retropleural and retroperitoneal approach is effective for deformity correction and can provide stability.
1320
P108: Return to sporting activities following long fusions to the sacrum in adult spinal deformity
Omri Maayan 1 , Bo Zhang 1 , Mitchell S. Fourman 1 , Anthony Pajak 1 , Hiroyuki Nakarai 1 , Leah Andrews 1 , John Clohisy 1 , Robert Merrill 1 , Jerry Du 1 , Francis Lovecchio 1 , Han Jo Kim 1
1 Hospital for Special Surgery, New York, USA
Introduction: Returning to recreational sporting activities after adult spinal deformity correction may significantly impact patients’ perceived quality of life after surgery. The present study sought to characterize participation in sports activities before and after adult spinal deformity surgery, and to identify factors associated with impaired return to sports. Material and Methods: Patients who underwent thoracolumbar adult spinal deformity surgery between 2016-2021 with ≥1 year follow-up were included (posterior-only, ≥3 levels of fusion to pelvis). A survey evaluated pre- and postoperative participation in sports, the timing of return to these activities, and the reasons for limited sport participation. Differences in demographics, surgical, and perioperative variables between patients who reported improved, unchanged, or worsened activity tolerance were evaluated. Results: Ninety-five patients were included (mean age: 64.3 ± 10.1 years; BMI: 27.3 ± 6.1 kg/m2; mean levels fused: 8 [range 3-16]; mean LL correction 17.8±11.3°). The survey was completed a 43.5 months after surgery. Sixty-eight (72%) patients participated in sports preoperatively. The most common sports were swimming (n = 33, 34.7%), yoga (n = 23, 24.2%), weightlifting (n = 20, 21.1%), elliptical (n = 19, 20.0%), and golf (n = 11, 11.6%). Fifty-seven (83.8%) returned to at least one sport postoperatively, most commonly (45%) 6-12 months after surgery. Elliptical had the highest rate of equal or improved participation (53%). Patients generally returned to below their preoperative level to all other sports. Reasons for reduced sporting activities included physical limitation (51.4%), fear (20.0%), pain (17.1%), and surgeon advice (8.6%). There were no differences in the demographic, surgical, or perioperative characteristics of those who returned to sports at the same or better level compared with those who returned at a lower level. Conclusion: Most patients successfully resumed sporting activities after undergoing fusion to pelvis for adult spinal deformity. However, this return is typically at a lower level of participation compared to their preoperative baselines, particularly in higher demand sports. Understanding trends in sporting activity may be valuable for counseling patients and setting expectations.
1322
P109: Utility of computerized tomography Hounsfield unit measurements to predict proximal junctional kyphosis in adult spinal deformity patients with long constructs
Josephine Coury 1 , Zeeshan Sardar 1 , Justin Reyes 1 , Gabriella Greisberg 1 , Natalia Czerwonka 1 , Matan Malka 1 , Joseph Lombardi 1 , Ronald A. Lehman 1 , Lawrence Lenke 1
1 Och Spine Hospital, Columbia New York Presbyterian, USA
Introduction: Several studies have examined the relationship between low CTHU and postoperative complications. Low CTHU, specifically scores below 159, at the UIV and UIV+1 have been shown to increase the likelihood to develop PJK, pseudarthrosis, and pedicle screw loosening. In contrast, greater CTHU values have been associated with greater osteologic fusion potential at 1 year follow-up. For this study, we aimed to study the relationship of CTHU at the UIV, UIV+1, UIV+2 in patients with long constructs undergoing deformity correction and postoperative complications with a minimum two-year follow-up. Material and Methods: 152 ASD patients were identified retrospectively at a single center. Patients with UIV distal to L2, prior anterior fusion at UIV, or UIV at C2 were excluded. CTHU were measured at the UIV, UIV+1, and UIV+2 of each patient. Statistical analysis was performed with significance set to p < 0.05. Results: 152 patients were identified with 94 primary procedures and 58 revisions with average follow up 2.1 years. 19 patients (12.5%) developed PJK. No significant differences in PJK rate were found based on gender (p = 0.66) and BMI (p = 0.202). Patients who developed PJK were significantly older than those who did not (p = 0.006). Patients undergoing revision surgery had a higher rate of PJK 19.6% (11/56) compared to primary 7.3% (7/96) (p = 0.006177). UIV ranged from C5-L2 with T2 the most common UIV (n = 61). Most of the 19 patients that developed PJK were within 15 months, ranging from 1 week to 3 years postoperatively. For patients with a thoracic UIV who developed PJK, the CTHU at the vertebral levels proximal to UIV was lower on average by 17 per level than the UIV. In contrast, for patients who did not develop PJK, the CTHU was higher by 12 on average in the vertebral levels proximal to UIV (p < 0.00001). At the UIV+1, the relative risk was 0.13 [95% CI: 3.22, 18.98] and number needed to harm was calculated to be 2.91 [95% CI: 2.18, 4.38]. At the UIV+2, the relative risk was 0.16 [95% CI: 2.92, 13.1] and the number needed to treat was 2.39 [95% CI: 1.73, 3.82]. Conclusion: CTHU of less than 160 in the thoracic spine was identified as a risk factor for developing PJK in patients undergoing adult spinal deformity surgery, a higher threshold than recently discussed in the literature. The UIV +1 and +2 CTHU were also identified as important predictors of PJK. Patients with lower HU in vertebral bodies proximal to UIV are at a significantly increased risk of developing PJK in long fusion constructs and surgeons should consider an alternate UIV.
1341
P110: The learning curve for pelvic fixation with the bedrock technique
Christopher Martin 1 , Jason Haselhuhn 1 , Paul Soriano 1 , Jonathan N. Sembrano 1 , Nathan Hendrickson 1 , Kristen Jones 2 , David Polly 1
1 Department of Orthopedic Surgery
2 Department of Neurosurgery, University of Minnesota, Minneapolis, USA
Introduction: Spinal fusion to the sacrum increases the stress on the sacroiliac (SI) joint, and literature has shown an increased rate of new SI joint symptoms with increased length of fusion. Computed tomography (CT) navigated open SI joint fusion using porous triangular titanium rods (TTR) cephalad to S2AI screws has been employed to prevent hardware failure and promote SI joint fusion to decrease the risk of new SI joint pain postoperatively. In our initial 21 cases we found a 7.1% rate of implant malposition requiring intraoperative repositioning. The objective of this study was to determine the rate of intraoperative TTR repositioning at our institution since our experience has grown. Material and Methods: Surgeries in which pelvic fixation was performed via CT navigated open SI joint fusion with TTR cephalad to S2AI screws between 5/1/2019 and 5/27/2021 were reviewed. Operative reports were analyzed and any TTR or S2AI screw repositions that occurred were recorded. Demographic and surgical information and TTR and S2AI specifications were obtained. Height was used as a surrogate for pelvic size. Results: A total of 43 patients (14M:29F) with a mean age of 62.3 ± 11.0 years were included. Average BMI and height were 31.5 ± 7.1 kg/m2 and 1.7 ± 0.1 m, respectively. Cephalad extent of fusion ranged from T4 to L5, with a mean of 4.8 (range 1-14) levels fused. Surgeries were performed by a co-surgeon team in 28 cases and by a single surgeon in 15 cases. 86 TTR were implanted, ranging 7.0-7.5 mm in diameter and 65-90 mm in length. Four (4.6%) TTR were repositioned intraoperatively and one (1.2%) was subsequently removed and replaced with crushed cancellous allograft. All malpositions were medial and/or cephalad. 86 S2AI screws were implanted, ranging 9.5-10.5 mm in diameter and 80-110 mm in length. No (0%) S2AI screws required intraoperative repositioning. In the initial 21 cases, 3/42 (7.1%) TTR required intraoperative repositioning; this decreased in the subsequent 22 cases to 2/44 (4.5%). Conclusion: Stacked pelvic fixation with TTR is technically demanding. Overall, our reposition rate was 5.8%. The initial cohort was 7.1% and the subsequent cohort was 4.5%. This indicates there is a learning curve even with the use of navigation.
1363
P111: The effect of osteoporosis on complications and reoperation rates after surgical management of adult thoracolumbar spinal deformity: a systematic review and meta analysis
Elizabeth Lechtholz-Zey 1 , Mina Ayad 1 , Brandon Gettleman 2 , Emily Mills 1 , Hannah Shelby 1 , Andy Ton 1 , Jeffrey C. Wang 1 , Raymond Hah 1 , Ram Alluri 1
1 Orthopaedic Surgery, Keck School of Medicine of the University of Southern California, Los Angeles, USA
2 Orthopaedic Surgery, University of South Carolina School of Medicine, Columbia, USA
Introduction: While a substantial body of research has explored the impact of osteoporosis on patients undergoing adult spinal deformity (ASD) correction, reports within the literature remain inconclusive. As such, the purpose of this study is to synthesize and analyze the existing array of high-quality investigations pertaining to osteoporosis as a predictor of postoperative outcomes in ASD surgery. Material and Methods: We performed a systematic review and meta-analysis to determine the effect that a diagnosis of osteoporosis has on the incidence of adverse outcomes following surgical correction of ASD. We queried the Medline (PubMed) database from 1990 through August 2022 using the following terms: “osteoporosis” AND “deformity” AND (“outcomes” OR “revision” OR “reoperation” OR “complication”). Patients were defined as having a diagnosis of osteoporosis based on ICD-10 coding or a confirmed diagnosis of decreased bone density on dual-energy X-ray absorptiometry or computed tomography. A data collection sheet was created using the Cochrane Consumers and Communication Review Group's Data Extraction Template for Included Studies. Statistical analysis was performed using Comprehensive Meta-Analysis (Version 2) using a random effects model to account for the heterogeneity between different studies. Results: A total of 36 and 28 articles were included in the systematic review and meta-analysis, respectively. The meta-analysis identified greater rates of screw loosening amongst osteoporotic patients (70.5% vs 31.9%, p = 0.009), as well as decreased bone mineral density in patients who developed proximal junctional kyphosis (0.69 vs 0.79 g/cm2, p = 0.001). Through the systematic review, there was a significantly increased risk of any complication, reoperation, and proximal junctional failure associated with reduced bone density. Outcomes that did not seem to differ between the two groups include fusion rates, readmission rates, and patient-reported and/or functional outcome scores. Conclusion: This study summarizes the literature comparing outcomes between patients with and without osteoporosis and establishes a higher incidence of screw loosening, proximal junctional kyphosis, and revision surgery amongst osteoporotic ASD patients. Preoperative pharmacotherapy with anti-osteoporotic medications may have impacted the findings across the included articles, so future research should consider stratifying patients based on treatment status. In addition, future investigations should prioritize reporting of outcomes at various follow-up intervals in order to better characterize how risk changes with time and to tailor preoperative planning based on patient-specific characteristics.
1375
P112: Prevalence of total joint arthroplasty in the adult spinal deformity population
Dustin Kress 1 , Dylan Thomas 1 , Jason Haselhuhn 1 , David Polly 1,2
1 Department of Orthopedic Surgery, University of Minnesota, Minneapolis, USA
2 Department of Neurosurgery, University of Minnesota, Minneapolis, USA
Introduction: The spine, hip, and knee are anatomically and biomechanically connected. Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are commonly employed to treat degenerative changes in the hip and knee, while fusion is used for degeneration of the spine. Spine deformity correction results in changes in sagittal alignment and pelvic parameters, and patients with stiff spines have higher rates of THA dislocation and revision due to instability. The prevalence of total joint arthroplasty (TJA) was previously estimated to be 2.35% in the general population, but there is no data in the literature on the prevalence in adult spinal deformity (ASD) patients. Thus, the goal of this study was to determine the prevalence of TJA in ASD patients at our institution. Material and Methods: Following Institutional Review Board approval, we retrospectively reviewed a list of cases performed by the senior author from 4/2017-5/2021. Patients > 18 years old undergoing pre-operative evaluation for ASD were included. Patients < 18 years old, those diagnosed with adolescent idiopathic scoliosis, and non-fusion cases were excluded. Pre-operative full-length standing radiographs were examined for the presence or absence of THA, TKA, or both. Demographic data was collected from patient electronic medical records and statistical analyses completed. Results: 572 consecutive cases were reviewed, and 322 were excluded. 250 cases (97M:153F) were included in final analysis, with a mean age of 61.8 ± 11.2 years. A total of 74 patients had a TJA (29.4%). THA was present in 41 patients (16.4%), and TKA was present in 49 patients (19.6%). Males had a higher prevalence of TJA, THA, and TKA (29.9%, 16.5%, and 21.6%) than females (29.4%, 16.3%, and 18.3%). Conclusion: This study revealed a high prevalence of TJA in ASD patients at our institution. This rate surpasses the estimated prevalence amongst the general population. Surgeons must be aware that many ASD patients have a preexisting TJA and account for potential changes in spinopelvic alignment after deformity correction to avoid complications such as dislocation.
1435
P113: Selection of fusion level in osteoporotic vertebra compression fracture (OVCF) with spinal kyphosis: the importance of Hounsfield Unit
Junyu Li 1,2,3 , Yiqiao Zhang Zhang 1,2,3 , Xueshi Tian Tian 1,2,3 , Zhuo Ran Sun 1,2,3 , Yongqiang Wang 1,2,3 , Miao Yu 1,2,3 , Weishi Li 1,2,3 , Yan Zeng 1,2,3
1 Peking University Third Hospita, China
2 Engineering Research Center of Bone and Joint Precision Medicine, China
3 Beijing Key Laboratory of Spinal Disease Research, China
Introduction: The treatment of Osteoporotic Vertebral Compression Fracture (OVCF) has become more prevalent. However, severe osteoporosis, high postoperative mechanical complications and adjacent segment degeneration (ASD) increased the difficulty and challenge, which made it difficult to develop a unified standard on how to select the fusion level. Recently, many studies have suggested that the HU value should be taken into account when making a surgical decision, because of its excellent reflection of regional bone mineral density. But for OVCF patients with severe osteoporosis, whether the HU value of the vertebras also made sense to the selection of fusion level and internal fixation need further study. For the first time, we defined that upper maximal vertebra (UMV) was the vertebra above the compressed section, and that had a higher HU value than two vertebras proximal to the fracture level. Also, upper sagittal reverse vertebra (USRV) was defined as the first vertebra that presented opposite from anterior to posterior part of the vertebra with proximal vertebras, counting up from the compressed vertebra. For example, if all the posterior HU values of T8 to T11 were higher than that of anterior parts except T9, whose anterior HU value was higher, then T9 was the USRV. Corresponding to difference in images, we believed that UMV and USRV might play an important role in the biomechanical stability of the spine. Therefore, the purpose of this retrospective study is to verify whether locating upper instrumented vertebra (UIV) on upper maximal vertebra (UMV) or upper sagittal reverse vertebra (USRV) can decrease the risks of ASD and proximal junctional kyphosis (PJK). Material and Methods: This clinical research selected 70 OVCF patients received surgeries between April 2006 and November 2021. Whole spine CT were obtained for each patient. Patients were divided into groups according to whether their UIV was UMV or USRV. Incidence of ASD and PJK were evaluated in subgroups. Results: 70 patients (13 males and 55 females) with a mean age of 63.60 ± 7.878 years and mean follow-up of 54.19 ± 20.59 months met the study inclusion criteria. Among all the cases L1 (28.6%) was the most common compressed vertebra, followed by T12 (24.3%). The average HU value of all patients was 76.57 ± 36.79. And the average of duration of surgy, peroperative bleeding and hospital stays were 364.53 ± 173.10 minutes, 1135.48 ± 796.99 milliliter and 10.41 ± 4.27 days respectively. For UIV, the UIV of 25 OVCF patients were located on UMV while 45 patients were not. There was a significant difference in the rate of ASD (p = 0.004) and PJK (p = 0.017) between 2 groups. 55 patients (78.57%) were identified the exist of USRV. UIV of 16 patients were located on USRV while 39 UIV did not. There was a significant difference in the rate of ASD between two groups (p = 0.005). Conclusion: HU value should be taken into consideration in selection of UIV. Locating UIV on UMV decreases the incidence of PJK and ASD, while taking USRV into fusion level reduce the occurrence of ASD.
1532
P114: The evaluation of association between paraspinal muscles degeneration and postoperative complications in osteoporotic vertebral compression fracture patients with kyphosis deformity
Junyu Li 1 , Zimo Wang 1 , Gengyu Han 1 , Zhuo Ran Sun 1 , Yongqiang Wang 1 , Miao Yu 1 , Yan Zeng 1 , Weishi Li 1
1 Orthopaedics, Peking University Third Hospital, Beijing, China
Introduction: Osteoporotic vertebral compression fracture (OVCF) causes pain, kyphosis and neurological damage, which significantly affect patients’ quality of life. Patients with OVCF are often elderly and have severe osteoporosis, which makes surgery more challenging and the incidence of postoperative complications high. The paraspinal muscles have been well studied in adult spinal deformities, but there is no conclusive evidence that their findings can be applied to OVCF. The purpose of this study was to evaluate the association between paraspinal muscle parameters including fat infiltration (FI) and relative functional sectional area (rFCSA) and the incidence of common OVCF postoperative complications. Material and Methods: 80 patients undergoing surgeries for OVCF were included. The selected posyoperative complications are ASD, screw loosening, PJK and DJP. Paraspinal muscle parameters FI, relative gross-sectional area (rGCSA) and rFCSA of multifidus were measured at corresponding fracture segment. To study the association between paraspinal muscle degeneration and complications, patients are divided into two groups according to whether each complications occur. The relevance between muscle parameters and CT values were evaluated in this study. Results: MF FI was significantly higher in ASD group (p = 0.001), screw loosening group (p = 0.050), DJP group (p = 0.006) and PJK group (p = 0.043). MF rFCSA were significantly smaller in ASD group (p = 0.032) and DJK group (p = 0.021). Conclusion: Higher MF FI is associated ASD, screw loosening, PJK and DJK in patients with OVCF. Small MF rFCSA is associated with ASD and DJP. The use of cemented screws and perioperative paravertebral muscle exercises can prevent or reduce postoperative complications. For OVCF patients with high FI and low rFCSA of the multifidus muscle, it is necessary to use more stable internal fixation systems, such as bone cement-reinforced screws, to avoid postoperative loosening of the implant. At the same time, it is necessary to take rehabilitation training for lumbar and back muscle strength after surgery to improve paravertebral muscle function.
1548
P115: 20 hours to become good at anything? Pedicle Screw Insertion - a training concept
Bethan Armes 1 , Sebastian Siller 2 , Sarah Abbott 2 , Bisola Ajayi 2 , Mathew Gallagher 2 , Jason Bernard 2 , Timothy Bishop 2 , Darren Lui 2
1 St George's University of London, London, United Kingdom
2 Department of Neurosciences, Complex Spinal Surgery, St George's Hospital, London, United Kingdom
Introduction: It is becoming increasingly important for medical training to be more efficient, partly due to restrictions like the European Working Time Directive, enforcing a 48-hour working week, limiting the number of hours available for training. J. Kauffman, the author of ‘The First 20 hours’, shows you can accelerate learning to be good at anything in 20 hours, based on K. Anders-Ericsson’s psychological study, showing a person requires 10,000 hours to become an expert in a field. Applying the 20 hours of accelerated learning to surgical training can help combat the issue with reduced hours for training so trainees can become competent and confident. Material and Methods: Eight junior Spinal Surgeons and one control Candidate (Physiotherapist) attended a Cadaveric Pedicle Screw Insertion Course with 20 hour focused training. Competence pre-and post-course questionnaire (Likert scale) was conducted. Each candidate had 2 cadavers. Examination of left/right Thoracic Screw, Lumbosacral, Cervical screw insertion by time was measured. Complications such as pedicle breaches were recorded by a senior trainer after screw removal with a ball tipped probe. Results: Candidate mean time Thoracic were: 96.8; 72.2; 61.4; 57.4 minutes with mean pedicle errors 2.6; 2; 2.1; 2.2. Mean Lumbar: 51.9; 50.1; 42.0; 33.7 minutes with mean errors: 0.2; 0.3; 0.7; 0.2. Mean Cervical: 43.6; 44.9 minutes and mean errors: 1.2; 0.3. Control Thoracic: 142, 134, 145, 93 minutes; Control Lumbar: 92, 93; 65; 60 minutes Candidates Total Mean Pre-course Competence; 5.41, post-course; 7.35 and change in score; +1.94 Control: Pre 2.4; Post:5.0; Change: +2.6. Conclusion: Pedicle screw insertion can cause significant morbidity, including paralysis, and therefore is not an easy skill to acquire or practice. This focused pedicle screw course showed that a junior spinal surgeon can achieve improved competency, effectiveness and efficiency in 20 hours but furthermore a complete novice can learn to be competent.
1573
P116: Is there utility for preoperative carotid Dopplers in adult spinal deformity?
Matan Malka 1 , Prerana Katiyar 1 , Yong Shen 1 , Grant Feuer 1 , Justin Reyes 1 , Joseph Lombardi 1 , Zeeshan Sardar 1 , Lawrence Lenke 1
1 Orthopedic Surgery, Columbia University Medical Center, New York, USA
Introduction: Carotid stenosis is a comorbidity that may be exacerbated during adult spinal deformity (ASD) surgery leading to postoperative complications such as a transient ischemic attack (TIA) or cerebrovascular accident (CVA). Preoperative doppler ultrasound studies may be of utility to identify carotid stenosis and assess the extent of stenosis to optimize preoperative planning. However, given the low rate of CVA complications postoperatively in the spine patient population, the utility of these studies as a screening tool is not known. Thus, this study aims to assess the utility of performing preoperative bilateral carotid doppler studies to prevent postoperative CVAs. Methods: A consecutive cohort of 265 patients undergoing ASD surgeons by two surgeons at a single institution between the years 2017-2022 was retrospectively reviewed. The official read and assessment of the extent of the carotid stenosis in the radiology report was used for. Results of the carotid duplex ultrasound were classified as mild or no stenosis (0-49%), moderate carotid stenosis (50-69%), severe carotid stenosis (70-99%), and occluded carotids (100%). For patients with above 50% stenosis, further chart review was done to note any preoperative intervention and a two-year follow-up to assess for any postoperative complications. Postoperative complications included mortality, TIA, and CVA, where a CVA was defined as any new neurological deficit caused by impaired blood supply to the brain with a duration of > 24 hours. Otherwise, the neurological deficit was noted as a TIA. Results: Among the 265 patients who underwent ASD surgeries, 102 (38.49%) had preoperative carotid duplex ultrasound studies. The patients who had pre-operative studies were older (p < 0.001) and had a higher rate of smoking history (p = 0.029). 93 patients (91.2%) were found to have < 50% stenosis bilaterally. Overall, 6 patients (5.9%) had 50-69% carotid stenosis on either internal carotid artery (ICA), 2 (2.0%) had stenosis bilaterally. None of the patients had > 70% stenosis, unilaterally or bilaterally. 3 patients (2.9%) had an indeterminate read, according to the radiology department, but did not have a repeat study. None of the patients underwent any intervention for the stenosis before surgery. 50 patients (49.02%) had two-year follow-up data, none of which had a postoperative complication of any type at two-year follow up. Conclusions: The preoperative incidence of carotid stenosis was 8.8%, with no preoperative interventions done. There were no postoperative complications. Therefore, preoperative carotid doppler studies are of limited utility.
1618
P117: Risk factor for postoperative coronal imbalance after surgical correction of adult spinal deformities: a systematic review with pooled analysis
Marco Manzetti 1 , Francesca Barile 2,3 , Giovanni Viroli 1 , matteo traversari 1 , Marco Ialuna 1 , fabio vita 1 , Alberto Ruffilli 1 , Cesare Faldini 1
1 Ist Traumatologic and Orthopedic Clinic, IRCCS - Istituto Ortopedico Rizzoli, Bologna, Italy
2 G Spine 4, IRCCS Galeazzi - Sant'Ambrogio, Milan, Italy
3 DIBINEM Dipartimento di Scienze Biomediche e Neuromotorie, Bologna, Italy
Introduction: Maintaining or restoring global alignment is a key goal of adult spinal deformity (ASD) surgery. Achieving this goal improves clinical and functional outcomes avoiding mechanical complications; indeed, both sagittal and coronal imbalance negatively affect outcomes and patient satisfaction. However, while much attention has been paid to studying sagittal plane less has been devoted to the coronal balance. Recent literature indicates that greater postoperative coronal imbalance (CIB) is associated with lower outcomes, higher pain, and higher risk of complications. Therefore, achieving good balance on the coronal plane when addressing ASD should be considered an important objective. Aim of the present study is to identify preoperative risk factors for postoperative coronal imbalance in patients who undergo surgical correction for adult spinal deformities. Material and Methods: A systematic search of articles about risk factors for postoperative coronal imbalance was conducted on electronic databases (Pubmed, EMBASE and Cochrane Library) according to the PRISMA guidelines. Studies were included if they: included patients with a diagnosis of adult scoliosis (both adolescent idiopathic scoliosis in adult and degenerative scoliosis), analysed risk factors for postoperative coronal imbalance The methodological quality of the included articles was assessed using the Institute of Health Economics Quality Appraisal (IHEQA) Checklist for Case Series Studies. Data about population (demographics, diagnosis, follow-up), pre and postoperative radiographical and clinical data, surgical procedure details and complications were extracted and summarized. Meta-analysis was performed when there were at least three studies to be compared. Heterogeneity was assessed using the Inconsistency statistic (I2 > 75% was considered as high). Random-effects models (using restricted maximum likelihood estimators) were used to calculate the odds ratios and statistical parameters (95% confidence interval, regression slopes and intercepts). Results were represented with forest plots. p-value < 0.05 was considered significant. Results: Nine studies and a total of 838 patients were included. All included studies were of acceptable quality (> 14 yes responses at IHEQA checklist). Pooled incidence of postoperative coronal imbalance (CIB) was 26% (CI 95% [0.20, 0.32]). When stratifying patients by preoperative C7-CVA (preoperatively balanced vs imbalanced patients), the incidence of postoperative CIB was not significantly different between the two groups (Weighted Mean Difference (WMD) -0.86 CI 95% [-2.07, 0.34] p = 0.16). Preoperative sagittal vertical axis (SVA) and type C unbalance (trunk shift towards convexity) resulted to be the only primary risk factors for iatrogenic CIB (WMD 0.55 CI 95% [0.21, 0.90], p = 0.002, and (OR 2.10 CI 95% [1.29, 2.91], p < 0.001, respectively). Conclusion: Baseline evaluation of global alignment of the patient is of outmost importance when planning surgery for adult spinal deformities. Type C coronal unbalance (trunk shifted towards convexity of the main curve) and increased preoperative SVA put the patient at risk of postoperative coronal imbalance. Intraoperatively, care should be taken to properly correct lumbosacral fractional curve.
1700
P118: High grade spondylolisthesis - Can we dodge Lamartina
Mukhesh Thangavel 1 , Charanjit Singh Dhillon 1
1 Spine Surgery, MIOT Internation Hospital, Chennai, India
Introduction: High-grade spondylolisthesis, characterized by Meyerding grade III or IV with over 50% slippage, often presents with neurologic compromise, particularly at the L5-S1 level, commonly attributed to isthmic spondylolisthesis. The treatment approach has traditionally focused on correcting segmental lordosis and global sagittal balance. In 2001, Lamartina introduced a technique to address sagittal imbalance through the formulation of an instability square. Material and Methods: This study aimed to investigate whether the Lamartina principle could be safely ignored to preserve motion segments. A retrospective analysis was conducted on 50 patients with high-grade (grade three and above) spondylolisthesis who underwent all posterior single-stage single-level reduction and fixation over the past two decades. The evaluation included pain relief, neurological improvement, fusion rates, reduction loss, sagittal balance, and adjacent segment degeneration. Results: Complete reduction of spondylolisthesis was not achieved in all high-grade cases; instead, the focus was on achieving acceptable sagittal balance and addressing symptoms. More than 80% of follow-up patients demonstrated positive outcomes based on our defined criteria when treated with all posterior single-stage single-level reduction and fixation for high-grade spondylolisthesis. This study was conducted at a single center and lacked a control group. Some patients were excluded due to insufficient clinical data or lost follow-up. Conclusion: Managing high-grade lumbosacral spondylolisthesis remains a complex issue with ongoing controversies. While surgical treatment is generally agreed upon for symptomatic patients experiencing severe pain, neurologic deficits, or progressive deformity, the optimal surgical approach and techniques remain subjects of debate. While the Lamartina principle has gained widespread acceptance in high-grade spondylolisthesis management, our study suggests that acceptable outcomes can also be achieved through all posterior single-stage single-level reduction and fixation for this condition.
1801
P119: The efficacy of halo traction in the treatment of patients with severe and rigid scoliosis
Murat Korkmaz 1 , Yekta Furkan Altin 1 , Taha Furkan Yağci 1 , Turgut Akgul 1
1 Orthopedics, Istanbul Faculty of Medicine, Fatih, Turkey
Objective: Many challenging factor in the treatment of pediatric patients with severe and rigid scoliosis has been desrcibed. It is known that preoperative halo traction reduces several surgical risks. In this study, we aimed to show the efficacy of preoperative halo traction in the treatment of severe and rigid scoliosis. Methods: Patients with severe and rigid scoliosis before whose surgery halo traction was placed, were analysed retrospectively. Traction force was increased gradually up to 50% of body weight by halo traction that was applied under general anaesthesia. During treatment, patients' major coronal curvature, thoracal kyphosis, and T1-L5 length at the coronal plane were measured 3 different times, that are before halo traction, in the 3rd week of the treatment and just before definitive surgery. Results: 5 patients (mean age was 12.8) were retrospectively evaluated. Before halo traction major coronal curvature was 112°, thoracal kyphosis was 78.6° and T1-L5 height was 261 mm. The mean traction period was 43 days. There was a statistically significant change between pretraction, 3rd week, and posttraction values. It was observed that 85% of the improvement in the Cobb angle, 100% of thoracic kyphosis, and 84% of the T1-L5 length were achieved after 3 weeks of halo traction. Pin site infection developed in one patient and was treated with oral antibiotics. There was no neurological complication. Conclusions: Halo traction provides a statistically significant improvement in the coronal and sagittal plane deformities of patients with severe and rigid scoliosis, before definitive surgery. It was observed that approximately 85% of the improvement was achieved after the first three weeks. Therefore, whereas the use of halo traction for at least three weeks is recommended in these patients, the improvement after three weeks was not found to be statistically significant.
1853
P120: What factors are associated with post-operative coronal imbalance after adult spinal deformity surgery? Result of a retrospective study on 127 patients
Matteo Traversari 1 , Francesca Barile 1 , Alberto Ruffilli 1 , Giovanni Viroli 1 , Marco Manzetti 1 , Marco Ialuna 1 , Cesare Faldini 1
1 Clinica Ortopedica 1, Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Adult Spinal Deformity (ASD) surgery has the main goal of maintaining or restoring global alignment. Both sagittal and coronal imbalance (CIB) have a negative impact on post-operative outcomes, resulting in decreased patient satisfaction and increased disability. Postoperative CIB is associated with pain, loss of function, and decreased quality of life. This is mainly due to the paucity of compensatory mechanisms to coronal decompensation, especially when the spinal fusion is extended distally to the pelvis. Up to date there is not a substantial consensus regarding the influence of pre-operative radiographic parameters on post-operative CIB. The aim of the present study is to elucidate preoperative risk factors for inadequate correction of coronal imbalance and/or occurrence of iatrogenic postoperative CIB in patients who underwent surgery for ASD. Material and Methods: A retrospective review of adults who underwent posterior spinal fusion (> 5 levels) for ASD was performed. Inclusion criteria were age at surgery > 18 years; diagnosis of ASD Aebi types 1 or 2, coronal Cobb angle of main curve > 30°, posterior spinal fusion of at least 5 levels with all pedicle screws constructs extended distally to L5 or below. Patients were divided into groups according to the Nanjing classification: type A (CSVL < 3 cm), type B (CSVL > 3 cm and C7 plumb line shifted to major curve concavity), and type C (CSVL > 3 cm and C7 plumb line shifted to major curve convexity). They were also divided according to postoperative coronal balance in balanced (CB) vs. imbalanced (CIB) and according to iatrogenic coronal imbalance (iCIB). Preoperative, postoperative, and last follow-up radiographical parameters and intraoperative data were recorded. A multivariate analysis was performed to identify independent risk factors for CIB. Results: A total of 127 patients were included. Preoperatively, most patients (85/127, 67%) had Type A coronal alignment, while 30 (23.6%) were shifted to the concavity of the main curve (type B) and 12 (9.4%) were shifted to the convexity (type C). Pre-operative L4-S1 Lumbosacral Fractional (LSF) curve and L4 and L5 tilt were not significantly different between the groups. Type C patients showed higher post-operative L4 tilt (15.7 ± 5.2, p = 0.005) and a higher risk of postoperative CIB (p = 0.04). Multivariate regression analysis indicated L5 tilt angle as a preoperative risk factor for CIB (p = 0.007) and indicated L5 tilt angle and age as a preoperative independent risk factors for iatrogenic CIB (p = 0.01 and p = 0.008). Conclusion: Patients with a preoperative trunk shift towards the convexity of the main curve (type C) are more prone to postoperative CIB and leveling the L4 and L5 vertebrae may be the key to achieve coronal alignment preventing the “takeoff phenomenon”. Surgical correction of type C patients requires dosed correction of main curve and lumbosacral fractional curve. In cases of severe stiffness of lumbosacral fractional curve, asymmetrical three-columns osteotomies of lower lumbar levels may be a feasible procedure in order to obtain an acceptable coronal balance.
1870
P121: Association between chronic preoperative opioid utilization and perioperative complications, reoperations, and readmissions after multilevel spinal fusion (>6 levels) for adult spinal deformity
Aboubacar Wague 1 , Anna Filley 1 , Avionna Baldwin 1 , Khuzaima Rangwalla 1 , Sigurd Berven 1
1 Department of Orthopaedic Surgery, University of California, San Francisco, San Francisco, USA
Background: Almost one-third of patients with complex spinal deformities report chronic use opioid medication to manage symptoms. However, there remains a paucity of information regarding the effects of chronic opioid use on surgical outcomes after complex spinal fusions. The purpose of this study is to assess whether chronic opioid use is associated with perioperative complication rates, readmission rates, and length of hospital stay after multilevel spine fusion. Methods: This retrospective cohort study included a consecutive series of patients from a single institution undergoing primary multilevel spinal fusion (≥ 6 levels) for adult spinal deformity between December 2017 and December 2019. Patients were included if they had ≥ 3 months of preoperative data and age ≥45 years. Patients were categorized according to preoperative opioid prescription information available in the electronic medical record. Chronic Opioid Users (COU) had prescribed opioid use of ≥ 3 continuous months prior to surgery. We controlled for variables that may be independent predictors of postsurgical outcomes including age, gender, co-morbidities, duration of surgery, and surgical invasiveness score (SSI). Results: Of 442 patient records reviewed, 135 were Non-Chronic Opioid Users (NOU) and 307 were COU prior to surgery. The COU cohort was found to have significantly higher ASA scores [2.56 ± 0.52 vs. 2.39 ± 0.55, p = 0.001], and more patients with depression/anxiety [26.1% vs. 14.8%, p = 0.008] compared to the NOU cohort. There was no difference between the groups regarding other co-morbidities including, preoperative neural symptoms [30.3% vs. 31.9%, p = 0.742], cardiovascular disease [76.9% vs. 76.3%, p = 0.889], osteoporosis [75.2% vs. 77.0%, p = 0.685], and obesity [43.6% vs. 41.5%, p = 0.675]. Comparison of opioid morphine milligram equivalence (MME) between the two groups revealed that the COU cohort utilized significantly higher prescription dosages of opioids at the time of surgery [53.9 ± 78.9 vs. 24.6 ± 31.5, p < 0.001]. Regarding postoperative outcomes, the COU cohort had a significantly longer mean length of hospital stay [9.07 days ± 4.37 vs. 8.20 days ± 3.98, p = 0.041] and lower rates of 90-day infections [3.91% vs. 8.89%, p = 0.043]. No differences were observed in discharge disposition or in 30-day and 90-day readmissions and other complications. Conclusion: Our findings suggest that chronic preoperative opioid use is associated with increased length of stay after multilevel spinal surgery for adult spinal deformity and non-significant for 30-day and 90-day complications and readmission. Consideration of additional factors, such as Social Determinants of Health, may aid in detecting additional risk factors that significantly impact surgical outcomes in this patient population.
2188
P122: Comparative study of two reconstruction procedures for osteoporotic thoracolumbar vertebral fracture with neurologic deficits: posterior single approach versus anterior and posterior combined approach
Yuichi Ono 1 , Yuji Kasukawa 1 , Daisuke Kudo 1 , Hayato Kinoshita 1 , Ryota Kimura 1 , Michio Hongo 1 , Naohisa Miyakoshi 1
1 Orthopedic Surgery, Akita University Graduate School of Medicine, Akita, Japan
Introduction: Osteoporotic vertebral fractures sometimes cause delayed neurological symptoms due to progressive vertebral compression. Surgical techniques for osteoporotic vertebral fractures are still controversial, but in cases of vertebral endplate damage, severe vertebral body collapse or severe local kyphosis deformity, anterior column reconstruction is required. The aim of this study is to compare surgical invasion, clinical and radiological outcomes 2 years after surgery between two reconstruction procedures for osteoporotic thoracolumbar vertebral fracture with neurologic deficits; posterior single approach with posterior vertebral column resection, and anterior/posterior combined surgery. Material and Methods: The study design was a retrospective cohort study. The subjects were 38 patients (74.7 ± 7.2 years, 6 males and 32 females) who underwent anterior column reconstruction for osteoporotic vertebrae in the thoracolumbar transition (Th10-L3) with neurological symptoms at four associated hospitals in Akita Prefecture from January 2011 to October 2022 and followed up over two years. Medical record data were used for a retrospective study. 22 patients underwent anterior and posterior combined surgery (group X) and 16 patients underwent posterior alone (group P). Patients with high-energy trauma, pathological fractures, vertebroplasty or previous thoracolumbar spine surgery were excluded. Re-operation rate within two years after surgery, surgical complications, clinical outcomes (operative time, blood loss, Frankel classification, activities of daily living [ADL]), and sagittal alignment were investigated. Results: The re-operation rate within two years after surgery was 9.1% (2 cases) in group X and 12.5% (2 cases) in group P. Intraoperative blood loss was significantly lower in group X (297.5 ± 244.4 ml) than in group p (408.4 ± 235.5 ml). There were no significant differences in operative time, local kyphosis angle, angle of corrected loss, ADL and Frankel classification at preoperative, postoperative and 2 years postoperative. Conclusion: Anterior/posterior combined surgery might be less invasive than posterior single approach with posterior vertebral column resection, but there was no difference in post-operative results between the two procedures. It was considered useful to understand the characteristics of each technique and to use both techniques in different cases.
2235
P123: Gradual anterior column lengthening at the level of PVCR provides both regional and global ideal sagittal alignment and prevents iatrogenic neurological deficit
Hamisi Mraja 1 , Halil Gok 1 , Cem Sever 1 , Tunay Sanli 1 , Selhan Karadereler 1 , Meric Enercan 1 , Azmi Hamzaoglu 1
1 Orthopedics and Traumatology, Scoliosis-Spine Center Istanbul, İstanbul, Turkey
Introduction: The correction technique of rigid kyphosis should be different from correction of relative flexible deformity. Rigid kyphosis causes pain, deformity progression and deteriorating neurological deficit. We aimed to evaluate the efficacy, safety and clinical results of gradual sequential posterior compression and simultaneous anterior lengthening technique following PVCR for the correction of rigid kyphotic deformity in adults. Methods: From 2000 through 2021, an analysis of patients who underwent PVCR for severe rigid kyphotic and kyphoscoliotic were evaluated. Following PVCR, correction technique included anterior column lengthening with gradual posterior compression sequentially and placement of an expandable cage anteriorly to prevent any dural buckling. Preoperative, postoperative, and final follow-up clinical and radiological analysis were performed. Results: 73 pts (23M, 50F), mean age 46.3 yrs (20-81). Mean follow-up was 8.9 (2-23) years. Etiologies included posttraumatic kyphosis (26 pts), neglected kyphosis and kyphoscoliosis (23 pts), congenital kyphosis (11 pts) and proximal junctional failures (PJF) (13pts). Rigid kyphosis/kyphoscoliosis deformity was located at cervicothoracic-upper thoracic (11), thoracic (25), thoracolumbar (32), and lumbar (5) spine. 39 pts had undergone primary surgery and 34 pts had revision surgery. Preop local kyphosis angle (LKA) restored from 62.4° to 16.9° (72.7%) and preop thoracic kyphosis (TK) restored from 76.6° to 42.3°. All sagittal parameters including SVA, cSVA, C2 slope, T1 slope, and TPA improved significantly. 28 pts who had preoperative neurologic deficit (14 ASIA D, 8 ASIA C, 6 ASIA B) had at least one grade improvement at the final follow-up. Most common complication was dural tears in 12 (16%) pts. Oswestry functional scores decreased from a mean of 62 to 14. Solid fusion was achieved in all patients without significant loss of correction at the final follow-up. Conclusion: Gradual anterior column lengthening at the level of PVCR provides both regional and global ideal sagittal alignment and avoids iatrogenic neurologic deficit by preventing dural bucking. This technique provides ideal restoration of kyphosis, decompression of neural structures, improves preoperative neurological deficit and iatrogenic neurological deficit.
2301
P124: Antibiotic use in spine deformity surgery: results from the AO spine surveillance of the management of patients with adult spine deformity
Brett Rocos 1 , So Kato 2 , Stephen Lewis 3 , Christopher Shaffrey 1 , Lawrence Lenke 4
1 Division of Spine Surgery, Duke University Hospital, Durham, USA
2 Department of Orthopaedic Surgery, University of Tokyo, Tokyo, Japan
3 Orthopaedic Surgery, Toronto Western Hospital, Toronto, Canada
4 Department of Orthopaedic Surgery, The Och Spine Hospital, New York, USA
Introduction: The perioperative use of prophylactic antibiotics remains a topic of debate amongst clinicians caring for patients undergoing complex adult spine deformity surgery. In order to bring clarity to the difficult situation, this study seeks to evaluate the evidence for these strategies and to understand the current trends in prophylactic antibiotic use during ASD surgery through an international survey, in order to feed later consensus guidelines. Material and Methods: An online survey was conducted among international AO Spine members regarding the peri-operative management of patients with ASD. The details of perioperative systemic and topical antibiotic use were solicited. Descriptive data were summarized for the responding surgeons who perform at least 10 long-segment fusions of > 5 levels extending to the pelvis annually. Results: The literature supports the use of prophylactic antibiotic effective against gram positive organisms. The use of topical vancomycin remains debated, and there is limited evidence for topical tobramycin use. A total of 116 responses were received. 74 (64%) surgeons use topical vancomycin, most usually deep to the fascia only 45 (61%). The most usual dose used is 1-2g. 4 (3%) surgeons use topical tobramycin deep to fascia. Following surgery, 90 (78%) surgeons use prophylactic cephalosporin with 3 (3%) using cloxacillin, 5 (4%) using ciprofloxacin and 9 (8%) using vancomycin and 6 (5%) using clindamycin either in addition or alone. Conclusion: The present survey identifies a trend towards systemic and topical antibiotic prophylaxis primarily targeted at gram positive pathogens. The use of topical tobramycin, proposedly effective against gram negative infections, remains uncommon. There is a lack of consensus in the selection of perioperative antibiotic prophylaxis, thus a prospective study of the rates of infection with each strategy would be useful to inform guidelines.
2302
P125: Opioid use at baseline is associated with greater baseline and 2 year back pain scores in older patients undergoing adult spinal deformity surgery
Brett Rocos 1 , Juan Pablo Sardi 2 , Anastasios Charalampidis 3 , Jeffrey Gum 4 , Stephen Lewis 5
1 Division of Spine Surgery, Duke University Hospital, Durham, USA
2 Department of Neurosurgery, University of Virginia, Charlottesville, USA
3 Department of Orthopaedic Surgery, Spine Program, Karolinska University Hospital, Stockholm, Sweden
4 Orthopaedic Surgery, Norton Leatherman Spine, Louisville, USA
5 Orthopaedic Surgery, Toronto Western Hospital, Toronto, Canada
Introduction: Opioids are commonly prescribed to provide some pain relief and to allow for functional improvement in patients with back pain. The purpose of this study was to assess and compare patient reported pain outcomes in older patients undergoing spinal deformity surgery, with the hypothesis being that pre-operative opioid use affects self-reported post-operative pain scores in elderly patients undergoing this complex procedure. Material and Methods: Patients ≥ 60 years of age from 12 international centers undergoing spinal fusion of at least 5 levels for spinal deformity were included. Pain scores were collected using a Numeric Rating Scale (NRS) for both back and leg pain. Opioid use was defined as the consumption of prescribed opioid drugs and from question 11 from the SRS 22r questionnaire. The patient reported outcome scores for leg and back pain at 2 years were compared to the baseline scores. Results: 219 patients were eligible for inclusion. There were 176 (80.4%) females, and the mean age was 67.5 years. 75 (34%) patients reported opioid (Opioid) use pre-operatively of which 63 reported an NRS for back pain and 61 reported NRS for leg pain at 2 years. 144 patients (NoOpioid) denied opioid use at baseline of which 114 reported an NRS for back pain and 113 an NRS for leg pain at 2 years. The baseline back pain NRS was 7.0 (SD 2.0) in the Opioid group compared to 5.7 (2.8) in the NoOpioid group (p = 0.001). The baseline NRS for leg pain was 4.8 (3.4) in the Opioid group compared to 4.0 (3.3) in the NoOpioid patients (p = 0.159). At 2 years, NRS for back pain was 3.2 (2.5) in the Opioid group and 2.3 (2.6) in the NoOpioid group (p = 0.012), whilst NRS for leg pain was 2.2 in the Opioid group and 2.4 in the NoOpioid group (p = 0.63). At 2 years, 39.1% (25/64 patients) of the Opioid group were no longer taking opioids while 16/115 patients (13.9%) of the NoOpioid group reported taking opioids. Conclusion: Despite using pre-operative opioids, patients on opioids had significantly more back pain at baseline that persisted to 2 years of follow up. Leg pain NRS were similar in those with and without opioid use pre-op. Both Opioid and NoOpioid groups benefitted from the surgery as noted by improvements in the NRS scores at 2 years. Close to 40% of opioid users no longer required them at 2 years.
2337
P126: The Roussouly classification in adult spinal deformity: are lumbar lordosis apex and upper/lower lordosis arcs predictors of outcomes?
Hani Chanbour 1 , Graham Johnson 1 , Jeffrey Chen 2 , Jacob Jo 1 , Tyler Metcalf 3 , Iyan Younus 1 , Soren Jonzzon 1 , Steven G. Roth 4 , Adam Wegner 5 , Amir Abtahi 6 , Byron Stephens 6 , Scott Lawrence Zuckerman 1
1 Neurosurgery, Vanderbilt University Medical Center, Nashville, USA
2 Neurosurgery, Baylor college of Medicine, Houston, USA
3 Orthopedics, Ohio State University, Ohio, USA
4 Orthopedics, New York Presbyterian Hospital, New York, USA
5 Orthopedics, Orthovirginia, Virginia, USA
6 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: According to the Roussouly classification, the lordosis apex can be at any vertebrae or disc space, and spinal lordosis involves an upper and lower arc. In patients undergoing adult spinal deformity (ASD) surgery, we sought to: 1) report the preoperative/postoperative lordosis apex and number of vertebrae in the upper/lower arc of lordosis, and 2) determine if lordosis apex location and number of vertebrae in upper/lower arc are associated with mechanical complications. Materials and Methods: A single-institution, retrospective cohort study was performed for patients undergoing ASD surgery from 2009-21. Inclusion criteria were: ≥ 5-level fusion, sagittal/coronal deformity, and 2-year follow-up. Multivariable logistic regression was performed to test the significance of preoperative and postoperative change in lumbar apex and upper/lower arc on postoperative outcomes, including mechanical complications and reoperations, controlling for age, BMI, and comorbidities. Results: Of 202 patients undergoing ASD surgery, the most common preoperative lordosis apex was L5 in 75 patients (37.1%), followed by L4 in 40(19.8%), and L4-L5 in 35 (16.8%). The average number of vertebrae in the lower and upper lordotic arc was 1.3 ± 1.0 and 2.4 ± 1.2, respectively. Postoperatively, the most common apex was L4 in 63 patients (31.2%), followed by L3-L4 in 35(17.3%) then L4-L5 in 33(16.3%). The average number of vertebrae in the lower and upper arcs postoperatively was 1.6 ± 0.8 and 3.0 ± 1.3 respectively. There was an average postoperative cranially-directed change of 0.3 ± 0.9 levels of the lower arc and 0.6 ± 1.4 levels of the upper arc. Lordosis apex location and change in upper/lower arc was not associated with mechanical complications or reoperation. Conclusion: After ASD surgery, most patients had a cranially-directed change in the lordosis apex, an increase in the total number of lordotic vertebrae, and an increase in the number of vertebrae involved in the upper and lower lordosis arcs; however, the degree of change was not associated with postoperative outcomes. While lordosis apex location and lordosis arcs dictate sagittal alignment, no impact on postoperative outcomes was seen.
2354
P127: What Are the bloodiest adult spinal deformity surgeries with the longest length of stay?
Hani Chanbour 1 , Graham Johnson 1 , Jeffrey Chen 2 , Tyler Metcalf 3 , Alexander Lyons 1 , Jacob Jo 1 , Soren Jonzzon 1 , Iyan Younus 1 , Christopher Bonfield 1 , Amir Abtahi 4 , Byron Stephens 4 , Scott Lawrence Zuckerman 1
1 Neurosurgery, Vanderbilt University Medical Center, Nashville, USA
2 Neurosurgery, Baylor college of Medicine, Houston, USA
3 Orthopedics, Ohio State University, Columbus, USA
4 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: Identifying risk factors associated with increased blood loss and longer LOS in adult spinal deformity (ASD) surgery may help improve outcomes. We sought to elucidate which preoperative and intraoperative factors were most associated with blood loss and length of stay (LOS) after ASD surgery. Materials and Methods: A single-institution, retrospective cohort study was performed for patients undergoing adult spinal deformity surgery between 2009-2021. Inclusion criteria were: ≥ 5-level fusion, sagittal/coronal deformity, and 2-year follow-up. The primary independent variables were demographics, preoperative factors, extent of sagittal/coronal deformity, and intraoperative factors. The primary outcomes were the highest quartile of decreased hemoglobin (g/dL) and length of stay (days). Blood loss was calculated according to Hemoglobin (Hb) drop based on the following formula: Hb preop + (Units transfusion x Hb transfusion) – Hb postop. Bivariate statistics were performed. Results: A total of 238 patients undergoing ASD surgery were identified with a mean age of 63.4 ± 17.4. Patients in the highest quartile of blood loss had a mean decreased hemoglobin of 8.5 ± 2.3 g/dL and an estimated blood loss of 2,594.0 ± 1,550.5 mL. Between groups, no differences were observed in demographics, comorbidities, or radiographic measurements (p > 0.050). Intraoperatively, the highest quartile had significantly greater operating time (516.2 ± 141.4 vs. 388.2 ± 134.3mins; p < 0.001), and more 3-column osteotomies (30.5% vs. 14.8%; p < 0.008). Blood loss was influenced by the operating surgeon (p = 0.005). The highest quartile of LOS had a mean of 14.5 ± 18.5 days. Patients in the top quartile LOS had a higher incidence of ≥ 2 comorbidities (54.5% vs. 36.3%, p = 0.013). Intraoperatively, patients with longer LOS had greater total instrumented levels (11.9 ± 3.7 vs. 10.1 ± 2.9; p = 0.001), higher number of 3CO (27.3% vs. 14.3%; p = 0.045), and longer operative time (492.1 ± 167.9 vs. 398.0 ± 133.3 mins; p < 0.001). Conclusion: Operative time and 3-column osteotomies were both significantly associated with the highest quartiles of blood loss and length of stay. Blood loss was also heavily influenced by operating surgeon.
2368
P128: How does the severity of baseline sagittal imbalance affect the postusurgical outcomes after corrective surgery in patients with adult spinal deformity?
Se-Jun Park 1 , Jin-Sung Park 1 , Dong-ho Kang 1 , Hyun-Jun Kim 1
1 Orthopedic Surgery, Samsung Medical Center, Seoul, South Korea
Introduction: Optimal restoration of spinopelvic malalignment is a cornerstone of the surgical management of ASD to achieve good clinical outcomes. It is possible that those with severe sagittal imbalance would require more invasive surgery, which increases the surgical burden. It is unclear how the severity of the baseline sagittal imbalance affects clinical outcomes. Therefore, this study aims to determine the clinical impact of the baseline sagittal imbalance severity in patients with adult spinal deformity (ASD). Material and Methods: We retrospectively reviewed patients who underwent ≥ 5-level fusion including the pelvis, for ASD with a ≥ 2-year follow-up. Using the SRS-Schwab classification system, patients were classified into three groups according to the severity of the preoperative sagittal imbalance: mild, moderate, and severe. The SRS-Schwab classification consists of three sagittal modifiers of PI-LL mismatch, SVA, and PT.12 Each sagittal modifier was graded as 0 (< 10°), + (10 – 20°), ++ (> 20°) for PI-LL mismatch, 0 (< 40 mm), + (40 - 95 mm), ++ (> 95 mm) for SVA, and 0 (< 20°), + (20 - 30°), ++ (> 30°) for PT. Scores were assigned to each item of the sagittal modifiers, for example, 0 points for grade 0; 1 point for grade +; and 2 points for grade ++. Based on the sum of the total scores, patients were classified into three groups: mild (score: 1 or 2 points), moderate (score: 3 or 4 points), and severe (score: 5 or 6 points). No patients had a total score of 0 point. Postoperative clinical and radiographic results were compared among the three groups. Results: The study cohort consisted of a total of 259 patients; 42, 62, and 155 patients were included in mild, moderate, and severe groups, respectively. Although the perioperative surgical burden was greatest in the severe group, there were no significant differences in the inpatient complication rates among the groups. The postoperative pelvic incidence minus lumbar lordosis mismatch was greatest in the severe group, indicating a trend toward under-correction in the severe group. There were no statistically significant differences in mechanical failures such as proximal junctional complications and rod fractures. Clinical outcomes, such as the VAS score for back pain and the SRS-22 score, were comparable among the groups. Conclusion: Patients with severe sagittal imbalance were treated with more invasive surgical methods along with increased the perioperative surgical burden. However, the final clinical outcomes were comparable among the groups. Surgical treatment appears worthwhile, even for patients with severe sagittal imbalance; however, more rigorous surgical planning is necessary to achieve optimal sagittal alignment in such patients.
2444
P129: Evaluating the origins of coronal malalignment prior to adult spinal deformity surgery: how does prior lumbar fusion surgery affect presentation and correction?
Hani Chanbour 1 , Graham Johnson 1 , Jeffrey Chen 2 , Iyan Younus 1 , Soren Jonzzon 1 , D. Campbell Liles 1 , Adam Wegner 3 , Amir Abtahi 4 , Byron Stephens 4 , Scott Lawrence Zuckerman 1
1 Neurosurgery
2 Neurosurgery, Baylor College of Medicine, Houston, USA
3 Orthopedics, Orthovirginia, Arlington, USA
4 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: Coronal malalignment (CM) remains a challenging problem in adult spinal deformity (ASD) surgery and understanding its origins may help with prevention/treatment. In patients with CM undergoing ASD surgery, we sought to compare those with prior lumbar fusion surgery to those without regarding the: 1) lumbosacral fractional curve and 2) major curve contributing. Materials and Methods: A single-institution, retrospective cohort study was performed of patients undergoing ASD surgery from 2011-21. Inclusion criteria were: ≥ 5-level fusion, coronal vertical axis (CVA) > 3 cm, and > 2-year follow-up. Coronal Cobb angles were divided into proximal thoracic (PT), main thoracic (MT), thoracolumbar/lumbar (TL/L), and fractional curve. The fractional curve was measured either from L3/L4/L5-S1. The major curve was defined as the largest curve. Bivariate statistics were performed. Results: Of 58 patients presenting with preoperative CM, mean age was 66.1 ± 14.2, 45 (79.3%) were females, and 17 (29.3%) had prior lumbar fusion surgery. Mean preoperative CVA was 5.9 ± 2.7 cm. Diagnoses were: degenerative (58.6%), idiopathic (39.7%), and neuromuscular (1.7%). Of patients WITH a prior fusion: 11/17 (64.7%) had a preoperative fractional curve > 5° with a mean curve of 8.1 ± 6.4º. Postoperatively, no significant improvement in the fractional curve was seen (8.1 ± 6.4º vs. 5.7 ± 6.9º, p = 0.089). The most common major curve was: TL/L (41.2%), MT (29.4%), fractional (17.6%), and PT (11.8%). Of patients WITHOUT prior fusion: 28 (68.3%) had a preoperative fractional curve > 5° with a mean curve of 11.8 ± 9.1º Postoperatively, there was a significant improvement in the fractional curve (11.8 ± 9.1º vs. 6.9 ± 6.0, p < 0.001). The most common major curve was: TL/L (87.8%), MT (7.3%), and fractional curve (4.9%). The fractional curve was more often the major curve in patients with prior lumbar fusion surgery, though this finding was not statistically significant (17.6% vs. 4.9%, p = 0.144). Conclusions: Of patients presenting with preoperative coronal malalignment, almost one-third had a prior lumbar fusion, and approximately two-thirds of these patients were fused with a fractional curve > 5°. Of the remaining patients with no prior fusion, the fractional curve was > 5° in over two-thirds, yet the major curve was most often the TL/L curve. While the fractional curve was significantly improved in patients without prior surgery, it was not significantly improved in patients with prior lumbar fusion surgery. These results underscore that in patients undergoing ASD surgery with coronal malalignment, those with prior lumbar fusions had a fractional curve that was more often the major curve and less often corrected than patients without prior lumbar fusion surgery.
2450
P130: Who is discharged home after adult spinal deformity surgery?
Hani Chanbour 1 , Jeffrey Chen 2 , Graham Johnson 1 , Tyler Metcalf 3 , Alexander Lyons 1 , Iyan Younus 1 , Soren Jonzzon 1 , Steven G. Roth 1 , Amir Abtahi 4 , Byron Stephens 4 , Scott Lawrence Zuckerman 1
1 Neurosurgery
2 Neurosurgery, Baylor College of Medicine, Houston, USA
3 Orthopedics, Ohio State University, Columbus, USA
4 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: Patients often require postoperative rehabilitation at inpatient rehab (IPR) or skilled nursing facilities (SNF) after adult spinal deformity surgery; however, discharge to home is often preferred by the patient and less costly. The current objectives were to: 1) report the incidence of discharge to home after ASD surgery, and 2) determine the preoperative and perioperative variables associated with discharge to home. Materials and Methods: A single-institution, retrospective cohort study was undertaken for patients undergoing ASD surgery from 2009-2021. Inclusion criteria were: ≥ 5-level fusion, sagittal/coronal deformity, and 2-year follow-up. The primary outcome was discharge home vs. IPR/SNF. A sub-analysis comparing IPR to SNF was conducted. Bivariate analysis was performed. Results: Of 221 patients undergoing ASD surgery with a mean age of 63.6 ± 17.6, 112 (50.6%) were discharged home, 71 (32.2%) were discharged to IPR, and 38 (17.2%) were discharged to SNF. Patients who were discharged home were significantly younger (55.7 ± 20.1 vs. 71.8 ± 9.1, p < 0.001) and had lower incidence of two or more comorbidities (38.4% vs. 45.0%, p = 0.001). Perioperatively, patients who were discharged home had significantly fewer levels instrumented (10.0 ± 3.0 vs. 10.9 ± 3.4, p = 0.030), shorter operative times (381.4 ± 139.9 vs. 461.6 ± 149.8 mins, p < 0.001), less blood loss (1,101.0 ± 977.8 vs. 1,739.7 ± 1,332. 9 mL, p < 0.001), and shorter length of stay (5.4 ± 2.8 vs. 9.3 ± 13.9, p < 0.001). The operating surgeon also significantly influenced disposition status (p < 0.001). When comparing IPR (N = 71) vs. SNF (N = 38), patients discharged to SNF were significantly older (74.4 ± 8.6 vs. 70.4 ± 9.1, p = 0.029) and were more likely to be female (89.5% vs. 70.4%, p = 0.024). Conclusion: Approximately 50% of patients were discharged home after ASD surgery. Those discharged homer were younger, had fewer comorbidities, and underwent less extensive operations with fewer levels instrumented, shorter operative time, and less blood loss.
2481
P131: Roussouly classification in adult spinal deformity surgery: are postoperative Roussouly types predictors of outcomes?
Hani Chanbour 1 , Graham Johnson 1 , Jeffrey Chen 2 , Tyler Metcalf 3 , Jacob Jo 1 , Iyan Younus 1 , Soren Jonzzon 1 , Steven G. Roth 4 , Adam Wegner 5 , Amir Abtahi 6 , Byron Stephens 6 , Scott Lawrence Zuckerman 1
1 Neurosurgery
2 Orthopedics, Baylor College of Medicine, Houston, USA
3 Orthopedics, Ohio State University, Columbus, USA
4 Orthopedics, New York Presbyterian Hospital, New York, USA
5 Orthopedics, Orthovirginia, Arlington, USA
6 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: The Roussouly classification of spinopelvic alignment is a framework of common healthy variants of lumbar lordosis that has been expanded to patients with adult spinal deformity (ASD). In a cohort of ASD patients undergoing surgery, we sought to: 1) report the postoperative Roussouly Type of each patient, and 2) determine which postoperative Roussouly type most prone to mechanical complications and worse postoperative outcomes. Materials and Methods: A single-institution retrospective cohort study was performed for patients undergoing ASD surgery from 2009-2021. Inclusion criteria were: ≥ 5-level fusion, sagittal/coronal deformity, and 2-year follow-up. The primary outcome variable was the postoperative Roussouly type. Retroversion was defined as pelvic tilt>50% of pelvic incidence. Postoperative outcomes included mechanical complications, reoperations, proximal junction kyphosis (PJK), pseudarthrosis, and patient-reported outcomes measures (PROMs). Results: Of 202 patients undergoing ASD surgery, postoperative Roussouly Types were Type 1 for 41 (20.3%) patients, Type 2 for 129 (63.9%), Type 3 for 30 (14.9%), and Type 4 for 2 (1.0%). The postoperative Roussouly classification was not associated with the surgical parameters of total instrumented levels (p = 0.851), combined anterior-posterior vs. posterior approach (p = 0.101), number of interbodies (0.792), procedure time (p = 0.704), estimated blood loss (p = 0.103), or length of stay (p = 0.957). Furthermore, postoperative Roussouly types were not associated with mechanical complications (p = 0.167), PJK (p = 0.330), rod fracture (p = 0.188), pseudarthrosis (p = 0.308), reoperations (p = 0.752), or MCID of PROMs. A sub-analysis found that retroverted Type 2 (N = 88, 68.2%) had similar mechanical complications (70.5% vs. 68.4%, p = 0.819) compared to non-retroverted Type 2. Similarly, no association was found between retroverted Type 1 (N = 24, 58.5%) and non-retroverted Type 1 in mechanical complications (70.8% vs. 60%, p = 0.485) or other outcomes. Conclusion: The postoperative Roussouly classification was not associated with surgical outcomes in this cohort. This could be a result of most patients being corrected to similar spinopelvic alignments and not receiving individualized tailored surgeries.
2487
P132: Roussouly classification in adult spinal deformity surgery: is preoperative Roussouly type associated with outcomes?
Hani Chanbour 1 , Graham Johnson 1 , Jeffrey Chen 2 , Tyler Metcalf 3 , Jacob Jo 1 , Iyan Younus 1 , Soren Jonzzon 1 , Steven G. Roth 4 , Adam Wegner 5 , Amir Abtahi 6 , Byron Stephens 6 , Scott Lawrence Zuckerman 1
1 Neurosurgery
2 Orthopedics, Baylor College of Medicine, Houston, USA
3 Orthopedics, Ohio State University, Columbus, USA
4 Orthopedics, New York Presbyterian Hospital, New York, USA
5 Orthopedics, Orthovirginia, Arlington, USA
6 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: The Roussouly classification is a framework to describe normal spinopelvic alignment that has been expanded to patients with adult spinal deformity (ASD). In a cohort of ASD patients undergoing surgery, we sought to apply the Roussouly classification through the following objectives: 1) determine demographic differences in preoperative Roussouly classification, 2) compare what surgical procedures are performed on each Roussouly type, and 3) identify which preoperative Roussouly type is associated with suboptimal outcomes. Materials and Methods: A single-institution retrospective cohort study was performed for patients undergoing ASD surgery from 2009-2021. Inclusion criteria were: ≥5-level fusion, sagittal/coronal deformity, and 2-year follow-up. The primary exposure variable was the preoperative Roussouly type. Outcomes included mechanical complications and minimal clinically important difference (MCID) 30% of patient-reported outcomes measures (PROMs), which included Oswestry Disability Index (ODI), Numeric Rating Scale (NRS)-Back/Leg pain, and EQ-5D. Results: Of 219 patients undergoing ASD surgery, Roussouly Type 4 patients were younger compared to Types 1-3 (54.8 ± 18.4 vs. range of means 65.6-67.3, p = 0.014), with no significant difference in other demographics, comorbidities, or preoperative PROMs. The preoperative Roussouly types were not associated with the surgical parameters of total instrumented levels (p = 0.257), combined anterior-posterior vs. posterior approach (p = 0.643), number of interbodies (p = 0.334), procedure time (p = 0.416), or estimated blood loss (p = 0.052). However, types 2 and 4 were most likely to have a shorter length of stay vs. types 1 and 3 (5.6 ± 1.9 and 5.2 ± 1.9 vs. 8.5 ± 17.9 and 8.6 ± 6.6, p = 0.004), with no difference in discharge disposition, mechanical complications, reoperations, or MCID of PROMs across the four preoperative Roussouly types. Conclusion: Type 4 Roussouly patients undergoing ASD surgery were younger, indicating earlier symptomatic degeneration requiring surgery than Types 1-3. Types 2 and 4 had a shorter length of stay. No other intraoperative and postoperative differences were seen, perhaps due to similar procedures being performed on very different spinopelvic malalignments.
2492
P133: Is there a difference in coronal malalignment based on roussouly classification of patients undergoing adult spinal deformity surgery?
Hani Chanbour 1 , Graham Johnson 1 , Jeffrey Chen 2 , Tyler Metcalf 3 , Iyan Younus 1 , Soren Jonzzon 1 , Steven G. Roth 1 , Adam Wegner 4 , Amir Abtahi 5 , Byron Stephens 5 , Scott Lawrence Zuckerman 1
1 Neurosurgery
2 Neurosurgery, Baylor College of Medicine, Houston, USA
3 Orthopedics, Ohio State University, Columbus, USA
4 Orthopedics, Orthovirginia, Arlington, USA
5 Orthopedics, Vanderbilt University Medical Center, Nashville, USA
Introduction: Roussouly classification is used to classify sagittal alignment, yet little is known how it impacts coronal malalignment (CM) in ASD surgery. In a cohort of patients undergoing adult spinal deformity (ASD) surgery, we sought to: 1) report the rate of CM in each Type of preoperative Roussouly classification, and 2) determine whether preoperative Roussouly classification is associated with postoperative CM correction. Materials and Methods: A single-institution, retrospective cohort study was undertaken for patients undergoing ASD surgery from 2009-21 with 2-year follow-up. The primary independent variable was preoperative Roussouly classification. The primary outcome was CM, defined as coronal vertical axis (CVA) ≥ 3 cm, in each Roussouly Type. Secondary outcomes included CM correction. Absolute value of CVA was used. Results: Of 218 patients undergoing ASD surgery with a mean age of 65.8 ± 15.2, Roussouly Type 1 was observed in 77 (35.3%), Type 2 in 89 (40.8%), Type 3 in 34 (15.6%), and Type 4 in 18 (8.7%). Mean preoperative CVA was 2.7 ± 2.8 cm and 57 (26.1%) had preoperative CM. Preoperative CM was found in 23/77 (29.8%) of Type 1, 22/89 (24.7%) of Type 2, 6/34 (17.6%) of Type 3, and 6/18 (33.3%) of Type 4, with no significant difference among the four groups (p = 0.493). No difference was found in preoperative/postoperative CVA among the four groups (p = 0.291, p = 0.927). Postoperatively, CM was present in 33 (15.1%), 14 (18.2%) in Type 1, 13 (14.6%) in Type 2, 3 (8.8%) in Type 3, and 3 (16.7%) in Type 4, with no significant differences among the four groups (p = 0.637). Though patients with Type 4 had the highest CVA correction (3.5 ± 34.0 cm), no difference was found among Roussouly Types (p = 0.883). Similarly, though Type 1 had the highest max Cobb angle correction (32.3 ± 29.6°), no difference was found in max Cobb angle correction among Roussouly Types (p = 0.597). Conclusion: In patients undergoing ASD surgery, no difference was found in CM rate, CVA, or coronal max Cobb angle correction based on Roussouly types.
2555
P134: Adjacent segment failure after multilevel fusion for degenerative spinal disorders - is Alignment the only reason?
Gerrit Lewik 1,2 , Clifford Pierre 1 , Rod Oskouian 1 , Jens Chapman 1
1 Neurosurgery, Swedish Neuroscience Instiate, Seattle, USA
2 Department of Trauma Surgery, BG University Hospital Bergmannsheil Bochum, Bochum, Germany
Introduction: Adjacent segment failure (ASF) is a common-detected complication following spinal fusion and occurs throughout the spine (1). The risk of ASF is reported in literature between 5 and 30% (2) (3) (4). According to the current literature, the most frequently described risk factor for ASF following an initial/primary surgical fusion of the spine is the postoperative alignment (5) (6). But although the alignment is still seen as one of the key risk factors influencing complications as well as the necessity for re-surgical intervention (7), recent studies have placed more attention to additional patient-related risk factors. Such risk factors include obesity /body mass index, history of smoking, and certain medications (8–10). So far, most of these studies have concentrated on only one-level spinal fusion, and still little is known regarding risk factors for adjacent segment failure after multilevel spinal fusion surgery. We hypothesized that adjacent segment degeneration is, in fact, a far more complex and multifactorial process beyond alignment and thus deserved more formal statistical analysis. Material and Methods: This retrospective analysis studied 78 elective multilevel thoracolumbar spine fusion patients with minimum of three motion segment fusion starting from the sacrum rostrally performed for degenerative disorders between September 1, 2015 and February 28, 2020 and completion of a minimum of 2 years of follow-up. We evaluated the following additional co/variables outside of alignment parameters:
- patient demographics (age, sex, body mass index)
- number of fusion levels
- chronic opioid use
- chronic steroid intake
- antimetabolite and cytostatic therapy
- osteoporosis measured by Hounsfield Units (HU)
- diabetes
- smoking history
- spinal infections
- inflammatory arthropathy
- ankylosing spine disorders
- quantified sarcopenia
Alignment variables were:
- Total coronal alignment
- Total sagittal angle (SVA)
- Lumbar lordosis (LL)
- Thoracic kyphosis (TK)
- T1 slope
- Pelvic incidence (PI)
- LL – PI mismatch calculation
Results: Evaluating the retrieved data, the statistical analysis revealed an important role of the individual patient risk factors beyond alignment factors. Compared to the radiographic parameters, the individual risk factors seem to show even a higher impact on the risk of adjacent segment failure following multilevel fusion. Specifically, BMI with an RR of 3.4 and sarcopenia with a RR of 3.1 exceeded the RR for spinal misalignment with an RR of 2.2. Conclusion: We were able to provide a substantial impact on how the risk of adjacent segment failure is influenced be not only alignment, but also by individual risk factors. These results need further confirmation and should be a subject or future research projects. In our study of 78 carefully screened and comprehensively assessed patients we found a significant preponderance of other risk factors for early adjacent segment degeneration after multilevel fusion surgery for degenerative thoracolumbar conditions. Specifically, a BMI > 35 and a Sarcopenia Index < 0.85 were significantly higher risk factors than patients with radiographic misalignment. This study confirms the need to take a more circumspect approach to the imported study of adjacent segment disease beyond focusing primarily on radiographic parameters.
Degenerative cervical
56
P135: Comparison of three grafting options for anterior cervical corpectomy and fusion : a retrospective 3-arms case control study
Marc-Antoine Rousseau, Mathilde Gaume, Baptiste Boukebous, Mohamed Zoghlami, Cédric Maillot
Introduction: The surgical procedure of anterior cervical corpectomy and fusion (ACCF) achieves foraminal radicular and central medullar decompression, and spinal stabilization for staged lesions on two consecutive levels or more. However, the reconstruction requires a significant amount of bone graft for replacing the vertebral body. The use of a synthetic cage with fragmented bone from the former vertebral body has gradually come to replace the "tri-cortical" one-block structural autologous bone graft, harvested from the iliac crest. However, few studies have directly compared the outcomes of different types of cages. The purpose of this retrospective study was to compare the radiological outcomes and early complications of the use of a windowed rectangular cage made of PolyEtherKetoneEtherKetoneKetone (PEKEKK) reinforced with carbon fiber polymer whose particularity is to be oriented, to the use of a titanium mesh cylindrical cage and to the use of structural iliac bone graft. Material and Methods: We compared 3 consecutive historical cohorts of patients operated from 2013 to 2019. We matched on the number of corpectomy levels 45 patients with a rectangular oriented PEKEKK/carbon fiber polymer cage, 15 patients with a titanium mesh cylindrical cage, and 15 patients with a cortico-cancellous structural bone graft taken from the iliac crest. The measured parameters were the restoration of the vertebral height and cervical lordosis after surgery, as well as the subsidence of the construct during the follow-up. The revisions related to a failure of the construct were also noted. Two independent observers assessed the radiologic parameters. All parameters were measured before (PreOp), immediately after the surgery (PostOp) and at the last follow-up > 6 months (Last FU). Results: A better - but non-significant - gain of height after surgery was noted for the PEKEKK/carbon (+8%) or titanium cages (+8%) with fragmented vertebral bone in reference to the iliac crest tri-cortical autograft reconstruction (+2%, p = 0.119). The mean subsidence at last follow-up was more important for titanium cages but also non-significant, with respectively -6% for the PEKEKK/carbon cages, -4% for the iliac crest tri-cortical autografts, and -10% for the titanium cages (p = 0.223). Segmental Cervical Lordosis gain was significant (p < 0.001) and remained stable. Regional Cervical Lordosis gain and subsidence changes were not significant. No early revision was noted for the 3 groups. Conclusion: The use of fragmented vertebral bone autograft within an oriented PEKEKK/carbon fiber polymer cages is an interesting option when performing an ACCF. While some improvement in the radiologic anatomical parameters can be achieved with both cages compared to the classical iliac bone block, the oriented PEKEKK/carbon fiber cage seems to lead to less subsidence.
59
P136: What perioperative factors are associated with high-risk morphine milligram equivalents in cervical spinal fusions?
Eeric Truumees 1 , Devender Singh 1 , Ashley Duncan 1 , Cortney Matthews 1 , Sophia Stokes 2 , Matthew Geck 1 , John Stokes 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
2 UT Austin, Austin, USA
Introduction: Morphine milligram equivalent (MME) dosing recommendations were introduced in 2016 by the Centers for Disease Control and Prevention (CDC) as a guideline for primary care providers to aid in understanding the cumulative effect of opioids and the risk associated with long term use in chronic pain patients. The formula is defined as: Strength per Unit X (Number of Units/Days Supply) X MME = MME/Day. Daily dosages of ≥ 100 MME/day are associated with an almost nine-fold increased risk of overdose. Current general recommendations endorse the lowest effective dose and ≤ 50 MME/day. We sought to understand how many patients undergoing cervical spinal fusions received opioids at higher risk doses and which patient demographic and historical factors could predict this higher risk. Materials/Methods: Retrospective analysis was conducted on 237 patients that underwent one to six level cervical fusion within a multi-center network over 2 years. All surgeries were conducted in a hospital system that encourages surgeons to deploy multi-modal post-operative pain pathways. Average MME/day was calculated as the sum of qualifying inpatient MMEs administered divided by the sum of inpatient length of stay (LOS). 14 independent variables were collected from demographic, clinical and surgical domains and were subject to comparative analysis. Data was then grouped and coded for logistic regression analysis. Results: Overall mean MME per day was 67.32 ± 42.34, with a range of 0-188.54 MME/day. “High MME” was defined as greater than the overall upper quartile value, 95.02 MME/day. A total of 60 patients were determined to have “High MME” during their inpatient stay. Patients with high MMEs were significantly younger than those with MMEs within normal limits (WNL), 52.87 ± 11.33 vs 59.49 ± 11.94 respectively (p = 0.0002). Patients age ≤ 60 accounted for 70% (n = 42) of the High MME group. 23.3% were categorized “young” (25-44 years) and 46.7% were “middle” aged (45-60 years). There were also significant differences between the two groups in terms of preoperative prescriptions for opioids. 32.3% (n = 32) of patients with High MMEs had an active preoperative opioid prescription vs 20.3% (n = 28) of those with MMEs WNL. There we no significant demographic or intraoperative differences between the groups, nor any significant difference in length of stay. When subject to logistic regression the final optimized model returned a test recall value of 0.61, identifying age as the only significantly variable affecting the odds ratio. For each unit decrease in age, risk increased by 0.48 or 51.9%. Conclusion: Patients with high MME/day who underwent one to six level cervical fusions were significantly younger and more likely to have been prescribed preoperative opioids than cervical fusion patients with MME WNL. Younger age at the time of surgery significantly impacted the risk of high MME. As a result, pre-operative opioid risk education and mitigation strategies should be considered for those at risk, especially in the younger spine population.
61
P137: What effect does T1 slope have on sagittal balance and the relationship with caudal end of three or more level posterior cervical fusions?
Eeric Truumees 1 , Devender Singh 1 , Ashley Duncan 1 , Cortney Matthews 2 , John Stokes 1 , Matthew Geck 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
2 UT Austin, Austin, USA
Introduction: The study investigated the effect of T1 slope on post-operative Sagittal Vertical Axis (SVA) and whether extension of posterior cervical fusions into the upper thoracic spine provides improved sagittal balance in comparison to C7 caudal level. Our hypothesis was does extension of posterior cervical fusions across the cervicothoracic junction lead improved sagittal balance in comparison to C7 caudal level. Materials/Methods: A database of 327 patients who underwent a three or more level posterior cervical fusion with two years follow up was created. Two cohorts were created based on fusion caudal level, those whose fusion terminated at C7 and those whose fusions extended to T1 or T2. The cohorts were then divided again into two subgroups, high T1 slope (> 25°) and low T1 slope (≤ 25°) and subject to comparative analysis. Results: 224 patients were included in the C7 caudal cohort and 103 were included in the T1/T2 caudal cohort. The mean age of C7 and T1/T2 groups were 61 ± 12 yrs and 63.1 ± 12.6 yrs, respectively. Mean BMI of the C7 cohort was 28.9 ± 6.8, and 29.1 ± 5.8 in the T1/T2 cohort. Mean SVA was significantly higher in patients with high T1 slopes (mean range 34.2-44.1 mm) as compared to patients with Low T1 slopes (mean range 21-28.9 mm) across all time intervals (pre-op to 24 months post-op). Additionally, the 25th percentile SVA of High T1 slopes were greater than the median SVA values of Low T1 slopes at all intervals. For both the high and low T1 slope cohorts, patients with a caudal T1/T2 had comparatively higher SVA values than their C7 counterparts at all intervals despite maintenance of cervical lordosis, however these differences were not statistically significant. Conclusion: Increased sagittal imbalance was comparatively higher in patients with > 25° T1 slope ranging across preoperative to 24 months postoperative radiographic measurements. Extension of the posterior cervical fusion to T1 or T2 did not improve sagittal balance in patients with high T1 slopes. In fact, extension of posterior cervical fusions across the junction lead to increased positive sagittal imbalance. The results of this study do not support routinely extending posterior cervical fusions into T1 or T2 to improve post-operative sagittal balance. Longer thoracic extension or other intra-operative measures must be sought in patients at high risk for sagittal decompensation.
65
P138: When to initiate post-operative physical therapy in multilevel posterior cervical-thoracic fusions?
Eeric Truumees 1 , Devender Singh 1 , Ashley Duncan 1 , Cortney Matthews 1 , Sophia Stokes 2 , Matthew Geck 1 , John Stokes 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
2 UT Austin, Austin, USA
Introduction: The role of Physical Therapy (PT) in patients undergoing surgery for cervical spondylotic myelopathy is understudied and not well understood. Current literature reports varied effects on outcomes, and thus post-operative standards of care neither address nor include PT in post-op posterior cervico-thoracic fusions. The aim of this study was to analyze when neck strengthening exercise should be initiated after multilevel posterior cervical-thoracic fusions. Materials/Methods: Retrospective chart reviews were conducted between 2016-2020 on patients who underwent a ≥ 3 level posterior cervico-thoracic fusion with caudal levels as C7 and T1/T2. Prescription and completion of PT were study inclusion criteria. Demographic, clinical, and radiographic data was collected at structured intervals from preoperative to two years postoperative. % improvement for cervical lordosis, T1 slope and C2-C7 sagittal plumbline was compared at 2 weeks and 2 years post-op. Visual Analog Scale (VAS) for pain and Oswestry Disability Index (ODI) scores were similarly analyzed. Results: 105 patients were included in the study and were divided into two cohorts: those that initiated PT ≤ 6 weeks post-op and those who initiated PT > 6 weeks post-op. 58 patients were included in the Early PT cohort, and 47 were included in the Late PT cohort. Demographically, the Early PT and Late PT cohorts were similar in age (62.8 vs 61.1 years, respectively) and predominantly female (64.5% vs. 67.6%, respectively). No significant difference was reported between the groups in body mass index, with a mean of 30.7 for Early PT and 31.2 for Late PT. While both cohorts showed improvement in radiographic parameters and patient reported outcomes at 2 years post-op, there were significant differences in level of improvement between the two groups. The Early PT group had a comparatively better % improvement in cervical lordosis (25.2% vs 14.2%); mean T1 slope (-5.6% vs. -2.6%); and mean C2-C7 sagittal plumbline (-15.2% vs -11.7%). Patients who started PT ≤ 6 weeks post-op also reported greater VAS % improvement 61.9% vs 41% and Oswestry Disability Index % improvement 46.3% vs. 29.6% at 2 years post-op. Discussion: Patients who underwent a three or more-level posterior cervico-thoracic fusion and started PT at or before 6 weeks post-op exhibited greater radiographic and patient reported outcomes benefits than those starting PT more than 6 weeks post-op. The results of this study support the early initiation of neck strengthening PT in most uncomplicated post-cervical fusion adult patients.
204
P139: Correlation of T1 slope and its use as an early indicator for detection of degenerative cervical myelopathy
Manojkumar Gaddikeri 1 , Sudhir Srivastava 2
1 Lilavati Hospital and Research Center, We are Spine, Mumbai, India
2 KJ Somaiya Hospital and Research Center, Orthopaedics, Mumbai, India
Introduction: Cervical spondylosis is a chronic progressive degenerative disorder with end point being development of myelopathy. It is a common condition seen in orthopaedic OPD. Loss of cervical alignment to neutral or kyphosis is an early radiological marker. Radiological parameters when used appropriately gives information regarding present condition and future prognosis of the patient. Cervical spondylosis though commonly seen,the risk of development of myelopathy cannot be known with certainty. In a country with limited resources and over a billion population, use of radiographs to screen for those asymptomatic patients at risk of development of myelopathy will reduce the financial burden on patients and that of healthcare system. Materials and Methods: A retrospective study was conducted which included three groups, group-A with 102 subjects in the age group of 18-30 years without any cervical complaints to be used as controls, group-B included 100 patients of symptomatic cervical spondylosis without myelopathy and group-C included 71 patients diagnosed with cervical spondylotic myelopathy. Clinico-radiological data was collected, analysed and computed. Results: Mean C2-7 Cobb’s angle in group-A was 14.8° ± 4.8°,7.67° in group-B and -1.66°(kyphosis)in group-C. Mean cSVA was -21.2mm in group-A, +8.864 mm in group-B and +24.32 mm in group-C. Mean T1 slope was 24.974° in group-A, 18.1° in group-B and 13.6° in group-C. T1slope minus C2-C7 Cobb’s angle value was 10.174° in group A,10.43° in group B,15.26° in group C. Conclusion: CSM is a leading cause of cervical myelopathy with good prognosis if detected & treated early. Our study was aimed to find a way for selecting those patients of cervical spondylosis who are at high risk of progression to myelopathy using simple lateral radiographs of cervical spine. Our study showed that T1 slope <18° highly correlated with the development of myelopathy symptoms (Nurick grade ≥ 2) in patients of cervical spondylosis. These are the candidates for getting MRI, to look for any actual cord compression and to keep a watch for development of myelopathy.
Keywords: Cervical spondylotic myelopathy, cSVA, T1 slope, Cobb’s method, Nurick grade
245
P140: Utility of winged expandable titanium cages for stabilisation after corpectomy in sub axial cervical spine
Dattaprasanna Katikar 1
1 Neurosurgery, Balwant Institute of Neurosurgery and Intensive Trauma Care, Solapur, India
Background: Various methods were used for stabilization after corpectomy in subaxial cervical spine. These methods had multiple issues like collapse, psuedoarthrosis, subsidience or even extrusion. Now winged expandable titanium cages (WETC) are available which can effectively address majority of these issues. Objective: To asses utility of WETC for stabilization after corpectomy in subaxial cervical pathologies in various pathologies. Methods and Material: WE retrospectively studied 130 patients who were operated at our institute for cervical corpectomy and stabilization with WETC for various pathologies. We studied their clinical profile, postoperative improvement and fusion. Fusion was assessed with lateral flexion-extension radiographs at six months post operatively. Results: In our series of 130 patients operated over a period of 14 years, following pathologies were seen, spondylotic myelopathy 38.04%, trauma 26.08%, ossification of posterior longitudinal ligament (OPLL) 23.02%, disco vertebral osteomyelitis 9.78% and tumor 2.17%. In patients of trauma improvement depended on severity of injury. Good to excellent improvement was seen in all other patient groups. We got good fusion in all the patients. Conclusion: We present a personal series of 130 patients which illustrates the utility of WETC in subaxial cervical spine stabilization in various pathologies which need corpectomy. It is easy to apply, gives excellent fixation and fusion, can effectively maintain cervical curvature with very low incidence of complications.
Keywords: expandable cage; cervical myelopathy; corpectomy; OPLL
Key massage: WETC provides excellent stabilization and fusion in patients who need corpectomy in subaxial cervical spine. It is easy to apply and has very low complication rate.
388
P141: Multi-level anterior cervical disectomy and fusion using zero-profile anchored cages: a minimum 5-year follow-up study
Lei Kuang 1 , Haoyu He 1 , Guohua Lv 1
1 Department of Spinal Surgery, The Second Xiangya Hospital of Central South Unviersity, Changsha, China
Introduction: Anterior cervical discectomy and fusion (ACDF) is increasingly used in multilevel degenerative cervical spinal disorders. However, the profile of the anterior cervical plate often lead to prolonged operation time and increased incidence of complications such as postoperative dysphagia, especially in multilevel diseases. Therefore, zero-profile implant was developed to overcome these setbacks and has been confirmed to be superior to the traditional cage-plate in their preliminary practice. However, there is a paucity of mid- to long-term results of these zero-profile cages in multilevel cases. In this study, we retrospectively reviewed a series of cervical spondylotic disorders treated with 3- or 4-level ACDF using zero-profile anchored cages that were followed for at least 5 years to investigate the correlation between their clinical results and radiological outcomes. Material and Methods: Thirty-four patients aged 54.1 ± 8.8 years (range, 41-64 years) who underwent 3- or 4-level ACDF with zero-profile anchored cages for degenerative cervical spondylosis in a single institute between January 2014 and 2016 were included. Clinical outcomes were assessed using the visual analogue scale (VAS), modified Japanese Orthopaedic Association (JOA) scores, and Neck Disability Index (NDI) preoperatively and postoperatively at the 1-, 2-, and 5-year. Radiological outcomes including fusion, disc height, subsidence, fused segment angle and cervical lordosis were also assessed at the same intervals. Results: The mean follow-up time was 68 months. All patients had significant recovery of neurological function. Compared with the preoperative scores, the postoperative VAS, JOA and NDI scores were improved at each time point (p < 0.05). The fused segment angle and cervical lordosis were improved at each follow up time point after the operation (p < 0.05). All surgical segments were fused and there were 32 cage subsidence (31.3%) was observed at the 5-year follow-up. The differences in VAS, JOA scores, NDI, fused segment angle and cervical lordosis between the 5-year and the 2-year follow-up were not statistically significant (p > 0.05). The loss of lordosis was not related to the postoperative symptoms. Conclusion: ACDF using a zero-profile anchored cages for multilevel cervical spondylopathy achieved satisfactory midterm outcomes. Cage subsidence and the loss of cervical lordosis occurred in the first two years after surgery, but remained stable afterwards and were not related to postoperative symptoms.
390
P142: Factors affecting length of stay following anterior cervical discectomy and fusion in Cipto Mangunkusumo National General Hospital, Jakarta
Muhamad Aulia Rahman 1 , Mohamad Saekhu Saekhu 1 , Renindra Ananda Aman Nanda 1 , Setyo Widi Nugroho Widi 1
1 Neurosurgery Department, Cipto Mangunkusumo National General Hospital, Universitas Indonesia, Jakarta, Indonesia
Introduction: Anterior Cervical Discectomy and Fusion (ACDF) procedure is a surgical procedure for cervical disc herniation with symptoms of severe/progressive neurological deficits, or due to persistent radicular pain. The successful treatment of cervical disc herniation by ACDF has been successfully reported in the literature. However, one of the most important goals besides the success of surgery is to shorten the length of stay (LOS) to keep patients as comfortable and free as possible while preparing for long-term recovery at home. Many factors play a role both preoperatively and intraoperatively which correlate with prolonged hospital LOS. This paper is to identify factors that contribute to increasing hospital LOS in patients who have had an ACDF patients at Cipto Mangunkusumo Hospital, Jakarta. Methods: Retrospective cohort study of 108 consecutive patients who underwent elective ACDF at Cipto Mangunkusumo General Hospital, Jakarta. Data collection and analysis were carried out on prognostic factors that were thought to increase LOS. Multivariate analysis to analyze the effect of patient and hospital characteristics on hospital LOS. Results: A total of 27 patients who met the inclusion and exclusion criteria had carried out the ACDF procedure at Cipto Mangunkusumo General Hospital Jakarta for the 2020-2022 period. The age range was 53.52 ± 1.174 (mean ± SD) with a male predominancy in 70.4%. As many as 18.5% of patients had a history of diabetes mellitus and 40% had a history of hypertension. During the surgical procedure the average surgical time the average lasted 5 ± 1.802 (mean ± SD) hours with an estimated 25.00 - 850.00 (min - max) blood loss. The duration of treatment is 5 – 16 (min – max) days. 63% of patients complained of neck pain, 48.1% radicular pain, 77.8% paresthesia, 69.3% hypesthesia, and 69.3% weakness. Complications experienced in patients were urine infections 37% and pulmonary complications 29.6%. Multivariate analysis was carried out to find out which factors significantly influenced the patient's hospital LOS. In this study it was found that the duration of surgery (p = 0.045, logistic regression test), and urinary complications (0.001 logistic regression test) had a significant impact on increasing the LOS of patients after ACDF surgery at RSCM. Conclusion: We found that the most significant factors that contribute to the increasing LOS in patients after ACDF surgery at RSCM are duration of surgery and urinary complications. Neurosurgeons should learn to manage both factors optimally to reduce LOS. The results of this study are beneficial for patients, clinicians, and healthcare facility for better treatment and prognostic outcome.
Keyword: Anterior Cervical Discectomy and Fusion, length of stay, cervical disc herniation
417
P143: Segmental slope is a predictor of fusion rate in single level anterior cervical discectomy and fusion
Xiaqing Sheng 1 , Yang Meng 1 , Beiyu Wang 1 , Chen Ding 1 , Hao Liu 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: According to previous studies, many preoperative factors may affect fusion rate after anterior cervical discectomy and fusion (ACDF), including osteoporosis, smoking, preoperative T1 slope, and range of motion (ROM). However, the T1 slope is often difficult to measure because T1 cannot be observed on X-ray film. Thus, this measure only reflects the overall force lines of the cervical spine and does not visually reflect the mechanics of the index level. Previous studies have found that in multilevel ACDF, the caudal level has a larger slope and slower fusion speed, suggesting that the preoperative slope may be related to the fusion rate. Furthermore, we have also observed in our clinical work that patients with a large preoperative segmental slope show slower fusion speed in single-level ACDF. However, the relationship between segment slope and fusion rate in single-level ACDF has not been reported to date. Therefore, the purpose of this study was to explore whether the preoperative segmental slope may serve as a predictor of fusion rate. Methods: Data of consecutive patients with single-level cervical spondylosis who underwent ACDF between 2011 and January 2019 were retrospectively reviewed. Preoperative parameters including baseline characteristics, segment slope, T1 slope, range of motion, intervertebral disk height, and bone density were evaluated. Data were analyzed using Student’s t-test, Mann-Whitney U test, χ2 test, Fisher’s exact test, multivariate logistic regression analysis, and receiver operating characteristic curve. Results: In total, 253 patients were selected. The mean follow-up was 32.1 months (range 24-99 months). Male sex, body mass index, preoperative segment slope, T1 slope, operative levels, and osteoporosis or osteopenia were associated with non-fusion at an early stage after surgery. However, no statistically significant difference was observed at the last follow-up. Multivariate logistic regression analysis revealed that the preoperative segment slope was an independent predictor for non-fusion at 3, 6, and 12 months postoperatively. Osteoporosis or osteopenia was an independent predictor of non-fusion at 6 and 12 months postoperatively. The area under the curve was 0.874 at 3 months (p < 0.001, cutoff value 10.21°), 0.888 at 6 months (p < 0.001, cutoff value 14.56°), and 0.825 at 12 months (p < 0.001, cutoff value 21.08°). Conclusion: Preoperative segment slope can be used as a predictor of early fusion rate after single-level ACDF. We determined detailed cutoff values. This study may help surgeons take measures to promote early fusion in advance.
574
P144: Risk factors for allograft resorption after anterior cervical discectomy and fusion: a novel quantitative analysis of bone density in allograft spacers
Bum-Joon Kim 1
1 Neurosurgery, Korea University Ansan Hospital, South Korea
Introduction: Anterior cervical discectomy and fusion (ACDF) is a widely performed treatment for degenerative cervical diseases. However, subsidence may occur in some patients due to nonunion or delayed union at the graft site, and it is associated with a poor prognosis. Despite numerous studies on subsidence following ACDF, accurate and timely diagnosis of this complication remains difficult. Material and Methods: Patients who underwent 1- to 3-level ACDF with an allograft intervertebral spacer and anterior cervical plate placement between January 2016 and December 2020 with a follow-up period of > 1 year were enrolled. We divided each allograft implant according to the level and location (3rd, 2nd, and 1st floors) of the fusion. The Cobb’s angle, range of motion (ROM), interspinous distance (ISD) and total intervertebral height (TIH) at the operated level were measured on the preoperative and 1-year postoperative radiographs. Computed tomography (CT) was performed preoperatively and 1-year postoperatively to measure the degree of bridging bone growth and allograft resorption. The bone density in the spacer was measured in pixels. To assess the diagnostic accuracy of three commonly used radiographic fusion criteria and CT for the quantification of bone bridging, correlations between bone density according to the number of surgical levels and relative allograft location were analyzed. Results: Fifty-two patients (mean age, 53.54 years; 73.08% men) were included in the study. After multi-level ACDF, the TIH reduction tended to gradually increase caudally. The generalized estimating equation (GEE) model revealed that TIH reduction at the lowest location (1st floor) was significantly greater than that at the highest location (3rd floor) (p = 0.01). In contrast, ISD and ROM showed no differences according to implant location. In the GEE analysis, the bone density of the allograft on the 3rd and 2nd floors at 1 year postoperatively was significantly higher than that on the 1st floor (p < 0.01 and p < 0.01, respectively). Conclusion: Allograft resorption tends to be more severe in multi-level surgeries and in caudally placed allografts. In patients with plate fixation-enhanced ACDF, ROM and ISD underestimated the micro-motion-induced delayed bone fusion. By measuring the pixels of bone density using follow-up CT scans, allograft resorption and resulting subsidence can be detected and predicted more precisely.
591
P145: Does cervical flexibility affect clinical outcomes in patients undergoing multi-level posterior cervical fusions?
Eeric Truumees 1 , Devender Singh 1,1 , Ashley Duncan 1 , Cortney Matthews 2 , Matthew Geck 1 , John Stokes 2
1 Spine, Ascension Texas Spine and Scoliosis, Austin, USA
2 Spine, University of Texas Austin, Austin, USA
Introduction: Standing multi-view X-rays and MRIs/CTs are standards of care in preoperative planning for patients undergoing cervical fusions. However, the positioning of the patient varies between the two different types of imaging. When positioned for an MRI/CT, the patient is supine, and the neck bolstered or supported. Whereas for standing X-Rays, the patient adopts their native posture and head alignment. This creates a discrepancy in values of radiographic measurements when comparing film to scan. The purpose of this study was to quantify and compare the imaging measurements between the two imaging modalities and determine if the degree of cervical flexibility had an impact clinical outcome. Materials/Methods: This retrospective study assessed 227 adult patients who underwent a three or more level posterior cervical fusion. Data collected included demographics, smoker status, radiographic measurements (T1 Slope, C2-C7 Lordosis, C2-C7 Sagittal Vertical Axis) from both XR films and MRI/CT scans, surgical and complication, as well as patient reported outcome measures for pain (Visual Analog Scale, VAS) and disability (Oswestry Disability Index, ODI). For each measurement technique, three cohorts were created based on distribution of the Δ between XR and MRI/CT values. Finally, the effect of demographic variables on measurement Δ was assessed. Results: Overall, the cohort (n = 227) was 53.7% female, with a mean age of 63 ± 13 years and BMI of 28.93 ± 6.6, 44% were never smokers. The most frequently treated (42.3%) spinal levels were C3-C7. Median Δ T1 Slope was 9°, with a range of -1° to 45°. T1 Slope cohorts: Group I with a Δ of < 4°; Group II ≥ 4° to < 15°; Group III ≥ 15°. Significant differences between Group I and Group III existed in VAS (4.19 and 6.59, respectively) and ODI (35.4 and 45.9, respectively). For Δ C2-C7 Lordosis, the median Δ value was 4°, with a range of -11° to 44°; Group I had a Δ lordosis of < 2°; Group II ≥ 2 to < 7°; Group III ≥ 7°. Significant differences between Group I and III existed in VAS (4.6 and 6.3, respectively) and ODI (36.7 and 45.5, respectively). Median Δ C2-C7 SVA was 14.37 mm, with a range of 37.6 mm to 110.2 mm. SVA Group I had a Δ of < 7.87 mm; Group II ≥ 7.87 mm to < 27.82 mm; Group III ≥ 27.82 mm. There were significant differences between Group I and Group III in VAS (4.8 and 6.4, respectively) and ODI (34 and 45.6, respectively). Revision and complication rates positively correlated with increased Δ measurement. ANOVA analysis of the effect of age, sex, gender, BMI and smoking status on each measurement technique demonstrated age having a significant effect on Δ C2-C7 SVA (p < 0.05). Conclusions: Larger Δ or cervical flexibility between XR and MRI/CT measurements are positively correlated with higher complication and revision rates. Patients with greater incidences of cervical flexibility reported significantly higher pain and disability scores compared to those with lower measurement Δ. Age was found to significantly impact Δ SVA measurement.
604
P146: Subaxial cervical fixation with lateral mass screws - A variant technique
Carlos Erosa Velázquez 1,2 , Apolinar de la Luz Laguna 3 , Sergio Ivan Reyna Heredia 1 , Edwin Rolando Sánchez Vallejo 4
1 Neurosurgery - Spine Surgery, Centro Médico Nacional 20 de Noviembre, Mexico City, Mexico
2 Spine Surgery, Neurosurgery, Hospital General Agustín O Horán, Merida, Yucatán, Mexico
3 Centro Medico Nacional 20 de Noviembre, C.P. 03100, Mexico City, Mexico
4 Neurosurgery-Spine Surgery, Instituto Mexicano del Seguro Social, Monterrey, N.L., Mexico
Introduction: The technique of fixation with lateral mass screws is a biomechanically effective management option for various pathologies of the subaxial cervical spine. The commonly known techniques include Magerl, Anderson, An, and Roy Camile, with the main differences lying in the entry point, divergent direction, and caudocephalic angulation of the screw placement. Material and Methods: The "20 de Noviembre" technique involves an entry point in the lower inner quadrant with a caudocephalic angulation of 50° and a 30° divergence. Preoperative planning is performed using tomography to obtain screw measurements, and intraoperative guidance is provided by placing the aspirator at the theoretical exit point. Results: Adaptations in subaxial cervical lateral mass fixation techniques have demonstrated success in preserving neural and vascular structures. The proposed "20 de Noviembre" technique shows promising results in maintaining neurovascular integrity. Current statistics, following a review of cases from the last two years, suggest success rates are closely related to the surgeon's experience. Conclusion: The "20 de Noviembre" technique for subaxial cervical lateral mass screws offers promising prospects for improving cervical spine stability. Its theoretical foundations and initial results support its effectiveness. Interdisciplinary collaboration and the integration of technologies such as augmented reality are essential for advancing medical techniques for the benefit of patients.
688
P147: Partial uncinatectomy combined with anterior cervical discectomy and fusion for the treatment of one-level cervical radiculpathy: analysis of clinical efficacy and sagittal alignment
Haimiti Abudouaini 1 , Hao Liu 2 , Beiyu Wang 2
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
2 Department of Orthopaedics, Sichuan University West China Hospital, Chengdu, China
Background: Biomechanical studies have demonstrated that uncovertebral joint contributes to segment mobility and stability to a certain extent. Simultaneously, osteophytes arising from the uncinate process are a common cause of cervical spondylotic radiculopathy (CSR). For such patients, partial uncinatectomy (UT) may be required. However, the clinical efficacy and sagittal alignment of partial UT during anterior cervical discectomy and fusion (ACDF) have not been fully elucidated. Methods: A total of 87 patients who had undergone single level ACDF using a zero-profile device from July 2014 to December 2018 were included. Based on whether the foraminal part of the uncovertebral joint was resected or preserved, the patients were divided into the ACDF with UT group (n = 37) and the ACDF without UT group (n = 50). Perioperative data, radiographic parameters, clinical outcomes, and complications were compared between the two groups. Results: The mean follow-up was 16.86 ± 5.63 and 18.36 ± 7.51 months in the ACDF with UT group and ACDF without UT group, respectively (p > 0.05). The average preoperative VAS arm score was 5.89 ± 1.00 in the ACDF with UT group and 5.18 ± 1.21 in the ACDF without UT group (p = 0.038). However, the average VAS arm score was 4.22 ± 0.64, 4.06 ± 1.13 and 1.68 ± 0.71, 1.60 ± 0.70 at 1 week post operation and at final follow up, respectively, (p > 0.05). We also found that the C2-7 SVA and St-SVA at the last follow-up and their change (last follow-up value − preoperative value) in the ACDF with UT group were significantly higher than ACDF without UT group (p < 0.05). No marked differences in the other cervical sagittal parameters, fusion rate or complications, including dysphagia, ASD, and subsidence, were observed. Conclusions: Our result indicates that ACDF using a zero-p implant with or without partial UT both provide satisfactory clinical efficacy and acceptable safety. However, additional partial UT may has a negative effect on cervical sagittal alignment.
Keywords: anterior cervical discectomy and fusion; uncinatectomy; uncovertebral joint; sagittal alignment; cervical spondylotic radiculopathy
727
P148: Vertebral ankylosis is associated with poorer cervical paraspinal muscle health
Junho Song 1 , Alex Ngan 1 , Austen Katz 1 , Priya Duvvuri 1 , John Fallon 1 , Luke Zappia 1 , Jeff Silber 1 , David Essig 1 , Sohrab Virk 1
1 Orthopedics, Northwell Health, New York, USA
Introduction: Spinal disorders such as ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH) are associated with ankylosis of the vertebrae, which can lead to spinal stiffness and back pain. The biomechanical changes secondary to vertebral ankylosis can predispose patients to spinal deformity, degeneration, and fractures (Britto 2018). The potential influence of vertebral ankylosis on paraspinal muscle health has not been previously investigated, however, recent literature has correlated paraspinal muscle health with functional outcomes in spine patients (He 2023). Therefore, investigating this topic may provide additional insight into the complex pathophysiology of vertebral ankylosis. Material and Methods: Retrospective review of a consecutive series of patients with degenerative cervical spine disease. Patients with confirmed diagnoses of AS or DISH were identified and matched with patients without AS or DISH based on age, sex, and body mass index. Radiological muscle health measurements were performed on axial T2-weighted MRI at all intervertebral levels between C2 and T1. Bilateral cross-sectional areas (CSA) of the cervical deep flexors (DF) and deep extensors (DE) were measured. The degree of muscle fatty infiltration was assessed by applying the Goutallier classification. Muscle health measurements were compared between the two matched cohorts. Results: Seventeen patients with diagnosis of AS or DISH were matched with 17 patients without AS/DISH diagnoses. Compared to the control group, patients with vertebral ankylosis had smaller DE CSA at C2-C3 (351.3 vs. 590.2 mm2, p = 0.048), C4-C5 (327.6 vs. 572.4 mm2, p = 0.027), C5-C6 (360.6 vs. 554.0 mm2, p = 0.039), and C6-C7 (441.1 vs. 644.7 mm2, p = 0.033). There was no significant association between vertebral ankylosis and DF CSA at any level between C2-T1 (p > 0.05). Additionally, patients with vertebral ankylosis had higher average Goutallier grades at C5-C6 (2.92 vs. 1.85, p < 0.001) and C7-T1 (3.23 vs. 2.02, p < 0.001). Conclusion: Vertebral ankylosis was found to be associated with worse cervical paraspinal muscle health at multiple intervertebral levels. On average, patients with diagnoses of AS or DISH were found to have smaller CSAs of cervical DE muscles. Vertebral ankylosis was also associated with greater amounts of paraspinal muscle fatty infiltration, particularly at the lower cervical levels. These findings highlight a potential link between vertebral ankylosis and paraspinal muscle health. Additional analyses including greater sample sizes are warranted to confirm these findings.
792
P149: Surgery for non-inflammatory degenerative atlantodental instability: operative strategy and clinical outcome in 36 patients
Vicki Butenschön 1 , Raimunde Liang 1 , Bernhard Meyer 1
1 Department of Neurosurgery, Technical University Munich, Munich, Germany
Introduction: Patients suffering from C1-C2 instability with spinal cord compression may suffer from burdening neck pain and myelopathy, reducing their mobility and quality of life. Formerly known as a distinct entity in rheumatoid arthritis, C1-C2 instability may occur due to severe degenerative arthrosis in older patients without being caused by former autoimmune or inflammatory factors. Material and Methods: We retrospectively assessed all patients undergoing C1-2 stabilization for symptoms and radiographical signs of C1-2 instability with a retrodental pannus in our neurosurgical department from January 2012 to December 2021. We excluded all patients with inflammatory diseases. Radiological parameters, surgical data, and clinical follow-up data were retrieved from our records to investigate the clinical outcome. Results: In total, we included 36 patients for further analysis. The mean age was 72 years. All patients underwent C1-2 fixation with a fusion of the C1-C2 joint, and 61% underwent a decompression via C1 laminectomy for clinical symptoms of myelopathy. The median mJOA score improved from 14/18 preoperatively to 15/18 after surgery and a score of 16/18 at a median follow-up of 3 months. The mean preoperative atlantodental distance was 2mm. 71% of the patients improved clinically after surgery, 29% remained stable, and 9.7% deteriorated at follow-up. The overall complication rate was low at 8.6%, including two asymptomatic vertebral artery injuries and one CSF leakage. Conclusion: C1-C2 fixation achieved satisfying results in our large series of patients suffering from non-inflammatory atlantoaxial instability. Patients suffering from neck pain and symptoms of myelopathy improved until follow-up with the posterior approach.
867
P150: Why does it hurt? Why doesn't it hurt? In particular Keegan Palsy Symptoms associated with C5 palsy of cervical spondylosis and rationale for its surgical treatment
Takahiro Iizuka 1 , Toyohito Iwami 1 , Tokuji Kashiro 1 , Hiroshige Debata 1 , Tetsuro Takai 1
1 Orthopedic Spine Surgery, Kouseikai Takai Hospital, Nara, Japan
Introduction: Patients come to the clinic with sudden onset of a dropped arm often necessary to differentiate pathologies because C5 palsy isn't associated with sensory symptoms. This is widely called Keegan palsy. In those patients, we require differentiation between C5 palsy, brain disorders, motor neuron diseases, and others. We discussed the pathological state and the cause of the difficulty in making a definitive diagnosis. Subjects and Methods: The subjects were 6 patients with C5 palsy that occurred with degenerative changes during the 10-year from 2013, who were treated surgically without improvement more than 3 months after onset. All patients complained of difficulty in raising the upper limbs. Although they complained of elbow flexion disorder and/or mild numbness, they did NOT complain of radiating pain like a cervical hernia. Results: # 1: Image Findings
1. Radiography: Only mild degenerative changes in the Luschka joint with osteophyte.
2. MRI: Three cases of spinal canal stenosis were found in our series. The problem is in particular poor MRI resolution in the cervical spine especially in the parasagittal plane at the C4 -6 level to evaluate foraminal stenosis.
3. Myelography and axial CT myelography have a similar amount of information. However, in the reconstructed Coronal view on CT myelography, the deformative changes in the Luschka joint and the osteophytes in the intervertebral foramen can be identified, which is quite useful for finding pathological change.
# 2 Symptoms: C5 palsy (Keegan Paly) is commonly acute onset without other symptoms (pain and/or numbness). Is it a physical disorder in which neurological damage occurs only in the C5 Motor Segment? The causes of pain induction are (1) direct encroachment of pain receptors and (2) Dorsal Root Ganglia irritation, but C5 palsy occurs in the cervical spinal canal without impairment of the C5 Sensory Segment. Just after it branches from the cord, the rootlets join and exit the intervertebral foramen, which forms DRG and migrates to the peripheral nerve. If there could be a condition in which the anterior rootlet was only damaged in the dura of the canal, none of the six patients experienced NO myelopathy, and NO pain/NO sensory disturbances. It was a unique condition in which only the anterior rootlet derived from C5 was damaged in a tiny space. C 4/5 anterior fixation was performed in order to enlarge C4/5 foramen, and within 1 -2 months after surgery, all patients were able to elevate their arms. Discussion: We experience C5 palsy as a unique first symptom, it does NOT accompany pain. The diagnosis is more essential. This condition can be identified in the CT coronal view over a narrow range from the DRG to the spinal canal. Enlargement of the foramen with anterior fixation of C 4/5 solved the foraminal stenosis and the motion irritation. The palsy has improved in all cases. Above all, it is crucial to scrutinize the disease state and ultimately select a treatment method. we are convinced that C4/5 anterior fixation is the right choice, good results will always be obtained.
906
P151: Clinical efficacy of single-open door laminoplasty for multilevel cervical spondylotic myelopathy and morphology analysis
yong xu 1 , Feng Li 1
1 Department of Orthopedics, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, WuHan, China
Objectives: To investigate the clinical efficacy of single-open door laminoplasty for multilevel cervical spondylotic myelopathy. Anderson using the JOA score and postoperative MRI images to analyze the factors leading to different postoperative efficacy. Methods: 39 patients were successfully followed up. They are divided in two groups duo to the postoperative MRI sagittal images. The ‘free group’ contains patients without spinal cord compression while the ‘contact group’ contains patients with spinal cord compression. Patients’ data such as age, gender, duration of disease, causes of spinal cord compression, preoperative and postoperative JOA score and JOA improvements were recorded; Other data such as preoperative postoperative cervical curvature, activity of cervical vertebra, the occupation rate of the spinal canal and the diameter of compression were recorded as well. Results: There were no significant differences in the age, follow-up time and preoperative JOA score between two groups (p > 0.05). The postoperative JOA scores of the two groups were all superior to those before operation (p < 0.05). The improvement rate of JOA in group Free was better than that of Contact group, and there were statistical differences between the prevalence of OPLL and between the duration of disease of the two groups (p < 0.05). The maximum diameter of the anterior compression, the average rate of vertebral canal invasion between the two groups are statistically different (p < 0.05). Correlation analysis showed that the postoperative JOA improvement rate is relate to the following factors: duration of disease, preoperative cervical curvature and the maximum size of the anterior compression, the occupation rate of spinal canal, preoperative cervical activity. Superior correlation with preoperative and postoperative patients with spinal cord (p < 0.01). Regression equation was obtained for the above data. In the final regression equation, the rate of postoperative JOA improvement was related to the duration of disease and the rate of preoperative spinal canal occupation. Conclusions: Cervical posterior single open-door laminoplasty surgery is an effective way for the treatment of multi segmental cervical spondylotic myelopathy.Postoperative improvement rate was closely related to the patients' preoperative morbidity and the spinal canal occupation rate. Patients with less spinal canal occupation rate would be better after operation.
1119
P152: Zero-profile screw-locking stand alone spacer (Titanopeek) for treatment of cervical degenerative disc disease and avoiding adjacent segment disease
Dimitar Haritonov 1
1 Neurosurgery and Spine Surgery, Heart and Brain Hospital Pleven, Pleven, Bulgaria
Introduction: Screw-locking stand-alone cages have increasingly been used in anterior cervical discectomy and fusion (ACDF) for cervical degenerative disc disease (CDDD). We studied clinical and radiological outcomes of patients who underwent zero-profile screw-locking spacer (Titanopeek) – assisted ACDF without anterior plate fixation in cervical degenerative disc disease for prevention of adjacent segment disease (ASD). Material and Methods: Thirty five patients (69 segments - 10 single level, 18 - two levels, 5 - three levels and 2 - four levels ACDF) suffering from cervical degenerative disc disease with various symptoms, such as radiculopathy, myelopathy, or both, were retrospectively evaluated. The cervical degenerative disc disease (including spinal canal stenosis - mono or multisegmental, disc herniation, lost of cervical lordosis) was confirmed by plain radiographs, CT scan and magnetic resonance imaging. The patients underwent radiological evaluation to assess cervical lordosis, intervertebral height, OPLL. Clinical assessment was graded using a visual analog scale, Modified Japanese Orthopedic Association score, and the Neck Disability Index. Results: There were 69 levels of surgery - 10 single level, 18 - two levels, 5 - three levels and 2 - four levels ACDF). In the postoperative period, our study revealed significant improvement in the clinical outcome. The cervical curvature and intervertebral height were significantly improved at 18-months follow-up (p < 0.05). The fusion rate was 100% (filled with glassbone), whereas no subsidence occurred. There was only one case of mild dysphagia, which resolved in less than 2 weeks. The 18 months follow-up showed only 2 patients (5.71%) with evidence for adjacent segment disease (ASD) - no clinical, only radiological signs. Conclusion: This study indicates that zero-profile screw-locking spacer (Titanopeek) in the treatment of cervical degenerative disc disease provides improvement of clinical outcomes, restoration of lordosis, high fusion rate, and low incidence of dysphagia. However, radiological evidence for adjacent segment disease occurred in 5.71% of cases, but did not cause clinical symptoms.
Keywords: zero profile cervical cage, screw-locking stand alone cervical cage, cervical degenerative disc disease
1130
P153: Cervical spine injury with underlying cervical myelopathy: a case series analysis
Fikri Hasif Mohd Nordin 1,2 , Asrul Syamim Hisyam Yong 1 , Satpal Charl 1 , Amir Zakaria 3
1 Orthopaedic, Hospital Sultan Idris Shah, Kajang, Malaysia
2 Orthopaedic, Universiti Sains Malaysia, Kota Bharu, Malaysia
3 Orthopaedic, Hospital Sungai Buloh, Sungai Buloh, Malaysia
Introduction: Cervical spine injuries with underlying cervical myelopathy pose a significant clinical challenge, as they have the potential to lead to substantial neurological impairments and unfavorable outcomes, even when caused by low-energy trauma. This case series seeks to analyze the clinical presentation, treatment approaches, and resulting outcomes of patients admitted with this particular diagnosis. Material and Methods: A retrospective analysis was conducted on four male patients admitted to our institution with a diagnosis of cervical spine injury with underlying cervical myelopathy. The mean age of these patients was 59 years old. All cases were a result of low energy trauma. Among them, three patients had incomplete Spinal Cord Injury ASIA B, while one patient presented with complete Spinal Cord Injury ASIA A. Visual Analog Score (VAS) for all patient average at around 5-7. Imaging revealed spinal cord stenosis with spondylitic changes, along with the presence of Ossification of Posterior Longitudinal Ligament (OPLL) and cord edema in all cases. Treatment commenced with high dose Intravenous Corticosteroid. All patients underwent Immediate Posterior Decompression and Stabilization. Results: Two patients survived and demonstrated good neurological progress. Initially, both patients were classified with ASIA B for their spinal cord injury. However, postoperatively, they both achieved an advancement to ASIA D. Their postoperative VAS scores ranged from 0-2. The remaining two patients passed away due to Hospital Acquired Infection. Conclusion: This case series highlight the severity of spinal cord injury even when caused by low-energy trauma in patients with underlying cervical myelopathy. The use of high dose corticosteroids and surgical intervention proved to be effective in improving neurological outcomes. Vigilant postoperative care, good rehabilitation program and infection prevention is crucial to achieve favourable outcomes.
1151
P154: Combined retropharyngeal release with posterior fixation for the treatment of irreducible atlantoaxial dislocation: a retrospective study of 37 patients
Feng Li 1
1 Orthopaedics, Tongji Hospital of Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
Introduction: Irreducible atlantoaxial dislocation (IAAD) has been challenging for surgeons. Various methods have been used to treat IAAD, but no consensus has been reached. Although widely applied, transoral approach is accompanied with high morbidity and mortality. Anterior retropharyngeal approach could be an alternative method with several advantages relative to transoral approach. This study aimed to retrospectively analyze efficacy and safety of anterior retropharyngeal releasing and posterior fixation for IAAD. Material and Methods: From March 2010 to May 2020, a total of 37 patients diagnosed with IAAD underwent anterior retropharyngeal release and sequential posterior instrumented fusion in our department. Atlantoaxial release was gained by resecting the scar, ligament and interarticular osteophyte around atlantoaxial articular through Smith-Robinson approach. The operation time, blood loss, post-operation hospital stay and peri-operation complications were retrospectively recorded. Clinical outcomes were assessed by Japanese Orthopedic Association (JOA) score, and radiological reduction by atlantodental interval (ADI) and cervicomedullary angle (CMA). Results: The series included 26 males and 11 females with a mean age of 48.0 ± 18.7 years (range, 18-79 years). Average follow up duration was 40.8 ± 12.4 months (range, 24-72 months). The pathology of IAAD included 12 cases of nonunion of odontoid fracture, 10 cases of os odontoideum, 12 cases of occipitalisation of C1, and 3 cases of rheumatoid arthritis. Occipitocervical fixation was performed in 14 patients and C1-2 pedicle screw fixation in 23 patients. The mean operation time was 215.6 ± 41.5 min (range, 150-300 min) with a mean blood loss of 246.5 ± 123.7 ml (range,100-600 ml). All patients discharged home with a mean post-op hospital stay of 6.6d ± 1.5 (range, 4-10d), without deteriorated neurological function. The JOA significantly improved from 9.94 ± 1.53 pre-op (range, 7-12) to 14.69 ± 1.13 post-op (range, 12-16) (p < 0.001). 29 patients had anatomic reduction while 8 had partial. The mean ADI significantly decreased from 9.94 ± 1.01 mm (range, 8.4-11.6 mm) to 3.03 ± 0.45 (range, 2.0-3.6 mm) post-operation (p < 0.001). The CMA significantly improved from a mean pre-op angle of 125.50 ± 5.37° (range, 117-133) to a mean post-op angle of 149.25 ± 4. 23° (range, 141-158) (p < 0.001). 2 patients suffered cerebrospinal fluid leakage when releasing the ligament around odontoid process, which successfully treated by continuous lumbar subarachnoid drainage. Besides,6 patients suffered dysphagia and hoarseness, and 5 relieve within 3 months completely. Only 1 patient suffered nonunion and subsequent reduction loss at 1 year follow up with recurrent myelopathy. Then trans-oral odontoidectomy and fixation was performed with postoperative neurological improvement. No hardware failure occurred during the follow-up duration. Conclusion: This series prove the safety and efficacy of anterior retropharyngeal release for reduction of IAAD. Anterior retropharyngeal release could remove the pathological factors hindering reduction of atlantoaxial dislocation effectively without major complications. Retropharyngeal release and posterior instrumented fusion are a alternative method for IAAD.
1243
P155: Impact of smoking status on outcomes following anterior cervical discectomy and fusion surgery
Jillian Mohn 1 , Madilyn Riegel 1 , Joseph Lee 2 , Leo Spector 3 , Benjamin Chen 4 , Bruce Darden 3 , Anthony Kwon 3 , Eric Laxer 3 , Alden Milam 3 , Alfred Rhyne 3 , Paul Bradley Segebarth 3 , Hallie Murray 1
1 Tyber Medical, LLC, Clinical Research, Bethlehem, USA
2 Rothman Orthopaedic Institute, Tarrytown, USA
3 OrthoCarolina, Charlotte, USA
4 MultiCare, Puyallup, USA
Introduction: Previous research has proven that smoking is highly detrimental to overall health and is associated with several diseases including, but not limited to, respiratory disease, cancer, and cardiovascular disease. Furthermore, research has shown that smoking is a significant risk factor for poor surgical outcomes following spine surgery. Nevertheless, some researchers have disputed such findings and did not find a relationship between smoking and adverse surgical outcomes. The objective of this study was to assess the clinical and radiographic outcomes of smoking status when patients are treated with porous titanium coated polyether-ether-ketone (ProTi) interbody fusion devices for degenerative cervical spine conditions. Materials and Methods: Institutional Review Board approval was obtained to perform a retrospective and prospective registry gathering data on subjects treated with ProTi interbody fusion devices to correct degenerative spine conditions. Subjects were divided into three categories: non-smoker, ex-smoker, and current smoker. Subjects were then evaluated for clinical healing and radiographic fusion. Patient reported outcome measurements (PROMs), including the Neck Disability Index (NDI) and Visual Analog Scale (VAS), assessed patient functionality and pain before and after treatment in a subset of subjects. Statistical significance was calculated between pre-operative and final post-operative measurements using a two-tailed, paired T-test with significance set at p < 0.05. Results: Included in the analysis were 54 patients who underwent a 1-level, 2-level, or 3-level fusion, with 28 (51.85%) non-smokers, 16 (29.63%) ex-smokers, and 10 (18.52%) current smokers. Radiographically, non-smokers achieved a mean time to fusion of 12.25 ± 6.73 months, whereas ex-smokers achieved a mean time to fusion of 10.56 ± 7.90 months, and current smokers achieved a mean time to fusion of 12.05 ± 4.89 months. A subset of patients (N = 25) completed PROMs at pre-operative and final clinic visits. Non-smokers demonstrated significant improvement in NDI (p = 0.017) scores, VAS neck scores (p = 0.004), and improvement in VAS right upper extremity (p = 0.151) and left upper extremity scores (p = 0.064), although not statistically significant. Alternatively, former and current smokers had no statistically significant improvement in PROMs although ex-smokers had a trend in improved NDI (p = 0.066) and VAS upper extremity scores (p = 0.087). Additionally, ex-smokers and current smokers reported higher post-operative complications: 3 patients (1 ex-smoker, 2 current smokers) (5.5%) had subsidence, 2 patients (1 ex-smoker, 1 current smoker) (3.7%) had adjacent level disc disease (1 patient required revision surgery), and 1 patient had dysphagia (current smoker) that resolved by 3.5 months post-operative. Conclusion: Results suggest that smoking status does not negatively impact the mean time to fusion when patients are treated with ProTi interbody fusion devices for degenerative spine conditions. The porous titanium coating has been shown to accelerate bony deposition preclinically and may encourage osseointegration supporting fusion outcomes. However, former and current smokers did not have a statistically significant improvement in pain or functionality scores and were more likely to develop post-operative complications. While ProTi interbody fusion devices can support successful outcomes in patients at risk for impaired bone healing, including smokers, patient education on the risks associated with smoking is important to support the best clinical outcomes.
1310
P156: Association between postoperative fever and readmission rates following cervical fusion
Parker Brush 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Alexa Tomlak 1 , Michael Carter 1 , Michael McCurdy 1 , Matthew Meade 2 , Blaire Adler 3 , Amar Vadhera 3 , Saurav Sumughan 3 , Alan Hilibrand 1 , Jose Canseco 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Gregory Schroeder 1
1 Spine Department, Rothman Orthopaedic Institute, Philadelphia, USA
2 Rowan University, Glassboro, USA
3 Thomas Jefferson University, Philadelphia, USA
Introduction: This study aimed to assess the rate of postoperative fever in cervical fusion patients and evaluate its impact on readmission rates, length of hospital stay, healthcare utilization, and rates of revision surgery. Material and Methods: This study was conducted at an urban academic medical center by ten fellowship-trained spine orthopaedic surgeons. The electronic medical record was retrospectively reviewed for patients who underwent elective cervical fusion procedures utilizing either a combined anterior and posterior approach or posterior only approach from 2016 to 2021. Revision procedures for adjacent-level or recurrent same level disease were also included, all other revision cases were excluded. Cases related to trauma, infection, malignancy, staged anterior and posterior procedures, or incomplete temperature documentation were excluded. Patient data, including demographics, comorbidities, surgical indications, operative details, and length of hospital stay, were collected. Readmission rates within one year of surgery were also documented. Patients were categorized into "No-Fever" (no documented fever) and "Fever" (documented postoperative fever) groups, with postoperative fever defined as a temperature > 100.4°F. Additional temperature-related data and medical tests ordered in response to fever were documented. Patients with identified fevers were propensity-matched to those without fevers based on sex, age, BMI, diabetes, smoking status, and levels fused posteriorly. Bivariate analyses employed chi-square or Fisher's exact test for categorical variables, and t-test or Mann-Whitney U-test for continuous variables. Results: Among 884 patients, 54 (6.1%) developed postoperative fever during their hospitalization. After propensity matching, the fever group was compared to 108 fever-free patients. No significant differences were found in demographics, comorbidities, surgical details, or preoperative diagnosis between the two groups. Likewise, there were no significant disparities in preoperative diagnosis, primary vs. revision procedures, surgical approach, number of fused levels, or operative duration. Patients with postoperative fever had an average hospital stay that was significantly longer than the no-fever group (5.14 days vs. 3.17 days, p = 0.001). Fever workup included various tests, but only 14.8% of tests conducted identified an underlying cause for the fever. In other words, within the "Fever" group, only 7.4% of patients had a discernible reason for their postoperative fever, with infection found in only 1.9% of patients. The "Fever" group had a significantly higher mean number of chest radiographs ordered per patient compared to the "No-Fever" group (0.33 vs. 0.05, p = 0.006). The two cohorts showed similar numbers of blood cultures, urine cultures, or vascular ultrasounds per patient. White blood cell counts did not significantly differ between the groups. There were no significant differences in readmission incidence (p = 0.316) or time to readmission (11.8 days vs. 24.8 days, p=0.395) between the groups. Conclusion: Postoperative fever following cervical spine surgery is relatively common but rarely indicates infection. It leads to extensive diagnostic workups and longer hospital stays without increasing readmission rates. This study underscores the need for a more focused and cost-effective approach to evaluating postoperative fever, suggesting that early discharge may reduce healthcare costs without compromising patient safety.
1323
P157: Impact of collar use on patient reported outcomes measures after anterior cervical decompression and fusion
Olivia Opara 1 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , William DiCiurcio 2 , Nicholas Pohl 1 , Omar Tarawneh 1 , Sebastian Fras 1 , Thomas Swiderski 3 , Sam Alfonsi 3 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Orthopaedics, Rothman Orthopaedic Insitute, Philadelphia, USA
2 Orthopaedics, Rowan University, New Jersey
3 Thomas Jefferson University, Philadelphia, USA
Introduction: Using cervical collars after cervical fusion postoperatively has been used to immobilize the neck with the proposed benefits of relieving postoperative pain and improving patient comfort. However, the scientific literature on the clinical use of collars after anterior cervical decompression and fusion (ACDF) remains controversial. This study aims to determine the effect of no-collar versus collar on patient-reported outcome measures (PROMS) after ACDF surgery. Material and Methods: After obtaining Institutional Review Board approval, we retrospectively identified patients at a single tertiary-referral care center undergoing ACDF surgeries between 2017-2022. Patients were grouped into no collar and soft or hard collar use. Patient demographics, surgical characteristics, and outcomes were collected from the institution's electronic medical records. Patient-reported outcome measures (PROMs) preoperatively and postoperatively at 3 months, 6 months, and 1 year, including VAS neck/arm score, Neck Disability Index (NDI), mental health component score (MCS-12), and physical component scores (PCS-12) of the short form-12 survey and Modified Japanese Orthopedic Association (mJOA) were analyzed. ΔPROMS were calculated by subtracting postoperative from preoperative values. Bivariate analysis was analyzed by comparing both groups and multivariate linear regressions were used to identify factors independently associated with ΔPROMS. All statistical analyses were performed using R Studio Version 4.1.2 (Boston, MA), with p values < 0.05 considered statistically significant. Results: Of the 253 patients included in our study, 78 did not receive a collar, and 175 received a soft or hard collar postoperatively. Demographically, there was no significant difference among both groups (p > 0.05). However, the total number of levels operated on demonstrated a significant difference in both groups, with three-level surgery having twice as many patients receiving collars (12.8% vs. 29.7%; p = 0.003). Both collar and non-collar groups had no significant difference in preoperative and postoperative NDI, VAS neck/arm, MCS, and PCS scores, except for an improvement in 6-month ΔmJOA in the no collar group (0.46 vs. -0.05, p = 0.029). There were no significant differences between the collar and no-collar groups regarding 90-day readmissions, revisions, and complications. Multi-regression analysis shows that collar use significantly predicted worsening outcomes in 6-month ΔVAS Arm (Est 20.67, CI = 14.78 – 26.56, p ≤ 0.001). Conclusion: Our results show that in one- to three-level ACDFs, collar use postoperatively is not associated with a significant positive difference in functional outcomes in the short or long term. Instead, it may even be associated with reduced improvement of arm pain postoperatively.
1346
P158: Statistical power of a smartphone app to objectively monitor performance outcomes in degenerative cervical myelopathy: power analysis of a simulated randomised controlled trial using data from an observational cohort
Benjamin Davies 1,2,3 , Alvaro Yanez 2 , Tatiana Houhou 2 , Zerina Rahic 2 , Mark Kotter 1
1 Neurosurgery, University of Cambridge, Cambridge, United Kingdom
2 MoveMed Ltd, Cambridge, United Kingdom
3 Myelopathy.org, Cambridge, United Kingdom
Introduction: Developing new clinical measures for degenerative cervical myelopathy (DCM) is an AO Spine RECODE-DCM Research priority. Difficulties detecting DCM, and change in DCM, cause diagnostic and treatment delays in clinical settings and heightened costs in clinical trials due to elevated recruitment targets. Digital outcome measures can tackle these challenges due to their ability to measure disease remotely, repeatedly, and more economically. This study aimed to assess the statistical power of MoveMed, a battery of performance outcome measures performed using a mobile phone application, in a simulated research trial. Material and Methods: This was a quantitative modelling using prospective data from an observational and decentralised study in England, United Kingdom. 27 adults aged 60 (SD: 11) who live with DCM, possess an approved smartphone, and participated in the decentralised EMPOWER study. The primary outcome was the sample size required by the simulated clinical trial to demonstrate superiority of a treatment or intervention using a continuous outcome measure. Sample size was modelled using a validated power calculator (Sealed Envelope Ltd) and benchmarks from peer-reviewed DCM literature (alpha: 5%, power: 80%, standard deviation of the modified Japanese Orthopaedic Association Score, mJOA: 2.7). There were no secondary outcomes. Results: MoveMed reduced the sample size of the simulated trials by two-thirds, on average. Power analysis found that a simulated trial using the mJOA to detect a one-point decrease in control vs. experimental group would need to recruit 230 patients (115 per arm) to demonstrate superiority. Preliminary results found that endpoints from the Fast Tap, Hold, Typing, and Stand and Walk Tests could detect the equivalent point decrease with 118 (59 per arm), 22 (11 per arm), 16 (8 per arm), and 146 (73 per arm) patients, respectively. This would entail a 40%-90% reduction in the sample size required to demonstrate superiority of treatment or intervention in DCM. Conclusion: Improving measurement of DCM is an AO Spine RECODE-DCM research priority. In silico analysis of preliminary EMPOWER findings suggest MoveMed’s digital endpoints could reduce trial recruitment importantly. The potential for MoveMed to transform trials could be significant.
1351
P159: Usability and patient perception of a smartphone app to objectively monitor performance outcomes in degenerative cervical myelopathy: an observational study
Benjamin Davies 1,2,3 , Zerina Rahic 2 , Tatiana Houhou 2 , Alvaro Yanez 2 , Mark Kotter 1
1 University of Cambridge, Cambridge, United Kingdom
2 MoveMed Ltd, Cambridge, United Kingdom
3 Myelopathy.org, Cambridge, United Kingdom
Introduction: Developing new clinical measures for degenerative cervical myelopathy (DCM) is an AO Spine RECODE-DCM Research priority. Difficulties detecting DCM, and change in DCM, cause diagnostic and treatment delays in clinical settings and heightened costs in clinical trials due to elevated recruitment targets. Digital outcome measures can tackle these challenges due to their ability to measure disease remotely, repeatedly, and more economically. This study aimed to assess the usability and patient experience of MoveMed, a battery of performance outcome measures performed using a mobile phone application. Material and Methods: 27 adults aged 60 (SD: 11) who live with DCM and possess an approved smartphone, and participated in the EMPOWER prospective observational study. Draft guidance from the Food and Drug Administration (FDA) were used to assess usability. The primary outcome was the completion rate of the MoveMed battery of digital performance tests. The secondary outcomes were the test adherence rates and optimised compliance rates. Patient perception was also used as a qualitative surrogate. Results: 100% (27/27) of participants were able to enter all data into the MoveMed App. Median adherence to the prescription ‘Do 1 test every 14 days’ was ≥ 80% for all tests in the battery: 100% for the Fast Tap, Hold, and Stand and Walk Tests, and 80% for the Typing Test. Mean rates differed across the battery: 100% and 90% for the Fast Tap and Hold Tests, and 77% and 72% for the Stand and Walk and Typing Tests. Nonetheless, in absolute terms, more participants used the Stand and Walk and Typing Tests (N ≥ 20) than the Fast Tap and Hold Tests (N ≥ 12). Qualitative feedback suggested differences were attributable to individual test preferences (e.g., participants with DCM predominantly affecting lower limb function preferred performance testing of lower limbs over upper limbs, or participants deriving more enjoyment from certain performance methods over others). Optimised compliance rates suggested the ideal prescriptions for the Fast Tap and Hold Tests were ‘once every 10 days’; ‘once every 8 days’ for the Typing Test; and ‘once every 13 days’ for the Stand and Walk Tests. Taken together, these results suggest that the MoveMed App is a highly usable and feasible digital health technology for remote data acquisition in DCM. Conclusion: Improving measurement of DCM is an AO Spine RECODE-DCM research priority. Parameters from FDA draft guidance found the MoveMed App usable in an adult population living with DCM. MoveMed’s digital outcome measures could have a transformative impact in the measurement of DCM.
1352
P160: Reliability of a smparthone app to objectively monitor performance outcomes in degenerative cervical myelopathy: an observational study
Benjamin Davies 1,2,3 , Zerina Rahic 2 , Tatiana Houhou 2 , Alvaro Yanez 2 , Mark Kotter 1
1 University of Cambridge, Cambridge, United Kingdom
2 MoveMed Ltd, Cambridge, United Kingdom
3 Myelopathy.org, Cambrige, United Kingdom
Introduction: Developing new clinical measures for degenerative cervical myelopathy (DCM) is an AO Spine RECODE-DCM Research priority. Difficulties detecting DCM, and change in DCM, cause diagnostic and treatment delays in clinical settings and heightened costs in clinical trials due to elevated recruitment targets. Digital outcome measures can tackle these challenges due to their ability to measure disease remotely, repeatedly, and more economically. This study aimed to assess the reliability of MoveMed, a battery of performance outcome measures performed using a mobile phone application, in the measurement of DCM. Material and Methods: 30 adults aged 58 (SD: 10) who live with DCM and possess an approved smartphone, participated in a prospective and decentralised observational study (EMPOWER). Criteria from the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) manual were used to assess reliability and risk of bias. Briefly, longitudinal repeats of MoveMed outcomes were assessed for test-retest reliability against consensus thresholds. The primary outcome was the test-retest reliability of the MoveMed performance outcomes and was measured using the intra-class correlation of agreement (ICCagreement) statistic. The threshold for test-retest reliability was 0.7. The secondary outcomes was the measurement error of the MoveMed performance outcomes and was measured using the standard error of agreement of the mean (SEMagreement) and the smallest detectable change of agreement (SDCagreement). Results: All tests obtained a sufficient rating for test-retest reliability (ICCagreement ≥ 0.7). ICCagreement values for the Fast Tap, Hold, Typing, and Stand and Walk Tests were, respectively: 0.74-0.84, 0.85-0.86, 0.89, and 0.90. SEMagreement values for the same were: ±1.4-1.5 taps, ±3-5% stability score points, ±0.09 keys per second, and ±7 steps per minute. SDCagreement values were ±4 taps, ±9-14% stability score points, ±0.3 keys per second, and ±18 steps per minute, respectively. No risk of bias factors from the COSMIN Risk of Bias checklist were recorded. Overall, this was equivalent to ‘very good’ quality evidence of sufficient reliability in DCM, as per COSMIN guidance. Conclusion: Improving measurement of DCM is an AO Spine RECODE-DCM research priority. COSMIN criteria provide ‘very good’ quality evidence of the reliability of the MoveMed tests in an adult population living with DCM. MoveMed’s digital outcome measures could have a transformative impact in the measurement of DCM.
1356
P161: Validity of a smartphone app to objectively monitor performance outcomes in degenerative cervical myelopathy: an observational study
Alvaro Yanez 1 , Zerina Rahic 1 , Tatiana Houhou 1 , Mark Kotter 2 , Benjamin Davies 1,2
1 MoveMed Ltd, Cambridge, United Kingdom
2 University of Cambridge, Cambridge, United Kingdom
Introduction: Developing new clinical measures for degenerative cervical myelopathy (DCM) is an AO Spine RECODE-DCM Research priority. Difficulties detecting DCM, and change in DCM, cause diagnostic and treatment delays in clinical settings and heightened costs in clinical trials due to elevated recruitment targets. Digital outcome measures can tackle these challenges due to their ability to measure disease remotely, repeatedly, and more economically. This study aimed to assess the validity of MoveMed, a battery of performance outcome measures performed using a mobile phone application, in the measurement of DCM. Material and Methods: 30 adults aged 58 (SD: 10) who live with DCM and possess an approved smartphone, participated in a prospective and decentralised observational study (EMPOWER). Criteria from the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) manual were used to assess validity and risk of bias. Briefly, each MoveMed outcome was compared to two patient-reported comparators, and a priori hypotheses of convergence/divergence were tested against consensus thresholds. The primary outcome was the correlation coefficient between the MoveMed outcome and the patient-reported comparators. The comparators were the patient-derived modified Japanese Orthopaedic Association (P-mJOA) score and the World Health Organization Quality of Life Brief Version (WHOQOL-Bref) questionnaire. Thresholds for convergence/divergence were ≥ 0.3/< 0.3, and > 0/< 0 for directionality. The secondary outcome was the percent of correlations in correspondence with a priori hypotheses. Results: As expected, MoveMed’s tests of neuromuscular function correlated most with questionnaires of neuromuscular function (≥ 0.3) and least with questionnaires of quality of life (< 0.3). Directly related constructs, furthermore, correlated positively to each other (> 0), while inversely related constructs correlated negatively (< 0), as hypothesised. Furthermore, over 70% of unidimensional correlations were in accordance with hypotheses, as were 50% of multidimensional correlations. No risk of bias factors from the COSMIN Risk of Bias checklist were recorded. Overall, this was equivalent to ‘very good’ quality evidence of sufficient construct validity in DCM, as per COSMIN guidance. Conclusion: Improving measurement of DCM is an AO Spine RECODE-DCM research priority. COSMIN criteria provide ‘very good’ quality evidence of the validity of the MoveMed tests in an adult population living with DCM. MoveMed’s digital outcome measures could have a transformative impact in the measurement of DCM.
1430
P162: A rare case of phrenic nerve palsy after posterior cervical spine surgery
Tanmay Datey 1 , Akash Mane 1 , Sangram Rajale 1 , Umesh Kanade P 1 , Mandar Borde 1 , K Venugopal Menon 1
1 Spine Surgery, Bharati Vidyapeeth Medical College and Hospital, Pune, India
Introduction: Phrenic nerve palsy is a rare complication of cervical spine surgery. There are very few previously reported cases of unilateral diaphragmatic paralysis following posterior cervical spine surgery. In our case study, we presented a case of a 61-year-old male with cervical canal stenosis and myelopathy for which we did C4 to C7 laminectomy and lateral mass screw fixation. Postoperatively the patient developed right C5 palsy affecting his deltoid function which gradually improved. Materials and Methods: A 61-year-old gentleman presented to the spine outpatient department with neck pain, spastic gait, and right upper limb radiculopathy. A history of slipping footwear was present. He has a known case of Diabetes mellitus, hypertension, and ischemic heart disease and is on medications. On Physical examination, gait was myelopathy gait. Rest Systemic examination was unremarkable. He had weak right side handgrip and finger abduction and adduction, the rest of the upper limb and lower limb motor power was 5/5, And sensations over C5,C6 dermatomes were reduced on the right side. Bilateral biceps, triceps, brachioradialis, knee, and ankle reflexes were Brisk and plantars were extensor with Bilateral Hoffmann sign positive. Pre-operative imaging was obtained and imaging of the chest demonstrated no evidence of phrenic nerve dysfunction prior to surgery. Imaging and presentation were most consistent with severe cervical stenosis with associated myelopathy. Results: The patient developed respiratory distress post-operatively and was found to have an elevated hemidiaphragm secondary to phrenic nerve palsy. He was treated with respiratory support, with significant improvement in dyspnea. Conclusions: It is a very rare case of unilateral diaphragmatic paralysis causing dyspnea due to phrenic nerve palsy following cervical spine surgery. This rare complication should be kept in mind when assessing any patient with respiratory distress following cervical spine surgery.
1505
P163: Inter- and intra- rater reliability of magnetic resonance imaging findings assessing degenerative changes in the cervical spine
Dipak Shrestha 1 , Elisabet Danielsen 2 , Subindra Karki 3 , Sumarga Simkhada 3 , Bikash Parajuli 1 , Tore Soldberg 4,5 , Margreth Grotle 6,7 , Øystein Nygaard 8,9
1 Dept. of Orthopaedics
3 Dept. of Radiodiagnosis, Dhulikhel Hospital, Kathmandu University Hospital, Dhulikhel, Nepal
2 Department of Clinical Medicine, UiT The Arctic University of Norway, Tromsø, Norway
4 University of North Norway, Tromsø, Norway
5 The Norwegian Registry for Spine Surgery (NORspine), Norway
6 Centre for Intelligent Musculoskeletal Health, Faculty of Health Science, Oslo Metropolitan University, Oslo, Norway
7 Communication Unit for Musculoskeletal Disorders (FORMI), Oslo University Hospital, Oslo, Norway
8 Dept. of Neuromedicine and Movement Sciences, Norwegian University of Science and Technology, Trondheim, Norway
9 National Advisory Unit on Spinal Surgery, St. Olavs Hospital, Trondheim, Norway
Introduction: Few studies have assessed the reliability of Magnetic Resonance Imaging (MRI) findings of degenerative changes in the cervical spine, which is crucial to ensure diagnostic accuracy. The present study aims to determine the intra- and inter-rater reliability of cervical degeneration seen on MRI. Material and Methods: Standardised MRI examinations of the cervical segments C2/3 to C7/Th1 were conducted as part of a cross-sectional, case-control study of presumably healthy professional porters and age matched white-collar workers. Two experienced radiologists independently assessed the following ten parameters: Pfirrmann grade, anterior osteophytes, posterior disc-osteophyte complex, neural foraminal stenosis, uncovertebral arthrosis, Schmorl’s node, Modic changes, spinal canal stenosis, scoliosis, and kyphosis. The same parameters were reassessed with a one-week interval. The Gwet’s agreement coefficient (AC1) was used to assess reliability. Results: Of the 126 individuals evaluated, 50 porters and 50 white-collar workers were included. The intra-rater reliability, for both radiologists (rater I and rater II) had almost perfect agreement (AC1 range: 0.82 - 0.98), except for Pfirrmann (AC1 0.75 and AC1 0.63 (both substantial)), disc-osteophyte complex (substantial AC1 0.61 and almost perfect AC1 0.86) and spinal canal stenosis (substantial AC1 0.69 and almost perfect AC1 0.89). The inter-rater reliability had substantial or almost perfect agreement for all findings (AC1 range 0.68 - 1.00), apart from spinal canal stenosis (AC1 0.50), which had moderate agreement. Conclusion: The intra- and inter-rater reliability of the MRI findings assessing degenerative changes in the cervical spine was acceptable.
1526
P164: Validating a new assessment tool for degenerative cervical myelopathy
David Anderson 1 , Maggie li 1 , Yukai Wang 2 , Bocheng Zhu 2 , Alvaro Yanez 3 , Benjamin bd375@cam.ac.uk 4
1 Faculty of Medicine and Health, The University of Sydney, Australia
2 University of Technology Sydney, Australia
3 The University of Manchester, United Kingdom
4 Cambridge University, United Kingdom
Introduction: Degenerative Cervical Myelopathy is a progressive neurological condition that can result in debilitating physical impairments if left untreated. It is the leading cause of spinal cord injury. Due to a lack of awareness amongst clinicians, DCM diagnosis can often be delayed of missed. Detecting DCM earlier could lead to significantly improved outcomes for people with DCM. Methods: In this study, healthy controls and people with DCM were assessed with two new assessment tools. One a gait assessment tool that detects abnormalities in walking by an AI algorithm. The second a phone application that assess each of upper limb coordination, coordination and walking. Criterion validity and construct validity were calculated. Results: The gait assessment tool possessed both adequate criterion and construct validity compared with optitrack (i.e., biomechanical lab assessment) and the MJOA and Nurick grade questionnaire. Components of the phone application had adequate construct validity compared with the MJOA and Nurick grade questionnaire. Conclusions: Both new assessment tools can be deployed by clinicians to assess and monitor progression of people with DCM. The gait assessment tool specifically may have diagnostic capacity for early DCM, but will be assessed in a larger follow-up diagnostic accuracy study.
1530
P165: The utility and clinical relevance of the disc- endplate- bone marrow classification in cervical spine
Shanmuganathan Rajasekaran 1 , Jagadish T 1 , Sri Vijay Anand KS 2 , Pushpa BT 2 , Chandhan Murugan 1 , Ajoy P Shetty 1 , Rishi Kanna 1
1 Department of Spine Surgery
2 Department of Radiodiagnosis, Ganga Hospital, Coimbatore, India
Introduction: The ‘Disc-Endplate-Bone-marrow complex’ (DEBC) forms a single anatomical and functional interdependent unit and isolated degeneration of any one structure is rare. The existing Modic classification has its limitations. Recently a newer comprehensive classification, DEBC classification has been proposed for the lumbar spine1. However, its relevance and utility in the cervical spine is unknown. This study aims to assess the utility and application of recently evolved DEBC classification in the Cervical spine. Materials and Methods: The study includes two groups. Patients with isolated brain, thoracic, or lumbar spine injury with no history of neck pain who underwent whole spine MRI formed the control group (n = 200) while patients presented to OPD with complaints of neck pain who underwent MRI formed the cases (n = 301). Demographic data and radiological parameters from MRI of the Cervical spine in both groups were assessed and radiological parameters like prevalence and types of Modic changes (MC), End-Plate (EP) erosion, and presence of herniation (H+) were documented. With the addition of STIR in both groups, the categorization was revised using the DEBC classification, and clinical outcomes were associated. Results: 2400 EPs of 200 controls and 3612 EPs of 301 patients with neck pain were assessed. The incidence of MC in the control group was 12%, while it was 20.93% in the neck pain group. Of the controls with DEBC changes, the distribution was Type A-10.29%, Type B-29.41%, Type C-54.41%, and Type D - 5.88%, while in the neck pain group, the distribution was Type A-6.51%; Type B-19.53%; Type C-72.78%; Type D - 1.18%. 37 EPs required reclassification from MC 2 to DEBC 2 due to undetected edema in STIR (n = 33) or disc hyper-intensity (n=4). The co-occurrence of H+ with DEBC in controls and cases was 5.5% vs 13.95%. Among patients with neck pain number of patients who underwent surgery in pure H+ without DEBC was 10/127 (7.87%), only DEBC without H+ 1/21 (0.37%), and surgery in patients with both H+ and DEBC were 10/42 (23.81%). The odds ratio for the need for surgery was highest (OR: 3.9) when H+ and DEBC change co-occurred. Conclusion: Our study proves that DEBC classification can effectively be used in Cervical MC. Classification based on the classic MC was found to need a reclassification in 37 EPs showing the fallacy of results of previous studies. The presence of both H+ and DEBC changes significantly increases the chances of surgery.
References
1. The 'Disc-Endplate-Bone-Marrow Complex' classification - A progress in our understanding of the Modic vertebral endplate changes and its clinical relevance.’- The Spine Journal. Published: September 08, 2023. DOI:https://doi.org/10.1016/j.spinee.2023.09.002
1551
P166: The clinical significance of distal screw radiolucency in posterior cervical fusion
Audrey Chang 1,2 , James Whaley 2,3 , Christopher Como 2,3 , Jonathan Dalton 2,3 , Yunting Tang 2,3 , Andrew Croft 2,4 , Stephen Canton 2,3 , Anthony Oyekan 2,3 , Kevin Black 2,3 , Jeremy D. Shaw 2,3 , Joon Y. Lee 2,3
1 University of Pittsburgh School of Medicine, Pittsburgh, USA
2 Department of Orthopaedic Surgery, Pittsburgh Orthopaedic Spine Research (POSR) Group, Pittsburgh, USA
3 Department of Orthopaedic Surgery, UPMC, Pittsburgh, USA
4 Department of Orthopaedic Surgery, Vanderbilt University, Nashville, USA
Introduction: Radiolucency surrounding spinal instrumentation is a common radiographic finding concerning for lack of osseointegration after spinal fusion.1 However, there is a paucity of definitive evidence to support which patients with screw radiolucency would benefit from revision surgery versus observation.2-5 Although posterior cervical decompression and fusion is a common treatment for cervical myelopathy, no studies have evaluated the clinical significance of isolated postoperative screw radiolucency at the lower instrumented vertebra (LIV).6 The purpose of this study is to (1) determine the incidence of LIV screw radiolucency after posterior cervical decompression and fusion, and (2) investigate the difference in reoperation rate for hardware failure/pseudoarthrosis of patients with versus those without LIV screw radiolucency. Materials and Methods: This is a retrospective review of patients who underwent posterior cervical decompression and fusion at one of two academic centers from August 2012 to August 2019. Inclusion criteria included age ≥ 18 years old and history of posterior cervical laminectomy and fusion for cervical myelopathy due to trauma or degenerative indications. Exclusion criteria were patients undergoing spinal surgery for tumor, infection, or revision procedures, and any radiographic findings concerning for hardware failure/pseudoarthrosis other than isolated LIV screw radiolucency. LIV screw radiolucency was defined as radiologist-reported CT or x-ray radiolucent zone adjacent to screw ≥ 1 mm. Radiolucency was evaluated at 90 days, and at one year postoperatively, and at the most recent follow-up imaging available. Rate and reason for reoperation were compared between the two groups using Fisher’s exact test. Significance was defined as p < 0.05. Results: There were 235 patients identified who met inclusion/exclusion criteria. Of these patients, 5/235 (2.1%) and 8/235 (3.4%) were identified as having LIV screw radiolucency within 90 days and one year of the index operation, respectively. At the most recent follow-up imaging available (average follow-up: 772.2 days), 13/235 (5.5%) of patients were identified as having LIV screw radiolucency. The overall rate of reoperation was 3.8%. Patients with LIV screw radiolucency underwent revision surgery for hardware failure/pseudoarthrosis at a similar rate as those patients without LIV screw radiolucency (1/3 (33.3%) versus 2/9 (22.2%); p > 0.99). The most common reason overall for reoperation was adjacent segment disease. Conclusion: The incidence of LIV screw radiolucency increased over time during the post-operative course. However, this isolated radiographic finding was not associated with an increase in reoperation rate for hardware failure/pseudoarthrosis. Further study is needed to investigate if these trends continue over time, as well as the possible impact of LIV screw radiolucency on patient reported outcomes.
References
1. Marie-Hardy L, Pascal-Moussellard H, Barnaba A, Bonaccorsi R, Scemama C. Screw Loosening in Posterior Spine Fusion: Prevalence and Risk Factors. Global Spine J. 2020 Aug;10(5):598-602. doi: 10.1177/2192568219864341. Epub 2019 Jul 25. PMID: 32677565; PMCID: PMC7359691.
2. Goldstein, Ira & Singh, Rahul & Agarwal, Nitin. (2017). Resolution of screw radiolucency following instrumentation with a hybrid rigid to dynamic stabilization system. Interdisciplinary Neurosurgery. 9. 10.1016/j.inat.2017.03.009.
3. Galbusera, F., Volkheimer, D., Reitmaier, S., Berger-Roscher, N., Kienle, A., & Wilke, H. J. (2015). Pedicle screw loosening: a clinically relevant complication?. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 24(5), 1005–1016. https://doi.org/10.1007/s00586-015-3768-6
4. Sandén, B., Olerud, C., Petrén-Mallmin, M., Johansson, C., & Larsson, S. (2004). The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. The Journal of bone and joint surgery. British volume, 86(3), 457–461. https://doi.org/10.1302/0301-620x.86b3.14323
5. Kanematsu, R., Hanakita, J., Takahashi, T., Minami, M., Inoue, T., & Honda, F. (2021). Risk Factor Analysis of Facet Fusion Following Cervical Lateral Mass Screw Fixation with a Minimum 1-Year Follow-up: Assessment of Maximal Insertional Screw Torque and Incidence of Loosening. Neurologia medico-chirurgica, 61(1), 40–46. https://doi.org/10.2176/nmc.oa.2020-0206
6. Couch, B. K., Patel, S. S., Talentino, S. E., Buldo-Licciardi, M., Evashwick-Rogler, T. W., Oyekan, A. A., Gannon, E. J., Shaw, J. D., Donaldson, W. F., & Lee, J. Y. (2022). To Cross the Cervicothoracic Junction? Terminating Posterior Cervical Fusion Constructs Proximal to the Cervicothoracic Junction Does Not Impart Increased Risk of Reoperation in Patients With Cervical Spondylotic Myelopathy. Global spine journal, 21925682221083926. Advance online publication. https://doi.org/10.1177/21925682221083926
1554
167: Comparison of rigid and non-rigid interbody fusion device for cervical degenerative disc disease in adults - A randomized, prospective, multicenter clinical trial
Yun Heng Li 1 , Fon-Yih Tsuang 2
1 National Taiwan University College of Medicine, Taipei City, Taiwan
2 National Taiwan University Hospital, Taipei City, Taiwan
Introduction: The anterior cervical discectomy and fusion (ACDF) with interbody spacer has been the gold standard to treat cervical degenerative disc disease. General interbody cage was made of titanium alloy, such as Ti-6Al-4V, or polyetheretherketone (PEEK) has been demonstrated high biocompatibility and good mechanical strengths. Ti-6Al-4V is often used as spine cage that is attributed to excellent biocompatibility, enough mechanical properties, corrosion resistance and low specific gravity. But the mismatch of elastic modulus between Ti-6Al-4V implant (110 GPa) and the surrounding compact bone (8-30 GPa) may cause bone resorption and unstable fusion result. Those interbody cages are made in bulk configuration, which causes excess stiffness. To reduce stress shielding effect and the structure stiffness of Ti-6Al-4V interbody cages, the non-rigid, or dynamic design with micro-flexibility or micro-movement has been introduced. The relative study was only focused on finite element analysis, and it lacks of evidence of in vitro bone fusion condition. It is assumed that reduction of the cage stiffness or preservation of micro-movement might alleviate the post-fusion stiffness. Material and Methods: This study is a randomized, prospective, multicenter clinical trial comparing rigid (PEEK) interbody fusion device with non-rigid (Titanium Alloy, Z-Brace, Baui Biotech) interbody fusion device in ACDF surgery at 13 clinical sites. ACDF was performed with stand-alone interbody fusion device and artificial bone graft (hydroxyapatite/tricalcium phosphate). Patients have 1-level or 2-level cervical degenerative disc disease approved for ACDF surgery by National Health Insurance. Total 180 patients will be enrolled, and 180 patients will be randomized into either experimental (non-rigid) group or the control (rigid) group in a 2:1 ratio. Patient were evaluated preoperatively, one month postoperatively, and 3, 6, 12, 18, and 24 months postoperatively. Measured outcomes included overall success, Neck Disability Index (NDI), VAS neck and arm pain, adjacent range of motion, patient satisfaction, anxiety score, SF-12 MCS/PCS, major complications, subsequent surgery rate, and subsidence and fusion rate on radiological examinations. The primary endpoint was a FDA composite definition of success comprising clinical improvement and absence of major complications and secondary surgery events. Results: Currently, there are 43 patients enrolled in the trial, with 29 in the experimental group and 14 in the control group. A total of 13 individuals completed the 2-year follow-up, 30 completed the 1-year follow-up, and 40 completed the 6-month follow-up. When comparing preoperative and postoperative neck pain, limb pain, and NDI (Neck Disability Index) scores, both groups of patients showed a declining trend. There was also a decrease in anxiety and depression symptoms after surgery. We also observed an improvement in the patients' quality of life following the surgery. Conclusion: This clinical trial is still ongoing, and a longer duration and complete data are required for imaging assessments of bone fusion and subsidence. Both groups of patients have shown overall improvement in postoperative recovery.
1596
P168: Preoperative disability influences effectiveness of mcid and pass in predicting patient improvement following cervical spine surgery
Pratyush Shahi 1 , Omri Maayan 1 , Tejas Subramanian 1 , Nishtha Singh 1 , Sumedha Singh 1 , Kasra Araghi 1 , Olivia Tuma 1 , Chad Simon 1 , Tomoyuki Asada 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Maximillian Korsun 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: There are two metrics for the interpretation of Neck Disability Index (NDI) - minimal clinically important difference (MCID) and patient acceptable symptom state (PASS). MCID is defined as the smallest change in NDI following surgery that would be clinically significant for the patient. PASS is an absolute postoperative NDI score, unlike MCID which is a change score, below which patients are expected to achieve an acceptable symptom state. It is unclear if there is a better metric between the two and which metric should be utilized when. Answering these questions will substantiate our understanding regarding the clinical interpretation of NDI as an outcome measure. The objective of this study was to compare the characteristics and predictive power of MCID and PASS when interpreting NDI following cervical spine surgery. Material and Methods: This retrospective cohort study included patients who underwent primary anterior cervical discectomy and fusion (ACDF), cervical disc replacement (CDR), or laminectomy and had ≥ 6 months of follow-up data. Global rating change (GRC) and NDI data at 6 months/1 year/2 years were analyzed. Response on GRC was used as the anchor to assess the improvement status - “Compared to preoperative, you feel 1) much better, 2) slightly better, 3) same, 4) slightly worse, or 5) much worse.” It was collapsed to a dichotomous outcome variable – a) improved (response of 1 or 2), b) not improved (response of 3,4, or 5). MCID was said to be achieved if the difference between preoperative and 1-year NDI was ≥ 10.5. PASS was said to be achieved if the 1-year NDI was ≤ 21. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of MCID and PASS in terms of predicting improvement on GRC were calculated for the overall cohort and separately for patients with minimal (NDI < 30), moderate (NDI 30 - 49), and severe (NDI ≥ 50) preoperative disability. Two groups with patients who achieved PASS but not MCID and patients who achieved MCID but not PASS were also analyzed. Results: 141 patients (206 responses) were included. PASS had significantly greater sensitivity for the overall cohort (85% vs. 73% with MCID, p = 0.02) and patients with minimal disability (96% vs. 53% with MCID, p < 0.001). Contrastingly, MCID had greater sensitivity for patients with severe disability (78% vs. 57% with PASS, p = 0.05). Sensitivity was not significantly different for PASS and MCID in patients with moderate preoperative disability (83% vs. 92%, p = 0.1). 17% of patients achieved PASS but not MCID and 9% of patients achieved MCID but not PASS, with the preoperative NDI being significantly greater in the latter group. Most of these patients still reported improvement with no significant difference between the two groups (89% vs. 72%, p = 0.13). Conclusion: PASS is a better metric for patients with minimal preoperative disability and MCID is a better metric for patients with severe preoperative disability. Both metrics are equally effective for patients with moderate preoperative disability. Adequate interpretation of NDI using PASS and MCID metrics warrants individualized application as their utility is dependent on the degree of preoperative disability.
1780
P169: Endotracheal cuff pressure reduction during anterior cervical spine surgery and it's effect on post-operative dysphagia and hoarseness - A randomized control study
Kandarpkumar Patel 1,2 , Sandip Chatterjee 1
1 Department of Neurosurgery, Park Clinic, Kolkata, India
2 Department of Spine Surgery, New Sheth P.T. Multispeciality Hospital, Surat, India
Introduction: Oropharyngeal dysphagia and hoarseness of voice are the two most common complications seen after anterior cervical spine surgery. These complications are temporary in most cases. Duration of surgery, size of the implant, duration of retraction, esophageal injury and endotracheal cuff pressure are among the factors associated with these complications. The purpose of this prospective randomized control study was to determine severity of dysphagia and hoarseness of voice seen in postoperative case of anterior cervical spine surgery and its correlation with decreased endotracheal cuff pressure. Material and Methods: This study is prospective randomized control study. Its methodology was approved by the ethics committee of the institution. From January 2022 to May 2023, 40 patients were operated on with anterior cervical spine surgery and were included in this study. After randomization 2 groups were created. In the control group, we observed intraoperative endotracheal cuff pressure changes. While in the intervention group we maintained endotracheal cuff pressure less than 50 cm of H2O. After intubation base line ETCP was set below 50 cm H2O in all patients. Post-operative evaluation of dysphagia and hoarseness was done along with its severity. For evaluation of dysphagia, functional grading (1 to 6) was used. For evaluation of hoarseness of voice, grade 0 to 3 (none, mild, moderate, or severe) will be used. Post-operative evaluation was done after 24 hours, 48 hours, 72 hours and after 6 weeks. Results: Average age was 61.9 ± 12.40 and 55.059 ± 13.18 in intervention and control group respectively (p = 0.098). Numbers of Single level surgery were 12 and 10 in intervention and control groups respectively. Whereas two level surgeries were performed 8 and 10 in intervention and control groups respectively. The mean Endotracheal cuff pressure (ETCP) was measured 45.29 ± 3.44 in intervention group and 96.959 ± 19.23 in control group, which was statistically significant (p < 0.001). In this study we found that severity of dysphagia was higher in control group compared to intervention group on each post operative day. On the first postoperative day (after 24 hours) results were 3.959 ± 0.6 and 2.99 ± 0.78 in control and intervention group respectively which was statistically very significant (p = 0.00003). after 48 hours results were 2.859 ± 0.74 and 1.79 ± 0.86 in control and intervention group respectively which was statistically very significant (p = 0.00006). After 72 hours results were 1.659 ± 0.81 and 0.559 ± 0.94 in control and intervention group respectively which was statistically very significant (p = 0.0003). After 6 weeks follow up results were 0.259 ± 0.44 and 0.059 ± 0.22 in control and intervention group respectively which was statistically insignificant (p = 0.08). Severity of hoarseness was evaluated post operatively and severity was comparatively higher in control group however the results showed no statistically significant difference in two groups. Conclusion: Maintaining ETCP below 50 cm H2O decreases the severity of dysphagia in early post operative period which improves patients diet plan and satisfaction post-surgery. However, our study also observed that ETCP monitoring does not make significant difference regarding incidence and severity of Hoarseness.
1802
P170: Feasibility assessment of an extensive multimodal diagnostic work-up in patients with degenerative cervical myelopathy
Zoé Hunin 1 , Joost Dejaegher 1 , Joke Terryn 2 , Lien Solie 1 , Kaat Desloovere 3 , Catherine Huenaert 3 , Stefan Sunaert 4 , Daan Christiaens 4 , Ronald Peeters 4
1 Neurosurgery
2 Neurology
3 Gait Lab
4 Radiology, UZLeuven, Leuven, The Netherlands
Introduction: Degenerative Cervical Myelopathy (DCM) is the leading cause of acquired spinal cord disease worldwide, with an increasing incidence due to the aging population and improved diagnosis. According to the AO Spine guidelines, patients with moderate or severe myelopathy are usually treated with surgery. For patients with mild myelopathy or patients with non-myelopathic spinal cord compression, it is less clear what the best treatment is. This is also related to the fact that the natural course of the disease cannot be predicted for an individual patient. In research, there are promising new tools to evaluate spinal cord dysfunction, both technical (e.g. advanced MRI) and clinical (e.g. structured assessment of hand function). We believe that these tools can be used to estimate reliably the rate and severity of clinical progression and hence can be used to select patients for surgery. Furthermore, they can be useful to counsel patients about the disease and expected results after surgery. These advanced assessment tools are not part of the standard diagnostic work-up, and are time consuming. The goal of this pilot study was to assess whether an extensive multimodal assessment as described above is feasible and well-tolerated in DCM patients. Material and Methods: We performed a prospective interventional pilot study involving 10 DCM patients with a surgical indication. A full assessment was done preoperatively and 3 months postoperatively. This assessment consists of a standardized clinical examination supplemented by the Grassp-Myelopathy assessment of hand function, advanced microstructural MRI scan, 3D gait analysis, and electrophysiological evaluation using Motor- and Sensory Evoked Potentials. This project was supported by the 2021 AO Spine research Startup Grant. Results: Thirteen DCM patients with a surgical indication were proposed inclusion in the study, and 10 were willing to participate. The reason not to be part of the study in the 3 patients was the extensiveness of the study protocol, with the need for patients to come to the hospital several times. Of the 10 included patients, 9 completed the pre- and postoperative evaluations. 1 patients dropped out of the study after surgery because he felt the examinations were too stressful. Another issue was that the patients didn’t felt at ease during the extensive gait analysis. Finally, the long duration of advanced MRI scan was difficult for some patients. As a result, we emphasized keeping this scan as brief and robust to motion as possible. Conclusion: This extensive multimodal diagnostic work-up in patients with DCM was overall well tolerated, without significant side effects. However, the number of study visits need to be kept as low as possible to make an extensive protocol suitable for all DCM patients. Moreover, length of MRI scan and extensiveness of gait analysis need to be kept as low as possible in this patient population. With these adaptations, the multimodal protocol can be applied to a large prospective study.
1809
P171: Can cervical sarcopenia predict pseudarthrosis and clinical outcomes after anterior cervical discectomy and fusion
Teeto Ezeonu 1 , Jeremy Heard 1 , Michael McCurdy 1 , Michael Carter 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Maria Kazantsev 1 , Ahmad Hamid 1 , Ali Farooqi 1 , Emily Berthiaume 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1
1 Orthopaedic Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: Pseudarthrosis, or nonunion, is a postoperative complication that can occur when spinal fusion surgery fails. Previous literature has demonstrated a potential for worse outcomes in patients with poor muscle quality. Nevertheless, there are no studies that have comprehensively evaluated the effect of muscle quality on the rate of pseudarthrosis in patients undergoing anterior cervical discectomy and fusion (ACDF) and the implications poor muscle quality may have on patient-reported outcomes measures (PROMs). Thus, the aims of this study are to investigate the effect of cervical paraspinal muscle mass and quality on 1) the rate of pseudarthrosis and 2) PROMs after anterior cervical discectomy and fusion surgery. Materials and Methods: Upon obtaining Institutional Review Board approval, all patients ≥ 18 years who underwent ACDF from 2016-2019 were retrospectively identified. A structured query language was conducted, and chart review was performed to collect data regarding patient characteristics and one-year PROMs. Preoperative MRIs were analyzed by two independent reviewers to evaluate sternocleidomastoid muscle (SCM) at the level of the C5-6 disc space for total mass (mm2) and Goutallier grade. Patients were evaluated using two classification methods: the presence of pseudarthrosis on 1-year x-ray and SCM muscle size. To evaluate SCM muscle size, we used an SCM ratio to account for varying body mass index (BMI). Patients were classified based on SCM/BMI size by dividing the cohort into equal thirds (Group 1, Group 2, Group 3), with Group 1 consisting of the smallest SCM/BMI ratios and Group 3 consisting of the largest SCM/BMI ratios. Pseudarthrosis was identified by reviewing 1-year postoperative dynamic radiographs. PROMs included the Neck Disability Index (NDI), Visual Analog Scale Neck and Arm (VAS Neck and VAS Arm, respectively), and the mental and physical component of the short-form 12 survey (MCS and PCS). Results: We identified 205 patients who underwent ACDF with one-year radiographic and clinical follow-up. Patients in Group 1 were more likely to be female (85.3% vs. 70.6% vs. 20.3%, p < 0.001) and have higher BMI (31.1 vs. 27.8 vs. 27.5, p = 0.002). Pseudarthrosis rates were not significantly different between SCM/BMI groups (p > 0.05). There was no difference in SCM area, SCM/BMI ratio, or Goutallier grade between patients in the union and pseudarthrosis groups (p > 0.05). Multivariate logistic regression analysis showed that a higher Goutallier grade, indicative of more severe fatty degeneration, was associated with pseudarthrosis (odds ratio (OR) = 3.66, p = 0.007). Higher total levels fused (estimate = 2.53, p = 0.005) and previous adjacent level surgery (OR = 12.52, p = 0.035) were also predictors of pseudarthrosis. Patients in Group 3 had higher levels of preoperative PCS scores (30.6 vs. 35.1 vs. 36.3, p = 0.006), however there were no other significant differences in preoperative or postoperative PROMs. Conclusion: This analysis demonstrated no association between non-union rates and cervical paraspinal muscle mass and quality after ACDF. Furthermore, our results showed that no difference exists in PROMs after surgery. These findings provide optimistic support that patients of varying levels of paraspinal muscle size and quality can expect similar union outcomes and equivalent clinical improvement after ACDF surgery.
1835
P172: Association between the severity of cervical foraminal stenosis and paraspinal muscle parameters in patients undergoing anterior cervical discectomy and fusion
Thomas Caffard 1,2 , Artine Arzani 1 , Bruno Verna 1 , Vidushi Tripathi 1 , Samuel Medina 1 , Lukas Schönnagel 1,3 , Erika Chiapparelli 1 , Soji Tani 1,4 , Gaston Camino-Willhuber 1 , David Dalton 1 , Ali Guven 1 , Krizia Amoroso 1 , Jiaqi Zhu 5 , Ek Tsoon Tan 6 , John Carrino 6 , Hassan Malik 2 , Timo Zippelius 2 , Jennifer Shue 1 , Andrew Sama 1 , Federico Girardi 1 , Frank Cammisa 1 , Alexander Hughes 1
1 Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, USA
2 Klinik Für Orthopädie, Universitätsklinikum Ulm, Ulm, Germany
3 Universitätsmedizin Berlin, Charité, Berlin, Germany
4 Showa University Hospital, Tokyo, Japan
5 Biostatistics Core, Hospital for Special Surgery, New York, USA
6 Department of Radiology and Imaging, Hospital for Special Surgery, New York, USA
Introduction: As the cervical multifidus and rotator muscles (CMR) are segmentally innervated by the posterior rami of the spinal nerves, it is hypothesized that cervical foraminal stenosis (CFS) affecting the spinal nerves could result in changes in these muscles. However, the influence of CFS on cervical paraspinal muscles is not well understood. Material and Methods: Patients with preoperative cervical MRI imaging who underwent ACDF between 2015 and 2018 were reviewed. MRIs were segmented bilaterally from C3 to C7 and percent fatty infiltration (FI) was measured. The severity of the NFS was assessed by the Kim classification. Multivariable linear regression analyses were conducted for assessing the association between NFS and FI of the CMR, adjusting for age, sex, and body mass index. Results: A total of 149 patients were included. On the right side, regression analysis demonstrated that the severity of CFS at C3/4 was significantly correlated with higher FI of the right CMR at C4 and C5, CFS at C4/5 with FI of CMR at C5, CFS at C5/6 with FI of the right CMR at C6, and CFS at C6/7 with FI of the right CMR at C7. On the left side, our results showed significant positive correlations between the severity of the CFS at C4/5 and the FI of CMR at C5, CFS at C5/6 with FI of the left MF at C6 and C7, and CFS at C6/7 with the FI of the left CMR at C7. Conclusion: Our results demonstrated level- and side-specific correlations between the FI of the CMR and severity of CFS. Given the segmental innervation of the CMR, we hypothesize that the observed increased FI could be reflective of changes due to muscle denervation from CFS.
1852
P173: Middle- and long term postoperative outcomes in patients with trauma and degenerative spine disease after dorsal cervical stabilisation- a single-center review in the period of 2011-2022
Andrej Bodrov 1 , Nikolay Mirchev 1
1 Neurosurgery, Klinikum Fulda, Fulda, Germany
Introduction: The aim of the study was to present the long-term clinical and radiological results of operations on the cervical spine due to trauma and degenerative spine. All of the 250 patients in the present study were operated with mono- and multilevel dorsal or combined 360° stabilization in our clinic in the period from 2011 to 2016 due to a degenerative cervical spinal disease and trauma. Our patients were treated with stabilization systems with pedicular- and massa lateralis screws from dorsal or additionally with cages and plates from ventral. The patients were divided in 2 groups according to age- 0-65 and > 65. Material and Methods: To evaluate the clinical outcome were also used such criteria as age, gender, height and weight, BMI, Neck Disability Index before and after the operations and in the follow- ups, ASA index, the location of the operated segments as well as the number of operated segments, duration of the operation, bleeding, type of screws, screw fixation techniques including lateral mass, pedicle, intralaminar and transfacet screws, complications. important criteria for the evaluation of the fusion process were also the rate of the postoperative complications, such as misplacement of the implanted material, fistulas on the dura, postoperative bleeding, infection etc. The fusion was analyzed in the X-ray investigations as well as CT in the period of 3, 6 months and 1 and 2years after the operation. Results: There was a significant correlation between BMI and pre- and postoperative NDI. The age of patients over 65 has correlated with pre- and postoperative pain index (VAS). A female gender has also correlated with the postoperative VAS. In the first postoperative follow-up we have found correlations between age, morbidity (ASA index), as well as duration of the operation. In addition, a correlation between female gender and postoperative NDI (higher NDI in postoperative females as in males), as well as using of bone replacement (such as chronostrips, calcibon and bone chips intraoperatively) had a positive influence on postoperative NDI. Conclusion: The outcomes after the operations due to degenerative cervical spine disease and trauma are similar to most literature data. Most important factors affecting the outcome are: age, ASA Index (Pre-existing illness), BMI and Osteoporosis, as well as initial NDI (neck disability index). In the case of osteoporotically changed bone, differences in cervical fusion behavior are found due to the poor bone quality. It is also worth mentioning that factors such as diabetes, smoking or the use of NSAIDs and / or steroids have a negative impact on the fusion rate. We have found out that such factors as age, morbidity (ASA Index), pre- or postoperative pain index (VAS) and NDI influence the postoperative outcome in middle and long-term follow up.
1869
P174: Titanium coated PEEK interbody fusion devices support successful cervical fusion outcomes with both cellular and non-cellular allografts
Jillian Mohn 1 , Madilyn Riegel 1 , Leo Spector 2 , Joseph Lee 3 , Benjamin Chen 4 , Paul Bradley Segebarth 2 , Bruce Darden 2 , Anthony Kwon 2 , Eric Laxer 2 , Alden Milam 2 , Alfred Rhyne 2 , Hallie Murray 1
1 Clinical Affairs, Tyber Medical, Bethlehem, USA
2 Orthopaedic Surgery, OrthoCarolina Research Institute, Charlotte, USA
3 Orthopaedic Surgery, Rothman Orthopaedic Institute, Harrison, USA
4 Orthopaedic Surgery, Multicare Institute of Research and Innovation, Puyallup, USA
Introduction: Spine fusion is a complex process that can be affected by multiple factors including hardware, bone grafting materials and patient characteristics. Polyetheretherketone (PEEK) interbody fusion devices with a porous titanium coating (ProTi) have been designed to support osteointegration and have been shown preclinically to support bony deposition. However, the role of different bone grafting materials in supporting fusion outcomes with ProTi interbody fusion devices has not been evaluated. Therefore, the objective of this research was to evaluate the ability of ProTi interbody fusion devices to obtain successful clinical and radiographic outcomes when used with local autograft and demineralized bone matrix (DBM) compared to use with cellular allografts. Material and Methods: Institutional Review Board approval was obtained to gather healing outcomes data on patients treated with ProTi interbody fusion devices and anterior cervical plating to treat degenerative cervical spine conditions. Patients underwent 1-level (23 patients) and 2-level (25 patients) and 3-level (6 patients) spine fusion procedures and were stratified by the type of bone grafting material used (cellular bone matrix with or without local autograft (CBM) (38 patients) or local autograft with or without DBM (simple) (16 patients)). Patients were evaluated for time to fusion, adverse events, and a subset of patients completed the Neck Disability Index (NDI) (N = 12) the Visual Analog Scale (VAS) neck pain scores (N = 25). Results: Patients treated with the ProTi interbody fusion devices demonstrated osteo-integration and bridging bone across the interbody space at final follow-up regardless of the bone graft used. All 38 patients treated with CBM fused (in an average time of 12.1 ± 7.6 months), while 15/16 patients (93.8%) treated with simple bone grafts fused (in an average time of 10.8 ± 4.0 months). One patient treated with simple bone grafts had a 3-level procedure that fused at two levels and had pseudarthrosis at 1-level. Patient demographics, including age, comorbidities, and number of levels fused, were similar between the two treatment groups. Both treatment groups demonstrated improved ODI and VAS pain following treatment; however, improvements were only statistically significant (p < 0.02) in patients treated with CBM. With regards to complications, one patient (CBM group) had dysphagia (resolved by 3.5 months), one patient had subsidence (CBM group), and two patients had adjacent segment disease and subsidence (one in each treatment group; patient in CBM group required revision surgery). Conclusion: This preliminary analysis in an on-going study was the first to evaluate the differences between simple bone grafts and CBMs used with ProTi interbody fusion devices for cervical fusion applications. While time to fusion, complications, and clinical outcomes were not noticeably different between the treatment groups, only patients in the CBM group had significant improvements in patient reported outcomes (ODI and VAS). Additional research is needed to fully evaluate the effect of different bone grafting materials on cervical fusion outcomes; however, early data suggests that ProTi interbody fusion devices can support good clinical and radiographic outcomes regardless of the bone grafting material used.
1949
P175: Hounsfield units of the vertebral body predicts hardware-related complications in anterior cervcial corpectomy and fusion (ACCF)
Lei Kuang 1 , Xiaoxiao Wang 1 , Guohua Lv 1
1 The Second Xiangya Hospital of Central South University, Changsha, China
Background: Internal fixation has a high complication rate due to poor bone quality. The overall bone mineral density(BMD) of the whole body is usually based on the T-value of lumbar spinal BMD. However, there is insufficient quantifiable measure of bone quality of other areas, particularly the cervical spine. The effect of the cervical spine bone quality on internal fixation is not thoroughly studied, especially on the novel three-dimensional printed(3DP) prosthesis in recent years. The purpose of the study is to find out the correlation between Hounsfield units (HU) of the cervical vertebral body and the incidence of hardware-related complications in ACCF using either commercial 3DP prosthesis or Titanium mesh cage(TMC), so as to find out a threshold of HU that help in the selection of prosthesis in osteoporotic patients. Methods: A retrospective study was performed on Degenerative Cervical Spondylotic Myelopathy (DCSM) patients who had undergone ACCF from January 2014 to January 2019 in a single institute. Patients were divided into the 3DP group (106 patients) and TMC group (112 patients) according to the implant type. Hounsfield units of the cross-sectional cervical vertebral body on CT image, and the total bone mineral density (BMD) T-values of L1-L4 were obtained by dual-energy X-ray absorptiometry (DXA) before surgery. Radiological data of heights of the fusion segment, non-union, subsidence and displacement were measured on lateral cervical spinal radiograph on 1 day and 3 months after operation. Logistic regression model was used to test the correlations between the C2-C7 mean HU, the lumbar spinal T-value and hardware-related complications. Results: The subsidence rate in 3DP and TMC group was 27.5% and 26.8%, respectively. There was a significant positive correlation between the C2-C7 mean HU and the lumbar T value(p < 0.05). Using Logistic regression model, after adjusting gender and operation segment, the correlation between the subsidence, screw loosening or breakage and plate migration and the C2-C7 mean HU was statistically significant (p < 0.05); After adjusting gender and operation segment, the correlation between the hardware-related complications and the lumbar spinal T-value was not statistically significant (p > 0.05). The thresholds of HUs to predict implant subsidence occurrence in 3DP group was 102.4 and the number in TMC group was 101.3 (p > 0.05). Conclusion: Patients with higher preoperative HU of cervical vertebral had lower risk of hardware-related complications after ACCF using either 3DP or TMC prosthesis.
1978
P176: Persistent symptoms following cervical surgery: could double crush syndrome be responsible?
Hania Shahzad 1 , Nazihah Bhatti 1 , Alexandra Sheldon 1 , Varun Singh 1 , Goyal Kanu 1 , Safdar Khan 1 , Frank Epitropoulos 1
1 Orthopedics, The Ohio State University, USA
Introduction: In some cases, patients with cervical radiculomyelopathy do not experience symptom improvement after surgical treatment, particularly if they initially present with distal symptoms. Consequently, these patients often seek care in hand surgery clinics, suggesting the possibility of an underlying double crush syndrome. When a patient presents with distal symptoms attributed to double crush syndrome, it is advisable to prioritize treatment for distal nerve compression, potentially averting unnecessary cervical surgery. Given the syndrome's rarity, it becomes essential to identify patients who are more prone to developing distal symptoms related to double crush syndrome, ensuring they receive appropriate care. Material and Methods: The Pearldiver database was utilized to identify patients who had undergone cervical surgeries for cervical radiculomyelopathy. These patients were categorized into three groups: GROUP 1 consisted of patients who had not undergone prior nerve release and did not require additional nerve release after their cervical surgery; GROUP 2 included patients who had not undergone prior nerve release but needed additional nerve release following their cervical surgery, suggesting a potential underlying double crush syndrome; and GROUP 3 comprised patients who had undergone nerve release both before and after their cervical surgery. The primary outcome of interest was the prevalence of double-crush syndrome, while the secondary outcomes aimed to identify predictive factors for patients exhibiting underlying symptoms suggestive of double-crush syndrome. Results: The database included a total of 195,271 patient records of individuals who had undergone cervical surgery. Among them, 191,273 were in GROUP 1, 2,777 (1.42%) in GROUP 2 and 1,221 (0.63%) in GROUP 3. Patients from all three GROUPs underwent baseline characteristic evaluations, including age, with GROUP 2 having the highest mean age (57.88 years), followed by GROUP 1 (55.96 years) and GROUP 3 (54.42 years). The Elixhauser Comorbidity Index score also displayed the highest values in GROUP 2 (5.15), followed by GROUP 1 (4.53) and GROUP 3 (3.98). At baseline, the prevalence of diabetes, rheumatoid arthritis, tobacco use, and obesity significantly differed among the three GROUPs (p-value < 0.05). Multivariate analysis, after adjusting for these factors, identified diabetes (OR 1.17 [1.07, 1.29]) and obesity (OR 1.38 [1.26, 1.52]) as significant predictors of symptoms related to an underlying double crush syndrome (GROUP 2) (p-value < 0.05). Age, gender, ECI score, physician specialty, insurance plan type, rheumatoid arthritis, hypothyroidism, alcohol use, and tobacco use were not found to be predictive factors. Conclusion: The results of this study suggest that up to 1.42% of patients experience persistent symptoms following cervical surgery due to an underlying double crush syndrome, potentially negatively impacting their quality of life. This also implies that many of these patients might have benefited more from a nerve release procedure before undergoing cervical surgery, thus avoiding overutilization of healthcare resources. Additionally, patients with comorbid conditions such as diabetes and obesity may face an elevated risk and should be evaluated with a higher concern for double crush syndrome. The study also reveals that up to 0.63% of patients, even after receiving a prior nerve release procedure, still require additional nerve release following cervical surgery.
1984
P177: Cervical radiculopathy leading to scapular dyskinesia & as a causative factor of sub-acromial impingement syndrome
Karim Siddiqui 1 , Muzaffar Buriro 1
1 Orthopedic Surgery, Ziauddin University Hospital, Karachi, Pakistan
Introduction: Shoulder discomfort is often brought on by subacromial impingement syndrome (SAIS). Subacromial bursitis, rotator cuff tendinopathy, and partial and complete tears of the rotator cuff are all contributors to its pathogenesis. Shoulder discomfort can also be a result of cervical radiculopathy provided there is no primary shoulder pathology on imaging. The imperative is to treat cervical radiculopathy to assess improvement in shoulder discomfort. Material and Methods: A retrospective analysis was conducted from July 2020 to June 2022 on patients who Orthopedic outpatient clinics at Ziauddin Hospital with shoulder pathology. A total of 156 who underwent an MRI for their shoulder pathology were included with the help of the electronic medical records. Out of the 156 patients, 108 concurrently had symptoms of shoulder pain and clinical features of cervical radiculopathy. 48 patients with main shoulder disorders were excluded from the research. Patients with clinical features of cervical radiculopathy underwent an MRI of the Cervical spine which revealed disk herniation at multiple levels leading to significant nerve root compression. The MRI shoulder revealed rotator cuff pathology with no apparent anatomic cause. Radiculopathy of the cervical spine was treated with either non-invasive therapies or surgical interventions in these individuals. Results: Subacromial impingement was shown to be statistically associated with ipsilateral nerve root compression (p = 0.04). Root compression was seen on the afflicted side in 62% of individuals. Notably, sub-acromial impingement was detected in 54% of individuals who presented with cervical radiculopathy. When treated for cervical radiculopathy, 74% percent of patients reported full relief from shoulder discomfort. Conclusion: Sub-acromial impingement was shown to be directly related to cervical radiculopathy even in the absence of underlying shoulder disease. Improving patient outcomes requires addressing the underlying source of impingement.
2093
P178: Use of piezoelectric surgery versus surgical burr in cervical spondylotic myelopathy: a comparative study of 44 patients
Ahmed Jahwari 1 , Mohamed Othman 1
1 Orthopedics, Medical City for Military and Security Services, Muscat, Oman
Introduction: Piezoelectric bone surgery is relatively a new innovative technique allowing cutting of mineralized tissue rather than soft tissue with a high frequency vibration between 25 - 35 Hz via a metallic tip. It is known in literature that it causes less trauma to soft tissue, improves healing potential, preserves neurological and vascular structures, and minimizes thermal heat. Routinely used instruments such as Kerrison rongeur, high speed burr (HSD) result in complications such as Dural tear, thermal and mechanical damage to neurovascular structures and causes intra operative and post operative complications. None of the previous literature has compared piezoelectric device with HSD in cervical spine. The aim of the study is to compare the results of laminectomies using Piezotome or HSD. Material and Methods: 42 patients who were operated on for cervical spondylotic myelopathy were included. Primary laminectomy was performed on 21 patients using Piezotome and an HSD was used in the other 21 patients. The two groups were compared regarding demographic characteristics, laminectomy duration, blood loss, intra operative dural tear, neural injury, and post operative pain. Results: The Piezotome group included 8 women and 13 men with a mean age of 63 and a mean preoperative mJOA score of 12.4 ± 2.4. The HSD group included 5 women and 16 men with a mean age of 61.2 and a mean preoperative mJOA score of 12.2 ± 2.8. The mean laminectomy time per level was 2.2 ± 0.8 min in the Piezotome group compared to 6.4 ± 2.2 per level in HSD group. The mean blood loss was 220 ml in Piezotome group and 412 in the HSD group. There was no dural tear in the Piezotome group compared to 2 in the HSD group. Pain scores were also increased in patients who underwent use of burr compared to piezoelectric surgery. Conclusion: Piezoelectric surgery shows promising results in terms of safety and precision as evidenced by our experience. Compared with the high-speed drill and Kerrison rongeur, this instrument shortens laminectomy time by a significant degree, as well as reducing blood loss and neural injury.
2139
P179: Evaluation of cervical fusion rate and stability of anterior cervical discectomy and fusion (ACDF) patients who underwent more than 2 levels of fusion without anterior cervical plating
Prasanna Gunasena 1 , Anil Weerasinghe 1 , Eranga Ganewatte 2 , Anupa Walgamage 1
1 Neurosurgery
2 Radiology, Lanka Hospital, Colombo, Sri Lanka
Objective: Primary objective of this retrospective study is to radiologically evaluate the Cervical spine fusion rates and stability of cervical spine of the patients who underwent ACDF for two or three levels using PEEK cages without the use of anterior cervical plating. Anterior decompression and fusion are one of the most common indications for patients having moderate to severe cervical myelopathy or radiculopathy not responding to non-operative treatment [1]. It is considered even a single level ACDF is associated with high fusion rates when used in conjunction with anterior plating [2,3]. However, using anterior cervical plating has its own complications and limitations when used for fusion. Post-operative long-term dysphagia can be as high as 35% [4] and recurrent laryngeal nerve injury and post-operative hematomas have also contributed to post-operative morbidity. Literature suggests better fusion rates when used anterior cervical plate for ACDF than ACDF with cage alone [5]. Methodology: Forty Patients who underwent two or three levels of anterior cervical discectomy and fusion using PEEK cages without using anterior plates were evaluated between 2013 to 2020 from a single-center, under a single consultant surgeon at Lanka Hospitals Colombo Sri Lanka. The PEEK cages were filled with locally harvested bone graft. Prospective assessment of all 41 patients were done by doing post-operative cervical spine X-rays, anterior posterior views and lateral and flexion extension views at the end of six months’ period. Fusion rates and stability at the fused segments were evaluated by a board-certified radiology specialist. There were 32 Patients with two level fusion and 09 patients with three level fusions. 100% fusion was achieved at the fused segments and no instability was found according to the X-Ray appearance. Conclusion: Two or three level ACDF surgery can be done safely to achieve a good inter vertebral body fusion without using anterior cervical plates for the patients who require anterior cervical discectomy and fusion.
References
1. Tetreault L, Goldstein CL, Arnold P, et al. Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery. 2015; 77(suppl 4): S51-S67.
2. Lebl DR, Hughes A, Cammisa FP, Jr, et al. Cervical spondylotic myelopathy: pathophysiology, clinical presentation, and treatment. HSS J. 2011;7(2):170–178. doi: 10.1007/s11420-011-9208-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
3. Emery SE, Bolesta MJ, Banks MA, et al. Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976) 1994;19(6):660–663. doi: 10.1097/00007632-199403001-00004. [PubMed].
4. Nancy E. Epstein, M.D., A Review of Complication Rates for Anterior Cervical Discectomy and Fusion (ACDF); Surg Neurol Int.2019; 10: 10.
5. Justin F Fraser 1, Roger Härtl; Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. J Neurosurg Spine 2007 Apr; 6(4): 298-303. doi: 10.3171/spi.2007.6.4.2.
2145
P180: Gain of living independence following surgical intervention for cervical spondylotic myelopathy: a quality outcomes database (QOD) study
Nitin Agarwal 1,2 , Erica Bisson 3 , Mohamad Bydon 4 , Anthony Asher 5 , Andrew Chan 6 , Michael Wang 7 , Regis Haid 8 , John Knightly 9 , Oren Gottfried 10 , Christopher Shaffrey 10 , Michael Virk 11 , Mark Shaffrey 12 , Paul Park 13 , Kevin Foley 13 , Domagoj Coric 5 , Cheerag Upadhyaya 14 , Eric Potts 15 , Luis Tumialan 16 , Kai-Ming Fu 11 , Raj Lavadi 1 , Sarah Johnson 4 , Dean Chou 6 , Praveen Mummaneni 17
1 School of Medicine
2 Medical Center, University of Pittsburgh USA
3 University of Utah, Salt Lake City, USA
4 Mayo Clinic, USA
5 Carolina Neurosurgery & Spine Associates, USA
6 Columbia University Irving Medical Center, USA
7 University of Miami, USA
8 Atlanta Brain and Spine Care, USA
9 Atlantic Neurosurgical Specialists, USA
10 Duke University, Durham, USA
11 Weill Cornell Medical Center, New York, USA
12 University of Virginia, Charlottesville, USA
13 Semmes-Murphey Clinic, USA
14 University of North Carolina, Chapel Hill, USA
15 Goodman Campbell Brain and Spine, USA
16 Barrow Neurologic Institute, USA
17 University of California, San Francisco, USA
Introduction: Chronic spinal degenerative diseases have been associated with reduced quality of life and dependency on others for personal needs and care. The change between preoperative and postoperative care dependency has yet to be explored in patients with cervical spondylotic myelopathy (CSM). Material and Methods: The CSM dataset of the Quality Outcomes Database (QOD) was queried. Care dependency was assessed using the personal care component of the Neck Disability Index (NDI) questionnaire – an ordinal scale from 0 to 5; 5 being the inability to get dressed with activity restriction. Numeric rating scale (NRS) arm pain, neck pain, and EuroQol-5D (EQ-5D) in quality-adjusted life years (QALY) scores were recorded up to 24 months postoperatively. Multivariable logistic regression analyses were performed to identify baseline risk factors for the inability to care for oneself and the symptoms leading to care dependency at 24 months postoperatively. Results: Of the 1,137 patients with CSM who underwent surgical management, 167 patients (14.7%) were care-dependent at baseline (NDI personal care score > 2). Patients with care dependency were predominantly Medicare beneficiaries, of a high school or lower level of education, and had severe myelopathy at baseline. At 24-month follow-up, 112 (81.8%) patients who were dependent before surgery became independent in the ability to take care of themselves. Patients who experienced a resolution in their care dependency at 24 months had higher EQ-5D scores (p < 0.01). Lower extremity dysfunction, bladder dysfunction, upper extremity dysfunction, and neck pain were significantly associated with care dependency at 24 months follow-up (p < 0.01). Conclusion: Fifteen percent of patients with CSM depend on others for care preoperatively. After surgery to treat CSM, 81.8% of patients who depended on others for care, became independent. Patients with improvements in care dependency note higher postoperative satisfaction at 3-month and 24-month follow-up. Surgery has a significant impact on patients achieving independence.
2168
P181: Surgery for cervical myelopathy with congenital vertebral synostosis in craniovertebral junction and upper cervical spine
Hiroshi Kageyama 1 , Yukoh Ohara 2
1 Neurosurgery/ Spinal Surgery, Shin-Kuki General Hospital, Kuki, Japan
2 Neurosurgery, Juntendo University, Tokyo, Japan
Introduction: The purpose of this study is to examine the surgical treatment of cervical myelopathy associated with congenital vertebral synostosis in the craniovertebral junction and upper cervical spine. Material and Methods: We conducted a retrospective chart review of operative cases related to spinal diseases over the past five years. From this pool, we identified patients who had received a diagnosis of cervical myelopathy associated with congenital synostosis in the craniovertebral junction and upper cervical spine. Results: We conducted a review of 666 operative spinal cases, among which we encountered five cases. The mean age was 74.8 years, consisting of one male and four females. Three of the five cases had C1 assimilation and four had C2/3 fused vertebrae. Three of the five cases with C2/3 fused vertebrae showed atlanto-axial subluxation or basilar invagination. Two of these three cases were associated with C1 assimilation, and the other had hypoplasia of posterior arch like spina bifida. In addition, one of the combined cases of with C1 assimilation and C2/3 fused vertebrae had a foramen magnum decompression 50 years ago and showed extensive suboccipital bone loss. All five case showed instability and myelopathy in the adjacent segment of the fused vertebrae. Three-dimensional computed tomography angiography (3D-CTA) showed that all four cases of C2/3 fused vertebrae had anomalous vertebral artery (VA). Three of the four cases had unilateral VA hypoplasia, and the VA on the dominant side showed high riding type. One case had bilateral high riding VAs. Surgical treatment consisted of occipito-cervical fusion with endoscopic odontoidectomy (retropharyngeal approach) in two cases, posterior atlanto-axial fixation with endoscopic odontoidectomy in one case, occipito-cervical fusion with posterior decompression in 1 case, and posterior fixation with decompression between C3/4 vertebrae in 1 case. In one case of occipito-cervical fusion, a transarticular screw was used because placement of an occipital plate was impossible after the aforementioned foramen magnum decompression. Intraoperative navigation system was used for all fixation cases, and adequate bone grafting was performed using autologous iliac bone or allograft (Grafton™). In one case of occipito-cervical fusion, laminoplasty was performed simultaneously in the subaxial cervical spine. Conclusion: We encountered five operative cases of cervical myelopathy associated with congenital vertebral synostosis in the craniovertebral junction and upper cervical spine. The patients with C2/3 fused vertebrae often have high riding VAs, and the choice of screw for fixation should be carefully considered.
2230
P182: Degenerative cervical myelopathy: what information is required to make an informed management decision
Andrew Gamble 1,2 , David Anderson 1 , Benjamin Davies 3 , James Van Gelder 4 , Sophie Macpherson 5 , Marnee McKay 1 , Joshua Zadro 2
1 Faculty of Medicine and Health
2 Institute of Musculoskeletal Health, The University of Sydney, Australia
3 Cambridge University, United Kingdom
4 Sydney Spine Institute, Australia
5 The University of Sydney, Australia
Introduction: Degenerative Cervical Myelopathy (DCM) is the leading cause of spinal cord injury. It remains under diagnosed due to a lack of awareness amongst clinicians and the community. Decision aids offer patients and clinicians an opportunity to navigate current evidence for management and treatment options available to them. Methods: Using mixed methods, we developed and user tested an evidence-based patient decision aid for people with DCM who are considering surgery. Participants were people who have DCM or health professionals who manage these patients. Participants were recruited through social media (e.g., international charity group Myelopathy.org) and large public hospitals in Sydney, Australia. Semi-structured interviews and questionnaires were used to gather feedback on the decision aid. The feedback was used to refine the decision aid and assess acceptability. An iterative cycle of interviews, refining according to feedback and further interviews was used. Interviews were analysed using reflexive thematic analysis. Questionnaire data were analysed descriptively. Results: We conducted 40 interviews; 20 were with people with DCM and 20 with health professionals who manage DCM (Neurosurgeons, Physiotherapists). Most participants rated the decision aid acceptability as good or excellent. People with DCM and health professionals mostly agreed on the different aspects of the decision aid: introduction, treatment options, comparing benefits and harms, design, and questions to consider asking health professionals. However, some health professionals had differing views on the use of the modified Japanese Orthopaedic Associate (mJOA) scale to determine the appropriate management of people with DCM. Conclusion: Our patient decision aid is an acceptable tool to assist people with DCM to make appropriate management choices with health professionals. A randomised controlled trial evaluating the potential benefits of this decision aid is still needed.
2273
P183: Are there differences in outcome after posterior cervical foraminotomy performed for cervical radiculopathy caused by soft disc and hard disc
Inhee Kim 1 , Dong-Ho Lee 2 , Yong Min Kim 1 , Jae Hwan Cho 2 , Sehan Park 2 , Hyung Rae Lee 3 , Seung Hyun Baek 4 , Geon Jung Kim 1
1 Department of Orthopedic Surgery, National Police Hospital, Seoul, South Korea
2 Department of Orthopedic Surgery, Seoul Asan Medical Center, Seoul, South Korea
3 Department of Orthopedic Surgery, Uijeongbu Eulji Medical Center, Gyeonggi-do, South Korea
4 Department of Orthopedic Surgery, Daejeon Eulji Medical Center, Daejeon, South Korea
Introduction: PCF is a minimally invasive, motion-preserving surgery widely applied in the treatment of cervical radiculopathy. Several studies have compared it to anterior cervical laminectomy; however, there are few reports on whether outcomes after PCF differ depending on the underlying pathology. we hypothesized that because patients with radiculopathy caused by HD tend to have more spondylotic change of cervical spine than radiculopathy patients caused by SD, clinical outcome would be worse. This study was conducted to compare the clinical and radiologic outcomes of posterior cervical foraminotomy (PCF) in cervical radiculopathy due to SD and HD. Material and Methods: 53 patients who underwent PCF for the treatment of cervical radiculopathy and were followed-up for more than 2 years were retrospectively reviewed. Patient characteristics, cervical lordosis, C2-C7 sagittal vertical axis (SVA), T1 slope, and patient reported outcome measures such as neck pain visual analog scale (VAS), arm pain VAS, and neck disability index (NDI) were retrospectively reviewed. Results were compared between the SD group and the HD group. Results: 17 patients (32.1%) underwent PCF due to SD and were included in the SD group, and 36 patients (67.9%) who had operation due to HD were included in the HD group. There were no significant difference in patient characteristics, cervical lordosis, C2-C7 SVA, and T1 slope between the two groups. Neck pain VAS, arm pain VAS, and NDI significantly improved after the operation in both groups. Patient reported outcome measures at each follow-up time point did not demonstrate significant difference. the amount of improvement of NDI did not demonstrate significant difference. Conclusion: Despite the narrower baseline disc space and smaller neuroforaminal size in the HD group, PCF demonstrated good clinical outcomes in both groups. Thus, PCF is a procedure that can be recommended for patients with cervical radiculopathy without concern for preoperative pathology.
2276
P184: Posterior floating laminotomy versus wide laminectomy in posterior cervical decompression
Harkeerat Singh Sukhdarshan Singh 1 , Naveen Vijayasingham 2 , Jayamalar Thurairajasingam 3
1 Orthopedics, Hospital Sultan Ismail, Johor Baharu, Malaysia
2 Orthopedics, Hospital Tawau, Tawau, Malaysia
3 Hospital Sultan Ismail, Johor Baharu, Malaysia
Introduction: Posterior cervical decompression is a common procedure to treat multilevel degenerative cervical spine disease. Types of posterior decompression surgery range from fromaniotomy, laminoplasty, wide laminectomies. We would like to share our experience with floating laminoplasty first described by Dr. Yoshiharu Kawaguchi and his colleagues from Japan in the early 2000s.This technique which creates two throughs over the lamina-lateral mass with a high speed burr bilaterally, followed by flavectomy via the trough with a size 1 Kerrison rongeurs. The detached fragment is elevated en-bloc and secured to the cranial and caudal spinous processes via ethibond sutures to maintain the segment in situ. Decompression is augmented with bone grafting over the gutters to allow for “trough fusion”. Material and Methods: Patients underwent posterior decompression surgery at our centre from 1st July 2022 - 31st June 2023 were retrospectively included in this study. Pathologies included ranged from degenerative cervical disc disease, ossified posterior longitudinal ligament, and central cord syndrome Infective and metastatic pathologies were excluded from this study. A total of 21 patients were identified and data regarding demographics of the patients, type of surgery, number of levels decompressed, surgical time, and intra-operative blood loss were collected. Results: Demographic data showed patients were aged 26 - 72 years old, male to female ratio was 1.7:1, the most commonly performed surgery was wide laminectomy and fusion 10 patients (48%), followed by floating lamiotomy 8 patients (38%), and laminoplasty 3 patients (14%). Number of levels decompressed ranged from 2 to 5 levels, surgical time ranged from 168 minutes - 270 minutes. Intra-operative blood loss ranged from 350 mls - 900 mls. Statistical analysis was conducted among groups based on the type of surgery performed looking into intra-operative blood loss and surgical time, however no significant results were obtained. Limitations of this study include the small sample size and retrospective nature of the study construct. Being a new surgical procedure, experience and volume will definitely improve surgical times and intra-operative blood loss. Conclusion: Floating laminoplasty is a new addition to the armamentarium in posterior cervical decompression techniques. Although there was no statistical significance between intra-operative blood loss, and operative time between the floating laminoplasty and wide laminectomy group, floating laminoplasty has been described to combine the benefits of a laminoplasty and posterior cervical fusion, preventing progressive kyphosis, less axial neck pain while reducing the incidence of pseudomembrane formation and 3rd space hematoma collection seen in wide laminectomies.
2375
P185: Surgical management for degenerative cervical myelopathy anterior approach
Md Rezaul Karim 1
1 Spine Surgery Unit, National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Study Design: This prospective study involves 36 patients with degenerative cervical myelopathy who were surgically treated by anterior corpectomy, interbody fusion by titanium mesh cage (TMC) filled with autogenous bone, and stabilized by anterior cervical plate. Objectives: This study was conducted to determine the indications, efficacy, and complication rate associated with performing corpectomy to achieve anterior decompression of neural elements or for removing anterior lesions. Methods: Twenty-six patients with degenerative cervical myelopathy who had surgical treatment and average 30 months (range, 24–52 months) follow up were included. The mean age was 64.9 years (range, 55–74 years) and average period between myelopathic symptoms and surgery was 2.8 years (range,6months–5years). Preoperative evaluation of every patient consisted of anterior–posterior, lateral, bilateral oblique, flexion, and extension radiographs, computed tomography reconstructions and magnetic resonance imaging of the cervical spine, Degree of pre and postoperative myelopathy was determined according to the scoring systems developed by Nurick and Japanese Orthopedic Association (JOA). Eight patients had a mild balance problem and difficulty while walking but were able to perform their daily activities. Two patients had spastic quadriparesis ambulating on either crutches or with the help of others. Surgical treatment in all patients consisted of anterior decompressive corpectomy, and multilevel discectomy anterior plate stabilization in all patients. Results: Mean sagittal Cobb angle (C2-C7) was 9° (range, 0-23°) before surgery, 17.1° (range, 11-22°) on the third postoperative month, and 16.9° (range, 10-22°) at last follow-up. The difference in sagittal alignment on the third month and last follow up was not statistically significant. Average preoperative Nurick score was 3.5 (range, 2-5) and JOA score was 7 (range, 1-14). Major and statistically significant neurologic recovery was within the first 3 months, and average Nurick and JOA scores at 3 months were 2 (range, 0-3) and 8 (range, 8-17) respectively. All patients had improved neurologic status at final follow up. As confirmed by plain radiographs and some time computed tomography reconstructions, solid fusion was achieved and we had no implant related complication or failure. No major complications, 1patient (3.8%) postoperative CSF leaking developed improved spontaneously. At final follow up, all patients were able to ambulate without support and maintain their daily activities. Conclusions: Anterior decompression provides good neurologic recovery in patients with degenerative cervical myelopathy. Tricorticcal bone graft from iliac crest or titanium cage impregnated with cancellous bone provides good structural support, and solid fusion can be achieved with and anterior cervical plate.
2449
P186: The impact of cervical laminoplasty and cervical foraminotomy on axial neck pain: a systematic review and meta-analysis
Andrew Kim 1 , John Avendano 1 , Marc Greenberg 1 , RIchard Skolasky 1 , Mihir Gupta 2 , Sang Hun Lee 1
1 Department of Orthopaedic Surgery, The Johns Hopkins Hospital, Baltimore, USA
2 Department of Neurological Surgery, Yale University, New Haven, USA
Introduction: Significant axial neck pain is considered a risk factor of unfavorable outcomes or relative contraindication to non-fusion, posterior cervical decompressive surgery including cervical laminoplasty (CL) or cervical foraminotomy (CF) for degenerative cervical myelopathy and/or radiculopathy. However, consensus regarding persistence, aggravation or resolution of neck pain postoperatively remains controversial. The purpose of this study was to analyze patient-reported outcomes focused on axial neck pain following cervical laminoplasty and foraminotomy to determine if the non-fusion procedures provide relief of axial neck pain as well as compressive radiculopathy/myelopathy and their effect on clinical outcomes using systematic analysis. Material and Methods: The PubMed (NLM) and Cochrane Library (Wiley) databases were systematically searched in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines under keywords including ‘cervical laminoplasty’ and ‘posterior cervical (lamino)foramintomy’. The search included articles published from 2013 to 2023 and were independently evaluated by two reviewers. Data regarding patient-reported outcomes (PROs), including Numerical Rating Scale (NRS), Visual Analogue Scale (VAS), Nurick Scale, Japanese Orthopaedic Association (JOA) Scores, Neck Disability Index (NDI), EQ-5D, the 36-Item Short Form Health Survey (SF-36), risk factors of unfavorable outcomes and reoperation rates, were collected when available for each article. For each PRO, weighted means and standard deviations were calculated and compared using unpaired t-tests with significance level set at 0.05. Results: A total of 37 studies were selected for analysis, including 29 focusing on CL and 8 on CF. There were a total of 3,009 cases (2,396 CL and 613 CF) with a mean age of 63.57 ± 5.16 and 53.35 ± 15.23 years for CL and CF patients respectively. For studies with specified follow-up durations, median follow-up was 17.9 months for CL and 24.0 months for CF patients. Among CL patients, 64.86% (1,554/2,396) were males and 35.14% (842/2,396) were females. Among CF patients, 63.46% (389/613) were males and 36.54% (224/613) were females. From the studies analyzed, patients undergoing CL had improved mean postoperative VAS (2.35 ± 0.87) and NDI (17.08 ± 8.00) scores compared to their baseline values of 4.41 ± 1.34 (t(2378) = 44.4793, p < 0.0001) and 28.64 ± 8.90 (t(2636) = 35.0827, p < 0.0001). Patients undergoing CF had improved mean VAS (2.83 ± 1.11 vs. 4.84 ± 1.99) (t(1150) = 21.1705, p < 0.0001) and NDI (13.67 ± 4.48 vs. 26.31 ± 14.01) (t(954) = 18.7881, p < 0.0001) postoperative scores in relation to preoperative values. Presence of anterolisthesis, regional malalignment, higher axial neck pain intensity, current smoking status, diabetes, age, and radiographic Pfirrmann grade were all found to be independent predictors of postoperative axial neck pain. Conclusion: Non-fusion posterior cervical decompressive surgery including laminoplasty and foraminotomy provide significant relief of axial neck pain as well as radiculopathy/myelopathy symptoms with significantly improved postoperative patient-reported outcomes unanimously. These findings suggest that axial neck pain may not be a contraindication to non-fusion decompressive surgery for degenerative cervical radiculopathy/myelopathy. Preoperative risk factors predisposing unfavorable outcomes from axial neck pain following cervical laminoplasty/foraminotomy should be considered when determining surgical strategy.
2545
P187: Considering the effects of patient age and race when selecting implants or choosing to revise anterior discectomy and fusion: a retrospective cohort study
Jeffrey Weinreb 1 , Tyler Pease 1 , Ryan Smith 1 , Joseph Blommer 1 , Amit Ratanpal 1 , Anthony Chiu 1 , Idris Amin 1 , Julio Jauregui 1 , Louis Bivona 1 , Daniel Cavanaugh 1 , Eugene Koh 1 , Charles Sansur 1 , Steven Ludwig 1
1 Department of Orthopaedics, Division of Spine Surgery, University of Maryland School of Medicine, Baltimore, USA
Introduction: Anterior cervical discectomy and fusion (ACDF) is a mainstay of treatment for degenerative cervical pathology. However, revisions remain common, particularly in multilevel fusions. Common precipitants for revision include persistent symptoms, adjacent segment degeneration (ASD), pseudarthrosis, and infection. Demographic factors, such as age and race, may play a role. However, the literature is lacking on the interaction of these factors with the type of implant material used. The aim of this study is to assess the interaction of patient age, race, and spacer material with revision rates. We hypothesize that elderly patients, underrepresented minorities, and synthetic material use may place a greater risk of revision. Material and Methods: We conducted a retrospective chart review of 261 patients undergoing ACDF for degenerative pathology from 2012 to 2022. Inclusion criteria consisted of: 1) adult patients > 18 years old, 2) neck pain and radiculopathy lasting > 6 months, 3) ACDF at operative levels C3-4, C4-5, C5-6, C6-7, 4) radiographic follow-up in the immediate post-operative period, and 5) ≥ 6 months of clinical and radiographic follow-up. Exclusion criteria consisted of: 1) operative level at C7-T1, 2) indication of trauma, infection, or malignancy, and 3) history of prior cervical surgery. We collected demographic, surgical, and outcome data from the medical record and assessed radiographic outcomes. Statistical analysis included descriptive statistics, normality tests, Fisher’s Exact Test, Pearson’s Chi-Squared Test, and mixed effects linear models. Results: A total of 261 patients received ACDF, with 472 fused levels. The most common spacer material was structural allograft (83.1%), followed by titanium (14.6%) and PEEK (2.3%). Overall, 15.3% of patients received revision surgery within a mean follow-up period of 37.95 months. Of all revisions, the mean time to revision was 30.8 months. The majority of patients demonstrated fusion by six months (72.3%). The causes of revision were ASD (25 cases), pseudarthrosis (15 cases), and persistent symptoms (9 cases). Black patients had lower early radiographic fusion rates than white patients (53.4% vs 81.3%, p < 0.001), and higher radiographic pseudarthrosis rates (26.2% vs 8.2%, p = 0.013) at six months follow-up. Regression analysis found that black patients had higher rates of revision than white patients (β = 0.124, 95% CI [0.066 - 0.181], p < 0.001). When adjusted for race, BMI, and sex, it was found that titanium cages were associated with reduced subsidence at each level over time when compared to allograft (β = -0.168, 95% CI [-0.245 – -0.091], p = 0.029). PEEK implants were associated with greater rates of revision (β = 0.264, 95% CI [0.066 – 0.462], p = 0.009). Age was non-predictive of all-cause revision. Conclusion: This study reviewed outcomes of ACDF according to age, race, and choice of spacer material. It was found that PEEK implants were associated with greater revision rates, while age was not associated with any significant differences in outcomes. Regarding race, surgeons should remain aware that differences in rates of fusion and pseudarthrosis in black patients may be temporary. Thus, consider careful monitoring of these patients to avoid unnecessary revisions.
2596
P188: How I do it? UBE posterior spinous process sparing bilateral cervical laminectomy for sublaminar osteochondroma
Rohit Kavishkar 1
1 Department of Orthopaedics, Clinical Fellow in Spine Surgery, Ng Teng Fong General Hospital, Singapore, Singapore
Background: Cervical osteochondroma are rare cause of myelopathy. Traditional treatment is open laminectomy with or without fusion. There is limited literature on unilateral biportal endoscopic en-bloc resection of cervical osteochondroma. Methods: UBE en-bloc resection of extra-dural sublaminar osteochondroma on ventral surface of C4 lamina for patient who had cervical myeloradiculopathy. Osteotomy was performed to conserve the spinous process and supraspinous ligament. Complete laminectomy of C4 was performed. This preserves posterior ligamentous complex of the neck. Conclusion: UBE can effectively decompress spine by removing extra-dural compressions in experienced hands.
Keywords: Spine endoscopy, UBEendoscopic, ⋅ laminectomy, ⋅ osteochondroma
Degenerative lumbar
103
P189: The association between pelvic retroversion capacity and paralumbar muscle health in patients with lumbar degenerative conditions
Joshua Mathew 1 , Bongseok Jung 2 , Jonathan Elysee 1 , Basel Sheikh Alshabab 1 , Priya Duvvuri 2 , John Fallon 2 , Austen Katz 2 , Junho Song 2 , Adam Strigenz 2 , Luke Zappia 2 , Renaud Lafage 1 , Virginie Lafage 1 , Sohrab Virk 2
1 Orthopedic Surgery, Lenox Hill Hosptial, New York, USA
2 Orthopedic Surgery, North Shore University Hospital-Long Island Jewish Medical Center, Zucker School of Medicine at Hofstra University, New Hyde Park, USA
Introduction: With the increased prevalence of lumbar degenerative conditions, the association between posterior lumbar muscle and spinal alignment must be evaluated and whether or not they contribute to maintaining alignment. Therefore, the purpose of this study is to evaluate the association between lumbar sagittal alignment and posterior muscle characteristics. Materials and Methods: A retrospective single center review of lumbar degenerative patients with degenerative conditions and lumbar MRIs available. After assembling the cohort, associations were drawn between cohort demographics and muscle health parameters using bivariate correlations, t-tests, or chi-squared as appropriate. Following demographics analysis, associations between pelvic retroversion (PT) and spino-pelvic mismatch (PI-LL) with muscle health data were investigated. The associations were further stratified by sex, while controlling for age and PI using partial correlations. Results: The cohort consisted of 280 patients (Mean age: 57 ± 15 yo, BMI 29.2 ± 5.7, 62.1% Female). Sagittal alignment for the entire groups was: PI: 56.4 ± 11°, PT: 17.9 ± 9°, LL: 54.8 ± 14°, PI_LL: 1.61 ± 12.77°. Muscle LI ranged from 12.4 ± 7 at L1-2 to 15.5 ± 7 at L4-5, CSA/BMI from 150.2 ± 46 to 138.7 ± 44, and G grade ≥ 2 from 22.3% to 52.5%. Demographic analysis revealed significant associations between age and CSA/BMI (r = -0.3 to -0.39), and G (all p < 0.001), but no significant association regarding LI (all p > 0.1). LI was significantly different between the sexes at every level, except at L3-4 (p = 0.15) (all other p < 0.05). PI correlated significantly with LI (r = 0.28 to 0.18 all p < 0.01) but not CSA/BMI. Patients with G ≥2 at L1-2 (p = 0.022) and L4-5 (p = 0.029) had a significantly smaller PI. After stratifying by sex, no significant association was found between PI-LL and CSA/BMI while controlling for age and PI. There was a weak negative association between LI and PI-LL in Males (r = -0.20 to -0.28) and moderate negative association at L4-L5 for Females (L3-4: r = -0.17 and L4-5: r = -0.40). PI-LL was not significantly associated with G in either sex. PT was negatively associated with LI while controlling for PI and age for both sexes. There was no significant association between PT and CSA/BMI for Males (all p > 0.05). However, there was a significant negative association between PT and CSA/BMI at L4-L5 for females (L4-5 r = -0.24 and -031 respectively). G was negatively associated with PT except at L3-4 in both Males and Females. Conclusion: When investigating the association between pelvic retroversion and the muscle health measurements, while controlling for age and pelvic incidence, pelvic retroversion was significantly associated with muscle health outcomes. These findings suggest that the ability to retrovert the pelvis to compensate for spino-pelvic mismatch may be related to muscle health, especially at the distal lumbar spine. Understanding the association of muscle health and pelvic tilt may be of value when assessing post operative outcomes for surgical interventions aimed at correcting lordosis in patients with high spino-pelvic mismatch.
118
P190: 30- and 90-day readmissions i lumbar spine surgery. Differences in prevalence and causes
Anna Duc 1 , Stian Solumsmoen 1 , Tanvir Bari 1 , Rachid Bech-Azeddine 1
1 Copenhagen University Hospital, Copenhagen Spine Research Unit, Glostrup, Denmark
Introduction: The morbidity associated with surgical treatment of lumbar degenerative conditions has attracted increasing interest due to the economic impact on society, especially postoperative readmission. Limited studies have assessed this risk in a prospective, single-center consecutive fashion. To assess the incidence and causes of 30- and 90-day unplanned readmission and revision surgery following surgical treatment for lumbar degenerative spine conditions at a tertiary treatment center. Material and Methods: All patients undergoing degenerative lumbar spine surgery in a 1-year period from February 1st, 2016, were prospectively included. Patient characteristics, surgical information and information regarding postoperative complications, including readmission (30- and 90-days) and revision surgery were recorded. Readmissions were classified according to whether they were due to the surgical intervention specifically, or a medical complication. Results: A total of 1,399 patients underwent surgery for various lumbar degenerative pathologies in the study period and all were included. Of these, 9.4% (n = 132) were readmitted within 30 days of surgery and in some cases, multiple readmissions occurred (up to 3). The total 90-day readmission rate was 17.6%. Of these, 15% were related to the surgical procedure. The predominant medical related causes were systemic infection (30-day: 14.4%, 90-day: 10.7%), neurological symptoms (30-day: 6.3%, 90-day: 5.0%) and cardiovascular events (30-day: 8.1%, 90-day: 12.9%). The surgical related causes for readmission were pain (30-day: 13.1%, 90-day: 2.9%), wound complications (30-day: 11.3%, 90-day: 5.0% and re-herniation (30-day: 13.1%, 90-day: 2.9%). Age was the only factor with significant influence on readmission. Conclusion: The incidence of medical conditions causing unplanned 30-day readmissions following surgery for lumbar degenerative conditions, is significantly higher compared to readmissions related specifically to the surgical procedure. Examples of medical treatment included antibiotics, analgesics, laxatives, anticoagulants and beta blockers. The difference is even more pronounced for the 90-day readmissions. The predominant medical causes were systemic infections, neurological and cardiovascular events. Predominant causes related to the surgery were pain, wound complications and re-herniations. Readmissions may be reduced by optimizing the medical treatment and the pain management before discharge of the patient.
127
P191: Associations between low virulence organisms in different locations and intervertebral disc degeneration and Modic change in lumbar spine
Xiaolong Chen 1 , Shibao Lu 1
1 Department of Orthopedic Surgery, Xuanwu Hospital Capital Medical University, Beijing, China
Introduction: Many factors may trigger the presence of inflammation and chemical factor for intervertebral disc degeneration (IDD) process, microbiome dysbiosis has recently been implicated as one of the likely causes. However, the exact relationships between microbiome dysbiosis and IDD and endplate changes are not well understood. The aim of this meta-analysis is to investigate the impact of microbiome dysbiosis in different location and sample sources and to assess the potential relationships between microbiome dysbiosis and IDD and endplate changes. Material and methods: We searched four online databases for potential studies. The potential relationships between microbiome dysbiosis in different sample sources (e.g., skin, intervertebral disc, muscle, and serum) from lumbar and/or cervical spine and IDD and endplate changes were considered as primary outcomes. Odds ratio (OR) and their 95% confidence intervals (CI) were evaluated. GRADE approach was used to summarize the strength of evidence. Results: Thirty observational studies met the eligibility criteria. Overall pooled prevalence of infection in 3414 patients with spinal pain was 32.5% (23.9%-41.7%), including 33.2% (23.6%-43.6) in lumbar spine and 27.8% (17.1%-39.9%) cervical spine. The pooled prevalence of infection in 3923 samples was 27.8% (20.5%-35.8%). Proportion of disc infections was higher in patients with endplate changes than in patients without (OR = 2.02; 95% CI = 1.20–3.40; I 2 = 51.5%; p = 0.016), especially the measurement in lumbar spine (OR = 2.56; 95% CI = 1.47-4.46; I 2 = 37.6%; p = 0.108). The majority of infections were due to Propionibacterium acnes in 22.2% (13.3%-32.5%) and 13.2% (7.5%-20.2%) in lumbar and cervical spine, respectively. Conclusions: The results of this study found low-quality grade evidence for an association between disc infection with endplate changes, especially in lumbar spine. Due to the heterogeneity and methodological limitations, further studies will improve understanding the potential relationships and mechanisms.
Keywords: Microbiome dysbiosis, disc degeneration, endplate change, systematic review, meta-analysis.
141
P192: Clinical efficacy and complication rates of decompression with or without fusion for degenerative lumbar spondylolisthesis: a systematic review and meta-analysis
Xiaolong Chen 1 , Dongfan Wang 1 , Shibao Lu 1 , Ashish Diwan 2
1 Department of Orthopedics Surgery, Xuanwu Hospital Capital Medical University, Beijing, China
2 Spine Service, St. George Hospital Campus, UNSW, Sydney, Australia
Introduction: Currently, there is a lack of information on direct comparisons of clinical efficacy and complication rates between decompression alone and decompression with fusion for degenerative lumbar spondylolisthesis (DLS). Therefore, we compared the clinical efficacy and complication rates of decompression with or without fusion in the management of patients with DLS. Material and Methods: Relevant studies were identified from EMBASE, MEDLINE, Web of Science, and Cochrane Central Register of Controlled Trials. The inclusion criteria were 1) Randomized controlled trials (RCT) and observational studies, 2) Studies which reported the comparisons between decompression alone and decompression with fusion for DLS, and 3) Reported outcomes included clinical outcomes, complications, reoperations, operating time, or blood loss. The exclusion criteria included 1) Reviews, case series, case reports, letters, and conference reports, 2) In vitro biomechanical studies and computational modelling studies, and 3) No report on study outcomes. The RoB2 tool and the Newcastle-Ottawa scale was conducted to assess the risk of bias of RCTs and observational studies, respectively. Results: Five RCTs and nine observational studies met the eligibility criteria. Compared with decompression with fusion, there was moderate-quality evidence from RCTs suggesting that decompression alone was associated with lower postoperative back pain (SMD -0.21, 95% CI -0.4 to -0.03), and very low-quality evidence from observational studies suggesting that decompression alone led to higher leg pain (SMD 0.17, 95% CI 0.05 to 0.3) and ODI (MD 5.16, 95% CI 1.85 to 8.47). Moderate-quality evidence from RCTs indicating that decompression alone contribute to lower overall complication rates (RR 0.56, 95% CI 0.41 to 0.77), lower intraoperative complication rates (RR 0.53, 95% CI 0.30 to 0.94), lower postoperative complication rates (RR 0.59, 95% CI 0.38 to 0.90), and lower modified Clavien-Dindo classification (MCDC) Type II complication rates (RR 0.46, 95% CI 0.31 to 0.68) versus decompression with fusion. In addition, decompression alone was related to shorter operating time (MD -93.95, 95% CI -125.32 to -62.58) and less intraoperative loss (MD -320.62, 95% CI -389.66 to -251.57) based on low-quality evidence from RCTs. Conclusion: Results of this meta-analysis suggest that for the surgical treatment of DLS, the major strength of decompression alone over decompression with fusion was lower overall complication rates, lower intraoperative complication rates, lower postoperative complication rates, and lower Type II complication rates per MCDC.
197
P193: Which NASS herniation morphology descriptors are most associated with PROM improvement after microdiscectomy
Teeto Ezeonu 1 , Jeremy Heard 1 , Michael Carter 1 , Omar Tarawneh 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Meera Kohli 1 , Alec Kellish 1 , Tyler Henry 1 , Caleb Yeung 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1 , Ian Kaye 1
1 Rothman Orthopaedic Institute, Philadelphia, USA
Objectives: Lumbar disc herniation is a common etiology of low back pain. The North American Spine Society (NASS) nomenclature system was developed to provide a common language for surgeons to consistently and accurately characterize herniations. It has not yet been demonstrated how the classification system can be used to predict patient-reported outcomes. Therefore, the objectives of this study were (1) to determine which NASS descriptors are most predictive of patient-reported outcome measures (PROMs) after microdiscectomy and (2) to identify the inter-rater reliability of each NASS descriptor. Materials and Methods: All patients > 18 years who underwent lumbar microdiscectomy from 2014-2021 at a single academic institution were retrospectively identified. PROMs included the Oswestry Disability Index (ODI), Visual Analog Scale Back and Leg (VAS Back and VAS Leg, respectively), and the mental and physical component of the short-form 12 survey (MCS and PCS). Each herniation was classified using the NASS lumbar disc nomenclature specific to disc herniation. Characteristics for classification included (1) area of axial disc, (2) area of central canal, (3) percent central canal displacement, (4) focal vs. broad-based displacement, (5) protrusion vs. extrusion, (6) sequestered vs. non-sequestered, (7) laterality, (8) migration, (9) extent of migration, and (10) presence of Schmorl node. Backwards multivariate logistic regressions were used to analyze the predictability of each disc characteristic on improvement in three-month and twelve-month PROMs. Cohen’s kappa coefficient was used to measure the inter-rater reliability of each NASS descriptor. Results: A total of 213 patients (41.8% female) were identified. The disc herniation characteristics with greatest inter-rater reliability were area of central canal (k = 0.88) and sequestration status (k = 0.88), while area of migration (k = 0.53) and extrusion (k = 0.61) had the least inter-rater reliability. Multivariable logistic regressions demonstrated that at 3 months, non-sequestered herniation (OR = 0.11, p = 0.004) and larger axial disc areas (OR = 1.03, p = 0.003) predicted improvement in ODI. By 12 months, only non-sequestered herniation was predictive of improvement in ODI (OR = 0.07, p = 0.001). Improvement in MCS at 3 months was also predicted by non-sequestered herniation (OR = 0.25, p = 0.032) and larger axial disc areas. (O = 1.02, p = 0.009), though this prediction did not persist at 12 months. At 3 months, improvement in PCS could be predicted by protruded herniation (OR = 0.37, p = 0.035). Improvement in VAS leg could be predicted at 12 months by larger axial disc area (p = 1.05, p = 0.031), smaller central canal area (OR = 0.98, p = 0.042) and herniation protrusion (OR = 0.4, p = 0.034). Herniation descriptors that did not predict improvement in any PROM included focal vs. broad protrusion, presence of a Schmorl node, and zone of herniation. Conclusion: These results show that sequestration status based on MRI imaging is both reliable and able to predict improvement in clinical outcomes at 3 months and at 12 months after surgery. Extrusion was not a reliable herniation descriptor, however it was associated with improvement in multiple clinical outcomes. As this study is the first to evaluate this nomenclature system, additional investigation is needed to support our findings on the reliability and utility of the NASS system to predict outcomes.
285
P194: Platelet rich plasma vs corticotherapy for lumbar pain of facetary origin: a randomized clinical trial
William Zarza Santos 1 , Robert Meves 1
1 Ortopedia e Traumatologia, Santa Casa de Sao Paulo, Sao Paulo, Brazil
Introduction: Low back pain is one of the most common health problems, with high prevalence and social cost. Up to 20% of cases of acute low back pain do not resolve within 12 weeks, becoming chronic. In view of the increasing cost, incidence and prevalence of people with chronic low back pain, better treatment options have become a major point of discussion. It is precisely at this point that biological therapies appear as a promising alternative. The objective of this study is to compare PRP to the injection of corticosteroids in patients with chronic low back pain of facet joint origin. Methods: Randomized clinical trial with patients with chronic low back pain of facet joint origin, previously selected with positive dorsomedial branch block test, comparing the effect of PRP versus corticosteroids on facet joint injection. Epidemiological data as well as clinical outcomes were assessed using quality of life questionnaires (SF36), function (ODI and RM), in addition to the visual analogue scale (VAS) pain. Patients were evaluated before the procedure, after 1 month and after 3 months. Results: A total of 59 patients were included in the randomization between groups: 32 patients in the corticosteroid group and 27 patients in the PRP group. There was no difference regarding gender, age, BMI and comorbidities between the two groups, showing homogeneity between them. In the ODI assessment, although there was no difference between PRP and corticosteroids at any time, there was a significant interaction effect between treatment and time (p = 0.038), showing that the groups behaved differently over time. The same effect was evidenced in the RM evaluation (p = 0.010). As for the VAS, there was no significant difference between the treatments in the evaluated times, as well as in the quality of life questionnaire (SF36). Conclusion: The present study showed similar results in up to 3 months of PRP compared to corticosteroids in the assessment of pain, quality of life and function scores in the treatment of lumbar facet syndrome, and it was not possible to see differences between the methods in this sample.
292
P195: Clinico-radiological assessment of lumbar spinal canal stenosis and evaluation of its surgical treatment
Sarvdeep Dhatt 1
1 Orthopaedics, PGIMER, Chandigarh, India
Introduction: This study aimed to predict the absolute criteria for surgical intervention and study the outcome of surgical intervention. Materials and Methods: A prospective study was conducted from June 2002 to July 2003. A total of 35 patients were included in the study. Pre- and postoperative Oswestry Disability Index (ODI) scores were evaluated for all the patients. All patients underwent magnetic resonance imaging (MRI). The surgical indications were disabling backache with radicular pain, limited walking capacity, and neurological deficits leading to a poor ODI score. Surgical procedures done were discectomy and laminectomy with or without fixation with pedicle screws on a case-to-case basis. Follow-up was done for up to 1 year at three-monthly intervals. The final ODI score was taken at the last follow-up and was compared with preoperative scores. Results: A 50 ± 10 years was the average age of patients included in the study. The average walking capacity was 40 m; the average duration of symptoms was 41 months. ODI improved from average score of 71% ± 4% preoperatively to 22% ± 6% postoperatively. L4-L5 was the level most severely narrowed, with a mean cross-sectional area of 75 mm2. The most common surgical interventions done were discectomy and laminectomy, which were performed in 54% of the cases. We had good-to-excellent results in all our cases. None of the cases deteriorated after surgery. Conclusion: The findings in this study have important implications in clinical practice. The radiological findings in the MRI correlated well with the clinical signs and symptoms of the patients, i.e., patients with significant findings in the MRI had profound clinical symptoms and neurological deficits. Lumbar canal stenosis is a clinicoradiological diagnosis. ODI score is related to canal narrowing on MRI. Clinical improvement is related to preoperative disability and canal narrowing on MRI.
Keywords: lumbar canal stenosis, magnetic resonance imaging, Oswestry Disability Index
338
P196: Prevalence of neck and back pain among orthopedic surgeons in Tunisia
Adnene Benammou 1,2 , Meriem Souissi 1,2 , Ahmed Ben Abid 1,2 , Seddik Akremi 1,2 , Mondher Kooli 1,2 , Mehdi Bellil 1,2 , Mohamed Ben Salah 1,2
1 University Tunis el Manar, Faculty of Medecine of Tunis, Tunis, Tunisia
2 Orthopedic Surgery Department, Charles Nicolle Hospital, Tunis, Tunisia
Introduction: Orthopedic surgery is a physically demanding job, making orthopedic surgeons vulnerable to musculoskeletal pathologies. We aim to evaluate the prevalence of back and neck pain in orthopedic surgeons. Material and Methods: A survey was addressed through email to 89 actively-practicing orthopedic surgeons. We collected demographic, and clinical data as well as impact of pain on professional and personal daily activity. Results: 56.8% of participants reported back pain 1 to 3 times a week and 55% say it started during internship.75.5% of participants said the pain was mild. Neck pain was present at least once a week in 30% of participants and was considered light. Medical treatment was received by 7 surgeons and one took days off because of the pain. No surgeon has managed the OR but 2 had to adapt their type of surgical practice. Conclusion: Orthopedic surgery exposes to high risks of chronic musculoskeletal pathologies Future studies may lead to evaluate the relationship between the type of surgical practice and the pain, as well as the means to prevent it.
343
P197: Development of end-to-end artificial intelligence models for surgical planning in transforaminal lumbar interbody fusion
Anh Tuan Bui 1 , Meng-Huang Wu 2,3,4
1 Taipei Medical University, International Ph.D. Program in Medicine, Taipei, Taiwan
2 Department of Orthopedics, Taipei Medical University Hospital, Taipei, Taiwan
3 Department of Orthopaedics, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
4 Prospective Innovation Center, Taipei Medical University Hospital, Taipei, Taiwan
Introduction: Transforaminal lumbar interbody fusion (TLIF) is a commonly used technique for treating lumbar degenerative diseases. Here, we developed a fully computer-supported pipeline to predict the cage height and the degree of lumbar lordosis subtraction from the pelvic incidence (PI-LL) after TLIF surgery through preoperative X-ray images. Material and Methods: A total of 311 patients who underwent L4-L5 TLIF surgery were included. The automated pipeline included two primary stages. First, a deep learning model was used to extract essential features from X-ray images, and these features were then combined with clinical features to develop machine learning (ML). Model precision was evaluated by comparing magnetic resonance imaging measurements with model predictions. Second, five ML algorithms were trained to identify the optimal models to predict the interbody cage height and postoperative PI-LL. Subsequently, a subset of major features from each baseline model was selected, and the most critical features were examined in further analysis. Results: A total of 53 features were extracted from preoperative X-ray images by using a deep learning model. These features were determined to be highly reliable, as indicated by the adequate to excellent interobserver reliability within an intraclass correlation coefficient range of 0.78-0.947. Lasso regression exhibited superior performance for predicting the interbody cage height, and support vector regression had optimal results for predicting postoperative PI-LL. For cage height prediction, the root mean square error (RMSE) was calculated as 1.01, and the model achieved the highest accuracy at a height of 12 mm, with exact prediction achieved in 54.43% (43/79) of cases. In most of the remaining cases, the prediction error of the model was within 1 mm. In addition, the model demonstrated adequate performance for predicting PI-LL, with an RMSE of 5.19 and an accuracy of 0.81 for PI-LL stratification. For interbody cage height prediction, the intervertebral height at the midpoint of L4-L5 emerged as the pivotal factor, while preoperative lumbar lordosis (LL), relative LL, and pelvic incidence (PI) emerged as pivotal for predicting postoperative PI-LL. Conclusion: The interbody cage height and postoperative PI-LL can be reliably predicted using artificial intelligence and ML models, indicating their potential for use in clinical decision-making.
363
P198: Surgical management of hip-spine syndrome: a systematic review of the literature
Raj Lavadi 1 , Sharath Anand 2 , Lauren Culver 3 , Hansen Deng 2 , Alp Ozpinar 4 , Lauren Puccio 2 , Nitin Agarwal 1,2 , Nima Alan 5
1 Neurological Surgery, University of Pittsburgh School of Medicine, Pittsburgh, USA
2 Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, USA
3 Neurosurgery, Houston Methodist, Houston, USA
4 Oregon Neurosurgery, Springfield, USA
5 Neurological Surgery, University of California, San Francisco, USA
Introduction: Hip-spine syndrome was first described in 1983 to describe the symptomatology resulting from concomitant lumbar degenerative stenosis and hip osteoarthritis. Numerous studies have sought to understand the underlying pathology and appropriate management of this syndrome. The purpose of this article is to review the literature for specific imaging characteristics and the optimal surgical treatment of hip-spine syndrome. Material and Methods: We conducted a systematic review via an electronic database search through PubMed to identify all publications related to hip-spine syndrome. All publications that contained data on patients who underwent surgical treatment for hip-spine syndrome and reported patient outcomes or radiographic data were included. Exclusion criteria consisted of publications published in a language other than English, review articles, and technique articles. Results: We identified fifteen articles that focused on the surgical management of hip-spine syndrome. Of these 15 articles, eight reported radiographic outcomes with most reporting no significant change in spinopelvic parameters before and after surgery. Thirteen articles reported clinical outcomes with eight of those thirteen articles identifying patient reported outcomes to be significantly improved following surgery. Conclusion: Despite being first described almost forty years ago, the data on surgical management of hip-spine syndrome remains sparse. While there is some evidence that total hip arthroplasty in patients who previously underwent spinal fusion may have higher complications rates, there remains debate regarding which surgical problem to address first – the hip or the spine.
380
P199: Assessment of theoretical knowledge about degenerative sacroiliac joint disease among orthopedic surgeons in Tunisia
Adnene Benammou 1,2 , Cherif Kamoun 1,2 , Amal Abayed 1,2 , Ahmed Ben Abid 1,2 , Mondher Kooli 1,2 , Mehdi Bellil 1,2 , Mohamed Ben Salah 1,2
1 University Tunis el Manar, Faculty of Medecine of Tunis, Tunis, Tunisia
2 Orthopedic Surgery Department, Charles Nicolle Hospital, Tunis, Tunisia
Introduction: Sacroiliac (SI) is one of the main causes of chronic low back pain due to its rich presence of sensory nerves. Clinical and radiological diagnosis is often unrecognized among orthopedic surgeons which leads to unexplained persistent low back pain, unsatisfied patients and crowded doctor’s practice. Our purpose is to assess the theoretical knowledge of degenerative sacroiliac joint disease among this population in Tunisia. Material and Methods: We conducted our study over the period of a year utilizing a 12-question survey that collected the status of surgeons, years of practice, daily practice of spine surgery. We asked the participants about their current knowledge on the innervation of the sacroiliac joint, incidence of pain related to SI joint, provocative tests and criteria, surgical treatment and its indications. Results: 26 orthopedic surgeons participated in this study as following: resident (65.4%), teaching doctor (15.4%), specialist (15.4%) et associate professor (3.8%). Years of practice varied from 0 to 5 years in 57.7% of cases and from 5 to 10 years in 38.5%. 3.8% of surgeons had a daily practice of spine surgery whereas 46.2% never practiced spine surgery. 57% of our participants disregard that sacroiliac disease is responsible for 15-30% of low back pain. 4.3% of surgeons think that lumbar fusion was followed by early pain postoperatively, due to mechanical overload of the SI joint according to 56.5% of surgeons, to greater mobility of SI in 21.7% and that incidence of pain increased with the number of fusion levels in 13% of participants. Participants responded « I don’t know » to the questions regarding SI innervation in 34.6% and provocative tests in 34.9% of cases. 34.6% know that the positivity to three provocative tests predicts a good response to SI corticosteroid injection. More 60% of participants think that fluoroscopy-guided injection is ideal and permits pain healing. 61.5% indicated sacroiliac fixation for persistent low back pain in patients operated on with lumbar fusion. Sacroiliac screw fixation is the main technique according to the participants. Conclusion: Degenerative sacroiliac joint disease is often underdiagnosed by mostly young orthopedic surgeons. To the best of our knowledge, no previous study has been conducted in such perspective. Further studies regarding the optimal tools to improve their knowledge such as workshops, master classes etc., should be considered.
437
P200: Is concomitant lumbar spinal stenosis and diabetes associated with a reduced improvement in patient-reported outcomes after spine surgery? A propensity-matched registry-based cohort study
Peter Udby 1 , Søren Ohrt-Nissen 2 , Leah Carreon 3
1 Spine Unit, Zealand University Hospital, Køge, Denmark
2 Spine Unit, Rigshospitalet, Copenhagen Ø, Denmark
3 Spine Unit, Spine Center of Southern Denmark, Lillebaelt Hospital, Middelfart, Denmark, Middelfart, Denmark
Introduction: Low back pain is associated with increased mortality, obesity, depression, and risk of opioid overuse. In elderly patients, lumbar spinal stenosis (LSS), combined with an already increased risk of comorbidity, disability, and reduced physical activity, can have a severe impact on quality of life and overall frailty. Diabetes (DM) is associated with increased mortality, obesity, reduced physical activity, cardiovascular disease, and cancer. Previous studies on the association and impact of concomitant LSS and DM are limited. The aim of this study is to evaluate the impact of DM in patients with LSS undergoing spine surgery. Material and Methods: Patients from the Danish national spine registry, DaneSpine, scheduled for LSS surgery were identified. MRI of patients with and without DM was graded in regards to LSS, disc degeneration (DD), muscular fat infiltration, and Modic changes. In addition, preoperative and two-year postoperative data were collected including PROs. Patients with DM were propensity-matched to non-DM patients. Results: In total, 296 patients were included, 41 DM and 255 non-DM. Of these, 27 patients from each group were successfully matched. The PSM DM group had less improvement and worse leg pain at two-year follow-up compared to the non-DM group, VAS 58 vs. 36 (p = 0.004). Physical disability was significantly worse at two-year follow-up in the DM group compared to the non-DM group, Oswestry Disability Index score of 38 vs. 29 (p = 0.05). On the preoperative MRI, the number of patients with severe grade LSS and severe fat infiltration in Multifidus muscles was significantly higher in the PSM DM group compared to the non-DM group, (p < 0.01). Conclusion: Patients with concomitant LSS and DM have a significantly reduced improvement in leg pain, more physical disability, and worse leg pain scores at two-year follow-up post-surgery compared to patients without DM. In elderly patients with LSS, there should be an increased focus on DM and the clinically relevant threshold for spine surgery.
465
P201: Validity of Oswestry Disability Index (ODI) in elderly patients with co-existing Hip/Knee pathology
Sumit Batra 1 , Sovik Yadav 1
1 Orthopaedic Surgery, Marengo Asia Hospital, Faridabad, India
Introduction: Oswestry Disability Index is considered the gold standard of low back functional outcome tools. Almost all the factors measured are affected by spinal disorders as well as hip or knee pathology. Majority of elderly patients presenting with low back pain also have co-existent hip or knee arthritis/other pathology adding to leg pain and disability. Hence it is proposed that ODI score may not be a valid scoring system for assessment of success of treatment of spinal pathology in elderly patients with hip/knee pathology. Methods: 58 patients aged 50 years and above were included in the study. 29 patients (cases group) presenting with low back pain with associated Hip/Knee pathology were compared with 29 patients (control group) without any hip/knee pathology. ODI scores were recorded at first presentation and at 2nd, 6th and 12th week follow up visits. The changes in the ODI scores were compared against pain intensity (measured by VAS score) at each visit. Results: Significant positive correlation was seen between VAS scores and ODI scores at all visits in both the groups. The correlations were plotted on the graphs. As pain intensity (VAS) improved, there was improvement in functional disability (ODI score). However, the strength of correlation of VAS score with ODI score was found to be weaker in group A (cases) as compared to group B (control). However, the difference was statistically significant only at 2nd week (p-value 0.023). Conclusion: ODI score appears to be a useful tool for assessment of functional disability in elderly patients suffering from Low Back Pain with co-existing hip/knee pathology. However, changes in ODI scores with successful treatment of spinal pathology may not be very significant in this subgroup of patients.
527
P202: Kinetic analysis of structural parameters in degenerative lumbar spondylolisthesis
Andy Ton 1 , Nicole Hang 1 , Marc Abdou 1 , Christopher Lee 1 , Raymond Hah 1 , Jeffrey Wang 1 , R. Kiran Alluri 1
1 Orthopaedic Department, Keck School of Medicine of USC, Los Angeles, USA
Introduction: Kinetic magnetic resonance imaging (kMRI) is a novel technique which combines high image resolution with positional variability offered with conventional radiographs to allow characterization of degenerative changes in dynamic pathologies such as degenerative lumbar spondylolisthesis (DLS). This study evaluates the relationship between structural parameters of the lumbar spine and instability in DLS using kMRI. Material and Methods: This was a retrospective review of 129 consecutive lumbar spine kMRI images from patients presenting with low back pain from 2015-2017. Patients with history of prior fusion or presenting for trauma, malignancy, or infection were excluded. Segmental lordosis, facet angle, disc height and degeneration, and paraspinal muscle cross-sectional area (CSA) were measured on neutral T2-weighted images. Spondylolisthesis was categorized as stable or unstable at each lumbar segment from L3-S1. Instability was defined as translational motion > 3mm and/or angular motion > 10 degrees between flexion and extension images. Statistical analysis included independent t-test and chi-squared for continuous and categorical variables. Multivariable logistic regression controlling for age sex, and global lordosis were conducted to identify independent predictors of instability at individual lumbar segments. Results: Overall, 60 patients had single-level DLS (mean age = 44.7+12.3; 46% female), 20 of which were unstable. There were no significant differences in age (p = 0.135) or sex (p = 0.532) between stable and unstable DLS patients. On average, unstable DLS was associated with greater multifidus CSA (5.29 vs. 8.34cm2, p = 0.005). Increased multifidus CSA was significantly predictive of instability (OR:1.5, 95%CI: 1.20-1.82, p = 0.001). At L4-L5 DLS segments, increased translational motion at adjacent L5-S1 non-DLS segments was significantly predictive of instability (OR:2.2, 95%CI: 1.05-4.56, p = 0.037). Conclusion: Increased multifidus CSA was found to be an independent predictor of unstable DLS overall, while increased anteroposterior translational motion at adjacent, non-affected L5-S1 segments were predictive of unstable DLS at L4-L5 segments. As a dynamic stabilizer, multifidus hypertrophy is likely a compensatory mechanism to maintain spinal stability, while excessive translational motion at the lumbosacral joint may elicit further segmental instability at adjacent L4-L5 DLS segments where structural integrity is already compromised. Higher powered studies should be conducted to further investigate predictors of instability in DLS.
585
P203: SA - ALIF hyperlordotic cage for correction of segmental spinal lordosis in patients with single level DDD
Dimitar Haritonov 1
1 Neurosurgery and Spine Surgery, Heart and Brain Hospital Pleven, Pleven, Bulgaria
Introduction: Since the introduction of threaded devices in the mid-1990s, anterior lumbar interbody fusion (ALIF) has become a staple in the armamentarium of the spine surgeon.We aim at analysing the impact of stand alone anterior lumbar interbody fusion (SA- ALIF) with hyperlordotic cage in treatment of single level degenerative disc disease (DDD) and restoring the main spinopelvic parameters, along with its potentials and limitations in correcting sagittal imbalance of the approach and implanted hardware. Materials and Methods: Total 72 patients with single level DDD and spinal misalignment were treated surgically and followed up in Department of Neurosurgery and Spinal Surgery – University Hospital Heart and Brain Pleven for period of 2 years. The following spinopelvic parameters were observedand corrected: pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), segmental lumbar lordosis (LLseg) and sagittal vertical axis (SVA). Most of the patients (80 %) received hyperlordotic cages (HLC). The indirect decompression potential of ALIF was also assessed. The clinical outcome was obtained by collecting visual analogue scale (VAS) for back and leg pain and Oswestry Disability Index (ODI) scores. Global fusion rate and main complications were collected. Preoperative dynamic X-Ray, CT scan with venogram, bone density and MRI were performed. Postoperative CT scan on 3 and 6 month were done. Results: PT, SS, LL, LLseg and SVA spinopelvic parameters all improved postoperatively by - 4.3 ± 5.2°, 3.9 ± 4.5°, 10.6 ± 12.5°, 6.7 ± 3.5° and 51.1 ± 44.8 mm, respectively. HLC were statistically more effective in restoring LL and LLseg (p < 0.05). Postoperative disc height, anterior disc height, posterior disc height and foraminal height, respectively, increased by 58.5%, 87.2%, 80.9% and 18.1%. Postoperative improvements were observed in VAS back and leg and ODI scores (p < 0.05). The global fusion rate was 94.5 ± 5.5%; the overall complication rate was less than 5%. Conclusion: When managing degenerative disc disease and sagittal imbalance, SA-ALIF can be considered as a valid and reliable technique to achieve the correct spinopelvic parameterseven in single level surgery based on preoperative planning. This technique permits to obtain an optimal LL distribution and a solid anterior column support, with lower complications and higher fusion rates when compared to posterior approaches. Using a hyperlordotic cages is a milestone for improving the postoperative results.
664
P204: Diagnosis of depression has no effect on opioid consumption after lumbar spine fusion
Teeto Ezeonu 1 , Omar Tarawneh 1 , Olivia Opara 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Eric Teichner 1 , Lauren Micou 1 , Liam Gibbons 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1
1 Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: The prevalence of psychiatric disorders is more than 4 times higher in patients with disabling spine conditions compared to the general population. Orthopaedic procedures are associated with postoperative opioid usage, increasing the potential for opioid abuse. While evidence suggests that patients with mental health conditions are more likely to use opioids, there is limited research on the effects of mental health on opioid consumption in spine patients. Therefore, the objectives of this study were to determine the effects of preoperative diagnosis of depression on (1) postoperative opioid consumption after lumbar fusion surgery and (2) surgical outcomes. Material and Methods: Following IRB approval, patients > 18 years old who underwent 1-2 level primary lumbar spinal fusion from 2017-2021 at a single academic institution were retrospectively identified. Diagnosis of depression was confirmed using manual chart review. Outcome variables included 90-day pre- and postoperative opioid consumption in morphine milligram equivalents (MME), as well as surgical outcomes (length of stay, post-admission disposition, inpatient complications, and 90-day readmissions). Parametric data were compared with independent t-tests and non-parametric data were compared with Mann-Whitney U tests. Categorical variables were compared using Pearson's chi-square tests. Multivariable logistic regression models were developed to determine if depression was a significant independent predictor of postoperative opioid usage. Statistical significance was set at p < 0.05. Results: We identified 486 patients who underwent one- to two-level lumbar fusion surgery at a single academic institution. 105 patients (21.6%) had a diagnosis of depression. Patients with a diagnosis of depression were more likely to be female (68.6% vs. 45.9%, p < 0.001) and have a higher Elixhauser comorbidity index (2.00 [0.00;2.00] vs. 1.00 [0.00;3.00], p < 0.001). There was no difference between groups in 90-day opioid MME consumption in the pre- and postoperative periods (p > 0.05). Patients who had a diagnosis of depression had longer length of stays (3.39 [2.46;4.02], vs. 3.29 [2.58;4.22], p = 0.043) and were more likely to be discharged to inpatient rehab (12.4% vs. 5.77%, p = 0.033) or a skilled nursing facility (7.62% vs. 3.94%, p = 0.033). There was no difference in total inpatient complications or 90-day readmissions between groups (p > 0.05). A multivariate logistic regression showed that depression was not an independent predictor of 90-day postoperative opioid consumption. Higher preoperative pain level (est. = 1.81, Confidence Interval (CI): 0.69-2.93, p = 0.002) and longer length of stay (est. = 34.33, CI: 21.89-46.76, p < 0.001) were predictive of greater 90-day postoperative opioid usage. Conclusion: Patients with a diagnosis of depression did not consume more opioids than patients without depression after lumbar spinal fusion and they experienced no difference in surgical outcomes. Postoperative opioid usage was better predicted by preoperative comorbidity status and length of stay. While diagnosis of depression may have an effect on discharge outcomes, providers and patients should be reassured that post-surgical outcomes, including opioid consumption, will not be adversely impacted.
713
P205: Mini-open intercostal retroperitoneal appraoch for upper lumbar spine lateral interbody fusion
Dongwuk Son 1 , Suhun Lee 1 , Joonbum Woo 2 , Junseok Lee 1 , Geun Sung Song 1
1 Neurosurgery, Pusan National University Yangsan Hospital, Yangsan-si, South Korea
2 Neurosurgery, Inje University College of Medicine, Haeundae Paik Hospital, Busan, South Korea
Introduction: Conventional oblique lumbar interbody fusion (OLIF) approach is possible from the L2/3 to L4/5 levels. However, obstruction of the lower ribs (10th–12th) makes it difficult to maintain disc parallel maneuvers or orthogonal maneuvers. To overcome these limitations, we proposed an intercostal retroperitoneal (ICRP) approach to access the upper lumbar spine. This method does not expose the parietal pleura or require rib resection and employs a small incision. Material and Methods: We enrolled patients who underwent a lateral interbody procedure on the upper lumbar spine (L1/2/3). We compared the incidence of endplate injury between conventional OLIF and ICRP approaches. In addition, by measuring the rib line, the difference in endplate injury according to rib location and approach was analyzed. We also analyzed the previous period (2018–2021) and the year 2022, when the ICRP has been actively applied. Results: A total of 121 patients underwent lateral interbody fusion to the upper lumbar spine (OLIF approach, 99 patients; ICRP approach, 22 patients). Endplate injuries occurred in 34 of 99 (34.3%) and 2 of 22 patients (9.1%) during the conventional and ICRP approaches, respectively (p = 0.037; odds ratio, 5.23). When the rib line was located at the L2/3 disc or L3 body, the endplate injury rate was 52.6% (20 of 38) for the OLIF approach but 15.4% (2 of 13) for the ICRP approach. Since 2022, the proportion of OLIF including L1/2/3 levels has increased 2.9-fold. Conclusion: The ICRP approach is effective in reducing the incidence of endplate injury in patients with a relatively lower rib line, without pleural exposure or rib resection.
715
P206: A rare case of ligamentum flavum cyst presenting with lumbar radiculopathy and neurologic deficit
Aayush Aryal 1 , Alex Johnson 1 , Vikas Tandon 1
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
Introduction: Ligamentum flavum cyst, a rare type of extradural juxtafacetal cyst of the spine, can present with neurological symptoms due to spinal canal stenosis and lumbar nerve root compression. It is commonly associated with degenerative diseases of the spine, such as degenerative disc disease and spondylolisthesis. Ligamentum flavum cyst should be kept as a differential diagnosis in patients presenting with radiculopathy or claudication pain, where an epidural cystic lesion is seen on MRI. Surgical excision of such a lesion usually provides satisfactory pain relief in symptomatic patients. Material and Methods: We reported a case of ligamentum flavum cyst occurring at L4-L5 level on the right side in a 73-year-old lady, causing lumbar radiculopathy with a neurologic deficit in the form of weakness of great toe extension and hip abduction (Power 4/5), hypoactive ankle reflex on the right side, and 50% sensory loss at the right L5 dermatome. Plain radiographs of the lumbosacral spine showed degenerative spondylolisthesis at the L4-L5 level. MRI demonstrated degenerative changes with multilevel facet arthropathy, more marked at the L4-L5 level, with degenerative spondylolisthesis at the same level. There was an asymmetrically enlarged right ligamentum flavum with an intrasubstance cystic lesion (central hyperintensity on T2 and hypointensity on T1) without communication to the facet joint, consistent with a ligamentum flavum cyst. The cyst was compressing and displacing the right-sided cauda equina nerve roots. Results: The patient was treated surgically with spinal decompression, excision of the cyst, and transforaminal lumbar interbody fusion at the L4/L5 level. Histologic analysis of the cyst showed pseudocystic degeneration without lining epithelium. Postoperatively, the patient did well, was mobilized the next day, and was discharged home with a significant resolution of symptoms. There was no recurrence of the patient’s symptoms at 1-year follow-up. Conclusion: Ligamentum flavum cyst, though rare, should be included in the differential diagnosis of any patient presenting with radiculopathy or neurogenic claudication. MRI is the most useful investigation in the diagnosis of these cysts. Surgical management is usually successful with good recovery of neurological deficits and pain. Any instability associated with a ligamentum flavum cyst, or its excision, should be addressed while surgically managing the case.
716
P207: Postoperative MRI insights on OLIF: from hematoma incidence to contra-lateral root injury
Suhun Lee 1 , Dongwuk Son 1 , Joonbum Woo 2 , Junseok Lee 1 , Geunsung Song 1
1 Neurosurgery, Pusan National University Yangsan Hospital, Yangsan-si, South Korea
2 Neurosurgery, Inje University College of Medicine, Haeundae Paik Hospital, Busan, South Korea
Introduction: OLIF, with its strong points of minimal invasiveness and indirect decompression, is becoming increasingly popular in spine surgery. Nonetheless, as a relatively new surgical technique, comprehensive reports on its complications are lacking. There might be overlooked or yet-to-be-identified potential complications. Our study seeks to identify these and other potential complications of OLIF through postoperative MRI analysis. Material and Methods: Routine postoperative MRI (postMR) was conducted one week after surgery. We evaluated the cage's position at each level based on its insertion angle and depth. In addition, the relationship between this location and contralateral root injury was analyzed. We also assessed the incidence of hematomas at both the approach and contralateral sites. Specific post-OLIF complications, such as residual disc rupture and extensive synovial cyst formation, were further examined. Results: Of the study, 401 patients and 650 levels were included. The OLIF cage showed an increased obliqueness at lower levels (L2/3: 4.71 ± 4.82°, 3/4: 5.60 ± 4.42°, 4/5: 9.84 ± 6.29°, 5/1: 18.5 ± 4.91°). However, the cage depth remained relatively consistent (L2/3: 7.08 ± 2.68 mm, 3/4: 7.30 ± 2.52 mm, 4/5: 6.81 ± 2.67 mm, 5/1: 6.56 ± 2.99 mm). Cages with depths less than 5 mm were classified as the 'deep cage group', and their occurrences were 20.3%, 15.7%, 25.8%, and 46.2% at L2/3, 3/4, 4/5, and 5/1 levels, respectively. Symptomatic contralateral root injuries were only noted at L4/5 in the deep cage group. For the non-deep cage group, residual disc ruptures were observed in L4/5 and 5/1, central or foraminal in nature. Hematomas at the approach site were found in 65.2% of cases, with 4.9% having significant hematomas larger than 10 cc. contralateral psoas hematomas were seen in 19.0% of cases, but with no related symptoms. Extensive synovial cyst formation was found in 4 cases, causing foot drop in one. Notably, all patients with extensive synovial cyst formation had spondylolisthesis accompanied by facet joint subluxation. Conclusion: The most prevalent post-MR finding in OLIF was hematomas at the approach site, though these were mostly subclinical. Contralateral psoas hematomas were also common but weren't symptomatically significant. Symptomatic complications, like contralateral root damage and extensive synovial cyst formation, necessitate further risk factor exploration.
783
P208: A prospective multi-centric study of controlled thermal energy and rotational capsular tissue shaving system in patients with facet joint syndrome
Sahil Mhaisane 1 , Vikas Kapoor 1
1 Spinal Surgery, Stepping Hill Hospital, Stockport, United Kingdom
Introduction: Facet Joint Syndrome (FJS) is among the leading causes of low back pain and affects millions globally. Typically manifesting from spinal osteoarthritis (OA), FJS is a painful, chronic condition where treatment options, often temporary in nature, have remained unchanged in the past four decades. A novel, minimally invasive system has been developed to provide potential long-term relief via a combination of controlled thermal energy and rotational capsular tissue shaving off the facet capsule to disrupt nociceptive signals and receptors. Materials and Methods: Prospective study that included patients with chronic intractable pain of the low back resulting from FJS who had failed conservative treatments for pain. Period of study from July 2017 and August 2022 at three hospitals across Greater Manchester in the United Kingdom. This study recruited 80 patients. Outcomes of leg and back pain were assessed using the visual analogue score (VAS) at baseline and at follow-ups conducted at 1-, 3-, 6-, 12- and 24-months post-treatment. A second prospective study was undertaken in 2018 in Medellín, Antioquia, Columbia at Clínica CES and Clínica Las Vegas. It consisted of eight patients who received treatment for FJS. Clinical outcome was measured using VAS for back pain, at baseline and at follow-up conducted 48-months post-treatment. Results: Baseline mean scores for the 80 patients prior to treatment for VAS Back was recorded as 6.3 and VAS Leg as 2.1 on 1-10 scales. Post-treatment VAS Back mean scores reduced to 3.8, 3.0, 2.7, 2.3, 2.2, and VAS Leg mean scores reduced to 1.3, 1, 1, 1, 1.1, at follow-ups 1-, 3-, 6-, 12-, and 24-months respectively. The baseline mean scores for VAS Back for the eight patients in Medellín, Antioquia, Columbia, prior to treatment was recorded as 9.25 on a 1-10 scale, and reduced to a mean of 0.5 at 48-months post-treatment. Mean visual analogue scale (VAS) scores for back pain from Columbian clinical location at 0- (baseline) and 48-months post treatment. Conclusion: Rotational capsular shaving and controlled thermal ablation is effective in treating back pain and improving physical functioning in patients with facet joint syndrome. We have presented here two clinical studies looking at outcomes at two- and four-years post-treatment. Both studies showed significant post-treatment reduction in back pain, with mean VAS Back reducing 65% in two-years post-treatment (n = 69) and 95% in four-years post-treatment (n = 8). No adverse events or complications were reported in either study. Through outcome measures VAS Back and VAS Leg, collected at two separate clinical locations, it has demonstrated to offer a minimally invasive, non- opioid drug alternative that provides significant sustained long-term relief from pain in patients with FJS.
816
P209: Identifying efficiency improvement in microdiscectomy
Eric Mai 1 , Yeo Eun Kim 1 , Jerry Du 1 , Omri Maayan 1 , Kasra Araghi 1 , Nishtha Singh 1 , Maximillian Korsun 1 , Catherine Himo Gang 1 , Joshua Zhang 1 , Myles Allen 1 , Olivia Tuma 1 , Cole Kwas 1 , Eric Kim 1 , Chad Simon 1 , Tomoyuki Asada 1 , Avani Vaishnav 1,2 , Sravisht Iyer 1 , Sheeraz Qureshi 1
1 Hospital for Special Surgery
2 Boston Medical Center, USA
Introduction: With increased focus on value in healthcare, there is significant interest in optimizing efficiency and reducing costs. Although there is significant variation in efficiency among spine surgeons, identifying targets for improvement remains unknown. This study aims to demonstrate a method to determine variations in efficiency through measuring time with radical transparency for the peri-operative phases of a common spine procedure, microdiscectomy, and compare to time as measured by our hospital electronic medical record (EMR). Material and Methods: This is a case-series study of patients who underwent single-level tubular lumbar microdiscectomy by a single spine surgeon at a single academic center. The radical time transparency method was used to assess the discrepancy of time-efficacy. Two observers used stopwatches to directly measure time spent by patients in each area of the hospital, time dedicated to patient-care by patient-facing personnel, and key operating room (OR) time metrics. The measured times were compared to the times recorded in the EMR using the Wilcoxon sign-rank test. Professional staff interviews were conducted to identify targets for improving efficiency. Results: Direct observations and retrospective EMR review of time data were performed for nine microdiscectomies (six ambulatory and three inpatient surgery). The patients included five male and four female patients, with an average age of 48.3 ± 14.9. There were no statistically significant differences in time spent by patient in different areas of the hospital between direct observation versus EMR. By direct observation, the average total time spent in the hospital for ambulatory cases was 365 ± 56.8 minutes (range, 275-399 minutes). Patients on average spent 21.3 ± 18.3 minutes in registration, 82.4 ± 27.2 minutes in pre-op, 80.2 ± 13.6 minutes in the OR, and 185.2 ± 44.2 minutes in post-anesthesia care unit (PACU). The EMR lacked granularity in OR times metrics, particularly for staff times dedicated to patient care such as registration, pre-op, and PACU. The EMR overestimated the time from when the patient entered the room to the anesthesia start time (7.4 ± 2.5 min. vs. 4.2 ± 1.1 min., p = 0.007). Time for key OR personnel were also missing, including attending surgeon and radiology technicians. The EMR underestimated the time for the anesthesiologist dedicated to patient care in the OR (p = 0.011), while overestimating the time for neuromonitoring technicians (p = 0.038). Through interviews with staff, we identified methods for increasing efficiency for microdiscectomy cases, including encouraging mobile check-in/registration for eligible patients, ensuring vendors/reps are available in the OR to troubleshot technical issues with equipment, and coordinating with patients’ pharmacies in advance to facilitate smooth discharge. Conclusion: Our study highlights a method for determining variations in efficiency through directly measuring time for essential portions of microdiscectomies from both patient and staff perspectives. While some important time metrics can be collected from the EMR retrospectively, this data is often incomplete and less granular compared to direct measurements with the “stopwatch”. This method may identify areas of improved efficiency both objectively through perceived outliers of time as well as through comparisons of different surgeons and workflows.
859
P210: Comparetive study between the results of microlumbar discectomy and open discectomy
Anowarul Islam 1 , Suvradev Saha 1
1 Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Introduction: Lumbar disc herniations and lumbar canal stenosis are among the most common pathologies requiring spine surgery, and there has been a tendency of performing microlumbar discectomy for these indications in many spine surgeons in recent years. Very few comparative studies with homogenous cohorts of patients and long term follow up have been performed, to date. Material and Methods: This study was conducted from July 2015 to January 2023. 920 patients who underwent micro lumbar discectomy (MLD) or open discectomy, with minimum 2 years postoperative follow up were included. Retrospective review was performed. Outcomes were assessed by perioperative complications VAS score, modified odoms criteria and two year revision rates. Results: The 920 patients in this cohort underwent: 562 Open discectomy (age 43.1 ± 12.2,) and 358 MLD (age 47.6 ± 13.1,). The MLD group had significant greater operative time (62.2 vs. 40.3 min, p = .004) and higher rate of recurrence to open discectomy (2.8% vs.1.6%, p = .038). There were significant differences between the MLD and traditional technique where blood loss, length of stay, and surgical site infection rates were higher in traditional group (p < 0.05). Difference of pre and postoperative VAS was 5.2 ± 1.4 in traditional techniques and 3.8 ± 1.5 in MLD. Post-operative complications assessed included: acute postoperative neurological weakness, cardiac, neurological, pulmonary, urinary events, deep vein thrombosis or pulmonary embolism and ileus, those are higher in discectomy/laminectomy group (5.9% vs 2.4%). Conclusion: Traditional open techniques has better postoperative pain control with less recurrence rate. However, MLD has better postoperative recovery and minimum complication rate.
912
P211: Feasibility of oblong OLIF cages at L5-S1 level during oblique lumbar inter body fusion. Are they more secure than ALIF type cages?
Dhruvin Patel 1
1 Spine Surgery, SIDS Multispeciality Hospital, Surat, India
Introduction: OLIF at L5-S1 level is emerging as a promising minimally invasive technique. However, insertion of regular oblong OLIF cages is much easier than inserting regular ALIF shaped cages at L5-S1 level. Infact they are more secure in a pressfit manner with less chances of backing out and may not require additional screw fixation if they are properly rotated. Material and Methods: This is a restrospective study of 20 cases of OLIF at L5-S1 level from January 2019 to August 2023.They were all operated from left sided OLIF approach and regular titanium oblong OLIF cages were inserted without locking screws anteriorly. However, all cases were fixed posteriorly, either open or Minimally way.Pre and post. Op ODI were measured and Pre and post radiological outcome were assessed. Results: There was no back out iof cages in any cases. Although, many cages could be sufficiently rotated after oblique insertion, some could not be rotated due to LCIV position and iliac crest overhang. Clinical outcome was good. Conclusion: Regular oblong shaped OLIF cages are much more secure at L5-S1 level. They are easier to insert and need to be rotated after oblique insertion. Achievement of Lordosis was as good as other cage shapes.
938
P212: Comparison of the saftey of inpatient versus outpatient lumbar fusion: a systematic review and meta-analysis
Tejas Subramanian 1 , Izzet Akosman 1 , Troy Amen 1 , Neerav Kumar 1 , Austin Kaidi 1 , Kasra Araghi 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Tomoyuki Asada 1 , Pratyush Shahi 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Preforming lumbar fusion in an outpatient or ambulatory setting is becoming an increasingly employed strategy in an effort to provide effective value-based care. As this is an emerging option for surgeons to employ in their practices, the data is still in its infancy. The objective of this systematic review and meta-analysis is to synthesize the early data regarding and analyze the safety profile of outpatient lumbar fusion. Material and Methods: This study was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Studies that described outcomes of inpatient and outpatient lumbar fusion cohorts were searched from PubMed, Medline, The Cochrane Library, and Embase. Data regarding rates of individual medical and surgical complications, readmission, and reoperation were collected when applicable. Patient reported outcomes were additionally collected if reported. Individual pooled comparative meta-analysis was performed for outcomes of medical complications, surgical complications, readmission, and reoperation. Patient reported outcomes were reviewed and qualitatively reported. Results: The search yielded 14 publications that compared outpatient and inpatient cohorts with a total of 75,627 patients. Odds of readmission demonstrated no significant difference between outpatient and inpatient cohorts (OR = 0.94). Revision surgery similarly was no different between the cohorts (OR = 0.81). Pooled medical and surgical complications demonstrated significantly decreased odds for outpatient cohorts compared to inpatient cohorts (OR = 0.58, OR = 0.41 respectively). Patient reported outcome measures were largely the same between the cohorts when reported, with few studies showing better outcomes among outpatient cohorts compared to inpatient cohorts. Conclusion: Preliminary data regarding the safety of outpatient lumbar fusion demonstrates a favorable safety profile in appropriately selected patients, with patient reported outcomes remaining comparable in this setting. There is no data in the form of prospective and randomized trials which will be important to definitively change practice.
974
P213: Quality of spine surgery information on social media: a DISCERN analysis of Tik Tok videos
Tejas Subramanian 1 , Kasra Araghi 1 , Izzet Akosman 1 , Olivia Tuma 1 , Amier Hassan 2 , Ali Lahooti 2 , Anthony Pajak 1 , Pratyush Shahi 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
2 Weill Cornell Medical, New York, USA
Introduction: The use of social media applications to disseminate information has substantially risen in recent decades. Spine and back pain-related hashtags have garnered several billion views on TikTok. As such, these videos, which share experiences, offer entertainment, and educate users about spinal surgery, have become increasingly influential. Here we aim to assess the quality of spine surgery content TikTok from providers and patients. Material and Methods: Hashtags encompassing spine surgery (“#spinalfusion,” “#scoliosissurgery,” and “#spinaldecompression”) were searched using TikTok’s algorithm, and 50 videos were analyzed for each hashtag. Quality of information as rated by the DISCERN questionnaire. Two independent reviewers rated the quality of each video via the DISCERN questionnaire. Video metadata (likes, shares, comments, views, length) were all collected; type of content creator (musculoskeletal, layperson) and content category (educational, patient experience, entertainment) were determined. Results: The overall DISCERN score was, on average, 24.4. As defined by views per day, there was no statistically significant difference in popularity between the three hashtags. However, #spinalfusion videos demonstrated greater engagement, higher average likes (92,153 vs. 3,843 vs. 62,945; p = 0.02), and more comments (1,053 vs. 33 vs. 355; p < 0.0001) compared to #spinaldecompression and #scoliosissurgery, respectively. Interestingly, #spinaldecompression had the highest DISCERN score (27 vs. 24 vs. 22; p < 0.0001), likely explained by the higher percentage of videos that were educational (90% vs. 8% vs. 16%; p < 0.0001) and higher percentage created by MSK professionals (62% vs. 8% vs. 6%; p < 0.0001) when compared to both #spinalfusion and #scoliosissurgery. As rated by DISCERN, compared to laypersons, MSK professionals had significantly (27.7 vs. 23.3, p < 0.0001) higher quality videos. Similarly, the educational content category had significantly (26.4 vs. 18.9 vs. 23.9; p < 0.0001) higher quality videos. However, video interaction trended lower with MSK videos compared to Layperson; and educational videos had the lowest interaction of the content category (likes: 6,576 vs. 75,343 vs. 82.322; p = 0.023, comments: 77 vs. 412 vs. 774; p = 0.005). Conclusion: As rated by the DISCERN instrument, the quality of spine surgery videos on TikTok is low. #Spinaldecompression had higher quality videos than #spinalfusion or #scoliosissurgery though they tended to be less interacted with. Similarly, MSK videos and educational videos were of higher quality but also experienced less engagement. As the influence of the new social media landscape governs how the average person consumes their information, MSK providers should participate in disseminating high-quality content.
1016
P214: Anatomic variation with supine to prone positioning: implications for prone transpsoas single-position lumbar fusion
Andy Ton 1 , Brandon Gettleman 2 , Ryan Palmer 1 , Marc Abdou 1 , Emily Mills 1 , Michael Safaee 3 , Jeffrey Wang 1 , Raymond Hah 1 , R. Kiran Alluri 1
1 Orthopaedic Surgery, Keck School of Medicine at The University of Southern California, Los Angeles, USA
2 University of South Carolina School of Medicine, Columbia, USA
3 Neurological Surgery, Keck School of Medicine at The University of Southern California, USA
Introduction: The prone transpsoas (PTP) approach is a novel lumbar fusion technique performed entirely in the prone position, offering benefits of lateral-based fusions and posterior spinal column access. Preoperative supine magnetic resonance imaging (MRI), however, may misrepresent surgical anatomy in the prone position. As such, the present study describes relative anatomical shifts, with pertinence to the lumbar spine, from supine to prone. Material and Methods: This was a retrospective cohort review of posterior lumbar fusion patients from 2018-2022 with preoperative MRI and intraoperative prone CT-guided images. Deformity, infection, trauma, or malignancy were excluded. Anteroposterior (AP) and mediolateral (ML) distances (mm) were measured on axial slices from reference lines relative to vertebral endplates at each lumbar level. Both AP and ML distances to abdominal great vessels, psoas major, intervertebral discs (IVD) were measured. Dependent samples t-test and analysis of variance (ANOVA) were used to assess shifts from supine to prone and between segments, respectively. Subanalysis was performed in patients with a history of anterior/lateral-based lumbar surgery. Results: Across 58 patients (45% female), overall mean age and body mass index (BMI) were 62.4 + 11.0 years and 29.8 + 6.5 kg/m2, respectively. Eight patients (14%) had a history of anterior/lateral-based lumbar surgery (revision group). Significant AP translation was seen at L2-L3 and L3-L4 for the IVC (p < 0.001) and aorta (p < 0.05), and L4-L5 for common iliac arteries (p < 0.001) and veins (p < 0.05). Symmetric AP excursion of the psoas major was seen at L2-L3 and L4-L5 in prone (p < 0.05). Significant AP translation was limited to the IVC at L2-L3 and L3-L4 (p < 0.05) in the revision subgroup. No significant differences in mean translation were seen across levels. Conclusion: Intraoperative prone positioning may alter anatomical parameters seen on preoperative MRI, which can be further impacted by post-surgical changes. These shifts should be accounted for when performing PTP.
1077
P215: Which factor can predict the effect of indirect decompression using oblique lumbar interbody fusion?
Joonbum Woo 1 , Suhun Lee 2 , Dongwuk Son 2 , Geunsung Song 2
1 Neurosurgery, Inje University College of Medicine, Haeundae Paik Hospital, Busan, South Korea
2 Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, South Korea
Introduction: The aim of this study was to investigate the association between various factors of indirect decompression. Previous studies have demonstrated the effectiveness of indirect decompression. There is no consensus regarding the predictive factors for indirect decompression. Facet joint gap (FJG) and bulging disc thickness (BDT) have never been considered as factors in other studies. Material and Methods: We retrospectively reviewed 62 patients who underwent OLIF L4/5 between April 2018 and September 2020. The relationships between cross-sectional area (CSA) change, CSA change ratio, spinal stenosis grade, and various factors were studied. Various factors related to indirect decompression, such as ligament flavum thickness (LFT), foraminal area (FA), disc height (DH), bulging disc thickness (BDT), and facet joint gap (FJG), were measured. Results: CSA increased from 69.72 mm2 preoperatively to 115.95 mm2 postoperatively (p < .001). BDT decreased from 4.97 mm preoperatively to 2.56 mm postoperatively (p < .001). FJG (Right) increased from 2.99 mm preoperatively to 4.38 mm postoperatively (p < .001). FJG (Left) increased from 2.95 mm preoperatively to 4.52 mm postoperatively (p < .001). The improvement of spinal stenosis grade was as follows: 1 point up group, 38 patients; 2 point up groups, 19 patients; and 3 point up groups, 3 patients. The correlation factors were prespinal stenosis grade (0.723, p < .00), CSA change (0.490, p < .00), and FJG change ratio (left, 0.336, p < .008). Conclusion: FJG showed statistical significance with indirect decompression. Indirect decompression principles might be utilized in patients with severe spinal canal stenosis (even grade 4).
1108
P216: Incidence and risk factors of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion: minimum 2-year follow-up
Lei Yuan 1 , Weishi Li 1 , Yan Zeng 1
1 Orthopedic Department, Peking UniversityThird Hospital, Beijing, China
Introduction: There is no consensus on the risk factors of PJK in degenerative lumbar scoliosis (DLS), and the impact of lumbar muscle volume on PJK in DLS has not been previously evaluated. Material and Methods: 84 DLS patients undergoing long instrumented fusion surgery were retrospectively studied. Patient characteristics, surgical variables, radiographic parameters were analyzed statistically. The lumbar muscularity and fatty degeneration were evaluated on MRI. The region of interest (ROI) of the area of lean muscle tissue excluding fatty infiltration was drawn to determine the functional cross-sectional area (FCSA), the muscle-fat index of the lean muscle within the ROI was defined as lean muscle-fat index (LMFI). Gross cross-sectional area (GCSA) was determined by drawing the outer perimeter of the muscle including any areas of intramuscular fat and the muscle-fat index of the GSCA was defined as total muscle-fat index (TMFI). Results: The prevalence of PJK was 20.24%. Lower bone mineral density was observed in PJK group. The FCSA of PSE in PJK group was statistically smaller than Non-PJK group at all levels. No significant differences of the GCSA of PSE between the groups were observed. The LMFI and TMFI of PSE in PJK group were higher than in the Non-PJK group at all levels. Preoperative, immediate postoperative and follow-up TLK were significantly greater in the PJK group (p < 0.05). PJK group had smaller preoperative SS, larger preoperative sagittal vertical axis (SVA) and SVA correction. Logistic regression analysis showed that osteoporosis, preoperative TLK > 15°, SS < 24°, FCSA of PSE < 138.75 and TMFI of PSE > 44.08 were independently associated with PJK. The final follow-up VAS score for back pain was higher and SRS-22 subcategories of pain, function, self-image and total score were significantly lower in PJK group. Conclusion: Preoperative BMD, lower lumbar muscularity and higher fatty degeneration, preoperative greater TLK and smaller SS were found to be strongly associated with the presence of PJK.
1153
P217: Pedicle screw placement on lumbar spine 3D MRI and comparisons of geometric measurements against CT
Frederik Abel 1 , George Gorgy 2 , David Dalton 2 , Qian Li 1 , Elisha Lim 1 , Fedan Avrumova 2 , J. Levi Chazen 3 , Darryl Sneag 1 , Darren Lebl 2 , Ek Tsoon Tan 1
1 Radiology
2 Spine Surgery
3 Neuroradiology, Hospital for Special Surgery, New York, USA
Introduction: The objective of this study was to test for equivalency of virtual pedicle screw placement on 3D lumbar spine MRI with “CT-like” contrast, in comparison to CT, and to compare their geometric measurements, for the purpose of robotic navigated assistance (RNA) in spinal surgery. Materials and Methods: Between December 2021 and June 2022, 16 patients referred for spinal fusion and decompression surgery with pre-operative 3D lumbar spine MRI and CT were retrospectively assessed. Pedicle screws were virtually placed on the lumbar (L1-L5) and sacral vertebra (S1) by 3 spine surgeons and metrics (lateral deviation, axial and sagittal angles) were collected. Vertebral body length/width (VL/VW) and pedicle height/width (PH/PW) were measured on the lumbar vertebra (L1-L5) by 3 radiologists. For both pedicle screw placing and geometric measurements, an equivalency design was used to prove whether outcome differences did not differ by a predefined margin (± 1mm for lateral, and ± 2.08° for angle deviation). Inter- and intra-rater reliability was assessed by intraclass correlation coefficients (ICC). Results: Across all vertebral levels combined and separately, the 95% confidence interval (CI) limits were within the predefined margin and equivalency between CT and MRI proven for all pedicle screw metrics and geometric measurements, except for VL at L1 (mean difference: -0.64mm; [95%CI -1.05, -0.24]) , L2 (-0.65mm; [95%CI -1.11, -0.20]), and L4 (-0.78mm; [95%CI -1.11, -0.46]). Inter-and intra-rater ICC for pedicle screw metrics across all vertebral levels combined ranged from 0.69 – 0.91 and 0.89 – 0.98 for CT, and from 0.62 – 0.92 and 0.81 – 0.97 for MRI, respectively. Inter-and intra-rater ICC for geometric measurements ranged from 0.60 – 0.95 and 0.84 – 0.97 for CT, and 0.61 – 0.95 and 0.93 – 0.98 for MRI, respectively. Conclusions: This study demonstrated that DL reconstructed 3D MRI facilitates equivalent computer-simulated pedicle screw placements and geometric assessment for most lumbar vertebra compared to CT for pre-operative planning in patients being considered for RNA spine surgery.
1219
P218: Vertebral compression fractures in the elderly: an unpredictable aspect of osteoporosis
Paula Suárez 1 , Alicia Collado 1 , Tomasz Rumin 1
1 Orthopedics and Traumatolgy Surgery, Hospital Universitario Infanta Elena de Madrid, Madrid, Spain
Background: The prevalence of osteoporosis in the Spanish population amounted to 5.4%. The cost of osteoporotic fractures in Spain accounted for approximately 3.8% of healthcare spending. Occurrence of osteoporotic fractures make the elderly patient susceptible for further fractures and increases the morbidity and mortality, due to pain, kyphosis and loss of the “cone of economy”. Objectives: To describe our management of an osteoporotic lumbar compression fracture and raise awareness of the importance of an early diagnose and treatment of an osteoporotic fracture. Study Design & Methods: We present the case of a 76-year-old woman who reported an accidental fall. The patient was evaluated in our center months after the fall, as a result of the collapse to which our health system was subjected during the SARS-COV2 pandemic, due to poorly controlled pain and progressive deformity in flexion during ambulation with progressive impossibility to carry out daily activities. Physical examination revealed no peripheral neurological clinical evidence or pyramidalism. A first x-ray is indicated in which, a fracture-wedging of L1 and T12 with regional kyphosis that exceeds 40º can be seen. MRI is requested in which a severe crushing of D12 and L1 with wedging of the anterior part of the vertebral body (of L1) is observed and minimal displacement of the posterosuperior corner of both vertebras towards the canal. The objective is to restore the sagittal balance and provide a correct support to the fracture. Results: A corpectomy of the L1 vertebra is performed through a XLIF (Extreme lateral interbody fusion) left approach, with thoracotomy and partial exeresis of the 11th rib and of the left diaphragmatic pillar. A MOSS vertebral body replacement spaceris placed. Correct placement is verified by intraoperative fluoroscopy. A pleural parietal tear is detected and sutured, followed by the placement of a pleural drain. In a second time, in the same surgical act, transpedicular vertebral fixation from D9 to D11 AND L3-L4 bilaterally joined with bars was performed using a posterior percutaneous approach. L2 could not be instrumented due to pedicular hypoplasia. The preoperative sagittal index was of 17.5º while the postoperative period was of 3.5º. The immediate postoperative period evolved favorably, allowing the patient to walk with a thermoplastic thoracolumbar orthosis. During the following days, no incidence was recorded, so she was discharged on the 4th post-surgery day, after removal of the pleural drain with a score of 27 in the Oswestry Scale and a mild 5 EVA score. The SF-36 functional quality of life scale was used. Conclusions: Osteoporotic fractures occurring in the thoracic and thoracolumbar region have been considered a benign pathology. Nowadays we know that special attention to these patients is needed, due to the risk of a high morbimortality and the important loss of quality of life that can produced in the elderly. We believe that a correct treatment in acute stages can prevent severe collapse and further neurological deficit and increasing kyphosis. Avoiding more aggressive treatment as the one we need to provide to our patient.
1276
P219: Psoas muscle health is correlated with time to achieve MCID in patients with predominant axial back pain following decompression surgery: early results
Nishtha Singh 1 , Chad Simon 1 , Tomoyuki Asada 1 , Mitchell Johnson 1 , Pratyush Shahi 1 , Kasra Araghi 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , James Dowdell 1 , Evan Sheha 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Poor psoas muscle health has been implicated as a determining factor for predominant axial back pain (PBP) and leg pain (PLP) in patients undergoing decompressive procedures. However, there is a paucity of evidence regarding the impact of psoas muscle health on patient-reported outcome measures (PROMs) in PBP and PLP patients. The study aims to determine whether psoas muscle health affects the achievement of minimal clinically important differences (MCID) in PROMs following decompression surgery. Material and Methods: Patients with PBP (VAS back > VAS leg) and with PLP (VAS leg > VAS back) who underwent laminectomy were included. Axial T2 MRI images were analyzed for psoas muscle size. Based on the lowest-quartile normalized total psoas area (NTPA) thresholds of each gender, patients were divided into high and low NTPA groups. Prospectively-collected outcomes were analyzed at early (< 6 months) and late (≥ 6 months) time points. Kaplan-Meier survival analysis was conducted to determine the probability of achieving clinically significant outcomes as a function of time. Results: Of 106 PBP patients, 83 (78.3%) had high psoas muscle health, while 23 (21.6%) had low psoas muscle health. Of 139 PLP patients, 54 (38.8%) had high psoas muscle health, while 85 (61.1%) had low psoas muscle health. In the PBP group, higher NTPA was found to be associated with high psoas muscle health, and low psoas muscle health was associated with older age (p < 0.05). For both PBP and PLP cohorts, no differences in MCID achievement rate for any PROMs existed between the low and high psoas muscle health groups. For the PBP patients, low psoas muscle health was associated with a longer time to MCID achievement for VAS back, ODI, and PROMIS-PF (p < 0.05). No association was found for the PLP patients between psoas muscle health and time to MCID achievement. According to Kaplan- Meier survival analysis for the PBP group, the median time to achieve MCID-VAS back and MCID-ODI for patients with high psoas health was 14 and 42 days respectively. On the other hand, for patients with low psoas health, the median time to achieve MCID-VAS back and MCID-ODI was 42 and 84 days respectively. Conclusion: Good psoas muscle health is associated with lesser time to achieve MCID in exclusively the PBP group following decompression surgery. The early results suggest that poor psoas muscle health plays an important role in patients with predominant back pain.
1282
P220: DLIF versus circumferential fusion employing TLIF - a potential influence on spinal instrumentation stability
Andrey Bokov 1 , Svetlana Kalinina 1 , Anatoly Bulkin 1
1 Neurosurgical, Federal Budgetary Institution Privolzhskiy Medical Research University, Nizhniy Novgorod, Russian Federation
Introduction: Different techniques were introduced in clinical practice to provide fusion of altered segments in patients with degenerative diseases of the lumbar spine, however no evidence has been provided on advantages of one technique over another. The objective of this study is to assess influence of fusion type on rate of implant instability development and associated revision surgery. Material and Methods: This is a single-center prospective evaluation of consecutive 136 patients with degenerative diseases of the lumbar spine and instability of spinal segments. Patients with axial pain and neurogenic claudication or radiculopathy were enrolled. Either conventional transforaminal lumbar interbody fusion (TLIF) with a single cage supplemented with posterior fusion or direct lateral interbody fusion (DLIF) using cages of standard dimensions, were applied in this study. Conventional open technique was employed to supplement TLIF with pedicle screws while percutaneous screw placement was used in patients treated with DLIF. The duration of the follow-up accounted for 18 months. Signs of pedicle screws loosening and bone union after fusion were assessed by the results of CT imaging. All cases with pedicle screw loosening detected on CT were registered. Fisher`s exact test was used to assess the differences in rate of CT loosening signs and clinically significant cases that required revision surgery. Logistic regression was used to assess the association between potential factors and complication rate. Results: The rate of pedicle screw loosening signs detected on CT images and revision surgery applied because of implant instability in groups treated with TLIF and DLIF accounted for 25 (32.9%) versus 2 (3.2%) respectively for the former and 9 (12,0%) versus 0 (0%) for the latter respectively. The differences in rate of pedicle screw loosening detected on CT images and revision surgery were statistically significant, p < 0.0001 and p = 0.0043 respectively. Using general logistic regression analysis it has been estimated that a decrease in radiodensity values and greater number of levels fused were associated with a rise in pedicle screw loosening rate. DLIF application in patients with radiodensity below 140 HU was associated with a considerable decrease in pedicle screw loosening rate. Unipolar or bipolar pseudoarthrosis in patients operated on with TLIF was associated with a rise in number of pedicle screws loosening rate while even in case of nonunion grade 3 and 4 no increment in pedicle screws loosening rate was detected in a group of patients treated employing DLIF. In case of pseudoarthrosis after TLIF procedure supplementary total or partial posterior fusion resulted in a decline in pedicle screws loosening rate. The estimated logistic regression model had a specificity accounting for 96.3%, sensitivity 74.1% and preciseness of classification 91.91%. Conclusion: Even though the supplementary posterior fusion may considerably reduce the rate of pedicle screw loosening in patients treated with TLIF, application of DLIF provide greater stability resulting in a substantial decline in pedicle screws loosening rate.
1292
P221: Utility of preoperative whole-body imaging in candidates for lumbar spine surgery: the impact of concomitant lower extremity osteoarthritis
Omri Maayan 1 , Bo Zhang 1 , Anthony Pajak 1 , Pratyush Shahi 1 , Tejas Subramanian 1 , Troy Amen 1 , Tomoyuki Asada 1 , Sheeraz Qureshi 1 , Francis Lovecchio 1
1 Hospital for Special Surgery, New York, USA
Introduction: Concomitant hip or knee osteoarthritis may confound radicular complaints, introduce diagnostic uncertainty, and hinder postoperative recovery in patients with degenerative spine conditions. This study aimed to assess the utility of preoperative whole-body imaging in diagnosing lower extremity osteoarthritis, evaluate the association of lower extremity osteoarthritis with radiculopathy, and determine its impact on postoperative recovery. Material and Methods: Patients with preoperative whole-body imaging undergoing lumbar spine surgery for degenerative conditions were included. The Kellgren and Lawrence score was implemented to grade joint osteoarthritis as mild (score ≤ 2) or severe (score ≥ 3). Length of stay and side of radiculopathy were assessed. The Oswestry Disability Index, Patient-Reported Outcomes Measurement Information System, Visual Analog Scale Back/Leg, and Short Form-12 Physical Component Scale/Mental Component Scale were recorded at preoperative, early postoperative (2-, 6-, 12-week), and late postoperative (6-, 12-, 24-month) timepoints. Multivariate analysis was used to evaluate the association of hip and knee osteoarthritis with patient-reported outcomes and achievement of minimum clinically important difference. Results: A total of 207 patients were included (hip osteoarthritis: 130 (67.7%) mild, 62 (32.3%) severe; knee osteoarthritis: 141 (72.7%) mild, 53 (27.3%) severe). 28 hips (6.7%) and 22 knees (5.3%) were post-arthroplasty and excluded from the analysis. Patients with severe hip and knee osteoarthritis were significantly older compared to patients with mild osteoarthritis (p < 0.05). The laterality of osteoarthritis was not associated with the side of radiculopathy. After controlling for age, length of stay was approximately 50% greater for patients with severe hip (p = 0.031) and knee (p = 0.013) osteoarthritis compared to mild hip and knee osteoarthritis. Patients with severe knee osteoarthritis exhibited worse Patient-Reported Outcomes Measurement Information System at the early postoperative timepoint (p = 0.013) and late postoperative timepoint (p = 0.049), as well as worse Visual Analog Scale Back (p = 0.009) and Short Form-12 Physical Component Scale (p = 0.025) at the late postoperative timepoint. Severe hip and knee osteoarthritis reduced the likelihood of achieving the minimum clinically important difference for Short Form-12 Physical Component Scale (OR 0.44; p = 0.049) and Patient-Reported Outcomes Measurement Information System (OR 0.37; p = 0.027), respectively. Conclusion: Whole-body imaging captures a high prevalence of radiographic hip and knee osteoarthritis in the degenerative lumbar spine population. Severe hip and knee osteoarthritis was associated with decreased achievement of minimum clinically important difference for certain patient-reported outcomes and increased length of stay after lumbar spine surgery. Thus, obtaining preoperative whole-body imaging may uncover underlying lower extremity osteoarthritis and prompt patient-specific counseling regarding expectations after lumbar spine surgery.
1293
P222: Clinical and radiographic outcomes after indirect decompression with minimally invasive transforaminal lumbar interbody fusion
Omri Maayan 1,2 , Daniel Shinn 2 , Keith Lyons 2 , Karim Shafi 2 , Junho Song 2 , Pratyush Shahi 2 , Kasra Araghi 2 , Nishtha Singh 2 , Olivia Tuma 2 , Maximillian Korsun 2 , Tomoyuki Asada 2 , Chad Simon 2 , Avani Vaishnav 2 , Eric Mai 2 , Yeo Eun Kim 2 , Joshua Zhang 2 , Cole Kwas 2 , Myles Allen 2 , Eric Kim 2 , Sravisht Iyer 2 , Sheeraz Qureshi 2
1 Weill Cornell Medical, New York, USA
2 Hospital for Special Surgery, New York, USA
Introduction: With the availability of large-footprint expandable interbody cages for minimally invasive transforaminal lumbar interbody fusion, many surgeons have increasingly begun to rely on indirect decompression alone. However, the degree of indirect decompression achieved has not yet been fully determined. Thus, the objective of the present study was to assess the extent of indirect decompression achieved with minimally invasive transforaminal lumbar interbody fusion and determine its impact on patient-reported outcome measures. Material and Methods: Adult patients who underwent primary one- or two-level minimally invasive transforaminal lumbar interbody fusion without direct decompression between March 2017-2021 with ≥1-year clinical follow-up were included. CT scans were used to measure disc height, cross-sectional foraminal area, and central canal area at the operative levels. Sagittal radiographs were implemented for assessment of pelvic incidence, lumbar lordosis, and segmental lordosis. The most recent preoperative and postoperative patient-reported outcomes (Oswestry Disability Index, Patient-Reported Outcomes Measurement Information System, Visual Analog Scale Back/Leg, Short Form-12) ≥ 1-year after surgery were evaluated. Paired t-tests were performed to compare preoperative and postoperative CT measurements, radiograohic measurements, and patient-reported outcomes. Bivariate analysis was also used to identify correlations between changes in radiographic measures and patient-reported outcomes. Results: A total of 40 patients were included (Single Level: 80%; L5-S1: 52.1%). The average length of follow-up was 17.9 ± 7.9 months for patient-reported outcomes and 14.6 ± 8.1 months for CT imaging. Indirect-decompression resulted in significant increases in disc height (4.2 to 6.3 mm, p < 0.001), operative side foraminal area (140.8 to 180.8 mm2, p < 0.001), contralateral foraminal area (146.9 to 170.7 mm2, p < 0.001), and central canal area (228.6 to 266 mm2, p < 0.001). Sagittal alignment measures did not differ significantly between preoperative and postoperative radiographs (p > 0.05). Likewise, all patient-reported outcomes except SF-12 MCS (p = 0.439) showed a statistically significant improvement postoperatively. Percentage change in disc height was significantly correlated with change in Short Form-12 Physical Component Score (r = -0.379, p = 0.03). No other associations between percentage change in CT measurements and patient-reported outcomes were observed. Conclusion: Overall, minimally invasive transforaminal lumbar interbody fusion yielded a significant degree of indirect decompression and notable improvements in patient-reported outcomes at ≥ 1-year postoperative follow-up. Therefore, MI-TLIF may provide good clinical outcomes with indirect decompression alone.
1336
P223: Relationship between facet joint osteoarthritis and lumbar paraspinal muscle atrophy - a cross-sectional study
Ali Guven 1 , Lukas Schönnagel 1,2 , Gaston Camino-Willhuber 1 , Erika Chiapparelli 1 , Krizia Amoroso 1 , Jiaqi Zhu 3 , Soji Tani 1,4 , Thomas Caffard 1,5 , Artine Arzani 1 , Ek Tsoon Tan 6 , Jennifer Shue 1 , Andrew Sama 1 , Federico Girardi 1 , Frank Cammisa 1 , Alexander Hughes 1
1 Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, USA
2 Center for Musculoskeletal Surgery, Charité - Universitätsmedizin Berlin, Berlin, Germany, Berlin, USA
3 Biostatistics Core, Hospital for Special Surgery, New York, USA
4 Department of Orthopaedic Surgery, Showa University Hospital, Japan
5 Klinik Für Orthopädie, Universitätsklinikum Ulm, Germany
6 Department of Radiology and Imaging, Hospital for Special Surgery, New York, USA
Introduction: The paraspinal muscles play an essential role in the stabilization of the lumbar spine. Atrophy of the paraspinal muscles, characterized by decreased functional cross-sectional area (fCSA) and increased fatty infiltration (FI) has been linked to chronic back pain and degenerative processes of the lumbar spine, including facet joint osteoarthritis (FJOA). However, the relationship between the different paraspinal muscle groups and FJOA has not been fully explored. Material and Methods: In this cross-sectional study, we analyzed adult patients who underwent lumbar spinal surgery between December 2014 and March 2023 for degenerative spinal conditions and had preoperative MRI and CT scans. Exclusion criteria were lumbar scoliosis with a Cobb angle over 20° and previous lumbar surgery. The FI and fCSA of the psoas, erector spinae and multifidus muscles were assessed on T2-weighted axial MRIs at the level of the upper end plate of L4 based on established studies and calculated using custom-made software. The fCSA was adjusted by height in meters squared, similar to body mass index (BMI). Intervertebral disc degeneration at each lumbar level was evaluated using the five-grade Pfirrmann grading system on T2 weighted lateral images. The grades from each level were summed to report the cumulative lumbar Pfirrmann grade. Weishaupt classification (0-3) was used to assess FJOA at all lumbar levels (L1 to S1) on preoperative CT scans. In addition, the total lumbar FJOA score was determined by adding the grade of both sides at all five levels, resulting in 30 as the highest possible score. Correlation and linear regression analyses were conducted to assess the relationship between FJOA and paraspinal muscle parameters. Results: A total of 225 patients (49.7% female) with a median age of 61 years (IQR 54 – 70) and a median BMI of 28.3 kg/m2 (IQR 25.1 – 33.1) were included. The total FJOA score was significantly associated with age (rho = 0.624, p < 0.001), the FI of the multifidus (rho = 0.529, p < 0.001) and erector spinae (rho = 0.333, p < 0.001) muscles, as well as the fCSA of the multifidus (rho = -0.459, p < 0.001) and erector spinae (rho = -0.188, p = 0.004) muscles. After adjustment for age, sex, BMI and the cumulative lumbar Pfirrmann grade, only multifidus fCSA (Est = -4.69, 95% CI = -6.91 – -2.46, p < 0.001) and FI (Est = 0.64, 95% CI = 0.33 – 0.94, p < 0.001) were independently predicted by the total FJOA score. A similar relation was seen with individual FJOA grades of each lumbar level after controlling for age, sex, BMI and the Pfirrmann grade of the corresponding level. Conclusion: Atrophy of the multifidus muscle is significantly associated with FJOA in the lumbar spine. The lack of such correlation for the erector spinae and psoas muscles highlights the unique involvement of the multifidus muscle in the degeneration of the spinal motion segment. Further research is necessary to understand the causal relationship and the clinical implications of these findings.
1424
P224: Evaluation of treatment outcomes for chronic pain arising from lumbar spinal disorders using trans sacral canal plasty (TSCP): a comparative study between the monotherapy group and the rehabilitation-combined group
Yoshikazu Yanagisawa 1
1 Orthopedic Surgery and Spinal Disease Center, Fukuoka Miral Hospital, Fukuoka City, Japan
Introduction: Transsacral canal plasty (TSCP) has been reported to have some therapeutic effects for chronic pain originating from lumbar spinal disorders, but the surgical technique remains limited to adhesiolysis, and its effectiveness is restricted. Therefore, in our department, we have implemented inpatient treatment combining TSCP with physical therapy. In this study, we report on whether there is a difference in clinical outcomes between the TSCP monotherapy group and the group receiving combined physical therapy. Material and Methods: We conducted a study involving 34 patients with lumbar degenerative diseases who underwent TSCP in our department from 2019 to October 2022. The patients were divided into two groups: the TSCP monotherapy group (T group) consisting of 11 cases (mean age: 68.3 years) and the rehabilitation combined group (Re group) consisting of 23 cases (mean age: 73.7 years). In the Re group, after TSCP, we provided training in activities of daily living (ADL), core muscle training, and stretching, and encouraged patients to continue these practices after discharge if possible. The evaluation parameters included pain Visual Analog Scale (VAS) scores, the need for repeat surgery, and the duration required. The average follow-up period was 30.6 months (ranging from 9.2 to 52.3 months). Results: The preoperative VAS scores were 75.5 and 77.8 mm for both groups, showing no significant difference. The VAS scores at 1 month postoperatively were 36.4 and 33.3 mm, at 2 months 50.0 and 43.1 mm, and at 3 months 55.0 and 50.8 mm for T group and Re group, respectively, with Re group having lower values up to 3 months (no significant difference). However, at 6 months postoperatively, the scores were 53.6 and 56.6 mm, and at 1 year 58.0 and 60.0 mm, with no significant difference. Repeat surgery was required in 3 cases (27.3%) in the T group and 7 cases (30.4%) in the Re group, with a mean time to repeat surgery of 1.8 months in the T group and 6.6 months in the Re group. Conclusion: The course of VAS scores was favorable in the Re group up to 3 months postoperatively, but a tendency for recurrence was observed from 6 months postoperatively onwards. One contributing factor could be the slightly higher average age of the Re group at the time of surgery (with no significant difference). Although there was no significant difference in the rate of repeat surgeries, the Re group required a longer time to reach repeat surgery, possibly due to the continued effect of rehabilitation. While TSCP has been reported to provide pain relief for approximately three months in cases of chronic pain arising from lumbar spinal disorders, combining rehabilitation suggested the potential to extend the pain relief effect beyond what TSCP monotherapy can achieve.
1457
P225: Classification and management of adjacent segment disease after lumbar fusion
Rishi Kanna 1 , Nishat Ahmed 1 , Ajoy P Shetty 1
1 Spine Surgery, Ganga Hospital, Coimbatore, India
Introduction: Adjacent segment disease is a symptomatic degenerative disease of the lumbar spine developing adjacent to a spinal fusion. A working classification for the disease is desired since it would help to plan the treatment and prognosticate the outcomes. Methodology: Consecutive patients (n = 85) who experienced significant back /leg pain following a previous lumbar fusion surgery involving one or two motion segments (> 1 year) were studied. The clinical data collected included age, sex, duration, back pain or radiculopathy, primary diagnosis, surgical treatment, and ODI. The pre-operative MRI scans documented disc degeneration and the facet joints at the adjacent levels (proximal and distal). Post-operative images were examined for the type of ASD, presence of instability, and status of fusion. ASD was classified anatomically as Proximal, Distal, Or Combined. It was further sub-classified pathologically as: Type 1: Disc prolapse, Type 2: Disc instability, Type 3: Anterolisthesis and facet instability, Type 4: Retrolisthesis and Type 5: Stenosis. Results: Proximal ASD was the most common type (74%, 63/85). Among these, Type 5 ASD - Stenosis was the most prevalent subtype (33%, 21/63), followed by retrolisthesis (26%) and discal instability (19%). Distal ASD was relatively uncommon (11/85), but disc prolapse (45%) and intradiscal instability (27%) were the predominant subtypes. Eleven patients had combined ASD. Pre-operative disc degeneration, facetal angle, or laminectomy did not determine the type of ASD. Patients with LSTV had a higher incidence of Type 3 ASD anterolisthesis. 54% (46/85) were managed conservatively, while 10 (11%) received spinal injections and surgical intervention in 31% (27/85). Only 28% of proximal ASD required surgical management (18/63). In contrast, 6 /11 patients with distal ASD underwent surgery (54%). Conclusion: The classification provided in this study gives an insight into the different pathologies of ASD and their line of management. Proximal ASD was more common. The management of ASD varied, with conservative approaches being predominant, but surgical intervention was required in disc prolapse.
1519
P226: Cage displacement after anterior decompression and interbody titanium mesh cage placement in caries spine
Atif Ali 1 , Ali ijaz Ahmad 1
1 Orthopaedics and Spine Department, Ghurki Trust Teaching Hospital Lahore, Lahore, Pakistan
Background: Spinal tuberculosis patients present with various signs and symptoms which may include back or leg pain, kyphotic deformity, palpable mass in the paraspinal region, and neurological compromise. Treatment of spine tuberculosis may be conservative when it presents in early stage. Surgical treatment is preferable when patient presents with problems of deformity and neurologic deficit. Pseudo-arthrosis, pain or failure of chemotherapy is an issue. Surgical intervention may be limited to debridement, or radical resection with auto-grafting and instrumentation. Aim: To determine the percentage of cage displacement after anterior decompression and interbody titanium mesh cage placement in caries spine. Study design: Descriptive case series. Setting: Department of Orthopaedics and Spinal Surgery, Ghurki Trust Teaching Hospital/Lahore Medical & Dental College, Lahore. Duration of study: Six months (1st July 2011 to 31 December 2011). Methods: All patients fulfilling the inclusion criteria were included. Interbody Titanium Mesh Cage with packed bone graft was placed. Post-operative anterior & lateral radiographs were taken to check and record the position of the cage. Brace was applied for at least 6 months. Results: There were 34 males and 16 females with ratio 2.2:1. The patients age range was 15-60 years with mean age being 35.65 ± 12.12 years. 28 patients underwent thoracolumbar decompression, 13 thoracic decompression while 9 had lumbar decompression. Forty eight patients had no cage displacement while 2 patients had cage displacement. Conclusion: Titanium mesh cage was used as an interbody spacer in caries spine exhibiting immediate rigid fixation and successful bone union.
Keywords: Caries spine, Titanium mesh cage, Anterior decompression
1591
P227: Outcomes of minimally invasive decompression alone versus fusion in patients with predominant back pain
Pratyush Shahi 1 , Tejas Subramanian 1 , Omri Maayan 1 , Nishtha Singh 1 , Sumedha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Tomoyuki Asada 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Kasra Araghi 1 , Evan Sheha 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: No previous study has compared the outcomes of decompression alone and fusion in patients with predominant back pain and evidence is lacking on whether back pain alone, in absence of radiological indications for fusion, should influence surgical decision-making. The objective of this study was, therefore, to compare outcomes of minimally invasive decompression alone versus fusion in patients with predominant back pain. Material and Methods: This retrospective cohort study included patients who had undergone primary one- or two-level tubular minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) or decompression (unilateral laminotomy for bilateral decompression, ULBD) for the treatment of degenerative conditions of the lumbar spine and had preoperative Visual Analog Scale (VAS) back > preoperative VAS leg (predominant back pain). All patients had a minimum of 1-year follow-up. The following outcome measures were compared between the decompression and fusion groups: 1) patient-reported outcome measures (PROMs) (VAS back and leg; Oswestry Disability Index, ODI; 12-Item Short Form Survey Physical Component Score; SF-12 PCS), 2) minimal clinically important difference (MCID) achievement, 3) patient acceptable symptom state (PASS) achievement, and 4) global rating change (GRC). Two postoperative timepoints were defined – early (< 6 months) and late (> 6 months). As a subgroup analysis, MCID, PASS, and GRC rates were also compared between the decompression and fusion groups for patients with preoperative back pain < leg pain. This was done to assess if the demonstrated differences between decompression and fusion in patients with predominant back pain were actually specific to this particular patient cohort or could also be seen in patients with back pain < leg pain. Results: 510 patients were included. All analyses were done on 200 patients (120 decompression, 80 fusion) with preoperative VAS back > VAS leg. A subgroup analysis was done on 310 patients (196 decompression, 114 fusion) with preoperative VAS back < VAS leg. There were statistically significant improvements in all PROMs in both groups at < 6 and > 6 months compared to preoperative with no significant difference in the magnitude of improvement between the groups. The fusion group, however, showed significantly higher MCID achievement rates for VAS back at < 6 months (85% vs. 70%, p = 0.02) and ODI at > 6 months (67% vs. 51%, p = 0.04). Proportion of patients achieving PASS and feeling better after surgery based on response to GRC showed no difference between the two groups. The subgroup analysis for decompression versus fusion in patients with preoperative back pain < leg pain showed no differences in MCID, PASS, or GRC rates. Conclusion: In patients with predominant back pain, minimally invasive decompression alone had significantly less MCID achievement rates in VAS back at < 6 months and ODI at > 6 months compared to fusion. However, decompression alone led to an overall significant improvement in PROMs, similar PASS achievement rates, and similar responses on the GRC scale. Back pain alone, therefore, should not preclude a patient from undergoing laminectomy without fusion but act more as a reminder for appropriate patient selection and adequate counseling before surgery.
1606
P228: Impact of age on outcomes of decompression alone versus fusion for L4-5 degrative spondylolisthesis
Pratyush Shahi 1 , Sumedha Singh 1 , Kyle Morse 1 , Tomoyuki Asada 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Kasra Araghi 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Evan Sheha 1 , James Dowdell 1 , Todd Albert 1 , Harvinder Sandhu 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Although there is good data in the literature on the topic of decompression alone versus fusion for degenerative lumbar spondylolisthesis (DLS), no study has been conducted examining the possible impact of age on the comparison of outcomes after the two surgeries. This is despite the fact that age is a common factor determining the choice of surgery for DLS, as demonstrated by multiple previous studies. The objective of this study was to compare the outcomes of decompression alone and fusion for DLS in two different age cohorts (< 70 years, > 70 years) and assess if age impacts how the two surgeries fare against each other. Material and Methods: This retrospective cohort study included patients who underwent minimally invasive decompression or fusion for L4-5 DLS and had a minimum of 1-year follow-up. Outcome measures were: 1) patient-reported outcome measures (PROMs) (Oswestry Disability Index, ODI; Visual Analog Scale back and leg, VAS; 12-Item Short Form Survey Physical Component Score, SF-12 PCS), 2) minimal clinically important difference (MCID), 3) patient acceptable symptom state (PASS), and 4) response on the global rating change (GRC) scale. Two postoperative timepoints were analyzed – early (< 6 months) and late (> 6 months). The decompression and fusion groups were compared for outcomes separately in the < 70-year and > 70-year age cohorts. As a secondary analysis, the < 70-year and > 70-year age cohorts were also compared for outcomes, irrespective of the surgery type. Results: 233 patients were included, out of which 52% were < 70 years. 22% and 54% of patients < 70 years and > 70 years, respectively, underwent decompression alone. Analysis of the < 70-year age cohort showed non-significant improvement in SF-12 PCS at < 6 and > 6 months but significant improvement in other PROMs after decompression. The fusion group showed significant improvement in all PROMs at both timepoints. Patients < 70 years who underwent decompression also showed significantly lower MCID achievement rates for VAS back at < 6 months (50% vs 72% after fusion, p = 0.02) and > 6 months (47% vs 76% after fusion, p = 0.02) compared to fusion. MCID achievement rates for other PROMs, PASS achievement rates, and responses on the GRC scale did not show any significant differences. Analysis of the > 70-year age cohort showed that both decompression and fusion groups attained significant improvement in all PROMs at < 6 and > 6 months compared to the preoperative baseline with no significant difference in the magnitude of improvement between the two groups. MCID achievement rates for all PROMs, PASS achievement rates, and responses on the GRC scale did not show any significant differences between the decompression and fusion groups. When analyzed irrespective of the surgery type, both < 70-year and > 70-year age cohorts showed significant improvement in PROMs with no significant difference in the magnitude of improvement, MCID/PASS achievement rates, and responses on GRC. Conclusion: Patients < 70 years undergoing decompression alone did not show significant improvement in physical function and had significantly less MCID achievement rate for back pain compared to fusion. Patients > 70 years, on the other hand, showed no difference in outcomes between decompression alone and fusion.
1617
P229: Carbon fiber reinforced-polyetheretherketone (CFR-PEEK) instrumentation in degenerative disease of lumbar spine: a pilot study
Riccardo Ghermandi 1 , Giovanni Tosini 1 , Alberto Lorenzi 2 , Cristiana Griffoni 1 , Luigi La Barbera 3 , Marco Girolami 1 , valerio pipola 1 , Giovanni Barbanti Bròdano 1 , Stefano Bandiera 1 , Silvia Terzi 1 , Giuseppe Tedesco 1 , Gisberto Evangelisti 1 , Annalisa Monetta 1 , Luigi Emanuele Noli 1 , Luigi Falzetti 1 , Alessandro Gasbarrini 1
1 Department of Spine Surgery, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
2 Ortopedia e Traumatologia 3 ad indirizzo Chirurgia Vertebrale, AOU Città della Salute e della Scienza (Presidio CTO), Turin, Italy
3 Department of Chemestry, Materials and Chemical Engineering “G. Natta”, Laboratory of Biological Structure Mechanics, Politecnico di Milano, Milano, Italy
Introduction: CFR-PEEK is gaining popularity in spinal oncological applications due to the reduction of imaging artifacts and radiation scattering compared to titanium, which allows for better oncological follow-up and efficacy of radiotherapy. We evaluated the use of these materials also for the treatment of lumbar degenerative diseases (DD), considering the biomechanical potential of the carbon fiber related to its modulus of elasticity similar to that of bone. Material and Methods: Twenty-eight patients with DD were treated using CRF-PEEK instrumentation. Clinical and radiographic outcomes at 12-month FU were collected. Spinal fusion was evaluated on CT scans by Brantigan score, while clinical outcomes were evaluated with VAS, SF12 and EQ-5D. Results: 90% of patients evaluated at the 12-month FU showed complete or almost certain fusion (Brantigan score D and E) and presented a significant improvement in all clinical parameters. No mechanical complications related to the implant were detected and the patients reported a better tolerance of the instrumentation compared to titanium. Conclusion: No other series of patients affected by DD stabilized with carbon fiber implants have been reported in the literature. The results of this pilot study indicate the efficacy and safety of these implants and support their use also for spinal degenerative diseases.
1620
P230: Clinical and radiological predictors of slower and non-improvement following surgical treatment of L4-L5 degenerative spondylolisthesis
Sumedha Singh 1 , Pratyush Shahi 1 , Tejas Subramanian 1 , Kyle Morse 1 , Avani Vaishnav 1,2 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Kasra Araghi 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Tomoyuki Asada 1 , James Dowdell 1 , Todd Albert 1 , Harvinder Sandhu 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Although studies have been conducted demonstrating good outcomes after surgical treatment and comparing decompression alone and fusion, there is very little data on non-improvement and its associated predictors following surgery for degenerative spondylolisthesis. Also, the concept of slower improvement has never been investigated. The objective of this study was to identify the predictors of slower and non-improvement following surgical treatment of L4-5 DLS. This is the first study assessing both clinical and radiological (X-ray, CT, and MRI-based) preoperative factors as predictor variables. Material and Methods: This retrospective cohort study included patients who underwent minimally invasive decompression or fusion for L4-5 degenerative spondylolisthesis and had a minimum of 1-year follow-up. Outcome measures were: 1) minimal clinically important difference (MCID), 2) patient acceptable symptom state (PASS), and 3) global rating change (GRC). Clinical variables analyzed for predictors were age, gender, body mass index (BMI), surgery type (decompression or fusion), comorbidities, American Society of Anesthesiologists (ASA) class, anxiety, depression, smoking, osteoporosis, and preoperative patient reported outcome measures (PROMs) (Oswestry Disability Index, ODI; Visual Analog Scale, VAS back and leg; 12-Item Short Form Survey Physical Component Score, SF-12 PCS). Radiological variables analyzed were slip percentage, translational and angular motion, facet diastasis, facet cyst, facet orientation, laterolisthesis, disc height, scoliosis, main and fractional curve Cobb angles, lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and PI-LL. Two postoperative timepoints were defined - early (< 3 months) and late (> 6 months). Regression analyses were performed to identify predictors for MCID and PASS non-achievement and the response of “not better compared to preoperative” on the GRC scale following surgery. Failure to achieve MCID or response of “not better” on GRC by 3 months was regarded as slower improvement whereas failure to achieve MCID/PASS or response of “not better” on GRC at 6 months or more was regarded as non-improvement. Results: 233 patients (37% laminectomy, 63% fusion) were included. At < 3 months, high PT (Odds ratio, OR 0.92; p 0.02) and depression (OR 0.28, p 0.02) were predictors of MCID non-achievement and GRC non-betterment, respectively. Neither retained significance at > 6 months and hence, were identified as predictors of slower improvement. At > 6 months, low preoperative VAS leg (OR 1.26, p 0.01) and high facet orientation (OR 0.95, p 0.03) were predictors of MCID non-achievement, high L4-5 slip percentage (OR 0.86, p 0.03) and L5-S1 angular motion (OR 0.78, p 0.01) were predictors of GRC non-betterment, and high preoperative ODI (OR 0.96, p 0.04) was a predictor of PASS non-achievement. Surgery type (laminectomy or fusion) was not statistically significant on univariate or regression analyses. Conclusion: High PT and depression were predictors of slower improvement and low preoperative leg pain, high preoperative disability, high facet orientation, high slip percentage, and L5-S1 angular motion were predictors of non-improvement following surgical treatment of L4-5 degenerative spondylolisthesis. Choice of decompression versus fusion did not seem to impact outcome after surgery.
1623
P231: Minimally invasive decompression alone versus fusion for L4-5 degenerative spondylolisthesis with translational motion
Sumedha Singh 1 , Pratyush Shahi 1 , Tejas Subramanian 1 , Kyle Morse 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Kasra Araghi 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Chad Simon 1 , Tomoyuki Asada 1 , Avani Vaishnav 1,2 , Evan Sheha 1 , James Dowdell 1 , Todd Albert 1 , Harvinder Sandhu 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, USA
Introduction: Translational motion is likely the most common parameter that influences surgical decision-making for degenerative lumbar spondylolisthesis (DLS) to favor a fusion procedure. Although it seems rational to fuse an unstable listhetic level, a decompression alone might be needed in some cases depending on the patient’s preference and surgical fitness. In addition, the role of translational motion in favoring fusion is mainly backed up by evidence focused on traditional open techniques and its applicability in the realm of minimally invasive spine surgery (MISS) has not been tested. We believe that this topic needs to be explored further in order to improve our understanding and fill this gap in the literature. The objective of this study was, therefore, to compare minimally invasive decompression alone and fusion for L4-5 DLS with translation motion > 2 mm. Material and Methods: This retrospective cohort study included patients who underwent minimally invasive decompression or fusion for L4-5 DLS with translational motion > 2 mm and had a minimum of 1-year follow-up. The following outcome measures were compared between the decompression and fusion groups: 1) patient-reported outcome measures (PROMs) (Oswestry Disability Index, ODI; Visual Analog Scale back and leg, VAS; 12-Item Short Form Survey Physical Component Score, SF-12 PCS), 2) minimal clinically important difference (MCID), 3) patient acceptable symptom state (PASS), and 4) response on the global rating change (GRC) scale. Two postoperative timepoints were analyzed – early (< 6 months) and late (> 6 months). Results: 84 patients with translation > 2 mm were included, out of which 60 (71%) underwent fusion. The decompression group had significantly higher average age compared to fusion (70.9 vs. 64.8 years, p = 0.001). There was no significant difference in the average translational motion between the two groups (decompression 2.95 + 1.57 mm, fusion 2.84 + 1.09 mm; p = 0.704). There was no significant difference between the groups in other demographic variables and preoperative PROMs. Both groups showed significant improvement in PROMs at < 6 and > 6 months compared to preoperative with no significant difference in the magnitude of improvement. Most patients achieved MCID for PROMs (> 50%) and PASS (decompression 67%, fusion 74%; p = 0.61) in both groups at both timepoints with no significant difference in the achievement rates between the two groups. > 80% of patients reported feeling better on the GRC scale at both timepoints with no significant difference in the responses between the two groups. There were no significant differences between the decompression and fusion groups in the intraoperative or in-hospital complication reoperation rates. The decompression group had 2 cases (8.3%) that required conversion to fusion due to failure of decompression. The fusion group had 2 cases (3.3%) that required reoperation due to pseudarthrosis and adjacent segment disease (ASD), respectively. Conclusion: The findings of this study suggest that minimally invasive decompression alone might lead to similar outcomes as fusion in patients with DLS and translational motion > 2 mm, up to 2 years. However, these are preliminary results in an older decompression-alone cohort and future research with larger sample size and longer follow-up is required to establish these findings.
1634
P232: Posterior lumbar interbody fusion using an unilateral cage: a case series of clinical outcome and stability in unilateral lumbar radiculopathy patients
Adhi Prayoga Ida Bagus 1
1 Orthopaedic, Bangkalan General Hospital, Bangkalan, Indonesia
Introduction: Posterior lumbar interbody fusion (PLIF) is a widely used surgical procedure that relieves pain and restores spinal instability resulting from various spinal pathologies while restoring disc height and supporting the anterior and middle columns. Nowadays, PLIF involving the insertion of bilateral interbody cages has been a standard treatment that restores segmental alignment and balance, but the procedure carries the risk of introducing bilateral nerve root injury or dural tearing because of the marked retraction of the nerve roots. Specifically, in patients with unilateral radiculopathy, minimal nerve root manipulation on the contralateral asymptomatic side should be considered. This group of patients would benefit from PLIF using a unilateral cage. The requirement of PLIF using a unilateral cage in such cases turn up the question of whether this procedure can provide acceptable balance, clinical outcome, and fusion. Material and Methods: Six patients from March 2020 – February 2022 that visited Bangkalan General Hospital – East Java were prospectively enrolled in this study, All the patient came with unilateral radiculopathy who underwent bilateral open pedicle screw fixation combined with a single fusion cage inserted on the symptomatic side for treatment of focal degenerative lumbar spine disease. Their clinical results, radiological parameters, and related complications were assessed 2 weeks, 3 months, and 12 months postoperatively. Results: Five patients showed good result in which the surgery restored the disc space height and maintained lumbar lordotic and scoliotic angles 12 months postoperatively and there was no excacerbation. They had excellent or good outcomes according to the modified MacNab’s criteria. The mean pain score according to the visual analogue scale was 6 preoperatively but had improved to 3 when reassessed 3 months postoperatively and was maintained as of 12 months postoperatively. Unfortunately for one patient, after 8 months postoperatively, Showed a worsening in symptoms due to adjacent segment disesase. Conclusion: In patients with unilateral radiculopathy, unilateral cage insertion followed by compact bone graft packing and bilateral percutaneous screw fixation can provide adequate mechanical construct that leads to good clinical and radiological outcomes. However, bone mineralization status of the patients must be evaluated carefully to prevent further complication.
1640
P233: Racial and ethnic disparities in outpatient microdiscectomy utilization: a comprehensive trends analysis using national and regional state data
Troy Amen 1 , Abhinaba Chatterjee 1 , Mihir Dekhne 1 , Tejas Subramanian 1 , Pratyush Shahi 1 , Avani Vaishnav 1,2 , Eric Mai 1 , Chad Simon 1 , Olivia Tuma 1 , Kasra Araghi 1 , Myles Allen 1 , Nishtha Singh 1 , Eric Kim 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Maximillian Korsun 1 , Tomoyuki Asada 1 , Cole Kwas 1 , Sheeraz Qureshi 1
1 Hospital for Special Surgery, New York, USA
2 Boston Medical Center, USA
Introduction: Although racial and ethnic disparities within spine surgery have been well documented, no data exists on disparities in outpatient procedures including lumbar microdiscectomy, one of the most performed procedures within spine surgery. The purpose of this study was to 1) assess disparities in the utilization of outpatient microdiscectomy amongst white, Black, and Hispanic patients on a national and state level and 2) trend these disparities over time to see whether they have improved, persisted, or worsened. Material and Methods: We conducted a retrospective cohort study using data from the 2015-2018 Healthcare Cost and Utilization Project (HCUP) New York State Ambulatory Surgery Database and the 2018 HCUP National Ambulatory Surgery Sample (NASS). Patients who underwent same-day discharge microdiscectomy were identified using common procedural codes. In our primary analysis, differences in per-capita utilization rates of same-day outpatient microdiscectomy were assessed and trended over time by race and ethnicity using the New York statewide data. Poisson regression was used to evaluate the association between utilization rates for microdiscectomy and race/ethnicity after adjustment for age, insurance, socioeconomic status, and comorbidities. Results: During the study period, Black and Hispanic patients were significantly less likely to undergo outpatient microdiscectomy when compared to white patients in New York state (adjusted rate ratio [aRR], 0.26; 95% Confidence Interval [CI], 0.25-0.27; p < 0.001). This disparity was also observed at the national level (white vs. Black vs. Hispanic OP-microdiscectomy rate per million person-years: 408.7 vs. 148.5 vs. 129.8), with disparities being most pronounced in the Midwest and South (p < 0.001 for both). From 2015 to 2018, there was a persisting disparity in microdiscectomy utilization for Black patients over time (e.g. white vs. Black OP-microdiscectomy rate per million person-years: 443.4 vs. 115.3 in 2015 compared with 383.2 vs. 106.1 in 2018, P trend < 0.001) and an improving disparity for Hispanic patients over time (e.g. white vs. Hispanic OP-microdiscectomy rate per million person-years: 443.4 vs. 115.3 vs. 74.1 in 2015 compared with 383.2 vs. 106.1 vs. 115.1 in 2018, P for trend < 0.001). These results held in adjusted Poisson regression models. Conclusion: In this study, we found evidence of racial and ethnic disparities in outpatient microdiscectomy utilization between white, Black, and Hispanic patients both on a national and state level. Racial and ethnic disparities in microdiscectomy utilization on the national level across the USA were most pronounced in the Midwest and South. Disparities on the state level, specifically New York state, were found to be improving between white and Hispanic patients over time. These encouraging trends in New York may reflect the effectiveness of several governmental legislative enactments within the state that have encouraged the emergence of hospital affiliated outpatient centers and free-standing ASCs in rural and underserved areas. Further research is needed to see if these trends have also held in other states and on a national level and why trends have not also simultaneously improved for Black patients.
1647
P234: Are lumbar disc re-herniations common: incidence and long term outcomes
Melissa Baker 1 , Evan Chaladoff 1 , Alex LaPoche 2 , Michael Gerling 1,3 , Zorica Buser 1,3
1 Gerling Institute, New York, USA
2 SUNY Downstate College of Medicine, Brooklyn, USA
3 Orthopedic Surgery, NYU Grossman School of Medicine, New York, USA
Introduction: Lumbar disc herniations are a frequent cause of low back pain and radiculopathy, impacting a substantial portion of the population. While lumbar discectomy is a common and effective treatment, clinical evidence regarding the possibility of re-herniations and the impact on patients is limited. The aim of the current study is to determine the rate of re-herniations, the need for revision surgery, and their relationship with clinical outcomes, providing essential insights into the long-term management of lumbar disc herniation patients. Material and Methods: This was a retrospective single-center study of patients who underwent revision surgery after undergoing a single or multi-level discectomy between 2020 and 2022. Demographic data (age, gender, ASA grade, smoking status), history of epidural steroid injections, radiographic parameters, and intraoperative variables were recorded. Data on new-onset postoperative complications was collected. Data on revision surgery, post-operative complications, pre- and post-operative PROs (VAS, and ODI) were collected at various time points up to one year. Paired sample two-tailed t-test and multivariate regression with p < 0.05 being significant will be utilized. Results: The current study included 234 patients who underwent single or multi-level endoscopic or tubular lumbar discectomy between 2020 and 2022. 168 of the discectomies were performed at a single level (71.8%), 64 at two-levels (27.4%), and 2 at three levels (0.8%). 158 (67.5%) patients were male, with the average age being 42.6 ± 11.0 years. Of the 234 patients who underwent discectomy surgery, 36 (15.4%) underwent lumbar revision surgery. 26 (72.2%) revision patients underwent Transforaminal Lumbar Interbody Fusion (TLIF) and 4 underwent Posterior Spinal Fusion (PSF). The rest included SI fusion or decompression. 6 patients (17% of revisions) required revision surgery that included at least one additional level not previously operated on in the index surgery. The average time between Index and Revision surgery was 417.1 ± 161.9 days. 27 revisions (75%) were single-level procedures and 7 (19%) were two-level (2 were SI Joint Fusions). The average pre-index surgery Visual Analogue Scale (VAS) score for the lower extremities reported was 7.7 ± 2.1. Patients reported improvement in VAS at 3-month post-index surgery (5.7 ± 3.3). However, at the time of revision surgery VAS score was 6.8 ± 3.3. The pain improvement was seen after the revision with 1-year values of 5.6 ± 3.4. Patients who underwent revision surgery did not show improvements in ODI scores before and after the index surgery (0.56 ± 0.16 and at 3-month post-op 0.57 ± 0.24). The ODI values remained at the similar level after the revision procedure up to 1 year posy-op 0.52 ± 0.11. Conclusion: In the current study 15.4% of the patients with disc herniation had revision surgery. The reason for revision was re-herniation and the most common revision procedure was a TLIF. Patients who had revision surgery reported improvement in VAS leg pain scores, however the ODI values did not change. The relationship between the revision surgery and disc herniation size and location will be evaluated, including the predictiveness with reported outcomes.
1649
P235: The effect of paravertebral muscle mass on lumbar lordosis after posterior decompression surgery
Teeto Ezeonu 1 , Michael McCurdy 1 , Alexa Tomlak 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Sebastian Fras 1 , Sydney Somers 1 , Akshay Khanna 1 , Anthony Labarbiera 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Gregory Schroeder 1
1 Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: Lumbar lordosis is an essential component of sagittal alignment that allows for adequate balance of the compressive forces of gravity. Restoration of lumbar lordosis following spine surgery has significant implications for clinical outcomes. While the association between sarcopenia and poor postoperative outcomes has been established, there is a paucity of literature exploring the impact of sarcopenia on sagittal alignment after spinal surgery. The purpose of this study is to determine the effect of paravertebral muscle mass on lumbar lordosis correction after posterior lumbar decompression surgery. Materials and Methods: Upon obtaining IRB approval, patients > 18 years old who underwent primary 1-2 level posterior lumbar decompression (PLD) without fusion during 2018-2022 were retrospectively identified. Preoperative and postoperative radiographs were reviewed by blinded research personnel. The sagittal parameters included lumbar lordosis (LL), sacral slope (SS), and pelvic tilt (PT). Pelvic incidence (PI = PT+SS) and pelvic incidence minus lumbar lordosis (PI-LL) were also calculated. Muscle quality measures included psoas area, normalized total psoas area (NTPA), paravertebral muscle (PVM) area, paravertebral muscle/body mass index (PVM/BMI), and Goutallier grade. The cohort was divided into 3 equal groups based on PVM/BMI, which accounted for body size. The cohort was also stratified based on achievement of PI-LL < 10°. Results: We identified 143 patients who underwent posterior lumbar decompression surgery without fusion. Patients in the small muscle size group were more likely to be female (64.6% vs. 35.4% vs. 25.5%, p = 0.001) and have larger BMIs (35.0 vs. 27.6 vs. 26.4, p < 0.001). Patients in the smallest muscle size group were more likely to have higher Goutallier grade (1.96 vs. 1.33 vs. 1.30, p = 0.004). LL was highest in patients in the largest muscle size group preoperatively (30.0 vs. 32.1 vs. 35.2, p = 0.003) and postoperatively (47.8 vs. 50.5 vs. 53.6, p = 0.026). SS was highest in patients in the largest muscle size group preoperatively (30.0 vs. 32.1 vs. 35.2, p = 0.003) and postoperatively (31.7 vs. 33.0 vs. 36.1, p = 0.015). There was no difference in the proportion of patients with PI-LL < 10° preoperatively (50.0% vs. 70.8% vs. 70.2%, p = 0.082) or postoperatively (56.2% vs. 70.8% vs. 68.1%, p = 0.379). Multivariate logistic regression analysis demonstrated that a higher PVM/BMI was a predictor of greater preoperative LL (est. = 0.05, p = 0.039) and postoperative LL (est. = 0.06, p = 0.031). Furthermore, higher Goutallier grade was associated with decreased SS preoperatively (est. = -1.85, p = 0.006). Discussion: This analysis showed that smaller muscle mass is associated with the smallest degree of lumbar lordosis before and after posterior lumbar decompression. Interestingly, patients with the smallest muscle mass were more likely to have larger BMIs and a greater degree of fatty degeneration. These findings highlight the role of BMI and body fat, in particular, in sagittal alignment parameters.
1653
P236: Evaluating the impact of lumbar bracing on patient-reported outcomes measures after one and two-level posterior lumbar decompression & fusion and transforaminal interbody lumbar fusion surgery
Olivia Opara 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Adam Kohring 2 , Otitochukwu Ezeonu 1 , Nicholas Pohl 1 , Preston Carey 3 , Quinn Kirkpatrick 3 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Orthopaedics, Rothman Orthopaedic Insitute, Philadelphia, USA
2 Orthopaedics, Rowan University, Philadelphia, USA
3 Thomas Jefferson University, Philadelphia, USA
Introduction: The use of postoperative bracing after spine fusion surgery is not consistent amongst providers in clinical practice. Among some orthopaedic spine surgeons, the efficacy and indications of these devices after lumbar fusion surgery remains controversial. This study aims to assess the effect of bracing on patient-reported outcome measures (PROMs) after one and two-level posterior lumbar decompression fusion (PLDF) and transforaminal lumbar interbody fusion (TLIF) surgery. Material and Methods: Retrospective analysis of patients from a single tertiary-referral care center who underwent 1-2 level PLDF/TLIF with or without bracing between 2015-2020 were identified. Patients were grouped into brace use and no brace. Patient demographics, surgical characteristics, and outcomes were collected from the electronic medical records. Patients with braces were identified from chart review, and the type of lumbar brace administered was an off-the-shelf Lumbar Sacral Orthosis (LSO). Patient-reported outcome measures (PROMs) were collected at baseline, 3, 6, and 12 months postoperatively. PROMs included VAS-back/leg score, Oswestry Disability Index (ODI), Mental health Component Score (MCS-12), and Physical Component Scores (PCS-12). ΔPROMS score was calculated by subtracting preoperative from postoperative values. Bivariate analysis was performed based on groupings, and multivariate linear regression was used to identify factors independently associated with ΔPROMs. All statistical analyses were performed using RStudio Version 4.0.2 (Boston, MA), with P values < 0.05 considered statistically significant. Results: Of the 170 identified, 83 patients were treated with no brace, and 87 were treated with a brace. There was no significant difference in revisions within 60 days and less than 90-day readmissions (p = 1.000) among patients in both groups. Compared to the no-bracing group, patients treated with bracing demonstrated a significant increase in the 1-year MCS-12 postoperatively (48.3 vs. 51.8 p = 0.032). When accounting for significant predictors in the multi-regression analysis, bracing had no considerable effect on ΔPROMS at three months (ODI, VAS Back, VAS Leg, PCS, and MCS). However, consistent with bivariate analysis, multivariate linear regression of 1-year ΔPROMs identified bracing as an independent predictor of improved MCS-12 scores (β = 5.08, 95% CI: 0.13 to 10.02, p = 0.044). Conclusion: Our findings suggest that postoperative bracing following 1-2 level PLDF and TLIF surgery did not have any significant effect on PROMS except for MCS-12 at one year. This may imply that bracing may have a potential psychosomatic benefit for certain patients at one year following surgery.
1661
P237: Commonly used patient-reported outcome measures (PROMs) do not adequately reflect patient-perceived changes in health status following lumbar microdiscectomy
Avani Vaishnav 1,2 , Jung Kee Mok 2 , Joshua Zhang 2 , Myles Allen 2 , Cole Kwas 2 , Eric Kim 2 , Nishtha Singh 2 , Chad Simon 2 , Olivia Tuma 2 , Eric Mai 2 , Kasra Araghi 2 , Tomoyuki Asada 2 , Maximillian Korsun 2 , Yeo Eun Kim 2 , Sravisht Iyer 2 , Sheeraz Qureshi 2
1 Boston Medical Center, USA
2 Hospital for Special Surgery, New York, USA
Introduction: In recent years there has been a growing focus on patient-reported outcome measures (PROMs) as important metrics in spine surgery. Numerous outcome measures have been developed and validated in spine surgery, but there is relatively little data on how these PROMs correlate with changes in patients’ overall perception of health status. This study aimed to determine the correlation between various PROMs and perceived changes in spine-related health status in patients undergoing lumbar microdiscectomy. Material and Methods: This was a retrospective review of prospectively collected data on consecutive patients who underwent ACDF at a single academic institution between April 2017 and February 2023. Various PROMs, including Neck Disability Index (NDI), Visual Analogue Scale (VAS) for neck and arm pain, Short-Form 12 (SF-12 PCS/MCS) and patient reported outcomes measurement information system physical function (PROMIS-PF), were collected at the preoperative visit and postoperatively at 6 weeks, 12 weeks, 6 months, and 1 year. Patients also completed a ‘Global Rating Change (GRC)’ questionnaire, a 5-item Likert Scale (‘much better’, ‘slightly better’, ‘about the same’, ‘slightly worse’, ‘much worse’) which addressed how a patient’s spine condition compared to preoperatively and to their prior visit. Spearman correlation coefficient (Rho) was used to determine the correlation between changes in PROMs and GRC. Results: This study included 397 patients with a mean age of 48.4 years, mean BMI of 26.8 kg/m2, and comprised of 59.7% males. A majority of patients underwent one-level microdiscectomy (97%) and were discharged on the day of surgery (74.9%). The percentage of patients feeling ‘much better’ compared to pre-operatively was 70% at 6 weeks, 74% at 12 weeks, 76.1% at 6 months, and 80.8% at 1 year. Less than 4% of patients reported feeling ‘much worse’ compared to pre-operatively at all time points. Changes in PROMs from pre-operatively demonstrated a statistically significant correlation with GRC at all time-points for ODI, VAS Back, VAS Leg, SF-12 PCS, and PROMIS-PF, and three out of four time-points for SF-12 MCS. The strengths of the correlations were weak-to-moderate (Spearman’s Rho range: 0.198 to 0.514). Changes in PROMs compared to the previous visit demonstrated statistically significant correlation with GRC at all time points for ODI, VAS Back, SF-12 PCS, and PROMIS-PF, and two out of three time-points for VAS Leg. The strength of the correlations were very weak-to-weak (Spearman’s Rho range: 0.195 to 0.327). Conclusion: The results of this study showed that a majority of patients undergoing lumbar microdiscectomy experienced notable improvement in the early post-operative period. Furthermore, patients continue to have improvements at longer follow-ups, with approximately 60% of patients reporting feeling much better at 1 year compared to 6 months. However, commonly utilized PROMS demonstrated weak-to-moderate correlation with perceived changes in overall spine-related health status from preoperatively to postoperatively, and very weak-to-weak correlation with postoperative changes. These findings suggest that currently used PROMs may not be as sensitive at detecting these changes, or may not be adequately reflecting changes in health condition that are meaningful to patients.
1662
P238: Exploring the association between inpatient physical therapy and outcomes after lumbar fusion surgery
Teeto Ezeonu 1 , Jeremy Heard 1 , Michael McCurdy 1 , Michael Carter 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Jeffrey Zucker 1 , Akshay Khanna 1 , Yoni Dulitzki 1 , Dylan Resnick 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Gregory Schroeder 1
1 Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: Previous studies have emphasized the role of early ambulation in postoperative spine patients as an effective method for improving pain scores and decreasing length of stay. Despite the current body of literature supporting the use of postoperative physical therapy as a strategy to encourage postoperative ambulation, discrepancies in reported outcomes exist. Thus, the purpose of this study is to investigate how inpatient physical therapy outcomes, as a proxy for postoperative ambulation, affects outcomes after lumbar spine surgery. Materials and Methods: Upon obtaining IRB approval, all patients > 18 years old who underwent primary single-level posterior lumbar decompression and fusion from 2019-2020 at a single academic institution were retrospectively identified. Physical therapy data including time to first inpatient PT session, gait trial distance achieved, post-treatment pain rating and Activity Measure for Post-Acute Care (AM-PAC) scores were collected using manual chart review. Outcome variables included length of stay, inpatient complications, 90-day readmissions, and reoperations within 1 year of primary surgery. Parametric data were analyzed with independent t-tests, while non-parametric data were analyzed using Mann-Whitney U tests. Multivariate logistic regressions were run using a stepwise function to identify the strongest modest that could be used to predict inpatient complications, 90-day readmissions, 1-year reoperations, and length of stay. Statistical significance was set at p < 0.05. Results: A total of 425 patients (48.2% female) were included in this analysis. On average, patients in the study cohort had their first physical therapy session within 15.0 ± 10.5 hours of surgery. Almost all patients attended their first PT session within 24 hours of surgery (90.1%), while a smaller portion had their first session within 6 hours of surgery (35.5%). Forty-nine patients (11.5%) experienced an inpatient complication. There was no difference in hours to PT or total gait trial distance achieved between patients who experienced a complication and those that did not. Patients in the non-complication group had higher AM-PAC scores than patients in the complication group (17.7 ± 2.56 vs. 16.3 ± 2.92, p = 0.023). There were 20 readmissions (4.71%) within 90 days of surgery and 15 revision surgeries (3.53%) within 1 year of surgery. There was no difference with regards to time to PT, AM-PAC score, or gait trial distance achieved between readmitted patients and non-readmitted patients or revision patients and non-revision patients. Stepwise logistic regression showed that having a physical therapy session within 6 hours of surgery was predictive of a decreased length of stay both in patients who had an inpatient complication (est. = -0.70, Confidence Interval (CI): -1.08- -0.32, p < 0.001) and those that did not (est. = -0.73, CI:-1.12 - -0.33, p < 0.001). Discussion: This analysis showed that a shorter time to inpatient physical therapy was not associated with a difference in inpatient complications, 90-day readmissions or one-year reoperations. Nevertheless, time to physical therapy was an independent predictor of hospital length of stay. Thus, while inpatient physical therapy within 6 hours of surgery does not appear to impact surgical outcomes, surgeons should encourage early ambulation postoperatively to decrease extended hospital stays and cut down on unnecessary medical costs.
1679
P239: Commonly used patient-reported outcome measures (PROMs) do not adequately reflect patient-perceived changes in health status following lumbar decompression
Avani Vaishnav 1,2 , Jung Kee Mok 2 , Myles Allen 2 , Olivia Tuma 2 , Chad Simon 2 , Eric Mai 2 , Maximillian Korsun 2 , Tomoyuki Asada 2 , Eric Kim 2 , Yeo Eun Kim 2 , Nishtha Singh 2 , Cole Kwas 2 , Joshua Zhang 2 , Kasra Araghi 2 , Sravisht Iyer 2 , Sheeraz Qureshi 2
1 Boston Medical Center, USA
2 Hospital for Special Surgery, New York, USA
Introduction: In recent years there has been a growing focus on patient-reported outcome measures (PROMs) as important metrics in spine surgery. As a result, they are increasingly being utilized to assess healthcare expenditure, determine compensation and evaluate cost-effectiveness. However, there is little data on whether changes in PROMs correlate with patients’ perceptions of improvement. Thus, the purpose of this study was to assess the correlation between patient perceived changes in health and commonly utilized PROMs in patients undergoing lumbar decompression surgery. Material and Methods: We performed a retrospective review of prospectively collected data on consecutive patients who underwent lumbar decompression at a single academic institution between April 2017 and February 2023. PROMs, including Oswestry Disability Index (ODI), Visual Analogue Scale (VAS), Short-Form 12 (SF-12 PCS/MCS), and PROMIS physical function (PROMIS-PF), were prospectively completed by patients pre-operatively and at 6 weeks, 12 weeks, 6 months and 1 year postoperatively. In addition, at each post-operative visit patients completed a ‘Global Rating Change (GRC)’ question, which assessed how the patient’s spine condition compared to before surgery and to their previous visit. This was assessed using a 5-item Likert Scale (‘much better’, ‘slightly better’, ‘about the same’, ‘slightly worse’, ‘much worse’). Spearman correlation coefficient (Rho) was used to assess the correlation between change in PROMs and GRC. Results: This study included 965 patients with a mean age of 59.1 years, mean BMI of 27.5 kg/m2, and comprised of 61% males. Most patients underwent one-level surgery (82.5%) and were discharged on the day of surgery (62.6%). The percentage of patients feeling ‘much better’ compared to pre-operatively was 66.6% at 6 weeks, 70.5% at 12 weeks, 71.7% at 6 months, and 71.1% at 1 year. Less than 3% of patients reported feeling ‘much worse’ compared to pre-operatively at all time points. Changes in PROMs from pre-operatively demonstrated a statistically significant correlation with GRC at all time-points for all PROMs. The strengths of the correlations were weak-to-moderate (Spearman’s Rho range: 0.201 to 0.556). Changes in PROMs compared to the previous visit demonstrated statistically significant correlation with GRC at all time points for ODI, VAS Back, SF-12 PCS, and PROMIS-PF, two out of three time-points for VAS Leg, and one time-point for SF-12 MCS. The strengths of the correlations were very weak-to-weak (Spearman’s Rho range: 0.101 to 0.301). Conclusion: The results of this study showed that a majority of patients undergoing lumbar decompression experienced notable improvement in the early post-operative period. Furthermore, patients continue to have improvements at longer follow-ups, with approximately 50% of patients reporting feeling much better at 1 year compared to 6 months. However, commonly utilized PROMS demonstrated weak-to-moderate correlation with perceived changes in overall spine-related health status from preoperatively to postoperatively, and very weak-to-weak correlation with postoperative changes. These findings suggest that currently used PROMs may not be as sensitive at detecting these changes, or may not be adequately reflecting changes in health condition that are meaningful to patients.
1682
P240: Neurological outcomes after anterior decompression and and stabilization with cage in tuberculosis spinein thoracilumbar spine
Atif Ali 1
1 Orthopaedic and Spine, Ghurki Trust Teaching Hospital Lahore, Lhore, Pakistan,
Background: Tuberculous spondylitis being endemic in developing countries including Pakistan has considerable socio-economic and orthopaedic concern. In spite of all the advances regarding diagnosis, treatment and total control of many diseases, this slow but grave disease still aff ects considerable number of cases and makes them disabled and even paralyzed. Objective: The objective of the study was to determine the neurological outcome in terms of the Frankel Scale aft er anterior decompression and stabilization with a titanium mesh cage in the thoracolumbar caries spine. Methodology: The case series (descriptive) study was conducted in the Orthopaedic ward of Ghurki Trust Teaching Hospital/Lahore Medical & Dental College, Lahore from 1st Jan. 2015 to 31st Dec. 2015. In this randomized controlled trial of 150 patients who were admitt ed either through OPD or through emergency. Data was collected by using a non-probability consecutive sampling technique. The patient was prepared for surgery. A locally made fixed interbody Titanium Mesh Cage, with packed bone graft, was placed. A Boston brace was applied for at least 6 months to provide external support to the spine. Th e neurological outcome was assessed in terms of the Frankel Scale post-operatively at the end of one month, 6 months, and 12 months. Results: In our study, out of 150 cases, 42% (n = 63) were between 15-30 years of age while 58% (n = 87) were between 31-60 years of age, mean+sd was calculated as 32.85 ± 8.35 years, 45.33% (n = 68) were male and 54.67% (n = 82) were females. The frequency of neurological outcome regarding improvement was recorded as 52% (n = 78). Conclusion: We concluded that the neurological outcome in terms of Frankel Scale aft er anterior decompression and stabilization with titanium mesh cage in thoracolumbar caries spine is good and this technique may be used in future in our population.
Keywords: tuberculous spondylitis, caries spine, anterior decompression, titanium mesh cage, neurological outcome, Boston brace, Frankel Scale, neurological outcome
1698
P241: Titanium coated PEEK interbody fusion devices alleviate risk to fusion for patients with comorbidities
Madilyn Riegel 1 , Jillian Mohn 1 , Matthew Gary 2 , Joseph Lee 3 , Safdar Khan 4 , Elizabeth Yu 5 , Benjamin Chen 6 , Hallie Murray 1
1 LLC, Clinical Affairs, Tyber Medical, Bethlehem, USA
2 Spine Surgery, Emory University, Atlanta, USA
3 Orthopaedic Spine Surgery, Rothman Orthopedics, Harrison, USA
4 Orthopaedic Spine Surgery, The Ohio State University, Dublin, USA
5 Orthopaedic Spine Surgery, The Ohio State University, Columbus, USA
6 Orthopaedic Spine Surgery, Multicare Institute of Research and Innovation, Puyallup, USA
Introduction: Bone healing is influenced by biological, mechanical, and systematic factors that make up a complex process. Growing evidence shows that comorbidities including smoking and obesity can cause delays or inhibit bone healing. Porous titanium coated polyether-ether-ketone (ProTi) interbody fusion devices have been designed to encourage osseointegration and have been shown to accelerate bony deposition in a pre-clinical model. Therefore, the objective of this research is to examine whether ProTi devices can alleviate the risks to fusion for patients with underlying comorbidities, including smoking and obesity, to support successful clinical and radiographic outcomes. Material and Methods: Institutional Review Board approval was obtained to gather clinical and radiographic outcomes for patients undergoing single or multi-level transforaminal or posterior lumbar interbody fusion procedures with ProTi devices for the treatment of degenerative lumbar conditions. Patients were stratified for the presence and/or absence of bone healing risk factors, including smoking and obesity, and evaluated for fusion outcomes, time to fusion, and the Oswestry Disability Index (ODI) and the Visual Analog Scale (VAS) in a subset of patients to determine the differences in outcomes with and without comorbidities. Patients were divided into the following groups: smokers (former and current), non-smokers, obese, overweight, and normal weight. Results: All patients (N = 21) demonstrated solid bony fusion with radiographic outcomes displaying bone bridging across the interbody space with the ProTi device. Average time to fusion for all patients was 10.69 ± 4.91 months with fusion rates being consistently similar amongst each group. Return to normal activity was also substantially the same amongst the groups (range 6.5 to 9.41 months). VAS pain scores for smoking and non-smoking groups revealed that both groups had pain alleviation from pre-operative to postoperative. Non-smokers achieved significant improvement in ODI (p = 0.02), VAS back (p = 0.01), and VAS right leg (p = 0.02) pain scores. Former smokers demonstrated improvement in ODI, VAS back, and VAS right leg from preoperative to postoperative but the improvement was not statistically significant. Although normal BMI patients did not provide patient reported outcomes, obese and overweight patients demonstrated significant improvement in ODI (p = 0.04), VAS back (p = 0.006), and VAS right leg (p = 0.02) pain scores from preoperative to final visit. These results demonstrated the ability of ProTi devices to successfully alleviate pain and provide solid bony fusion in a comparable manner regardless of the patient's smoking status or BMI. Conclusion: This preliminary analysis for this on-going study was the first to evaluate ProTi interbody fusion device’s performance in patients with bone healing risk factors, including smoking and obesity. Study results demonstrated similar time to fusion and return to normal activity in patients with and without risk factors. Additionally, patients with and without comorbidities reported alleviation of pain and restoration of functionality. While additional research is needed to fully evaluate the performance of ProTi devices in patients with comorbidities, this study shows that ProTi devices can alleviate bone healing risks. Furthermore, it is important to educate patients on the risks associated with smoking and obesity on bone healing to support the best clinical outcomes.
1766
P242: Does clinical and magnetic resonance imaging characteristics predict Oswestry Disability Index in a symptomatic patient with single level disc herniation?
Dipak Shrestha 1 , Suman Lamichhane 1 , Bikash Parajuli 1 , Jagadish Thapa 1 , Sabik Kayastha 1
1 Dept. of Orthopedics, Dhulikhel Hospital, Kathmandu University Hospital, KUSMS, Dhulikhel, Nepal
Introduction: Magnetic resonance imaging (MRI) findings in a patient with lumbar disc herniation has been poorly correlated with low back pain and functional disability. However, clinical characteristics and MRI characteristics of disc herniation together has not been studied sufficiently to predict functional outcome in patient with symptomatic patient lumbar disc herniation. The present study aims to assess the relationship of clinical characteristics and MRI findings to functional disability (ODI) in patients with single level lumbar disc herniation. Material and Methods: One hundred and five Individuals of age ≥ 18 years with a single level lumbar disc herniation with clinical sign and symptoms of disc herniation presented between August 2022 to July 2023 were included. Michigan State University (MSU) classification, Pfirrmann Grade, Pathological Grade, Disc migration, High-Intensity Zones (HIZs) and Modic changes were included in MRI characteristics. Oswestry Disability Index (ODI) was used to assess the functional status of the patient at the time of presentation. The ODI score was transformed in normal distribution and Spearman correlation test was applied to evaluate the correlation of the demographic, clinical and MRI characteristics of the patients. Variables showing significant correlation with the normalized ODI score were put into the hierarchical regression model to evaluate the predictors of ODI. Results: There was an equal distribution of males (49.5%) and females (50.5%) with a median age of 37 (IQR 30-42). Majority (37.1%) were in the age group (31-40) years. Majority (87.6%) had radiating leg pain followed by back pain (63.8%). L5S1 disc herniation was found in 55.2%. The median ODI score was 44 (IQR: 28-63). Regression analysis revealed clinical factors being the most predictive of functional disability; motor deficit and presence of neurogenic claudication being the most predicting clinical factors (p < 0.01). Among the MRI characteristics, higher Michigan State University (MSU) grade of herniation was the only predicting variable for functional disability. Conclusion: Motor deficit and presence of neurogenic claudication are the most predicting clinical characteristics for functional disability among patients with single level disc herniation. Similarly, MSU Grade of disc herniation is the only predicting MRI variable for functional disability. Other MRI characteristics such as degeneration, Modic changes, HIZs, migration do not appear to influence the Oswestry Disability Index.
1770
P243: Investigating the association between disc herniation morphology and lumbar muscle quality
Teeto Ezeonu 1 , Jeremy Heard 1 , Olivia Opara 1 , Nicholas Pohl 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Meera Kohli 1 , John Bodnar 1 , Hamd Mahmood 1 , Anthony Labarbiera 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1
1 Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: Lumbar disc herniation is one of the most common causes of low back pain and is one of the leading causes of years lived with disability globally. While symptoms may resolve with conservative treatment measures, some patients will ultimately require a microdiscectomy procedure. There is evidence to suggest that the mechanics of low muscle mass and fatty degeneration may have significant implications for the natural history of spine pathology. However, no prior studies have investigated the implications of poor muscle quality as it relates to disc herniation morphology. Therefore, the aim of this study was to determine whether an association exists between muscle mass and quality and disc herniation morphology. Materials and Methods: Upon obtaining Institutional Review Board approval, patients > 18 years with disc herniations treated with microdiscectomy or epidural steroid injection (ESI) from 2020-2021 at a single academic institution were retrospectively identified. Preoperative MRIs were evaluated by two independent reviewers to assess disc herniation morphology and muscle quality. Herniation variables included herniation size (mm2), canal area (mm2), percent (%) canal compromise and Pfirrmann grade. Muscle quality measures included total psoas area (mm2), normalized total psoas area (NTPA) (mm2/m2), paralumbar muscle area (PL-CSA) (mm2) and Goutallier grade. Patients were grouped based on severity of canal compromise and disc herniation size for analysis. Those with % canal compromise < 33.3% were grouped in the ‘Mild’ group and those with % compromise > 33% were grouped in the ‘Moderate/Severe’ group. Patients were classified based on disc herniation size by dividing the cohort into equal thirds (‘Mild’, ‘Moderate’, ‘Severe’). Results: We identified 391 patients (44.1% female) with disc herniations treated with microdiscectomy or ESI. There were 184 patients (42.6% female) in the ‘Mild’ group and 207 patients (45.4% female) patients in the ‘Moderate/Severe’ group when stratified by % canal compromise. On bivariate analysis, there was no significant difference in total psoas area, NTPA, PL-CSA, or Goutallier grade between patients when evaluated based on % canal compromise (p > 0.05). Similarly, there was no difference in muscle quality variables when herniations were stratified by total size (p > 0.05). Logistic regressions accounting for sex, age, and ECI showed no association between muscle quality measures and herniation size, canal area, and % canal compromise (p > 0.05). Discussion: As muscle characteristics continue to be studied in various spine contexts, it is important to understand which features may predict disease severity and prognosis. While degree of degeneration of the multifidus muscle have been shown to correlate with presence of lumbar disc herniation, in the case of psoas and paralumbar muscle area, there does not appear to be an association with disc herniation size.
1784
P244: Young spine surgeon - A bookie - the one who goes by the book or a rookie?
Nishant Juva 1
1 Spine Surgery, Juva Orthopaedic Hospital, Godhra, India
Purpose: This retrospective study was performed to analyze the clinical effects and complications of Long segment decompression and fixation in degenerative lumbar scoliosis with lumbar spinal stenosis. Methods: A total of 30 patients (mean age, 60.42 y; 12 men, 8 women) with degenerative lumbar scoliosis with lumbar spinal stenosis were included and Long segment decompression and fixation surgery was performed. Preoperative, postoperative, and follow-up questionnaires were obtained to assess clinical outcomes. Results: The average follow-up period of this study was 12.5 months. The operation time and blood loss of patients were 146.8 min and 352.6 ml. The clinical effects of all patients in terms of visual analogue scale (VAS) and Oswestry disability index (ODI) have been significantly improved at the final follow-up postoperatively (p < 0.05) in 60% patients. Complications such as infection (3 cases), cerebrospinal fluid leakage (2 cases) and wound dehiscence (2 cases) were noted. Nerve injury, and internal fixation failure, etc. were not observed. Postoperative generalised ill health was noted in 3 cases during the follow-up period. Conclusion: The long segment decompression and fixation in degenerative lumbar scoliosis with lumbar spinal stenosis is a safe and effective treatment But with due risks of complications. Decision of such a surgery should only be made after weighing the risks and benefits over other options like only decompression or decompression with short segment fixation.
1860
P245: Comparative analysis between urban vs rural hospitals for patient demographics and perioperative outcomes after lumbar spinal fusion: an analysis of the national inpatient sample (2009-2020)
Alexander Aguirre 1 , Mohamed Soliman 1 , Cathleen Kuo 1 , Ali Khan 1 , Asham Khan 1 , Esteban Quiceno Restrepo 1 , Jeffrey Mullin 1 , John Pollina 1
1 Neurosurgery, University at Buffalo, Buffalo, USA
Introduction: Rural location of patient’s primary residence has previously been shown to be associated with worse outcomes secondary to limited resource availability in these parts of the USA. However, there is paucity of literature investigating the possible impacts a rural hospital location may have on the outcomes of lumbar spine fusions. We aimed to assess the impacts of rural hospital location on the outcomes of lumbar spine fusions. Materials and Methods: Using the National Inpatient Sample (NIS) database a search identified all patients who underwent a lumbar spinal fusion in the years, 2009-2020. These patients were then separated according to whether the treatment hospital was considered rural or urban. Univariate and multivariate linear/logistic regression models were utilized to analyze the data. Results: A total of 2,863,816 patients were identified from this database, where 120,298 (4.2%) patients had their operation at a rural hospital, with the remaining patients in an urban hospital. Patients in the rural cohort were older (p < .001), more likely to be white (89.97% vs. 81.73%, p < .001), and have an increased rate of patients in the first (43.00% vs. 22.52%) and second (38.90% vs. 25.96%) quartiles of median household income when compared to the urban cohort. However, the urban population had patients had significantly increased rates of venous thrombosis (0.57% vs. 0.24%, p < .001), and neurological injury (0.79% vs. 0.36%, p < .001) after surgery. On multivariate analysis urban patients has significant increased odds of venous thrombosis (OR, 1.79; 95% CI, 1.32-2.41; p < .001) and neurological injury (OR, 1.92; 95% CI, 1.46-2.53; p < .001). Conclusions: Patients who have surgery in rural hospitals are at risk for adverse outcomes after spinal fusion, and future research should investigate this to potentially resolve these disparities.
1878
P246: Interspinous process devices for treatment of degenerative lumbar spine disease: 5 year follow up
Hugo Arturo González Martínez 1 , Gustavo Martín González Mendieta 2 , Pablo Tadeo Atlitec Castillo 1 , Jaime Antonio Sánchez Sandoval 1 , Sergio Alberto Ávalos Calderón 1
1 Ortopedia y Traumatología, Hospital Central Sur de Alta Especialidad, Mexico
2 Cirugía de Columna, Corporativo Hospital Satélite, Mexico
Introduction: Degenerative low back pain is characterized by functional limitation caused by biomechanical alterations of the intervertebral disc, bone and ligamentous tissues; among which are disc protrusion, damage to vertebral platforms, decreased intervertebral space, ligamentous and facet joint hypertrophy; which in the long term may predispose vertebral instability causing compression of neurological structures. The treatment of this pathology may be solved through spinal surgery, however it is important to limit the vertebral rigidity leaded by invasive methods, so the use of interspinous spacers may be an appropriate treatment method. Material and Methods: Observational, descriptive, analytical and retrospective study of detailed information in the clinical record of patients undergoing interspinous spacer placement in the Orthopedic Service of a concentration hospital in Mexico City. A 5-year follow-up case series of the medical evolution of patients undergoing lumbar spine surgery with placement of interspinous spacers for low back pain with radiculopathy is described. Results: Results of a case series composed of 35% female and 65% male with age distribution of 20 to 40 years 73% and over 40 years 12% are presented. A normal body mass index was find in 54% of the related population, overweight in 31% and grade I obesity in 12%. Patients report pain according to the analogue visual scale of pain with an average of 9 of 10 during preoperative and 3 of 10 in the postoperative period at 2 months and less than 3 of 10 at 5 year follow up with improve of spine mobility. Oswestry disability index was reported with a mean greater than 65%, which decreased to 30% in the postoperative follow-up. Conclusion: The increase in the current trend of degenerative pathology in young patients makes it imperative to implement less invasive surgical techniques that may lead to long-term clinical improvement with least functional limitation. The use of interspinous spacers is promoted as an effective method, however long-term studies are required to confirm their benefit compared to traditional techniques.
1887
P247: Social determinants of health associated with lower patient-reported outcomes in lumbar spine patients
Aboubacar Wague 1 , Jennifer O'Donnell 1 , Sigurd Berven 1
1 Department of Orthopaedic Surgery, University of California, San Francisco, USA
Background: Social determinants of health (SDoH) are environmental and personal factors that impact healthcare access and outcomes. Patient-reported outcome measures are validated survey instruments that help physicians get a detailed understanding of a patient’s health status. By evaluating the relationships between SDoH and patient-reported outcome measures, we can understand how social factors influence our surgical patients’ health status. Methods: A retrospective review was conducted on a prospectively maintained database. The cohort included consecutive patients who underwent 1-2-level lumbar decompression and/or fusion at a single institution from 2019-2021. Patients completed PROMIS Anxiety, Depression, Fatigue, Pain Interference (PI), Physical Function (PF), Sleep disturbance (SD), and Social Roles (SR) surveys preoperatively and 12-months postoperatively. Each metric was independently evaluated with ten SDOH factors: age, gender, race, preferred language, ethnicity, work status, community median income, religious belief, insurance status, and marital status. These metrics were also evaluated with four health-related behaviors (HRB): tobacco use, alcohol use, drug use, and physical activity level. Community median income was determined using 2019 American Community Survey data. Physical activity level was measured using metabolic equivalence of task (METS) which was recorded by an anesthesiologist during preoperative intake. Additional metrics including co-morbidities and intraoperative variables were also collected. ANOVA and t-test were used for linear variables, and chi-square test for categorical variables. Univariate and multivariate regression were conducted independently for each patient-reported outcome measure. Results: One hundred fifteen patients were included in the study, with mean age 63.9 years, 52.2% female, 80.0% white, 93.9% non-Hispanic, and 41.7% employed. The cohort was 61.7% above the low-income limit, 46.1% privately insured, and 66.1% were married. Thirty-five percent have ever smoked, 17.4% have high-risk alcohol use, and 25.2% have history of drug use. Improvement was seen at 1-year in PROMIS PF, PI, and SR as well as Oswestry Disability Index (ODI). In multivariate analysis, chronic opioid use (COU), depression/anxiety (DA), and per unit decrease in METs were significant predictors for lower preoperative baseline patient-reported outcome measures in ODI [COU:β = 11.5, p = 0.002; METs: β = 3.37, p < 0.001], PROMIS Anxiety [COU:β = 4.15, p = 0.021; DA: β = 5.07, p = 0.002; METs: β = 1.45, p = 0.011], PROMIS Depression [COU:β = 3.41, p = 0.046; DA: β = 6.67, p < 0.001], PROMIS Fatigue [COU:β = 5.68, p = 0.022; DA: β = 6.53, p = 0.003], PROMIS PI [DA: β = 3.13, p = 0.036; METs: β = 1.52, p = 0.001], and PROMIS PF [COU:β = -2.94, p = 0.039; DA: β = -2.50, p = 0.042; METs: β = -0.80, p = 0.036]. At one-year follow-up, DA was the most significant predictor of lower patient-reported outcome scores in PROMIS Anxiety [β = 4.51, p = 0.022], PROMIS Depression [β = 5.29, p = 0.002], PROMIS PI [β = 3.98, p = 0.023]. Discussion: Several SDoH and HRB factors predict worse baseline preoperative patient-reported outcome metrics. COU, DA, and METs represent modifiable factors that impact several patient-reported outcome domains. Further work is needed to understand the role of opioid weaning, psychiatry consultation, and physical therapy as part of presurgical optimization.
1936
P248: Use of artificial intelligence to predict complications in degenerative thoracolumbar spine surgery: a systematic review
Guillermo Ricciardi 1 , Ignacio Cirillo 2 , Rodrigo Pons Belmonte 3 , Lyanne Romero Valverde 4 , Felipe Lopez Muñoz 2 , Alan Manriquez Díaz 5
1 Centro Médico Fitz Roy, Argentina
2 Hospital del Trabajador, Chile
3 Hospital Marcial Quiroga, San Juan, Argentina
4 Sanatorio Guemes, Ciudad de Buenos Aires, Argentina
5 Clínica Francesa, Mendoza, Argentina
Introduction: We aim to identify existing machine learning prediction models in predicting complications in adult patients undergoing surgery for degenerative thoracolumbar pathology and summarize the predictive performance. Material and Methods: A systematic literature review was conducted in Medline/Pubmed, Cochrane Library, and Lilacs/Portal de la BVS to identify machine learning models in predicting complications in patients undergoing surgery for degenerative thoracolumbar spine pathology between January 1, 2000, and May 1, 2023. The risk of bias was assessed using the ROBINS-I and PROBAST tools. Study characteristics and outcomes focusing on general or specific complications were recorded. Results: A total of 2,341 titles were identified (763 were duplicates). Screening was performed on 1,578 titles, and 22 were selected for full-text reading, with 18 exclusions and 4 publications selected for the subsequent review. Additionally, 16 publications were retrieved from other sources (Argentine Association of Orthopedics and Traumatology Library; manual citation search), of which 8 were included in the review. In 5 (41.6%) articles, the effectiveness of artificial intelligence predictive models was compared with conventional techniques. All were globally classified as having a very high risk of bias. Due to heterogeneity in samples, outcomes of interest, and algorithm evaluation metrics, a meta-analysis was not performed. Conclusion: Limited evidence is available to support the benefits of using artificial intelligence predictive models as compared to traditional statistical methods. Regardless, machine learning algorithms seem to be effective for predicting the individual risk of surgical patients, based on the outstanding performance demonstrated by published models.
2066
P249: Factors that influence radiological results ofindirect decompression in patients with lumbar spinalstenosis
Andrey Bokov 1 , Svetlana Kalinina 1 , Anatoly Bulkin 1
1 Neurosurgical, Federal Budgetary Institution Privolzhskiy Medical Research University, Nizhniy Novgorod, Russian Federation
Introduction. Anterior interbody fusion employing DLIF ALIF and DLIF is getting more popular because of effectiveness to obtain optimal sagittal balance parameters along with indirect decompression. The information concerning the results of indirect decompression remain insufficient to predict postoperative results. The aim of this study is to assess factors that influence the radiological results of indirect decompression. Materials and methods. This is a cross-sectional study of 80 patients who underwent OLIF or ALIF supplemented with pedicle screw fixation because of either lumbar stenosis with instability of the affected segment, or unstable spondylolisthesis. Preoperatively CT examination was given and spinal channel square with lateral recess depth were measured in axial plane at the level of maximal constriction. Postoperatively CT examination was used to assess the same parameters. The following factors we chosen in terms of potential impact on radiological results: preoperative values of spinal channel square and lateral recess, disc height change on the ventral and dorsal margin in the middle sagittal plane, difference in the upper vertebra translation in the sagittal plane after reduction, and degenerative changes in facet joints corresponding Weishaupt 4 grade. Either linear regression or ANCOVA were used to assess the relationship between variables. Results. The distribution of data and estimated equations for postoperative CT parameters were different in patients who were operated on with the reduction or fixation in situ. In cases when reduction of the upper vertebra was not used the median of relative vertebral channel square increase accounted for 24% with upper and lower quartile borders [16.3%-33.3%]. The parameters of linear regression for the postoperative vertebral channel square were: r = 0.9508; p < 0.0001. Statistically significant variables were: B1preoperative value of vertebral channel square (B1 = 0.9968, p < 0.0001) and the difference in disc space height along the dorsal boarder (B2 = 4.2827, p = 0.0287). The relative approximation error of the estimated model accounted for 8%. The effect of indirect decompression was greater if the reduction of vertebra was achieved. The median of the relative vertebral channel square increase reached 49.5% with the borders of upper and lower quartile [22.35%; 99.7%]. The parameters of linear regression for the postoperative vertebral channel square were: r = 0.8980; p < 0.0001. Statistically significant variables were: intercept (B0 = 39.2163, p = 0.0001); B1preoperative value of vertebral channel square (B1 = 0.8893, p < 0.0001) and the difference in preoperative and postoperative upper vertebral body translation (B2 = 6.2508, p = 0.0029). The relative approximation error of the estimated model accounted for 16%. The median for the left and right lateral recess depth change accounted for 0.9 mm, however estimated models were of poor explanatory value as far as correlation coefficients achieved 0.7801 for left lateral recess and 0.7068 for right lateral recess. Conclusion. Patients with unstable spondylolisthesis are the best candidates for indirect decompression because of greater relative increase in vertebral channel square. The results of indirect decompression are predictable in patients with central stenosis, however estimated equations may differ for those who underwent reduction versus those who were stabilized in-situ. Patients with lateral stenosis are poor candidates for indirect decompression because postoperative values are less predictable.
2067
P250: Bioactive glass versus iliac crest bone: comparable fusion in ALIF
Sami Bahroun 1,2 , Marc Szadkowski 1 , Henri D'Astorg 1 , Vincent Fiere 1
1 Santy Orthopaedic Center, Lyon, France
2 Kassab Institute, Ksar Said Tunisia, Tunisia
Introduction: Spinal fusion is a common surgical procedure, with over 400,000 surgeries performed in the USA every year. Fusion is used increasingly for the treatment of spondylolisthesis, scoliosis, disc degeneration, herniation and stenosis. Its main goal is to fuse two or more vertebrae by inducing bone growth between segments, though fusion is not always successful, with pseudarthrosis reported in up to 50% of cases. Autologous iliac crest bone is the gold standard graft material used during spinal fusion. Harvesting autologous iliac crest bone has been associated with increased operative time and blood loss, donor site pain and morbidity, as well as increased complication rates. Therefore, synthetic alternatives to autologous iliac crest bone graft continue to be developed and evaluated, of which various formulations of bioactive glass have shown promising results, when used alone or in combination with autologous bone. The purpose was to determine within-patient fusion rates of chambers filled with bioactive glass versus autologous iliac crest bone on computed tomography (CT) following anterior lumbar interbody fusion (ALIF). Material and Methods: A consecutive series of 40 patients (58 levels) that underwent single-level (L5-S1 only) or two-level (L5-S1 and L4-L5) ALIF were assessed. Indications for fusion were one or more of the following: degenerative disc disease with or without Modic changes, spondylolisthesis, and stenosis. Each intervertebral cage had a middle beam delimiting two chambers, one of which was filled with bioactive glass and the other with autologous iliac crest bone. CT scans were graded using the Bridwell classification (grade I, best; grade IV, worst). Patients were evaluated using the Oswestry Disability Index (ODI), and by rating pain in the lower back and legs on a Visual Analog Scale (pVAS); complications and reoperations were noted. Results: At 15 ± 5 months follow-up, there were no significant differences in fusion across chambers filled with bioactive glass versus chambers filled with autologous bone (p = 0.416). Two patients with Bridwell grade III at both chambers of the L4-L5 cages required reoperation using posterior instrumentation. Clinical assessment of the 38 remaining patients (54 levels) at 25 ± 2 months, revealed ODI of 15 ± 12, lower back pVAS of 1.4 ± 1.5 and legs pVAS of 1.9 ± 1.6. Conclusion: For ALIF at L5-S1 or L4-L5, within-patient fusion rates were equivalent for bioactive glass compared to autologous iliac crest bone. The findings of this study suggest that for patients undergoing ALIF, bioactive glass can be used as a substitute to autologous iliac crest bone; thus, avoiding increased operative time and blood loss, as well as donor site morbidity.
2085
P251: Comparative evaluation of clinical and radiological outcomes in minimally invasive stand-alone ALIF procedures at L4-L5 and L5-S1 levels
Sami Bahroun 1,2 , Marc szadkowski 1 , Henri D'astorg 1 , Vincent Fiere 1
1 Santy Orthopaedic Center, Lyon, France
2 Kassab Institute, Ksar Said Tunisia, Tunisia
Introduction: In contrast to alternative surgical approaches, anterior lumbar interbody fusion (ALIF) is often perceived as a more efficacious method for restoring segmental lordosis and minimizing the risk of adjacent-segment disease. Nevertheless, the impact of stand-alone ALIF on global lumbar lordosis and its potential influence on pelvic parameters have stirred debate. This controversy may stem from the varied selection of implants and the diverse levels studied in previous research. The objective of this investigation is to assess and contrast the clinical results between stand-alone ALIF procedures performed at the L4-L5 and L5-S1 levels while also evaluating their impact on spino-pelvic parameters. Material and Methods: We reviewed the records of all patients with DDD that underwent stand-alone minimally invasive ALIF at L4-L5 using the self-locking SynFix cage (DePuy Synthes, PA, USA) and at L5-S1 using the self-locking Idys-ALIF cage (Clariance,Beaurains, France). Patients in both groups were followed up for a minimum duration of 1 year postoperatively. They were evaluated clinically using the Oswestry Disability Index (ODI), Short Form 12, and lower back and legs pain on Visual Analog Scale. Spino-pelvic parameters were measured from whole-spine standing radiographs. Results: Incorporated into our study were 45 patients comprising Group A (those who underwent stand-alone ALIF at the L4-L5 level) and 69 patients forming Group B (those who underwent stand-alone ALIF at the L5-S1 level). In Group A, four patients underwent reoperation due to pseudarthrosis, representing 8% of the cases. Conversely, in Group B, two instances of pseudarthrosis were identified, accounting for 2.8% of the cases. This disparity was deemed statistically significant (p = 0.01). Both surgical procedures showed substantial clinical enhancements across all scoring parameters. Within Group B, multivariable analyses substantiated superior postoperative Oswestry Disability Index (ODI) outcomes among patients who received 18-degree cages (b = 9.0, p = .017). Conversely, in Group A, no correlation was discerned between cage lordosis and clinical outcomes. Within Group B, we observed a more pronounced elevation in both global and segmental lordosis at the operated level in comparison to Group A. Regarding pelvic parameters, in Group B, there was a notable decrease in pelvic tilt by 2.5 ± 4.1 degrees (p < 0.001), accompanied by an increase in sacral slope by 3.3 ± 4.7 degrees (p < 0.001). Conversely, in Group A, we did not observe substantial modifications in pelvic parameters. Conclusion: The use of minimally invasive stand-alone ALIF for Degenerative Disc Disease (DDD) yields favorable initial clinical results and has the potential to enhance both segmental and global lordosis, regardless of the specific level. However, it is worth noting that stand-alone ALIF at the L4-L5 level demonstrated a higher incidence of pseudoarthrosis compared to the L5-S1 level.
2114
P252: Reassessing the minimum two-year follow-up standard after lumbar decompression surgery: a 2-month follow-up seems to be an acceptable minimum
Anna-Katharina Calek 1 , Bettina Hochreiter 1 , Aaron Buckland 2
1 Orthopedic Department, Balgrist University Hospital, Zurich, Switzerland
2 Spine, Melbourne Orthopaedic Group, Melbourne, Australia
Background: Academic orthopaedic journals and specialty societies emphasize the importance of two-year follow-up for patient-reported outcomes (PROs) after spine surgery, but there are limited data evaluating the appropriate length of follow-up. This study evaluates the changes in PROs out to two years after lumbar decompression surgery for disc hernation or spinal stenosis. Methods: Retrospective analysis of prospectively and consecutively enrolled patients undergoing lumbar decompression surgery between 2020 and 2021 from a single surgeon spine registry. Patients without a preoperative baseline score were excluded. The median Oswestry Disability Index (ODI) was compared at time baseline, 2-month, 1-year and 2-year follow-up. Risk of reoperation was assessed with receiver operator characteristic (ROC) analysis to identify at risk ODI thresholds of requiring reoperation. Results: Sixty-nine patients were identified. The median ODI significantly improved at all time points compared to baseline (median baseline ODI: 42.2; 2-month ODI: 9.4, p = 0.001; 1-year ODI: 7, p = 0.001; 2-year ODI: 6, p = 0.001). Post-hoc analysis demonstrated no difference between 2-month, 1-year and 2-year postoperative ODI (p = 0.9, p = 0.468, p = 0.606). The minimum clinically important difference (MCID) was met in 87.9% of patients at two months, 80.7% at one year, and 87.3% at two years postoperatively. Eight patients (11.6%) underwent a revision surgery between 2 months and 2 years after the index surgery (median time to revision: 8.5 months). ROC curve analysis demonstrated that an ODI score ≥ 24 points at 2-months yielded a sensitivity of 80% and a specificity of 86% for predicting revision after lumbar decompression (AUC = 0.847; 95% CI: 0.678-1.02). The Youden optimal threshold value of ≥ 24 points at 2-month postop ODI yielded an odd’s ratio (OR) for revision of 24.7 (CI: 2.3-259.9; p = 0.005). The positive predictive value (PPV) and negative predictive value (NPV) were 40% and 97.4%, respectively. Conclusion: Two-year clinical follow-up may not be necessary for future peer-reviewed lumbar decompression surgery studies given that ODI plateaus at 8 weeks. Patients with a score ≥ 24 points at 2-months postoperatively have a higher risk of requiring a second surgery within the first two years and warrant continued follow-up.
2148
P253: Prevalence of impaired traveling ability and postoperative outcomes in patients with grade I lumbar spondylolisthesis: a quality outcomes database study
Nitin Agarwal 1 , Andrew Chan 2 , Erica Bisson 3 , Steven Glassman 4 , Kevin Foley 5 , Christopher Shaffrey 6 , Oren Gottfried 6 , Luis Tumialan 7 , Eric Potts 8 , Mark Shaffrey 9 , Domagoj Coric 10 , John Knightly 11 , Rida Mitha 1 , Asimina Dominari 12 , Paul Park 13 , Michael Wang 14 , Kai-Ming Fu 15 , Jonathan Slotkin 16 , Anthony Asher 10 , Michael Virk 15 , Jian Guan 17 , Regis Haid 18 , Dean Chou 2 , Mohamad Bydon 12 , Praveen Mummaneni 19
1 University of Pittsburgh School of Medicine, USA
2 Columbia University Irving Medical Center, USA
3 University of Utah, USA
4 Norton Leatherman Spine Center, USA
5 Semmes-Murphey Neurologic and Spine Institute, USA
6 Duke University, USA
7 Barrow Neurologic Institute, USA
8 Goodman Campbell Brain and Spine, USA
9 University of Virginia, USA
10 Neuroscience Institute, Carolina Neurosurgery & Spine Associates, USA
11 Atlantic Neurosurgical Specialists, USA
12 Mayo Clinic, USA
13 University of Michigan, USA
14 University of Miami, USA
15 Weill Cornell Medical Center, USA
16 Geisinger Health, USA
17 Pacific Neuroscience Institute, USA
18 Atlanta Brain and Spine Care, USA
19 University of California, San Francisco, USA
Background: Lumbar spondylolisthesis associated pain can affect traveling ability or duration. Patients often recite traveling in the back seat of a vehicle to be particularly aggravating. The benefits of surgery to improve the ability to travel are investigated. Methods: The low-grade spondylolisthesis database of the Quality Outcomes Database was utilized. Traveling ability was evaluated using the traveling subcomponent of the Oswestry Disability Index (ODI), with limited traveling ability being defined as having an ODI Traveling score (ODITS) of ≥ 3. Improvement in traveling ability was evaluated as follows: improvement of ≥ 1 point in ODITS and best response to treatment, defined as ODITS = 0 among patients with baseline ODITS = 5. Multivariable logistic regression models were fitted to evaluate mediators of impaired traveling ability at baseline and by 1 year postoperatively. Results: Of 601 patients surgically treated for Grade I lumbar spondylolisthesis, 38.4% had limited traveling ability. Dependent ambulation (OR = 1.2, 95%CI:1.1-1.4, p < 0.01), age ≤ 63 years (OR = 1.2, 95%CI:1.1-1.3, p < 0.01), body mass index (BMI) > 29 (OR = 1.1, 95%CI:1-1.2, p < 0.01), and depression (OR = 1.2, 95%CI: 1.0-1.3, p = 0.01) were associated with limited baseline traveling ability. At 3 months, 58.8% experienced improvement, while 67.9% reported improvement by 1 year. Improvement by 1 year was more common in patients who were younger (61.9 vs. 64.7, p = 0.02), underwent fusion (81.9% vs. 68.2%, p < 0.01), and had higher baseline leg (6.8 vs. 5.9, p < 0.01) and back pain (NRS) scores (6.9 vs. 6.1, p < 0.01), and ODI scores (48.9 vs. 41.2, p < 0.01). Best response to treatment was noted in 29.3% by 1 year. Improvement was sustained in 72% by 1 year, and 66.7% by 5 years. At both time points, sustained improvement was significantly more common in patients with lower BMI (30.1 vs. 32.5, p < 0.01; 29.8 vs. 31.8, p = 0.02) and higher socioeconomic status index (53.7 vs. 51.9, p = 0.02; 53.7 vs. 52.2, p = 0.03). Sustained improvement at 5 years was more likely in patients with lower leg (1.6 vs. 3.7, p < 0.01) and back pain (NRS) scores (2.3 vs. 4.8, p < 0.01), ODI scores (13.7 vs. 33.5, p < 0.01), and higher EQ-5D scores (0.843 vs. 0.660, p < 0.01) at 1 year. Conclusion: Following surgery for grade I lumbar spondylolisthesis, significant improvement in traveling ability is achieved by 1 year, and this positive outcome remains largely durable at 5 years postoperatively. Improved traveling ability drives patient satisfaction and is associated with improved quality of life.
2160
P254: Feasibility assessment of an expandable lumbar interbody cage in patients with high-risk factors for subsidence: a preliminary report
Kwang-Sup Song 1 , Dae-Woong Ham 1 , Byung-Il Yoon 1 , Jeuk Lee 1
1 Department of Orthopedic Surgery, Chung-Ang University Hospital, Seoul, South Korea
Introduction: Expandable cages are becoming increasingly popular due to their advantages, including easier insertion and reduced risk of iatrogenic endplate injury. These factors suggest that expandable cages may exhibit lower rates of cage subsidence compared to static cages. This study aimed to assess the clinical feasibility of expandable cages in patients at high risk of subsidence. Methods: In this cohort study, we employed propensity score matching from a prospectively maintained database. We included 20 patients with high-risk factors for subsidence who underwent posterior lumbar interbody fusion (PLIF) using expandable cages. High-risk subsidence patients met one or more of the following criteria: 1) low BMD (Hip T-score < -2.5), 2) previous multilevel fusion surgery at the adjacent segment (at least 3 levels), or 3) spondylolisthesis (grade 2 or more). Propensity score matching was performed on demographic data and subsidence risk factors using a pool of 387 cases from our institution's PLIF cohort. Twenty patients who underwent PLIF with static cages and had high-risk subsidence factors were selected as the control group. Clinical outcomes were evaluated using the EuroQol-5-Dimensional questionnaire (EQ-5D) and Oswestry Disability Index (ODI). Radiological parameters, including segmental lordotic angle (SLA), disc angle (DA), foraminal height (FH), and disc height index (DHI), were measured at preoperative, immediate postoperative, and last follow-up stages using standing lateral radiographs. Results: The study included 40 patients with a minimum follow-up of 6 months. Of these, 31 (77.5%) were female, and the mean age was 71.9 ± 5.9 years, with no significant difference between the static and expandable groups (p = 0.694). Significant clinical improvements were observed at 6 months postoperative compared to preoperative, including ODI, EQ-5D, and back and leg VAS in both groups. The expandable cage group demonstrated significantly higher immediate postoperative DHI compared to static cage group (0.35 ± 0.06 and 0.27 ± 0.04, respectively, p < 0.001). Moreover, the expandable cage group maintained greater DHI at the last follow-up compared to the static cage group (0.31 ± 0.05 and 0.22 ± 0.04, respectively, p < 0.001). The ratio of last-immediate disc height was higher in the static cage group (0.203 ± 0.075 and 0.104 ± 0.079, respectively, P < 0.001), indicating a higher subsidence degree in the last follow-up compared to the expandable cage group. No other significant differences were observed in radiographic measurements between the two groups, including the FH, SLA, and DA. Conclusion: The study demonstrated that the expandable cage group had significantly higher immediate postoperative DHI and maintained it until the last follow-up compared to the static cage group, indicating better resistance to subsidence. These findings suggest that expandable cages could be clinically feasible and offer advantages over static cages for patients with a high risk of subsidence undergoing PLIF surgery.
2172
P255: A rare case of spontaneous giant pneumorrhachis presenting with cauda equina syndrome - A case report and review of literature
Mayukh Guha 1 , Kuldeep Bansal 1 , Anuj Gupta 2
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
2 Spine Surgery, Max Superspeciality Hospital, Ghaziabad, India
Introduction: Pneumorrachis is presence of air in the epidural space. It could be the result of trauma, barotrauma, iatrogenic or spontaneous. The pneumorrachis per se is an underdiagnosed entity as most of the patients are asymptomatic or has subclinical symptoms. The spontaneous occurrence of pneumorrachis has been reported in literature but giant spontaneous occurrence causing cauda equina syndrome has not been reported so far. Material and Methods: We report a case of 56-year-old male patient who came to our OPD on wheelchair with complains of difficulty in walking for 6 months with dribbling of urine for 2 months with on and off backpain. Results: On clinical examination, there was bilateral partial foot drop as well as weakness in both plantar flexors. His perianal sensation was reduced with absent voluntary anal contraction. Imaging revealed giant air pockets in the spinal canal of L5-S1 extending upto L4-L5. It was managed surgically wherein laminectomy without fusion was done. The patient responded well to the treatment. Although his motor power improved significantly, his bladder was not recovered. Discussion: There are many causes of pneumorrachis described in literature. Most of the cases of pneumorrachis are asymptomatic and incidentally diagnosed. With the improvement in radio-diagnostic modalities, the diagnosis of pneumorrachis can be easily established. When symptomatic, they can be managed conservatively. Those presenting with neurological deficit may require surgical intervention or other invasive intervention.
2231
P256: Developing a new valid, reliable and responsive tool for lumbar spinal stenosis
Evi Drakoulidou 1 , James Van Gelder 1 , David Anderson 2
1 Sydney Spine Institute
2 The University of Sydney, Faculty of Medicine and Health, Australia
Introduction: Lumbar spinal stenosis is the leading cause of pain and disability in older adults and leading indication for spinal surgery. Despite its prevalence, current assessment of lumbar spinal stenosis relies upon questionnaires and self-reported measures. This approach is prone to bias and may not provide representative outcomes when used in clinical trials to determine effectiveness of treatments. Methods: In this study, 127 people with lumbar spinal stenosis, considered eligible for lumbar decompression by a neurosurgeon were assessed using a new low cost activity monitor. Existing tools were also used to determine construct and criterion validity. Reliability and responsiveness was also assessed by repeating assessments before and after lumbar decompression surgery. COSMIN criteria was used to determine adequate or inadequate results. Results: The low cost activity monitor possessed adequate validity, reliability, and responsiveness. Existing tools, such as the Oswestry Disability Index, Swiss Spinal Stenosis Questionnaire, and Self Paced Walking Test had a mixture of both adequate and inadequate measurement properties. Conclusions: A lost cost activity monitor provides clinicians with a valid, reliable and responsive assessment tool for the assessment of lumbar spinal stenosis. Clinicians and researchers should consider using updated assessment tools when determining effectiveness of treatments for lumbar spinal stenosis.
2300
P257: Validation of the Arabic version of EuroQol-5 Dimension-5 Level (EQ-5D-5L) in patients with spinal degenerative diseases
Ahmed Shawky Abdelgawaad 1 , Mohammad El-Sharkawi 2 , Ahmed Sarhan 2 , Mohamed Hassanin 2 , Mirette Aziz 3
1 Spine Center, Helios Klinikum Erfurt, Erfurt, Germany
2 Orthopaedics and Trauma
3 Public Health, Assiut University, Assiut, Egypt
Introduction: This study aims to provide a validated Arabic version of EQ-5D-5L so that it would be used as a quality-of-life assessment tool for Arabic-speaking patients. Material and Methods: The study was conducted on 150 patients operated upon for degenerative spine diseases coming for follow up in the outpatient clinic of a university hospital between November 2018 to December 2019. The criterion validity was assessed by comparing the responses of 100 patients to the EQ-5D-5L with scores of two questionnaires: the Arabic version of the Oswestry disability index and the Arabic version of short-form health survey-36. The construct validity was assessed using known-groups comparison to test for hypothesized differences concerning socio-demographic variables. Test-retest reliability was assessed by another 50 patients. Results: One hundred subjects were included in the validation study. The mean age was 41.27 ± 9.17 years, with 58% males. The proportion of respondents reporting problems ranged from 36% for problems with self-care to 72% for pain/discomfort. Test-retest reliability was evaluated using Cohen’s κ, which was 0.816. Conclusion: Reliability and validity of the Arabic version of EQ-5D-5L were established for assessing the quality of life in Egyptian patients with spinal degenerative diseases.
2320
P258: Hospital length of stay: a swift drop following lumbar spine surgery in tetiary-care vs. university hospitals
Olivia Opara 1 , Rajkishen Narayanan 1 , Adam Kohring 2 , Yunsoo Lee 1 , Michael McCurdy 1 , Nicholas Pohl 1 , Cordero McCall 1 , Preston Carey 1 , Rioke Diejomaoh 1 , Sean Lowitz 1 , Evan Bradley 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Rothman Orthopaedic Institute, Philadelphia, USA
2 Jefferson Health, New Jersey, USA
Introduction: The anticipated rise in lumbar fusions in the coming decades, spurred by an aging population, is likely to strain healthcare resources significantly. In spine surgery, comparing patient outcomes between university-affiliated hospitals and tertiary-care hospitals is limited in the literature. Therefore, our study aims to compare outcomes and complication rates based on the surgical setting in patients following elective lumbar spine surgery. Material and Methods: Retrospective analysis of patients who underwent elective lumbar fusion surgery at either a single tertiary care hospital (TCH) or a single non-tertiary, university-affiliated hospital (UAH) from 2017 to 2022 were identified. Patient demographics, surgical characteristics, and surgical outcomes were collected from an electronic medical record. Patients were identified and separated into two cohorts based on where their surgery was performed. Patients were excluded if they were less than 18 years of age or if surgery was performed due to trauma, infection, or tumor. Propensity score matching was performed in a matched 2:1 comparison based on (Age, CCI, Procedure type, and Total levels fused). All statistical analyses were performed using R Studio Version 4.0.2 (Boston, MA), with P values < 0.05 considered statistically significant. Results: Of the 180 patients identified, 120 were surgically treated at a TCH, and 60 were surgically treated at a non-tertiary care UAH. Patients treated at the TCH had a significantly longer length of stay (LOS) compared to their matched counterparts at the UAH (4.12 vs. 2.67 days, p < 0.001). Additionally, both hospitals exhibited no significant difference in procedure type (p = 0.958), the total number of levels fused (p = 0.488), or levels decompressed (p = 0.308). Similarly, there was no significant difference demonstrated regarding 90-day readmission rates (p = 0.097), revision rates (p = 0.111), and complication rates (p = 1.000) between both cohorts. Regarding discharge destinations, patients at the UAH had an increased home discharge rate (95%), whereas at the TCH, 10 (8.33%) patients were discharged to an inpatient rehab (IPR), and 13 (10.8%, p = 0.016) were admitted to a skilled nursing facility (SNF). Conclusion: Our study identified that patients at the non-tertiary care, university-affiliated hospital experienced a significantly shorter hospital length of stay with an increased discharge rate to home compared to patients at the tertiary-care hospital who stayed longer and were more likely to be discharged to a rehab or skilled nursing facility. There were also no discernible differences in readmissions, revision, and complication rates between the two hospitals, indicating that the expedited recovery at a university-affiliated hospital did not compromise surgical quality or postoperative outcomes. These findings suggest that for certain patient populations, university-affiliated hospitals may offer a more efficient, cost-effective model for lumbar spine surgery without sacrificing the quality of patient care compared to tertiary-care hospitals.
2323
P259: Neurosurgeons prefer minimally invasive surgery versus open procedures in L4-5 spondylolithesis pateints while performing fusion. Results from a surgeon demographic-impact study for L4-5 degenerative spondylolithesis
Jinho Park 1 , Michael Virk 2 , Ashish Diwan 3 , Timothy S. Yoon 4 , Juan P. Cabrera 5 , Jeffrey C. Wang 6 , Patrick Hsieh 6 , Samuel Cho 7 , Ho-Joong Kim 1
1 Orthopaedic Surgery, Seoul National University Bundang Hospital, Seongnam-si, Gyeonggi-do, South Korea
2 Neurosurgery, Weill Cornell Medicine Brain & Spine Center, New York, NY, USA
3 Orthopaedic Surgery, St. George Hospital, University of New South Wales, NSW, Australia
4 Orthopaedic Surgery, Emory University Hospital, Atlanta California, USA
5 Neurosurgery, Hospital Clínico Regional de Concepción, Concepción, Bío Bío, Chile
6 Spine Surgery, Keck Hospital of USC, Los Angeles, CA, USA
7 Spine Surgery, Icahn school of Medicine at Mout Sinai, New York, NY, USA
Introduction: Over the past 30 years, there has been significant advancement in minimally invasive spinal surgery, driven by both patient demand and technological progress. The aesthetic benefits, along with advantages such as rapid recovery and reduced pain, have made minimally invasive surgery (MIS) a preferred choice for many patients. This study aimed to investigate surgeon preferences for open or MIS in decompression and fusion for the common clinical condition of grade 1 L4-5 spondylolisthesis, based on surgeon demographics. Material and Methods: The survey was distributed online to over 6000 AO Spine members between July 27 and September 8, 2023. 943 responded and 479 completed the survey. Questions pertained to decision making parameters and surgical technique preferences in the treatment of three cases of grade 1 L4-5 spondylolisthesis. We then analyzed the preference for MIS versus open procedures among surgeons who chose laminectomy and fusion as treatment for three representative cases. We conducted this analysis based on surgeon demographics, including country of practice, sex, age, years of experience in spine surgery, specialty, practice setting, fellowship training status, and the volume of lumbar spondylolisthesis cases in their practice. All statistical analyses were conducted using the chi-square method. Results: In the first case of severe central stenosis minimal instability (1-2mm anterior translation in flexion) in elderly patient, 309 (64.5%) surgeons chose laminectomy and fusion as the preferred treatment. Out of these, 233 individuals (75.4%) opted for the open procedure, while 76 individuals (24.6%) chose MIS. A significantly notable difference in procedure preference was neurosurgeons demonstrating a stronger inclination towards MIS compared to orthopedic surgeons (p = 0.033). For the second case of severe central and foraminal stenosis with severe instability (5mm anterior translation in flexion) in middle-aged patient, 365 individuals (76.2%) opted for laminectomy and fusion as their treatment. Among these, 265 individuals (72.6%) favored the open procedure, while 100 individuals (27.4%) opted for MIS. Again, neurosurgeons showing a greater preference for MIS compared to orthopedic surgeons (p = 0.001). In the third case of no significant stenosis, moderate instability (3mm anterior translation in flexion), and facet arthrosis in middle-aged patient, a total of 207 individuals (43.2%) opted for laminectomy and fusion as their treatment. Among these, 136 individuals (65.7%) chose the open procedure, while 71 individuals (34.3%) opted for MIS. A Significant difference in procedure preference was observed based on sex and age. Female surgeons (p = 0.023) and the 55-64 age group (p = 0.007) exhibited a preference for the open procedure compared to other age groups and male surgeons. Conclusion: There was a trend for neurosurgeons to prefer MIS over orthopedic surgeons in the case of elderly patient with severe stenosis and middle-aged patient with severe instability and stenosis. However, in middle-aged patient with moderate instability and no significant stenosis, there was a tendency for female surgeons and those aged 55-64 to prefer the open procedure.
2334
P260: Fusion preference-profile among AO Spine members for degenerative lumbar spondylolisthesis. Insights for AO Spine KF Degen Spondylolisthesis Survey
Sathish Muthu 1,2 , Michael Virk 3 , Jeffrey C. Wang 4 , Ashish Diwan 5 , Samuel Cho 6 , Patrick Hsieh 7 , Timothy S. Yoon 8
1 Spine Surgery, Orthopaedic Research Group, Coimbatore, India
2 Department of Orthopaedics, Government Karur Medical College, Karur, India
3 Department of Neurosurgery, Cornell University, New York, USA
4 Department of Orthopaedic Surgery and Neurological Surgery, Keck School of Medicine, California, USA
5 Department of Orthopaedic Surgery, University of New South Wales, Sydney, Australia
6 Department of Orthoapedic Surgery and Neurosurgery, Icahn School of Medicine at Mount Sinai, Mount Sinai, USA
7 Department of Neurosurgery, Keck School of Medicine, Los Angeles, USA
8 Department of Orthopaedic Surgery, Emory University, Atlanta, USA
Introduction: Surgical approaches when clinically required for lumbar degenerative spondylolisthesis in the real world is not consistent with randomized controlled trials and big data registries that indicate the superiority of decompression over fusion in controlled setting. This study analyzes the fusion preference-profile among the AO spine members to a given case of lumbar degenerative spondylolisthesis. Methods: A survey was distributed online to over 6000 AO Spine members between July 27 – September 8, 2023. Surgeons were presented a case of L4-L5 grade I degenerative spondylolisthesis in a middle aged individual with significant back and leg pain with neurological deficits with radiological dynamic translation without canal stenosis. The participants were queried about their treatment choices for decompression and their decision to offer fusion. Data that may impact that decision were collected that include age, region of practice, training background, years of experience, practice setting, case volume, and their final treatment decisions. Comparative analysis of the responder characteristics was performed using Pearson’s chi-squared test. Results: A total of 943 surgeons responded and 479 completed the survey. We noted a comparable distribution of the responder demographics across age, region of practice, training background, years of experience, practice setting, and case volume. 91% of surgeons opted for fusion in their management, while 9% chose direct decompression alone. Of 429 responders those who opted for fusion procedure, 56% surgeons employed direct decompression techniques while 44% chose indirect decompression resulting from instrumentation. We noted that surgeons with fellowship training (p < 0.05) and higher case load surgeons (p < 0.05) had significantly higher inclination towards fusion. Conclusion: Fusion is commonly employed in the treatment decision combined with decompression in the management of degenerative spondylolisthesis. Surgeons choice of fusion in this setting needs to be systematically studied, as there is a disconnect with the available data from the randomized clinical trials in the field.
2387
P261: Posterior lumber-interbody fusion for the treatment of spondylolisthesis
Md Rezaul Karim 1
1 Spine Surgery Unit, National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Background: The posterior lumbar interbody fusion (PLIF) procedure allows restoration of the weight-bearing capacity to a more physiological ventral position and maintenance of disc space height. However, the procedure can be technically difficult and may cause complications. It has always been performed bilaterally; central fusion has not been commonly used. Methods: Forty-eight patients who met the interbody fusion criteria from March 2013 to July 2023 were included in the study. Surgery was performed from the posterior with chips of bone graft for interbody fusion supplemented with transpedicular screws and rod. The follow-up period from 8 to 30 months with a mean of 14.4 months. It was a prospective study irrespective of age & sex. Results: Overall, 92.86% of the patients were satisfied after surgery. Radiography study showed the rate of bony fusion being 82.14%. Fibrous union was noted in two patients. One patient experienced tear of the dura without clinical sequel. One patient had misdisplacement of screws in disc space. Overall, the complications were negligible and none of the patients sustained a motor deficit and permanent complication. Conclusions: The PLIF procedure using central bone graft combined with bilateral pedicle screws fixation obtained satisfactory outcome within a short-term or long-term follow-up period. Since the implant-related complications have seldom been observed, it may be used as an alternative option for recurrent lumbar disc herniation or low-grade spondylolisthesis with apparent degenerative disc disease.
Keywords: posterior lumbar interbody fusion, bilateral pedicle screw
2399
P262: Deroofing and medial facetectomy one of the treatment modality for multilevel degenerative lumbar spinal canal stenosis
Md Rezaul Karim 1
1 Spine Surgery Unit, National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Background: Conventional laminectomy is a simple procedure that provides adequate decompression in case of lumbar spinal canal stenosis. However, with this surgical modality, important posterior osteo-ligamentous elements necessary for spinal stability are lost; and it is often accompanied by damage to the facet joint. Bilateral inter-laminar fenestration and deroofing of the intervertebral foramen to achieve decompression of the nerve roots and also dural sac. Materials and Methods: This is a prospective study done in NITOR and Private hospital in Dhaka from July 2016 to July 2023. Fifty-eight patients who met the criteria from July 2016 to July 2023 were included in this study. At each level involved, a bilateral sub-articular fenestration is performed under high magnification. The medial third of each facet joint is first removed with a fine and sharp chisel; then the thickened ligametum flavum and adjacent lamina is removed. All tissue responsible for neural compression is removed, but the spinous processes, inter-spinous ligaments and much of the facet joints and lamina are preserved. Spinal stability is maintained because tissue disruption is minimized. Results: Post-operative discomfort is usually reduced, promoting early mobility and reduced hospital stay. The results of operation in 38 patients are assessed. The follow-up periods range from 6 months to 12 months. 38 patients who were presented with neurogenic claudication, 24(63.15%) obtained complete relief and 14(36.85%) improved significantly. The mean hospital stay was 5 days (range, 3 to 7 days). Conclusion: This procedure of decompression provided satisfactory results.
Keywords: Spinal canal stenosis; Medial facetectomy; deroofing
2417
P263: Evaluating the benefits of enhanced recovery for spinal fusion surgery for degenerative spinal diseases: a retrospective study
Yew weng Fong 1 , Chih-Ju Chang 1 , Shu-Lin Guo 1
1 Division of Neurosurgery, Cathay General Hospital, Department of Surgery, Taipei, Taiwan
Introduction: Lumbar degenerative diseases significantly impact the quality of life in the elderly population. They face higher surgical risks and poorer clinical outcomes. This retrospective study aimed to evaluate the outcomes of patients undergoing lumbar fusion surgery who received the ERAS protocol compared to those who underwent traditional care. The study sought to assess the benefits of implementing a modified ERAS protocol in improving patient treatment outcomes. Materials and Methods: The study analyzed data from 88 patients who underwent lumbar fusion surgery at a tertiary center, collected by two experienced spine surgeons. The patients were divided into two groups: the ERAS group (n = 43) and the non-ERAS group (n = 45). Comparable patient groups were matched based on age and surgical level. The ERAS group followed a modified version of the ERAS protocol consisting of 19 elements, while the non-ERAS group did not participate in this protocol and received patient-controlled intravenous anesthesia. The pain severity was measured using the Visual Analog Scale (VAS). The primary outcome measures focused on pain control during motion and rest in the first three days postoperatively, as well as the total amount of rescue morphine and opioid medications used for pain management. Secondary outcome measures included hospital stay, intravenous fluid administration, self-voiding, days of bed rest before ambulation, days of continuous drain usage, and time to removal of urinary catheter. Results: The study showed no significant differences between the two groups regarding surgical duration or total blood loss (p = 0.11 and p = 0.25, respectively). However, compared to the non-ERAS group, the ERAS group exhibited significantly improved temperature control at the end of the surgery (36.59 vs 35.95, p < 0.05). Furthermore, the ERAS group showed a significant reduction in the amount of rescue morphine (0.24 mg vs 1.49 mg) and total postoperative opioid medication (8.2 mg vs 26.5 mg) compared to the non-ERAS group (p < 0.05), indicating a 69% reduction in opioid medication usage. The ERAS group demonstrated better pain control during bedside movement on the first day (VAS score 2.31 vs 1.93) and the second day (VAS score 2.2 vs 1.76) compared to the non-ERAS group, with no significant difference observed at rest. The ERAS group also showed a shorter hospital stay (6.78 days vs 8.47 days, p < 0.05), earlier self-voiding (3.56 days vs 4.35 days, p < 0.05), earlier out-of-bed ambulation (3.37 days vs 4.27 days, p < 0.05), earlier removal of urinary catheter (3.4 days vs 4.03 days, p < 0.05), and earlier removal of intravenous catheter (4.39 days vs 5.33 days, p < 0.05). Conclusion: This retrospective study compared the ERAS protocol with traditional care for lumbar fusion surgery and highlighted several significant benefits associated with the ERAS group. These measures included improved pain control, reduced opioid medication usage, better temperature control during perioperative period, shorter hospital stay, accelerated recovery, and earlier removal of medical equipment. These findings strongly support the implementation of an enhanced ERAS protocol in lumbar fusion surgery to enhance treatment outcomes and promote a faster recovery process for patients. However, further prospective research is needed to validate these results.
2457
P264: Overview of clinical outcomes following lumbar laminectomy and laminotomy: a systematic review
Alexandra Seidenstein 1 , Gabriel Nazario-Ferrer 1 , Andrew Kim 1 , Amit Jain 1
1 Department of Orthopaedic Surgery, The Johns Hopkins Hospital, Baltimore, USA
Introduction: Spinal decompression procedures such as lumbar laminectomy and laminotomy are considered the standard of care for the treatment of neural structure compression. Although existing literature suggests an association between laminectomy and postoperative spinal instability, laminectomy remains the preferred surgical technique. This study aims to analyze patient-reported outcomes and postoperative complications following lumbar laminotomy and laminectomy to understand the clinical impact of each procedure. Material and Methods: A systematic review using the PubMed (NLM), Google Scholar, and Scopus databases was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines using keywords including ‘laminectomy,’ ‘laminotomy,’ ‘spinal decompression,’ ‘spine clinical outcomes,’ ‘partial laminectomy,’ and ‘spinal stability.’ Studies were excluded if they involved cervical levels and staged same-day procedures. Data on study design, sample size, surgical techniques, length of surgery, length of hospital stay, complications, reoperation rates, and patient-reported outcomes, such as Visual Analog Scale (VAS) and Oswestry Disability Index (ODI), were collected when available. Results: Ten studies were included for analysis: five focused on laminectomy and nine only aminotomy. A total of 1,439 cases (984 laminotomy and 455 laminectomy), with a mean age of 65.59 years and 66.26 years for each procedure respectively. Among laminotomy patients, 45.12% (444/984) were male and 53.76% (529/984) were female. Among laminectomy patients, 55.16% (251/455) were male and 51.87% (236/455) were female. Average mean follow-up was 24.87 months for patients undergoing laminotomy and 35.07 months for patients undergoing laminectomy. From the studies analyzed, there was no significant difference in patient-reported outcomes with regards to VAS and ODI between the laminotomy and laminectomy groups. Laminotomy patients had lower mean estimated blood loss (91.32 mL vs. 131.14 mL) and reoperation rates (3.40% vs. 9.48%) compared to laminectomy patients. Operative time was longer in patients undergoing laminotomy compared to laminectomy (77.94 minutes vs. 69.63 minutes). Conclusion: Among spinal decompression procedures, laminotomy offers similar patient-reported outcomes but with lower mean estimated blood loss and reoperation rates when compared to laminectomy. These findings suggest that laminotomy is a safe alternative to laminectomy in the treatment of lumbar spinal stenosis, with the added benefit of potentially reducing the risk of postoperative instability. Understanding the potential complications and need for reoperation can assist orthopaedic surgeons in selecting the most appropriate surgical treatment, thereby improving clinical outcomes.
2499
P265: Preoperative opioid use and patient-reported outcomes following lumbar spine surgery
Aboubacar Wague 1 , Jennifer O'Donnell 1 , Sarah Stroud 1 , Khuzaima Rangwalla 1 , Anna Filley 1 , Avionna Baldwin 1 , Ashraf El Naga 1 , David Gendelberg 1 , Sigurd Berven 1
1 Department of Orthopaedic Surgery, University of California, San Francisco, USA
Background: Patient-reported health-related quality-of-life measures have important utility in quantifying changes in health status and clinical outcomes. The Patient-Reported Outcomes Measurement Information System (PROMIS), created by the National Institute of Health, is a reliable and valid survey for patients with lumbar spine pathology. Preoperative opioid use is an important predictor variable of self-reported health status in patients with spinal disorders. This study aims to investigate the impact of preoperative opiate use on self-reported health status and change in health status in patients treated with surgery for lumbar degenerative pathology. Methods: Patients who underwent lumbar decompression ± ≤ 2 level fusion at a single institution between March 2019 and January 2021 were identified from a prospectively maintained database. PROMIS Anxiety, Depression, Fatigue, Pain Interference (PI), Physical Function (PF), Sleep disturbance (SD), and Social Roles (SR) surveys were recorded at preoperative intake with subsequent follow-up at 6 and 12 months postoperatively. Patients were categorized according to preoperative opiate use. Chronic Opioid Users (COU) had prescribed opioid use of ≥ 3 continuous months prior to surgery. Between cohort comparisons of the mean for each PROMIS measure were performed using simple t-test. We controlled for variables that may be independent predictors of self-reported health status including age, gender, co-morbidities, length of stay, duration of surgery, and American Society of Anesthesiology (ASA) score. Results: One hundred and twenty-one patients met our inclusion criteria of completed PROMIS surveys at the designated time points. A total of 27 (22.3%) were chronic opioid users (COU) prior to surgery. Analysis of patient-reported health outcomes shows that long term opioid use correlated with worse ODI (53.8 ± 17.7 vs. 35.7 ± 16.9, p < 0.001) and PROMIS Anxiety (58.0 ± 10.1 vs. 53.3 ± 8.10, p = 0.034), Depression (55.7 ± 9.05 vs. 50.5 ± 7.82, p = 0.011), Fatigue (60.1 ± 10.0 vs. 52.2 ± 10.2, p < 0.001), PI (66.1 ± 7.87 vs. 62.1 ± 7.53, p = 0.023) and PF (34.1 ± 5.39 vs. 38.3 ± 6.58, p = 0.001) scores at baseline compared to non-chronic users (NOU). At 1 year follow-up, the COU cohort continued to have significantly worse ODI (31.8 ± 20.1 vs. 16.3 ± 16.7, p < 0.001), PROMIS PI (59.4 ± 8.12 vs. 53.0 ± 8.85, p < 0.001), and PROMIS PF (40.0 ± 7.66 vs. 46.1 ± 8.29, p < 0.001) scores. There is a statistical difference in the magnitude of change in health status between the two cohorts in PROMIS Anxiety (-7.62 ± 7.18 vs -2.90 ± 8.5, p = 0.006), Depression (-5.73 ± 7.07 vs. -1.72 ± 8.29, p = 0.016) and Fatigue (-8.90 ± 9.12 vs. -4.14 ± 11.0, p = 0.017) at after one-year follow-up, with the COU cohort experiencing significantly greater improvement in these domains. Mean improvement in PROMIS scores for the COU cohort exceeded minimal clinically important difference (MCID) in all domains except PROMIS SR and SD. The NOU cohort exceeded MCID in PROMIS PF and PI domains. Conclusion: Patients with chronic opioid use status have worse baseline PROMIS scores and longer LOS after surgery. However, patients in the COU cohort displayed significant postoperative improvement in multiple PROMIS domains. These results show that chronic opioid users may benefit greatly from surgical intervention and will allow physicians to better set expectations with their patients. Further work is needed to understand the role of opioid weaning as part of rehabilitation for surgery.
2533
P266: Evaluation of clinical outcomes and accuracy in transpedicular screw fixation for lumbar spondylolisthesis using a novel CT-guided navigation system
Gianluca Vadalà 1 , Giuseppe Francesco Papalia 1 , Fabrizio Russo 1 , Luca Ambrosio 1 , Paolo Brigato 1 , Domenico Franco 1 , Rocco Papalia 1 , Vincenzo Denaro 1
1 Research Unit of Orthopaedic and Trauma Surgery, Department of Orthopaedic and Trauma Surgery, Campus Bio-Medico University of Rome, Rome
Introduction: The use of intraoperative navigation and robotic surgery for minimally invasive lumbar fusion has been increasing over the past decade. Navigated and robotic systems have shown significant advantages in both patient care and surgical performance. The aim of this study was to evaluate postoperative clinical outcomes, intraoperative parameters, and accuracy of pedicle screw insertion guided by intraoperative navigation in patients undergoing lumbar interbody fusion for degenerative spondylolisthesis (DLS) using the novel navigation suite. Material and Methods: Patients affected by DLS who underwent posterior lumbar fusion interbody using intraoperative 3D navigation since April 2022 were included. Visual Analogue Scale (VAS), Oswestry Disability Index (ODI), and Short Form Health Survey-36 (SF-36) were assessed preoperatively (T0) and postoperatively at 1, 3, and 6 months (T1, T3, T6). Screw placement accuracy, measured by Gertzbein and Robbins classification, and facet joint violation, measured by the Yson classification, were assessed by intraoperative cone-beam CT performed at the end of instrumentation. Finally, operation time, intraoperative blood loss, hospital stay, and screw insertion time were evaluated. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 26. Continuous variables were presented as mean ± standard deviation. The paired samples t-test was used to compare the clinical scores at different follow-ups. Pearson correlation coefficient was used to correlate intra- and perioperative parameters. Values of p < 0.05 were considered statistically significant. Results: This study involved 50 patients with a mean age of 63.7 years. VAS decreased from 65.8 ± 23 (T0) to 35 ± 27.3 (T1), 22.7 ± 20.3 (T3), and 20 ± 22 (T6) (p < 0.01). ODI decreased from 35.4 ± 15% (T0) to 26.7 ± 16.3% (T1), 16 ± 12.4% (T3) (p < 0.01), and 11.8 ± 14% (T6) (p < 0.01). An increase of SF-36 from 51.5 ± 14 (T0) to 58.9 ± 18.6 (T1), 67.9 ± 18.4 (T3) (p < 0.01), and 76 ± 13 (T6, p < 0.01) was demonstrated. The accuracy of “perfect” and “clinically acceptable” pedicle screw fixation was 89.5% and 98.4%, respectively. Regarding facet violation, 96.8% of the screws were scored grade 0. Finally, the average screw insertion time was 4.3 ± 2 min, hospital stay was 4.2 ± 0.8 days, operation time was 205 ± 53 min, and blood loss was 169 ± 107 ml. Finally, statistically significant correlations between surgical time and hospital stay (p < 0.05), surgical time and blood loss (p < 0.01), surgical time and screw placement time (p = 0.01) were found. Conclusion: In this study, excellent results were demonstrated with regard to the accuracy of pedicle screw fixation and violation of facet joints with intraoperative navigation. VAS, ODI and SF-36 showed statistically significant improvements during the follow-up. Navigation is associated with reduced pedicle screw insertion time, hospital stay and blood loss, and adequate surgical time. However, this was influenced by decompression and number of instrumented levels. Navigation with intraoperative 3D imaging represents an effective approach to improve operative performance in the surgical treatment of DLS.
2581
P267: Treatment of a giant Tarlov cyst with intra-abdominal extension associated with hydronephrosis and recurrent urinary tract infections in a 46 year old male with Marfan Syndrome
Rani Nasser 1 , Daniel Webb 1 , Daryn Cass 1 , Rebecca Garner 1
1 Department of Neurosurgery, University of Cincinnati College of Meidicine, Cincinnati, USA
Tarlov cysts are a type of spinal meningeal cyst that arises from the perineurium of the dorsal root ganglion of nerves of the sacrum and are in communication with the spinal fluid in the thecal sac. They occur in up to 2% of the population but are largely asymptomatic. When symptomatic, symptoms frequently involve sacral pain, specifically when sitting, leg pain, changes in bowel and bladder function, as well as sexual dysfunction. In rare cases Tarlov cysts may erode through the sacral bone, and rarely into the prevertebral pelvic cavity. Previously reported cases have been predominantly in patients with Marfan syndrome, possibly related to weakened collagen.
Here we report the case of a 46 year old man with Marfan syndrome, prior ventriculoperitoneal shunting at birth, spinal fusion, aortic valve repair. He was known to have multiple Tarlov cysts, the largest of which was intra-abdominal and measured 20x10x11 cm and had increased significantly in size since imaging four years prior. He denied any sacral pain or radiculopathy, however, over the course of a year he developed progressive abdominal distention and recurrent urinary tract infections and was diagnosed with left sided hydroureter and hydronephrosis.
We describe the successful surgical treatment of the cyst via a posterior approach involving a left sacral two-three laminectomy with cyst drainage and imbrication with dural repair and revision of his non-functioning ventriculoperitoneal shunt.
2592
P268: How i do it: transforaminal endoscopic lumbar decompression by extraction of extravasated cement in upper lumbar spinal canal
Rohit Kavishkar 1
1 Department of Orthopaedics, Ng Teng Fong General Hospital, Singapore, Singapore
Objective: To evaluate the feasibility of transforaminal endoscopy in symptomatic cement extravasation into the spinal canal after vertebroplasty. Methods: A 71-year-old female after T12, L1 vertebroplasty for osteoporotic vertebral compression fracture at local hospital had relief of her back pain but started having new onset bilateral anterior thigh pain (Left > Right). On further evaluation at the local hospital her symptoms were diagnosed to have been due to T10-T11, T11-12 spinal stenosis for which she underwent T10-T12 posterior instrumented decompression and fusion. Her bilateral anterior thigh pain (Left > Right) did not resolve after the second operation and she was referred to us for second opinion. Evaluation of the CT and MRI scan showed extravasated cement into spinal canal of index vertebroplasty procedure was the cause for her symptoms. This was confirmed by temporary relief obtained after bilateral L1 selective nerve root block. We excised the cement through left transforaminal lumbar endoscopic decompression under local anaesthesia and she was completely relieved of her pain post-procedure. Discussion: Most common complication of vertebroplasty is cement extravasation. Although most of the cases of cement extravasation are clinically asymptomatic, some symptomatic cases require clinical intervention. New onset radiating pain or weakness should raise a suspicion of symptomatic cement extravasation. Results: Transforaminal endoscopic lumbar decompression is a safe and viable option to remove extravasated cement from vertebroplasty.
Keywords: cement extravasation, transforaminal endoscopy, radiculopathy, endoscopic spine surgery.
2595
P269: A technical note on combined uniportal unilateral laminotomy with bilateral decompression and interlaminar endoscopic lumbar discectomy surgery for cauda equina syndrome due to lower lumbar disc herniation with highly compromised spinal canal
Rohit Kavishkar 1
1 Dept of Orthopaedics, Clinical Fellow in Spine Surgery, Ng Teng Fong General Hospital, Singapore
Background: Traditionally open wide laminectomy and discectomy has been advocated in treatment of cauda equina syndrome caused by lumbar disc herniation. Our aim was to evaluate technical feasibility of uniportal interlaminar endoscopy in treatment of cauda equina syndrome. Methods: Nine patients with cauda equina syndrome underwent uniportal endoscopic decompression and discectomy from December 2020 to December 2022. Data was collected retrospectively. Patients diagnosed with cauda equina syndrome were operated within 6 hours of presentation to hospital. Visual Analogue Score (VAS), Oswestery Disability Index (ODI) and Bladder/Bowel scores were used to measure the outcome. Results: Analysis showed VAS scores for leg pain and back pain significantly decreased from preoperative scores of 8.22 ± 0.79 and 4.67 ± 1.76 to postoperative day 1 scores of 0.67 ± 0.67 and 2.56 ± 1.42, (p < 0.05). ODI scores improved from preoperative 52.33 ± 11.93 to postoperative (Day 1) 14 ± 6.80. Eight patients had early recovery (1 week) of bladder and bowel functions and one patient had delayed recovery at 8 months. None of the patient had residual bowel/bladder deficit. Based on Macnab’s criteria outcomes were excellent in all the patients at final follow-up. Conclusion: Uniportal endoscopic unilateral laminotomy for bilateral decompression with subsequent interlaminar endoscopic lumbar discectomy is safe and effective minimally invasive method of treatment in cauda equina syndrome as an alternative to open laminectomy in our cohort of patients.
Diagnostics
156
P270: In subjects with back and leg pain, does neuropathic pain exclusively correlate to neuronal compression? A correlation study of PainDETECT Questionnaire and corresponding MRI and X-ray findings
Stone Sima 1 , Sam Lapkin 2 , Ashish Diwan 1,3
1 Spine Labs, St George and Sutherland Clinical School, UNSW, Sydney, Australia
2 Southern Cross University, Faculty of Health, Bilinga, Queensland, Australia
3 Spine Service, St George Orthopaedics, Sydney, Australia
Purpose: Understanding the complex nature of low back pain (LBP) is crucial for effective management. The PainDETECT questionnaire is a tool that distinguishes between neuropathic (NeP), nociceptive (NoP), and ambiguous pain. This study aimed to investigate the relationship between PainDETECT scores and lumbar intervertebral degenerative and stenosis parameters obtained from paired imaging. Methods: A secondary review was conducted involving 279 consecutive patients, aged 18 years and above, who completed PainDETECT questionnaires and underwent lumbar MRI and/or X-ray scans. The study included 102 patients with nociceptive pain, 78 with ambiguous pain, and 99 with NePaccording to the PainDETECT questionnaire. Results: The NeP group had lower mean age (58.21 vs. 53.63, p < 0.05) and higher mean numerical rating scale score (7.9 5.9, p < 0.001) compared to the NoP group. A negative correlation was found between PainDETECT scores and pelvic incidence (τ = -0.177, p = 0.45). The neuropathic group exhibited significantly higher severity of foraminal stenosis (U = 18.962, p = 0.002), spinal stenosis (U = 14.481, p = 0.005), and Pfirrmann grade (U = 14.221, p = 0.028) compared to the nociceptive group. A significantly higher proportion of neuropathic patients had intervertebral disk bulge (96% vs. 78% vs. 78%, p = 0.002) and high-intensity zones (51% vs. 41% vs. 19%, p < 0.001) compared to those with nociceptive and ambiguous pain. Conclusion: Neuropathic pain, as determined by the PainDETECT questionnaire, is associated with more severe neural compression, increased presence of discogenic disease and inflammatory disk severity, and decreased pelvic incidence. This pioneering study establishes a connection between pathological findings and pain categorization, providing clinicians with valuable guidance for formulating tailored management plans and reducing the need for unnecessary pharmacotherapy, imaging, and non-targeted surgical interventions.
Keywords: low back pain, PainDETECT, NeP, nociceptive pain, stenosis, discogenic, instability
225
P271: Evaluating reliability and validity of the SOSGOQ 2.0 in Russian-speaking patients with spinal metastases
Nikita Zaborovskii 1,2 , Anton Denisov 3 , Adam Schlauch 4 , Dmitry Ptashnikov 1,5 , Sergei Masevnin 1 , Oleg Smekalenkov 1 , John Shapton 4 , Dimitriy Kondrashov 6
1 Spinal and Bone Oncology Surgery, Vreden National Medical Research Center of Traumatology and Orthopedics, Saint-Petersburg, Russian Federation
2 Saint-Petersburg State University, Saint-Petersburg, Russian Federation
3 Spinal Unit, Hospital Quirónsalud San José, Madrid, Spain
4 San Francisco Orthopaedic Residency Program, San Francisco, USA
5 Orthopedic Department, North-Western State Medical University named after I.I.Mechnikov, Saint-Petersburg, Russian Federation
6 Spinal Surgery, Dignity Health / Saint Mary’s Hospital, San Francisco, USA
Introduction: Patient-reported outcome measures evaluating health-related quality of life (HRQOL) provide valuable insights into the impacts of disease and treatment effectiveness. The Spine Oncology Study Group Outcome Questionnaire (SOSGOQ) is a validated tool specifically designed to assess HRQOL in patients with spinal metastases. The SOSGOQ 2.0 is the most recent iteration, demonstrating excellent psychometric properties across multiple language versions. Our objective was to translate and culturally adapt the SOSGOQ 2.0 into a Russian language version (SOSGOQ2.0_RUS), and validate its use as an HRQOL assessment tool in Russian-speaking patients with spinal metastases. Availability of a Russian SOSGOQ 2.0 will enable inclusion of this population in international multi-center studies utilizing this questionnaire. Material and Methods: We performed translation and back-translation of the SOSGOQ 2.0 according to established guidelines. The translated Russian version underwent pilot testing in 15 patients to confirm understandability, clarity and cultural appropriateness. After expert committee review, the final Russian version was tested in a prospective study of 64 patients with spinal metastases. Participants completed the SOSGOQ2.0_RUS alongside EQ-5D-5L, SF-36, and visual analog scales for pain intensity. Internal consistency of the SOSGOQ2.0_RUS was evaluated using Cronbach’s alpha. Test-retest reliability was assessed in a subset of 51 patients who completed the questionnaire twice within a 4-7 day interval. Reliability was quantified using intraclass correlation coefficients (ICC). Construct validity was examined through correlation of SOSGOQ2.0_RUS domains with the validated SF-36 questionnaire. Results: The SOSGOQ2.0_RUS demonstrated excellent internal consistency, with an overall Cronbach’s alpha of 0.87. The ICC for test-retest reliability was 0.88 (95% CI 0.81-0.93), confirming excellent reproducibility. ICC values for individual domains ranged from 0.65 to 0.94, indicating acceptable to high reliability. Construct validity was evidenced by significant correlations between SOSGOQ2.0_RUS and SF-36 domains measuring similar attributes. The Physical Function and Bodily Pain domains showed strong correlations (r = 0.71 and r = 0.65, respectively), while Mental Health showed more moderate correlation (r = 0.58). These findings align with validation studies of SOSGOQ 2.0 in other languages. Conclusion: The Russian version of the SOSGOQ 2.0 questionnaire was successfully translated and validated, and showed high reliability and construct validity. The questionnaire can be used as a reliable tool for assessing health-related quality of life in Russian-speaking patients with spinal metastasis. This study adds to the growing body of evidence supporting the use of SOSGOQ 2.0 in different languages and populations. The SOSGOQ2.0_RUS questionnaire can be used in clinical practice and research to evaluate HRQOL outcomes in Russian-speaking patients with spinal metastases. This will help to improve the management and treatment of these patients and ultimately improve their quality of life.
237
P272: Is it time to rethink traditional pain assessment methodologies? A correlation study between neuropathic low back pain defined by the PainDETECT questionnaire and patient reported outcome measures
Zachary Gan 1 , Stone Sima 1 , Sam Lapkin 2 , Ashish Diwan 1,3
1 Spine Labs
2 Faculty of Health, Southern Cross University, Bilinga, Australia
3 Spine Service, Department of Orthopaedic Surgery, St George and Sutherland Clinical School, University of New South Wales, Sydney, Australia
Purpose: The character of pain in the lower back remains complex. The painDETECT questionnaire (PD-Q) is a screening tool aimed at differentiating pain of primarily nociceptive, neuropathic, or indeterminate origin. The purpose of this study was to assess relationships between pain categories as described by the PD-Q and other measures of pain, disability, quality-of-life, and sociodemographic status. Methods: A retrospective analysis of patients presenting to the Spine Service at St George Private Hospital was performed. Completed PD-Q, Oswestry Disability Index (ODI), European Quality-of-Life 5 Dimensions 3-Level Version (EQ5D3L) and Numerical Rating Scale (NRS) forms were required. An analysis of covariance (ANCOVA) test was conducted comparing PD-Q to ODI and EQ5D3L. Subgroup ANCOVA concerning individual ODI and EQ5D3L components was also performed. Results: A positive association was found between PD-Q score and both ODI (τ = 0.369, p < 0.001) and NRS (ρ = 0.491, p < 0.001) scores. A negative association between PD-Q score and EQ5D3L score (τ = -0.322, p < 0.001) was shown. When confounded for NRS = 6.62, ANCOVA demonstrated a 22.9% higher ODI score (p < 0.001) and 28.41% lower EQ5D3L score (p < 0.001) in the neuropathic compared to nociceptive group. Individual EQ5D3L scores in the self-care (p < 0.05), usual activities (p < 0.05), pain/discomfort (p < 0.01) and anxiety/depression (p < 0.05) categories were higher in neuropathic pain compared to nociceptive. Individual ODI scores in pain intensity (p < 0.01), personal care (p < 0.001), lifting (p < 0.001), walking (p < 0.01), sitting (p < 0.01), standing (p < 0.001), sleeping (p < 0.001), sex life (p < 0.05), social life (p < 0.001) and travelling (p < 0.01) categories were higher in the neuropathic compared to nociceptive group. There was a higher prevalence of smokers in the neuropathic pain group compared to the nociceptive and ambiguous group (48.5% vs. 32.0% vs. 29.5%, p < 0.05). Conclusion: Patients suffering neuropathic pain as defined by the PD-Q experienced increased pain and disability levels in conjunction with lower quality-of-life, as demonstrated by higher NRS and ODI scores alongside lower EQ5D3L scores respectively. Smoking was associated with an increased likelihood of neuropathic pain. Various categories within both the ODI and EQ5D3L were more strongly associated with neuropathic pain. Overall, this study exemplifies the need to continue developing pain assessment methodologies that do not reduce an individual’s pain profile to a number or score.
330
P273: The utility of MRI-based vertebral bone quality scores as a predictor of cage subsidence following transforaminal and posterior lumbar interbody fusion
Ara Khoylyan 1 , Mina Girgis 2 , Alex Tang 2 , Frank Vazquez 1 , Tan Chen 3
1 Geisinger Commonwealth School of Medicine, Medicine, Scranton, USA
2 Orthopaedic Surgery Northeast Residency
3 Department of Orthopaedic Surgery, Geisinger Health, Wilkes-Barre, USA
Introduction: Interbody cage subsidence is a known complication following lumbar fusion procedures and can lead to poor surgical outcomes. Prior studies have demonstrated an association between cage subsidence and bone mineral density. In recent literature, Vertebral Bone Quality (VBQ) scores had been a proposed measure for bone density utilizing Magnetic Resonance Imaging (MRI). Spinal MRIs, which are frequently performed prior to fusion surgery and readily available, can offer a potential new and convenient method for preoperative screening for risk of subsidence. The purpose of this study was to determine: (1) if VBQ scores are associated with interbody cage subsidence following transforaminal and posterior lumbar interbody fusion (TLIF/PLIF) and (2) if there is a clinically sensitive threshold for subsidence. Material and Methods: A retrospective study was conducted on single-level TLIF or PLIF patients from 2007-2022 in a large integrated health system. Patients with non-degenerative diagnoses, multilevel or revision surgeries, inadequate radiographs, pre-operative MRI studies greater than two years prior to surgery were excluded. VBQ scores were calculated at L1-L4 using pre-operative T1-weighted MRI images. Changes in disc height (DH) and segmental lordosis (SL) were measured by comparing intraoperative and latest postoperative lateral radiographs. Cage subsidence was defined as > 2 mm difference in DH or > 5 degrees difference in SL. Descriptive and inferential statistics were performed. Results: A total of 96 patients met inclusion criteria. Average follow up was 18.6 months. Subsidence was found in 24 patients using the SL parameter (25%) and in 61 patients using the DH parameter (64%). VBQ scores were not significantly associated with the degree of cage subsidence based on DH (OR = 1.098, p = 0.717; correlation coefficient =.037; p = 0.720) or SL (OR = 1.296, p = 0.363; correlation coefficient = 0.093; p = 0.366) parameters. A VBQ cutoff value of 2.47 resulted in a sensitivity of 95.8% and specificity of 20.8% [area under curve (AUC) = 0.582] for detecting subsidence with SL. For detecting subsidence with DH, a VBQ cutoff score value of 1.69 resulted in a sensitivity of 98.4% and specificity of 2.9% (AUC = 0.500). No difference was found between subsidence and non-subsidence groups for age [p =.609 (DH); p =.884 (SL)], BMI [p =.703 (DH); p =.908 (SL)], gender [p =.059 (DH); p =.349 (SL)], or cage type [p = 0.594 (DH); p =.633 (SL)]. Conclusion: MRI-based VBQ scores were not associated with and should not be utilized as a pre-operative assessment tool for the risk of cage subsidence in patients undergoing TLIF/PLIF. Although not always clinically readily available, Dual-Energy X-ray Absorptiometry (DEXA) and Hounsfield Units (HU) derived from lumbar computed tomography (CT) scans appear to be superior clinical tools for pre-operative prediction of subsidence and bone mineral density.
335
P274: Diffuse idiopathic skeletal hyperostosis: a rare cause of dysphagia
Adnene Benammou 1,2 , Cherif Kamoun 1,2 , Ahmed Ben Abid 1,2 , Seddik Akremi 1,2 , Sofiene Kallel 3 , Mehdi Bellil 1,2 , Mohamed Ben Salah 1,2
1 University Tunis el Manar, Faculty of Medecine of Tunis, Tunis, Tunsia
2 Orthopedic Surgery Department, Charles Nicolle Hospital, Tunis, Tunsia
3 Maghreb Medical, Tunsia
Introduction: Diffuse Idiopathic Skeletal Hyperostosis (DISH) is an ossification of spinal entheses and tendons. Its cervical location can lead to dysphagia. We report a case report of a patient treated for dysphagia caused by cervical DISH. Material and Methods: A 65-year-old male was addressed for cervical DISH. Symptoms were dysphagia with neck pain and limitation of spinal mobility. Esophago-gastro-duodenal transit showed brutal stop of contrast agent at the level of C4. Surgery was decided mainly on dysphagia not on pain. Computed Tomography (CT) scan showed anterior osteophytes and reduction of the diameter of the trachea. Osteophytes were removed from an anterior cervical approach. Results: At day one postoperative, swallowing was significantly improved with reduction of local pain. At 6 months postoperative, the patient reported a significant improvement in swallowing, breathing and range of motion. Conclusion: Although rare, dysphagia in DISH patient is a rising problem. Surgical treatment with removal of osteophytes is effective for treating it. Surgery can be decided mainly on dysphagia with no other signs.
370
P275: Anxiety symptoms improvement after tubular microdecompression: a prospective study
Pedro Henrique Couri 1 , Alberto Gotfryd 1 , Eliane Antonioli 1 , Roberto Meves 1
1 Orthopaedics, Hospital Israelita Albert Einstein, São Paulo, Brazil
Introduction: The main indication for spine surgery is lumbar neural compression, mainly due to stenosis and disc herniation. When there is failure of conservative treatment or motor neurological damage, operative treatment should be indicated, with neural decompression being the gold standard. This procedure can be performed openly or microsurgical (with conventional or tubular retractors or endoscopic). When compared to open laminectomy, minimally invasive technique demonstrates similar effectiveness, however with less blood loss, shorter hospital stays and lower incidence of reoperation. Previous studies have shown association between symptoms of anxiety, depression, and chronic low back pain, but the relationship between symptoms and surgical results in individuals with radiculopathy is not well established in literature. Thus, the present study investigates the association between surgical outcomes and the presence of preoperative anxiety symptoms, in addition to the effects of surgery on patients’ mental health over time. Material and Methods: A prospective cohort study with 44 patients, with 6 months of follow-up (from 2020, January to 2022, July). Inclusion criteria: Patients who had symptoms of lumbar neural compression – radiculopathy or neurogenic claudication, with failure of the minimum conservative treatment for 6 weeks (or less if presence of acute motor damage). Exclusion criteria: Reoperations, complications, or lack of response to questionnaires six months after surgery. All patients included underwent minimally invasive decompression surgery at a single anatomical level, using the soft tissue tubular retraction method and microscopic magnification. Collected data were sent and stored in RedCap software before the surgery and 6 months after the surgery. Results: Comparing clinical scores preoperatively and 6 months after the procedure, improvement was observed in all scores (p < 0.05), regardless of group. Clinical improvement was observed by increases in self-perceived improvement (GPE), reductions in leg and back pain scores, and HADS scores for both subscales (depression and anxiety). 6 months after surgery, anxious patients maintained statistically worse mental health scores compared to non-anxious patients. However, the reduction in scores over the 6-month period was greater in anxious patients. That is, anxious patients maintained worse mental health scores after surgery compared to non-anxious patients, but had greater improvement, and indication a greater therapeutic effect of surgery. Conclusion: Lumbar microtubular decompression surgery seems to be not affected by preoperative symptoms of anxiety. These, in turn, improved after the operation.
570
P276: Unveiling the unexpected: co-occurrence of brain tumor and cervical spine pathology revealed after spine surgery
Shih Hsiang King 1 , Chih-Ju Chang 1
1 Department of Surgery, Division of Neurosurgery, Cathay General Hospital, Taipei City, Taiwan
Introduction: Brain tumors present with a variable clinical presentation, ranging from asymptomatic cases to seizure disorders, persistent headaches, cranial neuropathies, focal neurological deficits such as motor and sensory disorders, ataxia, and even behavioral abnormalities. These symptoms occasionally mimic other pathological conditions, including cervical radiculomyelopathy. We reported two cases diagnosed with huge meningioma done with recent cervical spine surgery, aims to differentiate between these two pathologies, which initially presented with comparable symptoms. Material and Methods: We present two patients admitted due to paresthesia, slight motor weakness in the upper limbs, and gait disturbances, led to an initial diagnosis of cervical radiculomyelopathy, supported by evidence of cord compression revealed by cervical MRI. Both patients subsequently underwent open-door laminoplasty. Results: In one patient, persistent symptom prompted further investigation, which led to the identification of a sizable meningioma shown in brain MRI three months post-surgery. The other patient experienced symptom relief after the surgery but was later diagnosed with a meningioma three years following the initial procedure due to seizure attack. Both patients ultimately underwent tumor excision, demonstrating favorable surgical outcomes. Conclusion: The diagnosis of the disease can be guided by history, physical exam, and imaging. Thorough neurological assessments, particularly involving mental status evaluation, cranial nerve examinations, and analysis of neurologic defect patterns and distributions, are crucial for early detection of brain lesions. Radiological assessments, involving brain MRI to determine location, mass effect, and edema, as well as cervical spine MRI to correlate degenerative findings with clinical symptoms. When a patient with cervical radiculomyelopathy presents atypical symptoms, or do not correlate with the findings from imaging, the potential existence of a brain lesion should be considered.
814
P277: The risk of misdiagnosis in spinal hypertrophic pachymeningitis
Hiroshi Kageyama 1
1 Neurosurgery / Spinal Surgery, Shin-Kuki General Hospital, Kuki, Japan
Introduction: Hypertrophic pachymeningitis (HP) is a relatively rare inflammatory disease of the central nervous system, with an incidence rate of 9.9 per one million in Japan. While it typically manifests in the cranium, spinal cases are exceptionally rare and may present with mass effect. Material and Methods: We conducted a retrospective chart review of operative cases related to spinal diseases over the past five years (from July 2018 to June 2023). From this pool, we identified patients who had received a diagnosis of HP. Results: We conducted a review of 666 operative spinal cases, among which we encountered two cases of spinal HP. Case 1: A 69-year-old female with a medical history of autoimmune hepatitis and left breast cancer presented with severe back pain without paresis or sensory disturbance in her lower extremities. MRI scans of her thoracic spine revealed an intradural extramedullary mass with strong contrast enhancement in the ventral side of the spinal cord at the T1-T4 vertebral level. The initial radiological diagnosis indicated a thoracic meningioma, leading to a consultation with our team. However, her condition was accompanied by mild elevation in CRP (3.16 mg/dL), prompting consideration of HP. Further blood test revealed markers suggestive of an autoimmune disease (IgG4: 139 mg/dL, MPO-ANCA positive). We performed thoracic laminectomy, biopsied the thickened dura on the dorsal side, and conducted expansive duraplasty. The pathological diagnosis confirmed HP. Treatment included immunosuppressive therapy with rituximab and prednisolone, resulting in the disappearance of the mass four weeks later. Case 2: A 67-year-old male with a history of L4/5 lumbar disc hernia, for which he underwent TLIF surgery three years prior, reported bilateral thigh pain two years post-operation. MRI revealed a mass resembling a disc hernia at the L2/3 intervertebral level. Over time, the mass increased in size, and his thigh pain persisted. Initially planning microdiscectomy, we encountered difficulties during the extradural approach. Subsequently, we opened the dura and removed the extramedullary mass located between the cauda equina nerves. Pathological analysis confirmed HP associated with IgG4-related disease. Treatment involved administration of prednisolone and azathioprine, and follow-up MRI scans revealed the complete disappearance of the mass two months later. Conclusion: We encountered two operative cases of spinal pachymeningitis, and in both instances, the initial diagnoses differed. Due to its rarity, spinal HP has the potential to be misdiagnosed, particularly when it presents with characteristics resembling tumours or disc hernia.
916
P278: Indocyanine green as a marker for tissue ischemia following extended operative times in spinal surgery
Max Ward 1 , Roee Ber 1 , Daniel Schneider 1 , Daniel Sciubba 1 , Dennis Knobel 2 , Larry Lo 1
1 Neurosurgery
2 Plastic Surgery, Zucker School of Medicine at Hofstra/Northwell, Manhasset, USA
Introduction: Complex spine surgeries such as spinal tumor resections or long-segment spinal fusions often require large exposures, extended periods of tissue retraction and significant blood loss. In these cases, the spinal musculature is exposed to various forms of hemodynamic compromise and as a result may be prone to intraoperative ischemia. Indocyanine green (ICG) is a fluorescing dye with emission within the infrared spectrum making it easier to penetrate deeper tissues for visualization than other dyes. Commercially available handheld imaging systems allow for real-time visualization of tissue perfusion using infrared light, and has shown utility in DIEP flap reconstruction, tissue debridement, and colorectal anastomosis. This study aims to assess the usability of ICG to analyze soft tissue viability following complex spine procedures extending over 8 hours. Material and Methods: Three cases requiring over 8 hours of operative time were chosen for ICG utilization. Cases included one en bloc malignant peripheral nerve sheath tumor resection and two long-segment fusions with corpectomies and anterior column reconstruction for metastatic spine disease. Following the conclusion of hardware placement and tumor resection, 12.5mg of ICG was intravenously injected. A handheld infrared camera was utilized to visualize tissue fluorescence prior to plastic surgery closure. The ICG fluorescence was qualitatively assessed by the neurosurgery and plastics surgeons involved in the cases, and images were recorded. Results: Prior to injecting ICG, there was no clear identification of the non-coagulated devascularized tissue. After injection of ICG, a clear difference between vascularized (fluorescing) and devascularized (non-fluorescing) tissue was identified. Coagulated and extensively retracted musculature tended to express no fluorescence. This has been consistent over all three cases. In one case where a horizontal limb was incorporated to get exposure to the S1 ala and iliac wing from a posterior approach for a T-shaped incision, it was clear that transaction of the muscles and subsequently, the gluteal artery perforators lead to large segments of the muscle being ischemic and devascularized compared to the contra lateral side. Conclusion: ICG is frequently utilized in tissue perfusion studies, but its use for this purpose in spine surgery is novel. It may be particularly useful in longer operations, in the post-radiation setting, or revision surgeries where soft tissue viability is potentially compromised at the end fo the case. The ramifications of leaving large areas of ischemic tissue during spinal closure has not yet been shown. This study serves as a proof of concept for using ICG as a marker for tissue ischemia after complex spine surgery. Further studies are warranted in order to establish the clinical implications of this method such as the extent of debridement and reconstruction necessary to prevent wound dehiscence and infections.
1003
P279: Mathematical evaluation for influence of pelvic rotation on pelvic incidence using point rotation in the three-dimensional coordination system
Yunjin Nam 1 , Jungwook Lim 1 , Sangmin Lee 1 , Young Bin Lee 1 , Seung Woo Suh 1
1 Department of Orthopaedics, Korea University Guro Hospital, Seoul, South Korea
Introduction: Measure of pelvic incidence may be influenced by position and orientation of the pelvis because the three-dimensional anatomic parameter is measured on a two-dimensional radiograph. To evaluate the difference between the actual pelvic incidence (aPI) and measured pelvic incidence (mPI) in rotated pelvis using geometric calculation. Material and Methods: Assuming that the center of the femoral head is symmetrically positioned on the Z-axis of the three-dimensional coordinate system and the center of the upper surface of the sacrum on the XY plane. Then, the angle between the line with a slope of (90º - pelvic tilt) and a line with a slope of (90º - sacral slope) is aPI. The mPI of the rotated pelvis can be measured by angle between two lines after rotation of φ about X-axis (vertical rotation) and rotation of θ about Y-axis (horizontal rotation) and then drawing a positive projection on the XY plane. The rotational transformation was calculated using a rotation matrix. The difference between aPI and mPI less than 6 ° was considered as acceptable. Results: According to mathematical calculations, the mPI value of the rotated pelvis appears as a function of the four values of aPI, PT, θ, and φ. For example, when aPI = 50º, PT = 10º, θ = 10º and φ = 20º, mPI is 53.2º. More horizontal rotation makes mPI smaller and more vertical rotation makes the mPI larger. In aPI of 30º, 40º, 50º, 60º, 70º and PT of 10º, acceptable vertical and horizontal rotation is (34º, 37º), (30º, 33º), (26º, 31º), (23º, 31º), (20º, 32º). In aPI of 30º, 40º, 50º, 60º, 70º and PT of 20º, acceptable vertical and horizontal rotation is (34º, 37º), (30º, 32º), (28º, 30º), (26º, 28º), (24º, 28º). 20º of vertical rotation and 16º of horizontal rotation is acceptable for every aPI and PT. Conclusion: The error of measured PI according to the pelvic rotation could be calculated using geometric model. Acceptable horizontal and vertical rotation changes according to the aPI and PT.
1196
P280: The guiding value of ultrasound-guided selective nerve root block in the treatment of multi-level lumbar degeneration disease
Chao-Yuan Ge 1 , Ding-Jun Hao 1
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
Introduction: At present, the surgical decision making for multi-level lumbar degenerative disease remains controversial. The aim of this study is to explore the guiding value of ultrasound-guided selective nerve root block (SNRB) in surgical treatment decision making in patients with multi-level lumbar degenerative diseases. Material and Methods: A retrospective analysis was performed on 86 patients with multi-level lumbar degenerative disease who were surgically treated in our hospital from January 2019 to October 2021. The patients were divided into SNRB group and non-SNRB group according to whether or not they underwent SNRB before surgery. There were 46 patients in the SNRB group. Their responsible segments were identified by ultrasound-guided SNRB, combined with symptoms and imaging examination before surgery. Then decompression was performed on the responsible segments. A total of 40 patients in the non-SNRB group, and extensive multi-level lumbar spinal canal decompression was performed because their responsible segments were not clear. The operative time, intraoperative blood loss, the VAS score and JOA score of lumbar and leg pain before surgery, the 3rd day after surgery, 6 months after surgery, and the last follow-up were recorded and compared between the two groups, and the occurrence of intraoperative complications were also recorded. Results: The operation was successfully completed in both groups, and no serious complications occurred during surgery. One case of dural tear occurred in the non-SNRB group and was repaired intraoperatively. In the SNRB group, the operative time was (90.5 ± 17.5) min and the blood loss was (280.7 ± 29.7) ml, while in the non-SNRB group, the operative time was (180.4 ± 25.3) min and the blood loss was (945.6 ± 175.3) ml. The operative time and blood loss in SNRB group were significantly smaller than those in non-SNRB group. The VAS scores and JOA scores of low back pain and leg pain in SNRB group were better than those in the non-SNRB group on the 3rd day after surgery, 6 months after surgery and at the last follow-up, with statistical significance (p < 0.05). No loosening, or displacement of the internal fixation were found in the two groups, and the bone grafting healed well. Conclusion: This study showed that preoperative ultrasound-guided SNRB could identify the responsible segments that really need decompression for patients with multi-level lumbar degenerative diseases, and could provide very important guiding value for surgery.
1298
P281: Multicenter validation of CT criteria for posterior ligamentous complex injury of the thoracolumbar spine
Mohamed Ali 1
1 Prince Mohamed Bin Abdelaziz Hospital, Riyadh, Saudi Arabia
Introduction: Two recent single-institution studies have proposed criteria for posterior ligamentous complex (PLC) status in Computed Tomography (CT) based on the number of positive CT findings. PLC should be considered injured if ≥ 2 positive CT findings based on a high positive predictive value (PPV, 91%) for PLC injury in MRI, indeterminate PLC (M1 modifier) if there is a single positive CT finding (PPV 31%), and intact if there are no positive CT findings (PPV 9%). This retrospective multicenter study aims to validate those CT criteria for PLC injury in a large, independent population from diffident settings. Materials & Methods: Three hundred fifty-seven consecutive patients with at least one vertebral body fracture (T1-L5) who underwent CT and MRI within ten days of injury will be enrolled in participating centers. Patients with translation injury, osteoporotic or pathological fractures or incomplete imaging were excluded. At least two reviewers from each center will assess CT for the following findings according to proposed definitions: facet joint malalignment, facet joint widening, horizontal laminar fracture, spinous process fracture, and interspinous widening. The reference standard is PLC injury defined by black stripe discontinuity due to supraspinous or ligamentum flavum rupture. Each reviewer will interpret all de-identified CT/ MRI images independently, blinded to clinical data and other readings, within a 4-week interval. When the two reviewers disagreed about the MRI's PLC status or the Number of CT findings, the case was resolved by a third reviewer. Prior consensus training will be done for all reviewers to standardize the imaging interpretation protocol. Multivariate association between CT findings and PLC injury will be examined. Results: The preliminary results from multiple centers will be presented. The diagnostic accuracy of combinations of those CT findings with independent association with PLC injury will be examined (0, 1, ≥ 2 findings). The following measures will be reported: sensitivity, specificity, accuracy, positive and negative predictive values, and positive and negative likelihood ratio. Inter-intraobserver reliability in identifying each CT finding or combinations of CT findings will be assessed using Cohen’s kappa (k) and Fleiss kappa statistics. Conclusion: We provided a comprehensive methodology for a multicenter validation of a CT criteria for PLC injury. A multicenter design is needed to improve generalizability of the findings. A retrospective study with well balanced study population is more feasible thana prospective design.
Keywords: posterior ligamentous complex, thoracolumbar fractures, imaging algorithm, computed tomography, magnetic resonance imaging
1549
P282: Comparing MRI-findings and tissue results in patients with clinically suspected spinal tuberculosis: preliminary results of the Spinal TB X cohort
Julian Scherer 1,2 , Maritz Laubscher 1 , Tessa Kotze 1 , Sandra Mukasa 1 , Ferdinand Oompie 1 , Karen Wolmarans 1 , Reto Guler 1 , Prof Rob Dunn 1 , Michael Held 1 , Friedrich Thienemann 1,2
1 University of Cape Town, Cape Town, South Africa
2 University of Zurich, Zurich, Switzerland
Introduction: The diagnosis of extrapulmonary tuberculosis (EPTB) remains challenging simply because sample collection requires invasive procedures in the absence of a blood-based diagnostic test. The gold-standard imaging modality for detecting spinal tuberculosis (STB) is magnetic resonance imaging (MRI) with a reported specificity and sensitivity of above 90% in detecting spondylodiscitis. In this preliminary analysis we assessed the diagnostic accuracy of MRI of the first 17 participants enrolled in Spinal TB X (clinicaltrials.gov: NCT05610098). Material and Methods: The Spinal TB X cohort is an ongoing prospective cohort study describing the clinical phenotype of spinal TB using whole-body 18FDG-PET/CT (PET/CT) and MRI at baseline with repeated PET/CT at six- and 12-months to monitor treatment respond. In addition, gene-expression profiling is being conducted at these time-points. Results: At the time of submission, 49 patients were screened of which 17 patients have been enrolled (35.3% female, 23.5% HIV-infected, median age 47.0 years, IQR 19.5) and underwent PET/CT and MRI. One patient was excluded due to loss to follow-up. Of the remaining 16 patients with suspected STB on MRI, 14 patients have completed microbiological workup of the spinal lesions at the time of submission. Eleven (78.6%) patients had microbiological confirmed STB on spinal tissue specimens. The other three patients with suspected STB on MRI had the following confirmed diagnosis on biopsy: Plasmocytoma, Mycobacterium avium complex spondylodiscitis and metastatic adenocarcinoma. The mean count of spinal lesions detected by MRI did not differ between patients with confirmed STB and patients with other diagnosis (mean 1.20, SD 0.63 versus mean 1.0, SD 0.00, p = 0.343). The mean count of vertebra per spinal lesion detected by MRI did also not differ between the groups (mean 2.30, SD 0.48 versus 2.0, SD 0.00, p = 0.319). The following accuracy for the detection of spondylodiscitis and tuberculous spondylodiscitis was calculated using our preliminary data set. MRI detected spondylodiscitis correctly in 12 patients (85.7%). STB was correctly detected in 11 patients (78.6%). Conclusion: Despite being imaging gold-standard modality in detecting spondylodiscitis and STB, in our preliminary analysis MRI performed acceptable in patients with microbiologically confirmed STB. More detailed analysis will be made available with increasing sample size.
1592
P283: Role of CT based Hounsfield Units in identifying spinal osteoporosis and patients at risk for inferior outcomes after lumbar spinal fusion
Delano Trenchfield 1 , Omar Tarawneh 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Olivia Opara 1 , Michael McCurdy 1 , Nathaniel Pineda 1 , Fatimah Alhassan 1 , Michael Vo 1 , Matthew Meade 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Orthopaedic Surgery, Rothman Institute, Thomas Jefferson, Philadelphia, USA
Introduction: Rates of osteoporosis is a growing public health concern, and the burden is expected to increase with an aging population. Poor bone quality is a significant risk factor for complications after spine surgery. Despite this, osteoporosis remains underdiagnosed and undertreated. Although cost effective modalities for assessment of osteoporosis exist, nearly one-half of women indicated for screening do not undergo screening. Adding to this, 80% of fragility fractures occur in patients without a prior DEXA while historically underserved patients continue to have osteoporosis screening rates of < 10%. Considering the low rates of screening, opportunistic CT scans represent a viable opportunity to identify patients at risk for postoperative complications and decreased PROMs without additional cost or radiation. Moreover, CT scans are often obtained during preoperative assessment, therefore evaluating bone attenuation on CT as a surrogate for BMD may prove valuable in risk stratification of at-risk groups. To date, the literature remains sparse when assessing the utility of bone attenuation as measured by Hounsfield Units (HU) to predict PROMS after lumbar fusion. Therefore, the purpose of this study was to determine if decreased bone density on abdominal CT predicts inferior PROMs after lumbar fusion. Secondarily, we compared radiographic and surgical outcomes between groups. Material and Methods: All patients ages > 18 from 2017-2022 who underwent lumbar fusion for degenerative lumbar disease at our academic center were included. Exclusion criteria consisted of revision surgery, trauma, infection, absence of preoperative abdominal CT within six months of surgery, and incomplete 1-year PROMs. HU was used as a surrogate for assessing bone mineral density. HU was obtained from click and drag of the L1 vertebral body as studies suggest L1 has the greatest correlation with Tscore on DEXA. Attenuation thresholds for HU were set at < 110 which has been shown to achieve a sensitivity of 90% in differentiating osteoporosis from normal bone. Baseline demographics, surgical characteristics and PROMs were collected. Postoperative radiographs, screw loosening and subsidence were measured. Bivariate analyses were used to compare preoperative characteristics and postoperative outcomes between osteoporotic and non-osteoporotic patients. A multivariable regression model accounting for demographics and surgical characteristics was conducted to measure the effect of osteoporosis on PROMs. Results: A total of 119 patients met inclusion criteria, of which 38% were osteoporotic. Compared to patients with normal bone architecture, osteoporotic patients were more likely to be older (66.4 ± 11.8, p < 0.001) but no difference in patient characteristics were identified. Patients in both groups experienced a similar rate of subsequent revisions (p = 0.216), 90-day readmissions (p = 0.633), and complications (p = 0.776). Osteoporotic patients had greater rates of screw loosening (16.0% vs 8.2%, p = 0.011) but there was no difference in incidence by proportion of patients (51.6% vs. 34.5%, p = 0.117). On bivariate analysis, there were no differences in the degree of improvement postoperatively for all PROM measures. Conclusion: Osteoporotic patients encountered greater rates of screw loosening. Osteoporotic status was shown to be independently associated with significantly less improvement in VAS-Back. There was no significant difference shown with regards to 90-day readmissions, complications or need for revision.
1613
P284: Spinal Instability Neoplastic Score (SINS): where does it fall short?
Michael McCurdy 1 , Parker Brush 1 , Jeremy Heard 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Tyler Henry 1 , Teeto Ezeonu 1 , Alexa Tomlak 1 , Thomas Swiderski 1 , Emma Hammelef 1 , Caleb Yeung 1 , William Conaway 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1
1 Orthopaedic Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: Due to the medical and surgical complexity of patients with metastatic spine disease, various grading criteria have been developed to determine who should receive surgical intervention. One score that has been used effectively and commonly since its creation in 2010 is the Spinal Instability Neoplastic Score (SINS). Patients with scores ≤ 6, 7-12, and ≥ 13 are indicative of stability, indeterminate instability, and instability, respectively. Though the SINS criteria has proven a reliable tool for assessment of stability in patients with spine tumors among clinicians within orthopaedics and across other specialties, it has not provided clear insight into management recommendations for patients in the indeterminate instability group. Given the paucity of literature on patients that fall into this indeterminate group, we aim to evaluate this subset of patients at our own institution to identify characteristics and symptoms that led providers to proceed with either operative or nonoperative management. Material and Methods: After Institutional Review Board approval, surgical consults for patients with documented neoplastic spine disease at a single, tertiary care institution were identified from 2008-2021. Patient characteristics, surgical details, and cancer diagnoses were collected via chart review. If a patient received operative treatment, the indication for intervention listed in the corresponding operative note was also recorded. A trained orthopaedic resident calculated a Spinal Instability Neoplastic Score (SINS) for each patient by summation of six domains that were identified on computed tomography (CT): 1) location 2) mechanical pain 3) bone lesion 4) alignment 5) vertebral body collapse 6) posterolateral involvement. Descriptive analysis was performed to characterize differences between patients who were treated operatively vs. nonoperatively. Results: 82 patients were identified with neoplastic spine disease and consult to orthopaedic spine surgery. Four patients had a SINS of ≤ 6 and were treated nonoperatively. Three patients had a SINS ≥ 13, two of which were treated operatively, and one of which was recommended surgery and subsequently lost to follow-up. 75 patients (91.5%) had a SINS between 7-12, placing them in the indeterminate stability category. 61 of these patients (81.3%) were treated operatively and 14 (18.7%) were treated nonoperatively. In the operative group, indications for surgery included cord compression (47.5%), progressive neurological deficits (44.3%), progressive pain (24.6%), instability (24.6%), cauda equina (11.5%), and need for biopsy (11.5%). In the nonoperative group, indications for conservative management included no focal deficit (50%), stable fracture (28.6%), non-spine pathology (21.4%), patient declining surgery (14.3%), and chemoradiation therapy (14.3%). In the SINS 7-12 group, 1-year mortality was higher in the operative vs. nonoperative cohort (22.95% vs. 14.29%). Prevalence of metastatic disease was similar between the two groups (78.7% vs. 78.6%). Conclusion: Our study found that management of patients in the 7-12 group is determined predominantly by neurological symptoms, pain, and need for biopsy. Given the large proportion of patients that fall into the indeterminate stability category, development of a more comprehensive grading system may be useful to aid in optimizing operative or nonoperative management of patients with neoplastic spine disease.
1795
P285: Characteristics of spinal morphology according to "current" and "theoretical" Roussouly Classification Systems in a diverse, asymptomatic cohort: multi-ethnic alignment normative study (MEANS)
Yong Shen 1 , Zeeshan Sardar 2 , Matan Malka 2 , Prerana Katiyar 1 , Gabriella Greisberg 1 , Fthimnir Hassan 2 , Justin Reyes 2 , Jean Charles Le Huec 3 , Stephane Bourret 3 , Kazuhiro Hasegawa 4 , Wong Hee Kit 5 , Gabriel Liu 5 , Denni Hey 5 , Hend Riahi 6 , Michael Kelly 7 , Joseph Lombardi 2 , Lawrence Lenke 2
1 Orthopedic Surgery, Columbia University Medical Center, New York, USA
2 Orthopedic Surgery, Columbia University Medical Center/NewYork Presbyterian Och Spine Hospital, New York, USA
3 Spine Unit 2, Surgical Research Lab, Bordeaux University Hospital, Bordeaux, France
4 Niigata Spine Surgery Center, Niigata City, Japan
5 Department of Orthopedic Surgery, National University Hospital (Singapore), Singapore
6 Institut Kassab d'Orthopédie, Ksar Said La Manouba, Tunis, Tunisia
7 Orthopedic Surgery, Rady Children's Hospital, San Diego, USA
Introduction: The Roussouly classification system is commonly used to classify spine morphology into distinct types. Recent literature suggests that the system could be applied to the adult spinal deformity (ASD) population and that restoration of parameters to a “theoretical” Roussouly type based on pelvic incidence (PI) may improve outcomes. We analyzed a large, multiethnic, asymptomatic cohort to classify spinal morphology using the Roussouly system and assessed sagittal alignment. Methods: 467 healthy volunteers without spinal disorders were recruited from spine centers in 5 countries as part of the Multi-Ethnic Alignment Normative Study (MEANS). Radiographic parameters were measured via the EOS imaging system. “Current” and “theoretical” Roussouly classification was assigned to 467 volunteers with sagittal whole spine imaging using sacral slope (SS) and PI, respectively, and the lumbar apex. One-way analysis of variance (ANOVA) was performed to compare subject characteristics across Roussouly types, followed by post hoc Bonferroni correction. The significance level was set to p < 0.05. Results: In the MEANS cohort, “current” Roussouly Type 1 constituted 7.5% (35/467), Type 2 21.4% (100/467), Type 3 47.5% (222/467), Type 4 23.6% (110/467). A subgroup of Type 3 with anteverted pelvis (Type 3AP) constituted 11.1% (52/467). “Theoretical” Roussouly Type 1 comprised 5.8% (27/467), Type 2 18.6% (87/467), Type 3 55.9% (261/467), Type 4 19.7% (92/467) of the cohort. 11.6% (54/467) of subjects had “theoretical” Type 3AP as a subgroup of “theoretical” Type 3. The mean PI in “current” Roussouly Type 1 was 40.8°, Type 2 43.6°, Type 3 52.4°, Type 4 62.4°, Type 3AP 43.7°. The mean PI in “theoretical” Roussouly Type 1 was 36.5°, Type 2 39.1°, Type 3 52.5°, Type 4 67.3°, Type 3AP 51.0°. The difference in PI between “current” and “theoretical” Roussouly types was significant for Type 1 (p = 0.02), Type 2 (p < 0.001), Type 4 (p < 0.001), and Type 3AP (p < 0.001) but not Type 3 (p = 0.85). PI-LL mismatch did not differ significantly between any “current” types but did between “theoretical” types. The mean PI-LL mismatch of Type 1 (-7.5°) differed from Type 4 (2.2°) (p < 0.001), Type 2 (-10.9°) from 3 (-6.1°) (p = 0.001) and 4 (p < 0.001), and Type 3 differed from Type 4 (p < 0.001). 34.7% (162/467) subjects had a “current” Roussouly type different from the “theoretical” type. Type 3 theoretical shape had the most frequent mismatch, constituting 61.1% (99/162) of the mismatched subjects, where 51.5% (51/99) of mismatched Type 3 become “current” Type 4. Discussion and Conclusion: The Roussouly classification system applies to a large, multi-ethnic, asymptomatic cohort. The distribution of Roussouly types differs depending on whether the “current” classification using SS, or the “theoretical” using the PI are employed. A sizeable proportion of asymptomatic, non-pathologic subjects exhibit “current” and “theoretical” mismatch, highlighting the need to interpret the influence of spinal deformity on sagittal alignment cautiously when utilizing the Roussouly system.
1862
P286: Cross-cultural validation and adaptation to Spanish of the AOSpine PROST (Patient Reported Outcome Spine Trauma) questionnaire in Latin America
Ignacio Cirillo 1,2,3 , José Via Dorado 1,4 , Ratko Yurac 5,6 , Gonzalo Kido 7 , Victor Barrientos 1 , Pablo Carreño 1,4 , Guillermo Ricciardi 8 , Hugo Vilchis Samano 9,10,11
1 Hospital del Trabajador, Santiago, Chile
2 Clínica Universidad de los Andes, Santiago, Chile
3 Hospital San José, Santiago, Chile
4 Facultad de Medicina, Universidad Nacional Andrés Bello, Hospital del Trabajador, Santiago, Chile
5 Department of Orthopedic and Traumatology, Universidad del Desarrollo, Santiago, Chile
6 Clínica Alemana de Santiago, Santiago, Chile
7 Instituto de Ortopedia y Traumatología “Carlos E. Ottolenghi”, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
8 Centro Médico Intefrel Fitz Roy, Buenos Aires, Argentina
9 Instituto Mexicano del Seguro Social, Torreón, Mexico
10 Hospital de Traumatología y Ortopedia Lomas Verdes, Ciudad de México, Mexico
11 Universidad Nacional Autónoma de México, Ciudad de México, Mexico
Introduction: The AOSpinePROST questionnaire is a reliable and valid tool for assessing physical functioning in patients with spinal cord injury. However, it has not yet been validated for use in Latin America. Therefore, this study aims to validate the Spanish version of the AOSpinePROST (Patient Reported Outcome Spine Trauma) questionnaire in Latin America. Material and Methods: Forty-eight patients were selected from medical centers in Chile, Argentina, Mexico and Peru. Patients completed the AOSpinePROST and SF-36 instruments to assess concurrent validity. Descriptive statistics were used to analyze demographic and clinical characteristics and floor and ceiling effects were examined. Internal consistency was assessed using Spearman correlation tests, and the relationship between items of the AOSpinePROST and the SF-36 was analyzed. Results: Of the 48 patients included, 54.2% were male, 75% of Chilean nationality, with a mean age of 50.9 years and a median of 91.5 days since the accident. The most common mechanisms of injury were vehicular accidents and falls (41.7% each). The most affected region was the thoracic spine (47.9%), and the most frequent type of fracture was type A according to the AO classification (66.7%). In terms of therapeutic management, 52.1% received conservative treatment. No floor or ceiling effects were observed. Significant Spearman correlations were found, ranging from moderate to strong, with a range of 0.4690 to 0.8638 (p < 0.001). The strongest correlation was observed for SF-36 Physical Function (r = 0.8638; p < 0.001). Conclusion: The Spanish version of the AOSpinePROST questionnaire has proven to be a reliable and valid tool to assess the physical function of spinal trauma patients in Spanish-speaking Latin America, providing valuable clinical information for the comprehensive approach of these patients in the region.
1916
P287: Defining cage subsidence in anterior, oblique, and lateral lumbar spine fusion approaches. A systematic review of the literature
Alexander Aguirre 1 , Mohamed Soliman 1 , Asham Khan 1 , Esteban Quiceno Restrepo 1 , Cathleen Kuo 1 , Jeffrey Mullin 1 , John Pollina 1
1 Neurosurgery, University at Buffalo Neurosurgery, Buffalo, USA
Introduction: One of the most common complications of lumbar fusions is cage subsidence, which leads to collapse of disc height and reappearance of the presenting symptomology. However, definitions of cage subsidence are inconsistent, leading to a variety of subsidence calculation methodologies and thresholds. The aim of this study was to review previously published literature on cage subsidence in order to present the most validated methods for calculating and defining subsidence in the anterior lumbar interbody fusion (ALIF), oblique lateral interbody fusion (OLIF), and lateral lumbar interbody fusion (LLIF) approaches. Materials and Methods: A search was completed in PubMed and Embase with inclusion criteria focused on identifying any study that provided descriptions of the methodology, imaging modality, or subsidence threshold used to calculate the presence of cage subsidence. Results: A total of 69 studies were included in the final analysis, of which 18 (26.1%) reported on the ALIF approach, 22 (32.0%) on the OLIF approach, and 31 (44.9%) on the LLIF approach, 2 of which reported on more than one approach. ALIF studies most commonly used the loss of disc height over time with a subsidence threshold of > 2 mm. Most OLIF studies used is the total amount of cage migration into the vertebral bodies, with a threshold of > 2 mm. LLIF was the only approach in which a large majority of studies applied the same method for calculation, namely, loss of disc height over time. Conclusion: We recommend future studies adhere to this series of the most validated methodologies to ensure accuracy and generalizability in reporting cage subsidence.
1948
P288: Measurement of spinal muscle function with spinal motion angle in normal Korean young adults using POM checker
Min-gu Jang 1 , Hyun-jae Cha 1 , Sung-jun Moon 1 , In-uk Yeo 1
1 Orthopaedic Surgery, Konyang University Hospital, Daejeon, South Korea
Introduction: As an alternative to directly measuring spinal muscle strength, the spinal angle of motion in normal Korean young adults were measured using a machine called POM checker. By presenting normal values for normal young adults and comparing them with indicators of pathological conditions, it can be used as an indicator of recovery after surgery and is expected to provide a standard for leading to good clinical results. Material and Methods: The spine motion angle was measured using a POM checker machine for normal 30 adult men and women in their 20s and 30s, from May 2023 to October 2023. POM checker is a markerless motion capture system. This is a machine that measures the angle when the patient is in the maximum possible flexion, extension, and side bending posture. Results: The overall average bending angle was 70.2 degrees, men 69.9 degrees, women 72.8 degrees. The overall average extension angle was 31.6 degrees for men, 32.5 degrees for women, 22.3 degrees. Left lateral bending angle overall average 33.1 degrees, men 33.1 degrees, women 33.3 degrees The overall average right lateral bending angle was measured at 34.5 degrees for men, 34.7 degrees, and 32.6 degrees for women. Conclusion: Through this study, by presenting the normal values of spinal motion angle according to gender/age, it is possible to check in advance the risk of the patient's surgery before surgery by comparing it with the patient's values, and the extent of the patient's recovery by comparing it with the normal values after surgery. Its significance is that it not only allows you to know, but also allows you to perform appropriate post-surgical rehabilitation treatment or obtain information about the degree of future recovery.
2057
P289: Do patients accurately recall their pain levels following sacroiliac joint steroid injection? A cohort study of recall bias in patient-reported outcomes
Davin Gong 1 , Aditya Muralidharan 1 , Bilal Butt 2 , Ronald Wasserman 1 , Ahmad Nassr 3 , Joshua Piche 1 , Rakesh Patel 1 , Ilyas Aleem 1
1 Orthopaedic Surgery, University of Michigan, Ann Arbor, USA
2 Orthopaedic Surgery, Cleveland Clinic, Cleveland, USA
3 Orthopaedic Surgery, Mayo Clinic, Rochester, USA
Introduction: Spine providers are increasingly using patient-reported outcomes (PROs) as a tool to measure disability and response to treatment to guide future therapy. Recall bias is an important component in PROs that has not been well studied in sacroiliac joint (SIJ) steroid injection. Material and Methods: Numeric pain scores (NPS) were recorded using standardized questionnaires. Baseline NPS for patients undergoing SIJ steroid injections were obtained prior to injection, at 4-hours post-injection, and at 24-hours post-injection. At a minimum of 2 weeks following the injection, patients were asked to recall their pre-injection, 4- and 24-hour post-injection NPS. Actual and recalled NPS were compared using paired t-tests for each time interval. Multivariable linear regression was used to identify factors that correlated with consistent recall. Results: Sixty patients with a mean age of 66 years (65% female) were included. Compared to their pre-injection pain score, patients showed considerable improvement at both 4 hours [Mean Difference (MD) = 3.28, 95% Confidence Interval (CI) 2.68 to 3.89], and 24 hours [MD = 3.23, 95% CI 2.44 to 4.03] post-injection. Patient recollection of pre-injection symptoms was more severe than actual (MD = 0.65, 95% CI 0.31 to 0.99). Patient recollection of symptoms was also more severe than actual at 4 hours (MD = 0.50, 95% CI.04 to 1.04), as well as at 24 hours post-injection (MD = 0.80, 95% CI 0.16 to 1.44). The magnitude of recall bias was mild and did not exceed the minimal clinically important difference (MCID). When analyzing net improvements in pain levels following SIJ injection, there was moderate correlation between actual and recalled pain levels when comparing pre-injection with 4-hour post-injection NPS [R = 0.64, p < .001] and moderate correlation when comparing pre-injection with 24-hour post-injection NPS [R = 0.62, p < .001]. Linear regression models for differences between actual and recalled NPS reveal that at pre-injection, patients with lower BMI and the presence of coexisting psychiatric diagnoses were better at recalling their pain [p < .003]. Patients with higher BMI also experienced less pain relief when comparing pre-injection with 4-hour post-injection NPS [p < .05]. Conclusion: Patients had favorable pain level responses to SIJ steroid injection for both actual and recall surveys, although patients with higher BMI experienced less pain level improvement at the 4-hour post-injection mark. Although patients demonstrated poor recall of absolute pain scores at pre-injection, 4-hour post-injection and 24-hour post-injection, they demonstrated robust recall of net pain score improvement at both 4- and 24-hours post-injection. These findings suggest that there is utility in using patient recollection to describe the magnitude of pain relief following treatment for sacroiliac joint dysfunction.
2465
P290: Sustained Hoffmann sign, a novel clinical sign in myelopathies' patients
Eslam Abourisha 1 , Kristine Logan 1 , Jason Braybrooke 1
1 Spine, University Hospitals of Leicester NHS Trust, Leicester, United Kingdom
Introduction: The Hoffmann sign is frequently utilised in clinical practise, particularly for disorders affecting the cervical spinal cord, as a finding suggestive of higher motor neuron dysfunction. The Hoffmann sign was first documented in the medical literature in 1911 by Hans Curschmann, a student of Johann Hoffmann, a German neurologist prominent in the late 19th century. "In our study, we identified a novel clinical observation among patients with cervical myelopathy – a sustained Hoffmann sign. The Hoffmann sign is a well-established clinical marker in these patient population; however, the persistence of this sign has not previously been documented in the medical literature except in one recent case report. We defined sustained Hoffmann sign as more than 3 beats of rhythmic flexion to the thumb or other fingers on Hoffmann test. Material and Methods: This is an observational study for new clinical sign associated with myelopathy. In the period spanning from February 2021 to March 2023, a cohort of five patients exhibiting sustained Hoffmann sign during clinical examination were identified. Results: The mean age of the patients was 67 years, with an age range of 42 to 90 years. Among them, four patients were male, and one was female, with male patients exhibiting a higher average age. Notably, two out of the five patients had no other concomitant medical conditions, as delineated in Table 1. All patients demonstrated evidence of cervical myelopathy on MRI scans. Specifically, three patients exhibited cervical compression at a single level, while the remaining two had predominant multi-level cervical compression, primarily affecting a single level. Compression was predominantly observed at levels C3-4 in three patients, and at levels C5-6 in the remaining two patients. The mean compression ratio, as determined from the MRI scans, was 0.47, with a range of 0.41 to 0.63. Male patients displayed a notably higher severity of compression, with a mean compression ratio of 0.44, contrasting with the only female patient who exhibited a compression ratio of 0.63. Clinical examination revealed that two patients presented with a spastic gait, hyper-reflexia, and sensory alterations, while one patient displayed sustained clonus. Additionally, all patients reported a decline in dexterity. Surgical intervention was pursued for two patients with progressive myelopathy, while the remaining three patients demonstrated a stationary course and were managed conservatively. Conclusion: Although our sample size was limited to five patients, this study represents an initial exploration of this intriguing phenomenon. While the significance of the sustained Hoffmann sign remains unclear at this stage, subsequent research efforts involving larger and more diverse populations will be essential to further elucidate the clinical implications and broader relevance of this finding.
2509
P291: Scoliosis detection and classification on plain radiographs using the deep learning method
Alim Can Baymurat 1 , Kemal Ureten 2,2 , Tolga Tolunay 1 , Gokhan Gultekin 3 , Muhammed Tosun 1 , Muhammed Calta 1 , Alpaslan Senkoylu 1 , Hakan Atalar 1
1 Orthopaedics and Traumatology, Gazi University Faculty of Medicine, Ankara, Turkey
2 Department of Rheumatology, Ufuk University Faculty of Medicine, Ankara, Turkey
3 Electrical and Electronics Engineering, Ankara Yıldırım Beyazit University, Ankara, Turkey
Introduction: The aim of this study was to employ deep learning (DL) techniques for the detection of scoliosis and the differentiation of various degrees of spinal curvature on plain radiographs. Material and Methods: The study was performed on the radiographs of patients aged 10-18 years who underwent postero-anterior chest radiography and standing plain abdominal radiography in our institution for any reason in the last year and a total of 1006 radiographs were included in the study. The radiographs were divided into 3 groups according to the degree of scoliosis: normal (0-9°), mild (10-29°) and moderate/advanced (30° and above). The data were randomly selected and 15% were used for testing, 15% for validation and the remaining 70% for training. Due to the limited data, the transfer learning method was used. Pre-trained VGG-16, ResNet-101 and GoogLeNet networks were used for transfer learning. The original classifier was replaced by a new one. Geometric transformations of radiographs were used for data augmentation. Rotation (-30, 30 degrees), translation (-30, 30 pixels) and scaling (0.9, 1.1 pixels) were applied to the images. The performance of the networks was evaluated with the performance parameters of accuracy, sensitivity, specificity, precision, and F1 score. Results: Overall accuracy after testing the models was determined to be 90.1% for VGG-16, 86.1% for ResNet-101, and 85.5% for GoogLeNet. The accuracy, sensitivity, specificity, precision and F1 score were 90.1%, 90.7%, 95.0%, 89.9% and 90.1% for VGG-16, respectively. The VGG-16 values were determined to be higher than the values of ResNet-101 and GoogLeNet networks. Conclusion: The results of the present study revealed promising outcomes regarding the discriminative efficacy of pre-trained networks in differentiating scoliotic deformities across diverse dimensions of the spine. The capacity to accurately discern normal, mild, and moderate/advanced spinal deformities on plain radiographs through DL-based labeling holds substantial significance for early disease detection, appropriate specialist referrals, and population-based investigations of disease prevalence (Figure 1,2) (Table 1-3).
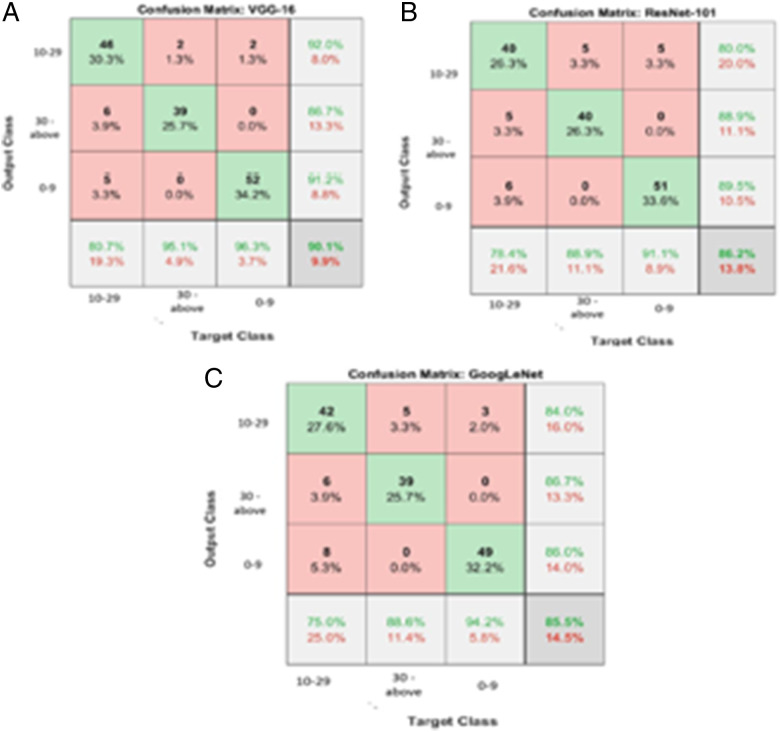
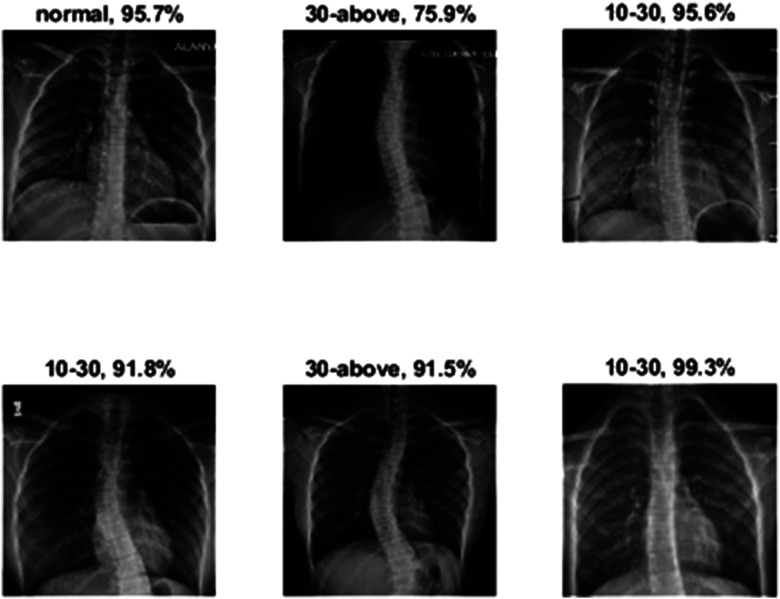
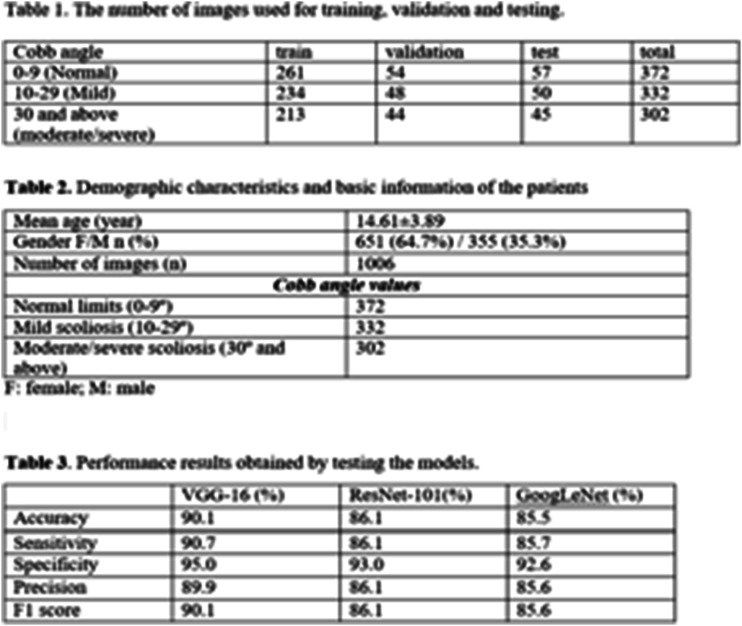
Disc degeneration
60
P292: Perioperative factors associated with high-risk daily morphine milligram equivalent total in spinal decompression
Eeric Truumees 1 , Devender Singh 1 , Ashley Duncan 1 , Cortney Matthews 1 , Sophia Stokes 2 , Matthew Geck 1 , John Stokes 1
1 Ascension Texas Spine and Scoliosis, Austin, USA
2 UT Austin, Austin, USA
Introduction: Morphine Milligram Equivalent (MME) dosing recommendations were introduced in 2016 by the Centers for Disease Control and Prevention (CDC) to aid in understanding the cumulative effect of opioids and the risks associated with long term use in chronic pain patients. Daily dosages of ≥ 100 MME/day are associated with an almost nine-fold increased risk of overdose. Current general recommendations endorse the lowest effective dose and ≤ 50 MME/day. We aim to determine what factors are associated with high-risk daily Morphine Milligram Equivalent totals in patients undergoing spinal decompression. Materials and Methods: Retrospective analysis was conducted on 85 patients that underwent spinal decompressive surgery within a multi-center network over 2 years. Average MME/day was calculated as the sum of qualifying inpatient MMEs administered divided by the sum of inpatient length of stay (LOS). 21 independent variables were collected from demographic, clinical and surgical domains and were subject to comparative analysis. Data was then grouped and coded for logistic regression analysis. Results: Overall mean MME per day was 56.05 ± 40.94, with a range of 1.67-220.02 MME/day. A total of 21 patients were determined to have “High MME” during their inpatient stay. Patients with high MMEs were significantly younger (mean age 50.9 ± 17.5) than those with lower MMEs/day (69.3 ± 12.2; p < 0.05). Patients with high MMEs were also significantly more likely to carry a psychiatric diagnosis (anxiety, depression, bipolar disorder) (43.8% [n = 14] vs 13.2% [n = 7], p = 0.00156). Additionally, patients who had high MMEs had lower ASA scores (2.43 ± 0.5 vs 2.7 ± 0.6) and reported higher preoperative Visual Analog Scale (VAS) pain scores (4.62 ± 2.8 vs 2.59 ± 3.6) than patients with lower MMEs/day. When subject to logistic regression, the final model identified for each unit decrease in age grouping increased the risk of high MME 0.31 times or 69.4%. A psychiatric comorbidity increased the risk of high MME by 8.7 times, or 770%. Conclusion: Patients with high MME/day who underwent spinal decompression were significantly younger with lower ASA scores, and higher preoperative VAS scores than those with lower MME/day. The incidence of psychiatric comorbidity was also higher in those with high MMEs. Psychiatric comorbidity in younger patients predicted a significantly increased risk of higher MME. Pre-operative opioid risk education and mitigation strategies should be considered in patients with high MME risk, especially in younger patients and those with psychiatric comorbidities.
218
P293: How to start full endoscopic discectomy
Mohamed Malabari 1
1 Orthopedic, Saudi German Hospital Jeddah, Jeddah, Saudi Arabia
Introduction: How to start the new Technique of lumbar endoscopic discectomy and how you must start to buld the learning curve. Material and Methods: Discuss multiple case presentation and surgical experience with the types of the pathology regarding the anatomical and pathological location of the herniated disc. After we did more than 60 case of full endoscopic discectomy At L5S1 disc herniation in our institution. Results: Good out come. Basic surgical technique to start doing full endoscopic discectomy. Conclusion: When to start full endoscopic discectomy the expected difficulty. Best approach for each pathology.
259
P294: A case series of lumber intervertebral disc herniation: intradural disc herniation
Zain Muhammad 1 , Muhammad Naveed 1
1 Orthopaedics and Spine Unit, Ghurki Trust Teaching Hospital Lahore, Lahore, Pakistan
Background: One of the rare presentations of the lumbar disc herniation is intra-dural disc. Therefore, thorough assessment is essential in cases of prolapsed intervertebral lumbar disc cases as imaging modalities like magnetic resonance imaging MRI is diagnostic; although not helpful in intradural disc prolapse and expecting this clinical entity preoperatively is essential. Case Descriptions: A 50-year-old male who had been suffering from lower back pain with bilateral lower limb radiations alongside numbness marked more on the right side for last 6 months. On examination power in quads & hams were 4/5 on right side. Whereas, bladder and bowel control was lost. Lasegue test (straight leg raise) was 45* on right and 60* on left. MRI revealed L5-S1 central disc prolapse, more towards the right side. During the procedure, disc was intradural and adherent to the dura from inside, though no dural rent was evident and also having hypertrophied ligamentum flavum. Thus, laminectomy was done and disc was removed after opening the dura. subsequently dural closure was done with 5-0 polypropylene suture. Another 22-year-old male who had been suffering from lower back pain with right lower limb radiations alongside perianal numbness for last 2 months. He also had urinary and fecal incontinence for the last 1 week. On examination power in right lower limb 3/5, sensations intact and planters were down going. Lasegue test (straight leg raise) was 45* on right and 80* on left. MRI showed L4-L5 disc. During the procedure, disc was intradural and dural rent was evident. Thus, laminectomy was done and disc was removed after opening the dura. subsequently dural closure was done with berriplast and fibrin glue. Similarly, a 37y/f patient who had been suffering from lower back pain with bilateral lower limb radiations alongside numbness for last 7 months. On examination all myotomes and dermatomes of bilateral lower limb as well as bowel bladder were intact. Lasegue test (straight leg raise) was 45* on right and 60* on left. MRI showed L5-S1. During the procedure, disc was intradural and to the dura from inside, though no dura rent was evident. Thus, laminectomy was done and disc was removed after opening the dura and left side root decompression done. subsequently dural closure was done with 5-0 polypropylene suture. Outcome: Patients were reviewed at 4 and 6 weeks postoperatively. Pain was settled and had no signs of local or systemic complications. On examination neurology were improved but bladder bowel was not recovered in those patients who has previously lost but patients were community mobilized and back to their normal daily lifestyle activities by 3 weeks postoperatively. Conclusions: Though intradural disc is a rare presentation but surgical excision of this entity is more cumbersome. Incising dura and subsequent water-tight repair with very fine suture is essential and requires good equipment and surgical experience. Therefore, preoperative planning is necessary. It is recommended that thorough assessment of preoperative imaging must be done and then postoperative histopathological analysis should be performed to expect the condition preoperatively and rule out other entities as other mass like incision postoperatively.
583
P295: Comparison between corticosteroid and platelet rich plasma transforaminal injection in single level lumbar disc herniation with radicular pain
Amit Raj 1 , Pradeep K Singh 1
1 LH Hiranandani Hospital, Orthopedics, Mumbai, India
Introduction: The aim of our study was to compare the efficacy of corticosteroid and platelet-rich plasma (PRP) therapy for the adult patients with single level lumbar disc herniation with radicular pain. Material and Methods: The present study was conducted with 20 patients between November 2021 to December 2022 who have tried conservative treatment for 6 months, and had radicular pain. All the patients were evaluated by the Visual Analog Scale (VAS) on the day of the procedure, at 2 weeks, at 1 month and 3 months. Results: The VAS score of the patients treated with Corticosteroid or PRP decreased during the study period. The results showed similar outcome for both transforaminal injections using PRP and steroid in the treatment of lumbar disc herniation. Conclusion: PRP can be used as an alternative to the Corticosteroid injection.
1094
P296: Intradiscal vaccuum phenomenon - Factors predicting selective occurrence in patients with lumbar disc degeneration
Rishi Kanna 1 , Ajoy P Shetty 1 , Shanmuganathan Rajasekaran 1
1 Spine Surgery, Ganga Hospital, Coimbatore, India
Introduction: Intradiscal vacuum phenomenon (IDVP), despite being ubiquitous, is poorly understood. The dynamic passage of peri-discal gases into the degenerated disc is a commonly accepted theory. But the reasons behind its selective appearance in some discs is unevaluated. Material and Methods: 721 patients with chronic low back pain ± radiculopathy, were evaluated with AP and flexion-extension lateral radiographs and MRI. IDVP was classified based on its morphology and location. Radiographic parameters including sagittal translation, sagittal angulation, lateral listhesis, eccentric disc collapse, Pfirrmann’s grade, disc height, Modic changes, anterior longitudinal ligament status and primary spinal disease at the level of IDVP was analyzed. Results: 342 patients had IDVP, and had a higher mean age (57.2 ± 12.5 years) than controls (p < 0.001). Eccentric disc space narrowing (26.5% vs 1.3%, p < 0.01), coronal listhesis (7.83% vs 1.1%, p < 0.001), sagittal angular motion difference (11.3 ± 4.6°, p < 0.001), higher mean disc degeneration (4.36 ± 0.69, p < 0.001), ALL disruption (30.3% vs 2.2%, p < 0.001) and Modic changes (88.6% vs 17.5%, p < 0.001) were significantly higher in IDVP discs (vs non-IDVP). Binary logistic regression analysis indicated sagittal angular motion difference was the most predictive factor. IDVP was classified into three types - dense type (47.5%), linear (29.5%), dot type (23%). Dense type matched radiological correlations of IDVP while dot types behaved like non-IDVP discs. Conclusion: Modic disc-endplate contacts, ALL disruption and coronal translation could be pathways for passage of peri-discal gases into the degenerated disc. In the pathogenesis of IDVP, advanced disc degeneration, presence of pathways of gas transfer and angular/coronal instability seem to play complimentary roles.
1125
P297: Clinical and radiographic features of adult thoracic calcific discitis with herniation: a retrospective analysis of 31 cases
Lei Yuan 1 , Zhongqiang Chen 1 , Chuiguo Sun 1 , Weishi Li 1
1 Orthopedic Department, Peking UniversityThird Hospital, Beijing, China
Introduction: Pediatric calcific discitis is well-described, most commonly at the lower cervical level, with a self-limiting process, and most symptomatic patients are recommended conservative treatment, even in rare cases with giant disc herniations and mild neurological deficits. However, adult thoracic calcific discitis with herniation (TCDH) differs from pediatric calcific discitis with disc herniation in several respects, including the natural history, clinical presentation, treatment, and prognosis. TCDH is rare, and rare literature exists regarding the features of the disease. Material and Methods: Subjects were 31 adult TCDH patients who underwent surgery from 2004 to 2021. Clinical and radiographic features of TCDH were retrospectively analyzed. Then according to preoperative radiographic examination, TCDH was divided into subtypes. Patient characteristics and radiographic data were compared between different subtypes. Results: Three (9.7%) patients of 31 had a history of trauma, and the rest had insidious onset. The average age of operation was 50.03 ± 9.60 years, and the mean preoperative disease duration was 17.05 months. The most common preoperative complaints were lower extremity numbness (80.6%) and lower extremity weakness (77.4%). The compression segments were mainly distributed in T7-11, and the average spinal canal ventral-occupying ratio was 74.90 ± 15.16%. The most prominent radiographic feature was the calcification of the nucleus pulposus in the intervertebral disc and calcified lesion contiguous with the disc space protruding into the spinal canal. There were 5 cases of central low-density type, 19 cases of heterogeneous calcification type, and 7 cases of homogeneous calcification type, respectively. The radiographic manifestations, intraoperative findings, and postoperative pathologies of the three subtypes were different. The central low-density type was younger and had a shorter preoperative duration and significantly lower mJOA score. A special case observed five years demonstrated that heterogeneous calcification could progress to a homogeneous calcification type. Conclusion: Adult TCDH is a special thoracic disc disease with insidious onset, a long course, and a high spinal canaloccupying ratio. Calcium deposits in the spinal canal originate from the nucleus pulposus. The intraoperative findings and postoperative pathology of subtypes are different, which might indicate different pathological mechanisms.
1277
P298: Healthcare utilization following open vs. minimally invasive discectomies across various BMI categories
Frank Epitropoulos 1 , Hania Scahzad 1 , Alexandra Sheldon 1 , Elizabeth Yu 1 , Safdar Khan 1
1 Orthopedics, Ohio State University Wexner Medical Center, Columbus, USA
Introduction: To compare the outcomes of traditional open versus minimally invasive discectomies across distinct BMI (Body Mass Index) categories, focusing on opioid consumption, hospital readmissions, infection rates, and medication costs. The aim is to provide surgeons with evidence-based guidance to select the most suitable surgical approach based on a patient's BMI thus enhancing individualized care. Material and Methods: We used the PearlDiver patient record database to assess individuals who had undergone open or minimally invasive discectomies. Minimally invasive discectomies included both endoscopic and microscopic approaches. Patients were divided into six groups based on their BMI measurements: < 20, 20-24.9, 25-29.9, 30-34.9, 35-39.9, and 40+. The study analyzed various metrics, such as postoperative opioid consumption, hospital readmissions, infections, and medication costs. Results: Our analysis showed no observable difference in opioid consumption between patients who underwent open discectomies and those who underwent minimally invasive discectomies across all BMI categories. However, for patients with a BMI over 40, open discectomies were associated with a higher 90-day readmission rate (OR = 1.47, p = 0.001) and had increased infection rates at both the 90-day (OR = 2.44, p = 0.009) and 1-year marks (OR = 2.41, p = 0.005) compared to minimally invasive discectomies. Medication costs were consistently increased for patients who received minimally invasive procedures. Conclusion: When considering postoperative readmissions and infection rates, minimally invasive discectomies appear more favorable than traditional open discectomies. Surgeons should consider their patient's BMI when deciding between the two surgical methods.
1546
P299: Machine learning-driven analysis reveals key genes and immune cell involvement in intervertebral disc degeneration
Haoju Lo 1
1 Orthopedic Surgery, Da-Chien General Hospital, Miaoli, Taiwan
Introduction: Low back pain, primarily attributed to Intervertebral disc degeneration (IDD), is a pervasive healthcare challenge. Its intricacies, while studied for years, remain elusive. Current treatments predominantly offer symptomatic relief, but a genuine solution lies in understanding IDD's core pathogenesis. With modern sequencing and computational methodologies, we're closer than ever to unravelling these mysteries. This study harnesses machine learning, aiming to spotlight ROR1 and ZC3H12A as diagnostic biomarkers. Additionally, we delve into the nuanced relationship between these biomarkers and immune cell infiltration, a key aspect of IDD's etiology. Material and Methods: We meticulously selected three microarray datasets from the GEO database, ensuring diverse and comprehensive data representation. Utilizing the "limma" R package, we ensured rigorous data preprocessing, setting the stage for credible analysis. The identification of DEGs was paramount, with stringent criteria guiding our choices. For holistic understanding, enrichment analyses, performed via "clusterProfiler", unveiled the potential roles and implications of our discovered genes. Our three-pronged approach - using SVM-RFE, LASSO, and Random Forest - for biomarker identification showcased the synergy of diverse algorithms. Furthermore, our emphasis on immune cell infiltration's role, deciphered through the CIBERSORT algorithm, highlighted the multifaceted nature of IDD. Results: From the GSE27494 dataset, 488 DEGs came under our spotlight. Further analyses revealed these genes' involvement in pivotal biological processes, chiefly the TNF and IL-17 signaling pathways. Machine learning's versatility was evident, with ROR1 and ZC3H12A emerging as promising IDD diagnostic biomarkers. Subsequent validation in other datasets reinforced our initial findings. The AUC values, a metric of diagnostic precision, underscored the biomarkers' clinical relevance. Our foray into immune cell infiltration painted a detailed landscape: ROR1 showed associations with specific immune cells, whereas ZC3H12A exhibited contrasting relationships, emphasizing the complexity of the immune environment in IDD. Conclusion: Our research bridges critical knowledge gaps in IDD. By spotlighting ROR1 and ZC3H12A and integrating bioinformatics with experimental validations, we've demystified the gene expression paradigms in IDD. The intricate ties between these biomarkers and immune cell dynamics further underscore the disease's complexity. Our findings not only elevate the scientific discourse around IDD but also offer tangible avenues for patient-specific immunotherapy and early diagnostics, heralding a paradigm shift in IDD management.
1557
P300: Delayed presentation of cauda equina syndrome treated with surgery with full recovery of bowel and bladder function
Kavinan Subramaniam 1 , Shen Liang Tey 1 , Zi Hao Phang 1 , Nur Aida Faruk Senan 1
1 Orthopaedics, Hospital Umum Sarawak, Kuching, Malaysia
Introduction: Cauda equina syndrome (CES) is a spinal surgical emergency (9). Patients with CES present with back pain radiating to the legs, motor and sensory dysfunction of the lower extremities, bladder and/or bowel dysfunction, sexual dysfunction and saddle anaesthesia. The acceptable standard of care is to perform surgical decompression within 48 hours of onset of symptoms to produce good recovery of neurological function (8). Occasionally, patients with CES may present to hospital late. We present a case of patient with CES who presented late to hospital who had undergone spinal decompression surgery. Materials and Methods: A 51-year-old lady, presented with three weeks worsening lower back pain, saddle anaesthesia, urinary and bowel incontinence. She presented to the tertiary hospital late to seek for treatment due to logistic problem. she had significant lower back pain, left lower limb weakness, bowel and urinary incontinence. Physical examination showed left lower limb myotome (Medical Research Council Scale for Muscle Strength) L2 (5/5), L3 (5/5), L4 (5/5), L5 (4/5), S1(4/5). Sensation was reduced over left L5 and S1 dermatome. Right lower limb myotome power and dermatome sensation was normal. Perianal sensation reduced. Anal tone was lax. Voluntary anal contraction was absent. Magnetic resonance imaging (MRI) spine showed large L5/S1 central and left paracentral disc compressing the cauda equina with some sequestrated disc migrated inferior to L5/S1 disc. The patient underwent wide laminotomy, discectomy of left L5/S1. Results: The patient had immediate improvement of motor function and sensation over the left lower limb after surgery. Two weeks post surgery she had regained full motor function and sensation over left lower limb and recovered from urinary and bowel incontinence. There was slight residual perianal numbness. Conclusion: Posterior Decompression and discectomy surgery is still worthwhile in patients with complete Cauda Equina Syndrome secondary to prolapsed disc who present late for treatment with chances of recovery in bowel and bladder function.
Epidemiology
39
P301: Racial disparities and surgical outcomes after anterior cervical discectomy and fusion: NSQIP analysis 2015-2020
Elias Elias 1 , Daoud Ali 2 , Zeina Nasser 3
1 Neurosurgery, University of Texas Southwestern, Dallas, USA
2 Department of Chemistry, Illinois College, Jacksonville, USA
3 Neuroscience Research Center, Faculty of Medical Sciences, Beirut, Lebanon
Objective: Anterior cervical discectomy and fusion (ACDF) is one of the most performed spine surgeries in the USA. Many published studies have focused on morbidity/complication rates of ACDF, however, the relationship between race and postoperative 30-day outcomes has not been fully explored previously. Our objective is to assess the effect of race on outcomes in patients undergoing anterior cervical discectomy and fusion. Methods: We identified 57913 adult patients who underwent elective ACDF spine surgery from 2015 to 2020. Data were extracted from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. Demographics, comorbidities, perioperative course, and 30-day post-op outcomes were stratified by race. Logistic regression and multiple linear regression were used to assess the influence of race on postoperative outcomes. Results: A total of 57913 patients, Caucasian (CA; n = 49016), African American (AA; n = 7200), Native American (NA; n = 565), and Asian (n = 1132) underwent ACDF fusion surgery. AA patients had higher comorbidities, including as diabetes (24.7%), dyspnea (5.9%), and hypertension (61.6%) compared to the other groups (p value < 0.001). NA and AA were higher tobacco users, (33.1%) and (28.7%), respectively (p value < 0.001). The majority of patients reported in this data set had single-level surgeries. AA had a longer average hospital stay and operative time (2.51 ± 7.31 days), (144.13 ± 82.26 min) p value < 0.001 respectively. Lower risk of superficial surgical site infection and greater risk of reintubation, pulmonary embolism, renal insufficiency, and return to operation room were reported in AA compared to CA ORadj 0.41 (0.22-0.77) p value 0.005, ORadj 1.65 (1.25-2.17) p value < 0.001, ORadj 1.88 (1.27-2.79) p value 0.001, ORadj 3.15 (1.38-7.20) p value 0.006, ORadj 1.41(1.18-1.65) p value < 0.001 respectively. NA showed an increased risk of superficial surgical site infection compared to CA ORadj 2.59 (1.05-6.36) p value 0.037. Conclusions: Racial disparities were found to independently affect rates of complications after surgery for anterior cervical discectomy and fusion. This study provides contributions to increase surgeons’ awareness of the impact of race on surgical outcomes and may help improve some of the presurgical conditions and postoperative planning.
Keywords: race; ACDF; fusion surgery; surgical outcomes; NSQIP
72
P302: Patient perception of orthopedic surgeon's empathy in adolescent idiopathic scoliosis telemedicine
Gerardo Olivella 1 , Jose Martines-Ramos 2 , Jose Acosta-Julbe 2 , Mariana Acuna 3 , Carlos Campa-Maldonado 1 , Norman Ramirez Lluch 4 , Humberto Guzman Perez 1
1 Orthopaedic Surgery, University of Puerto Rico Medical Sciences Campus, San Juan, Puerto Rico
2 School of Medicine, University of Puerto Rico, San Juan, Puerto Rico
3 Surgery Department, Ponce Health Sciences University, Ponce, Puerto Rico
4 Pediatric Orthopedic Department, Mayaguez Medical Center, Mayaguez, Puerto Rico
Introduction: Limited studies have examined the relationship between surgeon empathy and patient experience at initial evaluation by telemedicine. No study has explored patients' perceptions of their physician's communication skills and empathy among orthopedic surgeons who practice telemedicine versus in-person in adolescent idiopathic scoliosis (AIS) initial evaluation. Thus, the aim of this study was to assessed patient’s perception of orthopedic pediatric surgeon empathy during telemedicine as compared to in person consultation during initial clinical encounters for AIS patients. Materials and Methods: This is an institutional review board prospective cohort study of all AIS patients undergoing an initial evaluation by a single orthopedic surgeon between December 2021 to December 2022. AIS patients were stratified in two groups: those who underwent telemedicine versus in-person office evaluation. Patients were asked to fill out Consultation and Relational Empathy (CARE) questionnaires after their initial encounter with the direct supervision of their parents or legal guardian. Sociodemographic, radiographic, and questionnaire responses were compared between both groups using independent t-tests and Fischer exact tests. Results: A total of 92 patients were included with an average age of 15 years, 76% being female. Of these, 33 patients underwent telemedicine and 59 underwent in-person office evaluation. There were no differences between both groups regarding age (p = 0.07), body mass index (p = 0.62), sex (p = 0.96), educational level (p = 0.78), presence of back pain (p = 0.85), leg discrepancy (p = 0.29), left trunk shift (p = 0.07), riser stages (p = 0.66), coronal cobb angles (p = 0.89). Patients who underwent telemedicine reported similar CARE satisfaction scores when compared to those who underwent in-person office evaluation. An in-person office evaluation required significantly more time than telemedicine. Conclusion: Understanding patient perception of orthopedic surgeons’ empathy during AIS telemedicine evaluation can provide an appropriate alternative during initial medical encounter. The initial evaluation for AIS patients using telemedicine was found to be a safe and effective care practice, with high communication and empathy scores. Telemedicine platform is a reasonable initial encounter model to consider for patients seeking convenient and efficient care for AIS evaluation.
240
P303: Epidemiology of spinal trauma and related complication: a hospital based study at Karnali Academy of Health Sciences
Tufan singh kathayat 1 1 , Pujan Kumar Rokaya 1 , Mangal Rawal 1 , Prashanna Dip Karki 2 , Mohan Nath 3
1 Department of Othopaedics and Trauma Surgery, Karnali Academy of Health Scinces, Jumla, Nepal
2 Department of Othopaedics and Trauma Surgery, National Academy of Medical Sciences, Jumla, Nepal
3Department of Othopaedics and Trauma Surgery, Seti Hospital, Jumla, Nepal
Introduction: Traumatic spinal injury is leading cause of mortality and morbidity among the people of productive age group. This study aim to find the cause of spinal injury, site, and mode of injury, treatment option given so that a preventive measures and create awareness among people of this region. Methodology: This a prospective observation study done in Karnali Academy of Health Sciences from December 2021 to January 2023. Performa was filled to collect data. Data were entered in excel sheet and transported to SPSS 16.0 and statistical analysis was done. Result: Out of 117 patients male population had higher incidence of spinal trauma (69.2%) with average age 43.9 years. Fall injury was the commonest mode of injury. 65.8% had injury at the thoracolumbar junction followed by lumbar, thoracic and cervical respectively. Cervical injury patients had higher incidence of neurological deficit. The average duration of trauma to hospital presentation was 10.9 ± 11.2 hours. 19.7% were operated and 6.8% of patients were referred to other center. Conclusion: Fall injury being the commonest mode of injury in this art of world, prevention and awareness should be raised about the spinal trauma and its consequences is necessary. Adequate equipment with health facilities to the distant hospital may reduce the referral rate and duration of presentation to the hospital which ultimately prevent the further damage to the cord.
Keywords: spinal trauma; fall injury; Western Nepal.
251
P304: Causes associated to the delay in treatment of patients with pediatric scoliosis in the Brazilian public health system
Robert Meves 1
1 Orthopedic and Traumatology, Santa Casa of Sao Paulo, Sao Paulo, Brazil
Introduction: According to the Scoliosis Research Society (SRS), scoliosis is defined as an abnormal lateral curve of the spine in the coronal plane equal to or greater than 10 degrees. The causes may be idiopathic, congenital or neuromuscular, associated or not to other syndromes. The primary age of onset for scoliosis is 10-15 years old, occurring equally among both genders. Standard treatment in patients who have not reached skeletal maturity and have curves between 20 and 40 degrees is bracing. For patients with skeletal maturity or curves greater than 50 degrees, the treatment of choice is surgery. Observational studies have established high morbidity and mortality in patients that present non treated rapidly progressive curves1. There are a number of studies on the impact and cause of delayed treatment in adolescent idiopathic scoliosis (AIS) 2-5. However, there is a lack of studies on the causes of delayed treatment in other types of scoliosis, especially in a continental country such as Brazil, that has the largest public health system in the World. The Brazilian Unified Health System (Sistema Único de Saúde – SUS) was implemented in 1988 offering free health care to the population. The challenges of providing proper timely health care to its 211 million inhabitants has increased progressively, as the costs of medicine and the population continue to grow. The Brazilian Spine Society (SBC) launched a national multicenter survey to try to establish the specific causes of delayed treatment in pediatric scoliosis, such as delay in diagnosis, referral to and waiting lists in tertiary treatment centers, financing of braces, physical therapy and surgical instrumentation, thus providing accurate information for future public health planning and political interventions [1,2]. Material and Methods: This descriptive epidemiologic study using convenience sampling was carried out from January 2021 to February, 2023. The studied population consisted of patients under 18 years of age, with diagnosis of scoliosis, who had been waiting for treatment (bracing, cast, or surgery) in one of the enrolled referral Orthopedic Spine Centers, for over 6 months [3]. Data was collected by personal interviews with patients’ parents/legal guardians, after signing informed consent. The study variables, incorporated in to Red Cap® platform, were: age, gender, diagnosis according to the Scoliosis Research Society, date of entry into the study, how referral was made, date of first consult with Spine Surgeon, main cause for delayed treatment.
The objectives of the current study were:
1- To identify the specific causes of delayed treatment
2- To establish if causes vary according to regional differences in access to health care
3- To present suggestions of public policy interventions and better resource allocation in the Brazilian Unified Public Health System (SUS)
Twenty-one specialized treating centers were enrolled following requirements of the Brazilian Spine Society: 20% from the Northeast, 45% from the Southeast, 9% from the Midwest, and 26% from the South. Compiled data from these centers were statistically analyzed using commercially available software (SPSS® 25 for MAC). Continuous data were described in averages and standard deviation, and submitted to Kolmogorov-Smirnov test to establish normality of the distribution. Kruskal-Wallis test or Mann-Whitney test adjusted to Bonferroni, when necessary, were used for inferential statistical analysis. Categorical data were described in absolute and relative frequency. Statistical significance was established at p < 0.05.
Results: A total of 651 patients who were in a waiting list for treatment of pediatric scoliosis were enrolled, after formally consented. The mean age of the studied population was 13.3 ± 3.5 years; 74% were females and 26% were males; 53% were White, 35 % were mixed race, 10% were Black, and 2% were native Brazilian or Asian. The etiology of scoliosis was idiopathic in 371 patients (57%), syndrome related in 46 (7%), neuromuscular in 124 patients (19%), and congenital in 110 patients (17%). Focal meetings were held with the head of each participating Spine Center, either online or in presence, to discuss data and suggestions for better resource allocation to mitigate this public health problem. The average time elapsed between consult with primary care facility and the spine surgeon was 9.1 ± 19 months on average; the median was 2 months (minimum of less than one month and maximum of 138 months). There was no statistical difference between Brazilian regions (p > 0.05). The source of referral was: primary care SUS health clinic (56%), walk-ins (28%), interdepartmental referral in the same institution (13%), referral to a different center than the original due to lack of availability/beds (3%). The time elapsed between the primary care evaluation and that of the spine specialist depended on the origin of the referral: for the primary care SUS health clinic it was 9.1+17.5 months, for inter departmental referral it was 17.7 ± 30.2 months, for walk-ins it was 3.8 ± 10.2 months, from one spine center to another due to lack of availability/beds it was 5.2 ± 4.3 months. A significant delay in reaching the spine specialist was observed when comparing patients who followed the usual route of referral via primary care public health clinics (SUS) versus those that sought the specialist clinic directly (walk-ins) (p < 0.05). It is also interesting to note that 93% of patients were referred to surgical correction of the scoliosis after being seen by the orthopedic specialist. Bracing was suggested as treatment for only 6% of the studied population and serial casting in 1% of these patients. The average waiting time to get the suggested treatment, after being seen by the spine specialist, was 51.4 ± 39.5 months; up to 63% of patients waited another 12 months for treatment. The causes of delayed orthopedic treatment were: delay in transferring the patient from the primary care facility to the tertiary facility (30%), logistical problems (traction table and training) for cast placement (1%), difficulty in finding an orthopedic workshop that made the braces (6%), difficulty in obtaining pediatric hardware for surgery – insufficient financing by the institution and government (10%), lack of operating room schedule due to volume of emergency procedures/ lack of ICU beds/ lack of human resources/ lack of neurophysiological multimodal monitoring (44%), patient compliance due to social issues (3%), untreated or uncontrolled clinical problems impeding surgical intervention (6%). There was no difference between regions of the country (p < 0.05). The main consequences of the delay in treatment, as reported during the focal meetings with peer, were: Law suits, worsening of the spinal deformity with the consequent need for bigger more aggressive and costly surgical procedures, worse surgical outcomes, longer hospital stays, loss of timing for conservative treatment (bracing and casts).
The actions proposed for public policies focused on optimizing limited financial and human resources were:
1) Involve law makers to pass a law establishing a maximum 6-month wait for specialist treatment after primary care referral;
2) Create a unified national patient list prioritizing risk of progression;
3) Reduce directives of post-operative ICU stay;
4) Create and implement new codes recognized by SUS for low-cost pediatric hardware, neurophysiologic monitoring, and serial casting (currently unavailable, and therefore not covered by public funding);
5) National directives to finance Evidence Based studies;
6) Train health care team in Primary Care facilities to recognize the spinal deformities allowing early referral;
7) Expand telemedicine for specialist consults in remote locations;
8) Centralize the purchase of hardware by the Health Ministry;
9) Establish Tertiary Treatment Centers of Spine deformities throughout the country for better distribution of patients.
Conclusion: Health Care in Brazil is a constitutional right. The Brazilian Unified Health System (SUS) follows the model of the United Kingdom’s National Health System (NHS), offering universal healthcare to the entire population. However, as mentioned above, there is a significant and growing discrepancy between the health care demand and the ability to provide such care to a growing, aging population, especially in Latin America [5]. The consequences are long wait lists for surgeries, especially those of greater complexity, and worsening of the baseline disease, which at the end incur in greater public health costs and a negative financial impact for society. Long wait lists for Idiopathic Adolescent Scoliosis have been previously reported in Brasil and América Latina [5, 6, 11,12], pointing to the difficulties in getting a referral to a spine specialist and to additional waiting for a surgical spot at the tertiary treatment facilities [2]. Other countries with subsidized public health systems have also reported long wait lists for surgical treatment of scoliosis (UK 5-9 months [14], Canada 6-12 months [15], New Zeland 11 months [16]), but none as alarming as the ones reported in the current study (average 51 months). According to Wright et al the target interval between diagnosis and treatment for AIS should be a maximum of 6 months [3]. The excessively long wait for specialized treatment is likely to lead to greater deformities, that could have been originally treated conservatively with braces and serial casts, but will end up requiring complex surgery, longer hospital stay, rehabilitation and are likely to cause greater morbidity. It seems evident that the final cost for public resources will be greater secondary to this neglect. Thus, the importance to implement public policies that address these issues at an early stage. The SRS, represented by their Chair, Dr. Paul T. Rubery, in a recent Heath Policy Committee Meeting recognized the efforts of the Brazilian Spine Society to understand the issues involved in this complex situation and propose solutions for rationalization and optimization of the treatment of patients with scoliosis in Brazil. (Paul T. Rubery, Chair et al Jan, 29, 2022.Heath Policy Committee SRS https://us06web.zoom.us/j/82458407880?pwd=YkVycHNPYmdDU2RNMzhlNlFPY2l4QT09).
References
1. The impacts of waiting for surgical correction of Adolescent Idiopathic Scoliosis and its repercussions for publicly funded health systems: systematic review. Mariana Demétrio de Sousa Pontes1 · Thabata Pasquini Soeira1 · Mariangela Louzada Sampaio2 · Raphael de Rezende Pratali3 · Yuri Pompeu4 · Carlos Fernando Pereira da Silva Herrero. European Spine Journal (2023) 32:617–624.
2. Bressan-Neto M, Herrero CF, Pacola LM, Nunes AA, Defino HL. Community Care Administration of Spinal Deformities in the Brazilian Public Health System. Clinics. 017;72(8):485-490. https://doi.org/10.6061/clinics/2017(08)06
3. Wright JG, Li K, Seguin C, Booth M, Fitzgerald P, Jones S, et al. Development of pediatric wait time access targets. Can J Surg. 2011;54(2):107-10, https://doi.org/10.1503/cjs.048409.
4. Miyanji F, Newton PO, Samdani AF, et al. Impact of Surgical Waiting-List Times on Scoliosis Surgery: The Surgeon’s Perspective. Spine 2015;40(11):823–828
5. Time to surgery for adolescent idiopathic scoliosis: How long does it take? Amulticenter study. Alfredo Guiroya,b,*, Charles Carazzoc, Gaston Camino-Willhuberd, Alejandro Morales Ciancioe,Rodrigo Remondinof, Fernando Ning, Fernando Alvarado-Gomezh, Juan Reviriegoi,Baron Zarate Kalfopulosj, Murilo Daherk, Andre Luis Fernandes Andújarl, Jahangir Asgharb,Fabio Ferri-de-Barrosm, Robert Meves. World Neurosurgery: X 19 (2023) 100187
772
P305: The prevalence of sacroiliac joint disorders among backache patients compares with sickler patients in Basrah Iraq
Ahmed Alobaidi 1,2 , Mubder Mohammed Saeed 2 , Ali Al_Diwan 2
1 Orthopedic Surgery, Royal College of Surgeon of England, United Kingdom
2 Department of Surgery, Basrah Medical College, Basrah, Iraq
Introduction: Backache is a common complaint that every human being experiences it at least once in their life. One of the hidden causes of lower backache is sacroiliac joint. A study shows that sacroiliac joint causes were prevalent in 23% of patients presenting to an outpatient clinic with symptoms of low back pain. Diseases that affecting the Sacroiliac joint including inflammatory sacroiliitis, infective sacroiliitis, strain of sacroiliac joint, sacroiliac joint dysfunction. In addition to that there is a specific association between sacroiliac joint and sickle cell disease, which is not frequently reported in the literature. Sickle cell disease is a common hemoglobinopathy with a special geographical distribution in Basrah province, south of Iraq. Both inflammatory and non-inflammatory arthritis are described in association with sickle cell disease. The aim of this study is to show the number of patients present with backache and the causes of their symptoms related to sacroiliac joint. Furthermore, the number of Sickler patients present with backache and the sacroiliac joint were the cause. So, a Compares of the prevalence of sacroiliac disorder among Sickler and non-Sickler patients is clear. Material and Methods: Descriptive cross sectional study of the sacroiliac causes of backache and compares with Sickler patients in Basrah -Iraq. The study was conducted in Basrah Teaching Hospital and Private clinics in addition Basrah Hemoglobinopathy Hereditary Centre and Arthroplasty Centre were included for the Sickler patients. Evaluation of all backache patients regardless of the causes clinically and by investigations (radiograph, CT scan and MRI). Patients with backache due to sacroiliac disorder were recognized depending on clinical examination (SI distraction, SI compression, sacral thrust, FABER, thigh thrust, Gaenslen’s test) although its specificity is controversial. To add Radiological imaging was offered to all patients but CT scan and MRI to selected patients. Results: 543 patients with backache were involved. Most commonly it is of moderate severity 343 patients 63% according to VAS score. Point tenderness at the sacroiliac joint were positive in 157 patients (26.4%) and FABER test were positive in 167 (30%) patients. Plain radiograph was positive for 154 (28.9%) patients. MRI showed changes in 22/120 (18.3%) patients. Sixty-two Sickler patients have lower back pain, and it is most commonly of moderate severity forty-three patients (69%) according to VAS score. The FABER test was positive in 43 (69%) of patients with sickle cell disease and lower backache. Plain radiography was positive in forty-four of the enrolled patients in the study 44/62 (71%). MRI was able to detect an abnormality in 19 /31 (64.2%) of the examined cases, and the most common MRI finding is subchondral sclerosis. Conclusion: The sacroiliac joint is hidden cause of the lower backache. Diagnosis of sacroiliac disorders needs clinical awareness, meticulous examination, and correlation of the clinical finding with imaging results. In sickle cell disease sacroiliac joint is more commonly involved as a cause of lower backache due to inflammatory arthritis or associated hip problem (AVN).
797
P306: Trends in the treatment of cervical myelopathy during the COVID-19 pandemic
Henry Avetisian 1,2 , Andy Ton 1 , Nicole Hang 1 , Brandon Yoshida 1 , Jacob Ball 1 , Jeffrey C. Wang 1 , Raymond Hah 1 , Ram Alluri 1
1 Department of Orthopaedic Surgery, USC Keck School of Medicine, Los Angeles, USA
2 Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, USA
Introduction: At the inception of the COVID-19 public health emergency in January 2020, elective surgeries declined due to nationwide restrictions. As spinal surgery involves a combination of emergent and elective surgeries, this had a significant impact on the field. With the progressive nature of cervical spinal pathologies, this posed a burden for patients and physicians. In patients with cervical myelopathy, ongoing symptoms can abruptly precipitate neurological deficits. Deferring operative treatment in these cases therefore places these patients at substantial risk. Few studies have reported the nationwide trends in cervical spine surgery cases during the pandemic. Thus, the aim of this study is to identify treatment trends for degenerative cervical myelopathy prior to (2019) and following the inception of the COVID-19 pandemic (2020-2021). Material and Methods: The PearlDiver national database was queried using International Classification of Disease (ICD-9, ICD-10) and Current Procedural Terminology (CPT) codes for patients age > 35 years who underwent operative treatment for cervical myelopathy from January 2019-October 2021 through one of the following cervical procedures: posterior cervical fusion (PCF), anterior cervical decompression and fusion (ACDF), laminoplasty, corpectomy, and disc arthroplasty (CDA). Mean age and elixhauser comorbidity index (ECI) scores were recorded. Annual and monthly procedure utilization between January 2019 through October 2021 was recorded and compared. Monthly trends were compared to January 2020 case volumes as a reference. Results: Patients undergoing cervical myelopathy treatment during the COVID-19 pandemic were older and had a higher number of comorbidities (mean age = 60.75 +10.99 years, ECI = 5.88+ 3.93) compared to those prior (mean age = 58.54+10.5, ECI = 3.91+3.33). Degenerative cervical myelopathy treatment decreased overall by -11% in 2020 compared to 2019 and -2.1% in 2021 compared to 2019. April (-54.6%) and May (-26.3%) of 2020 had the largest decreases compared to January 2020. Concurrent with the rising incidence of COVID-19 cases reported in January 2021, procedure utilization remained decreased relative to January 2020 (-5.9%). Case volume, however, recovered shortly thereafter in March 2021, increasing by 19.2%. Increases in utilization were maintained from March to June 2021, sustaining an average monthly increase of 8.9% compared to January 2020. The monthly average for 2020 decreased by -11.1%, and for 2021 decreased by -2.1% relative to January 2020. Stratifying by procedure, the greatest decrease in the average annual utilization for 2020 compared to 2019 was seen with cervical laminoplasty (29.55%), while corpectomy experienced relatively minimal reduction in case volume (-7.3%). Conclusion: Patients who received cervical spine surgery during the pandemic had a greater comorbidity burden. This is likely due to the fact that only patients with severe cervical spine pathology met the criteria for emergent surgery. The greatest impact on cervical spine surgery during the pandemic occurred in April and May 2020, a few weeks following implementation of nationwide restrictions. Treatment for cervical myelopathy was on average decreased throughout 2020, but returned to baseline rates throughout 2021 with a transient upsurge in volume from March to June; these increases were likely attributable to necessary treatment of deferred cases from 2020.
868
P307: Impact of posterior lumbar interbody fusion for isthmic spondylolisthesis in Hispanics with predominant axial back pain versus radicular pain intensity
Gerardo Olivella 1 , Miguel Cartagena 2 , Jose Acosta-Julbe 3 , Christian Nieves-Rios 3 , Juan Carro-Rivera 1 , José Massanet-Volrath 1 , Jose Montañez-Huertas 1 , Norman Ramirez Lluch 4 , Enrique Escobar-Medina 1
1 Orthopedic Surgery
2 Surgery Department, Ponce Health Sciences University, Ponce, Puerto Rico
3 Medicine, University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
4 Pediatric Orthopedic Surgery, Mayaguez Medical Center, Mayaguez, Puerto Rico
Introduction: There is great controversy towards the preferred instrumented fusion method to reduce pain intensity for the treatment of isthmic spondylolisthesis (IS). Historically, Hispanics have reported worse postoperative pain improvement compared to non-Hispanics after spinal surgeries. The purpose of this study was to evaluate the impact of posterior lumbar interbody fusion (PLIF) for IS in Hispanics with predominant axial back pain versus radicular pain intensity. Materials and methods: This was a retrospective cohort study of Hispanics who underwent PLIF for IS from 2010 to 2020 with a minimum of two years of follow up. Sample data was divided in two groups; those who reported outcomes of predominant axial back pain and those who reported predominant radicular pain. Patient reported outcomes of pain intensity was evaluated using numerical rating scores (NRS) scores. Demographic and perioperative data was collected and compared between groups using ANOVA and chi-square for continuous and categorical variables, respectively. Correlations between sociodemographic, operative and pain intensity scores were calculated at preoperative and two-year follow up time periods. A p-value less than 0.05 was considered statistically significant. Results: Forty-five patients were included with an average age of 44 years, 40% being female. Predominant axial back pain intensity was reported in 26 patients and radicular pain intensity in 19 patients. A preoperative average severe NRS intensity was reported among those with axial back pain (9.1/10.0) and radicular pain (8.8/10.0). At the two-year evaluation, patients with predominant radicular pain (3.6/10) had the most significant post operative pain intensity improvement when compared to predominant axial back pain (4.3/10). Conclusion: This study shows a higher reduction in the magnitude of radicular pain intensity among Hispanics with IS who underwent PLIF at two-years of follow up. Compared to axial back pain, Hispanics with IS who undergo PLIF and present preoperatively with predominant radicular pain, may showed higher pain improvement after PLIF.
1058
P308: Bayesian tragedy in neural tube defect screening tests in orthopedics and neurosurgery
Nery Lamothe 1 , Mara Lamothe 1 , Alejandro Alonso-Altamirano 1 , Daniel Lamothe 2 , Jesus Hernandez-Coria 3 , Francisco Castillo-Vazquez 4 , Hugo Contreras-Blancas 3 , Pedro Mojica-Guerrero 3 , Eber Martinez-Joffre 3 , Anna De la Pena 2 , Armando Martinez-Aguilar 3 , Jose Talavera-Martinez 3 , Jose Hernandez-Ortiz 3 , Sharla Rivera-Baena 3 , Alejandro Bayo del Castillo 3 , Victor Renteria-Ferruzca 3 , Victor Perez-Aguilar 3 , Hair Galan-Rosalio 3
1 Division de Ciencias Biologicas y de la Salud, Universidad Autonoma Metropolitana, Mexico City, Mexico
2 Internal Medicine, Jersey City Medical Center, New Jersey, USA
3 Orthopedics,Hospital General de Xoco, Mexico City, Mexico
4 Orthopedics, Foot and Ankle, Prince of Wales Hospital, Sydney, Australia
Introduction: There are many entities in which patients undergo unnecessary procedures because of a positive screening test result. This tragedy arises because of not knowing Bayes Theorem, which is applied to calculate the probability of truly having the disease, given a positive test result, and according to the prevalence of the disease in the population to which the patient belongs. Material and Methods: We use Bayes theorem to calculate the percentage of patients that given a positive result, given the prevalence in that subpopulation is known as well as the sensitivity and specificity of the test, indeed they do have the disease. All this using conditional probability. Results: In the case of neural tube defect, the worldwide prevalence is 2/1000, and using an ultrasound as a screening test, with a sensitivity of 97% and Specificity of 99.9%, the probability of truly having neural tube defect, given that the ultrasound test was positive, the so-called positive predictive value is 66%, which correspond to a rate of 34% false positives, patients that will be undergoing unnecessarily invasive procedures. The calculated accuracy of this screening test is 99.9%, and the negative predictive value, which is the patients that have a negative test result indeed do not have the disease is 99.9%. When the prevalence of the disease is even lower, the positive predictive value decreases. In such cases, we could encounter a positive predictive value of 5%, corresponding to 95% of patients undergoing unnecessarily invasive procedures! Conclusion: Given the high sensitivity and specificity of a screening test, if the prevalence of a disease is very low, more than half of the positive results will be false positive results, so healthy patients will be undergoing invasive additional procedures, stress, and costs, due to doxastic logic, which is the logic of the beliefs.
1222
P309: Opioid prescribing patterns among specialties in patients undergoing spine surgery
Delano Trenchfield 1 , Sebastian Fras 1 , Michael McCurdy 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Tariq Issa 1 , Josh Rogers 1 , Yazan Oghli 1 , Hassan Siddiqui 1 , Michael Vo 1 , Michael Carter 1 , Olivia Opara 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Gregory Schroeder 1
1 Orthopaedic Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: The pervasive utilization of opioids has given rise to a public health crisis, characterized by distressing rates of morbidity and mortality. A significant contributing factor to the opioid epidemic has been the propensity of healthcare providers to engage in over-prescriptive practices. Patients suffering from both acute and chronic spinal conditions often receive oral opioids as part of their treatment regimen. The management of musculoskeletal pain often involves various healthcare providers from different specialties, owing to the multidisciplinary approach adopted in patient care. Primary care physicians, pain management specialists, and physiatrists all play significant roles in addressing musculoskeletal pain. There is a lack of literature looking at the prescribing habits across these specialties; thus, our study aims to analyze preoperative and postoperative opioid prescription habits of provider specialties frequently involved in the care of patients with spinal disease over a four-year span. Material and Methods: Upon obtaining Institutional Review Board (IRB) approval, all patients older than or equal to 18 who underwent lumbar or cervical spinal fusion from 2018-2021 were retrospectively identified at our academic institution. Patients were excluded if surgery was indicated for neoplasm, infection, or trauma. Patient demographics and surgical characteristics were collected through a Structured Query Language (SQL) search and manual chart review of the electronic medical record (EMR). Opioid prescription data from one-year preoperatively to one-year postoperatively were collected through the Prescription Drug Monitoring Program (PDMP) database and providers were identified by their National Provider Identifier (NPI). One-way ANOVA was used to analyze annual trends in opioid prescriptions for each group as well as differences in opioid prescription volume between groups at various pre- and postoperative time points. Results: From 2018 to 2021, there were no significant differences in total opioid prescription volumes in orthopaedic surgery (p = 0.892), primary care (p = 0.571), pain management (p = 0.687), or physiatry (p = 0.391). For patients undergoing cervical fusion, pain management and primary care prescribed more opioids than orthopaedic surgery and physiatry between 1 year and 2 months preoperatively (p = 0.003), 2 months and 1 year postoperatively (p = 0.018), and overall (p < 0.001). We found that pain management prescribed more opioids than all other specialties between 1 year and 2 months preoperatively (p = 0.002), between 2 months and 1 year postoperatively (p = 0.008), and overall (p < 0.001) for patients undergoing lumbar fusion. When looking at all patients together in the study, pain management prescribed more opioids between 1 year and 2 months preoperatively (p = 0.003), between 2 months and 1 year postoperatively (p = 0.018), and overall (p < 0.001). Conclusion: Despite increasing national attention surrounding the opioid epidemic, our study found prescription rates have not changed significantly in spine patients undergoing spinal fusion. Pain management and primary care physicians prescribe opioids at a higher rate in the chronic periods before and after surgery, likely in part due to longer longitudinal relationships with their patients. Given the increased risk for opioid persistence after surgery in patients taking opioids preoperatively, it is imperative that all healthcare providers improve communication both with their patients and other providers to help curb the opioid crisis.
1286
P310: Epidemiology of spinal column injuries in motorcyclists for a period of ten years (2012-2022) - A retrospective study
Milos Vasic 1 , Uros Novakovic 1 , Milos Mladenovic 1 , Jovana Grupkovic 1 , Valerija Teodosic 1 , Ivan Tulić 1 , Slavisa Zagorac 2
1 Clinic for Orthopedic Surgery and Traumatology, University Clinical Center of Serbia, Belgrade, Serbia
2 Medical Faculty University of Belgrade, Head of Department of Spine Surgery, Clinic for Orthopedic Surgery and Traumatology, University Clinical Center of Serbia, Belgrade, Serbia
Introduction: Traffic trauma is the leading cause of spinal column injuries, primarily in the younger population. Spinal column injuries in motorcyclists are serious injuries, because they are often polytraumatized patients, who often require a multidisciplinary surgical approach, as well as operative treatment in the first 24 or 48 hours. Material and Methods: Retrospective study, covering a period of ten years (2012 - 2022). During this period, 2,029 patients who were injured as motorcyclists were examined in the Emergency Center of University Clinical Center of Serbia. Of these, 190 patients (9.4%) had a spinal column injury, isolated or associated with injuries to other organ systems. Upon admission to the Emergency Center, the patients were examined according to the trauma protocol, the neurological findings were assessed (according to the ASIA score), depending on the presence of other injuries and the general condition, they were admitted to the Department of Intensive Care Unit or the Department of Spine Surgery, and a decision on non-operative or operative treatment was made. Results: The injured motorcyclists were predominantly male (180; 94.7%), the average age was 37 years, they were predominantly injured in the summer months. The most frequently injured segment was the thoraco-lumbar junction (129; 67.9%). The patients were most often polytraumatized, most often chest trauma and other orthopedic injuries. In 118 patients (62.1%), an indication for operative treatment was established. The majority of patients had no neurological disorder (ASIA E), 9 patients had quadriplegia (ASIA A) and 19 patients had paraplegia (ASIA A). After the surgical treatment, the neurological findings were followed (during the hospital and rehabilitation treatment, up to 12 months after the injury). Of the 118 operated patients, the same neurological findings were noted in 98 patients (90 patients with normal neurological findings, 5 patients with paraplegia, 3 patients with quadriplegia), and in 20 patients an improvement in neurological findings was noted (14 patients with paraplegia had postoperatively ASIA B/C/D/E; 6 patients with quadriplegia had postoperatively ASIA B/C/D). Conclusion: Patients injured in traffic trauma who have a spinal column injury, especially those with spinal cord injury and associated injuries, represent a special challenge, both in terms of diagnosis and treatment. In this study, in patients with spinal cord injury, drug therapy with methylprednisolone was applied according to the NASCIS protocol, and surgical decompression was performed in the first 24h or 48h, which had a favorable effect on the outcome of neurological findings postoperatively. During the following period, a increase in the number of injured motorcyclists with spinal column injuries was observed every year on the territory of Serbia, except for the period of the beginning of the COVID-19 pandemic, from March 2020 to the end of 2020, when a much smaller number of injured motorcyclists was recorded.
Keywords: spinal column injuries; motorcyclists; traffic accident; polytrauma
1325
P311: Vertebral column traumatic injuries: epidemiological analysis in Eastern European countries
Oleksii Nekhlopochyn 1 , Anna Nikiforova 2 , Vadim Verbov 3 , Tetyana Yovenko 2 , Ievgen Cheshuk 3
1 Spine Neurosurgery
2 Scientific and Organizational Department
3 Restorative Neurosurgery Department, Romodanov Neurosurgery Institute, Kyiv, Ukraine
Introduction: Vertebral column fractures, despite their relatively small proportion in the overall structure of human musculoskeletal trauma, represent a significant medical and social problem. Even injuries not accompanied by neurological deficits often lead to persistent impairments in the functional capacity of the affected individuals, significantly affecting their quality of life, employability, and social activity. The epidemiology of spinal trauma is insufficiently understood, largely due to the difficulty in accurately assessing its true frequency. Existing literature on the epidemiology of vertebral column trauma is mostly based on single-center or multicenter studies focused on specific regions. The aim of our study is to conduct a preliminary analysis of the epidemiological features of vertebral column trauma in Eastern European countries. Material and Methods: Statistical data from the Global Burden of Disease database were analyzed to investigate the epidemiology of spinal trauma. The study focused on countries located entirely within the European part of the Eurasian continent. A 30-year period prior to the onset of the COVID-19 pandemic (1990-2019) was selected as the optimal time frame to reflect the current state of the problem. The main analysis parameters included disease incidence and years lived with disability. Results: It was found that the relative frequency of vertebral column trauma is higher in countries with a higher gross domestic product. Over the analyzed period, all Eastern European countries exhibited a declining trend in the relative frequency of vertebral column trauma. In the overall structure of musculoskeletal trauma, vertebral column trauma accounts for 3.5-4.5% in Eastern European countries, and this figure is progressively increasing. Armed conflicts in the Republic of Moldova in 1992 and in Ukraine starting from 2014 are characterized by an increase in the frequency of vertebral column trauma. The proportion of males among those with vertebral column trauma is relatively stable and specific to each of the examined countries. In contrast to the conflict in Transnistria, the armed conflict in eastern Ukraine did not significantly alter the gender structure of vertebral column trauma patients, indicating a larger proportion of civilians among the affected individuals. Analysis of the causes of vertebral column injuries revealed that, on average, unintentional injuries account for approximately 81%, injuries resulting from road traffic accidents account for 16%, intentional injuries represent about 3%, with the latter two gradually decreasing. Almost half (42-46%) of vertebral column trauma cases occur in the age group of 20‒44 years. In countries with a high gross domestic product, a significantly higher frequency of injury among the elderly and the elderly population is recorded, possibly due to more efficient diagnostic methods. Conclusion: Gender and age characteristics of vertebral column trauma have a relatively stable pattern specific to each of the examined countries. Numerous socio-economic and behavioral factors influence the frequency of vertebral column trauma, but the significance of these parameters requires further research.
1334
P312: Cracking the spine ceiling: unveiling gender disparities in orthopedic spine match rates
Kathryn Jurenovich 1 , Hania Scahzad 2 , Lisa Cannada 3 , Nazihah Bhatti 2 , Melissa Erickson 4 , Elizabeth Yu 2 , Alexandra Sheldon 2
1 Southwoods Health, Boardman, USA
2 The Ohio State University, USA
3 Novant Health
4 Duke University, USA
Introduction: Examining a decade of data from the SF Match database, this study sheds light on the gender disparities within orthopedic subspecialty fellowship applications in the USA, particularly in spine fellowships. The spine fellowship match has become one of the most competitive orthopedic subspecialty matches. However, spine has the lowest percentage of female applicants matched compared to all orthopedic subspecialties. This research calls for increased efforts to address gender disparities in orthopedic training programs and advocates for greater diversity and equity within the field. Material and Methods: The SF Match is a residency and fellowship match service which is a platform that aids both applicants and residency programs in conducting applicant reviews and ranking processes. This study utilized match data from the SF Match database, analyzing orthopedic subspecialty trends in fellowship applications from 2011 to 2021. Results: In the 2011-2021 period, the SF Match dataset for orthopedics and its subspecialties included 6,976 successfully matched applicants, with 87.7% men and 12.3% women. Female applicants' match rates varied among subspecialties: Pediatrics (37.8%), Tumor (28.3% in 2019-2022), Foot and Ankle (19.5%), Trauma (15.3%), Sports (10.3%), Shoulder (8.8% in 2017-2021), Hip/Knee/Tumor (6.8%), and Spine (6.2%). Pediatrics consistently had the highest female match rate (30%-46%). Foot and Ankle ranged from 10% to 26%, while Trauma exhibited wider variations (5%-25%). The shoulder had a range of 3%-14%. Spine and Shoulder had the lowest percentages (4%-11%). The Tumor specialty, with data available from 2019, fluctuated between 21% and 38%. The data indicates that this trend began with 5 out of 53 (9%) female applicants in 2011, 4 out of 67 (6%) in 2012, 3 out of 69 (4%) in 2013, 3 out of 82 (4%) in 2014, 5 out of 79 (6%) in 2015, 3 out of 93 (3%) in 2016, 7 out of 82 (9%) in 2017, 5 out of 119 (4%) in 2018, 6 out of 108 (6%) in 2019, 6 out of 101 (6%) in 2020, and finally, 14 out of 129 (11%) in 2021. Conclusion: The study reveals significant gender disparities in orthopedic subspecialty fellowship applications, particularly in spine fellowships. Further exploration of the data uncovers that the percentage of female applicants matched remained relatively consistent despite an increase in the number of fellowship spots each year. This suggests that spine surgery has consistently attracted fewer female applicants over the past decade. This low representation is influenced by misconceptions about women being deterred by lifestyle and physical demands, which need to be debunked. Instead, intellectual interest should be the driving force behind career choices. Additionally, negative aspects of the application process, including discouragement and discrimination, are concerning. While early exposure and mentorship play pivotal roles in inspiring women in orthopedics, the limited representation in spine fellowships raises questions about inclusivity in leadership roles. To address these disparities, a multifaceted approach focusing on mentorship, early exposure, support networks, inclusive interviews, and eliminating discrimination is imperative.
1338
P313: Evaluation of the congruency of NSQIP outcomes with propensity matched ACDF, PLDF Cohorts from an Academic Institutional Registry
Parker Brush 1 , Omar Tarawneh 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Alexa Tomlak 1 , Nicholas Pohl 1 , Grace Bowen 1 , Patrick Fitzgerald 1 , Delano Trenchfield 1 , Alan Hilibrand 1 , Jose Canseco 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Orthopaedic Surgery, Rothman Institute, Thomas Jefferson University, Philadelphia
Introduction: Over the last decade large administrative and clinical databases such as the National Surgical Quality Improvement Program (NSQIP) have become valuable tools, offering insight into nationally representative samples thereby facilitating the study of trends and short-term postoperative outcomes. However, concerns regarding the validity and limitations of these databases have generated significant debate within the orthopaedic research community. The current study aimed to investigate these concerns by comparing a patient population undergoing anterior cervical discectomy and fusion (ACDF) and posterior lumbar decompression and fusion (PLDF) using our high-volume institutional data to the NSQIP database to determine the congruency of baseline characteristics and postoperative outcomes between these two data sets. Additionally, we sought to assess the comprehensiveness of short-term outcomes recorded in the NSQIP database and compared these findings to long term follow-up data within our institution’s registry. Material and Methods: Using current procedural and technology codes (CPT) codes this study compared single- institutional data from a high-volume academic setting to data obtained from the NSQIP database for one-level ACDF and PLDF procedures performed on adult patients between 2016-2020. Patients were excluded if they underwent surgery for infection, or tumor. Demographics and surgical characteristics were collected. Statistical analysis included either t-test or Mann Whitney U-test for continuous variables and chi-squared test or Fisher’s exact test for categorical variables. The institutional cohorts were propensity matched to the ACS NSQIP cohorts for both ACDF and PLDF procedures by patient sex, race, age, ASA class, BMI, smoking status comorbidities. P-values of less than 0.05 were considered statistically significant. Results: Following propensity score matching, baseline characteristics were not statistically different, between our institutional cohort and the NSQIP database, suggesting cohort congruency. Postoperative complication rates also did not differ significantly between the matched cohorts. Institutional ACDF patients had shorter operative times and length of hospital stays compared to the NSQIP cohort. Notably, the PLDF institution cohort had a higher 30-day readmission rates than the NSQIP cohort, while the ACDF cohort had similar 30-day readmission rates across the institutional and NSQIP cohorts. However, it is important to note that our institutional 90-day readmission rate was five times higher in the ACDF cohort and two times higher in the PLDF cohort comparted to the 30-day readmission rate of the NSQIP cohort displaying the NSQIP limitations. Conclusion: The current study describes a rigorous comparative analysis of matched NSQIP and institutional cohorts who underwent ACDF, PLDF at an academic institution. This works sought to contribute to a deeper understanding of the strength and limitations of large databases. Clinician should be advised of the inherent limitations of large databases while being open to the reliability of these databases in the context generating hypothesis and setting a foundation for future prospective and multi-institutional data. Finally, the current analysis underscores the importance of capturing long-term follow-up data and the necessity to improve the quality and comprehensiveness of large databases.
1399
P314: Return-to-golf following spine surgery
Kendra Cooper 1,2 , Aiyush Bansal 1 , Venu Nemani 1 , Philip Louie 1
1 Neurosurgery,Virginia Mason Medical Center, Seattle, USA
2 School of Medicine,University of Washington, Seattle, USA
Introduction: Despite the high prevalence of spinal injuries that occur within the golfing population, little information exists in the literature on when and how to safely return golfers to play following a spinal operation. The purpose of this study is to gain a deeper understanding of when players are able to return to golf across various levels following spine surgery. Secondarily, the data obtained in this study can help establish benchmarks related to ability to return to golf after these procedures. Materials and Methods: All patients between 18-89 years old that played at least one 18-hole round of golf per year and underwent a cervical or lumbar laminectomy or microdiscectomy, 1-level lumbar fusion, cervical disc replacement, or anterior cervical discectomy and fusion between January 2019 and July 2023 were eligible for this study. They completed a questionnaire, distributed via email, that retrospectively assessed varying aspects of the patient’s golf game before and after their operation [PL2]. Paired two sample t-tests were used to evaluate the difference in average, self-reported, club distances (yards) between pre-injury and 6 months post-operation as well as between pre-injury and 12+ months post-operation distances for the wedge, 7 iron, 5 iron, and 3 wood golf clubs. Results: To date, 8 patients have completed the study. The average age of the enrollees was 64.25 years (range, 51-78). 7 were males and 1 was a female. All respondents completed the survey 12 or more months post-operation. 75% (n = 6) of golfers returned to golfing 9 holes on average between 5-7 months post-operation and 62.5% (n = 5) of golfers returned to golfing 18 holes on average 5.8-7.8 months post-operation. 25% (n = 2) of participants who were greater than 12 months post-operation had not returned to golfing on a course at all. General trends indicate a near complete recovery of ability to hit the golf ball by 12+ months post-operation, however, there is no statistically significant difference between any of the average distances when comparing pre-injury to both post-operation time points. Conclusions: Early results show that the majority of golfers who undergo a spinal operation return to playing 18 holes between 5.8-7.8 months and return to near pre-injury levels of club distance performance at 12+ months post-operation. More time and data collection within this investigation will help better discern whether the timing of this return to play is safe and how these golf-game metrics differ based on type of spinal operation the golfer had.
1426
P315: Ergonomics in spine surgery: a systematic review
Murad Alostaz 1 , Aiyush Bansal 1 , Purnima Gyawali 1 , Philip Louie 1
1 Neurosurgery, Virginia Mason Medical Center, Seattle, USA
Introduction: Spine surgery is a physically demanding field that poses several risks to surgeons, particularly with musculoskeletal disorders. Despite the well-documented consequences of musculoskeletal injuries endured by surgeons, surgical ergonomics in spine surgery has received limited attention. This systematic review aims to synthesize existing studies and highlight the significance of ergonomic considerations for spine surgeons' well-being and the impact on patient outcomes. Materials and Methods: Following PRISMA guidelines, a comprehensive literature search was conducted in PubMed and Embase. Studies focusing on surgeon ergonomics in spine surgery were selected. Data extracted included study details, surgeon demographics, ergonomic factors, and outcomes. Qualitative analysis was performed due to the heterogeneous nature of study designs and criteria. Results: Nine studies met inclusion criteria. Six studies utilized surveys to explore physical challenges, prevalence rates of pain, work practices, and ergonomic tools. Two studies employed optoelectronic motion analysis to assess spinal angles of the surgeon during surgery. One study applied video analysis to scrutinize surgeons' neck postures during the case. The results demonstrated a varying prevalence and diverse presentations of musculoskeletal disorders, varying impact on surgical performance, and nuanced relationships between experience, workload, and ergonomic concerns. Conclusion: This systematic review summarizes the heterogenous evaluations of ergonomics in spine surgery. Understanding ergonomics risks in this population is the first to working towards the prevention of musculoskeletal injuries, promoting surgeon well-being, and improving patient care. Collaborative efforts are needed to integrate ergonomic considerations into the fabric of spine surgery, ensuring improved outcomes for both surgeons and patients.
1602
P316: A cross-sectional analysis of gender disparities among orthopaedic surgery faculty
Delano Trenchfield 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Alexa Tomlak 1 , Olivia Opara 1 , Teeto Ezeonu 2 , Tiffany Bridges 3 , Henley Spracklen 4 , Eddie Runquist 4 , Sydney Baker 2 , Alan Hilibrand 1 , Jose Canseco 1 , Christopher Kepler 1 , Gregory Schroeder 1 , Alex Vaccaro 1
1 Spine Department, Rothman Orthopaedic Institute, Philadelphia, USA
2 Thomas Jefferson University, Philadelphia, USA
3 Jefferson Health- New Jersey, Stratford, USA
4 Drexel University, Philadelphia, USA
Introduction: This study analyzed gender disparities in faculty rank between orthopaedic subspecialties among currently practicing orthopaedic surgeons in the USA. A secondary objective was to examine trends in female representation across orthopaedic subspecialties over time. Material and Methods: A cross-sectional analysis of current academic orthopaedic surgery faculty in January 2023 was conducted using data from the Doximity database and academic program websites. Data from 1962 to 2021 related to gender, academic rank, residency graduation year, and completed fellowships were collected. Academic rank was categorized as assistant professor, associate professor, or full professor with those holding other titles such as instructor, clinical assistant professor, clinical associate professor, clinical professor or faculty members who were in exclusively research positions, professor emeritus, and those classified as affiliated, courtesy, voluntary, or visiting faculty being excluded. Analyses were conducted based on type and number of fellowship(s) as well as graduation year. Specifically, surgeons were categorized as having completed no fellowships, multiple fellowships, or an adult reconstruction, foot and ankle, sports medicine, spine, trauma, pediatrics, hand, musculoskeletal oncology, or shoulder and elbow fellowship. Surgeons who completed multiple fellowships were grouped together regardless of the combination. Chi-squared analyses were performed to determine significant changes in female representation over time, with statistical significance set at p < 0.05. Results: Out of 2,220 orthopaedic surgery faculty, 86.6% were male, and 13.4% were female. The majority were assistant professors (48.7%), followed by associate professors (26.3%) and professors (25.0%). Spine (2.22%), adult reconstruction (5.02%), and general orthopaedics (8.11%) were found to have the smallest overall percentage of faculty positions held by women whereas pediatrics (27.4%), hand (21.46%), and oncology (21.05%) displayed the highest among the subspecialties. Over the past decade, sports medicine, adult reconstruction, hand, and pediatrics saw significant increases in female representation. However, spine, shoulder and elbow, oncology, foot and ankle, trauma, general orthopaedics, and multiple fellowship-trained surgeons showed no significant changes in female representation. Conclusion: This study highlights ongoing gender disparities in orthopaedic surgery faculty ranks in the USA. While some subspecialties have seen improvements in female representation, others remain male-dominated. Initiatives to promote gender diversity, enhance female involvement in academic events, and address gender biases in research are crucial to achieving gender parity in orthopaedic surgery academia and practice. Efforts should be made to encourage mentorship and support for female orthopaedic surgeons, particularly in traditionally male-dominated subspecialties like spine and adult reconstruction. Addressing these disparities will not only benefit female orthopaedic surgeons but also contribute to a more inclusive and diverse field.
1619
P317: Incidence of Vitamin D deficiency in spine patients in Sarawak - A cross sectional study
Nur Aida Faruk Senan 1 , Shen Liang Tey 1 , Kavinan Subramaniam 1 , Zi Hao Phang 1 , Sophia Allo Matthew 1 , Ying Chyi Chong 1 , Melissa Chong 1 , Joseph Lau 1 , Mohammad Zaki Mohd Amin 2
1 Orthopedics, Sarawak General Hospital, Kuching, Malaysia
2 Orthopedics, University Malaysia Sarawak, Kuching, Malaysia
Introduction: Vitamin D Deficiency / Insufficiency is considered as a worldwide endemic disease with systemic studies concluding the status of vitamin D deficiency in various parts of the world and its effects on not just calcium metabolism and haemostasis, but in immune system modulation as well as its role in hormone regulation. Vitamin D, one of the essential fat soluble vitamins, has always been known to be involved in regulation of overall health via calcium homeostasis and bone metabolism. A daily recommended supplemental dose of 100 - 800 IU per day, is severely underestimated as most of the current population is deficient to begin with. We suspect a high incidence of Vitamin D deficiency in Malaysia despite being located close to the equator due to lifestyle changes, reduced outdoor sun exposure and poor nutritional intake. The reference range was deficient if less then 50 nmol/L, insufficient if between 50 - 74 nmol/L and sufficient if more then 75 nmol/L. Material and Methods: Serum 25(OH) Vitamin D levels were taken and evaluated for all spine inpatient admissions and some spine clinic patients from February to June 2023. The results obtained are then reviewed with relation to gender, BMI, age and pathology. The serum vitamin D levels of 80 spine patients were collected in this study. Results: Out of 80 patients, nearly half of them (49.2%) are vitamin D deficient (< 50 nmol/L) and 22% having insufficient levels of serum vitamin D (50-74 nmol/L). Only 28.8% had levels more then 75nmol/L. In this sample size, female patients (45.86 nmol/L) have slightly lower average serum 25-OH vitamin D levels compared to male patients (49.28 nmol/L). Substantial Variations in vitamin D levels can be observed when comparing different age groups. Teenagers (13-19 years old) had the lowest average levels at 39 nmol/L, followed by the middle age (40 - 59 years old) at 55 nmol/L. The adult (20-39 years old) had the highest at 66nmol/l and elderly (> 60 years old) was 59 nmol/L. Out of the 4 subgroups of spine pathology (tumour, degenerative / osteoporosis, infection and trauma), the latter 3 groups were vitamin D deficient. Patients who are overweight (BMI 25 - 30), and obese (BMI > 30) show low levels of serum 25 (OH)D. Among 80 patients, 45% are obese (BMI > 30) or overweight (BMI 25-30), within these patients, 67% (24 out of 36) have vitamin of less than 74 nmol/L. Conclusion: The incidence of Vitamin D Deficiency and Insufficiency among patients with spine pathology makes up 71.2% of the total sample size collected with almost half of them having serum vitamin D levels of Less than 50 nom/L. When comparing Gender, male have higher average serum vitamin D compared to females, but both levels were still deficient. Obese patients have a higher rate of deficiency.
1632
P318: The unexpected national COVID experiment: decrease in elective lumbar surgery leads to higher incidence of cauda equina syndrome
Libby Gooda 1 , Mohamed Abdalla 1 , Emily Tsang 1 , Bisola Ajayi 1 , Samuel Walters 1 , Timothy Bishop 1 , Jason Bernard 1 , Darren Lui 1
1 St. George's University of London, London, United Kingdom
Introduction: Progressive degenerative disorders of the spine can lead to cauda equina syndrome (CES) in some patients. Elective surgeries were dramatically reduced during the COVID-19 pandemic to preserve NHS and ICU beds. We hypothesized that reduced elective lumbar surgery would lead to an increased incidence of CES. Material and Methods: We collected UK hospital episode statistics data from the pre-COVID era (01 April 2017- 31 March 2020) and the COVID-19 era (01 April 2020- 31 March 2021), for the following ICD-10 codes: M51.1 (lumbar and other intervertebral disc disorders with radiculopathy), M48.0 (spinal stenosis (main diagnosis), V33.7 (primary microdiscectomy of lumbar intervertebral disc), V25.9 (unspecified primary decompression operations on lumbar spine), V25.8 (other specified primary decompression operations on lumbar spine) and G83.4 (cauda equina syndrome). Individuals were subdivided according to their age and gender, and operations were subdivided into elective and emergency types. Results: During the COVID era, elective lumbar surgeries decreased by 44.5% (from 946 to 522) with a concurrent rise in emergency surgeries by 41.6% (from 1651 to 2349). The total incidence of CES increased by 13.0% (from 8524 to 9636). Those aged 18-59 experienced an 8.6% increase in incidence, and those aged 60+ suffered a 17.9% increase in the incidence of CES. There was a 41.0% decrease in CES incidence in those aged < 18. Total lumbar surgeries (elective and emergency) increased by 10.6% during the COVID era. Conclusion: Elective surgeries significantly decreased during the COVID era. This led to a 13.0% increase in the diagnosis of CES, as well as a 42% increase in emergency lumbar surgeries. Not operating during the COVID-19 pandemic was an unusual medical experiment for lumbar degenerative spondylosis revealing an upsurge in emergency CES surgery in patients > 50 years of age. Older adults are more likely to develop CES as a result of spinal degeneration (i.e., spinal stenosis), and therefore this is the demographic most likely to benefit from elective surgical intervention. This can explain the larger increase in CES incidence seen in > 50 year olds in this study. Inferences can be made about the importance of early surgical intervention in lumbar degeneration, particularly in those aged 50 and over.
1721
P319: The epidemiology of traumatic spine fractures in South Indian population
Goutham Santosh 1
1 Orthopaedics, Tejasvini Hospital and Shantharam Shetty Institute of Orthopaedics and Traumatology (SSIOT), Mangalore, India
Introduction: This passage discusses the distinction between Spinal Cord Injury (SCI) and Traumatic Spinal Injury (TSI), emphasizing that SCI specifically involves damage to the spinal cord resulting in neurological deficits and paralysis. TSI encompasses a wider range of spinal injuries, including damage to bones and ligaments, often caused by various traumatic events. The lack of comprehensive data, especially in low and middle-income countries, hinders understanding the global burden of TSI, hindering prevention efforts and medical care. Knowledge of injury patterns and causes is vital for prevention. The study focuses on demographics, injury severity, incidence, and causes in South India, highlighting regional variations. Material and Methods: This study took place at Tejasvini Hospital and SSIOT in Mangalore and focused on patients with traumatic spine fractures. The research had a sample size of 190 and was conducted from January 2019 to May 2022. It included patients over 18 years old with traumatic spine fractures, excluding those with pathologic fractures. Fractures were classified using radiographs and sometimes CT scans, following the AO classification system. Neurological assessments were done using the AIS, with prospective and retrospective data collection methods. Data analysis was carried out using Microsoft Excel, Word, and SPSS, and all assessments were performed by a single observer. Results: The study revealed that 66% of the patients with vertebral fractures were male, which differed from the global male-female ratio of 3.8:1, possibly due to fewer female professionals and drivers in India. High-energy accidents were more common among males, while females mostly had low-energy injuries, resulting in Type A fractures. Falls from height were the leading cause of spine fractures, followed by road traffic accidents. Unlike developed countries, sports-related injuries were not observed in this study, reflecting lower sports participation rates in India. Our data showed that there is no specific association between the mechanism and cervicothoracic and thoracolumbar fracture. Cause of the majority of the fractures was fall from height (73.7%/140 patients) and amongst which 55% (77 patients) fracture were at Thoracolumbar junction, involving T12 and L1 and only 2 patients fractures were having fracture cervicothoracic junction (C7 and T1). Amongst 40 patients with RTA, 25 patients sustained injury to thoracolumbar junction and no fracture at cervicothoracic junctional vertebrae. Thoracolumbar junction fractures were predominant, especially in falls from height. Associated injuries were common, with extremity injuries being the most frequent. Neurological deficits were found in 29% of patients, with Type B and C fractures having a higher incidence. Conclusion: The study highlights that spinal injury demographics in India differ notably from developed countries. There's a higher proportion of males, complete spinal cord injuries, and cases resulting from falls from heights and road traffic accidents involving two-wheelers. Falling from heights, particularly in the coastal belt of southern India where toddy tapping is a common profession, is a prevalent cause. This is due to the lack of proper protective equipment for those in such professions. The higher incidence of complete injuries and fewer cervical injuries underscores the urgent need for improved prehospital and acute care services. A large multicentric study is warranted to validate and expand on these findings, informing targeted prevention programs.
1912
P320: The impact of coexisting substance use disorder on perioperative outcomes in patients undergoing lumbar spinal fusion: an analysis of the National Inpatient Sample Data
Mohamed Soliman 1 , Alexander Aguirre 1 , Cathleen Kuo 1 , Ahmed Elbayomy 2 , Esteban Quiceno Restrepo 1 , Ali Khan 1 , Jeffrey Mullin 1 , John Pollina 1
1 Neurosurgery, University at Buffalo, Buffalo, USA
2 School of Medicine and Public Health, School of Medicine, University of Wisconsin Madison, Madison, USA
Introduction: Substance use disorders (SUD) hold a prominent position in global public health concerns and are associated with substantial societal and personal costs. Despite a significant increase in prevalence of patients with coexisting painful spinal conditions and SUD in recent years, perioperative outcomes and protocols to manage this emerging population are poorly characterized. This study aimed to explore the impact of comorbid SUD on lumbar spinal fusion outcomes. Materials and Methods: A retrospective analysis using National Inpatient Sample administrative data between 2009 and 2020 was carried out. Patients who underwent elective lumbar spinal fusion were identified using the International Classification of Diseases, Ninth Revision code. SUD was defined according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Variables collected included patient demographics, medical comorbidities, hospital characteristics, length of stay (LOS), perioperative complications, and total hospital charges. Univariate followed by multivariate logistic regression was performed. Results: A total of 2,877,241 lumbar spinal fusion patients were included, with 470,577 (16.4%) had a history of SUD. On multivariate analyses, patients with a history of SUB had higher risk of respiratory complication (OR = 1.21, 95%CI = 1.16-1.27, p < 0.001), greater mechanical injury (OR = 1.21, 95%CI = 1.13-1.29, p < 0.001), greater fusion disorder (OR = 1.34, 95%CI = 1.27-1.42, p < 0.001), less neurological injury (OR = 0.90, 95%CI = 0.83-1.02, p = 0.029), lower rate of wound complication (OR = 0.90, 95%CI = 0.83-0.98, p = 0.027), less hematoma (OR = 0.95, 95%CI = 0.93-0.98, p = 0.006), shorter LOS (odds ratio [OR] = 0.12, 95% confidence = 0.07-0.16, p < 0.001), and less routine discharge (OR = 0.92, 95%CI = 0.90-0.93, p < 0.001). Conclusion: This nationally representative study of inpatients in the USA provides evidence that coexisting SUD in patients undergoing lumbar spinal fusion increased the risk of respiratory complication, mechanical injury, fusion disorder, and nonroutine discharge. Development of a protocol focusing on patient-led care plans, adequate pain management, and identification of support network may contribute to better clinical outcomes.
1928
P321: Evolution of the use of social media in orthopedic surgery after the pandemic
Francoise Descazeaux 1,2 , Karen Weissmann 1,2 , Marcelo Costa 1,2 , Carlos Huaiquilaf 1,2
1 Spine Surgery, Patagonia Spine Foundation, Santiago, Chile
2 Spine Surgery, Clinica MEDS, Santiago, Chile
Introduction: During the pandemic there was an explosion in the use of Social Media as a conduit between doctors and patients. Our aim was to study if after the pandemic ended, this tendency remained. Material and Methods: Prospective, transversal descriptive study. We performed an online survey trough google forms (Google Corp., LA). This survey was designed using the Delphi method by a committee of Spine surgeons (Orthopedic surgeons). We measured demographic, academic, social traits and social media platforms used (Instagram (Meta platforms inc., CA), TikTok (ByteDance, Ch), Twitter (X Coro, DW), Youtube (Youtube, CA)) There were two cohorts named 2020 and 2023. The same survey that had been sent in 2020 was resent to the same cohort of orthopedic surgeons in 2023. The survey was sent by email and by WhatsApp (Meta platforms inc., CA) Statistical analysis was performed using paired samples t-student test (p < 0.05). Results: We analyzed 898 answers. 60.5% were females. The most frequent age groups were the 36-45 years old (37.3%), followed by the 25-35 years old (35%), 46-55 (12.6%), 56-65 (7.2%) and > 65 (4%) (p = 0.002). Considering specialization, 43.4% were subspecialists, 43.2% specialists and 13.3% were residents. 32.4% had a professional account on social media in 2023 and in 31.7% 2020 (p = 0.509). In 2020 orthopedic surgeons that used social media were 40%, decreasing to 31% in 2023 (p = 0.003). Women used fewer social media than men in 2020 (46.4% versus 53.6%); women increased their usage in 2023 (56%; p < 0.001), but remain less than men (67.3%; p = 0.021). The most used platforms are Instagram (p = 0.026), tiktok (p = 0.029), twitter (p = 0.001), and youtube (p = 0.001). Doctors who work in a private practice use more social media than those in public hospitals both in 2020 and 2023 (74% / 66% versus 65%/63%; p = 0.287). Subspecialists are the only groups that increased their use of social media post pandemic 7% in 2020 versus 9% in 2023 (p < 0.001). Since 2020, the practice of telemedicine decreased (46.4% 2020, 32.7% 2023; p < 0.001). The use of social media is more frequent among those who use telemedicine regularly (p <0 .001) and those who started their digital profile during the COVID-19 pandemic (p < 0.001). The use of social media is considered a positive aide among those who use social media in their practice (p < 0.001), those who don’t use social media considered it detrimental (p < 0.001). Conclusion: The use of social media in orthopedic surgery remained stable after the end of the COVID-19 pandemic, about 30% of doctors have a digital profile, however the use of telemedicine decreased.
2254
P322: Posterior approach as the workhorse to surgically treated spinal infection in a single center tertiary hospital in Malaysia
Ahmad Ikhwan Mohd Sharfuddin 1 , Zairul Anuar Kamarul Bahrin 1
1 Jabatan Ortopedik, Hospital Pulau Pinang, Georgetown, Malaysia
Introduction: Surgically treated spinal infection represents a major burden on the spine service. We present a retrospective case series of patients who was treated surgically for spinal infection. Material and Methods: A search was done in the local database of a single tertiary center in Malaysia from 1 July 2021 to 30 June 2023 for operatively treated spinal infection and the data was collected and tabulated on analyzed using Google sheets. Results: 56 patients whose average age was 54.3 years old ranging from 7 to 76 years old with 27 males and 29 females. 60.7% was pyogenic infection while 39.2% was tuberculous infection with 9 smear positive and 13 smear negative. 21.4% presented with neurological deficit. Tuberculous infection more commonly involved the thoracic and thoracolumbar junction (21.4%) while pyogenic infection more commonly involved the lumbar and thoracolumbar junction. 33.9% were more than 65 years old. 21.4% had pyogenic infection and 12.5% had tuberculous infection. Both pyogenic and tuberculous infection affects 2 levels with 21 and 12 respectively while only 2 cases involved more than 3 levels. 35 cases underwent anterior (2) and posterior (33) instrumentation while 37.5% had no instrumentation done. Conclusion: Surgically treated spinal infection continues to represent a major burden to the overall spine service in this country. Tuberculosis represents a significant proportion of cases in the community and must continue to be given special attention. A larger proportion of patients required posterior instrumentation reflected the workhorse of surgical management of spinal infection.
2433
P323: Epidemiological study of the prevalence of low back pain in spine surgeons in Brazil
Luiz Claudio Rodrigues 1 , Fernanda Andrea Navarro 2 , Rodrigo Nakao 2 , Nathalia Adelina Pereira 1 , Luiz Phelipe Tavares Rodrigues 1
1 Orthopedic Surgery, Santa Marcelina University of Medicine, São Paulo, Brazil
2 Spine Surgery, Hospital Santa Marcelina, São Paulo, Brazil
Introduction: Occupational low back pain is the largest single cause of work-related health disorders (37% of low back pain is attributed to occupational risk factors) and absenteeism (responsible for large economic losses), being responsible for approximately a quarter of disability cases. premature and temporary or permanent work incapacity.3,5 In the USA, approximately 149 million working days are lost every year because of low back pain, with a total indirect cost of US$100 to 200 billion per year, through loss of salary, productivity, legal and life insurance expenses. Material and Methods: Objective: To determine the prevalence of low back pain in spine surgeons. Method: A non-randomized quantitative cross-sectional clinical study was carried out on a sample of 95 spine surgeons in Brazil, using the Oswestry and visual analogue pain scales, in addition to a structured questionnaire to characterize the research participants. Results: Among the studied population, 69.5% were orthopedists and 30.5% were neurosurgeons and the average age of the sample was 46 years (±10.6), with neurosurgeons being older than orthopedists. In relation to BMI, the majority (77.8%) were overweight and obese and seventy-six percent performed physical activity. The prevalence of low back pain was 58.9%. No relevant differences were found in the time spent weekly in surgeries, between those who had low back pain and those who did not (p = 0.364). The average pain intensity was 2.0 (SD = 2.2), being statistically (p = 0.025) higher in orthopedists (2.3) when compared to neurosurgeons (1.3). Regarding the ODI score, 98.2% of surgeons had minimal disability (0-20%) for daily activities. Conclusion: In general, the present study concluded that the prevalence of low back pain in spine surgeons is high and that most individuals have a mild inability to carry out daily activities. However, the study was not able to correlate the time spent in weekly surgeries with the prevalence of low back pain.
2470
P324: Risk factor associated with unplanned surgical reoperations after spine surgery: joint analysis of time-to-event and latent classes
Julio Roberto Pérez Oliva 1 , Carla García-Ramos 1 , Alejandro Reyes-Sánchez 1 , Luis Migue Rosales Olivares 1 , Armando Alpizar 1 , Baron Zarate-Kalfopulos 1 , Omar Irving 1 , Fernando Reyes Tarrago 1
1 Spine Surgery, Instituto Naciona de Rehabilitación Luis Guillermo Ibarra Ibarra, México City, Mexico
Introduction: Unplanned reoperations (URs) after spine surgery constitute a highly undesirable outcome for everybody: increase patient morbidity and mortality, increase length of hospital stays and costs with no improvement in outcomes, and decrease access to care. Accordingly, preventing revision spinal surgery is a matter of cardinal significance for spine surgeons, their patients, and the healthcare system. Furthermore, reoperation rates after elective surgery have become established quality measures across multiple subspecialties, making it an important metric in evaluating and monitoring a hospital’s ability to provide safe and efficient care. A better understanding of the risk factors behind URs and their time of occurrence is warranted to approach decreasing its incidence. Either through risk factor modulation, better allocation of perioperative care or proper patient selection for elective procedures, shedding light as to why URs occur and how they can be prevented is of the utmost importance to improve surgical outcomes and prognoses. Material and Methods: Study Design. Retrospective single-center review of hospital administrative data. Objective. To investigate the risk factors for unplanned reoperation (UR) after spine surgery. Subgroups of patients who underwent spine surgery with different unplanned reoperation-free survivorship were estimated by way of a finite mixture of Cox proportional hazard models. Any spine reoperation (or death) was defined as a “terminal event”. We performed a retrospective cohort study of consecutive patients at the National Institute of Rehabilitation (Mexico) from January 2005 through December 2018. Demographics, comorbidities, region intervened (complexity) and preoperative laboratory results, were used to profile patients with different reoperation-free survivorship. Results: The analysis was completed on 1,529 patients with a mean follow-up of 7 years. Actuarial (Kaplan–Meier) estimates reveal rates of UR at 1 month,1, 3 and 5 years of 3.7%, 5.8%, 7%, and 8% respectively. The mixture modelling suggests two classes of patients that we can identify as “healthy” and “not-so-healthy”, the latter with significantly larger probabilities to encounter patients with diabetes, hypertension, smoking, ASA II, and bleeding over 300 ml in operations of over 4 hours of duration. The healthier group facing the lesser hazards of UR, which translates into a difference of 6.6 percentual points by the tenth year after the index spinal surgery. Conclusion: Patients with a vertebral compression fracture and those that require multilevel surgery should be counseled on the elevated risk of re-intervention associated with spine surgery.
Imaging
79
P325: Usefulness of side-bendings RX for fusion levels selections in adolescents idiopathic scoliosis
Sofía Frank 1 , Lucas Piantoni 1 , Rodrigo Remondino 1 , Eduardo Galaretto 1 , Mariano Noël 1 , Boris Falconi 1 , Carlos Tello 1
1 Spine Disease Unit, Hospital de Pediatría Juan P. Garrahan, Ciudad Autónoma de Buenos Aires, Argentina
Introduction: Adolescent idiopathic scoliosis (AIS) is a spinal deformity that affects the axial, coronal, and sagittal planes and changes over time. Among the traditional methods to evaluate the structurality of the curves, Cobb angle measurements in side-bending radiographs (SBR) has been described. Flexibility of the curve greater than 25° in the coronal plane in the SBR is one of the criteria defining curve structurality in the Lenke classification. Although it does not directly provide information on fusion levels, the classification of the curve type implies which regions should be included in the instrumentation and those regions that should be left unfused. The objective was to evaluate the usefulness of SBRs in patients undergoing AIS surgery to determine fusion levels. Material and Methods: An original electronic survey with images of eight AIS patients was sent to 16 surgeons experienced in the treatment of spinal deformity. In the first section of the survey the participants were asked to indicate if they routinely request SBR as well as to indicate the proximal (UIV) and distal (LIV) fusion levels based on anteroposterior (A-P) and lateral radiographs of the spine. In the second section of the same survey, both SBR were added and they were again asked to indicate the fusion levels. Results: All 16 surgeons surveyed completed the entire questionnaire in which they analyzed eight patients with 18 curves. Fifty-six percent felt that SBR are useful to define fusion levels. Five surgeons had a kappa coefficient of 0.81 to 1 indicating almost perfect agreement for selection of fusion levels with and without SBR, three had substantial agreement, five had moderate agreement, two had fair agreement, and only one participant had insignificant agreement. Conclusion: Our results and those of other authors suggest that it may not be necessary to use imaging studies to assess flexibility in all AIS patients to select fusion levels. Nevertheless, further studies are needed to determine which curve patterns would benefit from their use and in what cases SBR may be avoided.
134
P326: Facet joint morphology and tropism in adolescents: association with lumbar disc herniation and spondylolysis
Yoshihiro Ishihama 1,2
1 Tokushima University Graduate School, Japan
2 Masaki Orthopedic Rehabilitation Clinic, Tokushima, Japan
Introduction: Facet tropism is an older concept, but has recently seen a resurgence of interest. There have been many reports on the relationship between facet tropism and various degenerative diseases of the lumbar spine. However, most conclusions regarding facet tropism have been based on the results of studies that have evaluated this parameter only in the axial plane, studies that have been performed in middle-aged or elderly patients. There is limited information on facet joint asymmetry in the sagittal plane in adolescents. This study was performed to elucidate the bidirectional characteristics of the facet joints in adolescents. Material and Methods: The orientation of all lumbar facet joints was measured in the axial and sagittal planes on computed tomographic images for 191 patients with low back pain. The patients had a mean age of 15 (range 8-20) years and were divided into four groups according to age (< 15 or ≥ 15 years) and sex. The facet joint angle and tropism rate were compared among the groups. Facet tropism was defined as a difference in bilateral angle of > 10° in the axial plane and >5° in the sagittal plane. The association of facet tropism with disease was investigated further by analyzing facet joint orientation and the incidence of facet tropism in 116 patients with single-level lumbar disease using one-way analysis of variance followed by Tukey’s test or the Games-Howell post hoc test for facet orientation and the Kruskal-Wallis test followed by Bonferroni’s post hoc test for facet tropism. Results: Facet tropism was observed in 8.7% of axial views and 7.5% of sagittal views. Facet tropism was found most often in the lower lumbar spine in the axial plane and in the upper lumbar spine in the sagittal plane. The incidence of axial facet tropism was significantly higher in male patients aged ≥ 15 years than in female patients aged < 15 years, especially at L4/5. Facet joint morphology in the axial plane was more coronal at L3/4 and L4/5 in male patients ≥ 15 years than in those < 15 years but remained unchanged in female patients at around 15 years of age. Facet joint morphology in the sagittal plane was unchanged at around 15 years of age in both sexes. Axial facet tropism was found at L4/5 in 55.6% of patients with herniated nucleus pulposus and at L5/S1 in 25.9%. There were no significant findings with regard to sagittal facet tropism in patients with lumbar spondylolysis or those with herniated nucleus pulposus. However, there was a significant difference in sagittal facet orientation in patients with spondylolysis at L5. The facet angle was significant larger in patients with L5 spondylolysis, indicating that these patients had vertically oriented facet joints at L3/4 and L4/5. Conclusion: The facet tropism rate in adolescents is similar in the axial and sagittal planes. Facet tropism and specific morphology may be related to lumbar disc herniation and spondylolysis in this age group.
359
P327: A new comprehensive MRI classification and grading system for lumbosacral central and lateral stenosis: clinical application and comparison with previous systems
Marco Manzetti 1 , Paolo Spinnato 2 , Miriana Petrera 2 , Anna Parmeggiani 2 , Giovanni Viroli 1 , matteo traversari 1 , Alberto Ruffilli 1 , Marco Miceli 2 , Cesare Faldini 1
1 Ist Ortopaedic and Traumatologic Clinic
2 Diagnostic and Interventional Radiology, IRCCS - Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Lumbar spine stenosis consists in the reduction of the space available for the neuronal and vascular elements of the lumbar spine, mostly because of degenerative changes (arthritis and degenerative disc disease). Depending on the anatomical position, lumbar spine stenosis may affect the central canal, the foramina, the lateral recess, or any combination of the previous. Low back pain, radicular pain, neurogenic claudication, and sensory or motor deficits in the lower extremities are common symptoms of this condition, generating varying degrees of disability. Many radiological parameters and morphologic MRI classification have been proposed to better define lumbar spine stenosis, but any correlation between radiologic parameters and symptomatology remains a debated topic. Thus the aim of the present work is to propose a new MRI grading system, with qualitative assessment of the cause of stenosis and a quantitative clinical score assessment in order to evaluate the association between symptoms and MRI findings. Material and Methods: The proposed MRI system consists of a severity grading scale for central and lateral (recess and foraminal) stenosis, together with the indication of the main causes of the disease (disc, arthritis, epidural lipomatosis and a combination of these conditions). The system was applied to a cohort of patients from a single institution in the last two-years. Two radiologists with different experience evaluated all the MRIs to determine intra- and inter-observer reliability. Two orthopedic surgeons evaluated all patients and provided a grading system for central and lateral stenosis clinical scores (CS-CS and LS-CS) based on patients’ symptoms. Lastly, the most used previous MRI systems have been applied, and their performances have been compared to the new proposed system. Results: One hundred and eighty-eight patients have been included in this study (92 females - mean age 61.3 ± 8.7 years old). A high intra-observer agreement for the assessment of central stenosis, foraminal stenosis, and lateral recess stenosis was found (weighted Kappa values: 0.939, 0.948 and 0.954 respectively). The inter-observer agreement was high for central stenosis and foraminal stenosis and was substantial for lateral recess stenosis (weighted Kappa values: 0.868, 0.832 and 0.638 respectively). The grading system revealed a strong association with CS-CS for both readers, with Goodman and Kruskal’s gamma index (with 95% confidence interval) of 0.678 (0.533-0.809) and 0.605 (0.459-0.750), respectively. The association with MRI grading and LS-CS resulted to be moderate for foraminal stenosis and the concomitant presence of foraminal and lateral recess stenosis, with Goodman and Kruskal’s gamma index of 0.333 (0.120-0.552) and 0.296 (0.096-0.5), respectively. A weak association was found between lateral recess grading alone and LS-CS with gamma index of 0.102 (0.193-0.397). The proposed grading system showed a good association with clinical symptoms, compared with previous systems, both for CS-CS and for LS-CS. Conclusion: A standardized grading system for lumbar spine stenosis that includes all of the major contributing factors (including disk, arthritis and lipomatosis), for the central canal, lateral recess, and neural foramina and could be useful and practical tool for defining the stenosis, lowering inter-observer variability, and potentially directing the various treatment options.
368
P328: Prospective cohort study investigating the impact of muscle degeneration in low back pain after lumbar decompression
Pedro Henrique Couri 1 , Alberto Gotfryd 1 , Eliane Antonioli 1 , Mario Lenza 1 , Adham Castro 2 , Frederico Miranda 2 , Eduardo Baptista 2
1 Orthopaedics
2 Radiology, Hospital Israelita Albert Einstein, São Paulo, Brazil
Introduction: The main reason for surgical procedures in the lumbar spine is nerve compression associated with radiculopathy or neurogenic claudication. Lumbar surgical decompression is effective to relieve neurogenic pain and restore walking ability [1-5]. However, the presence of associated preoperative low back pain (LBP) in patients with neurological symptoms is not uncommon, and its management is still controversial [6-9]. Chronic dysfunctions, such as atrophy and muscle fat replacement of the main spine muscles, are related to pain intensity. These dysfunctions can be identified and measured by means of magnetic resonance imaging (MRI), as muscle fat infiltration and reduction of muscular cross-sectional area [7-18]. The primary objective of this study is to correlate the degree of muscle degeneration with the presence of LBP before lumbar decompression surgery. The secondary objectives are evaluations of the impact of different surgical techniques in muscle degeneration, as well as of the association of pain, disability, quality life and psychosocial factors during recovery after lumbar decompression surgery. Material and Methods: This prospective cohort will include individuals older than 18 years, who underwent surgical lumbar decompression. Radiographic exams and MRI examination will be performed before surgical procedure. Changes in scores of pain [10], kinesiophobia, psychosocial risk prognosis [11-13], perception of improvement, anxiety, depression [13], disability [14] and quality of life [15] will be measured at baseline, 3, 6 and 12 months of follow-up. The primary outcome will be evaluation of the intensity of LBP. This study protocol complies with the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [16]. Study design: A single center prospective cohort. Inclusion criteria
• adults aged 18 years and older;
• symptoms of lumbosacral neural compression (radiculopathy or neurogenic claudication);
• failed conservative treatment for, at least, 6 weeks;
• undergoing surgery for neural decompression (discectomy and/or foraminotomy and/or hemilaminectomy);
• with preoperative MRI image.
Exclusion criteria
• need for lumbar fusion;
• spondylolisthesis > Meyerding Grade I [19];
• deep infection requiring surgical debridement;
• patients submitted to lumbar facet rhizotomy;
• active rheumatologic disease, including seronegative arthropathies;
• reoperation.
Results: We reported reductions in ODI score means in postsurgical estimates from baseline in patients with and without fat infiltration (p < 0.001 in all comparisons), and significant reductions in mean ODI scores at 3-, 6- and 12-months postoperative estimates from baseline in patients with and without fat infiltration (p < 0.05 in all comparisons). Recruitment Start Date: January/2020. Recruitment Estimated End Date: December/2022. Status: Recruiting. Conclusion: According to partial statistical reports, there is a suggestion that patients with less fat infiltration have less low back pain and less disability during serial postoperative evaluations, considering ODI scores.
873
P329: Computed tomographic morphologic analysis of cervical spine and considerations of parameters for pedicle screw placements in Indian population
Kandarpkumar Patel 1,2 , Hari Menon 1 , Ankit Chauhan 3
1 Department of Orthopaedics, Government Medical College, Surat, India
2 Department of Spine Surgery, New Sheth P.T. Multispeciality Hospital, Surat, India
3 Department of Radiology, Navkar Imaging Center, Surat, India
Introduction: Cervical pedicle screw fixation is a technically demanding procedure because of risk of damage to surrounding neurovascular structures. Understanding morphology of cervical spine would reduce the risk of catastrophic complication of neurovascular injury. The aim of the study was to understand morphology of cervical spine anatomy and parameters by using Computed Tomography Scan. Material and Methods: This is a retrospective observational study. 26 patients underwent cervical spine CT scan in our institute between 1st Jan 2021 to 30th June 2021. On reconstructed CT scan images various parameters were calculated. Dimensional parameters like Outer Pedicle Width (OPW), Inner Pedicle Width (IPW), Outer Pedicle Height (OPH), Inner Pedicle Height (IPH), Pedicle Axis Length (PAL), Lateral Pedicle Distance (LPD), Superior Pedicle Distance (SPD) and Angular parameters includes Pedicle Transverse Angle (PTA), Pedicle Sagittal Angle (PSA). Results: Total numbers of 260 pedicles were measured in this present study. The mean pedicle diameters were increasing from C3 to C7. The male patients had larger diameter of pedicles compared to females. Pedicle Axis Length which can be consider for maximum possible screw length was ranging from 29 mm to 32 mm. Lateral pedicle distance was ranging from 1mm to 3 mm. The PTA was wider in upper (C3, C4 – approx. 46-47) and lower cervical vertebrae (C7- approx. 44-45) while it was more acute in mid cervical vertebrae (C5, C6- approx. 49). The PSA changed from upward inclination at upper cervical spine to the downward inclination at lower cervical spine. Conclusion: This study has demonstrated that cervical vertebra has variable pedicle size and angular parameters. To enhance the safety of cervical pedicle screw insertion preoperative CT scan should be performed to understand the morphology and trajectories for screw insertion.
1099
P331: Application of a deep learning model for sagittal alignment and instability measurement in cervical spine radiographs
Huajiang Chen 1
1 Orthopedics, Shanghai Changzheng Hospital, Shanghai, China
Purpose: To automatically measure sagittal alignment and evaluate the instability of cervical spine by measuring the segmental Cobb angle and horizontal translation of cervical spine on lateral cervical X-rays, a deep-learning model was proposed and the reliability and accuracy were evaluated. Methods: A TCD net model as the core of the deep-learning model was proposed to separately detect and segment all vertebral bodies on lateral cervical X-rays, and the segmental Cobb angle and horizontal translation of cervical spine were measured from the output of the CNN model. The Cobb angle on 1126 lateral cervical X-rays and segmental Cobb angle and horizontal translation from 448 paired X-rays from Picture Archiving and Communication Systems (PACS) were measured automatically using a deep-learning model, the reliability, accuracy of the deep-learning model were fully evaluated, and two experienced observers separately measured Cobb angle and instability on the aforementioned X-rays manually. Results: For manual measurement of the Cobb angle on cervical plains, the intraclass correlation coefficient (ICC) analysis was calculated. The intra-observer coefficient of the two observers both was > 0.98, and the inter-observer coefficient in twice interval measurements was both > 0.98. The mean absolute differences (MAD) were both 1.55°and 1.71°. For deep learning method, the network achieved MAD at level of 1.9°and 2.0° respectively when measuring digital images and films. Using the value of segmental Cobb angle in manual measurements > 11° or horizontal translation >3.5mm as a reference standard for cervical instability, the deep learning method achieved a high level of sensitivity (99.4%) and specificity (97.4%) for diagnosing cervical spine instability on X-rays.Conclusion: Measurement of sagittal alignment and evaluation of instability of the cervical spine by measuring the segmental Cobb angle and horizontal translation on lateral cervical X-rays, a deep-learning method was proposed and demonstrated excellent reliability and accuracy in angulation and good sensitivity and specificity in detecting cervical instability.
Keywords: X-ray images; neurol network; deep learning; sagittal alignment; instability
1260
P332: Automated detection and measurement of dural sack cross-sectional area in lumbar spine MRI using deep learning
Frank Hassel 1 , Babak Saravi 2 , Alisia Zink 1 , Sara Ülkümen 2 , Sébastien Couillard-Després 3 , Wollborn Jakob 4 , Gernot Michael Lang 2
1 Department of Spine Surgery, Loretto-Krankenhaus, Freiburg, Germany
2 Orthopedics and Trauma Surgery, University Freiburg, Freiburg, Germany
3 Institut for Experimental Neuroregeneration, Paracelsus Medical University, Salzburg, Austria
4 Dept. of Anesthesiology, Havard Medical School, Boston, USA
Lumbar spine magnetic resonance imaging (MRI) is a critical diagnostic tool for the assessment of various spinal pathologies, including degenerative disc disease, spinal stenosis, and spondylolisthesis. The accurate identification and quantification of the dural sack cross-sectional area are essential for the evaluation of these conditions. Current manual measurement methods are time-consuming and prone to inter-observer variability.
Our study developed and validated deep learning models, specifically U-Net, Attention U-Net, and MultiResUNet, for the automated detection and measurement of the dural sack area in lumbar spine MRI, using a dataset of 515 patients with symptomatic back pain and externally validating the results based on 50 patient scans. The U-Net model achieved an accuracy of 0.9990 and 0.9987 on the initial and external validation datasets, respectively.
The Attention U-Net model reported an accuracy of 0.9992 and 0.9989, while the MultiResUNet model displayed a remarkable accuracy of 0.9996 and 0.9995, respectively. All models showed promising precision, recall, and F1-score metrics, along with reduced mean absolute errors compared to the ground truth manual method.
In conclusion, our study demonstrates the potential of these deep learning models for the automated detection and measurement of the dural sack cross-sectional area in lumbar spine MRI. The proposed models achieve high-performance metrics in both the initial and external validation datasets, indicating their potential utility as valuable clinical tools for the evaluation of lumbar spine pathologies. Future studies with larger sample sizes and multicenter data are warranted to validate the generalizability of the model further and to explore the potential integration of this approach into routine clinical practice.
Keywords: lumbar spine MRI; dural sack cross-sectional area; deep learning; automated detection; spinal pathologies; image segmentation; spine surgery; quantitative measurement; clinical application
1299
P333: Utility of cervical dynamic magnetic resonance imaging (MRI) in the diagnosis of cervical radiculopathy
Ignacio Cirillo 1 , Gabriel Perat 1 , Rodrigo Sanhueza 1 , Marcos Gimbernat 1 , Carlos Tapia 1 , Juan José 1 , Alejandro Urzúa 1 , Enrique Rubio Muñoz 1
1 Hospital del Trabajador, Santiago, Chile
Introduction: Cervical radiculopathy due to nerve root compression and/or irritation could lead to pain to the upper limbs, being spondylosis and disc herniation the most frequent etiologies. The most affected nerve roots are C6 and C7. When the MRI cannot be performed or if the result is not conclusive, Computerized Tomography (CT) Myelogram is suggested as an alternative, even though it has been reported to have risks such as high radiation dose. It is on this specific issue that dynamic MRI (in flexion and extension) could be a useful alternative as it can even reproduce the dynamic effects of the spinal pathology. There have been publications backing up its utility in degenerative cervical myelopathy (DCM), but there are not any reports of its usefulness in foraminal stenosis. The purpose of this study is to compare the foraminal size in static MRI with dynamic imaging in patients with clinical findings compatible with cervical radiculopathy and to determine if it is a useful tool for the diagnosis in this pathology. Material and Methods: We performed a retrospective revision of patients that consulted at our center, Hospital del Trabajador, (Santiago, Chile) from January 2010 to January 2021 presenting clinical findings compatible with cervicobrachialgia and that have been studied with both static and dynamic MRI with no more than 30 days apart from each imaging examination. This study includes 80 patients, measuring in millimeters (mm) the foramina, preforaminal spaces between C3-C4 to C6-C7 in the axial view, as well as de diameter of the spinal canal and the spinal cord in the sagital view in neutral, flexion and extension positions of the neck while performing these MRI studies. Pearson’s correlation (“r”) and p value where used, comparing neutral-extension and neutral-flexion for each of the measurements analyzed with these patients. Results: There was a difference in the foramina size and preforaminal space while comparing static and dynamic MRI in the axial view, though it had no statistical significance. There was no statistically significant difference between foramina diameter and preforaminal space. The “r” value was smaller or equal to 0,001 for all those cases. Conclusion: Even though there was a difference in foramina size in the axial view while comparing static and dynamic MRI, these do not have a significant statistical difference. We found the foramina in the higher cervical levels become smaller in diameter in flexion, while the foramina in lower cervical levels diminish their diameter in extension, but not as significantly different to consider the dynamic MRI as a diagnosis tool for patients with cervical radiculopathy. In the sagittal view, we observed a statistically significant difference when comparing the spinal canal diameter in neutral position, compared with on the C4-C5 to C6-C7 segments, confirming what has been described in previous studies, reinforcing that Dynamic MRI is a useful for the diagnosis of DCM. Further studies with a higher number of patients and healthy control group or cadaveric specimens should be performed to review more in depth this topic.
1343
P334: Obturator-inlet and iliac oblique views: fluoroscopy-guided technique for safe iliac screw placement
Ashraf El Naga 1 , David Gendelberg 1
1 University of California, San Francisco, Department of Orthopaedics, San Francisco, CA, USA
Introduction: There are many described techniques for the placement of posterior iliac screws for extension of lumbar posterior spinal instrumentation to the pelvis, including freehand technique, guidance under the “teardrop”, and guided CT navigation. However, each one has its limitations. Most notably, while it is a great confirmatory view, the teardrop view cannot be used practically to guide iliac screw placement as the fluoroscopy unit is in the way with the trajectory of the screw preparation tools. As such, we describe an alternative technique for fluoroscopic guidance of iliac screw placement utilizing the obturator inlet (OI) and iliac oblique (IO) views to visualize the entire supraacetabular corridor as well as a detailed review of how to obtain and interpret these views for safe iliac screw placement. The OI view is used to guide the medial-lateral screw trajectory and the IO view is used to guide the cranial-caudal screw trajectory. Material and Methods: A detailed review of our fluoroscopic technique is presented including how to obtain and interpret these views for safe iliac screw placement is to be presented. Patient charts of all patients undergoing OI-IO fluoroscopically guided iliac screw placement at an academic level 1 trauma center using the described technique between January 2019 and March 2022 were reviewed with screw length and bony breaches are reported. Results: 12 patients underwent posterior lumbopelvic fixation with a total of 23 screws placed via either open or percutaneous technique. The mean screw length was 96.5 mm (Range 80 - 110, standard dev 7.75). There were no recorded breaches or re-cannulation attempts. Conclusion: We show how the OI-IO technique is a much more convenient alternative to placement of iliac screws as compared to the obturator outlet oblique (“teardrop” view) which necessitates that the C-arm be in line with instruments being placed and additionally does not rely on navigation. These described views can be used to safely place long screws with either open or percutaneous techniques and with either the posterior superior.
1359
P335: Lumbar dorsal root ganglion displacements between supine and prone positions are small when evaluated with 3D MRI
Frederik Abel 1 , Jake Fiore 1 , Marianne Belanger 1 , Fedan Avrumova 2 , Darryl Sneag 1 , Darren Lebl 2 , Ek Tsoon, Tan 1
1 Radiology
2 Spine Surgery, Hospital for Special Surgery, New York, USA
Introduction: Pre-operative lumbar spine MRI is usually acquired with the patient supine, whereas lumbar spine surgery is most commonly performed prone. For MRI to be used reliably and safely for intra-operative navigation for foraminal and extraforaminal decompression, the magnitude of dorsal root ganglion (DRG) displacement between supine and prone positions needs to be understood. Materials and Methods: A prospective study of a degenerative lumbar spine cohort of 18 subjects indicated for lumbar spine surgery. Three-dimensional T2-weighted fast spin echo and T1-weighted spoiled gradient echo sequences were acquired on 3 Tesla MRI. Displacement and cross-sectional area (CSA) of the bilateral DRGs at 5 motion levels (L1-2 to L5-S1) were determined via 3D segmentation by 2 independent evaluators. Wilcoxon rank-sum tests without correction for multiple comparison were performed against hypothesized 1-mm absolute displacement and corresponding 24% CSA change. Results: DRG mean absolute displacement was < 1 mm (p > 0.99, mean = 0.707 mm, 95% confidence interval (CI) = 0.659 to 0.755 mm), with the largest directional displacement in the dorsal-to-ventral direction from supine to prone (mean = 0.141 mm, 95% CI = 0.082 to 0.200 mm). Directional displacements caudal-to-cephalad were 0.087 mm (95% CI = 0.022 to 0.151 mm), and left-right were -0.030 mm (95%CI = -0.059 to - 0.001 mm). Mean CSA change was within 24% (p > 0.99, mean = -8.30%, 95% CI = -10.5 to -6.09%). Mean absolute displacement was largest for the L1 (mean = 0.811 mm) and L2 (mean = 0.829 mm) DRGs. Conclusions: Minimal, non-statistically significant soft tissue displacement and morphological area differences were demonstrated between supine and prone positions during 3D lumbar spine MRI.
1523
P336: Obturator inlet and iliac oblique fluoroscopic views allow for placement of longer iliac screws
Obiajulu Agha 1 , David Gendelberg 1 , Ashraf El Naga 1
1 Orthopedic Surgery, University of California San Francisco, San Francisco, USA
Introduction: Pelvic instrumentation is often used to create more robust distal fixation in posterior spine constructs with the use of long well-anchored screws. Described techniques for iliac screw placement include freehand, fluoroscopy-assisted, and CT navigation. Our team has described a fluoroscopically-guided screw placement method utilizing the obturator inlet (OI) and iliac oblique (IO) pelvic ring views (“OIIO” technique), which allows for full visualization of the iliac corridor and more favorable positioning of the C-arm in relation to the surgeon during instrumentation as compared to the “teardrop” view, which is in the way during corridor cannulation and instrumentation. In this study we report on early screw length and diameter results using the OIIO technique as compared to those placed with traditional freehand or navigation techniques. Incidence of cortical breeches of the screws was also reviewed. Material and Methods: We retrospectively reviewed patients undergoing PSF with pelvic fixation between 2020 and 2022 at two university affiliated hospitals. Method of screw placement, screw diameter, and screw length were recorded. Revision pelvic instrumentation cases were excluded. Incidence of cortical breaches during screw placement and subsequent revision pelvic fixation was recorded. Continuous variables were compared between the groups using one-way ANOVA, and categorical variables were analyzed using Fisher’s Exact tests. Significance was set at p < 0.05. Results: All patients whose screws were placed using OIIO technique during the study period were included (n = 12) for a total of 23 pelvic screws. Of the patients who did not undergo OIIO for pelvic fixation during the study period, a total of 99 patients were randomly selected. From these patients, 46 and 53 patients were identified with freehand and navigated techniques, respectively, for a total of 173 screws in the freehand group and 113 in the navigated group. Compared to freehand screws, OIIO screws significantly longer (96.52 ± 7.75 mm vs. 78.79 ± 5.17 mm; p < 0.0001) but of smaller diameter (8.51 ± 0.42 mm vs. 8.20 ± 0.42 mm; p = 0.0009). Compared to navigated screws, OIIO screws were longer (96.52 ± 7.75 mm vs. 85.00 ± 7.01 mm; p < 0.0001) but narrower (8.55 ± 0.41 mm vs. 8.20 ± 0.42 mm; p = 0.0002). There were no instances of cortical breach with OIIO screws compared to only 1 instance of lateral cortical breach which occurred during freehand technique (p > 0.9999). There were no differences in rates of subsequent iliac screw revision between the groups. Conclusion: Our early results using the OIIO fluoroscopic technique demonstrate that it can be used to place screws of longer lengths and without increased incidence in cortical breach when compared to screws placed using freehand and navigation techniques. In summary, the OIIO technique represents a viable and safe alternative for placing robust pelvic fixation in a manner that may be more ergonomic during instrumentation or in settings in which navigation may not be available.
1562
P337: Hounsfield unit in the upper cervical spine: a comparison between 201 patients with sandwich fusion and normal controls
Ye Ouyang 1 , Aodong He 1 , Bo Zhao 1 , Yirong Xia 1 , Yinglun Tian 1 , Feifei Zhou 1 , Shenglin Wang 1 , Nanfang Xu 1
1 Department of Orthopaedics, Peking University Third Hospital, Beijing, China
Introduction: Research on the lumbar spine and sub-axial cervical spine has shown that there is a high correlation between Hounsfield Units (HU) obtained from CT scans and bone mineral density (BMD) measured by dual-energy X-ray absorptiometry (DXA). This study aims to compare HU of the upper cervical spine in patients with concomitant C1 occipitalization and C2/3 non-segmentation, i.e. sandwich fusion, and those with normal anatomy of the craniovvertebral junction, and to investigate the feasibility of using HU to evaluate bone quality in the upper cervical region. Material and Methods: We retrospectively analysed the cervical spine CT scans of 201 patients with sandwich fusion. Six regions of interest (ROI) were selected as they were in the trajectory of the three most commonly used screws (C1 lateral mass screw, C2 pedicle screw, and C2 translaminar screw) for surgical instrumentation: A and B (left and right C2 lateral mass), C (C2 spinous process), D and E (left and right C2 laminae, and F (C2 vertebral body). The preoperative average HU in these regions on PACS were measured. 61 patients were above 50 years in age and were 1:1 matched by a control group of subjects with normal anatomy of the atlantoaxial region according to age and gender. Lumbar spine (L1-L4) BMD according to DXA was available for the control group and HU was measured in the same manner. We calculated the HU threshold values for screening bone loss (-2.5 < T < -1) and osteoporosis (T ≤ -2.5). Results: In patients with sandwich fusion, the HU in each region were as follows: 281.2 ± 113.4, 294.3 ± 133.5, 232.9 ± 97.0, 239.5 ± 107.2, 229.2 ± 98.8, and 298.8 ± 86.7 (A to F). Except for region F, all regions had lower HU values in males than in females (p < 0.05). There was no significant correlation between HU and age. Significant correlations were observed among all regions, suggesting internal consistency of our measurements. In the control group, HU for regions A, B, C and D were significantly correlated with age, and there were significant correlations among all regions. In the control group, the correlation coefficients between HU in various regions and DXA ranged from 0.444 to 0.697 (p < 0.001). The area under the ROC curve (AUC) for screening bone loss (AUC = 0.700, 95% CI (0.567, 0.833)) and osteoporosis (AUC = 0.952, 95% CI (0.894, 1.000)) was highest in ROI F (axial plane C2 vertebral body) in both cases. The HU threshold values were 345.3 (sensitivity 57.9%, specificity 91.3%) and 235.0 (sensitivity 85.5%, specificity 100%), respectively. Particularly, the average HU of ROI F was 273.1 in the sandwich fusion group, compared to 317.5 in the control group, suggesting that bone loss and osteoporosis was more prevalent in patients with sandwich fusion. Conclusion: HU can be reliably measured in different regions of bone in the craniovertebral junction. The HU threshold values of the axial plane C2 vertebral body was 345.3 for predicting bone loss and 235.0 for predicting osteoporosis. Sandwich fusion patients had lower HU values compared to normal controls.
1625
P338: Morphometric analysis of the C1-2 zygapophysial joint in atlantoaxial dislocation patients with sandwich fusion of the craniovertebral junction
Nanfang Xu 1 , Jinguo Chen 1 , Ye Ouyang 1 , Ming Yan 1 , Yinglun Tian 1 , Shenglin Wang 1
1 Department of Orthopaedics, Peking University Third Hospital, Beijing
Introduction: We previously described a subtype of Klippel-Feil syndrome with the combination of congenital C1 occipitalization and C2-3 non-segmentation as “sandwich fusion”. Significant clamp strain between C1 and C2 in these patients frequently results in early development of atlantoaxial dislocation (AAD), and hence the name "sandwich AAD". Surgical correction is the only effective treatment for sandwich AAD and a thorough understanding of the morphometry of the C1-2 zygapophysial joints is of essence to ensure a safe surgery. We herein aim to evaluate and analyze the morphometry of the C1-2 zygapophysial joint in patients with sandwich AAD. Material and Methods: Thin-slice computed tomography (CT) studies of the craniovertebral junction of 155 sandwich AAD patients and 51 AAD patients with os odontoideum (OO) were analyzed. The listhesis grade of the C1-2 zygapophysial joint was defined according to the ratio (in percentage) of the listhetic distance of the inferior facet of C1 over the superior facet of C2 to the sagittal diameter of the superior facet of C2 on the mid-parasagittal plane: less than 25% was defined as mild, 25-75% as moderate, and greater than 75% as severe. Additionally, the sagittal and coronal inclination angles of the C1 inferior facet (SIA and CIA, respectively) were measured and compared between the two groups. Results: Patients in the sandwich group had more significant listhesis of the C1-2 zygapophysial joint than the OO group (17.4% vs. 72.6%, 51.0% vs. 27.4% and 31.6% vs. 0.0% were of mild, moderate, and severe listhetic grade, respectively, p < 0.01). The average of SIA (30.1°) and CIA (36.6°) of the sandwich group were all significantly greater than those in the OO group (p < 0.01). SIA was positively correlated with both the CIA (r = 0.54, p < 0.01) and the listhetic distance of the C1-2 zygapophysial joint (r = 0.52, p < 0.01) in the sandwich group. In addition, asymmetric listhesis (defined as discordant listhetic grades between the C1-2 zygapophysial joints in the same patient) was found in 0.0%, 63.3%, and 85.7% of sandwich AAD patients with mild, moderate and severe listhetic grade of the C1-2 zygapophysial joint, respectively. Conclusion: Listhesis of the C1-2 zygapophysial joint was a more common finding in sandwich AAD patients than in the control group and was of moderate to severe listhetic grades in more than 80% of the cases, who also tended to have higher SIA and CIA. AAD in patients with sandwich fusion was frequently a three-dimensional deformity as suggested by the positive correlation between SIA, CIA, and the listhetic distance of the C1-2 zygapophysial joint, and was characterized by the high prevalence of asymmetric listhesis of the C1-2 zygapophysial joint among these patient.
1944
P339: Repeat MRI of the spine within 90 days: assessment of a single academic center
Joseph Rund 1 , Mary Kate Skalitzky 1 , Connor Littlefield 1 , Alex Coffman 1 , Catherine Olinger 1
1 Departments of Orthopedics and Rehabilitation, University of Iowa, Iowa City, USA
Introduction: Unnecessary magnetic resonance imaging (MRI) can lead to increased cost, inappropriate treatment, and patient anxiety. The incidence of inappropriate MRI studies can be upwards of 59%. This study seeks to identify and assess repeat MRIs within 90 days. We aim to evaluate the characteristics of repeat imaging studies and examine for change in surgical patient care. Material and Methods: A retrospective review of spine MRIs at a single institution between January 1, 2019, and January 1, 2022 was completed. Inclusion criteria were any pathology, age > 18, and repeat MRI of the same location within 90 days. Exclusion criteria were repeat MRI not within 90 days and repeat MRI with contrast when original was without. Outcome measurements included demographics, image location and indication, ordering physician specialty, and surgical intervention within 90 days. Chi-squared statistical analysis was utilized for categorical variables and student’s t-test was utilized for continuous variables. Statistical significance was set at p < 0.05. Results: The original cohort included 10,754 spine MRIs, 3,997 patients. 8,848 MRIs and 2,405 patients were excluded and served as comparison. 1,906 repeated MRIs and 592 patients were included. The repeat MRI cohort had a statistically significant decrease in percentage of females (46.06% vs. 53.60%, p < 0.001). Indications for repeat imaging included infection (34.73%), oncology/inflammatory (27.18%), trauma/fracture (5.56%), pain (16.79%), neurologic change (13.54%), and cerebral spinal fluid (CSF) leak (2.20%). Spine MRIs which were completed both with and without contrast were more likely to be repeated (p < 0.00001). Rate of repeat MRIs varied by specialty (orthopedic surgery-9.02%; neurosurgery-28.44%; emergency medicine-11.65%, and medicine-38.72%). Of 953 repeated MRIs, 98 (10.28%) underwent operative intervention within 90 days. Operative intervention following repeat imaging varied by specialty (orthopedic surgery-39.53%; neurosurgery-11.81%; emergency medicine-13.51%; and medicine-4.34%) and indication (infection-2.42%; oncology/inflammatory-3.86%; trauma/fracture-20.75%; pain-16.88%; neurologic change-32.56%; and CSF leak-0.00%). Conclusion: At a single institution, females were less likely to have repeat spine imaging and MRI both with and without contrast was more frequently repeated. Infection and oncologic/inflammatory processes more frequently had repeat imaging, however, were less likely to undergo operative intervention compared to trauma/fracture, pain, and change in neurologic exam indications. Although medicine teams more frequently ordered repeat imaging, patients were less likely to undergo operative intervention when compared to orthopedic surgery, neurosurgery, and emergency medicine.
2023
P340: Quantification of MRI artifacts in carbon fiber reinforced polyetheretherketone thoracolumbar pedicle screw constructs prior to spinal stereotactic radiosurgery
Romulo Augusto Andrade de Almeida 1 , Amol Ghia 2 , Behrang Amini 3 , Chenyang Wang 2 , Christopher Alvarez-Breckenridge 1 , Jing Li 2 , Laurence Rhines 1 , Martin Tom 2 , Rob North 1 , Thomas Beckham 2 , Claudio Tatsui 1
1 Neurosurgery
2 Radiation Oncology
3 Diagnostic Imaging, MD Anderson Cancer Center, Houston, USA
Introduction: Carbon fiber reinforced polyetheretherketone (CFRP) is a non-metallic material gaining interest in the manufacture of spinal instrumentation. The radiolucency and low magnetic susceptibility of CFRP has potential to create less interference with diagnostic imaging compared to titanium (Ti) implants. However, an objective comparison of the image artifact produced by titanium and CFRP implants has not been described. Spinal oncology, particularly after resection of spinal tumors and at the time of spinal stereotactic radiosurgery (SSRS) planning, relies heavily on imaging interpretation for evaluating resection, adjuvant treatment planning, and surveillance. We present a study comparing measurements of post-operative MRI artifacts between titanium and CFRP pedicle screw constructs in the setting of separation surgery for metastatic disease. Material and Methods: The diameter of the signal drop around the screws (Pedicle Screw Artifact, PSA) and the diameter of the spinal canal free from artifacts (Canal Visualization, CV) were measured in consecutive patients who had spinal instrumentation followed by SSRS in the June 2019 - May 2022 timeframe. Results: The spinal cord presented a shift at the screw level in sagittal images which was also measured (Sagittal Distortion, SagD). Fifty patients, corresponding to 356 screws and 183 vertebral levels, were evaluated overall. CFRP produced less artifacts in all the three parameters when compared to titanium: mean PSA (CFRP = 5.8 mm, Ti = 13.2 mm), CV (CFRP = 19.2 mm, Ti = 15.5 mm), and SagD (CFRP = 0.5mm, Ti = 1.9 mm), all p < 0.001. In practice, these findings translate into better-quality MRI. Conclusion: The initial perceived advantages are easier evaluation of post-operative imaging, facilitating radiation treatment planning, recurrence detection, and avoidance in repeating a suboptimal computed tomography myelogram. Further clinical studies analyzing long-term outcomes of patients treated with CFRP implants are necessary.
2076
P341: Diagnostic value of bone scintigraphy and single photon emission computerized tomography in the assessment of spinal complaints
Mara-Ioana Dimitriu 1 , Nikki Rommers 2 , Robin Brugger 3 , Victoria Schimmelpenning 3 , Martin Jaeger 3 , Johann Kunst 3 , Helena Milavec 4
1 Department of Orthopaedics, Schulthess Klinik, Zurich, Switzerland
2 Department of Clinical Research, University of Basel, University Hospital Basel, Basel, Switzerland
3 Department of Orthopaedic Surgery and Traumatology, Spine Unit, Aarau Canton Hospital, Aarau, Switzerland
4 Department of Orthopaedic Surgery and Traumatology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
Introduction: Single photon emission computed tomography (SPECT) is an advanced and increasingly used hybrid nuclear imaging technique for diagnosing degenerative bone and joint diseases. It involves a whole-body bone scan (BS) followed by a focused three-dimensional computer scan of the specific area of interest. The comprehensive BS may detect uptake beyond the targeted region. Data on the prevalence and diagnostic performance of these tools for patients with spinal complaints are currently limited. The aim of this study is to assess the prevalence of high uptake in BS and SPECT in relation to specific spinal complaints. Additionally, we aim to determine the sensitivity of BS in comparison to SPECT for detecting degenerative changes. Materials and Methods: This is a retrospective exploratory analysis using data from a single tertiary institution. All data sets are cross-sectional in nature and are limited to patients who signed the general consent. We enrolled patients who sought consultations for spinal concerns and subsequently underwent SPECT scans. We categorized these concerns into neck, thoracic, and lower back pain (LBP), which also encompassed discomfort in the sacroiliac joint (SIJ) region. The diagnostic measures of BS and SPECT were the primary outcome. We present the proportion of patients with a positive finding using the 95% Wilson confidence interval. To assess diagnostic measures, we categorized clinical diagnoses as either positive or negative for facet joint osteoarthritis or SIJ osteoarthritis or osteochondrosis. Results: Our analysis involved 111 patients, comprising 45 males and 66 females. Among them, 48 underwent a SPECT of the cervical spine, 34 of the thoracic spine, 92 received a SPECT of the lumbar spine, including the SIJ, and one underwent SIJ SPECT only. Symptoms were reported in 38 patients for the cervical spine, 18 for the thoracic spine, and 96 for the lower back region. Among the patients with neck pain, 32 underwent both BS and SPECT, and 15 (46.88%) had a positive BS, while 29 (90.63%) had a positive SPECT. Of the 10 patients complaining of thoracic pain, 3 (30%) had a positive BS, while 6 (60%) showed a positive SPECT. Among the 90 patients experiencing LBP including SIJ region, 52 (57.78%) exhibited positive BS findings in the lumbar spine, while 70 (77.78%) had positive results in the lumbar SPECT, 15 (16%) showed a positive BS outcome in the SIJ, while 31 (37.36%) had positive SPECT findings in the SIJ. The sensitivity of SPECT is lowest in the thoracic spine (0.600, 95% CI [0.313, 0.832]), higher in the lumbar spine region (0.889, 95% CI [0.807, 0.939]), and reaches its peak in the cervical spine (0.906, 95% CI [0.758, 0.968]). Conclusion: In detecting degenerative changes, BS is less sensitive than SPECT in each of the regions of the spine. The sensitivity of SPECT varies in relation to clinical symptoms across different regions of the spine being lowest in the thoracic and highest in the cervical spine. Among patients with LBP, twice as many exhibited uptakes in the lumbar spine compared to the SIJ.
2283
P342: Predicting the need for surgical or conservative management in symptomatic lumbar disc herniation patients, based on MRI findings of spinal canal
Venkatesh Dasari 1 , Sohael Khan 2 , Navin Singh 3 , Shantanu Gupta 4 , Rameez Bukhari 5
1 Orthopaedics, Raipur Institute of Medical Sciences, Raipur, India
2 Orthopaedics, JNMC, DMIHER, India
3 Raipur Institute of Medical Sciences, India
4 Healthcare Hospital, Bilaspur, India
5 JNMC, DMIHER, Wardha, India
Introduction: Prolapsed Inter-vertebral disc PIVD is common spine pathology, which is well visualized using magnetic resonance imaging (MRI). Two major treatment modalities for this condition are: Surgical – decompression & discectomy, and Conservative – Medications and Blocks.[1-3]. There is scarce data on the impact of morphometric parameters of PIVD and spinal canal on the probability of success of selected management protocol. Hence there isn’t a widely accepted objective radiological criterion for selecting a patient’s candidacy for conservative or surgical management. Patients having minimal backache and/or radicular pain, along with minimal or no disc bulge on MRI can be treated with conservative modalities, while patients having severe pain, severe neurological deficit, and/or cauda equina syndrome are indication for surgery. But in the middle of this spectrum lie the patients with a variable amount of pain, having a variable size of disc herniation, and they constitute a ‘grey area’ of treatment modality where a selection of conservative or surgical treatment is purely based on the surgeon’s practice and acumen. The rationale of this study is to try to define this ‘grey area’ of decision-making regarding the treatment of symptomatic PIVD and to find out the role of disc-herniation-related-canal-compromise in the lumbar spine in predicting the need for surgical or conservative treatment in patients. Methods: In this observational study, 64 patients were enrolled in each group: surgical & conservative groups. These were 64 PIVD patients who underwent surgery and got pain relief, and 64 PIVD patients underwent conservative treatment and got relief. The pre-treatment MRI findings of these patients were studied and various measurements were taken. These measurements were then further studied to establish a predicting value for surgical or conservative management in symptomatic lumbar disc herniation patients. Measurements taken on MRI axial section were:
• Area of herniated disc.
• Area of spinal canal.
• Anteroposterior disc length.
• Anteroposterior canal length.
• Mid-width of the herniated disc
• Mid-width spinal canal
Canal compromise ratio was calculated using herniated disc area by canal area.
Results: The mean age of the surgical group was 45.26 ± 11.20 years and of the conservative group was 49.43 ± 13.74 years. The mean disc length (5.43 ± 1.11 mm), mean disc area (211.78±6.60mm2), and canal compromise ratio (0.453 ± 0.015) of the surgical group were found significantly higher than the conservative group, while the mean canal cross sectional area (467.50 ± 4.61 mm2) was found to be significantly smaller in the surgical group. Conclusions: Our study suggests that of the patients presenting with symptomatic single-level intervertebral disc herniations, with initial imaging values:
1) Larger disc herniation length (≥ 5.43 ± 1.11 mm)
2) Lager disc herniation area (≥ 211.78 ± 6.60 mm)
3) Smaller canal cross-section area (≤ 467.50 ± 4.61 mm2)
4) Larger canal compromise ratio (≥ 0 .453 ± 0.015)
are more likely to fail with conservative treatment and should be advised surgical interventions.
References
1 Atlas SJ, Keller RB, Chang Y, Deyo RA, Singer DE. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine 2001; 26: 1179-87.
2. Goel A. Prolapsed, herniated, or extruded intervertebral disc-treatment by only stabilization. Journal of craniovertebral junction & spine. 2018 Jul; 9(3): 133.
3. Carlisle E, Luna M, Tsou PM, Wang JC. Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. The spine journal 2005 Nov 1; 5(6): 608-14.
2305
P343: Prevertebral vascular studies using computed tomography angiography prior to anterior lumbar spine procedures
Zhihong Chew 1,2 , David Zurita 1 , Rachel Cengia 3 , Michael Janssen 1
1 Center for Spine & Orthopedics, Scientific Education and Research Foundation, Denver, USA
2 Department of Orthopaedic Surgery, Changi General Hospital, Singapore
3 Center for Spine & Orthopedics, Scientific Education and Research Foundation, USA
Introduction: The use of anterior access to the lumbar spine has increased in popularity in recent years. This approach provides direct exposure of the disc space and allows for direct decompression through an adequate discectomy, and an effective distraction of the disc space, which consequently allows indirect decompression by increasing the size of the neural foramina. Two common procedures that utilize this access are anterior lumbar interbody fusion and lumbar disc arthroplasty. A key consideration of the anterior approach to the lumbar spine is the mobilisation of the great vessels as vascular injuries are one of the most significant complications. This paper aims to study the prevertebral vascular anatomy using computed tomography (CT) angiography prior to anterior access lumbar spine surgery, and to document rates of significant intra-operative vascular complications. Material and Methods: This is an institution review board approved prospective cohort study of patients who underwent elective surgery for lumbar disc arthroplasty and anterior lumbar interbody fusion at a single center for the study. period Patients who underwent anterior lumbar access surgery for trauma, infective or neoplastic etiologies were excluded. All included patients underwent a pre-operative CT angiography study. A single approach surgeon performed all accesses and closures, while a single spine surgeon (senior author of this study) performed all decompression and instrumentation procedures. Data was collected pre-, and intra-operatively. Results: Data collection and analysis for an estimated 120-150 patients is in progress at the time of abstract writing. Pre-operative demographic parameters to be noted are patient gender, age, habitus and body mass index and previous abdominal surgery. The CT angiography studies will be used to map out the level of aortic bifurcation, the level of iliac vein confluence, as well as other vascular anomalies such as aneurysms and atherosclerotic disease. Also to be documented is the accessibility of disc spaces at L3/4, L4/5 and L5S1 in relation to the great vessels. Significant intraoperative events, in particular vascular injuries requiring repair, will be detailed and discussed. Conclusion: There is significant variability in the prevertebral vascular anatomy. Thorough knowledge is essential to allow precise mobilization of the great vessels during anterior access lumbar surgery. In this regard, CT angiography studies provide invaluable information to the access and spine surgeons. With adequate pre-operative planning, feared complications can potentially be reduced.
2390
P344: Characteristics and relationships of computed tomography hounsfield units in the cervical, thoracic and lumbar spine
Liang Wang 1
1 Department of Orthopaedic Surgery, Qilu Hospital of Shandong University, Jinan, China
Background: The utilization of Hounsfield (HU) values from computed topography (CT) scan in screening and diagnosis for osteoporosis in the lumbar spine has been widely reported. It has been widely reported that there were significant positive correlations of HU value with bone mineral density and T-score from DEXA. Nowadays, most studies on CT-HU measurement focused on lumbar spine and research on cervical and thoracic spine is limited. Whether there were differences of CT-HU between the cervical, thoracic and lumbar vertebra? Whether the cervical and thoracic CT-HU could predict and screening osteoporosis? With such questions, we investigated and analyzed the CT-HU in 4874 cervical, thoracic and lumbar vertebras from 200 consecutive people. Methods: Consecutive subjects undergoing cervical, thoracic, lumbar spine CT and DEXA scanning within 3 months due to medical conditions or physical examination at our hospital between January 2019 and December 2022 were screened for eligibility in the current study. The exclusion criteria included spinal fracture, spine tumor, infectious spondylitis and previous spinal instrumentation surgery, previous spinal fusion, previous vertebroplasty or kyphoplasty. HU measurement was performed via a previously described method using Philips EasyVision Picture Archiving and Communication System (PACS). HU were recorded in the axial, sagittal and coronal plane from C2-L5. Results: A total of 167 subjects with 3743 vertebras were enrolled in the study, including 85 males and 82 females, with the mean age of 67.7 years old. Base on the T-score of DEXA, 60 patients were diagnoses with osteoporosis, 58 with osteopenia and 49 with normal BMD. As for the same vertebra, there was no significant difference of HU between axial, sagittal and coronal plane. It was observed that the mean HU values displayed a significant decrease tendency from cervical to thoracic and lumbar spine, but with significant correlation between them. As for the correlation between CT-HU and T-score, C4, T7 and L3 was the most significant vertebra for cervical, thoracic and lumbar spine. As for the subjects with osteoporosis, the correlation between the HU and T-score was lower than osteopenia and normal BMD. Conclusion: There were distinct difference of CT-HU between the cervical, thoracic and lumbar spine, which showed significant decrease tendency from cranial to caudal spine. CT-HU has been proved to have obvious correlation with T-score and might be more useful to assess the BMD of osteoporosis patients.
Infections
83
P345: A new minimally invasive percutaneous procedure performing simultaneous pedicle screw fixation and endoscopic debridement under real-time intraoperative 3-dimensional imaging navigation for pyogenic spondylodiscitis
Rina Therese Madelar 1,2 , Manabu Ito 2 , Hidekazu Yoshizaki 2 , Yuichi Hasegawa 2 , Katsuro Ura 2
1 Department of Orthopedics, The Medical City, Pasig City, Philippines
2 Orthopedic Surgery, Hokkaido Medical Center, Sapporo, Japan
Introduction: Traditionally, procedures of choice for the surgical treatment of pyogenic spondylodiscitis include anterior decompression and fusion with titanium cages or strut grafts and one- or two-stage posterior stabilization. However, minimally invasive techniques have been emerging due to the high risks that open surgery entails. Together with the development of new technologies and the added value of having lesser blood loss, faster recovery time and shorter hospital length of stay, these have been employed in the treatment of spine infections. There are no reports regarding simultaneous percutaneous fixation and endoscopic debridement for pyogenic spondylodiscitis under navigation. We propose a new surgical technique using single-stage percutaneous pedicle screw fixation and endoscopic debridement for considerable spinal destruction with instability under real-time intraoperative 3-dimensional (3D) imaging navigation (RT3D-nav). Material and Methods: The patient is prone on a spine table under general anesthesia. A tracker is placed on the posterior superior iliac spine. Intraoperative 3D CT scanning of the lumbar spine and pelvis is done using Airo® TruCT. Once the scanned levels are deemed adequate, images are imported onto the navigation system. Percutaneous pedicle screws are placed and endoscopic lumbar debridement through the caudal aspect of Kambin’s triangle on the infected intervertebral space is performed all under real-time intraoperative 3-dimensional imaging navigation. Proper trajectory and depth are visualized through the system during pedicle probing, tapping and screw insertion, maintaining accurate direction. The location of the scope is seen ensuring adequate and safe debridement and curettage of disc and endplates. Rods are contoured to regain spinal alignment. Results: This procedure allows for improvement in pain, resolution of infection and maintenance of spinal alignment. Conclusion: This technique suggests the use of one-stage minimally invasive lumbar fusion using percutaneous pedicle screws and endoscopic debridement under real-time intraoperative 3D imaging navigation for pyogenic spondylodiscitis. Curettage and copious lavage on the infected site are done which help improve antibiotic penetration and effectivity. Correction of local kyphosis is performed through properly contoured rods and was seen to result in maintenance of alignment on follow up. This method is an effective and promising technique providing safer surgery due to less invasiveness, lower blood loss and maintenance of correction, delivering good outcomes for patients with pyogenic spondylodiscitis.
85
P346: In vitro testing of silver-containing bone cement in infection management
Renate Krassnig 1 , Gebhard Feierl 2 , Walter Gössler 3 , Gloria Hohenberger 4
1 Rehabilitation Clinic Tobelbad, AUVA, Tobelbad, Austria
2 Medizinische Universität Graz, Austria
3 Karl-Franzens-Universität Graz, Austria
4 Landeskrankenhaus Feldbach, Feldbach, Austria
Introduction: Deep infection is a serious complication in orthopaedic trauma surgery. In correlation to the patient local or systemic compromising factors conservative and surgical proceedings has to be evaluated. Systemic antibiotic therapy is the gold standard in infection management. Implanted silver-coated or silver-containing medical devices have been proven to their antimicrobial effectiveness since the 1990s by several investigators. The outcomes showed that long time implantation could cause damaging of the surrounding tissues, especially of adjacent nerves. The aim of our study was to evaluate the release of silver (I) ions from bone cement mixed with either nanosilver particles (AgNPs), different concentrations of silver sulfate (Ag2SO4) or from pure metallic silver strips. Material and Methods: To evaluate the release of silver (I) ions choose two methods: the first, called “static model”, was chosen to evaluate the maximal accumulative concentration of silver (I) ions, with the second, called “dynamic model”, we simulated a continuous reduction of the ions over a period of 9 weeks. In an additional test design, the different materials were evaluated for their antimicrobial activity using an agar gel diffusion assay. Results: The outcome showed that neither the addition of 1% (w/w) nanosilver nor 0.1% silver sulfate (w/w) to polymethylmethacrylat bone cement has the ability to release silver (I) ions in a bactericidal/antifungal concentration. However, the results also showed that the addition of 0.5% (w/w) and 1% (w/w) silver sulfate (Ag2SO4) to bone cement is an effective amount of silver in infection management. Conclusion: Silver containing bone cement might be an alternative option in infection management.
87
P347: The comparisons of surgery and conservative treatment in prognosis of infective spondylodiscitis - Chang Gung Research analysis
Po Hsiang Kao 1 , Yu-Cheng Yeh 1 , Tsung-Ting Tsai 1
1 Department of Orthopedic Surgery, Chang Gung Memorial Hospital, Linkou, Taoyuan, Taiwan
Introduction: The overall annual incidence of infective spondylodiscitis was approximately 0.4 to 7.4 cases per 100,000 and the incidence has increased attributing to an increase in susceptible patients such as intravenous drug users, individuals undergoing hemodialysis, and immunocompromised hosts. A total of 6 weeks of parenteral or highly bioavailable oral antimicrobial therapy is recommended for patients with bacterial infective spondylodiscitis. Although it is the gold standard to use antibiotics, antimycobacterial or antifungal agents to treat infective spondylodiscitis, it is still unclear whether these treatments should be combined with surgery. Therefore, this study aims to examine whether antibiotics with surgical interventions are better than antibiotics alone for the treatment of infective spondylodiscitis. Materials and Methods: This retrospective study is based in part on data from the Chang Gung Research Database, which is a multi-institutional database in Taiwan provided by Chang Gung Memorial Hospital. A total of 3,882 patients were reviewed and divided into two groups, a surgical group with surgical interventions and antibiotics and a medical group with antibiotics alone. In addition, we also further divided the surgical group into those with and without spinal fusion. The primary outcomes were all-cause mortality rate and infection recurrence rate. Multivariate COX regression analysis was used to compare the prognosis of different groups. Using a propensity score approach, inverse probability of treatment weighting was applied to balance the specific clinical characteristics at the baseline between different groups to assess the outcomes. Results: All-cause mortality rate was significantly lower in patients with surgery in both one-year and three-year outcome (p < 0.001). Moreover, in the surgical group, patients who received spinal fusion had better all-cause mortality rate and infection relapse rate in one-year outcome (p = 0.021 and 0.007, respectively) and three-year outcome (p = 0.015 and 0.020, respectively). Conclusion: In conclusion, these data suggest that a combination of surgery and antibiotics is an effective treatment to reduce all-cause mortality for patients with infective spondylodiscitis, and spinal fusion can further benefit patients in terms of both mortality and infection recurrence.
98
P348: Clinicoradiological outcome of surgical treatment of cervicothoracic junction tuberculosis: a 10-year retrospective study
Aayush Aryal 1 , Tej Dawadi 1 , Gururaj Sangondimath 1 , Kalyan Kumar Varma Kalidindi 2 , Kuldeep Bansal 1 , Nirdesh Hiremaglur Jagadeesh 1 , Umash Karki 1 , Jitendra Thakur 1 , Harvinder Singh Chhabra 3
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
2 Department of Orthopedics and Spine Surgery, AIG hospitals, Hyderabad, India
3 Spine Services, Sri Balaji Action Medical Institute, New Delhi, India
Introduction: Cervicothoracic junctional pathologies are rare, and tuberculosis (TB) is also quite rare at this area, accounting for about 5% of all spinal TB. Most cases of cervicothoracic TB are successfully treated conservatively with antitubercular drugs and external immobilization with a brace. Therefore, there is a paucity of literature on the surgical management of cervicothoracic junctional tuberculosis (CTJTB). In this study, we aimed to analyze the clinical as well as radiological outcomes of surgically treated CTJTB cases. Material and Methods: We conducted a retrospective study of all CTJTB cases that were surgically treated at our institute from January 2010 to December 2019. The demographic and clinical data of 22 patients fulfilling our inclusion and exclusion criteria, with a complete follow-up of at least two years, were obtained from the patient records and radiological data were obtained from Picture Archiving and Communication System (PACS) and analyzed with SPSS v25.0. Results: The mean pre-op ODI was 79.91 ± 2.04, while the mean ODI at the final follow-up was 45.82 ± 2.05, and this change was statistically significant (p = 0.04). The difference in Cobb angle between pre-op, immediate post-op, and final follow-up was also statistically significant (p < 0.001). The mean VAS score improved from 8.18 ± 0.15 to 2.73 ± 0.24 at the final follow-up. However, this improvement was not statistically significant (p = 0.64). Conclusion: CTJTB with progressive neurological involvement or with kyphosis, when treated surgically, gives a better clinicoradiological outcome in terms of statistically significant improvement in ODI and the degree of kyphosis.
124
P349: Spondylodiscitis and endocarditis
Artem Ilgeldiev 1 , Anne-Elisabeth Carolus 1 , Murat Yavuz 1 , Yahya Habib 1 , Victoria Yushenko 1 , Veit Braun 1
1 Neurosurgery, Diakonie Hospital, Jung-Stilling, Siegen, Germany
Introduction: Spondylodiscitis and infective endocarditis rarely occur together, resulting in complex clinical presentations. This retrospective study investigates the relationship between these conditions by analyzing data from a monocentric patient population. Materials and Methods: Electronic hospital charts from the Department of Neurosurgery, Klinikum Diakonie, Jung-Stilling, Siegen, Germany, covering a ten-year period (2001-2020), were retrospectively analyzed. The study included 97 patients diagnosed with spondylodiscitis, among whom 8 were also diagnosed with endocarditis. The charts were anonymized and password-protected. Results: Patients with endocarditis underwent thoracic surgeries more frequently compared to those without endocarditis (43% vs. 15%, respectively). Cervical spondylodiscitis were not associated with endocarditis. Thoracic spondylodiscitis was present in 14 patients without endocarditis (16%) and 3 patients with endocarditis (43%). Patients with endocarditis exhibited a higher prevalence of neurologic abnormalities (6/8) and leukocytosis (43%) compared to those without endocarditis (48/88 with leukocytosis, 28%). Elevated C-reactive protein (CRP) levels were observed in patients with endocarditis (median CRP = 19.15) compared to those with isolated spondylodiscitis (median CRP = 8.7), and this difference persisted even after surgical treatment. Preoperative creatinine levels were also higher in the endocarditis group but decreased after surgical treatment. Anemia was more prevalent in cases of mono-level spondylodiscitis combined with endocarditis (8.95 g/dL). Positive blood cultures were found in 4 out of 8 patients with endocarditis (57%) and in 39 out of 88 patients without endocarditis (44%). Thoracic spondylodiscitis was more frequently observed in patients with endocarditis (3/8) compared to those without endocarditis (14/89). Hematogenous infection was the predominant route of infection in endocarditis cases. Spondylodiscitis developing through contiguous spread did not exhibit concurrent endocarditis, even in multimorbid cases with a history of cardiac disease. Endocarditis was more frequent in cases with involvement of multiple spinal segments (10%) compared to single segment cases (7.27%). Endocarditis occurred in 75% of cases with a preexisting heart condition, compared to 23.53% in patients without a history of cardiac disease, and this difference was statistically significant (p = 0.00545). Hematogenous infection was the sole route of spontaneous infection. Psoas abscesses were more frequently detected in cases of spondylodiscitis through contiguous spread (46.15% vs. 26.51%). However, there was no clear tendency regarding epidural abscess development based on the infection pathway, although it was more frequently observed in spondylodiscitis patients with endocarditis. Conclusion: Non-normalization of CRP dynamics and initial renal insufficiency may indicate concurrent endocarditis. Patients with spondylodiscitis developing through contiguous spread did not exhibit associated endocarditis, even in multimorbid cases with a history of cardiac disease. Surgical intervention limited to the cervical region was not associated with an increased risk of endocarditis. Endocarditis occurred more frequently in cases with a preexisting heart condition.
Keywords: spondylodiscitis; endocarditis; infection; retrospective analysis; clinical presentation
We have ethics committee approval (2021-702-f-S).
192
P350: Practice preference and evidence analysis on topical use of tobramycin powder in lumbar spine surgery. A multi-national AO Spine Survey with systematic review of literature
Sathish Muthu 1,2 , Veranis Sotoris 3 , Matthew Gary 4 , Samuel Cho 5 , So Kato 6 , Stephen Lewis 7 , Hyeun Sung Kim 8 , Jeffrey C. Wang 9 , Amit Jain 10 , Timothy S. Yoon 11 , AO Spine Knowledge Forum Degenerative 12
1 Department of Spine Surgery, Orthopaedic Research Group, Coimbatore, India
2 Department of Orthopaedics, Government Medical College, Karur, India
3 Department of Neurosurgery, General Air Force General Staff Hospital, Athens, Greece
4 Department of Neurosurgery and Orthopaedic Surgery, Emory University, Atlanta, USA
5 Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, USA
6 Department of Orthopaedic Surgery, University of Tokyo, Tokyo, Japan
7 UHN-Orthopedics, University of Toronto, Toronto, Canada
8 Spine Center and Department of Orthopaedic Surgery, Seoul National University College of Medicine and Seoul National University Bundang Hospital, Seongnam, South Korea
9 Department of Orthopaedic Surgery and Neurological Surgery, Keck School of Medicine, California, USA
10 Department of Orthopaedic Surgery, Johns Hopkins University, Baltimore, USA
11 Department of Orthopaedics, Emory University, Atlanta, USA
12 Knowledge Forum Degenerative, AO Spine International, Davos, Switzerland
Introduction: There is an increasing interest in the topical use of antibiotics to prevent infection following spine surgery. To extend the antibiotic coverage to the gram-negative spectrum, the usage of tobramycin powder is being considered. We surveyed to analyze the current practice preference on the use of topical tobramycin in lumbar spine surgery and also aimed to analyze the literature for current evidence on the same. Methods: A multinational cross-sectional survey was conducted among AO Spine members worldwide to understand the use of topical tobramycin in 1 or 2-level open lumbar fusion surgeries. Also, an independent systematic review of four scientific databases (PubMed, Scopus, clinicaltrials.gov, Web of Science) was performed by two authors to identify relevant articles in adherence to the preferred reporting in systematic reviews and meta-analysis (PRISMA) guidelines. Studies reporting the usage of tobramycin in lumbar spine surgeries were included for analysis. Results: Among the 231 participating surgeons, only 1.7% (n = 4) reported utilizing tobramycin in 1 or 2-level open lumbar fusion surgery. Upon systematic review of the literature, two studies with 484 patients were included for analysis. With the usage of tobramycin as a topical antibiotic powder, both studies noted a reduction in the incidence of infection with change in the spectrum of infective organisms. Conclusion: Topical Tobramycin is not the common choice of topical antibiotic among surgeons worldwide. There is a lack of sufficient evidence in the literature to support the routine use of topical tobramycin in lumbar spine surgery.
304
P351: Outcome after vertebral body replacement with anterior stand-alone spinal cages in spinal tuberculosis patients
Atif Ali 1
1 Department of Orthopedics and Spine, Ghurki Trust Teaching Hospital Lahore, Lahore, Pakistan
Study design: Retrospective and prospective case series. Purpose: The aim of this study was to assess the results of reconstruction of anterior column, fusion with stand alone cages in TB spine patients and complications related to cages. Overview of Literature: studies have shown that tb spine can be effectively managed with anterior corpectomy because pathology is anterior without compromising the posterior column of spine. Anterior cage alone can provide same level of stability after anterior corpectomy as that of posterior instrumentation. In this study we assess the effectiveness and stability of anterior corpectomy and anterior column fusion with stand-alone cages without posterior instrumentation in spinal tuberculosis. Methods: Study was carried out in patients with spinal tuberculosis/Pott’s disease. We assessed 1200 patients who were treated with cages with/without any other instrumentation. Radiographs were obtained before and after the surgery. Total number of patients followed on OPD basis. A preoperative magnetic resonance imaging was obtained in every patient. Results: 1200 patients with tuberculosis spine were followed in Ghurki teaching trust hospital. Kyphotic angle correction was,16.6% patients with 0-10 degree improvement, 60% patients with 11-20 degree improvement and 23.4% patients with 21-30 degree improvement. However after 3 years change in post surgical change in kyphotic angle is insignificant. Regarding the Frankel Scale in patients with neurological involvement,47.49% patients show Frankel scale “E”, 22.61% patients showed Frankel scale “D”, 16.83% showed “C”, 6.03% showed “B” while 7.04% patients showed no improvement after 3 years follow up. Conclusions: The study shows that the vertebral body replacement after anterior corpectomy by reconstructive cages and bone graft provides a reconstruction of the anterior column, good correction of the mean kyphotic angle, effective biopsy of pathology, drainage of pus and a correction maintained with cage without any cage related complication at long term follow up. The fusion can be achieved with reconstructive cage plus bone graft without posterior instrumentation.
655
P352: Craniovertebral junction tuberculosis: how to manage
Arun Kumar 1
1 Neurosciences, Samford Superspecialty Hospital, Ranchi, India
Introduction: Tuberculosis (TB) of craniovertebral junction (CVJ) occurs in 1-5 % of cases of TB spondylitis. This can be a life-threatening condition due to mass effect of infective process or resultant instability. Literature is quite divided on management of patients with tuberculosis involvement of the craniovertebral junction. Material and Method: All patients with CV junction spine tuberculosis admitted in hospital were evaluated and managed accordingly. Total 4 cases were selected as a prototype. This was prospective observational study. Results: 25 % of all cases were managed conservatively whereas in 75 % surgery was done. Conclusion: Treatment of CVJ tuberculosis cannot be standardized, it has to be tailored to each patient broadly, abscess formation, atlanto-axial subluxation with cervico-medullary compression, severe or progressive neurological deficit should undergo surgical intervention at the earliest. Surgery provides for immediate neurological recovery, stability, and allows for early mobilization and also reduces the cost of staged surgery.
Keywords: tuberculosis (TB); craniovertebral junction (CVJ)
658
P353: Cervical spondylodiscitis: a potentially serious disease
Imen Chaabeen 1 , Sabrine Bachrouch 1 , Jlidi Mohamed 2 , Walid Bouaicha 2 , Ibrahim Najjar 2 , Haifa Tounssi 1 , Mariem Elfekih 1 , Mouldi Lamouchi 2 , Karim Mallek 2 , Asma Belhadj 3 , Raja Amri 1 , Selim Daas 2 , Zeineb Alaya 1
1 Internal Medicine Department
2 Orthopedics and Traumatology Department
3 Biology Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia
Introduction: Cervical spondylodiscitis is a rare pathology. The clinical signs are non-specific and lead to diagnostic error or delay and late treatment. We report the case of complicated C0-C1 spondylodiscitis in a diabetic patient. Material and Methods: Patient aged 57, diabetic with degenerative complications and left mid-leg amputation, hospitalized for management of vascular purpura. Two weeks later, he complained of a progressively worsening neck pain, dysphagia, appearance of skin lesions without any recorded fever. On examination, the patient was afebrile. He had infiltrated vascular purpura with a necrotic center in both lower limbs and the abdomen and pain on pressure of the spinous processes (C1, C2, C3) associated with paravertebral contracture. The peripheral white blood cell count was 11000/mm3, and C-reactive protein was elevated to 39mg/l. The thoraco-abdominopelvic CT scan and MRI showed: C0 C1 arthritis associated with a prevertebral collection extended to the retropharyngeal space with epiduritis without spinal cord compression, bilateral foci of nephritis and collection of the left gluteus medius associated with a cortical irregularity of the greater trochanter. Ultrasound of the hear showed 6 mm vegetation on the aortic valve. Blood cultures were positive for methicillin-susceptible Staphylococcus aureus. The diagnosis retained is methicillin-sensitive staphylococcus aureus bacteremia with multiple secondary locations: Bone, cardiac, renal and soft tissues. Results: The patient received antibiotic therapy with cefazolin intravenously for 3 weeks and gentamicin for 5 days, followed by an oral relay with ciprofloxacin associated with rifampicin for 5 weeks. He underwent ultrasound-guided drainage of the gluteus maximus collection and immobilization with a cervical collar. The evolution was favorable with regression of the neck pains, improvement of the general state. The control ETT showed the disappearance of the vegetation after 4 weeks. Conclusion: Spondylodiscitis is a rare and complex pathology. She is burdened with a heavy morbidity and mortality. Clinical manifestations may be nonspecific. Rapid diagnosis and microbiological documentation improve the prognosis.
730
P354: Staphylococcal spondylodiscitis: clinical and therapeutic aspects
Imen Chaabeen 1 , Sabrine Bachrouch 1 , Jlidi Mohamed 2 , Walid Bouaicha 2 , Ibrahim Najjar 2 , Yosra Abid 1 , Haifa Tounssi 1 , Mouldi Lamouchi 2 , Karim Mallek 2 , Asma Belhadj 3 , Selim Daas 2 , Raja Amri 1 , Zeineb Alaya 1
1 Internal Medicine Department
2 Orthopedics and Traumatology Department
3 Biology Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia
Introduction: Infectious spondylodiscitis (SPDI) caused by staphylococci remains a diagnostic and therapeutic challenge for the clinician. They carry a high risk of treatment failure and long-term morbidity. The objective of our work was to identify the clinical and therapeutic aspects of staphylococcal SPDI. Material and Methods: A retrospective study was carried out at our department over a period of 5 years, including SPDI cases with staphylococci confirmed by microbiological examination. Results: Our study included 27 cases (24 men and 3 women) of SPDI staphylococci (20 cases staphylococcus aureus SA and 7 cases coagulase- negative staphylococcus SCN). The patients’ average age was 59 years old. Nine patients were diabetic. The factors predisposing to the development of staphylococcal SPDI were mainly: Chronic renal failure at the hemodialysis stage in 6 patients, drug addiction in one patient. Spinal pain was present in all patients. The SPD was cervical (4 cases), dorsal (6 cases), dorso-lumbar (3 cases), lumbar (13 cases) and lumbosacral (1 case). The neurological examination showed bladder and sphincter disorders in 1 case, motor deficit in 20 cases. Blood cultures were performed on all patients. SA was isolated in 20 cases. One strain produced Panton Valentine leukocidin toxin (S PVL). Eleven strains were sensitive to methicillin (SASM). The bacteriological examination of the PBDV made it possible to isolate SA in 2 cases and SCN in 2 cases. An extra-spinal sample was performed on three patients (joint puncture, lumbar puncture and drainage of a psoas abscess). The culture of these samples was positive for SA. The associated localizations were mainly: psoas abscess (4 cases), sacroillitis (2 cases), pulmonary (4 cases, one of which was necrotizing) cerebral empyema (1 case). The antibiotic treatment was adapted to the results of the antibiogram. The evolution was favorable in 26 cases. Conclusion: The clinical presentation of the infectious staphylococcal spondylodiscitis is polymorph. The presence of secondary septic localizations determines the prognosis.
732
P355: Infectious spondylodiscitis in chronic hemodialysis patients
Sabrine Bachrouch 1 , Imen Chaabeen 1 , Jlidi Mohamed 2 , Walid Bouaicha 2 , Ibrahim Najjar 2 , Haifa Tounssi 1 , Manel Lajmi 1 , Mouldi Lamouchi 2 , Karim Mallek 2 , Asma Belhadj 3 , Selim Daas 2 , Raja Amri 1 , Zeineb Alaya 1
1 Internal Medicine Department
2 Orthopedics and Traumatology Department
3 Biology Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia
Introduction: Spondylodiscitis (SPD) is considered as a diagnostic and therapeutic challenge, especially in particular areas such as chronic hemodialysis patients. The aim of our work is to describe the epidemiological, clinical, radiological and microbiological characteristics of SPD in chronic hemodialysis patients. Material and Methods: Retrospective descriptive study carried at our department over a period of 5 years including chronic hemodialysis patients hospitalized for SPD, confirmed by CT and/or spinal MRI. Results: We collected 13 patients (3 women and 10 men). The average age was 57 years old. Diabetic nephropathy was the main cause of CKD. Hemodialysis was provided by arteriovenous fistula (5 patients) and central venous catheter (8 patients). Inflammatory back pain was present in all patients. The average time to progression was 71 days. Fever was present in 4 patients. The SOFA score was greater than 2 in 2 patients. The SPD was multi-staged in 2 patients. The SPD was cervical (2 cases), dorsal (1 case), thoracolumbar (1 case), lumbar (7 cases) and lumbosacral (2 cases). It was complicated by epiduritis (6 patients), epidural abscess (3 patients), spinal cord compression (1 patient) and pachymeningitis (1 patient). Blood cultures were performed on all patients. The disco-vertebral biopsy (BDV) was performed on 2 patients (1 CT-guided and 1 surgical). Pyogenic SPD was found in 11 patients: microbiologically confirmed (7 patients) and presumed (4 patients). The main organism isolated was staphylococcus aureus (5 patients). Tuberculous SPD was diagnosed in two patients. Pathological examination revealed a tuberculoid granuloma on a BDV sample and a pleural biopsy. BK PCR was negative on both samples. The associated locations were mainly psoas abscess (4 patients), sacroillitis (2 patients), pulmonary (4 patients, one of them was necrotizing). The evolution was favorable in 11 patients. Conclusion: SPD in chronic hemodialysis patients remains a health problem with high morbidity and mortality linked to atypical clinical presentations and delay in consultation. Therefore, a multidisciplinary care is required.
786
P356: Unusual organism causing vertebral infection with paraplegia - Salmonella typhimurium
Mukhesh Thangavel 1 , Tarun Roy 1 , Charanjit Singh Dhillon 1
1 Spine Surgery, MIOT Internation Hospital, Chennai, India
Introduction: Salmonella spondylitis is an uncommon type of vertebral infection. We present a case of acute onset paraplegia following pathological fracture caused by Salmonella spondylitis and epidural abscess. Material and Methods: The patient on irregular treatment for his psoriasis presented to us seven days post-acute onset of paraplegia (Frankel A) without any pre-existing trauma. His X rays showed Collapse of D11 vertebrae with multiple healed osteoporotic fractures. MRI revealed signs of D11 pathological fracture, prevertebral and epidural collection with cord compression. He underwent posterior stabilization D9-L1 decompression left costotransversectomy corpectomy D11 and cage reconstruction. Intra-operative cultures sent turned out to be Salmonella Typhimurium. He was treated with IV antibiotics for 8 weeks followed by oral antibiotics for 6 weeks. Results: A follow-up assessment conducted 6 months later revealed no complications stemming from the surgery, and the patient's neurological status improved to Frankel grade D. Laboratory and radiological investigations also demonstrated no evidence of infection. Conclusion: Salmonella infection of the spine are unusual in healthy individuals. They have been sparsely reported in immunocompromised individual undergoing invasive spine procedures and post systemic infection. Our patient though undertook irregular treatment for psoriasis neither underwent any invasive procedure nor showed any systemic symptoms of salmonella. Therefore, it is crucial to consider Salmonella infection as a potential diagnosis in patients with spondylitis.
855
P357: Post-tuberculer kyphotic deformity correction: an analysis of 67 cases
Shah Alam 1 , Sharif Ahmed Jonayed 2 , Abdullah Al Mamun 2 , Md Sarwar Jahan 2 , O Z M Dastagir 2
1 Spine Surgery, Bangladesh Spine & Orthopedic Hospital, Dhaka, Bangladesh, Bangladesh
2 Spine Surgery, National Institute of Traumatology & Orthopaedic rehabilitation, Dhaka, Bangladesh
Introduction: Kyphosis is one of the most common complications of spinal tuberculosis. Patients are never satisfied with the residual kyphosis even if the disease is cured or arrested. Patients with hunchback live secluded lives both mentally & socially. To achieve correction and prevention, surgery is desirable. Nonetheless, satisfactory surgical correction is very difficult and dangerous as well. Materials & Methods: This prospective case series was conducted in a tertiary-level hospital and a private hospital from January 2003 to December 2023. Most of the patients operated posteriorly to achieve correction. Correction of deformity was easier in wet TB than the dry TB. Global reconstruction was done using the single posterior approach in all the cases. Results: This study comprises 67 cases (M = 20, F = 47), with an average age of 17 years. The mean kyphosis angle was 85 ± 9o preoperatively which came down to 13 ± 7o finally. There was no major complication. None of the patients developed or worsened neurologically after surgery. Finally, the patients achieved a satisfactory cosmetic appearance. Conclusion: Prevention of deformity should be the primary aim. Long-standing severe kyphosis produces painful costo-pelvic impingement, reduced vital capacity, lumbar canal stenosis, and late-onset paraplegia. With improved surgical technique and rigid spinal instrumentation involving three columns - the posterior is the only approach for the prevention and correction of kyphosis.
927
P358: Clinical outcome of single stage decompression and fixation for thoraco lumber spine tuberculosis
Biswaranjan Nayak 1
1 Neurosurgery, Kalinga Hospital Limited, Bhubaneswar, India
Objective: To assess the clinical outcome of single stage decompression and posterior stabilization in thoracolumbar spinal tuberculosis. Methods: All patients aged between 18 and 70 years with clinically and radiologically proven symptomatic thoracolumbar spinal tuberculosis who failed with conservative treatment for 4 weeks or developed neurologic weakness between the treatments are included in this study. All patients were offered decompression and posterior stabilization with transpedicular screws and rods after explaining the above procedure. Clinical outcome was measured by modified Frankel grading; AIS (American Spinal Injury Association impairment score) grade impairment score; and pain assessment done with visual analog scale (VAS) pre- and postoperatively and at 3, 6, and 9 months of interval. Results: The postoperative pain relief, neurologic improvement as per modified Frankel grade, AIS grade, and improvement in erythrocyte sedimentation rate and C-reactive protein were significant as compared with the preoperative status. The surgical interventions thus prove to have adequate relief to the patient and arresting the disease progression. The surgical outcome has very minimal intra- and postoperative complications. Conclusion: Single-stage decompression and posterior stabilization in thoracolumbar spinal tuberculosis is safe, effective, and results in good clinical outcome. The advantages of surgery include thorough debridement, decompression, and achievement of spinal stabilization.
1183
P359: Isolated C3 pott's spine and its management
Vishnu Senthil Kumar 1
1 Orthopaedics, Government Royapettah Hospital, Chennai, India
Introduction: Cervical vertebral osteomyelitis is rare and most dangerous manifestation of TB. Diagnostic challenges are enhanced when cervical spine is involved. Isolated vertebra makes the diagnosis more elusive. We describe this case because of the importance of TB as one of the differential diagnosis. Case report: 38 year old adult female presented with neck pain with radiculopathy for 2 month duration. No significant past history or constitutional symptoms. Radiograph of cervical spine showed loss of cervical lordosis with C3 superior end plate destruction. MRI showed destruction and loss of C3 height with collection in the pre-vertebral region stripping the Posterior longitudinal ligament with bilateral root compression with impending canal compromise. Provisional diagnosis was Tuberculosis osteomyelitis of C3. CT guided biopsy failed to obtain material for HPE. In view of abscess and impending quadriparesis. Surgical debridement was performed and anterior C3 corpectomy with mesh cage placed from C2-C4 with supporting anterior plate with screws. Now patient at 1 year follow up, with no subsidence of cage and no evidence of recurrence. HPE diagnosis proved to be caseating granulomas suggesting TB but gram stain was negative. She was started with Anti-TB drugs with four drugs for 3 months and two drugs (Isoniazid+Rifampicin) for 9 months with serially monitored ESR. Discussion: Literature review showed only few case report involving the cervical spine. Manouri et al in their case report described C3 Pott’s in a 10 yr old girl presented with neck pain and torticollis. Differential diagnosis of Langerhans cell histiocytosis should also be taken into account. Conservative management was done in their case. Conclusion: In developing country, TB should always be taken as a differential diagnosis in long standing neck pain with muscular spasm. Early prompt diagnosis and treatment with surgery + Anti-tuberculosis cover is needed to prevent neurological deficit.
1189
P360: Missed multi-focal non-contiguous spinal TB (steroid misuse in Covid -19 pandemic) - A rare case with literature review
Vishnu Senthil Kumar 1
1 Orthopaedics, Government Royapettah Hospital, Chennai, India
Introduction: Spinal TB contributes to 5% of extra-pulmonary TB. Thoraco-lumbar region is the most commonly affected with cervical spine least affected. Skipped lesions contribute 7% of spinal TB cases. We report such a rare case and its management. Case Report: 39 yr old male presented with neck and back pain with radiation to bilateral upper and lower limb. Loss of weight and appetite for 6 month duration. Steroid intake for 6 months because of COVID-19. On examination. Power was 3/5 in all 4 limbs, DTR reduced, decreased sensation in B/L upper and lower limb, ankle clonus present with normal bladder and bowel sensation. Radiological evaluation showed C6-C7,D7 and L4 spondylodiscitis, vertebra collapse and cord compression. CT chest showed consolidated mass in right apical lobe. Other screening normal. We proceeded with open biopsy and anterior cervical corpectomy with fusion (mesh cage and plating). Biopsy suggested granulomatous lesion probably TB. Patient was started on ATT with symptomatic improvement in upper limb compared to lower limb. At 1 month follow up, D7 lesion regressed and L4 lesion persisted with significant cord compression. Open biopsy with decompression and posterior stabilisation with pedicle screws in L2,L3 and L5 levels. HPE proved caseating granulomatous lesion. At 1 year follow up, neurology completely recovered with resumed activities of daily living. Discussion: Skipped multifocal extensive spinal TB is very rare with 6 cases reported so far. The rarity of this disease makes the diagnosis difficult and management challenging. Careful physical examination, sequential radiographs and whole spine MRI plays an important role in early diagnosis and treatment to prevent neurological deterioration. Decompression should be done from top to bottom with immune suppression and HIV playing an important role in extensive non-contiguous spinal TB. Conclusion: This case is reported because of its rarity and dilemma in clinical presentation. It can be mistaken for metastasis because of the skip lesions. Advent of COVID and misuse of steroids can exacerbate mild infections.
1203
P361: Function outcome of dorsal and lumbar koch's spine operated with decompression and long segment pedical screw fixation
Pratik Sidhdhapuria 1 , Shahrukhkhan Pathan 1
1 Orthopaedics, Surat Municipal institute for Medical Education and Research, Surat, India
Introduction: Koch’s spine is granulomatous infection of mycobacterium tuberculosis bacteria, endemic in developing counties. Dorso-lumbar junction area remains most common region to be affected in extrapulmonary tuberculosis infection. Anti-tubercular therapy (ATT) is effective in eliminating the disease, many patients develop neurological weakness and mechanical instability that needs to be addressed by surgery. Though TB is an anterior column pathology, now a days posterior surgical decompression, pedical screw fixation with or without anterior column reconstruction is becoming the main stay of the surgery. Material and Methods: Retrospective analysis of data collected from January 2021 to December 2022 at tertiary care hospital was done and all the patients with thoracolumbar Koch spine operated with posterior decompression and long segment fixation with atleast 6 months of follow-up were included. Xrays and MRI was used as primary tool for the diagnosis which was confirmed by tissue biopsy CBNAAT (gene xpert). All the patients were put on ATT regime for 1 year. Patients who developed neurological weakness or symptoms of spine instability at any time during the therapy were considered for the surgery. All patients were analysed preoperatively and post operatively at 1 month and at 6 months by VAS score, ASIA grading for neurological involvement and Xrays and MRI for radiological outcomes. Results: 20 patients were included in the study,12 patients were treated with pedical screw fixation, direct decompression with anterior column fixation with cage and bone graft and 8 were treated with pedical screw fixation with direct decompression. Mean age of the patients were 32.6 years and 12 (60%) were males. 10 (50%) patients had dorso-lumbar junction, 6(30%) patients had dorsal and 4(20%) patients had lumbar region Koch’s spine. 3 (15%) patients were having multi drug resistant (MDR) TB. 10(50%) patients had ASIA grade C preoperatively. 2 (10%) patients had complications that needed re-surgery. Conclusion: Improvement in VAS, ASIA grade and radiological outcome at 6 months was significant (p < 0.05). Decompression with pedical screw fixation with/without anterior column reconstruction with posterior approach should be standard of surgical treatment.
1525
P362: Does two eggs per day keeps the doctor away?
Mak Rongqi 1 , Nur Aida Faruk Senan 1
1 Orthopedics, Sarawak General Hospital, Kuching, Malaysia
Introduction: Recently, there is an epidemic of newly diagnosed diabetics presenting with soft tissue infections and spine discitis in our wards. Demographics of such patients are getting younger and ‘bigger’. Most orthopaedic patients are in a catabolic state with multiple wounds and infection and a high protein diet will expediate patient recovery. A movement was started within the orthopedic department of our hospital to tackle the root cause of the problem which is glucose intolerance. We introduced a new diet regime within the orthopedic wards, which consist of 2 eggs for breakfast, and high protein diet (HPD) for lunch and dinner. Snacks were eliminated. The hospital daily meals provide about 50gm/day and about 80gm/day for the high protein diet. Material and Methods: Data was collected from 10 patients in the main orthopedic ward who received the HPD and 10 patients from regular ward who received the standard hospital diet. Results: The Intervention group showed high satisfaction to the new implemented diet, they all expressed satiety after the meals. Sugar control improved tremendously after 48 hours into the introduction of HPD. There was average reduction of blood sugar levels from the baseline by 18.4% in the study group and increase of 20.8% in the control group. 100% of those patients had anti-hypertensive and anti-hyperglycemic medication de-prescribed within 48 hours to 72 hours of introducing the HPD. The average weight lost was 7.60 kg lost in the study group versus 0.93 kg in the control group. The control group showed spikes of high blood sugar in the ward after consuming the standard hospital meal consisting of mainly refined carbohydrates (2 slices of white bread, plain porridge and rice with small amount of protein for lunch and dinner). Conclusion: Standard hospital diet does not provide enough protein that the patient needs for adequate wound healing. This initiative has shown that a small alteration to the diet has a big impact on the sugar control and general health of the patient. This improvements lead to better patient outcomes and cost savings with deprescription of medication and shortened hospital stay.
1570
P363: Tackling cervical spine spondylodiscitis using a metabolic approach - The Sarawak approach
Nur Aida Faruk Senan 1 , Mohammad Zaki Mohd Amin 2 , Ying Chyi Chong 1
1 Orthopedics, Sarawak General Hospital, Kuching, Malaysia, 2 Orthopedics, University Malaysia Sarawak, Kuching, Malaysia
Introduction: Spondylodiscitis is an up and rising pathology due to the increasing number of immunocompromised patients in Malaysia. The incidence of diabetes mellitus and end stage renal failure have increased 200% over the last 20 years in this country. Treatment at our center not only involves operative stabilization but we also advocate lifestyle modification in the form of dietary and lifestyle modifications. These additional approach has shown to improve patients glycemic control, reduce dependency on pain medications and better neurological recovery. Material and Methods: We present our case series of 14 patients with cervical spondylodiscitis treated from 2019 to 2021. 93% of the patients were male with only one female. All patients had a metabolic disease of either diabetes or were pre diabetic and had a body mass index of more than 24. Results: 70% were treated anteriorly with anterior cervical plating (with mesh cage/ bone graft) while others only posterior stabilization. 79% had bacterial spondylodiscitis while the rest were tuberculous spondylodiscitis. 50% of the patients presented with neurological deficit with improvement of one or more ASIA grade post operatively. There was one sudden death in the cohort due to an underlying heart condition. All patients with pyogenic discitis were treated with intravenous antibiotics for a total of 6 weeks followed by oral antibiotics for another 6 weeks. Those with tuberculous infection was treated with oral anti tuberculous medication for one year. All patients showed radiological solid fusion at time of follow up, with 20% of patients developing loss of correction. However those patients were asymptomatic. During the admission all patients were given nutritional advise by the treating orthopedic team which involved therapeutic carbohydrate restriction and increasing the total protein and healthy fats intake. All patients showed improved in glycemic control which resulted in deprescription of diabetic and hypertensive medications during the course of their stay. They also all experienced weight reduction of at least 5% of their body weight. Conclusion: This additional dietary and lifestyle modification will not only help the patient recover faster but also reduce the healthcare burden in our country. This new approach taken by the orthopedic spine team has helped to put many patients diabetes in remission and thus reduce their risk of chronic diabetic complications.
1627
P364: “Screwing through the two”: single centre experience of one-stage posterior spinopelvic fixation for lumbosacral junction spondylodiscitis using S2AI screws
Charlene Yeoh 1 , Jayathilak Shanmugam 1 , Han Sim Lim 1 , Zairul Anuar Kamarul Bahrin 1
1 Orthopaedic, Hospital Pulau Pinang, Penang, Malaysia
Introduction: The S2-alar-iliac (S2AI) technique, originally described in 2007 by Sponseller and Kebaish, is gaining prominence as an alternative pelvic fixation method to the traditional method of iliac screws in spinopelvic fixation. The advantages of doing so include a lower profile construct, reduction of prominent hardware related complications and in line rod placement. Violation of the sacroiliac joint has been pointed out by detractors of this technique, but evidence of complications related to this have remained inconclusive and insignificant. Material and Methods: A retrospective case series of 6 patients (age ranging from 32 - 65), who underwent surgical debridement and posterior spinopelvic fixation were reviewed. All patients were diagnosed with lumbosacral junction spondylodiscitis - a subset of patients prone to developing complications due to their underlying comorbidities and immunocompromised status. Intractable pain and poor response to antibiotic were the main indications for surgery. All cases were done in a single centre, Penang General Hospital, Malaysia. Results: A total of 5 males and 1 female patient were included in this review. The affected level of spondylodiscitis ranged from L3/4 to L5/S1. 5 patients had bacterial spondylodiscitis and 1 patient had tuberculous spondylodiscitis which were confirmed via intraoperative cultures. All of these patients experienced instability pain while only 2 had significant progressive neurological deficit. Trial of intravenous antibiotic therapy did not alleviate their symptoms. Post operatively, there was a significant improvement in pain score, neurological deficit and Oswestry Disability Index (ODI). None of the patients required revision surgery for hardware related complications. One patient developed a surgical site infection which required debridement but a delayed primary closure was able to be done prior to discharge. One patient unfortunately succumbed to severity of his illness. Conclusion: We conclude that the S2AI technique is a feasible method of spinopelvic fixation with a lower risk of postoperative complications, suitable in the treatment of spondylodiscitis patients. The theoretical drawback of the S2AI technique has not been conclusively proven to be problematic. However, we acknowledge the small sample size and understand that further research is necessary to strengthen the evidence base for the use of S2AI screws in the management of spondylodiscitis patients.
1797
P365: Postoperative infection after anterior versus lateral lumbar interbody fusion: a systematic review and meta analysis
Ali Khan 1 , Alexander Aguirre 1 , Mohamed Soliman 1 , Cathleen Kuo 1 , Asham Khan 1 , Esteban Quiceno Restrepo 1 , Jeffrey Mullin 1 , John Pollina 1
1 Neurosurgery, University at Buffalo Neurosurgery, Buffalo, USA
Introduction: Postoperative infections are one of the most common complications of any surgery. Anterior Lumbar Interbody Fusion (ALIF) and Lateral Lumbar Interbody Fusion (LLIF) are both commonly performed spinal fusion procedures. Material and Methods: A search of the literature was completed using the PubMed and Embase databases until May 2023 with adherence to the PRISMA guidelines. Studies were included if they directly compared the postoperative infection after ALIF and LLIF. Pooled weighted odds ratios were calculated, and the result of the common effect model was reported. Results: We included a total of 8 studies which had a direct comparison of 694 patients who underwent ALIF and 1453 patients who underwent LLIF. Postoperative infection was reported in 28 (4.0%) of ALIF cases while postoperative infection was reported in 24 (1.7%) of LLIF cases. There was no significant difference in the risk of wound infection between the ALIF and LLIF reported through the common effect model (odds ratio, 1.10; 95% confidence interval, 0.60-2.01; I2 = 9%; p = .36). Conclusion: This systematic review and meta-analysis demonstrates that there are no significant differences in postoperative infection rates between the ALIF and LLIF patients.
1875
P366: Epidemiologicol and clinical profile of spinal tuberculosis patients at Kassab Institute, Tunisia
Benjeddou Wassim 1 , Khalil Habboubi 1 , Amine Chabchoub 1 , Meddeb Mehdi 1 , Hassen Makhlouf 1 , Mondher Mestiri 1
1 Adults, Med Taieb Kassab Institute, Mannouba, Tunisia
Introduction: Despite being one of the oldest known diseases, tuberculosis remains a significant public health concern, particularly in developing nations, where it exerts substantial medical, social, and economic burdens. This study aimed to investigate the epidemiological and clinical characteristics of individuals treated for spinal tuberculosis at Kassab Institute in Tunisia. Material and Methods: This retrospective observational study involved the extraction of data from the medical records of all patients diagnosed with spinal tuberculosis between January 2018 and December 2020 at the institute. The collected data encompassed epidemiological details, clinical characteristics, imaging findings, laboratory test results, and treatment modalities, which were subsequently analyzed. Results: Over a three-year period, 189 cases of spinal tuberculosis were identified. The mean age of the patients was 46 ± 14.5 years, with a slight male predominance (55.7%). Axial pain emerged as the primary clinical symptom (79.5%), and more than half of the patients (54.2%) had experienced symptoms for over six months before seeking medical attention. A history suggestive of pulmonary tuberculosis was noted in 15.5% of cases. The most frequently employed imaging technique was X-ray (92.3%), followed by Magnetic Resonance Imaging (85.6%). The lumbar spine was the most commonly affected site (48.7%), followed by the thoracolumbar spine (24.1%), with less than three vertebral segments involved in 71.3% of cases. Elevated Erythrocyte Sedimentation Rates (ESR) were observed in 76.8% of patients at the time of diagnosis. Neurological impairment of varying degrees was present in 88 (46.6%) patients, and 18.4% presented with spinal deformities. All patients received combination anti-tuberculosis chemotherapy and were followed up for a minimum of 12 months. The majority (88.9%) were managed non-operatively, with 61.5% of those with neurological deficits showing improvement. No mortality was recorded. Conclusion: Spinal tuberculosis predominantly affected individuals in the economically productive age groups. Late presentation and a significant incidence of neurological impairment were notable findings. The persistence of neurological deficits underscores the importance of early intervention and appropriate management to mitigate morbidity. Strategic interventions are warranted to promote timely diagnosis and treatment in this patient population.
1953
P367: Poor prognostic factors in the treatment of spinal instrumentation infection
Shinji Tanishima 1 , Tokumitsu Mihara 1 , Chikako Takeda 1 , Satoshi Fujiwara 1 , Hideki Nagashima 1
1 Division of Orthopedic Surgery, Department of Sensory and Motor Organs, School of Medicine, Faculty of Medicine, Tottori University, Yonago, Japan
Introduction: Spinal instrumentation infections, once they occur, are difficult to treat and sometimes require removal of the implants. The purpose of this study was to investigate the factors associated with poor prognosis in the treatment of spinal instrumentation infections. Subjects and Methods: Between 2004 and 2021, 22 patients (16 males and 6 females, mean age 70.7 years) who were able to be followed for at least 3 months after spinal instrumentation infection at our hospital were included. Patients whose implants were not removed or who did not achieve CRP-negative results were classified as the poor group, while those whose implants were preserved, and CRP-negative results were classified as the good group. The background factors were sex, age, Body Mass Index (BMI), total protein at the time of surgery for the underlying disease, albumin, the organism causing the infection, CRP at the time of infection, and white blood cell count, while the treatment factors were time from onset to surgery, number of operations for infection, concurrent hyperbaric oxygen therapy, and whether vancomycin spraying was used or not. Results: There were 12 cases in the cured group and 10 cases in the failure group. BMI was 23.3 ± 4.1 in the cured group and 18.9 ± 3.5 in the failure group and was significantly lower in the failure group (p = 0.02). The white blood cell count at the time of infection was 7575 ± 1766 μ/L in the cured group and 12570 ± 7005 in the failure group, which was significantly higher in the failure group (p = 0.047). The percentage of resistant bacteria was significantly higher in the failure group (P=0.04). No treatment factors differed significant between the two groups. Binomial logistic analysis showed that low BMI was an associated factor for poor prognosis (odds ratio: 14.6; 95% CI: 1.1-187.3, p = 0.041). Conclusion: Lower BMI was associated with implant removal. On the other hand, the number of surgeries, hyperbaric oxygen therapy, and other measures such as concomitant vancomycin may not lead to effective implant preservation measures in implant preservation, and at present there is no better strategy than infection prevention.
2045
P368: Clinical outcomes of postoperative surgical site infections in patients undergoing posterior thoracolumbar and lumbar instrumentation at The Kassab Orthopedic Institute, Tunisia
Benjeddou Wassim 1 , Khalil Habboubi 1 , Safouen Ben Brahim 1 , Meddeb Mehdi 1 , Hassen Makhlouf 1 , mondher mestiri 1
1 Adults, Med Taieb Kassab Institute, Mannouba, Tunisia
Introduction: Postoperative surgical site infections (SSIs) pose significant challenges following instrumented spinal surgeries, often leading to disability. This study aims to evaluate the incidence and characteristics of postoperative SSIs associated with posterior thoracolumbar and lumbar instrumentation procedures conducted at the Kassab Orthopedic Institute, Tunisia, involving 22 patients. Material and Methods: We conducted a comprehensive analysis of patient demographics, infection profiles, treatment modalities, and perioperative factors within the institute's database, spanning from January 2010 to December 2020. Preoperative and postoperative assessments included Oswestry Disability Index (ODI), Patient Health Questionnaire-9 (PHQ-9), and Visual Analog Scale (VAS) scores for both back and leg pain. Results: Among the 285 patients undergoing procedures at the Kassab Orthopedic Institute, Tunisia, a total of 22 SSIs (7.7%) were diagnosed, with 14 (63.6%) requiring at least one revision surgery for SSI management. Notably, the incidence of infection was significantly higher in patients with lumbar spinal stenosis compared to those with scoliosis or kyphosis (p < 0.01). Meticillin-susceptible Staphylococcus aureus (43.4%) was the most frequently isolated pathogen. Complications attributed to antibiotic treatment were observed in 7.8% of cases, while long-term antibiotic therapy was indicated for 47.2% of patients. Remarkably, instrumentation was successfully retained in 18 patients (81.81%), and all SSIs were effectively controlled without recurrence during the follow-up period. Conclusion: Our analysis, involving 22 patients, revealed an average SSI rate of 7.7% at the Kassab Orthopedic Institute, Tunisia. Patients with deep wound SSIs demonstrated favorable outcomes with the preservation of instrumentation. Timely diagnosis, precise revision surgery encompassing rigorous irrigation and thorough debridement, along with an extended course of antibiotics, played pivotal roles in infection eradication, implant retention, morbidity reduction, and achievement of wound healing.
2087
P369: Preventing implant infection on spine surgery; 1-year follow-up 114 cases
Halit Ozcan 1 , Busra Erdem 1 , Betul Yaman 1 , Inan Uzunoglu 1 , Baris Yasar 1 , Mehmet Kalan 1 , Ahmet Gunaydin 1 , Rafet Ozay 1 , Levent Gurses 1
1 Neurosurgery, Ankara Etlik City Hospital, Ankara, Turkey
Introduction: Surgical site infections are an important postoperative complication of surgical procedures. Although the risk of postoperative infection in neurosurgery is low compared to other surgical procedures, surgical site infections pose a significant problem in terms of increasing mortality, morbidity, hospital stay, and health costs. The risk of surgical site infections depends on the patient's chronic diseases, operation duration, irrigation of the operation area, application of antibiotics to the area during closure, use of double or single layer gloves during surgery, intraoperative complications, postoperative drain time and postoperative wound follow-up. may depend on factors related to It is important to reveal the relationship between these factors and wound healing. Material and methods: 114 patients who underwent surgical treatment and follow-up in our clinic between October 2022 and September 2023 and underwent spinal instrumentation were included in the study. Patients were evaluated in terms of criteria such as preoperative blood values, complications developing during surgery, use of double or single layer gloves during surgery, duration of surgery, irrigation of the operation lodge, application of antibiotics to the lodge during closure, and postoperative drain time. Results: The average age of 114 patients was 59.03, 40.3% (46 patients) were male and 59.6% (68 patients) were female. Dural tear developed in 2.6% of the patients (3 patients), and no wound site problems were observed in the patients who developed dural tear. Postoperative drain time was 24 hours in 77.1% (88 patients) and 48 hours in 5.2% (6 patients); Drainless follow-up was performed in 17.5% (20 patients). There was wound discharge in 5 patients whose drains were monitored 24 hours a day, and skin flora was grown in the wound culture of 3 of them. No growth was observed in the wound culture of 2 patients. No problems were observed in the wound area of the patients whose drains were monitored for 48 hours. Wound discharge was observed in 2 of 20 patients who were followed up without drainage, and skin flora grew in one patient and enterobacteria grew in the other. Double gloves were used in 7.8% of the patients (9 patients) during surgery, wound discharge was observed in 1 of 9 patients, and wound culture was negative. In 50.8% of the patients (58 patients), the bed was washed with rifampicin during surgical closure. There was wound discharge in 6 patients, skin flora was grown in the culture of 4 of them, 1 culture was negative, and 1 had enterobacter growth in his culture. One of the 56 patients in whom rifampicin was not used during surgical closure had wound discharge and no growth was detected in the culture. Conclusion: Factors such as intraoperative complications, surgery duration, use of double gloves, surgical site irrigation, operation time, and postoperative drain follow-up periods affect the wound healing of patients. In this study, it was aimed to reveal the effect of the examined factors on the postoperative wound healing of cases with spinal instrumentation.
2275
P370: Result of only posterior decompression and fixation in dorso-lumbar tuberculosis of spine
Mehulkumar Chandana 1
1 Orthopaedics, Zydus Medical College Dahod, Dahod, India
Introduction: Tuberculosis has been predicted to be the largest single infectious cause of death. Tuberculosis at dorsal and lumbar level of spine is inherently unstable. tuberculosis of spine is a common cause of anterior column destruction of spine and thus resulting into kyphosis, a sequel which can present as late onset weakness. If the patients are diagnosed early, they can be treated conservatively. However, with proper indications, surgical procedures are superior in the prevention of neurological deterioration, maintenance of stability, prevention of deformity, early recovery & early mobilization. In present study, we have studied the results of only posterior decompression and fixation in Dorso lumbar Koch’s spine in view of neurological status, amount of fusion, amount of correction of kyphotic deformity & life style status over the period of time. Material and Methods: Total 60 Patients admitted in hospital were taken in the study initially and final analysis were done for 50 patients. All patients (n = 50) who had tuberculosis of spine at dorsal and/or lumbar with or without neurological deficit and with or without deformity &were managed by only posterior decompression and fixation. Study were done for the cases for development of deformity at dorsal and lumbar spine treated by posterior decompression and fixation and their neurological status. Minimum follow up were done for 12 months. Result: Out of total 50 patients 54% were males and 46%were females. 31-40 years age group had 28% incidence of disease among all patients. As per Frankel grades 40% of the patients had Frankel grade E, 24% had Frankel grade D, 20% patients had Frankle grade A & 14% had grade C. As per Dennis Pain score 36% patients were pain free and 54% patients had occasional pain. 18% Lumbar group patients had occasional pain whereas 12% Dorso lumbar group of patients had occasional pain. As per Dennis work score, 50% patients returned to previous heavy work and 28% patients returned to light work and lumbar group had best outcome whereas 22% of them could return to their previous heavy work. 18%patients of Dorsal group were returns to previous heavy work. As per Bridwell fusion Score 72% patients had definitive fusion. 30% of dorsal group and 28% of lumbar group of patients had definitive fusion, as per Seybold & Bayley Scale patients with dorsal tuberculosis had an average score of 13.78 (good). Lumbar region tuberculosis had marginally better score 15.72 (good). Dorso lumbar region tuberculosis patients had score of 13.66 (good). Average is 14.66 (good). Functional outcome was better in patients treated with posterior fixation and decompression. Conclusion: Dorsal and lumbar level prone to instability and deformity which affects the functional performance in future life. functional outcome is better according to Seybold and Bayley Scale, in form of pain relief, work performance, fusion and neurological outcome after posterior decompression and fixation. Thus Progression of deformity is prevented. Posterior fixation is safe and helps in early mobilization and rehabilitation & Posterior decompression facilitating possible neurological recovery.
2339
P371: Spondylodiscitis due to Candida albicans: a case report and narrative review
Pedro Torres 1 , Andre Castilho 1 , Haroldo Oliveira De Freitas Junior 1 , Henrique Darmstadter 1 , Rodrigo Cruzeiro 1
1 Spine Surgery, Hospital UNIMED, Brazil
Introduction: Spondylodiscitis is an infectious condition involving the vertebral bodies and adjacent intervertebral discs. It represents approximately 2-7% of all bone infections and typically affects individuals in their fifth and sixth decades of life. Spondylodiscitis most commonly involves the lumbar region (58%) followed by the thoracic region (30%), with Staphylococcus aureus being the causative agent in over 50% of cases. Other causative agents include enteric Gram-negative bacteria, Streptococcus, and Mycobacterium tuberculosis. Fungal spondylodiscitis is relatively rare (0.5 – 1.6%), primarily occurring in immunosuppressed patients. Candida albicans is the predominant causative agent (62%), followed by C. tropicalis (19%) and C. glabrata (14%). In this study, we present a case of a female patient with spondylodiscitis due to Candida albicans, detailing her treatment and clinical progress. Additionally, we conducted a narrative review of the literature to explore aspects of this topic, including epidemiology, pathophysiology, and available treatments. Materials and Methods: We report the case of a 35-year-old immunocompetent female patient who was admitted to our service with subacute low back pain refractory to conservative treatment, including analgesia and physiotherapy. The patient did not exhibit any changes in strength, sensory function in the lower limbs, or abnormalities in laboratory tests but reported recurrent episodes of vaginal candidiasis. Nuclear Magnetic Resonance Imaging of the thoracic and lumbar spine revealed hyperintensity on T2 and STIR sequences and hypointensity on T1, suggesting a localized infectious process. Two percutaneous biopsies performed one week apart both yielded positive results for Candida albicans. A comprehensive search was conducted on the PubMed database for relevant review studies and case reports concerning fungal spondylodiscitis due to Candida albicans. The most recent and pertinent articles were selected for our analysis. Results: Fourteen days after the second biopsy, the patient underwent posterior arthrodesis from T10 to L1 due to severe kyphotic deformity in the affected segment of spondylodiscitis. Two months postoperatively, imaging studies continued to show changes consistent with spondylodiscitis, necessitating additional surgical intervention. A lateral thoracic approach was employed, involving thoracotomy at the 10th intercostal space, resection of devitalized bone tissue, and management of the inflammatory process. Additionally, T11-T12 arthrodesis was performed via the anterior approach. The patient received a six-month course of 450 mg of Fluconazole, resulting in complete remission of the infectious condition in her spine. Conclusion: Fungal spondylodiscitis typically arises from three main etiologies: contiguous spread, direct inoculation (as seen in lumbar punctures, anesthesia, and spinal surgery), and hematogenous dissemination, the most common mechanism following a Candidemia focus. In the case reported, the leading hypothesis is that Candida albicans from the vaginal region disseminated to the spine via the bloodstream. The literature offers varying recommendations regarding the choice between conservative or surgical treatment for immunocompetent patients with fungal spondylodiscitis. Key surgical indications include the onset of neurological deficits, disease progression, the presence of a large epidural abscess, spinal instability, intractable pain, and failure of conservative management. Generally, patients undergoing treatment for fungal spondylodiscitis exhibit a favorable prognosis, with complete recovery rates ranging from 67% to 100%.
2352
P372: Full endoscopic interbody fusion for pyogenic spondylodiscitis
Takaoki Kimura 1
1 Spinal Surgery, Tokyo Spine Clinic, Tokyo, Japan
Background: Treatment of pyogenic spondylodiscitis is often difficult, but few surgical methods have been established. In recent years, full endoscopic discectomy and lavage by transforaminal approach has been reported, and this time we performed full endoscopic surgery as an anterior reconstruction in addition to posterior fusion for the cases of pyogenic spondylodiscitis that required interbody fusion. We report that we obtained good results by performing intervertebral discectomy and autologous bone grafting using full endoscopy by a bilateral transforaminal approach. Case: Case 1 was a 62-year-old man who underwent laminectomy at another hospital for lumbar canal stenosis two years ago, and his diabetes was poorly controlled. This time, he developed lower back pain and was diagnosed with discitis on MRI and underwent endoscopic discectomy and lavage. After 4 weeks of antibiotics, a mild inflammatory reaction remained, low back pain, and severe destruction of the vertebral body. After posterior fusion, we performed endoscopic discectomy and autologous bone grafting by bilateral transforaminal approach. Case 2 was a 32-year-old man with no past medical history who developed the disease due to lower back pain. After 4 weeks of antibiotics, a mild inflammatory reaction remained, as well as lower back pain and kyphotic deformity, so similar surgery was performed. In both cases, the postoperative low back pain disappeared, the inflammation turned negative, and the patients were discharged. Discussion: Full endoscopic discectomy has been reported for some time, and it is an approach that avoids complications such as nerve damage and allows for effective disc removal directly. In this study, we demonstrated that by using an endoscope for anterior reconstruction, in addition to these advantages, destruction of other supporting tissues and expansion of infection during intraoperative manipulation can be minimized, and it is also minimally invasive for the patient. It has been suggested as one of the future treatments for pyogenic spondylodiscitis. Conclusion: We reported a minimally invasive surgical treatment using an endoscope for pyogenic spondylodiscitis.
2379
P373: One-stage posterior approach in surgical treatment of single-segment thoracolumber spinal tuberculosis with neurological deficits in adults - Our experience
Md Rezaul Karim 1
1 Spine Surgery Unit, National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Background: Surgical management of spinal tuberculosis (TB) has been classically the anterior, then combined, and of late increasingly by the posterior approach. There are quite a few controversies on the surgical management of single-segment thoraco-lumbar spinal tuberculosis with neurological deficits (STSTND). In this study, the clinical efficacy and feasibility of one-stage posterior- debridement, interbody fusion, and posterior instrumentation for treating STSTND in adults were retrospectively evaluated. Our study is a retrospective analysis by authors in variable disease pattern of TB Spine operated at an institute using a single posterior approach. Methods: Twenty cases with STSTND underwent one-stage posterior debridement, interbody fusion and posterior instrumentation at the different institution from January 2017 to January 2022. Follow-up time was 24.4 ± 10.2 months (range, 12-36 months), and kyphosis angle was 34.1 ± 12.3°. The American Spinal Injury Association (ASIA) classification of spinal cord injury was employed to evaluate neurological deficits, while visual analogue scale (VAS) was employed to assess the degree of pain. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were used to evaluate the activity of tuberculosis (TB). Results: All 20 patients with spinal tuberculosis (ST) were completely cured, and there was no recurrence of TB. Postoperative kyphosis angle was 8.2 ± 1.8°, and there was no significant loss of correction during the final follow-up. Solid fusion was achieved and pain was relieved in all cases. Neurological condition in all patients improved after surgery. Conclusions: One-stage posterior debridement, interbody fusion, and posterior fixation followed by chemotherapy seems to be adequate for obtaining satisfactory healing of single-segment thoraco-lumbar spinal tuberculosis with neurological deficits. Careful patient selection is critical to the successful outcome with this technique.
Keywords: spinal tuberculosis; single-segment; neurological deficits; posterior-only approach; thoraco-lumbar
Medical economics
320
P374: Clinical utility and patient compliance with mobile applications for home-based rehabilitation following transforaminal lumbar interbody fusion
Adam Cole 1 , Alex Tang 2 , Matthew Parry 2 , Tan Chen 3
1 Medicine, Geisinger Commonwealth School of Medicine, Scranton, USA
2 Orthopaedic Surgery Northeast Residency
3 Department of Orthopaedic Surgery, Geisinger Health, Wilkes-Barre, USA
Introduction: Transforaminal lumbar interbody fusion (TLIF) via open or minimally invasive (MI) techniques is commonly performed to treat degenerative diseases of the lumbar spine. Postoperative rehabilitation and therapy protocols are widely employed. Mobile applications for home-based therapy programs have grown in popularity and have been widely used following orthopedic procedures. There is, however, limited data describing the utility and compliance with such self-directed programs and its effects on patient-reported outcome measures (PROMs) following TLIF. The purpose of this study was to (1) compare PROMs between post-operative patients who were the most and least compliant in using the mobile-based rehabilitation programs, (2) compare PROMs between patients undergoing open vs. MI-TLIF, and (3) quantify the overall compliance rate of such home-based rehabilitation programs. Material and Methods: A retrospective review was performed from 2019-2023 identifying patients who underwent one- or two-level open or MI-TLIF for degenerative lumbar pathology. All patients were automatically enrolled in the rehabilitation program. Patient-Reported Outcomes Measurement Information System (PROMIS) and Oswestry Disability Index (ODI) scores were collected perioperatively and assessed longitudinally. Patients were separated into two study groups for comparison based on application compliance and surgical technique. Patient compliance and engagement were defined as those who downloaded the application (DL+) and had set therapy session reminders (R+) on their mobile devices. Compliance rate was calculated as the difference between the number of active participants at the preoperative phase and final follow-up. Descriptive and inferential statistics were performed. Results: A total of 220 patients (MI-TLIF: n = 38; open TLIF: n = 182) were included. Average follow-up time was 23.2 months. No difference was found in ∆PROMIS scores (DL+R+: 6.1 ± 5.0; DL-R-: 4.0 ± 6.9; p = 0.261) or ∆ODI scores (DL+R+: 23.7 ± 16.3; DL-R-: 24.1 ± 9.2; p = 0.690) regardless of patient compliance and engagement. No difference was found in the improvement of outcomes scores between open vs. MI-TLIF techniques as stratified by DL+/DL- and R+/R- at any postoperative time point. Both open and minimally invasive cohorts demonstrated clinical improvement exceeding minimal clinically important difference at final follow-up. Overall patient compliance to the program was 71% at final postoperative follow up (MI-TLIF: 37%, Open-TLIF: 79%). Conclusion: Despite high long-term compliance and rising popularity, mobile applications for home-based postoperative rehabilitation programs have low clinical utility in patients undergoing transforaminal lumbar interbody fusion.
430
P375: Perioperative transverse abdominal plane blockade as part of multimodal analgesic treatment in lumbar surgery, anterior approach and posterior fixation (ALIF - FPP)
Ana Sofia 1 , Diana Chavez 2 , Alberto Perez 2
1 Neuroanesthesia
2 Neurosurgery, Hospitales Angeles, Mexico City, Mexico
Introduction: Transverse abdominal block (TAP) have become more relevant and currently constitute a real alternative to neuraxial techniques. These blocks are a complement within the multimodal strategy for postoperative pain control in abdominal approach spine surgery. Ultrasound in regional anesthesia provides greater efficacy and safety, because of the direct visualization of the neural structures, adjacent structures and distribution of the local anesthetic, the detection of anatomical variants, reduction of the volume of local anesthetic and increased patient satisfaction. Within spine surgeries, anterior approach lumbar interbody fusion (ALIF) is one of the most widely used techniques for restoration of lordosis and indirect decompression, combined with lumbar fixation with transpedicular screws increases the requirement of opioid analgesics in the first postoperative hours to control abdominal and lumbar pain. The main objective of this study is to decrease the use of trans and postoperative opioids and its adverse effects in lumbar spine surgery with anterior approach and posterior fixation. As well as promote early mobilization and decrease times in hospital stay associated with post-surgical pain. Material and Methods: A database of patients undergoing ALIF + FPP lumbar spine surgery will be made, between the months of may to september 2023, using the analogue visual assessment of pain in the preoperative, immediate and medium postoperative after the application of TAP block, guided by ultrasound. Demographic data will be collected, pathological history, use of analgesics and neuromodulators, surgical times, bleeding time, neurophysiological changes, hospitalization time. Results: Anterior arthrodesis and posterior lumbar fixation L5S1 was made in 9 patients, with an average of 41.2 years, mean BMI 25.9. Average surgery time of 86 minutes with 163 cc average bleed amount. The mean preoperative scores for the pain was VAS 8/10, VAS 4/10 at 6 and 12 hours and VAS 1/10 at 18 hrs. Of the 9 patients, only 3 required the use of a rescue analgesic, Ketorolac in a single dose at 12 hours after surgery and when starting mobilization out of bed, referring pain in the posterior lumbar area, denying pain in the abdominal region. All patients were discharged within 24 hours post-surgery. Conclusion: The use of USG-guided bilateral tap block decreases opioid consumption in the trans surgical period and in the immediate postoperative period in patients undergoing ALIF + FPP surgery. TAP block is very useful to decrease times of hospital stay by reducing post-surgical pain.
594
P376: ChatGPT answers patient focused questions in cervical spine surgery
Tejas Subramanian 1 , Kasra Araghi 1 , Troy Amen 1 , Austin Kaidi 1 , Brandon Sosa 1 , Tomoyuki Asada 1 , Pratyush Shahi 1 , Yeo Eun Kim 1 , Myles Allen 1 , Avani Vaishnav 1 , Eric Mai 1 , Cole Kwas 1 , Chad Simon 1 , Maximillian Korsun 1 , Eric Kim 1 , Evan Sheha 1 , James Dowdell 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Artificial intelligence (AI) and its utilization to improve patient experience across medicine is seeing remarkable growth. Ever since ChatGPT was released, its potential uses have been increasingly explored. One such usage is patient education. For the first time on a large scale, patients are able to ask targeted questions and receive similarly targeted answers. While patients may use these recourses to assist in decision making, there still exists little data regarding their accuracy especially within orthopedic surgery and more specifically spine surgery. The current study aimed to examine the quality of responses to cervical spine questions surgeons frequently get asked in clinic. Material and Methods: We compiled 9 frequently asked questions cervical spine surgeons receive in clinic to test ChatGPT’s version 3.5 ability to answer a nuanced topic. Questions included were: 1) What are the different types of cervical spine surgery? 2) What are the indications for cervical spine surgery? 3) What is the difference between an ACDF and a CDR? 4) What are the benefits and drawbacks of ACDF and CDR? 5) Will my neck pain improve after ACDF or CDR? 6) Will my arm pain improve after ACDF or CDR? 7) Is there a chance I will not improve or get worse after cervical spine surgery? 8) What are the chances I will have swallowing difficulties following cervical spine surgery? 9) How long is the recovery following cervical spine surgery? Responses were reviewed by two independent reviewers on a Likert scale for the accuracy of information presented (0-5 points), appropriateness in giving a specific answer to specific question asked (0-3 points), and readability for a layperson (0-2 points). Readability was assessed via the Flesh-Kincaid Grade Level analysis for the original prompt and for a second prompt asking for rephrasing at the 6th grade reading level. Results: On average, ChatGPT’s responses scored a 7.1/10. Accuracy was rated on average a 4.1/5. Appropriateness was 1.8/3. Readability was a 1.2/2. Readability was determined to be at the 13.5 grade level originally and at the 11.2 grade level after prompting. Conclusion: As chatbots such as ChatGPT become increasingly popular, they are sure to become another resource for patients considering orthopedic surgery. Assessing ChatGPT’s capacity to address cervical spine related patient questions revealed several strengths and limitations. On average, ChatGPT scored a 4.1 out of 5 points for accuracy. This is an impressive demonstration of the data the chatbot has access to as these specific spine surgery questions are not easily answered. However, more significantly, both observers noted that despite ChatGPT’s accuracy, it failed to provide a comprehensive response, often omitting important considerations that compromise the utility of the response. We were especially surprised by the poor readability of ChatGPT. Often times if a patient searches for a specific question, it can be 1) difficult to understand research literature or 2) not available on websites such as WebMD. ChatGPT was able to provide answers that answer the specific question asked in a way that most can understand. And because of this, it becomes a very powerful tool for the dissemination of information to patients looking to understand their pathologies and surgical options. ChatGPT is still useful, but its utility might be limited to those with higher medical proficiency. Additionally, while ChatGPT would provide a response, it importantly always prefaced with a statement regarding consulting a spine professional for specific medical advice. We believe that patients will increasingly utilize ChatGPT as a resource for informing their medical decision-making. Since the information may not always be fully accurate or inclusive, surgeons should know patients will be using it as a tool and should be aware of its limitations.
818
P377: Clinical utility and patient compliance with mobile applications for home-based rehabilitation following cervical spinal fusion
Christopher Lloyd 1 , Katie Lee 1 , Arpitha Pamula 1 , Alex Tang 2 , Tan Chen 3
1 Medicine, Geisinger Commonwealth School of Medicine, Scranton, USA
2 Orthopaedic Surgery Northeast Residency
3 Department of Orthopaedic Surgery, Geisinger Health, Wilkes-Barre, USA
Introduction: Cervical degenerative disease leading to progressive radiculopathy or myelopathy is frequently addressed surgically with anterior cervical discectomy and fusion (ACDF) or posterior decompression and instrumented fusion (PDIF). Postoperative rehabilitation and therapy protocols are widely employed. Mobile applications for home-based therapy programs have grown in popularity and have been widely used following orthopedic procedures. There is, however, limited data describing the utility and compliance with such self-directed programs and its effects on patient-reported outcome measures (PROMs) following cervical fusion. The purpose of this study was to (1) compare PROMs between post-operative patients who were the most and least compliant in using mobile-based rehabilitation programs, (2) compare PROMs between patients undergoing ACDF vs. cervical PDIF, and (3) quantify the overall compliance rate of such home-based rehabilitation programs. Material and Methods: A retrospective review was performed from 2019-2023 identifying patients who underwent elective ACDF or cervical PDIF procedures for degenerative pathology. All patients were automatically enrolled in the rehabilitation program. Patient-Reported Outcomes Measurement Information System (PROMIS) and Neck Disability Index (NDI) scores were collected perioperatively and assessed longitudinally. Patients were separated into two study groups for comparison based on application compliance and fusion construct. Patient compliance and engagement were defined as those who downloaded the application (DL+) and had set therapy session reminders (R+) on their mobile devices. Compliance rate was calculated as the difference between the number of active participants at the preoperative phase and final follow-up. Descriptive and inferential statistics were performed. Results: A total of 775 patients (ACDF, n = 571; PDIF n = 204) were included. Average follow-up time was 41 weeks (ACDF: 41.7 weeks, PDIF: 38.6 weeks). A greater proportion of DL+R+ patients underwent ACDF than DL-R- patients (86% vs. 69%, p < 0.0001). No difference was found in ∆PROMIS (DL+R+: 4.2 ± 6.2; DL-R-: 3.0 ± 6.2; p = 0.205) or ∆NDI (DL+R+: -23.6 ± 17.6; DL-R-: -21.4 ± 19.3; p = 0.441) regardless of patient compliance and engagement to the therapy program. No difference was found in the improvement of outcomes scores between ACDF or PDIF cohorts as stratified by DL+/DL- and R+/R- at any postoperative time point. Both surgical approaches demonstrated clinical improvement exceeding minimal clinically important difference at final follow-up. Overall patient compliance to the program was final postoperative follow up was 71% (ACDF: 71.8%, PDIF: 69.2%). Conclusion: Mobile applications for home-based post-operative rehabilitation demonstrated low clinical utility following anterior cervical discectomy and fusion or cervical posterior decompression and instrumented fusion for spondylotic diseases, despite high long-term compliance and growing patient popularity.
934
P378: Racial disparities in spine surgery are significantly reduced in outpatient setting
Troy Amen 1 , Izzet Akosman 1 , Tejas Subramanian 1 , Mitchell Johnson 1 , Sam Rudsill 1 , Kasra Araghi 1 , Chad Simon 1 , Avani Vaishnav 1 , Eric Mai 1 , Yeo Eun Kim 1 , Joshua Zhang 1 , Cole Kwas 1 , Myles Allen 1 , Eric Kim 1 , Nishtha Singh 1 , Olivia Tuma 1 , Maximillian Korsun 1 , Tomoyuki Asada 1 , Pratyush Shahi 1 , Sheeraz Qureshi 1 , Sravisht Iyer 1
1 Hospital for Special Surgery, New York, USA
Introduction: Racial disparities in spine surgery have been thoroughly documented in the inpatient (IP) setting. However, despite an increasing proportion of procedures being performed as same-day surgeries, whether similar differences have developed in the outpatient (OP) setting remains to be elucidated. The purpose of this study aimed to (1) investigate racial differences in utilization and postoperative outcomes between Black and White patients following OP lumbar and cervical spine surgery and (2) compare any differences to those found in the IP setting. Material and Methods: This is a retrospective cohort study. Patients who underwent IP or OP microdiscectomy, laminectomy, anterior cervical discectomy and fusion (ACDF), or cervical disc replacement (CDR) between 2017 and 2021 was conducted using the National Surgical Quality Improvement Program (NSQIP) database. Disparities between Black and White patients in (1) adverse event rates, (2) readmission rates, (3) reoperation rates, (4) non-home discharge rates, (5) mortality rates, (6) operative times, and (7) hospital LOS between Black and White patients were measured and compared between IP and OP surgical settings. Multivariable logistic regression analyses were used to adjust for potential effects of baseline demographic and clinical differences. Results: Of 81,696 total surgeries, 49,351 (60.4%) were performed as IP and 32,345 (39.6%) were performed as OP procedures. White patients accounted for a greater proportion of IP (88.2% vs. 11.8%) and OP (92.7% vs. 7.3%) procedures than Black patients. Following IP surgery, Black patients experienced greater odds of serious (OR 1.214, 95% CI 1.077 – 1.370, p = 0.002) and minor adverse events (OR 1.377, 95% CI 1.113 – 1.705, p = 0.003), readmission (OR 1.284, 95% CI 1.130 – 1.459, p < 0.001), reoperation (OR 1.194, 95% CI 1.013 – 1.407, p = 0.035), and non-home discharge (OR 2.304, 95% CI 2.101 – 2.528, p < 0.001) after baseline adjustment. Disparities were less prominent in the OP setting, as Black patients exhibited greater odds of readmission (OR 1.341, 95% CI 1.036 – 1.735, p = 0.026) but were no more likely than White patients to experience adverse events, reoperation, individual complications, non-home discharge, or death (p > 0.050 for all). Conclusion: Racial inequality in spine surgery utilization and postoperative complications is evident, however disparities in complication rates are relatively reduced following OP compared to IP procedures. Efforts to promote greater access to quality OP spine care for patients of color may therefore serve as a viable method of reducing racial disparities in the field of spine surgery.
1122
P379: Utilization of in-hospital orthopaedic spine consultations: evaluating the impact of health care policy
Parker Brush 1 , Alexa Tomlak 1 , Nicholas Pohl 1 , Michael McCurdy 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Mark Lambrechts 1 , Matthew Meade 2 , Charles Lawall 1 , Jackson Weber 1 , Amit Syal 1 , Jose Canseco 1 , I. David Kaye 1 , Mark Kurd 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Alan Hilibrand 1 , Gregory Schroeder 1
1 Department of Orthopaedic Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
2 Department of Orthopaedic Surgery, Philadelphia College of Osteopathic Medicine, Philadelphia, USA
Introduction: Access to specialty and private practice providers has been a divisive policy issue over the last decade, complicated by the conflict between a reduction in government-funded health care reimbursement and the need for health care providers to sustain a financially sound practice. This study evaluates the orthopaedic spine consult service at an academic tertiary care center at two separate time points over a five-year period to better understand the impact of decreasing orthopaedic reimbursement rates and increasing prevalence of federally supported medical insurance on the access to specialty care. Material and Methods: The internally managed database for orthopaedic surgery patient consultations at the urban tertiary care center of interest was reviewed for the years 2017 and 2021, omitting the years in between, to evaluate for differences in patient care over time. The institution’s electronic medical record was reviewed for patient demographic information, consult location, reason for the consult, radiologic resource utilization, consult diagnosis, when and how many patients went on to require spine surgery, and the insurance provider for the encounter. Consult locations were divided into consults from the emergency department or consults from hospital inpatient teams. Any patient with a spinal cord injury was classified by the American Spinal Injury Association Impairment Scale (AIS) score and grouped (AIS A and AIS B vs AIS C, AIS D, and AIS E). The insurance providers were categorized as Medicare, Medicaid, private insurance, uninsured, or other (i.e. car insurance, worker’s compensation, and veteran insurance). Statistical analysis compared the consult information for patients in 2017 to the patients in 2021. Mann Whitey U Test or -test were used to compare continuous variables while Fisher's exact test or chi-squared test were used to compare categorical variables. Results: 500 patients in 2017 and 480 patients in 2021 were included for final analysis. A higher percentage of consults in 2021 came from the emergency department (74.0% versus 60.4%, p < 0.001), however, the emergency department saw fewer spinal cord injuries (11.9% versus 21.4%, p < 0.001) and the spinal cord injuries were less severe (3.1% versus 6.2% AIS A or B, p = 0.034). A smaller percentage of patients in 2021 went on to receive orthopedic spine surgery following consultation (35.2% versus 43.8%, p = 0.007), and those receiving surgery had an operation performed farther out from the initial consultation (4.73 versus 4.09 days, p < 0.001). Additionally, fewer patients with Medicare insurance (23.5% versus 30.8%) and more patients with Medicaid insurance (20.2% versus 12.4%) were seen in 2021 compared to 2017 (p = 0.003). Conclusion: Overall, this study found an increased proportion of Medicaid patients seen by the spine consult service, but a decrease in the acuity of consults. Measures to improve access to health insurance under the Affordable Care Act (ACA) have revealed the complexity of this issue in healthcare. This study's findings have demonstrated that while more patients did have insurance coverage following ACA, they still face a barrier to accessing outpatient orthopedic spine providers.
1283
P380: Extended surgical spine team organization: a 2-years experience of inclusive practice of neurosurgery in an pediatric orthopaedics team
Timothée de Saint-Denis 1 , Elie Saghbiny 1 , Laura Marie-Hardy 1 , Mathilde Gaume 1 , Raphael Vialle 1
1 Pediatric Orthopaedics, University Institute for Spine Surgery, Sorbonne University, Paris, France
Introduction: Spine surgery has emerged during the last decades and is now shared between neurosurgery and orthopedic teams. Pediatric spine surgery cases are presently mainly managed in orthopedic unit, diseases varies from trauma and idiopathic scoliosis to rare constitutional bone diseases and others neurological impairment and their innovative treatment. Neurosurgery emerged at the end of the nineteen century thanks to development of anesthesia, innovative tools and techniques. Recent evolution of practice has seen emergences of subspecialties such as pediatric, oncology, functional, leading to multiple units in large neurosurgical departments. We intend to renew the collaboration between orthopedic and neurosurgical teams for pediatric patients with rare diseases involving spine and spinal cord. Materials and Methods: After collaborating occasionally for cases and prenatal surgery from another hospital, a pediatric neurosurgeon specialized in spine and spinal cord was welcomed in a conventional pediatric orthopedic department in September 2021. Fields of collaborations has been dictated by the needs of the patients and the national policy for neurosurgical practice. Results: 100 patients have been operated with ortho-neuro collaboration (i.e neurosurgeon and orthopedic surgeon) during the first 18 months. Prenatal surgery, complex spine deformity surgery, spinal cord surgery (dysraphisms), extramedullary oncology and skull isolated lesions have been treated in a pluridisciplinary team including orthopedic surgery, ENT, anesthesiology, pediatric surgery, foetal surgery ressources. Low rate of complications has been encountered (1 complex spine surgery deep infection, 2 CSF leak). No patients needed to be referred to a reference neurosurgical unit. Conclusion: Focusing resources in national care organization is needed to reduce the cost and increase the expertise offered to patients. Building a specialized multidisciplinary team addressing specific technical issues as in rare diseases is an alternative to large specialty units. Building a multidisciplinary team around complex spine and spinal cord disorders at our institution seems to be promising in term of efficient care proposals and safety.
1327
P381: Determinants of operative duration and blood loss in adult spinal deformity surgery
Omri Maayan 1 , Bo Zhang 1 , Anthony Pajak 1 , Hiroyuki Nakarai 1 , Han Jo Kim 1 , Francis Lovecchio 1
1 Hospital for Special Surgery, New York, USA
Introduction: Protracted operative duration (OD) and blood loss (EBL) are associated with postoperative complications and inferior patient-reported outcomes. The purpose of this study is to identify factors exhibiting the greatest influence on OD and EBL to improve operating efficiency and reduce variability in adult spinal deformity (ASD) surgery. We also sought to determine the impact of increased OD and EBL on postoperative outcomes. Material and Methods: Patients who underwent ASD surgery (posterior-only, ≥ 5 levels of fusion to the pelvis) were included. The primary outcome of interest was OD, defined as time from skin incision to closure. The following variables were evaluated: surgeon experience (date of surgery), body mass index (BMI), estimated blood loss (EBL), incidental durotomy, levels fused, posterior column osteotomies, three column osteotomies (3CO), transforaminal interbody fusions, lumbar lordosis (LL) correction, and max cobb angle correction. EBL was also included as a secondary outcome. Multiple linear regression was implemented to assess the influence of each variable on the outcomes of interest. Postoperative variables including length of stay (LOS), Patient-Reported Outcome Measurement Information System Physical Function (PROMIS PF), and complications were compared between patients with > average OD/EBL and ≤ average OD/EBL. Results: 259 patients were included (mean age: 64.6 ± 11.2 years; BMI: 27.8 ± 6.0 kg/m2; OD: 4.9 ± 1.5 hours, levels fused: 8 [range 5-25], 3CO: 18.5%). Average LL and Cobb angle corrections were 20.0 ± 16.1° and 16.8 ± 10.4°, respectively. Increased OD was associated with EBL (β:0.39, p < 0.001) and number of levels fused (β: 0.31, p < 0.001). Increased EBL was associated with OD (β:0.47, p < 0.001) and 3CO (β:0.005, p = 0.005). Date of surgery, a proxy for surgeon experience, was negatively correlated with OD (β:-0.31, p < 0.001) and EBL (β:-0.33, p < 0.001). Cases performed in the second half of the case log demonstrated significant decreases in both OD (Δ-42.6 minutes, p < 0.001) and EBL (Δ-378.8 mL, p < 0.001), as well as increased consistency demonstrated by decreased standard deviation for OD after approximately case 170 (Δ-12.6 minutes, p = 0.048). Increased LOS was found to be associated with > average OD (5.8 ± 3.4 vs. 7.0 ± 2.7 days, p = 0.004) and EBL (6.0 ± 3.4 vs. 6.9 ± 2.8 days, p = 0.03). A greater rate of postoperative complications was likewise associated with > average OD (7.2% vs. 17.9%, p = 0.009) and EBL (9.0% vs. 17.3%, p = 0.04). All patients showed significant improvement in PROMIS PF postoperatively (p < 0.05 for all). Conclusion: OD and EBL exhibited the strongest independent relationship. Other significant determinants of increased OD and EBL were number of levels fused and performance of a 3CO, respectively. Date of surgery, a gauge for surgeon experience, was negatively associated with both OD and EBL. Above average OD and EBL were associated with increased LOS and postoperative complications. However, all patents exhibited significantly improved PROMs postoperatively.
2011
P382: Does intraoperative multi-drug wound infiltration relieve postoperative pain following single-level TLIF surgery? A randomized controlled trial
Liang Wang 1 , Lei Qi 1
1 Department of Orthopaedic Surgery, Qilu Hospital of Shandong University, Jinan, China
Introduction: How to minimize postoperative pain following spinal surgery has been a great challenge for both surgeons and patients. Transforaminal lumbar interbody fusion (TLIF) has been widely used around the world for the treatment of degenerative lumbar spine disorders, such as lumbar spondylolisthesis and degenerative intervertebral disc diseases. We hypothesized that intraoperative multi-drug wound infiltration could relieve postoperative pain following single-level transforaminal lumbar interbody fusion (TLIF) surgery. The objective of the current study was to evaluate the effect of intraoperative multi-drug wound infiltration for postoperative pain following single-level TLIF surgery. Material and Methods: A randomized, double-blinded controlled trial (RCT) was preformed and the clinical trial number of this study was ChiCTR2200056420. The patients with lumbar degenerative diseases (including spondylolisthesis, lumbar instability, lumbar spinal stenosis, etc.) who received single-level TLIF surgery were included. 50 patients were recruited eventually and each individual was randomly allocated to the study group or control group. The study group received intraoperative wound infiltration of mixed solution with lidocaine, ropivacaine, and epinephrine before wound closure. The control group was infiltrated with an equal amount of normal saline. The primary outcome measure was the visual analog scale (VAS) of postoperative incision pain. The secondary outcome measures were the postoperative opioids dosage, the time of first analgesic demand, and the Oswestry Disability Index (ODI). Results: The VAS of postoperative pain in the study group was significantly lower than the control group within postoperative 24 hours. The opioid dosage was significantly less and the time of first analgesic demand of patient-controlled analgesia (PCA) in the study group was significantly longer than the control group. None of the patients in the study group required analgesic supplementation. The side effects of opioids were significantly less in the study group. There was no significant difference in ODI, operation time, intraoperative blood loss, postoperative drainage, and postoperative incision complications between the 2 groups. Conclusion: Intraoperative multi-drug wound infiltration before closure could significantly relieve postoperative pain following single-level TLIF surgery. It could reduce postoperative opioid requirements and prolong the time of first analgesic demand with no increased side effects. Intraoperative multi-drug wound infiltration is a simple, safe, effective,and low-cost method and a good choice for postoperative pain management.
2440
P383: COVID-19's impact on elective cervical spine surgery: temporary decrease in volume with minimal change in overall length of stay
Anuj Singla 1 , Brook Mitchell 1
1 Orthopedics, University of Virginia, Charlottesville, USA
Introduction: The COVID-19 pandemic caused by the novel coronavirus, SARS-CoV-2, has had lasting impacts on patient care. At many institutions, elective procedures were cancelled or postponed in order to decrease patient exposure to COVID-19. Specialties with the largest decrease in surgical volume included orthopaedic surgery, especially elective cervical spine procedures. Some institutions reported a decrease of surgical volume by up to 75% at the peak of the pandemic, with many sources predicting an extensive period until surgical volume would rebound to normal levels. The present study aimed to assess the impact on a national level and compare case volumes and length of stay to historical trends. Material and Methods: The Mariner database was utilized to identify patients ages 18-84 undergoing elective cervical procedures using Current Procedural Terminology (CPT) codes, and international classification of disease (ICD)-10 procedure codes. Total volumes of cervical procedures performed during COVID (March 2020 to October 2020) were compared to those occurring during the same months a year before the pandemic (2019) (Pre-COVID). This was further split into an early and late time period, COVID Time 1 (March 2020-June 2020), and COVID Time 2 (July 2020-October 2020). After obtaining total surgical volumes, cases were stratified by cervical procedure: anterior cervical discectomy and fusion (ACDF), cervical disc arthroplasty (CDA), and posterior cervical fusion (PCF), as well as by number of levels (single of multiple). Additionally, volumes were reported for 4 regions Northeast (NE), South (SO), Mid-West (MW), West (W). ICD-10 Procedure based hospital billing codes were used to assess inpatient procedures and report total length of stay for each time period. Patient cohorts were matched by total Charlson comorbidity index (CCI) score prior to assessing length of stay to account commodity burden. A linear regression was used to determine average change in length of stay between the Pre-COVID and COVID cohorts. CPT based billing codes were used to additionally report cervical case volume including outpatient cases. The total percentage change for each respective cohort across time comparisons was reported. Results: Overall inpatient case volume decreased the greatest during the first four months of COVID (COVID Time 1). Similarly, outpatient cases were additionally lowest during COVID Time 1. Length of stay was significantly longer for both single and multilevel ACDF procedures during COVID 3.7 ± 6.3 days vs. 3.3 ± 5.6-day 0.40 (0.04-0.76) p = 0.025, 2.9 ± 4.2 vs. 3.2 ± 6.3 0.40 0.33 (0.11-0.55) p = 0.006 respectively. When stratified by COVID time period 1 and 2 length of stay was longest during time period 2, 4.0 ± 7.3 days vs. 3.4 ± 5.3-day 0.58 (0.36-0.79) p = 0.050. Conclusion: While COVID did indeed have a significant impact on surgical volume the total decrease in surgical cases did not decrease as significantly as some initial reports had indicated. Additionally rebound time for surgical cases occurred quickly from July 2020 to October 2020. Overall length of stay was significantly increased for ACDF but remained similar for all other cervical procedures.
Minimally invasive spine surgery
73
P384: Comparing posterior oblique and lateral techniques for minimally invasive sacroiliac joint fusion: a retrospective study on pain relief and functional improvement
Mario Cahueque 1 , Javier Grajeda 2 , Javier Ardebol 3 , Enrique Azmitia 4
1 Orthopaedic Surgery, Hospital Centro Médico, Guatemala City, Guatemala
2 Faculty of Medicine, Universidad Francisco Marroquín, Guatemala City, Guatemala
3 Southern Oregon Orthopedics, Medford, Oregon, USA,
4 Neurosurgery, Hospital Herrera Llerandi, Guatemala City, Guatemala
Introduction: Chronic sacroiliac joint (SIJ) pain is a debilitating condition that often presents significant treatment challenges. Increasingly, SIJ fusion—particularly through minimally invasive surgical (MIS) techniques—is becoming a preferred solution for chronic SIJ pain. Among these MIS techniques, the lateral technique has been extensively investigated, while the posterior oblique technique remains relatively understudied. This study aimed to compare these two techniques for minimally invasive SIJ fusion and evaluate their impact on both pain relief and functional improvement. The hypothesis was that there would be no difference in outcomes between the two techniques. Material and Methods: A retrospective review was conducted on prospectively collected data from a series of SIJ fusions performed at a single institution between January 2020 and December 2022. Included subjects were 50 years of age or older who did not respond to conservative management with 6 months of physical therapy and a positive joint block. Subjects were stratified according to surgical technique. Primary outcomes - pain relief, as measured by the Visual Analog Scale (VAS), and functional improvement, as determined by the Oswestry Disability Index (ODI) - were recorded and assessed both preoperatively and at the 12-month follow-up, with pre-to-post improvements being calculated. The potential confounding effect of previous lumbar fusion on outcomes was assessed during the same time periods, with patients stratified by history of this procedure. Other variables, including demographic, clinical, and surgical data, were also collected and analyzed. Results: A total of 45 patients (22 lateral and 23 posterior oblique) met the inclusion criteria. Baseline demographic and clinical characteristics were similar between the two groups. A history of lumbar fusion did not influence the outcomes at any stage. The posterior oblique group demonstrated shorter operative times (by over 50%) and duration of hospital stay compared to the lateral group. Patients in the posterior oblique group also experienced significantly lower scores in both postoperative VAS and ODI scales (VAS: lateral 3.5 ± 1.7 vs. posterior oblique 2.4 ± 1.5, [p = 0.02]; ODI: lateral 29.6 ± 7.3 vs. posterior oblique 21 ± 5.7, [p = < 0.001]) compared to the lateral group. Pre- to postoperative improvement analysis demonstrated a significant reduction in pain for the posterior oblique group (VAS: lateral -4.4 ± 1.9 vs. posterior oblique -6.1 ± 1.5 [p = 0.002]); however, improvement in functionality was similar between groups (ODI: lateral -16.6 ± 9.6 vs. posterior oblique -21.3 ± 6.5 [p = 0.07]). Conclusion: Compared to the lateral technique group, patients who underwent minimally invasive SIJ fusion using the posterior oblique technique experienced greater pain relief and demonstrated a trend towards improved functionality, with shorter operative time and duration of hospital stay.
142
P385: Endoscopic spine surgery the next gold standard techniques in spine surgery
Ghazwan Hassan 1
1 Orthopedic & Spine Dept., Al-Kindy Teaching Hospital, Baghdad, Iraq
Minimally invasive surgeries continue to advance at an immensely fast pace, moving from open discectomy surgeries to microscopic ones using tubular systems, to do fusions, to correct deformities, until we reached a place where we’re tackling most spinal pathologies in a minimally invasive fashion, For many spine surgeons, the field of spine endoscopy, whether uniportal or biportal, is still unexplored, to some extent due to their mastery in open and microscopic techniques, and to another extent the learning curve that it takes to master endoscopic spine, as well as a lack in well-structured clearcut data regarding its indications and limitations, and this chapter will hopefully shed the proper lighting on the field of spinal endoscopy, making surgeons understand its utility in treating different pathologies, discussing the research and data comparing spinal endoscopy with more traditional techniques, as well as understanding endoscopic spine surgery’s learning curve, and how to overcome the timeline in mastering its basic techniques.
We present our experience in the last four years in the field of endoscopic spine surgeries, starting to overcome the learning curve, expand the indications and manage the complications.
151
P386: Percutaneous pedicle screw fixation in various spinal dissorder with two dimensional fluoroscopy guide: Analysis of accuracy and clinical outcome of 600 screws placement
Farid Yudoyono 1,2
1 Neurosurgery, Universitas Padjadjaran, Faculty of Medicine, Hasan Sadikin Hospital, Bandung, Indonesia
2 Neurosurgery, Neurospine and Pain Center, Bandung, Indonesia
Background: Percutaneous pedicle screw fixation (PPSF), which is a minimally invasive procedure, has now become popular in treating disorders of the spine. This study aimed to evaluate whether two-dimensional (2D) fluoroscopy is effective for PPSF insertion in patients with various spine disorder including degenerative, infection, trauma and tumor. Methods: This study is a retrospective study covering variuos spine disorders that underwent surgery. PPSF was performed in all patients. Several parameters were evaluated for pedicle screw breach, complications, Visual Analog Scale, and Oswestry Disability Index during 6 months of follow-up. Results: A total of 600 screws were percutaneously installed in 2-dimensions anteroposterior and lateral view. Five screw indicated sideways penetration of the pedicle, whereas three screw indicated upward penetration of the pedicle. two screws were attached medially. At the end of the follow-up, there was a significant improvement in pain and disability scales in patients undergoing PPSF. There were no postoperative complications. Conclusions: 2D fluoroscopy-guided percutaneous pedicle screws placement with the appropriate technique is an acceptable and reliable procedure with low rates of screw-related complications and revisions. However, this technique is associated with an initial learning curve and technical that can be gained by tough skills experience.
Keywords: Flouroscopy, minimally invasive procedure, percutaneous pedicle screw, retrospective study
169
P387: Case reports: the effectiveness of fully endoscopic disc surgery in managing low back pain characterized by annular high-intensity zone
Haoju Lo 1
1 Orthopedic Surgery, Da-Chien General Hospital, Miaoli, Taiwan
Introduction: Annular High-Intensity Zone (HIZ) lesions on T2-weighted MRI, characteristic of disc degeneration, represent high signal intensities within the annulus fibrosus of intervertebral discs. Thought to be markers for annular tears in painful discs, they indicate inflammation and neovascularization. However, Teraguchi et al. (2016) observed that their presence doesn't always correlate with symptoms, and they can exist in asymptomatic individuals without annular tears. These lesions are frequent signs of painful internal disc disruption, especially in degenerated discs. With drug therapies offering limited relief for chronic discogenic low back pain linked with HIZ lesions, the focus is shifting to alternatives, like fully endoscopic disc surgery. This minimally invasive surgery, as highlighted by Namboothiri et al. (2018), offers multiple advantages like reduced recovery time, direct visualization, and targeted treatment. We present a case that employed this method for treating HIZ lesions in disc degeneration. Material and Methods: A 45-year-old woman, with persistent low back pain and left-sided radicular leg pain, displayed disc degeneration at L4/L5 on MRI, accentuated by an Annular High-Intensity Zone lesion. We adopted the fully endoscopic disc surgery approach. Starting with an 8-mm incision, a tapered cannulated obturator was positioned in the interlaminar space, facilitating endoscopic navigation. Post laminoplasty with a high-speed drill, the cannula was secured in the interlaminar area, granting access to the affected disc and the HIZ lesion. The surgical goal was to relieve nerve root stimulation, alleviate pain, and support disc recovery through careful disc debridement, inflammatory tissue extraction, and healthy tissue preservation. Results: Postoperative MRI evaluations gauged the efficacy of endoscopic disc surgery on disc degeneration and the annular HIZ lesion's resolution. It was evident that patients experiencing this surgical intervention saw considerable improvement in disc conditions and a resolution of the HIZ lesion. MRI scans highlighted a reduction in the HIZ lesion's size and intensity, underlining the successful treatment of disc degeneration. Moreover, the scans showcased potential disc healing and regeneration post-surgery. Conclusion: Endoscopic surgery for low back pain associated with HIZ has proven beneficial in both treatment and disc regeneration. As the horizon of minimally invasive spine surgery broadens, focus might shift towards refining surgical instruments, improving imaging technology for superior pre and postoperative assessments, and long-term outcome evaluations for endoscopic interventions. Furthermore, to counter the limitations of present treatment options, there's a potential direction towards novel treatments like regenerative medicine to bolster disc healing and regeneration. In summary, fully endoscopic disc surgery emerges as a promising solution for addressing disc degeneration accompanied by annular high-intensity zone lesions.
273
P388: How efficient is percutaneous iliosacral fixation in managing pelvic fractures in Tunisia?
Amal Abayed 1 , Mehdi Bellil 1 , Meriem Souissi 1 , Adnene Benammou 1 , Mondher Kooli 1 , Mohamed Ben Salah 1
1 Orthopedic Surgery, University of Tunis El Manar, Faculty of Medicine of Tunis, Charles Nicolle's Hospital, Tunis, Tunisia
Introduction: Percutaneous sacroiliac fixation has nowadays replaced the conventional treatment of unstable pelvic ring fractures. The objectives of our study were to describe the functional and radiologic outcome of this technique and its main advantages. Material and Methods: A retrospective, descriptive study was conducted in two centers over a period of six years. We included 25 patients with unstable pelvic ring fractures treated with percutaneous sacroiliac screw fixation with a minimum follow-up period of 18 months. Results: The mean age was 40 (sex ratio: 2.57). Circumstances of the accidents were road traffic (64%), fall from height (24%), crush (12%). Mean ISS score was 27. Ninety-six percent of pelvic ring fractures were associated to head trauma (36%), abdominal (40%), spine (40%) et limbs (40%). A transverse process of L5 fracture was present in 28%. Seven patients were admitted in ICU. Fractures were classified 28% Tile B and 72% Tile C. Hemodynamic instability was observed in three cases, urethral trauma in two cases and open wounds in two cases. In seven cases, traction was applied. Patients had surgery within a mean period of eight days (1-21). Percutaneous sacroiliac fixation was bilateral in three cases. An anterior open reduction internal fixation was associated in 92%. Mean operative time was of 40 minutes. Mean blood loss of 0.8 g/dl. Mean length of stay of 13 days (3-21). Weight bearing was authorized within 45 to 75 days. Bone healing was obtained in 92%. Complications were infections (16%), neurological (4%), urogenital (24%), nonunion (8%) and vicious callus (4%). The pubic symphysis diastasis was reduced of 76%, posterior vertical displacement of 96% and deformity index of 60%. Mean Majeed score 93 (45-100): poor (4%), fair (4%), good (24%) and excellent (68%). The physical component of SF-36 was reduced no significantly in comparison with the Tunisian population. Majeed score was correlated with age, work and fracture type, bone healing, reduction of the pubic symphysis diastasis and SF-36 score. Conclusion: Percutaneous sacroiliac fixation is a safe method that allows an anatomical reduction with satisfactory functional results and a major reduction of perioperative morbidity.
284
P389: Clinical outcomes of unilateral approach bi-portal endoscopic decompression in lumbar degenerative central stenosis
Thant Zin Naing 1
1 Spine, Yangon General Hospital, Yangon, Myanmar
Introduction: Conventional surgical procedures for lumbar degenerative diseases are microdiscectomy and laminectomy with foraminotomy respectively. Recently, minimally invasive spinal surgical (MISS) methods have developed to improve preservation of the surrounding normal anatomical structures. Even minimally invasive surgeries including various endoscopic procedures might damage the medial multifidus, which is innervated by the medial branch of the dorsal ramus. The multifidus muscle is very important in its function as a stabilizer of spine and locomotor action. Unilateral approach biportal endoscopic(UBE) surgery through spatium intermusculare with biportal endoscope and small cannula can prevent the erecta spinae from the injury by over distracting procedures Furthermore, variable access angles permit wider and further view of the contralateral side and provide sufficient decompression safely. Material and Methods: Total of 23 patients with degenerative lumbar central canal stenosis were treated using UBE between March 2017 and February 2018. The patients were single level, lumbar central canal stenosis without instability and no previous surgery at the current site, refractory to conservative management for at least 12 weeks. The following clinical parameters were assessed: visual analog scale (VAS) score for leg pain, Oswestry Disability Index (ODI) and modified Macnab criteria, operative time and complications related to the operation. Preoperative and postoperative ODI and VAS at final follow-up were compared. Surgical procedure is similar to a knee arthroscopic surgery. Two portals were used: one portal was used for continuous irrigation and endoscopic viewing and the other portal was used for procedures under general anaesthesia. Two standard entry points were going to be made at 1 cm above and below the disc space on an anteroposterior view. The upper border of the lower lamina is removed for the ipsilateral foraminotomy as needed. Contralateral decompression can be performed at high magnification and with a good endoscopic field of vision. Complete removal of the contralateral ligamentum flavum and sublaminar decompression were performed using shaver, cutting bur and curette. The endoscope was moved to the contralateral side by taking advantage of muscle and skin elasticity rather than adjusting the patient’s position or performing additional skin incisions. Contralateral decompression was performed until the contralateral existing nerve root was identified and decompressed. Results: Mean operation time was 94 minutes (62-113 minutes) and the mean hospital days after surgery was 5.1 days (3-8 days). The mean VAS scores for leg pain preoperatively and at 1 month and 6 month follow-ups were 7.6 ± 1.9, 1.7 ± 1.3 and 1.5 ± 1.1 respectively. The mean ODI result at preoperatively, 1 month and 6 month follow-ups were 67.2 ± 11.3, 24.3 ± 4.5 and 18.1 ± 3.2. The outcome of the procedure was excellent for 11patients and good in 10 patients and fair in 2 patients according the modified Macnab’s criteria,1 cases of cerebrospinal fluid leakage and 1 case of neuropraxia at post surgery. Conclusion: UBE is newly tried technique in MISS for lumbar spine stenosis and certain complications could be expected in an early learning with favorable outcomes.
355
P390: Technical report - Far out syndrome managed with unilateral biportal endoscopy (UBE)
Ashwinkumar Khandge 1
1 Clinical Associate Professor in Orthopedics, Dr D Y Patil Medical College and University Hospital, Pune, India
Introduction: Far-out syndrome is extraforaminal L5 nerve root compression secondary to the formation of a pseudo joint between the L5 transverse process and the sacral ala. The hypertrophied S1 superior articular process (SAP), the transverse process and the ipsilateral sacral ala along with the pseudo joint create a osteo-ligamentous triangle where the L5 nerve root is entrapped extra-foraminal. After a fair trial of conservative management, surgery is indicated following partial relief with L5 selective nerve root blocks. Material and Methods: We present a case of 61-year-old female with left L5 leg pain for 6 months. Conservative management had failed and 2 selective L5 nerve root blocks provided partial relief. Unilateral Biportal endoscopy (UBE) was selected to drill out the hypertrophied pseudo joint, transverse process and the SAP. The landing points and entry points are specific for far-out syndrome. Results: VAS Back and leg pain went down from 5 and 8 preoperatively to 2 and 2 at 6 months follow-up. Macnab criteria reported a good score. Conclusion: UBE is an excellent choice to treat far-out syndrome who have failed conservative management. UBE can avoid need for fusion and extensive surgeries. These patients report excellent to good outcomes at long-term follow-up.
358
P391: Comparison of manual vs. endoscopic foraminoplasty for placement of a large-footprint interbody cage with endoscopic/percutaneous TLIF
Christian Morgenstern 1 , Rudolf Morgenstern 2
1 Centro Médico Teknon, Morgenstern Institute of Spine, Barcelona, Spain
2 Endospine SLU, El Tarter, Canillo, Andorra
Introduction: Endoscopic/percutaneous transforaminal lumbar interbody fusion (TLIF) uses Kambin’s triangle to place an interbody device into the disk. Reported complications include post-operative transient radiculitis due to compression of neural structures in the neuroforamen. To avoid this complication, an extensive foraminoplasty is usually performed either percutaneously with manual reamers and/or with a high-speed burr under direct endoscopic view. Furthermore, small interbody cages specifically designed to fit through the neuroforamen are usually employed. However, large-footprint interbody devices report the best long-term clinical/radiologic outcome. Aim of this study is to evaluate the clinical outcome for manual vs. endoscopic foraminoplasty when placing a large footprint interbody cage with a trans-Kambin TLIF technique. Material and Methods: This is a prospective case-control study. Inclusion criteria comprised degenerative disk disease, foraminal stenosis and spondylolisthesis up to grade II. Exclusion criteria comprised infection, tumor and vertebral body fracture. Surgically, foraminoplasty was performed for one group percutaneously with progressive manual reamers up to 12 mm of diameter (manual group), while an extensive foraminoplasty was performed under direct endoscopic view with a high-speed burr for the endo-group. After disk preparation, a large-footprint expandable titanium interbody cage (size 39x13x15mm; Vertaconnect, Signus GmbH, Germany) was placed in the intervertebral disk through Kambin’s triangle. Demineralized Bone Matrix (DBM) was employed as graft. Posterior fixation was completed with percutaneous transpedicular screws. Visual Analogic Scale (VAS) and Oswestry Disability Index (ODI) scores were evaluated pre-operatively and post-operatively at hospital discharge, as well as 1, 3, 6, 12 and 24 months. Post-operative radiologic control with standing X-ray and CT scan of the lumbar spine was performed at hospital discharge. Statistical analysis was performed with Student’s paired and unpaired T-Test and statistical significance was defined for p < 0.05. Results: 40 patients (20 (50%) female) were included with a mean age 61 ± 11.9 years. A total of 53 cages were placed, including 9 two-level cases and 2 three-level cases. Total mean follow-up was 21.6 ± 3.7 months. The endo group included 16 patients (40%), while the manual group included 24 patients (60%). There were no significant differences in age and sex distribution between both groups. Post-operative VAS back, VAS leg and ODI scores at latest follow-up showed significant improvement (p < 0.01) compared to pre-operative scores for both groups, respectively. There were no significant differences of the pre- and post-operative scores between both groups, respectively. Post-operative complications included 2 cases (12%) of radiculitis for the endo-group, which were significantly less (p < 0.05) than the eight cases (32%) of the manual group that also presented 2 cases (8%) with post-operative motor weakness that partially recovered during follow-up. Mean operative time was significantly (p < 0.05) higher for the endo group with 50 minutes per level compared to the manual group with 26 minutes per level. Conclusion: Endoscopic foraminoplasty is significantly safer (12% radiculitis, no motor weakness) but surgically more demanding and time consuming compared to percutaneous foraminoplasty with manual reamers (25% radiculitis, 8% cases with motor weakness) for trans-Kambin TLIF with a large-footprint interbody cage.
374
P392: My learning curve in biportal endoscopic spine surgery: from observe to perform
Muhamad Aulia Rahman 1 , Harris Istianggoro John 1 , Wawan Mulyawan Wawan 1 , Heri Aminuddin Heri 1 , Ibnu Benhadi Ibben 1
1 Brain and Spine, Bunda Medic, Jakarta, Indonesia
Introduction: Biportal Endoscopic Spine Surgery (BESS) is one of minimal invasive surgery (MIS) that being performed in our hospital since 2021. From 2021 we have done 250 cases of BESS (lumbal and cervical). I have experience in transsphenoidal endoscopic surgery (TSSES) but, not a single spine endoscopic surgery that I ever performed before. Here about to share my learning curve in BESS. Objective: To inform about my learning process of BESS in our hospital as a non endoscopic spine surgeon previously. The cases was taken from February - June 2023. Methods: The learning process compressed of 3 phases: observing phase (OP), assisting phase (AP), and performing phase (PP). The observing step has a goal to understanding the nuances of the BESS. AP has goals to prepare the operating theatre (patient position, draw the projection, electrical device preparation, irrigation preparation, and assisting) and knowing how to control intra operative complication. PP is being supervised from Senior Endoscopic Surgeon to do BESS. Discussion: I have 5 observing phase cases, 10 assisting phase cases, and 20 performing phase cases. The cases varying from lumbar stenosis (LS) and foraminal stenosis (FS), from 1 level to 3 level pathology, with the most common site is L4-5. The approach was done from paramedian (left side and right side), for 2 or 3 levels we choose sliding technique. The left side is undemanding for right handed surgeon like me. In BESS we get fulcrum effect pivoting in skin just like TSSES pivoting in nostril. The dural tear happened in 5 cases (2 during OP, 2 during AP, 1 during PP) and treated conservatively without primary closure. The ultrasonic bone cutter fracture happened in 1 case during PP and taken out by senior supervisor. Bleeding from dorsal rami branch of segmental artery in 2 cases during PP, controlled with bone docking technique combined with ablator coagulation. We didn’t use any kind of drain. Each port has been stitched with 2 interrupted sutures prolene. The duration of surgery per level still above 75 minutes in 20 PP cases. All of the patient doesn’t have any post operative complication such as leaks, infection, or bleeding and discharged in 1-2 day post operatively. Conclusion: The 3 phases of learning BESS combined with mentorship and proctorship from senior endoscopic spine surgeon make the learning curve promising. Intraoperative complication can be handled with direct supervision. Previous TSSES help in the term of instrument handling.
Keywords: biportal endoscopic spine surgery; learning curve; minimal invasive
461
P393: A time-saving and effective technique using SURGICEL packing for controlling bleeding during spinal endoscopy surgery
Chun Tseng 1,2,3 , Se-yi Chen 4,5 , Pang-Hsuan Hsiao 1 , Hsien-Te Chen 1,6 , Chien-Min Chen 7
1 Department of Orthopaedic Surgery
2 Department of Orthopaedic Surgery, China Medical University Beigang Hospital, Yunlin County, Taiwan
3 Graduate Institute of Biomedical Sciences, China Medical University, Taichung City, Taiwan
4 Department of Neurosurgery, Chung-Shan Medical University Hospital, Taichung City, Taiwan,
5 School of Medicine, Chung-Shan Medical University, Taichung, Taiwan
6 Department of Sport Medicine, China Medical University Hospital, Taichung City, Taiwan
7 Division of Neurosurgery, Department of Surgery, Changhua Christian Hospital, Changhua, Taiwan
Introduction: Lumbar canal stenosis (LCS) is characterized by back pain, radiating pain, claudication, and difficulty walking due to the narrowing of the spinal canal, compressing nerve roots and causing neurological symptoms. Surgical intervention, such as minimally invasive microscopic unilateral laminectomy with bilateral decompression (ULBD) and spinal endoscopic decompression surgery, is often necessary as the disease progresses. However, bleeding during surgery increases the risk of nerve injury and prolongs surgical time. The Surgicel™ packing technique, using oxidized cellulose, offers a safe and efficient method to control epidural vein bleeding during spinal endoscopic surgery. Material and Methods: A retrospective study was conducted on central spinal stenosis patients treated with Lumbar Endoscopic Unilateral laminectomy for Bilateral Decompression (LE-ULBD) by an experienced spine endoscopic surgeon in central Taiwan. Patients were divided into a control group (n = 24 patients/36 levels) and a Surgicel™ packing group (n = 16 patients/24 levels). Results: The surgical time was significantly lower in the Surgicel™ packing group (72.58 ± 9.78 minutes) compared to the control group (89.03 ± 11.67 minutes), with a p < 0.005. Additionally, only one patient in the Surgicel™ packing group required hemostatic agents compared to eight patients in the control group, indicating a significant difference (p < 0.005). No complications, including dura tear, new-onset neuralgia, or delayed bleeding, were observed in any of the patients. Conclusion: The Surgicel™ packing technique effectively controlled epidural vein bleeding during endoscopic spinal surgery, reducing surgical time, and the need for additional hemostatic agents, without any complications. This technique represents a valuable option for controlling epidural vein bleeding during spinal endoscopic decompression surgery. Further research is necessary to confirm its safety and efficacy in a larger population and other types of spinal surgeries.
466
P394: Unilateral biportal endoscopy (UBE) in patients with lumbar prolapsed intervertebral disc: early results of a prospective study of 29 patients
Archit Gupta 1 , Mukesh Phalak 1 , Ashwinkumar Khandge 1
1 Orthopaedics, Dr DY Patil Medical College Pimpri Pune, Pune, India
Introduction: Unilateral Biportal endoscopy (UBE) is the most recent advance in spine endoscopy and utilizes an arthroscope and routine spine instruments. This study aims to correlate patient satisfaction based on the Visual Analogue Scale (VAS) for back and leg pain, Oswestry Disability Index, and Macnab criteria, preoperatively and at postoperative day 1, 1 month, 3 months, and 6 months in patients with Acute Lumbar Prolapsed intervertebral disc PIVD) operated using UBE technique. Material and Methods: The inclusion criteria were patients aged 20-70 years old with PIVD at one level not responding to conservative management for at least 6 weeks with pain radiating to the lower extremity. The senior author consecutively performed UBE surgeries for 47 patients PIVD. We included in the study only patients who were followed up for more than six months after surgery. Clinical outcomes were evaluated using modified Macnab criteria, the visual analogue scale (VAS) for legs, and the Oswestry Disability Index (ODI). Results: A total of 47 patients were selected after applying the inclusion and exclusion criteria. 29 patients were followed up for 6 months and their outcomes evaluated. The VAS improved from mean 3 (range 2-5) to 2 (range 1-4) for back pain and 7 (range 4-9) to 2 (range 1-5) for leg pain at 6 months follow-up. While the ODI improved from a mean 44.6 (range 32-68) to 20.2 (range 16-42) at 6 months follow-up. The average satisfied outcome based on the Macnab criteria was excellent to good. Conclusion: A marked early improvement was seen in the perception of pain and symptoms after undergoing UBE surgery in cases of acute PIVD. We need further randomised controlled studies to establish long term efficacy of UBE in PIVD.
632
P395: Minimally invasive screw cement augmentation in pedicle technique (MIS CAPT) for spine fixation in osteoporosis fragility fracture and non-fracture patient : surgical technique, indication and 1-year outcome evaluation
Tayard Buranakarl 1 , Sarush Nimmankiatkul 2 , Patchara Pornsopanakorn 2 , Kanoknard Jaisanuk 1
1 Spine center, Bangkok International Hospital, Bangkok, Thailand
2 BDMS Spine fellowships program 2022, Bangkok Hospital Headquarters, Thailand
Introduction: Spinal fixation in the elderly patients with osteoporosis has been increasingly studied and challenging due to its difficulty and high risk. Using cement augmentation in pedicular screw fixation has been introduced to yield high strength, but the procedure is commonly done in open wound surgery. Nowadays, minimally invasive spine surgery (MIS) using percutaneous pedicle screw fixation along with cement augmentation is limited due to the specialized screws and techniques available. The aim of this study is to describe novo technique of cemented augmentation with percutaneous pedicle screws called “Minimally Invasive Screw Cement Augmentation in Pedicle Technique (MIS CAPT)” which can be used with ordinary percutaneous screws in both fracture and non-fracture osteoporotic fragile bone patients. Material and Methods: A retrospective analysis was conducted on 24 patients of both sexes aged between 50 to 92 years old with osteoporosis and fragile bone who underwent minimally invasive screw cement augmentation in pedicle technique (MIS CAPT) with and without interbody fusion at Bangkok Hospital between December 2015 and June 2022. A total of 190 screws were implanted. Results: Mean ages of patient were over 70 years old. Mean estimated blood loss and the operative time were lower in the fracture group than those of the non-fracture group (107.5 vs. 758.3 ml and 174.7 vs. 405.5 min., respectively). All patients in the fracture group were discharged from intensive care unit within 24 hours, while 25% of the non-fracture were unable. The mean time to start ambulation in the fracture and the non-fracture group was 17.5 and 48.5 hours, respectively. The hospital stay was approximately 7-9 days in both groups. All patients had no postoperative neurological complications or infections. Minor cement leakage (9.4%) was found in the fracture group without any effect on health or outcome. Within 1-year follow-up, no loosening was found in all MIS CAPT screws and in the fracture group, only 2.8° loss of kyphosis reduction was presented in the fracture group. Conclusion: MIS CAPT is an effective-versatile minimally invasive spinal fixation technique in osteoporotic or fragility bone condition. The outcome is excellent in terms of successful operation, minimal complication, and rigid fixation in both fracture and non-fracture elderly fragility bone patients.
Keywords: cement augmentation; fragility fracture; minimally invasive; MIS CAPT; osteoporosis
740
P396: Full-endoscopic assisted surgery for anterior double odontoid screw fixation in the odontoid fracture type II: a clinical study and new surgical technique
Peem Sarasombath 1 , Anuchit Chaiamporn 1 , Sitthikorn Kaensuk 1 , Korapuk Lerswanichwattana 1 , Suthipas Pongmanee 1
1 Department of Orthopaedics, Chiang Mai University, Chiang Mai, Thailand
Introduction: The most common complication of odontoid fracture type II, according to Anderson and D'Alonzo classification, is nonunion. The current standard is offer to surgical treatment. The anterior odontoid screw was a minimally invasive surgery with an effective outcome. Full endoscopically assisted spine surgery is an option for good visualization of the screw entry point. The aim of this study is to present a clinical case study of an acute displaced fracture type II patient following the new double odontoid screw technique with full endoscopic assisted surgery. Material and Methods: A 79-year-old male presented with severe neck pain with ASIA E following a motor vehicle accident. A radiographic study showed a type II odontoid fracture. The patient received urgent surgical intervention by endoscopically assisted double anterior odontoid screw fixation. Results: Intraoperatively, the fracture was reduced and compressed by double anterior odontoid screws without complication. Postoperatively, the radiographic analysis showed the screw was in a good position. The patient's symptoms were completely resolved, and the fracture was in complete union at 1-year follow-up. Conclusion: The anterior odontoid screw technique is a minimally invasive surgery and challenge technique. The full endoscopically assisted surgery is effective and desirable for the anterior double odontoid screw. This new technique could be an option for spine surgeons who deal with odontoid type II fractures.
750
P397: Less is more: a technical case report of biportal endoscopic bilateral L2/3 discectomy using a single sided approach
Walter-Soon-Yaw Wong 1 , Yilun Huang 1
1 Orthopaedic Surgery, Sengkang General Hospital, Singapore
Introduction: Endoscopic surgery for degenerative spinal conditions has been gaining popularity due to its advantages in a smaller incision and lesser tissue damage when compared to the conventional microscopic surgery whilst demonstrating comparable clinical outcomes. Recent studies have demonstrated quicker perioperative recovery at three months with endoscopic surgery. We wish to present a technical case report and surgical approach on a successful case of a unilateral biportal endoscopic L2/L3 discectomy to share our experiences and pearls to flatten the learning curve. Materials and Methods: Mr X, a 54-year-old presented to clinic with a 3-week history of non-resolving lower back pain and left lower limb radiculopathy from posterior thigh to knee after lifting a heavy load. On examination displayed a right L3 (knee extensor) weakness and a left L3 (anterior knee) sensory deficit. An MRI was completed 7 weeks after the initial injury, showing a bilaterally prolapsed L2/3 disc worse in the left than right with narrowing of the respective lateral recesses with impingement onto the bilateral L3 traversing nerves. He endoscopic decompressive surgery following failure of conservative management for > 8 weeks. The surgery was performed through a unilateral biportal approach over the left L2/L3 region. A left partial laminotomy of L2 and L3 was performed. The left L3 traversing nerve root was decompressed through removal of the ligamentum flavum and removal of the left protruded intervertebral disc. The right protruded intervertebral disc was subsequently removed by passing a ball tip probe anteriorly to the spinal cord. Video clips will be presented to demonstrate the crucial steps of the procedure. Results: On post-op day one patient was discharged from hospital with minimal post operative pain. 4 weeks after surgery, patient displayed complete resolution of left radicular pain and improvement in both right knee extensor strength and left anterior knee sensation with all tension signs being negative. A repeat MRI at 4 weeks showed interval resolution of the bilateral prolapsed intervertebral disc. There was a recorded improvement of his visual analogue score (VAS) for his radicular pain from 7 to 0 and lower back pain from 5 to 2 at four weeks post operatively. Conclusion: In this review, we outline a successful case of a unilateral biportal endoscopic approach to a bilateral discectomy of a prolapsed intervertebral disc alongside our steps, techniques as well as common pitfalls and complications from this procedure. In this scenario, most using the conventional microscopic/open surgery would opt for a bilateral approach, however as demonstrated endoscopic surgery does prove highly versatile in furthering minimally invasive surgery. We would suggest that its benefits are certainly worth its learning curve and should be taken into consideration as an alternative to the conventional open and microscopic approach to prolapsed intervertebral discs.
758
P398: Ambulatory endoscopic transforaminal decompression and nucleotomy - feasability and first results
Michael Kraus 1 , Stephanie von dem Berge 2
1 Spine Surgery, Orthix Zentrum, Augsburg, Germany
2 Anaesthesiology, Praxisklinik Augsburg, Augsburg, Germany
Introduction: Endoscopic spine surgery is worldwide on the rise [1]. Due to socio-economic reasons in some countries these surgeries are performed in an outpatient setting. However, in Germany these surgeries still are performed requiring a couple of nights in a hospital. We analysed the first 30 cases of ambulatory endoscopic transforaminal nucleotomy to demonstrate its feasibility. Material and Methods: Prospectively, 30 cases were enrolled. All received a endoscopic transforaminal decompression and nucleotomy and were discharged on the day of surgery. We measured the duration of the procedure, the stay in the facility, the satisfaction of patients and the complication rate. Results: 50 cases were enrolled. The average duration of surgery was 73 minutes (±28, Min 30, Max 150). After surgery, patients were discharged on average after 121 minutes (±43, Min 87, Max 203). No patient was admitted to a hospital. One patient showed a worsening of a preexisting paresis of foot extension, which subsided after two weeks. Three patients showed a prolonged stay in the facility due to postoperative vomitting, none of these was admitted to a hospital. Discussion: In some regions endoscopic techniques are already applied in ambulatory settings [2]. We were able to show that in the German health care systems this is also applicable. The published excellent result of endoscopic procedures [3] is achievable without the necessity of in hospital stay for patients meeting the criteria of ambulatory surgery. In the future, this procedure can safely be performed in this manner and should be further investigated.
References
1. Choi G, Pophale CS et al. Endoscopic Spine Surgery. J Korean Neurosurg Soc 2017 Sep; 60 (5): 485-497.
2. Jian Cao 1, Wenzhou Huang, Tianlong Wu, JingYu Jia, Xigao Cheng. Percutaneous Endoscopic Lumbar Discectomy for Lumbar Disc Herniation as Day Surgery - Short-Term Clinical Results of 235 Consecutive Cases. Medicine (Baltimore) 2019 Dec; 98 (49): e18064.
3. Liu X, Yuan S et al. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results. J Neurosurg Spine 2018 Mar; 28 (3): 317-325.
798
P399: A de facto proctorship description for ideal placement of two cages using navigation-guided biportal endoscopic transforaminal lumbar interbody fusion
Siravich Suvithayasiri 1,2 , Young-Jin Kim 2 , Yanting Liu 2 , Changik Lee 2 , Ashwinkumar Khandge 3 , Jin-Sung Kim 2
1 Department of Orthopedics, Chulabhorn Royal Academy, Bangkok, Thailand
2 Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea
3 Department of Orthopedics, Dr. D. Y. Patil Medical College and Research Centre, Pune, India
Introduction: Endoscopic spine surgery (ESS) has emerged as a pivotal technique within the sphere of minimally invasive spinal surgery. While both the full-endoscopic (FE-TLIF) and unilateral biportal endoscopic (UBE-TLIF) methods have been reported, concerns linger regarding the limited corridor for cage insertion and potential long-term complications. This study showcases a novel CT-navigation-guided UBE-TLIF technique employing dual cages in a convergence pattern. Material and Methods: After obtaining approval from the Institutional Review Board, a retrospective analysis was conducted on a 59-year-old female presenting with osteoporosis and symptomatic grade I degenerative spondylolisthesis at the L4-L5 level. The patient underwent a right-sided UBE-TLIF procedure with unilateral laminectomy for bilateral decompression, guided by an intraoperative CT navigation system. Results: Postoperative findings displayed rapid pain alleviation, with the visual analog scale rating plummeting to 3 by the third day. Three months post-operation, the patient exhibited no back or leg discomfort and could engage in continuous walking sessions lasting over 30 minutes. Plain radiographs showcased the repositioning of the L4 vertebra and restoration of the L4-L5 intervertebral disc height. This procedure's success underscores the potential advantages of using dual cages, offering a more balanced distribution of load on the endplate and potentially reducing complications like cage subsidence or migration. Conclusion: The newly introduced CT-navigation-assisted UBE-TLIF with a convergent dual cage insertion offers a promising approach for lumbar interbody fusion procedures. This method not only enhances anatomical visualization for surgeons but may also decrease complications associated with traditional single-cage techniques. The integration of intraoperative CT navigation further bolsters its potential by minimizing radiation exposure and maximizing patient safety.
801
P400: The adoption of endoscopic spine surgery as a palliative decompression surgery in spinal metastases
Siravich Suvithayasiri1,2, Young-Jin Kim2, Yanting Liu2, Khanathip Jitpakdee3, Kandarpkumar Patel2, Jin-Sung Kim2
1 Department of Orthopedics, Chulabhorn Royal Academy, Bangkok, Thailand
2 Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea
3 Department of Orthopedics, Queen Savang Vadhana Memorial Hospital, Chonburi, Thailand
Introduction: Spinal metastasis is an increasing concern in cancer patients. The primary focus in managing such patients is on palliating symptoms and enhancing quality of life. Traditional surgery, although effective, poses several complications. Recent advancements in Minimally Invasive Spine Surgery (MISS) and, specifically, endoscopic spine surgery offer promising results with fewer complications. However, its use in spinal metastasis remains scarcely documented. This study aims to fill this knowledge gap. Material and Methods: This was a retrospective single-center case series. We reviewed spinal metastasis patients who underwent MISS between 2012-2022 in our university hospital. Data collected included demographic details, radiographic findings, baseline scores like Spinal Instability Neoplastic Score (SINS) and Metastatic Epidural Spinal Cord Compression (MESCC) Grade, and quality of life measures. Our methodology also entailed detailed surgical intervention procedures. Statistical analyses were performed, and the PROCESS guideline was followed. Results: We identified seven patients (median age: 64 years) who underwent endoscopic decompression surgery. The majority had hematologic primary tumors (57.14%). Thirteen metastatic vertebrae were identified, with most located in the thoracolumbar region. Significant improvements were seen in Pain NRS scores postoperatively. In terms of complications, one patient showed tumor recurrence, and another had hematoma post-surgery. Both patients, however, showed symptom resolution post-revision surgery. Conclusion: Endoscopic spine surgery, despite being relatively new, offers a promising option for patients with spinal metastasis. With its potential to reduce complications, speed up recovery, and overall provide an enhanced quality of life, it may soon become the preferred surgical intervention for these selected patients. Further research, preferably with larger sample sizes and multicenter collaborations, is warranted.
843
P401: A superior alternative? Unilateral biportal endoscopic spine surgery in revision lumbar spine decompression
Walter-Soon-Yaw Wong 1 , Yilun Huang 1
1 Orthopaedic Surgery, Sengkang General Hospital, Singapore
Background: Endoscopic approaches to degenerative spinal conditions have gained popularity due to their potential for reducing blood loss, preserving paraspinal muscles, and enabling quicker post-operative recovery compared to microsurgery and open surgery. One area that has garnered increasing interest is the application of endoscopy for diagnostic and therapeutic purposes in patients requiring surgical revision following previous lumbar decompression surgery. Studies have indicated a high incidence of lumbar dural tears during revision operations, ranging from 2.1% to 15.9%. This is largely attributed to the challenge of visualizing and distinguishing scar tissue from healthy tissues that should be protected. With the improved visibility provided by endoscopic spine surgery, thanks to positive water pressure facilitating tissue plane separation and higher magnification, endoscopy emerges as a highly viable alternative compared to traditional open and microscopic surgery. This technical note outlines the approach, technique, pearls and pitfalls associated with using unilateral biportal endoscopy in revision lumbar spine decompression. Method: Patients are first evaluated with clinical examination and routine imaging, including anteroposterior and lateral radiographs, as well as magnetic resonance imaging (MRI) of the lumbar spine to precisely localize the lesion. As part of pre-operative planning, the lesion is superimposed onto pre-operative radiographs to facilitate intra-operative localization. Patients are positioned prone on a radiolucent table with flexed knees and hips, while the operating surgeon stands on the ipsilateral side of the lesion. Two longitudinal incisions are made under fluoroscopic guidance to confirm the endoscope's trajectory. The procedure begins with blunt dissection down to the bony landmarks. Subsequently, a diagnostic spine endoscopy is performed at the previous surgical site, followed by decompression. Key procedural considerations include:
1. When encountering difficulties in visualizing tissue planes between scar tissue and healthy tissue, bringing the endoscope closer to the operating field can allow positive water pressure to separate tissue planes.
2. Confirming the extent of decompression by comparing intra-operative radiographs with pre-operative planning.
3. Ensuring meticulous hemostasis using techniques such as radiofrequency ablation or bone wax to maintain clear visibility.
4. If scar or flavum tissue adheres too tightly to the dura sac, to consider decompressing them en masse to allow for combined free-floating without the risk of dural tears.
5. Having human thrombin and fibrinogen sponge sealant on standby in case of a dural tear.
Conclusion: Endoscopy in revision spine surgery offers two critical advantages: magnification and positive water pressure, enhancing tissue plane visualization and differentiation. Based on our experience, these benefits are highly valuable for defining tissue planes and identifying tissue types, both of which are paramount in revision spine surgery. However, utilising endoscopy particularly in cases without conventional visual landmarks requires overcoming a steep learning curve which we hope this technical can reduce.
892
P402: Learning curve of lumbar endoscopic unilateral laminotomy for bilateral decompression(LE-ULBD): single surgeon's experience of successful transition from interlaminar endoscopic lumbar discectomy
Jungwoo Hur 1 , Jae-Taek Hong 1
1 Neurosurgery, Eunpyeong St. Mary's Hospital, The Catholic University of Korea, Seoul, South Korea
Introduction: Lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD) is a minimally invasive surgical technique to treat degenerative lumbar stenosis in the spinal canal and lateral recess using uniportal endoscope and interlaminar approach. However, endoscopic spine surgery is usually associated with a steep learning curve and high complication rates, and much time and experience are needed before surgeons become familiar with the technique. The purpose of this study is to define and analyze the learning curve for LE-ULBD with a single spine surgeon’s experience based on intra- and perioperative parameters. This study is retrospective analysis of single surgeon’s consecutive case series in a single institution and experience of successful transition from interlaminar endoscopic lumbar discectomy. Material and Methods: Ninety-seven consecutive patients with single or multi-level degenerative lumbar canal stenosis and lateral recess stenosis who were treated by LE-ULBD were included in the study. Surgeries were performed using standard LE-ULBD technique using interlaminar approach with a uniportal endoscope, and out-and-in unilateral and contralateral decompression using an over-the-top maneuver by a single surgeon. Corrected operative time per level, operative blood loss, postoperative drainage, transfusion rate, and ambulation recovery time were measured. Intraoperative and postoperative complication incidences were also identified. Clinical results were assessed using the visual analogue scale (VAS). The learning curve was assessed using a logarithmic curve-fit regression analysis. In the single-level LE-ULBD, patients were stratified into “early” group (among the first 50 cases of the series, n = 30) and “late” group (n = 23), depending on their case number. After the 50th case, the procedural time reached a plateau and subsequent patients were assigned to the second group for comparison. Results: Corrected operative time gradually decreased as the series progressed, and an asymptote was reached after about 30 cases. Average VAS scores for lower back pain and radiating pain also significantly decreased from an average of 6.9 to 3.8 and 7.6 to 2.5, respectively. In the single-level LE-ULBD series, operative time was significantly shorter in the late group (99 ± 54 min) than the early group (141 ± 21 min), and blood loss during the operation was significantly reduced in the late group (182 ± 69 mL) compared with the early group (142 ± 57 mL). The length of hospitalization, postoperative improvement in VAS and ODI, and reoperation rates were not different between the groups. In both groups, stenotic spinal canals were effectively decompressed. There were two cases of inadequate decompression in the early group requiring revision surgeries. Conclusion: The LE-ULBD is a technically difficult procedure to the practicing spine surgeon with regard to small working view and time-consuming decompression procedure. Although it is not easy to master this minimally invasive technique, operative time and blood loss improved with the surgeon’s experience. After the initial learning curve, this technique could be a safe, clinically-feasible, and effective option for the surgical treatment of lumbar degenerative stenosis. Further studies are warranted to delineate the methods to minimize the complications associated with the learning curve.
919
P403: Minimally invasive spine (MIS) fixation without decompression for High grade (A4) thoraco lumber spine injury without neurological involvement: our experience
Biswaranjan Nayak 1
1 Neurosurgery, Kalinga Hospital Limited, Bhubaneswar, India
Objective: Traumatic thoracolumbar fractures are common, and surgical fixation is a well-established treatment option, with the aim to achieve spinal stability and preserve neurological function. Pedicle screw fixation using a minimally invasive spine (MIS) surgical approach has emerged as an alternative approach for the treatment of thoracolumbar fractures. The aim of this study is to collect data regarding epidemiology, management, and outcomes of patients treated with MIS pedicle screw fixation for traumatic thoracolumbar fractures in our neurosurgical department. Materials and Methods: This was a prospective study including all patients who underwent MIS fixation from June 2021- june2023 for high grade (A4) thoraco lumber spine injury without neurological involvement. Results: A total of 45 patients were included, 31 males and 14 females; the mean age was 59 years. The majority of injuries were from falls. In 28 cases, the fracture involved a thoracic vertebra and in 17 cases a lumbar vertebra. The average length of hospital stay was 4-5 days. MIS fixation achieved a satisfactory regional sagittal angle (RSA) postoperatively in all patients. The vast majority of patients had no or mild postoperative pain and achieved a good functional outcome. Conclusions: MIS fixation is a safe surgical option with comparable outcomes to open surgery and a potential reduction in perioperative morbidity. MIS surgery achieves a rapid and significant improvement in pain score, functional outcome, Frankel Grade, and RSA. We expect that MIS fixation will become the predominant technique in the management of traumatic thoracolumbar fractures.
942
P404: First experiences with endoscopic cervical foraminotomy in comparison to foraminotomy as described by Frykholm
Bastian Stemmer 1 , Tülü Selma 2 , Ertl Sebastian 1 , Ehab Shiban 1
1 Department of Neurosurgery, UK Augsburg, Augsburg
2 Department of Neurosurgery, Uniklinik Salzburg, Salzburg, Austria
Introduction: Although the endoscopic posterior cervical foraminotomy might be a less traumatic alternative to the classic posterior foraminotomy as described by Frykholm, there is limited data regarding its safety and outcome. Methods: In a retrospective case series, we compared outcome parameters including pain relief, volume of blood loss, duration of surgery, rate of complications and length of stay between the two surgical approaches. Results: Between 2017 and 2022 thirteen patients underwent posterior cervical foraminotomy at our department by either open foraminotomy as described by Frykholm (n = 4) or by an endoscopic approach (n = 9). Blood loss was lower (< 50ml vs. 320 ml) and the length of stay (1.9 days vs. 6.5 days) and duration of surgery (77 minutes vs. 104 minutes) were shorter in patients who were operated endoscopically as compared to patients who received an open posterior foraminotomy. Pain relief (drop in VAS) was comparable among the groups (5.24 vs 4). The only complication in the endoscopic group was a dural tear, while one patient of the open foraminotomy group developed a temporary C5 palsy. Conclusion: In this small case series the endoscopic cervical foraminotomy showed to be a feasible and safe approach with a comparable pain relief, less blood loss and shorter hospital stays. These data need to be verified in larger randomised prospective trials.
962
P405: Laminoplasty does not impact improvement in arm pain or space available for the spinal cord
Robert Merrill 1 , Tejas Subramanian 1 , Tomoyuki Asada 1 , Sumedha Singh 1 , Amy Lu 1 , Maximillian Korsun 1 , Omri Maayan 1 , Izzet Akosman 1 , Sravisht Iyer 1 , Francis Lovecchio 1 , Han Jo Kim 1
1 Hospital for Special Surgery, New York, USA
Introduction: Laminoplasty treats cervical myelopathy while preserving range of motion in the cervical spine. Some evidence suggests that laminoplasty alone may also be effective in treating radicular arm pain. One specific laminoplasty technique is open door laminoplasty, in which a single side of the lamina serves as a hinge, and the other side is completely opened. The objective was to determine if side of opening the laminoplasty effects arm pain or superior decompression. Material and Methods: We conducted a retrospective review of adult patients who underwent unilateral open door laminoplasty cervical myelopathy. The side opened was dependent on surgeon discretion. We recorded preoperative side of symptoms, side of radiographic compression, arm pains scores, and canal diameter. Patients with open side ipsilateral or contralateral to dominant symptoms or compression were compared to determine any effect on arm pain outcomes or spinal canal diameter. If the symptoms were equal bilaterally, patients were neutral. Results: A total of 167 patients were included in the study with an average age of 64 ± 11 years and average follow-up time of 64.5 ± 72 weeks. The average preoperative arm pain visual analog score (VAS) was 2.13 ± 2.86, and the average arm VAS after 6 months was 1.52 ± 2.68. For dominant symptoms, the ipsilateral, contralateral, and neutral groups had a significant improvement in arm VAS at > 6 months postoperatively. For dominant compression, the ipsilateral and contralateral groups had a significant improvement in both arm VAS and canal diameter at > 6 months postoperatively. No differences were seen between groups for either. We observed a significant correlation between size of plate and change in canal diameter, however no differences were noted in arm pain. Conclusion: Laminoplasty may be effective in addressing radicular arm pain by increasing spinal canal diameter and space available for the cord. The laterality of opening the laminoplasty did not affect arm pain improvement or canal expansion.
983
P406: Simultaneous single position oblique lumbar interbody fusion and robot-assisted pedicle screw placement: technique, early outcome, and lessons learned
Leo Shaw 1 , Han-Ting Shih 1 , Kao-Chang Tu 1 , Cheng-Hung Lee 1 , Chien-Chou Pan 1 , Kun-Hui Chen 1
1 Taichung Veterans General Hospital, Taichung, Taiwan
Introduction: The objective of this study is to evaluate the safety and short-term outcomes of simultaneous single-position oblique lumbar interbody fusion (OLIF) with robot-assisted posterior instrumentation. Additionally, the article provides insights into essential surgical technique considerations for the procedure. Material and Methods: In this retrospective study, we analyzed a cohort of 25 patients who underwent single-position oblique lumbar interbody fusion (OLIF) with robot-assisted posterior instrumentation. Post-operatively, the patients were followed for a minimum of one month. Results: The average operative time for the procedure was 184 ± 35 minutes, with an average blood loss of 85 ± 17 cc's, and an average length of stay of 4.4 ± 0.75 days. Notably, no intraoperative complications, readmissions, or revision surgeries occurred, and there were no instances of hardware malposition. Remarkably, significant improvement in pain and Oswestry Disability Index (ODI) scores was observed during the postoperative first-month follow-up. Conclusion: The study demonstrates the safety and short-term clinical efficacy of simultaneous single-position oblique lumbar interbody fusion (OLIF) with robot-assisted posterior instrumentation. Crucially, adherence to specific surgical technique considerations is imperative to ensure an optimal surgical workflow and achieve predictable outcomes.
1136
P407: Where is the location of the highest radiation exposure in the operating room during surgery using a 3D C-arm? Effect of patient obesity on occupational exposure
Nodoka Manabe 1 , Daisuke Tsunoda 1 , Sho Ishiwata 2 , Kunio Kamatani 1 , Kazuro Tsuge 1
1 Department of Orthopaedic Surgery, East Maebashi Orthopaedic Hospital, Maebashi, Gunma, Japan
2 Department of Orthopaedic Surgery, Iwai Orthopaedic Hospital, Tokyo, Japan
Study Design: A prospective clinical study. Objective: The purpose of this study was to examine where in the operating room radiation exposure increases during spine surgery, and to investigate the influence of the patient's obesity on occupational exposure. Materials: This study included 62 male and 54 female patients with lumbar spinal canal stenosis, lumbar degenerative spondylolisthesis, and degenerative scoliosis, undergoing lumbar surgery using 3D C-arm and navigation system that could do the minimally invasive surgery. The average age was 61 years (range: 48-78 years). Methods: To measure radiation dose, the electronic pocket dosimeter were placed at the surgeon, on the anesthesia machine; anesthesiologist, in front of the C-arm, behind the C-arm; radiologist, and at the entrance to the operating room. The Operating time, Blood loss, and Fluoroscopy time were measured. The KAP: Kerma-area product (Gycm2) and CAK; Cumulative Air Kerma (mGy) were measured as indexes of patient radiation exposure. Results: There was a positive correlation (p < 0.05) between operating & fluoroscopy time and dose of radiation exposure. The body weight & BMI was also affecting the dose of radiation occupational exposure. Discussion and Conclusion: It is important to examine the safety zones in the operating room from radiation exposure during the surgery. The surgeon should use the C-arm considering the direction of scattered radiation. Obesity can be a major risk for general anesthesia, but it also carries the risk of increased occupational exposure.
1231
P408: Percutaneous arthrodesis as surgical management of thoracolumbar fractures: case series in a health center in Dominican Republic
Miguel Venegas Cruz 1 , Shantalle Diaz Cruz 2
1 Department of Neurosurgery, Corominas Clinic, Santiago
2 School of Medicine, Pontificia Universidad Católica Madre y Maestra, Santiago
Introduction: The advent of technological advances in the field of imaging, as well as the greater understanding of axial biomechanics and its implications has greatly impacted the field of neurosurgery and the therapeutic options available for thoracolumbar fractures, which, being the most common within vertebral fractures, have undergone important changes around surgical treatment, advocating for less invasive options whenever possible. It is well known that the novel techniques of percutaneous fusion in thoracolumbar fractures confer less tissue transgression, blood loss, risk of infection, greater preservation of the paraspinal musculature and therefore, less postoperative pain and less perilesional scar tissue that could eventually lead to long-term low back pain. Despite the above, the option of surgical treatment of fractures of the T10-L2 region should be supported by the type of injury, neurological involvement, stability of the fracture, and expertise of the surgeon. The following description will be the clinical history, surgical management, and evolution of two men aged 20 and 44 years with a diagnosis of thoracolumbar fracture due to a high impact motor vehicle accident, plus data on lumbar instability, with the first two percutaneous fusion procedures at regional level, taking place in a health center in the Dominican Republic. In addition, a review of the current literature available on the topic in question will be conducted. Material and Methods: Through a retrospective descriptive study carried out during the period August-December 2022, the clinical history, surgical management and post-procedure evolution of two men aged 20 and 44 years with a diagnosis of thoracolumbar fracture due to a high impact motor vehicle accident and consequent lumbar instability, with percutaneous thoracolumbar fusion of segments T10-L2, was studied; being these the first two minimally invasive spine surgeries of this type in patients with high complexity fractures at the regional level in a developing country. Results: In the two patients studied in this research, a surgical time of 5 and 4.5 hours, respectively, was observed. Regarding the hospital stay, the 44-year-old patient had an admission of 3 days, while the 20-year-old patient was admitted for 4 days for internal medicine follow-up and metabolic control. Regarding postoperative pain, both patients reported significant improvement in their clinical picture, with an analogous visual scale of 4/10 and 5/10, respectively, tolerating early ambulation. Only one of the cases experienced an episode of rhabdomyolysis with mild myalgias, which satisfactorily yielded to pharmacological treatment within the course of one day. Nearly 12 months after each procedure, the patients exhibit excellent tolerance of activities of daily living, including occupational related actions like construction working and motorcycle riding, respectively. Conclusion: Among the posterior vertebral fixation options currently available, the importance of the percutaneous screw placement technique with respect to the conventional open and open paraspinal technique, stands out, as it means a shorter hospital stay, less muscle retraction and ischemia, improvement in the visual analog scale of pain, and reproducible results around the reduction of the Cobb angle in the long term.
1249
P409: Interlaminar endoscopic lumbar discectomy versus microscopic lumbar discectomy: a preliminary analysis of L5-S1 lumbar disc herniation outcomes in prospective randomized controlled trials
Yanting Liu 1 , Siravich Suvithayasiri 1,2 , Khanathip Jitpakdee 1,3 , Jin-Sung Kim 1
1 Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea, Seoul
2 Department of Orthopedics, Chulabhorn Hospital, Chulabhorn Royal Academy, Bangkok, Thailand
3 Department of Orthopedics, Thai Red Cross Society, Queen Savang Vadhana Memorial Hospital, Sriracha, Thailand
Introduction: Lumbar disc herniation (LDH) at the L5-S1 level is a prevalent issue, often leading to severe lower back pain and sciatica. As this level bears significant mechanical load, it is commonly implicated in LDH, making surgical intervention necessary when conservative treatments fail. Recently, minimally invasive surgical techniques (MIS) like Interlaminar Endoscopic Lumbar Discectomy (IELD) and Microscopic Lumbar Discectomy (MLD) have gained traction for their benefits in quicker recovery and reduced tissue damage. However, there's a lack of robust, comparative data on the safety and efficacy of IELD vs. MLD at the L5-S1 level. Our study aims to fill this gap by presenting the first preliminary randomized controlled trial (RCT) results comparing these methods, focusing on clinical outcomes, complications, and patient satisfaction. Material and Methods: This study is designed as a prospective, single-center, non-inferiority RCT. Ethical approval and registration were granted by our Institutional Review Board (IRB No. KC15OISI0665). Inclusion criteria targeted individuals above 18 years suffering from symptomatic radiculopathy with L5-S1 LDH, as confirmed through magnetic resonance imaging (MRI). A robust computer-generated randomization sequence was employed to allocate patients either to the IELD or MLD groups. Blinded allocation was maintained by a trained clinical research coordinator, not involved in patient care, using sequentially numbered, opaque, sealed envelopes. These measures aimed to curtail selection bias. Surgeons remained unaware of group assignments until the day before surgery to maintain the blinding process. All surgical procedures were conducted by a single senior spine surgeon experienced in both techniques. Primary outcomes were measured through Visual Analogue Scale (VAS) scores for pain and Oswestry Disability Index (ODI) scores for disability. Secondary outcomes encompassed patient satisfaction, walking endurance, and radiologic measures like disc height and lumbar lordosis. Data collection was rigorously controlled, with independent assessors involved in both preoperative evaluations and postoperative follow-ups. Statistical analyses were conducted using STATA/MP 17, adhering to intention-to-treat principles. A one-sided P-value of less than 0.05 was predetermined as the threshold for statistical significance in non-inferiority tests. Results: Of 37 assessed patients, both IELD and MLD groups demonstrated significant improvements in VAS scores for pain over time, with no significant difference between them. For secondary outcomes, the IELD group had a shorter hospital stay and reduced blood loss but a longer operation time than the MLD group. Radiographic evaluations showed no change compared to preoperative data. Patient satisfaction and recovery rates were slightly higher for the MLD group, but both groups were comparable in most evaluations, with complications being minimal. Conclusion: The IELD was non-inferior in improving the intensity of back and leg pain and functional disability, compared to the MLD. Additionally, the IELD showed no difference in clinical outcomes for patients in terms of radiographic results and patient satisfaction rates. The results of this research preliminarily demonstrate that the IELD could be considered an effective alternative to MLD for L5-S1 central or paracentral LDH.
1312
P410: One decade of XLIF for spinal deformity: have the advances in minimally invasive surgery improved the results in degenerative scoliosis?
Pablo Jover Carbonell 1 , Miguel Sanfeliu Giner 1 , Pablo Badia Ferrado 1
1 Spine Unit, Hospital General y Universitario de Valencia, València
Introduction: During the last fifteen years, several minimally invasive techniques in spine surgery have been developed. These techniques and new surgical instruments can yield comparable results to open surgery and can lead to a reduction of the complications in adult degenerative scoliosis. Material and Methods: We performed a retrospective observational study. Our case serie has 58 patients treated with XLIF and posterior instrumentation for degenerative scoliosis between January 2013 and January 2022. The sample was divided into two groups: those treated on during the first 4 years of using the technique in our institution (Group A) and those treated on during the subsequent 4 years (Group B). In addition to the temporal criteria, the mean difference between groups was that in Group B proximal level cementation, expandable metal tulip heads, and titanium cages were used. Clinical variables (age, surgical time, etc.), radiological parameters (such as Cobb angle, sagittal balance and Bridwell fusion scale) as well as the outcomes with scales such as VAS (Visual Analog Scale) and Oswestry Disability Index, were collected. Results: The mean age was 65 years, and 2.6 levels of lumbar interbody cages were placed on average using XLIF, along with posterior instrumentation in all cases. The mean clinical-radiological follow up was 39,7 months for group A and 28.8 months for group B. The overall fusion rate was 83% (82% for Group A and 84% for Group B). The mean preoperative and postoperative Cobb angles were 46° and 21° in Group A, and 47° and 12° in Group B, with this difference being significant (p < 0.05). Lumbar lordosis, coronal and sagittal balance showed variations but without significant differences between groups (p > 0.05). The mean postoperative VAS score decreased by 4.9 points overall (Group A: 9.1 to 4.4 (p < 0.05) and Group B: 8.1 to 3.7 (p < 0.05)) and 81.3% of patients exhibited minimal to moderate disability one year after the intervention according to the Oswestry Disability Index, being similar this clinical outcome in both groups and showing a clear clinical improvement. In the first two postoperative years, a 44% complication rate was recorded in Group A compared to 31% in Group B. Conclusion: XLIF combined with posterior instrumentation improves both radiographic parameters and clinical outcomes in degenerative scoliosis. Performing this technique with specialized teams, along with the implementation of elements such as proximal level cementation, the use of expandable metal tulips, and the introduction of titanium cages, enhances outcomes and reduces complications.
1474
P411: Minimally invasive spine surgery for intradural pathology
Chandan Mohanty 1 , Chandrashekhar Deopujari 2
1 Neurosurgery, Bombay Hospital & Wadia Children's Hospital, Mumbai, India
2 Neurosurgery, Bombay Hospital, Mumbai, India
Introduction: Minimally invasive spine surgery (MISS) is being recognized as a treatment option in the treatment of intradural tumours by minimizing access-related morbidity from a conventional open approach. Material and Methods: We retrospectively analysed all the intradural lesions treated with the MISS approach. The clinical, radiological, and surgical techniques and the outcomes were analysed in detail. Results: A total of 26 intradural lesions were treated with the MISS approach. Out of these, 20 were intradural extramedullary tumours, 4 cases of fatty filum, and 2 cases of spontaneous subdural bleed were identified. The patient's age ranged from 28 years to 64 years. All these cases were successfully treated with an excellent outcome. No surgical complications like CSF leak, worsening of neurological deficit, incomplete tumour removal, or wound infection were noted. Patients with preoperative neurological deficits made at least 1 grade improvement as per the McCormick scale with the majority 91.7% (22/24) showing complete neurological recovery at the time of follow-up. Conclusion: The MISS approach can be safely used in carefully selected cases of intradural tumours as well as other non-tumour intradural pathology. There were no surgical complications or access-related difficulties in this series.
1492
P412: Posterior oblique technique for minimally invasive sacroiliac joint fusion
Javier Grajeda 1 , Mario Cahueque 2
1 Faculty of Medicine, Universidad Francisco Marroquín, Guatemala City, Guatemala
2 Orthopedic Surgery, Hospital Centro Médico, Guatemala City, Guatemala
Introduction: With the advent of minimally invasive surgical (MIS) techniques, several approaches for sacroiliac joint (SIJ) fusion have emerged. The lateral technique is the most widely accepted and studied approach, while the posterior and posterior oblique techniques remain less explored. Given the lack of comprehensive reports on the latter, this technical note aims to detail the preoperative evaluation, surgical procedure and technical considerations, and postoperative management for the posterior oblique fusion of the SIJ. Material and Methods: Data from 23 surgeries employing the posterior oblique technique from January 2020 to December 2022 were iteratively reviewed. This information, combined with a comprehensive review of previous technical and anatomic descriptions of MIS techniques for SIJ fusion, led to the development and standardization of a detailed procedural protocol. Results: A preoperative guideline was formulated based on clinical diagnosis, surgical indications, and preoperative imaging, the latter allowing for personalization of the trajectory and device size to each patient's anatomy. The surgical procedure and technical considerations were thoroughly outlined. In particular, our findings indicate the need to adjust the bone needle insertion angle, suggesting 20° to 40° to maintain obliquity, a significant deviation from the traditionally recommended 5° to 20°. Necessary fluoroscopic views during the procedure were defined, requiring only the use of outlet oblique and inlet view, leaving the lateral view as optional. A postoperative guideline was established for both pain management and return to activity, which was noteworthy for patients walking on the same day of surgery due to the outpatient nature of the procedure. A technical and anatomical comparison with previous descriptions of the techniques was performed. In particular, the posterior oblique technique offers a direct route to the SIJ through the ilium, starting from the upper outer surface of the iliac crest, without dissecting the gluteal fascia or SIJ ligaments, and decreasing the risk of damaging neurovascular structures, unlike the other techniques. Conclusion: The posterior oblique approach is a safe and effective minimally invasive technique for sacroiliac joint fusion. It represents a less invasive alternative that focuses on patient-specific anatomy and considerations. The standardized guideline ensures consistent reproducibility of the procedure.
1495
P413: Preoperative planning with CT scans optimizes the posterior oblique for minimally invasive sacroiliac joint fusion
Javier Grajeda 1 , Mario Cahueque 2
1 Faculty of Medicine, Universidad Francisco Marroquín, Guatemala City, Guatemala
2 Orthopedic Surgery, Hospital Centro Médico, Guatemala City, Guatemala
Introduction: Management of low back pain (LBP) originating from the sacroiliac joint (SIJ) via fusion is challenging, especially given the importance of anatomical variations of the SIJ. Evidence suggests that anatomic variations of the joint must be considered when planning a fusion procedure. While various minimally invasive surgical (MIS) techniques have been described for this procedure, the evidence for tailoring the procedure to each patient's individual anatomy remains limited to the traditional lateral approach, leaving the remaining techniques - posterior and posterior oblique - underexplored in this area. The posterior oblique technique, while effective, lacks guidance for individual anatomical adaptation. This technical note highlights the value of preoperative CT imaging for posterior oblique SIJ fusion and introduces the “Iliac-Angle Rule” for patient-specific surgical planning. Material and Methods: Preoperative CT images of five subjects who underwent the posterior oblique procedure were analyzed, focusing on both the coronal and axial planes of the SIJ. This analysis, combined with a review of previous descriptions of the technique and an understanding of the anatomical variations of the SIJ, was designed to refine preoperative planning for the posterior oblique procedure. Results: Using CT-based preoperative planning, the “Iliac-Angle Rule” has been proposed. It posits that the proximity of the iliac crests in the axial plane directly correlates with the angle of insertion from the midline, allowing for a tailored trajectory for both needle and screw insertion. This approach challenges the accepted fixed range of insertion angles and emphasizes the need for individualized surgical planning. Correct determination of the screw size is an added benefit of the evaluation. Our findings also underscore the importance of recognizing SIJ anatomic variations, as they have been shown to affect fusion outcomes. Conclusion: The integration of preoperative CT imaging and the “Iliac-Angle Rule” offers a new approach to posterior oblique SIJ fusion that promotes an individualized surgical plan. By recognizing and accommodating SIJ anatomic variations, this tailored approach has the potential to improve surgical outcomes by increasing the precision of implant positioning.
1497
P414: Pyogenic sacroiliitis managed by minimally invasive posterior oblique sacroiliac joint fusion: a case report
Javier Grajeda 1 , Mario Cahueque 2
1 Faculty of Medicine, Universidad Francisco Marroquín, Guatemala City, Guatemala
2 Orthopedic Surgery, Hospital Centro Médico, Guatemala City, Guatemala
Introduction: Pyogenic sacroiliitis, an infection of the sacroiliac joint (SIJ), is a rare condition with a low incidence of 1% to 2%. Management is complex and can be exacerbated by the often-delayed diagnosis due to the non-specific nature of its symptoms. While antibiotic therapy remains the standard of care for pyogenic sacroiliitis, surgical intervention may be required for cases unresponsive to conservative treatment or those presenting with complications. Both open debridement and joint fusion are established procedures with proven efficacy. In particular, the evidence for the management of various cases of pyogenic sacroiliitis using minimally invasive SIJ fusion has focused primarily on the lateral and posterior techniques, leaving the remaining posterior oblique approach underexplored for this setting. Therefore, the purpose of this report is to present a case of pyogenic sacroiliitis treated with minimally invasive posterior oblique SIJ fusion. Material and Methods: We present a case of a 42-year-old man with severe low back pain and walking difficulty. His clinical history and physical examination led to the performance of MRI imaging of both pelvic and lumbar areas, in addition to blood tests. Pelvic MRI revealed increased T2 signal intensity over the right sacroiliac joint, along with a joint effusion extending below the iliopsoas muscle. Blood tests were consistent with an active infection. Based on the imaging and laboratory findings, septic arthritis of the SIJ was suspected. Drainage and biopsy of the SIJ were ordered and confirmed the diagnosis of pyogenic sacroiliitis due to Staphylococcus aureus. Despite a 12-week course of vancomycin, only marginal symptom relief was achieved. Given the patient's medical history and ongoing chronic low back pain with joint instability, the decision was made to perform sacroiliac fusion using the minimally invasive posterior oblique technique. Results: The procedure was performed without complications and the patient was discharged the same day after the procedure. At the 6-week follow-up consultation, the patient reported significant improvement in pain and functionality, with no walking difficulties observed or reported. At the 1-year follow-up, the patient reported a complete resolution of pain. Conclusion: The posterior oblique technique is a potentially effective way to treat cases of pyogenic sacroiliitis that don't respond adequately to conservative management with antibiotics. Patient-reported outcomes showed a significant improvement in both functionality and pain relief.
1536
P415: Improvement in spino-pelvic alignment in patients operated for high grade lumbar spondylolisthesis with MIS-TLIF
Rahul Chavan 1 , Vishal Peshattiwar 1 , Shreenidhi Kulkarni 1
1 Orthopaedic Spine, Kokilaben Dhirubhai Ambani Hospital, Mumbai, India
Introduction: Over decades lumbar interbody fusion is used to treat various disease of lumbar spine. TLIF achieves decompression and interbody arthrodesis with lesser tissue injury and thecal sac retraction. High grade spondylolisthesis poses unique questions in achieving adequate reduction to restore spino-pelvic alignment. Our study is to evaluate the clinical and radiological outcomes of MIS TLIF for high grade sondylolithesis. Material and Methods: Conducted at Kolkilaben Hospital, Mumbai. Duration-2017-2020. Type of study: Retrospective analysis and 2 year follow up. Radiological outcomes: pelvic incidence, sacral slope, pelvic tilt, lumbar lordosis, disc height ratio, and Bridwell grading for fusion. Results: 53 patients included in the study both male and female with mean age of 47.3 ± 8.5 years all operated at a single institute by a single surgeon had out of bed mobilization on the same day of surgery with Bridwell grade 1 fusion was seen in 51 patients by the end of 2 years. Conclusion: MIS-TLIF is a safe and effective method for treating high grade lumbar spomdylolisthesis showing recurrent, replicable results with improvement in sacral slope and pelvic tilt with excellent union rate.
1659
P416: Do the patients after the robotic transforaminal lumbar interbody fusion (MIS TLIF) Fair better than traditional transforaminal lumbar interbody fusion surgery a single centre prospective study
Harith Reddy 1 , Sharan Achar Thala 1 , Akshya Raj 1 , Umesh Kanade P 1 , Vignesh Badikillaya 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Spine Surgery, Apollo Hospitals, Chennai, India
Introduction: Transforaminal lumbar interbody fusion (TLIF) is a widely accepted surgical technique for the management of numerous spinal conditions requiring spinal stabilization and fusion. Transforaminal lumbar interbody fusion (TLIF), a posterior spinal fusion approach, was initially described by Harms and Rollinger in 1982, and gained popularity after work by Harms and Jeszenszky in 1998. Compared with posterolateral and lateral approaches, Transforaminal may be advantageous, providing a wider area of intervertebral interbody graft bone contact surface, improved load-sharing, adequate access for complete decompression of the neural elements, restoration of neural foraminal height, and the ability to restore segmental lordosis at the involved level. Robot assisted TLIF surgery has more favorable outcomes then the open TLIF surgery in various modalities. Material and Methods: This is a prospective study including 95 patients who underwent Robot-assisted minimally invasive transforaminal lumbar interbody fusion (robot-assisted MIS-TLIF) and 95 patient who underwent traditional open TLIF surgery. All patients included in the study underwent single level Transforaminal lumbar interbody fusion. These patients were skeletally mature predominantly having single level pathology with single leg radicular symptoms and patients with grade I degenerative spondylolisthesis, failed conservative management for a period of 3 months. All the cases which fulfilled the inclusion criteria were segregated on basis of age and sex. Pre op regular standing X-RAYS ap and lateral views were taken, and Pre-op CT scan was done, and the images were uploaded to the robot and planned the screws placement. Intra-op blood loss is noted, surgical time is noted, time for screw placement is noted, post op patient’s requirement for analgesics is noted between the two groups. Results: In our study we compared the efficacy and outcomes of 95 patients who underwent Robot-assisted minimally invasive transforaminal lumbar interbody fusion (robot-assisted MIS-TLIF) and 95 patient who underwent traditional open TLIF surgery. In Robot assisted MIS-TLIF The age group range was from a minimum of 28 years to a maximum of 80 years 57.6 = /- 2.55 years. The mean age for the traditional open TLIF is around 57.5 ± 2.67 years ranging from 30 to 82 years. Among the Robotic MIS-TLIF surgery group 40 were male patients and 55 were female patients, the other group has 45 male patients and 50 female patients. when compared with the average duration of surgery 105.6 for the Robot TLIF surgery and 166.4 for the traditional open TLIF surgery. average blood loss for the Robot MIS-TLIF surgery is 40ml whereas in the case of open TLIF is 130ml of blood loss. Conclusion: In conclusion Robot-assisted minimally invasive transforaminal lumbar interbody fusion (robot-assisted MIS-TLIF) provides the patients safe spinal fusion surgery with accurate screw placements, less blood loss, early mobilization and reduce dependency on post op analgesics, reduced days of hospitalization.
1740
P417: “Is bigger always better” - Or a minimally invasive spine surgery can help save the golden years of an athletes career?
Nishant Juva 1,2
1 Spine Surgery, We are Spine, Mumbai, India
2 Spine Surgery, Juva Orthopaedic Hospital, Godhra, India
Study Design: This study was a retrospective analysis. Purpose: This study aimed to analyse the functional outcome following Microlumbar discectomy surgery in elite athletes using return-to-play criteria. Overview of Literature: Spinal ailments are relatively common in athletes and are bound to increase due to the ever-growing popularity of contact sports. One of the common ailments is lumbar intervertebral disc prolapse. Athletes are highly motivated to make a rapid recovery and return to full participation in sports which is a high demand situation. Hence, there always lies a confusion weather to go for conservative management or to choose a minimally invasive procedure versus a fusion procedure in order to get the athlete back to the sport as soon as possible and with full confidence. Methods: This study was a retrospective analysis of the data of 15 athletes who chose to undergo Microlumbar discectomy surgery for symptomatic lumbar intervertebral disc prolapse. Outcome measures were investigated using return-to-training and return-to-sports criteria, as indicated by the length of time between surgery and return to competitive sports as parameters. Results: Of the 15 patients, Eleven were males and Four were females. The average age of the patients at the time of surgery was 28.2 years (range, 16-42 years). All patients returned to active participation of their sports. The average time for return to training was 6.2 weeks (range, 3-12 weeks). The average time for return to sports was 26.4 weeks (range, 20-52 weeks), and the average follow-up period was 24 months (range, 8-60 months). Conclusions: Microlumbar discectomy surgery in an athlete involved in contact sports is a fast, safe and effective. An athlete needs to be symptom-free, with full range of motion and full strength before returning to sports. A minimally invasive Discectomy serves as a trick up the sleeve to get the athlete back on the field in a shortest duration possible and provide them with an opportunity to cash in the golden years of their career.
Keywords: Athletes; Functional outcome; Return to sport; Microlumbar discectomy surgery.
Conflict of interest: None
1810
P418: Integration of monoportal endoscopic spine surgery technique in a university hospital setting
Tuong LU 1 , Richard Assaker 1 , Leroy Henri Arthur 1
1 Neurosurgery, CHU de Lille, Lille, France
Introduction: Minimal invasive surgery is on a rise. Here, we report the initial results of the launch of spinal monoportal endoscopy activity in a French university hospital. Material and Methods: This study describes the outcomes of monoportal endoscopic surgery activity at CHU de Lille and the Calot Institute in France. Between March 2021 and July 2023, 63 patients (average age of 51.71 years) underwent surgery for lumbar disc herniations (n = 56), foraminal stenoses (n = 5), and lumbar canal stenosis (n = 2). The surgical approaches used were transforaminal in 51% of cases, extraforaminal in 6%, and interlaminar in 43%. Both operating rooms were equipped with monoportal rigid endoscopy columns (JOIMAX, Tessys, and Ilessys). Results: The entire patient series reported early postoperative clinical improvement. The average duration of surgery was 1 hour and 17 minutes (min: 30 minutes; max: 3 hours and 16 minutes). Ambulatory care was provided in 45% of cases. For hospitalized patients, the average length of hospital stay was 1.7 days (min: 1 day; max: 6 days). Conversion to a tubular approach was performed in 3 cases (5%) for: dural suture, management of epidural bleeding, and anatomical exposure difficulty. No permanent neurological deficits (sensory or motor) were reported. There were no observed hemorrhagic or infectious complications. Conclusion: This study highlights the successful integration of monoportal endoscopic surgery into the surgical toolkit of an experienced team that has been performing tubular surgery since the 2000s. The favorable results obtained by various operators and its low morbidity rate make it an increasingly prominent technique within the surgical activities at the university hospital of Lille.
1850
P419: Weighting the outcomes: does BMI tip the scales in minimally invasive spinal fusion? A cohort study
Froukje Koremans1,2, Charmian Stewart2, Alisha Sial1,2, Stone Sima1,2, Neha Chopra2, Ashish Diwan2
1 Medicine, University of New South Wales Sydney, Sydney, Australia
2 Orthopaedics, Spine Labs & Spine Service, Kogarah, Australia
Objectives: In the realm of spinal surgery, minimally invasive transforaminal lumbar interbody fusion (MAS-TLIF) and extreme lateral interbody fusion (XLIF) have revolutionized the landscape (collectively MISS-Fusions or minimally invasive spinal surgery for fusion). However, the influence of patient-specific factors, particularly body mass index (BMI), on surgical outcomes remains a topic of keen interest predominantly because traditional spinal fusion surgery has been said to provide poorer outcomes for the obese. This study aimed to assess the influence of BMI on the outcomes of MISS-Fusions. Methods: This is an IRB-approved retrospective analysis of patients who had undergone MAS-TLIF and XLIF from January 2012 to August 2020 for various indications and followed up with PROM at clinic visits. Changes in ODI scores were assessed by Delta-ODI. The functional outcomes were analysed using Oswestry Disability Index (ODI), Delta ODI and Short Form-36 Item Survey. Descriptive statistics, Independent T-test and Spearman’s rank correlations were used for statistical analysis, considering a P-value < 0.05 as statistically significant. Results: Of the cohort, 126 patients had undergone minimally invasive transforaminal interbody fusion and 95 patients had undergone extreme lateral interbody fusion. The mean BMI of the patients was 28.8 ± 4.7, with 39% categorized as BMI ≥ 30. The analysis revealed no correlations between BMI, and both Delta-ODI and SF-36. Functional outcomes via the SF-36 and ODI were consistent across BMI categories, and notably, a higher BMI did not correlate with diminished ODI improvement. No higher complication rates were observed in the patients categorised as obese. In total seven complications were observed, including surgical site infection (n = 1), persistent pain leading to the removal of implants (n = 2), Impingement on nerve roots leading to revision (n = 1), dislodged bone graft leading to revision (n = 1), and pseudo-arthrosis (n = 2). Conclusion: Results of the study revealed that improvement in patient-reported disability post minimal invasive spinal fusion are consistent across all BMI categories. Elevated BMI does not adversely impact disability improvement in patients receiving minimal invasive spinal fusion interventions, suggesting the equitable efficacy and safety of these procedures in relation to BMI. These results suggest that obesity should not be considered a limiting factor for MISS-Fusion surgery suitability.
1922
P420: First report of full endoscopic removal of cervical calcium pyrophosphate deposition (CPPD) induced myelopathy: report of two cases and review of literature
Woo-Keun Kwon 1
1 Department of Neurosurgery, Korea University Guro Hospital, Seoul, South Korea
Cervical calcium pyrophosphate deposition (CPPD) is a relatively uncommon condition marked by the accumulation of calcium pyrophosphate crystals within the joints adjacent to the cervical spine, leading to inflammation and the gradual degeneration of these joints. While this ailment is considered exceedingly rare, in some unfortunate cases, CPPD may aggregate within the ligamentum flavum, a critical structure in the cervical spine. When this occurs, it can exert pressure on the spinal cord, subsequently resulting in myelopathy symptoms such as muscle weakness, numbness, and coordination difficulties in the arms and legs. Given the potential severity of this condition, it is imperative to swiftly diagnose and manage it to alleviate symptoms and prevent further neurological deterioration.
For individuals suffering from CPPD-related cervical myelopathies, the preferred course of treatment has traditionally been surgical intervention. However, up until now, all such surgical procedures have been open and invasive. Due to the extreme rarity of this disease, there have been very limited reports on the application of full endoscopic techniques for its removal. Notably, one advantage of full endoscopic surgery lies in its minimally invasive nature, which can potentially lead to reduced postoperative pain, shorter hospital stays, and faster recovery times for patients. In this comprehensive report, we present two compelling cases of cervical ligamentum flavum CPPD-induced myelopathies that were successfully treated with full-endoscopic procedures. Our report not only delves into the unique challenges posed by this rare condition but also offers an in-depth review of the disease itself. Additionally, we provide a detailed insight into the surgical techniques employed, shedding light on the potential benefits of full endoscopy in addressing this complex issue with intra-op images and videos.
2047
P421: Full-endoscopic foraminotomy and transforaminal discectomy for the management of stable herniated discs: a report on three cases
Benjeddou Wassim 1 , Khalil Habboubi 1 , Amine Chabchoub 1 , Meddeb Mehdi 1 , Hassen Makhlouf 1 , Mondher Mestiri 1
1 Med Taieb Kassab Institute, Adults, Mannouba, Tunisia
Introduction: Stable herniated discs are a prevalent condition affecting approximately 8.2% of the global population. Although often associated with segmental instability in the realm of surgical intervention, a minority of cases truly exhibit radiological instability. Nevertheless, even in stable scenarios, neurological symptoms can arise due to radicular compression within the lateral recess or foraminal region. Traditional open foraminal decompression typically necessitates concurrent fusion procedures due to the muscular, osseous, and ligamentous disruptions incurred during the surgical approach. In such cases, full-endoscopic techniques offer the potential to decompress the affected nerve root while preserving segmental stability, obviating the need for instrumented fusion. Material and Methods: We present a case series comprising three consecutive patients diagnosed with low-grade, stable herniated discs accompanied by symptomatic radiculopathy. These patients were managed using full-endoscopic foraminotomy and transforaminal discectomy. We collected baseline patient data, imaging characteristics, preoperative back pain Visual Analog Scale (VAS) scores, leg pain VAS scores, and Oswestry Disability Index (ODI). The surgical procedures were conducted by four of the authors, following a "module-based" approach previously published. We recorded the extent of intervertebral disc breach during each surgical procedure. Outcome measures encompassed postoperative back pain VAS scores, leg pain VAS scores, and ODI. Postoperative CT scans and dynamic X-rays were performed to evaluate the extent and precision of bony resection and assess segmental stability. Follow-up consultations were scheduled every six months. Results: The study comprised two male and one female patient, with a mean age of 68 years. A transforaminal approach was utilized in 76% of cases, while the remaining 24% underwent an interlaminar contralateral approach. Approximately 76.5% of patients exhibited high Pfirrmann values (4-5). Postoperative assessments revealed statistically significant reductions in ODI, leg pain VAS, and back pain VAS scores when compared to preoperative values. No intraoperative or postoperative complications were observed. One patient experienced a high-level disc breach during the surgical procedure, resulting in subsequent radiological instability necessitating lumbar fusion as a separate intervention. However, no instances of recurrent leg pain were observed during the follow-up period. Conclusion: In this series, full-endoscopic foraminotomy and transforaminal discectomy proved effective in alleviating radicular symptoms among patients with stable herniated discs. Importantly, these procedures largely preserved segmental stability, with only one patient experiencing postoperative instability, potentially attributable to a high-level disc space breach.
2176
P422: Biportal endoscopic spinal surgery (BESS) via interlaminar approach is a reliable and effective surgical technique for symptomatic conjoined nerve root
Inhee Kim 1 , Hyung Rae Lee 2 , Yong Min Kim 1 , Dong-Ho Lee 3 , Chang Ju Hwang 3 , Jae Hwan Cho 3 , Sehan Park 3 , Seung Hyun Baek 4 , Geon Jung Kim 1 , Nam Jun Baek 1
1 Orthopedic Surgery, National Police Hospital, Seoul, South Korea
2 Department of Orthopedic Surgery, Uijeongbu Eulji Medical Center, Gyeonggi-do, South Korea
3 Orthopedic Surgery, Seoul Asan Medical Center, Seoul, South Korea
4 Department of Orthopedic Surgery, Daejeon Eulji Medical Center, Daejeon, South Korea
Introduction: Conjoined nerve root (CNR) is an uncommon congenital anomaly in which two adjacent nerve roots share a common sheath. Even with advanced imaging techniques, identifying CNR can pose a challenge, leading to potential complications during and after surgery. Surgeons may be unaware of the presence of an additional nerve root, increasing the associated risks of the procedure. Here, we present a technical note on a case of symptomatic L4, 5 conjoined nerve root which was successfully treated using Biportal Endoscopic Spinal Surgery (BESS) via the interlaminar approach. Recently, several studies applying BESS to various cases have been reported. One of the advantages of this technique is that it allows for the use of existing surgical instruments. There have been numerous reports that decompression surgery through microscopic spine surgery is useful for CNR, but there are almost no reports for BESS. Therefore, I aim to present a technical note along with a specific case. Material and Methods: 1) Patient. A 54-year-old man presented with persistent right-sided lumbar radiculopathy that had been present since his youth. Over the years, he had undergone conservative treatments, including medicine and root blocks, at various hospitals, but the symptoms persisted. Approximately eight months prior to his arrival at our hospital, the symptoms worsened significantly, impacting his daily life activities. Despite receiving two nerve root blocks and one percutaneous epidural neuroplasty in our hospital, the symptoms continued. Although the physical examination did not show any motor or sensory deficits, the intensity of the symptoms made routine activities difficult. 2) Technical note. The patient was positioned in a prone position on a spine surgical table and draped in the usual manner. The surgeon marked the portal entries, locating them 1cm below and above the L4-5 interlaminar space. A skin incision was made and gently dissected using a dilator. The scope and instruments were then inserted. To achieve a clear visual field, the muscle and fascia were debrided using an arthroscopic shaver and radiofrequency ablator. Once a clear view of the interlaminar space was obtained, partial laminectomy was done with high speed burr and removed the ligamentum flavum. Subsequently, the surgeon gained visual access to the dura and the right L4,5 conjoined nerve root. Results: In this case, CNR mobility was confirmed after adequate decompression around the CNR using BESS. After surgery, the patient's right leg radiating pain was completely relieved, and the distal motor and sensory functions remained normal. There was no dynamic instability of the spine in follow-up radiographs at 1 year postoperatively, and the patient's clinical symptoms remained improved. Conclusion: In conclusion, accurate diagnosis, thorough clinical and image evaluation, meticulous surgical planning, and effective management are pivotal in cases involving a conjoined nerve root anomaly. The utilization of BESS, which provides excellent visualization of the surgical field, proves to be a reliable and safe procedure for treating conjoined nerve root. It enables optimal exposure of the conjoined nerve root, ensuring successful relief of clinical symptoms.
2429
P423: Does LLIF malalign patients with convex coronal malalignment? An analysis of the obeid coronal malalignment classification
Timothy Yee 1 , Andrew Chan 2 , Praveen Mummaneni 1 , Paul Park 3 , Vivian Le 2 , Jay Turner 4 , Juan Uribe 4 , Robert Eastlack 5 , Richard Fessler 6 , Kai-Ming Fu 7 , Michael Wang 8 , Adam Kanter 9 , David Okonkwo 10 , Pierce Nunley 11 , Neel Anand 12 , Gregory Mundis 5 , Peter Passias 13 , Shay Bess 14 , Christopher Shaffrey 15 , Dean Chou 2
1 Neurological Surgery, University of California, San Francisco, San Francisco, USA
2 Neurosurgery, Och Spine Hospital at NewYork-Presbyterian Columbia University, New York, USA
3 Neurosurgery, Semmes-Murphey Clinic, Memphis, USA
4 Neurosurgery, Barrow Neurological Institute, Phoenix, USA
5 Orthopedic Surgery, Scripps Clinic, La Jolla, USA
6 Neurosurgery, Rush Medical College, Chicago, USA
7 Neurological Surgery, Weill Cornell Medicine, New York, USA
8 Neurosurgery, University of Miami, Miami, USA
9 Neurosurgery, Hoag Neuroscience Institute, Newport Beach, USA
10 Neurosurgery, UPMC Neurological Institute -Presbyterian, Pittsburgh, USA
11 Orthopedic Surgery, Spine Institute of Louisiana, Shreveport, USA
12 Orthopedic Surgery, Cedars-Sinai, Los Angeles, USA
13 Orthopedic Surgery, NYU Langone Spine Institute, Westbury, USA
14 Orthopedic Surgery, Denver International Spine Center, Denver, USA
15 Neurological Surgery, Duke University, Durham, USA
Introduction: Compared to concave coronal malalignment (CM) (Obeid Type 1 [O1] CM > 20 mm), there is a concern that lateral lumbar interbody fusion (LLIF) for convex CM (Obeid Type 2 [O2] CM > 20 mm) may worsen coronal alignment. We compared 2-year (2Y) LLIF outcomes for concave and convex CM using the Obeid Classification. Material and Methods: This was a bispective analysis of a multicenter adult spinal deformity (ASD) database. Patients undergoing cMIS LLIF for ASD with CM > 20 mm (Obeid) were included. 2Y outcomes were adjusted for age and preoperative SVA. Results: Overall, 85 patients were prospectively enrolled with 2Y follow-up - 30 met inclusion criteria (14 O1 [46.7%];16 O2 [53.3%]). O1 were older and had higher preop SVA than O2 (p < 0.05). Otherwise O1/O2 were well matched. Of note, only 1 patient in each O1/O2 cohort had fusions that did not involve the fractional curve (FC). There was no difference between O1/O2 for 2YCVA (38.2 vs. 34.4 mm, p = 0.851), 2YΔCVA (Δ-7.4 vs. -10.4 mm, p = 0.256), and 2YΔ max coronal cobb (CC) (Δ-7.6 vs. -10.1º, p = 0.922), respectively. A similar proportion reached 2YCVA < 20 mm (O1:35.7% vs. O2:31.3%, p = 0.550). There were no other significant differences for 2Y CC, SVA, PI-LL, PT, and FC (p > 0.05) for O1/O2. Clinical outcomes and complications were similar (p > 0.05) for O1/O2 at 2Y. Conclusion: Following cMIS for ASD with CM, patients undergoing LLIF with convex CM did not have a significant worsening of coronal alignment and shared similar coronal parameters as LLIF for concave CM. This may be due to control of the fractional curve in the convex CM surgeries. Radiographic and clinical outcomes, and complications, were similar for O1/O2.
2550
P424: Endoscopic resection of a cervical perineural cyst
Neptali Torres 1 , Fernando Rascon 1 , Borja Ferrandez Pujante 1 , Albert Trondin 1 , Andres Vargas 1 , Gustavo Villalobos 1 , Pedro Alonso 1
1 Neurosurgery, Hospital Clinico San Carlos, Madrid, Spain
Introduction: Perineural cyst are common in lumbar or sacral roots, but in cervicothoracic region are rare. The symptoms are not specific like pain, numbness and other sensory disorders but in cervical cyst can cause neck, chest or back pain. Material and Methods: 57 years old female patient who has history of neck pain with irradiation to her upper left arm, she was continuously diagnosticated of cervicalgia with oral medication without total relief. She was sent to neurosurgery and ask a cervical MRI where was found an perineural cyst on C7 left root. Results: We perform an endoscopic resection. First a minimal 1,5cm incision, then foraminotomy with visualization of the cyst on C7 root. We open the cyst an coagulate the sack. Then we close with dural sutures. In the follow up, the patient have complete relief on the upper limb and do not have fistula. Conclusion: It is possible to do an endoscopic foraminotomy for resection of perineural cyst on cervical roots. We have to do more cases with minimal invasive spine surgery to be more comfortable.
Navigation
426
P425: Automatic image registration on intraoperative CBCT compared to surface matching registration on preoperative CT for spinal navigation: accuracy and workflow
Henrik Frisk 1 , Gustav Burström 1 , Oscar Persson 1 , Victor Gabriel El-Hajj 1 , Luisa Coronado 2 , Susanne Hager 2 , Erik Edström 1 , Adrian Elmi Terander 1,3
1 Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
2 Clinical Affairs, Brainlab AG, Munich, Germany
3 Department of Surgical Sciences, Uppsala University, Uppsala, Sweden
Introduction: Spinal navigation solutions have been slower to develop compared to cranial ones. To facilitate greater adoption and use of spinal navigation the relatively cumbersome registration processes need to be improved upon. This study aims to validate a new solution for automatic image registration and compare it to a traditional surface matching method. Material and Methods: Adult patients undergoing spinal surgery requiring navigation were enrolled after providing consent. A reference matrix (Universal Air) was placed in the surgical field and used for automatic registration based on intraoperative 3D imaging. A standard surface matching method was used for comparison. Accuracy measurements were obtained by comparing planned and acquired coordinates on the vertebrae. Results: 39 patients with 42 datasets were included. The mean accuracy of Universal AIR registration was 1.20 ± 0.42 mm, while the mean accuracy of surface matching registration was 1.94 ± 0.64 mm. Universal AIR registration was non-inferior to surface matching registration. Post hoc analysis showed a significantly greater accuracy for Universal AIR registration. In surface matching, but not automatic registration, user related errors such as incorrect identification of the vertebral level were seen. Conclusion: Automatic image registration for spinal navigation using Universal AIR and intraoperative 3D imaging provided improved accuracy compared to surface matching registration. In addition, it minimizes user errors and offers a standardized workflow, making it a reliable registration method for navigated spinal procedures.
972
P426: Comparison of pedicle screw placement accuracy between preoperative CT and intraoperative CT registration using ExcelsiusGPS
Hiroto Makino 1 , Shoji Seki 1 , Taketoshi Yasuda 1 , Kayo Suzuki 1 , Hayato Futakawa 1 , Katsuhiko Kamei 1 , Yoshiharu Kawaguchi 1
1 Orthopeadic Surgery, University of Toyama, Toyama, Japan
Introduction: Robotic-assisted spine surgery has become available recently in Japan, and our hospital has started using the Excelsius GPS® spine robot system (EGPS). There are few studies, however, which compared between registration methods in robotic-assisted spine surgery. The purpose of this study was to compare and examine the accuracy and time required for pedicle screw insertion in the early stages of EGPS introduction by different registration methods. Material and Methods: The subjects were 35 patients (18 men, 17 women, mean age 69.9 years) who underwent surgery after planning to use EGPS. We planned to insert 158 pedicle screws and 6 SAI screws under EGPS guidance. The following items were evaluated: registration method (preoperative CT, intraoperative CT), whether robot-assisted insertion was achieved, and postoperative CT to assess screw violation from the pedicle and anterior vertebral wall. We also examined the time required for registration and screw insertion. Results: The registration method used preoperative CT in 22 cases and intraoperative CT in 13 cases. Screw insertion using EGPS was completely achieved in 29 of 35 cases. EGPS could not be used in 6 cases due to poor registration or arm interference. As a result, we were able to insert 141 screws (including 6 SAI) under EGPS guidance. Violation from the pedicle/anterior wall was more significant when using preoperative CT, as it was 1/98 (1%) using preoperative CT, compared to 4/43 (9.3%) using intraoperative CT (p = 0.03). The registration time per vertebra was 9.3 minutes for preoperative CT and 7.0 minutes for intraoperative CT (p = 0.17), and the time required for insertion per screw was 8.2 minutes and 6.9 minutes, respectively (p = 0.26), but there was a tendency for both to be shorter when intraoperative CT was used. Conclusion: In the initial 35 cases of spinal surgery in which EGPS was introduced, accurate screw placement was achieved. An analysis of each registration method revealed that using intraoperative CT can shorten the time but reduces accuracy. These factors need to be considered to improve accuracy.
2059
P427: Spinal navigation: beyond screws
Joaquim Cruz Teixeira 1 , João Levy Melancia 1
1 Hospital CUF Tejo, Lisboa, Portugal
Introduction: Navigation is tool with proven benefits on spinal surgery. Data supports the superior accuracy of screw placement guided by navigation when compared with free-hand technique. Nonetheless, various novel applications of spinal navigation can also be valuable as an aid to minimally invasive techniques beyond screw placement. Material and Methods: We describe three cases of minimally invasive techniques enhanced by spinal navigation in order to increase accuracy of the approach and procedure, further reducing approach related muscular trauma and blood loss while achieving the desired surgical goal.
Results:
Case 1: A 68-year-old female patient with a previous L4-S1 fusion presenting with recurrent radiculopathy due to foraminal stenosis. A tubular extraforaminal foraminoplasty was performed.
Case 2: A 37-year-old male patient presenting with T10 right radiculopathy due to a T9-T10 thoracic disc herniation who underwent a tubular microdiscectomy, via transpedicular approach.
Case 3: One 19-year-old female patient also presenting with a T10 radiculopathy on the left side due to a T9-T10 osteoma osteoid. An en bloc resection was performed through a posterior tubular approach.
Conclusion: Navigation is a powerful tool beyond screw placement as it allows to enhance accuracy and effectiveness of various minimally invasive techniques in a multitude of spinal disorders, from degenerative to oncology.
2120
P428: Evaluation of accuracy of C2 pedicle screw placement using 3D navigation system
Prasanna Gunasena 1 , Dilshan Munidasa 2 , Anil Weerasinghe 1 , Eranga Ganewatte 3 , Anupa Walgamage 1
1 Neurosurgery
2 Orthopaedics
3 Radiology, Lanka Hospital, Colombo, Sri Lanka
Summary: This retrospective study was performed to assess the accuracy of C2 pedicle screw placement using the stealth 3 D navigation system. Primary Objective: Placement of C2 pedicle screw for trauma or degenerative cervical pathologies involving C2 vertebra has been a challenge to spine surgeons due to risk of injury to vertebral artery [1] and violation of vertebral canal medially due to the anatomical variation in the C2 pars interarticularis. The rate of vertebral artery canal violation was around 8- 9 % according to the data available [2,3]. In order to prevent such inaccuracy strenuous pre-operative planning and meticulous surgical technique is a must. However stealth Navigation using 3 D navigation images [4] help to appreciate the anatomical variations and place C2 pedicles screws accurately [5]. Methodology: All patients who presented between 2017 – 2021 for C2 fixation due to trauma or degenerative spine were included into the study. They all were operated standard posterior approach and the C2 pedicle screw placement was done using stealth navigation system supported by 3D fluoroscopic C arm. 3.5 self-tapping titanium screws were used. All patients were operated by a single spine surgeon at Lanka Hospitals Pvt. Ltd. All the patients were evaluated with CT scan of upper cervical spine to assess the accuracy of the C2 pedicle screw placement six months after the surgery. The accuracy was evaluated by an independent board certified radiology specialist. Encroachment of the vertebral artery canal and medial cortex of the pedicle by the crews was examined to assess the breaches. No breaches were found in all 22 patients where there were 44 C2 pedicle screw placement were done. Conclusion: Using 3 D C arm assisted navigation system is a highly accurate way of placing the C2 pedicle screws in trauma and degenerated spinal disorders.
References
1. Yeom JS, Buchowski JM, Kim H-J, et al. Risk of vertebral artery injury: comparison between C1-C2 trans articular, and C2 pedicle screws.
2. Xiauhoi T, Wei T, Bo L, Quin L, Guilin S. Accuracy and complications of posterior C2 fixation using intraoperative 3 D fluoroscopy based navigation. Chin Med J 2014; 127(14).
3. Mueller C-A, Roesseler L, Podlogar M, Kovacs A, Kristof RA. Accuracy and complications of transpedicular C2 screw placement without the use of spinal navigation. European Spine Journal 2010; 19: 809-814.
4. Garg B, Gupta M, Singh M, Kalyanasundaram D. Outcome and safety analysis of 3D-printed patient-specific pedicle screw jigs for complex spinal deformities: a comparative study. Spine J 2019; 19: 56-64. doi: 10.1016/j.spinee.2018.05.001. Epub 2018 May 3. PMID: 29730456.
5. Azimi P, Yazdanian T, Benzel EC, et al. Accuracy and safety of C2 pedicle or pars screw placement: a systematic review and meta-analysis. J Orthop Surg Res 2020; 15: 272. https://doi.org/10.1186/s13018-020-01798-0
Nonoperative clinical treatments
5
P429: Hirayama disease and its management - Experience of a tertiary care centre
Selvin Vijayan 1 , Christopher Gerber 2 , Anindya Basu 2 , Mona Tiwari 2 , Tosaddeque Hussain 2 , Jacky Ganguly 2
1 Brain and Spine Surgery, Kauvery Hospital, Chennai, India
2 Brain and Spine Surgery, I-NK, Institute of Neurosciences, Kolkata, India
Introduction: Hirayama disease (HD) is a unique, benign and self-limiting cause of compressive myelopathy. It presents as asymmetric weakness and atrophy of one, less commonly both distal upper extremities. Treatment of HD is controversial, traditionally conservative management is advocated while recently surgical management is preferred in refractory cases. We present our experience in management of HD using different modalities. Material and Methods: Data of patients diagnosed to have HD from 2016 to 2022 were collected, multiple clinical and radiological (dynamic MRI) parameters were noted. Total of 17 patients were identified out of which 14 were managed conservatively and 3 surgically. Patient outcomes were analysed at final follow up. Results: All were males with a mean age of 25 years. Seven had bilateral and ten had unilateral upper limb symptoms. Most common clinical finding was weakness and wasting of distal hand muscles (100%) followed by forearm weakness (59%). MRI finding seen in all was abnormal cervical curvature followed by enhancing epidural component (71%). Functional assessment was done using Jebsen Taylor Hand Function test (JTHFT). At follow up, 10 out of 14 patients managed conservatively had successful outcome (5 improved, 5 plateaued). Mean JTHFT score improved from 69.5 to 62.5 seconds. In four patients with failed conservative treatment had JTHFT score worsening from 62 to 75 seconds. All three who underwent surgery improved, with JTHFT score of 79 seconds from 54. Conclusion: HD is a rare condition warranting high index of suspicion for diagnosis, especially in patients of atypical age group. Reasonable outcomes are seen with conservative management in mild cases with gradual progression. Surgery is useful in failed conservative management or with severe weakness and rapid deterioration of symptoms, giving good outcomes.
189
P430: Bilateral erector spinae plane block for postoperative pain relief in lumbar spine surgery: systematic review & meta-analysis
Sathish Muthu 1,2 , Vibhu Krishnan Viswanathan 1,3
1 Department of Spine Surgery, Orthopaedic Research Group, Coimbatore, India
2 Department of Orthopaedics, Government Medical College, Karur, India
3 Department of Spine Surgery, Rela Institute and Medical Centre, Chennai, India
Introduction: Erector spinae plane block (ESPB) is growing in popularity over the recent past as an adjuvant modality in multimodal analgesic management following LSS. The current meta-analysis was performed to analyze the efficacy of ESPB for postoperative analgesia in patients undergoing LSS. Methods: We conducted independent and duplicate electronic database searches including PubMed, Embase and Cochrane Library till June 2023 for randomized controlled trials (RCTs) analyzing the efficacy of bilateral ESPB for postoperative pain relief in lumbar spine surgeries. Post-operative pain scores, total analgesic consumption, first analgesic requirement time, length of stay and complications were the outcomes evaluated. Statistical analysis was performed using STATA 17 software. Results: 32 RCTs including 1464 patients (ESPB/Control = 1077/1069) were included in the analysis. There was a significant pain relief in ESPB group, as compared to placebo across all timelines such as during immediate post-operative period (p < 0.001), 4 hours (p < 0.001), 8 hours (p < 0.001), 12 hours (p < 0.001), 24 hours (p = 0.001) post-surgery. Similarly, ESPB group showed a significant reduction in analgesic requirement at 8 hours (p < 0.001), 12 hours (p = 0.001), and 24 hours (p < 0.001). However, no difference was noted in the first analgesic requirement time, time to ambulate or total length of stay in the hospital. ESPB demonstrated significantly improved overall satisfaction score for the analgesic management (p < 0.001), reduced intensive care stay (p < 0.05) with significantly reduced post-operative nausea and vomiting (p < 0.001) compared to controls. Conclusion: ESPB offers prolonged post-operative pain relief compared to controls, thereby reducing the need for opioid consumption and its related complications.
385
P431: A comparison of interferential current efficacy in elderly intervertebral disc degeneration patients with or without sarcopenia: a retrospective study
Lei Kuang 1 , Hui Yuan 1 , Jing Li 1 , Ou Zhang 2 , Lini Dong 3
1 Department of Spinal Surgery, The Second Xiangya Hospital of Central South Unviersity, Changsha, China
2 Department of Medical Education, California University of Science and Medicine, Colton, USA
3 Department of Geriatrics, The Second Xiangya Hospital of Central South Unviersity, Changsha, China
Introduction: Intervertebral disc degeneration and sarcopenia are both age-related diseases without effective treatments. Their comorbidities may worsen the prognosis, and further studies on interaction and therapy are needed. Evidence suggests that IDD patients and patients with muscle atrophy or skeletal muscle dysfunction achieved good results after interferential currents(IFC) electrical stimulation, which decreases skin impedance to reach deep muscle tissue without increasing the patient's discomfort, and is effective in increasing neuromuscular excitability, relieving inflammation, eliminating edema, reducing nerve or muscle pain, promoting nerve regeneration, enhancing muscle strength, and improving physical mobility. Despite the growing popularity of IFC therapy in various clinical settings, there have been few studies on its efficacy on intervertebral disc degeneration with sarcopenia patients.The purpose of the study was to investigate the prevalence of sarcopenia in intervertebral disc degeneration, and to compare the characteristics of intervertebral disc degeneration with sarcopenia and without sarcopenia and effects of interferential current. Material and Methods: One hunderd and twenty disc degeneration patients were included from 2021 to 2022 in a single institude. Medical records, examination results and radiological reports were reviewed. Patients with sarcopenia were screened and grouped according to Asian working group for sarcopenia2019. VAS, ODI, SARC-F, SMI, gait speed(GS), grip strength, disc Pfirrmann grading, standard cross-sectional area(SCSA), degree of fatty infiltration(DFF), and nerve conduction velocity(NCV) were assessed before and after treatment. Results: The prevalence of sarcopenia in intervertebral disc degeneration was 28.3%. The difference of VAS, ODI, disc Pfirrmann grading, SCSA, DFF and NCV between two groups were significant before intervention (p < 0.05), SCSA and DFF were related to the degree of disc degeneration. The improvement of SMI, GS, grip strength, VAS, SARC-F and ODI in intervertebral disc degeneration with sarcopenia group was significant after intervention, as well as SMI, GS, grip strength, VAS and ODI in those without sarcopenia (p < 0.05). The improvement of grip strength, GS, ODI and SARC-F in intervertebral disc degeneration with sarcopenia group were greater than without sarcopenia (p < 0.05), whereas there was no significance in improvement degree of other indicators between the two (p > 0.05). Conclusion: The prevalence of sarcopenia was high in intervertebral disc degeneration, and paravertebral muscles degeneration correlated with the degree of disc degeneration. Compared to those without sarcopenia, intervertebral disc degeneration with sarcopenia patients have more severe pain, poorer mobility and neurological function. Interferential current is effective in intervertebral disc degeneration patients and sarcopenia patients.
692
P432: Can single low-dose intrathecal morphine reduce perioperative morphine use following posterior cervical spine surgery?
Andrew George 1 , Sudarshan Munigangaiah 1 , John John 1 , Sujay Dheerendra 1 , Birender Balain 1 , Jayesh Trivedi 1 , Matthew Ockendon 1 , Sarfraz Ahmad 1 , Aashish Ghodke 1 , Fouzia Kader 1 , Jan Kuiper 1
1 The Robert Jones & Agnes Hunt Orthopaedic Hospital, Oswestry, Regno Unito
Introduction: Posterior cervical spine surgery is associated with significant pain in the early post-operative period. Multimodal analgesia is often required including the use of systemic morphine. Side effects such as sedation, nausea and constipation are detrimental to patient recovery and can lead to delayed discharge. The use of intrathecal morphine (ITM) has been shown to provide good levels of analgesia following surgery for scoliosis, thoracic and lower limb surgery, however, literature on its use in posterior cervical surgery is lacking. Control of acute post-surgical pain is critical to allow earlier mobilisation of patients, reduction of hospital stay and reduces the development of chronic post-operative surgical pain. We hypothesised that the use of lumbar ITM injection in patients undergoing posterior cervical surgery would be able to demonstrate a morphine-sparing effect in the early post-operative period, reducing post-operative morphine requirements and hospital length of stay. Material and Methods: Retrospective data were collected on 62 patients undergoing posterior cervical surgery. Thirty-one patients received a lumbar intrathecal injection at a dose of 0.2 mg morphine and received no further long-acting opioids in theatre. Outcomes were compared to a 1:1 matched cohort of patients based on: age, gender, type of surgery and number of spinal levels. The control treatment group received an intravenous opioid-based general anaesthetic. Both groups received additional multimodal analgesia, including: paracetamol, non-steroidal anti-inflammatories (NSAIDs) and surgical local anaesthetic (LA) infiltration (60 ml 0.25% Bupivacaine). The primary outcome measure was intravenous morphine equivalent dose (MEq) over 48 hours. Secondary outcomes included: perioperative MEq, worst VAS score at 24 and 48 hours, time to independent mobility and length of stay (LOS), including LOS over 7 days. Statistical significance was set at p < 0.05. Results: In the spinal group, 26 patients (81%) were completely opioid-free both intraoperatively and in recovery. No patients in the matched control group were opioid-free. Average perioperative morphine use in the spinal group was markedly reduced to 1.11 mg vs. 10.52 mg (p < 0.01) with total morphine use over the first 48 hours reduced to 21 mg vs. 80 mg (p < 0.01). Time spent in recovery was reduced to 59.4 min vs. 84.5 mins (p < 0.01). Patients receiving ITM reported an almost 2-point lower mean worst VAS for pain during the first and second post-operative days (p < 0.05 and p < 0.01 respectively). Mean reduction in LOS was 2.2 days (p = 0.21). Conclusion: Utilisation of a single lumbar intrathecal injection of low-dose morphine provides a substantial opioid-sparing effect in posterior cervical spine surgery. This results in significant improvements in pain scores over the first 48 hours and faster discharge from recovery. There also appears to be some benefit in reduction of LOS. Additional work is required to further elucidate the full benefits of this technique including the impact on chronic post-operative surgical pain and the potential cost-saving advantage.
1104
P433: Physical therapy does not improve patient-reported outcomes after lumbar fusion
Michael McCurdy 1 , Rajkishen Narayanan 1 , Delano Trenchfield 1 , Yunsoo Lee 1 , Mina Ebrahimi 1 , Akshay Khanna 1 , Nicholas Pohl 1 , Alexa Tomlak 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1
1 Orthopaedic Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: As value-based care grows in popularity across the USA, more payers have turned away from fee-for-service and toward bundled payment models for surgical procedures. Episode-of-care (EOC) costs in spine are highly variable and multifactorial, but several drivers of 90-day cost in lumbar decompression and fusion surgeries include length of stay, readmissions, and outpatient physical therapy. Though routinely prescribed across all orthopaedic specialties, there is scarce literature providing evidence of outpatient physical therapy’s efficacy in improving outcomes after spine surgery. The goal of this study is to utilize bundled episode-of-care data to more accurately assess the impact of postoperative physical therapy on patient-reported outcomes and cost of care after lumbar fusion surgery. Material and Methods: After Institutional Review Board approval, bundled payment information of lumbar fusion EOC from a private payer from January 2019 to December 2021 was reviewed to identify patients at a single, urban, tertiary care center. EOC patient information was matched with medical record numbers from our own electronic medical record and a structured query language (SQL) search was performed to collect patient demographics, surgical characteristics, complications, readmissions, and patient-reported outcomes (PROMs) in our cohort. Claim-level data was searched to identify any claims that were associated with physical therapy after the date of surgery for each patient. Total cost of physical therapy was calculated by adding the cost of each claim relating to physical therapy within a patient’s episode of care. Patients were grouped into physical therapy (PT) and no physical therapy (no PT) groups for statistical analysis. Results: 758 patients were identified, with 448 (59.1%) participating in at least one physical therapy session after surgery. On bivariate analysis of patient and surgical characteristics, patients in the PT group were older (61.6 vs. 59.4, p = 0.024), had a greater body mass index BMI (30.6 ± 6.11 vs. 29.6 ± 5.67, p = 0.029), and had more levels fused (1.54 ± 1.09 vs. 1.42 ± 0.94, p = 0.034) than patients in the no PT group. Patients that did not participate in postoperative PT had significantly better preoperative PCS (33.2 ± 6.26 vs. 31.1 ± 6.78, p = 0.003), six-month postoperative PCS (41.1 ± 10.1 vs. 35.7 ± 9.78, p = 0.001), and six-month ΔPCS (9.24 ± 10.3 vs. 4.92 ± 9.65, p = 0.026) compared to patients who participated in postoperative PT. At one-year follow-up, patients who did not participate in PT had less leg pain (VAS Leg 2.89 ± 2.68 vs. 3.99 ± 3.15, p = 0.041) than those who did participate in PT. Correlation analysis of the number of physical therapy sessions attended after surgery and all PROMs at six months and one year showed no relationship. Average cost of physical therapy per patient was $1,521.57. Conclusion: Our study finds that physical therapy after lumbar fusion is not associated with significant improvement in patient-reported outcomes. Given the significant cost traditional physical therapy contributes to lumbar fusion episodes of care, alternatives such as home-exercise plans and cognitive-behavioral therapy should be considered to provide high quality, cost-effective care.
1443
P434: Unguided injections are effective for sacro-iliac joint dysfunction: intra-articular placement of injectate may not be mandatory
Aditya Goparaju 1 , Kalidutta Das 1 , Harvinder Singh Chhabra 2
1 Spine Services, Indian Spinal Injuries Centre, New Delhi, India
2 Spine Services, Sri Balaji Action Medical Institute, New Delhi, India
Study Design: Prospective, single-arm, observational cohort study. Introduction: For non-inflammatory and inflammatory sacroiliac dysfunction, intra-articular steroid and local anesthetic injections have been used for a long time. Most researchers have emphasized the accuracy of intra-articular placement of the injectate to ensure efficacy, recommending image guidance (image intensifier, ultrasound, computerized tomography and even MRI) to achieve this. A small body of evidence also points out that periarticular injection might be as effective as intra-articular. We have hypothesized that using no guidance will reduce the costs and time for the procedure at the same time ensuring pain relief whether the injectate is dispersed in the intra- or peri-articular space. Materials and Methods: Sacroiliac joint dysfunction patients (diagnosed clinically by at least 3 positives out of 6 defined clinical tests) underwent blind (anatomic landmark guided) sacroiliac injections using 1 ml of 2% lignocaine, 1 ml of 0.5% bupivacaine, with (40 mg/ml) of triamcinolone or 1 ml (40 mg/ml) of methylprednisolone acetate. Clinical back pain scores (VAS, ODI, RMDQ) and quality of life score (WHOQoL-BREF) were measured before and 3 months after the injection. Results: Of the 113 consecutive patients recruited in the study (57.5% female), 96 completed at least 3 months of follow-up. Mean age was 53.7 years (range 20 – 83 years) and the mean symptom duration was 5.4 months (range 2.0 – 9.0 months). Mean follow-up was 106.7 days (range 92 – 149 days/ 3 months – 5 months). Pain score VAS (Pre VAS – 6.2, Post VAS – 2.4, % difference – 60.1%, p < 0.001) and disability indices ODI (Pre ODI – 37.8%, Post ODI – 26.4%, % difference -30.15%, p < 0.001) and RMDQ (Pre RMDQ – 15.7, Post RMDQ – 10.1, % difference -35.67%, p < 0.001) had significantly improved at the last follow-up. In the WHOQoL-BREF score only 83 patients completed the questionnaire at both times. Among these, the physical (Pre Physical - 63.8, Post Physical – 68.7, p < 0.001), psychological (Pre Psych.score – 54.5, Post Psych.score – 57.8, p < 0.001), and environmental (Pre Env.score – 66.1, Post Env.score – 67.4, p < 0 .001) components had significantly improved with the social component (Pre Social – 32.7, Post Social 32.4, p = 0.73) showing no significant change. There was no correlation between pain scores and any component of the WHOQol-BREF. Immediate adverse events were minor (injection site pain -22/113, transient lower limb numbness – 18/113, vasovagal syncope – 4/113) with no other events reported in the 96 patients who completed follow-up. Conclusions: Sacroiliac joint injections without image guidance produce statistically significant short-term pain relief. The site of injectate deposit might not affect the efficacy of the injection, hence the increased cost and time associated with image guidance may be reduced by adapting unguided injections.
1490
P435: Assessing the presentation of adolescents seeking bracing treatment in the UK, using SRS bracing guidelines
Sam Walmsley 1 , Anna Courtney 1 , Jack Choong 1 , Tim Bishop 2 , Jason Bernard 2 , Darren Lui 2
1 Orthotics, The London Orthotic Consultancy, United Kingdom
2 Orthopaedics & Trauma, St George's University Hospital, London, United Kingdom
Introduction: Studies have shown that bracing can be successful in the treatment of idiopathic scoliosis. Extensive research has directed the formation of clinical inclusion criteria which document an adolescent’s suitability for bracing. The Scoliosis Research Society (SRS) report the criteria for bracing to be: age of 10 years plus, Risser 0-2, Cobb angle of 25-40°, no previous treatment and before menarche or less than one year after menarche. However, it is theorised that the United Kingdom’s abolishment of scoliosis screening in schools in the 1990s may be contributory to adolescents receiving their eventual diagnosis when their condition is at a more advanced stage. Thus, the adolescent is more likely to fall out of SRS bracing guidelines. Aims: This study aims to assess the presentation of all adolescents who attended a private orthotic clinic for the assessment of a scoliosis brace as first-line treatment. All patients were seen within a week of first referral. This study will firstly state the percentage of presenting adolescents who were within SRS guidelines and those who were out of guidelines. The study will assess and compare in-brace corrections between the two groups. Patients and Methods. We retrospectively reviewed all adolescents that attended our clinic for the assessment of a scoliosis brace from the years of 2017-2022 (n = 210). We considered age, Cobb angles, Risser and menarche status where suitable. We studied the criteria they met and where they may have failed, based on the SRS guidelines above. The bracing design employed was changed in January 2022. Due to protected data from the initial bracing design, this study will only review in-brace Cobb angle correction for the 2 groups using the latest brace design – the LOCScoli Brace, which is an asymmetric Cheneau derivative brace. We used the data from all assessments as of January to September 2022 for the latter part of this project (n = 64). Results: Of the 210, 95 (45%) were within and 115 (55%) were out of SRS guidelines on the day of their assessment. Of the 115 who were out of SRS guidelines, 79 (38%) adolescents failed on one criterion and 35 (17%) failed on 2 criteria or above. The in-brace correction of the 2 groups from January 2022 onwards highlight a mean in-brace correction of 86.04% for those within SRS guidelines and 75.95% for those out of guidelines. Conclusion: Our preliminary data may suggest that the UK is now in a national position where less than 50% of patients attending an orthotic clinic for first-line bracing treatment are within SRS bracing criteria. Our work highlights the possibility of achieving greater than the internationally acceptable Cobb angle correction in what we term as “hyper corrective braces” for patients both within and out of SRS guidelines. This suggests that adolescents falling outside of the recommended guidelines can be treated with a high level of bracing efficacy. Further studies are required assessing the impact of bracing in those with larger curves and/or those who exceed recommendations. The conversation surrounding in-school screening remains essential.
1684
P436: Opiod use after short-term-stay scheduled surgeries: is it necessary? - A consecutive series of 139 patients
Juan Lourido 1 , Juman Rasheed 2 , Thooba Saeed 2
1 Neurosurgery, TreeTop Hospital, Hulhumale, Maldives
2 Medicine, TreeTop Hospital, Hulhumale, Maldives
Introduction: Spinal Surgery is a stressful event in the life of the patient, often associated with fear for the future and anticipation of failure, regardless of the statistical reassurance provided by the modern practice. Beyond technical prowess, postoperative management is key in providing a satisfactory outcome, and pain control is perceived as a major factor. Material and Methods: Retrospective review of 139 consecutive patients who underwent scheduled spinal surgery. Trauma and emergency cases were excluded. As per protocol, all patients have their iv-line removed 24h after surgery, after finishing antibiotic prophylaxis. Naproxen 500mg q12h + Paracetamol 650mg q8h is prescribed, as well as Tramadol 50mg pro re nata (SOS). A tailored support for the patient, including frequent and extensive interviews with the patient and family by the surgeon, as well as ad hoc use of physiotherapy or lumbar brace is included in the postoperative period. We examined the number of events where tramadol was administered. Results: Surgeries performed > Anterior Cervical Fusion (24 pts) / Posterior Spinal Fusion (27 pts) / Spinal Stenosis Surgery (27 pts) / Lumbar Discectomy (57 pts) / Spinal Tumor (4 pts). No patients requested additional analgesia beyond 24h after surgery, and tramadol was not used in any case. Conclusion: In our quest for the best postoperative “quantifiable” outcomes and patient satisfaction, it is tempting to use the most aggressive/effective medical treatment for pain, notably opioids, without further consideration. This risks overtreating the patient, and arguably could artifact the true effect of surgery or delay identification of early complications. From our experience, and for the largest number of spine surgery cases (low and mid-complexity), we see no need to include opioid therapy as standard procedure in the postoperative management.
2134
P437: Identifying revision lumbar fusion diagnoses that achieve minimal clinically important difference and patient acceptable symptom state
Omar Tarawneh 1 , Tariq Issa 1 , Rajkishen Narayanan 1 , Alexa Tomlak 1 , Otitochukwu Ezeonu 1 , Michael McCurdy 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Orthopaedic Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: As the volume of primary lumbar fusions increases in the USA, rates of revision procedures are expected to increase. PROMs remain the preeminent tool for assessing postoperative outcomes, however, there remain significant shortcomings among these metrics. The minimally clinically important difference (MCID) has been proposed to calculate the meaningful change in patient reported outcomes as perceived by the patient. Similarly, patient acceptable state (PASS) is a concept increasingly used to assess the threshold at which patients are satisfied with postoperative outcomes as it is the metric most closely aligned with patient satisfaction. Collectively, MCID and PASS potentially provide a meaningful clinical context to the statistical significance of PROMs. The primary aim of this study was to calculate MCID based on indication for revision and to assess the temporality of symptom improvement. Secondarily, in patients who underwent revision assessed whether patients achieved a PASS based on revision indication to assess the clinical utility of this metric in spine surgery. Materials and Methods: Between 2011-2021, patients > 18 years who underwent revision 1-3 level lumbar spinal fusion at a single center were included. Indication for revision surgery was obtained by manual review of operative notes and included adjacent segment disease (ASD), nonunion, and recurrent stenosis. Exclusion criteria consisted of non-elective admission, and incomplete records. Primary outcomes consisted of preoperative, 90 day and 1-year postoperative Oswestry Disability Index (ODI). New MCID for ODI was calculated based on our study population’s statistical change in clinical PROMs using a distribution-based method of 0.5*SD of baseline scores. Achievement of MCID was then assessed by comparing ΔODI to our internally calculated new MCID. Additionally, we compared ΔODI to the acceptable MCID in the literature of ≤ 6.8. A PASS threshold of ≤ 22 for ODI was set in line with previously validated measures. Results: Of the 197 patients with revision procedures, the majority were indicated for ASD (56%), followed by recurrent stenosis (28%), and non-union (15%). Our cohort's new MCID was calculated to be 10.05 and 10.23 at three months and one year, respectively. Patients who underwent revision for nonunion (81%) or recurrent stenosis (73%) were more likely to achieve MCID. Those with ASD were less likely to benefit from revision as only 52% of ASD patients achieved MCID. However, when compared to the consensus MCID in the literature we observed no significant difference in the different revision groups likely to achieve MCID. In patients who achieved MCID, mean ΔODI at one year was 27, representing a marked change in ODI. Rates of achieving one year PASS was 33% for ASD patients, 48% for nonunion, and 37% for recurrent stenosis. Risk factors for not achieving PASS were increasing BMI, and CCI. Conclusion: The majority of patients undergoing revision achieved MCID at one-year. Regardless of revision indication, the majority of patients did not achieve PASS. This underscores the need for continued improvement in managing patient’s expectations prior to surgery while raising questions about the clinical utility of the PASS measure in spine surgery as it fails to align with high rates of one-year MCID.
2318
P438: Does post-op marijuana use affect opioid consumption after spine surgery?
Michael Carter 1 , Otitochukwu Ezeonu 1 , Omar Tarawneh 1 , Rajkishen Narayanan 1 , Gregory Toci 1 , Sebastian Fras 1 , Nathaniel Pineda 1 , Shiraz Mumtaz 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Alan Hilibrand 1 , Jose Canseco 1 , Gregory Schroeder 1
1 Rothman Institute, Thomas Jefferson University, Philadelphia, USA
Introduction: The use of marijuana for pain management is a controversial topic that lacks extensive research. As social and legal acceptance of marijuana increases, questions have arisen about its therapeutic potential alongside opioids, necessitating more comprehensive studies on this topic. This study aims to explore the usage of postoperative opioids and morphine milligram equivalents (MME) among patients undergoing ACDF and lumbar fusion who have consumed marijuana, comparing them to a matched cohort of non-users. Material and Methods: A retrospective analysis covering the period from 2017 to 2021 was conducted to identify patients who had undergone ACDF and lumbar fusion and subsequently used marijuana. Age, gender, race, and BMI, Elixhauser scores, and levels fused were documented. A comparable cohort of patients who did not use marijuana post-surgery was assembled based on these criteria to facilitate comparison. Opioid utilization, including the total number of prescriptions and morphine milligram equivalents (MME) per day, was tracked for both sets of patients from one year prior to the surgery up to one year post-surgery, utilizing data from the Pennsylvania Prescription Drug Monitoring Program (PDMP). Opioid-related data was further categorized by time intervals (60-30 days and 30-0 days before surgery, 0-30 days and 30-90 days after surgery). Results: We identified 41 patients who underwent ADCF surgery who consumed marijuana and 111 matched patients who did not. We also identified 50 patients who underwent lumbar surgery who consumed marijuana and 135 matched patients who did not. No significant differences existed between either groups with regards to age (p = 0.708 ACDF, 0.508 lumbar fusion), gender (p = 0.778 ACDF, 0.982 lumbar fusion), BMI (p = 0.852 ACDF, 0.478 lumbar fusion), marital status (p = 0.978 ACDF, 0.063 lumbar fusion), DCI score (p = 0489 ACDF, 0.561 lumbar fusion), Elixhauser (p = 0.905 ACDF, 0.870 lumbar fusion), or number of levels fused (p = 0.959 ACDF, 0.866 lumbar fusion). There were no significant differences in pre-operative opioid use (p = 0.365 ACDF, 0.910 lumbar fusion), total prescriptions taken (p = 0.135 ACDF, 0.838 lumbar fusion), and total MME (p = 0.241 ACDF, 0.681 lumbar fusion) one year prior to surgery. Post-operatively, there were no significant differences in the percentage of patients using opioids 0-30 days (p = 0.661 ACDF, 0.564 lumbar fusion), 30-90 days (p = 0.906 ACDF, 0.249 lumbar fusion), and beyond 90 days (p = 0.774 ACDF, 0.694 lumbar fusion) post-operatively. There were also no significant differences in total prescriptions taken (p = 0.797 ACDF, 0.646 lumbar fusion), and total MME (p = 0.848 ACDF, 0.664 lumbar fusion) during that time. A sub-analysis of MME use revealed no significant differences from 0-30 days (p = 0.168 ACDF, 0.407 lumbar fusion), 30-90 days (p = 0.705 ACDF, 0.110 lumbar fusion), and 90-365 days (p = 0.256 ACDF, 0.470 lumbar fusion) between the marijuana group and non-marijuana group. Conclusion: Our study suggests that post-operative marijuana does not appear to impact the rate of post-operative opioid use following spine surgery. While it may not be advisable to recommend marijuana as a method to reduce postoperative opioid use, it also does not appear to be associated with increased opioid use after surgery.
2413
P439: Halo traction evaluation of cranio-cervical instability in hereditary connective tissue disorder patients: case series
Hussain Bohra 1 , Joseph Maalouly 2 , Neha chopra 2 , Charmian Stewart 2 , Ashish Diwan 2 , Kevin Seex 3 , Prashanth Rao 1
1 Department of Neurosurgery, Norwest Private Hospital, Bella Vista, Australia
2 Department of Orthopedic Surgery, Spine Service, Kogarah, Australia
3 Department of Neurosurgery, Macquarie University Hospital, Macquarie University, Australia
Introduction: Cranio-cervical instability (CCI) is a condition commonly found in patients with connective tissue disorders such as Ehlers-Danlos Syndrome (EDS), leading to various symptoms. Assessing patients for surgical fusion as a treatment for CCI is challenging due to the complex nature of EDS-related symptoms. This study aimed to evaluate the role of pre-fusion Halo traction in alleviating symptoms and determining suitable candidates for fusion surgeries. Methods: A case series of 15 EDS patients with neurological symptoms underwent halo traction between 2019 and 2022. Patients completed a CCI Questionnaire before and after the traction, reporting symptoms related to headache, vision, hearing, equilibrium, and performance. Symptom groups were assigned scores based on patient responses, with one point for each affirmative answer. The scores were statistically analyzed using a paired t-test. Patients experiencing over 50% improvement in the majority of symptoms were considered for fusion surgery, and 10 out of 15 patients subsequently underwent the procedure. Results: The average age of the patients was 31 years, with a female-to-male ratio of 14:1, consistent with existing literature. Significant improvements were observed in various symptom categories after halo traction, including headache (63% improvement, p < 0.001), brainstem functions (72% improvement, p < 0.001), cerebellar functions (59% improvement, p < 0.001), hearing (65% improvement, p < 0.001), motor functions (62% improvement, p < 0.001), vision (53% improvement, p < 0.001), cardiovascular functions (58% improvement, p < 0.05), sensory and pain (54% improvement, p < 0.001), high cortical functions (49% improvement, p < 0.01), GI functions (41% improvement, p < 0.05), bladder functions (55% improvement, p < 0.001), and Modified Karnofsky score (26% improvement, p < 0.05). Conclusion: Halo traction proved to be a simple and effective method for both evaluating patients for surgery and providing symptomatic relief in EDS-related CCI cases. It also allows surgeons to monitor patients with stable cranio-cervical junctions before committing to surgery. However, the study's limitations include the small sample size and the absence of a validated questionnaire with a scoring system.
Novel technologies
104
P440: Virtual reality as an educational tool in spinal surgery; academic stress assessment
Alberto Perez 1 , Diana Chavez 1
1 Neurocirugia, Hospitales Angeles, Ciudad De Mexico, Mexico
Introduction: Evaluation of academic stress in medical students and residents is of great interest due to the big challenges during their learning with habitual teaching methods. Use of technologies such as virtual reality offers to improve their skills with simulations and training. Main objective of this study is to qualitatively assess the stress of medical studentsand residents by combining their current learning methods with virtual reality, to improve management of stressors in their practice. Material and Methods: A questionnaire was carried out based on the evaluation of the SISCO inventory of academic stress, granting levels of stress. A virtual reality class focused on spinal surgery was given, training users with Non Nocere SharpSurgeon software platform and using Oculus Quest 2 virtual reality glasses. A second questionnaire related to the practice with virtual reality was carried out. Results: 12 students from Hospital Angeles Mexico, CDMX and 12 residents at Hospital Santa Fe, Bogota were evaluated. With an average qualitative stress of 28.50% in habitual practices and an average qualitative stress of 14.67% after virtual reality practice, determining that the use of virtual reality qualitatively improves stress levels. Conclusion: The use of virtual reality as a learning method for medical students and residents qualitatively improves stress levels. Further studies are required to define the potential uses of Virtual Reality to improve learning methods and emotional state in medical students and residents also to determine the cost - effectiveness with respect to the current forms of teaching and to validate the training as certified learning methods.
326
P441: Anterior cervical X-shape-corpectomy and fusion vs. anterior cervical corpectomy and fusion for two-level cervical spondylosis
Hong Wang 1 , Hao Liu 1
1 Department of Orthopedics, West China Hospital of Sichuan University, Chengdu City, Sichuan Province, China
Introduction: Cervical spondylosis (CS) with moderately intricate compressions, such as disc prolapse, moderate osteophytes, localized ossification of posterior longitudinal ligament (OPLL) could be challenging to treat, in which case, radical surgery is often considered. However, the choice between two mainstream surgical techniques, anterior cervical corpectomy and fusion (ACCF) and anterior cervical discectomy and fusion (ACDF), could be a dilemma that ACCF shows sufficient surgical field decompression range while ACDF has fewer adverse events. To realize better management for patients suffering from above condition, Anterior cervical X-shaped-corpectomy and fusion (ACXF) was proposed. ACXF aims to blend the strengths of both ACCF and ACDF to provide an alternative surgical option for two-level CS. ACXF was anticipated to have a broad surgical field, sufficient decompression range and fewer surgical adverse events. The purpose of this study was to verify the clinical effect of ACXF in treating two-level CS by comparing to ACCF. Material and Methods: A retrospective comparative study was conducted in two cohorts of patients who underwent ACXF or ACCF to treat two-level CS between September 2019 and May 2021. Clinical and radiographical data of all the patients were collected preoperatively and at 3 months, 6 months, and 1 year postoperatively. This was followed by intra- and intergroup analyses and comparisons. Results: A total of 57 patients were included, among whom 24 underwent ACXF and 33 underwent ACCF. The baseline data showed no intergroup significant difference. The ACXF group has significantly shorter drainage durations (2.13 ± 0.61 vs. 3.48 ± 1.30, p < 0.001) and drainage volumes (30.21 ± 26.88 vs. 69.30 ± 37.65, p < 0.001) than the ACCF group. ACXF could reach a transverse decompression range (TDR) of 11.72 ± 1.26 mm, and significantly enlarged anteroposterior canal diameter (p < 0.01) and spinal canal area (SCA) (p < 0.01). Though ACCF had a greater TDR (16.29 ± 1.91 mm, p < 0.001) and SCA (p < 0.01 for all time points) than ACXF, both techniques significantly improved clinical outcomes with comparable effects (p > 0.05). Meanwhile, every complication rate in ACXF group was lower than that in ACCF group without significant difference (p > 0.05). Two techniques had similar well performance in reshaping sagittal alignment. ACXF achieves comparable fusion rate (p > 0.05) and significantly lower subsidence rate (p < 0.01) than ACCF at all time points. Conclusion: As an innovative technique that combines ACCF and ACDF, ACXF has shown excellent clinical effects with a broad surgical field, sufficient decompression range, smaller subsidence rate and fewer complications. Thus, ACXF would be an ideal alternative treatment for part of two-level CS patients. However, further improvement and modification needs to be explored, especially about the development of ACXF-specialized internal fixation system.
360
P442: Stand-alone endoscopic/percutaneous TLIF for severe unilateral foraminal stenosis:feasibility and preliminary results
Christian Morgenstern 1 , Rudolf Morgenstern 2
1 Centro Médico Teknon, Morgenstern Institute of Spine, Barcelona, Spain
2 Endospine SLU, El Tarter, Canillo, Andorra
Introduction: Severe unilateral foraminal stenosis can be solved by direct decompression with (endoscopic) foraminoplasty and/or indirect decompression with interbody fusion. A known complication of foraminoplasty only, is the possibility of re-stenosis due to subsidence of the operated level. Endoscopic/percutaneous transforaminal lumbar interbody fusion (TLIF) is a relatively novel technique that uses Kambin’s triangle and foraminoplasty of the superior articulating process (SAP) to place an interbody device into the disk. We hypothesized that placing a stand-alone trans-Kambin TLIF cage would allow to decompress the foramen directly and indirectly, as well as avoiding long-term re-stenosis due to subsidence of the operated level. Aim of this study is to evaluate the feasibility and long-term clinical and radiologic outcome of trans-Kambin TLIF using a stand-alone interbody cage. Material and Methods: This is a prospective case series study. Inclusion criteria comprised severe unilateral foraminal stenosis. Exclusion criteria comprised instability, spondylolisthesis, severe osteoporosis, infection, tumor and vertebral body fracture. Surgically, a wide foraminoplasty was performed either percutaneously with manual reamers and/or endoscopically with a high-speed burr. After percutaneous disk preparation, a stand-alone expandable titanium interbody cage was placed into the intervertebral disk through Kambin’s triangle. Demineralized Bone Matrix was employed as graft. No posterior fixation was employed (stand-alone). Visual Analogic Scale (VAS) and Oswestry Disability Index (ODI) scores were evaluated pre-operatively and post-operatively at hospital discharge, as well as 1, 3, 6, 12, 24 months and every 12 months thereafter. Post-operative radiologic evaluation was performed with a standing X-ray and CT scan of the lumbar spine at hospital discharge and every 24 months thereafter. Statistical analysis was performed with Student’s T-Test and statistical significance was defined for p < 0.01. Results: 10 patients (3 (30%) female) were included with a mean age 71.4 ± 11.1 years. Operated level distribution was 1 at L3/L4 and 9 at L5/S1. Total mean follow-up was 36.9 ± 26.6 months (minimum 3 months; maximum 6 years). VAS back scores improved from 5.6 ± 4.0 pre-op to 1.29 ± 1.89 post-op at latest follow-up (p = 0.013). VAS leg scores improved from 7.9 ± 3.36 pre-op to 0.71 ± 1.89 post-op at latest follow-up (p < 0.001). ODI scores improved from 31.0 ± 10.36 pre-op to 9.57 ± 10.13 post-op at latest follow-up (p < 0.001). A median subsidence rate of 2mm of the interbody cages was measured and a fusion rate of 90% was radiologically assessed. Post-operative complications included one case (10%) that presented with a post-operative motor weakness of the left quadriceps (grade 4/5) that completely recovered in the follow-up. However, radicular pain persisted, and the patient underwent revision surgery elsewhere. Conclusion: According to our preliminary results, a stand-alone interbody spacer placed with endoscopic/percutaneous TLIF allows solving unilateral radicular pain caused by severe foraminal stenosis without suffering re-stenosis nor requiring revision surgery for 90% of the operated patients at a mean follow-up of 3 years (maximum follow-up 6 years). However, indications for this technique should be strict, while further research is required given the limited size of our cohort.
485
P443: A GPT-based osteoporotic question and answer chatbot and a phantom-less QCT bone mineral density measurement system
Mian Huang 1 , Yuanzhi Weng 1 , Chi Ma 1 , Huan Qi 2 , Aaron Feng Zhu 1 , William Weijia Lu 1
1 Department of Orthopaedics and Traumotology, University of Hong Kong, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, Hong Kong, Hong Kong
2 Bone's Technology (Shenzhen) Limited, Shenzhen, China
Introduction: Bone health attracts more attention recently and an intelligent question and answer (QA) chatbot for osteoporosis is helpful for science popularization. With Generative Pretrained Transformer (GPT) technology developing, we build an osteoporosis corpus dataset and then fine-tune LLaMA, a famous open-source GPT foundation large language model (LLM), on our self-constructed osteoporosis corpus. Evaluated by clinical orthopaedic experts, our fine-tuned model outperforms vanilla LLaMA on osteoporosis QA task in Chinese. Three-dimensional quantitative computed tomography (QCT) measured bone mineral density (BMD) is considered as more accurate than DXA for BMD measurement in recent years. We develop an automatic Phantom-less QCT (PL-QCT) that is more efficient for BMD measurement since no need of an external phantom for calibration. Combined with LLM on osteoporosis, our PL-QCT provides efficient and accurate BMD measurement for our chatbot users. Material and Methods: We build a novel osteoporosis corpus containing about 30,000 Chinese literatures whose titles are related to osteoporosis. The whole process is done automatically, including crawling literatures in.pdf format, localizing text/figure/table region by layout segmentation algorithm and recognizing text by OCR algorithm. We train our model by continuous pre-training with Low-rank Adaptation (LoRA, rank = 10) technology to adapt LLaMA-7B model to osteoporosis domain, whose basic principle is to mask the next word in the text and make the model predict that word. The loss function is defined as cross-entropy between the predicted and ground-truth word. Experiment is implemented on single NVIDIA A800 GPU for 15 days. Our automatic PL-QCT BMD measurement adopt AI-associated region-of-interest (ROI) generation algorithm for localizing vertebrae-parallel cylinder in cancellous bone. Due to no phantom for BMD calibration, we calculate ROI BMD by CT-BMD of personal muscle and fat. Results and Discussion: Clinical orthopaedic experts are invited to design 5 osteoporosis questions in Chinese, evaluating performance of vanilla LLaMA and our fine-tuned model. Our model outperforms LLaMA on over 80% of these questions, understanding ‘Expert Consensus on Osteoporosis’, ‘QCT for osteoporosis diagnosis’ and ‘Effect of age on osteoporosis’. Detailed results are shown in appendix. Future work may be done by training a larger LLM on the whole orthopaedics with more high-quality domain data, or a multi-modal GPT combining and understanding X-ray and medical text for orthopaedic computer-aided-diagnosis. However, GPT model gives unexpected outputs sometimes, such as repetitive text or seemingly normal but wrong answer (called ‘hallucination’). Even though GPT give correct answers, it cannot be considered as valid clinical diagnoses instead of clinical doctors. The PL-QCT BMD system provided by Bone’s QCT (Bone’s Technology - Shenzhen) Limited) achieves 0.1448mg/cm2 (spine) and 0.0002 mg/cm2 (hip) mean absolute error (MAE) and linear correlation coefficient R2 = 0.9970 (spine) and R2 = 0.9991 (hip) (compared to QCT-Pro (Mindways)) on 155 patients in three-center clinical trial in Guangzhou. Conclusion: This study builds a Chinese osteoporosis corpus and develops a fine-tuned and domain-adapted LLM as well as a PL-QCT BMD measurement system. Our fine-tuned GPT model shows better capability than LLaMA model on most testing questions on osteoporosis. Combined with our PL-QCT BMD system, we are looking forward to providing science popularization and early morning screening for potential osteoporotic patients.
496
P444: Design and development of a novel positioning device used to monitor pressure over the iliac crest of patients in the prone position using pattern recognition to highlight at risk patients intra-operatively
Nikki Sizer 1 , Charly Dalbert 2 , Steffen Loeser 2 , Yang Wei 3 , Julia Fleischer 4 , Pascal Stark 4 , Francesco Siena 5 , Philip Breedon 1
1 Medical Engineering Design Research Group
2 R&D Innovation Team, Baxter Medical Systems GmbH+ Co. KG, Saalfeld, Germany
3 Smart Wearable Research Group, Department of Engineering
4 Inter-Spitzen AG, Business Unit FRTI, St Gallen, Switzerland
5 Product Design Department, Nottingham Trent University, Nottingham, United Kingdom
Introduction: Hospital acquired pressure injuries (HAPIs) are associated with known risk factors including decreased mobility, surgical duration, vasopressor infusion, excessive moisture, and altered perfusion. HAPIs are still mostly unexamined in the critical care population [1] with very few risk assessments taken intra-operatively; patients who undergo surgery and older than 65 years are higher risk compared to younger patients acquiring PIs [2,3]. Peri-operatively, skin assessment is performed pre/post-operatively. With high-risk surgeries ranging up to 6+ hours, patients’ skin is left unobserved. Subsequently post-operative PIs occur. Pressure relieving devices have been developed for other hospital settings such as the use of redistribution and low air mattresses or manual repositioning [4]. However, during surgeries such as spinal surgeries this is impossible. In most cases the use of these redistribution devices is impossible to integrate intra-operatively as they could distract, cause injury to the patient and disrupt the clinician’s workflow. The prevalence of PIs in surgical patients undergoing spinal surgery in prone position was 23% [5], thus supporting further investigation into intra-operative monitoring or assessment during surgery. This research investigates the use of intra-operative sensors to identify patients at risk of developing a PI during surgery. Materials and Methods: A study was conducted to determine location of bone and high-pressure areas on a carbon spinal frame provided by Baxter Healthcare. Participants were placed in the prone position for 5 minutes and documented their perceived comfort levels using a visual analog scale and complete a survey on their demographic information. To collect data from suspected bone/ high pressure areas, pressure sensor matrices were developed. The sensor matrices comprised of four, 16x16 custom flat matrices designed to be integrated to the specific frame and are connected to a microcontroller. Analog signals are collected/ processed into data visualisation and data collection; visualisation is collected every 10 seconds (10000 milliseconds) with jpeg files created of each 10 second frame in MATLAB. Each frame was analysed using Unsupervised Classification methods identifying image patterns. Results: The results collected in the ongoing study that have been examined have highlights themes/questions, these themes include:
- Can the sensor data be used in the initial stages of patient positioning to limit areas of high pressure; can it be used as a positioning aid to mitigate and reduce the risk of PI development.
- Can pattern recognition be used to identify those at higher risk intra-operatively during positioning and throughout surgery and assist in streamlining incident reporting of pressure injuries peri-operatively.
- When comparing the pattern recognition and BMI of the participants do the results create a U-shaped relationship where the pattern recognition shows a participant at a either extremes of BMI (extremely low and extremely high) are at higher risk of PIs than those at a normal range of BMI.
Conclusion: The study findings identify patients at risk of PI development by use of pattern recognition thus providing an opportunity to monitor the risks of PI development intra-operatively demonstrating the need for integration of intra-operative risk assessment scales to help streamline incident reporting.
References
1. Tayyib N, Coyer F, Lewis P. Saudi Arabian adult intensive care unit pressure ulcer incidence and risk factors: a prospective cohort study. Int Wound J 2016; 13(5): 912-919. doi:https://doi.org/10.1111/iwj.12406
2. Chen HL, Chen XY, Wu J. The incidence of pressure ulcers in surgical patients of the last 5 years: a systematic review. Wounds 2012; 24(9); 234-241.
3. Alderden J, Rondinelli J, Pepper G, Cummins M, Whitney J. Risk factors for pressure injuries among critical care patients: a systematic review. Int J Nurs Stud 2017; 71: 97-114.
4. Wang L, Jones D, Chapman GJ, et al. A Review of Wearable Sensor Systems to Monitor Plantar Loading in the Assessment of Diabetic Foot Ulcers. IEEE Trans Biomed Eng 2020; 67: 1989-2004. DOI: https://doi.org/10.1109/TBME.2019.2953630. [PubMed], [Web of Science ®], [Google Scholar]
5 Lin S, Hey HW, Lau ET, et al. Prevalence and Predictors of Pressure Injuries From Spine Surgery in the Prone Position: Do Body Morphological Changes During Deformity Correction Increase the Risks? SPINE. 2017 Nov 15; 42(22): 1730-1736. doi:10.1097/BRS.0000000000002177.
558
P445: Evaluation of the basal metabolism of degenerative lumbar intervertebral discs based on Pfirrmann Grade and presence of instability
Chaiyapruk Pundee 1 , Theodore Choma 2 , Don Moore 2
1 Orthopedics, Samitivej Srinakarin Hospital, Bangkok, Thailand
2 Orthopedics, Missouri Orthopedic Institute, Columbia, USA
Introduction: Intervertebral disc (IVD) degeneration is implicated in back pain, a leading cause of spine-related disability. It may also cause segmental instability. Both local and systemic inflammatory processes have been implicated in the pathophysiology of IVD degeneration, though it is unclear if Pfirmann grade severity or presence of instability affects degenerative IVD metabolism. These differences have not previously been investigated. Hence, this study was designed to examine the basal metabolism of degenerative lumbar IVD tissues collected from patients undergoing lumbar microdiscectomy or fusion with the hypothesis that tissues from patients with higher Pfirmann grades and those with radiologic evidence of instability would produce significantly higher levels of degradative enzymes and inflammatory mediators. Material and Methods: Tissue Collection and Culture: With IRB approval (IRB#2010692) and informed patient consent, degenerative IVD tissue excised as part of a standard-of-care spinal surgery, which would otherwise be discarded was obtained from patients (n = 7, mean age 53, 4 female) being treated for symptomatic degenerative lumbar IVD disorders. Pfirmann grading (0-5) of the IVD was determined by evaluation of MRI by a single reviewer (grade 3 n = 3, grade 4 n = 4), and for instability as defined by the presence of a spondylolisthesis on upright lateral radiographs by two reviewers (unstable n = 2, stable n = 5). Tissues comprised of degenerative nucleus pulposus (NP) were collected and explants were created with a 6 mm diameter biopsy punch. Two explants per disc were cultured for 3 days, after which media were collected for biomarker evaluation. Media Analyses: Media were tested for MMP-1, MMP-2, MMP-3, MMP-7, MMP-8, MMP-9, MMP-13, TIMP-1, TIMP-2, TIMP-3, TIMP-4, GRO-α, MCP-3, PDGF-AA, PDGF-AB/BB, IL-2, IL-4, IL-6, IL-8, MCP-1, MIP-1α, MIP-1β, RANTES, TNF-α, and VEGF using commercially available assays according to the manufacturer’s protocol. Statistical analysis: Significant differences between groups were determined by t-test or rank sum test based on normality of the data using SPSS with significance set at p ≤ 0.05. Results: In this study, we did not identify any significant differences between basal biomarker production by degenerative IVD tissues of Pfirmann grade 3 versus 4 discs. However, tissues from degenerative IVDs with instability were found to produce significantly higher levels of MMP-8, and significantly lower levels of MMP-1, MMP-2, and MMP-13 compared to tissues from stable spine. Conclusion: The data from this study indicates that there is not a significant difference in the metabolism of IVD tissues with a Pfirrmann grade of 3 or 4. However, the presence of instability in the degenerated lumbar IVD resulted in a significant increase in the production of MMP-8, but the production of other degradative enzymes was significantly decreased. Further study is required to determine how observable changes in IVD architecture relates to changes in tissue metabolism, as understanding how gross findings of IVD degeneration relate to its pathophysiology may provide insight into potential therapies for prevention and treatment of lumbar intervertebral disc degeneration.
560
P446: Basal and cytokine-stimulated biomarker production by degenerative lumbar discs from microdiscectomy versus interbody fusion patients
Chaiyapruk Pundee 1 , Theodore Choma 2 , Don Moore 2
1 Orthopedics, Samitivej Srinakarin Hospital, Bangkok, Thailand
2 Orthopedics, Missouri Orthopedic Institute, Columbia, USA
Introduction: Intervertebral disc (IVD) degeneration is implicated in back pain, a leading cause of a spine-related disability. Both local and systemic inflammatory processes have been associated with IVD degeneration, though it is unclear if differences between these processes exist in degenerative IVDs of patients undergoing lumbar microdiscectomy versus lumbar interbody fusion. To the authors’ knowledge, these differences have not previously been investigated. Hence, this study was designed to examine basal and cytokine-stimulated metabolic responses of degenerative lumbar IVD tissues collected from patients undergoing lumbar microdiscectomy or interbody fusion with the hypothesis that tissues from patients undergoing fusion would produce significantly higher levels of degradative enzymes and inflammatory mediators under both basal and cytokine-stimulated conditions when compared to tissues from microdiscectomy group. Material and Methods: Tissue Collection and Culture: With IRB approval (IRB#2010692) and informed patient consent, degenerative IVDs excised as part of a standard-of-care spinal surgery, which would otherwise be discarded after lumbar microdiscectomy (n = 3) or fusion (n = 4) surgery was obtained from patients (n = 7, mean age 53, 4 female) being treated for symptomatic degenerative lumbar IVD disorders. Tissues comprised of degenerative nucleus pulposus (NP) were collected and explants of combined NP were created with a 6 mm diameter biopsy punch. Two explants per disc were randomly assigned to the 10ng/ml IL-1β stimulation group (IL) or the untreated basal metabolism group (BASAL). Tissues were cultured for 3 days, after which media were collected for biomarker evaluation. Media Analyses: Media were tested for MMP-1, MMP-2, MMP-3, MMP-7, MMP-8, MMP-9, MMP-13, TIMP-1, TIMP-2, TIMP-3, TIMP-4, GRO-α, MCP-3, PDGF-AA, PDGF-AB/BB, IL-2, IL-4, IL-6, IL-8, MCP-1, MIP-1α, MIP-1β, RANTES, TNF-α, and VEGF using commercially available assays according to the manufacturer’s protocol. Statistical analysis: Significant differences between groups were determined by t-test or rank sum test based on normality of the data using SPSS with significance set at p ≤ 0.05. Results: In the BASAL group, only the production of MMP-8,TIMP-4 and PDGF AA was significantly higher in the IVD tissues from the fusion cohort compared to the microdiscectomy group. In response to cytokine stimulation with IL-1β, tissues in the fusion group responded with significantly greater production of TIMP-2, TIMP-4, PDGF-AA, IL-6, IL-8, MIP-1β, and VEGF when compared to the response by the tissues from the microdiscectomy patients. Conclusion: These findings indicate that the basal inflammatory and degradative metabolism of degenerative lumbar IVD tissues collected from lumbar microdiscectomy versus fusion patients was not significantly different, since MMP-8 and TIMP-4 were the only biomarkers significantly different between the two patient groups. However, tissues from the lumbar fusion patients do appear to be more sensitive to cytokine stimulation compared to those from the microdiscectomy cohort. The biochemical processes underlying, and clinical significance of, this observed difference require further study. A deeper understanding of this phenomenon may provide insight into potential therapies for prevention and treatment of lumbar intervertebral disc degeneration.
621
P447: Analysis of the efficacy and safety of posterior ultrasound bone scalpel two-step decompression with internal fixation for the treatment of thoracic spinal stenosis
Le-qun Shan 1
1 Oncologic and Degenerative Spine Surgery, Xi’an Honghui Hospital, Xi’an, Shaanxi, China
Introduction: To compare the clinical efficacy of ultrasound bone scalpel two-step decompression and traditional laminectomy with pedicle screw fixation for treating thoracic spinal stenosis. Material and Methods: We retrospectively analyzed 50 patients with thoracic spinal stenosis who were treated from October 2016 to October 2021. Among them, 25 patients were treated with ultrasound bone scalpel two-step decompression and posterior internal fixation (observation group), and 25 patients were treated with traditional laminectomy with pedicle screw fixation (control group). We compared the surgical time, intraoperative decompression and fixation segments, intraoperative blood loss and transfusion volume, postoperative drainage volume and drainage time, intraoperative and postoperative complications, and other indicators between the two groups. In addition, we used the Japanese Orthopaedic Association (JOA) score and the American Spinal Injury Association (ASIA) classification to evaluate the patients' neurological function. Results: Compared with the traditional method, the observation group showed better results in surgical time, intraoperative decompression and fixation segments, intraoperative blood loss and transfusion volume, postoperative drainage volume and drainage time. There was no significant difference in the preoperative JOA score between the two groups, but at the last follow-up, the JOA score of the ultrasound bone scalpel two-step decompression group was significantly higher than that of the traditional method control group (p < 0.05). There was no significant difference in the incidence of intraoperative and postoperative complications between the two groups. Conclusion: The results of this study show that ultrasound bone scalpel two-step decompression for thoracic spinal stenosis has advantages of shorter surgical time, less blood loss, less drainage volume, and shorter hospital stay compared with traditional decompression methods. Although there was no significant difference in the incidence of complications between the two groups, ultrasound bone scalpel two-step decompression is safer and more reliable while ensuring surgical efficacy. Therefore, ultrasound bone scalpel two-step decompression can be considered as an effective surgical method for treating thoracic spinal stenosis.
635
P448: Comparison study of lumber nerve root block under ultrasound and fluoroscopy guidance
Le-qun Shan 1
1 Oncologic and Degenerative Spine Surgery, Xi’an Honghui Hospital, Xi’an, Shaanxi, China
Introduction: The aim of this study was to compare the accuracy and effectiveness of Selective nerve root closure of lumbar vertebrae under ultrasound guidance and fluoroscopy guidance, and to explore the feasibility of ultrasound guidance. Material and Methods: This retrospective study included patients with lumbar nerve root disease who underwent selective nerve root block under ultrasound or fluoroscopy guidance at the Affiliated Honghui Hospital of Xi'an Jiaotong University from August 2020 to August 2022. The patients were divided into the U-SNRB group (ultrasound-guided selective nerve root block) and the F-SNRB group (fluoroscopy-guided selective nerve root block). A total of 43 patients were included in the U-SNRB group and 20 patients in the F-SNRB group. The visual analogue scale (VAS) scores and Japanese Orthopaedic Association (JOA) scores before block, 30 minutes after block, 1 month after block, and 6 months after block were recorded and compared between the two groups. The feasibility, accuracy, and effectiveness of ultrasound-guided nerve root block were evaluated. Results: No complications were reported during the nerve root block procedure in either group. The operation time and number of needle angle adjustments in the U-SNRB group were superior to those in the F-SNRB group, with statistically significant differences (p < 0.05). The VAS scores and JOA scores at 30 minutes, 1 month, and 6 months after block were significantly improved compared to before block in both groups, with statistically significant differences (p < 0.05). There was no statistically significant difference between the two groups (p > 0.05). Conclusion: The accuracy and degree of pain relief of ultrasound-guided selective nerve root block are similar to fluoroscopy guidance, but the operation time and number of needle angle adjustments are significantly less than fluoroscopy, and it can effectively reduce radiation exposure. Therefore, ultrasound guidance can be considered as a preferred guidance method for selective nerve root block.
641
P449: Application of 3D model prefabricated nail path technology in atlantoaxial pedicle screw implantation
Le-qun Shan 1
1 Oncologic and Degenerative Spine Surgery, Xi’an Honghui Hospital, Xi’an, Shaanxi, China
Introduction: This study aims to explore the main clinical value of 3D model prefabricated nail path technology in atlantoaxial pedicle screw implantation. Material and Methods: We retrospectively analyzed the data of patients who underwent atlantoaxial pedicle screw implantation with the assistance of 3D printed models from January 2018 to December 2022. The patients were divided into two groups: the 3D printed guide group (15 cases) and the 3D printed prefabricated nail path group (12 cases). Preoperative thin-layer CT scans, medical image sampling, computerized modeling of the atlantoaxial joint, and determination of the optimal pedicle screw trajectory were performed. In the 3D printed nail path group, the nail path was directly printed, and the pedicle screw entry point and trajectory parameters were measured. Intraoperatively, the pedicle screws were placed based on anatomical landmarks. In the 3D printed guide group, the anatomical data of the atlantoaxial pedicle, spinous process, lamina, and lateral mass were collected, and the optimal pedicle screw trajectory was designed. A reverse template was then created. Intraoperatively, the navigation template was securely fixed to the atlantoaxial joint to assist in pedicle screw placement. The observed indicators included VAS score, JOA improvement rate, operation time, and blood loss. Results: Both groups had successful surgeries without any surgery-related complications. The postoperative ODI score and VAS score in both groups were better than those before surgery (p < 0.05). There were no significant differences in operation time, intraoperative blood loss, and postoperative hospital stay between the two groups (p > 0.05). Postoperative CT examination showed no significant difference in the success rate of screw placement between the two groups according to the Kawaguchi classification. However, in some cases of complex atlantoaxial fractures and dislocations, the navigation template did not match well after general anesthesia and skull traction, which posed certain difficulties in the operation. Conclusion: The application of 3D model prefabricated nail path technology in atlantoaxial pedicle screw implantation is recommended as it improves the accuracy of screw placement, enhances patient safety, and may have advantages in complex atlantoaxial fracture and dislocation surgeries.
833
P450: Initial experience in the first 62 robot-guided screws for spinal surgery fellowship as part of a highly experienced center
Pablo de la Fuente 1 , Maria Dolores Varela 1 , Pablo Clavel 1
1 Neurosurgery, Clavel, Barcelona, Spain
Introduction: Robot-guided spinal surgery has experienced exponential rise in recent years. However, due to the novelty of this technology, there is limited literature regarding the learning curve, specially when considering a fellow or a young spine surgeon. Material and Methods: The recorded data on the first 62 robot-guided screws for a Neurosurgeon in his first year of fellowship are analyzed. We looked at the type of pathology, the specific procedure performed, precision of screw placement (Gertzbein-Robin classification), set up time, time per screw, X-ray time per Screw, X-ray dose per screw, total surgical time complications, and need for revision. Results: A total of 62 screws were placed in 12 patients. The most frequent surgery was percutaneous instrumentation after Anterior lumbar interbody fusion (ALIF). Set up time ranged between 27 and 60 minutes, (mean 46 min). No registration or merge issues was recorded. The time per screw varied between 3.75 minutes and 13.3 minutes (mean 7.55 min). Total surgical times ranged from 85 to 168 minutes (mean 115 min). X-Ray time per screw varied between 4.25 and 22.5 seconds. (Mean 11.2 secs). The Gy/cm2 per screw varied between 0.32 and 1.74 (mean 0.92Gy/cm2/screw). All screws presented an ''A'' in the Gertzebein robin classification on postoperative CT and no patient required surgical revision related to instrumentation or for any other reason. Conclusion: Robot-guided spinal instrumentation is a safe and precise procedure from the first cases for a spine surgeon in training, when he is part of a high-volume and experienced spine surgery team. It is important to emphasize that having a dedicated and experienced nursing and robot operating technical team, helped to overcome the potential complications in a learning young surgeons curve.
976
P451: Intraoperative radiotherapy combined with spinal stabilization surgery. A novel treatment strategy for spinal metastases
Ehab Shiban 1 , Maximilian Bonk 1 , Klaus-Henning Kahl 2 , Krauss Philipp 1
1 Department of Neurosurgery
2 Department of Radiooncology, University Hospital Augsburg, Germany
Introduction: Contemporary treatment of spinal metastases (SM) aims on preserving spinal stability, neurological status, local control and functional status. It consists of spinal surgery followed by radio- and chemotherapy. Adjuvant therapy is performed after several weeks to prevent wound healing issues. Intraoperative radiotherapy (ioRT) is a solution to shorten treatment time, successfully applied in brain tumor, breast and colorectal surgery but not SM to date. Objective: We describe the feasibility, morbidity and mortality of a novel treatment protocol for SM combining spinal stabilization surgery with ioRT. Methods: Results on morbidity and mortality of ioRT combined with stabilization surgery in SM in a first single center series are described. Stabilization is performed as CT-navigated open or percutaneous procedure using a carbon screw-rod system followed by 50kV photon-ioRT using the ZEISS Intrabeam during a single session in prone position. The ioRT probe is placed through a guide canula via navigation and positioning is controlled by ioCT to enable RT isodose planning in the OR. Patient characteristics, perioperative specifications and postoperative follow up along with adverse events (AE) are reported. Results: 11 (7 female) patients (69 ± 9.4 y) received treatment from 07/22-04/23. Median SINS was 8 [7-10] IQR, with metastasis located in thoracic (n = 9) and lumbar (n = 2) spine. 6 patients receive open, 4 percutaneous stabilization and 1 decompression only. Mean length of surgery was 153 ± 52 min. with 2 Patients receiving 4 and 8 patients receiving 8 screws respectively. In 2 Patients radiotherapy was not completed due to bending of the guide canula with consecutive security abortion of ioRT. All other patients received 8Gy isodoses during 2-6 min. Patients treated had ESCC 1a-2. Mean follow up was 63 ± 49 days. 4 patients experienced AEs including 1 case of fatal surgical site infection. Conclusion: 50kV photon ioRT for SM can be a promising technique for selected cases of SM.
1001
P452: Augmented reality technology in minimally invasive spine surgery: case reports and literature review
Chiruei Li 1 , Chung-Hsin Lee 1
1 Department of Neurosurgery, Neurological Institute, Taichung Veterans General Hospital, Taichung City, Taiwan
Introduction: Throughout the past decade, navigational systems have helped improved the accuracy of spine instrumentation. When compared with traditional free-hand techniques, the systems provide accuracy from 93.0% to 98.5%, as seen in the available literature. Nevertheless, these navigational systems are limited due to their shortcoming to shift the attention of the operator. To address the limitations of current navigation systems, Augmented Reality (AR) surgical technology is designed to facilitate instrumentation efficiency and precision, while offering surgeons real-time feedback on precise anatomical locations. Material and Methods: In this article, we present 3 patients diagnosed with L4-5 spondylolisthesis. These patients received AR-assisted minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) surgery under AR-based navigation. After the AR-assisted MIS-TLIF surgery, patient’s post-operative image data, intraoperative blood loss, operation time and VAS score were all documented compared with existed data and literature. Results: Correct screws position was documented using final intraoperative computed topography. Postoperatively, these 3 patients showed promising relief in symptoms. All patients were mobilized uneventfully soon after surgery and discharged on the fourth and sixth day, respectively. Conclusion: Due to the progress currently being seen in AR technology, this novel technique will likely be increasingly adopted for use in both surgical applications and education. Despite its limitations of high set-up and maintenance costs, the AR technique still has the potential to provide promising results, not only in conventional spine surgery but also in deformity pathologies or tumor resection surgery. Further larger cohorts taken from randomized studies are still needed to confirm the procedure’s accuracy and effectiveness.
1112
P453: A novel retractor (Teijin Nakashima, Japan) for the cervical anterior approach
Takahiro Iizuka 1 , Tetsuro Takai 1 , Toyohito Iwami 1 , Hiroshige Debata 1 , Tokuji Kashiro 1
1 Orthopedic Spine Surgery, Kouseikai Takai Hospital, Nara, Japan
Introduction and Background: Spinal surgery based on surgical technologies is supported by surrounding devices like microscopes, endoscopes, retractors, screws, and rods. Muscle retractors play important roles in spinal surgeries for a wide and clear view during surgeries. Cervical anterior approach requires retraction of the trachea, the esophagus, and the internal carotid artery. Conventional cervical retractors provide a wide view of the anterior aspect of the cervical spine. However, we experienced sometimes a retractor slippage in the surgical site. This slippage may cause severe damage to surrounding organs. For example, esophagus tear and over-compression to the carotid artery are quite severe complications of the cervical anterior approach. Material and Methods: We report a Novel Cervical Retractor designed for the anterior approach. This retractor is a directory connected to the operation table with long steel bars that are flexible. This retractor is able to fix at any place you like. 1. Secure the surgical site at just the center of cervical vertebrae. 2. Prevent inadequate retractor movement during surgeries. 3. Prevent over-compression to the Carotid artery. We would like to introduce this retractor for the cervical anterior approach showing surgery with pictures and videos. Conclusion: We believe we must pay more attention to every organ like the esophagus, trachea, and carotid artery though the surgeon tends to surgery itself while the cervical anterior approach. Two types of retractor blades are available widely. One is sharp engaging Longus Coli Muscles and the other is round spreading anterior cervical vertebrae. The sharp blade is often dislodged without noticing. This dislodgement is quite dangerous for surrounding organs. If you spread the space with conventional blades, the retractor will press soft tissues with the same compression force to the carotid artery and the esophagus. We are able to lessen the compression force to the carotid artery and fix this device by connecting it to the operation table. We recommend using this type of retractor for the anterior cervical approach in terms of preventing unexpected dislodgement of retractors and safety for surrounding soft tissues.
1162
P454: Can pre-perfusion of bone wax and gelatin sponge further reduce bone cement leakage than pre-perfusion of gelatin sponge alone during percutaneous kyphoplasty? A retrospective case-controlled study with a 2-year follow-up
Chao-Yuan Ge 1 , Ding-Jun Hao 1
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
Introduction: Although pre-perfusion with gelatin sponge (GS) in percutaneous kyphoplasty (PKP) has been proven to effectively prevent bone cement leakage (BCL), it is unknown if pre-perfusion of bone wax (BW) and GS could be more potent. We aimed to evaluate the effect of pre-perfusion of BW and GS to reduce BCL during PKP. Material and Methods: We retrospectively analyzed the prospectively collected data of patients with single-level painful osteoporotic vertebral compression fracture (OVCF) who underwent PKP between January 2016 and December 2018. They were divided into group A (pre-perfusion of GS only) and group B (pre-perfusion of BW and GS). Clinical outcomes in terms of visual analogue scale (VAS) scores of backpain, Oswestry disability index (ODI) and BCL during PKP were compared between the two groups. Results: A total of 426 patients were included in this study, including 106 males and 320 females, with an average age of 69.6 ± 5.6 years. Among them, 216 patients in group A and 210 patients in group B. The average follow-up time was 28.8 ± 5.6 months. All patients in both groups showed significant improvements in VAS and ODI scores compared with their preoperative values after the surgery; these improvements remained significant until the last follow-up (p < 0.05). However, there was no significant difference between the two groups (p > 0.05). The overall incidence rates of BCL and anterior leakage, respectively, were 19.5% (42/216) and 6.5% (13/216) in group A and 11.9% (25/210) and 0.5% (1/210) in group B. Thus, group B showed significantly lower rates of BCL and anterior leakage than group A (p < 0.05). Conclusion: Either pre-perfusion of BW and GS or GS alone during PKP could both achieve satisfactory clinical outcomes for patients with painful OVCF. However, pre-perfusion of BW and GS could further reduce BCL compared with pre-perfusion of GS alone, especially leaking forward.
1181
P455: Percutaneous vertebroplasty in lateral position for elderly patients with acute osteoporotic thoracolumbar fractures
Chao-Yuan Ge 1 , Ding-Jun Hao 1
1 Department of Spine Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
Introduction: For some elderly patients with acute osteoporotic vertebral compression fractures (OVCFs) that cannot tolerate prone position during surgery of percutaneous vertebroplasty (PVP), We proposed to perform PVP in the lateral position. The aim of this study is to investigate the safety and clinical effect of PVP in the lateral position. Material and Methods: A retrospective analysis was performed on 36 elderly patients with acute OVCFs who underwent PVP in lateral position in our hospital from January 2016 to December 2020, including 12 males and 24 females, with an average age of 68.2 ± 5.3 years. The reasons for the failure to tolerate prone position included severe pulmonary heart disease, combined with fracture of one limb or rib. The PVP surgery was performed in 16 patients with left lateral position, and 20 patients with right lateral position. The VAS score and ODI index of patients were compared before and 24 hours after surgery, 3 months, 6 months, 12 months after surgery and at the last follow-up, to evaluate the surgical treatment effect, and the intraoperative bone cement diffusion and leakage were also recorded. Results: All patients were successfully operated and followed up for an average of 42.5 ± 5.6 months. VAS scores were (8.2 ± 1.2), (4.3 ± 0.7), (3.7 ± 0.6), (2.2 ± 0.6), (1.8 ± 0.2), (1.2 ± 0.3) before surgery, 24 hours after surgery, 3 months, 6 months, 12 months and the last follow-up, respectively. ODI scores were (64.1 ± 16.0), (48.2 ± 16.2), (41.9 ± 15.8), (35.2 ± 14.8), (31.3 ± 12.8), (16.6 ± 8.6), respectively. VAS scores and ODI scores were significantly improved after surgery and during follow-up compared with those before surgery (p < 0.05). During the operation, bone cement was well dispersed to both sides of the injured vertebra. Bone cement leakage occurred in 2 cases, with an incidence of 5.6%, including 1 case leaking to the paravertebral space and 1 case leaking to the intervertebral space. No corresponding symptoms were produced and no special treatment was given. Conclusion: For elderly patients with acute OVCFs who cannot tolerate PVP in prone position, PVP in lateral position can significantly improve the symptoms of low back pain, significantly improve the quality of life, and have fewer complications.
1331
P456: Artificial Intelligence in the management of adolescent idiopathic scoliosis
Aaron Hui 1 , Samuel Goldman 1 , Sharlene Choi 1 , Emmanuel Mbamalu 1 , Parsa Tirabady 1 , Jaime Gomez 1 , Ananth Eleswarapu 1 , Leila Alvandi 1 , Eric Fornari 1
1 Department of Orthopaedics, Montefiore Medical Center, New York, USA
Introduction: Adolescent idiopathic scoliosis (AIS) is a common spinal deformity mainly affecting adolescent girls, with a lateral spine curve > 10°, vertebral rotation, and reduced thoracic kyphosis. Disease variability complicates care, making treatment decisions challenging. AI and ML have recently gained importance in orthopedic care, showing promise in diagnosis, outcome prediction, and treatment guidance. This systematic review explores AI's potential applications in AIS, offering a comprehensive overview. Materials and Methods: This study followed PRISMA guidelines and focused on pediatric populations, humans, and English-language studies. It used a combination of MeSH and free text searches in titles and abstracts, along with a topic search in Web of Science Core Collection. COVIDENCE software managed the identified literature. Included articles reported the development, use, or validation of AI models in pediatric orthopedics for treating, diagnosing, or predicting clinical outcomes in adolescent idiopathic scoliosis, regardless of publication year. Excluded were editorials, conference abstracts, technique papers, non-English studies, reviews, meta-analyses, overviews, systematic reviews, and studies lacking AI or AIS content. Results: The initial search yielded 7,882 articles, with 7,741 meeting title and abstract screening criteria after removing duplicates. Following full-text review, 41 studies were included. Commonly employed machine learning techniques included convolutional neural networks (53.6%), decision trees/random forests (14.6%), artificial neural networks (14.6%), and support vector machines (12.2%). AIS-related AI applications predominantly focused on AIS prediction (68.2%), categorized into AIS progression (57.1%), Cobb angles (50%), and clinical outcomes (17.8%). Additionally, AI played a significant role in radiographic imaging (56%), contributing to AIS identification (47.8%), classification (39%), and spine segmentation (34.8%). Clinical decision support accounted for 9.8% of applications. Radiographic imaging was the primary input feature (92.6%), with 44.7% incorporating 3D spine modeling. Key radiographic features included Cobb angle (94.7%), apical vertebra (28.9%), lumbar lordosis angle (28.9%), and axial rotation (23.7%). The mean Cobb angle across studies was 30.4º, ranging from 11.4º to 62.7º. Training sets averaged 702 patients with an average age of 13.8 (range 9-18). Validation techniques included fold cross-validation (36.6%), unspecified cross-validation (22.0%), and leave-one-out cross-validation (12.2%). The AI achieved an average accuracy of 86.8%, assessed on an average of 276 patient radiographs. Conclusion: This systematic review assessed AI and ML applications in complex AIS care. It highlighted ML techniques (CNN, ANN, decision trees, and random forests) trained on radiographic imaging for AIS detection, progression, and decision support. AI has potential for better outcomes, reduced radiation exposure, and individualized predictions, with room for further research on clinical outcomes and image-guided surgery in AIS.
1576
P457: Awake micro-endoscopic discectomy without fluoroscopy performed in a 14-week pregnant lady in lateral decubitus position and use of a novel marking technique: a case report
Saurabh Kapoor 1 , Dr Muralidharan Venkatesh 2 , Neha Jain 3 , Munish Khurana 4 , Sonal Bathla 5 , Mohanjeet Juneja 4 , Shekhar Srivastav 6
1 Spine Surgery
2 Spine Surgery, Apollo Hospital, Chennai, India
3 Radiology
4 Anaesthesia
5 Gynaecology
6 Orthopaedic Surgery, Sant Parmanand Hospital, New Delhi, India
Background: Severe lumbar radiculopathy pain during pregnancy requiring surgical intervention poses significant risks to foetal and maternal health from use of potentially teratogenic general anaesthetic drugs, prone positioning and intra-operative radiation from fluoroscopy. Case Report: A 28-year-old 14 weeks primigravida patient suffering from severe lumbar radiculopathy due to right sided L5-S1disc herniation was offered a discectomy procedure after failed conservative treatment. A multidisciplinary team including anaesthetists, gynaecologist, radiologist and spine surgeon was constituted. A novel two-tier marking technique utilizing ultrasonography and magnetic resonance imaging (MRI) was used to accurately plan the L5-S1 surgical incision. The surgery was performed under spinal anaesthesia in left lateral decubitus position to avoid pressure on foetus and inferior vena cava. A tubular minimally invasive approach was used to access the L5-S1 disc. No intra-operative fluoroscopy marking was used. Post-operatively patient reported complete relief from radiating right leg pain and MRI confirmed adequate nerve decompression. Post-operative foetal scans were performed at regular intervals which were normal. Patient delivered a normal term baby girl without any complications. Conclusion: Our two-tier marking technique and use of regional anaesthesia in lateral decubitus position avoids potentially teratogenic general anaesthetic agents and intra-operative radiation. It can be used to effectively decompress lumbar spine disc herniation and represents an advancement in ensuring safe spine surgery in pregnant females.
Keywords: pregnancy, awake spine surgery, regional anesthesia, fluoroscopy
1601
P458: Detecting perioperative body composition changes in elective spine surgery through bioimpedance analysis
Sarah Ryan 1 , Alex Coffman 1 , Catherine Olinger 1 , Natalie Glass 1 , Cassim Igram 1 , Andrew Pugely 1 , Ariana Dalamaggas 1 , Gage Christenson 1
1 Orthopedics and Rehabilitation, University of Iowa, Iowa City, USA
Introduction: The prevalence of degenerative spinal disease continues to increase in the US population, creating an expanding number of potential surgical candidates. Although body mass index (BMI) is a common tool for perioperative risk assessment, it provides an incomplete picture of body composition and overall health. Sarcopenia, characterized as low muscle mass or quality, is an independent predictor of perioperative complications and mortality after spine surgery. In conjunction with elevated BMI, this is termed ‘sarcopenic obesity’. The purpose of this study is to establish the prevalence of sarcopenia, sarcopenic obesity, and other body composition parameters among elective spine surgery candidates and monitor longitudinal body composition trends in this patient cohort. Material and Methods: A total of 97 patients (47 males, 50 females) between ages 21-81 were enrolled. Patients underwent bioimpedance analysis (BIA) scans at the preoperative visit, which collects body composition variables including weight, body mass index (BMI), skeletal muscle mass (SMM) and appendicular skeletal muscle index (SMI). Sarcopenia is defined as SMI < 8.5 kg/m2 for men and 6.3 kg/m2 for women. Results: The median age, BMI, and skeletal muscle index (SMI) of patients at enrollment were 61.35 ± 13.1 years, 31.67 ± 5.9 kg/m2, and 8.17 ± 1.45 kg/m2, respectively. 52% of participants were female (n = 50). At 6 weeks post-procedure, patients experienced an average weight loss of 2.19 lbs (p = 0.12), a decrease in SMM by 1.81 (p = 0.36), and a decline in SMI by 0.43 (p = 0.87). Preoperatively, 19% of patients met the criteria for sarcopenia (n = 18) and 4% met the criteria for sarcopenic obesity (n = 4), while over half of patients were obese (BMI > 30) without sarcopenia (57%, n = 55). The overall percentage of sarcopenic patients increased to 21% at 2 weeks post-procedure and 25% at 6 weeks post-procedure. When categorized by gender, sarcopenia was present in 6% of female patients (n = 3) and 32% of males (n = 15) at the preoperative visit. Postoperative sarcopenia prevalence remained consistent with preoperative levels for both genders. Accounting for both gender and BMI, males with a BMI < 30 exhibited the highest sarcopenia prevalence. Specifically, 80% (12/15) of males with BMI < 30 met criteria for sarcopenia during the preoperative assessment, 100% (4/4) at the 2-week post-procedure follow-up, and 85.7% (6/7) at the 6-week post-procedure evaluation. In contrast, males with a BMI > 30 and females across all weight categories consistently displayed sarcopenia rates of < 20% both before and after the procedure, with the lowest sarcopenia rates observed among females with a BMI > 30 (< 5%). Conclusion: Sarcopenia is prevalent among preoperative spine surgery patients at our institution, particularly among male patients of lower BMI. Although further data collection is needed to establish trends in body composition and correlation with surgical outcomes, this preliminary data identifies patients that might benefit from increased surveillance and targeted nutritional intervention in the preoperative period.
1645
P459: Efficiency and workflow of the remi robotic navigation system technical note and case series
Asham Khan 1 , Mohamed Soliman 1 , Esteban Quiceno Restrepo 1 , Alexander Aguirre 1 , Cathleen Kuo 1 , Jeffrey Mullin 1 , John Pollina 1
1 Neurosurgery, University at Buffalo Neurosurgery, Buffalo, USA
Introduction: The rate of evolution in spine surgery continues to increase. Alongside advancements in technology, robotic navigation systems have been developed to aid surgeons. There are multiple benefits to using robotic navigation systems such as increased accuracy of screw placement thus reducing complication rates and decreased radiation exposure. A major drawback of robotic systems is operative workflow inefficiency due to excessive calibrations and set-up times. A recently developed hybrid platform utilising in part shared-control system and telesurgical interaction system, REMI robotic navigation platform, has the potential to improve operative workflow. Materials and Methods: Using operative video to discuss operational workflow of this new platform for the entirety of a procedure. Additionally, provide a retrospective review of patients for those who underwent lumbar fusion surgery using REMI between April 2022 and August 2022. Electronic patient records used to identify patients, gather patients’ demographic data, presenting symptoms, surgery type, operative duration, and radiation exposure time. Post-operative radiographic imaging used to grade pedicle screw with Ravi grading system. Results: Five patients identified (Median age 71-year-old, 60% female). Utilizing REMI resulted in a mean total operative time of 204.8 minutes and a mean total fluoroscopy time of 8.7 seconds, both are shorter total durations when compared to other robotic systems mentioned in literature. Using Ravi grading, all screws placed with REMI were Grade I. On post-operative follow-up, patient reported outcomes using VAS were significantly improved (p < 0.05). Conclusions: Our experience shows use of the REMI robotic navigation system resulted in a similar accuracy of screw placement compared to other robotic navigation systems, as well an improved workflow (operative time) and radiation exposure.
1697
P460: Safe, accurate and efficient-robotic guided S2 alar-iliac screw placement - A single centre experience
Akshya Raj 1 , Sharan Achar Thala 1 , Harith Reddy 1 , Vigneshwara Badikillaya 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Spine Surgery, Apollo Hospital, Chennai, Chennai, India
Introduction: S2-alar iliac screw fixation is a powerful tool in the armamentarium of the spine surgeon. It allows good correction of sagittal and lumbopelvic parameters with a strong distal anchor for the construct. The trajectory of S2AI screws however is closely related to major neural elements highly variable as per patient profile and can potentially injure sciatic nerve and violate the hip joint. It also involves considerable usage of intraoperative imaging and radiation exposure. Robotic Guided S2AI screw insertion provides a fast and efficient minimally invasive technique, which obviates the need for intraop imaging. Material and Methods: Study Design: Prospective case series. Objectives: To study the duration required, accuracy, safety and radiation exposure of robotically placed S2AI screws and to compare with freehand S2AI screw placement. Methods: 18 consecutive patients who underwent spino-pelvic fixation with s2-alar iliac screws, placed robotically, from 2021 to 2023 were included in the study. The screws were placed robotically guided with the use of a proprietary spine robotics system (ExcelsiusGPS, Globus Inc, Philadelphia), for a variety of primary and revision surgeries. The duration required for placement of each screw, associated blood loss were recorded. The radiographic outcomes in terms of accuracy of screw position any breaches were studied on postoperative images. Results: A total of 36 S2AI screws were robotically placed using preoperative CT scans merged to intraop images. 6 were complex deformity corrections, 5 were revision scoliosis corrections, 6 were failed back syndrome cases, 1 was caudal regression syndrome with deformed dysmorphic pelvis. A mean of 3.5 + 1.0 fluoroscopic exposures were required for merging the Preop CT to intraop position and check shot post screw placement. No fluro was used while inserting the screws. The mean duration for the placement of an S2AI screw robotically was 5.5+ 1.5 minutes. No breaches were seen in this series. There was no injury to neural, vascular or pelvic visceral structures in any patient. In comparison with mean duration of freehand S2AI screw insertion in the authors’ institute, the duration required was significantly lower, 16.6+ 3.25 minutes, using a mean 20.4+ 5.6 fluoroscopic images oer screw, which was significantly lower (p < 0.001). Conclusion: The robotic guided S2AI screw placement technique has very high accuracy and time efficiency, with minimal use of introperative fluoroscopy. Hence it is a efficient,safe and reliable method for spinopelvic fixations for various indications, particularly in complex spinal deformity surgeries and revision surgeries.
1752
P461: Convolutional neural networks in the diagnosis of cervical myelopathy
Murat Korkmaz 1 , Yekta Furkan Altin 1 , Taha Furkan Yağci 1 , Turgut Akgul 1
1 Orthopedics, Istanbul Faculty of Medicine, Fatih, Turkey
Objective: Artificial intelligence technologies have been used increasingly in spine surgery as a diagnostic tool. The aim of this study was to demonstrate the effectiveness of the convolutional neural networks in the diagnosis of cervical myelopathy (CM) compared to conventional cervical Magnetic Resonance Imaging (MRI). Methods: A total of 125 participants with clinical and radiological diagnosis of CM were included to study. Sagittal and axial MRI images in the T2 sequence of the cervical spine were used. All image parts are obtained as 8 byte/pixel in two different categories which are CM and normal, both in axial and sagittal views. Results: Triple cross validation was performed to prevent overfitting during the training process. 242 sample images were used for training and testing the model created for axial views. In the axial view, the calculated values are 97.44% for true positive rate (sensitivity), 97.56% for true negative rate (specificity). 249 sample images were used for training and testing the model created for sagittal views. The calculated values are 97.50% for true positive rate (sensitivity), 97.67% for true negative rate (specificity). After the training, the average accuracy value was 96.7% (±1.53) for the axial view and 97.19% (±1.2) for the sagittal view. Conclusion: Deep learning (DL) has shown a great improvement especially in the spine surgery. We found that DL technology works with a higher accuracy than other studies in the literature for the diagnosis of CM.
1753
P462: Complete correction of a rare case of scoliosis associated with spinal osteoblastoma using 3D printed model to guide excision
Akshya Raj 1 , dr.sharan achar thala 1 , Vignesh Badikillaya 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Spine Surgery, Apollo Hospital, Chennai, India
Introduction: Osteoblastoma is a rare benign bone forming tumor, usually seen in long bones, less commonly in the spine. Spinal osteoblastomas tend to involve posterior elements. Spinal osteoblastomas are painful and induce asymmetrical muscle spasm on the side of the lesion. Since the age of presentation is in the second decade for these tumors, a case of painful scoliosis due to osteoblastoma might be treated as adolescent idiopathic scoliosis. Their location in posterior elements of spine mean they are in ver close proximity to the nerve roots and the cord. Hence accurate surgical planning requires comprehensive planning. The current paper reports a case of in a 16 year old male with painful levoscoliosis due to osteoblastoma of T11 in its right lamina, treated initially at a centre different from the authors’, as a case of adolescent idiopathic scoliosis, who presented with back pain associated with tilting of trunk to the left. He reported a VAS score for his back pain of 7 to 8 out of 10. Clinically, the patient had a left sided curve of his thoracolumbar spine, which was accentuated on forward bending, and not correcting on sitting. Previously the patient was treated as a case of adolescent idiopathic scoliosis for 8 months at another centre, with worsening of pain over last 2 months. X-rays showed a levoscoliosis of the thoracolumbar spine with a Cobb angle of 32 degrees. Due to extremely close proximity to the cord at the T11 level, a high resolution CT scan was taken and a high fidelity 3D model was rendered. This data was used to fabricate a detailed 3D bone model of the T9-T12 vertebrae. This allowed the authors to study the anatomy of the tumor in relation to the canal. Surgical excision of the tumor was done using the 3D model as an introperative guide during the surgery. Complete excision was achieved. Postoperative course was uneventful. Histopathology showed the lesion to be consistent with an osteoblastoma. At 3 month follow-up, his VAS score for pain was 1-2 out of 10. The patient showed complete resolution of the left-sided thoraco lumber curve, with restitution of normal posture, radiological assessment showed a Cobb angle of 5 degrees, with normal coronal balance. Conclusion: This report demonstrates the significance of prompt diagnosis and surgical treatment of spinal osteoblastomas. Early surgical excision will not only prevent neurological deficit but also the progression of scoliosis. Atypical scoliosis, with pain needs how to be evaluated with a high index of suspicion. Novel 3-D printing technology enables the surgeon to plan the surgical resection in areas of complex Anatomy with a higher degree of fidelity and accuracy.
1792
P463: Treatment of chronic spinal cord injury. Is there any hope?
Muhammad Jawad Saleem 1 , Rizwan Mohammad 1
1 Orthopedic Spine Surgery, Orthopedic Spine Institute, Lahore, Pakistan
Introduction: To study the outcome of Arachnoidectomy+Adhesiolysis of cord +Dentectomy (AAD) for chronic spinal cord Injury (CSCI). Material and Methods: Patients with ASIA A, ASIA B Spinal Cord Injury sustained at least 12 months ago as a result of blunt trauma, qualified for the study approved by IRB under compassionate protocol. 7 patients satisfied the criteria and were enrolled in the study. Each patient underwent AAD. Outcomes were determined by improvement in neurological status, sphincter control and dysesthetic pain control. Routine follow up was carried out at 3 months interval. We present the short term outcome with minimal 6 months follow up on this set of patients. Results: 7 patients (6 male, 1 female) with mean age 24 years (16-36 years) underwent the surgical procedure (AAD) with a mean operative time of 3 hours. No post-operative worsening of neurological status was seen in any patient. 4 patients with ASIA B improved to ASIA C with improvement in sphincter control. 2 patients showed no improvement in neurology but showed significant improvement in dysesthetic pain. One patient showed no improvement in any outcome measures. Conclusion: AAD of spinal cord at the effected level was a safe and promising method for treatment of CSCI in our pilot study. No other treatment modality has yet shown any promising results in CSCI. We urge a larger study with long term follow up to establish efficacy of this treatment modality.
1800
P464: Do 3D printed templates aid in exposure, improve the accuracy and safety of pedicle screw insertion in complex spinal kypho-scoliotic deformities? A comparative cohort study
Sharan Achar T 1 , Akshya Raj 1 , Harith Reddy 1 , Vigneshwara Badikkilaya 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Orthopaedics, Apollo Hospitals, Chennai, India
Introduction: Surgical treatment of severe complex spinal deformities involves inherent difficulties such as anatomic anomalies, dysmorphic or absent pedicles, vertebral rotations and rib deformities. In India, these deformities are often neglected and present at a very late, much more deformed state when their treatment becomes even more challenging. Pre-operative imaging (including 3D reconstructed CT images) provide limited morphometric information, cannot show full scale spine and cannot be directly used on the operating table. Various techniques have been introduced to assure safe and accurate pedicle screw placement. One such promising and safe tool is 3D printed bone models and patient-specific drill templates. The aim of this study is to evaluate the safety of 3D printed ABS thermoplastic bone models for safe surgical exposure, freehand placement of pedicle screws and accuracy of patient-specific screw guides with pre-drawn, pre-validated trajectory in management of complex kypho-scoliotic deformity. Material and Methods: Of the 40 cases, 20 were operated with the help of 3D models/jigs and 20 were operated with free hand technique. Primary outcomes were measured in terms of screw violation, assessed by post op CT scan and secondary outcome were measured in terms of surgical time, blood loss, radiation exposure (no. of c-arm shoots required) and complications. Two-sample test of proportion for pedicle screw placement, T-test with equal variance for other parameters were statistically analyzed. Results: The mean cobbs of the scoliotic curves were 98.1˚ ± 19.4°. Each group had matched 30% cases of Congenital scoliosis, 60% Adolescent Idiopathic Scoliosis, 10% post tubercular kyphosis. 3D printed group over freehand group had significantly less medial violation, surgical time and fluoroscopic shots. There was no neurological deficit in any of the cases with no difference in the mean blood loss between the groups. We found significant (p = 0.04) difference between 2 groups regarding surgical time (298.5 ± 59.3 minutes in free hand group vs 235.5 ± 55.7 in 3D bone model group, p = 0.03), lesser dural tear incidence, perfect screw placement in favor of 3D printed jigs. There was statistically significant decreased medial violation (18 in free hand group vs 9 in 3D group, p = 0.005), no superior or inferior violation in any of our patients in either group. Mean Blood loss was higher in free hand group (840 ± 533.3 ml Vs 630 ± 227.6 ml in 3D model group), however it was not statistically significant (p-value: 0.3). There were a total of 42 fluoroscopic shots required in 3D printing group (2.1/patient) while 113 fluoroscopic shots were obtained in freehand group, which was significantly higher. Conclusion: The use of 3D printed models/ guides provided statistically significant faster, safer surgical exposure, higher rate of accurate screw positioning and higher number of inserted screws, particularly at apical levels, providing more accurate morphometric information and facilitate surgical correction of complex severe spinal deformity.
1803
P465: Impact of multimodal intraoperative neuro monitoring of the spinal cord during spine and spinal cord surgeries
Rajkumar P R 1
1 Neurosurgery, PSG Institute of Medical Sciences and Research, Coimbatore, India
Introduction: Multimodal intraoperative neurophysiological monitoring (IONM) during spine and spinal cord surgeries, provides an opportunity to recognize functional changes of the neural elements, usually in the reversible stage, during complex surgical manipulations. The aim of the study was to evaluate the efficacy of multimodal IONM for preventing and predicting iatrogenic neurological dysfunction during spinal cord and spine surgeries. Material and Methods: From August 2019 to August 2023, Multimodal intra operative Neuro physiological monitoring was used in 42 spine surgery patients, of which 16 were severe compressive myelopathy in cervical spine, 21 were spinal cord tumor and 5 were tethered cord syndrome. Age group from 9 years to 76 years. 27 were male and 15 were female. Results: Significant alerts had occurred in 13 out of 42 patients; however, most of the changes were reversible and did not contribute to postoperative clinical deterioration. Only one case got worsened in the early postoperative follow-up period, with stable intraoperative monitoring. Conclusion: Intraoperative Neuro monitoring is a valuable tool in spine and spinal cord surgeries. Combined trans cranial motor-evoked potential (TcMEP), somato sensory-evoked potential (SSEP), and spontaneous and triggered electromyography (EMG) monitoring may prevent permanent motor deficit and enhance the postoperative outcomes.
1820
P466: Acute effects of natural standing on diffusion properties of human lumbar intervertebral discs. A post-contrast MRI study in supine and standing
J Naresh-Babu 1 , Gajendra Dr 1 , Bala Murugan Duraipandi 1
1 Mallika Spine Centre, Spine Surgery, Mallika Hospital, Guntur, India
Introduction: Intervertebral disc health is crucial for maintaining spinal function and overall wellbeing. Disc degeneration is multifactorial and alterations in nutrition is considered as one of the main reason. Serial post contrast MRI studies have thrown light on the diffusion properties of intervertebral disc in supine position. The effects of natural standing and load bearing on disc diffusion is largely unknown. This study investigates the acute effects of standing on solute transport across the intervertebral disc. Material and Methods: 15 healthy volunteers representing various age groups formed the study group. Diffusion over 24 hours following intravenous gododiamide injection (0.3 mmol/kg) was studied at precontrast, 10 minutes and 2, 4, 12 and 24 hrs after contrast injection in supine, standing posture and followed by in recovery supine position. The enhancement percentage, time taken to achieve peak enhancement and time intensity curves were utilised to understand the diffusion properties of the intervertebral disc in Supine and standing. Results: The mean peak enhancement percentage in recovery supine and standing for of centre nucleus pulpous were 30 and 15, 25 and 12 for superior nucleus pulpous was and for inferior nucleus pulpous was 40 and 20 respectively. Overall 50% higher peak enhancement (EPmax) than standing. Conclusion: For the first time, Acute effects of standing on intervertebral disc nutrition and solute transport were observed through Post Contrast MRI, provides valuable insights into dynamic nature of spinal health. The findings suggest that act of standing can have a discernible impact on nutrition and solute transport within intervertebral discs highlighting the importance of posture and mechanical loading in maintain spinal health. Results of this study could help elucidate the long term implications of loading on intervertebral disc diffusion.
2119
P467: Novel technique (GW Closure method) of surgical wound closure of the spine to prevent CSF leaks in surgeries where dura is opened
Prasanna Gunasena 1 , Anil Weerasinghe 1 , Anupa Walgamage 1
1 Neurosurgery, Lanka Hospital, Colombo, Sri Lanka
Summary: This retrospective study analyzed 21 patients from July 2022 till August 2023, who underwent modified surgical wound closure (GW-Gunasena:Weerasinghe) to prevent CSF leaks after opening the dura and compared the outcome with the standard surgical wound closing technique augmented with tissue glue and artificial Dural covers. Primary Objective: Post-operative CSF leak is a known complication of spinal surgeries where dura is opened. Commonly encountered in intradural spinal tumor excisions. Even though the incidence is low it can lead to many squealy such as prolong hospital stay, meningitis and Dural cutaneous-fistulae. Incidence as per present data is around 6.6% ≤ 5.8% [1, 2]. In most of the cases, pre-operative preventive measures such as abdominal fat grafts, meticulous suturing of dura, closing the dead space and using fibrin glue to cover the suture line has been attempted to prevent CSF leaks [3]. In our practice out of 133 patients from 2014 April to 2022 July who underwent Dural opening 9.7% had CSF leaks. Additional surgeries to prevent CSF leak and prolong hospital stay caused additional financial burden to the patients [4]. To prevent CSF leaks, we modified the surgical closure technique. Instead of approximating the paraspinal muscles after the closure of dura using Non-absorbable monofilament polypropylene, we innovated GW closure method, (GW- Gunasena:Weerasinghe) mobilized the para spinal muscles off the subcutaneous fat laterally up to the lateral boarder of erector spinae muscle. Fascial covering was split and muscles were mobilized medially. Tension free muscles were approximated using 1-polyglycolic sutures in the midline without creating a dead space. A closed suction drain was placed under the muscle layer. Subcutaneous layer and skin was approximated with absorbable sutures. No fibrin glue or fat grafts used to secure the dural opening. Patients’ follow-up was done up-to three months for any SCF fistulae or pseudo meningoceles. The results were compared with a similar group of patients from 2014 April to 2022 July, where fibrin glue has been used to augment the Dural closure and standard midline wound closure was done. The incident of CSF leak in the standard suturing group is 9.7% whereas patients who had modified (GW method) closure had no CSF leaks or meningoceles up to three months after surgery. Conclusion: Modified (GW method) closure, midline suturing with mobilization of erector spinae muscle gives excellent results to prevent development of SCF leaks or pseudo-meningocele.
References
1. Akeyson EW, McCutcheon IE. Single-stage posterior vertebrectomy and replacement combined with posterior instrumentation for spinal metastasis. 1996.
2. Wong AP, Lall RR, Dahdaleh NS, et al. Comparison of open and minimally invasive surgery for intradural-extramedullary spine tumors. 2015.
3. Arnautovic KI, Kovacevic M. CSF-related complications after intradural spinal tumor surgery: utility of an autologous fat graft. 2016.
4. Jallo J, Pharmd FRE, Baird CJ, et al. The cost of cerebral spinal fluid leaks after spinal surgery in the USA. 2009.
2380
P468: Transpedicular intravertebral augmentation using expandable cage in Kummell disease: technical note and case series
Kwang-Sup Song 1
1 Orthopaedic Surgery, Chung-Ang University Hospital, Seoul, South Korea
Introduction: Most patients with Kummell disease with intractable back pain or neurologic deficits require firm stabilization surgery. However, there are difficulties to support anterior and posterior support simultaneously in most patients with severe osteoporosis and medical comorbidity in the old age population. We aimed to introduce the novel technical note, transpedicular intravertebral cage augmentation (TPICA) using an expandable cage combined with posterior stabilization in a single posterior approach, less invasive anterior and posterior column supports in severe osteoporotic frail patients. Methods: Six consecutive frail patients underwent the surgical procedures, the average age was 83.7 years old, unable to walk for over 1 month due to intractable back pain, and with severe frailty. All patients underwent TPICA procedures at the index vertebra in a single posterior approach and pedicle screw instrumentation one or two-level above and below the vertebra, which augmented with cement. The average follow-up period was > 6 months and analyzed the radiologic outcomes, including the restored ratio of anterior vertebral height (RAVH) and local kyphosis angle (LKA), and the patient's demographic characteristics and surgical data, including operation time and external blood loss, were also collected. Results: All expandable cages were expanded to 4 mm after insertion in the index vertebra. All patients were able to walk independently (n = 5) and with a cane (n = 1) at postoperative 2 weeks and much improved back pain and ambulatory capacity were sustained at 6 months. The mean operation time was 156 (149-160) min, and the mean external blood loss was 100 (50-150) cc. The postoperative RAVH was 0.64, 1.64 times higher than the preoperative AVH, and LKA was corrected postoperatively from 15.7' to 6.5'. Some losses of corrected angles were observed at 6 months compared to immediate postoperative periods, however, there was no its related clinical symptom. Conclusion: The introduced technique, TPICA using expandable cage, might be a valuable minimal invasive anterior column support technique in severely osteoporotic patients with collapsed Kummel disease, especially, expandable cage in TPICA seems to have the advantages of minimizing the destruction of pedicle structures and effectively recovering the collapsed endplates.
2446
P469: Improvement of chronic urethral and perineal pain with spinal cord stimulation
Neptali Torres 1 , Fernando Rascon 1 , Borja Ferrandez Pujante 1 , Andres Vargas 1 , Albert Trondin 1 , Gustavo Villalobos 1
1 Neurosurgery, Hospital Clinico San Carlos, Madrid, Spain
Introduction: Spinal cord stimulator (SCS) have been establish safe to treat chronic pain of multiple etiologies. Indications are neuropathic pain that have failed with conventional medical treatment. The mechanism of action consists of neuromodulation through the application of electricity in the dorsal column, intervening in the ascending pathways that carry painful impulses to the brain. Material and Methods: 53-year-old patient with a history of childhood cerebral palsy with secondary dystonic tetraparesis, treated with baclofen pump. He developed chronic urethral and perineal pain. He was diagnosed with pudendal neuralgia in follow-up with the pain unit and urology. Moderate pain relief with direct perineal stimulation using vibrators. Urology decided to place a sacral root stimulator without improving his pain significantly. Later, he went to the neurosurgery for post-surgical follow-up of the L5-S1 laminectomy accompanying his wife who is a carrier of a spinal pain stimulator and asked about the possibility of this treatment. Results: We decided to implant a surgical spinal cord stimulator with an electrode at the level of D9 D10. The next day after surgery, the stimulator was turned on and after a week he reported complete improvement in urethral and perineal pain, improving his quality of life, without oral medication or direct stimulation on perineal area. Conclusion: Spinal cord stimulator is a minimally-invasive procedure, safe and cost-effective therapeutic option for numerous chronic pain conditions. other indications are cases of refractory neuropathic pain complicated by drugs side effects, tolerance, or the need for re-operation. The uretral pain in this patient improve significantly with subsequent reduction of pain treatment.
2452
P470: Use of hydraulic dissection and irrigation in spinal surgery: video presentation of the technique
Suresh Jayabalan 1
1 Department of Neurosurgery, Kovai Medical Center Hospital, Coimbatore, India
Introduction: Saline irrigation and dissection used in Neurosurgery for many decades. It helps to clear the blood filled field in the brain and spine as well as for debridement and irrigation during bipolar cautery. The same can be used for Haemostasis in Spinal special situation and for dissection and removal of disc material during Micro lumbar discectomy. The technique is described as a video in this presentation. Material and Methods: Saline irrigation used in two areas of spinal surgery in this presentation. Anterior cervical discectomy and Micro Lumbar Discectomy were commonly performed in any spinal center. We have used this technique in all surgeries performed from January 2010 till date. The instruments, technique and the indications explained in this presentation. Results and Conclusion: Saline irrigation and Jet dissection definitely useful in haemostasis during the anterior cervical discectomy and maximal removal of disc material during Micro lumbar discectomy. So it avoids major hemorrhagic complications and recurrence of symptoms and signs.
2454
P471: Effects of natural standing on biomechanical and diffusion properties of unfused lumbar intervertebral discs in AIS patients 5 years after fusion. A serial MRI post contrast diffusion study in supine and standing
J Naresh-Babu 1 , Prudvi Kumar Reddy Kamazala 1
1 Spine Surgery, Mallika Spine Centre, Guntur, India
Introduction: Adolescent Idiopathic Scoliosis (AIS) patients managed with Posterior Spinal Fusion (PSF) often experience intervertebral disc degeneration in the distal unfused lumbar segments. To gain a comprehensive understanding of these degenerative changes, our study employs a multi-modal approach. We aim to analyze the biomechanical and diffusion properties of the unfused lumbar discs, utilizing positional MRI in both supine and standing postures, and investigate solute transport changes occurring 5 years after fusion. Material and Methods: Our study group comprises 10 AIS patients who underwent PSF more than five years ago. We conducted clinical, functional, and radiographic evaluations, including plain and contrast-enhanced MR imaging of the lumbar spine in both supine and standing positions. After intravenous gadodiamide injection, we captured serial MR T1 weighted images at 2, 4, 6, 12, and 24 hours in both positions. We measured the signal intensity of the end plate zone (EPZ), Peripheral nucleus pulposis (PNP), and Central nucleus pulposis (CNP) in sagittal sections of discs adjacent to the fused segment and the one below. We calculated Peak Enhancement Percentage (EPmax) and time to attain EPmax (Tmax). We analyzed 24-hour diffusion patterns using statistical methods. Results: The intervertebral discs in our study were categorized as Pffirrmann's Grade-I. Anthropometric changes included increased disc wedging, lumbar lordosis, listhesis index, and lateral translation on standing. Conversely, we observed reductions in disc height, foraminal cross-sectional area, axial CSA, and mid-sagittal thecal sac area. Spinal curvature remained unchanged. While no significant biomechanical changes were noted, the unfused lumbar disc immediately below the fusion (Fusion-1) exhibited significant alterations in solute transport properties compared to the distal unfused segments (fusion-2 onwards). Fusion-1 displayed a double-peak pattern of enhancement with multiple endplate breaks in both supine and standing positions. Interestingly, the peak enhancement percentage decreased by approximately 50% on standing, suggesting a leaky endplate-disc-contact zone. Conversely, the distal unfused segments (fusion-2 onwards) showed a steady increase in enhancement percentage, reaching a peak at 12 hours, indicating a relatively healthy pattern of disc diffusion in both positions. Unlike Fusion-1, these discs exhibited a 50% increase in peak enhancement percentage on standing, suggesting healthy disc diffusion. Conclusion: Our study highlights the early effects of long fusion on the unfused intervertebral discs 5 years post-fusion. While degeneration changes were not apparent on MRI in either supine or standing positions, the disc immediately below the long fusion (Fusion-1) exhibited significant alterations in diffusion patterns and multiple endplate breaks, with a notable reduction in disc diffusion on standing. This study is the first of its kind to document diffusion pattern alterations in both supine and standing positions in unfused lumbar segments. These findings open up new avenues for further research in this field.
2515
P472: Positioning accuracy and facet joint violation after percutaneous pedicle screw placement with robot assisted vs fluoroscopy guided technique: systematic review and meta-analysis
Maria Ilaria Borruto 1 , Andrea Perna 2 , Calogero Velluto 1 , Domenico Alessandro Santagada 1 , Franco Lucio Gorgoglione 2 , Francesco Ciro Tamburrelli 1 , Luca Proietti 1
1 Policlinico Universitario A Gemelli IRCSS, Rome, Italy
2 Fondazione Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy
Introduction: minimally invasive spine surgery (MISS) became the gold standard for the treatment of many spinal diseases. Only a few comparative studies were performed regarding the superiority of robotic assisted (RA) surgery over fluoroscopic guidance (FG) surgery during percutaneous pedicle screws (PPS) placement. Therefore, the aim of the present study was to conduct a systematic literature review and meta-analysis to evaluate the accuracy, and potential advantages of RA compared with FG. Material and Methods: the present study is a systematic literature review conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The review questions were formulated according to the PICO scheme. Forest plot was used to present the measured outcomes. Heterogeneity between included studies was evaluated by the χ2, while the I2 statistic was performed to estimate the proportion of total variation among the studies; a value higher than 50% was interpreted as substantial heterogeneity. Results: Seven studies that met inclusion criteria were finally included in this meta-analysis. These 7 studies include: 447 patients, 228 patients (931 screws) treated with robotic guide and 219 patients (767 pedicle screws) using fluoroscopic guide, with a mean age of 55.2. The percentages of clinically acceptable screws were 94.3% in the robot assisted group and 89% in the fluoroscopic guided group. The percentages of non-acceptable screws were 5.7% in the robot assisted group and 11% in the fluoroscopic guided group. We reported statistically significant differences between the two groups in terms of radiographic and clinical outcomes with longer operative times in the robotic-assisted pedicle screw group. The robot technology should be used as a support for the correct placement of the screws, helping the surgeon in the most challenging screws placement for anatomical variants or in patients with spinal deformities. Conclusion: the accuracy of pedicle screw placement with robotic technology is higher than with FG. In fact, the robotic approach allows significantly lower complication rates, fewer cases of violation of the proximal articular facet, less intraoperative exposure to radiation, even if it requires longer surgical times than the FG technique.
2544
P473: Active exoskeleton robots in spinal cord injury (SCI) show improved neuroplasticity and function in mobility: a systematic review
Ka Ioi Argus Chiu 1 , Mathew Gallagher 2 , Sarah Abbott 2 , Bisola Ajayi 2 , Jason Bernard 2 , Timothy Bishop 2 , Darren Lui 2
1 Complex Neurosurgery, St Georges University of London, London, United Kingdom
2 Complex Neurosurgery, St Georges Hospital, London, United Kingdom
Introduction: Exoskeleton robots can be classified as active or passive and powered or stationary; used in rehabilitation for SCIs. Some ‘improve’ function where neuroplasticity is induced whereas some focus on ‘performance’ which rehabilitate by repetitive movement. Newer active exoskeletons identify electrical signals in the paralysed limbs to initiate limb movements promoting neuroplasticity through positive feedback. Material and Methods: A search between 2011 to June 2023 on Pubmed Central, Pubmed, Web of Science and Embase resulted 29 papers to be selected for the review. Active exoskeletons include the Hybrid Assisted Limb (HAL). Passive exoskeletons include the ReWalk, Ekso, Hyundai Medical Exoskeleton (H-MEX), Atlante, Indego, Lokomat, Assistive Device for Paralysed Patients (AIDER) and HANK. All the exoskeletons are powered except for Lokomat which is a stationary exoskeleton. Acute SCI was defined as less than one year since injury; chronic SCI was defined as more than one year. Ambulatory distance in the 6 minute walking test (6MWT) and ambulatory speed in the 10 metre walking test (10MWT) were outcomes of interest. They’re further analysed based on the time since SCI.
Results:
6MWT and 10MWT with Exoskeleton: Only passive exoskeletons examined mobility with aid of the robot. H-Mex and Ekso demonstrated significant improvements with 10 H-MEX users and 3 Ekso users showing a 137.9% and 102.8% increase in the 6MWT respectively. 10 Ekso users also showed a 26.8% increase in the 10MWT.
6MWT and 10MWT without Exoskeleton: 212 patients across 5 HAL studies showed an average increase of 77.82% in the 6MWT. 4 Ekso users and 11 HANK users showed 34% and 60.1% increase in 6MWT respectively. 256 patients across 7 HAL studies showed an average increase of 116.8% in the 10MWT. Notably HANK was the only passive exoskeleton to produce a significant increase in 10MWT with a 67.4% increase in 4 patients.
6MWT without Exoskeleton for Acute and Chronic SCI: For acute SCI, 97 HAL users in two studies and 11 HANK users in one study showed an average increase of 82.45% and 60.1% respectively. 137 chronic SCI patients across 3 HAL studies showed an increase of 75%. Ekso and ReWalk demonstrated a 34% increase in 4 patients and 9.7% increase in 5 patients respectively.
10MWT without exoskeleton for Acute and Chronic SCI: 98 acute SCI patients across 3 HAL studies showed an average increase of 186.2%. 11 patients using HANK showed an increase of 67.6%. One Lokomat study showed an increase of 191.9% in 31 patients. 137 chronic SCI patients across 3 HAL studies showed an average increase of 92.4%. 4 patients using Ekso, 7 using Lokomat and 5 using ReWalk only showed an increase of 29.4%, 55.7% and 38.7% respectively.
Conclusion: Only HAL showed consistent improvements in all outcome measures. HAL excelled in most areas except 6MWT for acute SCI, suggesting that active, powered exoskeletons show greatest improvement in function and neuroplasticity. Lokomat, the passive, stationary exoskeleton demonstrated greatest improvement in the 6MWT for acute SCI, suggesting HAL and Lokomat induce more neuroplasticity following rehabilitation compared to the passive, powered exoskeletons.
2561
P474: Passive exoskeleton robots in spinal cord injury (SCI) show greater improvements in secondary complications: a systematic review
Ka Ioi Argus Chiu 1 , Mathew Gallagher 2 , Sarah Abbott 2 , Bisola Ajayi 2 , Jason Bernard 2 , Timothy Bishop 2 , Darren Lui 2
1 Complex Neurosurgery, St Georges University of London, London, United Kingdom
2 Complex Neurosurgery, St Georges Hospital, London, United Kingdom
Introduction: SCIs extend beyond mobility, impacting factors like continence and pain which can both diminish an individual’s quality of life (QoL). Exoskeleton robots can be used as a rehabilitation tool to not only improve an individual's mobility, but also help address these secondary complications. Active exoskeletons can help amplify existing cerebral signals which can promote neuroplasticity to help address secondary SCI complications contrasting passive exoskeletons that rehabilitate patients by repetition of movement. Materials and Methods: A search was carried out between 2011 to June 2023 on Pubmed Central, Pubmed, Web of Science and Embase. 14 papers were selected for the review. Active exoskeletons include the Hybrid Assisted Limb (HAL). Passive exoskeletons includes the ReWalk, Hyundai Medical Exoskeleton (H-MEX), Atlante, Indego, Ekso, Lokomat, SuitX Phoenix and Rex Bionics. We focused on measuring continence, pain and QoL. Results: Continence: In one HAL study, 35 patients exhibited a significant Wexner score improvement from 8.89 to 6.51. Among 22 patients with chronic SCI, the score reduced significantly from 9.55 to 7.05. However, this effect was not seen in 13 patients with acute SCI. 21 patients using the ReWalk used parts of the neurogenic bladder symptom score and neurogenic bowel dysfunction score to assess bladder control. Significant improvements were observed in patients from a median of 3 (neutral) to 4 (mostly satisfied). Atlante, Ekso, Lokomat, Indego, H-MEX and another ReWalk study did not show statistically significant improvements in 80 patients. Pain: In one HAL study with 19 patients, pain assessed via the neuropathic pain symptom inventory showed no significant changes. A case study with 2 patients using HAL showed statistically significant reductions in the numerical rating scale from 4.3 to 0.6. Among 113 patients using passive exoskeletons including Ekso, Atlante, Indego, ReWalk and SuitX Phoenix there were no statistically significant improvements in pain except for 1 patient using the ReWalk. Quality of Life: 19 patients in a HAL study analysed QoL using the Short Form 36 (SF36) questionnaire and there was no statistically significant changes. Another HAL study with 2 patients showed positive changes in all domains of the SF36 with overall a statistically significant improvement. Ekso and ReWalk were the only passive exoskeletons that showed significant improvements in QoL. 21 patients using the Ekso showed significant improvements in the Short Form 12 (SF12). 10 ASIA A patients improved from 21.1 to 35 and 11 ASIA B patients improved from 26.9 to 35.7. 21 patients using the ReWalk showed improvements in total score of the SF36 from 571 to 621 but improvements were only statistically significant in 4 out of 8 subcategories. The H-MEX, Indego, Rex Bionics and another ReWalk study did not show statically improvements in QoL in 62 patients. Conclusion: Both active and passive exoskeletons demonstrated significant improvements secondary complications post-SCI. The small HAL sample size for for pain and QoL implies potential superiority of passive exoskeletons in these areas, suggesting that active exoskeletons only induce limited neuroplasticity.
Spine biologics
95
P475: Standarized method for lumbar fusion techniques using P15/ABM measured by clinical and radiological outcomes
Alberto Perez 1 , Diana Chavez 1
1 Neurosurgery, Hospitales Angeles, Ciudad de Mexico, Mexico
Introduction: Lumbar fusion as low back pain treatment continues to be a challenge because of the multiple techniques and materials available, Techniques include: Transforaminal lumbar interbody fusion (TLIF), Lateral lumbar interbody fusion (LLIF, XLIF, OLIF) and Anterior lumbar interbody fusion (ALIF). Successful lumbar fusion is associated with better clinical outcomes and it is enhanced and targeted through the use of bone graft materials, for example i-FACTOR Bone Graft, osteogenic cell binding peptide P-15, bound to an anorganic bone mineral (ABM). This peptide improves bone formation when used in fixation devices in a targeted and limited way to the implant surface by activating osteoblast precursor cells; by the osteogenic, osteoinductive and osteoconductive stimuli. The main objective of this study is to standardize the lumbar fusion process in the 3 techniques and achieve a more efficient and predictable lumbar fusion, evaluating results with radiological and clinical scales. Material and Methods: 67 patients underwent lumbar fusion with the use of i-factor bone graft (5cc) in three different techniques (TLIF, LLIF, ALIF) achieving a total of 100 lumbar levels. Radiological outcomes included fusion rates per the Lenke scale. Clinical outcomes were evaluated via the Oswestry Disability Index (ODI), Short Form Performance (SPF-36) and Visual Analog Scale (VAS and VASS) for pain and satisfaction. Results: At the moment, 44 patients completed 6 months follow up and 35 patients completed 12 months follow up with lateral lumbar radiographs and CT scan with no differences in fusion rates between techniques. Successful fusion was observed in 44% at 6 months and 75% at 12 months with Lenke A. Clinical scales showed no disability at ODI, improvement at VAS and VASS scales, absence of health restrictions at SPF-36 score since 6 months follow up. Conclusion: Volume of bone graft used (5cc) seems to be enough to achieve fusion on any technique. Fusion rates seems to be improved since 3 months control and continues fusion process till 12 months follow up. Fusion rates are non dependent on the technique using p15/ABM. It is necessary to complete 12 months follow up with all patients studied to obtain variability and validity.
572
P476: Lateral decubitus anterior exposure of the L4-5 disc maintains safety compared with supine positioning
Nam Hunyh 1 , Domenic Robinson 2 , J. Alex Thomas 3 , Aaron Buckland 1
1 Spine and Scoliosis Research Associates Australia, Windsor, Australia
2 St Vincent's Hospital Kew, Kew, Australia
3 Atlantic Brain and Spine, Wilmington, USA
Introduction: Anterior lumbar spinal exposure has been traditionally performed with the patient positioned supine. Recent advances in lateral single position surgery (LSPS) has resulted in advocacy for anterior access to the L4-5 disc in the lateral decubitus position where trans-psoas or anterior-to-psoas approaches may not be safe. While L5-S1 access is well described, no series of L4-5 access in the lateral position has been published. Methods: A retrospective analysis of patients undergoing anterior lumbar spinal exposure including the L4-5 disc was performed via chart review. Patients were classified based on the patient positioning in which the anterior exposure was performed: lateral decubitus (LAT) or supine (SUP). Patient demographics, surgical characteristics, intraoperative and postoperative complications and reoperation at 30- and 90-days were compared using independent samples t-tests and chi-squared analysis as appropriate with significance set at p < 0.05. Results: 129 patients with 216 levels anterior exposure were performed that included the L4-5 disc level, including 57 LAT patients (99 levels) and 72 SUP patients (117 levels). LAT patients were older (66.1 vs. 52.7 yrs, p < 0.001), but gender and BMI were similar. The mean anterior column levels fused were significantly higher in the LAT group (2.49 vs. 1.58, p < 0.001), but levels of ALIF exposure (1.74 vs. 1.58, p = 0.074) and posterior levels fused (1.42 vs. 1.16, p = 0.188) were similar between groups. The difference in anterior column levels fused was due to concurrent LLIFs performed in the LAT group (22.8% vs 0.0%, p < 0.001). The lateral group had a higher proportion of patients treated for spinal deformity (22.60% vs. 7.20%, p = 0.012). The differences in procedural characteristics reflects the higher complexity of cases performed in the lateral position. Intraoperative complication rates (8.90% vs. 7.10%, p = 0.803) were similar between groups. In contrast, postoperative complications (17.50% vs. 36.10%, p = 0.020) were significantly higher in the SUP group. The rate of vascular injury (1.80% vs. 1.40%, p = 0.857) and there was no difference between vascular injury rates between L4-5 and L5-S1 exposure. Abdominal wall complications (1.80% vs. 4.20%, p = 0.432) were similar between groups. No patients experienced ileus in the LAT patients, whilst it was observed in 5.6% of SUP patients (p = 0.044). Reoperation rates at 30-days (3.60% vs. 6.90%, p = 0.405) and 90-days (3.60% vs. 11.10%, p = 0.115) were similar between groups. Conclusion: Anterior exposure of the L4-5 disc in the lateral decubitus position is safe and reduces ileus when compared to supine exposure, despite higher case complexity in the lateral position. Lateral decubitus ALIF is a viable alternative to ATP and trans-psoas approaches to the L4-5 disc for anterior column reconstruction and LSPS.
1047
P477: Hypermagnesemia and hyperphosphatemia associated cardiac arrest after injection of a novel magnesium-based bone cement in spinal surgery: a case report
Jia Yi Loh 1 , Allan Dizon 1 , Zhixing Marcus Ling 1 , Lei Jiang 1 , Yee Gen Lim 1
1 Department of Orthopaedic Surgery, Singapore General Hospital, Singapore, Singapore
Introduction: We report a case of into pulseless electrical activity (PEA) associated with profound hypermagnesemia immediately after cementation of a novel magnesium-based cement in spine surgery. Background: During T8 to T12 posterior instrumentation and decompression laminectomy for vertebral metastasis secondary to lung cancer, a 61 year old Chinese female developed sudden hypotension and went into PEA immediately after injection of a novel magnesium-based cement. Intraoperative fluoroscopic imaging did not show any significant cement extravasation. Resuscitation using intravenous adrenaline with 5 doses of 1mg adrenaline 1:10,000 dilution was instituted and the patient had return of spontaneous circulation (ROSC) after 5 minutes. After successful resuscitation, surgery was expedited and completed. Intraoperative and postoperative investigations were significant for profound hypermagnesemia and hyperphosphatemia requiring diuresis. There were no echocardiographic or computerised tomographic evidence of pulmonary embolism. The patient was transferred to the surgical intensive care unit (SICU) and remained on dual inotropic support over the next few days. She subsequently weaned off inotropic support and electrolyte imbalances resolved before making a full recovery. Conclusion: This case report demonstrates the severe magnesium toxicity and PEA related to the use of novel magnesium-based cement in spine surgery. Further studies need to be conducted to understand the potential complications related to its use and compare them to the traditional bone cement implantation syndrome.
1564
P478: Safety and efficacy of autologous bone marrow clot as a multifunctional bioscaffold for instrumented posterior lumbar fusion: a one-year follow-up pilot study
Giovanni Barbanti Bròdano 1 , Francesca Salamanna 2 , Giuseppe Tedesco 1 , Cristiana Griffoni 1 , Maria Sartori 2 , Paolo Spinnato 3 , Paolo Romeo 3 , Milena Fini 4 , Gianluca Giavaresi 2 , Alessandro Gasbarrini 1
1 Spine Surgery
2 Surgical and Technological Sciences
3 Diagnostic and Interventional Radiology
4 Scientific Direction, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Bone marrow aspirate (BMA) in association to graft substitutes has long been introduced as a promising alternative to iliac crest bone graft in spinal fusion. However, BMA use is limited by the lack of a standardized procedure, of a structural texture and by the possibility of diffusion away from the implant site. Recently, the potential use of a new formulation of BMA, named BMA clot, has been preclinically described. We report here the results of a prospective pilot clinical study aimed to evaluating the safety and efficacy of autologous vertebral BMA (vBMA) clot as three-dimensional and multifunctional bio-scaffold in instrumental posterior lumbar fusion. Material and Methods: Clinical outcomes were evaluated by the Visual Analog Scale (VAS), Oswestry Disability Index (ODI), and EuroQoL-5L (EQ-5L) preoperatively and at 3 and 12 months after spinal fusion. Bone fusion quality was evaluated at 12 months of follow-up by Brantigan classification on radiography (XR) imaging. Bone density was measured on computed tomography (CT) scans at 6 and 12 months of follow up visits and expressed in Hounsfield Unit (HU). Results: Results show a successful degree of fusion of about 100% (considering the levels with C, D, and E grades, Brantigan classification) at 12-month follow-up and an increase in bone density from 6 to 12 months follow-up. An improvement of quality of life and health status following surgery, as evaluated by clinical scores (ODI, VAS, and EQ-5L) was also observed already at 3 months follow-up. No adverse events related to the vBMA clot were reported. Conclusion: This prospective pilot study shows the effectiveness and the safety profile of vBMA clot as advanced bio-scaffold able to achieve posterior lumbar fusion in the treatment of degenerative spine diseases, laying the groundwork for a larger randomized clinical study.
1735
P479: Interobserver reliability and intra observer repeatability of AO Spine classification of osteoporotic vertebral fractures
Sushruth Raj 1 , Srinivasa Moolya 1
1 Orthopedics, Tejasvini Hospital & SSIOT, Mangalore, India
Introduction: Osteoporosis is a condition characterized by weakened bones, making individuals more susceptible to fractures. Diagnosis is based on bone mineral density criteria, and vertebral fractures are a common consequence. In India, millions of people have osteoporosis or low bone mass, with vertebral fractures often going unnoticed due to their asymptomatic nature. These fractures can lead to back pain, physical limitations, and kyphosis. Current classification systems for vertebral fractures are inadequate for osteoporotic cases. A German working group developed an MRI-based AO Spine classification to address this gap. Treatment is essential for pain relief and to prevent complications. Vertebroplasty and kyphoplasty are minimally invasive options, while open surgery may be necessary in severe cases. This study aims to assess the reliability of the AO Spine classification system among observers, given its potential complexity. With an aging population, the incidence of osteoporotic vertebral fractures is expected to rise. Material and Methods: This study was conducted at the Department of Orthopaedics in Tejasvini Hospital & SSIOT. It focused on patients aged 45 or above for women and 50 or above for men, who were experiencing acute low back pain and underwent MRI scans for suspected osteoporotic vertebral fractures. The research employed a retrospective and prospective observational design with a sample size of 56 patients. Three orthopaedic surgeons, each with varying years of experience, independently evaluated the MRI images using the AO Spine (DGOU) classification for osteoporotic vertebral fractures. The reliability of this classification was assessed through intraobserver and interobserver agreements using weighted Kappa coefficients. Statistical analysis was performed using SPSS. The study aimed to validate the classification system's consistency in diagnosing osteoporotic vertebral fractures. Results: In India, approximately 50 million people suffer from osteoporosis or low bone mass, with a 17.9% prevalence of radiographic vertebral fractures in older adults. Vertebral fractures, often asymptomatic, cause significant morbidity, including back pain and kyphosis-related pulmonary issues. The absence of a universally accepted classification system for osteoporotic vertebral fractures hinders prognosis and treatment. Existing systems like Genant et al. and Sugita et al. are based on plain radiographs and lack specificity. The AO Spine(DGOU) classification, based on MRI, provides better accuracy and guides early recognition and treatment. Intraobserver and interobserver reliability in classifying these fractures varied, with experienced surgeons demonstrating higher agreement. MRI is superior to plain radiographs and CT scans in detecting these fractures, emphasizing its importance in diagnosis. Anterior tension band failure can be challenging to identify and classify. Conservative treatment, including rest and osteoporosis management, is effective for most fractures, with surgery considered for specific cases. Conclusion: Osteoporotic vertebral fractures are challenging due to their diverse patterns. A good classification system should describe and guide treatment. Advances in MRI improve understanding. A useful system should be easy to use, aid communication, guide treatment, offer prognosis, and allow outcome comparison. AO Spine (DGOU) works well, especially among experienced observers. Better understanding can lead to improved outcomes. MRI with STIR is valuable for diagnosis. More multicentric research is needed to enhance the system's use.
2385
P480: The clinical efficacy and safety of P-15 peptide enhanced bone graft in bone regeneration: a systematic review
Barend Spanninga 1 , Thomay Hoelen 2 , Scott Johnson 3 , Boyle Cheng 4 , Praveer Vyas 5 , Taco Blokhuis 2,6 , Paul Willems 2 , Chris Arts 1,2,7
1 Laboratory for Experimental Orthopaedics, Department of Orthopaedic Surgery,Maastricht University, Maastricht, The Netherlands
2 Department of Orthopaedic Surgery, Maastricht University Medical Centre+, Maastricht, The Netherlands
3 Cerapedics Inc, Westminster, USA
4 Neurosurgery, Drexel University, USA
5 Allegheny Health Network, Pittsburgh, USA
6 Department of Surgery, NUTRIM, Maastricht University Medical Centre+, Maastricht, The Netherlands
7 Orthopaedic Biomechanics, Department of Biomedical Engineering,Eindhoven University of Technology, Eindhoven, The Netherlands
Introduction: Recent bone graft advancements have focused on supporting and enhancing host bone regeneration. The use of growth factors is controversial with known clinical complications and high costs. Peptides offer the potential to retain specific biological activity without the potential risks associated with growth factors. P-15 is a peptide found in Type I collagen which has been found to enhance osteogenic cell attachment, proliferation and differentiation. The objective of this study was to conduct a systematic review to determine the efficacy and safety of P-15 peptide in bone regeneration. Materials and Methods: A PRISMA compliant systematic review was performed. PubMed, Embase, Web of Science and Cochrane Library were searched on June 30, 2022 for relevant articles (search terms: Cell-binding peptide P-15] OR P-15 OR i-FACTOR AND general surgery OR surgical procedures, operative OR bone regeneration). Full text English language articles considering P-15 peptide published from 1990 were eligible. Studies including systematic bone disease, malignancy or infection were excluded. Risk of bias of the eligible studies was evaluated using the methodological index for non-randomized studies tool and the ROB2.0 assessment tool for RCTs. Results: 25 articles were included in the systematic review. Eighteen publications focused on the application of P-15 in oral cavity procedures, next were cervical spine (n = 3), lumbar spine (n = 3) and long bone interventions (n = 1). Most studies displayed low bias (1-B or 2-B). All published results showed quick bone formation and remodeling. In spine surgery, i-FACTOR Bone Graft outperformed autograft in bone formation speed and does not show the complications reported for growth factors. Few postoperative complications related to P-15 were reported. Conclusions: High-quality clinical evidence exists for the safety and efficacy of P-15 in multiple surgical contexts. Compared to autograft, bone forms faster and remodels quicker. We conclude that i-FACTOR’s P-15 peptide is safe and effective biomaterial resulting in a standardized bone formation reaction with low probability for complications.
2445
P481: Predictive factors for vertebral fracture in elderly: BMD, Calcium, Vit-D, BALP, OC, and CTX
Kwan Ho Park 1 , Da Hoon Hong 1 , Tae Wan Kim 1
1 Neurosurgery, VHS Medical Center, Seoul, South Korea
Introduction: Measurement of bone mineral density (BMD) is the gold standard for the diagnosis of osteoporosis. However, the BMD measurement does not provide information on bone quality. We report factors that predict vertebral fractures in relation to laboratory results (BMD, calcium, Vit-D, and Bone turnover markers (BTMs) in patients with vertebral fracture and non-vertebral fracture groups. Material and Methods: We reviewed retrospectively medical records of patients who were treated in our institution. A comparative analysis was carried out between 58 patients with vertebral fracture (Group A) and 82 patients admitted with non-vertebral fracture (Group B). The following predictors of vertebral fracture occurrence were analyzed: Sex, age, BMD, calcium, Vit-D and BTMs. BTMs are divided to formation markers [serum bone-specific alkaline phosphatase (BSAP), osteocalcin (OC)] and resorption markers [serum C-terminal telopeptide of type I collagen (CTX). Results: The average age of the subjects was 75.0 ± 8.2 years. The mean BMD were 2.6 ± 1.2 in group A and 1.5 ± 1.3 in group B, respectively. The mean serum calcium levels were 9.0 ± 0.7 ng/dL and 9.1 ± 0.9 ng/dL, respectively. The mean serum 1,25(OH) vit-D levels were 15.6 ± 10.8 ng/mL and 15.8 ± 7.2 ng/mL, respectively. The mean serum OC levels were 15.9 ± 8.1 ng/mL and 14.8 ± 6.5 ng/mL, respectively. The mean serum CTX levels were 0.5 ± 0.4 ng/mL and 0.4 ± 0.3 ng/mL, respectively. The mean serum BSAP levels were 12.2 ± 5.3 mcg/L and 10.4 ± 4.3 mcg/L, respectively. BMD of group A was lower than that of group B (p < 0.05). In this study, variables such as sex, age, calcium, Vit-D, BASP, OC, and CTX showed no differences between the 2 groups. Conclusion: In Korean elderly population, BMD of patients with vertebral fracture showed significant difference from that of no vertebral fracture group. The occurrence of vertebral fracture is mainly related to lower BMD than another laboratory findings. It is important to prevent vertebral fractures by maintaining and normalizing BMD.
Surgical complications
92
P482: Disparities in postoperative outcomes by insurance status following elective spine surgery: a systematic review and meta-analysis
Neerav Kumar 1 , Izzet Akosman 1 , Richard Mortenson 2 , Grace Xu 3 , Abhinav Kumar 4 , Troy Amen 5 , Mitchell S. Fourman 6 , Ibrahim Hussain 7
1 Weill Cornell Medical College, New York, USA
2 Duke University, Durham, USA
3 Princeton University, Princeton, USA
4 Stanford University, Palo Alto, USA
5 Hospital for Special Surgery, New York, USA
6 Orthopaedic Surgery, Montefiore Medical Center, Bronx, USA
7 Neurological Surgery, Weill Cornell Medicine, New York, USA
Introduction: With increasing evidence demonstrating adverse outcomes for government insured patients following spine surgery, the expanding disparity between the care of privately and government insured patients is concerning. However, no pooled analyses have previously characterized differences in post-operative outcomes among patients with varying insurance types. The purpose of our review is to use an AI-assisted review platform to assess the effects of insurance status on postoperative outcomes following elective spine surgery. Material and Methods: A comprehensive literature search of PUBMED, MEDLINE(R), ERIC, and EMBASE was performed using a semi-automated cloud-based platform. 25 meta-analyses were performed to calculate pooled incidence rates and odds ratios for each outcome: 90-day readmission, non-routine discharge (NRD), extended length of stay (LOS), any complication (surgical and medical), and all medical complications. For each of these five outcomes, meta-analyses of the following comparisons were performed: (1) private versus government (Medicaid, Medicare, Veterans Affairs, Managed Care, and Triwest) insurance; (2) sub-analysis comparing Medicaid to private insurance; (3) sub-analysis comparing Medicare to private insurance; (4) Medicare versus Medicaid; and (5) Medicare versus non-Medicare (private and other government). Results: 38 studies (5,018,165 total patients) were included. Compared to private insurance, patients with government insurance had an increased incidence of 90-day readmissions (OR 1.84, p < 0.0001), NRD (OR 4.40, p < 0.0001), extended LOS (OR 1.82, p < 0.0001), post-operative complication (OR 1.61, p < 0.0001), and any medical complication (OR 1.93, p < 0.0001). These differences persisted across outcomes in sub-analyses comparing Medicare or Medicaid to private insurance. Similarly, across all examined outcomes, Medicare patients had a higher risk of experiencing an adverse event compared to non-Medicare patients. Compared to Medicaid patients, Medicare patients were only more likely to experience NRD (OR 2.68, p = 0.0007). Conclusion: Patients with government insurance have a greater likelihood of morbidity across several peri-operative outcomes. Additionally, Medicare patients fare worse than non-Medicare patients across outcomes, potentially due to age-based factors. These results warrant further granular analyses evaluating clinical and socioeconomic factors associated with suboptimal outcomes for government-insured patients. Based on our results, directed measures should be taken to ensure that underinsured patients receive equal access to resources and quality care.
191
P483: Does the choice of chemoprophylaxis affect the prevention of deep vein thrombosis in lumbar fusion surgery? A systematic review of literature
Sathish Muthu 1,2 , George Mavrovounis 3 , Stipe Corluka 4 , Zorica Buser 5 , Giovanni Barbanti Bròdano 6 , Yabin Wu 7 , Meisel Hans-Jorg 8 , Jeffrey C. Wang 9 , Timothy S. Yoon 10 , Andreas Demetriades 11 , AO Spine Knowledge Forum Degenerative 12
1 Department of Spine Surgery, Orthopaedic Research Group, Coimbatore, India
2 Department of Orthopaedics, Government Medical College, Karur, India
3 Department of Neurosurgery, University of Thessaly, Larissa, Greece
4 Department of Traumatology, University Hospital Centre Sestre milosrdnice, Zagreb, Croatia
5 Gerling Institute, Brooklyn, USA
6 IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
7 Research Department, AO Spine International, Davos, Switzerland
8 Department of Neurosurgery, Bergmannstrost Hospital, Halle, Germany
9 Department of Orthopaedic Surgery and Neurological Surgery, Keck School of Medicine, California, USA
10 Department of Orthopaedics, Emory University, Atlanta, USA
11 Department of Neurosurgery, Royal Infirmary Edinburgh, Edinburgh, United Kingdom
12 Knowledge Forum Degenerative, AO Spine Ineternational, Davos, Switzerland
Introduction: To date, the available guidance on venous thromboembolism (VTE) prevention in elective lumbar fusion surgery is largely open to surgeon interpretation and preference without any specific suggested chemoprophylactic regimen. This study aims to comparatively analyze the incidence of deep vein thrombosis (DVT) and pulmonary embolism (PE) with the use of commonly employed chemoprophylactic agents such as unfractionated heparin (UH) and low molecular weight heparin (LMWH) in lumbar fusion surgery. Methods: An independent systematic review of four scientific databases (PubMed, Scopus, clinicaltrials.gov, Web of Science) was performed by two authors to identify relevant articles in adherence to the preferred reporting in systematic reviews and meta-analysis (PRISMA) guidelines. Studies reporting on DVT/PE outcomes of lumbar fusion surgery in adult patients with UH or LMWH chemoprophylaxis were included for analysis. Analysis was performed using the Open Meta[Analyst] software. Results: Twelve studies with 8495 patients were included in the analysis. A single-arm meta-analysis of the included studies found an incidence of DVT 11.80 (95%CI [6.40% - 17.10%]) and 1.30% (95%CI [0.50% - 2.10%]) with LMWH and UH respectively. Both the chemoprophylaxis agents prevented PE with a noted incidence of 0% (95%CI [0% - 0.10%]) and 0.40% (95%CI [0% - 0.90%]) with LMWH and UH respectively. The risk of bleeding-related complications with their usage was 0.20% (95% CI [0.10% - 0.30%]). Conclusion: Both LMWH and UH are effective in reducing the overall incidence of DVT/PE, but there is a paucity of evidence analyzing the comparative effectiveness of the chemoprophylaxis regimens in lumbar fusion procedures. The heterogeneity in data prevents any conclusions, as there remains an evidence gap. We recommend future high-quality RCTs to investigate in this regard to help develop recommendations on thromboprophylaxis usage.
224
P484: Hardware failure in spinal tumor surgery: a hallmark of longer survival?
Nikita Zaborovskii 1,2 , Anton Denisov 3 , Adam Schlauch 4 , John Shapton 4 , Dmitry Ptashnikov 1,5 , Sergei Masevnin 1 , Oleg Smekalenkov 1 , Dimitriy Kondrashov 4,6
1 Spinal and Bone Tumor Surgery, Vreden Orthopedic Institute, Saint-Petersburg, Russian Federation
2 Saint-Petersburg State University, Saint-Petersburg, Russian Federation
3 Spinal Unit, Hospital Quirónsalud San José, Madrid, Spain
4 San Francisco Orthopaedic Residency Program, San Francisco, USA
5 North-Western State Medical University named after I.I.Mechnikov, Saint-Petersburg, Russian Federation
6 Spinal Surgery, Saint Mary’s Hospital, USA
Introduction: The incidence of spinal tumors is increasing, and surgical interventions for spinal tumors are becoming more common. Instrumentation failure in spine tumor surgery is a common reason for a revision operation. With recent surgical and medical advances, patient survival is expected to increase, which will demand a better understanding of the hardware longevity. A fusion is not always feasible in the setting of metastatic disease, which will mean that hardware will have to potentially withstand physiological stresses for life. The objective of this study was to investigate risk factors for instrumentation failure requiring revision surgery in patients with spinal tumors. Material and Methods: This was a retrospective cohort from a single tertiary care specialty hospital from January 2005 to January 2021, for patients with spinal primary or metastatic tumors who underwent surgical intervention with instrumentation. Demographic and treatment data were collected and analyzed. Kaplan-Meier analysis was performed for overall survival, and separate univariate and multivariate regression analysis was performed. Results: A total of 351 patients underwent surgical intervention for spinal cord tumor, of which 23 experienced instrumentation failure requiring revision surgery (6.6%). Multivariate regression analysis identified pelvic fixation (OR = 10.9), spinal metastasis invasiveness index (OR = 1.11), and survival of greater than 5 years (OR = 3.6) as significant risk factors for hardware failure. One- and five-year survival rates were 57% and 8%, respectively. Conclusion: Instrumentation failure after spinal tumor surgery is a common reason for revision surgery. Our study suggests that use of pelvic fixation, invasiveness of the surgery, and survival greater than 5 years are independent risk factors for instrumentation failure.
316
P485: Knotless tailless running subcuticular skin closure using non-barbed monofilament suture may reduce the risk for surgical site infection in posterior spine surgery
Philip Hanna 1 , Valerie Kiers 2 , Saechin Kim 1
1 Orthopaedic Surgery, MassGeneral Brigham/Harvard Medical School, Boston, USA
2 Hasbro Children's Hospital, Providence, USA
Introduction: Surgical site infections (SSIs) can add significant costs to patient care as well as societal and personal costs. SSI can start prior to or after the wound closure. For the latter, the infection most likely occurs through the incision. Optimal surgical wound skin closure method would provide good cosmesis while minimizing the risk for SSI. Subcuticular running wound closure with non-barbed absorbable sutures is often used in spine surgery. Two common methods of managing the ends of the sutures are buried knots or tails/knots outside the skin. Suture reactions seen with both methods and loss of wound closure tension seen with tails/knots outside the skin can increase the risk for wound breakdown. Our hypothesis is that a knotless tailless subcuticular closure (KT) method that maintains wound closure tension reduces this risk and decreases the rate of return to the operating room (ROR) because of SSI. Materials and Methods: After IRB approval, a retrospective review of billing and hospital records was used to obtain all surgeries performed by spine surgeons in a department of a tertiary referral center. Inclusion criteria were posterior cervical, thoracic, and lumbar spine surgery and running subcuticular wound closure using non-barbed absorbable sutures. Exclusion criteria were previous infection in the same site, oncologic surgery, and percutaneous screws, and less than 3 months of follow up (f/u). Rotating residents, fellows, and advanced practitioners in the department help close the surgical wound in layers. Since 2014, the senior author has used a novel KT method in which the suture tension is maintained by running overlapping stitches at the ends of the incision and the ends of the suture are cut at the skin once the subcuticular closure is completed, resulting in a knotless tailless closure. We compared rates of ROR for SSI within one year of the index surgery between cases done by the senior author between 2014 and 2021 using the KT method (KTG) and by other spine surgeons in the department in 2018 (CG) when only the senior author was using this KT method. Patient demographics, medical and surgical history, and ROR rates were compared between the two groups. Results: No differences were seen in demographics, BMI, smoking or diabetes history, history of previous surgery in the same site or the number of levels fused per case between KTG (n = 268) and CG (n = 559). There were statistically more instrumented cases in KTG (174/268 = 65%) than CG (201/559 = 36%) (p < .0001) that would increase the risk for SSI in KTG. The rate of ROR for SSI in KTG (1/268 = 0.4%) was less than that in CG (22/559 = 4%) and the difference was statistically significant (p = .0035). Discussion: Our current study shows a statistically lower rate of ROR for SSI when the described KT method is used to close the wound with running subcuticular closure in posterior spinal surgery. We believe that the risk is decreased because the described KT method avoids suture reactions due to buried knots or knots/sutures outside the skin while maintaining wound closure tension better than tails left outside the skin.
387
P486: Is low regional Hounsfield Units of screw trajectory being one of the risk factors of hardware failure after posterior cervical fusions with instrumentation?
Lei Kuang 1 , Zejun Chen 1 , Guohua Lv 1
1 Department of Spinal Surgery, The Second Xiangya Hospital of Central South University, Changsha, China
Introduction: For patients with multilevel degenerative cervical myelopathy, laminectomy and posterior cervical fusions (PCFs) with instrumentation are widely accepted technique for symptom relief. However, hardware failure is not rare which results in neck pain or even permanent neurological leision. The prevalence of hardware-related complications of laminectomy and posterior cervical fusions (PCFs) with instrumentation are lack of in-depth study. This study aims to investigate risk factors of hardware failure after laminectomy and posterior cervical fusions (PCFs) with instrumentation in patients with degenerative cervical myelopathy. Material and Methods: Fifty-six patients who underwent laminectomy and posterior cervical fusions (PCFs) with instrumentation between January 2019 and January 2021 were included in a single institution. Patients were divided into the hardware failure group (n = 14) and no hardware failure group (n = 42). The sex, age, screw density, end vertebra (C7 or T1), cervical sagittal alignment parameters (C2-C7 lordosis, C2-C7 sagittal vertical axis, T1 slope, CL correction), and regional Hounsfield units (HU) of screw trajectory, commorbity of osteoporosis were collected and compared between the two groups. Results: There were no significant statistical differences in general information (age, gender, follow-up period) of patients between the two groups. The differences of fixation levels and screw density between the two groups were not statistically significant (p > 0.05). The failure rate of the fixation endpoint at T1 was lower than that at C7 (9% vs. 36.3%) (p < 0.05). The regional HU of pedicle screw (PS) and lateral mass screw(LMS) in failure group were lower than the ones of no failure group (PS: 267 ± 45 vs. 368 ± 43; LMS: 308 ± 53 vs. 412 ± 41) (p < 0.05). The saggital alignment parameters did not show significant differences between the two groups before surgery and at final follow-up (p > 0.05). The hardware failure rate in cases without osteoporosis was lower than that in cases with osteoporosis (14.3% vs. 57.1%) (p < 0.05). Conclusion: Hardware failure was not uncommon after laminectomy and PCFs with instrumentation in patients with degenerative cervical myelopathy. Osteoporosis, fixation ended at C7, and low regional HU of screw trajectory were the independent risk factors.
396
P487: In lumbar posterior decompression surgery, is there a change in postoperative pain with the number of surgical vertebrae?
Yushi Hoshino 1 , Hajime Nishida 1 , Ryousuke Ikeda 1 , Ichiro Okano 2 , Ryo Yamamura 2 , Yoshinori Imaizumi 1 , Yoshifumi Kudo 2
1 Department of Orthopedic Surgery, Asahi University Hospital, Gifu, Japan
2 Department of Orthopedic Surgery, Showa University Hospital, Tokyo, Japan
Introduction: Postoperative pain has been shown to affect patient satisfaction and treatment efficacy. Moreover, it is clear from previous reports that postoperative pain in spine surgery is one of the most intense among various surgical procedures. However, few reports have examined whether there is a difference in postoperative pain depending on the number of intervertebral segments operated on. In this study, we investigated whether differences in the number of intervertebral spaces are related to the intensity of postoperative pain in lumbar posterior decompression surgery. Material and Methods: A total of 129 patients underwent consecutive lumbar posterior decompression surgeries (longitudinal split spinous process widening) at our hospital from January 2020 to August 2022. Pain was evaluated preoperatively, 1.3.6 hours postoperatively, and 1.2.3.7 days postoperatively using the Numerical Rating Scale (NRS). Postoperative pain management consisted of IV-PCA and multimodal analgesia with acetaminophen plus pentazocine time IV. The number of patients who required rescue due to postoperative pain was also compared. Results: 76 males, 53 females, mean age: 64,4 years, by number of decompressed intervertebral spaces: 1 intervertebral space: 46 cases, 2 intervertebral spaces: 54 cases, 3 or more intervertebral spaces: 29 cases. Preoperative pain (NRS): 7.1/7.8/ 7.8/ 7.8 (1 intervertebral/ 2 intervertebral/ 3 or more intervertebral), 1h postoperative: 3.9/3.2/4.7, 6h postoperative: 2.8/2.3/2.4, 1d postoperative: 4.4/4.6/5.1, 3d postoperative: 3.6/3.4/3.6, 1w postoperative: 2/2.1/2. Results showed that at any time There was no significant difference in NRS values. The number of cases requiring rescue due to postoperative pain was 5/4/5. No significant difference was found between the number of cases used. Discussion: Postoperative pain has been reported to be a factor in chronic low back pain and is associated with decreased patient satisfaction. Postoperative pain in spine surgery is severe, and it is often difficult to improve the pain. It is conventionally thought that the greater the intraoperative invasiveness, the greater the postoperative pain in proportion to the invasiveness, but in the present study, no relationship was found between the number of surgical vertebral segments and postoperative pain. Even if the decompression is performed on a single vertebra, the patient feels and expresses pain in the same way as with multiple vertebrae. Therefore, aggressive postoperative pain management is necessary regardless of the number of intervertebral spaces. However, the number of cases is small, and further studies with a larger number of patients are needed. Conclusion: There was no significant difference in the number of operated vertebrae and postoperative pain intensity in lumbar posterior decompression surgery.
427
P488: Bispectral EEG to predict delirium after spine fracture in older adults
Elisabeth Martin 1 , Aspen Miller 2 , McKenzie Temperly 1 , Steele McCulley 2 , Alex Coffman 2 , Michael Willey 2 , Catherine Olinger 2
1 Carver College of Medicine
2 Department of Orthopaedics and Rehabilitation, University of Iowa, Iowa City, USA
Introduction: Delirium is a frequent and serious complication among older patients with spine fracture. Negative consequences of delirium such as medical complications, prolonged skilled nursing facility admission, and mortality can be mitigated with early detection. Screening questionnaires to detect delirium are available; however, their effectiveness declines when implemented in busy hospital workflows. Bispectral electroencephalography (BSEEG) is an objective point-of-care test previously validated to detect onset of delirium in older hospitalized adults. Its simplified 2-measurement-lead placement and rapid, hands-off measurement make it an attractive alternative to traditional questionnaire-based methods. The aim of this study is to evaluate the effectiveness of BSEEG as a delirium screening tool for older adults with spine fracture. We hypothesize that the BSEEG can effectively predict delirium in this population. Material and Methods: Patients over 50 years with spine fracture were prospectively enrolled from University of Iowa Hospitals & Clinics. Patients were excluded if they were non-English speaking, had an active psychotic disorder, or were on a ventilator. Baseline demographics were recorded including age, sex, and Charlson Comorbidity Index. Baseline cognitive function was measured using the Mini-Mental State Examinations (MMSE). Delirium was assessed clinically using the 3-Minute Diagnostic Interview for Confusion Assessment Method (3D-CAM) twice daily. BSEEG measurements were collected twice daily for up to 6 days of hospital admission and compared to a previously established power spectral density ratio threshold to determine a binary delirium prediction. Statistics were executed with GraphPad. This study was approved by IRB. Results: 18 subjects were enrolled in the study. The subject demographics are as follows: 44% female, age 73.4 ± 11.6, and 100% white/non-Hispanic. 5/18 subjects (33%) experienced delirium. Nutritional status and baseline cognition are not significantly different for patients who did and did not experience delirium. The following preliminary performance metrics were determined for the device: sensitivity = 0.21, specificity = 0.5, positive predictive value = 0.60, and negative predictive value = 0.15. Conclusion: Results are limited by sample size and pending enrollment of 49 subjects for sufficient power. Preliminary results do not support the conclusion that BSEEG is an effective method of predicting delirium in older adults with spine fracture. Ongoing enrollment is needed to determine if BSEEG can effectively detect delirium for this population. If effective, bispectral encephalography would provide a simple, novel, and objective screening tool for delirium in patients with spinal fracture. Effectively identifying patients at risk for delirium would allow the healthcare team to prevent negative effects such as medical complications, extended admission, and skilled care after discharge for older adults with spinal fracture.
507
P489: Lumbar fusions in patients with sickle cell disease: a propensity-matched analysis of postoperative complications
Andy Ton 1 , Michael Brown 2 , Kevin Mertz 3 , Siddharth Patel 1 , Hannah Shelby 1 , Brandon Gettleman 4 , Emily Mills 1 , Jeffrey Wang 1 , Raymond Hah 1 , R. Kiran Alluri 1
1 Keck School of Medicine of USC, Los Angeles, USA
2 Orthopaedic Surgery,Keck School of Medicine of USC, Los Angeles, USA
3 Orthopaedic Surgery, Harbor-UCLA Medical Center, Los Angeles, USA
4 Orthopaedic Surgery, University of South Carolina School of Medicine, Columbia, USA
Introduction: Sickle cell disease (SCD) is an inherited hemoglobinopathy that confers considerable perioperative risks. Lumbar spinal fusions can impose high physiological demands that precipitate further adverse outcomes in this population. This study therefore compares postoperative complications across patients with and without SCD undergoing one to three-level lumbar fusion for degenerative pathologies. Material and Methods: Patients who underwent one to three-level lumbar fusion for degenerative lumbar pathologies from 2010-2021 were identified using the PearlDiver database. Patients with sickle cell trait, previous lumbar surgery, preoperative opioid use, deformity, trauma, malignancy, infection were excluded. Patients were separated into 1) SCD or 2) non-SCD and propensity-matched 1:1 for age, sex, elixhauser comorbidity index (ECI), surgical approach, and various comorbidities. Chi-squared analysis and Mann-Whitney-U were conducted to separately compare complications by single- and multi-level procedures. Results: Propensity-score matching identified 1,934 SCD and 2,111 non-SCD patients who underwent single-level fusion and 2,094 SCD and 2,111 non-SCD who underwent multi-level fusion. Across single-level fusions, SCD had significantly higher risk of neurovascular complications (OR: 16.10; 95%CI: 12.85-20.17; p < 0.001), short-term complications (OR: 2.33; 95%CI: 2.05-2.66; p < 0.001), venous thromboembolism (OR: 1.71; 95%CI: 1.19-2.45; p = 0.004), myocardial infarction (OR: 2.26; 95%CI: 1.42-3.60; p = 0.001), pneumonia (OR: 1.37; 95%CI: 1.04-1.82; p = 0.032), and UTI (OR: 1.44; 95%CI: 1.16- 1.79; p = 0.001). SCD patients additionally demonstrated increased opioid usage at 1- (OR: 1.34; 95%CI: 1.18-1.52; p < 0.001), 6- (OR: 1.26; 95%CI: 1.02-1.56; p = 0.033), and 12-months (OR: 1.46; 95%CI: 1.07-1.97; p = 0.018). In the setting of multi-level fusions, SCD carried higher risk for neurovascular complications (OR: 11.27; 95%CI: 9.21-13.79; p < 0.001), short-term complications overall (OR: 2.12; 95%CI: 1.85-2.41; p < 0.001), pneumonia (OR: 1.42; 95%CI: 1.09-1.85; p = 0.010), and UTI (OR: 1.45; 95%CI: 1.20-1.76; p < 0.001). Opiate use at one (OR: 1.23; 95%CI: 1.09-1.39; p = 0.001) and six months (OR: 1.32; 95%CI: 1.08-1.62; p = 0.009) were significantly greater in patients with SCD across multi-level procedures. Conclusion: Patients with SCD undergoing lumbar spine fusion for degenerative pathologies demonstrate higher risks for coagulopathic, ischemic, and infectious-related complications, compared to matched, non-SCD patients. Despite excluding patients with preoperative opioid use, patients with SCD were at greater risk for long-term opioid utilization, highlighting the need for specialized and interdisciplinary care to adequately meet the needs of this patient population. As such, awareness of the unique complication risks in patients with SCD may help guide spine surgeons in refining perioperative management strategies to optimize outcomes in this demographic.
625
P490: Revision surgery is associated with highly increased length of stay in posterior spinal fusion surgery
Alexander Hammer 1,2 , Denis Rappert 1 , Olga Cheremina 1 , Klaus Schnake 1,3
1 Center for Spinal and Scoliosis Surgery, Malteser Waldkrankenhaus St. Marien, Erlangen, Germany
2 Department of Neurosurgery
3 Department of Orthopedics and Traumatology, Paracelsus Medical University, Nürnberg, Germany
Introduction: We examined a collective of posterior thoracolumbar spinal fusion surgery up to 4 segments in order to detect significant factors for increasing length of stay (LOS). Material and Methods: We analyzed 223 patients with the aim to detect factors having a significant impact on the LOS. The investigated factors were: dural tear, previous local surgery, revision surgery during hospital stay, BMI (Body Mass Index), age, sex, ASA-grade (American Society of Anesthesiologists), diabetes mellitus, preoperative anticoagulation and number of segments. Univariate testing was performed with the Mann-Whitney-U-Test. Multivariate testing comprised linear regression analysis. Results: The mean LOS was 11.9 d (5-51d ± 6.1d). Mann-Whitney-U-Testing revealed the factors revision surgery (p < 0.0001; without revision surgery LOS 10.3d, with revision surgery LOS 19.3d), dural tear (p = 0.018; without dural tear LOS 11.6d vs with dural tear LOS 13.8d), age (p = 0.00052; < 64 years LOS 10.7d vs ≥ 65 years LOS 13.3d), ASA Grade (p = 0.043; ASA 1+2 LOS 10.8d vs ASA 3 LOS 13.6d), anticoagulation medication (p = 0.038; no anticoagulation LOS 11.6d vs anticoagulation LOS 13.5d) and the number of levels of surgery (p < 0.0001; 1 or 2 levels LOS 11.2d vs 3 or 4 levels LOS 13.9d) as significant factors associated with increased length of stay. In linear regression analysis revision surgery (unstandardized B 9.5; p < 0.0001; 95% CI 7.6 - 11.5) and number of levels of surgery (unstandardized B 2.0; p = 0.017; 95% CI 0.4-3.7) remained significant factors which predicted a higher LOS (R Square: 0.45, Durbin-Watson 1.65). Conclusion: Both, revision surgery during the initial hospital stay and the number of levels of surgery have an effect on the LOS in posterior thoracolumbar spinal fusion surgery up to 4 segments.
677
P491: Lateral lumbar interbody fusion at L4-5 has a low rate of neurologica, psoas-related and abdominal complications in appropriately selected patients when utilising a standardised surgical techniques
Aaron Buckland 1 , Nam Hunyh 1 , Cristiano Menezes 2 , Ivan Cheng 3 , Brian Kwon 4 , Themistocles Protopsaltis 5 , Brett Braly 6 , J. Alex Thomas 7
1 Spine and Scoliosis Research Associates Australia, Windsor, Australia, Orthopaedics, Columna Instituto, Cidade Jardim, Brazil
3 St. David's Medical Center, Austin, USA
4 Orthopaedic Surgery, Tufts University School of Medicine, Boston, USA
5 Orthopaedic Surgery, Langone Health, New York, USA
6 The Spine Clinic of Oklahoma City, Oklahoma City, USA
7 Atlantic Neurosurgical and Spine Specialists, Wilmington, USA
Introduction: This study aims to reassess the rate of neurological, psoas-related and abdominal complications associated with L4-5 lateral lumbar interbody fusion (LLIF) with standardised preoperative assessment and procedural technique. Material and Methods: A multi-centre retrospective cohort review of consecutively enrolled patients that underwent LLIF including the L4-5 disc level by 7 surgeons at 7 institutions in 3 countries over a 5-year period was performed. Patient demographics, procedural characteristics, reoperations and complications, including femoral and non-femoral neurapraxia, thigh pain, hip flexor weakness and abdominal complications were analysed. Neurological and psoas-related complications were attributed to LLIF or posterior instrumentation and presence of persistent symptoms determined at 1-year postoperatively. Results: In total, 517 patients were included with a mean age of 65.0 ± 10.3 years and BMI of 29.2 ± 5.5 kg/m2. A mean 1.2 ± 0.6 levels were fused with LLIF and 1.6 ± 0.9 posterior levels were fused. Femoral neurapraxia occurred in 1.2% of patients, of which 0.8% were LLIF-related and 0.4% persistent at 1-year postoperatively. Non-femoral neurapraxia occurred in 1.9% of patients, 0.2% were LLIF-related and 1.0% persistent at 1-year. All LLIF-related neurapraxias resolved by 1-year. Thigh pain was experienced in 6.2% of patients, 6.0% were LLIF-related and 0.6% were persistent at 1-year. Hip flexor weakness occurred in 2.7% of patients, 1.6% were LLIF-related and 0.6% were persistent at 1-year. No patients experienced bowel injury, 0.6% experienced intraoperative vascular injury (not LLIF-related) and 1.0% experienced ileus. Reoperations occurred in 1.2% of patients within 30-days, 6.8% within 90-days and 7.7% within 1-year postoperatively. Conclusion: LLIF involving the L4-5 disc level has a low rate of persistent neurological, psoas-related and abdominal complications in appropriately indicated patients and maintaining standardised surgical technique.
731
P492: Postoperative ketamine may increase risk of venous thromboembolism in chronic opioid users after spine surgery
Michael McCurdy 1 , Yunsoo Lee 1 , Rajkishen Narayanan 1 , Delano Trenchfield 1 , Tariq Issa 1 , Sebastian Fras 1 , Ryan Cha 1 , Mina Ebrahimi 1 , Michael Carter 1 , Olivia Opara 1 , John Mangan 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Christopher Kepler 1 , Gregory Schroeder 1
1 Orthopaedic Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: Venous thromboembolism (VTE) is a serious adverse event that affects anywhere from 0.29 – 31% of patients after spine surgery. Risk factors and prophylaxis have been well-characterized in other specialty fields of orthopaedics, specifically hip and knee arthroplasty, but research is not as robust in spine. Although numerous risk factors for VTE exist in the literature, little exists on the impact of opioid use and postoperative pain management on VTE risk. Opioid use is especially prevalent in patients undergoing spine surgery, with at least 20% of patients reporting taking opioids leading up to surgery. Although recent literature has shown perioperative ketamine can reduce opioid consumption postoperatively, there is scarce literature on postoperative ketamine use and its impact on complications after spine surgery. The aim of this study was to assess the risk of VTE in chronic opioid users undergoing spine surgery, particularly those who received postoperative ketamine for pain management. Material and Methods: After Institutional Review Board approval, we conducted a structured query language (SQL) search to identify patients with diagnosis of venous thromboembolism (VTE) after spine surgery from 2017-2021 at a single, urban, tertiary care center. Chart review was performed to confirm patient demographics, surgical details, surgical outcomes, and postoperative ketamine use. Opioid use was identified using the Prescription Drug Monitoring Program (PDMP) for each patient. Chronic opioid users were defined as having > 182 days or > 9 opioid prescriptions prescribed in the 12 months before surgery, following guidelines from the CDC and other recent spine literature. Statistical analysis was performed to compare patients with VTE after spine surgery to patients without VTE. A 3:1 propensity match of the two groups was then performed utilizing age, BMI, race, sex, and levels fused. Results: 328 total patients were identified with complete PDMP and postoperative ketamine data, including 33 patients with confirmed VTE after spine surgery. Patients in the VTE group had significantly longer operating room times (258 vs. 192 minutes, p = 0.009) than patients in the no VTE group. Additional surgery (1.36% vs. 9.09% p = 0.025) and takeback for infection (0.68% vs. 9.09%, p = 0.008) were also significantly associated with the VTE group. Bivariate analysis of postoperative ketamine use found significant association with VTE occurrence after surgery (15.2% vs. 4.07%, p = 0.019). Chronic opioid users were similarly distributed between the VTE and no VTE group (36.4% vs. 24.1%, p = 0.184). After matching, postoperative ketamine (6.06% vs. 15.2%, p = 0.141) and chronic opioid users (25.3% vs. 36.4%, p = 0.314) were found to be similar between the VTE and no VTE groups. Conclusion: Recent alternative methods of postoperative pain management, including ketamine, have become increasingly popular in attempts to reduce postoperative opioid consumption. Our study found that postoperative ketamine may have unintended effects on outcomes, such as a potential increase in the risk of VTE after spine surgery.
744
P493: Risk factors for wound-related complications following spine surgery for primary and metastatic spine - Systematic review
Amir Khadmy 1
1 Orthopedic Surgery, Rabin Medical Center, Petah Tikva, Israel
Introduction: Wound-related complications commonly occur following spine surgery and can lead to significant morbidity and mortality. The purpose of this systematic review was to identify the risk factors for wound-related complications following spine surgery for primary and metastatic spine tumors. Material and Methods: A systematic literature search was conducted to identify studies that investigated the risk factors for wound-related complications following spine surgery for primary and metastatic spine. The search was conducted PubMed, Embase, and Cochrane databases was conducted for all retrospective studies published between 2013 and 2023 that included the keywords "metastatic spine," "spine," "surgical site infection", "tumor", "surgery", "metastatic tumor,", "wound complications", and "retrospective study". Studies were excluded if they were systematic reviews, case reports, or did not report on risk factors for wound-related complications. A total of 25 studies were included in the review.
Results:
The most common risk factors for wound-related complications were:
• Obesity (odds ratio (OR) 2.2, 95% confidence interval (CI) 1.4-3.5)
• Diabetes (OR 1.7, 95% CI 1.1-2.7)
• Smoking (OR 1.4, 95% CI 1.1-1.8)
• Preoperative wound infection (OR 4.2, 95% CI 2.0-8.9)
• Emergency surgery (OR 1.6, 95% CI 1.1-2.3)
• Operation time > 3 hours (OR 1.4, 95% CI 1.1-1.8)
Conclusion: The findings of this systematic review suggest that obesity, diabetes, smoking, preoperative wound infection, emergency surgery, and operation time > 3 hours are the most important risk factors for wound-related complications following spine surgery for primary and metastatic spine tumors. These findings can be used to help identify patients at high risk for wound complications and to develop strategies to prevent these complications.
864
P494: Surgical site infection in thoracolumbar junction fractures treated surgically with posterior fusion instrumentation
Jlidi Mohamed 1 , Amine Soussou 1 , Walid Bouaicha 1 , Ibrahim Najjar 1 , Mouldi Lamouchi 1 , Karim Mallek 1 , Mohssen Chamekh 1 , Imen Chaabeen 2 , Sabrine Bachrouch 2 , Achref Abdennadher 3 , Selim Daas 1
1 Orthopedics and Traumatology Department
2 Internal Medicine Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia
3 Orthopedics and Traumatology Department, Military Hospital of Instruction, Tunis, Tunisia
Introduction: Common thoracolumbar junction fractures often necessitate surgical treatment to stabilize and restore spinal anatomy, aiming for improved outcomes. Sepsis is one of the most serious complications of spinal surgery in terms of patient health status and clinical outcomes. It complicates 3.1% of all spine surgeries. Several factors including patient’s history, type and duration of the surgery were reported as predisposing factors. We aim to evaluate the incidence of sepsis in patients treated surgically with posterior fusion instrumentation and to identify the risk factors. Material and Methods: A retrospective study including patients with thoraco-lumbar junction fractures treated surgically with posterior fusion instrumentation between January 2010 and January 2020. We recorded socio demographic data, hospital stay, operative delay, technique, and duration of the surgical procedure. The neurological status was assessed using the Frankel-ASIA score. We evaluated the risk factors of sepsis in thoraco-lumbar junction fractures. Results: One hundred twenty patients were included with a mean age of 48.39 ± 14 years. Gender Ratio was 1.6. Surgical treatment was complicated with sepsis in 6 patients (4 females 2 males). All the cases were early sepsis. The organism causing the infection was identified in all cases. Patients with higher BMI were found to be prone de develop more sepsis with statistical significance (p = 0.01). Multivariate logistic regression analysis identified only one risk factor: diabetes (Ratio Odds = 1.7 CI 95% [0.02 -0.514]). The incidence of sepsis was associated with the BMI (r = 0.02). Neurological deficit (r = 0.409), Frankel-Asia score (r = 0.545), hospital stay (r = 0.593), operative delay (r = 0.104) and operative duration (r = 0.09) were not associated with infection. With regards to the operative technique, infection was not associated with the different procedures such as laminectomy (r = 0.05), bone grafting (r = 1,055). Furthermore, intra canalar fragments (r = 0.45), vertebral dislocations (r = 0.689) and articular fracture (r = 0.79) didn’t seem to increase the risk for sepsis. Conclusion: Post-operative wound infection is a significant complication of posterior spine surgery. This causes distress for both patients and surgeons alike. Surgical site infections in spine surgery remain a significant cause of morbidity and prolonged hospitalization. The review of the literature reported that uncontrolled diabetes, spine instrumentation and long duration of surgery are significant risk factors for surgical site infection. In our study, diabetes and obesity were the most reported risk factors. Prevention and control of patient’s comorbidities are the first steps to reduce the incidence of sepsis.
935
P495: Anterior thoracic surgery - Transpleural versus retropleural approach
Pavlos Bountliakis 1 , Sebastian Ruetten 1 , Martin Komp 1
1 Center for Spine Surgery and Pain Therapy, Center for Orthopaedics and Traumatology of the St. Elisabeth Group-Catholic Hospitals Rhein-Ruhr, St. Anna Hospital Herne, Marienhospital Herne University Hospital, Marien Hospital Witten, Germany
Question: There are several possible approaches for anterior surgery of pathologies of the thoracic spine. The lateral transpleural approach is very important because it enables direct access to the spine and can be performed minimally invasively as a mini-thoracotomy, however, perioperative problems have been reported with this approach. This prospective study was conducted to clarify whether the retropleural approach has any advantages over the transpleural approach in a lateral thoracotomy. Method: A total of 60 patients (30 per group) were included in the study. Inclusion criteria were: fractures, tumors, monosegmental spondylodiscitis in T5 to T12 with an indication for anterior stabilization following prior posterior instrumentation. Exclusion criteria were multisegmental pathologies, deformities, and previous ipsilateral pulmonary/thoracic operations. The approach was via a lateral mini-thoracotomy for all patients. A retropleural approach was used for the patients in group 1; transpleural approach in group 2. The follow-up observation period was 12 months and 51 (25/26) patients were available for follow-up. In addition to intra- and perioperative parameters, validated measuring instruments were used. Results: In group 1, injuries of the parietal pleura occurred in two patients. These patients were fitted with a Bülau drain post-operatively, as were all patients in group 2. The mean operation time was shorter in group 1. In group 2, post-operative pneumonia occurred in two patients; a clinically relevant pleural effusion required aspiration in six cases. Atelectasis was detected in the postoperative chest X-ray in two patients in group 2. In one patient in group 1, an extrapleural seroma required aspiration. The mean hospital stay was one day shorter in group 1 than in group 2. After 12 months, there were no significant differences between the two groups in the constant results of the measuring instruments. Conclusions: In a lateral mini-thoracotomy, a retropleural approach is a viable alternative to a transpleural approach. Aside from advantages during surgery, there were significantly fewer postoperative pulmonary complications. This is also reflected in the reduction of the hospital stay. No significant difference between the two groups was found after 12 months. This correlates with available data in literature.
952
P496: Failure rate of decompression-only procedure for lumbar degenerative spondylolisthesis - Evidence from a PRISMA compliant systematic review of literature
Sathish Muthu 1,2 , Stipe Corluka 3 , Zorica Buser 4 , James Malcolm 5 , Zhuojing Luo 6 , Prajwal G S 7 , Luca Ambrosio 8 , Cristiana Griffoni 9 , Andreas Demetriades 10 , Stjepan Dokuzovic 3 , Yabin Wu 11 , Jeffrey C. Wang 12 , Meisel Hans-Jorg 13 , Timothy S. Yoon 5
1 Spine Surgery, Orthopaedic Research Group, Coimbatore, India
2 Department of Orthopaedics, Government Karur Medical College, Karur, India
3 Department of Traumatology, University Hospital Center Sestre Milosrdnice, Zagreb, Croatia
4 Gerling Institute, Brookyln, USA
5 Department of Orthopaedic Surgery, Emory University, Georgia, USA
6 Department of Orthopaedics, Fourth Military Medical University, Xian, China
7 Department of Orthopaedics and Spine Surgery, Bangalore Hospital Kengeri, Kengeri, India
8 Department of Orthopaedics & Trauma, Università Campus Bio-Medico di Roma, Rome, Italy
9 University of Bologna, Instituto Ortopedico Rizzoli, Bologna, Italy
10 Department of Neurosurgery, Royal Infirmary Edinburgh, Edinburgh, United Kingdom
11 Research Department, AO Foundation, Davos, Switzerland
12 Department of Orthopaedic Surgery, Keck School of Medicine, California, USA
13 Department of Neurosurgery, BG Klinikum Bergmannstrost Halle, Halle, Germany
Introduction: To identify the failure rates of individual methods of decompression-only procedures to aid in the selection of the best possible method to achieve decompression that works the best in the hands of a given surgeon. Methods: An independent systematic review of four scientific databases (PubMed, Scopus, clinicaltrials.gov, Web of Science) was performed to identify relevant articles as per the preferred reporting in systematic reviews and meta-analysis (PRISMA) guidelines. Studies reporting on failure rates of decompression-only procedure for degenerative lumbar spondylolisthesis were included for analysis. Analysis was performed using the Open Meta [Analyst] software. Results: The overall failure rate of decompression-only procedure 9.1% (95% CI [6.5, 11.7]). Further, open decompression had the highest failure rate of 10.9% (95% CI [6.5, 11.7]), while micro-endoscopic decompression had the least failure rate of 6.7% (95% CI [2.9, 10.6]). Similarly, the highest failure of 15.4% (95% CI [9.4, 21.4]) was noted at 2 years while the least failure of 5.8% (95% CI [-7.0, 18.6]) was noted during the first year following surgery. Single level decompression had a failure rate of 10.5% (95% CI [7.1, 13.9]), while multi-level decompression recorded a failure rate of 6.2% (95% CI [2.8, 9.5]). Conclusion: High-quality evidence on the decompression-only procedure for degenerative spondylolisthesis is limited. The decompression-only procedure had an overall failure rate of 9.1% with open decompression approach resulting in the highest failure rates compared to other minimally invasive approaches.
1027
P497: Incidence and risk factors for symptomatic spinal epidural hematoma following posterior thoracic spinal surgery in a single institute
Longjie Wang 1 , Hui Wang 2 , Zhuo Ran Sun 1 , Zhongqiang Chen 1 , Chuiguo Sun 1 , Weishi Li 1
1 Orthopedics, Peking University Third Hospital, China
2 Orthopedics, The Third Hospital of Hebei University, China
Introduction: Symptomatic spinal epidural hematoma (SSEH) is one of the most devastating complications after spinal surgery. Numerous studies have identified many risk factors for SSEH, but most of them have drawn conclusions based on a cohort of lumbar and cervical spine patients. Therefore, the purpose of this study was to investigate the incidence of SSEH and recognize the risk factors based on patients who underwent posterior thoracic surgery. Material and Methods: From January 2010 to December 2019, patients who developed SSEH after posterior thoracic surgery and underwent hematoma evacuation were enrolled. For each SSEH patient, 2 or 3 controls who did not develop SSEH and underwent the same procedures with similar complexity at the same section of the thoracic spine in the same period were collected. The preoperative and intraoperative factors, blood pressure-related factors and radiographic parameters were collected to identify possible risk factors by comparing between the 2 groups. Results: A total of 24 of 1612 patients (1.49%) were identified as having SSEH after thoracic spinal surgery. Compared to the control group (53 patients), SSEH patients had significant differences in the APTT (p. 0.028), INR (p. 0.009), ratio of previous spinal surgery (p. 0.012), ratio of cerebrospinal fluid leakage (p. 0.004), thoracic kyphosis (p < 0.05), local kyphosis angle (p < 0.05), epidural fat ratio at T7 (p. 0.003), occupying ratio of the cross-sectional area (p < 0.05) and spinal epidural venous plexus grade (p < 0.05). Multiple logistic regression analysis revealed 3 risk factors for SSEH: cerebrospinal fluid leakage, the local kyphosis angle (> 8.77") and the occupying ratio of the cross-sectional area (> 49.58%). Conclusion: The incidence of SSEH was 1.49% in posterior thoracic spinal surgeries. Large local kyphosis angle (> 8.77"), high occupying ratio of cross-sectional area (> 49.58%) and cerebrospinal fluid leakage were identified as risk factors for SSEH.
1138
P498: Comparison of anterior approach and posterior circumspinal decompression in the treatment of giant thoracic disc herniation
Lei Yuan 1 , Zhongqiang Chen 1 , Chuiguo Sun 1 , Weishi Li 1
1 Orthopedic Department, Peking UniversityThird Hospital, Beijing, China
Introduction: The treatment of giant thoracic disc herniation (gTDH)remains challenging for surgeons worldwide because of its large volume and calcified or ossified nature and the limitations of the prior small-sample-size, single-center studies reporting comparative effectiveness. We aim to compare the anterior decompression and spinal fusion (ASF) and posterior circumspinal decompression and spinal fusion (PCDF) for patients with myelopathy due to gTDH in the largest study to date by sample size. Material and Methods: Preoperative and postoperative functional status, surgical details, and complication rates were compared between the two groups. Results: A total of 186 patients were included: 63 (33.9%) ASF and 123 (66.1%) PCDF. The PCDF group had significantly shorter operation duration (163.06 ± 53.49 min vs. 180.78 ± 52.06 min, p = 0.032) and a significant decrease in intraoperative blood loss (716.83 mL vs. 947.94 mL, p = 0.045), and also a shorter hospital length of stay (LOS) and postoperative LOS (6 vs. 7, p = 0.011). The perioperative complication rate (13.8% vs. 28.6%, p = 0.015) and surgery-associated complication rate (13.0% vs. 27.0%, p = 0.018) were significantly higher in the ASF group. A higher rate of complete decompression was achieved in the PCDF group. There were no observed significant differences in changes in functional status between the two groups. Conclusion: PCDF for central or paracentral gTDHs is a highly effective and reliable technique. It can be performed safely with a low complication rate. If either procedure can adequately excise a central or paracentral gTDH, a PCDF approach may be a better option.
1195
P499: Antidepressant use does not impact intraoperative blood loss in lumbar fusion
Michael McCurdy 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Jeremy Heard 1 , Nicholas Pohl 1 , Omar Tarawneh 1 , Grace Bowen 1 , Yoni Dulitzki 1 , Abbey Glover 1 , Saurav Sumughan 1 , Emmanuel Dean 1 , Emma Boyajieff 1 , Alec Giakas 1 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Gregory Schroeder 1 , Christopher Kepler 1
1 Orthopaedic Spine Surgery, Rothman Orthopaedic Institute, Philadelphia, USA
Introduction: In recent years, mental health has increasingly been recognized as an influential determinant of patient outcomes after surgery across many specialties. Patients with back pain, a common manifestation of spine pathology, experience high concomitant rates of depression. The impact of antidepressants on surgical outcomes, particularly in relation to blood loss, is an important consideration in spine surgery. To our knowledge, no study has comprehensively examined the relationship between antidepressants and their effects on intraoperative blood loss in patients undergoing lumbar fusion. Therefore, this study aims to investigate the impact of antidepressants on intraoperative blood loss during lumbar fusion procedures. Material and Methods: After approval was obtained by the Institutional Review Board, patients undergoing primary 1-3 level lumbar fusion at a single, tertiary care institution from 2017-2021 were retrospectively identified. Patient characteristics, surgical details, and surgical outcomes were collected via chart review. Antidepressant use was collected based on current medication lists at the patient’s preoperative and first postoperative appointment. Patients were considered to be “taking antidepressants” only if antidepressants were listed as current medications at both appointments. To report blood loss, we calculated total blood loss (mL) rather than reporting estimated blood loss (EBL) to account for hidden blood loss that occurs in surgery. Total blood loss (mL) was calculated using the formula proposed by Gross et al. in order to account for hemodilution secondary to fluid resuscitation. Results: Of the 1,812 patients included in the study, 496 were taking antidepressants perioperatively. Female (64.7% vs. 45.5%, p = 0.001) patients were more likely to take antidepressants than their male counterparts. Patients in the antidepressant group were more likely to be discharged to an inpatient rehabilitation facility than patients without antidepressant use (11.3% vs. 7.14%, p = 0.029), but length of stay was not different between the two groups (3.70 vs. 3.74, p = 0.618). Surgical characteristics were not significantly different between the two groups. Posterolateral decompression and fusion (PLDF) (1,255 vs. 1,246, p = 0.730), transforaminal lumbar interbody fusion (TLIF) (1,252 vs. 1,292, p = 0.695), and anterior lumbar interbody fusion (ALIF) (1,237 vs. 1,210, p = 0.660) all showed similar intraoperative blood loss (mL) between the two groups. Selective serotonin reuptake inhibitor (SSRI) (1,255 vs. 1,266, p = 0.875), selective norepinephrine receptor inhibitor (SNRI) (1,255 vs. 1,254, p = 0.986), atypical (1,255 vs. 1,259, p = 0.893) and tricyclic antidepressant (TCA) (1,255 vs. 1,161, p = 0.306) sub-groups were all observed also to not have significantly different intraoperative blood loss compared to patients in the control group. Conclusion: Our study found that antidepressant use, specifically SSRIs, SNRIs, atypicals and TCAs, has no impact on intraoperative blood loss. We additionally observed no increase in transfusions among patients taking antidepressant medication when compared to those who were not. These findings suggest that antidepressants pose no increased risk of surgical blood loss in the context of primary lumbar fusion procedures. Therefore, caution should be taken when considering discontinuing antidepressants prior to surgery. Further research is necessary to elucidate the effect of serotonergic and non-serotonergic antidepressant medications on blood loss in other surgical procedures.
1197
P500: Effect of anterior cervical surgery on spinal cord tension in the treatment of cervical kyphosis
Huajiang Chen 1
1 Orthopedics, Shanghai Changzheng Hospital, Shanghai, China
Objective To propose a new indirect method of measuring spinal cord tension and to investigate changes in spinal cord tension after anterior cervical surgery for cervical kyphosis. Methods: A total of 53 patients with cervical kyphosis treated by anterior cervical surgery were retrospectively analysed, including 35 males and 18 females, aged 54.7 ± 19.1 years. There were 36 cases of degenerative cervical kyphosis, 6 cases of neurofibromatosis, 3 cases of adolescent idiopathic cervical kyphosis, 5 cases of cervical tuberculosis, and 3 cases of post-traumatic cervical kyphosis. JOA score and VAS score were obtained before and after surgery. Cervical sagittal balance parameters (cervical Cobb angle, c2-7 SVA, T1 slope) were measured. Changes in spinal cord tension were evaluated indirectly by measuring changes in spinal cord length and sagittal diameter before and after surgery. Results: At 2 months, 6 months and last follow-up, Cobb angle of kyphosis, SVA and ROM were significantly lower than those before surgery (p < 0.01); JOA score and VAS score were significantly improved after surgery (p < 0.01). Compared with preoperative values, there was no significant difference in C2-7 spinal cord length at 2-month, 6-month and final follow-up (p > 0.05). The sagittal diameter of the spinal cord was significantly larger than before surgery (p < 0.05). Patients were further divided into two groups according to the degree of cervical kyphosis: Group A (n = 32): the angle of cervical kyphosis was less than 30°; Group B (n = 21): the angle of cervical kyphosis was greater than 30°. In group A, there was no significant difference in C2-7 spinal cord length before and after surgery (p > 0.05), and there was a significant difference in sagittal spinal cord diameter before and after surgery (p < 0.05). There were significant differences in C2-7 spinal cord length (p < 0.01) and spinal cord sagittal diameter (p < 0.05) in group B before and after surgery. The change in spinal cord length was significantly correlated with Cobb angle correction (r = 0.753, p < 0.01). According to univariate linear regression analysis, the cut-off value of Cobb angle correction corresponding to a significant reduction in spinal cord length (at least 5 mm) was 26.8°. Conclusion: Anterior cervical surgery can be used to correct cervical kyphosis. The results of imaging measurements showed that spinal cord tension was significantly improved after surgery. Neurological function was also significantly improved after surgery.
Keywords: cervical vertebrae; kyphosis; surgical procedures, operative; spinal cord; treatment outcome
1206
P501: Pneumoencephalus after lumbar spine surgery: an uncommon but extremely serious complication
Paula Suárez 1 , Alicia Collado 1 , Tomasz Rumin 1 , María jose Villanueva 1
1 Orthopedics and Traumatolgy, Hospital Infanta Elena, Madrid, Spain
Introduction: Lumbar spine surgery is an increasingly common procedure today. Pneumocephalus and pneumorachis are rare complications after spinal surgery, but they are life-threatening for the patient. This event has been related to the rupture of the dura mater during surgery and usually presents itself with non-specific symptoms such as headache, vomiting or cognitive alterations, among others. Objective: To evaluate the diagnostic-therapeutic management of this complication by describing the case of a patient who underwent lumbar arthrodesis in our center. Materials and Methods: We present the case of a 54-year-old patient who underwent a circumferential arthrodesis of the L4-S1 levels is presented. No intraoperative complications were observed. 24 hours after surgery, the patient begins to experience a very intense frontal headache that does not respond to analgesia and involuntary spasmodic contractions. A craniocerebral CT scan was performed due to suspicion of a subarachnoid hemorrhage. Imaging revealed a pneumoencephalus in the frontal lobe. The study was completed with a CT scan of the lumbar spine where a linear image was observed anterior to the dural sac compatible with subdural/epidural emphysema. No collections were delimited and the screws were normally positioned. The case was discussed with Neurosurgery, who recommended an urgent transfer to the ICU. Result: Medical treatment was started in the ICU, which included bed rest, oxygen therapy, neurological monitoring, symptomatic measures, and antibiotic and antithrombotic prophylaxis. The patient evolved satisfactorily, and after adequate medical stabilization for 3 days in the ICU, he was discharged to the hospital ward. Seven days after surgery, he was discharged home and is currently asymptomatic from a neurological point of view and is progressing satisfactorily in the orthopedic level. Conclusions: Pneumocephalus is a very rare complication of spinal surgery but it can put the patient's life at risk. Its pathophysiology is little known; it seems to be related to cerebrospinal fluid leakage and the pressure difference between the intracranial and extracranial spaces. Even in the presence of severe symptomatic manifestations, conservative treatment is recommended initially.
1251
P502: The effect of the diffenence in C2-7 angle on the occurrence of dysphagia after cervical discectomy and fusion with the Zero-P Implant System
Chengyi Huang 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: We noticed that after the ACDF with Zero-P, the changes of lordosis in some patients are obvious, especially the C2-7 angle, and these could cause changes in the anatomical relationship between the cervical spine and the anterior esophagus, which may cause dysphagia. However, there have been few reports describing the effect of difference between postoperative and preoperative C2-7 angle (dC2-7A) on postoperative dysphagia after ACDF with Zero-P. Thus, the purpose of this retrospective study was to investigate the effect of the difference in C2-7 angle on dysphagia after anterior cervical discectomy and fusion (ACDF) with the Zero-P Implant System. Material and Methods: A retrospective analysis of 181 patients who underwent ACDF with the Zero-P Implant System and had at least one year of follow-up was performed from January 2011 to November 2018. All patients were divided into a non-dysphagia group and a dysphagia group to explore the effect of difference between postoperative and preoperative C2-7 angle (dC2-7A) on postoperative dysphagia. At the same time, other possible related factors including the difference between postoperative and preoperative O-C2 angle (dO-C2A), sex, age, body mass index (BMI), intraoperative time, estimated blood loss, diabetes mellitus, hypertension, smoking, alcohol consumption, prevertebral soft-tissue swelling (PSTS), the highest segment involved in the surgery and the levels of surgery segments were analyzed. Results: There were 139 patients in the non-dysphagia group and 42 patients in the dysphagia group. The single-factor analysis showed smoking, PSTS and dC2-7A was significantly different between two groups (p < 0.05). Spearman’s correlation coefficient showed no significant correlation between degree of dysphagia and dC2-7A (p > 0.05). The results of multiple-factor analysis with an ordinal logistic regression model showed that smoking, PSTS and dC2-7A were significantly associated with the incidence of dysphagia (p < 0.05). Conclusion: The postoperative C2-7 angle has an important effect on the occurrence of dysphagia in patients undergoing Zero-P implant system interbody fusion surgery.
Keywords: dysphagia; Zero-P; cervical vertebrae; related factors
1342
P503: Abdominal aortic calcification is an independent predictor of perioperative blood loss in posterior spinal fusion surgery
Ali Guven 1 , Lukas Schönnagel 1,2 , Krizia Amoroso 1 , Erika Chiapparelli 1 , Gaston Camino-Willhuber 1 , Jiaqi Zhu 3 , Soji Tani 1,4 , Thomas Caffard 1 , Artine Arzani 1 , Jennifer Shue 1 , Andrew Sama 1 , Frank Cammisa 1 , Federico Girardi 1 , Ellen Soffin 5 , Alexander Hughes 1
1 Department of Orthopaedic Surgery
3 Biostatistics Core, Hospital for Special Surgery, New York, USA
2 Center for Musculoskeletal Surgery, Charité- Universitätsmedizin Berlin, Berlin, Germany
4 Department of Orthopaedic Surgery, Showa University Hospital, Japan
5 Department of Anesthesiology, Critical Care and Pain Management
Introduction: Posterior spinal fusion (PSF) is associated with substantial blood loss, which can complicate the perioperative course, necessitate blood transfusion and worsen postoperative outcome. Determining risk factors for blood loss can help to optimize perioperative patient blood management. Abdominal aortic calcification (AAC) is regarded as a marker of advanced atherosclerotic vascular disease and has gained attention in spinal surgery due to its association with degenerative disc disease, decreased vertebral bone mineral density and sarcopenia. Although AAC has been shown to correlate with postoperative morbidity while also altering cardiovascular hemodynamics, its effect on blood loss remains unexplored. Therefore, this study aimed to analyze the impact of AAC on perioperative blood loss in PSF surgery. Material and Methods: Patients with degenerative lumbar spinal conditions who underwent single or multilevel PSF between March 2016 and July 2023 were retrospectively analyzed. Total blood volume (TBV) and estimated blood loss (EBL) were calculated via established formulae. AAC was assessed on lateral lumbar radiographs according to the Kauppila classification by measuring the calcification of the anterior and posterior aortic wall at the L1 to L4 vertebral levels. Patients were categorized into the no AAC (AAC = 0) and AAC groups (AAC ≥ 1). Predictors of the EBL to TBV ratio were examined via univariate and multivariable regression analyses, controlling for age, sex, body mass index, multilevel fusion, surgery duration, tranexamic acid (TXA), osteopenia/osteoporosis, hypertension, diabetes, smoking history, preoperative daily aspirin intake, and AAC. The statistical significance level was set as p < 0.05. Results: A total of 199 patients (47.2% female) with a median age of 65 years (IQR 57 - 72) and a median BMI of 29.4 kg/m2 (IQR 26.4 - 32.7) met inclusion criteria and were analyzed. AAC was present in 106 patients (53.3%). The AAC group consisted of an older cohort (p < 0.001), with a higher rate of hypertension (p < 0.001), diabetes (p = 0.005), positive smoking history (p < 0.001), osteopenia or osteoporosis (p < 0.001), and daily aspirin use (p = 0.004). Also, more patients in the AAC group received intravenous TXA intraoperatively compared to the No AAC group (p < 0.001). The groups did not differ in surgical parameters such as multilevel fusion and surgery duration. After adjustment for all confounders, AAC was independently associated with the EBL to TBV ratio, accounting for an increase in blood loss of 4.65% of TBV (95% CI: 1.29 - 8.00, p = 0.007). Furthermore, female sex (p < 0.001), multilevel fusion (p < 0.001), and surgery duration (p < 0.001) were identified as additional independent positive predictors for the EBL to TBV ratio. Only TXA administration negatively predicted the EBL to TBV ratio (p < 0.001). Conclusion: This is the first study to identify AAC as an independent risk factor of perioperative blood loss in PSF surgery. In addition to its link to degenerative spinal conditions and adverse postoperative outcomes, the relationship between AAC and increased blood loss warrants attention in adults undergoing PSF.
1366
P504: A systematic review of mortality rates and life expectancy after adult spinal deformity surgery
Kari Odland 1 , Paul Soriano 1 , Jason Haselhuhn 1 , Breanne Richins 2 , David Polly 1,3
1 Department of Orthopedic Surgery
2 Center for Financial and Actuarial Mathematics
3 Department of Neurosurgery, University of Minnesota, Minneapolis, USA
Introduction: Adult spinal deformity (ASD) encompasses a wide range of conditions that result in abnormal sagittal coronal spinal alignment. ASD surgery offers significant reduction in pain and improved quality of life however, surgical mortality has been shown to be higher in the ASD population. There are a number of studies that report on the risks associated with complications in this population. Among the largest to date, are the retrospective studies from the Scoliosis Research Society (SRS) register of Morbidity and Mortality of adult scoliosis surgery published in 2011, 2016 and 2022 respectively. Reported overall mortality rates range from 0.3% between 2004 and 2007, 0.07% to 0.12%. between 2009 and 2012, and from 0.14% to 0.09% between 2015 and 2018. Therefore, the aim of this systematic review is two-fold: 1) to analyze mortality rates within 90 days of surgery reported in the literature to provide a standardized reference for determining risk of surgical intervention in the ASD population, and 2) determine survival rates between individuals undergoing ASD surgery versus the general population. Material and Methods: A systematic review of retrospective studies was performed by searching PubMed to identify studies that analyzed mortality rates in the adult spinal deformity population between 1995-2020. The following search phrases were used: (mortality, adult spinal deformity, adult spinal deformity surgery, post-operative, morbidity, scoliosis, spondylolisthesis, kyphosis) using Boolean operators AND, OR and NOT. Surgeries performed for infection, trauma, fractures, or tumors, and patients’ ≤ 18 years of age were not included. Mortality rates were analyzed. Results: A total of 20 studies met inclusion criteria, including 142,231 ASD patients who underwent ASD surgery (mean age, 58.7 years; range, 42-74 years) for the purposes of analyzing mortality rates. Overall, the mean log proportional mortality rate was 0.53% (CI 95% 5.62 - 4.79) which is consistent with reported rates in the literature. Conclusion: Adult spinal deformity surgery remains challenging and is associated with variable mortality rates. This systematic review has presented a normative range for expected mortality rates in a large sample of adult spinal deformity patients which can serve as means for preoperative risk stratification and post-operative outcomes for spine surgeons when considering ASD surgery in at-risk populations.
1372
P505: Spinal cord reperfusion injury in posterior cervical surgery
Satpal Charl 1 , Syarul Arwiz Sahruzaman 1 , Asrul Syamin Hisyam Yong 1 , Amir Zakaria 2
1 Orthopaedic Department, Hospital Sultan Idris Shah, Selangor, Malaysia
2 Orthopaedic, Hospital Sungai Buloh, Selangor, Malaysia
Introduction: Reperfusion injury of spinal cord is rare but potentially severe complication that could arise following cervical spine decompressive surgery. The reperfusion injury is described as when a chronically compressed canal is released, immediate blood flow return triggers a chemical cascade of damaging effect. The restoration of blood flow to chronic ischaemic spinal cord, known as reperfusion injury or “White Cord Syndrome” can lead to temporary or permanent paralysis. Material and Methods: A 48-year-old Malay gentleman diagnosed with cervical spondylomyelopathy with ossification posterior longitudinal ligament (OPLL) involving C2-C6 region. The patient had weakness in both upper and lower limb and right sided worse with best of 4 out of 5. Sensation had been reduced in all limbs and right sided thoracic region. Calculated Japanese Orthopaedic Association (JOA) score was 11 preoperatively. Patient had undergone posterior cervical spinal instrumentation and fusion (PSIF) over C3-C5 with decompressive laminectomy C3-C5 and dome decompression over C2. Lateral mass screws were inserted over C3, C4 and C5 first followed by decompressive laminectomy. Spinal cord monitoring, somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP) was performed continuously. During decompressive laminectomy, MAP was maintained to above 85 mmHg. The decompression was done in a step wise fashion from C5 to C4 then C3. MEP was checked after each level of decompression and showed return to baseline for C4& C5. However, immediately after laminectomy of C3 was performed, MEP had reduced by more than 50% from baseline at level C3 to S1 whereas SSEP remain intact throughout surgery and remained the same thereafter. The surgery continued with placement of rods and closing of operative site. No perceivable injury had occurred during screw insertion and decompression. Results: Two hours postoperative, neurological assessment revealed acute quadriplegia from the level C4. Intravenous Dexamethasone 8mg 3 times per day was started immediately. At 6 hours post laminectomy neurological assessment shows improvement to Frankel C. Serial neurological assessment on post-operative day 3 showed return of power to preoperative state with improvement in sensation compared to pre-operative assessment. Patient was subjected to rigorous rehabilitation and physiotherapy care. Two weeks post operatively, calculated JOA score 13. No MRI was repeated postoperatively as suspicion of mal-placed hardware or dura injury was not evident during surgery and MEP had dropped after decompression. This patient was treated as reperfusion surgery as clinical events and outcomes matched the literature description of reperfusion surgery. Conclusion: Cervical spinal cord reperfusion surgery is a rare but devastating complication which can occur despite meticulous monitoring and intra-operative measures. Reperfusion injury being unpredictable but foreseeable and can manifest in varying presentations from incomplete to complete paralysis and recovery as seen in this case can return as soon as 6 hours postoperatively.
1405
P506: Venous thromboembolism and mortality rates have not improved in cervical spine surgery from 2012-2021
Bongseok Jung 1 , Alex Ngan 1 , Junho Song 1 , Austen Katz 1 , Sohrab Virk 1 , David Essig 1
1 Department of Orthopaedic Surgery, Northwell Health, Manhasset, USA
Introduction: Venous thromboembolism (VTEs), deep vein thrombosis (DVTs), and pulmonary embolism (PEs) are among the most catastrophic yet preventable post-operative complications following orthopedic surgery. However, current literature regarding the temporal trends and predictors of VTE following cervical spine surgery is limited. This study aimed to identify within the past decade 2012-2021 1) the temporal trends in the rates of VTE, DVTs, PEs, and mortality and 2) identify independent predictors of VTE following cervical spine surgery. Material and Methods: The ACS-NSQIP database was queried to determine annual incidences of VTEs, DVTs, PEs, and mortality following cervical spine surgery in each operation years between 2012-2021. Differences in baseline characteristics were quantified using Chi-Squared test and ANOVA. Variables that were analyzed included demographic variables: age, sex, race, Hispanic ethnicity BMI, operation time, outpatient surgery, length of stay, non-home discharge, posterior fusion, comorbidities: current smoker, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), dialysis, bleeding disorder, functional dependence, chronic steroid use, and preoperative lab values: blood urea nitrogen (BUN), creatinine, albumin, total bilirubin, platelet count, partial thromboplastin time (PTT), and international normalized ratio (INR). Incidences of VTEs, DVTs, PEs, and mortality were first stratified by operation year and differences quantified using the Chi-Squared test. A binary multivariate logistic regression model was constructed to compare the primary outcomes with operation years while accounting for significant baseline characteristics. Another multivariate regression analysis was then performed to identify significant independent and protective predictors of VTEs following cervical spine surgery. Finally, results were reported as odds ratios (OR) with 95% confidence intervals (CI), with p<0.05 defined as significant. Results: A total of 91,025 patients were included in our study. For the entire cohort, the average age was 56.2 years, 49.4% female sex, 11.8% black race, 4.4% Hispanic ethnicity, with a BMI of 30.6 kg/m2. Annual rates of VTEs, DVTs, PEs, and mortality did not change (p > 0.10) across any of the operation years between 2012-2021. When accounting for significant baseline characteristics, multivariate regression analysis further demonstrated no significant difference of VTEs, DVTs, PEs, and mortality across operation years (p > 0.10). Significant independent predictors of VTEs included older age, black race, high BMI, longer operation time, length of hospital stay, non-home discharge, history of COPD, functional health, and high INR, while protective factors for VTE included female sex, outpatient surgery, and smoking status in this cohort. Conclusion: Despite many advances in surgical techniques and training, rates of thromboembolic complications following cervical spine surgery have not improved over the last decade (2012-2021). Factors such as older age, black race, high BMI, longer operation time, length of hospital stay, non-home discharge, history of COPD, functional dependence, and high preoperative INR values were independent predictors of VTEs while female sex, outpatient surgery, and smoking status were the protective factors.
1416
P507: Iatrogenic hemodilution and blood transfusion in adult spine deformity surgery
Marcus Mazur 1
1 Neurosurgery, University of Utah, Salt Lake City, USA
Introduction: Perioperative transfusion for patients undergoing long-segment thoracolumbar fusion surgery is common. To date no work has been done to standardize intra- and perioperative management of transfusion administration. We sought to identify risk factors for transfusion, and further the analysis by identifying benchmark cutoffs that could be utilized by the operative team to guide transfusion. This data will be used to create perioperative protocols with the goal of decreasing transfusion rates when not indicated, and earlier administration when indicated. Material and Methods: A single-center retrospective cohort study of thoracolumbar fusion surgeries of 8 or more levels at our institution between 2015 and 2020 was conducted. Patient demographics, surgical details, anesthesia and critical care records, and laboratory data were compared between patients who received intraoperative and postoperative blood transfusions and those who did not. Univariate and multivariate propensity-matched analyses were performed to identify independent predictors for blood transfusion, and ordinal analysis was performed to identify possible benchmark cutoffs. Results: We identified 233 patients undergoing long-segment fusions, of whom 133 (57.1%) received a blood transfusion. Multivariate propensity-matched logistic regression showed that IVF volume was an independent predictor for transfusion (total IVFs (8051 mL transfusion vs 5070 non-transfused, p < 0.01). Patients who received ≥ 4L total IV fluids were more likely to undergo transfusion compared to those who received < 4L (93.2% vs. 50.7%, p < 0.01). Using cutoffs of > 60 mL/kg and > 9/mL/kg/hr, patients receiving high volume of IVF had an increased risk of blood transfusion (OR = 10.45, 95% CI [2.62, 41.72], p < 0.01) and (4.46, [1.39, 14.32], p < 0.01), respectively. Conclusion: IVF administration is an independent predictor for blood transfusion after long-segment fusion surgery. Limiting IVF administration may prevent iatrogenic hemodilution and decrease transfusion rates.
1455
P508: Risk factors for 30-day morbidity and mortality after spinal trauma
Rishi Kanna 1 , Ajoy P Shetty 1 , Shanmuganathan Rajasekaran 1
1 Spine Surgery, Ganga Hospital, Coimbatore, India
Background: Traumatic Spinal Injuries (TSI) often follows high velocity injuries and frequently accompanied by polytrauma. While most studies have focussed on outcomes of spinal cord injuries, the incidence and risk factors that predict morbidity and mortality after TSI has not been well-defined. Methods: Data of consecutive patients of TSI (n = 2065) treated over a 5-year-period were evaluated for demographics, injury mechanisms, neurological status, associated injuries, timing of surgery and co-morbidities. The thirty-day incidence and risk factors for complications, length of stay and mortality were analysed. Results: The incidence of spinal trauma was 6.2%. Associated injuries were seen in 49.7% (n = 1028), and 33.5% (n = 692) patients had comorbidities. The 30-day mortality was 0.73% (n = 15). Associated chest injuries (p = 0.0001), cervical spine injury (p = 0.0001), ASIA-A neurology (p < 0.01) and ankylosing spondylitis (p = 0.01) correlated with higher mortality. Peri-operative morbidity was noted in 571 patients (27.7%) and were significantly associated with age > 60 (p = 0.043), ASIA-A neurology (p < 0.05), chest injuries (p = 0.042), cervical and thoracic spine injury (p < 0.0001). The mean length of stay in hospital was 8.87 days. Cervical spine injury (p < 0.0001), delay in surgery > 48 hours (p = 0.011), Diabetes mellitus (p = 0.01), Ankylosing spondylitis (p = 0.009), associated injuries of chest, head, pelvis and face (p < 0.05) were independent risk factors for longer hospital stay. Conclusion: Key predictors of mortality after spinal trauma were cervical spine injury, complete neurological deficit, chest injuries and ankylosing spondylitis, while additionally higher age and thoracic injuries contributed to higher morbidity and prolonged hospitalisation. Notably multi-level injuries, higher age, co-morbidities and timing of surgery did not influence the mortality.
1485
P509: Post operative bilateral chylothorax after posterior correction of scoliosis
Jack Van Loo 1 , Nitin Adsul 1 , Peter Loughenbury 1 , Nigel Gummerson 1 , Mantaran Bakshi 1
1 Spinal Surgery, Leeds General Infirmary, Leeds, United Kingdom
Introduction: Chylothorax is an extremely rare complication of spinal surgery with only 15 previously reported cases and only 5 when a posterior approach has been utilised, this paper presents a further case of chylothorax following the posterior spinal fusion of the T4-L4 vertebra for correction of scoliosis in a 16-year-old female patient. After the procedure the patient developed respiratory distress due to bilateral pleural effusions confirmed by gross and laboratory analysis to be the result of an accumulation of chyle. Material and Methods: The patient underwent a T4-L4 posterior instrumented spinal fusion and correction of scoliosis with motor and sensory evoked potential spinal cord monitoring and autologous cell salvage. During the procedure there was no injury to the thoracic duct or any branches of the lymphatic system.3 days after the procedure the patient developed respiratory distress, desaturating to 77% on room air and requiring a venturi device with an Fi02 of 45% to maintain safe levels of oxygenation prompting a chest x-ray and CTPA to be done. The CTPA demonstrated a large left pleural effusion and moderate right pleural effusion with associated basal atelectasis/consolidation bilaterally. The chest drain produced of milky white fluid which was confirmed to be chylothorax following further analysis of the fluid. The patient was commenced on a low long chain triglyceride regimen under the supervision of specialist dietetics staff. The patient made a good recovery under these conservative measures and the chest drain was removed after X days and the patient was discharged X days after the procedure. Results: Chylothorax is a rare cause of pleural effusion accounting for between 2-3% of all fluid collections surrounding the lungs [9], most cases are unilateral and recent studies show an increasing number of cases of chylothorax result from trauma rather than the previously held belief that the majority of chylothoraxes were secondary to malignancy [10]. Approximately half of all chylothoraxes are traumatic with the leading causes being vertebral fractures, penetrating trauma, sudden spinal hyperextension and, closed trauma causing an increase in thoracic pressure leading to damage of the thoracic duct. Iatrogenic causes as seen in this case also fall under traumatic aetiologies and include incidents occurring during surgical approach most commonly in the thoracic cavity but also in the abdominal cavity, additionally iatrogenic injury is seen during procedures such as the placement of central catheters [10]. Whilst accounting for around 50% of cases of chylothorax the incidence of iatrogenic damage to the thoracic duct is low occurring in less than 1% of spinal procedures, however its diagnosis and management is often complex [11]. Conclusion: Whilst extremely rare chylothorax is a possible complication in spinal surgery and should be considered amongst the range of differentials in the postoperative dyspnoeic patient. Failure to recognise chylothorax early and manage it appropriately can result in a sequalae of pathology that can lead to significant morbidity and mortality.
1567
P510: The impact of prevertebral soft tissue swelling on the severity of post-operative dysphagia in patients undergoing anterior cervical discectomy and fusion
Rudy Zambrano 1 , Gregory Bibbs 1 , Michael Gerling 1,2 , Zorica Buser 1,2
1 Geling Institute, New York, USA
2 Orthopedic Surgery, NYU Grossman School of Medicine, New York, USA
Introduction: Recent studies have demonstrated that patients who develop dysphagia after Anterior Cervical Discectomy and Fusion (ACDF) show significant alteration in swallowing biomechanics, which include increased aspiration, thickening of the pharyngeal wall, poorer pharyngeal constriction and peristalsis. Furthermore, the number of surgical levels and location might play a role. The aim of the current study was to assess an association between soft tissue swelling and dysphagia and to determine the most common levels associated with dysphagia after ACDF. Material and Methods: Patients who underwent ACDF between June 2019 and June 2022. Patients diagnosed with postoperative dysphagia were included in the study and followed up to 12-months. Patients with past medical history or other causes of dysphagia were excluded. A control group was matched based on the surgery, operated levels, gender, and age. Demographic information, comorbidities, treatment, smoking status, and revision surgeries were included. Measurements of prevertebral soft tissue were performed using pre op and post op neutral radiographs. The prevertebral soft tissue was measured from anterior vertebral body to tracheal silhouette. Dysphagia treatment and duration of the symptoms were also documented. All statistical analyses will be conducted using Stata/IC Version 17.0 including direct comparison and multivariate regression. Results: A total of 536 ACDF surgeries were performed from June 2019 to June 2022. During this period 25 patients were diagnosed with dysphagia (4.7%). Among the patients with dysphagia 18 were male and 7 were female; age average was 54.8 ± 12.7. Nine surgeries (36%) were single level, 14 (56%) were two-level and 2 (8%) were three-levels ACDF. 73% of patients with postoperative dysphagia developed an increase of > 25% of prevertebral soft tissue swelling compared to preoperative radiographs. Among those patients the increase in tissue swelling of 25-70% was seen in three patients,75%-100% in five and > 100% in seven patients. In the control group most patients had < 25% of soft tissue swelling. C3-4, C4-5 were the most common levels associated with dysphagia and tissue swelling. The average time for recovery was 8.3 ± 5.9 months. Conclusion: The current study found a large number of patients who had substantial (> 25%) swelling in prevertebral tissue related to significant dysphagia. The most affected levels were C3-5. Post-operative dysphagia has been a reported complication after ACDF, however the association with soft tissue swelling has not been fully investigated yet. The current study suggests that severe soft tissue swelling plays an important role in the onset of dysphagia and certain surgical levels might be at a higher risk.
1685
P511: The impact of timing of inpatient physical therapy on venous thromboembolic events after elective spine fusion surgery
Olivia Opara 1 , Rajkishen Narayanan 1 , Yunsoo Lee 1 , Jeremy Heard 1 , Tariq Issa 1 , Alexa Tomlak 1 , Michael Carter 1 , Eric DiDomenico 2 , Daniel Kwak 2 , Jose Canseco 1 , Alan Hilibrand 1 , Alex Vaccaro 1 , Chris Kepler 1 , Gregory Schroeder 1
1 Rothman Orthopaedic Insitute, Philadelphia, USA
2 Thomas Jefferson University, Philadelphia, USA
Introduction: Venous Thromboembolism (VTE) is the third leading cause of death in the world. While surgical procedures have been associated with an increased risk of VTE, recent studies have suggested that early ambulation can be an effective form of VTE prevention. Physical therapy is one of the most common postoperative care measures after spinal fusion surgery; however, the impact of timing of initial physical therapy after surgery on VTE outcomes is not well described in the literature. We seek to investigate if the time to physical therapy has an effect on the rate of postoperative VTE events in patients undergoing spine fusion surgery. Material and Methods: After approval from our Institutional Review Board, we retrospectively identified patients over 18 years of age who underwent cervical, thoracic, and spinal fusion surgery at a tertiary urban medical center from 2017-2021. Electronic medical records were reviewed for physical therapy variables such as Activity Measure of Post-Acute Care Basic Mobility (AM-PAC Basic Mobility), gait trial distance achieved (distance walked in feet), and time to physical therapy. Time to physical therapy was defined as surgery end time to time of the first inpatient physical therapy session. Patients who had surgery for trauma, infection, or malignancy were excluded. Continuous variables were assessed using either an independent t-test or Mann -Whitney U test for parametric and nonparametric data. Logistics regression was performed to assess predictors of postoperative VTE events. Statistical analysis used R studio version 4.02 (Boston, Massachusetts, USA). A P value. Results: Of the 2130 patients identified, 32 had a VTE event and 2098 did not. Patient's age, past medical history of lower extremity VTE, and pulmonary embolism were significantly associated with future VTE events (p = 0.029, 0.049, 0.001), respectively. Additionally, operative duration (303 vs. 241 minutes, p = 0.039) and length of stay (4.75 vs. 3.60 days, p = 0.001) were significantly longer in patients with VTE events. Time to initiating physical therapy (< 6, 6-24, or > 24 hrs) was not significantly associated with VTE rate (p = 0.179). The AM-PAC Basic Mobility Score (15.7 vs. 17.2, p = 0.107) and total gait trial distance (48.4 vs. 69.9 feet, p = 0.055) were also not associated with VTE frequency. Stepwise logistic regression showed that operative duration time and past medical history of lower extremity VTE were independent predictors of VTE (Odds ratio 1.003, CI: 1.0001 - 1.01, p = 0.032) and (Odds ratio: 3.51, 95% CI: 1.15 - 8.87, p = 0.014), respectively. Conclusion: Our study found that the time that physical therapy or mobilization protocols are initiated after elective spine fusion surgery does not affect rates of postoperative VTE significantly. Additionally, the extent of patient mobilization and activity during PT sessions did not predict VTE likelihood. While physical therapy is encouraged, other preventive measures such as medications, mechanical compression, and close patient monitoring should be continued. Therefore, we encourage continuous interdisciplinary communication between members of the postoperative care team to implement timely clinical actions.
2002
P512: Minimizing post-operative opioid use in common spine surgeries: a non-inferiority quality improvement study
Arianna Dalamaggas 1 , Catherine Olinger 1 , Alex Coffman 1 , Natalie Glass 1 , Lee Kral 2
1 Department of Orthopaedics and Rehabilitation
2 Department of Anesthesia, University of Iowa Hospitals and Clinics, Iowa City, USA
Introduction: The goal of this study is to minimize opioid-related adverse effects in post-operative patients by establishing a quantity and duration of opioid analgesia following surgical intervention. The opioid epidemic continues necessitating thoughtful prescribing patterns following posterior thoracolumbar spinal fusions (PSF) and anterior cervical discectomies and fusions (ACDF). This study will also survey patients’ handling of excess pills and include options for safe disposal. Material and Methods: This is a prospective quality improvement study with inclusion of patients >18 years of age, who underwent primary PSF divided into >3 levels or ≤ 3 levels, as well as ACDF of any number of levels. Patients with a pre-operative diagnosis of infection, malignancy, trauma, or those undergoing any additional surgery in a 6-month pre- and post-operative period were excluded. Those with primary diagnoses of cervical or thoracolumbar spinal stenosis, myelopathy, radiculopathy, or degenerative spondylolisthesis were included. Patients will be surveyed for their quantity and duration of opioid pills consumed, adverse opioid-related side effects, and method of pill disposal. Patient-reported outcomes including mJOA, ODI, and PROMIS Global General Health are also utilized pre- and post-operatively, as well as pre- and post-intervention to assess clinical function. Results: In preliminary, pre-intervention review of data, 377 patients met inclusion, 158 were excluded for incomplete data. The remaining 219 patients (89 ACDF, 130 PSF) shared common diagnoses of cervical myelopathy (n = 47), cervical radiculopathy (n = 17), low back pain (n = 49), and lumbar spinal stenosis (n = 21). Of the prescriptions provided, the average quantity was 44 pills; 23% (50/219) were prescribed pre-operatively. The average mJOA score was 13.38 (12.96 pre-op, 13.73 post-op), representing moderate myelopathy. The average ODI score was 31.3 (31.6 pre-op, 31.0 post-op) representing moderate disability. The average PROMIS general health value was 3 (1-5). Conclusion: Limiting opioid utilization in the pre- and post-operative periods is of great value to reduce adverse medication effects. With the preliminary data collected, we will begin our intervention by decreasing the total prescription quantity. We do acknowledge patients may benefit from additional opioid analgesia greater than the initial prescription may allow for, but we believe less over time will lead to unchanged patient-reported outcomes and will result in similar scores for MJOA, ODI, and PROMIS data, with fewer adverse medication effects. Ultimately, we aim to provide guidance to the field on opioid pill quantity and duration that results in satisfactory outcomes with no difference in PROs, function, or overall outcome while minimizing adverse medication effects from prolonged use.
2157
P513: Routine opioid prescription is not necessary following one-level lumbar surgery with single epidural analgesia: The EPIPCA trial
Kwang-Sup Song 1 , Dae-Woong Ham 1 , Hyun Kang 1 , Youngbae B Kim 2 , Sang-Min Park 3 , Dong-Gune Chang 4
1 Orthopaedic Surgery, Chung-Ang University Hospital, Seoul, South Korea
2 Orthopaedic Surgery, VHS Medical Center, Seoul, South Korea
3 Orthopaedic Surgery, Spine Center, Seoul National University Bundang Hospital, Seoul, South Korea
4 Orthopaedic Surgery, Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, South Korea
Introduction: Despite an increased focus on opioid over-prescription, it is still inconclusive that routine opioid use is necessary for postoperative analgesia in one-level lumbar surgery. The study aimed to investigate the analgesic and opioid-sparing effects of a single epidural injection and to explore the necessity of routine opioid prescription in one-level lumbar surgery. Material and Methods: A Randomized trial was conducted at four hospitals with the patients who underwent one-level lumbar decompression or fusion surgery, each surgery subject was divided into the EPI group (0.2%, 10 ml, ropivacaine epidural injection before wound closure with opioid-free patient-controlled analgesia (PCA)) and PCA group (routine opioid use in PCA) and other analgesic protocol was the same. The primary outcomes were assessed by a self-reported numeric rating scale (NRS) for postoperative 48h. Secondary outcomes included frequency of pushing the button (FPB), 48h-use of ketorolac and rescue fentanyl, Likert satisfaction scores at discharge, opioid-related adverse events (postoperative nausea and vomiting, urinary retention (POUR), and constipation), and Oswestry Disability Index (ODI) for postoperative 12 months. Results: Ninety-eight patients (decompression: 50, fusion: 48 subjects) were randomized. The EPI group demonstrated a lower 48-h NRS in both subjects, especially a statistical significance in fusion subjects. Satisfaction for analgesia in fusion subjects was significantly higher and opioid-related adverse events were less in the EPI groups, with notable significance for POUR. Total fentanyl 48-h use in the PCA group was about 12 and 20 times greater in fusion and decompression subjects respectively. Conclusion: Our study has shown that the postoperative analgesic effect of single ropivacaine epidural injection (0.2%, 10 ml) with opioid-free PCA versus the routine use of opioids in PCA was significantly effective and satisfactory, particularly in fusion subject. Compared to the routine use of opioids in PCA, this approach offers benefits by reducing opioid consumption and related adverse events. Therefore, a single ropivacaine epidural injection administered prior to wound closure is an effective and recommended opioid-sparing analgesic technique, capable of preventing unnecessary routine opioid use in one-level lumbar surgery.
2173
P514: A pig model of symptomatic spinal epidural hematoma
Zihe Li 1 , Jiasheng Chen 1 , Shengxin Zeng 1 , Haozheng Li 1 , Hua Zhou 1 , Xiao Liu 1 , Pan-pan HU 1 , Xiaoguang Liu 1 , Zhongjun Liu 1 , Feng Wei 1
1 Department of Orthopaedics, Peking University Third Hospital, Beijing, China
Purpose: The purpose of this study was to establish an animal model capable of simulating the development and decompression process of symptomatic spinal epidural hematoma (SSEH). Methods: A total of 16 male Bama miniature pigs were included in this study and were randomly assigned to four groups: Group A (4-hour 20 mmHg hematoma compression), Group B (4-hour 24 mmHg hematoma compression), Group C (4-hour 28 mmHg hematoma compression), and Group Sham (control). Real-time intra-wound hematoma compression values were obtained using the principle of communicating vessels. Electrophysiological analysis, including the latency and amplitude of somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP), as well as behavioral observation (Tarlov score), were performed to assess this model. Results: ANOVA tests demonstrated significant differences in the latency and relative amplitude of SSEP and MEP between group C and Sham after 4 hours of hematoma compression and 1 month after surgery (p < 0.01). The behavioral assessment 8 hours after surgery indicated that the animals subjected to 28 mmHg hematoma compression suffered the most severe spinal cord injury and Pearson correlation coefficient test suggested that epidural pressure was negatively correlated with the Tarlov score (r = -0.700, p < 0.001). With the progression of compression and the increase of epidural pressure, the latency of SEP and MEP gradually prolonged, while the relative amplitude gradually decreased. Conclusions: When the epidural pressure reaches approximately 24mmHg, the spinal cord function occurs progressive dysfunction. Monitoring epidural pressure would be an effective way to identify the occurrence of postoperative spinal epidural hematoma.
2197
P515: Operating room size is associated with postoperative wound infection and reoperation following elective spinal surgery
Jessica Ryvlin 1 , Kurt Widmaier 1 , Isabella Pecorari 1 , Mousa Hamad 1 , Anne Schlumprecht 1 , Rose Fluss 1 , Rafael De la Garza Ramos 1 , Saikiran Murthy 1 , Reza Yassari 1 , Yaroslav Gelfand 1
1 Montefiore Medical Center/Albert Einstein College of Medicine, New York, USA
Study Design: Single institution retrospective cohort. Objective: To determine if operating room size is associated with postoperative surgical site infection (SSI) and unplanned reoperation in patients undergoing spinal surgery. Summary of Background Data: Patients undergoing spinal surgery are at significant risk of perioperative complications. Many risk factors have been identified to increase rates of SSI and reoperation, but the impact of operating room size has not yet been established. Methods: A total of 681 patients who underwent elective spinal surgery between 2021 and 2022 underwent chart review. Our primary outcomes were any new SSI within 30 days postoperatively and any unplanned spinal reoperation within 30 days. Operating room floor areas were obtained, where a large room was defined as > 550 ft2 and a small room was defined as < 550 ft2. Univariate and multivariate logistic regression was used to determine odds ratios (OR) with 95% confidence intervals (CI). Results: All surgeries occurred in one of six operating rooms, where 49% of patients (33/681) had surgery in a large room. The overall SSI incidence was 6% (43/681), of which 28% (12/43) occurred in a large room. After controlling for ASA class, diabetes, and surgical approach, large operating rooms were associated with decreased odds of postoperative SSI (OR 0.46; 95% CI 0.22-0.96; p = 0.039). The overall reoperation rate was 7% (50/681), of which 32% (16/50) had index surgery in a large room. After controlling for ASA class, revision, and approach, large operating rooms were associated with decreased odds of reoperation (OR 0.46; 95% CI 0.22-0.93; p = 0.032). Conclusions: Operating room size > 550 ft2 was found to be associated with decreased postoperative SSI and reoperations in patients undergoing elective spine surgery. Although further validation of these results is needed, the operating room environment may represent a modifiable risk factor for future quality improvement.
2268
P516: Overload vertebra body: a unique radiographic phenomenon following multilevel anterior cervical discectomy and fusion
Shihao Chen 1
1 Sichuan University, West China Hospital, Chengdu, China
Introduction: Because previous studies have not focused on postoperative cervical collapse, the purpose of the present study was to introduce the overload vertebra body (OVB) phenomenon following multilevel anterior cervical discectomy and fusion (ACDF) as well as to investigate its effects on clinical and radiographic outcomes. Methods: We conducted a retrospective study involving patients with three-level cervical degenerative disc disease (CDDD) who underwent ACDF at our institution between March 2015 and June 2021. A total of 32 patients were included in the analysis, including 64 OVB and 64 non-OVB. The evaluated vertebral parameters included the vertebral cross-sectional area (CSA), wedge angle (WA), vertebral height (anterior [AH] and posterior [PH]) and anterior-posterior vertebral diameter (upper [UD] and lower [LD]). Results: A total of 32 patients in both groups were demographically matched for comparison. The CSA and WA were significantly lower in the OVB group than in the non-OVB group at 3, 6, and 12 months after surgery as well as at the final follow-up (p < 0.01). The AH of the OVB group was significantly lower at 3, 6, and 12 months after surgery as well as at the final follow-up compared to 1 week after surgery (p < 0.01). According to the vertebral height loss at the final follow-up, 39 cases (60.9%) had < 1/5 height loss, 20 cases (31.3%) had 1/5-1/3 height loss, and 5 cases (7.8%) had a height loss > 1/3. In addition, there were 13 cases (20.3%) with grade 1, 13 cases (20.3%) with grade 2, 31 cases (48.4%) with grade 3, and 7 cases (10.9%) with grade 4 V-deformity at the final follow-up. Conclusions: OVB, a new phenomenon following multilevel ACDF, is defined as the cervical vertebra located in the middle of the surgical segments in multilevel anterior cervical spine surgery. Statistical analysis of vertebral parameters, including CSA, WA, AH, PH, UD, and LD, showed that OVB occurs mainly at the anterior edge of the vertebra and that its largest radiographic manifestation is the loss of height at the anterior edge of the vertebra in the early postoperative period.
Keywords: overload vertebra body; radiological outcomes; anterior cervical discectomy and fusion; three-level surgery
1229
P517: Establishing a common term and definition for postoperative radicular pain following lumbar decompression: a scoping review
Samuel Goldman 1 , Jorden Xavier 1 , Evan Rothchild 1 , Hyun Song 1 , Aaron Hui 1 , Kai Parker-Fong 1 , Anne Schlumprecht 2,3 , Noel Akioyamen 2 , Yaroslav Gelfand 3 , Saikiran Murthy 3 , Jonathan Krystal 2 , Ananth Eleswarapu 2 , Reza Yassari 3 , Mitchell Fourman 2
1 Albert Einstein College of Medicine, Bronx, NY, USA
2 Department of Orthopedic Surgery
3 Department of Neurological Surgery, Montefiore-Einstein, Bronx, NY, USA
Introduction: After lumbar decompression surgery, patients often report new or recurring radicular pain. While some cases are linked to structural etiology like implant subsidence or incomplete decompression, many cases lack a clear structural cause. While in our experience such pain is self-limited and resolves within 3 months of surgery, this postoperative radicular pain can serve as a source of significant short-term morbidity, limiting recovery. One challenge in analyzing postoperative radicular pain is the wide variability in terminology and definitions used to describe it. This scoping review aims to clarify the terminology used to describe this postoperative phenomenon and establish a unified clinical definition, permitting better exploration of its risk factors, diagnostic criteria, and treatment options. Material and Methods: This scoping review adhered to the JBI methodology for scoping reviews and PRISMA-ScR guidelines. A comprehensive search strategy was employed on PubMed and Embase. Included studies were published within the last 10 years, involved subjects over 18 years old with postoperative radicular leg pain following lumbar decompression and/or fusion, and included at least one postoperative follow-up between one week and six months. Exclusions applied to studies involving endoscopic surgical techniques or subjects with severe structural deformities (scoliosis), autoimmune/ rheumatic disease, severe trauma to the operated region, or active malignancy. Results: We identified 21 articles for data extraction and analysis. The terminology used for new-onset radicular pain following lumbar decompression and/or fusion surgery included “postoperative radiculitis” (8 studies, 38.1%), “Failed Back Surgery Syndrome” (FBSS) (5 studies, 23.8%), “Post-Laminectomy Syndrome” (PLS) (2 studies, 9.5%), “persistent spinal pain syndrome” (PSPS) (1 study, 4.8%), “postdecompressive neuropathy” (PDN) (1 study, 4.8%), “persistent low back pain” (PLBP) (1 study, 4.8%), “battered root syndrome” (BRS) (1 study, 4.8%), “immediate failed back surgery syndrome” (iFBSS) (1 study, 4.8%), “persistent postoperative pain” (PPP) (1 study, 4.8%), “post-spinal surgery syndrome” (PSSS) (1 study, 4.8%), and “postoperative dysesthesia” (POD) (1 study, 4.8%). Terminology such as radiculitis, PDN, POD, BRS/iFBSS generally described acute (< 6 months), transient, purely radicular pain. Conversely, FBSS, PLS, PSPS, PPP, PSSS, and PLBP broadly described chronic (> 6 months) refractory back and/or leg pain. The reported incidence of newonset radicular pain following lumbar decompression and/or fusion ranged from 0.9% - 65. Identified risk factors included, long-term numbness and pain (3/21 studies, 14.3%), and a history of depression (2/21 studies, 9.5%). Conclusion: We propose defining “postoperative radiculitis” as distinct, radicular nerve pain in the absence of structural pathology, without motor weakness, occurring after the initial symptom resolution, typically within 3 months, and resolving within 6 months of lumbar decompression and fusion surgery. Clear differentiation from terms describing chronic post-spine surgery pain, such as FBSS, is crucial. Given the heterogeneous definitions for terms like FBSS and PLS, we recommend adopting the classification system by Christelis et al., which employs “Persistent Spinal Pain Syndrome” with ICD-11 subdivisions for long-term spinal pain (> 6 months). Future studies should focus on validating diagnostic metrics, exploring risk factors, prevention strategies, and potential treatment options for postoperative radiculitis.
Trauma - cervical
113
P518: To avoid misdiagnosis traumatic atlanto-occipital dislocation
Takahiro Tanaka 1 , Tsuyoshi Watanabe 2 , Gakuji Gondo 2
1 Neurosurgery, Yokohama City University School of Medicine, Yokohama, Japan
2 Neurosurgery, Shonan Kamakura General Hospital, Kamakura, Japan
Introduction: Traumatic atlanto-occipital dislocation (AOD) is being recognized increasingly as a result of advancement of critical care medicine and diagnostic modality. AOD is often overlooked by severe coexistent complication. Even if coexistent complications are mild, AOD may be overlooked by the anatomical specificity. Material and Methods: We report a case of traumatic AOD in a 38-year-old woman. She had fallen from 4th floor, was unconscious and had a Glasgow Coma Scale GCS) of three points. In the emergency ward, chest drain was inserted for left traumatic hemopneumothorax. After vital sign became stable, clinical and radiological work-up revealed traumatic AOD together with subarachnoidal hemorrhage at the craniocervical junction. Furthermore, multiple rib fracture, traumatic aortic dissection, T10 burst fracture and dislocation of temporomandibular joint were diagnosed. After intensive care treatment, she awaked and could move her limbs fully except left deltoid muscle (MMT 4/5). Fixation for ribs and thoracic burst fracture was performed before Occipital-C2 fusion. She was able to walk and manage all the activities of daily life after two months of clinical treatment. Results: Traumatic subarachnoid hemorrhage of the craniocervical junction is associated with 55% of AOD. Patients with AOD generally have severe disturbance of consciousness due to high-energy trauma or are intubated, and are often unable to complain symptoms by themselves. Therefore, when traumatic subarachnoid hemorrhage in the cranio-cervical transition region is observed, it is important to consider AOD. Conclusion: As emergency medicine and care develops, AOD will increase. So immediate and appropriate diagnosis, treatment will be required in future. Traumatic subarachnoidal hemorrhage at the craniocervical junction is often complicated with AOD. This can be the adjuvant of the diagnosis for doctors who do not specialize in spinal cord.
255
P519: Odontoid fracture: treatment, prognosis and associated morbimortality in a high concetration hospital
Jorge Andres Esparza Piña 1
1 Traumatología y Ortopedia, Instituto Mexicano del Seguro Social, Bahía de Banderas, Mexico
Background Context: The odontoid process is a superior bone element, protruding from the body of the second cervical vertebra C2. The atlas rotates around the odontoid process to provide the single largest component of lateral rotation of the cervical spine. Odontoid fractures are relatively common fractures of the C2 vertebral body that can be seen in low-energy falls in older patients and in high-energy traumatic injuries in young patients. Objectives: To analyze the associated morbidity and mortality, prognosis and treatment of patients with fracture of the odontoid process in the West in a high-concentration hospital and treatment updates. Material, Methods and Study Design: Cases and controls. Retrospective analysis with diagnosis of type II odontoid process fracture. Conservative treatment vs. surgical anterior fixation or posterior instrumentation is evaluated. For qualitative variables, frequencies and percentages are used. For quantitative variables, means and standard deviations will be used. Inferential statistics: Chi2 and fisher test. Any value of p < 0.05 will be considered statistically significant. Results: 29 patients were identified who met the inclusion criteria, of which 93.1% (27 patients) were classified as Anderson and D´Alonso type II and 6.9% (2 patients) as Anderson and D´Alonso type III. The mean age of the patients was 50.93 ± 20.90 years. Conclusions: Surgical treatment in patients with odontoid fracture has a higher rate of success in the resolution of patients with this pathology but does not modify the associated morbidity and mortality rate.
Keywords: odontoid process; c2 fracture; axis; Anderson D’Alonso; Odontoid fracture type II
339
P520: Lethal fracture dislocation of C6-C7 in patient with ankylosing spondylitis after hyperextension and neck brace removal
Adnene Benammou 1,2 , Cherif Kamoun 1,2 , Ahmed Ben Abid 1,2 , Seddik Akremi 1,2 , Mondher Kooli 1,2 , Mehdi Bellil 1,2 , Mohamed Ben Salah 1,2
1 Faculty of Medecine of Tunis, University Tunis el Manar, Tunisia
2 Orthopedic Surgery Department, Charles Nicolle Hospital, Tunis, Tunisia
Introduction: Ankylosing spondylitis may cause sever fracture dislocation of the spine after minor trauma due to biomechanical properties changes. These spine traumas are associated to neurological deficit in 65% of patients due to the high instability of these fractures. Neck brace should in correct always be worn until surgical stabilization. Material and Methods: Case report. Results: A 62-year-old male with history of ankylosing spondylitis victim of low energy road traffic accident-causing fracture dislocation of C6-C7 with no neurological deficit. Patient was immobilized with neck brace and transferred to our service. Due to the discomfort caused by the neck brace, the patient relatives removed it and removed the pillow under the patient head leaving the cervical spine in hyperextension. The patient presented neurological deficit with respiratory distress and cardiorespiratory arrest leading to death. Conclusion: Bad manipulation of cervical spine injured patient with ankylosing spondylitis can cause severe complications and even death. Doctors and patients should be aware of the injury mechanism and its care.
445
P521: Neglected traumatic subaxial bifacet dislocation without neurological deficit
Mohd Daniel Djamalludin 1 , Heng Keat Tan 1 , Hishamuddin Salam 1
1 Orthopaedic Department, Hospital Sultanah Aminah, Johor Bahru, Malaysia
Introduction: Bifacet cervical dislocations can be challenging to detect initially, often due to misinterpretation of clinical signs and radiographic findings. Neglected dislocations in the subaxial cervical spine pose difficulties in achieving reduction and surgical stabilization. Various surgical approaches have been proposed for their management, including anterior, posterior, posterior-anterior, posterior-anterior-posterior, and anterior-posterior-anterior-posterior approaches. Material and Methods: A 51-year-old male presented to our clinic complaining of persistent neck pain that had persisted for ten weeks since a road traffic accident. He had sought medical attention immediately following the trauma before coming to our facility. Upon clinical examination, midline cervical tenderness was noted, with no signs of neurological deficits. A cervical radiograph revealed bilateral facet dislocation at the C4/C5 level, along with spondylolisthesis. An MRI was performed, which did not indicate disc bulge or evidence of spinal canal stenosis. Following the failure of skeletal traction, we opted for a dual-position (posterior-anterior) approach for posterior and anterior fixation of the cervical spine. To achieve reduction, we carried out a partial resection of both C4 to C5 facet joints using a posterior approach. Half of the C4 to C5 facet joint was resected on both sides, and lateral mass screws were utilized for fixation. Half of the reduction was achieved through compression. Subsequently, we proceeded with anterior cervical fusion and employed a Caspar pin as the reduction tool for the remaining half of the reduction process. Results: Cervical spine injuries frequently go undetected, with radiograph misinterpretation identified as a prevalent cause of diagnostic oversights. Delayed patient presentation, often due to the absence of neurological deficits, further compounds the issue, with some patients seeking medical attention even a year after the initial dislocation. In such cases, radiographs may reveal the fusion of dislocated facets, allowing for nonoperative management when neurological deficits are absent. The role of preoperative traction in addressing neglected dislocations remains a contentious subject, with variable success rates reported among surgeons. The overarching objective is to achieve anatomical reduction and establish stability in dislocated spinal segments without affecting functional spinal regions. This necessitates mandatory release of both anterior and posterior soft tissues for reduction and comprehensive circumferential stabilization for fusion. Consequently, a combined surgical approach becomes the sole viable solution for such cases. Several authors have documented surgical interventions for longstanding subaxial cervical spine dislocations, including bilateral facet joint involvement. These procedures have demonstrated outstanding fusion rates and symptom improvement post-surgery. Multiple surgical methods have been reported, encompassing anterior, posterior, and combined approaches, often incorporating instrumentation for managing chronic bilateral cervical facet joint dislocation fractures. There are still no clear guidelines on this matter. Conclusion: Cervical spine fracture dislocation is an important injury that must be diagnosed accurately and managed acutely. A delay in surgical treatment will likely result in the progression of neurological deficits or injuries and difficulty in surgical reduction, potentially requiring more than one surgical approach. Future multicenter randomized controlled trials will be beneficial to develop proper guidelines.
605
P522: Long-term outcomes after surgery for subaxial spine injuries in octogenarians, a matched controlled analysis
Henrik Frisk 1,2 , Victor Gabriel El-Hajj 1 , Aman Singh 1 , Alexander Fletcher-Sandersjöö 1,2 , Ali Buwaider 1 , Simon Blixt 3 , Gunnar Nilsson 4 , Paul Gerdhem 3,5,6 , Erik Edström 1,4 , Adrian Elmi Terander 1,4,5
1 Department of Clinical Neuroscience
3 Clinical Science, Intervention and Technology (CLINTEC), Karolinska Institutet, Stockholm, Sweden
2 Department of Neurosurgery, Karolinska University Hospital, Stockholm, Sweden
4 Capio Spine Center Stockholm, Löwenströmska Hospital, Stockholm, Sweden
5 Department of Surgical Sciences, Uppsala University, Uppsala, Sweden
6 Department of Orthopedics and Hand Surgery, Uppsala University Hospital, Uppsala, Sweden
Introduction: Spinal fusion surgeries have been increasing worldwide due to a rise in aging population and advances in surgical techniques and anesthesia. An increasing life expectancy has necessitated changes in various medical disciplines to effectively address the healthcare needs of the elderly. Although surgical treatment for subaxial cervical fractures in octogenarians is common practice, the associated outcomes have been poorly described. Identifying risk factors that predict outcomes can affect decision-making and increase the safety of surgical interventions in the elderly. Purpose: To identify the differences in, and predictors of, surgical outcomes between octogenarians and a matched cohort of younger patients with subaxial cervical spine injuries. Study Design/Setting: Retrospective matched cohort study. Material and Methods: Eligible for inclusion were all patients surgically treated between 2006 and 2018, with either anterior or posterior fixation for subaxial cervical spine injuries at the study center. A cohort of octogenarians was identified and matched 1:1 to a corresponding cohort of younger adults based on the American Spinal Cord Injury Association (ASIA) Impairment Scale (AIS) at admission, surgical approach and number of fused levels. The primary outcomes were postoperative complications and mortality. Secondary outcomes were estimated blood loss and operative times. Results: Fifty-four patients were included in each of the octogenarian and younger groups (median age: 84.0 vs. 38.5). Surgery was performed at a median of 2 days from the cervical trauma in both groups. There were no significant differences in estimated blood loss (p = 0.403) or operative time (p = 0.625). While the risks for surgical complications, including dural tears and wound infections, were similar between groups, the risks of postoperative medical complications, including respiratory or urinary tract infections, were significantly higher among the elderly (p < 0.001). Screw loosening occurred more frequently in the elderly (p = 0.027), however there were no significant differences between groups in terms of revision surgeries (p = 0.495). Short- and long-term neurological outcomes (AIS) did not significantly differ between groups (p = 0.860 and p = 0.775). The 30 and 90-day mortality rates were significantly higher among the elderly (19% vs. 2%; p = 0.004 and 28% vs. 2%; p < 0.001). These differences were due to comorbidities in the octogenarian cohort and were abolished when propensity score matching was performed to account for the differences in American Society of Anesthesiology (ASA) grade. Conclusion: Octogenarians with comorbidities were more susceptible to postoperative complications such as postoperative infections, explaining the increased short-term mortality in this group. However, octogenarians without comorbidities had similar outcomes compared to the younger patients. These findings indicate that overall health, including comorbidities, rather than chronological age should be considered in surgical decision-making regarding octogenarians.
610
P523: Comparison of outcomes and complication rates between anterior cervical discectomy and fusion (ACDF) and anterior cervical corpectomy and fusion (ACCF) for treatment of subaxial cervical spine injuries: a single center matched analysis
Henrik Frisk 1,2 , Victor Gabriel El-Hajj 1,3 , Aman Singh 1,3 , Alexander Fletcher-Sandersjöö 1,2 , Simon Blixt 4 , Gunnar Nilsson 3 , Paul Gerdhem 4,5,6 , Erik Edström 1,3 , Adrian Elmi Terander 1,3,5
1 Department of Clinical Neuroscience
2 Department of Neurosurgery, Karolinska University Hospital, Stockholm, Sweden
3 Capio Spine Center Stockholm, Löwenströmska Hospital, Stockholm, Sweden
4 Clinical Science, Intervention and Technology (CLINTEC), Karolinska Institutet, Stockholm, Sweden
5 Department of Surgical Sciences, Uppsala University, Uppsala, Sweden
6 Department of Hand surgery and Orthopedics, Uppsala University Hospital, Uppsala, Sweden
Introduction: Anterior Cervical Discectomy and Fusion (ACDF) and Anterior Cervical Corpectomy and Fusion (ACCF) are both common surgical procedures in the management of pathologies of the subaxial cervical spine. While recent reviews have demonstrated ACCF to provide better decompression results compared to ACDF, the procedure has been associated with increased surgical risks. Nonetheless, the evidence regarding the ideal approach for the treatment of subaxial cervical spine injuries is still conflicting. The aim of this study was to compare surgical outcomes and complication rates of ACDF and ACCF for the treatment of subaxial cervical spine injury in a matched cohort. Material and Methods: All patients undergoing ACCF (one-level) or ACDF (two-levels) for subaxial cervical spine injuries between 2006 and 2018, at the study center, were eligible for inclusion. Patients were matched based on age and preoperative ASIA score. Results: A total of 104 patients met the inclusion criteria and were included in the unmatched analysis. After matching, 60 patients were included in the matched analysis, where 30 underwent ACDF and ACCF, respectively. Vertebral body injury was significantly more common in the ACCF group (p = 0.002), while traumatic disc rupture was more frequent in the ACDF group (p = 0.032). There was no statistically significant difference in the rates of surgical complications, including implant failure, wound infection, dysphagia, or CSF leakage, between the groups; p ≥ 0.05. The rates of revision surgeries (p = 1.0) and mortality (p = 0.222) were also similar. Conclusion: Results of both unmatched and matched analysis indicate that ACCF has comparable outcomes and no additional risks compared to ACDF. It is thus a safe approach and should be considered for patients with extensive anterior column injury.
853
P524: Acute traumatic sub-axial central cord syndrome: delay surgery causes disaster?
Shah Alam 1 , Sharif Ahmed Jonayed 2 , Abdullah Al Mamun 2 , Md Sarwar Jahan 2 , O Z M Dastagir 2
1 Spine Surgery, Bangladesh Spine & Orthopedic Hospital, Dhaka, Bangladesh
2 National Institute of Traumatology & Orthopaedic Rehabilitation, Dhaka, Bangladesh
Introduction: Based on the unfavorable outcomes of a small number of operated patients, they believed surgery to be inappropriate when Schneider first characterized the syndrome of acute central cervical SCI in 1954. Without the benefit of preoperative sophisticated imaging, such as magnetic resonance imaging or computed tomography, the patients had laminectomies and transdural discectomies. However, even after receiving conservative treatment, there may still be significant residual impairments, especially in the hands. Material and Methods: A retrospective evaluation of 62 patients who underwent surgery between 2011 and 2023 and had subaxial acute traumatic central cord syndrome (CCS) without fracture or dislocation was conducted. 40 of the men and 12 of the women were between the ages of 44 and 74. (mean 61.2). Following motor vehicle accidents (32%), falls were the most frequent cause of injury (68%). The American Spinal Injury Association (ASIA) Impairment Scale was used to collect motor scores during admission and follow-up. CT and MRI scans were performed on each patient (MRI). Three patients with one or two levels of lesions underwent anterior decompression and fusion. Nine patients had posterior decompression and fusion procedures done for multilevel lesions. The time between the injury and operation was anything between 11 and 37 days (mean 19.0). Following surgery, every patient improved clinically. Results: Within the first six months following surgery, a significant improvement in ASIA score was made. Patients who received surgery within 7 days of the injury or after 7 days of the injury, using various methods, did not significantly differ from each other. Conclusion: Patients with TCCS can receive surgical surgery without risk. The first six months of follow-up saw a significant improvement in the ASIA score. The type of lesion, the timing of surgery within or after 7 days of the injury, and the surgical technique were all unimportant factors in determining the final ASIA score. Age upon injury was favorably connected with the ASIA motor score.
925
P525: Posterior C1-C2 fixation forunstable C2 fractures: our experience
Biswaranjan Nayak 1
1 Neurosurgery, Kalinga Hospital Limited, India
Introduction: Posterior fixation for complex C2 fracture with instability is a very good method with excellent outcome. Methods: A total of 9 patients were included in the study (8 males and 1 female). Their age ranged from 43 to 76 years. The patients were diagnosed with complex fractures of the axis of the upper cervical spine and underwent posterior C1-2 pedicle screws fixation. The patients underwent a serial postoperative clinical examination at approximately 3, 6, 9 months, and annually thereafter. The neck disability index (NDI) and the range of neck rotary motion were used to evaluate the postoperative clinical efficacy of the patients. Results: The mean follow-up was 1-3 years. The average operation time and blood loss were 105-150 min and 50-75 ml, respectively. The neck disability index was improving after surgery to a great extent. The patients with myelopathy (specifically in old C2 fracture with cord compression) also showed significant improvement as assessed by Nurick grading. Conclusions: Posterior screw fixation is a good surgical treatment option for unstable complex C2 fractures.
932
P526: Results early versus delayed decompression of traumatic cerival spinal cord injury: a single center prospective study
Biswaranjan Nayak 1
1 Neurosurgery, Kalinga Hospital Limited, Bhubaneswar, India
Objective: This study was done with the aim to compare the clinical outcome and patient's quality of life between early (within 24 hours post-injury) versus delayed (after 24 hours to 7 days) surgically treated patients of acute cervical spinal cord injury. The current study was based on the hypothesis that early surgical decompression and fixations in acute cervical spinal cord trauma are safe and are associated with improved outcome as compared with delayed surgical decompression. Methods: A total of 54 patients were recruited and divided into early decompression surgery group A (operated within 24 hours of trauma; n = 25) and late/delayed decompression surgery group B (operated between 24 hours and 7 days of trauma; n = 29). The patients in both groups were followed up, and comparative differences noted in the neurological outcome, quality of life, and bony fusion. Results: The early surgery group had lesser postoperative complications. In group A, 54.17% patients had 1 American Spinal Injury Association Impairment Scale (AIS) grade improvement, while 29.17% experienced > 2 AIS grade improvement (p = 0.015). In group B, the neurological improvement was 50 and 21.43%, respectively (p = 0.003). There was a significant improvement in the postoperative quality of life scores in early surgery group. Conclusion: Early surgery in patients with acute cervical spinal cord injury should be considered strongly in view of the lesser complications, better neurological recovery, and reduced mortality.
937
P527: Artifical neural networks for the detection of odentiod fracture by KNIME analytic platform
Wongthawat Liawrungrueang 1 , Peem Sarasombath 2
1 Orthopaedic Department, School of Medicine, University of Phayao, Phayao, Thailand
2 Orthopaedic Department, Faculty of Medicine Chiang Mai University, Chiang Mai, Thailand
Introduction: Artificial neural networks (ANNs) are computing systems inspired by the biological neural networks that constitute human brains. Computer-assisted diagnosis with ANNs from radiographic x-ray imaging was increasingly popular in the fields of medical image processing. Odontoid fracture is a common fracture of the axis and account for 10-15% of all cervical fractures. A literature review computer-assisted diagnosis with ANNs was not previously reported. This study proposes the ANNs for the detection of odontoid fracture by the Konstanz Information Miner (KNIME) analytics platform to offer a technique for computer-assisted diagnosis from radiographic x-ray imaging. Material and Methods: This study obtained four hundred thirty-two open-mouth (odontoid) radiographic views of cervical spine x-ray images for dataset repositories to develop an ANNs model base on a convolutional neural network (CNN) theory. All of the images contained diagnostic information, including normal radiographic images (n = 216) and fracture images of the acute odontoid fracture (n = 216). The model would classify whether the patient was odontoid fracture or not. Seventy percent of the images were training data sets used for model training, and thirty percent were used for testing. KNIME’s graphic user interface-based programming enabled class label annotation, data preprocessing, model training, and performance evaluation. Results: All radiographic x-ray imaging was reported under the graphic user interface program by KNIME. The ANNs model has performed 50 epochs of training. Performance model evaluation for detecting odontoid process fracture by the sensitivity (recall), specificity (predictive value) f-measure and prediction error were all 100%, 95.4% 97.77% and 2.3%, respectively. The model’s accuracy was equal to 97% of the area under the receiver operating characteristic (ROC)curve for the diagnosis of odontoid process fractures. Conclusion: ANNs models with KNIME analytics platform were successfully utilized for computer-assisted diagnosis of odontoid fractures using radiographic x-ray images. This approach can assist the radiologist in the screening or assist in the detection and diagnosis of acute fractures.
992
P528: Cervical bilateral facet dislocation without neurological abnormality: a case series in single tertiary hospital
Aries Rakhmat 1 , Aliefio Japamadisaw 1
1 Orthopedic and Traumatology, Dr Soetomo General Hospital, Universitas Airlangga, Indonesia
Introduction: Traumatic subaxial cervical fracture- dislocation with spinal cord injury (SCI) can cause long-lasting dysfunction in many organ systems resulting in significant financial burden and functional disability. The patient may come with complete or incomplete neurological deficit, and however, there is also a possibility of no neurological deficit. Material and Methods: This case series presented three cases of 68-year-old man, 54-year-old man and 44-years old woman that came to the emergency department after traffic accident and fall from height. Surprisingly there was no neurological deficit was found on both patients. The patient underwent emergency open reduction and posterior stabilization. Several weeks after, the neurological function was still excellent. Results: In the subaxial cervical spine (C3-C7), bilateral pedicle fractures, bilateral locked facets, with or without fracture of the laminae, are the most common causes of post-traumatic spondylolisthesis. Enlargement of the spinal canal is significant when the vertebral body and the shattered posterior arch separate, which may play a protective role on the spinal cord. In the first and third case, neurological deficit was not happened due to widening of the spinal canal, but in second case the patient’s neurological condition remained excellent even there was no disruption on the posterior arch after cervical bilateral facet dislocation. Conclusion: Mostly, the neurological deficit has not happened in the fracture and bilateral facet dislocation with disruption of the posterior arch due to the widening of the spinal canal, but in our case the patient’s neurological condition remains excellent even though there is no disruption on the posterior arch after cervical vertebrae bilateral facet dislocation. Treatment of this injury should be done properly to prevent other morbidities and even mortality.
1075
P529: Non-surgical approach to combined C1 and C2 fractures
Ahmad Faizal Razali 1 , Asrul Syamin Hisyam Yong 1 , Satpal Charl 1 , Amir Zakaria 2
1 Orthopaedic, Hospital Sultan Idris Shah, Serdang, Selangor, Malaysia
2 Orthopaedic, Hospital Sungai Buloh, Selangor, Malaysia
Introduction: Combined fractures of the C1 and C2 vertebrae represent a distinct subset of spinal injuries that demand particular attention due to their critical location within the cervical spine. This region is particularly susceptible to injury given its anatomical characteristics and its integral role in the stability and rotational function of the neck. Combined fractures of C1 & C2 account for 3% of all acute injuries to the cervical spine. An individualistic approach is required to manage these fractures. This case report highlights the conservative management of a patient with simultaneous C1 (Landells Type 1) and C2 (Anderson and D'Alonzo Type III) fractures. Material and Methods: A 38-year-old male came with Spinal cord injury AIS C with anterior arch C1 fracture and a Type 3 dens fracture of C2 after an MVA. MRI revealed spinal cord oedema with no cord compression. Intravenous dexamethasone was started immediately and the patient had significant neurological improvement. To stabilize the fracture, we opted for halo vest application to preserve the motion of the neck. Despite the challenging and unfavorable fracture pattern, surgical intervention was deferred in favor of the patient's improving neurological status. Results: At 3 months post-trauma, X-ray images show a bony union of the fractures and subsequently the halo vest fixator was removed. The patient has complete neurological recovery and has started work. There is some limitation to the range of motion of the neck but not disturbing his daily functions. Conclusion: Combined atlantoaxial fractures are life-threatening injuries that require an individual approach to each patient. Although surgery is warranted due to the neurological injury, at times, conservative approaches may emerge as the more beneficial and less traumatic option for the patient, ultimately yielding superior outcomes. In this case, complications that could arise from surgery were also avoided.
1257
P530: Posterior ligamentous complex reconstruction with artificial ligament in patients without cervical vertebral fracture: a technical note
Chengyi Huang 1
1 Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China
Introduction: Posterior ligamentous complex (PLC) offers restraints to deformation as a complex with an interconnected manner. The stability and range of motion of the posterior cervical spine is greatly restricted when the posterior ligamentous complex is damaged, even without bone disruptions. We describe an original surgical technique, advantages with the novel technology, and postoperative condition of patient who was first used of artificial ligament in reconstruction surgery of posterior complex ligamentous injuries in patients without lower cervical vertebral fracture. The aim of this technique is to retain the mobility of the injured segment as much as possible on the basis of spinal stability, and try to treat these patients with dynamic reconstruction. Material and Methods: Detailed description of the reconstruction surgery with artificial ligaments carried out for C4-6 posterior complex ligamentous injuries in a 27-year-old male, with neck pain and restricted movement due to high fall injury accompanied by impaired movement of limbs, is presented. Results: Immediately postsurgery, the patient's neck pain and quadriparesis had been improved. The spinal canal decompression and cervical spine sequence was satisfactory, the facet joint face was in good position and spinous process spacing returned to normal. After three months of rehabilitation, the patient reported improvement of symptoms, physical and imaging examination showed a significant improvement in the patient's condition. The patient's neck mobility motor function had improved further. Conclusion: The present data demonstrates that the novel technique for reconstruction of PLC injury is feasible and safe. However, familiarity with cervical anatomy and adequate experience for the lateral mass screws placement during surgery are crucial for this procedure. Therefore, this surgery should be best conducted by a highly experienced cervical surgery team.
Keywords: cervical vertebra; posterior ligamentous complex; injury; non-fusion; reconstruction
1516
P531: The impact of surgical strategies on patient outcomes in acute traumatic central cord syndrome
Niklas Rutsch 1 , Christoph Albers 1 , Martin Müller 2 , Sebastian Bigdon 1
1 Department for Orthopedic Surgery and Traumatology
2 Department for Emergency Medicine, Inselspital, Bern, Switzerland
Introduction: Acute Traumatic Central Cord Syndrome (ATCCS) is the most prevalent acute incomplete spinal cord injury. Its clinical presentation is diverse, marked by pronounced upper-extremity motor weakness and a loss of sensation along the shoulder girdle. Surgical intervention is the standard approach for ATCCS management, but the lack of surgical guidelines makes the surgeon's experience pivotal. This study aims to investigate the clinical utility of anterior and posterior surgical approaches in ATCCS, their influence on patient outcomes, and their economic implications. Additionally, we explore whether the choice of surgical approach is influenced by patient characteristics and its subsequent impact on clinical outcomes and cost-effectiveness. Materials and Methods: We will conduct a retrospective analysis of fully anonymized data sourced from German health insurance records provided by GWQ Serviceplus AG. Our study will encompass patients diagnosed with ATCCS who received surgical treatment (Operation and Procedure Code [OPS] 5-03). We will include patients with ATCCS (ICD-10-GM S14.10, S14.12, S14.13) and exclude patients with complete spinal cord injury (ICD S14.11). The population will include patients from 2011 to 2022, stratified by age groups and sex, and we will assess outcomes within a one-year follow-up period following their initial diagnosis. Thus, we will split the patients into two cohorts by the surgical approach they received (anterior vs. posterior) according to their respective OPS coding. Our primary outcome is the comparison of rehospitalization and reoperation rates between the two surgical cohorts. Secondary objectives involve characterizing ATCCS incidence, hospitalization frequency and duration, mortality rates, comorbidities (e.g., Charlson index), and healthcare costs, encompassing both inpatient and outpatient care as well as medication expenses. Results: The dataset provided by the GWQ Serviceplus AG comprises 5 million insured people, making up a total of over 600 million cases from the beginning of 2010. It combines insights into population demographics with data on acute and inpatient hospital care, medication prescription, and involved healthcare providers. A preliminary search identified a total of around 1,000 patients with ATCCS who received subsequent surgical treatment. Conclusion: While our study is ongoing, we anticipate that our research will yield valuable insights into the management of this rare yet significant injury. As surgical treatment is crucial for patient outcomes in ATCCS, we aim to better understand how to determine the correct surgical approach for the individual patient.
1524
P532: Percutaneous fixation of Hangman's fracture
Petr Vachata 1 , Jan Lodin 1
1 Neurosurgery Department, Spine Center Ústí nad Labem, Masaryk Hospital, UJEP, Usti nad Labem 11, Czech Republic
Introduction: Open anterior and/or posterior C2–3 fixation and fusion are standard treatment modalities for dislocated hangman's fractures requiring surgery. In certain situations, transpedicular fixation with fracture reposition and compression via Judet screws can serve as an alternate treatment option. Materials and Methods: From 2016 to 2022, we treated 13 cases of dislocated Hangman fractures type I or type IIa with posterior percutaneous fixation. Patient ages ranged from 38 to 88 years (mean average 51 years), with 8 men and 5 women forming the cohort. MRI ruled out disruption of the C23 disc in each instance. After the K-wires were placed, lag titanium screws were implanted utilizing frameless navigation, using intraoperative cone beam CT scan (O-arm). In ten cases, bilateral transpedicular screws were used, and in two cases, transpedicular and translaminar screws were combined. Due to a technical issue, only one patient received a unilateral transpedicular screw. Results: There were no complications during the surgery or follow-up. Screw malposition did not occur. After three months, osseous union, determined by a CT scan, was achieved in 12 cases. The final case had severe osteoporosis and osseous fusion occurred after one year. At the one-year, there no patients exhibited instability or angulation at the C2-3 segment. Twelve patients had full range of motion, based on clinical examination. Conclusion: Minimally invasive percutaneous intraoperative CT guided fixation of selected Hangman fractures is a safe and technically feasible procedure that preserves physiological range of motion.
1842
P533: Dysphagia as a symptom of hardware failure following anterior cervical spine fusion: a case report and review of literature
Jlidi Mohamed 1 , Ibrahim Najjar 1 , Walid Bouaicha 1 , Karim Mallek 1 , mouldi lamouchi 1 , Amine Soussou 1 , Mohssen Chamekh 1 , Achref Abdennadher 2 , Selim Daas 1
1 Orthopedics and Traumatology Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia
2 Orthopedics and Traumatology Department, Military Hospital of Instruction, Tunis, Tunisia
Introduction: Dysphagia is a common multifactorial complication following cervical spine surgery. It can occurs at any time after surgery and can be life threatening. We describe the case of tardive dysphagia as a symptom of hardware failure. Material and Methods: We present the case of a 60-year-old male who was admitted to our department after falling from 02 meters. Physical examination revealed cranial trauma without loss of consciousness. Cervical spine was painfull with limited motion. The neurological exam showed incomplete motor and sensory deficit. X-rays and CT-scan showed a bilateral C5-C6 dislocation associated to C6 superior articular process fracture. The procedure was done at 5 hours post traumatic. The reduction was done by external maneuvers under fluoroscopic guidance. Through an anterior approach, arthrodesis was performed by a plate using a tricortical bone graft taken from the iliac crest. Post operatively neurological exam was unchanged. X ray showed an acceptable reduction. The patient was discharged at home. Results: Three months after surgery the patient complained of a progressive dysphagia. On physical examination, we noted a recovery of the neurological deficit. X-rays revealed hardware failure with a screw migration. Infection was ruled out and we opted for screw extraction. At the last follow-up, there was no neurological sign, no residual pain and the reduction was judged acceptable. Conclusion: Dysphagia following anterior cervical spine surgery remains frequent. Cervical plating appears to be one of the risk factors. A regular follow-up is a must, to detect and treat this complication as early as possible.
1917
P534: Traumatic cervical spondyloptosis C4-5 treated by slow traction - Reduction then internal fixation
Rakesh Kumar 1 , John Small 1
1 Orthopedics, University of South Florida, Tampa, USA
Introduction: Delayed onset of traumatic spondyloptosis is rare. Often, vertebrectomy is considered as reduction is often not possible. We describe a patient with minimal radiologic findings who later developed cervical spondyloptosis and mild neurologic deficits. For such a problem traction is often done short-term; if at all. We describe a different management strategy. Case report: A 25-year-old woman catapulted over barbed wire fence in the ATV accident. The initial studies seemed unremarkable, and she was discharged without a brace though still in pain. Three months later, spondyloptosis of C4-5 was noted when she presented with paresthesiae in the upper extremities and mild myelopathic features. Progressive increase in traction was done, with the patient awake. This was over 4 days, starting with 10 pounds, and gradually increasing to 40 pounds. Finally a change in direction of traction resulted in significant improvement. Reduction was finally completed intraoperatively by combined anterior and posterior approach and internal fixation; with anatomic alignment. She had full neurologic recovery, remained free of pain; and with solid fusion on long term follow-up. Conclusions: Follow-up after cervical spine injury is important to prevent such a complication of missing ligamentous injury. Though seemingly un- reducible, a trial of traction is warranted to determine if it is indeed fused. The principles of traction to reduce a fracture can also be applied to the cervical spine.
2041
P535: C1-C2 sublaminar taping for displaced odontoid synchondrosis fracture in an infant: a case report and novel surgical technique
Ryan Campbell 1 , Motofumi Yasutomi 1 , Sarah Nicholls 1 , Stephen Ruff 1 , Randolph Gray 1
1 Orthopaedics, Royal North Shore Hospital and The Children's Hospital at Westmead, Sydney, Australia
Purpose: Paediatric cervical spine injuries are rare, and the diagnosis and management can be challenging. Surgical intervention has been recommended in unstable odontoid synchondrosis injuries or those which have failed non-operative measures. However, the literature remains sparse on the operative management of severe injuries due to the low incidence. Methods: An 18-month-old female sustained an unstable odontoid synchondrosis fracture from a motor vehicle accident. Due to ongoing instability after initial immobilisation in a Halo, the decision was made to proceed with surgical management. With the patient positioned prone and neural monitoring throughout, a posterior approach was utilised. Subperiosteal exposure of the C1 posterior arch was performed bilaterally. A spinal fixation band was passed under the right C1 posterior arch, around the C2 spinous process, under the left C1 posterior arch and finally back under the C2 spinous process. The C1-C2 distraction was reduced using intraoperative imaging and the sublaminar tape construct was secured and reinforced. The halo was then reattached. Results: Post-operative recovery was complicated by a Halo pin site infection which was treated with oral antibiotics. The Halo was removed after 3 months, following a CT which demonstrated union. X-Rays at 6 months revealed anatomical alignment with union. Conclusion: Surgery is recommended in paediatric odontoid synchondrosis fractures refractory to non-operative management. Sublaminar taping of C1-C2 with a spinal fixation band has demonstrated to be an effective surgical technique in the management of an unstable odontoid synchondrosis fracture.
2081
P536: Novel approach of using dual mini rods reduction technique for bifacet cervical dislocation
Shun Herng Tan 1 , Han Sim Lim 1 , Jayathilak Shanmugam 1 , Jun Jie Chew 1 , Ban Heng Teh 1 , Zairul Anuar Kamarul Bahrin 1
1 Penang General Hospital, Malaysia
Introduction: There is no consensus in treatment of sub-axial facet dislocation. In literatures, posterior open reduction often involves facetectomy and use of instruments such as periosteal elevator, pedicles screw, bone holding forceps, curette, interlaminar spreader. Traditional reduction techniques for facet dislocation can be challenging in case of end plate and spinous process fracture. The use of pedicle screws and mini rods represents a potential alternative to traditional methods, offering improved outcomes and reduced risk of complications. Report: We report a case of an 82-year-old man with no prior medical illness who was involved in a motor vehicle accident resulting in neck pain with no neurological involvement. Imaging revealed a C6/C7 bifacet fracture dislocation with C6 laminar and spinous fracture. The patient underwent posterior spinal instrumentation and fusion of C4-T1. Intraoperatively, difficulties in performing reduction were encountered due to the fracture of the involved spinous process. Pedicle screws insertion were made over bilateral lateral mass and pedicles of C7 and T1 respectively, followed by the application of two short rods acting as a frame, and to manipulate the upper vertebra using power rod gripper to achieve reduction. Bilateral partial facetectomy was made prior reduction. Intraoperative neuro monitoring showed no signal change, and post-surgery, the patient had no neurological deficits. Conclusion: Use of dual mini rods reduction for cervical facet dislocation allows better control of the cranial vertebrae, provided there is strong bone, good pedicle screw placement, and intraoperative neuromonitoring.
2174
P537: An experience of treating unstable cervical flexion tear-drop fracture via combined anterior and posterior fixation
Kesavan Ramachandran 1 , Saravanan Shanmugam 1
1 Orthopedic Department, Hospital Seri Manjung, Perak, Malaysia
Introduction: Flexion tear drop fracture represent a fracture pattern occurring in severe axial/flexion injury of the cervical spine. They are important to recognize because they indicate extensive underlying ligamentous injury and spinal instability. Although most cases of tear drop fracture can be treated conservatively, surgical treatment is indicated in cases of the unstable type. Material and Methods: Based on reported studies and our clinical experience, we consider a massive avulsed fragment, intervertebral disc injury, and displacement of ≥ 3 mm as features of an unstable fracture. To our knowledge, there are few reports on surgical procedures treating cervical flexion tear-drop fracture, and the ideal surgical treatment for unstable flexion tear drop fractures remains controversial. We present our experience and the outcome of treating unstable cervical flexion tear drop fracture via combined 360° fixation. Results: We performed combined anterior and posterior fixation to ensure adequate stabilization. The advantages of this procedure were as follows: (I) the avulsed fragment, which may compress the esophagus and lead to dysphagia, could be reduced and fixed directly. (II) The instability at the injured disc could be addressed, and decompression could be achieved directly. (III) The procedure could provide both anterior and posterior support, ensure immediate postoperative stability, and enhance the bony union and fusion. Our patient was allowed early mobilization 3 days post operation and manage to return to work by 6 weeks post operation. Conclusion: The clinical and radiological outcomes of combined anterior and posterior internal fixation for the treatment of unstable Cervical flexion tear drop fracture were satisfactory and could be considered as a safe and effective method for managing such injury.
2182
P538: Os odontoideum fracture in adults: a clinical case study of evaluation and management
Esteban Espinoza 1 , Ratko Yurac 1
1 Unidad de Traumatología de Columna, Clínica Alemana de Santiago, Vitacura, Chile
Introduction: Os odontoideum (OO) is a rounded ossicle that is separated from the body of the axis by a transverse space. Some authors associate it with a previous injury to the odontoid process, in which an unrecognized fracture is distracted by the alar ligaments and produces a pseudoarthrosis, while others suggest that it is congenital. Presentation varies from neck pain, symptomatic myelopathy to even sudden death. Diagnosis is usually made in adolescence or early adulthood and can be detected on lateral radiographs of the cervical spine, visualizing the defect with flexion-extension and a displacement of C1 over C2. In most cases, surgery is necessary for symptomatic patients, but the best treatment for patients with OO is controversial, as it is difficult for clinicians to predict which patients will require surgery to prevent further symptoms. Case Presentation: The case of a 38-year-old male patient with insulin-dependent diabetes mellitus is presented, with an episode of syncope with loss of consciousness of about 5 minutes. He was admitted with a diagnosis of diabetic ketoacidosis and probable cardiogenic syncope, and was hospitalized for study, presenting persistent post-traumatic neck pain without focal neurological deficit. An angiotomography of the neck vessels was performed, detecting a probable OO fracture in the bone-windowed images, without signs of vertebral artery stenosis. Computed tomography and magnetic resonance imaging of the cervical spine were requested, reporting acute subluxation of the C1-C2 lateral joints, a small avulsive fracture of the OO, and disruption of the regional posterior longitudinal ligament, as well as C5-C6 vertebral block. Dynamic cervical radiography shows a slight increase in the space between the OO and the anterior arch of the atlas, with no modification in flexion. It is worth noting that the patient recently began to experience sleep apneas without recent weight gain. In this case, orthopedic therapy with a Miami collar and outpatient follow-up was chosen, where a Harms-type surgery was planned. Discussion: The presented case is a typical example of a symptomatic os odontoideum fracture in an adult, confirmed by CT and MRI. The patient's symptoms, neck pain and syncope, are two of the most common of this condition. Diabetes mellitus is a known risk factor for vertebral fractures, with a 4.5-fold increased risk of vertebral fractures in diabetic patients. The treatment of symptomatic os odontoideum fracture in adults depends on the severity of the fracture. Stable fractures can be treated with a cervical collar, while unstable fractures may require surgery, as in the presented case.
2315
P539: Upper cervical spine injuries, orthopedic versus surgical treatment: a dual center experience and review of litterature
Elouni Emna 1 , Mohamed Amine Hadj Taieb 1 , Atef Ben Nsir 1 , Wiem Boudabbous 1 , Mohamed Ali Kharrat 1 , Mehdi Darmoul 1
1 Department of Neurosurgery, Fattouma Bourguiba, University Hospital of Monastir, Monastir, Tunisia
Introduction: The upper cervical spine, including C0-C1-C2, is a unique anatomical and functional unit. Since it is a highly mobile functional unit, traumatic events in this area may produce devastating neurological complications and death. Material And Methods: We conducted a retrospective study, collecting data from the neurosurgical departments of the university hospital of Monastir and the university hospital of Sfax, within 6 years from the survey date. Results: We included 40 patients in our study. Median age was 40.6 years (5-83 years) with a male to female sex ratio of approximately 1.5. We assessed the neurological status using the AIS (American Spinal Injury Association Impairment Scale) score, revealing that 90% of the cases were classified as grade E, 7.5% as grade B, and 2.5% as grade A. The radiological findings indicated various types of upper cervical spine injuries, including 19 cases (47.5%) of odontoid fractures, 3 cases (7.5%) of Hangman's fractures, 7 cases (17.5%) of isolated atlas fractures, 9 cases (22.5%) of combined Atlas and Axis fractures, and 2 cases (5%) of occipital condylar fractures. 50% of our patients had orthopedic treatment. They all had an AIS grade of E. Among them, 10% experienced radiologically unfavorable progression to pseudoarthrosis, while maintaining an AIS grade of E. 50% of our patients underwent surgical treatment. Only one patient had an initial AIS grade of A and unfortunately passed away postoperatively. Three patients had an initial AIS grade of B, with one patient succumbing and another progressing to AIS grade C. Conclusion: Upper cervical spine injury usually results from high-energy events such as falls, sports injuries, traffic accidents. These traumatic injuries can sometimes be very difficult to diagnose, to manage, and to treat.
2317
P540: Atlanto-axial fusion using C2 translaminar screws and C1 hooks: a case report
Raddaoui Walid 1 , Atef Ben Nsir 1 , Gallaoui Slim 1 , Ghorbel Mohamed 1 , Elouni Emna 1 , Mehdi Darmoul 1
1 Department of Neurosurgery, Fattouma Bourguiba, University Hospital of Monastir, Monastir, Tunisia
Introduction: The atlantoaxial (C1-C2) complex is a different unit from the rest of the cervical spine because of its mobility and its bony and vascular anatomy. Its dislocation caused frequently by trauma can threat a patient’s life if not treated. Since the beginning of the 20th century, several surgical techniques have been developed to fix this C1-C2 complex dislocations. Material and Methods: A 32-year-old doctor consulted the emergency department in October 2021 for a direct cervical spine trauma following a traffic accident. The patient had isolated neck pain without motor or sensitive deficit. He was immobilized by a cervical collar and had an urgent spinal CT scan which revealed a C1-C2 dislocation without bone fracture. The patient underwent a posterior atlantoaxial fusion using C2 translaminar screws combined with a bilateral C1 hooks without bone grafting. Results: The surgery went well without incident with a satisfying assembly confirmed by a postoperative imaging. Neck pain was disappeared few days after surgery and the patient is now living without health issues. Conclusion: The fusion technique using bilateral C1 hooks combined with C2 translaminar screws can be used to fix C1-C2 dislocations to avoid neurovascular risks.
2319
P541: Distractive flexion injuries of subaxial cervical spine, anterior or posterior surgical approach? A case report and review of litterature
Elouni Emna 1 , Atef Ben Nsir 1 , Raddaoui Walid 1 , Wiem Boudabbous 1 , Mohamed Ali Kharrat 1 , Belkahla Ghassen 1 , Mehdi Darmoul 1
1 Department of Neurosurgery, Fattouma Bourguiba, University Hospital of Monastir, Monastir, Tunisia
Introduction: Injuries to the subaxial cervical facets causing dislocation with or without fracture are due to complex flexion and distraction forces with accompanying element of axial rotation. In recent years, anterior surgery has become popular for the management of cervical distractive flexion (DF) injuries. Material and Methods: We report the case of a 58-year-old male patient presented with left lower limb weakness and bilateral upper limb numbness following a cervical spine trauma. A computed tomography (CT) scan of the cervical region revealed a grade II anterolisthesis of C6 over C7 and a grade III anterolisthesis of C7 over T1. The decision was to perform a C6-D1 anterior arthrodesis procedure with C7 corpectomy and inter-body graft insertion. Results: Intraoperatively, despite multiple attempts at reduction using external maneuvers and a partial corporectomy of C7, there was a secondary displacement of T1, which became no longer visible through the anterior surgical approach. An emergency cervical CT scan showed a 26mm high diastasis between C6 and T1. The patient was reoperated using posterior approach and fixation were done using pedicle screws at T2/T3 and lateral mass screws at C5/6 level. Conclusion: Although there have been several reports regarding DF injuries that were treated by anterior plating with good clinical outcomes, 10-14 several biomechanical studies have shown the superiority of posterior fixation over anterior plating for this type of injury, and anterior fixation alone has proven insufficient.
Trauma - thoracolumbar
23
P542: Outcome assessment of surgical management of patients with thoracolumbar fracture
Virendra K Verma 1
1 Orthopedics, All India Institute of Medical Sciences, Bhopal, India
Intoduction: To assess radiological outcome following surgical management in patients with thoracolumbar fractures using Local Kyphotic Angle( LKA), Traumatic Regional Angle (TRA), Anterior Vertebral Height Ratio( AVHR), Posterior Vertebral Height Ratio (PVHR) at follow-up of 6 months. To assess functional outcome following surgical management in patients with thoracolumbar fractures using Visual Analogue Scale (VAS), Oswestry Disability Index (ODI), & American Spinal Injury Association (ASIA) scale at follow-up of 1 years. Material and Method: This study was conducted at AIIMS, Bhopal during the study period from July 2019 to October 2021. A total of 52 patients were included. This was an observational prospective study. We recorded demographic data, age, sex, occupation, mode of injury, level and type of fracture and ASIA grades in participants. For assessment of radiological outcome LKA, TRA, AVHR, and PVHR were measured preoperatively and at the final follow-up of 6months post-operatively. For assessment of functional outcome, VAS score for pain and ASIA impairment scale was measured preoperatively and at the final follow-up of 6-months post-operatively. The ODI was assessed during the postoperative period only at the follow-up of 6 weeks and final follow-up of 1 years post-operatively. Result: Thoracolumbar fractures are common in the young male patients. The most common mode of injury is due to fall from height and commonly involved the thoracolumbar junctional area (L1 vertebrae followed by D12 vertebrae) due to sudden transition between the rigid thoracic spine and flexible lumbar spine. All the radiological parameters showed statistically significant changes (p-value < 0.05) when preoperative values were compared with values at 6months of the postoperative period which suggests surgical intervention restores the spinal alignment up to the acceptable level and maintains the correction till the healing of fractures. All the functional parameters showed statistically significant (p-value < 0.05) changes, except ASIA grading. Pre-operative VAS was improved from severe in all patients to mild category 1 year postoperatively. Functional disability (ODI) was severe to crippled disability improved to minimal or moderate disability from 6 week post-operative period to 1 year postoperatively. Although results were insignificant as per the ASIA impairment scale, 22 patients out of 15 patients with complete or incomplete neurological deficit showed at least 1 grade of improvement in the ASIA scale and showed no improvement in 4 patients. Conclusion: Fixation of fractured vertebrae in patients with complete or incomplete neurological deficit helps in early mobilization, rehabilitation, deformity correction, and improvement in the quality of life. Trends of functional and radiological outcomes following surgery for thoracolumbar vertebral fractures may differ. Although major progress has been made in the treatment of thoracolumbar trauma, accurate assessment of radiological and clinical outcomes following surgical management is still a challenge for surgeons because of the lack of standardized clinical and radiological outcome measures.
206
P543: Comparative analysis of neurosurgical intervention and conservative therapy in managing stable thoracolumbar junction fractures
Zayed Almadidy 1 , Ankit Mehta 1 , Sam Jiang 1
1 UI Health Department of Neurosurgery, The University of Illinois at Chicago, Chicago, USA
Introduction: The Thoracolumbar Junction (TLJ), extending from T11-L2, is crucial for mobility as it links the relatively rigid thoracic spine to the more flexible lumbar spine. Stable TLJ fractures are a common injury, and there is ongoing debate in the medical community about whether conservative therapy or surgical intervention offers better outcomes for patients. Objective: This study aims to evaluate the impact of surgical intervention versus conservative therapy on the length of hospital stay (LOS) and in-hospital complications in patients with stable TLJ fractures. Methods: We queried the National Trauma Data Bank for adult patients with a stable compression or burst fracture of the TLJ from T11-L2 who underwent surgery or conservative therapy between 2017-2019. One-to-one propensity score matching was performed based on demographics, comorbidities, injury severity, and insurance type, comparing patients who underwent neurosurgery to those who received bracing alone. Standardized Mean Differences (SMD) were calculated to ensure balance between groups. Differences in outcomes were compared using paired Student’s t-tests and Pearson’s chi-square tests, with a false discovery rate controlled using the Benjamini-Hochberg multiple comparisons correction. Results: Out of 17,969 patients who met the inclusion criteria, 2,976 patients were identified in each group following propensity score matching. After matching, 37 out of 42 variables had a post-match SMD < 0.1. The surgery group had a significantly longer LOS (11.29 days vs. 5.75 days, p < 0.001) and higher rates of in-hospital complications and discharges to rehabilitation or intermediate care. Conclusions: This study, being the largest to date, suggests that surgical intervention is associated with a longer LOS and worse short-term outcomes compared to conservative therapy in patients with stable TLJ fractures. While existing literature suggests potential long-term functional benefits of surgery, a consensus is yet to be reached. These findings underscore the importance of careful patient selection when considering surgical intervention for stable TLJ fractures.
477
P544: Efficacy, safety & reliability of single posteror approach for unstable thoracolumbar burst fracture treated with anterior reconstruction and posterior instrumentation
Sharif Ahmed Jonayed 1
1 Dept. of Orthopaedics & Spine Surgery, National Institute of Traumatology & Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Introduction: Management of unstable thoracolumbar burst fracture is still a controversial issue. Fracture morphology, neurologic status, and surgeon preference play major roles in deciding the appropriate approach. Though the combined anterior and posterior instrumentation provides the most stable repair, but optimizing neural decompression & stable internal fixation using a single approach over the least number of spinal segments is the goal. Moreover, the use of both approaches on a trauma patient may increase morbidity. Anterior reconstruction of spine through only one approach can provide an effective outcome. Aims & objectives: The purpose of this study is to evaluate neurological, functional and radiological outcome of the anterior reconstruction of spine by single posterior approach in cases of unstable thoracolumbar burst fractures. Methods: Eighteen patients with acute unstable thoracolumbar burst fractures (T-11 to L-4) with neurological deficit from July 2012 to June 2021 in the age group of 16-60 years with McCormack’s score six or more and thoracolumbar injury severity score (TLISS) five or more were included. Neurological status, visual analogue scale (VAS), angle of kyphotic deformity, McCormack’s score and TLISS score were evaluated. Results: The mean duration of surgery was 255 minutes. The mean blood loss was 440 ml. Mean improvement of ASIA scale was 1.67 in a patient with incomplete spinal injury whereas patient with complete spinal injury remain same at last follow-up. The mean preoperative kyphotic angle was improved from 25 degrees to 5 degrees postoperatively. Visual analogue score improved from 6.1 to 1.7. Conclusions: Single posterior approach is a safe, cost effective and reliable surgical approach for reconstruction of all the columns of spine. It reduces the operative time, blood loss, the morbidity associated with combined approach with a good outcome.
Keywords: anterior reconstruction; posterior approach; unstable; burst fracture; titanium cage
681
P545: Bamboozled: brown sequard in anklosing spondylitis
Michael Dev 1 , Sook Kwan Chan 1 , Manharpreet Singh Sandhu 1 , Rachel Ting 1
1 Orthopaedic Department, Queen Elizabeth Hospital Kota Kinabalu, Kota Kinabalu, Malaysia
Introduction: Spinal cord injury (SCI) in Ankylosing Spondylitis (AS) is more prevalent than in the general population. This is due to the rigid hyperkyphotic deformity as a sequelae ligamentous ossification and syndesmophytosis of AS. We present a case of an incomplete spinal cord injury following a fracture in a patient with axial spondyloarthritis. Materials and Methods: A 48-year-old man, afflicted with AS since the young age of 12 was brought to the emergency department having met with a motor vehicle accident. He was brought in by paramedics fully conscious, hemodynamically unsupported with a vague complaint of lower back pain and right hip pain. Assessment in the casualty department yielded reduced pinprick sensation over his right side and marked weakness over his left lower limb below the level of T9. Results: A chest radiograph showing widened intervertebral disc space between T9 and T10, led to an urgent CT scan and the diagnosis of chalk stick fracture of T9/T10. An MRI was obtained which showed a grade 1 anterolisthesis of T10 over T9, a calcified disc with features suggestive of discal injury as well as abnormal thickening of the posterior longitudinal ligament and ligamentum flavum. He underwent posterior instrumentation and fusion. He had minimal neurological recovery following the operation. Conclusion: It has been reported AS is 11.4 times more likely to develop SCI following trauma [2] with a higher incidence attributed to cervical injury. Our case presents a patient with a fracture at the thoracic level presenting with an incomplete spinal cord injury. One possible reason for the lack of reporting of such cases could be due to the fact that fractures in AS are often under diagnosed or detected late, leading to patients with complete SCI. With a higher index of suspicion the incidence of incomplete SCI following trauma in AS could potentially be more pronounced.
789
P546: Risk factors analysis for predicting vertebral body re-collapses after posterior instrumented fusion in thoracolumbar junction burst fractures
Jlidi Mohamed 1 , Ibrahim Najjar 1 , Walid Bouaicha 1 , Amine Soussou 1 , mouldi lamouchi 1 , Karim Mallek 1 , Mohssen Chamekh 1 , Achref Abdennadher 2 , Selim Daas 1
1 Orthopedics and Traumatology Department, Hospital of Mohamed Taher Maamouri, Nabeul, Tunisia, 2 Orthopedics and Traumatology Department, Military Hospital of Instruction, Tunis, Tunisia
Introduction: In the instrumented posterior fusion for thoracolumbar (T-L) junction compression fractures, early postoperative re-collapse can occur even in the case of a well-reduced vertebral body fracture. Serious complications can be caused by this re-collapse such as loss of reduction, progressive post-traumatic kyphosis, and metal failure, often resulting in indicating secondary revision surgery. Furthermore, this collapse is usually unpredictable owing to the multiplicity of the predisposing factors and the absence of a widely accepted accurate prediction systems. The aim of our study is to evaluate risk factors and predictors for postoperative re-collapse in T-L burst fractures. Material and Methods: It is a retrospective study including patients with T-L junction compression fractures who underwent posterior instrumented fusion. The surgical procedure consisted in short, long or combined segment fusion. The population was divided into two groups: well maintained (G1) and re-collapse (G2) group. Patients were assigned to the re-collapse group if their vertebral body height loss was greater than 20% at any follow-up compared with immediate postoperative results. Results: Our study included 102 patients. We noticed a slight dominance of male gender with a ratio of 1.2. Seventeen (17) patients had diabetes. Re-collapse occurred in 29 of 102 patients (28.43%). In this group, the mean of age was 65 years. The mean of BMI was 27.48; More than 70% of the population had at least a BMI > 25. The age (p = 0.01), and BMI (p = 0.01) were significantly greater than those of the well-maintained group. We also found a significant difference for the type of fixation (p = 0.001). We didn’t find any significant difference between the two groups for age, diabetes, posterior wall recession, intra-canal fragment and pedicle and articular fractures. Multivariate logistic regression analysis identified two independent risk factors: BMI (Ratio odds = 1.44; 95% CI [1.61 - 3.38]) and short segment fixation (Ratio odds = 2.66 ; 95% CI [1.47 - 4.81]). The long segment fixation is a protector factor for re-collapse (Ratio odds = 3.59; 95% CI [1.46 - 8.80]). Laminectomy and bone grafting were not risk factors for re-collapse. Conclusion: The occurrence of re-collapse remains possible but unpredictable no matter the surgical technique used. The type of segment fixation is a crucial parameter to consider. Moreover, obesity is a predisposing factors. Regular and carefull follow-up is a must, inorder to detect and treat complications.
1040
P547: Occult hyperextension AO type B3 injury of thoracic spine
Mukhesh Thangavel 1 , Charanjit Singh Dhillon 1
1 Spine Surgery, MIOT Internation Hospital, Chennai, India
Introduction: Hyperextension thoracic spine injury typically involve the anterior ligament complex of spine. They are often found in spine with previous hyper ossification processes such as ankylosing spondylarthritis (AS) or diffuse idiopathic skeletal hyperostosis (DISH). Sporadic occurrences in healthy spine due to high-energy trauma have been reported. Material and Methods: A 64-year gentleman, known diabetic and hypertensive presented to us after RTA (Stationary 2-wheeler hit by van from behind) post his initial management at nearby hospital. He sustained multiple rib fractures with hemothorax and left distal third humerus fracture. His spine examination was relatively normal expect for a subtle tenderness at the lower dorsal spine. CT thorax picked up D9 anterosuperior vertebral body fracture which turned out to be AO type B3 in MRI with D8 Spinous process involvement and discontinuity of ALL. He was treated with long segment post stabilization D7-D10 and fusion. Results: A follow-up assessment conducted 6 months later revealed no complications stemming from the surgery and X rays showed implants in stable position with evidence of fusion. Conclusion: Hyperextension Thoracic spine injury though rare can occur in high velocity trauma in normal spine. They can be masked by normal neurological presentation, distracting injuries and benign X rays. High index of suspicion and adherence to schematic steps of clinical and radiological evaluation can aid us in not ignoring these three column injuries.
1070
P548: Anterior spinal cord decompression via a posterolateral approach for the treatment of ossification of the posterior longitudinal ligament in the thoracic spine: a prospective cohort study
Satoshi Kato 1 , Noriaki Yokogawa 1 , Takaki Shimizu 1 , Satoshi Nagatani 1 , Masafumi Kawai 1 , Takaaki Uto 1 , Yuji Ishino 1 , Kazuhiro Nanpo 1 , Satoru Demura 1
1 Orthopaedic Surgery, Kanazawa University, Kanazawa, Japan
Introduction: Several surgical procedures have been developed to treat ossification of the posterior longitudinal ligament (OPLL) in the thoracic spine. However, favorable surgical results are not always achieved, and standard protocol and procedure for the surgical treatment of thoracic OPLL have not been established yet. Beak-type OPLL in the thoracic spine is known to be the most complicated in terms of clinical symptoms and surgical management. We developed a novel procedure to remove or float the OPLL in the thoracic spine via a posterolateral approach. This procedure allows the surgeon to perform anterior decompression for thoracic OPLL more safely and effectively than in conventional procedures. In this study, we describe this surgical procedure and report the clinical outcomes according to our surgical strategy for thoracic OPLL. Material and Methods: For a large and localized OPLL, particularly beak-type OPLL, which occupies more than 50% of the spinal canal diameter, the appropriate treatment strategy is anterior decompression using our technique, followed by posterior instrumented fusion. In this technique, with the patient in the prone position, we performed total resection of the posterior elements at the anterior decompression levels. This maneuver includes laminectomies and removal of the transverse processes and pedicles, which allows space creation bilateral to the dural sac and the targeted OPLL for subsequent anterior decompression. The thoracic nerves at the levels of anterior decompression were ligated bilaterally. They were cut and lifted to improve the view of the OPLL and the anterolateral aspect of the dural sac with controlled bleeding. Anterior decompression was then performed postero-laterally using a surgical airtome or ultrasonic bone scalpel. For other types of OPLL, posterior decompression with instrumented fusion is indicated. Between 2011 and 2021, using this strategy, we operated on 40 patients with myelopathy due to thoracic OPLL. Fifteen patients underwent anterior decompression via a posterolateral approach. We prospectively analyzed clinical outcomes over a minimum 2-year follow-up period. Results: The recovery rate, according to the Japanese Orthopedic Association score, was 65% in the anterior decompression group and 52% in the posterior decompression group. In all 15 patients in the anterior decompression group, adequate OPLL removal or floating was achieved without significant complications. Of the 9 patients in the anterior decompression group who had been non-ambulatory preoperatively due to severe myelopathy, all recovered ambulatory status. Of the 8 patients in the posterior decompression group who had been non-ambulatory preoperatively due to severe myelopathy, 2 remained non-ambulatory. Conclusion: Our results in terms of postoperative clinical outcomes for thoracic OPLL were favorable without significant complications. The results indicate that anterior decompression is appropriate for patients with beak-type OPLL, who generally have severe neurological symptoms. Thus, anterior spinal cord decompression using our technique appears to be safe and effective.
1198
P549: Traumatic lumbosacral spondylolisthesis - A rare case with reduction technique
Vishnu Senthil Kumar 1
1 Orthopaedics, Government Royapettah Hospital, Chennai, India
Introduction: Traumatic Spondylolisthesis is a rare injury. This injury results from a complex high-energy mechanism including hyper-extension, hyperflexion and compression stress or tangential force. We Report a case of traumatic lumbar spondylolisthesis, treated using posterior approach with stable 3 column fixation and solid inter-body fusion. Case Report: A 38 year old male, presented with ASIA A paraplegia following a traumatic injury by fall from 8 feet height (from tree). Bladder sensation, Peri-anal sensation and tone was lost. X-ray showed grade-2 spondylolisthesis of L5 over S1. MRI demonstrated traumatic spondylolisthesis with cauda equine syndrome. Patient was posted on emergency basis. Under GA, Posterior approach with exposure of L4, L5 and S1 Pedicles. Complete disruption of bilateral pars inter-articularis, Inter-spinal ligaments and flaval ligaments of L5-S1. L5 annulus disrupted. Pedicle screws were inserted in L4,L5 and S1 pedicles. L5 over S1 was reduced under C-ARM with help of MC Donald spine dissector. Posterior decompression was done, Left L5 nerve root was damaged with Dural thecal sac damage. L5-S1 disc was removed with inter-body fusion. Bone grafting from posterior iliac crest was harvested and added. The procedure lasted 2.5 hrs with intra-operative loss of 500 ml and no intra-operative complications. At 2 yr follow up,lower limb function regained. Bilateral quadriceps was 5/5, left L4 4/5 and L5 3/5. Right L4 and L5 – 5/5. Perianal sensation and Tone regained but bladder function yet to regain. Discussion: Surgical management was the treatment of choice in our case with ASIA –A paraplegia. Literature search revealed cases managed with various approaches. In our case, posterior approach was selected to reduce listhesis with stabilisation and fusion. Posterior approach is safe, easy and rod-pedicle system resulted in perfect reduction and 3 column fixation. Conclusion: Our case is rare, early diagnosis and treatment with posterior stabilisation has provided satisfactory functional outcome.
1484
P550: Spinal injuries due to fall from height are uniquely different
Rishi Kanna 1 , Gnana Prakash T 1 , Ajoy P Shetty 1 , Shanmuganathan Rajasekaran 1
1 Spine Surgery, Ganga Hospital, Coimbatore, India
Introduction: Traumatic spinal injury (TSI) is a significant source of disability and a burden to the healthcare system worldwide. The primary causes of TSI are road traffic accidents and falls. Among these causes, falls from height are unique in their injury mechanism, morphology and severity. Therefore, it is crucial to have a comprehensive understanding of the incidence and detailed epidemiology of TSI resulting from falls from height. Methods: A review of case records of all traumatic spine injury patients treated at a tertiary-level trauma center over a 5-year period (2015-19) was performed. Epidemiological, clinical, and radiological data were analyzed. Results: The incidence of traumatic spine injuries (TSI) from falls was high, with 52.1% (1069/2065) of spine trauma patients affected. The mean age of patients was 44.45 ± 16.76 years, with 74.55% (n = 797) between 21 and 60 years, and 81.67% of patients being male with a male-to-female ratio of 4.5:1. Falls from the workplace were the major cause of injury (35.17%, n = 376), with 49.8% being high-energy falls (> 10ft). The various locations of TSI include the workplace (n = 376), at home (n = 309), from tree (n = 151), into wells (n = 77), and electric poles (n = 57). Patients from lower socio-economic strata accounted for 48.36% (n = 517) of cases. The most common region of spine injury was lumbar spine (48.64%, n = 520), with 25.93% (n = 277) of patients having multiple-level spine injuries. AO type B was the most common type of spine injury (35.43%, 377 patients), with 47.33% (n = 506) of patients having spinal cord injuries and 27.13% (n=290) having associated injuries to other organ systems. The most common associated limb injuries were calcaneum fractures (7.01%, 75 patients) and distal radius fractures (6.17%, 66 patients). Conclusion: Our study indicates clear demographic and epidemiological disparities in TSI resulting from falls from heights as compared to other forms of injury. We have observed a high frequency of workplace injuries and a preponderance of young male patients. These findings suggest a general lack of awareness among the public and policymakers regarding the implementation of effective safety protocols.
Keywords: spine; trauma; spinal injury; spinal cord injury; epidemiology; falls
1556
P551: Should we remove implants after spinal percutaneous fixation? Evaluation of spine mobility
Amal Abayed 1 , Adnene Benammou 1 , Souha Bennour 1 , Seddik Akremi 1 , Mondher Kooli 1 , Mohamed Ben Salah 1
1 Orthopedic Surgery, Faculty of Medicine of Tunis, University of Tunis El Manar, Charles Nicolle’s Hospital, Tunis, Tunisia
Introduction: Posterior stabilization is a reliable procedure for thoracolumbar spine fractures. It tend to restore the spinal anatomy and prevent neurological signs. Spinal implant removal is a considered a safe procedure indicated in case of implant loosening, infection or symptoms. However, studies had shown there is no consensus regarding its benefits on functional results. Material and Methods: A retrospective, descriptive study was conducted in Charles Nicolle’s hospital over a period of 6 years (2017-2022). We included 25 patients with traumatic thoracolumbar fractures without neurological signs treated with posterior stabilization without fusion followed by implant removal with a minimum follow-up period of 6 months. Clinical and radiological outcome were evaluated based on Visual Analog Scale (VAS), Oswestry Disability Index (ODI), Euroquol 5 dimensions (EQ-5D), flexion/extension range of motion (ROM) and Cobb’s angle before and stabilization and after implant removal. Informed consent was obtained from patients before implant removal. Results: A total of 10 men (40%) and 15 women (60%) were included. Mean was 30 years. Predominant injury mechanism was a fall from height. Number of fractured vertebral bodies was 22 single and 3 multiple with predominant level of T10-L2. Fractures were classified according to AO spine with 70% type A and 30% type B. Mean time of removal was of 26 months. Mean follow-up time of 12 months after implant removal. Mean kyphotic deformity was of 15 degrees with a mean number of fixation of 2 segments. Prior to implant removal, patients presented with mild back pain (20%), pedicle screw breakage (4%), wound infection (4%). All patients underwent implant removal successfully, and no severe operation-related complications occurred. Mean VAS was 3-6 preremoval and < 3 on last follow-up. ODI score was of 4 preremoval and 3 on last follow-up. Mean EQ-5D score was of 70% preremoval and 75% on last follow-up. Mean ROM was 4°. Mean Cobb’s angle was 15.66° before stabilization, 11.22° after stabilization and 11.33° at last follow-up. Conclusion: Spinal implant removal is a considered a safe procedure when performed after fracture healing at least at one year postoperatively, and offers the patient good functional results.
1560
P552: Does magnetic resonance imaging predict neurologic deficit in patients with traumatic lower lumbar fractures
Shanmuganathan Rajasekaran 1 , Karthik Ramachandran 1 , Ajoy P Shetty 1 , Rishi Kanna 1 , Sri Vijay Anand KS 1 , Pushpa BT 2
1 Department of Spine Surgery, 2 Department of Radiodiagnosis, Ganga Hospital, Coimbatore, India
Introduction: Although several research studies have analyzed the radiological risk factors for the neurological deficit in thoracolumbar fractures, very few have looked at lower lumbar fractures (LLF). Moreover, the potential utility of MRI in LLF has not been evaluated. The main aim of the study is to understand the role of MRI in predicting neurological deficits in traumatic lower lumbar fractures (LLF) (L3-L5). Methods: This is a retrospective cohort study. One hundred and eight patients operated for traumatic LLF between January 2010 to January 2020 were reviewed to obtain demographic details, level of injury, and neurology at the time of presentation (American Spinal Injury Association [ASIA] grade). Preoperative computed tomography (CT) scans were used to measure parameters like anterior vertebral body height (AVBH), posterior vertebral body height (PVBH), loss of vertebral body height (LOVH), local kyphosis (LK), retropulsion of fracture fragment (RFF), interpedicular distance (IPD), canal compromise (CC), sagittal transverse ratio (STR), presence of vertical lamina fracture. Magnetic resonance imaging was used to measure the canal encroachment ratio (CER), the cross-sectional area of thecal sac (CSAT), and the presence of epidural hematoma. Results: Among 108 patients, 9 (8.3%) had ASIA A, 4 (3.7%) had ASIA B, 17 (15.7%) had ASIA C, 21(19.4%) had ASIA D and 57 (52.9%) had ASIA E neurology at the time of admission. On multivariate logistic regression analysis, TLICS score (p = 0.000), CER (p = 0.050), and CSAT (p = 0.019) were found to be variables independently associated with neurological deficits. ROC curve analyses showed that only CER (AUC 0.926, CI 0.860 - 0.968) and CSAT (AUC 0.963, CI 0.908 - 0.990) had good discriminatory ability and the optimal cut-off value for CER was 50% and for CSAT was 65.3 mm2. Conclusion: Based on the results of the study, canal encroachment ratio (CER) > 50% and cross-sectional area of thecal sac (CSAT) > 65.3 mm2 can be used as an optimal cut-off value to predict the incidence of neurological deficit in LLF.
1654
P553: Technical solutions that influence clinically significant instrumentation failure in patients with traumatic injuries of the lumbar spine and thoracolumbar junction
Andrey Bokov 1 , Ivan Brattsev 1 , Svetlana Kalinina 1
1 Neurosurgical, Federal Budgetary Institution Privolzhskiy Medical Research University, Nizhniy Novgorod, Russian Federation
Introduction: Pedicle screw loosening is the most frequently accoutered complication after spinal nstrumentations on the other hand a considerable number of those cases remain asymptomatic. The objective of this study is to determine factors that influence the rate of clinically significant instrumentation failure in patients with traumatic injuries of a lumbar spine and thoracolumbar junction. Materials and Methods: This is a retrospective evaluation of 204 spinal instrumentations performed in cases of traumatic injuries of lumbar spine and thoracolumbar junction. Patients with A3, A4 and B2 injuries were selected for this study. Preoperatively patients underwent CT examination and bone radiodensity was measured in Hounsfield units (HU) at standard level of L3. Pedicle screws fixation was used either as a stand-alone technique or in combination with anterior interbody fusion. In cases with posttraumatic spinal stenosis a either anterior or posterior decompression of nerve roots and spinal cord were performed. Cases with implant malposition were excluded from this study. The duration of follow up was 24 months. Cases with screws loosening, were registered and general discriminant analysis was used to assess the relationship between clinically significant complication rate and potential contributing factors. Results: Even though the number of patients with bone density below 110 HU accounted for 63 (30,9%), the given factor turned out insignificant. The most contributing factors were related to technical solutions used. While anterior column reconstruction and intermediate fixation resulted in a decline in clinically significant pedicle screw loosening, the extensive decompression with total facet joint and lamina resection was associated with a rise in complication rate. Anterior decompression was not associated with risk of instrumentation failure. Either partial or total posterior fusion on instrumented levels resulted in a decrease in clinically significant instrumentation failure rate. The parameters of discriminant model for complication rate were: F = 8.6966, p < 0.0001, r = 0.6108, Eigen value = 0.5950 Wilkes λ = 0.6169, χ2 = 91.277. Regression coefficients for significant components of the model: B0=0,5679, p=0,0008; B1(for partial or total posterior fusion)= -0 < 1684, p = 0.0006, B2 (anterior reconstruction) = -0.0780, p = 0.0040; B3(extensive posterior decompression) = 0.1194, p = 0.0003; B4 (intermediate fixation) = -0.1262, p = 0.0025 Classification of cases - 89.7% correctly predicted with sensitivity and specificity accounted for 63.0% and 93.8% respectively. Conclusion: Bone quality is significant contributing factor for implant stability however the result of current study demonstrate that surgical solutions are capable to reduce its significance. The necessity of excessive posterior decompression should be assessed thoroughly in patients with poor bone quality while anterior decompression does not have negative impact on long term instrumentation stability. Patients who are at risk of implant related complications may benefit from anterior reconstruction and intermediate fixation by getting load on pedicle screws decreased. Additional posterior fusion may also contribute to long term stability of spinal instrumentation.
1673
P554: Procedural complications and implant failures of percutaneous stent-kyphoplasty: a retrospective analysis of 226 implants from a Level-1 Trauma center in Switzerland
Julian Scherer 1,2 , Magdalena Karner 1 , Osterhoff Georg 3 , Kai Sprengel 1,4 , Hans Christoph Pape 1
1 Traumatology, University Hospital of Zurich, Zurich, Switzerland
2 University of Cape Town, Cape Town, South Africa
3 Department of Orthopaedics, Trauma Surgery and Plastic Surgery, University Hospital of Leipzig, Leipzig, Germany
4 University of Lucerne, Hirslanden Clinic St. Anna, Lucerne, Switzerland
Introduction: Implant failures in spinal fixations and fusions are uncommon complications with significant potential for morbidity and neurological or vascular damage. Implant failure can either result from fracture of the implant`s parts itself or secondary due to patient factors such as osteoporosis (cut-out). A common implant failure of conventional balloon-kyphoplasty is a fracture of the endplate (cut-out) while inflating the balloon during height restoration. This can lead to fractures of adjacent vertebras and intervertebral disc disturbance. The relatively new SpineJack®-system has been advocated as a safe alternative to the balloon kyphoplasty in thoracolumbar fractures. However, little is known about procedural implant failures. Thus, the aim of this study was to assess implant-related complications, especially focusing on intraoperative cut-out of the vertebral endplate. Material and Methods: All patients with vertebral fractures who were treated with a stand-alone SpineJack®-system from November 2014 to December 2022 were assessed. In total, 226 implants were analyzed. Demographics, fracture characteristics (AOSpine and OF-classification) as well as intraoperative complications were analyzed. Sub-group analysis was performed for traumatic VCFs vs. osteoporotic vertebral fractures (OVFs) as well as patients` age. Results: The mean age of the assessed cohort was 64.76 years (range 19 to 93, SD 16.89) with a male majority of 53.1%. Most of the assessed fractures were OVFs (57.1%, n = 129), followed by VCFs (33.2%, n = 75) and malignant fractures (9.8%, n = 22). The mean age of the OVF group was 74.30 years, (SD 10.44) versus VCF group 48.75 years, (SD 15.26) (p ≤ 0.001). Most of the fractures occurred in the lumbar region (63.24%) with no difference between OVFs and VCFs (p = 0.634). Most of the VCFs were classified as A3 (45.3%) followed by A1 (33.3%), A4 (14.7%) and A2 (6.7). The most frequently recorded OVFs were OF 2 (38.8%), followed by OF 4 (32.6%), OF 3 (24.8%), OF 1 (2.3%) and OF 5 (1.6%). In total, we recorded two intraoperative bleedings (0.9%) which both occurred in the OVF group. There were no technical complications (e.g., expansion failure of the SpineJack®-system) and no conversion to a different procedure assessed in this cohort. Intraoperative cement leakage was found in 18 cases (8.8%) with no difference between the assessed groups (10.0% OVF versus 6.66% VCF, p = 0.408). Intraoperative cutout of the SpineJack®-system was observed in 16 cases (7.8%) with no difference between OVF (10.0%) and VCF (4%) (p = 0.120). Most of the cutouts occurred in the thoracal region (11.63% versus 5.1%, p = 0.086). There was no correlation between intraoperative cement leakage and implant cutout (p = 0.591, Pearson = 0.038). Significantly more cutouts occurred in the OF 4 classified OVFs (p = 0.004) and there was no difference in between the AO classification (p = 0.273). Conclusion: The SpineJack®-system as a stand-alone procedure seems to be a safe operational option in thoracolumbar fractures with low complication rates in both, high-energy and osteoporotic vertebral fractures. Cutouts seemed to occur more frequently in more severe osteoporotic fractures. Further studies should assess the long-term outcomes of patients treated with the SpineJack®-system with intra-operative complications.
1746
P555: Short-segment fixation in AO type B and C thoracolumbar spine fractures without neurological deficit: Clinical and imaging follow-up
Carolina Meneses 1 , Felipe Espinosa 1 , Giovanni Canessa 1 , Guillermo Izquierdo 1 , Oscar Bravo 1
1 Servicio de Traumatología, Equipo de Columna, Hospital Clínico Mutual de Seguridad, Santiago, Chile
Introduction: The thoracolumbar segment (T10-L2) is the most injured segment in patients with spinal fractures (up to 20%). Surgical management is indicated if there is instability or neurological impairment, to achieve medullary decompression, stability, early rehabilitation, and adequate pain management. Length of the fixation varies according to type and lesion level, instrumentation type, and surgeon's preferences and training. Short-segment fixations (1 or 2 levels) present less bleeding, shorter surgical time, lower costs, and motion preservation of adjacent healthy spinal levels. Long-segment fixations (3 or more levels) are better in preventing postoperative deformities. It is important to consider the expected activities that the patient will achieve post rehabilitation, because it defines the axial load over the fixation and won't be the same in paraplegic patients and patients that recover previous activities. Nowadays, it is still a matter of debate whether short-segment fixations are sufficient to achieve the required objectives in this type of injury. Material and Methods: This is a retrospective descriptive study, where the information was extracted from clinical data from 2020 to 2022 in a level 1 trauma center in Santiago, Chile. The patient selected, had thoracolumbar distraction and translation injuries (type B and C from the AO Spine Thoracolumbar Injury Classification System) undergoing open monosegmental fixation (USS Schanz) by the same surgical team, and had complete clinical and imaging follow-up up to one year. We excluded patients with neurologic deficit and less than 1 year of follow-up. We analyzed demographic variables, level and type of fracture, time between injury to surgery, and postoperative complications. Imaging was assessed to determine the anterior vertebral body compression percentage, regional kyphosis by Cobb's angle, and the progression during the follow-up. Results: We included seven patients, six of them were male, the mean age was 35 years old. Four were type B2 fractures and three were type C. 57,1% of the injuries were located at the T11-T12 segment, followed by L1-L2 (28.7%). The average surgical time was 1,5 hours and intraoperative bleeding was 200 mL. Immediate postoperative radiograph showed an average regional kyphosis of 8,6° and an average anterior vertebral body compression percentage of 4.2%. At one year follow-up, we observed an average of regional kyphosis of 16.9°, with no perioperative complications or need of a new surgical intervention. These results are comparable to other international case series. Conclusion: Monosegmental fixation is a valid alternative to manage type B and C thoracolumbar fractures in patients that return to previous activities, with acceptable clinical and radiological outcomes. Comparative studies are needed to determine that short fixation is as effective as traditional long-segment fixation surgery in non-paraplegic patients.
1847
P556: Comparative analysis of open and minimally invasive approaches in thoracolumbar fracture management
Benjeddou Wassim 1 , Khalil Habboubi 1 , Safouen Ben Brahim 1 , Meddeb Mehdi 1 , Hassen Makhlouf 1 , Mondher Mestiri 1
1 Adults, Med Taieb Kassab Institute, Mannouba, Tunisia
Introduction: Vertebral fractures account for 17% of hospital discharges from the Emergency unit and orthopedic department at our hospital. Among these, 40% involve injuries to the thoracic and lumbar segments, with approximately half necessitating surgical intervention. Since 2019, our institute has regularly performed surgeries using minimally invasive techniques, including mini-open approaches and percutaneous procedures, as an extension of our prior experience in treating thoracolumbar spine fractures. Material and Methods: This retrospective study comprises a case series of adult patients who sustained fractures in the thoracic and/or lumbar segments and received surgical treatment via a posterior approach, including traditional open, mini-open, or percutaneous procedures. All patients were treated at Kassab Institute, Tunisa between January 2019 and December 2022. Osteoporotic and pathological bone fractures were excluded. Data were collected from electronic clinical records and neuroimaging records. The MAGERL thoracolumbar fracture classification was used to categorize all CT scans. Statistical analysis was conducted using IBM SPSS Statistics. Results: 29 cases were included in the analysis, with 63% being male and 37% female. The average age was 53.2 years (SD 17-81). Falls (42.3%) and traffic accidents (36%) were the most common mechanisms of injury. The most frequent fracture types were A3, B1, and C. The thoraco-lumbar hinge (65%) was the most frequently affected segment, followed by thoracic injuries (30%). Most patients presented with ASIA E (85%), while 4% were ASIA D and 12% ASIA A. Surgical techniques included open surgery in 47.4% of cases, less invasive techniques (mini-open or MIS) in 52.6%, and one hybrid case. The mean time from injury to surgery was 4.0 days (SD: 0 - 16), with no differences between groups. The open surgery group experienced longer hospital stays and more postoperative days. Additionally, this group had a greater average number of levels operated on and a higher average number of screws used per surgery. Surgical time and intraoperative blood loss were also higher in the open surgery group. Post-surgical complications and the need for reoperation were observed exclusively in the open surgery group. No significant differences were found between the two groups regarding post-surgery angulation and decreased vertebral body height. Conclusion: Minimally invasive techniques for thoracolumbar fracture management offer a safe and effective alternative to open surgery. These approaches provide advantages such as reduced hospitalization times, lower intraoperative blood loss, and decreased postoperative pain, facilitating early rehabilitation. They are particularly beneficial in polytraumatized patients and for damage control surgery, making them a viable option for a wide range of traumatic spinal injuries.
1895
P557: A quarter of elderly patients in major trauma centres die in 30 days of admission: a 5-year retrospective study
Zion Hwang 1,2,3 , Tesfaladet Kurban 1 , Emily Tsang 1 , Priyanshu Saha 4 , Bisola Ajayi 1 , Jack Williams 4 , Paavan Shah 4 , Reina Sng 4 , Rhys Owen 4 , Jason Bernard 1 , Timothy Bishop 1 , Darren Lui 1
1 St. George's University Hospital, London, United Kingdom
2 Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust, United Kingdom
3 University of Sheffield, United Kingdom
4 St. George's University of London, London, United Kingdom
Introduction: Acute spinal injuries and major trauma orthopaedic admissions and their appropriate management in the aging population pose significant challenges to healthcare systems. In these patients, high energy injuries and polytrauma with spinal fractures further confound surgical decision-making. Material and Methods: We reviewed all trauma patients admitted to a level 1 major trauma centre between 2018 and 2022 via electronic patient database. From this dataset we identified patients with spinal injuries, their demographics and the characteristics of the trauma. Results: A total of 357 patients aged > 65 years with spine trauma were identified, making up 41.5% (357/860) of all traumatic spinal injuries over the 5-year period. Out of the 357 patients, 160 (44.8%) were female, 213 (59.7%) had polytrauma, 147 (41.2%) had head injuries, 180 (50.4%) had chest injuries, 44 (12.3%) had abdominal injuries, 80 (22.4%) had peripheral limb, and 84 (23.5%) patients were admitted to ITU. 24.0% (86/357) of these patients resulted in mortality by 30-days post-admission. Of those, 70.9% (61/86) had polytrauma and 94.2% (81/86) were managed conservatively. Conclusion: Major trauma involving spinal injuries are less common in the elderly population yet result in higher mortality rates compared to their younger counterparts. Almost a quarter of elderly patients admitted to level 1 trauma centres with acute spinal injuries and polytrauma result in mortality.
1931
P558: Evaluation of AO Spine-DGOU osteoporotic fracture classification system in a major trauma centre
Zion Hwang 1,2,3 , Mak Macapagal 4 , Reina Sng 4 , Emily Tsang 3 , Tesfaladet Kurban 3 , Bisola Ajayi 3 , Priyanshu Saha 4 , Jason Bernard 3 , Timothy Bishop 3 , Darren Lui 3
1 Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust, United Kingdom
2 University of Sheffield, United Kingdom
3 St. George's University Hospital, London, United Kingdom
4 St. George's University of London, United Kingdom
Introduction: The AO Spine-DGOU Osteoporotic Fracture Classification System was established to develop a specific system for Osteoporotic Fractures which utilises radiological (CT/MRI) imaging to inform surgical assessment and management. However, a wide-scale validation of this classification system is yet unpublished and a recent evaluation study reported poor intra- and inter- observer agreement. So, we conducted a retrospective audit to assess the pragmatic application of the novel classification system in a level 1 major trauma centre. In the United Kingdom, trauma centres work as part of a “spoke and hub” network, where all high energy injuries are diverted from “spoke” (district general hospitals) to “hub” (level 1 major trauma centre). Material and Methods: We identified all patients > 65 with suspected Osteoporotic Fragility Fractures over a 4-year period and retrospectively graded their CT/MRI guided by the AO-DGOU classification system. Patients without accessible images were excluded from this audit. We then reviewed patient notes to assess the other parameters in the guidelines and used the cumulative score to assess whether management was concordant to the new AO-DGOU classification. Results: A total of 312 trauma patients were identified to have osteoporotic spine fractures. Of those, 125 (40%) were female and the mean age was 78 years. 207 (66%) presented with polytrauma, including 143 (46%) head, 160 (51%) thorax, 45 (14%) abdomen, and 83 (27%) limb injuries. 91 (29%) were admitted to ITU. The distribution of fracture morphology was 91 (29%) OF1, 93 (30%) OF2, 35 (11%) OF3, 32 (10%) OF4, 17 (5%) OF5 and 43 (14%) unknown/indeterminate. Spinal deformity progressed (score +1) in 7 (2%) patients, did not progress (score -1) in 65 (21%), and was not documented in 223 (71%). 18 (6%) patients scored +1 for pain under analgesia VAS > 5, 158 (51%) scored -1 for VAS < 5, and this was unrecorded in 136 (44%). Neurological deficit was present (score +2) in 21 (7%). Mobilisation was achieved under anaesthesia (score -1) for 40.0% (43/108), not achieved (score +1) in 47 (15%), and not tested/not recorded in 107 (34%) of patients. 170 (54%) patients did not meet the criteria for negative scoring on health status assessment, 94 (30%) patients scored -1, and 11 (4%) patients scored -2. 0% had any mention of osteoporotic severity on the hospital system. Patients scored 3.6 on average. 11% patients did not receive management concordant with AO-DGOU guidelines: 3% due to patient death, 2% due to comorbid factors, and 6% reason unclear. Furthermore, 10% did not receive surgery when it would have been beneficial. Conclusion: Pragmatic evaluation of this classification is flawed as osteoporotic severity was not assessed, nor were Hounsfield units. This highlights the need for standardised assessment of these variables and wider accessibility to aids to guide this. The high percentage of unrecorded variables draws attention to which important variables are often overlooked by clinicians’ assessments of elderly trauma patients with potential osteoporotic spine fractures. Despite this, the authors note that the majority of osteoporotic spinal injuries were treated concordantly to classification.
1937
P559: Comparison of short-term outcomes of percutaneous vertebral augmentation with and without posterior spinal fusions in patients with vertebral compression fractures
Bongseok Jung 1 , Junho Song 1 , Justin Han 1 , Austen Katz 1 , David Essig 1
1 Department of Orthopaedic Surgery, Northwell Health, Manhasset, USA
Introduction: Prior studies have demonstrated the combination of posterior pedicle spinal fusions (PPSF) with percutaneous kyphoplasty/vertebroplasty (PK/PV) as a potentially superior long-term alternative to augmentation alone especially in cases of very severe and complicated compression fractures. There is however a lack of evidence comparing the short-term effectiveness of vertebral augmentation with or without posterior fusions. Material and Methods: A retrospective analysis was performed on all patients in the ACS-NSQIP database between 2011-2016 that underwent PK or PV. Patients were stratified based on CPT codes, and exclusion criteria included any other spinal procedures, add-on spinal fusions, < 18 years old, and missing data. Univariate regression was performed to evaluate for significant association with primary outcomes, and along with significant variables in baseline differences were analyzed as independent predictors using multivariate regression. Significant outcomes (p < 0.05) were subject to backward elimination regression models and adjusted for baseline differences. Results from the multivariate regression were reported as odds ratio with 95% confidence intervals (OR ± 95% CI). Results: A total of 3104 patients were assessed (2994 PK/PV without PPSF vs 110 having PK/VP with PPSF). PK/VP without PPSF were significantly older (69.7% vs 60.9%, p = 0.048). 5 out of 20 comorbidities showed significant differences between groups including BMI (26.6 vs 28.0, p = 0.015), smoking status (12.8% vs 20.9%, p = 0.013), disseminated cancer (6% vs 20%, p < 0.001), and preoperative WBC (7.7 vs 8.6, p = 0.0047) and platelet (243.9 vs 266.7, p = 0.007) levels. Operative time was greater in the group with concurrent PPSF than without (256.8 vs 38.7, p < 0.000), which was similar in the case of length of stay in the hospital (8.75 vs 2.98, p < 0.001). Primary outcomes revealed no significant differences in 30-day readmission and reoperation between the two groups. Morbidity was higher in patients that underwent concurrent PPSF than without (7.3% vs 3.1%, p = 0.014). In multivariate regression, neither PK/VP with nor without PPSF were independent predictors of 30-day outcomes. Conclusion: This study demonstrated that vertebral augmentation with PPSF is associated with significant comorbidities, longer OR time and length of hospital stay post-operatively compared to augmentation without PPSF. There may however be no differences in primary short-term outcomes between these procedures when accounting for significant baseline differences. Future studies should therefore aim to evaluate the viability of conjunctive PPSF with PK/PV over a long period of time, controlling for patient characteristics.
2219
P560: Monoaxial pedicle screws and a novel percutaneous reduction device significantly keep the vertebral body angle after surgery
Okuda Akinori 1,2 , Keisuke Masuda 1,2 , Hironobu Konishi 1,2 , Kenichi Nakano 1,2 , Naoki Maegawa 1,2 , Hideki Shigematsu 2 , Hidetada Fukushima 1
1 Emergency and Critical Care Medicine
2 Orthopedic Surgery, Nara Medical University, Kashihara, Japan
Introduction: Although monomaxial screws (MoAS) are effective for good vertebral body reduction in spinal trauma, precise rod placement is difficult under the fascia in percutaneous surgery. We have been performing percutaneous vertebral body reduction and fixation using a Sagittal adjusting screw (SAS) with a uniplanar screw head and a percutaneous vertebral body reduction device. This screw can be used like a MoAS during reduction and has angular acceptability in the sagittal plane at the time of rod placement, but due to its characteristics, postoperative loss of correction in the sagittal plane is a concern. Materials and Methods: A new percutaneous vertebral body reduction device, MoAS, and a three-dimensional rod bender were introduced for thoracolumbar spine injuries, and a comparison with SAS was made. Of the 193 cases of thoracolumbar spine injuries with 213 vertebrae that underwent surgical treatment at our center from June 2016 to September 2022, 35 cases with injuries from the 11th thoracic spine to the 3rd lumbar spine under 65 years of age that were fixed with above1-below1 and followed for at least 6 months were included. SAS was used from June 2016 to December 2018, and MoAS was used from January 2019 to September 2022. The SAS group was the S group and the MoAS group was the M group, and The two groups were compared with respect to age, gender, load sharing classification (LSC), operative time, blood loss, postoperative correction loss (injured vertebral body angle(VBA), superoinferior adjacent endplate angle of above1 - below1(SIEA: sagittal Cobb angle between adjacent vertebrae above1 and below1 of injured vertebra), and change in postoperative spinal canal composition (ΔCC). Results: The mean age was 45.8 years, 17 males and 18 females, mean observation period of 18 months, 14 patients in group S and 21 patients in group M. There were no significant differences between the two groups (group S and M) in age (47.7, 44.4), sex, LSC (5.5, 5.1), bleeding volume (22.1 g, 40.8 g), SIEA (8.5 degrees, 5.0 degrees, p = 0.1), ΔCC (15.4%, 15%), but there were significant differences in operative time (109 minutes,83 minutes, p < 0.01) and VBA (6.7 degrees, 2.1 degrees, p < 0.01). Conclusion: Percutaneous vertebral body reduction and fixation with the new percutaneous vertebral body reduction device, three-dimensional rod benders and MoAS is equal to SAS in reduction of injured vertebral body, and more effective than SAS in preserving postoperative VBA for thoracolumbar spine injuries because it has a significantly lower postoperative loss of correction of VBA compared to SAS.
2258
P561: Assessment of intervertebral disc lesions among thoracolumbar high-energy and fragility fractures treated with percutaneous stent-kyphoplasty: a retrospective analysis of 204 fractures
Julian Scherer 1,2 , Magdalena Karner 1 , Osterhoff Georg 3 , Kai Sprengel 1,4 , Hans Christoph Pape 1
1 Traumatology, University Hospital of Zurich, Zurich, Switzerland
2 University of Cape Town, Cape Town, South Africa
3 Department of Orthopaedics, Trauma Surgery and Plastic Surger,University Hospital of Leipzig, Leipzig, Germany
4 University of Lucerne, Hirslanden Clinic St. Anna, Lucerne, Switzerland
Introduction: Traumatic vertebral compression fractures (tVCFs) and osteoporotic vertebral fractures (OVFs) are common injuries to the spinal column. Concomitant intervertebral disc lesions are believed to increase the risk for early degeneration in these patients. However, little is known about the incidence and severity of disc injuries in these fractures. Thus, the aim of this study was to assess the frequency of sustained concomitant disc injuries in the above fractures and to correlate severity with fracture severity. Material and Methods: All patients with vertebral fractures who were treated with the SpineJack®-system and underwent preoperative MR-imaging from November 2014 to December 2022 were assessed. In total, 408 intervertebral discs (204 superior and 204 inferior; 204 fractures) were analyzed. Demographics, fracture characteristics (AOSpine A1-4 and OF-classification) as well as adjacent disc injury severity according to Sander et al. based on MR-imaging were analyzed. To assess differences in disc injury severity (ordinal data) between groups (nominal data) the Mann-Whitney-U test was used. Correlation analysis between ordinal and ordinal data was performed using Spearman`s correlation coefficient (ρ) whereas to assess correlation between ordinal and nominal data, Pearson`s correlation was used. Results: The mean age of the assessed cohort was 63.1 years (SD 17.2) (50.5% female) with a significantly higher mean age in OVFs (p ≤ 0.001). Of all assessed fractures (58.3% OVFs), 139 had an injury to the superior adjacent disc (68.1%) and 119 (58.3%) to the inferior adjacent disc. Amongst all assessed discs (n = 408), 150 (36.8%) were not injured (grade 0), 72 (17.6%) had an edema (grade 1), 106 (30.0%) had an intradiscal tear (grade 2) and 80 (19.6%) showed an infraction into vertebral body/annular tear (grade 3). Significantly more superior disc injuries were assessed in OVFs (73.9% vs. 60.0%; p = 0.047). Injury to both discs were observed in 110 fractures (53.9%) with no difference between sex (p = 0.486) and OVFs vs. tVCFs (p = 0.200). Amongst all assessed discs, we assessed a positive correlation between inferior disc injury severity and neurology at admission (pearson 0.142, p = 0.041). No correlation between superior disc injury (pearson -0.056, p = 0.430) but a negative correlation between inferior disc injury and intraoperative cement leakage was assessed amongst all fractures (pearson -0.170, p = 0.015). Inferior discs were more severely injured in OVFs (p = 0.012) whereas no difference in superior disc injuries between the groups was assessed. (p = 0.059). There was no correlation between OF-classification and superior disc injury severity (ρ = -0.024, p = 0.798) as well as inferior disc injury severity (ρ = 0.93, p = 0.314). We assessed a positive correlation between AOSpine-classification and inferior disc injury severity (ρ = 0.248, p = 0.023) but no correlation was found with superior disc injury severity (ρ = 0.129, p = 0.240). Conclusion: Intervertebral disc injuries in tVCFs and OVFs are common concomitant injuries with a higher incidence of superior disc injuries in OVFs. Inferior disc injury seems to be associated with less cement leakage but more neurological symptoms. The OVF severity has no influence on disc injury severity, whereas more severely tVCFs are associated with more severe inferior disc injuries. Further studies should assess the clinical long-term outcome of patients with concomitant intervertebral disc injury.
2436
P562: Investigation of facet fusions after surgery for thoracolumbar vertebral fractures: more than half of cases had spontaneous facet fusions
Ryo Sasaki 1
1 Orthopedics, Osaka Saiseikai Nakatsu Hospital, Japan
Introduction: Some reports showed percutaneous spinal fixation without bone grafting provided spontaneous facet fusion in some patients. However, few reports have mentioned spontaneous facet fusion after surgery for thoracolumbar vertebral body fractures. The purpose of this study is to evaluate spontaneous facet fusion after surgery for thoracolumbar vertebral body fractures and investigate the predictors of spontaneous facet fusion. Material and Methods: We retrospectively reviewed 36 patients who were undergone surgery without bone grafting for thoracolumbar vertebral body fractures and evaluated facet fusion with Computed Tomography at 1 year after surgery. 23 patients were diagnosed as osteoporotic vertebral fractures. We used three surgical procedures: (1) balloon kyphoplasty (8 patients), (2) percutaneous posterior fixation (22 patients), (3) lateral approach corpectomy and percutaneous posterior fixation (6 patients). We investigated level of facet fusion and measured the preoperative and postoperative local kyphotic angle of a fractured vertebra. Results: 21 patients (58%) had at least single-level facet fusion (F group) and 15 patients (42%) had no facet fusion (C group). Level of facet fusion was adjacent to a fractured vertebra in all patients. 13 patients had facet fusion at only cranial side of a fractured vertebra, 2 patients had facet fusion at only caudal side of a fractured vertebra, and 6 patients had facet fusion at both cranial and caudal side of a fractured vertebra. Preoperative local kyphotic angle was 7.7° in F group and 4.4° in C group (p = 0.11), and Postoperative local kyphotic angle was 9.8° in F group and 2.8° in C group (p = 0.03). There were no significant differences in age, gender, the prevalence of osteoporosis, level of fractured vertebra, and surgical procedures between two groups. Conclusion: 58% of patients who were undergone surgery without bone grafting for thoracolumbar vertebral body fractures had spontaneous facet fusion at 1 year after surgery. 90% of the patients had facet fusion at cranial side of a fractured vertebra. The predictor of spontaneous facet fusion was large postoperative local kyphotic angle. This tendency was observed regardless of the surgical methods. In the future, we will investigate whether this tendency is observed in patients who are treated conservatively.
2462
P563: Risk factors of subsequent vertebral fractures in patients with compression fracture and intravertebral vacuum cleft treated by percutaneous vertebroplasty
Kwan Ho Park 1 , Tae Wan Kim 1
1 Neurosurgery, VHS Medical Center, Seoul, South Korea
Objective: We evaluated the risk factors of subsequent vertebral fractures after vertebroplasty for vertebral compression fractures (VCFs) with intravertebral vacuum cleft (IVC). Materials and Methods: We retrospectively reviewed the medical data of 31 patients treated by vertebroplasty. 31 patients (17 male, 14 female) with a total of 36 levels were treated. Mean age was 73.3 years (range, 60-88 years). We evaluated BMD, level of fracture, type of fracture, amount of deformity, fracture of posterior cortex, and endplate fractures. Results: Mean follow-up was 12 months (range, 5-22 months). Mean BMD was -3.1. The level of fracture was T11-L2 in 27 levels, L3-5 in 4 and T6-10 in 5. The type of fracture was wedge in 29 levels, biconcave in 5 and crush in 2. The amount of deformity was mild in 29 levels and moderate in 4 and severe in 3. Five of 31 patients with VCFs and IVC showed subsequent vertebral fractures after vertebroplasty. 4 refractures, 1 adjacent fracture, and no remote fracture were obtained. The history of previous vertebral fracture was in 1 patient. All 5 patients had mild vertebral fractures. Fracture of posterior vertebral cortex and endplate fracture in 3. Conclusions: Subsequent fractures could be developed in patients with mild vertebral fracture, fractures of posterior vertebral cortex and endplate. Refracture was most common subsequent fracture. Careful vertebroplasty and long-term follow-up is required.
Trauma – other
968
P564: Spine fractures in the frame of Thom's mathematical theory of catastrophe
Nery Lamothe 1 , Mara Lamothe 1 , Alejandro Alonso-Altamirano 1 , Daniel Lamothe 2 , Jesus Hernandez-Coria 3 , Francisco Castillo 4 , Hugo Contreras-Blancas 5 , Pedro Mojica-Guerrero 3,5 , Armando Martinez-Aguilar 3 , Eber Martinez-Joffre 3 , Anna De la Pena 2 , Jose Talavera-Martinez 3 , Victor Renteria-Ferruzca 3 , Sharla Rivera-Baena 3 , Alejandro Bayo del Castillo 3 , Victor Perez-Aguilar 3 , Hair Galan-Rosalio 3
1 Division de Ciencias Biologicas y de la Salud, Universidad Autonoma Metropolitana, Mexico City, Mexico
2 Internal Medicine, Jersey City Medical Center, New Jersey, USA
3 Orthopedics, Hospital General de Xoco, Mexico City, Mexico
4 Foot and Ankle Fellow, Prince of Wales Hospital, Sydney, Australia
5 Orthopedics, Hospital Angeles Mocel, Mexico City, Mexico
Introduction: The physical properties orthopedists encounter are force, momentum, pressure, torque, energy, and power; all these, constitute compound physical properties, such that, it is essential to comprehend the fundamental units, of which they are a combination. This work constitutes the apodictic research of the unit transformations and electromagnetic interactions of atoms, that generated the catastrophic event of fracture. Material and Methods: The methods used are, exclusively, the apodictic inferences within the frame of the mathematical theory of communication of Shannon, from the conversion of fundamental units of physics to the effects in the bone, which is our object of analysis. A matter of differential and integral calculus. Results: We investigate the true mechanism of the fracture since they are, the result of a mathematical catastrophe of Thom: sudden transition of the contiguous bone cortical layer, and an infinitesimal instant later, the cortical breaks. This catastrophic event is modeled with the hyperbole equation y = a(x-b)/(x-b). Precisely at point x = b, is the catastrophic change, from continuous corticals to broken corticals. The hyperbole before point x = b represents continuous cortical, and the hyperbole after x = b is the bone after the cortical has been broken. What breaks a bone not only depends on the force exerted on it but also on the area on which it is applied and the duration of it. It is not the same to have a 3,000 Newtons force required to fracture a vertebra, distributed along all the vertebra, over one minute, rather than the same force, occurring during one second, applied to a tiny area of the vertebra. In both cases, it is the same force applied to the bone, but what changes it is the area and time the force is being applied! Force breaking bones is applied in an infinitesimal area of bone, which is pressure. Force is also applied during an infinitesimal time. So, what generates the fracture, is the derivative of pressure (force/area) relative to time. Multiplying pressure units N/m2 by (m/m), units will be Nm/m3 or Joul units (J) divided by volume; which is energy per volume. As such, the force applied to an area of bone, is energy distributed over bone volume or energy density. The fracture is produced, because of the change in pressure during an infinitesimal period. The derivative of pressure, in energy per volume units, relative to time, is what breaks the bone. This energy corresponds to the kinetic energy of the object, exerting force on the bone. KE = (1/2) mv2. Energy per volume units J/m3, multiplied by (1/seg)/(1/seg), correspond to power(J/seg) per flux units (m3/seg). This flux is the amount of the object getting inside the first atomic layer of atoms of the bone cortical, during the precise moment of the fracture. Conclusion: Fracture is not only dependent on the force exerted on bone but also on the time and area in which the force is applied. The fracture threshold, is the derivative of the pressure relative to time, energy density, or Power per flux, in differential calculus terms.
1512
P565: Validation of the AO Spine CROST (Clinician Reported Outcome Spine Trauma) in the clinical setting
Said Sadiqi 1 , Sander Muijs 1 , Erin E.A. de Gendt 1 , Marcel Post 2 , Cumhur Oner 1
1 Department of Orthopaedics, University Medical Center Utrecht, Utrecht, The Netherlands
2 De Hoogstraat Rehabilitation, Utrecht, The Netherlands
Introduction: There may be discrepancies when comparing patients’ perspective with clinicians’ perspective on what is considered as a good outcome of a specific treatment. Next to a patient reported outcome measure, there is also need for a simple, reliable and quick to administer tool that is completed by the treating surgeons and reflects their perspectives adequately. Consisting of the most relevant clinical and radiological assessment parameters, the AO Spine CROST (Clinician Reported Outcome Spine Trauma) was developed by the AO Spine Knowledge Forum Trauma. The aim of the current study was to evaluate the feasibility, internal consistency, inter-rater reliability, and prospective validity of AO Spine CROST in the clinical setting. Also, the correlation between the clinician-reported CROST and patient-reported PROST (Patient Reported Outcome Spine Trauma) was investigated. Material and Methods: Patients were included from four trauma centers. Two surgeons with substantial amount of experience in spine trauma care were included from each center. Two separate questionnaires were administered at baseline, 6-months and 1-year: one to surgeons (CROST and additional evaluation questions) and another to patients (PROST). Descriptive statistics were used to analyze patient characteristics and feasibility, Cronbach’s α for internal consistency. Inter-rater reliability through exact agreement, Kappa statistics and Intraclass Correlation Coefficient (ICC). Prospective analysis, and relationships between CROST and PROST were explored through descriptive statistics and Spearman correlations. Results: 92 patients were included. CROST showed excellent feasibility results. Internal consistency (α = 0.58-0.70) and reliability (ICC = 0.52 and 0.55) were moderate. Mean total scores between surgeons only differed 0.2-0.9 with exact agreement 48.9-57.6%. Exact agreement per CROST item showed good results (73.9-98.9%). Kappa statistics revealed moderate agreement for most CROST items. In the prospective analysis a trend was only seen when no concerns at all were expressed by the surgeon (CROST = 0), and moderate to strong positive Spearman correlations were found between CROST at baseline and the scores at follow-up (rs = 0.41-0.64). Comparing the CROST with PROST showed no specific association, nor any Spearman correlations (rs = -0.33-0.07). Conclusion: The AO Spine CROST showed moderate validity in a true clinical setting including patients from the daily clinical practice. In future studies, the validation will be further investigated among larger patient and clinician samples. With its unique approach as a clinician-rated outcome measure, this tool has the potential to be valuable for use in clinics and research.
1538
P566: Intraoperative neurophysiological monitoring as a predictor for functional recovery following spinal cord injury
Samuel Adida 1,2 , Michael Calcaterra 1,2 , Christopher Como 2,3 , Yunting Tang 2,3 , Emma Bodo 2,4 , Isabella Valentino 2,4 , Parthasarathy Thirumala 2,4 , Joon Y. Lee 2,3 , Jeremy D. Shaw 2,3
1 University of Pittsburgh School of Medicine, Pittsburgh, USA
2 Department of Orthopaedic Surgery, Pittsburgh Orthopaedic Spine Research (POSR) Group, Pittsburgh, USA
3 Department of Orthopaedic Surgery
4 Department of Neurology and Clinical Neurophysiological Laboratory, UPMC, Pittsburgh, USA
Introduction: The capability of patients to recover following traumatic spinal cord injury (SCI) is not well understood. The American Spinal Injury Association (ASIA) impairment scale is the most widely utilized predictor for functional recovery, with ASIA-A injuries exhibiting the lowest recovery levels.1 Somatosensory-evoked potentials (SSEPs) and motor evoked potentials (MEPs) are commonly utilized neurophysiological modalities recorded throughout the course of spinal surgery and correlate to functional recovery after SCI.2-4 However, the prognostic value of intraoperative SSEPs and MEPs on long-term outcomes has not previously been investigated.4 This study aims to determine the neurophysiologic profiles of SCI patients stratified by postoperative predischarge ASIA exam scores. Patients with worse postoperative deficits (ASIA-A/ASIA-B) are hypothesized to have more absent or abnormal intraoperative neurophysiological modalities than patients with less severe postoperative deficits (ASIA-D/ASIA-E). Materials and Methods: Retrospective review of 927 patients that underwent surgery for traumatic SCI at a Level 1 Trauma Center was performed (2017-2022). Patients who were < 18 years old, underwent revision, or did not receive ASIA exams were excluded. Patient characteristics were recorded. Upper extremity (UE) and lower extremity (LE) SSEPs and MEPs were collected continuously throughout the procedure. Baseline, significant changes, and improvements to the amplitude of signals were recorded. After stratifying patients by ASIA score, one-way ANOVA and χ2 tests were performed to compare continuous and categorical variables, respectively. Post-hoc Bonferroni corrections were used to determine differences in neurophysiologic modalities between groups. Results: Of 927 patients, 205 (22.2%) met the inclusion criterion. Patients were assigned to ASIA-A (24.7%), ASIA-B (12.6%), ASIA-C (14.1%), ASIA-D (46.0%), and ASIA-E (2.5%) groups. There were no differences in sex (p = 0.523) or BMI (p = 0.585) amongst the groups. Patients in the ASIA-A and ASIA-B groups were younger than patients in the ASIA-D group (p = 0.003 and p < 0.001, respectively). Within the ASIA-A and ASIA-B groups, 21 patients (28.4%) had a normal UE SSEP signal and 1 patient (1.4%) a normal LE SSEP signal. Patients in the ASIA-A group had more abnormal LE SSEP signals compared to patients in the ASIA-D (p < 0.001) and ASIA-E (p < 0.001) groups. Additionally, patients in the ASIA-B group had more abnormal LE SSEP signals than patients in the ASIA-E group (p < 0.001). There were no differences in abnormal UE SSEP responses (p = 0.938) or changes in SSEP signals (p = 0.182) between all five groups. As for MEP signals, no differences were found when comparing baseline UE signals (p = 0.182), baseline LE signals (p = 0.134), or changes in MEP signals (p = 0.884). Conclusion: Patients with ASIA-A and ASIA-B scores were found to have had more abnormal SSEP signals when compared to patients with ASIA-D and ASIA-E scores. This study reaffirms the prognostic value of the ASIA classification system, as quantifiable differences in intraoperative SSEPs and MEPs between ASIA groups were determined. Only 1 patient that received either an ASIA-A or ASIA-B score (1.4%) had a recorded SSEP signal below the level of lesion. Further evaluation to identify these patients’ recovery after surgery will address the value of SSEPs and MEPs to aid in prognostic evaluation after SCI.
References
1. Spiess MR, Müller RM, Rupp R, Schuld C, EM-SCI Study Group, & van Hedel HJ. Conversion in ASIA impairment scale during the first year after traumatic spinal cord injury. Journal of neurotrauma 2009; 26: 2027-2036. https://doi.org/10.1089/neu.2008.0760
2. Spiess M, Schubert M, Kliesch U, EM-SCI Study group, & Halder P. Evolution of tibial SSEP after traumatic spinal cord injury: baseline for clinical trials. Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology 2008; 119: 1051-1061. https://doi.org/10.1016/j.clinph.2008.01.021 Bottom of Form
3. Eck JC, Martin CJ, Lapinsky A, et al. Does intraoperative neurophysiological monitoring have predictive value for functional recovery following spinal cord injury? A case report. J Clin Monit Comput 2013; 27: 93-96. https://doi.org/10.1007/s10877-012-9395-4
4. Costa P, Faccani G, Sala F, et al. Neurophysiological assessment of the injured spinal cord: an intraoperative approach. Spinal Cord 2014; 52: 749-757 (2014). https://doi.org/10.1038/sc.138
1643
P567: Influential factors in post-spine trauma employment among patients treated at a tertiary hospital in Tanzania: a cross-sectional study
Chibuikem Ikwuegbuenyi 1,2 , Francois Waterkeyn 3 , Hiten Solanki 2 , Rahel Mwavika 4 , Arthur Okembo 2 , Julieth Joseph 2 , Consolata Shayo 2 , Susan Stolla 2 , Stephanie Van Hoppe 2 , Julie Woodfield 1,2 , Ibrahim Hussain 1 , Halinder Mangat 5 , Hamisi Shabani 2 , Roger Härtl 1
1 Department of Neurological Surgery, Weill Cornell Medicine-Och Spine, USA
2 Department of Neurological Surgery
4 Department of Orthopedic Surgery, Muhimbili Orthopedic and Neurosurgery Institute, Dar Es Salaam, Tanzania
3 Department of Neurosciences, Grand Hôpital de Charleroi, Charleroi, Belgium
5 Department of Neurology, University of Kansas Medical Center, KS, USA
Introduction: Employment and its sustainability is a priority for many patients following spine trauma, as it is associated with numerous health, psychosocial and financial benefits, including better quality of life. Little is known about the factors affecting post-injury employment in low- and middle-income nations. This study highlights the employment rate after spine trauma and associated sociodemographic and clinical characteristics in East Africa. Methods: This was a telephone-based survey utilizing a prospectively maintained spine trauma database at Muhimbili Orthopedic Institute (MOI). Four hundred fifty patients managed at MOI for TSI between September 2016 and October 2021 were eligible. Sociodemographic data, injury characteristics, employment status before the injury, and complications were collected. The outcome measure was employment after injury. Simple logistic regression was used to assess the association between independent variables and outcome measures. Statistical analysis was conducted using R studio. Results: One hundred thirty patients completed the interview. The median age at injury was 33 years, and most were male (87.7%). The median length of follow-up and time since injury were 31.4 and 33 months, respectively. Most patients were married (65.4%) and had primary education only (54.6%). 86.9% reported having a complication post-discharge. 61.5% were employed before the injury, but only 40% had employment after the injury. Patients were more likely to be employed post-injury if they were married/cohabiting (OR = 5.23; 95% CI 2.20, 13.99 p < 0.001), had higher education (OR = 3.22; 95% CI 1.39, 7.79 p = 0.007), employed before injury (OR 86.17; 95% CI 17.41, 1565.71 p < 0.001), had insurance (OR 2.96 95%CI 1.27 7.18 p = 0.009). Patients were less likely to be employed after injury if they reported any complications (OR 0.23 95%CI 0.06 0.66 p = 0.014), had complete injuries (OR 0.35 95%CI 0.14 0.80 p = 0.017), and reported access to wheelchairs (OR 0.24 95%CI 0.11 0.52 p < 0.001). Conclusions: Our research identifies several variables that are associated with employment following spinal trauma. The results of the current study can help target resources to subsets of the spine trauma population that need greater aid or intervention to improve their chances of finding employment, such as through vocational rehabilitation services or programs.
1716
P568: Assessing the long-term outcomes among spine trauma patients treated at a tertiary hospital in tanzania: a cross-sectional study
Chibuikem Ikwuegbuenyi 1 , Francois Waterkeyn 2 , Hiten Solanki 3 , Rahel Mwavika 4 , Arthur Okembo 3 , Julieth Joseph 3 , Consolata Shayo 3 , Susan Stolla 3 , Stephanie Van Hoppe 3 , Julie Woodfield 1,3 , Ibrahim Hussain 1 , Halinder Mangat 5 , Hamisi Shabani 3 , Roger Härtl 1
1 Department of Neurological Surgery, Weill Cornell Medicine-Och Spine, USA
2 Department of Neurosciences, Grand Hôpital de Charleroi, Charleroi, Belgium
3 Department of Neurological Surgery
4 Department of Orthopedic Surgery, Muhimbili Orthopedic and Neurosurgery Institute, Dar es Salam, Tanzania
5 Department of Neurology, University of Kansas Medical Center, USA
Introduction: Traumatic spinal injuries (TSI) globally result in significant and prolonged disability, especially in low-income countries (LMICs), but there is a dearth of long-term outcome data, particularly in Sub-Saharan Africa, which our study addresses by conducting telephone interviews to explore complications, post-injury employment, and quality of life determinants in East Africa. Methods: Telephone interviews were conducted with 450 eligible TSI patients treated at Muhimbili Orthopedic Institute (MOI) between September 2016 and October 2021. We collected sociodemographic and injury data from a maintained database and used a structured questionnaire to gather information on employment status, complications, neurological improvements, and quality of life (QoL) using WHO's QoL tool. Statistical analysis was performed using R studio. Results: We could contact 173 (38.4%) patients or their surrogates, of which 37 (21.4%) were reported dead, with a median time from injury to death of 5 months. Lack of documented telephone numbers and non-response were significant obstacles. 130 (75.1%) of those contacted were able and willing to complete the interview. The median age at injury was 33 years, and most were male (87.7%). The median length of follow-up and time since injury were 31.4 and 33 months, respectively. Most patients were married (65.4%) and had primary education only (54.6%). 61.5% were employed before the injury, but only 40% had employment after the injury. 86.9% reported having at least one complication post-discharge, with pain (63.8%) being the most common. Regarding the quality of life, 21.5% rated their Qol as poor, and 26.2% were dissatisfied with their health. The best-scoring domain was the psychological domain, 62.5 (50 - 81.3). After multivariable adjustment, complete injury (B -16.91 95%CI -25.55 -8.29 p < 0.001), lower education level (B -15.19 95%CI -23.84 -6.53 p < 0.001), pain (B -20.13 95%CI -27.70 -12.55 p < 0.001), and contractures (B -19.44 95%CI -30.99 -7.89 p < 0.001) contributed to worse overall quality of life and general health. Sociodemographic characteristics (age at injury, lower education level, living alone, insurance status), injury characteristics (lumbar and complete injuries), and complications (pain, contractures, sexual dysfunction, spasticity, and pneumonia) were significant negative determinants of the Qol score in different domains. 59.2%, 55.8%, and 68.5% had access to physiotherapy, physician, and wheelchair/crutches services. Most patients reported substantial (48.5%) neurological improvement. Conclusions: This preliminary study underscores the challenges of obtaining long-term outcome data in Tanzania through telephone-based interviews. Key obstacles encountered included the absence of documented telephone numbers and instances of non-response. Nevertheless, this method of collecting long-term data holds potential, particularly in regions with widespread telephone usage, and its effectiveness could be enhanced by capturing multiple contact points for patients. Additionally, the integration of electronic health records, mobile health applications, collaborations between non-governmental organizations (NGOs) and international entities, the establishment of more longitudinal prospective cohort studies, and government support can significantly enhance the gathering of long-term data in resource-constrained environments.
2028
P569: Outcomes of pars defect repair using pedicle-translaminar screw technique
Emily Zielinski 1 , Jason Ye 2 , David Foley 1 , Barrett Boody 2 , Rick Sasso 2
1 Department of Orthopedic Surgery, Indiana University School of Medicine, Indianapolis, USA
2 Indiana Spine Group, Carmel, USA
Introduction: Adolescents suffering from spondylolysis present with low back pain hindering their participation in sports. Mainstay of treatment is conservative management with rest and brace immobilization. If this fails, single-level lumbar fusion is traditionally indicated to eliminate motion and improve pain. While successful, lumbar fusion in a young individual can have long-term consequences resulting from loss of motion and potentially increased stress at adjacent segments. We describe the outcomes of a pedicle and translaminar screw technique that was developed to provide rigid fixation across the defect while avoiding arthrodesis. Material and Methods: Institutional record query from 2011-2021 yielded 15 patients operatively treated for single-level lumbar spondylolysis. Operative technique involved a limited posterior approach with debridement of pars fracture site(s), followed by instrumentation with a 5.5 mm pedicle screw and 3.5 mm translaminar screw connected via a short rod. Decortication and bone grafting with autograft and bone morphogenetic protein (BMP) was also performed. Demographic and surgical patient data, visual analog scale (VAS) scores, and complications were retrospectively reviewed. Treatment success was determined by symptomatic improvement and evidence of healing on follow-up radiographs and/or CT. Descriptive statistics were used to analyze the data. Results: Seven patients (47%) were female. Mean age at surgery was 16.5 years (range 14 - 21). Most common offending sport was football (3 patients). L5 was the most affected level in 12 patients, followed by L4 in 2 patients, and L3 in one. Thirteen patients underwent bilateral pars repair at the affected level. VAS scores for back pain improved from an average of 5.8 pre-operatively to 1.6 post-operatively. Fourteen patients (93%) demonstrated intact hardware with radiographic healing at final follow-up. One patient reported persistent pain with pseudarthrosis 9 months post-operatively, resulting in subsequent spinal fusion. There were no complications. Conclusion: The 93% success rate of the pedicle-translaminar screw construct observed in this series is comparable to that of other previously described fixation constructs. One failure was observed in a patient who presented with Meyerding Grade 1 spondylolisthesis. The pedicle-translaminar screw construct is a safe and effective motion-preserving alternative to lumbar arthrodesis, but patients with pre-existing spondylolisthesis may be at higher risk for failure.
2205
P570: Indirect decompression with posterior stabilisation and anterior reconstruction with transpedicular intrabody cage insertion in Kummell’s disease
Sanjay Dhar 1 , Taarini Johri 1 , Rohan Gala 1 , Shashwat Anand 1
1 Orthopaedics, D.Y. Patil Hospital and Research Centre, Navi Mumbai, India
Introduction: Hermann Kümmell first described Kümmell disease in 18911 as delayed post-traumatic vertebral collapse. It affects the elderly population and is slightly more prevalent in men than women with osteoporosis being one of the important factors. Not only do these lesions at thoracolumbar junction. Indirect decompression with various augmentation techniques have been well described to address the dynamic instability and improving functional outcome. We report 2 cases of indirect decompression with posterior stabilisation and anterior reconstruction with transpedicular cage insertion (Cageplasty). Material and Methods: We report two patients diagnosed with Kümmell disease presenting with delayed onset neurological deterioration (incomplete) operated by posterior stabilisation and intrabody transpedicular cage insertion without any direct decompression. Pre operative function, radiology and neurology were noted from the digital medical record and imaging database. Post operative assessment of function (VAS & ODI), improvement in neurology (FRANKEL) and radiological changes were noted at each follow-up quarterly. Complications if any were noted. Results: A females and a males patient with a mean age of 63 years and an average lumbar spine T score of -3.0 were assessed. Both of them had fractures in the thoracolumbar junction and had neurological deterioration at least 6 weeks after trauma. Both patients presented with significant kyphosis, instability and retropulsion of fragment causing canal compromise. At presentation, the male patient was Frankel grade D while the female patient was Frankel C. Both patients were treated operatively with posterior fixation with intrabody cage insertion in the index vertebra. Both patients had post operative improvement in neurology by at least one grade at 6 weeks and could ambulate independently at 1 year follow-up. There was significant symptomatic improvement in (Mean VAS with improvement in functional score (ODI). At 2 year month follow-up both patients did well with no signs of implant loosening. Conclusion: Indirect decompression using posterior fixation with intrabody transpedicular cage insertion is an effective method to treat osteoporotic burst fractures not only promising symptomatic, functional and neurological improvement but allowing preservation of posterior elements thereby reducing chances of failure.
2324
P571: Clinical and radiological outcomes of 150 osteoporotic thoracolumbar fractures: a retrospective cohort study with a mean 4-years follow-up
Shankar Acharya 1 , Sai Viksheth Raj Basani 1 , Yudhisthir Raj Khadka 1 , KL Kalra 1 , Rupinder Chahal 1
1 Ortho-Spine Surgery, Sir Ganga Ram Hospital, New Delhi, India,
Introduction: The prevalence of osteoporotic vertebral fractures (OVCF) rises steadily with age. Most of these fractures respond well to conservative care. However, it is crucial to identify suitable candidates for conservative treatment to prevent a decline in their quality of life. This study aims to identify predictors of favorable outcomes in the management of osteoporotic fractures and assess how patients with these fractures respond to various treatment approaches. Material and Methods: A retrospective cohort study was conducted at a tertiary care spine center. The study included patients aged 50 years or older who presented with radiological evidence of OVCF in the thoracolumbar region, had evidence of reduced bone density as indicated by a DEXA scan (T score of -2.5 or lower), and had a minimum follow-up of one year within the past decade. Fracture classifications were based on the DGOU classification system using X-rays/CT scans and the Kanchiku T1 and Tsujio T2 classifications using MRI scans, focusing on collapse analysis. Radiological parameters, including kyphotic angles, were assessed through serial radiographs. Quality of life was evaluated via a telephonic questionnaire, the QUALEFFO-41. Statistical analysis involved One-way ANOVA to compare preoperative clinical and radiological parameters with final radiological and clinical outcomes. Results: 151 patients completed a minimum one-year follow-up, with an average follow-up duration of four years. The mean age of the cohort was 65.64 years, consisting of 60% females and 40% males. Among them, 91 patients initially underwent conservative treatment trials, while 60 received primary surgical intervention. Of the conservative group, 30 achieved successful results, while 61 required surgical intervention at various points. Nine postoperative complications were reported. DGOU 1 and 2 were managed conservatively, whereas types 4 and 5 required long segment fixation. T1-weighted intensity changes, with central and total types undergoing long segment fixation, while the superior type was linked with cement augmentation procedures. T2 MRI classification, diffuse high-intensity was best suited for conservative management, while confined high-intensity and diffuse low-intensity correlated with long segment fixation. Quality of life assessment at the final follow-up did not reveal significant differences among treatment groups. None of the preoperative radiological parameters were predictive of clinical outcomes. Predictors of Failed Conservative Trial: Age, with each year above 50, increases the likelihood of failure by 9%. DEXA score played a significant role, with an 81% higher risk of failure for each decrease in DEXA score points. DGOU types 4 and 5 had a 36-fold higher probability of failure than types 1 and 2. Furthermore, the T2 MRI Diffuse High-intensity type reduced the odds of a failed conservative trial by 97% compared to other types. Conclusion: Certain fracture types are not suitable for conservative treatment. While conservative management may lead to increased local and regional kyphosis, it still offers a better quality of life compared to alternative treatment modalities. Patients experiencing persistent pain, nonunion, and progressive deformity can benefit from percutaneous cement augmentation. For more unstable fractures, chronic non-unions, and cases with neurological deficits, spinal instrumentation surgeries may be necessary.
2443
P572: Current concepts: high volume polytrauma have high volume spinal fractures in level 1 trauma centres
Zion Hwang 1,2,3 , Bisola Ajayi 1 , Tesfaladet Kurban 1 , Emily Tsang 1 , Priyanshu Saha 4 , Jason Bernard 1 , Timothy Bishop 1 , Darren Lui 1,4
1 St. George's University Hospital, London, United Kingdom
2 Doncaster and Bassetlaw Teaching Hospitals NHS Foundation Trust United Kingdom
3 University of Sheffield, United Kingdom
4 St. George's University of London, United Kingdom
Introduction: Spine trauma involves high energy forces applied to the body. Therefore, these patients often have polytraumatic presentations. The AO Spine Group’s classification systems for spinal injuries incorporates a scoring element for polytrauma (M2 modifier). Therefore, this is an important factor for informing management decisions of spine trauma patients. This study explores the frequency and type of polytrauma that faces spine departments, and its implications. Methods: A review of all trauma patients admitted to a level 1 major trauma centre in 2022 was conducted using electronic patient database. Subsequently, patients with spinal injuries, their demographics and the characteristics of the trauma were identified from this dataset. Results: A total of 95 patients with spine trauma were identified. Patient demographics were 60 (63%) male, and average age 53 years old. 85 (89%) of these patients presented with polytrauma, including 45 (47%) head, 17 (18%) face, 64 (67%) neck, 24 (25%) upper limb, 20 (21%) lower limb, 49 (52%) thorax, 14 (15%) abdomen, and 17 (18%) pelvic injuries. Spinal injuries were classed according to the respective AO Spine Injury Classification Systems. We found 17 patients with upper cervical injuries (Type A: n = 7, Type C: n = 3); 25 patients with sub-axial cervical injuries (Type A: n = 18, Type C: n = 1, Type F: n = 9); 67 thoracolumbar injuries (Type A: n = 55, Type B: n = 4, Type C: n = 3), and 11 sacral injuries (Type A: n = 2, Type B: n = 5). Neurological deficit was found in 17 (18%) patients (N1: n = 3, N2: n = 3, N3: n = 10, N4: n = 1). 21 (22%) had unstable injuries, and 19 (20%) were admitted to ITU. 30-day mortality was at 5% (5/95). Conclusion: 9 out of 10 of patients presenting to major trauma centres with spinal injuries have polytrauma, most commonly of the neck followed by the thorax. This is an important factor for early escalation to other disciplines and thus informing surgical management decisions of these patients.
2552
P573: Evaluation of polytrauma in conjunction with spinal injury as a predictor of 30-day mortality
David Ajayi 1 , Zion Hwang 1 , Darren Lui 1 , Bisola Ajayi 1 , Priyanshu Saha 1
1 Complex Spine Surgery, St George's Hospital NHS Trust, Neuroscience, London, United Kingdom
Introduction: Level 1 trauma centers are designed to tackle the severely injured. Trauma that includes spinal fractures is associated with significant morbidity and mortality. Polytrauma in conjunction with spinal injury represents a medically demanding cohort. We examined whether this is a direct predictor of poorer outcomes by examining 30-day mortality. Material and Methods: A retrospective analysis of patients with polytrauma and spinal injury was extracted from a prospectively collected clinical database between January 2017, and December 2022. Analysis of trauma characteristics, demographics, and mortality at 30 days. Results: Analysis of 1,340 patients presenting with spinal trauma were identified between 2017 and 2022. A cohort of 4.7% had a 30-day mortality (n = 63). The predominant mechanism of injury was Falls (n = 37). 32% had Isolated spinal trauma (n = 20). 68% had Poly-injury (n = 43). Mean (8.6), SD (5.35), 95% CI (8.6 ± 4.689) and p-value (0). The Spine injuries include Cervical (n = 36), Thoracic (n = 23), Lumbar (n =30,) Sacrum (n = 5). Both single spine (n =10) and multisegmented spine injuries (n = 32) occurred. Based on AOTLICS classification: A0 (n = 24), A1 (n = 14), B3 (n = 5), B1 (n = 4), A3 (n = 4,) C (n = 4), A2 (n = 2), A4, B2 and F were (n = 1). Spinal cord injuries (n = 44) classified according to FRANKEL score: A (n = 32), B (n = 1), C (n = 1), D (n = 1), E (n = 9). Abbreviated Injury Scale: (AIS) Spine (n = 44), Head (n = 45), Face (n = 14), Neck (n =16), Thorax (n =31), Upper Limb (n =16), Lower Limb/Pelvis (n =14, 11), Abdomen including pelvic content (n = 18) External (n = 0). Polytrauma patients with Injury Severity Score (ISS) > 15 predicting 10% mortality (n = 34). Average age of cohort was 74years and largely male at 54% (n = 34). The average time of death was 16 days. Conclusion: Polytrauma associated with spinal injury contributes significantly to 30-day mortality. We identified that almost three quarters of spinal trauma patients who died had polytrauma in our level 1 trauma center.
Tumors
31
P574: Feasibility of multimodal intraoperative neurophysiological monitoring for extramedullary spinal cord tumor surgery in elderly patients
Sebastian Siller 1 , Akela Sixta 1 , Joerg-Christian Tonn 1 , Andrea Szelenyi 1
1 Department of Neurosurgery, LMU Hospital, Munich, Germany
Introduction: Extramedullary spinal cord tumors (EMSCTs) are mostly benign tumors which are increasingly diagnosed and operatively treated in the elderly. While there are hints that multimodal intraoperative neurophysiological monitoring (IONM) could be influenced by age and age-related comorbidities, no study has ever systematically evaluated its feasibility and value for EMSCT-surgery in elderly patients. Material and Methods: We retrospectively evaluated all patients with microsurgical EMSCT-resection under continuous multimodal IONM with SSEPs, MEPs and electromyography between 2016-2020. Epidemiological, clinical, imaging and operative/IONM records as well as detailed individual outcomes were analyzed and compared for the cohort </≥ 65 yrs. Results: Mean age was 45yrs in cohort < 65 yrs (n = 109) and 76 yrs in cohort ≥ 65 yrs (n = 64), while baseline/operative characteristics did not significantly differ. Mean baseline SSEPs’ latencies (left-right average) were significantly higher in the cohort ≥ 65 yrs for both median (20.9 ms vs. 22.1 ms; p < 0.01) and tibial nerve (42.9 ms vs. 46.1 ms; p < 0.01) without significant differences for SSEPs’ amplitudes. Stimulation intensity to elicit intraoperative MEPs was significant higher in the cohort ≥ 65 yrs (surrogate-marker: left-right-averaged quotient ID1-muscle/abductor-hallucis-muscle; 1.6 vs. 2.1; p < 0.001). Intraoperatively, SSEPs- and MEPs-monitoring were feasible in 99%/100% and 99%/98% for the cohort </≥ 65 yrs without significant differences in rates for significant IONM-changes during surgery. Postoperatively, 3.7% of the patients had a transient new motor deficit (permanent in 0.9%) and 4.6 % a transient new sensory deficit (permanent in 3.7%) for the cohort < 65 years, while 6.3% had a transient new motor deficit and 4.7% a transient new sensory deficit (permanent in 1.6%) in the cohort ≥ 65 years (no significant differences between both cohorts). Sensitivity of IONM was 29%/43%, specificity 99%/98%, positive- and negative-predictive-value 67%/75% and 95%/93% for the cohort </≥ 65 yrs. Overall, age was no risk factor for IONM-feasibility or rate of significant IONM-changes. Conclusion: Multimodal IONM is feasible and reliable for EMSCT-surgery in elderly patients. An age-related prolongation of SSEPs’ latencies and demand for higher stimulation intensities for MEPs’ elicitation has to be considered.
105
P575: The Oxford Spinal Sarcoma Service: excellent oncological outcomes with a multidisciplinary centralised approach to primary spinal tumour care
Jiong Hao Jonathan Tan 1,2 , Euan Stirling 2 , Gerard Mawhinney 2 , Jeremy Reynolds 2
1 Department of Orthopaedic Surgery, National University Hospital, Singapore, Singapore
2 Oxford Spinal Surgery Unit, Oxford University Hospitals, Oxford, United Kingdom
Introduction: The Oxford Spinal Sarcoma Service is one of 4 designated primary spinal tumour referral centres in the United Kingdom and serves a population of more then 10 million residents. Prior to its inception in 2008, there was a wide variation in practice with mixed clinical results. An educational outreach program and ease of access to the Spinal sarcoma service has led to centralization of care. We wish to report the outcomes of this approach. Material and Methods: This is a retrospective review of surgically treated primary spinal tumour patients treated between January 2008 to January 2022. Patient demographic, clinical, tumour and perioperative data was collected. Patients were divided into Enneking Appropriate (EA) and Enneking Inappropriate (EI). EA margin was defined as one where final pathological margins and surgical impression matched the Enneking-recommended surgical margins, EI margin was one where EA surgical margins were not obtained or where a previous intralesional procedure had been performed. Patient outcomes studied included local recurrence, metastases and overall survival. Statistical significance was set p < 0.05. Cox regression was performed to determine the risk predictors for survival time and time to local tumour recurrence with death as competing. Significant univariate variables were used for the multivariate analysis. Due to multicollinearity, some variables, although significant in the univariate analysis were not used for multivariate analysis. Results: 119 patients were included of which 75 (63.0%) were male. The mean age at time of surgery was 46 (8-86) years. Chordoma (30/119 (25.2%)), followed by chondrosarcoma (13/119 (10.9%)) were the most common tumours and most tumours involved the mobile spine (86/119 (72.3%)) compared to sacral tumours (33/119 (27.7%)). 96/119 (80.7%) patients were virgin cases and we managed to achieve EA margins in 81 (68.1%) of our patients. There were 38 (31.9%) EI patients, of this group 23/38 (60.5%) were non-virgin cases which precluded EA resection. In patients whom EA surgery was attempted, we achieved EA margins 81/90 (90.0%) of the time. Notably in EA patients with mobile spine tumours the local recurrence rate was 1/51 (2.0%) compared to 5/28 (17.9%) in EA patients with sacral tumours and 7/35 (20%) in EI patients with mobile spine tumours and 4/5 (80%) in EI patients with sacral tumours. Mean local recurrence free (LRF) survival was 5.2 (1-13.5) years and local recurrence rate was 14.3%. Mortality rate was 21.0% with a mean survival of 5.63 (1-13.5) years post-surgery. On multivariate analysis EI (p = 0.019) and post-operative systemic treatment (p = 0.004) were significant risk factors for local recurrence while the presence of metastases (p = 0.012) and pre-operative systemic therapy (p = 0.025) were significant risk factors for mortality Conclusion: Inappropriate diagnostic procedures and treatment is associated with poor outcomes and mortality in primary spinal tumour patients. Centralization of primary spinal tumour care has led to excellent oncological results with a local recurrence rate comparable to most large spinal tumour centres. In primary tumors of the mobile spine our local recurrence rate (2.0%) is one of the lowest reported in the literature. We believe that our experience will be of benefit to other centres.
178
P576: Minimally invasive lateral corpectomy of thoracolumbar spine: early experience
Padungcharn Nivatpumin 1 , P. Decharin 1
1 Neurosurgical Unit, Department of Surgery, Chulabhorn Hospital, Chulabhorn Royal Academy, Bangkok, Thailand
Introduction: The minimally invasive lateral corpectomy to the thoracolumbar junction by retropleural or retroperitoneal approaches has been increasingly more indicated in the treatment of various conditions, such as deformities, trauma, infection and tumors. The development of technique allowed not only fusion to be performed, but also direct decompression under direct visualization of the neural elements in their ventral portion. Objectives: To decribe the minimally invasive technique for the lateral retropleural and retroperitoneal approach to the thoracolumbar spine using expandable tubular retractor, as well as its feasibility, complications, and necessary precautions. The results of the initial experience of the Neurosurgical service of the Chulabhorn hospital, Bangkok, Thailand, will be presented. Methods: After a review of literature, the initial experience of the service is reported in 2 spinal tumor cases, comparing it to the published results. The surgical technique used is described with emphasis on the surgical anatomy of the diaphragm. Results: The minimally invasive lateral corpectomy of thoracolumbar spine by retropleural or retroperitoneal approach with the application of an expandable tubular retractor was described step-by-step in this study, with emphasis on important issues, such as preoperative planning, access to the retropleural or retoperitoneal space, approach for corpectomy and implant placement and major complications during surgery. It allows for adequate interbody fusion rates associated with a smaller skin incision and less tissue damage, blood loss, and post operative pain. Conclusion: Corpectomy and reconstruction of the TL spine is feasible and safe using a minimally invasive lateral retropleural or retroperitoneal approach. Since this is a relatively new technique, more studies are needed to compare radiographic and clinical outcomes in many aspects.
Keyword: minimally invasive surgery (MIS); lateral corpectomy; thoracolumbar spine; retropleural approach; retroperitoneal approach
226
P577: Redefining prognosis: conditional survival trends after surgery for spine metastases
Nikita Zaborovskii 1,2 , Anton Denisov 3,4 , Adam Schlauch 5 , John Shapton 5 , Sergei Masevnin 1 , Oleg Smekalenkov 1 , Dmitry Ptashnikov 1,6 , Dimitriy Kondrashov 7
1 Spinal and Bone Oncology, Vreden National Medical Research Center of Traumatology and Orthopedics, Saint-Petersburg, Russian Federation
2 Saint-Petersburg State University, Saint-Petersburg, Russian Federation
3 Spinal Unit, Hospital Quirónsalud San José, Madrid, Spain
4 Biostatisctis, University Hospital 12 of October, Madrid, Spain
5 San Francisco Orthopaedic Residency Program, San Francisco, USA
6 Orthopedic Department, North-Western State Medical University named after I.I.Mechnikov, Saint-Petersburg, Russian Federation
7 Spinal Surgery, Dignity Health / Saint Mary’s Hospital, San Francisco, USA
Introduction: Despite spinal metastases being a common site of skeletal metastases, data on conditional survival (CS) after spine metastasis surgery is lacking. We aimed to evaluate CS and associated factors among patients undergoing spine surgery for metastatic tumors. Material and Methods: This single-center retrospective study included 361 patients who underwent surgical intervention for metastatic spine tumors between 2000-2021. Clinical data collected included demographics, American Spinal Injury Association Impairment Scale grade, ambulatory status, comorbidities assessed by Charlson Comorbidity Index, Eastern Cooperative Oncology Group performance status, tumor characteristics including Spinal Metastasis Invasiveness Index, type and invasiveness of surgery, complications and administration of adjuvant therapies. Overall survival (OS) was measured from date of surgery until death or last follow-up. CS was determined as the probability of surviving an additional time 't' given the patient has already survived 's' months after surgery. Kaplan-Meier method identified OS and CS curves. Multivariate Cox regression identified factors associated with OS and CS. Results: Median OS was 15 months with 6-, 12-, 18- and 24-month OS of 78.4%, 57.1%, 43% and 34.7%, respectively. CS improved from 57% at baseline to 70% at 24 months (+13%). On multivariable analysis, shorter OS was associated with high Charlson Comorbidity Index, rapid tumor growth, lung metastasis, non-ambulatory status and stabilization-only surgery. Longer OS correlated with metastasectomy and postoperative therapy.Stratifying by covariates showed:
Higher CS gains in severe comorbidity and lung metastasis patients
Lower gains in rapid tumor and non-ambulatory patients
Metastasectomy and post-op therapy improved baseline CS more than gain over time.
Conclusion: Despite initial prognosis, CS after surgery for spinal metastases improves over time, particularly in subsets with poor baseline survival. Postoperative treatment and metastasectomy provide initial survival benefit but gain diminishes thereafter. Time dependent risk stratification is needed to personalize prognosis.
266
P578: "Axisplasty" or C2 vertebroplasty for the treatment of a metastatic lytic lesion - A case report and review of literature
Nigil Palliyil 1 , Jim Vellara 1
1 Orthopaedics (Spine Surgery), Amrita Institute of Medical Sciences, Cochin, India
Introduction: Upper cervical spine (C1-C2) metastasis is quite rare with an incidence of 1% of all the spinal metastases. Management of C2 metastatic lesions is particularly challenging due to its location and surrounding delicate neurovascular structures. Lytic metastatic lesions can lead to debilitating neck pain, pathological fractures, spinal cord compression and overall poor outcome. Extensive surgical procedures like vertebrectomy and occipito-cervical fusions may not be suitable for patients with advanced metastatic disease. Vertebroplasty as a minimally invasive procedure has only rarely been performed for upper cervical spine lesions. We report a case of vertebroplasty done for a patient with C2 metastatic lytic lesion. Materials and Methods: A 53-year-old lady (with previous history of breast cancer) presented with excruciating neck pain of 1 month duration. Examination revealed restriction of her neck movements. She had no neurological deficits. MRI and CT scan revealed a lytic lesion involving the body of C2 extending to the dens with no evidence of spinal cord compression. The SINS score of the lesion was 8. She underwent vertebroplasty using a Jamshidi needle with 2.5 cc of cement. The approach was via the right sided Smith Robinson approach. A radiolucent retractor was placed to protect the vital structures. Two concomitant C-arms were used to ensure accurate placement of the Jamshidi needle. A radiopaque contrast was injected initially to ensure that there was no leak posteriorly into the vertebral canal. There were no peri-operative complications. Results: Patient had excellent pain relief following the procedure. She subsequently underwent radiotherapy and remained asymptomatic at the latest follow-up at 6 months. Conclusions: Axisplasty or C2 vertebroplasty is an effective, minimally invasive treatment option for the management of metastatic lytic lesions.
Keywords: C2 vertebroplasty; axisplasty; cervical vertebroplasty; cervical metastasis; cement augmentation
297
P579: Custom made connectors for the use of carbon fibre rods in the treatment of cervical spinal tumours
Jiong Hao Jonathan Tan 1,2 , Simone Mazzoli 1 , Gennaro Scotto 1 , Alessandro Luzzati 1
1 Center for Orthopedic Oncology and Spine Reconstructive Surgery, IRCCS Galeazzi Hospital - Sant'Ambrogio Milan, Italy
2 National University Hospital, Singapore
Introduction: Carbon fibre composite rods have the advantage of biocompatibility, good biomechanical characteristics and minimal interference with radiotherapy planning/delivery and imaging in spinal tumour surgery. Despite these advantages, Carbon fibre rods are not used in the cervical spine as there are currently no carbon fiber rods that possess a calibre suitable for the tulips of cervical screws. In the literature there is only one series reporting the use of carbon fiber rods in the cervical spine, by anchoring to the cervical vertebrae with sublaminar bands and titanium connectors with supplementary anterior stabilization. We propose a new technique that allows the use of carbon fibre bars in the cervical and cervical-thoracic spine without anterior reconstruction. A hybrid system of titanium connectors is used to link the tulips of the cervical screws and the occipital plate to the carbon fibre rods and thus exploit the advantages of using carbon fiber bars without sacrificing mechanical stability. Material and Methods: This is a retrospective case series of patients who underwent surgery for cervical or cervical-thoracic junction spinal tumours between November 2020 to September 2022. A customized titanium connector made up of a tulip for connection to the carbon fibre rod and a rod for connection to the cervical/occipital fixation was utilized. In C3-C7 3.5 mm titanium lateral mass screws were placed, while in C2 and the occiput, pedicle screws and a occipital plate and screw construct was used. In patients whom Ostapek® rods were utilised, 6mm titanium implants were placed in the thoracic spine, while in patients whom CF-PEEK implants were utilised, 6mm or 5mm CF-PEEK screws were utilized. Results: A total of 11 patients were enrolled for this study, 8 males and 3 females with a mean age of 59.4 (range 21-80) years. 5 patients had primary spinal tumours while 6 patients had spinal metastases. In 2/11 cases an en-bloc resection was performed, in 4/11 cases intralesional debulking, while in the remaining 5/11 cases separation surgery was performed. In 9 cases Ostapek® bars were used and in 2 cases Carbon-PEEK bars. In 2 cases anterior reconstruction was performed with non-vascularized iliac crest graft. Mean length of construct was 9 (range 7-13) levels and mean number of un-instrumented levels was 4 (range 2-6) levels. On final follow up, 7/11 patients had no evidence of local recurrence or local progression, while 1 patient was loss to follow up. There was no evidence of loss of spinal alignment, implant pullout or breakage for all patients at final follow up. Conclusion: In view of the decreased need for anterior reconstruction secondary to improved mechanical stability and ease of radiological surveillance and radiotherapy, we believe that our technique is a valid method to utilise the biomechanical advantages of carbon rods. Further prospective studies comparing our method to conventional methods of cervical thoracic fixation in terms of blood loss, operative time, mechanical stability, ease of post-operative radiological surveillance and radiotherapy is needed.
336
P580: Mini-open C2 vertebroplasty for odontoid ostelytic lesion
Adnene Benammou 1,2 , Cherif Kamoun 1,2 , Ahmed Ben Abid 1,2 , Seddik Akremi 1,2 , Mondher Kooli 1,2 , Mehdi Bellil 1,2 , Mohamed Ben Salah 1,2
1 University Tunis el Manar, Faculty of Medecine of Tunis, Tunisia
2 Orthopedic Surgery Department, Charles Nicolle Hospital, Tunis, Tunisia
Introduction: Percutaneous vertebroplasty is a well-established technique in treating multiple painful lesions of the thoracolumbar spine. It can provide pain relief, bone strengthening and vertebral stabilization. However, its use in the upper cervical spine is rare due to the difficult access and multiple potential complications. We report a safer technique with a mini-open vertebroplasty of a C2 osteolytic lesion. Material and Methods: A 71-year-old man, with history of neck pain for which he did not seek medical treatment, sustained a road traffic accident. He presented to our emergency room. Physical examination revealed only pain of the right clavicle. No neurological deficit was noted. A full body Computed Tomography (CT) was conducted due to the violence of the trauma. It revealed a fracture of the right clavicle and an osteolytic lesion of C2 involving the left half of C2 vertebral body. The fracture of the clavicle was treated conservatively. The decision for the C2 osteolytic lesion was to proceed with a mini-open vertebroplasty. Surgery was realized in supine position with head on horseshoe. Fluoroscopy marking of vertebral levels was realized. We realized a mini right anterior cervical approach exposing the edge of C2. We inserted the Jamshidi needle on the lytic region under fluoroscopic control. Biopsy was taken and addressed to the laboratory. We injected then the PolyMethyl MethAcrylate (PMMA) using the eggshell technique with injecting in the posterior part, waiting for the cement to harden and then proceed to injecting the cement to fill the lesion. We used the eggshell technique to avoid cement leakage and its possible complications especially at the level of C2. No extravasation was noted. Results: Intra and postoperative was uneventful. Pain relief was immediate after surgery. Visual Analog Scale (VAS) decreased from 8 in preoperative to 2 in postoperative. Postoperative CT-scan showed PMMA in the body of C2 with no sign of extravasation. The patient was ambulated and discharged the day next surgery and addressed to a medical department to establish the etiology of the lesion. At 3 months postoperative, there was a complete pain relief (VAS = 0). Conclusion: Osteolytic lesions of C2 are rare. They can cause serious neurovascular complications. Percutaneous vertebroplasty has shown great result in treating thoracolumbar spine but can be difficult in upper cervical spine. This technique of mini-open vertebroplasty can be a safer less demanding technique in treating osteolytic lesions of C2. It has the advantages of vertebroplasty such as early pain relief and vertebral stabilization without the risk of the percutaneous technique in the upper cervical spine which can lead to serious complications.
487
P581: 3D-printed protheses for upper cervical chordomas - A personalized approach to reconstruction
Zan Chen 1
1 Department of Neurosurgery, Xuanwu Hospital, Capital Medical University, Beijing, China
Objective: Each vertebra of the upper cervical spine has unique morphological and biomechanical characteristics. Traditional techniques for reconstructing upper cervical stability are often associated with a high risk of implant failure. Three-dimensional (3D) printing is an additive manufacturing method that creates 3D models through successive layers based on a computer-aided design. It is widely used in spinal surgery due to its favorable mechanical strength, capacity to manufacture highly individualized shapes, potent osteoinductivity, and osseointegration. Here, we present the clinical efficacy of customized 3D-printed prostheses in treating upper cervical chordomas. Methods: A retrospective study was conducted on the clinical data of 10 patients with chordoma involving axial vertebral treated with 3D-printed prostheses in our department from December 2018. All patients underwent vertebral body resection via a posterior-anterior combined approach. One case received a posterior approach, high retropharyngeal approach, and transoral approach while others underwent posterior- high retropharyngeal approach. All patients underwent axial anterior column reconstruction with a customized 3D-printed cervical prosthesis. All patients were followed up regularly after surgery. Results: There was no vascular or nerve injury or dura sac. All wounds healed in the first stage, no disunion or infection occurred. The patients were followed up for an average of 15 months. 3 patients had tumor recurrence and underwent tumor resection again. No fixation failure was found. Conclusion: Personalized 3D-printed prostheses can effectively reconstruct the axial anterior column structure and satisfactory short-term clinical efficacy was obtained.
Keywords: upper cervical tumor; chordoma; 3D-printed prostheses; reconstruction
573
P582: Hematologic malignancy influences the survival prediction accuracy of solid-tumor spinal metastasis patients undergoing surgery
Thamrong Lertudomphonwanit 1 , Pongsathorn Chanplakorn 1
1 Orthopaedics, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Introduction: Regarding the evolution of new techniques in spinal surgery along with adjuvant modern therapy, the surgical outcome of spinal metastasis surgery has much improved particularly in multiple level spinal metastasis. However, considering with the patient’s survival period, selection of patients who would have benefit from the surgery is still debatable. Previous studies revealed significant higher median survival period in hematologic malignancy compared to solid-tumor spinal metastasis. This study aimed to compare the predictors and survival prognosis scheme between the patients with spinal metastasis including hematologic malignancy (All-malignancy group) and the patients with spinal metastasis excluding hematologic malignancy (Non-hematologic malignancy group). Material and Methods: The inclusion criteria were patients aged more than 18 years, diagnosed with spinal metastasis, and underwent the surgical treatment at our hospital between October 2008 and August 2018. The patient’s demographic data, treatment modalities and Laboratory results were retrospectively reviewed and were analyzed. The exclusion criteria were the patient who underwent only spinal biopsy without additional procedure and the patient who had no definite pathological diagnosis. A COX regression analysis was used to identify the independent factors for survival prediction for each group. Then, the individual score was divided into 3 subgroups according to the survival probability as A:good prognosis, B: fair prognosis and C: worst prognosis. The survival rate of the individual scoring scheme was calculated using Kaplan-Meier survival analysis. Results: One hundred eighty-six patients were included in the analysis. There were 101 males, the mean age was 57.1 ± 13.4 (18-87) years. The hematologic malignancy was found in 18 patients. The median survival time were 201 days in All-malignancy group and 168 days in Non-hematologic malignancy group, respectively. There were difference independent factors between these two groups. ECOG status (HR 2.59 95% CI 1.87-3.60 for All-malignancy group and HR 2.20 95% CI 1.57-3.08 for Non-hematologic malignancy group, respectively) and response to preoperative chemotherapy (HR 1.73 95% CI 1.23-2.43 for All-malignancy group and HR 1.78 95% CI 1.25-2.53 for Non-hematologic malignancy group, respectively) were identified as independent factors in both groups. Radiosensitivity (HR 1.92 95% CI 1.39-2.64) and central nervous system metastasis (HR 2.79 95% CI 1.41-5.52) were identified as independent factors only in All-malignancy group while tumor growth potential (HR 2.42 95% CI 1.69-3.47), serum albumin level (HR 1.55 95% CI 1.12-2.15) and numbers of vertebral involvement (HR 1.49 95% CI 1.08-2.06) were identified as independent factors only in Non-hematologic malignancy group. The ROC for both scoring schemes were comparable, 0.75 in All-malignancy group and 0.77 in Non-hematologic malignancy group. The median survival time comparing between All-malignancy group and Non-hematologic malignancy group were as follow; group A: 461 days VS 427 days, group B: 81 days VS 79 days and group C: 50 days equally in both groups. Conclusion: Prolong survival of hematologic malignancy patients influences survival prediction scheme of solid-tumor spinal metastasis patients undergoing surgery. Tumor specific prognostic may be needed to improve survival prediction accuracy and may help to select patients who would have benefit from the surgery for spinal metastasis.
645
P583: Spinal intradural extramedullary cystic schwannoma: a case-based systematic review
Alexis Terrapon 1 , Martin Stienen 1 , Anand Veeravagu 2 , Michael Fehlings 3,4 , Oliver Bozinov 1 , Nader Hejrati 1
1 Department of Neurosurgery & Spine Center of Eastern Switzerland, Kantonsspital St.Gallen & Medical School of St. Gallen, St. Gallen, Switzerland
2 Neurosurgery, AI Lab & Department of Neurosurgery, Stanford University School of Medicine, Stanford, USA
3 Division of Neurosurgery and Spine Program, Department of Surgery, University of Toronto, Toronto, Canada
4 Division of Neurosurgery, Toronto Western Hospital, University Health Network, Krembil Neuroscience Centre, Toronto, Canada
Introduction: Schwannomas are the second most common intradural extramedullary tumors but they rarely present as predominantly cystic lesions. Thus, cystic schwannomas may be misdiagnosed, which could delay optimal treatment. Because of their rarity, cystic schwannomas are only documented in a few case reports and series. As a result, a standardized approach in the management of these tumors remains challenging to establish. The aim of this study was to review all cases of spinal, intradural, extramedullary schwannomas that exhibit predominant or very large cystic components, in order to infer management strategies and analyze the perioperative course of patients with such lesions. Material and Methods: We conducted a structured search of the MEDLINE and CENTRAL databases on 2nd June 2023 for spinal intradural extramedullary cystic schwannomas. All title/abstracts were screened, and a full-text review of the remaining articles was conducted. The results were compiled in tables and summarized using means and standard deviation (SD), median and interquartile range, and percentage and 95% confidence intervals. Results: We identified 263 articles, of which 35 reporting 54 cases were included. Patients had a mean age of 48 years (SD ±13.1 years) at presentation, 57% were males, and most lesions were lumbar (43%). The most common symptoms were pain (81%) and muscle weakness (67%) with 83% of patients showing some sort of neurological abnormality. 69% of patients showed a complete relief of symptoms after surgery and 96% an improvement. Only four complications were reported. Additionally, we present a case of a 44-year-old female with back pain, mild paraparesis, sub T12 hypoesthesia, gait ataxia, and sphincter dysfunction, that showed a cystic schwannoma extending from T7 to T11. The patient was operated and showed significant improvements at 6 weeks and 6 months following surgery. Conclusion: Schwannomas should be considered in the differential diagnosis of intradural extramedullary cystic lesions. Patients typically present with subacute to chronic pain and/or neurologic changes. Surgical resection is the primary therapeutic modality and usually has a good to excellent outcome.
662
P584: A critical appraisal of the frailty and sarcopenia assessment tools in the spinal oncology population applying clinimetric assessment: a systematic review
Miltiadis Georgiopoulos 1 , Mark Maclean 2 , Antoinette Charles 3 , Raphaële Charest-Morin 4 , C. Rory Goodwin 3 , Michael Weber 1
1 Spine Surgery Program, Division of Orthopaedic Surgery, Department of Surgery, McGill University, Montreal, Canada
2 Division of Neurosurgery, Department of Surgery, Dalhousie University, Halifax, Canada
3 Spine Division, Department of Neurosurgery, Duke University, Durham, USA
4 Spine Surgery Institute, Vancouver General Hospital, University of British Columbia, Vancouver, Canada
Introduction: Worse surgical outcomes have been associated with frailty and sarcopenia by many publications regarding patients with degenerative or deformity disorders of the spine. However, this relationship is less clear in the context of spinal oncology. We aimed to identify all frailty and sarcopenia tools used in spinal oncology and evaluate their clinimetric properties. Material and Methods: We performed a systematic review that included studies published from January 1st, 2000, to June 2022. Study characteristics, frailty tools, and measures of sarcopenia were collected. Component domains, individual items, cut-off values, and measurement techniques of the identified tools were recorded. Moreover, a clinimetric evaluation of all included tools was conducted according to the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN). Results: Twenty-two studies with 42,514 patients overall were included. Seventeen studies applied 6 frailty tools with the three most applied being the Metastatic Spine tumor Frailty Index (MSTFI), Modified Frailty Index-11 (mFI-11), and the mFI-5. Eight studies employed measures of sarcopenia; the three most common were the L3-Total Psoas Area (TPA)/Vertebral Body Area (VBA), L3-TPA/Height2, and L3-Spinal Muscle Index (L3-Cross-Sectional Muscle Area/Height2). Sarcopenia and frailty tools lacked or had uncertain content and construct validity. All tools were feasible except the Hospital Frailty Risk Score (HFRS). Frailty tools were objective, except the Johns-Hopkins Adjusted Clinical Groups, and all of them had floor or ceiling effects. Positive predictive validity was found for the HFRS and in some studies investigating the mFI-5, MSTFI, and L3-TPA/VBA measures. Conclusion: Unfortunately, available frailty and sarcopenia measures concerning patients operated due to spinal tumors were found to have poor clinimetric properties. On the other hand, most frailty and sarcopenia measures were feasible, and most frailty tools were objective. We also aimed to provide a pragmatic approach to applying existing frailty and sarcopenia instruments, until more clinimetrically robust tools are presented.
738
P585: Defining spine cancer pain syndromes: a systematic review and proposed terminology
Markian Pahuta 1 , Ilya Laufer 2 , Sheng-Fu Larry Lo 3 , Stefano Boriani 4 , Charles Fisher 5 , Nicolas Dea 5 , Michael Weber 6 , Dean Chou 7 , Arjun Sahgal 8 , Laurence Rhines 9 , Jeremy Reynolds 10 , Aron Lazary 11 , Alessandro Gasbarrini 12 , Jorrit-Jan Verlaan 13 , Ziya Gokaslan 14 , Chetan Bettegowda 15 , Mohamed Sarraj 16 , Ori Barzilai 17
1 McMaster University, Hamilton, ON, Canada
2 NYU Grossman School of Medicine, New York, NY, USA
3 Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New York, NY, USA
4 IRCCS Istituto Ortopedico Galeazzi, Bologna, Italy
5 The University of British Columbia, Vancouver, BC, Canada
6 McGill University, Montreal, QC, Canada
7 Columbia University Irving Medical Center, New York, NY, USA
8 Sunnybrook Health Science Center, Toronto, ON, Canada
9 The University of Texas, MD Anderson Cancer Center, Houston, TX, USA
10 Nuffield Orthopaedic Centre, Oxford, United Kingdom
11 National Center for Spinal Disorders, Budapest, Hungary
12 IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
13 UMC Utrecht, Utrecht, The Netherlands
14 The Warren Alpert Medical School of Brown University, Providence, RI, USA
15 Johns Hopkins University School of Medicine, Baltimore, MD, USA
16 McMaster University, Hamilton, ON, Canada
17 Memorial Sloan Kettering Cancer Center, New York, NY, USA, Neurosurgery, New York, USA
Introduction: Formalized terminology for pain experienced by spine cancer patients are lacking. The common classification scheme of spine cancer pain as mechanical or non-mechanical is not exhaustive of all potential pain sources. Misdiagnosed spinal pain may lead to ineffective treatment recommendations. Materials and Methods: We conducted a systematic review of reported pain syndromes that may be encountered in spinal oncology patients. We provide a comprehensive and unbiased summary of the existing evidence, not limited to the spine surgery literature, and subsequently consolidate these data into a practical, clinically relevant nomenclature for spine oncologists. Results: Our literature search identified 3515 unique citations. Through title and abstract screening, 3407 citations were excluded, resulting in 54 full-text citations for review. Data regarding the putative mechanisms of pain are typically categorised into nociceptive pain (somatic vs visceral), neurologic pain and treatment related pain. We then consolidated these data and categorized into a clinically relevant nomenclature of tumor related/biologic tumor pain, mechanical pain, radicular pain, neuropathic pain and treatment-related pain. Biologic tumor pain will respond temporarily to steroid administration and will ultimately resolve when local tumor control is achieved. Mechanical pain is fracture-related pain and will resolve with stabilization or cement augmentation. Radicular pain is secondary to mechanical nerve root compression and will resolve with nerve root decompression and / or stabilization when secondary to fracture related bone fragment or to local therapy (radiation or systemic) when the compression is secondary to soft tissue from tumor growth. Neuropathic and other treatment related pain are important to consider as they are unlikely to respond to interventions and require multimodality pain regimens to control. Conclusion: We propose a clinical nomenclature of spinal tumor related pain syndromes to facilitate and standardize diagnosis, communication and reporting.
741
P586: Denosumab as off-label treatment in patient with aneurysmal bone cysts of the spine: a case series wit long term follow-up
Gisberto Evangelisti 1 , Luigi Falzetti 1 , Emanuela Palmerini 2 , Alessandro Gasbarrini 1
1 Spine Surgery
2 Bone and Soft Tissues Oncology, Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Aneurysmal bone cyst (ABC) is a rare skeletal tumor. It represents the 1.4% of primary bone tumors (15% of spinal bone tumor), has a Prevalence of 0.32/100,000 inhab./year (= 192 patients/year). Surgical treatment, embolization or autologous stem cells injections have been described to approach this disease. We hypothesized that owing to similarities with giant cell tumor of bone (GCTB), in which denosumab has been previously described as successful treatment, it could be active also in ABC. Material and Methods: A retrospective analysis of prospectively collected data of patients affected by aneurysmal bone cysts treated with denosumab at the dose of 120 mg at day 1, 8, 15, 29 and later every 4 weeks was performed. Patients underwent radiologic and clinical assessment every 3 months for at least 24 months. Symptoms and adverse events were noted. Results: Six patients were enrolled in the present study (5 male, 1 female), with a median age of 24 years (range 16-42 years). Distribution within the spine were 3 cervical spine, 2 lumbar spine, and 1 thoracic spine. Patients were followed for a median time of 57.2 months (range 24-96 months). Patients received a median of 17.5 denosumab administrations (range 5-42). All symptomatic patients had pain relief and 2 had paresthesia improvement. Signs of denosumab activity were observed after 3 to 6 months of administration: bone formation by computed tomography scan was demonstrated in all patients. Adverse events were negligible. At last follow-up, all patients were progression-free:1 still on denosumab treatment, 2 off denosumab were disease-free 13 and 17 months after surgery, and the last 3 patients reported no progression 12 and 24 months after denosumab interruption and no surgery. Conclusion: Denosumab has substantial activity in ABCs, with favorable toxicity profile. We strongly support the use of surgery, embolization or autologous stem cells injection, but denosumab could have a role as an alternative therapeutic option in patients affected by rapidly destructive or recurrent disease and in patient not eligible to embolization or cell stems infiltrations.
760
P587: Characteristics and risk factors of instrumentation failure following total en bloc spondylectomy
Takaki Shimizu 1,2 , Satoshi Kato 1 , Noriaki Yokogawa 1 , Satoru Demura 1
1 Department of Orthopaedic surgery, Graduate School of Medical Sciences, Kanazawa University, Kanazawa, Japan
2 Department of Orthopaedic Surgery, Kanazawa Municipal Hospital, Kanazawa, Japan
Introduction: Total en bloc spondylectomy (TES) was developed for complete oncological resection of spinal tumors. Recent advances in surgical techniques and multidisciplinary treatments for various tumors are considered to further extend survival following TES. Therefore, spinal reconstruction after TES is crucial for prolonged function and quality of life. Nevertheless, the incidence of instrumentation failure (IF) after TES is high (20–40%) due to the destabilization of all three columns of the affected spine. Several studies have focused on IF after TES, however, most of these studies have small sample sizes, and only a few have conducted multivariate risk factor analysis. Therefore, this study investigated what risk factors for IF exist following TES by retrospectively investigating the incidence and characteristics of IF after TES using a relatively large sample size. Material and Methods: Data from 136 patients (65 men, 71 women) with a mean age of 52.7 years (range, 14–80) who underwent TES were retrospectively reviewed. The mean follow-up period was 101 months (range, 36–232). Analyzed factors included incidence of IF, age, sex, body mass index, history of chemotherapy or radiotherapy, tumor histology (primary or metastasis; benign or malignant), surgical approach (posterior or combined), tumor location (thoracic or lumbar; junctional or non-junctional), number of resected vertebrae (single or multi-level), anterior resection line (disc-to disc or intra-vertebra), type of bone graft (autograft or frozen autograft), cage subsidence (CS), and local alignment (LA). A survival analysis of the instrument was performed, and relationships between IF and related factors were investigated using the Cox regression model. Results: A total of 44 patients (32.4%) developed IF at a median of 31 months (range, 3-129) following TES. Most IFs were rod fractures preceded by a mean CS of 6.1 mm (range, 2-18) and LA kyphotic enhancement of 10.8° (-1 to 36). IF-free survival rates were 75.8% at 5 years and 56.9% at 10 years. The interval from TES to IF peaked at 2-3 years postoperatively and continued to occur over a long period of time thereafter. In a comparison between the group in which IF occurred within 3 years postoperatively (early IF group) and the group in which IF occurred after 3 years postoperatively, the early IF group had greater cage subsidence at one month postoperatively (CS1M) and more lumbar TES. CS1M ≧ 3 mm (HR, 5.20; 95% CI, 2.82-9.58; p < 0.001) and sole use of frozen autografts (HR, 2.86; 95% CI, 1.52-5.39; p = 0.001) were identified as independent risk factors for IF. Conclusion: The incidence of IF after TES was high, with most failures being rod fractures preceded by cage subsidence and kyphotic enhancement of the instrumented level. IF can occur not only several years postoperatively but also in the late postoperative period. Cage subsidence in the early postoperative period and sole use of frozen autografts were independent risk factors related to IF. More robust spinal reconstruction and high-quality bone grafting should be employed for successful reconstruction after TES.
819
P588: Management of aggressive vertebral hemangioma (AVH) and assessment of radiological differentiating pointers between AVH and metastases - A systematic review
Subramaniam Haribabu 1 , Victor Moirangthem 2 , Muralidharan Venkatesh 3
1 Spine Surgery, Apollo Specialty Hospitals, Perungudi, Chennai, India
2 Dept. of Orthopaedics and Spine Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India
3 Spine Surgery, Apollo Hospitals, Chennai, India
Study design: Systematic review. Objective: Vertebral haemangioma has been classified into typical and aggressive vertebral haemangioma (AVH). Management options for AVH are many and clinician has decision making dilemma in choosing the right option. Metastases mimic AVH in clinical and radiological presentation. Differentiating pointers between them has not been clearly delineated in literature. Aim of our review is to identify treatment options; to formulate a management algorithm for AVH based on clinical presentation and to identify radiological differentiating pointers between them. Materials and Methods: Systematic review was conducted according to PRISMA guidelines. We systematically reviewed all available literature from year 2001 to 2020. Randomized controlled studies, observational studies including retrospective and prospective studies were searched via PubMed, Science Direct, and Ovid Medline databases. The keywords “Vertebral” AND haemangioma, “Aggressive” AND haemangioma, “Atypical” AND haemangioma, “Spinal” AND haemangioma and their combination MeSH terms were searched for analysis. Studies conducted before year 2000, studies quoting the number of patients less than 5, meta-analyses, systematic reviews, and case reports were not included in the evaluation. Grand rounds, expert comments, studies with follow-up less than one-year, non-spine studies were excluded. Abstracts of all the articles obtained with electronic database search were reviewed. The risk of bias assessment of included studies were assessed using MINORS -methodological index for non-randomised studies criteria. The systematic review was registered with ‘PROSPERO’ vide reference number: CRD42021266613. Results: We included 8 studies into the systematic review of AVH, of which four were retrospective and four were prospective in nature. 99 patients had undergone management, of which female were 59 in number and male were 40. Mean age of patients was 44.8 years and mean follow-up period was 26.1 months. A total of 88 haemangiomas have been treated with predominant location being thoracic spine (59), followed by lumbar spine (23), cervical spine (4) and sacrum (2). Mean duration of symptoms was 11.3 months (3 studies had not provided mean duration of symptoms). Clinical presentation of patients include back pain and myelopathic symptoms (45.4%), local back pain alone (34.3%), back pain and radicular symptoms (9.0%), pathological fracture (9.0%) and 2% of patients had presented during their pregnancy. Patients with backpain-myelopathic symptoms had improved following Surgery; patients with back pain alone had improved with either Percutaneous vertebroplasty or CT guided alcohol ablation. Dynamic contrast MRI, Diffusion weighted MRI and ratio of signal intensity between T1w and fat suppression T1w MR help the clinician in the differentiation of AVH from metastases. Conclusion: Management of AVH can be based on patient’s clinical presentation. Patients presenting with AVH and back pain can be managed with either Percutaneous vertebroplasty or CT guided alcohol ablation. Patients presenting with AVH and neurological symptoms could be managed with surgery. Dynamic contrast enhanced MR, Diffusion weighted MR, ratio of signal intensity betweenT1w and Fat suppressionT1w MR imaging could help clinician in differentiating the two before contemplating biopsy. Grade practice recommendation: C
Keywords: vertebral haemangioma; haemangioma; metastases; systematic review; surgery
930
P589: Management of spinal cavornous malformation - Our experience
Biswaranjan Nayak 1
1 Neurosurgery, Kalinga Hospital Limited, Bhubaneswar, India
Introduction: Cavernous malformations (CMs) of the central nervous system are abnormally dilated blood vessels, lined by a thin endothelium without intervening normal nervous tissue. Spinal CMs account for 5-12% of all spinal vascular lesions. Intramedullary CMs are very rare. CMs in the conus medullaris account for 4% of all intramedullary spinal CMs. The male:female ratio varies from 1:1 to 1:3. Patients become clinically symptomatic during the third and fourth decade of life. These lesions are usually solitary but in about 27% cases, they are associated with intracranial CMs. The usual clinical presentation is pain, weakness, sensory deficit and bladder/bowel dysfunction. Since the advent of magnetic resonance imaging (MRI), only few cases of this relatively rare lesion have been reported. Here, we describe the clinical, neuroradiological, and surgical features of a case of intramedullary CM in the conus medullaris of the spinal cord. Material and Methods: Surgical excision is the management of choice in these cases. Complete excision under the guidance of neuromonitor is ideal. We have encountered some interesting cases of this rare entity, which were removed completely with excellent results. Conclusion: Spinal CMs are very rare lesions. Appropriate neurological evaluation, and hence, an early diagnosis and proper treatment can prevent rebleeding, enlargement of the lesion, and dangerous clinical consequences associated with the lesion.
982
P590: Giant spinal chwannomas. Presentation of two cases with interdisciplinary surgical resection
Carlos Erosa Velázquez 1,2 , Edwin Rolando Sánchez Vallejo 3 , Sergio Ivan Reyna Heredia 1 , Apolinar de la Luz Laguna 1
1 Neurosurgeon - Spine Surgeon, Centro Médico Nacional 20 de Noviembre, Mexico City
2 Neurosurgery, Hospital General Agustín O Horán, Merida, Mexico
3 Neurosurgery, SNTE 50 Hospital, Monterrey, Mexico
Introduction: Schwannomas originating from Schwann cells in the neural sheath are typically benign and slow-growing tumors. While spinal schwannomas are relatively rare, giant spinal schwannomas, defined by their size and extension, pose unique challenges in diagnosis and treatment. Material and Methods: This study reports two cases of giant spinal schwannomas—one in the cervical spine and the other in the thoracic spine. Both cases presented with distinct clinical symptoms, requiring thorough diagnostic evaluation using MRI and CT scans. Surgical resection was chosen as the treatment modality due to the severity of symptoms and the involvement of critical neural structures. Results: In both cases, surgical resection achieved complete remission of symptoms with no major deficits postoperatively. The procedures were performed by multidisciplinary teams, combining neurosurgical and oncosurgical expertise for optimal outcomes. The surgeries were successful, with minimal blood loss and no intraoperative complications. Conclusion: This study highlights the clinical significance of giant spinal schwannomas, which can lead to visible lumps in the back and radicular symptoms. When symptomatic, surgical resection, often involving interdisciplinary teams, offers excellent results. Understanding the complex nature of these tumors and their varied clinical presentations is crucial for effective management.
1012
P591: Surgical outcomes of total excision for tumors of cervical spine
Kazuhiro Nanpo 1 , Satoshi Kato 1 , Noriaki Yokogawa 1 , Takaki Shimizu 1 , Masafumi Kawai 1 , Yuji Ishino 1 , Satoru Demura 1
1 Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kanazawa University, Kanazawa, Japan
Introduction: Due to anatomical features such as the presence of vital structures like the vertebral artery and cervical spinal nerves, as well as the anterior Luschka joint, en bloc resection of cervical spine tumors is often impractical, and complete tumor removal can also be challenging. Therefore, while surgery for cervical spine tumors has many limitations, our department actively performs total tumor resection procedures for cases where curative resection is desirable. This study examined the clinical outcomes of radical surgery for cervical spine tumors. Material and Methods: We targeted 16 cases that underwent total tumor resection surgery for cervical spine tumors at our hospital between January 2007 and December 2022, and were observable for over 1-year post-surgery (average age: 34.3 years, average observation period: 78.7 months). They included 13 cases undergoing initial surgeries and 3 cases undergoing revision surgery for recurrence after surgery at other institutions. They consisted of 11 cases with primary tumors (5 giant cell tumors, 3 osteoid osteomas, 1 osteochondroma, 1 chondrosarcoma, and 1 chondroblastoma), and 5 cases with metastatic tumors (primary origin: 3 renal cancers and 2 thyroid cancers). Results: While total tumor resection was achieved in all 16 cases, total en bloc spondylectomy was performed in only 2 cases of C7 tumors, with the remaining 14 cases requiring piecemeal total resection. During surgery, all cervical spinal nerves were preserved. Posterior approach was performed in 9 cases (56.3%) and combined anterior and posterior approach in 7 cases (43.7%). Local recurrence after curative surgery was observed in only 1 case (6.3%), which was a chondrosarcoma that recurred after surgery at another institution, with a recurrence period of 23 months. Among the 13 cases of initial surgery, no recurrences were observed, while recurrence was noted in 1 case (33.3%) of recurrence after surgery at another institution. There were 2 cases of postoperative mortality (12.5%), and the median survival was 119 months. Complications after surgery included upper limb muscle weakness in 6 cases (37.5%), reoperation due to infection caused by esophageal perforation in 1 case (6.3%), and reoperation due to cerebrospinal fluid leakage in 2 cases (12.5%). There were no cases of implant breakage requiring reoperation. Discussion: Complete resection of cervical spine tumors is feasible, although in most cases, piecemeal total resection was employed. Since there were no cases of highly malignant tumors among the cases studied, local recurrence was observed in only 1 case that recurred after surgery at another institution. Complications, including upper limb muscle weakness, were often observed, indicating that surgery for cervical spine tumors is technically demanding. Nonetheless, locally curative surgery for cervical spine tumors is possible and has shown favorable outcomes.
1145
P592: Lumbar spinal xanthoma - A rare tumour
Vishnu Senthil Kumar 1
1 Orthopedics,Government Royapettah Hospital, Chennai, India
Introduction: Xanthomas are non-neoplastic lesions often found in sub-cutaneous tissue. Primary Skeletal Xanthomas are rare. They are diagnosed incidentally and commonly present with pressure symptoms. Only four cases of spinal xanthoma have been reported in literature. We report of a rare case of solitary lumbar spinal xanthoma and its management. Case Report: 47 year old male presented with pain and swelling in the lumbar region for 6 month duration with no associated radiculopathy or myelopathy. Clinical examination revealed a diffuse swelling over the postero-lateral aspect of lower back. Swelling was tender on palpation. Radiologically, a lytic lesion involving the right L3 hemi-vertebrae was seen in both X-Ray and CT. Extension of tumour into the para-vertebral region was seen in MRI. Blood investigations were within normal limits. There was a dilemma regarding the diagnosis and proceeded with a trans-pedicular biopsy. Histo-pathological examination confirmed as Xanthoma. Tumour was approached retro-peritoneally through antero-lateral approach. Tumour was excised in piecemeal and antero-lateral stabilisation done with titanium MESH cage extending from L2 to L4. Patient was on routine follow up and at 5 months showed Scoliosis and was planned for posterior stabilisation to avoid further collapse. Now at one year follow up, patient is not having any functional limitation. Conclusion: Skeletal xanthomas are rare expansive lytic lesions of the bone which mimic malignant bone tumours and other pathological conditions. HPE is confirmatory. Regular follow up is needed to watch for Xanthomatous degeneration of tumour and dyslipidaemia because it often co-exists with disorders of lipid metabolism.
1167
P593: Are there situations where minimal invasive spine surgery is less preferred over open spine surgery in the treatment of metastatic spine disease?
Si Jian Hui 1 , Naresh Kumar 1 , Renick Lee 1 , Sahil Athia 1 , Praveen Jeyachandran 1 , Shahid Ali 1 , Jiong Hao Tan 1
1 Orthopaedic Surgery, National University Health System, Singapore, Singapore
Objective: Metastatic Spine Tumour Surgery (MSTS) is an important treatment modality of Metastatic Spinal Disease (MSD). Open spine surgery (OSS) was previously the gold standard of treatment till the early 2010s. However, advancements in MSTS in recent years have led to the advent of minimally invasive spinal surgery (MISS) techniques for the treatment of MSD. The clear benefits of MISS have resulted in a current paradigm shift towards today’s gold standard of MISS and early adjuvant RT in treating MSD patients. Nonetheless, despite the improvements in surgical techniques and the rise of literature supporting MISS for MSD, there are still certain situations whereby MISS is not desirable or even suitable. There has also yet to be any literature describing the considerations for not using MISS in MSD in today’s clinical context. Methods: This narrative review was conducted using PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), The Cochrane Library and Scopus databases through 31 Aug 2023. Inclusion criteria for the review were studies with discussion on the type of surgery in MSTS. All studies that had no description regarding the surgical procedure performed were excluded. The vast personal experiences of the senior authors also circumstantiated the various situations that were inappropriate for MISS. Results: A total of 43 studies were included in this review. We discussed advantages and various situations appropriate for MISS for MSD in today’s clinical context. Nonetheless, there are still various unique circumstances in which MISS may be less suitable. These are important considerations for MSTS surgeons, and OSS should be undertaken if MISS is less feasible. The considerations can be split into i) the profile of MSD patients, ii) the location of vertebrae involved with metastasis, iii) tumour characteristics, as well as iv) other miscellaneous factors such as equipment and adjuvant therapy availability. MISS is less feasible in patients of paediatric profile, having short stature or having had previous surgery at the level of operation. Occipitocervical and cervicothoracic location of vertebrae metastasis also makes MISS less feasible due to access and imaging difficulty. MISS for tumours which are hypersclerotic and hypervascular can also result in more difficulty for cannulation of MISS probes as well as control of bleeding respectively, and hence will be less encouraged in the above settings. The recommendations for the above considerations before undertaking MISS surgery should also be guided by the experience of the operating surgeon. Conclusion: Our manuscript is the first to discuss circumstances in which MISS is less applicable, despite the advantages it may confer over traditional OSS. MSTS should be individualized to the patient, depending on the experience of the surgeon. OSS is still a time-tested approach that holds weight in MSTS and should be readily utilised depending on the clinical situation.
Keywords: metastasis; spine, tumour; open surgery; minimally invasive surgery
1178
P594: Resection of sacral chordoma - A technical note
Vishnu Senthil Kumar 1
1 Orthopaedics, Govt Royapettah Hospital, Chennai, India
Introduction: Primary sacral tumours are rare. Sacral chordomas are common primary malignant tumours. They are often missed because of their vague presentation. CT and MRI are done for pre-operative planning. En bloc resection is the treatment of choice, however its anatomy can cause damage to vital perineal structures. Depending upon the size and extent of tumours, approach can vary. In our case series, we have approached the tumour by a single stage posterior approach. Materials and Methods: Retrospective analysis in a tertiary care institute from 2013-2016. Four cases of sacral chordoma were included in our study. Case 1:50 year old female was diagnosed with S2-S5 chordoma and minimal follow up of 4 years. Case 2: 38 year old male presented with low back ache and was diagnosed with S2-S4 sacral chordoma with minimal follow up of 3 years. Case 3: 48 year old female presented with low back ache and swelling was diagnosed with S3-coccyx chordoma with minimal follow up of 3 years. Case 4: 40 year old female presented with low back ache with S2-S3 sacral chordoma with minimal follow up of 3 years. Operative technique. Indwelling foley’s catheter and surgical pack in rectum. Patient placed in prone position with Relton-Hall four poster frame with hip and knee flexed to 90 degree. A curved bucket handle incision was made and the apex of incision was 5-7 cm cranial to the pre-determined proximal resection margin. A full thickness flap was elevated to expose the sacrum and sacro-iliac joint. Gluteus maximus, pyriformis, sacrospinous, sacrotuberous and sacro-coccygeal ligaments were divided and retro-peritoneal space was reached. Sacrum was separated from its anterior structures by blunt dissection. The posterior elements of S1 and S2 were removed by using Kerrison rongeur exposing the dural sac, S1,S2 and S3 nerve roots. Dural sac distal to S3 root root was ligated and exposing the post surface of body of sacrum. Proximal resection of tumour was carried out with osteotome through normal bone. Finally ano-coccygeal ligament was divided and tumour removed en bloc. If ilium osteotomy done, spino pelvic fixation is done. Post-operative mobilisation done as tolerated. Radiotherapy was given to chordoma patients and follow done at regular intervals to watch for recurrence, metastasis and measure functional outcome. Results: All patients had low back ache with no intra-operative complications. 2 patients had tumour margin positive and remaining negative. Tumour recurrence for 1 patient was at 3 years and another 1.5 years. No metastasis and recurrence was managed with radiotherapy. Discussion: All tumours were Wei type 2. Advantages of single stage posterior approach are shorter operation time with less blood loss. In our case series, 90 degree positioning, deliberate hypotension and bucket handle shaped incision allowed easier lateral soft tissue dissection with better exposure of sacro-iliac joints. Cranial apex in incision prevented exposure to rectum and sacrum. Laminectomy of S1 and S2 allowed identification of caudal roots of sciatic nerve. Conclusion: Sacral chordomas can be safely resected through a single stage modified posterior approach which carries minimal intra-operative complications. The functional and oncological outcomes are comparable to other surgical procedures. Limitations were sample size and medium term follow up.
1180
P595: Primary tumor resection prolongs survival in spinal chondrosarcoma patients with distant metastasis
kaiyuan lin 1 , Xinsheng Peng 2
1 Department of Orthopaedic Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
2 Department of Orthopaedic Surgery, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, China
Summary of background data: Surgical resection is the mainstay of treatment for spinal chondrosarcoma, as chondrosarcoma is inherently resistant to radiotherapy and chemotherapy. However, evidence which justifies resection of the primary tumor for patients with metastatic spinal chondrosarcoma is still lacking. Methods: We retrospectively included 110 patients with metastatic spinal chondrosarcoma in the Surveillance, Epidemiology, and End Results database from 1983 to 2016. The association between primary tumor resection and survival was evaluated using Kaplan-Meier analyses, log-rank tests, and multivariable Cox analyses. The effect of primary tumor resection on survival was further assessed in subgroups stratified by histologic subtype, tumor grade, and age. Results: Overall, 110 patients were divided into surgery group (n = 55, 50%) and nonsurgery group (n = 55, 50%). Primary tumor resection was associated with both prolonged overall survival (hazard ratio 0.262, 95% confidence interval 0.149-0.462, p < 0.001) and cancer-specific survival (hazard ratio 0.228, 95% confidence interval 0.127-0.409, p < 0.001). When we focused on surgical effects in subgroups, primary tumor resection conferred survival advantage on patients with conventional subtype, grade I to III malignancy, and an age younger than 70 years old (p < 0.001 for overall and cancer-specific survival). However, primary tumor resection brought limited survival benefit for patients with dedifferentiated subtype and patients over 70 years old. Conclusion: The present population-based study for the first time reports a clear association between primary tumor resection and prolonged survival in metastatic spinal chondrosarcoma patients. Specifically, primary tumor resection was associated with improved survival in patients with conventional subtype, grade I to III malignancy, and an age younger than 70 years old.
1186
P596: Predict overall survival of spinal conventional chordoma: development and assessment of a new predivtive nomogram
Kaiyuan Lin 1 , Xinsheng Peng 2
1 Department of Orthopaedic Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
2 Department of Orthopaedic Surgery, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, China
Objective: To predict the 5-year overall survival (OS) rate in patients with conventional chordoma of the spine. Patients and Methods: The Surveillance, Epidemiology, and End Results (SEER) Registry was used to identify patients with conventional chordoma of the spine from 1994 to 2013. The entire cohort (n = 294) was randomly divided into training (n = 147) and validation (n = 147) cohorts to construct a nomogram. We used the univariate Log-rank test and multivariate Cox model to examine the independent prognostic factors associated with OS. These prognostic factors were integrated to construct a nomogram through R studio. The predictive and validating capacity of the nomogram was calculated by Harrell's concordance index (C-index) and calibration curves. Results: A total of 294 patients were identified with conventional chordoma of the spine. The patients' age at diagnosis, tumor size, EOD (extent of disease), and treatment were independent prognostic factors and associated with OS. These prognostic factors were incorporated to construct a nomogram. The concordance index for the nomogram was 0.771 and 0.732 in the training cohort and validation cohort, respectively. Internal and external calibration curves for 5-year OS showed excellent matching between nomogram prediction and observed outcomes. Conclusions: The findings of this study provide population-based estimates of patients with conventional chordoma of the spine. Using this nomogram, surgeons can classify patients into different risk groups and achieve individualized treatment.
1191
P597: Microstructural features of the endplate are associated with the failure of metastatic vertebrae
Marco Palanca 1 , Giulia Cavazzoni 1 , Camilla Morbidelli 1 , Erica Turchi 1 , Luca Cristofolini 1 , Enrico Dall'Ara 2
1 Department of Industrial Engineering, Alma Mater Studiorum - University of Bologna, Bologna, Italy
2 Department of Oncology and Metabolism, The University of Sheffield, Sheffield, United Kingdom
Introduction: Bone metastases compromise the optimization of the vertebral trabecular pattern [1]. Indeed, the vertebral microstructure can be affected in different ways resulting in an increase of the risk of fracture. Despite it has already been observed that failure frequently initiates from the endplates, the mechanisms underlying failure need to be elucidated [2]. This study aims to identify the features of the vertebral endplates that are associated with the failure of metastatic vertebrae. Materials and Methods: 15 spine segments consisting of a metastatic vertebra (6x lytic, 6x mixed, 3x blastic) and a control vertebra were tested in axial compression up to failure inside a microCT scanner (VivaCT80, Scanco Medical Ltd, CH). The specimens were imaged (isotropic voxel size = 39 um) in their unloaded configuration and after failure. The unloaded scans were used to evaluate the microstructural features of the endplates. Two regions of interest (ROI, 2mm thick) were manually segmented below the cranial and above the caudal endplate. Each ROI was divided in nine squared sub-regions of interest (subROI), by diving the ROI in three parts along the anterior-posterior and the left-right directions. Microstructural properties (i.e. bone volume fraction (BV/TV), trabecular thickness (Tb.Th.), trabecular separation (Tb.Sp.), trabecular number (Tb.N.), trabecular pattern factor (Tb.F.)) were evaluated (CTAn, Bruker, USA) [3] on each ROI and sub-ROI. The unloaded and failure scans were used to evaluate the internal deformations through a global Digital Volume Correlation approach (BoneDVC, University of Sheffield, UK). One-way ANOVA was used to evaluate the significance of microstructural differences, measured in the ROIs, among the different types of vertebrae. The association between the microstructural features of the endplate and deformation maps of the failed endplates [2] was explored [4] to identify the most critical sub-ROIs. Results: The BV/TV, Tb.N. and Tb.F. measured in the ROIs for vertebrae with lytic, mixed, and blastic metastases and control vertebrae differed significantly (p < 0.05). In particular, endplates of vertebrae with blastic metastases showed the largest BV/TV and Tb.N., followed by vertebrae with mixed metastases, control vertebrae and vertebrae with lytic metastases. Opposite trend was found for the Tb.F. that was lowest for the endplates of vertebrae with blastic metastases, followed by the mixed metastases, lytic metastases and control vertebrae. The largest compressive deformations, close to failure ones, were measured with BoneDVC in the subROIs with the smaller BV/TV (4/19 times), the smaller Tb.Th. (4/19), the smaller Tb.N. (7/19), the largest Tb.Sp. (5/19), the smaller Tb.F. (3/19). Conclusion: In situ biomechanical tests and high-resolution imaging allowed to identify the association between the local variation of the microstructure and failure patterns in metastatic vertebrae [4]: areas with a high average distance between the trabeculae, characterized by low trabecular density, are more subjected a deflection and at risk of fracture.
References
1. Cavazzoni et al. Front BioeEng Biotech 2023
2. Palanca et al. Bone 2023
3. Bouxsein et al. JBMR 2010
4. Hussein and Morgan. Osteoporosis In 2013
Acknowledgements
The study was partially funded by AOSpine (AOSDIA_2019_063), Marie Skłodowska-Curie (MSCA-IF-EF-ST, 832430/2018) and EPSRC Multisim Grant (EP/K03877X/1 and EP/S032940/1).
1317
P598: Unusual location of a malignant paraganglioma: about a case
Hassan Hachicha 1 , Habboubi Khalil 1 , Mohamed Ali Triki 1 , Meddeb Mehdi 1 , Hassen Makhlouf 1 , Mondher Mestiri 1
1 Adultes Department, Mohamed Kassab Institute, Mannouba, Tunisia
Introduction: Thoracic paragangliomas are neuroendocrine chromaffin tumors of extra-adrenal location, representing approximately 1/5th of chromaffin tumors. These are benign tumors. Only 10 to 15% are malignant and defined by the presence of metastases in nonchromaffin tissue. The management of malignant paragangliomas requires a multidisciplinary collaboration. Presentation of the Cases: This was a 35-year-old patient, single, with no notable pathological history, smoker (8PY) weaned 4 months ago. The main symptomatology was epigastralgia dating back 4 years, not improved by symptomatic treatment. The general condition was preserved with a weight of 70 kg, a height of 1.75 m and a BMI of 22.9 kg/m2. The patient was eupneic, a blood pressure of 12-6. The biological assessment was normal as well as the ECG. The AP chest X-ray showed right mediastinal opacity. The thoraco-abdomino-pelvic CT scan showed a large oval right posterior mediastinal mass, with regular contours, well limited, hypo dense, heterogeneous enhancement measuring 12*10*11 cm. It invades the posterior chest wall with lysis of the posterior arch, of the costo-transverse and costo-vertebral joints of the right 9th rib as well as the vertebral hemibody of T9 and T10 exerting a scalloping on the post arc of the 10th right side with extension of the tumor coming into contact with T8 and T11. This mass invades the midline, pushes back the right lower lobe and comes into contact with the posterior wall of the descending thoracic aorta next to T9. It is vascularized by a voluminous tortuous intercostal artery. Our patient benefited from an embolization before the biopsy which confirmed the diagnosis of a malignant paraganglioma. The intervention took place in 3 stages: 1st stage: a postero-lateral left thoracotomy freeing the descending aorta and the anterior surface of the vertebral bodies from T6 to T10. 2nd stage: a right posterolateral thoracotomy for the costotomy of the 8th and 9th ribs, excision of the tumor. 3rd stage: posterior approach to the dorsal spine from D5 to L2 for a right hemi-laminectomy D7 D8 D9, ligation of the straight D7 D8 D9 roots, transcorporeal bone section D8 D9 carrying half of the vertebral bodies, anterior fibula graft taken from the side left and unilateral synthesis D5D6-D10D11. Results: The post operative exam were simple with disappearance of the epigastralgia. The neurological examination showed right D7,8,9 anesthesia. The postoperative X-ray showed disappearance of the tumor and arthrodesis and a graft in place. Histological examination confirmed the initial diagnosis. Conclusion: Malignant paragangliomas are rare and aggressive tumors. However, their management remains very complex and specific. Prospective trials are necessary for a better characterization of these tumors in order to be able to improve the management of this tumour.
1408
P599: Conditional survival analysis for spinal chondrosarcoma patients after surgical resection
Kaiyuan Lin 1 , Xinsheng Peng 2
1 Department of Orthopaedic Surgery, Honghui Hospital, Xi'an Jiaotong University, Xi'an, China
2 Department of Orthopaedic Surgery, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, China
Summary of Background Data: Survival estimates are usually reported as survival from the time of surgery, but survival probabilities can change over time. Conditional survival, which is a measure of prognosis for patients who have survived a defined period of time, may be more clinically precise and relevant. However, data on conditional survival for spinal chondrosarcoma patients after surgical resection are still lacking. Methods: We used the Surveillance, Epidemiology, and End Results (SEER) database to identify 436 spinal chondrosarcoma patients who underwent surgical resection from 1994 and 2013. Kaplan-Meier analyses and Cox regression modeling were performed to evaluate prognostic factors associated with overall survival. Five-year conditional survival (i.e., probability of surviving an additional 5 years, given that a patient has already survived x years) was calculated as 5-CS(x) = OS(x+5)/OS(x). The effect of prognostic factors on conditional survival was also explored. Results: Four hundred thirty six patients were included in the study cohort. Overall, 1-, 3-, and 5-year overall survival were 92.8%, 79.1%, and 70.3%, respectively. Five-year conditional survival at 1, 3, and 5 years after surgery were 72.9%, 79.0%, and 87.5%. The overall survival rates were lower in cases of age more than or equal to 60 years, male patient, dedifferentiated subtype, Grade III tumor, tumor size more than or equal to 10 cm, distant metastasis, and radiotherapy. Conditional survival improved over time in each subgroup divided by age, sex, race, year of diagnosis, grade, tumor size, extent of disease (EOD), and radiotherapy. In addition, patients with the least favorable prognosis at baseline experienced the greatest increase in 5-year conditional survival over time (e.g., Grade I/II: 78.0%-89.7%, Δ11.7% vs. Grade III: 36.5%-66.6%, Δ30.1%; Localized/Regional: 72.9%-88.1%, Δ15.2% vs. Distant: 43.5%-74.1%, Δ30.6%). Conclusion: Conditional survival for spinal chondrosarcoma patients after surgical resection improves over time, especially for patients with initial high-risk characteristics. Information derived from conditional survival analysis may provide individualized approaches to surveillance and treatment of spinal chondrosarcoma.
1431
P600: In vitro and in vivo investigation of tumor treating fields for treatment of spinal metastasis
Daniel Ledbetter 1 , Claudio Tatsui 1 , Christopher Alvarez-Breckenridge 1
1 Neurosurgery, M.D. Anderson Cancer Center, Houston, USA
Introduction: Metastatic disease to the spine is a significant source of disability and suffering for cancer patients. Despite advances in treatment, many cases will recur and reach the limits of the standard of care, highlighting the need for novel therapies. While tumor treating fields (TTFields) are used for treatment of glioblastoma, TTFields use in spinal metastasis has never been described. Here, we evaluate the ability of TTFields to inhibit the growth of human cancer cells in models of spinal metastasis, in vitro and in vivo. Methods: In vitro: Luciferase-tagged human osteosarcoma (KRIB-mCherry-Luc) and lung adenocarcinoma (A549-mCherry-Luc) cells were seeded in human demineralized cancellous bone grafts with and without titanium screws (simulating spinal fusion instrumentation) and maintained in culture while treated with 150 kHz TTFields for 14 days. Bioluminescence images (BLI) were obtained at baseline and 14 days. Following the treatment period, cell growth was analyzed by CellTiter-Glo (CTG) viability assay. In vivo: KRIB-mCherry-Luc cells were surgically implanted via transperitoneal approach into L3 vertebral body in nude mice. Animals were treated with TTFields at a frequency of 150 kHz or 0 kHz (control) for 40 days or until paralysis. Tumor growth was monitored by BLI (weekly), MRI at days 14 and 22 after tumor implantation, and cord compression-associated neurological deficits. Histological analysis was performed following the treatment period. Results: In vitro: Analysis of BLI at day 14 relative to baseline imaging showed a decrease in luminescence of the 150 kHz TTFields groups to 10% (KRIB-mCherry-Luc) and 80% (A549-mCherry-Luc), while control groups had increased to 448% and 936%, respectively, and there was no detectable disruption to the therapeutic effect in bone grafts containing titanium screws. Viable cell number within control groups increased 125-fold and 6-fold over 150 kHz TTFields groups (p < 0.0005, p < 0.05). In vivo: Milestones of spinal cord compression, (tail drop, dorsal-stepping, and hind limb paralysis) were observed at 16.5 days and 31 days post-implantation in control animals, while only 50% of TTFields-treated animals showed signs of cord compression (median 24 days) and no TTFields-treated animals were paralyzed by the study endpoint (day 40). MRI confirmed smaller tumors corroborating BLI (2.1x109 vs 1.7x1010 photons/sec) (p < 0.05) when the TTFields treatment group was compared to controls. Conclusions: Application of TTFields at a frequency of 150kHz reduced cellular proliferation in both in vitro and in vivo models of spinal metastasis. This is the first report of utilization of TTFields for treatment of bony tumors and represents the first evidence that TTFields may be a feasible and novel therapy for spinal metastasis.
1439
P601: Shade of Brown: Browns tumor of the thoracic spine
Nachimuthu Maniventhan 1 , Logheswaren Suppiah 1
1 Orthopaedics, Hospital Raja Permaisuri Bainun, Ipoh, Malaysia
Introduction: Brown tumor of the bone, also known as osteitis fibrosa cystica or osteoclastomas is a rare manifestation of hyperparathyroidism, most seen nowadays in association with secondary and tertiary hyperparathyroidism. Material and Methods: 34 years old lady with underlying renal failure for the past 13 years on regular hemodialysis, presented to us with the chief complaint of difficulty in standing and walking due to leg weakness for nearly 1 week. She has not been able to ambulate, gradually weakening power of the lower limbs. She had no prior trauma or systemic infection. Suspecting possible malignant tumor of the spine due to the acuteness of the condition, she was admitted for further investigation. Blood tests were uneventful except for Alkaline Phosphatase value was 923 and also had elevated Parathyroid Hormone (PTH) with value of 335.73 pmol/L. she then proceeded with Magnetic Resonance Imaging (MRI). MRI revealed expansile soft tissue mass measuring 1.6cm x 5.8cm x 4.8cm seen involving the bilateral pedicles, laminas and transverse process of T9 vertebrae body as well as bilateral superior articulating process and spinous process, leading to stenosis at this level. Bilateral T9/T10 exit foramina was also obliterated. Patient underwent decompressive spine surgery followed by posterior instrumentation and fusion. Tumor was excised, posterior decompression followed by T7-11 posterior instrumentation and fusion. Results: Her neurological impairment unfortunately, didn’t recover and remains to be same as during presentation. She proceeded to mobilize herself with the help of a wheelchair postoperatively up to the date of her discharge from ward. Histopathological report were consistent Brown’s tumor. Conclusion: The diagnosis of brown tumors can easily be missed when we are more concerned about more sinister conditions such as malignancy, more so in patients with neurological deficit. Although imaging could help identify the location, suggest possible diagnosis and guide your treatment, a biopsy is always more useful in distinguishing the lesion between benign from malignant lesion. Although less reported, instances of spinal cord involvement that leads to impairment of lower limb neurology is still present, such as our patient. Early detection would lead to timely treatment.
1458
P602: The effectiveness of preoperative arterial embolization for metastatic spinal tumors
Satoshi Fujiwara 1 , Tokumitsu Mihara 1 , Shinji Tanishima 1 , Chikako Takeda 1 , Hideki Nagashima 1
1 Division of Orthopedic Surgery, Faculty of Medicine, Tottori University, Yonago, Japan
Introduction: In surgery for metastatic spinal tumors, it is important to control blood loss. With advances in cancer treatment, the number of surgical cases is increasing and the primary sites vary. Preoperative arterial embolization of hypervascular tumors has been reported to be useful, but there are not many reports including other types of cancer. After our experience with a case in which embolization reduced the amount of blood loss, we have been actively requesting embolization from the radiology department. Objective: To compare the usefulness and complications of preoperative arterial embolization for metastatic spinal tumors from a retrospective perspective. Methods: Thirty-seven patients who underwent decompression and fusion surgery for metastatic spinal tumors at our hospital between April 2011 and December 2021 were included in the study, and were compared with and without preoperative arterial embolization (embolization group: 10 patients, non-embolization group: 27 patients). The study items were age, gender, primary site, elevation, surgical technique (number of decompressed and fixed vertebrae), operative time, and blood loss. Results: Age was significantly higher in the embolization group. There were no significant differences in other parameters including blood loss. The primary site of embolization varied from lung cancer, breast cancer, and colorectal cancer to prostate cancer, multiple myeloma, and other cancers. The mean time for embolization was 185 minutes, and there were no complications from embolization. In one case of primary kidney cancer, the presence of Adamkiewicz artery prevented adequate embolization. The patient required reoperation due to complete paralysis from a postoperative hematoma caused by increased intraoperative blood loss. Discussion and Conclusion: In this study of various cancer types, there was no significant difference in the amount of blood loss between embolization and no embolization. The degree of tumor invasion varied from case to case, and embolization may have resulted in adequate resection. Therefore, it is quite possible that embolization reduces the amount of bleeding, although there were no significant differences in this study. On the other hand, there have been reports of spinal cord infarction caused by arterial embolization, so careful indication in cooperation with the Department of Radiology is recommended.
1473
P603: Clinical outcomes of recapping T-saw laminoplasty for thoracic spinal cord tumors
Masafumi Kawai 1 , Satoshi Kato 1 , Noriaki Yokogawa 1 , Takaki Shimizu 1 , Yuji Ishino 1 , Kazuhiro Nanpo 1 , Satoru Demura 1
1 Orthopedic Surgery, Kanazawa University, Kanazawa, Japan
Introduction: Surgical resection of spinal cord tumors is generally performed using a posterior approach with a wide laminectomy; however, several postoperative complications, such as kyphotic deformity and the formation of laminectomy membranes, may occur. Laminoplasty solves these problems; however, its conventional approach does not provide a sufficient surgical field of view, making it difficult to completely resect large tumors or those that invade the intervertebral foramen like dumbbell tumors. Although resection of the intervertebral joint provides a wider field of view, spinal stability is lost and instrumented reconstruction is required after tumor resection. To provide an excellent surgical field and allow for the physiologic and anatomic reconstruction of the vertebral arch after the excision of spinal cord tumors, we have developed and performed a surgical technique in which the requisite posterior elements are removed and replaced (“Recapping T-saw laminoplasty”). This study investigated the surgical outcomes of recapping T-saw laminoplasty for spinal cord tumors. Material and Methods: We retrospectively analyzed the clinical and radiological data of 40 patients who underwent recapping T-saw laminoplasty for thoracic spinal cord tumors at our hospital between January 2011 and March 2021. Patients who were followed up for more than two years after surgery were included in the study, with a mean follow-up duration of 62.7 months (range 24-109 months). Surgical outcomes included operative time, blood loss, tumor resection rate, intraoperative and postoperative complications, postoperative back pain, functional status assessment (the modified Japanese Orthopedic Association [JOA] scoring system and Frankel grade), radiological assessment (bone union, kyphosis deformity > 10°), and rates of local recurrence and reoperation. Results: The mean age at the time of surgery was 56.1 years; there were 13 men and 27 women. The number of resected vertebral arches was one for 28 cases, two for 10 cases, and three for 2 cases. The tumor types included schwannomas in 19 patients, meningiomas in 16, and others in 5; dumbbell tumors were observed in 9 patients. The mean operative time and blood loss were 226 min and 142 ml, respectively. Complete resection was performed for 38 tumors, and 2 tumors were partially resected. Postoperative complications were observed in 8 patients, including neurological complications in 5 and continuous cerebrospinal fluid leakage in 5. Two patients complained of back pain one year postoperatively. Improvement in the modified JOA score was observed in 34 patients one year postoperatively. Bone union was observed in all cases on computed tomography at the 1-year follow-up. Postoperative kyphotic deformity was observed in 7 cases, with all of these having two or more vertebral arches resected. Tumor recurrence was observed in two cases with meningiomas, which required reoperation, and no revision surgeries were performed due to kyphotic deformity or postoperative complications. Conclusion: Recapping T-saw laminoplasty for thoracic spinal cord tumors has shown favorable clinical outcomes. This procedure allows anatomical reconstruction of the posterior arch and reservation of biomechanical function, as well as a wide surgical field of view for a safe and complete tumor resection.
1513
P604: Implant and construct decision making in metastatic spine tumour surgery: a review of current concepts and illustration of a decision making algorithm
Naresh Kumar 1 , Si Jian Hui 1 , Sahil Athia 1 , Renick Lee 1 , Praveen Jeyachandran 1 , Jiong Hao Tan 1
1 Department of Orthopaedic Surgery, National University Hospital
Introduction: Metastatic Spine Tumour Surgery (MSTS) is an important treatment modality of Metastatic Spinal Disease (MSD). Increase in MSTS has been due to improvements in our oncological treatment, as patients have increased longevity and even those with poorer comorbidities are now being considered for surgery. However, there is currently no guideline on how MSTS surgeons should select the appropriate levels to instrument and which type of implants should be utilised. We aim to review the literature and highlight personal experiences from our own unit and senior authors, regarding the various crucial factors to be considered in decision making for the implant and construct in MSTS. Material and Methods: A narrative review was conducted for this paper using PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), The Cochrane Library and Scopus databases through 27 March 2023. The keywords used were “spine” AND “metasta*” AND (“instrument* OR implant*)”. All studies that were related to instrumentation in MSTS were included to create the guideline and algorithm. All studies that had no description regarding the surgical procedure performed were excluded. The concept of our instrumentation decision-making algorithm was done as an expert opinion by the two senior spine surgeons in this manuscript, with experiences from treating and observing patients with MSTS, as well as interaction with members of ‘Arbeitsgemeinschaft für Osteosynthesefragen (AO) – Knowledge Forum Tumour’ and ‘FTEG - Fracture Tumour Expert Group’. Results: A total of 60 studies were included in this review. We discussed a new decision-making model that should be taken into account when planning for surgery in patients undergoing MSTS. These factors include the quality of bone for instrumentation, the extent of the construct required for MSTS patients, the use of cement augmentation and the choice of implant. Various studies have advocated for the use of these modalities and demonstrated better outcomes in MSTS patients when used appropriately. Our proposed stepwise algorithm involves first considering MSD patients’ fitness for surgery, to see if MSTS should be undertaken. This can be done through generic tumour surviving scoring systems, and frailty of patients assessed through internationally validated performance scores. The discussion and approach to surgery for patients with intermediate SINS has to be individualised, taking into account other factors such as their pre-existing comorbidities and tumour subtype, which have all shown to be important factors influencing survival outcomes. If patients are fit for surgery, the various factors affecting instrumentation choice should be deliberated on pre-operatively prior to surgery itself to ensure optimal outcomes for MSD patients. However, if they are not fit for surgery, either radiotherapy or palliative care should be discussed with them. Conclusion: We are the first to discuss and establish a new algorithm that should be taken into consideration for patients undergoing MSTS. It serves as an important guide for surgeons who are treating MSD with MSTS, due to the continuous evolvement of our treatment capacity in MSD.
Keywords: instrumentation; metastasis; spine; tumour; implant; algorithm
1594
P605: Application of a new co-axial bipolar electrode for the treatment of vertebral metastases: a pilot study in sheep
Francesca Salamanna 1 , Matilde Tschon 1 , Giuseppe Tedesco 2 , Lucia Martini 1 , Giovanni Barbanti Bròdano 2 , Gianluca Giavaresi 1 , Alessandro Gasbarrini 2 , Milena Fini 3
1 Surgical and Technological Sciences
2 Spine Surgery
3 Scientific Direction, IRCCS Istituto Ortopedico Rizzoli, Bologna, Italy
Introduction: Skeletal metastases are a common cause of severe morbidity, reduced quality of life, and often early mortality. Consequently, improvements in therapies are necessary. Electroporation uses electrical energy to alter cancer cell membrane permeability and enhance the local uptake of chemotherapeutics, thus leading to local tumor control. The aim of this study was to investigate the safety of delivering electric field protocols causing electroporation using new co-axial bipolar electrodes in healthy bone and clinically relevant structures, employing a large animal model. Material and Methods: Irreversible electroporation was used on six sheep vertebral bodies by applying 120 pulses, each 100 ms long, at 1750 V/cm. Three treatment configurations were performed to identify the maximum volume of effectively ablated area. Each configuration was tested on n = 2 sheep: i) insertion of a single co-axial bipolar electrode into vertebral body; ii) insertion of 2 co-axial bipolar electrodes into 2 adjacent vertebrae; iii) insertion of 2 co-axial bipolar electrodes into 2 non-adjacent vertebrae. To label bone formation, oxytetracycline was injected on the third day after surgery. At 7 days post-surgery, animals were pharmacologically euthanized, and vertebral bodies and surrounding sensitive structures, such as the spinal cord, vertebral pedicles, and spinal nerves, were harvested. Results: Macroscopic, histological, and histomorphometric investigations demonstrated that irreversible electroporation removes bone lining cells from trabeculae in the vertebral bodies of sheep and does not cause structural or morphological alterations in the spinal cord, vertebral pedicles, or spinal nerves. These results were observed with all tested configurations. Conclusion: Collectively, the results of this study show that electroporation using the new co-axial bipolar electrodes can be safely applied to bone even in proximity to neuronal structures. These findings support the translation of this methodology into clinical practice, providing the rationale for the treatment of tumor nodules, even in the presence of critical anatomical structures, such as vertebral bone metastases.
1642
P606: Clinical profile and surgical management of sacral tumor: a national referred institutional experience in Indonesia
Mohamad Saekhu 1 , Fabianto Santoso 1 , Eka Susanto 2 , Syaiful Ichwan 1 , Renindra Ananda Aman 1 , Setyo Widi Nugroho 1
1 Department of Neurosurgery
2 Department of Pathological Anatomy, Faculty of Medicine Universitas Indonesia - Dr. Cipto Mangunkusumo General National Hospital, Jakarta, Indonesia
Introduction: Sacral tumors are rare, comprising 1%-7% of all spinal tumors. Histopathology of sacral tumors varies and can be benign or malignant. However, clinical demography or profile reports of sacral tumors are still limited. Sacral tumor management is a big challenge, especially in big-size tumors. Until now, patient criteria for aggresivity in sacral tumor resection is debatable. So, this study is a case series that shows the clinical profile and management of sacral tumors at our hospital as Indonesia's nationally referred hospital. Material and Methods: This is a retrospective study about sacral tumor patients treated between 2018 and 2022 at Dr.Cipto Mangunkusumo General National Hospital, Jakarta, Indonesia, a nationally referred hospital. We collect data about demography, clinical presentation, tumor size, histopathology, and management of sacral tumors from medical records. We analyzed descriptively to explain the profile and management of each case. Results: In five years, we have had 454 spinal cases patients who were operated on (1.7%) with four spinal tumor patients (9.5%) and eight of them were sacral tumor patients. The majority gender is female (75%) with a median age of 39 (15-67) years old. The symptoms of our cases are similar to other sacrum diseases. All cases have autonomic dysfunction, such as alvi and urine retention until overflow urine incontinence. The other symptoms were mono paresis and radicular pain (37.5%). Four patients (50%) had chordoma histopathological results; each had adenocarcinoma metastasis, Ewing sarcoma, solitary fibrous Tumor/hemangiopericytoma, and giant cell tumor. For chordoma patients, the volume of the tumor has a median of 1,200 (718.4 - 1,774) cm3. All the patients had subtotal resection tumor surgery and continued with adjuvant therapy, such as chemotherapy and radiotherapy. A chordoma patient had internal iliac artery embolization with Polyvinyl Alcohol (PVA) embolization. All of the chordoma patients only biopsy until subtotal resection without sacrectomy and continue with adjuvant therapy. A giant cell tumor had radiotherapy before surgery to reduce bleeding. All the patients had good outcomes. Conclusion: Sacral tumors have a clinical profile that mimics other sacrum diseases. Because of silent disease, sacral tumor patients come to hospitals with giant size. The principle of management in sacral tumors is decompression and adjuvant therapy perioperatively.
1665
P607: Feasibility of unilateral biportal endoscopic surgery removal intradural tumor: a case report and literature review
Warayos Trathitephun 1 , Siravich Suvithayasiri 1 , Jackapol Kamolpal 1
1 Orthopedic, Chulabhorn Royal Academy, Bangkok, Thailand
Introduction: Spinal cord tumors can be found in around 15% of all central nervous system tumors with annual incidents of less than 1 per 10000. Extramedullary, intradural spinal tumors (EISTs) is a very rare condition and comprise around 40% of all spinal tumor. Tumor removal for EISTs is challenging because of opening up thecal sac and awareness of spinal cord manipulation. Here we include the case of EISTs for unilateral bi-portal endoscopic (UBE) removal and a review of the literature. Material and Methods: A 61-year-old woman presented with chronic myelopathy and radiculopathy of both legs 1 year and 2 months ago. Her symptoms progress until cannot walk due to ataxia, right lower limb weakness motor power grade 4, and numbness below T8 level. The magnetic resonance imaging (MRI) showed intradural extramedullary Thoracic T8 level size 1.4x1.6x1.7 cm homogenous enhancement on the right side of the spinal cord. The provisional diagnosis was schwannoma and the differential diagnosis was meningioma. We planned to use endoscopic tumor removal because the tumor was located more posteriorly and the MRI signal was likely to be a well-defined capsulated mass. UBE also benefits many types of equipment was feasibility to use in the working portal can ease during dural opening and closure. We perform UBE tumor removal T8. Translaminar T7-8 approach by Located T7 and T8 levels under fluoroscope then mark medial pedicular line and line bisected to endplate T7 for working portal and bisected to lower endplate for working portal. Then all blur technique was done for partial lower T7 laminectomy and total T8 laminectomy. We tilt the patient's head up to reduce the increased intracranial pressure while opening the dura. After identifying the proximal and distal stalk of the tumor resection the tumor was adherent to the remnant of thecal sac so piecemeal resection was done and dural closure was by simple interrupt stitches with prolene6-0 and used knot pusher for knot tightening. Results: MRI confirms gross tumor removal without CSF leakage. The patient gets neurapraxia with weakness in both lower legs as motor power grade 2. But recovery to normal after post-operative 6 weeks without any radiculopathy. The pathological report was meningioma grade 1 WHO criteria. Conclusion: Unilateral bi-portal endoscopic benefit feasibility and adaptation for intradural extramedullary tumor removal. However, surgeon experience, size, and location of the tumor could be factors for better results. A large-size study could provide an important factor for endoscopic tumor removal.
Keywords: unilateral bi-portal endoscopic; intradural extramedullary tumor; meningioma; spinal cord tumor
1738
P608: Denosumab treated dorsal spine and adjacent rib giant cell tumor: its histological features and potential diagnostic pitfalls and treatment strategies
Tanmay Datey 1 , Umesh Kanade P 1 , Mandar Borde 1 , K Venugopal Menon 1 , Akash Mane 1 , Sangram Rajale 1
1 Spine Surgery, Bharati Vidyapeeth Medical College and Hospital, Pune, India
Introduction: Giant cell tumor (GCT) is classified as benign locally aggressive tumor. It usually affects metaphyseal ends of long bones in mature skeleton. GCT of the ribs and dorsal spine is rare. This case aims at reporting the histopathological features, clinical characteristics and the treatment strategies used for appropriate management of GCT. Materials and Methods: A 45 years old gentleman presented to the spine outpatient complaints of pain over upper dorsal spine since 3 months. Pain was on and off in nature. Pain was aggravating after doing daily activities specially at evening. There was no radiation and sleep disturbances.no bowel/bladder involvement and no known comorbidities. After radiological imaging confirmation we did CT guided biopsy and it was suggestive of GCT then we planned definitive treatment protocol 1) inj. Denosumab 60 mg 2 doses 15 days apart preoperatively. 2) en bloc resection of tumour with partial Hemispondylectomy with costo- transversectomy with D3-D7 posterior spinal fixation and D5 anterior reconstruction. 3)Intraoperative intralesional Denosumab. 4) Histopathology of specimen 5) Post-operative inj. Denosumab 120 mg every month. Result: We observed dramatic changes in the histopathology of the tumor pre and post treatment effect with Denosumab. There were striking depletion of tumor giant cells. Reduction of neoplastic stromal cells. Replacing them with non-proliferating, differtiated, densely woven new bone, hemorrhage and fibro-osseous tissue. Conclusion: GCTs are very rare in ribs and dorsal spine. the treatment for benign GCT should be determined based on the patient’s clinical and radiological study. Recommendations are en bloc resection for benign tumors plus adjuvant and neoadjuvant Denosumab therapy.
1742
P609: The role of mini-invasive surgery (MIS) in metastatic spinal disease from solid tumors
Stefano Telera 1 , Roberto Gazzeri 2 , Laura Raus 1 , Andrea Pace 3 , Veronica Villani 3 , Fabrizio Rasile 1 , Mario Lecce 1 , Francesco Crispo 1 , Laura Marucci 4 , Alessia Farneti 4
1 Neurosurgery
3 Neuro-Oncology
4 Radiotherapy, IRCSS Istituto Nazionale Tumori “Regina Elena”, Rome, Italy
2 Pain Therapy, Azienda Ospedaliera “San Giovanni Addolorata”, Rome, Italy
Introduction: The combination of surgery and radiotherapy/radiosurgery has been demonstrated to be effective in achieving pain relief, maintaining or restoring ambulatory function and improving overall quality of life in patients with symptomatic spinal metastases. In the last fifteen year significant advancements in radiotherapy and radiosurgery as well as improvements in surgical mini-invasive surgery (MIS) techniques have led to a shift in treatment paradigm for spinal metastases toward less invasive surgical approach and ablative radiation treatments. Material and Methods: A consecutive series of patients affected by symptomatic spinal metastases due to solid tumors, operated between August 2018 and August 2023 with MIS variable combined techniques, at National Cancer Institute “Regina Elena “, Rome, Italy, has been analyzed. Results: During this time frame 83 patients have been operated through MIS variably combined approaches involving spinal decompression, kyphoplasty, open kyphoplasty, augmentation techniques, short percutaneous fixation. Median age was 63 years (range 20-80); 45 females and 38 males. Median Tokuhashi score was 10; median SINS score 10. In 45 cases the level of compression was lumbar, in 40 cased it was dorsal, in 3 cases cervical. More levels were treated simultaneously in 10 patients. There were two perioperative deaths, due to medical issues, in one case there was a durotomy during surgery. Two patients presented a deterioration of their neurologic conditions, all patients significantly improve their spine pain according to VAS and Dennis Pain Scale. 65 were able to be treated with radiotherapy/radiosurgery within three weeks. No patients presented wound problems. Median LOS was 8 days. Median follow-up was 11 months. Conclusion: The combination of different MIS spinal techniques seems to be very effective to deal with patients with spinal cord compression, pain or vertebral instability in the setting of metastatic spine disease.
1744
P610: Osteoid osteoma of the body of cervical vertebrae - A case report of an unusual presentation
Harith Reddy 1 , Sharan Achar Thala 1 , Akshya Raj 1 , Vignesh Badikillaya 1 , Appaji Krishnan 1 , Sajan Hegde 1
1 Spine Surgery, Apollo Hospitals, Chennai, India
Introduction: Osteoid osteoma (OO) is a benign bone producing tumor. It was first described by Bergstrand in 1930, but described as a separate clinical entity by Jaffe, in 1935. OO can occur in any part of the skeleton, 56% of the cases seen in the tibia and femur. Incidence of spinal OO is 10-25%, lumbar spine being the most common site. The occurrence in the cervical spine is relatively uncommon, an incidence of 4%. There is also a well-known predilection of posterior vertebral element involvement with centrum being involved in less than 10% cases. Material and Methods: Case report: 15 years female, presented with complaints of restriction of neck movements for the last 3 months, insidious in onset and progressive. Associated with pain on trying to move her neck past the stiff range. She reported no periodicity/ radiation of her pain. On examination, the range of motion of her cervical spine was globally restricted, with only 200 movements possible. There was no posterior midline tenderness. Her neurological examination was essentially normal. X-rays revealed only loss of the normal cervical lordosis with no lysis or abnormal soft tissue shadows. MRI done earlier revealed a T2/STIR hyperintensity in the body of the C4 vertebra, which was reported as spondylitis? / hemangioma? CT scan of the cervical spine revealed a focal lytic lesion (nidus) measuring 4x4x4.5 mm with a tiny central sclerotic focus of calcification noted in the left posteroinferior corner of the C4 body. MRI showed no neural compression. Radionucleotide Bone scan showed a circumscribed nidus at the postero-inferior aspect of the left side of C4 vertebra with increased osseous activity. Results: A standard Smith-Robinson approach to the C4-5. The inferior endplate of the C4 and cavity was curetted. The cavity was then packed with gel foam soaked in bone marrow aspirate. A stand-alone cage with two integrated screws was used for interbody fixation. Postoperatively, the patient was mobilized 6 hours after the surgery, reported significant relief of the neck pain and stiffness. Histopathological examinations were consistent with OO showing haphazard trabeculae of woven bone with osteoblastic rimming. There was varying degree of mineralization. Discussion: This case report details the rare occurrence of an OO in the cervical spine in this part of the world and a further rare location, the vertebral body. The patient in this report was 14 years old. Almost all patients with OO are aged 5-20 years old. In general, patients with OO present with localized pain, characteristically aggravated at night and with physical activity, responding to NSAIDs, typically salicylates. Radiographic imaging is usually the first investigation modality; however the classic appearance is seldom seen. MRI highlights the tissue reaction and inflammatory processes in the vicinity of the tumor, without clearly delineating the tumor focus i.e. the nidus. The most sensitive investigation for OO is Bone scintigraphy scan. It characteristically shows the lesion with double density appearance, with a central concentration of radiotracer and surrounding area of less intense radiotracer uptake.
1758
P611: Spinopelvic fixation and microscopic decompression in a case of long segment neurofibroma of lumbosacral region: a case report
Kandarpkumar Patel 1 , Prashant Patel 2 , Hari Menon 3
1 Department of Spine Surgery, New Sheth P.T. Multispeciality Hospital, Surat, India
2 Department of Neurosurgery, Seven Day Advantis Mission Hospital METAS, Surat, India
3 Department of Orthopaedics, Government Medical College, Surat, India
Introduction: Spinal neurofibroma is commonly seen in Neurofibromatosis type 1 disease. Location is more prevalent in thoracic region followed by cervical and lumbar region. It is rarely seen in the Sacral region. We encountered a case of lumbosacral neurofibroma which was treated surgically with debulking of intradural extramedullary tumor and spinopelvic fixation. Case description: A 55-year-old lady presented with low back pain for the past 2 years. She had progressive weakness of both lower limbs for past 1 year. She had bilateral foot drop with urinary incontinence for the past 4 months. She had not been able to sit, stand and walk due to severe lower back pain for the last 1 month. She was bedridden and was brought to hospital in a stretcher. She had power in both hips grossly grade 4, right knee grade 3 and left knee grade 4. Bilateral foot drop. She had hypoesthesia below bilateral inguinal ligaments. MRI and CT scan images confirm intradural spinal tumor extending from conus to sacrum with eroding L3L4L5 vertebrae and sacrum with expansion in paraspinal region and pelvic cavity. Patient was operated with L2 to S1 Laminectomies, debulking of tumor from spinal canal part and decompression of nerve roots under microscope followed by L1, L2, L3 transpedicular and S2AI screw fixation. Results: Postoperatively patient had significant pain reduction. Patient neurology remained the same. She was mobilized with Taylor Brace and walker assistance. She had no sign of CSF leak and wound complications in subsequent follow-ups. Conclusion: Lumbosacral region is a relatively less common site for spinal neurofibromas. Symptomatic patients require surgical management. This case report highlights microscopic decompression of nerve roots gives better visualization and debulking of tumor, whereas spinopelvic fixation provides good mechanical stability for weight bearing and mobilization of the patient.
1783
P612: Enhanced impedance and D-wave recording acquisition with subdural spinal electrode placement: a case series
Harshal Shah 1 , Adrian Chen 1 , Ross Green 2 , Roee Ber 1 , Randy D'Amico 3 , Daniel Sciubba 1 , Larry Lo 1 , Justin Silverstein 4,5,6
1 Department of Neurological Surgery
5 Neurology, North Shore University Hospital/Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Neurosurgery, Manhasset, NY, USA
2 Department of Neurological Surgery, Northern Westchester Hospital/Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Neurosurgery, New York, NY, USA
3 Neurosurgery
4 Neurology, Lenox Hill Hospital/Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New York, NY, USA,
6Neurophysiology, Neuro Protective Solutions, New York, NY, USA
Introduction: Direct-wave (D-wave) neuromonitoring is conventionally performed by placing electrodes epidurally over the spinal cord, to directly measure corticospinal tract (CST) function. Evaluation of D-wave recordings can assist in the detection and prevention of spinal cord injury during surgery. However, epidural placement of the electrodes often results in high electrical impedances which can interfere with signal acquisition and interpretation. In this study we report the safety and analyze the signals of subdurally placed D-wave electrodes. Material and Methods: A retrospective review of medical records of patients undergoing spinal cord surgery was performed. Demographics, clinical data and epidural vs subdural placement of D-wave electrodes were recorded. Neuromonitoring data were reviewed, including recorded impedances and signal amplitudes. Nonparametric statistics were used to compare epidural and subdural D-waves. Results: Ten patients who underwent surgery for intradural spinal lesions were included in this study (50% female, median age 50.5 years). The most common lesions were tumors: 3 ependymomas, 2 meningiomas, 1 subependymoma, and 1 high-grade glioma. Additional lesions included 1 cavernous malformation, 1 arachnoid cyst, and 1 ventral spinal cord herniation. D-wave recordings from an epidurally placed electrode and subdurally placed electrode were compared in all surgeries. D-wave recordings were acquired subdurally in 8 cases and epidurally in 3 cases. Subdural electrode placement was associated with lower impedance values (p = 0.011) and a higher baseline D-wave amplitude (p = 0.007) relative to epidural placement. No adverse events related to D-wave electrodes placement were recorded. Conclusion: In this report of 10 patients undergoing surgery for intradural spinal lesions, subdural placement of D-wave electrodes resulted in lower impedances, higher signal amplitudes, and better acquisition rate when compare to epidural electrodes. No adverse events were associated with subdural electrodes placement. For spinal surgeries where access to the subdural compartment is technically safe and feasible, surgeons should consider subdural placement when monitoring D-waves to optimize clinical interpretation.
1954
P613: Surgical outcome of the metastatic spinal tumor with neurological deficits
Tokumitsu Mihara 1 , Shinji Tanishima 1 , Chikako Takeda 1 , Satoshi Fujiwara 2 , Hideki Nagashima 1
1 Department of Orthopedic Surgery, Tottori University Faculty of Medicine, Yonago, Japan
2 Department of Orthopedic Surgery, Division of Orthopedic Surgery, Department of Sensory and Motor Organs, School of Medicine, Faculty of Medicine, Tottori University, Yonago, Japan
Introduction: We sometimes have to perform emergency surgery when neurological deficits were occurred in patients with metastatic spinal tumors. However, surgical indication is a very worrisome clinical problem for us. The purpose of this study was to investigate the surgical outcome of the patients with metastatic spinal tumors who underwent emergency surgery due to the neurological deficits. Methods: We performed surgery in 60 cases with metastatic spinal tumors from 2009 to 2021. Thirty-eight cases were extracted as the cases underwent emergency surgery due to the neurological deficits. The 38 cases were divided into two groups according to survival periods after emergency surgery. The cases survival periods after surgery were less than 3 months and 3months or more were divided into group A (12 cases) and B (26 cases), respectively. We investigated age, sex, primary lesion of the tumor, Tokuhashi score, Katagiri score, predicted prognosis, pre- and post-operative ASIA impairment score and when the timing performed surgery. Results: In group A, Tokuhashi score and Katagiri score was significant lower and higher, respectively, compared with those in group B. The predicted prognosis was significant longer than the survival periods after emergency surgery in group A. Conclusions: It was thought that the predicted prognosis was extended due the progress of treatment of tumors. However, surgical treatment for cases with a short prognosis based on scoring systems such as Tokuhashi score and Katagiri score should be carefully considered. Surgery for the patients of metastatic spinal tumors with a short prognosis based on scoring systems should be carefully considered.
2051
P614: Scoliosis in childhood as a potential indicator of spinal cord tumors: a retrospective study about 10 cases
Sami Bahroun 1 , Mohamed Samih Kacem 1 , Wajih Weslaty 1 , Hamdi Grami 1 , Mohamed Samir Daghfous 1
1 Spine Surgery, Kassab Institute, Ksar Said Tunisia, Tunisia
Introduction: Spinal cord tumors often exhibit gradual and subtle development, and occasionally, scoliosis emerges as the sole initial manifestation of these growths. This study seeks to identify the clinical or imaging indicators that can aid in revealing the root cause behind a seemingly 'idiopathic' scoliosis. Material and Methods: We conducted a retrospective analysis of 10 cases involving spinal cord tumors that initially presented as scoliosis. These cases were examined at our institution between 2010 and 2020. Each patient underwent a comprehensive clinical evaluation, which included a thorough medical history, physical examination, and neurological assessment. The study group consisted of eight males and two females, with ages ranging from 4 to 10 years and a mean age of 6 years. All of these patients initially displayed predominantly postural symptoms and signs suggestive of scoliosis. We employed a two-step diagnostic approach. First, all patients underwent radiographs of the spine. Subsequently, magnetic resonance imaging (MRI) of the entire spine was performed. Results: In all cases, scoliosis was accompanied by spinal pain and/or stiffness. Among the ten cases, one exhibited a double curve, while the remaining nine had single curves. Notably, one child presented with "torticolis", another with localized thoraco-lumbar hyperkyphosis, six had left-sided thoracic curves, and two displayed right-sided thoracic curves. Neurological examinations revealed motor deficits in three patients and mild neurological signs in the remaining seven, which included the absence of abdominal reflexes, sensory level abnormalities, and lower limb hyperesthesia. Radiographically, plain X-rays indicated a widened spinal canal in five patients, along with erosion of the posterior vertebral wall. Magnetic resonance imaging (MRI) was performed in diagnosing spinal cord tumors in all cases. These tumors exhibited high signal intensity on T2-weighted sequences, low signal intensity on T1-weighted sequences, and displayed marked enhancement following Gadolinium injection. The majority of tumors were situated in the cervico-thoracic or thoracic spine (seven cases), followed by the thoraco-lumbar spine (two cases) and the cervico-bulbar junction (one case). Associated syrinx was observed in seven cases, with one above the tumor, one below it, and four having both features. Upon histological examination, the tumors were identified as astrocytomas (n = 6), ependymoma (n = 3), and epidermoid cyst (n = 1). After an 18-month follow-up period, six patients who underwent complete resection experienced a favorable post-operative course, while four cases showed persistent motor signs and recurrence. Conclusion: The classification of scoliosis as idiopathic should only be made once alternative causes have been thoroughly ruled out. It is imperative for patients to undergo a precise neurological assessment, and several clinical and radiographic criteria should be meticulously examined. These criteria include early onset, the presence of spinal pain and/or stiffness, the occurrence of a left-sided curve, male gender, the manifestation of neurological symptoms, and the observation of radiographic widening of the spinal canal. The presence of any of these indicators should prompt further investigation via magnetic resonance imaging (MRI).
2063
P615: Machine learning-based detection of sarcopenic obesity and association with adverse outcomes in patients undergoing surgical treatment for spinal metastases
Syed Khalid 1,2 , Elie Massaad 2 , Ali Kiapour 2 , John Shin 2
1 Department of Neurosurgery, University of Illinois at Chicago, Chicago, USA
2 Department of Neurosurgery, Massachusetts General Hospital, Harvard Medical School, Boston, USA
Introduction: The distribution and proportions of lean and fat tissues may help better assess the prognosis and outcomes of patients with spinal metastases. Specifically, in obese patients, sarcopenia may be easily overlooked as a poor prognostic indicator. The role of this body phenotype, sarcopenic obesity (SO), has not been adequately studied among patients undergoing surgical treatment for spinal metastases. Methods: We identified patients undergoing surgical treatment for spinal metastases between 2010 and 2019. A validated deep-learning approach evaluated sarcopenia and adiposity on routine preoperative CT images. Based on composition analyses, patients were classified with SO or non-sarcopenic obesity. Following nearest-neighbor propensity matching that accounted for confounders, we compared the rates and odds of postoperative complications, length of stay, 30-day readmission, and all-cause mortality at 90 days and 1 year between the SO and non-sarcopenic obesity groups. Results: A total of 62 patients with obesity underwent surgical treatment for spinal metastases during the study period. Of these, 37 patients had non-sarcopenic obesity, while 25 had SO. After propensity matching, 50 records were evaluated, composed equally of patients with non-sarcopenic obesity and SO (n = 25). Patients with SO were noted to have an increased odds of non-home discharge (Odds Ratio (OR) 6.0, 95% confidence interval (CI) 1.69-21.26), 30-day readmissions (OR 3.27, 95%CI 1.01-10.62), 90-day mortality (OR 4.85 95%CI 1.29-18.26), and 1-year mortality (OR 3.78, 95%CI 1.17-12.19), and months to mortality following surgery (12.60 ± 19.84 vs. 37.16 ± 35.19 p = .002, standardized mean difference = 0.86). No significant differences were noted in the length of stay or postoperative complications when comparing the two groups (p > .05). Conclusion: The SO phenotype is associated with increased odds of non-home discharge, readmission, and postoperative mortality. Our study suggests that SO may be an important prognostic factor to consider when developing care plans for patients with spinal metastases.
2064
P616: CT image-based machine learning assessment for stratifying 90-day postoperative risks in spinal metastasis patients
Syed Khalid 1,2 , Elie Massaad 1 , Ali Kiapour 1 , John Shin 1
1 Department of Neurosurgery, Massachusetts General Hospital, Harvard Medical School, Boston, USA
2 Department of Neurosurgery, University of Illinois at Chicago, Chicago, USA
Introduction: Patients undergoing surgical interventions for spinal metastases face inherent risks associated with their clinical condition, nutritional status, primary tumor type, and functional status. These multifaceted factors play a pivotal role in determining their postoperative sequelae. Emerging evidence suggests that image-derived features from CT scans can offer invaluable insights into patient outcomes, yet their potential in predicting early postoperative outcomes after spinal metastasis surgery remains underexplored. Methods: Retrospective analysis was conducted on patient records undergoing spinal metastases surgery between 2010 and 2019. Demographic, clinical, functional, and radiographic data were processed. Radiographic data were analyzed using an advanced deep-learning methodology. Extra Trees algorithms were developed and optimized to predict 90-day postoperative mortality. Results: A total of 308 patient records were scrutinized (mean age 61.97 ± 12.20 years; 43% female). Extra Trees algorithms were constructed to assess the efficacy of 90-day postoperative mortality predictions. Feature importance analysis revealed that Preoperative Hemoglobin, Total Lean Body Mass, Standard Deviation of Hounsfield Units of Segmented Muscle at Lumbar Level 3, Platelet Count, and The New England Metastatic Spinal Score were among the most predictive indicators. An Area Under the Receiver Operating Characteristic (AUROC) of 0.89 was achieved. Conclusion: The study highlighted the significance of diverse parameters derived from CT imaging in predicting outcomes post-spinal metastasis surgery. The developed machine learning approach offers a comprehensive assessment tool for preoperative risk stratification, aiding in enhanced decision-making and patient consultation.
2068
P617: Assessment of survival prediction after surgery in spinal metastasis patients using the global spine study tumor group (GSTSG) risk calculator: an external validation from tertiary cancer hospital
Warayos Trathitephun 1 , Siravich Suvithayasiri 1 , Jackapol Kamolpal 1
1 Orthopedics, Chulabhorn Royal Academy, Bangkok, Thailand
Introduction: Spinal metastasis is the most common bone metastasis that affects lower quality of life. The main treatment is palliative surgery and systematic therapy by chemotherapy and radiation therapy. However, serious complication is high when compared to degenerative spinal surgery. So natural history prognosis and patient selection play essential roles in better outcomes. Treatment options may be based on prognostic scoring eq. Tomita Score, Revised Tokuhashi Score, and Skeletal Oncology Research Group (SORG) Nomogram. Global Spine Tumor Study Group (GSTSG) is one of the new scoring bases on important prognostic factors including tumor type, ambulatory status, analgesic use, and involvement level of the spine that may be more accurate for predicting survival rate but may need more validity assessment. Material and Methods: We conducted a retrospective study of spinal metastases patients which confirmed diagnosis with magnetic resonance imaging (MRI) from January 2013 to December 2022. Survival prediction and probability of survival compared between GSTSG risk calculator, Tomita Score, Revised Tokuhashi Score, and SORG Nomogram. A single variable factor associated with survival rate (marginally significant) analysis by univariate Cox regression. Then use a marginally significant variable for the multivariate Cox proportional hazard model. For external validity use receiver operating characteristic (ROC) analysis at 3, 6, 12, and 24 months. And report the overall survival rate by Kaplan-Meier survival curve. Results: We include 248 spinal metastases patients. mean age was 59.23 ± 12.55 years. The mean duration of follow-up was 470.29 ± 441.98 days. Most common tumor in origin were breast 82 (32.54%), Lung 68 (26.98%), prostate 29 (11.51%), colorectal 6 (6.35%), thyroid 8 (3.17%) and unknow 6 (2.38%). Univariate Cox regression analysis show significant factor for Karnofsky Status (PS), Eastern Cooperative Oncology Group (ECOG) level 2-4, The American Society of Anesthesiologists physical status classification (ASA) level 3-5, regular analgesia of both strong and weak opioid, extraspinal metastasis > 3 locations, visceral metastasis 2 or more location, present of liver or lung or brain metastasis, previous chemotherapy and Frankel Pre-op grade D-E. However, only regular analgesia of weak opioids, Lung metastasis, and previous chemotherapy were statistically significant for Multivariate Cox regression analysis. External validity was highest for GSTSG at all follow-up times (sufficiently accurate AUC > 0.7). At 3-month GSTSG (AUC = 0.76) and SORG (AUC = 0.76) were equally. And at 12 months GSTSG (AUC = 0.78) and SORG (AUC = 0.74) were higher than modified Tokuhashi (AUC = 0.61) and Tomita (AUC = 0.64). Conclusion: Multivariate Cox regression analysis with important factors such as regular analgesia of weak opioids, Lung metastasis, and previous chemotherapy. GSTSG shows the highest AUC for external validity at all follow-up times. GSTSG has been developed for more accuracy in proper treatment planning for spinal metastasis.
Keywords: vertebral metastasis; spinal metastasis; prognostic scoring system; Global Spine Tumor Study Group
2075
P618: Patient outcomes in spinal tumors: spotlight on impending spinal instability
Helena Milavec 1 , Victoria Schimmelpenning 2 , Robin Brugger 2 , Nikki Rommers 3 , Johann Kunst 2 , Martin Jaeger 2
1 Department of Orthopaedic Surgery and Traumatology, Bern University Hospital, Inselspital, University of Bern, Bern, Switzerland
2 Department of Orthopaedic Surgery and Traumatology, Spine Unit, Aarau Cantonal Hospital, Aarau, Switzerland
3 Departement of Clinical Research, University Hospital Basel, Basel, Switzerland
Introduction: Spinal metastases are on the rise, reflecting the global increase in cancer cases. Classification of spinal neoplastic conditions often relies on the assessment of tumor-related spinal instability through the Spinal Instability Neoplastic Score (SINS). Currently, there is a lack of clearly established treatment guidelines for patients exhibiting indeterminate spinal instability, falling within the range of 7 to 12 on the SINS scale. The aim of this analysis is to present a comprehensive overview of treatments and outcomes for patients with spinal metastases facing an indeterminate spinal instability with possible impending fracture risk. Materials and Methods: This is a retrospective, single-center study conducted using data collected from a tertiary hospital. The study population comprises patients with spinal metastases who were referred to the outpatient clinics of our spinal unit. We provide an overview of patient characteristics, SINS components, primary tumor type, spinal metastasis count, treatment approach, and treatment outcomes. As the primary objective, we compare the treatment (surgical vs. non-surgical treatment) between the two groups with indeterminate instability. We compared the number of tumors treated with surgery between the different groups of SINS with a Fisher exact test, and assessed the association between treatment outcome and SINS on a lesion level using a mixed effects logistic regression model, including patient as a random intercept to account for the dependence of multiple lesions within a single patient. Results: We analyzed 30 patients with a total of 147 spinal metastases. Among them, 28 patients had at least one lesion with an indeterminate SINS (7-12), and 15 of these patients (53.57%) passed away before data extraction. Each patient had between 1 and 10 metastases, with a median of 7. In total, 101 lesions had an indeterminate SINS indicating possible impending fracture risk. The median follow-up time was 133 days for all patients, and 136.5 days for those in the indeterminate group. Within the indeterminate group, a substantial 93% of patients opted for conservative treatment. Among the non-surgically treated lesions in this group, 59% exhibited improvement, 22% remained stable, and 19% stayed asymptomatic - with none deteriorating. The primary reasons for surgery were pain and neurological symptoms. Within the indeterminate group, there was no discernible difference in treatment success between patients who underwent surgery and those who did not (p = 0.906). We subdivided the intermediate group into two categories: lower scores (SINS 7-9) and higher scores (SINS 10-12). Nevertheless, there was no statistically significant change in treatment approaches observed (p = 1.00). Conclusion: Among patients with indeterminate (possible impending) spinal instability (SINS 7-12), our findings reveal that there was no statistically significant disparity in treatment success when comparing those who underwent surgery to those who did not. Moreover, a substantial majority of patients at risk of impending fractures were treated non-surgically, with more than half experiencing improvements, and none showing deterioration. These findings suggest a growing inclination toward non-surgical approaches for tumor patients of the indeterminate group.
2131
P619: Are sociodemographic or socioeconomic parameters associated with clavien-dindo grade III-IV or grade V complications after metastatic spinal tumor surgery?
Rafael De la Garza Ramos 1 , Jessica Ryvlin 1 , Anne Schlumprecht 1 , Mousa Hamad 1 , Mitchell Fourman 1 , John Shin 2 , Yaroslav Gelfand 1 , Saikiran Murthy 1 , Reza Yassari 1
1 Neurosurgery, Montefiore Einstein, New York, USA
2 Neurosurgery, Massachusetts General Hospital, Boston, USA
Introduction: Sociodemographic and socioeconomic factors are thought to contribute to disparities observed in oncologic surgery outcomes. However, it is unclear whether these factors are also associated with development of major complications or 30-day mortality in oncologic surgery for metastatic spine disease. The questions that we investigated in this study were: In patients undergoing metastatic spinal tumor surgery, (1) are sociodemographic or socioeconomic factors associated with major (Clavien-Dindo Grade III-IV) complications? (2) Are sociodemographic or socioeconomic factors associated with 30-day mortality (Clavien-Dindo Grade V) complications? Material and Methods: Between April 2012 and February 2023, we surgically treated 168 patients with spinal metastases and spinal cord compression, pathologic vertebral compression fractures, and/or spinal mechanical instability. Inclusion criteria were patients with complete demographic, social, oncologic, and follow-up data and patients who were followed until death or for at least 30 days postoperatively. Based on these criteria, 1% (2) patients were excluded because they had incomplete data, and < 1% (1) patient was excluded because they were lost before the minimum study follow-up period, leaving 98% (165) for final analysis. The primary outcome variable was development of at least one Clavien-Dindo Grade III or IV (major) complication and the secondary outcome was development of a Clavien-Dindo Grade V (mortality) complication within 30 days of surgery. Exploratory data analysis, univariate, and stepwise multivariate logistic regression analyses were performed. Results: After controlling for variables such as ECOG performance status, Frankel Grade, modified Bauer score, and PNI, independent factors associated with development of at least one Clavien-Dindo Grade III or IV Complication were Frankel Grade A – C (OR 6.2, 95% CI 2.4 to 15.5; p < 0.001) the modified Bauer score (OR 0.5, 95% CI 0.3 to 0.91; p = 0.02) and the Prognostic Nutritional Index (OR 0.9, 95% CI 0.8 to 0.9; p = 0.02). After controlling for variables such as ECOG performance status, Frankel Grade, primary cancer type, modified Bauer score, and PNI, independent factors associated with development of a Clavien-Dindo Grade V Complication were lung primary cancer (OR 5.2, 95% CI 1.1 to 24.5; p = 0.04), modified Bauer score (OR 0.4; 95% CI 0.2 to 0.9; p = 0.03), the Prognostic Nutritional Index (OR 0.9, 95% CI 0.8 to 0.9; p = 0.04), and use of internal fixation (OR 0.1; 95% CI, 0.1 to 0.4; p = 0.01). No sociodemographic or socioeconomic factor was associated with either outcome on univariate analysis. Conclusion: In the present study, no association was found between sociodemographic or socioeconomic parameters and major complications or 30-day mortality after surgery for metastatic spinal tumors. These findings suggest that short-term outcome does not differ based on patients’ age, race, or socioeconomic status, and that equitable care is being delivered.
2193
P620: Racial disparities in metastatic tumors of the spine: a systematic review
Jessica Ryvlin 1 , Andrew Brook 1 , Lucas Dziesinski 1 , Nitza Granados 1 , Anne Schlumprecht 1 , Mousa Hamad 1 , Mitchell Fourman 1 , Saikiran Murthy 1 , Yaroslav Gelfand 1 , Reza Yassari 1 , Rafael De la Garza Ramos 1
1 Montefiore Medical Center/Albert Einstein College of Medicine, New York, USA
Background: Disparities in access and delivery of care have been shown to disproportionately affect certain racial groups across multiple medical disciplines. To date, several studies have been conducted to assess these disparities within the metastatic spine disease population, but the extent of their effects in the setting of other measures of socioeconomic status remains unclear. Objective: The purpose of this study was to perform a systematic review of the literature to understand the effect of racial disparities on outcomes in patients with metastatic spine disease. Methods: The PRISMA guidelines were followed, where a comprehensive online search was performed using Pubmed, Medline, Web of Science, Cochrane, Embase, and Science Direct using MeSH terms related to metastatic spine tumor surgery and racial disparities up to February 2023. Two independent reviewers screened and analyzed articles to include studies assessing the following primary outcomes: clinical presentation, treatment type, postoperative complications, readmission, reoperation, survival and/or mortality, length of hospital stay, discharge disposition, and advance care planning. Additional factors related to socioeconomic status were included and levels of evidence were assessed. Results: A total of 13 studies were included in final analysis; 12 were retrospective cohort studies and 1 was a prospective study. Two studies (15%) analyzed clinical presentation, four (31%) analyzed treatment type, six (46%) analyzed postoperative complications, three (23%) analyzed readmission, one (8%) analyzed reoperation, four (31%) analyzed survival and/or mortality, four (31%) analyzed length of stay, two (14%) analyzed discharge disposition, and one (8%) analyzed advance care planning. Overall, race was found to be significantly associated with at least one evaluated outcome in 9 of 13 (69%) studies. Nine studies (69%) included at least one other measure of socioeconomic status in multivariate analysis, with the two most common being insurance type and income. Levels of evidence were Level III (12 of 13 studies) and Level II (1 of 13 studies). Conclusion: Overall, Black patients were more likely to present with metastatic spinal cord compression, were more likely to have a nonroutine discharge, and had different treatment recommendations compared to White patients. Race was found to have no significant effect on postoperative non-ambulation, advance care planning, readmission, or mortality/survival. Finally, inconsistent results were seen regarding the role of race on postoperative complications and length of hospital stay. The association between race and outcome in oncologic spine surgery remains unclear, especially given the variation in inclusion of other important covariates such as insurance status, income, and social vulnerability.
2286
P621: The successful managment of Giant cervical dumbell shaped schwannoma using posterior unilateral approach only: A case report
Elouni Emna 1 , Atef Ben Nsir 1 , Mohamed Ali Kharrat 1 , Wiem Boudabbous 1 1 , Roua Latrach 1 , Mehdi Darmoul 1
1 Department of Neurosurgery, University Hospital of Monastir, Monastir, Tunisia
Introduction: Dumbbell-shaped tumors make up 18% of all spinal cord tumors. While these tumors are most commonly found in the cervical spine, there are only a few reported cases of giant lesions extending across multiple vertebral levels. Material and methods: A 63-year-old female presented with a one-year history of worsening motor impairment. Initially, the impairment affected the lower right limb and later extended to the upper right limb. Neurological examination revealed Brown-Sequard syndrome, characterized by right spastic hemiplegia, complete proprioceptive loss on the right side, and left-sided pain and temperature anesthesia. A cervical spine MRI showed a giant mass (12 cm) on the right side, extending both intra and extradurally at the C4-C5 level. The intraspinal component severely compressed the spinal cord, displacing it anteriorly. The patient underwent a gross total resection of the lesion using a posterior unilateral approach only with facetectomy, without the need for spinal fusion. Results: The patient experienced gradual improvement in motor and sensory functions, ultimately achieving full recovery within three years. At the final follow-up, there was no evidence of tumor recurrence or the development of cervical instability. Conclusion: Giant dumbbell-shaped cervical spine schwannomas are rare tumors, and their surgical management presents significant challenges. However, the posterior unilateral approach without spinal fusion, even with facetectomy, proved effective in preventing spinal instability and yielded satisfactory functional and clinical outcomes.
2314
P622: Is a vertebral body replacement still necessary in oncological cases? A single centre experience with 38 patients
Maximilian-Niklas Bonk 1
1 Department for Neurosurgery, University Hospital Augsburg, Augsburg, Germany
Background: Management of metastases has seen pivotal shifts in the 21st century. This study aims to evaluate the effectiveness and safety of Carbon-PEEK stabilization, with and without vertebral body replacement, in the treatment of metastatic spinal lesions. Methods: We retrospectively analyzed all patients who underwent Carbon-PEEK stabilization at the University Hospital Augsburg from January 2021 to December 2022. A total of 38 patients (28 males / 10 females) with an average age of 67 were included. A Match-Pair analysis was performed with 19 patients in each group, matching for age (±2 years), gender, histology, Karnofsky Performance Index and SIN-Score. Results: The most frequent tumors were Plasmacytoma (26%), Bronchial-Ca (16%), and Prostate (16%). The mean SIN-Score was 10.84. The average follow-up period was 552 days. Pre-operatively, 3 patients were non-ambulatory, but post-operatively all regained walking ability. There was an average improvement of 5 points in the Karnofsky Performance Index. In all cases, stabilization incorporated both the upper and lower segments. In the stabilization-only group without vertebral body replacement, due to high therapy pressure, the completion of the 360° stabilization by vertebral body replacement was omitted, and no negative consequences were observed during the study period. One complication arose, unrelated to the operation: pulmonary embolism. Conclusion: Carbon-PEEK stabilization is a safe and efficient method for the management of spinal metastases. Our findings suggest that, in cases with higher SINS, vertebral body replacement may not be imperative, provided there is regular close monitoring.
Keywords: Carbon-PEEK; spinal metastases; SIN-Score; Karnofsky Performance Index; 21st century treatment; vertebral body replacement
2325
P623: An artificial intelligence-based approach for clustering of patient characteristics and outcomes in oncologic surgery for metastatic tumors of the spine
Jessica Ryvlin 1 , Mousa Hamad 1 , Ariel Stock 1 , Mitchell Fourman 1 , Ananth Eleswarapu 1 , Yaroslav Gelfand 1 , Saikiran Murthy 1 , Reza Yassari 1 , Rafael De la Garza Ramos 1
1 Montefiore Medical Center/Albert Einstein College of Medicine, New York, USA
Background: Classification tools have been developed to stratify patients undergoing oncologic spine surgery based on perioperative risk and expected survival. An unsupervised machine learning approach may help identify patients at highest risk for perioperative morbidity or mortality. Study design: Retrospective study. Objective: To evaluate an artificial intelligence-based unsupervised machine learning approach to group patients’ characteristics and outcomes in oncologic spine surgery. Methods: The records of 142 patients who underwent surgery for metastatic spinal tumors at our institution were reviewed for perioperative characteristics including demographics, comorbidities, oncologic history, and intraoperative details. A hierarchical clustering algorithm using Ward distances was employed and a dendrogram was generated. The largest vertical drop was used to define the number of clusters. Our primary outcome was overall survival (OS). Secondary outcomes included any complication, major complication, in-hospital mortality, ambulatory status, and length of stay postoperatively. Results: Three distinct patient clusters were identified with significant differences in sex, race, chemotherapy history, pathologic fracture or instability on presentation, muscle mass, ambulatory status, primary tumor histology, tumor location, preoperative embolization status, surgical approach, and surgical extent. Clusters 1, 2, and 3 were found to be associated with significant differences in median OS (46 months, 27 months, 7 months; p = 0.025) and in in-hospital mortality incidence (5%, 3%, 16%; p = 0.037). No differences were found between clusters for any complication, major complication, ambulatory status, and length of stay. Conclusion: Artificial intelligence-based prognostication models may be useful to uncover patterns amongst patients undergoing surgery for spinal metastases who have poor postoperative outcomes. While additional validation is needed in larger populations, hierarchical clustering approaches can be ultimately utilized for improved clinical decision-making and surgical patient selection practices.
2502
P624: Outcomes of combined anterior and posterior approaches in spinal multiple myeloma surgery
Sami Bahroun 1 , Alaa Aloui 1 , Mohamed Samih Kacem 1 , Hamdi Grami 1 , Mohamed Samir Daghfous 1
1 Spine Surgery, Kassab Institute, Ksar Said, Tunisia
Introduction: Multiple myeloma is a hematologic cancer with a notably heterogeneous prognosis,it is characterized by the proliferation of malignant plasma cells in the bone marrow. It often manifests in the spine, causing various clinical complications including vertebral fractures and compression. Despite its prevalence, the optimal management of this condition remains a subject of ongoing debate. This study focuses on the pivotal role of surgery in managing spinal multiple myeloma and aims to elucidate the surgical outcomes achieved through the combined utilization of anterior and posterior approaches. Material and Methods: We conducted a retrospective study involving 20 patients who underwent combined anterior and posterior surgical approaches for spinal myeloma treatment between 2000 and 2021, with a minimum two-year follow-up period. Characteristics of this population, reconstructive techniques and surgery-related complications were reviewed. Neurological outcomes were assessed using the Frankel classification. Post-operative results and quality of life were evaluated using the Visual Analogue Scale (VAS) and the Eastern Cooperative Oncology Group (ECOG) score. Results: There were 12 males and 8 females with a mean age of 58,6 (range from 38 to 71 years). Mean follow-up time was 3.8 years. Pain was the predominant symptom in 14 cases, while 6 cases presented with incomplete paraplegia due to spinal cord compression. Distribution of lesion locations included, 13 in the thoracic spine and 7 in the lumbar spine. The mean postoperative VAS score was 2, indicating a notable improvement from the preoperative value of 7. Additionally, the postoperative ECOG median score was 1, contrasting with the preoperative score of 3. The median Frankel classification was level 5 in post-operative patients. We noted a substantial enhancement in neurological function, with all six patients who initially had neurological deficits showing improvement. Two of them even returned to normal function. The overall survival rates at 5 and 10 years stood at 60.5% and 41.7%. Local tumor recurrence occurred in two of 20 patients (10%). infection was seen in one patient with recovery after prompt surgical saline irrigation and adequate antibiotic therapy. Conclusion: In conclusion, surgical intervention with combined anterior and posterior approaches appears to be an effective treatment for spinal myeloma, offering improvements in both neurological function and quality of life.
2510
P625: Superior gluteal artery perforator flap for soft tissue reconstruction after resection of sacral tumors
Aron Lazary 1 , Csaba Halmy 2 , Ádám Biczó 1
1 National Center for Spinal Disorders, Buda Health Center, Hungary
2 Department of Surgey, Uzsoki Hospital, Hungary
Background: Reconstruction of the soft-tissue defects following sacrectomy is challenging, usually requiring flaps to fill in the surgical cavity and to provide optimal wound healing. Vertical rectus abdominis and gluteal muscle flaps - the gold-standard methods for soft tissue reconstruction after sacrectomy – are characterized by technically demanding preparation and necrosis or chronic atrophy in case of deteriorated blood supply. Use of perforator flaps have become more and more popular in different areas of reconstructive surgery. Superior gluteal artery perforator flap (S-GAP) is commonly used for the treatment of sacral pressure sores, chronic sacral wounds but its application for the complex soft tissue reconstruction after sacral tumor resections is sporadic in the literature. Objective: A technical note and institutional case-series about the use of S-GAP for the soft-tissue reconstruction after sacrectomy is represented. Method: Critical steps of the S-GAP preparation are the identification of the perforator vessels by intraoperative ultrasound and the partial de-epihelization to fill dead space. In our case-series, 10 patients after low, midsacral or eccentric sacral resection because of primary tumor have been managed with S-GAP so far. Results: Seven patients have got more than 1-year follow-up. Postoperative wound infection appeared in one case which was treated by debridement and temporary negative pressure wound therapy. No flap necrosis nor body wall herniation appeared. Control MRIs show good flap integration and stable soft tissue body wall even one year after the surgery. Revision plastic surgical procedure was not necessary in any case. Conclusion: S-GAP is a feasible and easy-to-use flap for soft tissue reconstruction after sacral tumor resections. Peripheral nerve muscle innervation can be preserved with the use of perforator flaps which can provide a comparable or even superior functional outcome compared to gluteal flaps.
2556
P626: Adenocarcinoma of the appendix with metastasis to the spine
Emmanuel Oladeji 1 , Peter Osuala 1 , Elizabeth Idowu 2 , Adefemi Afolabi 1
1 Department of Surgery
2 Department of Radiology, University College Hospital, Ibadan, Nigeria
Background: Adenocarcinoma of the appendix is rare and has remained so since the first documented case in the late 19th century. There are a few reported cases of bone metastasis from adenocarcinoma of the appendix and there is none from Africa.Case: We report a rare case of a 30-year-old man who presented with low back pain following a trivial fall and subsequently developed generalized peritonitis. He underwent laparotomy and had appendicectomy with biopsy of mesenteric lymph nodes. The histology of the samples confirmed adenocarcinoma of the appendix with metastasis to the mesenteric lymph nodes while MRI scan demonstrated spine metastasis. While he was being optimized for palliative chemotherapy and spine radiation, his clinical condition deteriorated and subsequently died from disease progression. Discussion: Adenocarcinoma of the appendix mostly presents after the 5th decade of life with features of appendicitis, and preoperative diagnosis is just as rare as the disease itself. There have been a few reports of malignant neoplasms of the appendix from Africa, however, this is the first reported case of spine metastasis from adenocarcinoma of the appendix. The clinical presentation of progressive abdominal pain which was preceded by a fall had led to a misdiagnosis of blunt abdominal injury with generalized peritonitis, and a traumatic lumbar spine injury. The late presentation, delay in diagnosis, as well as the inadequate oncologic resection may have contributed to the unfavourable outcome. Conclusion: Carcinoma of the appendix should be considered as a differential diagnosis in spine metastasis of unknown origin especially with coexisting abdominal symptoms.


