Abstract
Background
Growing evidence attests to the efficacy of mindfulness-based interventions (MBIs), but their effectiveness for healthcare workers remains uncertain.
Aims
To evaluate the evidence for MBIs in improving healthcare workers’ psychological well-being.
Methods
A systematic literature search was conducted on Medline, Embase, Cumulative Index for Nursing and Allied Health Literature, PsycINFO and Cochrane Central Register of Controlled Trials up to 31 August 2022 using the keywords ‘healthcare worker’, ‘doctor’, ‘nurse’, ‘allied health’, ‘mindfulness’, ‘wellness’, ‘workshop’ and ‘program’. Randomised controlled trials with a defined MBI focusing on healthcare workers and quantitative outcome measures related to subjective or psychological well-being were eligible for inclusion. R V.4.0.3 was used for data analysis, with the standardised mean difference as the primary outcome, employing DerSimonian and Laird’s random effects model. Grading of Recommendations, Assessment, Development and Evaluation framework was used to evaluate the quality of evidence. Cochrane’s Risk of Bias 2 tool was used to assess the risk of bias in the included studies.
Results
A total of 27 studies with 2506 participants were included, mostly from the USA, involving various healthcare professions. MBIs such as stress reduction programmes, apps, meditation and training showed small to large effects on anxiety, burnout, stress, depression, psychological distress and job strain outcomes of the participants. Positive effects were also seen in self-compassion, empathy, mindfulness and well-being. However, long-term outcomes (1 month or longer postintervention) varied, and the effects were not consistently sustained.
Conclusions
MBIs offer short-term benefits in reducing stress-related symptoms in healthcare workers. The review also highlights limitations such as intervention heterogeneity, reduced power in specific subgroup analyses and variable study quality.
PROSPERO registration number
CRD42022353340.
Keywords: Mood Disorders; Psychology, Medical; Public Health Administration; Psychology, Applied
WHAT IS ALREADY KNOWN ON THIS TOPIC
Healthcare workers worldwide are experiencing high levels of burnout and psychological distress, and mindfulness-based interventions have been implemented in this population, yielding mixed levels of success.
WHAT THIS STUDY ADDS
Data from the meta-analysis suggest that mindfulness interventions are effective in the short term for improving wellness in doctors, nurses and allied health staff, although there was a considerable variation in terms of occupational roles and specific outcomes that showed significant improvement.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Mindfulness-based interventions offer benefits for healthcare workers in terms of ameliorating stress and burnout-related symptoms, at least in the short term. Future work should also study the sustainability of such programmes and their long-term effects.
Background
Worldwide, burnout among healthcare workers is prevalent.1 Many studies also suggest that the coronavirus disease 2019 (COVID-19) pandemic placed an enormous burden on the health systems and greatly increased the perceived psychological distress of healthcare workers.2 3 High attrition rates were seen in many countries during the COVID-19 pandemic. This is an issue of grave concern as physician burnout is strongly associated with higher rates of physician suicide, increased medical errors and worse patient care outcomes.4 5
There is a pressing need for healthcare organisations and systems to prioritise the well-being of healthcare workers and provide support for addressing burnout. Healthcare is an inherently high-stress field. Given the frenetic pace and complicated nature of most health systems, system-wide infrastructure and policy changes have been slow and difficult to implement. On a personal level, it is evident that physicians at all stages of education and training are at risk for burnout.6 Moreover, individuals experiencing burnout often struggle to recognise their mental health needs or are unwilling to seek help.7 8
To address this issue, many organisations have invested heavily in mindfulness-based interventions (MBIs) such as meditation apps, mindfulness workshops and yoga classes for their employees.9 Mindfulness refers to being fully aware and present in the current moment, including thoughts, feelings and sensations. MBIs are therapeutic approaches that use mindfulness techniques to address mental and physical health concerns.10 These interventions include various practices, such as meditation, breathing exercises and yoga, to cultivate mindfulness and improve overall well-being. Research has shown that MBIs can be effective in alleviating myriad biopsychosocial conditions, including stress, anxiety, depression, mood disorders and physical pain.11 The techniques may also help individuals cultivate compassion, kindness and acceptance towards themselves and others.12
Although there is growing evidence supporting the efficacy of mindfulness-based stress reduction and mindfulness-based cognitive therapy,13 the evidence regarding the application of these programmes to healthcare workers remains conflicting.14 15 Previous meta-analyses of MBIs indicate a moderate to large within-group and between-group effect on stress in the general population11 and healthcare professionals,14 15 but these interventions did not appear as effective in reducing burnout or improving resilience for healthcare professionals.15 The analysis is further complicated by the wide range of interventions and employees in different occupational roles. In this systematic review, we aimed to investigate the current body of evidence for MBIs that have been used to help healthcare workers improve their subjective or psychological well-being. Well-being is the focal point of this review as it encompasses burnout as well as its opposite, that is, work engagement and optimal psychological functioning.
Methods
Search strategy and inclusion criteria
The review protocol was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO) (registration number CRD42022353340). A systematic literature search was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines16 and performed in Medline (Ovid), Embase, Cumulative Index for Nursing and Allied Health Literature (CINAHL), PsycINFO and Cochrane Central Register of Controlled Trials (CENTRAL) from inception until 31 August 2022 using combinations of the keywords ‘healthcare worker’, ‘doctor’, ‘nurse’, ‘allied health’, ‘mindfulness’, ‘wellness’, ‘workshop’ and ‘program’. The full search strategy can be found in online supplemental table S1.
gpsych-2023-101115supp001.pdf (3.2MB, pdf)
The inclusion criteria for the present review include original randomised controlled trials, published in English, involving healthcare workers, with a defined MBI and with quantitative outcome measures related to subjective or psychological well-being. Studies with populations including both clinical and non-clinical healthcare staff were included as long as clinical staff comprised a majority of the study participants, due to the heterogenous nature of the healthcare workforce. Both validated and self-reported scales were accepted. For the purposes of the review, pilot studies and feasibility studies were excluded as they did not provide a meaningful effect size estimate for planning subsequent studies.
Titles and abstracts of potential articles were screened independently against the eligibility criteria. Subsequently, full texts of relevant studies were then retrieved and reviewed independently. Both the title and abstract screening and full-text screening were completed independently by four authors (JZYE, FJJT, NYO, CEY). Conflicts were resolved by discussion and consensus with a senior author (JT, HKT or QXN). The reference lists of included studies were hand-searched to include studies omitted by electronic search.
Data extraction and analysis
A standardised data extraction sheet was used to extract the relevant data from the included studies. Data extraction was performed independently by two authors (JZYE and FJJT). Baseline characteristics including country, population, study design, sample size, intervention type, frequency and duration of intervention, type of control and assessment timepoints were extracted. Scores of outcomes such as level of burnout, mindfulness, well-being, job strain, anxiety, depression, stress, resilience, self-compassion and psychological distress were also extracted.
Measures of the above outcomes were assessed using the following scales in :
Anxiety: Beck Anxiety Inventory, 7-item Generalised Anxiety Disorder Scale, 4-item Patient Health Questionnaire, State Anxiety Inventory, Goldberg Anxiety Scale, Depression Anxiety Stress Scale (DASS), Profile of Mood States (Tension-Anxiety), Zung Self-Rating Anxiety Scale, Visual Analogue Scale, Symptom Checklist 90-Revised Somatization (Anxiety subscale).
Burnout: Maslach Burnout Inventory, Copenhagen Burnout Inventory, Shirom-Melamed Burnout Questionnaire.
Depression: Beck Depression Inventory, 9-item Patient Health Questionnaire, 4-item Patient Health Questionnaire, Goldberg Depression Scale, 21-item DASS, Profile of Mood States (Depression-Dejection), Symptom Checklist 90-Revised Somatization (Depression subscale), Zung Self-Rating Depression Scale.
Job strain: Irritation Scale, Work Related Strain Scale.
Mindfulness: Five Facets of Mindfulness Questionnaire, Mindfulness Attention Awareness Scale.
Positive well-being: Warwick-Edinburgh Mental Well-being Scale, Psychological Well-Being Scale, the World Health Organization (WHO)-5 Well-being Index.
Psychological distress: 28-item General Health Questionnaire, Brief Symptom Inventory, Symptom Checklist 90-Revised Somatization.
Resilience: Connor-Davidson Resilience Scale, 10-item Connor-Davidson Resilience Scale.
Self-compassion: Self-Compassion Scale.
Stress: Perceived Stress Scale, DASS.
The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach was used to evaluate the overall quality of evidence of the included studies.17 The Cochrane’s Risk of Bias 2 (RoB2) tool was used to assess the risk of bias in the included studies. The RoB2 tool assesses quality in five domains: the randomisation process, deviations from intended interventions, missing outcome data, outcome measurements and reporting.18 Studies were rated as having a low risk of bias if there were low risks of bias in all domains, a moderate risk of bias if there were one or more domains with ‘some concerns’, and a high risk of bias if there were high risks of bias in one or more domains. Ratings for both the RoB2 tool and the GRADE approach were based on the consensus of two study investigators (JZYE and FJJT) and a senior author (JT or QXN).
Data analyses were performed using R V.4.0.3 (R Foundation for Statistical Computing, Vienna, Austria). Two-tailed statistical significance was set at p<0.05. To account for any different units of analysis, continuous data were pooled with standardised mean difference (SMD),19 expressed as Hedges’ g.20 For effect sizes, SMD thresholds of 0.2, 0.5 and 0.8 represented small, moderate and large effect sizes, respectively.21 As some heterogeneity was expected, DerSimonian and Laird’s random effects model weighted by the inverse variance method was used.22 Heterogeneity was quantified using Cochran’s Q test and I2 statistics. I2 value thresholds of 25%, 50% and 75% indicated low, moderate and high heterogeneity, respectively.
For the purposes of the review, a 1-month postintervention cut-off was used to stratify outcomes. The effects were classified as either short-term (less than 1 month postintervention) or long-term (longer than 1 month). The cut-offs were established based on the follow-up assessment timepoints used in the majority of included studies. Most studies had assessment timepoints at baseline and immediately postintervention, and for a number of studies that continued to measure the effect of the intervention in the longer term, the assessment timepoint was commonly scheduled at more than 1 month postintervention. A previous meta-analysis on mindfulness-based programmes for promoting mental health also separated psychological distress measures measured less than 1 month after programme completion versus those measured months after programme completion.23 Subgroup analyses were performed for the mode of intervention delivery and occupation. Sensitivity analyses were performed using the leave-one-out method.
Results
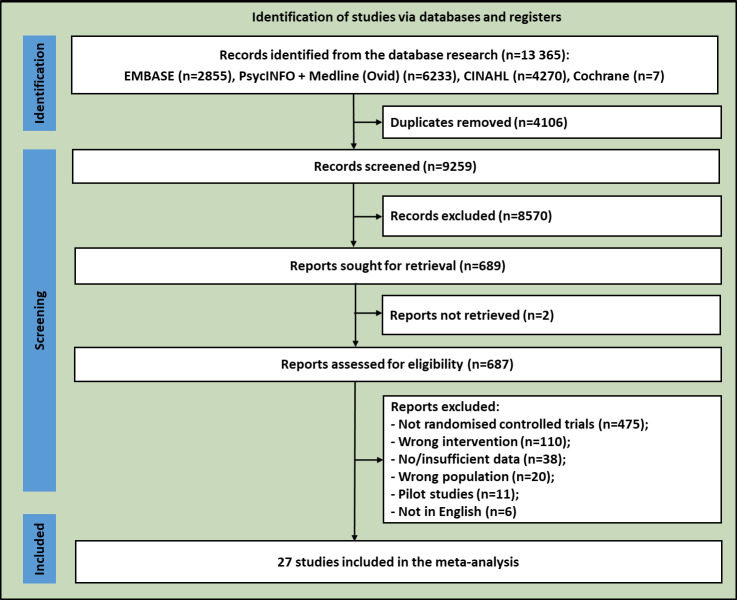
Figure 1 shows the literature search and retrieval process. As seen, the initial search yielded 13 365 studies. After duplicates were removed, 9259 studies were screened in the title and abstract stage. Full texts of 687 articles were reviewed and 27 articles (containing a total of 2506 healthcare professionals) were eventually included in the meta-analysis.24–50
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart showing the study abstraction process. CINAHL, Cumulative Index for Nursing and Allied Health Literature.
Characteristics of studies
The detailed characteristics of the 27 included studies can be found in online supplemental table S2. A large number of studies were conducted in the USA (n=8),25 31 34 35 42 44 45 47 followed by Spain (n=5).26 27 29 43 46 Five studies were conducted in China,30 38–40 49 two each in Australia36 48 and Germany,33 37 and one each in Colombia,41 Italy,28 Iran,24 Sweden32 and Turkey.50
Most of the studies (n=12) had mixed populations of healthcare workers. Seven studies only recruited doctors in their study population; six studies solely involved nurses; and only two studies focused exclusively on allied health professionals. Study participants for a large majority of the studies were recruited from hospital settings.
Characteristics of interventions
There was significant variation in the duration, frequency and assessment timepoints among the studies. Mindfulness-based stress reduction programme (n=10) was the most common intervention type among the included studies. Other interventions used include mindfulness apps, mindfulness-based meditation and mindfulness-based training.
Interventions ranged from 10 min to 8 hours28 in duration for each session, with the overall intervention duration ranging from 1 day to 10 weeks. Assessment points ranged from immediately postintervention to 12 months postintervention. Interventions in 24 studies were delivered in person, while three were delivered remotely. A single study45 was delivered in a mostly remote format, with one session in person and the remaining five sessions remotely.
Short-term outcomes (less than 1 month postintervention)
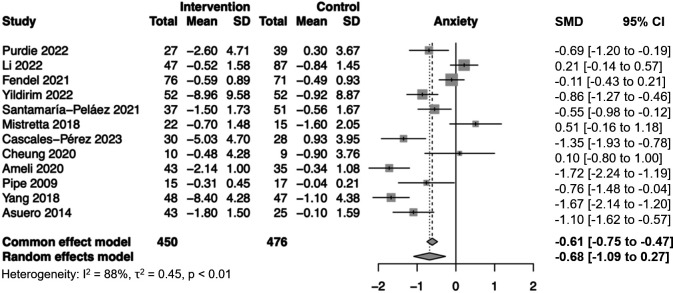
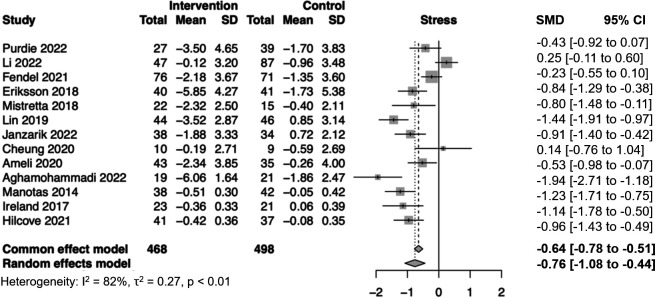
MBIs had small to large effects on deficit-based outcomes such as anxiety (SMD=−0.68, 95% confidence interval (CI): −1.09 to −0.27, p=0.001, I2=88%) (figure 2), burnout (SMD=−0.44, 95% CI: −0.74 to −0.13, p=0.005, I2=69%), stress (SMD=−0.76, 95% CI: −1.08 to −0.44, p<0.001, I2=82%) (figure 3), depression (SMD=−0.50, 95% CI: −0.87 to −0.13, p=0.008, I2=83%), psychological distress (SMD=−0.85, 95% CI: −1.11 to −0.59, p<0.001, I2=0%) and job strain (SMD=−0.49, 95% CI: −0.82 to −0.16, p=0.003, I2=40%) (online supplemental figures S1, S2, S7 and S8).
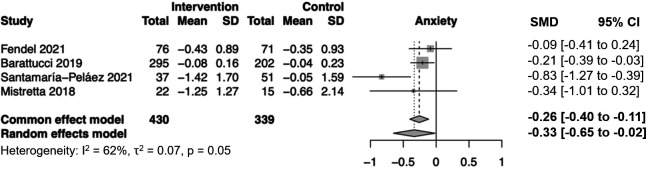
Figure 2.
Forest plot showing meta-analysis of anxiety outcomes within 1 month. SD, standard deviation; SMD, standardised mean difference.
Figure 3.
Forest plot showing meta-analysis of stress outcomes within 1 month. SD, standard deviation; SMD, standardised mean difference.
Small to large effects were also observed in asset-based outcomes such as self-compassion (SMD=0.86, 95% CI: 0.24 to 1.49, p=0.007, I2=73%), and empathy (SMD=0.42), mindfulness (SMD=0.92, 95% CI: 0.48 to 1.37, p<0.001, I2=81%) and positive well-being (SMD=0.55, 95% CI: 0.16 to 0.94, p=0.005, I2=63%), while no statistically significant effect was observed for the outcome of resilience (SMD=0.29, 95% CI: −0.18 to 0.77, p=0.221, I2=70%) (online supplemental figures S3, S4, S5 and S6).
The sensitivity analysis performed for the meta-analyses is presented in supplemental figures S31 and S34. By excluding one study at each analysis, we confirmed the statistical validity of the estimates (online supplemental figuresS31 and S34).
Subgroup analysis by occupation
Among nurses, moderate to large effects were observed for the outcomes of anxiety (SMD=−1.12, 95% CI: −1.70 to −0.55, I2=74%), depression (SMD=−1.14, 95% CI: −1.96 to −0.33, I2=73%), stress (SMD=−1.18, 95% CI: −1.70 to −0.66, I2=58%), positive well-being (SMD=0.58, 95% CI: 0.08 to 1.07, I2=74%) and psychological distress (SMD=−0.82, 95% CI: −1.14 to −0.51, I2=0%). No significant effect was observed for outcomes of resilience (SMD=0.29, 95% CI: −0.18 to 0.77, I2=70%) or burnout (SMD=0.14, 95% CI: −0.31 to 0.58) (online supplemental figures S16-S19 and S22-S24).
Among allied health professionals, a moderate improvement in stress outcomes (SMD=−1.35, 95% CI: −2.43 to −0.27, I2=83%) was observed (online supplemental figure S19).
Among doctors, MBIs had no significant effect on outcomes of anxiety (SMD=−0.28, 95% CI: −0.72 to 0.17, I2=53%), burnout (SMD=−0.34, 95% CI: −0.77 to 0.08, I2=65%), depression (SMD=−0.07, 95% CI: −0.34 to 0.20, I2=0%), stress (SMD=−0.43, 95% CI: −0.88 to 0.02, I2=60%) and mindfulness (SMD=0.86, 95% CI: −0.26 to 1.98, I2=91%) (online supplemental figures S16-S20).
For studies with mixed populations, moderate to large effects were observed for outcomes of burnout (SMD=−0.83, 95% CI: −1.20 to −0.45, I2=0%), depression (SMD=−0.45, 95% CI: −0.88 to −0.02, I2=78%), stress (SMD=−0.63, 95% CI: −1.16 to −0.11, I2=87%) and mindfulness (SMD=0.91, 95% CI: 0.43 to 1.39, I2=74%). No significant effect was observed for outcomes of anxiety (SMD=−0.67, 95% CI: −1.37 to 0.04, I2=91%) and self-compassion (SMD=0.62, 95% CI: −0.19 to 1.43, I2=76%) (online supplemental figures S16-S21).
Differences between doctors, nurses, allied health workers and mixed populations were significant for outcomes of burnout (p=0.008) and depression (p=0.027) (online supplemental figures S17 and S18). No significant between-group differences were observed for the other outcomes of anxiety (p=0.073), mindfulness (p=0.995), stress (p=0.116) and self-compassion (p=0.158) (online supplemental figures S16, S19, S20 and S21).
Subgroup analysis by mode of intervention delivery
Moderate effects were observed in stress outcomes for both in-person (SMD=−0.79, 95% CI: −1.17 to −0.41, I2=85%) and remote (SMD=−0.64, 95% CI: −1.05 to −0.24, I2=31%) interventions. In-person interventions were associated with moderate reductions in burnout (SMD=−0.43, 95% CI: −0.83 to −0.04, I2=69%) while there was no significant effect on burnout associated with remote interventions (SMD=−0.47, 95% CI: −0.95 to 0.01, I2=52%) (online supplemental figures S14 and S15).
However, differences between remote and in-person interventions were not significant for both outcomes of burnout (p=0.908) and stress (p=0.614) (online supplemental figures S14 and S15). Subgroup analysis for other outcomes of wellness by mode of intervention delivery was not conducted due to the small number of studies.
Longer term outcomes (1 month or longer postintervention)
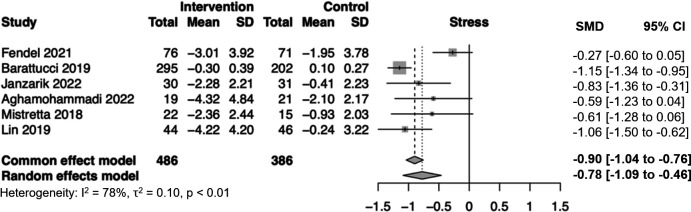
There was a significant improvement in positive well-being (SMD=0.87, 95% CI: 0.46 to 1.28, p<0.001, I2=37%), resilience (SMD=0.45, 95% CI: 0.06 to 0.83, p=0.023, I2=53%), stress (SMD=−0.78, 95% CI: −1.09 to −0.46, p<0.001, I2=78%) (figure 4) and anxiety outcomes (SMD=−0.33, 95% CI: −0.65 to −0.02, p=0.039, I2=62%) (figure 5). No significant effect was observed for outcomes of burnout (SMD=0.05, 95% CI: −0.76 to 0.85, p=0.913, I2=88%), depression (SMD=−0.39, 95% CI: −1.00 to 0.22, p=0.208, I2=84%) and self-compassion (SMD=0.56, 95% CI: −0.40 to 1.51, p=0.254, I2=83%) (online supplemental figures S9-S13).
Figure 4.
Forest plot showing meta-analysis of stress outcomes beyond 1 month. SD, standard deviation; SMD, standardised mean difference.
Figure 5.
Forest plot showing meta-analysis of anxiety outcomes beyond 1 month. SD, standard deviation; SMD, standardised mean difference.
Subgroup analysis by occupation
Among nurses, moderate to large effects were observed for outcomes of stress (SMD=−0.96, 95% CI −1.30 to −0.63, I2=80%), positive well-being (SMD=0.92, 95% CI 0.29 to 1.55, I2=37%) and resilience (SMD=0.45, 95% CI 0.06 to 0.83, I2=30%) (online supplemental figures S27, S29 and S30).
For studies with mixed populations, moderate to large effects were observed for outcomes of anxiety (SMD=−0.44, 95% CI −0.84 to −0.03, I2=69%), depression (SMD=−0.72, 95% CI −1.19 to −0.25, I2=32%) and stress (SMD=−0.98, 95% CI −1.47 to −0.49, I2=56%) (online supplemental figures S25, S26 and S27). No significant effect was observed for self-compassion outcomes (SMD=0.62, 95% CI −0.19 to 1.43, I2=76%) (online supplemental figure S28). Subgroup analysis for doctors and allied health staff was not conducted due to the small number of studies.
Quality of evidence
Based on the GRADE approach, the overall quality of evidence was rated as high for outcomes of stress, anxiety, depression, burnout, mindfulness, well-being, resilience, psychological distress, job strain and moderate for self-compassion outcomes (online supplemental table S4).
Risk of bias
Based on the risk of bias assessment, 15 studies (55.6%) had an overall moderate risk of bias (rated as having ‘some concerns’) and 12 studies (44.4%) had low risk of bias (online supplemental table S3). There were no studies rated as having a high risk of bias. However, as the quality of the studies was inconsistent, more high-quality randomised controlled trials are still necessary.
Publication bias
We qualitatively and quantitatively assessed for publication bias through visual inspection of funnel plot asymmetry (online supplemental figures S31–S47), trim-and-full imputation of potentially missing studies (online supplemental tables S5 and S6) and the Egger’s test (online supplemental tables S7 and S8). Funnel plots for all outcomes were largely symmetrical on visual inspection. Publication bias was largely absent for all outcomes.
Discussion
Main findings
The number of healthcare workers who report burnout, the emotional exhaustion and depersonalisation that arise from job fatigue and dissatisfaction, is reaching epidemic proportions.1 3 MBIs offer a promising solution to combat this growing issue. This meta-analysis represents the first comprehensive examination of the effects of MBIs across a range of healthcare professionals. Our findings indicate that these interventions have a beneficial impact on several aspects of well-being in the short term, thereby suggesting their potential to enhance the well-being of healthcare workers promptly. Over the long term, while significant improvements were observed in areas such as anxiety, stress, resilience, positive well-being, and mindfulness, the benefits were not consistently sustained across all outcomes, including burnout, depression, and self-compassion.
The magnitude of effect sizes was small to moderate and could vary depending on several factors, including the nature of the intervention being studied, the characteristics of the study population and the heterogeneity of the data. This finding concurs with a 2021 meta-analysis which evaluated the empirical status of MBIs.51 The authors also found a range of effect sizes and statistically significant meta-analytical effect sizes varied between small (Cohen’s d=0.21, for well-being) and moderate (Cohen’s d=0.55, for psychiatric symptoms) based on randomised controlled trials.51 This suggests that MBIs may have a differing level of impact on different aspects of healthcare workers’ well-being, although the researchers found few consistent moderators.51 The most significant improvements were typically observed in domains directly related to mindfulness practice, including mindfulness itself, as well as reductions in rumination, worry, and emotional reactivity.52
In our analyses, heterogeneity for some of the forest plots was high (I2 as high as 88%), likely due to the inherent heterogeneity of the intervention types, intervention duration, frequency, differing healthcare roles and disparate operating contexts of the various healthcare settings. In Lin et al’s study,39 the mindfulness-based stress reduction intervention for nurses resulted in a large reduction in stress outcomes (SMD=−1.44, 95% CI: −1.91 to 0.97). However, in Fendel et al’s study,33 where the programme was conducted for doctors, a similar mindfulness-based stress reduction intervention yielded a much smaller effect size (SMD=−0.23, 95% CI: −0.55 to 0.10).
Data from the subgroup analysis by occupation suggest that mindfulness interventions are effective in the short term for improving wellness in doctors, nurses and allied health staff, although there was a considerable variation between doctor, nurse and mixed populations with respect to the specific outcomes that showed significant improvement. It is notable that the improvements in a number of outcomes, such as stress and depression, were significant for nurses and mixed populations but not for doctors. As between-group differences were significant for outcomes of burnout and depression, this raises the possibility that mindfulness interventions may have differing impacts on doctors versus nurses. Similar to the main analysis, the effects of a number of outcomes were maintained over the longer term while others were not. The significant improvement in resilience outcomes in the longer term but not in the short term could be attributed to the few number of studies that evaluated resilience scores in the longer term postintervention, which limited our analysis.
Our results suggest that the effect of individual-based interventions diminishes over time, hence the need for such interventions to be repeated for their effects to be maintained in the long term. Moreover, there are likely many other factors within the workplace that influence well-being, pointing to the need for not only individual-based but organisation-wide interventions to improve well-being in the long term. Organisation-directed interventions that directly target workplace risk factors have also proven effective in reducing burnout,53 and such individual-directed and institutional interventions may complement each other to more comprehensively address burnout among healthcare workers.
Although there were only three studies in our analysis that carried out their interventions remotely,32 45 48 remote interventions produced significant improvements in various wellness outcomes. This highlights the potential of remotely delivered MBIs in having a comparable effectiveness to in-person interventions. As in-person workshops and classes may be more logistically challenging and resource intensive to organise compared with online resources, especially for a large group of people, remote interventions may be helpful in making such programmes more accessible and convenient for busy healthcare professionals. Additionally, previous meta-analyses have also provided evidence supporting the effectiveness of eHealth interventions in improving well-being.54 55 However, adherence to digital resources is often low,45 56 and it may be helpful to consider supplementing the provision of digital resources with in-person group mindfulness sessions.57 At least as an interim measure, it may still be worthwhile to put in place digital interventions that are more cost-effective, accessible, convenient and repeatable (eg, mobile app-based).
Limitations
Nonetheless, the findings of the present review should be interpreted in light of the following limitations. Previous research has pointed out that physicians were the most studied out of all healthcare professionals.58 Similarly, a majority of included articles in this review focused solely on physicians or nurses, and there is a paucity of research literature on the effectiveness of MBIs on allied health workers in particular. It is also unclear if the effects of these interventions can be sustained, as follow-up timepoints for many studies were limited to the short term, often directly postintervention. Going forward, studies should more closely examine whether the effects of such interventions are sustained in the long term, and what can be done to sustain the effects of such interventions. Some individuals may be more engaged and continue to practise their mindfulness skills compared with others. Studies also varied in the outcomes measured, for example, there were only a small number of studies that measured certain outcomes such as job strain, which led to reduced power in subgroup comparisons for such outcomes. The findings from this review may also lack generalisability given the heterogeneity of intervention types, duration, frequency and unique operating context of the various healthcare settings. The majority of the included studies were conducted in the USA and Europe, and there were few Asian studies, suggesting the need for future work to examine the effectiveness of such interventions in the Asian context as well. Future research should continue to examine the utility of remotely delivered or hybrid interventions, as well as compare the various modes of delivery of online interventions (eg, web-based vs app-based). More research could also be done to explore the effectiveness of different types of MBIs (eg, group discussions, breathing exercises, cognitive–behavioural therapy, etc).
Implications
MBIs may work to address the psychological and emotional aspects of well-being as they encourage individuals to pay closer attention to each moment in a non-judgemental way.59 They may also help alleviate stress by modulating the sympathetic-adrenal medulla system60 and modifying the way in which the brain reacts to stressful situations through neuroplasticity.61 62 Besides in-person interventions, remotely delivered MBIs may be effective as well.
Based on the analyses, nurses may benefit more from MBIs. To maximise the benefits of mindfulness interventions, it may be worthwhile to consider tailoring interventions to specific healthcare populations as different healthcare professions may encounter distinct stressors and challenges. Nevertheless, future studies should consider longer follow-up periods to assess the durability of the intervention effects and explore potential maintenance strategies to sustain the benefits beyond the intervention period, as evidence appears to be particularly lacking on this front.
Conclusion
Our review indicates that MBIs could positively impact healthcare workers’ well-being in the short term. While these interventions might work at the periphery rather than address the fundamental causes of workplace stress, they hold promise in alleviating symptoms related to stress and burnout among healthcare professionals. At present, there is notable heterogeneity in the types of interventions and the populations they target, leading to varied effectiveness across different groups. Identifying the factors that contribute to their effectiveness, as well as their limitations within diverse healthcare worker groups, is crucial for future research. Additionally, investigating how these programs can be maintained over time and their enduring impacts will be essential for their implementation and sustained benefit.
Biography
Natasha Yixuan Ong is currently a third-year medical student at the NUS Yong Loo Lin School of Medicine, National University of Singapore. She will be graduating in 2026. She has worked on a number of systematic reviews and meta-analysis research projects on a wide range of topics ranging from neurology, mental health to paediatrics. She hopes to further conduct studies examining the interplay of factors related to child health and genetics. She is particularly enthusiastic about investigating how genetic factors could influence the longitudinal course and long-term outcomes of paediatric diseases. She also has an interest in psychology.

Footnotes
@ChunEnYau, @ng_qin_xiang
NYO and QXN contributed equally.
Contributors: QXN conceived the original idea. NYO, FJJT, JZYE, CEY and QXN carried out the study and the relevant data analysis and interpretation. JT and HKT supervised the study. All authors contributed to the data analysis and interpretation. All authors discussed the results, contributed to the writing of the paper and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth 2020;13:171–83. 10.2147/LRA.S240564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Petrella AR, Hughes L, Fern LA, et al. Healthcare staff well-being and use of support services during COVID-19: a UK perspective. Gen Psychiatr 2021;34:e100458. 10.1136/gpsych-2020-100458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smallwood N, Karimi L, Bismark M, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. Gen Psychiatr 2021;34:e100577. 10.1136/gpsych-2021-100577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Laboe CW, Jain A, Bodicherla KP, et al. Physician suicide in the era of the COVID-19 pandemic. Cureus 2021;13:e19313. 10.7759/cureus.19313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Menon NK, Shanafelt TD, Sinsky CA, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw Open 2020;3:e2028780. 10.1001/jamanetworkopen.2020.28780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ 2016;50:132–49. 10.1111/medu.12927 [DOI] [PubMed] [Google Scholar]
- 7. Chong RIH, Yaow CYL, Chong N-Y, et al. Scoping review of the second victim syndrome among surgeons: understanding the impact, responses, and support systems. Am J Surg 2024;229:5–14. 10.1016/j.amjsurg.2023.09.045 [DOI] [PubMed] [Google Scholar]
- 8. Dyrbye LN, Leep Hunderfund AN, Winters RC, et al. The relationship between burnout and help-seeking behaviors, concerns, and attitudes of residents. Acad Med 2021;96:701–8. 10.1097/ACM.0000000000003790 [DOI] [PubMed] [Google Scholar]
- 9. Hilton LG, Marshall NJ, Motala A, et al. Mindfulness meditation for workplace wellness: an evidence map. WOR 2019;63:205–18. 10.3233/WOR-192922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shapiro SL, Carlson LE, Astin JA, et al. Mechanisms of mindfulness. J Clin Psychol 2006;62:373–86. 10.1002/jclp.20237 [DOI] [PubMed] [Google Scholar]
- 11. Eberth J, Sedlmeier P. The effects of mindfulness meditation: a meta-analysis. Mindfulness 2012;3:174–89. 10.1007/s12671-012-0101-x [DOI] [Google Scholar]
- 12. Lim D, Condon P, DeSteno D. Mindfulness and compassion: an examination of mechanism and scalability. PLoS ONE 2015;10:e0118221. 10.1371/journal.pone.0118221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pérez-Fuentes M del C, Molero Jurado M del M, Mercader Rubio I, et al. Mindfulness for preventing Psychosocial risks in the workplace: a systematic review and meta-analysis. Appl Sci 2020;10:1851. 10.3390/app10051851 [DOI] [Google Scholar]
- 14. Burton A, Burgess C, Dean S, et al. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress Health 2017;33:3–13. 10.1002/smi.2673 [DOI] [PubMed] [Google Scholar]
- 15. Kriakous SA, Elliott KA, Lamers C, et al. The effectiveness of mindfulness-based stress reduction on the psychological functioning of healthcare professionals: a systematic review. Mindfulness (N Y) 2021;12:1–28. 10.1007/s12671-020-01500-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schünemann H, Brożek J, Guyatt G, eds. GRADE handbook for grading guality of evidence and strength of recommendations. Available: https://gdt.gradepro.org/app/handbook/handbook.html [Accessed 10 Jan 2024].
- 18. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 19. Takeshima N, Sozu T, Tajika A, et al. Which is more generalizable, powerful and interpretable in meta-analyses, mean difference or standardized mean difference BMC Med Res Methodol 2014;14:30. 10.1186/1471-2288-14-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hedges LV. Distribution theory for glass’s estimator of effect size and related estimators. J Educ Stat 1981;6:107. 10.2307/1164588 [DOI] [Google Scholar]
- 21. Faraone SV. Interpreting estimates of treatment effects: implications for managed care. P T 2008;33:700–11. [PMC free article] [PubMed] [Google Scholar]
- 22. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 23. Galante J, Friedrich C, Aeamla-Or N, et al. Individual participant data systematic review and meta-analysis of randomised controlled trials assessing adult mindfulness-based programmes for mental health promotion in non-clinical settings. Nat Mental Health 2023;1:462–76. 10.1038/s44220-023-00081-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aghamohammadi F, Saed O, Ahmadi R, et al. The effectiveness of adapted group mindfulness-based stress management program on perceived stress and emotion regulation in midwives: a randomized clinical trial. BMC Psychol 2022;10:123. 10.1186/s40359-022-00823-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ameli R, Sinaii N, West CP, et al. Effect of a brief mindfulness-based program on stress in health care professionals at a US biomedical research hospital: a randomized clinical trial. JAMA Netw Open 2020;3:e2013424. 10.1001/jamanetworkopen.2020.13424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Amutio A, Martínez-Taboada C, Delgado LC, et al. Acceptability and effectiveness of a long-term educational intervention to reduce physicians' stress-related conditions. J Contin Educ Health Prof 2015;35:255–60. 10.1097/CEH.0000000000000002 [DOI] [PubMed] [Google Scholar]
- 27. Asuero AM, Queraltó JM, Pujol-Ribera E, et al. Effectiveness of a mindfulness education program in primary health care professionals: a pragmatic controlled trial. J Contin Educ Health Prof 2014;34:4–12. 10.1002/chp.21211 [DOI] [PubMed] [Google Scholar]
- 28. Barattucci M, Padovan AM, Vitale E, et al. Mindfulness-based IARA model® proves effective to reduce stress and anxiety in health care professionals. A six-month follow-up study. Int J Environ Res Public Health 2019;16:4421. 10.3390/ijerph16224421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cascales-Pérez ML, Ferrer-Cascales R, Fernández-Alcántara M, et al. Effects of a mindfulness-based programme on the health- and work-related quality of life of healthcare professionals. Scand J Caring Sci 2021;35:881–91. 10.1111/scs.12905 [DOI] [PubMed] [Google Scholar]
- 30. Chen H, Liu C, Cao X, et al. Effects of loving-kindness meditation on doctors' mindfulness, empathy, and communication skills. IJERPH 2021;18:4033. 10.3390/ijerph18084033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cheung EO, Barsuk JH, Mitra D, et al. Preliminary efficacy of a brief mindfulness intervention for procedural stress in medical intern simulated performance: a randomized controlled pilot trial. J Altern Complement Med 2020;26:282–90. 10.1089/acm.2019.0209 [DOI] [PubMed] [Google Scholar]
- 32. Eriksson T, Germundsjö L, Åström E, et al. Mindful self-compassion training reduces stress and burnout symptoms among practicing psychologists: a randomized controlled trial of a brief web-based intervention. Front Psychol 2018;9:2340. 10.3389/fpsyg.2018.02340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fendel JC, Aeschbach VM, Schmidt S, et al. The impact of a tailored mindfulness-based program for resident physicians on distress and the quality of care: a randomised controlled trial. J Intern Med 2021;290:1233–48. 10.1111/joim.13374 [DOI] [PubMed] [Google Scholar]
- 34. Grabbe L, Higgins MK, Baird M, et al. The community resiliency model® to promote nurse well-being. Nurs Outlook 2020;68:324–36. 10.1016/j.outlook.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 35. Hilcove K, Marceau C, Thekdi P, et al. Holistic nursing in practice: mindfulness-based yoga as an intervention to manage stress and burnout. J Holist Nurs 2021;39:29–42. 10.1177/0898010120921587 [DOI] [PubMed] [Google Scholar]
- 36. Ireland MJ, Clough B, Gill K, et al. A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Med Teach 2017;39:409–14. 10.1080/0142159X.2017.1294749 [DOI] [PubMed] [Google Scholar]
- 37. Janzarik G, Wollschläger D, Wessa M, et al. A group intervention to promote resilience in nursing professionals: a randomised controlled trial. Int J Environ Res Public Health 2022;19:649. 10.3390/ijerph19020649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Li J-M, Wu R, Zhang T, et al. Psychological responses of medical staff during COVID-19 and the adjustment effect of brief mindfulness meditation. Complement Ther Clin Pract 2022;48:101600. 10.1016/j.ctcp.2022.101600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lin L, He G, Yan J, et al. The effects of a modified mindfulness-based stress reduction program for nurses: a randomized controlled trial. Workplace Health Saf 2019;67:111–22. 10.1177/2165079918801633 [DOI] [PubMed] [Google Scholar]
- 40. Liu C, Chen H, Cao X, et al. Effects of mindfulness meditation on doctors’ mindfulness, patient safety culture, patient safety competency and adverse event. IJERPH 2022;19:3282. 10.3390/ijerph19063282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Manotas M, Segura C, Eraso M, et al. Association of brief Mindfulness training with reductions in perceived stress and distress in Colombian health care professionals. Int J Stress Manag 2014;21:207–25. 10.1037/a0035150 [DOI] [Google Scholar]
- 42. Mistretta EG, Davis MC, Temkit M, et al. Resilience training for work-related stress among health care workers. J Occup Environ Med 2018;60:559–68. 10.1097/JOM.0000000000001285 [DOI] [PubMed] [Google Scholar]
- 43. Pérula-de Torres L, Verdes-Montenegro-Atalaya J, Melús-Palazón E, et al. Comparison of the effectiveness of an abbreviated program versus a standard program in mindfulness, self-compassion and self-perceived empathy in tutors and resident intern specialists of family and community medicine and nursing in Spain. IJERPH 2021;18:4340. 10.3390/ijerph18084340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pipe TB, Bortz JJ, Dueck A, et al. Nurse leader mindfulness meditation program for stress management: a randomized controlled trial. J Nurs Adm 2009;39:130–7. 10.1097/NNA.0b013e31819894a0 [DOI] [PubMed] [Google Scholar]
- 45. Purdie DR, Federman M, Chin A, et al. Hybrid delivery of mindfulness meditation and perceived stress in pediatric resident physicians: a randomized clinical trial of in-person and digital mindfulness meditation. J Clin Psychol Med Settings 2023;30:425–34. 10.1007/s10880-022-09896-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Santamaría-Peláez M, González-Bernal JJ, Verdes-Montenegro-Atalaya JC, et al. Mindfulness-based program for anxiety and depression treatment in healthcare professionals: a pilot randomized controlled trial. J Clin Med 2021;10:5941. 10.3390/jcm10245941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Valley MA, Stallones L. Effect of mindfulness-based stress reduction training on health care worker safety: a randomized waitlist controlled trial. J Occup Environ Med 2017;59:935–41. 10.1097/JOM.0000000000001090 [DOI] [PubMed] [Google Scholar]
- 48. Xu HG, Eley R, Kynoch K, et al. Effects of mobile mindfulness on emergency department work stress: a randomised controlled trial. Emerg Med Australas 2022;34:176–85. 10.1111/1742-6723.13836 [DOI] [PubMed] [Google Scholar]
- 49. Yang J, Tang S, Zhou W. Effect of mindfulness-based stress reduction therapy on work stress and mental health of psychiatric nurses. Psychiatr Danub 2018;30:189–96. 10.24869/psyd.2018.189 [DOI] [PubMed] [Google Scholar]
- 50. Yıldırım D, Çiriş Yıldız C. The effect of mindfulness-based breathing and music therapy practice on nurses' stress, work-related strain, and psychological well-being during the COVID-19 pandemic: a randomized controlled trial. Holist Nurs Pract 2022;36:156–65. 10.1097/HNP.0000000000000511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Goldberg SB, Riordan KM, Sun S, et al. The empirical status of mindfulness-based interventions: a systematic review of 44 meta-analyses of randomized controlled trials. Perspect Psychol Sci 2022;17:108–30. 10.1177/1745691620968771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shapero BG, Greenberg J, Pedrelli P, et al. Mindfulness-based interventions in psychiatry. Focus (Am Psychiatr Publ) 2018;16:32–9. 10.1176/appi.focus.20170039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017;177:195–205. 10.1001/jamainternmed.2016.7674 [DOI] [PubMed] [Google Scholar]
- 54. Deady M, Choi I, Calvo RA, et al. eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta-analysis. BMC Psychiatry 2017;17:310. 10.1186/s12888-017-1473-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mackenzie A, Harvey S, Mewton L, et al. Occupational impact of internet-delivered cognitive behaviour therapy for depression and anxiety: reanalysis of data from five Australian randomised controlled trials. Med J Aust 2014;201:417–9. 10.5694/mja14.00293 [DOI] [PubMed] [Google Scholar]
- 56. Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app‘calm’ to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth 2019;7:e14273. 10.2196/14273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Xu HG, Kynoch K, Tuckett A, et al. Effectiveness of interventions to reduce emergency department staff occupational stress and/or burnout: a systematic review. JBI Evid Synth 2020;18:1156–88. 10.11124/JBISRIR-D-19-00252 [DOI] [PubMed] [Google Scholar]
- 58. White C. Doctors: the invisible patients. BMJ 2010:c2013. 10.1136/bmj.c2013 [DOI] [Google Scholar]
- 59. Dekeyser M, Raes F, Leijssen M, et al. Mindfulness skills and interpersonal behaviour. Pers Individ Differ 2008;44:1235–45. 10.1016/j.paid.2007.11.018 [DOI] [Google Scholar]
- 60. Creswell JD, Lindsay EK. How does mindfulness training affect health? A mindfulness stress Buffering account. Curr Dir Psychol Sci 2014;23:401–7. 10.1177/0963721414547415 [DOI] [Google Scholar]
- 61. Pagnoni G, Cekic M. Age effects on gray matter volume and attentional performance in Zen meditation. Neurobiol Aging 2007;28:1623–7. 10.1016/j.neurobiolaging.2007.06.008 [DOI] [PubMed] [Google Scholar]
- 62. Hölzel BK, Carmody J, Vangel M, et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res 2011;191:36–43. 10.1016/j.pscychresns.2010.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gpsych-2023-101115supp001.pdf (3.2MB, pdf)