ABSTRACT
Background:
Depression contributes to the major burden of mental illness in India. Assessment of burden is essential to develop interventions to address the problem at the primary care level.
Materials and Methods:
We carried out a systematic review and meta-analysis of studies documenting the prevalence of depression in primary care in India. A wide literature search strategy was developed using keywords and Medical Subject Headings. The literature search was done in MEDLINE (via PubMed), IndMed, and major Indian psychiatric journal websites. The protocol was registered at PROSPERO. Bias assessment was carried out using a Cochrane risk of bias tool.
Results:
A total of 186 studies were identified after an initial search, of which 17 were included in the final analysis using pre-specified inclusion and exclusion criteria. The aggregate point prevalence of depression at the primary care level of the 17 studies using the random-effect model was 23.0% (95% CI: 16.0-30.0%). Significant heterogeneity was reported among the studies attributed majorly to a variety of study tools for assessing depression. Sub-group analysis revealed the higher aggregated prevalence of depression among females as compared to males at the primary care level.
Conclusion:
The study provided updated evidence of higher and gender differential burden of depression at the primary care level in India.
Keywords: Depression, India, primary care
Background
Mental disorders were the second leading cause of disease burden in terms of years lived with disability (YLDs) and the sixth leading cause of disability-adjusted life-years (DALYs) in the world in 2017, posing a serious challenge to health systems, particularly in low-income and middle-income countries.[1] Mental health is being recognized as one of the priority areas in health policies around the world and has also been included in the Sustainable Development Goals.[2,3,4]
The total number of people living with depression in 2017 in the world was 322 million. Nearly half of these people live in the South-East Asia Region and Western Pacific Region, reflecting the relatively larger populations of those two regions.[5] The total estimated number of people living with depression increased by 18.4% between 2005 and 2015.[6]
The lifetime prevalence of major depressive disorders is 10-25% for women and 5-12% for men.[7] According to the World Health Organization (WHO), it is also the most important precursor of suicide and will be the second cause of Global Disease Burden by the year 2020, and WHO states that the burden of depression is 50% higher for females than males and Indians are reported to be among the world’s most depressed. National Mental Health Survey 2015-16 reveals that nearly 15% Indian adults need active intervention for one or more mental health issues and one in 20 Indians suffers from depression.[8]
Up to 20% of those attending primary health care in developing countries suffer from the often-linked disorders of anxiety and depression, but the symptoms of these conditions are often not recognized.[9] The preponderance of female cases of depressive disorder is consistent finding from India.[10,11] Women have the greatest risk for developing depressive disorders during their child-bearing years. Psychosocial events such as role stress, victimization, sex-specific socialization, internalization, coping style, disadvantaged social status, and perceived stigma of mental illness, more in females,[12] have all been considered to contribute to the increased vulnerability of women to depression. The prevalence of mental morbidity in married women from Mumbai was found out to be 27.2% using a self-reported questionnaire from WHO with higher reporting of somatic symptoms than emotional symptoms.[13]
However, it is crucial to benchmark the prevalence of depression in India and gender differences in depression. We conducted this systematic review and meta-analysis with objective to find the prevalence of depression in primary healthcare attenders in India and to assess gender differential of prevalence of depression at primary healthcare level in India.
Materials and Methods
Protocol and registration
The protocol of this systematic review was registered in PROSPERO (International prospective register of systematic reviews) at www.crd.york.ac.uk under the PROSPERO-ID CRD4201605403.
Search strategy
A wide literature search strategy was developed using keywords and Medical Subject Headings from four categories: population, outcome, intervention type, and study design. The search terms from each category were combined in order to locate all relevant literature using the following databases: MEDLINE (via PubMed), IndMed, and major Indian psychiatric journal websites. The search was last conducted on December 12, 2019. Following keywords were used: a) Depression, b) Prevalence, c) Primary Health Care, d) General Practitioner, and e) India. All grey literature whether published or not published was also searched. Only those articles that were in English were selected.
Search conducted in both manual and electronic searches. Electronic search was conducted in all major electronic databases like PubMed (Medline), IndMed, and major Indian psychiatric journal websites. Search strategy for PubMed search engine is provided in the Box 1.
Box 1.
Search strategy
| List of Keywords: |
| Depression |
| Prevalence |
| Primary Health Care |
| General Practitioner |
| India |
| Pub-Med Search Strategy: |
| ((Depression or Depressive disorder or Major depression or Common |
| Mental Disorder [MeSH Terms])) AND (Primary Health Care OR |
| General Practice OR General Physician [MeSH Terms])) AND India |
Data extraction
Initial review was conducted by HRS and RSR. Titles and/or abstracts of studies retrieved using the search strategy, and those from additional sources were screened independently by HRS and RSR to identify studies that potentially meet the inclusion criteria outlined above. The full text of these potentially eligible studies was retrieved and independently assessed for eligibility by HRS and RSR. Any disagreement between them over the eligibility of particular studies was resolved through discussion with RS. SV, RRS, JA, and SHR conducted the analysis. In case of non-availability of full text of article, authors contacted for full text. If gender-wise details were also not available, then authors contacted to provide gender-wise depression data.
Outcome
Primary Outcome: Prevalence of depression at primary healthcare level.
Secondary Outcomes: Gender differences in prevalence of depression.
Bias assessment
SHR and JA independently reviewed the selected articles for bias assessment using the Cochrane risk of bias tool. Disagreements between the review authors over the risk of bias in particular studies were resolved by discussion, with involvement of SHR where necessary. Sensitivity analysis was performed to see effect of studies on gender risk for depression, excluded due to non-availability of gender difference data.
Data analysis
Narrative synthesis of the findings from the included studies and structured around outcome was provided. Results were pooled using a random-effects meta-analysis, with standardized mean differences for continuous outcomes and odds ratios for binary outcomes, and 95% confidence intervals and two-sided P values for each outcome were calculated. Heterogeneity between the studies in effect measures was assessed using both the Chi-squared test and the I-squared statistic. I-squared value greater than 50% indicative was taken as measure of substantial heterogeneity. Sensitivity analyses done based on study quality. Stratified meta-analyses were done to explore heterogeneity in effect estimates according to study quality; study populations; the logistics of intervention provision; and intervention content. We assessed evidence of publication bias. Study setting wise and gender-wise subgroup analysis were done.
Results
Study identification
A total of 186 studies were identified after an initial search. After removal of duplicates, we reviewed 184 studies in full. After exclusion of the ineligible studies and addition of articles from the references of included studies, 17 studies were finally included. One study was specific to the elderly, and 14 studies were among adult age groups (years varied among different studies). The flow diagram of the search process is shown in Figure 1. The sample sizes of the reviewed studies ranged from 28 to 1366 (median 218), with a total of 6,522 participants. Characteristics of the included studies. The prevalence of depression and characteristics of the selected studies are presented in Tables 1 and 2. All the included studies reported point prevalence of depression. In terms of the assessment methods, studies used different tools to measure depression: IPSS (1), SDQ-9 (1), MDI (1), HS (1), SRQ (3), CID (1), CIDI (1), CISR (1), MINI (1), Goldberg scale (1), clinical (3), and interview schedule (1). Nine studies were conducted in primary health center (PHC), five studies were done in primary care clinics, two in general practice (GPs), and one in mobile health clinic.
Figure 1.

Review and meta-analysis flow diagram
Table 1.
Summary of studies included
| Author | Year | Community | Setting | Age group | Sample size | Sampling procedure | Tool | Prevalence depression % |
|---|---|---|---|---|---|---|---|---|
| Sen B et al. | 1978 | GPs | Calcutta | 28 | Consecutive | IPSS | 5 | |
| Wig NN et al. | 1980 | PHC | Calcutta | 340 | Patients attending psychiatric clinic | Clinical | 9.1 | |
| Kulhara P et al. | 1984 | PHC | Raipur Rani | All age group | 259 | Patients attending psychiatric clinic | Clinical | 12.7 |
| Kulhara P et al. | 1985 | PHC | Raipur Rani | All age group | 287 | Patients attending psychiatric clinic | Clinical | 8.4 |
| Sen B et al. | 1987 | Primary Care clinics | Calcutta | >15 Years | 202 | All patients >15 years of age | SDQ-9 | 44.5 |
| 1987 | Primary Care clinics | Calcutta | >15 Years | 202 | All patients >15 years of age | Manifest Depression Items | 42.6 | |
| 1987 | Primary Care clinics | Calcutta | >15 Years | 202 | All patients >15 years of age | Hamilton Scale | 23.3 | |
| Srinivasan TN et al. | 1990 | Primary care facility | Madras | Adult | 100 | Systematic random sampling | 11 item check list followed by Clinical examination | 44 |
| 1990 | Primary care facility | Madras | Adult | 200 | Systematic random sampling | SRQ | 37 | |
| Amin G et al. | 1998 | Curative and Preventive General Hospital | Vadodara | >18 Years | 200 | Systematic random sampling | CID | 21 |
| Gater R et al. | 1998 | Bangalore | 18-65 Years | 1366 | CIDI | 9 | ||
| Patel V et al. | 1998 | PHC | Goa | 16-65 Years | 303 | CISR | 19.5 | |
| Chisholm D et al. | 1997 | PHC | Bangalore | 16-60 Years | 120 | SRQ | 3.3 | |
| Nambi SK et al. | 2002 | Tamil Nadu | 16-65 Years | 101 | Consecutive | CISR | 17.8 | |
| Pothen M et al. | PHC | Vellore | >15 Years | 373 | Consecutive | CISR | 28.4 | |
| Patel V et al. | 2003 | PHC | Goa | Adult | 598 | CISR | 5.5 | |
| Tripathy A et al. | 2016 | PHC | Multi-centric | 551 | PHQ | 71.8 | ||
| Kishore J et al. | 1985 | PHC | Ballabhgarh | 18-60 Years | 218 | SRQ | 11.9 | |
| Murthy SK et al. | 1977-78 | GPs | Bangalore | 28 | Convenience | IPSS | 21.4 | |
| Salve H et al. | 2011 | Mobile Health clinic | Delhi | >18 Years | 350 | Systematic random sampling | MINI | 15.7 |
| Kamble SV et al. | 2003-05 | PHC | Maharashtra | >60 Years | 494 | Systematic random sampling | Goldberg Scale | 31.5 |
Table 2.
Summary of studies included for gender specific prevalence of depression
| Author | Depression prevalence total | Depression prevalence male | Depression prevalence female | OR (Female) | Upper C.I. | Lower C.I. |
|---|---|---|---|---|---|---|
| Sen B et al. | 44.5 | 27.08% | 50.00% | 2.69 | 5.48 | 1.32 |
| Sen B et al. | 42.6 | 29.17% | 72.08% | 6.27 | 12.82 | 3.07 |
| Sen B et al. | 23.3 | 10.42% | 42.21% | 6.28 | 16.73 | 2.36 |
| Gater R et al. | 9.0 | 4.83% | 13.32% | 3.03 | 4.58 | 2.00 |
| Tripathy A et al. | 71.8 | 67.42% | 75.96% | 1.53 | 2.22 | 1.05 |
| Kishore J et al. | 11.9 | 10.48% | 13.27% | 1.31 | 2.99 | 0.57 |
| Kamble SV et al. | 31.5 | 24.57% | 37.40% | 1.83 | 2.71 | 1.24 |
| Patel V et al. | 19.5 | 24.73% | 56.19% | 3.90 | 6.73 | 2.27 |
| Pothen M et al. | 28.4 | 25.00% | 30.23% | 1.30 | 2.18 | 0.77 |
| Salve H et al. | 15.7 | 18.52% | 15.20% | 0.79 | 1.68 | 0.37 |
Aggregate prevalence of depression
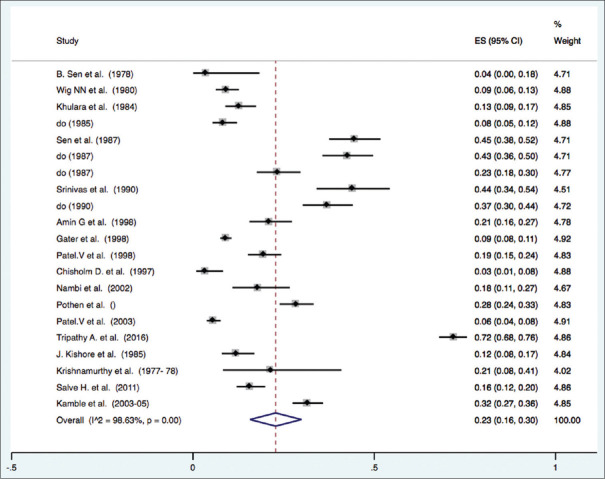
The aggregate point prevalence of depression of the 17 studies using the random-effect model was 23.0% (95% CI: 16.0-30.0%, Q value = 1462.67, d.f. =20, Tau square = 0.03) [Figure 2]. There was a significant and high level of heterogeneity between the studies (I-square 98.63%, P < 0.001).
Figure 2.
Forrest plot showing prevalence of depression
Publication bias
There was evidence of publication bias (intercept = 8.22, 95% CI: 1.08–15.35, t = 2.41, P = 0.026). Figure 3, is showing the funnel plot depicting all studies included in this review, which also shows evidence of publication bias.
Figure 3.

Funnel plot depicting all studies included in the review
Subgroup analysis
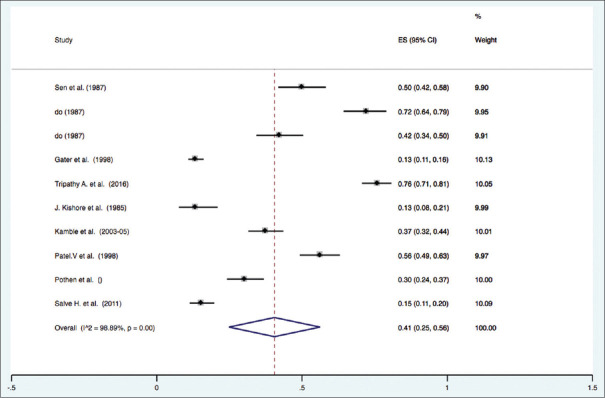
Gender distribution for depression: Subgroup analysis was performed by gender. Only studies were included which provided data on gender distribution in the study (eight studies). The prevalence of depression among females ranged from 13% to 72%. Pooled estimate of depression among females was 41% (C.I. 25% to 56%, I square = 98.89%, P < 0.001). The prevalence of depression among males ranged from 10% to 67%. Pooled estimate of depression in male gender was 24% (C.I. 10% to 38%, I square = 98.19, P < 0.001) [Figures 4 and 5].
Figure 4.
Depression prevalence among females
Figure 5.
Depression prevalence among males
Association of gender with depression: O.R. for female gender ranged between 0.79 and 6.28. Female gender was found to be a risk factor for the depression (pooled O.R. 2.27, C.I. 1.59 to 3.25). Heterogeneity among the studies was moderate (I square 75.4%, P < 0.001). Figure 6 is showing the Forrest plot for the Odds ratio for depression presence among females in comparison to males.
Figure 6.
Forrest plot showing the odds ratio for female gender versus male gender (depression)
Discussion
This meta-analysis provided an up-to-date estimate of the prevalence of depression among adults at the primary care level combining all the evidences available from the published literature in India. We observed that almost one fourth of the patients attending primary care were suffering from depression. Our findings suggest that depression is a common and substantial mental health problem at the primary care level in India. A wide range of populations was examined and contributed to the significant heterogeneity in prevalence across studies. According to the WHO, an important barrier to effective care for depression is covert feature of the disease and inaccurate assessment.[14,15]
World Mental Health (WMH) survey initiative reported comparatively higher prevalence of depression (DSM-IV/CIDI) in low- and middle-income countries than in high-income countries (lifetime prevalence of depression in low- to middle-income countries as 18.4 (Brazil), 14.6 (Ukraine) 13.3 (Colombia), 10.9 (Lebanon), 9.8 (South Africa), 6.5 (China), and 9.0 (India)).[16]
A meta-analysis from Brazil among adults reported the lifetime prevalence of major depressive disorder as 17% (95% CI 14-19; I2 = 91.6%).[17]
Female gender was found to be associated with depression in our analysis. Our findings support earlier findings that the prevalence of depression is higher among women[18,19] and there is still a gender effect on the prevalence of depression.[20,21] The prevalence of depression between women and men was reported to be in the ratio of 2:1.[22] WMH survey initiative also reported higher odds of depression among female gender compared to males, and the difference was more prominent in low- and middle-income countries compared to high-income countries (OR ranged from 1.2 in China, 1.9 in India and Colombia, 2.1 in Lebanon and Mexico, 2.2 in South Africa, 2.5 in Ukraine, and 2.6 in Brazil).[16] Silva MT et al. reported higher prevalence of depression among female than males among Brazilian adults.[17]
The strength of this current study includes a comprehensive systematic review and methodological synthesis of data from Indian studies and subgroup analysis. The findings are most applicable to family physicians and public health policy makers in formulating strategies to lessen the burden of depression in the community. Other strengths are the utilization of random-effects models to establish robust aggregate prevalence.
This study has following limitations. First, this meta-analysis has a high level of heterogeneity. Also, there is a presence of publication bias.
Conclusion
The study provides evidence for higher and gender differential burden of depression among primary care attenders in India. Integration of mental health services with existing primary care services is the way forward to address the issue. Capacity building of the primary care physician in identification and management of depression is an essential intervention in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Institute of Health Metrics and Evaluation GBD compare data visualisation. Available from: https://vizhub.healthdata.org/gbd-compare/
- 2.Chokshi M, Patil B, Khanna R, Neogi SB, Sharma J, Paul VK, et al. Health systems in India. J Perinatol. 2016;36:S9–12. doi: 10.1038/jp.2016.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017:A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Mental Health Action Plan 2013-2020. Geneva: World Health Organization; 2013. Available from: http://www.emro.who.int/mnh/mental-health-action-plan/index.html . [Google Scholar]
- 5.Depression and Other Common Mental Disorders:Global Health Estimates. Geneva: World Health Organization; 2017. Licence:CC BY-NC-SA 3.0 IGO. Available from: https://www.who.int/publications-detail-redirect/depression-global-health-estimates . [Google Scholar]
- 6.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators, and others. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015:A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rihmer Z, Angst J. Mood disorders:Epidemiology. In: Sadock BJ, Sadock VA, editors. Comprehensive Textbook of Psychiatry. 8th ed. Baltimore: Lippincott Williams and Wilkins; 2004. Available from: https://www.wolterskluwer.com/en/solutions/ovid/kaplan--sadocks-comprehensive-textbook-of-psychiatry-761 . [Google Scholar]
- 8.Gururaj G, Varghese M, Benegal V, Rao GN, Pathak K, Singh LK, et al. National Mental Health Survey of India, 2015-16:Summary. Vol. 128. Bengaluru: National Institute of Mental Health and Neuro Sciences, NIMHANS Publication; 2016. [Google Scholar]
- 9.World Health Organization (WHO) Gender and Women's Mental Health. 1997. [[Last accessed on 2006 June 09]]. Available from: http://www.who.int .
- 10.Nandi DN, Ajmany S, Ganguli H, Banerjee G, Boral GC, Ghosh A, et al. Psychiatric disorders in a rural community in West Bengal:An epidemiological study. Indian Journal of Psychiatry [Internet] 1975 Jun;17(2):87–99. Available from: https://journals.lww.com/indianjpsychiatry/Citation/1975/17020/PSYCHIATRIC_DISORDERS_IN_A_RURAL_COMMUNITY_IN_WEST.4.aspx . [Google Scholar]
- 11.Kapoor R, Singh G. An epidemiological study of prevalence of depressive illness in rural Punjab. Indian J Psychiatry. 1983;25:110–4. [PMC free article] [PubMed] [Google Scholar]
- 12.Kulesza M, Raguram R, Rao D. Perceived mental health related stigma, gender, and depressive symptom severity in a psychiatric facility in South India. Asian J Psychiatr. 2014;9:73–7. doi: 10.1016/j.ajp.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Tawar S, Bhatia SS, Ilankumaran M. Mental health, are we at risk? Indian J Community Med. 2014;39:43–6. doi: 10.4103/0970-0218.126359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kramer T, Als L, Garralda ME. Challenges to primary care in diagnosing and managing depression in children and young people. BMJ. 2015;350:h2512. doi: 10.1136/bmj.h2512. doi:10.1136/bmj.h2512. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. (2001). The World health report :2001 :Mental health :new understanding, new hope. World Health Organization. Available from: https://iris.who.int/handle/10665/42390 .
- 16.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva MT, Galvao TF, Martins SS, Pereira MG. Prevalence of depression morbidity among Brazilian adults:A systematic review and meta-analysis. Braz J Psychiatry. 2014;36:262–70. doi: 10.1590/1516-4446-2013-1294. [DOI] [PubMed] [Google Scholar]
- 18.Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med. 2010;71:305–13. doi: 10.1016/j.socscimed.2010.03.035. doi:10.1016/j.socscimed. 2010.03.035. [DOI] [PubMed] [Google Scholar]
- 19.Goodwin RD, Gotlib IH. Gender differences in depression:The role of personality factors. Psychiatry Res. 2004;126:135–42. doi: 10.1016/j.psychres.2003.12.024. doi:10.1016/j.psychres. 2003.12.024. [DOI] [PubMed] [Google Scholar]
- 20.Cheng HG, Shidhaye R, Charlson F, Deng F, Lyngdoh T, Chen S, et al. Social correlates of mental, neurological, and substance use disorders in China and India:A review. Lancet Psychiatry. 2016;3:882–99. doi: 10.1016/S2215-0366(16)30166-3. doi:10.1016/S2215-0366 (16) 30166-3. [DOI] [PubMed] [Google Scholar]
- 21.Kim HJ, Park E, Storr CL, Tran K, Juon HS. Depression among Asian-American adults in the community:Systematic review and meta-analysis. PLoS One. 2015;10:e0127760. doi: 10.1371/journal.pone.0127760. doi:10.1371/journal.pone. 0127760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Puri B, Hall A, Ho R. 3rd ed. Boca Raton: CRC Press; 2013. Revision Notes in Psychiatry; p. 846. Available from: https://www.taylorfrancis.com/books/mono/10.1201/b13188/revision-notes-psychiatry-basant-puri-annie-hall-roger-ho . [Google Scholar]