Abstract
Peer support specialists (i.e., lay interventionists representing one of the fastest-growing mental health workforce) are increasingly using technologies to support individuals with mental health challenges between clinical encounters. The use of technology by peers has been significantly increased During COVID-19. Despite the wide array of technologies available, there is no framework designed specifically for peer support specialists and service users to select technologies to support their personal recovery. The objective of the study was to develop a Decision-Support Tool for Peer Support Specialists and Service Users to facilitate shared decision-making when choosing technologies to support personal recovery. The study used an iterative co-production process, including item formulation and a series of group cognitive interviews with peer support specialists and service users (n=9; n=9, n=4). The total sample included 22 participants: peer support specialists (n=18, 81.8%) and service users (n=4, 18.2%). The final version of the Decision-Support Tool for Peer Support Specialists and Service Users (D-SPSS), includes 8 domains: (1) privacy and security; (2) cost; (3) usability; (4) accessibility; (5) inclusion and equity; (6) recovery principles; (7) personalized for service users’ needs; and (8) device set-up. Our study found that involving peer support specialists and service users in the design and co-production phase of a decisionsupport tool is feasible and has the potential to empower both peer support specialists and service users, and potentially increase engagement in the use of technologies that support individuals’ recovery from traditional clinical encounters.
Keywords: Peer support specialist, mental health, recovery, decision-support tools, shared decision making
Introduction
Peer support specialists are interventionists with a lived experience of a mental health and/or substance use challenges that are trained and accredited by their respective state to offer Medicaid reimbursable support services.1,2, 4 Commonly, peer support specialists provide support (i.e., social, instrumental, and emotional support) to individuals with mental health conditions (i.e., service users) via self-help groups, internet support groups, peer-delivered services, peer-run, or peer-operated services.1,2, 4 Empirical evidence indicates peer support services can promote hope, empowerment, self-determination, and wellness/recovery among service users of the mental health and substance use system.3 Since the expansion of the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act to include Medicaid billable telehealth services,5,6 peer support specialists have incorporated various technologies into their practice to reach individuals in their home environments, including virtual reality, video games, video conferencing, and smartphone applications. As such, Fortuna and Collins-Pisano (under review) reports that service users have also increased their usage of various technologies.
Despite increased access and use of technologies by peer support specialists and service users due to social distancing and the COVID-19 pandemic,5,7 the rapid switch to tele-mental health has raised concerns about the privacy and security, efficacy, and clinical utility of technologies implemented among end-users (Venegas & Fortuna, under review). Research suggests that mental health technologies tend to be largely unregulated 5, 8, 9 and few digital mental health interventions have received Food and Drug Administration approval for prescription of these technologies as digital therapeutics. According to Fortuna and Collins-Pisano (under review), the sheer number of unregulated mental health technologies already used by service users to support their recovery, coupled with the cognitively complex process of navigating between thousands of technologies, poses unique challenges for populations with mental health and substance use challenges who commonly experience functional and cognitive limitations.10 Thus, both peer support specialists and service users may benefit from resources that can aid peer support specialists and the individuals they serve in choosing appropriate technologies to meet their personalized needs.
To date, few decision-support frameworks exist. For example, the American Psychiatric Association (APA) initiated a framework to select smartphone apps for use in clinical settings. The APA’s framework provides clinicians with information about what smartphone apps to recommend for service users based on the best available information.11,12 The National Institute on Mental Health has also formulated suggestions to evaluate smartphone apps. Yet, many suggestions include asking a professional, reviewing research supporting the app, and/or reaching out to apps developer.13 All of which may be feasible for service users and peer support specialists, yet may require extensive functional or cognitive resources and may potentially lead to an overreliance on clinicians’ recommendations. Further, both frameworks focus on smartphone apps, yet many other technologies are available for mental health and/or substance use, including virtual reality,14 video games,15 social media (i.e., Facebook).16
As such, the development of a framework to support the selection of various types of technologies to support mental health and substance use recovery may have greater ecological validity than unidimensional technological frameworks. Further, a resource that places decision-making authority among the actual end-user (not a clinician) may facilitate service users’ personal empowerment, recovery, and even assist with engagement in digital technologies.17
Shared decision making (SDM) is a health communication approach emphasizing choice, autonomy, and engagement in decision-making of service users with clinicians and other providers such as peer support specialists.19 Decision aids and decision support tools facilitate SDM and collaboration, and involved sharing information, professional and lived experience, and expertise.20 Current SDM interventions in mental health focus on treatment and medication choice,17,18 psychiatric rehabilitation decisions,21 or care transition.21–23 SDM within mental health has found to promote engagement in services and treatment adherence.24
As service users commonly disengage in therapeutic digital technologies after two weeks or before intervention effects take place,25 the incorporation of SDM strategies within selecting technologies to support individuals’ recovery may counteract premature disengagement and guide individuals in selecting technologies based on available evidence, preferences, and their unique needs and socioenvironmental characteristics. The purpose of this study was to develop a decision-support tool for peer support specialists and service users designed to guide dyads in selecting technologies to support their personal recovery.
Methods
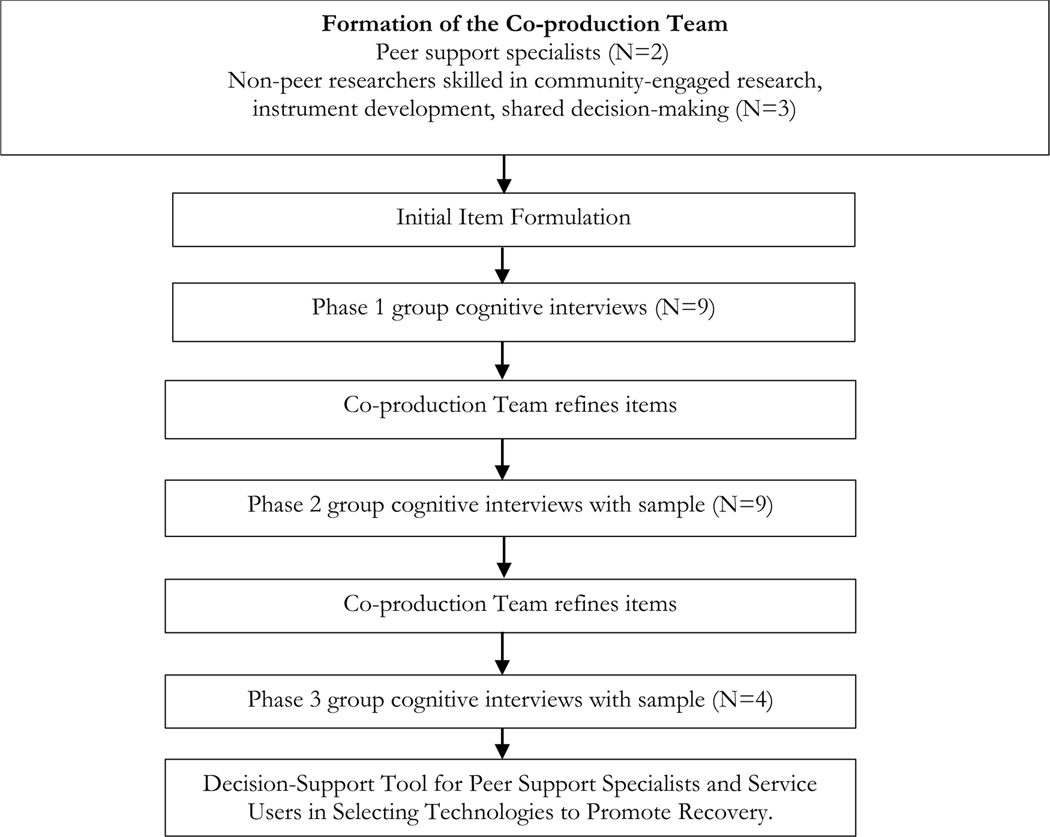
The qualitative study used a formative research approach to develop a Decision-Support Tool for Peer Support Specialists and Service Users (D-SPSS). A formative research incorporates service users in the research process which has been shown to improve trust and encourage partnerships between service users and academic researchers.26 The development of the Decision-Support Tool for Peer Support Specialists and Service Users (D-SPSS) included an iterative co-production process based on The International Patient Decision Aid Standards (IPDAS)27 and the Academic-Peer Partnership Model for Community Engagement.28, 29 This study included item formulation and a series of group cognitive interviews. The Committee for the Protection of Human Subjects at the [blinded for review] Institutional Review Board approved the project.
Item Formulation
Authors initially developed the first version of the decision-support items, which were based on digital peer support competencies that have been documented in Collins-Pisano and Fortuna (under review) and barriers and facilitators to using technologies as identified by service users and peer support specialists.30 The initial decision-support tool included the following domains: security/privacy, costs, usability, accessibility, and recovery.
Cognitive Interviews
Cognitive interviewing normally requires three rounds of 10–30 participants for large studies and 4 – 6 participants for small-scale projects.31 The authors conducted three phases of cognitive interviews, and we reached saturation after the third round of cognitive interviews. The initial items were assessed in phase one with (N=9) peer support specialists and service users. Refined items were assessed in phase two, with different peer support specialists and service users (N=9). In phase three, a final set of items was assessed with another group (N=4) of peer support specialists and service users to assess acceptability, ease of use, and items’ relevance. See Figure 1 for co-production process. All three rounds of interviews covered every critical question, and the participants received the same instructions. All members of the research team where trained in qualitative research which helped minimize bias and interpretation errors.
Figure 1.
Iterative Co-Production Process
Recruitment
The co-production team recruited peer support specialists (N= 22) via email listservs specifically for peer support specialists and peer support specialist Facebook groups to pilot the decision support tool, Table 1. Inclusion criteria included: (1) individuals were at least 18 years old; (2) individuals self-report as peer support specialists or service users; and (3) individuals were able to provide consent. Individuals who expressed interest were emailed a Zoom registration for the virtual group cognitive interview. Inability to complete the registration independently resulted in exclusion from the study. All end-users were emailed the draft items 48 hours before the group discussions and were instructed to read through the draft items before attending the one-hour group meetings. The group cognitive interviews were conducted on HIPAA compliant Zoom/video software, guided by the 1st, 3rd, and 5th author. There was no compensation for participating.
Table 1.
Demographic Characteristics of Group Cognitive Interview Stakeholders
| Stakeholder Participants (N=22) | % | |
|---|---|---|
|
| ||
| Age | ||
| 18–30 | 1 | 4.5 |
| 31–50 | 10 | 45.4 |
| 50≤ | 9 | 40.9 |
| No Report | 2 | 9.1 |
| Gender | ||
| Male | 8 | 36.3 |
| Female | 12 | 54.6 |
| Non-binary | 1 | 4.5 |
| Queer | 1 | 4.5 |
| Ethnicity | ||
| White | 17 | 77.3 |
| Black African American | 2 | 9.1 |
| Biracial * 1=White/Asian, 1=White Hispanic and 1=White Native American | 3 | 13.6 |
| Level of Education | ||
| Some college | 7 | 31.8 |
| Completed college/technical school | 5 | 22.7 |
| Completed an associate degree | 1 | 4.5 |
| Bachelor’s degree | 4 | 18.2 |
| Some graduate school | 1 | 4.5 |
| Master’s degree or higher | 4 | 18.2 |
| Employment status | ||
| Full-time | 16 | 72.7 |
| Part-time | 3 | 13.6 |
| Volunteer | 1 | 4.5 |
| Unemployed | 1 | 4.5 |
| Retired | 1 | 4.5 |
| Self-Reported Primary Mental Health or Substance Use Diagnosis | ||
| Bipolar Disorder | 3 | 13.6 |
| Major Depressive Disorder | 6 | 27.3 |
| Post-Traumatic Stress Disorder | 5 | 22.7 |
| Substance use | 6 | 27.3 |
| None of the above | 1 | 4.5 |
| No report | 1 | 4.5 |
Data collection and analysis
Three hour-long focus groups were conducted via video conferencing software. The 1st, 3rd, and 5th authors employed cognitive interviewing, which is an evidence-based method designed to investigate whether an item accomplishes its planned purpose.31 Researchers conducted three group cognitive interviews using HIPAA compliant video conferencing platform (i.e., Zoom for Healthcare). Participants could read the document using the share screen on zoom or could open the document via a zoom link in the chat. The researcher read the content word for word slowly and responded to any clarifying questions.
In the first group cognitive interview, researchers reviewed each domain with the participants, took note of the participant’s comments and questions, and incorporated them into a new iteration of the tool for the second group cognitive interview. Recorded data was transferred into a spreadsheet, and the themes were coded based on the domains. Participant comments, concerns, misunderstandings, and misinterpretations about each item were identified through thematic analysis 31 and compared. When no further new comments were received in the first interview phase, items were revised before the second set of interviews. The same data analysis process was repeated after the second group cognitive interview, with feedback iterated into a tool that was presented to the third group cognitive interview. The analysis from the third group led to the finalized decision tool. The goal of the thematic analysis was to have feedback from each group cognitive interview build on the tool presented to the next group cognitive interview. Supplemental materials delineate the revisions to the decision-support tool from group cognitive interview one through three based on stakeholders’ feedback.
Researchers employed verbal probing to elicit information to tailor the instrument to the specific needs and values of the target population. Verbal probing is an active form of data collection, in which interviewers administer a series of questions.32 Verbal probing interview guide was developed a priori with the co-production team. Sample verbal probing questions included the following: “what is your overall impression of the decision support tool?”; “how would this decision support tool help you offer digital peer support?”; “is there anything you can add, delete, or change about the information in the rows?”; “are there other questions that you feel would be important to include?”; and “how would this decision support tool bests be included in peer support specialists’ workflow?”
Results
The first author, third author, and last author conducted three group cognitive interviews with a total of peer support specialists (N=18, 82%) and service users (N=4, 18%); group cognitive interview one (N=9, 41%), group cognitive interview two (N=9, 41%), and group cognitive interview three (N=4, 18%).
Domain and Themes
Three group cognitive interviews were conducted with 22 participants. As such, the decision support tool went through three iterations with feedback collected from one group cognitive interview analyzed and incorporated into the next group cognitive interview. Table 2 (See Appendix) shows how the participant feedback from each group cognitive interview changed the tool over time. The final tool includes eight domains in the following order (note, order of domains was determined by stakeholders): (1) Principles of recovery (2) privacy and security; (3) cost; (4) usability; (5) accessibility; (6) Inclusion and equity; (7) personalized for service users’ needs; and (8) device set-up. Several themes emerged under each domain that led to the final checklist of the D-SPSS tool.
Privacy and Security
In discussing the domain of privacy and security, participants were concerned about whether personal information would be protected. Suggested changes to domain 1 included clarifications to the consenting process, such that users are aware if privacy policies are time-limited or expire. Feedback also included specifying that data would not be used to incriminate service users and clarifications to mandated reporting. Specifically, what data would need to be reported (e.g., danger to self or others) and who it is shared with (e.g., emergency services, treatment team). Participants made the following comments: “Is there a way in the privacy that can help the service user feel that what they share will not be used to incriminate them somehow? Like I know I would be hesitant to open up about certain things if I know my data is going to be shared and if it is shared, I could have repercussions from it.” For the concerns related to mandated reporting, participants made the following comment: “actually I had a question about how … mandated reporting fit into this. There’s usually a conversation between… mental health service providers and service users about conversations about suicidal ideations, self-harm, and hurting others. How would that be conveyed in this platform, like if you’re texting something like I want to kill myself in a week and have these plans? How is that information going to be passed on to maybe emergency services or other information that people should definitely have a discussion about?” Participants suggested that users be made aware of any of the app’s data shared with members of the treatment team or documented and should have specific limits to staff confidentiality and clear policies surrounding a course of action when a user is in emergent crisis.
Cost
Suggested changes to the domain cost; included clarifying if technologies are free for a time-limited trial period and incorporating an item related to competency in knowing if a technology uses cellular data (even if connected to Wi-Fi). Participants emphasized the importance of including possible risks to how data is used and potential harm to the device (e.g., software malfunction; cost of storage). Participants also suggested incorporating organization-wide considerations, specifically related to disclosing the organization/agency’s approval to use a specific technology and their responsibility to provide devices and equipment (e.g., headphones) to service users. Due to the cost of internet service and Wi-Fi, participants suggested that having an app or technology accessible offline would benefit service users who may not afford internet services. A participant made the following comment: “If it would be able to be used offline, many of our service users may not have access to the Internet, and a lot of them do not have or may not afford minutes and data on their phones, and they may be in a location where they do not get Wi-Fi.”
Usability
Discussions about usability centralized around accessibility (across locations, populations, and literacy levels) and engagement. Participants suggested incorporating the following items: copy-and-paste or hyperlink features to identify if a technology can be used offline, works as it’s supposed to, and is compatible with specific features (i.e., video conferencing, creating avatars). Participants emphasized the importance of knowing how to navigate technology, liking the technology’s appearance, and feeling excited and empowered when using the technology. Participants also highlighted the benefits of remote set-up/information technology [IT] assistance (either from a peer support specialist or a help/IT desk), especially for older adults, users with limited literacy, and individuals currently incarcerated. A participant made the following comments: “Many [of] our service users, if they have the literacy issues they also do not feel confident with the technology, or you know they some of the older service users are not as comfortable with technology.” Another participant commented, “ I had the same experience. I agree with that kind of and the one thing I did learn was some of my facilitators are from the older generation like I am, and they were getting very frustrated and frazzled because they couldn’t find the buttons and it took one visit to them to show them which buttons work and how to use it and now they’re flying through it. You have to make that extra effort to just spend one day with them to do it and then they love it, but you’re still going to be a little bit of hands-on to teach the older people how to do it, but I agree with [NAME]; once they learn they’re in heaven and now some of them are learning those avatars in their place, so the avatar has a cartoon expression, but it mimics everything you do.”
Accessibility
For user accessibility items, participants suggested adding closed captioning, voice-to-text, and read-aloud features to make them more accessible for users with specific disabilities. A participant commented: “You know how they have features that when you talk, you can either type a text message, or you could voice it, I think that would be helpful for a lot of mine [service users].” Additional feedback included translating the instructions for using the decision-support tool into a video and audio format. Participants suggested that apps and technology have face-to-face interaction and closed-captioning features such as voice to text and read-aloud features.
Inclusion and Equity
Participants indicated that the app should be inclusive to all users, including providing access across multiple languages and dialects. Participants commented, “Is this technology for all types of disabilities?….. does it allow me [the] ability to speak in my preferred language and dialect? Okay, so let’s say that someone speaks…French and Spanish, this person has the option to do that….You know there are a lot of people that don’t speak English, or they speak like a little bit of English.” In addition, participants suggested adding “religious beliefs” to the list of topics for technologies inclusive of all religions. According to participants, to be inclusive, apps should be accessible in various places like prisons and to all populations, including older adults, regardless of technology literacy. Participants emphasized that it was important for the app to provide enjoyment, have a nice appearance, and engage the users in their recovery.
Recovery Principles
Suggestions for the recovery principles domain included integration with other helpful apps/technologies to promote wellbeing (e.g., paying bills, finding housing, childcare, etc.), incorporating entertainment to promote engagement, reducing boredom, and encouraging that technologies and resources are evidence-based. Feedback also included incorporating measures to minimize exposure to possibly triggering or activating content (e.g., having language filters for substance use or suicide-related content and media) and providing readily available helpful resources to promote emotional safety in case of such exposure. Participants in the third group cognitive interview suggested moving the recovery principles domain to be the first to represent the overall importance of recovery and empowerment as the most important element of the tool. A participant noted, “I almost feel like this (Recovery) should be at the beginning…. because before you go into the technology and decide what you want to do, you need to think about ‘is it going to be good for me?’, ‘is it going to activate me?’ I almost feel like it should be at the very beginning.” Based on participants’ suggestions, the final version of the decision-support tool moved recovery to the top of the list of domains, as shown in Table 3 (See Appendix).
Personalized for service users’ needs
Participants shared how a decision-support tool may improve accessibility in their programs. A participant commented, “This kind of research would be really helpful to programs like ours just to be able to get as much access and communication out to our service users.” Participants discussed that the tool could potentially allow them, as peer support specialists, to offer their support to the service users they work with by giving them a resource that helps them focus on their recovery all in one area. Participants shared that an accessible app would allow people to connect to a broader recovery community faster for things like hope, choice, empowerment, positivity, social connections, and resilience. A participant made the following comment; “Let people know that it can help them connect with people, with others for right now when it’s not as safe, or as easy to do so during Covid-19 or during times where it’s just not accessible for them, like they’re feeling too sick to get on the bus and go to a meeting or don’t feel like calling a warm-line because they’re so anxious and if they could just text or type to someone, sometimes they would feel less anxious that way. I know from personal experience, so just letting people know how it can enhance the treatments that they’re familiar with.”
Device Set-Up
The need to remotely help with setting up technology devices and apps on behalf of service users was predominant across all group cognitive interviews. A participant noted, “If there was a way that from our access we could control user accounts in a sense like we could help them set up their accounts if need be because [NAME] has had multiple service users ask her to help her get into things and other than her being able to physically be with them, it would be helpful, if there is a way we could set up a person’s account and just send them the minimal information for them to access it in writing.” Another participant commented, “a lot of our service users like you said. If they have the literacy issues, they also don’t feel confident with the technology…Or you know some of the older service users aren’t as comfortable with technology. There’s just a wide range of that being an issue.”
The final version of the tool has eight domains in the following order: (1) Principles of recovery (2) privacy and security; (3) cost; (4) usability; (5) accessibility; (6) Inclusion and equity; (7) personalized for service users’ needs; and (8) device set-up. The order of domains was changed to move recovery to the top of the domain list as suggested by stakeholder participants because they believed recovery and empowerment were essential for any tool designed for people with mental health and/or substance challenges. The domain helpfulness was combined with usability after thematic analysis from all group cognitive interviews showed similar feedback in the usability domain. Table 3 (See Appendix) shows the final version of the “Decision Support Tool for Peer Support Specialists and Service Users (D-SPSS).”
Discussion
The purpose of this study was to develop the first decision-support tool for peer support specialists and service users to select technologies to promote recovery and wellness for people with mental health and substance use challenges. The Decision Support Tool for Peer Support Specialists and Service Users (D-SPSS) includes eight domains, in the following order: (1) Principles of recovery (2) privacy and security; (3) cost; (4) usability; (5) accessibility; (6) Inclusion and equity; (7) personalized for service users’ needs; and (8) device set-up.
The D-SPSS offers, for the first time, a tool to choose between technologies and that aimed for peers and service users. With over unregulated 88,000 mental health smartphone apps on the market in 2020,9, 33 and with the increasing number of service users using technology to support their recovery (Fortuna & Collins-Pisano, under review), the D-SPSS is a timely solution for navigating between multiple technologies.
The actual use of the D-SPSS may also have important clinical implications for peer support specialists and service users. The decision-making tool, as a tool under the SDM approach, has the potential not only to empower both peer support specialists and service users, but also to increase engagement and better health outcomes. D-SPSS is designed to promote self-determination (i.e., freedom of choice). Choice is an essential component of recovery as it allows the person autonomy and personal empowerment in their own recovery process. Many people in recovery often lose the ability to make choices related to their recovery, commonly due to stigma, discrimination, and stereotypes surrounding coercion, especially for people in recovery from substance use.34 Yet, self-determination in mental health and/or substance use care is associated with increased self-confidence, motivation and engagement in recovery.35 As service users and peer support specialists have reported not being involved in the decision-making regarding technology selection for clinical care (Collins-Pisano & Fortuna, under review), utilizing D-SPSS may have a clinical impact on increased involvement in mental health services.37 Future research may consider exploring the clinical utility of this tool on recovery outcomes (e.g., hope, empowerment) and clinical outcomes (e.g., engagement in services).
While the decision-support tool may facilitate selecting technologies that are accessible to people with mental health challenges and with co-morbid health conditions, further research in this area is needed. Of concern, federal agencies have mandated accessibility requirements through section 508 of the Rehabilitation Act of 1973, whereas non-federal agencies do not. Section 508 of the Rehabilitation Act of 1973, as amended (29 U.S.C. 794d), requires all federal departments and agencies to ensure that their electronic and information technology (EIT) is accessible to people with disabilities.27 This requirement is not mandatory for non-federal agencies, yet 61 million people in the United States have some type of disability.38 Of people with mental health challenges, 33.7% also experience cognitive and functional challenges (e.g., mobility).39 To be inclusive, and considering the potential impact of accessibility on engagement, commercial industry laws may be needed to require technologies for mental health and/or substance use care be accessible to people with disabilities. A potential solution gaining momentum is involving service users, persons with disabilities and peer support specialists in the software development lifecycle to ensure technologies developed will meet the accessibility needs of both peer support specialists and service users. Additional feedback included translating the instructions for using the decision-support tool into a video and audio format to meet the accessibility needs of individuals. Participants also suggested technology incorporate face-to-face interaction and closed-captioning features such as voice to text and read-aloud features.
Limitations
This study is not without limitations. First, while verbal probes are efficient and provide data that is easier to analyze than think-aloud 31 streams, verbal probes may create bias in the subjects’ responses as it may lead participants to provide more carefully thought-out answers than they would typically give in other modes.31 Second, bias may also be present due to sample size in instrument development.31 Through an iterative design process commonly accepted, we aimed to reduce bias through a series of interviews with different sample participants. The total sample is consistent with commonly accepted instrument development procedures.31 Third, variation may exist based on participants’ demographics. Exploring the utilization of the Decision Support Tool for Peer Support Specialists and Service Users with heterogeneous samples may demonstrate variations in utility and outcomes by characteristics (e.g., psychiatric diagnosis, age).
Conclusion
The development of a D-SPSS, decision-support tool for peer support specialists and service users, for selecting mental health apps and technology is timely, especially as a result of the Covid-19 era and health and mental health implications. Involving peer support specialists and service users in the co-production phase and pilot testing ensured that the framework incorporated the previous experiences of peer support specialists and service users to develop and refine digital peer support competencies. While most app and technology developers have only involved peer support specialists or services during the implementation stage of app roll-out or testing of technology, which may impact the opportunity for informed decision-making and leads to apps and digital technology being created that are not user-friendly and consider challenges faced by individuals with a lived experience. The current study is the first to involve peer support specialists and service users in the development and co-production of a tool to aid in selecting mental health apps and technology. To our knowledge, it is the first study to develop an app selection framework that aligns with the recovery model. As the use of technology in combination with peer support specialists in healthcare continues to expand, this decision-support tool may be essential to agencies.
Appendix
Table 2.
Decision-Support Tool for Peer Support Specialists and Service Users in Selecting Technologies to Promote Recover, Final Version 4
| Instructions: Peers should offer their lived experience of using these technologies | |
|---|---|
|
| |
| Domains | Checklist |
|
Principles of Recovery (or wellness) Does this technology embrace the general principles of recovery? |
❏This technology:
Recovery Principles ❏ Gives me hope ❏ Encourages me to choose the life I want to live ❏ Makes me feel empowered ❏ Promotes embracing health challenges ❏ Promotes body positivity ❏ Promotes social connection ❏ Promotes building resiliency This technology: Recovery Language ❏ Uses pro-recovery language ❏ Uses person-centered language ❏ Uses every day, non-clinical language ❏ Uses strengths-based language ❏ Demonstrates strong mental health literacy Emotional Safety ❏ The language used in this technology has a low risk of activating or triggering me ❏ If content in this technology does trigger or activate me, there are links to helpful resources or contacts to support me ❏ I am aware of the potential risks I may be exposed to when using this technology (referencing specific drugs, suicide, settings) This technology: Recovery Resources ❏ Contains helpful resources to learn about wellness ❏ Has activities that I am interested in to practice wellness ❏ Has Warm Line phone numbers built-in ❏ Links with other applications/technology that promote wellness (e.g., housing, finances, childcare, meetings) |
|
Privacy and Security Does this technology protect my personal information? |
Privacy Policy ❏ There is a clear privacy policy for me to read ❏ There is a clear privacy policy for me to consent to ❏ I am aware if this consent is time-limited ❏ I understand the privacy policy Data and Security ❏ I know how data is shared ❏ If my data is shared, I know it is shared securely ❏ If my data is shared, I know who it is shared with ❏ If my data is shared with others, I am aware of the limits to what they can keep confidential (e.g., if they are mandated reporters) ❏ If I am a guest/member/person supported at an agency, I am aware if my data (engagement, theme of discussion, etc.) will be documented ❏ If I am a guest/member/person supported at an agency, I am aware if my data (engagement, theme of discussion, etc.) will be shared with members of my treatment team ❏ I am aware if I can opt-out of data collection ❏ I am aware of how I can opt-out of data collection ❏ I am aware that this technology will not be used to incriminate me ❏ This technology protects the personal boundaries of all parties involved (including service users, peer support specialists, etc.) |
|
Cost Are there any monetary costs (or payments) involved in using this technology? If yes, who is paying? |
Monetary Costs ❏ This technology has no hidden costs ❏ I am aware if it is completely free ❏ I am aware if it is free but only for a certain number of days (e.g. if it is a trial period) ❏ I am aware of up-front monetary costs (if a one-time payment) ❏ I am aware of weekly, monthly, or yearly costs (if a subscription) ❏ I can afford using this technology ❏ I am aware if costs are covered by my health insurance provider ❏ I am aware if the agency/organization I work at or receive services from will cover any costs associated with using this technology (e.g., cost to purchase technology, cost to provide additional equipment such as headphones and chargers, etc) ❏ I am aware if costs are covered by an organization or program (such as through research or scholarships) ❏ I can use this technology offline (e.g., without Wi-Fi or cellular service) ❏ I am aware of how much of my monthly data plan is used by this technology ❏ I know how to double-check if this technology uses data (minutes), even if my device is connected to Wi-Fi. Costs to the Device ❏ If using the technology requires me to download an application or software, I am aware of the risks it poses to my hardware (e.g., phone, tablet, computer, etc.) ❏ I am aware of how much storage is taken up on my device if using this technology. ❏ I am aware of the extent to which using this technology will drain my battery. |
|
Usability Do I want to use this technology? Is this technology helpful? |
Engagement ❏ I want to use this technology ❏ I like the appearance of this technology ❏ I understand the terminology used ❏ I can easily use this technology (I feel comfortable) ❏ As a user, I feel confident that I can navigate the different features of the technology ❏ The content is relevant to me ❏ The content excites me ❏ The content keeps me engaged ❏ This technology promotes self-determination ❏ There are platforms for people to train and support me in using this technology ❏ I can customize this technology to make me feel comfortable and engaged (e.g., via creating avatars) This technology: Helpfulness ❏ Has evidence (e.g., scientific, clinical, reviews, blogs, etc.) of being effective ❏ Has been helpful for others with similar lived experiences (e.g., peers) ❏ Could be helpful for my wellness ❏ Could be helpful for my recovery Set-up and devices This technology: ❏ Is compatible with my device(s) (Works on my device (i.e., Android, iPhone, Windows vs. Apple, etc.) ❏ Works like it is supposed to (e.g., can open hyperlinks, copy and paste, etc.) ❏ Allows another person to help me set up an account remotely (e.g., peer support specialist, IT desk, customer service) |
|
Accessibility Am I able to use this technology? |
❏ I can access this technology from my device and or my location Sensory Accommodations ❏ This technology can accommodate all types of disabilities ❏ Visual - I can customize the display (e.g. lighting, text size, color scheme) ❏ Hearing - I can customize the sound (e.g. volume, alert) ❏ Touch - I can interact with this technology through touch (e.g. this includes vibrations, scrolling, etc.) This technology has: Additional Features ❏ A read-aloud feature ❏ A talk-to-text feature ❏ A “scribble” (or draw) to text feature ❏ This technology is formatted in my preferred language ❏ I can customize the technology to speak or scribe in my preferred and dialect |
|
Inclusion and Equity Is this technology inclusive and equitable? |
This technology is: ❏ Inclusive of different races ❏ Inclusive of different ethnicities ❏ Inclusive of different gender identities and sexual orientations (e.g., LGBTQIA+ friendly) ❏ Inclusive of different religious and spiritual beliefs ❏ Accessible to service users, regardless of socio-economic status ❏ Accessible to service users, regardless of location (urban, rural, etc.) ❏ Uses language and terms that make me feel comfortable, language and terms that are attuned to my culture and identity, etc.? |
|
Personalized for needs Can this technology be personalized for my needs to promote wellness? |
This technology allows users to: ❏ Create recovery plans ❏ Access an existing recovery plan(s) ❏ Create wellness plans ❏ Access an existing wellness plan(s) ❏ Create a crisis plan ❏ Access and existing crisis plan ❏ Contact my treatment team ❏ Contact people in my support network (such as families and friends) ❏ Consent to using a geofinder: granting someone access to an individual’s location for safety ❏ Add personal information ❏ Medical history ❏ List of medications ❏ List of allergies |
|
Devices/set-up What is this technology? What is this technology compatible with? |
This technology is compatible with my: ❏ Phone ❏ Web/Online ❏ Virtual ❏ Wearables (watches, heart rate monitors, etc.) ❏ This technology can sync with other devices ❏ This technology can sync with other applications (text, email, contacts, fitness, etc.) ❏ I have the devices required to use this technology (e.g., Wi-Fi, cellular service, headset) ❏ This technology has capabilities for remote access help |
Table 3.
Decision-Support Tool for Peer Support Specialists and Service Users (DSPSS) in Selecting Technologies to Promote Recovery: Summary of changes made to the tool after each focus groups
| Initial DSPSS Tool Domains | Initial Checklist-Version 1. developed by Co-production team | Version 2. Checklist post Focus group 2 | Version 3. Checklist post Focus group 2 | Final DSPSS Tool Domains | Version 4. Checklist post Focus group 3. Final Checklist |
|---|---|---|---|---|---|
|
| |||||
|
Privacy and Security Does this technology protect my personal information? |
❏ There is a clear privacy policy for me to read ❏ There is a clear privacy policy for me to consent to ❏ I understand the privacy policy ❏ I know how data is shared ❏ If my data is shared, I know it is shared securely ❏ I am aware if I can opt out of data collection ❏ I am aware how I can opt out of data collection |
❏ There is a clear privacy policy for me to read ❏ There is a clear privacy policy for me to consent to ❏ I am aware if this consent is time limited ❏ I understand the privacy policy ❏ I know how data is shared ❏ If my data is shared, I know it is shared securely ❏ If my data is shared, I know who it is shared with ❏ I am aware if I can opt out of data collection ❏ I am aware how I can opt out of data collection ❏ I am aware that this technology will not be used to incriminate me |
Privacy Policy ❏ There is a clear privacy policy for me to read ❏ There is a clear privacy policy for me to consent to ❏ I am aware if this consent is time limited ❏ I understand the privacy policy Data and Security ❏ I know how data is shared ❏ If my data is shared, I know it is shared securely ❏ If my data is shared, I know who it is shared with ❏ If my data is shared with others, I am aware of the limits to what they can keep confidential (e.g., if they are mandated reporters) ❏ I am aware if I can opt out of data collection ❏ I am aware how I can opt out of data collection ❏ I am aware that this technology will not be used to incriminate me ❏ This technology protects the personal boundaries of all parties involved (including peer support specialists, etc.) |
Principles of Recovery (or wellness) Does this technology embrace the general principles of recovery? |
❏This technology: Recovery Principles ❏ Gives me hope ❏ Encourages me to choose the life I want to live ❏ Makes me feel empowered ❏ Promotes embracing health challenges ❏ Promotes body positivity ❏ Promotes social connection ❏ Promotes building resiliency This technology: Recovery Language ❏ Uses pro-recovery language ❏ Uses person-centered language ❏ Uses every day, non-clinical language ❏ Uses strengths-based language ❏ Demonstrates strong mental health literacy Emotional Safety ❏ The language used in this technology has a low risk of activating or triggering me ❏ If content in this technology does trigger or activate me, there are links to helpful resources or contacts to support me ❏ I am aware of the potential risks I may be exposed to when using this technology (referencing specific drugs, suicide, settings) This technology: Recovery Resources ❏ Contains helpful resources to learn about wellness ❏ Has activities that I am interested in to practice wellness ❏ Has Warm Line phone numbers built-in ❏ Links with other applications/technology that promote wellness (e.g., housing, finances, childcare, meetings) |
|
Cost Are there any monetary costs (or payments) involved in using this technology? If yes, who is paying? |
❏ This technology has no hidden costs ❏ I am aware if it is free ❏ I am aware of up-front monetary costs (if a one-time payment) ❏ I am aware of weekly, monthly, or yearly costs (if a subscription) ❏ I can afford using this technology ❏ I am aware if costs are covered by my health insurance provider ❏ I am aware if costs are covered by an organization or program (such as through research or scholarships) ❏ I am aware how much of my monthly data plan is used by this technology |
❏ This technology has no hidden costs ❏ I am aware if it is free ❏ I am aware of upfront monetary costs (if a one-time payment) ❏ I am aware of weekly, monthly, or yearly costs (if a subscription) ❏ I can afford using this technology ❏ I am aware if costs are covered by my health insurance provider ❏ I am aware if costs are covered by an organization or program (such as through research or scholarships) ❏ I am aware how much of my monthly data plan is used by this technology ❏ I can use this technology offline (e.g., without wifi or cellular service) |
Monetary Costs ❏ This technology has no hidden costs ❏ I am aware if it is completely free ❏ I am aware if it is free but only for a certain number of days (e.g., if it is a trial period) ❏ I am aware of upfront monetary costs (if a one-time payment) ❏ I am aware of weekly, monthly, or yearly costs (if a subscription) ❏ I can afford using this technology ❏ I am aware if costs are covered by my health insurance provider ❏ I am aware if costs are covered by an organization or program (such as through research or scholarships) ❏ I can use this technology offline (e.g., without wifi or cellular service) ❏ I am aware how much of my monthly data plan is used by this technology ❏ I know how to double-check if this technology is using data (minutes), even if my device is connected to wifi Costs to the Device ❏ If using the technology requires me to download an application or software, I am aware of the risks it poses to my hardware (e.g., phone, tablet, computer, etc) ❏ I am aware of how much storage is taken up on my device if using this technology ❏ I am aware of the extent to which using this technology will drain my battery |
Privacy and Security Does this technology protect my personal information? |
Privacy Policy ❏ There is a clear privacy policy for me to read ❏ There is a clear privacy policy for me to consent to ❏ I am aware if this consent is time-limited ❏ I understand the privacy policy Data and Security ❏ I know how data is shared ❏ If my data is shared, I know it is shared securely ❏ If my data is shared, I know who it is shared with ❏ If my data is shared with others, I am aware of the limits to what they can keep confidential (e.g., if they are mandated reporters) ❏ If I am a guest/member/person supported at an agency, I am aware if my data (engagement, theme of discussion, etc.) will be documented ❏ If I am a guest/member/person supported at an agency, I am aware if my data (engagement, theme of discussion, etc.) will be shared with members of my treatment team ❏ I am aware if I can optout of data collection ❏ I am aware of how I can opt-out of data collection ❏ I am aware that this technology will not be used to incriminate me ❏ This technology protects the personal boundaries of all parties involved (including service users, peer support specialists, etc.) ❏ I am aware of possible risks to confidentiality (e.g., if video chatting with someone, knowing that another individual may walk into the room and overhear parts of the discussion) |
|
Usability Do I want to use this technology? |
❏ This technology is easy to use ❏ I like the appearance of this technology ❏ As a user, I feel confident that I can navigate the different features of the technology ❏ This technology has content that is relevant to me ❏ This technology has content that excites me ❏ I want to use this technology ❏ I think this technology could be helpful for my wellness ❏ I think this technology could be helpful for my recovery ❏ This technology works on my computer and/or phone (i.e. Android, IPhone, Windows vs. Apple, etc.) |
❏ This technology is easy to use ❏ I like the appearance of this technology ❏ As a user, I feel confident that I can navigate the different features of the technology ❏ I understand the terminology used ❏ This technology has content that is relevant to me ❏ This technology has content that excites me ❏ I want to use this technology ❏ I think this technology could be helpful for my wellness ❏ I think this technology could be helpful for my recovery ❏ This technology works on my computer and/or phone (i.e. Android, IPhone, Windows vs. Apple, etc.) ❏ This technology allows another person (e.g., peer support specialist, IT desk, customer service) to help me set up an account remotely ❏ I have access to this technology in my current setting |
Engagement ❏ I want to use this technology ❏ I like the appearance of this technology ❏ I understand the terminology used ❏ I can easily use this technology ❏ As a user, I feel confident that I can navigate the different features of the technology ❏ The content is relevant to me ❏ The content excites me ❏ The content keeps me engaged This technology: Helpfulness ❏ Has evidence (e.g., scientific, clinical, reviews, blogs, etc.) of being effective ❏ Has been helpful for others with similar lived experiences (e.g., peers) ❏ Could be helpful for my wellness ❏ Could be helpful for my recovery This technology: Set-up and devices ❏ Works like it is supposed to (e.g., can open hyperlinks, copy and paste, etc.) ❏ Works on my device (i.e. Android, iPhone, Windows vs. Apple, etc.) ❏ Allows another person to help me set up an account remotely (e.g., peer support specialist, IT desk, customer service) ❏ Is accessible from my current setting |
Cost Are there any monetary costs (or payments) involved in using this technology? If yes, who is paying? |
Monetary Costs ❏ This technology has no hidden costs ❏ I am aware if it is completely free ❏ I am aware if it is free but only for a certain number of days (e.g. if it is a trial period) ❏ I am aware of up-front monetary costs (if a one-time payment) ❏ I am aware of weekly, monthly, or yearly costs (if a subscription) ❏ I can afford using this technology ❏ I am aware if costs are covered by my health insurance provider ❏ I am aware if the agency/organization I work at or receive services from will cover any costs associated with using this technology (e.g., cost to purchase technology, cost to provide additional equipment such as headphones and chargers, etc.) ❏ I am aware if costs are covered by an organization or program (such as through research or scholarships) ❏ I can use this technology offline (e.g., without Wi-Fi or cellular service) ❏ I am aware of how much of my monthly data plan is used by this technology ❏ I know how to doublecheck if this technology uses data (minutes), even if my device is connected to Wi-Fi. Costs to the Device ❏ If using the technology requires me to download an application or software, I am aware of the risks it poses to my hardware (e.g., phone, tablet, computer, etc.) ❏ I am aware of how much storage is taken up on my device if using this technology. ❏ I am aware of the extent to which using this technology will drain my battery. |
|
Accessibility Am I able to use this technology? |
❏ Visual: I can customize the display (lighting, text size, color scheme) ❏ Hearing: I can customize the sound (volume) ❏ Written language: I can read and comprehend the words the technology uses ❏ Spoken Language: I can customize the technology to speak in my preferred language ❏ Touch: I am able to interact with this technology through touch (this includes vibrations, scrolling, etc.) ❏ Alternate formats are available ❏ General statement: This technology can accommodate all types of disabilities |
❏ Visual: I can customize the display (lighting, text size, color scheme) ❏ Hearing: I can customize the sound (volume, alert) ❏ Language: This technology has a read-aloud feature ❏ Language: This technology has a talk-to-text feature ❏ Written language: I can read and comprehend the words the technology uses ❏ Spoken Language: I can customize the technology to speak in my preferred language (and dialect) ❏ Touch: I am able to interact with this technology through touch (this includes vibrations, scrolling, etc.) ❏ Alternate formats are available ❏ General statement: This technology can accommodate all types of disabilities |
Sensory Accommodations ❏ This technology can accommodate all types of disabilities ❏ Visual - I can customize the display (lighting, text size, color scheme) ❏ Hearing - I can customize the sound (volume, alert) ❏ Touch - I am able to interact with this technology through touch (this includes vibrations, scrolling, etc.) Speech and Language ❏ This technology is formatted in my preferred language ❏ I can customize the technology to speak or scribe in my preferred language (and dialect) Additional This technology has: ❏ A read-aloud feature ❏ A talk-to-text feature ❏ A “scribble” (or draw) to text feature |
Usability Do I want to use this technology? Is this technology helpful? |
Engagement ❏ I want to use this technology ❏ I want to use this technology ❏ I like the appearance of this technology ❏ I understand the terminology used ❏ I can easily use this technology (I feel comfortable) ❏ As a user, I feel confident that I can navigate the different features of the technology ❏ The content is relevant to me ❏ The content excites me ❏ The content keeps me engaged ❏ This technology promotes self-determination ❏ There are platforms for people to train and support me in using this technology ❏ I can customize this technology to make me feel comfortable and engaged (e.g., via creating avatars) This technology: Helpfulness ❏ Has evidence (e.g., scientific, clinical, reviews, blogs, etc.) of being effective ❏ Has been helpful for others with similar lived experiences (e.g., peers) ❏ Could be helpful for my wellness ❏ Could be helpful for my recovery Set-up and devices This technology: ❏ Is compatible with my device(s) (Works on my device (i.e., Android, iPhone, Windows vs. Apple, etc.) ❏ Works like it is supposed to (e.g., can open hyperlinks, copy and paste, etc.) ❏ Allows another person to help me set up an account remotely (e.g., peer support specialist, IT desk, customer service) |
|
Inclusion and Equity Is this technology inclusive and equitable? |
This technology is: ❏ Inclusive of different races ❏ Inclusive of different ethnicities ❏ Inclusive of different gender identities and sexual orientations (e.g., LGBTQ+ friendly) ❏ Accessible to service users, regardless of socioeconomic status ❏ Accessible to service users, regardless of location (urban, rural, etc.) ❏ Uses language and terms I can understand ❏ Has help available for parts I don’t understand (e.g., calling a help desk) |
This technology is: ❏ Inclusive of different races ❏ Inclusive of different ethnicities ❏ Inclusive of different gender identities and sexual orientations (e.g., LGBTQIA friendly) ❏ Accessible to service users, regardless of socioeconomic status ❏ Accessible to service users, regardless of location (urban, rural, etc.) ❏ Uses language and terms I can understand |
This technology is: ❏ Inclusive of different races ❏ Inclusive of different ethnicities ❏ Inclusive of different gender identities and sexual orientations (e.g., LGBTQIA friendly) ❏ Inclusive of different religious and/or spiritual beliefs ❏ Accessible to service users, regardless of socioeconomic status ❏ Accessible to service users, regardless of location (urban, rural, etc.) ❏ Uses language and terms I can understand |
Accessibility Am I able to use this technology? |
❏ I can access this technology from my device and or my location Sensory Accommodations ❏ This technology can accommodate all types of disabilities ❏ Visual - I can customize the display (e.g. lighting, text size, color scheme) ❏ Hearing - I can customize the sound (e.g. volume, alert) ❏ Touch - I can interact with this technology through touch (e.g. this includes vibrations, scrolling, etc.) This technology has: Additional Features ❏ A read-aloud feature ❏ A talk-to-text feature ❏ A “scribble” (or draw) to text feature ❏ This technology is formatted in my preferred language ❏ I can customize the technology to speak or scribe in my preferred and dialect |
|
Helpfulness Does this help people? |
❏ There is evidence that this technology is helpful ❏ Scientific journal article ❏ Blog ❏ Online reviews ❏ Recommended by health professionals ❏ There is evidence that other individuals with lived mental health experience have found this technology to be helpful ❏ This includes peer support specialists, peer mentors, therapeutic mentors, etc. ❏ This technology was designed by or with peers |
❏ There is evidence that this technology is helpful ❏ Scientific journal article ❏ Blog ❏ Online reviews ❏ Recommended by health professionals ❏ There is evidence that other individuals with lived mental health experience have found this technology to be helpful ❏ This includes peer support specialists, peer mentors, therapeutic mentors, etc. ❏ This technology was designed by or with peers |
Inclusion and Equity Is this technology inclusive and equitable? |
This technology is: ❏ Inclusive of different races ❏ Inclusive of different ethnicities ❏ Inclusive of different gender identities and sexual orientations (e.g., LGBTQIA+friendly) ❏ Inclusive of different religious and spiritual beliefs ❏ Accessible to service users, regardless of socio-economic status ❏ Accessible to service users, regardless of location (urban, rural, etc.) ❏ Uses language and terms that make me feel comfortable, language and terms that are attuned to my culture and identity, etc.? |
|
|
Principles of Recovery (or wellness) Does this technology embrace the general principles of recovery? |
This technology: ❏ Uses pro-recovery language ❏ Gives me hope ❏ Encourages me to choose the life I want to live ❏ Promotes users to embrace health challenges ❏ Promotes body positivity ❏ Uses person-centered language ❏ Demonstrates strong mental health literacy ❏ Encourages users to seek help if they need it ❏ Contains helpful resources to learn about wellness ❏ Has crisis phone numbers built in ❏ Has activities to practice wellness that I am interested in |
This technology: ❏ Uses pro-recovery language ❏ Gives me hope ❏ Encourages me to choose the life I want to live ❏ Promotes users to embrace health challenges ❏ Promotes body positivity ❏ Uses person-centered language ❏ Demonstrates strong mental health literacy ❏ Encourages users to seek help if they need it ❏ Contains helpful resources to learn about wellness ❏ Has Warm Line phone numbers built in ❏ Has activities to practice wellness that I am interested in ❏ Links with other applications/technology that promote wellness (e.g., housing, finances, child-care, meetings) ❏ The language used in this technology has a low risk of activating or triggering me ❏ I am aware of the potential risks I may be exposed to when using this technology (referencing specific drugs, suicide, settings) |
This technology: Recovery Principles ❏ Gives me hope ❏ Encourages me to choose the life I want to live ❏ Makes me feel empowered ❏ Promotes embracing health challenges ❏ Promotes body positivity ❏ Promotes social connection This technology: Recovery Language ❏ Uses pro-recovery language ❏ Uses person-centered language ❏ Uses every day, nonclinical language ❏ Uses strengths-based language ❏ Demonstrates strong mental health literacy ❏ The language used in this technology has a low risk of activating or triggering me ❏ If content in this technology does trigger me, there are links to helpful resources or contacts to support me ❏ I am aware of the potential risks I may be exposed to when using this technology (referencing specific drugs, suicide, settings) This technology: Recovery Resources ❏ Contains helpful resources to learn about wellness ❏ Has activities that I am interested in to practice wellness ❏ Has Warm Line phone numbers built in ❏ Links with other applications/technology that promote wellness (e.g., housing, finances, child-care, meetings) |
Personalized for needs Can this technology be personalized for my needs to promote wellness? |
This technology allows users to: ❏ Create recovery plans ❏ Access an existing recovery plan(s) ❏ Create wellness plans ❏ Access an existing wellness plan(s) ❏ Create a crisis plan ❏ Access and existing crisis plan ❏ Contact my treatment team ❏ Contact people in my support network (such as families and friends) ❏ Consent to using a geofinder: granting someone access to an individual’s location for safety ❏ Add personal information ❏ Medical history ❏ List of medications ❏ List of allergies |
|
Personalized for needs Can this technology be personalized for my needs to promote wellness? |
This technology allows users to: ❏ Create recovery plans ❏ Access an existing recovery plan(s) ❏ Create wellness plans ❏ Access an existing wellness plan(s) ❏ Create a crisis plan ❏ Access and existing crisis plan ❏ Contact their treatment team ❏ Contact people in their support network (such as families and friends) ❏ Add personal information: ❏ Medical history ❏ List of medications ❏ List of allergies |
This technology allows users to: ❏ Create recovery plans ❏ Access an existing recovery plan(s) ❏ Create wellness plans ❏ Access an existing wellness plan(s) ❏ Create a crisis plan ❏ Access and existing crisis plan ❏ Contact their treatment team ❏ Contact people in their support network (such as families and friends) ❏ GEOFINDER: ranting someone access to location if individual is at heightened risk of homelessness or suicide ❏ Add personal information: ❏ Medical history ❏ List of medications ❏ List of allergies |
This technology allows users to: ❏ Create recovery plans ❏ Access an existing recovery plan(s) ❏ Create wellness plans ❏ Access an existing wellness plan(s) ❏ Create a crisis plan ❏ Access and existing crisis plan ❏ Contact their treatment team ❏ Contact people in their support network (such as families and friends) ❏ *GEOFINDER: ranting someone access to location if individual is at heightened risk of homelessness or suicide ❏ Add personal information: ❏ Medical history ❏ List of medications ❏ List of allergies |
Devices/set-up What is this technology? What is this technology compatible with? |
This technology is compatible with my: ❏ Phone ❏ Web/Online ❏ Virtual ❏ Wearables (watches, heart rate monitors, etc.) ❏ This technology can sync with other devices ❏ This technology can sync with other applications (text, email, contacts, fitness, etc.) ❏ I have the devices required to use this technology (e.g., Wi-Fi, cellular service, headset) ❏ This technology has capabilities for remote access help |
|
Devices/set-up Types of technology |
❏ Phone ❏ Web/Online ❏ Virtual ❏ Wearables (watches, heart rate monitors, etc.) ❏ This technology can sync with other devices ❏ This technology can sync with other applications (text, email, contacts, fitness, etc.) ❏ I have the devices required to use this technology (e.g., Wi-Fi, cellular service, headset) |
❏ Phone ❏ Web/Online ❏ Virtual ❏ Wearables (watches, heart rate monitors, etc.) ❏ This technology can sync with other devices ❏ This technology can sync with other applications (text, email, contacts, fitness, etc.) ❏ I have the devices required to use this technology (e.g., Wi-Fi, cellular service, headset) ❏ This technology has capabilities for remote access help |
❏ Phone ❏ Web/Online ❏ Virtual ❏ Wearables (watches, heart rate monitors, etc.) ❏ This technology can sync with other devices ❏ This technology can sync with other applications (text, email, contacts, fitness, etc.) ❏ I have the devices required to use this technology (e.g., Wi-Fi, cellular service, headset) ❏ This technology has capabilities for remote access help |
||
Contributor Information
Mbita Mbao, Simmons University.
Yaara Zisman, Temple University.
Karen L. Fortuna, Dartmouth Centers for Health and Aging
References
- 1.Solomon PL. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. 2004;27(4):392–401. [DOI] [PubMed] [Google Scholar]
- 2.Watson E. The mechanisms underpinning peer support: a literature review. J Ment Health. 2019;28(6):677–688. doi: 10.1080/09638237.2017.1417559 [DOI] [PubMed] [Google Scholar]
- 3.3 Samhsa.gov. https://www.samhsa.gov/sites/default/files/programs_campaigns/brss_tacs/value-of-peers-2017.pdf. Published 2021. Accessed January 7, 2021.
- 4.Fortuna KL, DiMilia PR, Lohman MC, et al. Systematic Review of the Impact of Behavioral Health Homes on Cardiometabolic Risk Factors for Adults With Serious Mental Illness. Psychiatr Serv. 2020b;71(1):57–74. doi: 10.1176/appi.ps.201800563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortuna KL, Naslund JA, LaCroix JM, et al. Digital Peer Support Mental Health Interventions for People With a Lived Experience of a Serious Mental Illness: systematic Review. JMIR Ment Health. 2020a;7(4):e16460. doi: 10.2196/16460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medicare Telemedicine Health Care Provider Fact Sheet | CMS. Cms.gov. https://www.cms.gov/newsroom/factsheets/medicare-telemedicine-health-care-providerfact-sheet. Published 2021. Accessed January 7, 2021.
- 7.Fortuna KL, Myers AL, Walsh D, Walker R, Mois G, Brooks JM. Strategies to Increase Peer Support Specialists’ Capacity to Use Digital Technology in the Era of COVID-19: Pre-Post Study. JMIR Ment Health. 2020;7(7):e20429. doi: 10.2196/20429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan S, Torous J, Hinton L, Yellowlees P. Towards a Framework for Evaluating Mobile Mental Health Apps. Telemedicine and e-Health. 2015;21(12):1038–1041. doi: 10.1089/tmj.2015.0002 [DOI] [PubMed] [Google Scholar]
- 9.Healthcare apps available Apple App Store 2020 | Statista. Statista. https://www.statista.com/statistics/779910/healthapps-available-ios-worldwide/. Published 2021. Accessed January 7, 2021.
- 10.Store.samhsa.gov.https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-0201-004_Final_508.pdf. Published 2021. Accessed January 7, 2021.
- 11.Torous JB, Chan SR, Gipson S, et al. A Hierarchical Framework for Evaluation and Informed Decision Making Regarding Smartphone Apps for Clinical Care. Psychiatr Serv. 2018;69(5):498–500. doi: 10.1176/appi.ps.201700423 [DOI] [PubMed] [Google Scholar]
- 12.APA App Advisor. Psychiatry.org. Accessed January 7, 2021. https://www.psychiatry.org/psychiatrists/practice/mental-health-apps
- 13.Technology and the future of mental health treatment. Nih.gov. Accessed January 7, 2021. https://www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-healthtreatment/index.shtml
- 14.Gregg L, Tarrier N. Virtual reality in mental health. Soc Psychiatry Psychiatr Epidemiol. 2007;42(5):343–354. doi: 10.1007/s00127-007-0173-4 [DOI] [PubMed] [Google Scholar]
- 15.Jones CM, Scholes L, Johnson D, Katsikitis M, Carras MC. Gaming well: links between videogames and flourishing mental health. Front Psychol. 2014;5:260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. Feasibility and acceptability of Facebook for health promotion among people with serious mental illness. Digit Health. 2016;2. doi: 10.1177/2055207616654822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zisman-Ilani Y, Shern D, Deegan P, et al. Continue, adjust, or stop antipsychotic medication: developing and user testing an encounter decision aid for people with first-episode and long-term psychosis. BMC Psychiatry. 2018;18(1):142. doi: 10.1186/s12888-018-1707-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaminskiy E, Zisman-Ilani Y, Ramon S. Barriers and Enablers to Shared Decision Making in Psychiatric Medication Management: A Qualitative Investigation of Clinician and Service Users’ Views. Front Psychiatry. 2021;12:678005. Published 2021 Jun 17. doi: 10.3389/fpsyt.2021.678005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zisman-Ilani Y, Lysaker PH, Hasson-Ohayon I. Shared Risk Taking: Shared Decision Making in Serious Mental Illness. Psychiatr Serv. 2021;72(4):461–463. doi: 10.1176/appi.ps.202000156 [DOI] [PubMed] [Google Scholar]
- 20.Zisman-Ilani Y, Barnett E, Harik J, Pavlo A, O’Connell M. Expanding the concept of shared decision making for mental health: systematic search and scoping review of interventions. Mental Health Review Journal. 2017;22(3):191–213. doi: 10.1108/mhrj-01-2017-0002 [DOI] [Google Scholar]
- 21.Zisman-Ilani Y, Roe D, Elwyn G, et al. Shared Decision Making for Psychiatric Rehabilitation Services Before Discharge from Psychiatric Hospitals. Health Commun. 2019;34(6):631–637. doi: 10.1080/10410236.2018.1431018 [DOI] [PubMed] [Google Scholar]
- 22.Tlach L, Wüsten C, Daubmann A, Liebherz S, Härter M, Dirmaier J. Information and decision-making needs among people with mental disorders: a systematic review of the literature. Health Expect. 2015;18(6):1856–1872. doi: 10.1111/hex.12251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salyers MP, Zisman-Ilani Y. Shared Decision-Making and Self-Directed Care. In: Goldman H, Frank R, Morrissey J, eds. The Palgrave Handbook of American Mental Health Policy. Cham: Palgrave Macmillan; 2020. doi: 10.1007/978-3-030-11908-9_8 [DOI] [Google Scholar]
- 24.Ramon S, Zisman-Ilani Y, Kaminskiy E. Guest editorial. Ment Health Rev (Brighton). 2017;22(3):149–151. doi: 10.1108/MHRJ-01-2017-0008 [DOI] [Google Scholar]
- 25.Dorsey ER, Yvonne Chan YF, McConnell MV, Shaw SY, Trister AD, Friend SH. The Use of Smartphones for Health Research. Acad Med. 2017;92(2):157–160. doi: 10.1097/ACM.0000000000001205 [DOI] [PubMed] [Google Scholar]
- 26.Cunningham-Erves J, Barajas C, Mayo-Gamble TL et al. Formative research to design a culturally-appropriate cancer clinical trial education program to increase participation of African American and Latino communities. BMC Public Health 20, 840 (2020). 10.1186/s12889-020-08939-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elwyn G, O’Connor A, Stacey D, et al. ; International Patient Decision Aids Standards (IPDAS) Collaboration. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. doi: 10.1136/bmj.38926.629329.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marrin K, Brain K, Durand M-A, et al. Fast and frugal tools for shared decision-making: how to develop Option Grids. Eur J Pers Cent Healthc. 2013;1(1):240. doi: 10.5750/ejpch.v1i1.657 [DOI] [Google Scholar]
- 29.Ahmed SM, Palermo AG. Community engagement in research: frameworks for education and peer review. Am J Public Health. 2010;100(8):1380–1387. doi: 10.2105/AJPH.2009.178137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fortuna KL, Muralidharan A, Goldstein CM, Venegas M, Glass JE, Brooks JM. Certified Peer Specialists’ Perspective of the Barriers and Facilitators to Mobile Health Engagement. J Technol Behav Sci. 2020;5(4):318–323. doi: 10.1007/s41347-020-00138-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Willis GB, Artino AR Jr. What Do Our Respondents Think We’re Asking? Using Cognitive Interviewing to Improve Medical Education Surveys. J Grad Med Educ. 2013;5(3):353–356. doi: 10.4300/JGME-D-13-00154.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 33.VR/AR market size 2020. Statista.com. Accessed January 7, 2021. https://www.statista.com/statistics/591181/globalaugmented-virtual-reality-market-size/
- 34.Brunette MF, Achtyes E, Pratt S, et al. Use of Smartphones, Computers and Social Media Among People with SMI: opportunity for Intervention. Community Ment Health J. 2019;55(6):973–978. https://doiorg.ezproxy.simmons.edu/10.1007/s10597-019-00431-7 doi: 10.1007/s10597-019-00431-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reports, Data. MHealth market size, share & forecast, by segmentation, 2020–2027. Reportsanddata.com. Accessed January 7, 2021. https://www.reportsanddata.com/reportdetail/mobile-health-mhealth-market
- 36.Institute of Medicine (US) Committee on Crossing the Quality Chasm: Adaptation to Mental Health, Addictive Disorders. Supporting Patients’ Decision-Making Abilities and Preferences. National Academies Press; 2006. https://www.ncbi.nlm.nih.gov/books/NBK19831/ [Google Scholar]
- 37.Piltch CA. The role of self-determination in mental health recovery. Psychiatr Rehabil J. 2016;39(1):77–80. https://doiorg.ezproxy.simmons.edu/10.1037/prj0000176 doi: 10.1037/prj0000176 [DOI] [PubMed] [Google Scholar]
- 38.IT accessibility laws and policies. Section508.gov. Accessed January 7, 2021. https://www.section508.gov/manage/laws-andpolicies
- 39.Chu J, Reeve A, Milan N, et al. Researching the Effectiveness of a Decision Support Tool for Adult Consumers with Mental Health Needs and Their Care Managers. Patient-Centered Outcomes Research Institute (PCORI); 2019. [PubMed] [Google Scholar]
- 40.Cdc.gov. Accessed January 7, 2021. https://www.cdc.gov/ncbddd/disabilityandhealth/documents/disabilities_impacts_all_of_us.pdf
- 41.Subjective Cognitive Decline — A Public Health Issue. Cdc.gov. Published March 25, 2019. Accessed January 7, 2021. https://www.cdc.gov/aging/data/subjectivecognitive-decline-brief.html