Abstract
Objectives
The transcription factor 7-like 2 gene (TCF7L2) is associated with a predisposition to type 2 diabetes mellitus (T2DM) in different ethnic populations. This article investigated the relationship between TCF7L2 gene expression and several biochemical indexes among different age categories of T2DM in a sample of the Iraqi population.
Methods
One hundred and fifty blood samples were collected from three groups: young T2DM (10–35 years), old T2DM (40–80 years), and healthy control (10–65 years) groups. Both sexes were enrolled. qPCR was performed to explore the expression of the TCF7L2 gene. Biochemical tests were performed to assess hemoglobin A1C (HbA1c), triglyceride (TG), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) levels. The body mass index (BMI) was calculated. The results were statistically analyzed.
Results
Patients with T2DM had higher BMI, TG, and LDL, and lower HDL than the control group. There was a strong positive correlation between hemoglobin A1C (HbA1c) and BMI, TG, and LDL and a negative correlation between HbA1c and HDL. Expression of the TCF7L2 gene showed a significant difference between old and young patients by 1.68 and 0.207 fold, respectively. These results showed that old patients had higher gene expression than young patients.
Conclusion
TCF7L2 gene expression was affected by age, with higher expression in old T2DM patients. This may influence beta cell functions and insulin secretion.
Keywords: Biochemical test, Diabetes mellitus, Gene expression, HbA1c, T2DM, TCF7L2
الملخص
أهداف البحث
يعتبر جين "عامل الانتساخ 7-مثل 2" من الجينات المهمة التي وجد أنها مرتبطة بالاستعداد لمرض السكري من النوع الثاني في مختلف المجموعات العرقية. هدف هذا البحث هو التحقيق في العلاقة بين التعبير الجيني جين "عامل الانتساخ 7-مثل 2" وعدة مؤشرات كيميائية حيوية بين فئات عمرية مختلفة من مرضى السكري من النوع الثاني في عينة من السكان العراقيين.
طرق البحث
تم جمع 150 عينة دم بالتساوي من 3 مجموعات: مرضى السكري من النوع الثاني الشباب (10-35 سنة)، مرضى السكري من النوع الثاني المسنين (40-80 سنة)، ومجموعة ضابطة صحية (10-65 سنة). تم إشراك كلا الجنسين. تم إجراء تفاعل البلمرة المتسلسل في الوقت الفعلي لاستكشاف التعبير الجيني جين "عامل الانتساخ 7-مثل 2". تم إجراء الاختبارات الكيميائية الحيوية: نسبة الهيموجلوبين السكري، والدهون الثلاثية، والبروتين الدهني منخفض الكثافة، والبروتين الدهني عالي الكثافة. تم احتساب مؤشر كتلة الجسم. تم تحليل النتائج إحصائيا.
النتائج
كان لدى مرضى السكري من النوع الثاني سجلات أعلى فيما يتعلق بمؤشر كتلة الجسم، والدهون الثلاثية، والبروتين الدهني منخفض الكثافة، ونتائج البروتين الدهني عالي الكثافة أقل من مجموعة الضبط. هناك ارتباط إيجابي قوي بين نسبة الهيموجلوبين السكري ومؤشر كتلة الجسم، والدهون الثلاثية، والبروتين الدهني منخفض الكثافة. كان هناك ارتباط سلبي بين نسبة الهيموجلوبين السكري والبروتين الدهني عالي الكثافة. أظهر التعبير الجيني جين "عامل الانتساخ 7-مثل 2" اختلافا كبيرا بين المرضى المسنين والشباب بنسبة 1.68 و 0.207 على التوالي. أظهرت هذه النتائج أن المرضى المسنين لديهم تعبير جيني أعلى مقارنة بالمرضى الشباب.
الاستنتاجات
تأثر التعبير الجيني جين "عامل الانتساخ 7-مثل 2 "بالعمر، وكانت السجلات الأعلى للمرضى المسنين من النوع الثاني من السكري. قد يؤثر ذلك على وظائف خلايا بيتا وإفراز الأنسولين.
الكلمات المفتاحية: الاختبار الكيميائي الحيوي، مرض السكري, التعبير الجيني, نسبة الهيموجلوبين السكري, السكري من النوع الثاني, جين "عامل الانتساخ 7-مثل 2"
Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder defined by elevated blood glucose levels resulting from insufficient insulin synthesis or impaired insulin function.1 It affects approximately 537 million people worldwide. It is predicted to affect 10.2% by 2030 and 10.9% by 2045. The World Health Organization expects that by 2030, such a metabolic pandemic will emerge as the seventh major cause of mortality globally, affecting more than 400 million people.2 DM is projected to have a global economic impact of $745 billion by 2030 due to economic expansion, nutritional changes, and population aging.3
In Iraq, DM caused 7279 deaths or 4.24% of total deaths.4 T2DM represents one of the most prevalent metabolic illnesses in the world.5 It is caused by a combination of two main causes: improper insulin secretion by pancreatic beta cells and failure of insulin-sensitive tissues to respond to insulin.6 Therefore, the molecular mechanisms involved in the synthesis and release of insulin and the insulin response in tissues must be extremely tightly controlled.7 Consequently, the defects in any of the involved could result in T2DM. Genetic and environmental variables impact its development. Obesity, overeating, lack of exercise, and hereditary factors affect insulin production and resistance.7 Based on twin family studies, T2DM complications have a 40% inheritance rate. In a study published in 2011, more than 36 genes were found to increase the risk of T2DM.8
Transcription factor 7-like 2 gene (TCF7L2) is one of the most well-studied genes for diabetic predisposition among many populations.9 TCF7L2 is a member of the T cell factor/lymphoid enhancer factor (TCF/LEF) family, with other members such as LEF1, TCF7, and TCF7L1 in humans. The term “T cell factor 4 (TCF4)” was previously mistaken for transcription factor 4.10 The TCF7L2 gene is located on chromosome 10q25.3 and contains a transcriptional element of about 215.9 kb. This gene consists of 17 exons, 5 of which are alternative splicing units. It encodes a transcription factor that interacts with β-catenin and works within the Wingless (Wnt) signaling pathway. It regulates several cellular processes including cell morphology, proliferation, motility, and oncogenesis.11 The gene TCF7L2 has received considerable interest among researchers due to its significant genetic association with increased susceptibility to T2DM. This genetic link has been shown to alter the function and survival of pancreatic beta cells.12 TCF7L2 is associated with metabolism, inflammation, and atherosclerosis.13 It is considered a key locus associated with the risk of T2DM by acting as a downstream effector of the Wnt/β-catenin signaling pathway. TCF7L2 risk variants interfere with the three mechanisms: glucose-stimulated insulin secretion, incretin-stimulated insulin secretion, and the conversion of proinsulin to insulin.14
Due to the importance of this gene in T2DM, the current study investigated its role in a sample of the Iraqi population and study age differences regarding gene expression.
Materials and Methods
Subjects and study design
The current study included the collection of 150 peripheral blood samples from patients with T2DM and healthy individuals as controls. These samples were equally divided into three groups: young T2DM patients (10–35 years), old T2DM patients (40–80 years), and healthy control (10–65 years) groups. Those patients were chosen randomly from private medical clinics in Baghdad, whereas the control group was randomly selected from apparently healthy individuals who did not have a diabetic history. All volunteers agreed to participate in this investigation after they were informed of the purpose of this study. American Diabetes Association criteria were followed by the physicians to diagnose T2DM if the fasting glucose was above 126 mg/dL (8.0 mmol/L). We included T2DM patients who had hemoglobin A1C (HbA1c) levels ≥8%. The exclusion criteria were pregnancy, alcoholism, liver disease, chronic renal infection, thyroid disease, and any endocrine disease.
Collection samples
Five milliliters of vein blood were drawn from each participant under aseptic circumstances, and then treated as follows.
-
1-
Two milliliters of blood were placed in an EDTA tube and stored at −20 °C for the HbA1c test.
-
2-
Two hundred and fifty microliters of blood from the first tube were added to an Eppendorf tube containing 750 μL of Triazole LS reagent, gently mixed, and stored at −20 °C for the gene expression test.
-
3-
The remaining 3 mL of blood was added to a clot activator tube, left at room temperature (20 °C–25 °C) for a few minutes, and then centrifuged for 15 min at 3000 rpm/min. The upper serum was collected and stored at −20 °C for subsequent biochemical tests.
Biochemical tests
Routine clinical procedures were followed to perform the biochemical tests according to the manufacturer's instructions for each kit. These kits were: I-Chroma HbA1c Glycosylated Hemoglobin Kit (Biotech Med Co., Barcelona, Spain), and Triglycerides, Cholesterol MR, and HDL-Cholesterol kits (Linear Chemicals, Barcelona, Spain).
Body mass index and low-density lipoprotein cholesterol measurements
The body mass index (BMI) index for each participant was determined as follows:
| BMI = mass (kg)/height (m)2 |
Total cholesterol was measured according to our previously published article.15 Low-density lipoprotein cholesterol (LDL) was calculated in the present study according to the following Friedwald formula:16
| LDL = total cholesterol – (high-density lipoprotein [HDL] + triglyceride [TG]/5) |
RNA extraction and cDNA synthesis
Total RNA was extracted using the Triazole Up Plus RNA Kit (TransGen Biotech Co., Ltd., Beijing, China), according to the manufacturer's instructions. Then the quantity and quality of the RNA samples were measured using the Nanodrop OneC spectrophotometer and the ratio of OD260/OD280 was measured for the total RNA samples. Then cDNA was prepared using the EasyScript One-Step gDNA Removal Kit and cDNA Synthesis Super Mix Reagent Kit (TransGen Biotech).
Quantitative PCR
Quantitative PCR (qPCR) was conducted to measure the threshold cycle (Ct) for all cDNA samples using the Rotor Gene Real-Time PCR System (Qiagen, Germantown, MD, USA). Reaction mixtures were prepared by utilizing the 2xTransStart® Top Green qPCR Super Mix. Each reaction was performed twice and individually. The primers were obtained from Alpha DNA (Montreal, Canada) according to the sequences in Table 1. The housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a reference gene. The melting temperature (Tm) for the forward and reverse primers was calculated according to the equation: Tm (°C) = 2 (A + T) + 4 (G + C). The annealing temperature (Ta) of the primers was estimated by the following equation: Ta (°C) = Tm − (2−5). We determined the lowest Tm for both the forward and reverse primers by comparing their Ta.17
Table 1.
Gene expression primers.
| Gene | Primer | Primer sequence (5ʹ→3ʹ) | Length | P | Reference |
|---|---|---|---|---|---|
| GAPDH | Forward | GAAATCCCATCACCATCTTCCAGG | 24 | 160 | 18 |
| Reverse | GAGCCCCAGCCTTCTCCATG | 20 | |||
| TCF7L2 | Forward | TGAAACCCAGATGTCACCAA | 20 | 158 | This study |
| Reverse | AACGAAGATGGTTCCCACTG | 20 |
P, Product size (bp)
qPCR cycling protocol for GAPDH gene expression
The cycling profile for GAPDH qPCR was programmed after following the optimization circumstances that accommodate the thermal profile, as shown in Table 2.
Table 2.
Thermal Profile of GAPDH gene expression.
| Step | Temperature (°C) | Time (s) | Cycle No. |
|---|---|---|---|
| Enzyme activation | 94 | 60 | 1 |
| Denaturation | 95 | 5 | 35 |
| Annealing | 58 | 15 | |
| Extension | 72 | 20 | |
| Dissociation | 55–95 | 1 |
qPCR cycling protocol for TCF7L2 gene expression
The cycling profile for TCF7L2 qPCR was programmed after following the optimization circumstances that accommodate the thermal profile, as shown in Table 3.
Table 3.
Thermal profile of TCF7L2 gene expression.
| Step | Temperature (°C) | Time (s) | Cycle No. |
|---|---|---|---|
| Enzyme activation | 94 | 30 | 1 |
| Denaturation | 94 | 10 | 35 |
| Annealing | 56 | 15 | |
| Extension | 72 | 20 | |
| Dissociation | 55–95 | 1 |
Statistical analyses
Data were statistically analyzed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA). The results are expressed as the mean ± standard deviation (SD). P < 0.05 was considered statistically significant. One-way analysis of variance and the chi-square test were used to statistically analyze the differences in means among the three groups. Duncan's multiple range test used different letters for statistically different means.
Distribution of age groups
The current study included 150 blood samples that were divided into three groups: young diabetic patients, old diabetic patients, and a healthy control group, as shown in Table 4. The ages of the three groups were 22.5800c ± 7.73830, 57.7400a ± 9.28420, and 37.6400b ± 17.82312, respectively. There was a significant difference among these groups (p = 0.0001) (Figure 1).
Table 4.
Age distribution for the three groups.
| Age groups | Young T2DM (n = 50) | Old T2DM (n = 50) | Control (n = 50) |
|---|---|---|---|
| <35 years | 50 (100%) | 0 | 27 (54%) |
| ≥40 years | 0 | 50 (100%) | 23 (46%) |
| Mean ± SD | 22.5800c ± 7.73830 | 57.7400a ± 9.28420 | 37.6400b ± 17.82312 |
| Std. Error | 1.09436 | 1.31298 | 2.52057 |
| Maximum | 35.00 | 85.00 | 70.00 |
| Minimum | 10.00 | 40.00 | 11.00 |
| p-value | 0.0001∗∗ | ||
| Chi-square | 0.004∗∗ | ||
∗∗ High significant result (p < 0.01).
Figure 1.
Mean age of the three groups (young T2DM patients, old T2DM patients, and healthy controls).
Results of the BMI
The BMI results for the three groups are shown in Table 5. There was a significant difference among the three groups (p = 0.001). The highest BMI level was for the elderly patients with a mean of 33.7645 ± 5.23186 kg/m2, followed by the young patients with a mean of 31.3372 ± 5.43931 kg/m2. The healthy control group had the lowest BMI level with a mean of 24.6428 ± 1.89878 kg/m2.
Table 5.
BMI results for the three groups.
| BMI (kg/m2) | Young T2DM | Old T2DM | Control |
|---|---|---|---|
| 18.5–24.9 | 2 (4%) | 1 (2%) | 25 (50%) |
| 25–29.9 | 20 (40%) | 10 (20%) | 25 (50%) |
| ≥30 | 28 (56%) | 39 (78%) | 0 |
| Mean ± SD | 31.3372b ± 5.43931 | 33.7645a ± 5.23186 | 24.6428c ± 1.89878 |
| p-value | 0.001∗∗ | ||
∗∗ High significant result (p < 0.01).
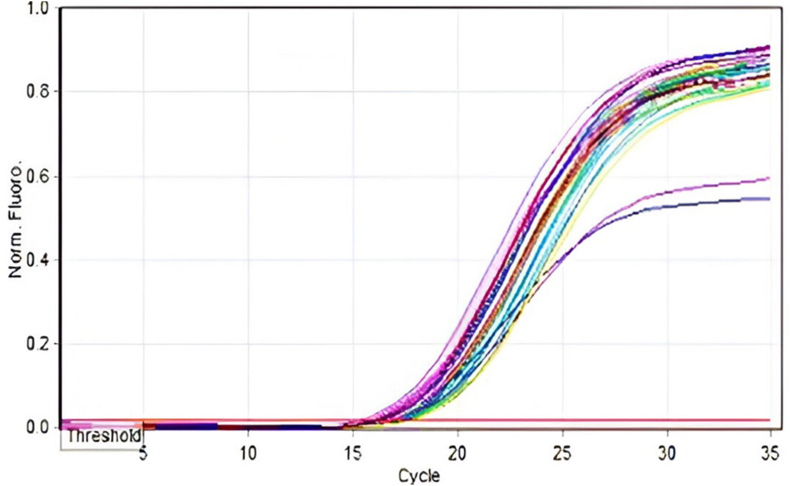
Results of TCF7L2 and GAPDH gene expression
TCF7L2 gene expression was evaluated using qPCR. The level of gene expression was normalized to that of the GAPDH housekeeping gene and quantified using the 2-ΔΔCt and ΔCt values presented in Figure 2, Figure 3. The Livak Method19 was used to quantify TCF7L2 gene expression after normalization to the reference gene GADPH, among the patients and healthy control groups.
Figure 2.
GAPDH amplification plots by qPCR.
Figure 3.
Amplification plots of TCF7L2 genes by qPCR.
The gene expression of TCF7L2 compared to the housekeeping gene GAPDH. The results were statistically analyzed and the fold expression of the TCF7L2 gene is shown in Table 6.
Table 6.
Gene expression of TCF7L2.
| TCF7L2 Ct Means | GAPDH Ct Means | ΔCt | ΔΔCt | Gene Expression Fold (2 −ΔΔCt) | p-value | |
|---|---|---|---|---|---|---|
| Young T2DM | 29.87 | 16.5794 | 13.29 | 2.27 | 0.207b | 0.0001∗∗ |
| Old T2DM | 26.90 | 16.6292 | 10.27 | 0.75 | 1.68a | |
| Control | 27.88 | 16.8614 | 11.02 | 0 | 1.00a |
∗∗ High significant result (p < 0.01).
Our results revealed a significant difference in TCF7L2 gene expression between the control and patient groups (p = 0.0001). TCF7L2 gene expression was 1.68-fold higher in old patients than in healthy controls, whereas there was a reduction in TCF7L2 gene expression in the young patient group by 0.207-fold, as shown in Figure 4.
Figure 4.
Heat map of TCF7L2 gene expression for the three groups.
Results of the biochemical tests
The results of the biochemical tests are shown in Table 7 and Figure 5. The results of the TG test for the three groups revealed a significant difference among the groups (p = 0.0001); the highest TG level was in the old patients with a mean of 273.9200 ± 182.19084 mg/dL, followed by the young patients with a mean of 193.0800 ± 82.83543 mg/dL, whereas the healthy control group had the lowest TG level with a mean of 89.5000 ± 14.57738 mg/dL. The LDL results in the three groups revealed a significant difference among the groups (p = 0.0001). The old and young groups had the highest LDL levels with means of 113.7600 ± 45.76629 and 110.1400 ± 43.42858 mg/dL, respectively. The healthy control group had the lowest LDL level with a mean of 73.4000 ± 9.24276 mg/dL. The HDL results revealed a significant difference among the groups (p = 0.03). In contrast to the LDL results, the healthy control group had the highest HDL level with a mean of 44.0866 ± 3.57163 mg/dL, whereas the young and old groups had lower levels of HDL than the control groups with means of 40.3600 ± 10.93349 and 38.8180 ± 13.97984 mg/dL, respectively.
Table 7.
Results of the biochemical test results for the three groups.
| N | Mean | SD | SEM | p-value | ||
|---|---|---|---|---|---|---|
| TG (mg/dL) | Young T2DM | 50 | 193.0800b | 82.83543 | 11.71470 | 0.0001∗∗ |
| Old T2DM | 50 | 273.9200a | 182.19084 | 25.76568 | ||
| Control | 50 | 89.5000c | 14.57738 | 2.06155 | ||
| LDL (mg/dL) | Young T2DM | 50 | 110.1400a | 43.42858 | 6.14173 | 0.0001∗∗ |
| Old T2DM | 50 | 113.7600a | 45.76629 | 6.47233 | ||
| Control | 50 | 73.4000b | 9.24276 | 1.30712 | ||
| HDL (mg/dL) | Young T2DM | 50 | 40.3600a | 10.93349 | 1.54623 | 0.037∗ |
| Old T2DM | 50 | 38.8180b | 13.97984 | 1.97705 | ||
| Control | 50 | 44.0866a | 3.57163 | 0.50510 | ||
∗ significant result (p < 0.05).
∗∗ High significant result (p < 0.01).
Figure 5.
Means of the tested parameters.
Results of correlation analysis of TCF7L2 gene expression and other parameters
Correlation analysis for our results was done to determine the relationship between TCF7L2 gene expression and each of the tested parameters (Table 8 and Figure 6). Our results showed the absence of any significant correlation between TCF7L2 expression and the other parameters (p > 0.05). Age showed a significant positive correlation with both BMI and TG (p < 0.01). The results revealed highly significant positive correlations between BMI and HbA1c, TG, and LDL (p < 0.01), whereas a significant negative correlation was observed between BMI and HDL (p < 0.01). The results also confirmed that there was a significant positive correlation between HbA1c and each TG and LDL (p < 0.01). TG was also significantly positively correlated with LDL and negatively correlated with HDL (p < 0.01).
Table 8.
Correlation of TCF7L2 gene expression with the biochemical tests.
| Age | BMI | HbA1c | TG | LDL | HDL | TCF7L2 fold | ||
|---|---|---|---|---|---|---|---|---|
| Age | r | 1 | 0.252 | 0.054 | 0.284a | 0.008 | −0.082 | 0.104 |
| p | 0.002 | 0.514 | 0.000 | 0.924 | 0.317 | 0.204 | ||
| BMI | r | 0.252a | 1 | 0.655a | 0.411a | 0.236a | −0.217a | 0.004 |
| p | 0.002 | 0.000 | 0.000 | 0.004 | 0.008 | 0.958 | ||
| HbA1c | r | 0.054 | 0.655a | 1 | 0.479a | 0.430a | −0.149 | −0.031 |
| p | 0.514 | 0.000 | 0.000 | 0.000 | 0.069 | 0.703 | ||
| TG | r | 0.284a | 0.411a | 0.479a | 1 | 0.339a | −0.374a | 0.016 |
| p | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.842 | ||
| LDL | r | 0.008 | 0.236a | 0.430a | 0.339a | 1 | 0.096 | −0.037 |
| p | 0.924 | 0.004 | 0.000 | 0.000 | 0.243 | 0.656 | ||
| HDL | r | −0.082 | −0.217a | −0.149 | −0.374a | 0.096 | 1 | 0.061 |
| p | 0.317 | 0.008 | 0.069 | 0.000 | 0.243 | 0.458 | ||
| TCF7L2 fold | r | 0.104 | 0.004 | −0.031 | 0.016 | −0.037 | 0.061 | 1 |
| p | 0.204 | 0.958 | 0.703 | 0.842 | 0.656 | 0.458 | ||
Correlation coefficient (r), significance (p-value).
Significant correlation at the 0.01 level (2-tailed).
Figure 6.
Heat map of Pearson's correlation for all data.
Discussion
The current study showed an increase in BMI level among Iraqi diabetic patients compared to the control group. These results are in accordance with a previous study showing that the Iraqi population suffers a steady increase in obesity and its health complications.8,20 Middle Eastern countries (such as Iraq) have witnessed overweight and obesity spatially among adults. A previous study confirmed that the BMI cut-off point for the occurrence was 25.6 kg/m2,21 which was consistent with our results. The prevalence of T2DM increases with increasing BMI.22 Obesity itself causes a certain degree of insulin resistance. Adipocytes release non-esterified fatty acids, which are considered the main cause of insulin resistance and impairment of beta cell functions.23 Ectopic fat distribution in the viscera alters fat metabolism and accelerates diabetes. Abdominal obesity is a greater metabolic risk factor than overall obesity. Adipose tissue factors can promote chronic inflammation, insulin resistance, and damage to pancreatic beta cells, leading to impaired glucose tolerance and diabetes progression.24
Recently, the TCF7L2 gene has been suggested to play a role in obesity and T2DM.8 Our results showed significant increases in HbA1c, TG, and LDL levels compared with healthy controls. These results are consistent with those of Klisic et al.25 who showed that an undesirable lipid profile was associated with T2DM, and recommended considering the lipid profile to predict high levels of HbA1c. The authors also advocated for the early detection of dyslipidemia (blood lipid level) and maintenance of normal lipid levels as a precautionary step to help with the diagnosis of diabetes.
Our results did not reveal a significant correlation between fold gene expression of TCF7L2 and HbA1c concentration, which may have been due to the limited sample number. We found significant correlations between BMI and both TG and LDL, which aligns with the fact that the rise in BMI is associated with dyslipidemia and diabetes.26 Dyslipidemia is thought to be related to T2DM due to insulin resistance.27 The causes of rising TG levels in T2DM are insufficient production or action of insulin.28 Gluconeogenesis and glucagon-like peptide-1 (GLP-1) production are affected by the action of TCF7L2. This gene may cause T2DM by affecting lipid metabolism and adipogenesis.29
Our results on TCF7L2 gene expression in older patients are consistent with those reported in a study conducted on human islets from diabetic patients, which showed a 5-fold increase in TCF7L2 gene expression in T2DM.30
TCF7L2 plays a crucial role in the regulation of glucose in the blood. It encodes a transcription factor that is expressed in the fetal pancreas and regulates the Wnt signaling pathway through GLPs. Genetic alteration in TCF7L2 may influence insulin resistance by modulating GLP-1. Saxena et al.31 showed that modification of the TCF7L2 gene increases the risk of developing T2DM by altering insulin secretion. The overexpression of this gene could impair beta cell functions.30
TCF7L2 polymorphisms are significantly linked to T2DM susceptibility in Caucasian and Asian populations.32 These polymorphisms cause T2DM in several ways such as impairment of insulin secretion, defects in glucose-induced glucagon suppression, abnormal insulin processing, and enhancement of liver glucose release during fasting.33 Our results also revealed a significant decrease in TCF7L2 gene expression in young patients, which may be related to the decrease in insulin resistance in these patients compared with older patients due to the efficiency of beta cells, which decrease with duration of T2DM.34 Younger patients are expected to have better beta cell proliferation and function compared with older patients.
The exact mechanism of how TCF7L2 gene expression is regulated during the development of T2DM has not been completely discovered, but many previous studies have focused on its role in beta cells and insulin production rather than insulin resistance. A study conducted by Shu et al.35 showed opposite regulation between the level of mRNA and protein levels of TCF7L2 in T2DM. There was a reduction in TCF7L2 protein expression at the same time as an increase in TCF7L2 mRNA expression due to post-transcriptional regulation. The authors confirmed that the increase in TCF7L2 mRNA in T2DM is a consequence of beta cell function.
Post-transcriptional regulation is disrupted in T2DM through inhibition of translation by the accumulation of unfolded protein. Beta cells can process and fold large amounts of protein (about 5% of the total protein is insulin). There are specific requirements for beta cells to function properly. Stress or accumulation of antioxidant molecules could alter post-transcriptional regulation. These facts are in accordance with our results showing increased TCF7L2 mRNA levels in old patients since stress increases with age. Previous studies have shown that the increase in TCF7L2 mRNA expression compensates for the lack of TCF7L2 protein. The presence of this protein is essential for the functioning and presence of beta cells.36
The loss of TCF7L2 protein results in a decrease in the GLP-1 receptor (GLP-1R) and gastric inhibitory polypeptide (GIP)-stimulated AKT phosphorylation, as well as a decrease in the phosphorylation of AKT-mediated forkhead box 1 and nuclear exclusion. The interaction between TCF7L2 and GLP-1R/GIP receptor expression is essential in the regulation and survival of beta cells and thus controls insulin production. Any disturbance in this relationship could alter glucose homeostasis and insulin production.35 However, age represents a main risk factor for T2DM, due to the decline in beta cells with disease duration. In addition, insulin secretion decreases with age.37 Higher glucose-stimulated insulin secretion has been observed in younger patients (<40 years) compared to older patients, which correlates with the ability of beta cells to generate ATP.38
Limitations and future research
The main limitation of this study was the limited sample size, due to the reliance on personal funding. We recommend examining a larger sample size and examining TCF7L2 single nucleotide polymorphisms.
Conclusion
TCF7L2 gene expression was affected by age. Old T2BM patients had the highest score, which may influence beta cell functions and insulin secretion.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This article was funded by the first author “AHY.” The tests were carried out at the Institute of the Laboratories of Genetic Engineering and Biotechnology/University of Baghdad-Iraq.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
The Ethics Committee of the Genetic Engineering and Biotechnology Institute of Baghdad, Iraq approved this study (Ref No. EC/1310-A) on May 15, 2022.
Author contributions
AHY and AMA conceived and designed the study. AHY conducted the research, provided the research materials, and collected and organized the data. AHY analyzed and interpreted the data. AHY wrote the initial and final drafts of the article and provided logistical support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Hamid S.M., Shani W.S. The association of IL-10 (-592A/C) gene polymorphism with progression of type 2 diabetes mellitus in Basrah province-Iraq. Iraqi J Sci. 2018:819–826. [Google Scholar]
- 2.Queen B.K., Mohammed A.A. Using bioinformatics and NCBI tools to sequence and structure analysis of transcription factor 7 like 2 gene (TCF7L2) in Iraqi diabetic mellitus type II patients. J Appl Sci Nanotechnol. 2021;2:1–10. [Google Scholar]
- 3.Wang S., Guo Y., Maitland E., Nicholas S., Sun J., Leng A. The economic burden of hospital costs on families with type 1 diabetes mellitus children: the role of medical insurance in Shandong Province, China. Front public Heal. 2022;10 doi: 10.3389/fpubh.2022.853306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hussein A.J., Ali S.K. Assessment the effect of WFS1 gene rs734312 G/A variant with type 2 diabetes in Iraqi Arab patients. Hum Genet. 2023;35 [Google Scholar]
- 5.Tahir N.T., Ahmed H.S., Ahmed H.S. Studies on the role of retinol binding protien-4 in type 2 diabetic Iraqi patients with metabolic syndrome. Nucleus. 2023:1–7. [Google Scholar]
- 6.Al-Okhedi M.J., Al-Ani mq, Rasheed M.N. Immunological study of coronary artery disease associated with diabetes mellitus type ii in Iraqi patients. Asian J Pharmaceut Clin Res. 2018;11:269–272. [Google Scholar]
- 7.Hasan H.R., Aburahma N.N.A., Al-kazaz A.K.A. Proteins level in Sera and Saliva of Type2 diabetic Iraqi patients with and without proliferative diabetic retinopathy. Orient J Chem. 2017;33:2776. [Google Scholar]
- 8.Mohammed A.K., Al-Thuwaini T.M., Al-Shuhaib M.B.S. Single nucleotide polymorphism rs7908486 of the tcf7l2 gene is highly associated with obesity in the Iraqi population. Arch Biol Sci. 2021;73:39–45. [Google Scholar]
- 9.Gaulton K.J., Ferreira T., Lee Y., Raimondo A., Mägi R., Reschen M.E., et al. Genetic fine mapping and genomic annotation defines causal mechanisms at type 2 diabetes susceptibility loci. Nat Genet. 2015;47:1415–1425. doi: 10.1038/ng.3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Y., Pan G.-P., Cai J.-W., Niu Y.-M., Xie L.-C. Association between transcription factor 7-like 2 C/T polymorphism and diabetic retinopathy risk: a meta-analysis. Ophthalmic Res. 2023;66:66–74. doi: 10.1159/000525803. [DOI] [PubMed] [Google Scholar]
- 11.Motamadinasab M., Dastgheib S.A., Golshan-Tafti M., Bahrami R., Javaheri A., Tabatabaie R.S., et al. Association of TCF7L2 polymorphisms with susceptibility to gestational diabetes mellitus: a systematic review and meta-analysis. World J Peri Neonatol. 2021;4(2):88–103. [Google Scholar]
- 12.Tomlinson B., Patil N.G., Fok M., Chan P., Lam C.W.K. The role of sulfonylureas in the treatment of type 2 diabetes. Expet Opin Pharmacother. 2022;23:387–403. doi: 10.1080/14656566.2021.1999413. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell R.K., Mondragon A., Chen L., Mcginty J.A., French P.M., Ferrer J., et al. Selective disruption of Tcf7l2 in the pancreatic β cell impairs secretory function and lowers β cell mass. Hum Mol Genet. 2015;24:1390–1399. doi: 10.1093/hmg/ddu553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.del Bosque-Plata L., Martínez-Martínez E., Espinoza-Camacho M.Á., Gragnoli C. The role of TCF7L2 in type 2 diabetes. Diabetes. 2021;70:1220–1228. doi: 10.2337/db20-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Younus A.H., Al-Faisal A.H.M. Assessment of HNF4A gene expression as a potential biomarker for T2DM predicting and its correlation with biochemical parameters in Iraqi population. Iraqi J Biotechnol. 2023;22:229–237. [Google Scholar]
- 16.Shahram B., Hassan B., Mahlagha Z. Effect of low serum triglyceride on LDL-cholesterol estimation by friedewald formula. Rev Latinoam Hipertens. 2020;15:21–25. [Google Scholar]
- 17.Aljoubory H.M., Altaee M.F. Correlation study between three different genes expression and chronic myeloid leukemia in Iraq. Iraqi J Agric Sci. 2021;52 [Google Scholar]
- 18.Wu D., Ding J., Wang L., Pan H., Zhou Z., Zhou J., et al. microRNA-125b inhibits cell migration and invasion by targeting matrix metallopeptidase 13 in bladder cancer. Oncol Lett. 2013;5:829–834. doi: 10.3892/ol.2013.1123. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2− ΔΔCT method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 20.Jawad R.S., Younus A.H., Abbas H.H., Shihab A., Jawad A.R., Al Muski N. Disinfection of drinking water from Escherichia coli and Pseudomonas aeruginosa by using silver nanoparticles. Mater Sci Forum. 2020;1002:478–488. doi: 10.4028/www.scientific.net/MSF.1002.478. [DOI] [Google Scholar]
- 21.Bays H.E., Chapman R.H., Grandy S., Group S.I. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. Int J Clin Pract. 2007;61:737–747. doi: 10.1111/j.1742-1241.2007.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sabri S.A., Ibraheem S.R. Comparing the disease severity in Iraqi psoriasis patients according to some immunological and biological factors. Iraqi J Sci. 2023:2774–2785. [Google Scholar]
- 23.Hameed E.K., Al-Ameri L.T., Hasan H.S., Abdulqahar Z.H. The cut-off values of triglycerides-glucose index for metabolic syndrome associated with type 2 diabetes mellitus. Baghdad Sci J. 2022;19:340. [Google Scholar]
- 24.Zhang F.-L., Ren J.-X., Zhang P., Jin H., Qu Y., Yu Y., et al. Strong Association of waist circumference (WC), body mass index (BMI), waist-to-height ratio (WHtR), and waist-to-hip ratio (WHR) with diabetes: a population-based cross-sectional study in Jilin province, China. J Diabetes Res. 2021;2021 doi: 10.1155/2021/8812431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klisic A., Kavaric N., Jovanovic M., Zvrko E., Skerovic V., Scepanovic A., et al. Association between unfavorable lipid profile and glycemic control in patients with type 2 diabetes mellitus. J Res Med Sci Off J Isfahan Univ Med Sci. 2017;22 doi: 10.4103/jrms.JRMS_284_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kowsar R., Mansouri A. Multi-level analysis reveals the association between diabetes, body mass index, and HbA1c in an Iraqi population. Sci Rep. 2022;12 doi: 10.1038/s41598-022-25813-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alkabi H.R., Alfatlawi W.R., Aldabagh M.A.H. Impact of vitamin D elements and osteoporosis factors in postmenopausal Iraqi Women with T2DM. J Appl Sci Nanotechnol. 2022;2:137–146. [Google Scholar]
- 28.Alzahrani S.H., Baig M., Aashi M.M., Al-Shaibi F.K., Alqarni D.A., Bakhamees W.H. Association between glycated hemoglobin (HbA1c) and the lipid profile in patients with type 2 diabetes mellitus at a tertiary care hospital: a retrospective study. Diabetes. Metab Syndr Obes targets Ther. 2019:1639–1644. doi: 10.2147/DMSO.S222271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mishra B.K., Velmurugan M., Gambhir J.K., Madhu S.V. Postprandial lipemia and its relation to TCF7L2 gene polymorphisms in normoglycemic first-degree relatives of type 2 diabetes patients. Int J Diabetes Dev Ctries. 2019;39:268–272. [Google Scholar]
- 30.Lyssenko V., Lupi R., Marchetti P., Del Guerra S., Orho-Melander M., Almgren P., et al. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest. 2007;117:2155–2163. doi: 10.1172/JCI30706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Verma A.K., Beg M.M.A., Saleem M., Al Reshidi F., Ahmad H., Alenazi F., et al. Cell free TCF7L2 gene alteration and their association with Type 2 diabetes mellitus in North Indian population. Meta Gene. 2020;25 [Google Scholar]
- 32.Ip W., Chiang Y.A., Jin T. The involvement of the wnt signaling pathway and TCF7L2 in diabetes mellitus: the current understanding, dispute, and perspective. Cell Biosci. 2012;2:1–12. doi: 10.1186/2045-3701-2-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah M., Varghese R.T., Miles J.M., Piccinini F., Dalla Man C., Cobelli C., et al. TCF7L2 genotype and α-cell function in humans without diabetes. Diabetes. 2016;65:371–380. doi: 10.2337/db15-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kovacs P., Berndt J., Ruschke K., Klöting N., Schön M.R., Körner A., et al. TCF7L2 gene expression in human visceral and subcutaneous adipose tissue is differentially regulated but not associated with type 2 diabetes mellitus. Metabolism. 2008;57:1227–1231. doi: 10.1016/j.metabol.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 35.Shu L., Matveyenko A.V., Kerr-Conte J., Cho J.-H., McIntosh C.H.S., Maedler K. Decreased TCF7L2 protein levels in type 2 diabetes mellitus correlate with downregulation of GIP- and GLP-1 receptors and impaired beta-cell function. Hum Mol Genet. 2009;18:2388–2399. doi: 10.1093/hmg/ddp178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scheuner D., Song B., McEwen E., Liu C., Laybutt R., Gillespie P., et al. Translational control is required for the unfolded protein response and in vivo glucose homeostasis. Mol Cell. 2001;7:1165–1176. doi: 10.1016/s1097-2765(01)00265-9. [DOI] [PubMed] [Google Scholar]
- 37.Aguayo-Mazzucato C. Functional changes in beta cells during aging and senescence. Diabetologia. 2020;63:2022–2029. doi: 10.1007/s00125-020-05185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ihm S.-H., Matsumoto I., Sawada T., Nakano M., Zhang H.J., Ansite J.D., et al. Effect of donor age on function of isolated human islets. Diabetes. 2006;55:1361–1368. doi: 10.2337/db05-1333. [DOI] [PubMed] [Google Scholar]