Abstract
Achromobacter xylosoxidans is a Gram-negative, aerobic, non-fermenting bacillus mainly responsible for nosocomial infections. We report the first case of community-acquired spondylodiscitis caused by Achromobacter xylosoxidans in a 61-year-old woman, immunocompromised with necrotizing dermohypodermitis of the right lower limb successfully treated with ertapenem and ciprofloxacin.
Keywords: Spondylodiscitis, Necrotizing dermohypodermatitis, Alcaligenes xylosoxidans, Achromobacter xylosoxidans
Introduction
Achromobacter xylosoxidans is a Gram-negative, aerobic, non-fermenting bacillus of aquatic reservoir, mainly found in nosocomial cases. Here we report the first case, to our knowledge, of community-acquired spondylodiscitis caused by Achromobacter xylosoxidans.
Case presentation
This is a case of a 61-year-old woman with type II diabetes and a history of right renal adenocarcinoma that was treated surgically by nephrectomy. Afterward, she developed a single- kidney chronic glomerular nephropathy that was treated by renal transplantation since 10 years. She presented with an acute red leg in the context of ulcers of the anterior tibia that had been evolving for a month. A diagnosis of non-necrotizing dermohypodermatitis of the right lower limb was made, for which antibiotic therapy with oral clindamycin was started.
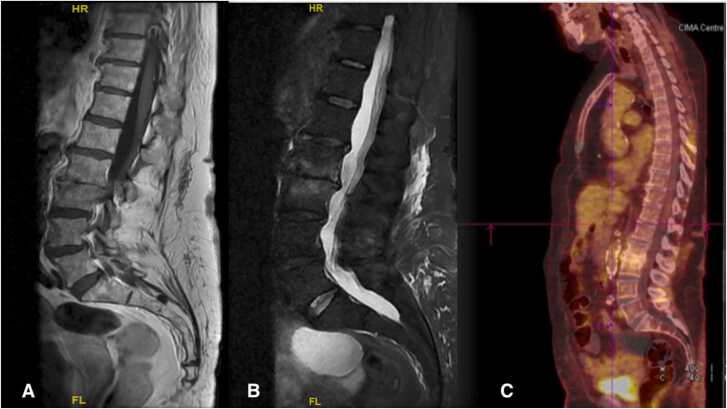
Shortly after a rapid deterioration was observed with the appearance of purpurics and necrotics areas and bullous on the anterior aspect of the right leg and the posterior aspect of the right foot (Fig. 1), leading to the diagnosis of necrotizing dermohypodermatitis of the right leg. Antibiotic therapy was extended with intravenous piperacilin-tazobactam and oral clindamycin, combined with surgical debridement. Bacterial culture from the surgical debridement and peripheral blood cultures were positive for Achromobacter xylosoxidans subsp xylosoxidans. Postoperative course was marked by the onset of inflammatory lumbar pain a week after, raising suspicions of infectious spondylodiscitis. This diagnosis was confirmed by an MRI scan of the dorsolumbar spine, showing an edema of the L2-L3 vertebral endplates associated with inflammatory infiltration of the right and left anterior and lateral paravertebral soft tissues at L2-L3 and an anterior epiduritis of L3-L4 (Fig. 2).
Fig. 1.
Necrotizing dermohypodermatitis before medical and surgical management.
Fig. 2.
A: sagittal section of initial MRI in T1 sequence injected with gadolinium; B: sagittal section of control MRI in T2 STIR sequence; C: sagittal section of control PET scan.
No signs of infective endocarditis were found on two trans-thoracic cardiac ultrasounds performed seven days apart. After obtaining an antibiogram and establishing MICs, and in view of the osteoarticular involvement, antibiotic therapy was continued with intravenous piperacillin-tazobactam released on Midline and oral ciprofloxacin, and a vertebral brace was put in place in the context of epiduritis and spinal instability.
Midline thrombosis was subsequently diagnosed. Given the low venous capital and the presence of a contralateral arteriovenous fistula, IV antibiotic therapy was replaced by subcutaneous ertapenem in combination with ciprofloxacin for a total of 12 weeks. The course was subsequently satisfying, with disappearance of pain and no recurrence of signs of inflammation. When the antibiotic treatment was stopped, the PET-scanner showed erosive lesions on the L2 and L3 plateaus, which appeared to be sequelae of the spondylodiscitis, as did the follow-up MRI (Fig. 2). One year follow-up had showed no relapse.
Discussion/ literature review
Achromobacter xylosoxidans is a Gram-negative, aerobic, non-fermenting bacillus [1] mainly from aquatic reservoirs, as hospitals [2]. A. xylosoxidans was first isolated in 1971 by Yabuuchi and Oyama [3] from chronic otitis media in seven patients.
It is an opportunistic bacterium that is mainly implicated in nosocomial infections, most often in immunocompromised patients, those suffering from haematological or solid neoplasia, and patients who have received antibiotic therapy in the month prior to infection [4] but can also occur in the community more rarely.
The most frequent clinical presentation is bacteremia [5] linked to the use of catheters, most often [6] or pneumopathy [7] depending on the study. More rarely, other sites may be involved: meningitis [8], colonization in cystic fibrosis [9], osteomyelitis [10], chronic otitis media [3], endocarditis on prosthetic valves [11], skin and soft tissue infections [12].
In this case report, we present the first community-acquired case to our knowledge of spondylodiscitis following dermohypodermatitis complicated by Achromobacter xylosoxidans subsp. xylosoxidans bacteremia. The patient was immunocompromised following renal transplantation and taking immunosuppressants. She was also a type 2 diabetic, which corresponds to the population most commonly affected by this germ.
A case of L5-S1 discitis following treatment of a herniated disc with oxygen-ozone has been described [13], which therefore corresponds to a nosocomial case following an interventional radiology procedure.
Closer to our case, a case of discitis caused by community-acquired Achromobacter xylosoxidans subsp. denitrificans has been described, treated with an intravenous combination of ampicillin and sulbactam with oral sulfamethoxazole and trimethoprim for six weeks, followed by six weeks of treatment with oral sulfamethoxazole and trimethoprim alone [14]. In addition, a case of spondylodiscitis caused by A. xylosoxidans has been reported, but it is not known whether this was a community-acquired or nosocomial case, or how it was managed [15].
The particularity of our case is the association of necrotizing dermohypodermatitis caused by A. xylosoxidans, a described but rare entity, with bacteremia caused by A. xylosoxidans subsp. xylosoxidans and spondylodiscitis caused by A. xylosoxidans subsp. xylosoxidans, an entity which has never been described in a community patient. Although the germ was not identified on bone biopsy because there was no indication for it, there was little doubt that A. xylosoxidans was involved after it was identified on intraoperative samples and on postoperative peripheral blood cultures taken at the same time as the onset of lumbar pain.
Treatment of A. xylosoxidans is not codified, as there are numerous natural and acquired resistance mechanisms. Around 40% of the germs isolated in the study by Pérez Barragan et al. [4] and 16% in the study by Marion-Sanchez et al. are multi-resistant germs [7]. It is generally sensitive to trimethoprim-sulfamethoxazole, anti-pseudomonal penicillins and carbapenems [4].
Conversely, it is naturally resistant to third-generation cephalosporins, aztreonam, aminoglycosides and ofloxacin. Moreover, recently, acquired resistance to ciprofloxacin has become common, and even to carbapenems, but very rarely to piperacillin-tazobactam [16].
The resistance mechanisms of A. xylosoxidans are based mainly on a constitutive oxacillinase, numerous beta-lactamases and, above all, on RND (resistant-nodulation-cell division) efflux pumps which are active against numerous molecules [17].
As regards the choice of antibiotic treatment, we were faced with the problem of the patient's chronic renal failure, which contraindicated the use of trimethoprim- sulfamethoxazole, which is classically active against this germ. Initially, piperacillin-tazobactam was introduced in dual therapy with ciprofloxacin, which showed in-vitro sensitivity in our case, which is unusual. However, given the difficulty of venous access, the in vitro activity of ertapenem, which is not classically used for this germ, was tested and showed that the germ was sensitive enough to be followed up subcutaneously with ertapenem. Progression at 3 months and then at one year was satisfying, with good tolerance of antibiotic therapy.
Conclusion
Achromobacter xylosoxidans is mainly responsible for nosocomial infections such as bacteremia and pneumonia in immunocompromised patients, although other rarer localizations have been described. Here we report the first case of Achromobacter xylosoxidans subsp. xylosoxidans community-acquired spondylodiscitis in a type II diabetic renal transplant patient.
Ethical approval statement
Not applicable.
Ethics statement
The patient described in this manuscript has given her informed consent for participation in the study and the use of her de-identified, anonymized, aggregated data and her case details (including photographs) for publication.
CRediT authorship contribution statement
T. Brochet: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. M. Tonnelier: Visualization, Validation, Conceptualization. E. Justinien: Visualization, Validation, Supervision. A.-L. Lecapitaine: Visualization, Validation, Supervision. A. Bouras: Supervision, Investigation, Conceptualization.
Conflict of interest statement
The authors declare no relevant conflict of interest.
Data availability statement
Data available on request from the authors.
References
- 1.Duggan J.M., Goldstein S.J., Chenoweth C.E., Kauffman C.A., Bradley S.F. Achromobacter xylosoxidans bacteremia: report of four cases and review of the literature. Clin Infect Dis. 1996;23:569–576. doi: 10.1093/clinids/23.3.569. PMID: 8879782. [DOI] [PubMed] [Google Scholar]
- 2.Marion-Sanchez K., Olive C., Platon M.G., Cesarine M., Derancourt C., Pailla K. Achromobacter xylosoxidans in hospital environments: still waters run deep. Trans R Soc Trop Med Hyg. 2020;114(6):470–472. doi: 10.1093/trstmh/trz109. PMID: 31836888. [DOI] [PubMed] [Google Scholar]
- 3.Yabuuchi E., Ohyama A. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol. 1971;15:477–481. doi: 10.1111/j.1348-0421.1971.tb00607.x. PMID: 5316576. [DOI] [PubMed] [Google Scholar]
- 4.Pérez Barragán E., Sandino Pérez J., Corbella L., Orellana M.A., Fernández-Ruiz M. Achromobacter xylosoxidans bacteremia: clinical and microbiological features in a 10-year case series. Rev Esp Quim. 2018;31(3):268–273. PMID: 29806765. [PMC free article] [PubMed] [Google Scholar]
- 5.Aisenberg G., Rolston K.V., Safdar A. Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer (1989-2003) Cancer. 2004;101(9):2134–2140. doi: 10.1002/cncr.20604. PMID: 15389476. [DOI] [PubMed] [Google Scholar]
- 6.Gómez-Cerezo J., Suárez I., Ríos J.J., Peña P., García de Miguel M.J., de José M., et al. Achromobacter xylosoxidans bacteremia: a 10-year analysis of 54 cases. Eur J Clin Microbiol Infect Dis. 2003;22:360–363. doi: 10.1007/s10096-003-0925-3. [DOI] [PubMed] [Google Scholar]
- 7.Marion-Sanchez K., Pailla K., Olive C., Le Coutour X., Derancourt C. Achromobacter spp. healthcare associated infections in the French West Indies: a longitudinal study from 2006 to 2016. BMC Infect Dis. 2019;19(1):795. doi: 10.1186/s12879-019-4431-3. PMID: 31500579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellissimo F., Pinzone M.R., Tosto S., Nunnari G., Cacopardo B. Achromobacter xylosoxidans meningitis in an immunosuppressed patient. QJM. 2014;107(1):65–66. doi: 10.1093/qjmed/hct170. PMID: 23970185. [DOI] [PubMed] [Google Scholar]
- 9.Cools P., Ho E., Vranckx K., Schelstraete P., Wurth B., Franckx H., et al. Epidemic Achromobacter xylosoxidans strain among Belgian cystic fibrosis patients and review of literature. BMC Microbiol. 2016;16(1):122. doi: 10.1186/s12866-016-0736-1. PMID: 27342812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pamuk G., Aygun D., Barut K., Kasapcopur O. Achromobacter causing a thrombophlebitis and osteomyelitis combination: a rare cause. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-210718. bcr2015210718. PMID: 26347234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawant A.C., Srivatsa S.S., Castro L.J. Alcaligenes xylosoxidans endocarditis of a prosthetic valve and pacemaker in a 62-year-old woman. Tex Heart Inst J. 2013;40(1):95–98. [PMC free article] [PubMed] [Google Scholar]
- 12.Tena D., Martínez N.M., Losa C., Solís S. Skin and soft tissue infection caused by Achromobacter xylosoxidans: report of 14 cases. Scand J Infect Dis. 2014;46(2):130–135. doi: 10.3109/00365548.2013.857043. PMID: 24325336. [DOI] [PubMed] [Google Scholar]
- 13.Fort N.M., Aichmair A., Miller A.O., Girardi F.P. L5-S1 Achromobacter xylosoxidans infection secondary to oxygen-ozone therapy for the treatment of lumbosacral disc herniation: a case report and review of the literature. Spine. 2014;39(6):E413–E416. doi: 10.1097/BRS.0000000000000195. PMID: 24384664. [DOI] [PubMed] [Google Scholar]
- 14.Shaikh H., Kishen T.J. Achromobacter spondylodiscitis. A case report and review of literature. Indian Spine J. 2018:144–147. [Google Scholar]
- 15.Navarro-Navarro R., Suárez-Cabañas A.H., Fernández-Varela T., Lorenzo-Rivero J.A., Montesdeoca-Ara A. Analysis of results of open and percutaneous disc biopsy in the diagnosis of spondylodiscitis. Rev Esp Cir Ortop Trauma. 2022;66(3):189–199. doi: 10.1016/j.recot.2021.09.005. PMID: 35590436. [DOI] [PubMed] [Google Scholar]
- 16.Amoureux L., Bador J., Siebor E., Taillefumier N., Fanton A., Neuwirth C. Epidemiology and resistance of Achromobacter xylosoxidans from cystic fibrosis patients in Dijon, Burgundy: first French data. J Cyst Fibros. 2013;12(2):170–176. doi: 10.1016/j.jcf.2012.08.005. PMID: 22944724. [DOI] [PubMed] [Google Scholar]
- 17.Bador J., Amoureux L., Duez J.M., Drabowicz A., Siebor E., Llanes C., Neuwirth C. First description of an RND-type multidrug efflux pump in Achromobacter xylosoxidans, AxyABM. Antimicrob Agents Chemother. 2011;55(10):4912–4914. doi: 10.1128/AAC.00341-11. PMID: 21807978. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.