Abstract
Background
Anxiety and depression affect many people. Treatments do not have complete success and often require people to take drugs for long periods of time. Many people look for other treatments that may help. One of those is Reiki, a 2500 year old treatment described as a vibrational or subtle energy therapy, and is most commonly facilitated by light touch on or above the body. There have been reports of Reiki alleviating anxiety and depression, but no specific systematic review.
Objectives
To assess the effectiveness of Reiki for treating anxiety and depression in people aged 16 and over.
Search methods
Search of the Cochrane Register of Controlled Trials (CENTRAL ‐ all years), the Cochrane Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR ‐ all years), EMBASE, (1974 to November 2014), MEDLINE (1950 to November 2014), PsycINFO (1967 to November 2014) and AMED (1985 to November 2014). Additional searches were carried out on the World Health Organization Trials Portal (ICTRP) together with ClinicalTrials.gov to identify any ongoing or unpublished studies. All searches were up to date as of 4 November 2014.
Selection criteria
Randomised trials in adults with anxiety or depression or both, with at least one arm treated with Reiki delivered by a trained Reiki practitioner.
Data collection and analysis
The two authors independently decided on inclusion/exclusion of studies and extracted data. A prior analysis plan had been specified but was not needed as the data were too sparse.
Main results
We found three studies for inclusion in the review. One recruited males with a biopsy‐proven diagnosis of non‐metastatic prostate cancer who were not receiving chemotherapy and had elected to receive external‐beam radiation therapy; the second study recruited community‐living participants who were aged 55 years and older; the third study recruited university students.
These studies included subgroups with anxiety and depression as defined by symptom scores and provided data separately for those subgroups. As this included only 25 people with anxiety and 17 with depression and 20 more with either anxiety or depression, but which was not specified, the results could only be reported narratively. They show no evidence that Reiki is either beneficial or harmful in this population. The risk of bias for the included studies was generally rated as unclear or high for most domains, which reduces the certainty of the evidence.
Authors' conclusions
There is insufficient evidence to say whether or not Reiki is useful for people over 16 years of age with anxiety or depression or both.
Keywords: Adult, Female, Humans, Male, Middle Aged, Anxiety, Anxiety/therapy, Depression, Depression/therapy, Prostatic Neoplasms, Prostatic Neoplasms/psychology, Randomized Controlled Trials as Topic, Therapeutic Touch, Therapeutic Touch/methods
Plain language summary
Reiki for the treatment of anxiety and depression
Review Question
This review summarises the evidence from randomised controlled trials that test whether Reiki if beneficial for people with anxiety or depression.
Background
Reiki is a non‐drug treatment that is used on people with anxiety, depression or both. Reiki is a 2500 year old treatment, described as a vibrational or subtle energy therapy and is most commonly facilitated by light touch on or above the body. But there is no systematic review of randomised trials evaluating whether it works in this group of people.
Study characteristics
We found three studies for inclusion in the review. One recruited males with a biopsy‐proven diagnosis of prostate cancer who were not receiving chemotherapy and had elected to receive external‐beam radiation therapy; the second study recruited community‐living participants who were aged 55 years and older; the third study recruited university students.These studies included people with anxiety or depression or both, and reported their results separately. This included only 25 people with anxiety, 17 with depression and 20 more with either anxiety or depression but which was not specified. The search is up to date as of 4 November 2014.
Key results
Very few people with anxiety or depression or both have been included in randomised studies. This means there is insufficient evidence to make any comment about the usefulness of Reiki for the treatment of anxiety and depression.
Quality of the evidence
At best, the quality of the evidence is moderate which, on top of a dearth of evidence, weakens the findings further.
Background
Description of the condition
Anxiety and depression are highly prevalent disorders and are often comorbid with each other. The Burden of Disease Project reported that mental disorders account for 9.1% of the global burden of disease in the world, almost one‐half of which is accounted for by anxiety and depressive disorders (Andrews 1998).
Anxiety is a natural response and a necessary warning adaptation in humans. However, anxiety can become a pathologic disorder when it is excessive and uncontrollable, requires no specific external stimulus, and manifests with a wide range of physical and affective symptoms as well as changes in behaviour and cognition (Rowney 2014). Anxiety disorders include generalised anxiety disorder (GAD), social anxiety disorder (also known as social phobia), specific phobia, panic disorder with and without agoraphobia, obsessive‐compulsive disorder (OCD), post‐traumatic stress disorder (PTSD), anxiety secondary to medical condition, acute stress disorder (ASD), and substance‐induced anxiety disorder, as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV) (APA 1994). In a community sample, the one‐year prevalence for GAD was approximately 3%, with a lifetime prevalence of 5% (APA 2000; APA 1994). For acute anxiety disorder, prevalence ranged from 14% to 33% in individuals exposed to severe trauma (APA 2000; APA 1994). Community‐based studies suggest a lifetime prevalence for PTSD of 8% of the USA adult population (APA 2000; APA 1994). As these definitions are redefined occasionally future versions of this review will use the most recent definitions.
Depressive disorders include major depressive disorder, major depressive episode, depressive disorders not otherwise specified and dysthymic disorder, as defined by DSM‐IV. According to DSM‐IV the lifetime prevalence for dysthymic disorder is six per cent. The point prevalence of major depressive disorder in a community sample of adults has been estimated at 5% to 9% for women and from 2% to 3% for men (APA 2000; APA 1994).
Description of the intervention
The most frequently used treatments for anxiety and depressive disorders include antidepressant and anti‐anxiety medications; however these can be unpopular with people, due to side effects and the dislike of taking long‐term medication. For example, from a systematic review of randomised controlled trials (RCTs) 36.9% of people treated for anxiety with the second‐generation antipsychotic drug quetiapine withdrew during the studies (Depping 2010); and 33.9% of people with depression withdrew due to side effects from treatment for depression (Arroll 2009). Psychological therapies may also be used as treatments for anxiety and depression and these are preferred over drugs (Prins 2008); however, a lack of trained practitioners and funding mean that many people explore self‐help options.
There is interest from the community in the use of self help and complementary therapies for anxiety and depression. A study in the US found that 20% of people with anxiety, and 19% with depression visited a complementary or alternative therapy provider (Kessler 2001), with 2.8% and 5.4% choosing 'energy therapy'.
'Energy therapies' are based on the belief in a universal flow of healing energy that flows around and through all living beings (Trepper 2013). Many ancient cultures have a name for this universal flow, for example: 'Prana' in India, 'Chi' in China, 'Ruarch' for Hebrews, 'Mana' in Hawaii and 'Wairua' for the Aotearoa New Zealand Maori people.
One of the complementary 'energy therapies' is the Japanese healing art of Reiki. In the Japanese language ‘rei’ means universal and ‘kei’ means life energy. A number of hospitals are now offering Reiki alongside other complementary therapies for management of pain and post‐operative depression. A website article by prominent Reiki writer William Rand gives examples of the use of Reiki in American hospitals (Rand 2014).
Reiki is a 2500 year old system of healing that was rediscovered by Dr Mikao Usui, in early 1900s Japan. He passed on his teachings to Dr Chujiro Hayashi, who opened the first Reiki clinic in Japan and standardised the hand placements of what is now known as the Usui system of Reiki. In his turn he trained the Japanese‐American woman, Mrs Hawayo Takata, who established the first Reiki clinic in the US in 1970 (Trepper 2013).
Reiki is based upon a holistic view of promoting whole‐person (mind‐body) health (Yeh 2004), and shares similar principles to the World Health Organization's (WHO) definition of health, namely, 'Health is a state of complete physical, mental and social well‐being and not merely the absence of disease or infirmity' (http://www.who.int/about/en/).
Reiki is described as a vibrational or subtle energy therapy most commonly facilitated by light touch on or above the body (Lubeck 2001; Rubik 2002). Practitioners describe it as a gentle, sequential treatment, which appears to be safe, comforting and relaxing. Reiki training involves several levels including 1, 2, 3 and 3A. Level 1 is generally for self‐help or for treating family members only. Dr Usui is credited with describing the symbols and attunement processes involved in becoming a practitioner. According to Reiki spiritual masters, Reiki attunement opens and expands the ki‐holding capacity of the practitioner (Lubeck 2001). Spiritual attunement is an advanced spiritual practice, which involves the transmission of energy from the teacher to the student (Trepper 2013). Those that have received such attunements describe powerful experiences of love and peace alongside emotional and physical reactions (Lubeck 2001).
The traditional Usui Reiki treatment, which is utilised in the studies, ranges from 45 to 90 minutes and usually involves placing the hands on 12 positions in total, on the head and on the front and back of the torso. Symbols may only be used during a treatment when a practitioner reaches level 2 and above. An understanding of the significance of using the symbols during a treatment can help to consolidate the benefits of the treatment. The symbols are usually drawn onto the practitioner's palm by the palm of the other hand. These symbols are said to enhance the quality of the energy transmitted to the physical, emotional, mental and spiritual levels of the person receiving the treatment (Nield‐Anderson 2000).
It is the attunement process that differentiates Reiki from other forms of energy therapies (Trepper 2013).
Miles 2003 studied the effect of Reiki on HIV‐related pain and anxiety. There was a significant reduction in both self‐reported pain and anxiety following a 20‐minute Reiki session. There was no significant difference between self administration of Reiki and administration by another person. Olsen 2003 conducted a trial to assess the effects of two treatment conditions on pain, quality of life and analgesic use in 24 cancer patients. One group received standard opioid treatment and rest, while the other group received standard opioid treatment and Reiki. No overall reduction in analgesic use was noted for either group. However, the Reiki group experienced improved pain control and quality of life scores, compared to the rest group. All studies reviewed used small samples ranging from 14 to 45 participants.
How the intervention might work
The putative mechanism of action for Reiki is said to be the transfer of energy by the Reiki practitioner acting as a channel for the energy to transfer to the client (Nield‐Anderson 2000). Some modern authors have suggested a bio‐field hypothesis that is similar to ancient yogic theory (Chaoul 2010; Feuerstein 2002; Kumar 2008). Ancient yogic theory views the body as having a field of energy around and within it, that is said to be responsive to various forms of healing touch (Hossi 2006; Kumar 2003; Rein 2004; Rubik 2002). This finds some similarities to the thoughts relating to the nature of the universe and consciousness that is emerging from the work in the field of quantum and particle physics (Bohm 1994; Capra 2000; Carrol 2012). However, in the medical literature the existence of such a biofield is refuted by some authors, particularly following the experiment which showed that under rigorous test conditions therapeutic touch practitioners were unable to sense a biofield (Rosa 1998). The study was conducted from a Western theoretical approach which may have been misleading and whilst this was a blinded and well‐designed experiment there was little acknowledgement or understanding of the subtle nature of the phenomena being studied. It is claimed that an Eastern theoretical framework may have elicited information that reconciled the laboratory findings with the lived, reported experience of real‐life human beings (Ho 2007; Sedlmeier 2012). Ancient traditions define the universal life force as a subtle energy that is not perceivable by the sense organs (Bahadur 1978; Dasgupta 1989). Some claim that it may be useful to consider that when practitioners state that they ‘see or feel the field’ they may instead be describing in a clumsy way the subtle experience of consciousness that develops specifically when one engages through the intent of love (Feuerstein 2002). There appears to be a paucity of words within the English language and culture to describe these particular states; although cultures with deeper traditions and study of these states have many terms available. For example, the ancient Sanskrit language has many terms that describe advanced spiritual conditions and stages in a precise manner (Dasgupta 1989). Most spiritual traditions state that as a human being spiritually refines there develop various states of consciousness that are currently indescribable with words (Chandra 1991). Often when a human being refines in this way, the capacities underlying energy therapies begin to show; however these states are often not stable and are subject to change and affected by thought (Dasgupta 1989). If this is the case then it is possible that Western laboratory test conditions may not be suitable for the study of the phenomena in question.
Within the literature many researchers have hypothesised that a generalised relaxation response may explain any Reiki treatment effect (Mackay 2004; Wardell 2001). There is some evidence that Reiki has an effect on depression and anxiety. Shore 2004 found Reiki resulted in significant reductions in depressive and stress symptoms when compared to controls. These findings were maintained at a one‐year follow‐up. Wardell 2001 explored the biological correlates of a single 30‐minute session of Reiki: results showed that anxiety was significantly reduced (as measured by Spielberger's State‐Trait Anxiety Inventory (STAI)) (Spielberger 1983), salivary immunoglobulin A levels rose significantly, and there was a significant reduction in systolic blood pressure. Salivary cortisol, skin temperature and electromyography (EMG) changes were not statistically significant. Bowden 2011 found that the participants (university students) with high anxiety or depression or both who received Reiki showed a progressive improvement in overall mood, which was significantly better at five‐week follow‐up, while no change was seen in the controls. While the Reiki group did not demonstrate the comparatively greater reduction in symptoms of illness seen in the earlier study (Bowden 2010), the findings of both studies suggested that Reiki may benefit mood.
Why it is important to do this review
Reiki appears to enjoy popular support by the public (Barnes 2007); and in some cases hospitals are beginning to include this therapy in treatment plans (Berger 2013). It is a therapy that intrigues and has aroused interest but in fairness little is known about its effects and possible health benefits despite several systematic reviews that included a wide range of different populations (Baldwin 2010; Jain 2010; Lee 2008; vanderVaart 2009; Vitale 2007). Jain 2010 found, in part, that "Biofield therapies show strong evidence for reducing pain intensity in pain populations, and moderate evidence for reducing pain intensity in hospitalised and cancer populations. There is moderate evidence for decreasing negative behavioral symptoms in dementia and moderate evidence for decreasing anxiety for hospitalized populations" but this was based not only on RCTs and in small, moderate‐quality studies. In contrast vanderVaart 2009 concluded: "The serious methodological and reporting limitations of limited existing Reiki studies preclude a definitive conclusion on its effectiveness". Lee 2008 concluded from RCTs in a variety of populations: "the evidence is insufficient to suggest that Reiki is an effective treatment for any condition"; and Vitale 2007 questions whether RCTs are the correct way to evaluate Reiki. Baldwin 2010 finds only a few studies with mixed findings and concludes that further good quality studies are required. Given the paucity of evidence based upon a few small studies, there is a place for a regularly updated systematic review of Reiki treatment for anxiety and depression.
Objectives
To assess the effectiveness of Reiki for treating anxiety and depression in people aged 16 and over.
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised controlled trials (where group allocation is by alternation, day of the week etc), published or unpublished.
Types of participants
Participant characteristics
Trial participants were both males and females, aged 16 or more, suffering from anxiety or depressive disorders, as defined by the study authors.
Diagnosis
Participants were to be diagnosed with anxiety or depression according to DSM‐III (APA 1980), DSM‐IV (APA 1994), ICD‐9 (WHO 1978) and ICD‐10 (WHO 1992); or identified through use of symptomology scales (such as Beck 1961, Hamilton 1960 or Spielberger 1983 scales, for example).
Comorbidities
Comorbid anxiety and depression was allowed as well as other comorbidities.
Setting
No restrictions were placed on setting.
Subset data
Reiki is sometimes used on people whose primary diagnosis is something that would naturally be regarded as something that would make them anxious (such as cancer). RCTs on such populations may only have a subgroup of participants that are clinically anxious or depressed. If only a subgroup of participants met the inclusion criteria and the results for this subgroup were reported separately or these data were supplied by the authors then the study was included, but only the subgroup data were used.
Types of interventions
Experimental intervention
Any type of Reiki, performed by a trained Usui‐initiated Reiki practitioner was allowed. This is a person who has completed courses and been initiated to Reiki one, Reiki two, and Reiki three (and above) levels of Reiki (McKenzie 1998). Treatment was with hands on or off the body or a combination of these. The Reiki practitioners had treatment fidelity: i.e., the Reiki practitioner needs to adhere to Reiki only, as many Reiki practitioners have had training in a range of energy therapies.
Comparator interventions
No intervention or placebo Reiki (e.g., relaxation exercises)
Sham Reiki (person not attuned or initiated to Reiki placing hands on body mimicking a Reiki session)
Standard care/treatment as usual
Wait list
Pharmacological treatments (e.g., antidepressants, anti‐anxiety medication)
Herbal medicine
Psychological therapies (e.g., cognitive behaviour therapy, psychodynamic therapy, interpersonal therapy, supportive therapy)
Exercise therapy
Any other intervention
Excluded interventions
There are several other treatments with similarities to Reiki. Therapeutic touch is a touch therapy that differs from Reiki, as it does not have an attunement process and practitioners work with conscious intent, assessing the client whilst their hands are usually, although not always, above the physical body (Potter 2003; Robinson 2007). Healing touch is a nursing technique which also uses touch and intention to create changes in the biofield. It includes placement of the hands in specific sequences on the body and use of healing intent (Wardell 2004).
There was no intention to exclude participants who were on other treatments for anxiety and depressive disorders or who started them during the course of the trial.
Types of outcome measures
Primary outcomes
The primary outcome measure in this review is the relief of symptoms, usually measured using rating scales. Depression is measured using self‐rating scales such as the Beck Depression Inventory (BDI) (Beck 1961); or clinician‐rated scales, such as the Hamilton Rating Scale for Depression (HRSD) (Hamilton 1960). Anxiety is measured using a self‐rating scale such as the Spielberger State‐Trait Anxiety Inventory (STAI) (Spielberger 1983).
The primary adverse event outcome is the acceptability of the treatments, measured by the dropout rates.
Secondary outcomes
3. Quality of life measures, such as the SF12 or SF36 (Ware 1993)
4. Self‐perceived stress, measured using self‐report measures such as: sleep improvements, reduced feelings of being overwhelmed or reduced tension/worry
5. Side effects of the Reiki treatment
Search methods for identification of studies
Electronic searches
CCDAN's Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK: a references register and a studies‐based register. The CCDANCTR‐References Register contains over 37,500 reports of randomised controlled trials in depression, anxiety and neurosis. Approximately 60% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Coordinator for further details.
Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950 to date), EMBASE (1974 to date) and PsycINFO (1967 to date); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); and review‐specific searches of additional databases. Reports of trials are also sourced from international trials registers via the World Health Organization’s (WHO) Trials Portal (ICTRP), drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies can be found on the Group‘s web site.
The CCDANCTR was searched using the following terms:
CCDANCTR Studies Intervention = Reiki or "Energy Heal*" or "Energy Channel*"
CCDANCTR References Free‐text = Reiki or "Energy Heal*" or "Energy Channel*"
Complementary searches were carried out on CENTRAL, MEDLINE, EMBASE, PsycINFO and AMED to ensure no study had been missed (Appendix 1).
Additional searches were carried out on the WHO Trials Portal (ICTRP) and ClinicalTrials.gov to identify ongoing or unpublished studies.
All searches were up to date as of 4 November 2014.
Searching other resources
Reference lists
The reference lists of all identified papers were searched for further information.
Personal communication
We contacted authors and experts in the field to see whether they knew of any unpublished studies.
Data collection and analysis
Selection of studies
Reports of all potentially eligible studies were independently evaluated for appropriateness for inclusion by the two authors prior to consideration of the results. Any disagreements were resolved by discussion. Excluded studies were listed with reasons for their exclusion.
Data extraction and management
Data extraction was undertaken independently by the two review authors using a form modified for this review. Data extracted were entered into an MS‐Word document and included details of the study, inclusion and exclusion criteria, elements of risk of bias, data on participants at baseline and any outcomes with the corresponding data.
Main comparisons that were to be examined
Reiki versus no treatment control, to include placebo, sham Reiki, standard care, treatment as usual, wait list
Reiki versus pharmacological treatments
Reiki versus herbal medicine
Reiki versus psychological therapies
Reiki versus exercise/other therapy
Assessment of risk of bias in included studies
Working independently, JJ and GPH assessed risk of bias of the included studies using the tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This tool encourages consideration of how the sequence was generated, how allocation was concealed, the integrity of blinding at outcome, the completeness of outcome data, selective reporting and other potential sources of bias. We included quotations from the text of included studies; comments on how we assessed the risk of bias; and judgements as follows:
Low risk of bias. Unclear risk of bias. High risk of bias.
Measures of treatment effect
Analyses were to be carried out for both continuous and dichotomous data where the data permitted.
Dichotomous data
We intended to use the risk ratio for dichotomous outcomes.
Continuous data
Continuous data were assessed using mean differences (MD). If it was possible to combine results that used different scales, standardised mean differences (SMD) were to be used.
All estimates were calculated with 95% confidence intervals.
Unit of analysis issues
We intended to treat cluster randomised trials and crossover trials and others with unit of analysis issues as is suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
Authors of included studies were contacted and asked to provide the missing details. The data supplied meant that there was no need to calculate standard deviations (SD) from other data or to use imputed data.
Assessment of heterogeneity
Heterogeneity of treatment effects between studies was to have been assessed by visual inspection of the forest plots, the I² statistic and the test for heterogeneity. To deal with suspected excess heterogeneity we were to look for plausible effect modifiers then use a summary estimate of effect, both with and without the different study, and discuss the results. If there were no plausible reasons for the heterogeneity then the studies were to be re‐examined to see if pooling was appropriate at all.
Assessment of reporting biases
We intended to use a funnel plot to help assess whether small sample bias (one form of which is publication bias) was present.
Data synthesis
If pooling of data was possible it was to be done using the random‐effects model.
Subgroup analysis and investigation of heterogeneity
We intended to carry out subgroup analysis and meta‐regression using Stata. Possible factors that could be analysed if there were more studies that may modify treatment effect were:
Inclusion criteria: DSM diagnosis versus other symptoms
Severity of symptoms: mild/moderate versus severe
Condition treated: e.g., if anxiety or depression are a secondary diagnosis with some other condition as the primary diagnosis
Scale used to measure the outcome: the SMD assumes that one standard deviation on one scale is the same as one standard deviation on other scales. This may not be so
Hands‐on versus hands‐off Reiki: touch may confer some additional benefit
Level of training/experience of the Reiki practitioner
Sensitivity analysis
Sensitivity analyses were planned to assess the robustness of our results. These were to include: 1. The effect of excluding low‐quality studies. Examining whether aspects of the quality of the studies (e.g., allocation concealment, blinding, withdrawals or dropouts) have an effect on the pooled estimate 2. The effect of using 'last observation carried forward' data 3. Intention‐to‐treat 'worst‐case' versus 'best‐case' scenarios 4. Use of diagnostic interview versus self‐rated depression and anxiety scales
Summary of findings tables
If data allowed, a 'Summary of findings' table was to be produced. This would include the following outcomes: degree of anxiety or depression or both, using rating scales; dropout rates; and Quality of Life. The 'Summary of findings' table would be produced according to recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Results
Description of studies
Results of the search
The search of CENTRAL, MEDLINE, EMBASE, PsycINFO, & AMED simply using the text word 'reiki' retrieved 708 studies, with 433 remaining after removing duplicates, so to ensure that studies were not missed the abstracts of all of these were scrutinised for eligibility. The more formal search of the Cochrane Depression, Anxiety and Neurosis Group's registers of studies retrieved two extra studies. Four studies had been registered and not reported and one thesis was found from references. Thirty‐one studies were identified as potentially eligible studies (Figure 1). The search was last run on 4 November 2014.
1.
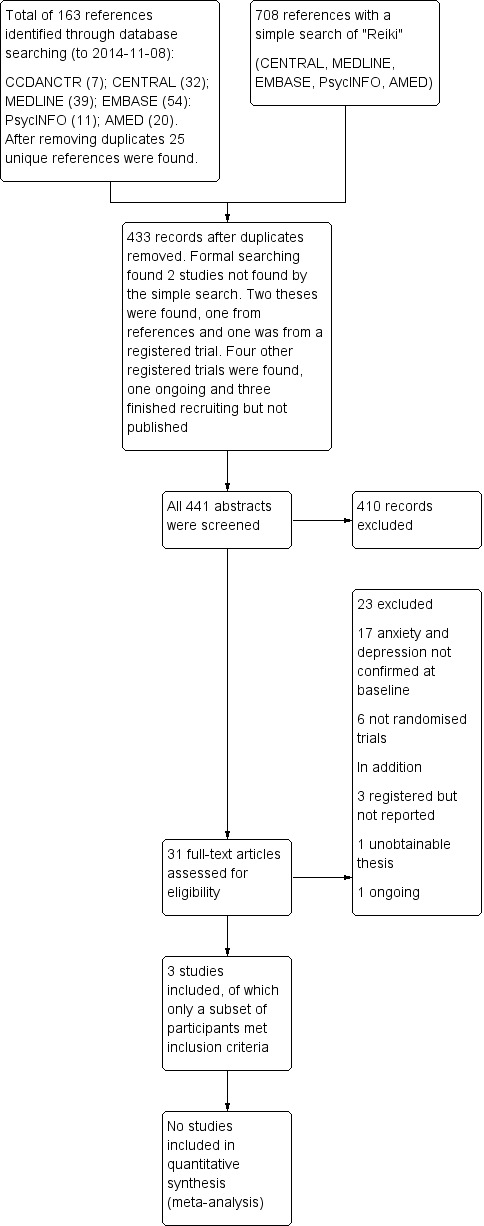
Study flow diagram.
The update search in 2014 retrieved an additional 62 references, after removing duplicate records 25 references were screened. No additional studies were found but there one additional report of Bowden 2011 (conference abstract).
Included studies
There were three included studies (Beard 2011; Bowden 2011; Richeson 2010). These three studies measured anxiety and depression at baseline but only a subgroup were anxious or depressed. Further description is in the table of Characteristics of included studies. Authors of two of these studies were contacted for further details about the subgroup with anxiety or depression or both at baseline and both provided the requested data (Beard 2011; Richeson 2010).
Design
All three studies were parallel randomised controlled trials, one with three arms (Beard 2011); and two with two arms (Bowden 2011; Richeson 2010).
Sample sizes
All studies were small (n = 59 in three arms; and n = 25 and n = 40 in the two‐arm studies).
Setting
Reiki treatment for one trial was carried out at the hospital before the treatment for prostate cancer (Beard 2011). In Bowden 2011 the interventions were carried out in a dimly‐lit room at the university. The room for Richeson 2010 was in a nursing skills laboratory within the College of Nursing and Health Professions at a university.
Participants
Beard 2011 recruited males 30 years old or older with a biopsy‐proven diagnosis of non‐metastatic prostate cancer who were not receiving chemotherapy and had elected to receive external‐beam radiation therapy (EBRx); whereas Richeson 2010 recruited community‐living participants by advertisements in several places, a mixture of men and women, 55 years and older, who had a doctor's diagnosis of pain, anxiety or depression. Bowden 2011 recruited university students.
Interventions and comparators
Beard 2011 randomised to three groups: Reiki, relaxation and waiting list control; Richeson 2010 had two arms: Reiki and waiting list controls; and Bowden 2011 had two arms: Reiki and relaxation‐treated controls.
Outcomes
Beard 2011 used the STAI to measure anxiety and the CES‐D to measure depression. Richeson 2010 used the GDS‐15 for depression and the HAM‐A for anxiety. Bowden 2011 used both the DASS and HADS to measure depression and anxiety.
Studies awaiting classification
One study was a thesis referenced in a paper that we could not get copies of to assess for eligibility (Mauro 2001 in vanderVaart 2009), so is listed in Studies awaiting classification. This dissertation reports the effect of Reiki on women undergoing their first amniocentesis and thus are unlikely to be clinically anxious or depressed but this could not be confirmed.
There were three studies that have been completed but have not yet been reported and we have been unable to contact the investigators (Fox 2005; Frost 2007; Stevens 1998). Fox 2005 studied 120 newly diagnosed prostate cancer patients and tested Reiki versus sham Reiki versus rest. The outcome instruments included 'psychometric instruments' and anxiety is mentioned separately. There is no requirement for the patients to be anxious or depressed or both by scales or clinical diagnoses at study entry.
Frost 2007 studies participants with chronic plaque psoriasis and tested usual care versus Reiki. There is no mention of depression or anxiety in the record on the study register.
Stevens 1998 studies the effect of Reiki versus an unspecified control treatment on people with type II diabetes with neuropathy. No anxiety or depression outcomes are mentioned.
Ongoing trials
There is one ongoing trial that may potentially be eligible (NCT01569269). It is reported to have finished recruiting but we cannot find any reports.
Excluded studies
Twenty‐three of the 31 potentially eligible studies were excluded (Assefi 2008; Barnett 2005; Bowden 2010; Catlin 2011; Clark 2012; Dressen 1998; Fox 2006; Gillespie 2007; MacKay 2004; Mansour 1999; Miles 2003; Olson 2003; Potter 2007; Shiflett 2002; Shore 2004; Thornton 1996; True 2002; Tsang 2007; Vitale 2006; Wardell 2001; Wetzell 1989; Wirth 1994; Witte 2001). Fourteen of these studies measured outcomes of interest (Assefi 2008; Bowden 2010; Catlin 2011; Clark 2012; Dressen 1998; Gillespie 2007; MacKay 2004; Mansour 1999; Olson 2003; Potter 2007; Shiflett 2002; Shore 2004; Tsang 2007; Vitale 2006) but these were impossible to interpret given that participants were not assessed for anxiety or depression at baseline. Six turned out to not be randomised trials (Miles 2003; Thornton 1996; Wardell 2001; Wetzell 1989; Wirth 1994; Witte 2001). See the table of Characteristics of excluded studies for further details.
Risk of bias in included studies
More details of risk of bias are included in the table of Characteristics of included studies. For depictions of the overall risk of bias across domains, see Figure 2 and Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
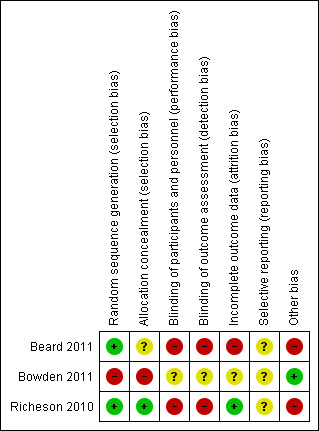
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Richeson 2010 recruited all the participants before randomisation, put their names in a hat and then drew names out for the treatment assignment. If done properly this should be at low risk of bias. Bowden 2011 randomised in pairs, stratified by high or low scores for anxiety or depression. The first person in a stratum was randomised and then the next person got the other treatment. This makes the group allocation of 50% of participants known before recruitment and so is clearly at high risk of bias.
Beard 2011 used a computer generated random sequence but there was no information about how this was implemented.
Blinding
In two of the included studies it was impossible to blind the treatments from either the provider or the participant. All of the outcomes were self reported so were impossible to blind also. Bowden 2011 made great efforts to blind the participants, the success of which was confirmed by questioning them. This was at the expense of limiting the Reiki treatment.
Incomplete outcome data
There appears to be no dropouts amongst those anxious or depressed in the study by Richeson 2010; but two of the anxious and depressed people (both in the relaxation therapy group) in Beard 2011 dropped out. Three of the proposed 20 people in the Reiki group dropped out in the study by Bowden 2011. This happened before recruitment was complete so they were replaced by the next eligible participant. This would have increased the number of participants whose allocation was known before they were randomised.
Selective reporting
It is unlikely that any study measured outcomes and did not report them, however it is difficult to be certain of this so each study was classified as having an unclear risk of bias.
Other potential sources of bias
In two of the included studies only a small subgroup of participants scored above agreed cutoff points on anxiety or depression scales at baseline. Randomisation was not stratified on the baseline results and as the subgroups were small it is unlikely that the groups would be very well matched for prognostic characteristics. Bowden 2011 stratified randomisation of the results of baseline evaluations of anxiety or depression or both so they should be more comparable in other factors, but the groups were small (10 in each arm).
Effects of interventions
Comparison 1. Reiki treatment versus waiting list controls
There were three arms in the study by Beard 2011 (Reiki, relaxation, and waiting list control); whereas the Richeson 2010 study compared Reiki with waiting list controls. Both only had a small number of participants who were anxious or depressed or both at the start if the study. In Bowden 2011 half of the group had high scores for anxiety or depression or both pre‐treatment and these are the ones used in this review.
Primary outcomes
1.1 Relief of symptoms
1.1.1 Anxiety
In the study by Beard 2011 the relaxation group (n = 6) started with a STAI mean score of 51 which reduced to 30 (but 2 dropped out and are not included) at the end of treatment; the Reiki group (n = 5) changed from a mean score of 49 to 40 and the control group (n = 5) went from a mean score of 49 to 45. These differences were not statistically significantly different.
In the anxious, depressed or both group in the Bowden 2011 study the 1‐week post‐treatment mean score for the anxiety subscale of the DASS in the Reiki group was 5 (standard deviation (SD) 3.5) and in the control group it was 5 (SD 3.7). At the 5‐week follow‐up the mean scores were 5.4 (2.8) and 7.3 (5.7) respectively (P = 0.357).
In the Richeson 2010 study there are two standard cutoffs for anxiety. When using the one with the more severely affected people there were 5 people with a mean HAM‐A score at the end of the study of 30 in the Reiki group and 2 in the control group with a mean score of 44. When using the less severe cutoff there were 7 people in the Reiki group with a final mean score of 25 and 4 in the control group with a mean score of 36. There was no evidence of a difference in the HAM‐A score between the groups.
1.1.2 Depression
In the relaxation group in Beard 2011, 3 people met the criteria for depression with an average CES‐D score of 26 but only one of these had a score at the end of treatment and that was 18 (two dropped out). In the Reiki arm 3 participants changed from a mean of 23 to a mean of 22, while in the control arm 1 person started at 31 and was 17 at the end of the study. There was no evidence of a difference between groups.
In the study by Bowden 2011, the mean depression score 1‐week post treatment for the anxious, depressed or both group was 5.3 (standard deviation 4.7) in the Reiki group and 7.9 (standard deviation 4.0) in the control group (P = 0.199). At 5‐weeks post treatment the mean scores were 4.7 (standard deviation 4.1) and 6.8 (standard deviation 5.3) respectively, P = 0.335.
In the study by Richeson 2010 there were also two cutoffs in the depression score. With the cutoff for the more severely affected people there were 4 in the Reiki group with a mean GDS‐15 score of 10; and 1 in the control group with a score of 14. With the less severe cutoff there were 10 in the Reiki group with a mean score of 6; and 3 in the control group with a mean score of 11. There was no evidence of a difference between groups.
1.1.3 HADS total score
Bowden 2011 also reported the total HADS score. At 1‐week post treatment the mean scores were 8.28 (SD 4.48) in the Reiki group and 10.2 (SD 6.14) in the control group (P = 0.435). At the 5‐week follow‐up the mean scores were 9.72 (SD 4.74) and 12.11 (SD 6.16) respectively (P = 0.345).
1.2 Acceptability of the treatments
None of the included trials reported on this outcome
Secondary outcomes
3. Quality of life
None of the included trials reported on this outcome
4. Self‐perceived stress
None of the included trials reported on this outcome
5. Side effects of the Reiki treatment
None of the included trials reported on this outcome for the subgroups of participants included.
Discussion
Summary of main results
The results that are available are from small subgroups of small studies with potential problems from risk of bias. Therefore there is insufficient information to draw conclusions about whether Reiki provides help to people with anxiety or depression. The data were so limited that the planned analyses to explore the data in more detail were not possible.
Overall completeness and applicability of evidence
Studies that aimed to improve anxiety and depression did not ensure that the participants had these problems to start with, so there is very little evidence as to whether Reiki is of benefit to these patients at all. All of the included participants had been rated as anxious or depressed by scores on scales, so did not have a clinical diagnosis. As a result of this the questions posed in this review remain unanswered.
Quality of the evidence
Study limitations (risk of bias)
On the whole these studies were not done in a manner that ensured internal validity although the randomisation sequence was well done on two of the three studies. The allocation was only securely hidden in one study and the other domains only infrequently were at low risk of bias.
Consistency
With so few data it was difficult to examine consistency. All the reported outcomes were not statistically significant, but the confidence intervals (CIs) were wide, thus not excluding beneficial or harmful effects.
Indirectness
Only one of the three included studies had a subgroup that may be typical of those seeking Reiki treatment for anxiety or depression, although these were otherwise fit and well university students. One other study recruited participants who were undergoing treatment for prostate cancer and the third recruited people from the general public aged 55 and over who had pain as well as anxiety or depression. Thus quality of the results would be downgraded because of indirectness.
Imprecision
The data are so few that CIs were wide, which would result in further downgrading of quality.
Publication bias
As every article in the databases that mentioned 'Reiki' were scrutinised for inclusion it is likely that all published work was included.
As well as not directly addressing the questions posed by this review the evidence found was likely to be downgraded to low quality. Better studies, addressing questions of interest to patients, need to be done. It is difficult to assess the evidence when there is so little of it and the included studies do not directly address the questions posed by this review. To answer the question of whether Reiki is useful for people who are anxious or depressed, studies need to include people who are anxious and depressed to start with. The participants in two of the three included studies were in stressful situations, but this does not necessarily correspond with being anxious to the extent that a clinical diagnosis could be made. It would also be of interest, if there was an effect present, to see if it persisted for some time after the Reiki sessions stopped. We identified four potentially relevant studies which have been registered and completed but have yet to be reported; all studies should be registered in a clinical trial database before recruiting participants, and should be published within a reasonable time after measuring all outcomes.
Potential biases in the review process
We only discovered three studies that examined whether the participants were anxious, depressed, or anxious and depressed at baseline. It is impossible to say whether these people were representative of those who may choose to be treated with Reiki.
Participants included were a subgroup of the participants in the studies who scored highly on scales for depression, anxiety, or both. Apart from one study the randomisation was not stratified for this so it is likely that the included participants were not balanced for important prognostic factors at baseline, but there is so little data available the decision was made to use all the available data. That means that any conclusions have to be very guarded: the lack of data and most of it coming from subgroups means that any conclusions might easily be changed with new data.
The control group in two of the included studies was a waiting list group, so the participants knew they were not getting any treatment but would get treatment in the future. It is unclear what effect this would have on the outcome but it is possible that it would be different from a placebo treatment.
We could not contact the named investigators for some studies that had a possibility of being included (e.g. NCT01569269) so we may have missed eligible studies/people.
Agreements and disagreements with other studies or reviews
There have been mixed results on studies looking at the effects of Reiki on the outcomes of anxiety and depression. This may be because people who are not anxious and depressed have been included in many studies and they have little to gain from any treatment.
Authors' conclusions
Implications for practice.
We could only include a few participants (45 anxious/depressed out of 124 randomised) from subgroups of the three studies meeting the inclusion criteria; this evidence was of moderate quality, at best. There is therefore insufficient evidence from randomised trials to draw any conclusions on whether Reiki is effective for the treatment of anxiety or depression.
Implications for research.
If Reiki is to be regarded as a serious treatment for anxiety or depression then well‐designed, well‐conducted, and well‐reported studies need to be done. Currently Reiki is a treatment of unproven effectiveness and thus more evidence is needed before it can be accepted as useful, or discarded as useless. Studies need to be in appropriate patient populations: in this instance in people with anxiety or depression, either clinically diagnosed or by being above cutoffs in anxiety or depression scores. Reiki should be administered by a trained Reiki practitioner, and it would be useful to compare it with something that facilitates blinding of the participants and different forms of Reiki (e.g. distance Reiki). Outcomes should include measures of anxiety or depression measured after a reasonable period. These outcomes should be measured again some time after the treatment sessions have stopped to check on the persistence of any effect. Studies should be large enough to answer questions about whether such treatments are efficacious. Studies should be reported in full within a reasonable time of the last outcome being measured.
History
Protocol first published: Issue 4, 2007 Review first published: Issue 4, 2015
| Date | Event | Description |
|---|---|---|
| 2 November 2008 | Amended | Converted to new review format. |
Acknowledgements
Nassim Assefi, 17 March 2008, provided extra information via email.
Nancy Richeson provided data on the subgroup of participants with problems at baseline.
Clair Beard and her co‐investigators provided data on the subgroup of participants with problems at baseline.
Appendices
Appendix 1. Additional Searches ‐ CENTRAL, MEDLINE, EMBASE and AMED
1. The Cochrane Central Register of Controlled Trials (CENTRAL) (2012‐01‐08) was searched using the following terms:
#1. MeSH descriptor Therapeutic Touch, this term only #2. reiki #3. energy NEXT heal* #4. energy NEXT channel* #5. (#1 or #2 or #3 or #4) #6. MeSH descriptor Depression, this term only #7. MeSH descriptor Depressive Disorder explode all trees #8. (depress* or dysthymi*) #9. MeSH descriptor Adjustment Disorders, this term only #10. MeSH descriptor Affective Symptoms, this term only #11. (adjustment NEXT disorder*) or (affective NEXT disorder*) or (affective NEXT symptom*) #12. exp Anxiety/ #13. exp Anxiety Disorders/ #14. (agoraphobi* or anxiety or anxio* or phobi* or panic or obsessi* or compulsi* or OCD or GAD or PTSD or posttrauma* or post‐trauma* or (post NEXT trauma*) or (stress NEXT disorder) or neurosis or neuroses or neurotic or psychoneuro*) #15. (#6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14) #16. #5 and #15
2. OVID MEDLINE (2012‐01‐08) was searched using the following search terms:
1. Therapeutic Touch/ 2. Reiki.tw. 3. energy heal*.tw. 4. energy channel*.tw. 5. or/1‐4 6. Depression/ 7. Depressive Disorder/ 8. (depress* or dysthymi*).tw. 9. (adjustment disorder* or affective disorder* or affective symptom*).mp. 10. exp Anxiety/ 11. exp Anxiety Disorders/ 12. (agoraphobi* or anxiety or anxio* or phobi* or panic or obsessi* or compulsi* or OCD or GAD or PTSD or posttrauma* or post‐trauma* or post trauma* or stress disorder or neurosis or neuroses or neurotic or psychoneuro*).tw. 13. or/6‐12 14. randomized controlled trial.pt. 15. controlled clinical trial.pt. 16. randomi#ed.ti,ab. 17. randomly.ab. 18. sham.ab. 19. trial.ab. 20. groups.ab. 21. (control$ adj3 (trial or study)).ab,ti. 22. ((singl$ or doubl$ or tripl$ or trebl$) adj3 (blind$ or mask$ or dummy)).mp. 23. (animals not (humans and animals)).sh. 24. or/14‐22 25. 24 not 23 26. 5 and 13 and 25
3. OVID EMBASE (2012‐01‐08) was searched using the following search terms:
1. Reiki/ 2. Reiki.tw. 3. therapeutic touch.tw. 4. energy heal*.tw. 5. energy channel*.tw. 6. or/1‐5 7. exp Depression/ 8. Anxiety/ 9. exp Anxiety disorder/ 10. (agoraphobi* or anxiety or anxio* or phobi* or panic or obsessi* or compulsi* or OCD or GAD or PTSD or posttrauma* or post‐trauma* or post trauma* or stress disorder or neurosis or neuroses or neurotic or psychoneuro*).tw. 11. (depress* or dysthymi*).tw. 12. (adjustment disorder* or affective disorder* or affective symptom*).mp. 13. or/7‐12 14. randomized controlled trial.de. 15. randomization.de. 16. randomi#ed.ti,ab. 17. randomly.ab. 18. sham.ti,ab. 19. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 20. factorial$.ti,ab. 21. allocat$.ti,ab. 22. assign$.ti,ab. 23. volunteer$.ti,ab. 24. crossover procedure.de. 25. (crossover$ or cross over$).ti,ab. 26. (quasi adj (experimental or random$)).mp. 27. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 28. ((animal or nonhuman) not (human and (animal or nonhuman))).de. 29. or/14‐27 30. 29 not 28 31. 6 and 13 and 30
4. OVID PsycINFO (2012‐01‐08) was searched using the following search terms:
1. reiki.tw. 2. therapeutic touch.tw. 3. energy heal*.tw. 4. energy channel*.tw. 5. or/1‐4 6. exp Major Depression/ [Major Depression or Anaclitic Depression/ or Dysthymic Disorder/ or Endogenous Depression/ or Postpartum Depression/ or Reactive Depression/ or Recurrent Depression/ or Treatment Resistant Depression/] 7. Atypical Depression/ 8. “Depression (Emotion)”/ 9. (depress* or dysthymi*).tw. 10. exp Anxiety Disorders [Anxiety Disorders/ or Acute Stress Disorder/ or Castration Anxiety/ or Death Anxiety/ or Generalized Anxiety Disorder/ or Obsessive Compulsive disorder/ or Panic Disorder/ or Phobias/or Acrophobia/ or Agoraphobia/ or Claustrophobia/ or Ophidiophobia/ or School Phobia/ or Social Phobia/ or Posttraumatic Stress Disorder/ or Separation Anxiety/] 11. exp Anxiety/ [Anxiety/ or Computer Anxiety/ or Mathematics Anxiety/ or Performance Anxiety/ or Social Anxiety/ or Speech Anxiety/ or Test Anxiety/] 12. Panic/ 13. Panic Attack/ 14. (agoraphobi* or anxiety or anxio* or phobi* or panic or obsessi* or compulsi* or OCD or GAD or PTSD or posttrauma* or post‐trauma* or post trauma* or stress disorder or neurosis or neuroses or neurotic or psychoneuro*).tw. 15. (adjustment disorder* or affective disorder* or affective symptom*).mp. 16. or/6‐15 17. treatment effectiveness evaluation.sh. 18. clinical trials.sh. 19. mental health program evaluation.sh. 20. placebo.sh. 21. placebo*.ti,ab. 22. randomly.ab. 23. randomi#ed.ti,ab. 24. sham.ti,ab. 25. trial.ti,ab. 26. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 27. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 28. factorial$.ti,ab. 29. allocat$.ti,ab. 30. assign$.ti,ab. 31. volunteer$.ti,ab. 32. (crossover$ or cross over$).ti,ab. 33. (quasi adj (experimental or random$)).mp. 34. "2000".md. [methodology=treatment outcome/clinical trial] 35. or/17‐34 36. 5 and 16 and 35
OVID AMED (2012‐01‐08) was searched using the following search terms:
1. Reiki/ 2. reiki.tw. 3. Therapeutic Touch/ 4. therapeutic touch.tw. 5. energy heal*.tw. 6. energy channel*.tw. 7. or/1‐6 8. Depression/ 9. Depressive Disorder/ 10. (depress* or dysthymi*).tw. 11. Anxiety/ 12. exp Anxiety Disorders [Anxiety Disorders/ Obsessive Compulsive Disorder/ or Phobic Disorders/or Agoraphobia/ or Stress Disorders Posttraumatic /] 13. Panic/ 14. (agoraphobi* or anxiety or anxio* or phobi* or panic or obsessi* or compulsi* or OCD or GAD or PTSD or posttrauma* or post‐trauma* or post trauma* or stress disorder or neurosis or neuroses or neurotic or psychoneuro*).tw. 15. (adjustment disorder* or affective disorder* or affective symptom*).mp. 16. or/8‐15 17. exp Clinical Trials/ 18. Randomized Controlled Trial.pt. 19. Comparative study/ 20. Random Allocation/ 21. Placebos/ 22. placebo*.ti,ab. 23. randomly.ab. 24. randomi#ed.ti,ab. 25. sham.ti,ab. 26. trial.ti,ab. 27. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 28. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 29. factorial$.ti,ab. 30. allocat$.ti,ab. 31. assign$.ti,ab. 32. volunteer$.ti,ab. 33. (crossover$ or cross over$).ti,ab. 34. (quasi adj (experimental or random$)).mp. 35. or/17‐34 36. 7 and 16 and 35
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beard 2011.
| Methods | 3‐arm parallel randomised controlled trial (called a Phase II trial). Recruitment June 2005 to April 2007. | |
| Participants | Sex: Males. Age: 30 years old or older Inclusion criteria: A biopsy‐proven diagnosis of non‐metastatic prostate cancer who were not receiving chemotherapy and had elected to receive external‐beam radiation therapy (EBRx). Exclusion criteria: Receiving ongoing psychotherapy or were receiving antidepressive medications, had prior experiences with Reiki or relation therapy, or had problems with comprehension of English. |
|
| Interventions | All patients received EBRx 5 days a week for 8 to 9 weeks with sessions averaging 15 minutes in length. 1. Reiki (n = 20). Twice weekly for a maximum of 8 weeks. Each session lasted approximately 50 minutes. Given by 1 of 3 nurses who were very experienced master level Reiki practitioners. Protocol was standardised to reduce variability. 2. Relaxation response therapy (n = 20). Weekly for 8 consecutive weeks. Each session was one hour. A psychologist guided the participant to evoke the relaxation response using a standardised script. The rest of the session was devoted to cognitive restructuring using a systematic and replicable methodology involving 5 standardised steps. Participants encouraged to practise the techniques daily and to document these in a journal. 3. Wait list control (n = 19). |
|
| Outcomes | Spielberger State‐Trait Anxiety Inventory (STAI). Center for Epidemiologic Studies Depression Scale (CES‐D). Functional Assessment of Cancer Therapy ‐ General (FACT‐G). All measured at the end of the treatment period. |
|
| Notes | The relaxation therapy group had 6 anxious participants at baseline, 4 of whom had scores at the end; the Reiki group had 5 anxious participants all of whom had scores after treatment and the control group also had 5 anxious participants, all of whom had measurements at the end of the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were randomized before starting EBRx using a computer‐generated randomization list derived from permuted blocks in equal proportions to the Reiki, RRT/CR, or wait‐list control groups". "Computer‐generated randomization was performed using permuted blocks of three." |
| Allocation concealment (selection bias) | Unclear risk | Nothing stated. With a block size of three it would be easy to know at least one third of the assignments. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible in this study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were self completed by participants |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In the subgroup with depression or anxiety or both the dropout was a large proportion (2/6 of those anxious and 2/3 of those depressed) because the subgroup was so small. All dropouts were in the relaxation therapy group. |
| Selective reporting (reporting bias) | Unclear risk | Outcomes of interest are reported |
| Other bias | High risk | Subgroup analysis on small numbers with no stratified randomisation. |
Bowden 2011.
| Methods | 2‐arm RCT. Stratified into two groups, those with low scores on depression or anxiety scales and those with high scores. | |
| Participants | Students, mainly from Psychology undergraduate classes. Sex: 37F, 4M ("The higher proportion of female participants was largely due to the high female‐to‐male ratio of Psychology undergraduates, and also perhaps because females were more inclined to take part.") Age: range 18 to 31 plus one 43 year old Inclusion criteria: Equal numbers had to have high or low scores on the Hospital Anxiety and Depression Scale (HADS). High scores were defined as a subscale score of 10/20 or if the sum of the subscale scores was 12/40 or more. Low scores were defined as both subscales less than 7/10 and a total score below 12/40. |
|
| Interventions | 1. Reiki (n = 20, 10 high and 10 low). Guided relaxation for 25 minutes with headphones and blindfold. Reiki was delivered by a Master‐Teacher level Usui Reiki practitioner with 4 years' experience. To maintain blinding this was done from behind each participant and sent non‐contact individualised Reiki to those in the Reiki group. 2. Control (n = 20, 10 high and 10 low). Guided relaxation as for the Reiki group. Both groups had 6 sessions over a period of two to eight weeks. |
|
| Outcomes | Depression Anxiety and Stress Scale (DASS). Hospital Anxiety and Stress (sic) Scale (HADS). Pittsburgh Quality of Sleep Index (PQSI). Illness Symptoms Questionnare (ISQ). Activation‐Deactivation Check List (AD‐ACL). The Reiki Blinding and Expectation Questionnaire. All measured at baseline, one week and five weeks post treatment. |
|
| Notes | Three dropped out at an early stage (all of whom were in the Reiki group) and were replaced until there were 20 with high scores and 20 with low scores . Only those with high scores for anxiety or depression are used in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The randomisation procedure consisted of the tossing of an unbiased coin to assign each new pair of High‐Mood or Low‐Mood participants to be recruited to the Reiki or Control groups, to ensure that there were equal numbers of participants in each group. If, for example, the first High‐Mood participant to be recruited was randomly assigned to the Reiki group, then the next High‐Mood participant was assigned to the Control group, and likewise with the Low‐Mood participants until there were 10 participants in each of the four subgroups. When participants dropped out, new recruits continued to be randomly assigned to the four subgroups by the method described, until the target sample size was achieved." This matched pair design could be open to all sorts of problems. |
| Allocation concealment (selection bias) | High risk | See above. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The person giving the Reiki treatment could not be blinded but there were considerable efforts to blind the participants : "...since the majority of Reiki participants either believed that they were not in the Reiki group or were uncertain of their group, it seems that they could not detect the experimenter sending Reiki." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self administered questionnaires but "...since the majority of Reiki participants either believed that they were not in the Reiki group or were uncertain of their group, it seems that they could not detect the experimenter sending Reiki." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All participants had outcomes measured but for the DASS two participants were excluded from the analysis as they were outliers (2.256 and 2.168 standard deviations from the sample mean). One of these was from each group. |
| Selective reporting (reporting bias) | Unclear risk | Wide range of outcomes and all were reported. |
| Other bias | Low risk | No reason to suspect this. |
Richeson 2010.
| Methods | Two arm RCT (Called a pilot study). Treatment during Northern hemisphere fall, 2008. | |
| Participants | Sex: 16F, 9M Age: 55 Years or older, ranged from 57 to 76, mean age 63.8, standard deviation 4.9 Inclusion criteria: Participants were community‐dwelling older adults recruited from various forms of advertising. They had to have a medical diagnosis of pain or depression or anxiety, or a combination thereof, be willing to undergo the intervention and have transportation available. . Participants reported a wide range of problems related to pain, anxiety and depression. |
|
| Interventions | Intervention (n = 13): 45 minute sessions, 1 day per week for 8 weeks. Individualised treatment based on the participant's needs. Traditional Reiki plus advanced techniques of Nentatsu‐ro, Byosen Reikian‐ho and Reiji‐ho. Treatments were provided by one of two Reiki Masters/Teachers with 8 to 10 years' experience. Control (n = 12): waiting list. |
|
| Outcomes | Geriatric Depression Scale Short Form (GDS‐15). Hamilton Anxiety Scale (HAM‐A). Faces Pain Scale (FPS). Heart Rate. Blood Pressure. All measured at the end of the treatment period. |
|
| Notes | There were no losses to follow up in the group with anxiety or depression at baseline. Five participants had depression at baseline, and 4 had anxiety. It was not clear whether these were the same, or different, people. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment of participants to an experimental or wait list control group was completed by drawing names from a hat." This was done after all participants were recruited so should have little risk of bias. |
| Allocation concealment (selection bias) | Low risk | See above. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not done. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome was self‐completed questionnaires. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There appears to be no dropouts. |
| Selective reporting (reporting bias) | Unclear risk | Unlikely to be unreported outcomes. |
| Other bias | High risk | This review is only interested in the outcomes on a subgroup, which was not stratified in the randomisation. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Assefi 2008 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Barnett 2005 | Never measured anxiety and depression |
| Bowden 2010 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Catlin 2011 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Clark 2012 | Pilot study and patients did not meet the criteria for being anxious or depressed |
| Dressen 1998 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Fox 2006 | Excluded participants with high scores for depression or anxiety |
| Gillespie 2007 | Participants did not meet the criteria for being anxious or depressed |
| MacKay 2004 | Participants did not meet the criteria for being anxious or depressed |
| Mansour 1999 | Participants did not meet the criteria for being anxious or depressed |
| Miles 2003 | Not an RCT |
| Olson 2003 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Potter 2007 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Shiflett 2002 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Shore 2004 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Thornton 1996 | Unsure if randomised and not able to contact author |
| True 2002 | Author contacted and said does not meet inclusion criteria. |
| Tsang 2007 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Vitale 2006 | Used included outcomes but participants did not meet the criteria for being anxious or depressed |
| Wardell 2001 | Not an RCT |
| Wetzell 1989 | Not an RCT |
| Wirth 1994 | Before and after study |
| Witte 2001 | Not an RCT |
Characteristics of studies awaiting assessment [ordered by study ID]
Fox 2005.
| Methods | Treatment, Randomised, Double Blind (Subject, Investigator), Placebo Control, Parallel Assignment, Efficacy Study |
| Participants | Inclusion criteria: ‐ Newly diagnosed with prostate cancer ‐ Scheduled for radial prostatectomy, external beam radiation, brachytherapy, or a combination of these. Exclusion criteria: ‐ Already involved in energy healing treatments ‐ Any patient whose medical intervention could not wait the 4‐weeks for intervention for medical reasons ‐ Any patient who gets neo‐adjuvant therapy or any herbal product that could affect PSA Age minimum: N/A Age maximum: N/A Gender: male |
| Interventions | Behavioral: Reiki Behavioral: pretend Reiki Behavioral: rest/guided imagery |
| Outcomes | To evaluate the effects of Reiki on anxiety states using validated psychometric instruments. (Time Frame: each 30 minute session) To evaluate the effects of Reiki on physiologic anxiety as measured by cortisol and DHEA levels (Time Frame: each 30 minute session) To evaluate the effects of Reiki on cancer progression as measured by PSA levels in plasma. (Time Frame: throughout study) To evaluate the effects of Reiki and guided imagery on post‐surgical pain and urinary symptoms. (Time Frame: throughout study) |
| Notes | The study has been completed |
Frost 2007.
| Methods | Two arm parallel RCT |
| Participants | Inclusion: stable chronic plaque psoriasis, 18 years old or older. Exclusion: pregnant women, severe disease, unstable psoriasis or pustular psoriasis, previous experience of healing, unable to give informed consent |
| Interventions | Reiki plus standard therapy which includes a long list of things versus Reiki plus moisturiser |
| Outcomes | Psoriasis area and severity index (PASI) validated by photos Quality of Life assessments with dermatology life quality index (DLQI) Psychological assessments GHQ‐12 Health economics assessment secondary: healing assessment (HA). |
| Notes | The study has been completed |
Mauro 2001.
| Methods | Unknown, but is an RCT |
| Participants | Pregnant women undergoing amniocentesis |
| Interventions | Unknown but does include Reiki |
| Outcomes | Unknown, but will include some measure of anxiety |
| Notes | Personal contact at the university was unable to find this in the library |
Stevens 1998.
| Methods | Randomised single blind |
| Participants | Inclusion: NIDDM, agree to 12 month follow up |
| Interventions | Reiki ‐ no comparison treatment specified |
| Outcomes | None given |
| Notes | This study has been completed |
Characteristics of ongoing studies [ordered by study ID]
NCT01569269.
| Trial name or title | A Randomized, Four‐Arm Study Comparing Reiki, Yoga, Meditation, or Patient Education Group for Addressing Symptoms of Chemotherapy‐Induced Peripheral Neuropathy (CIPN) |
| Methods | Allocation: randomised Endpoint Classification: efficacy study Intervention Model: parallel assignment Masking: single blind (investigator) Primary Purpose: supportive care |
| Participants | People with symptoms of chemotherapy‐induced peripheral neuropathy (CIPN) Inclusion Criteria:
Exclusion Criteria:
|
| Interventions | Behavioural: Yoga Intervention The yoga intervention will take place for one hour per week for six weeks. All sessions will be guided by a Registered Yoga Teacher (RYT) who is also a Licensed Clinical Social Worker (LCSW). Each yoga session will follow a similar protocol. The introductory period (10 minutes) will focus participants on increasing interoceptive and proprioceptive capacity. The main segment is comprised of a series of yoga postures that progress from lying or seated postures that provide gentle muscle stretching to standing stretches that increase balance and flexibility. The postures will be introduced, practised, and combined with breathing exercises for 40 minutes. The conclusion of the session will comprise 10 minutes of relaxation. Behavioural: Meditation Intervention The meditation intervention will be conducted weekly for six weeks. Each class will follow a similar protocol: during the one‐hour meeting, participants will focus on developing attention to the breath. In a supine or seated position and with eyes closed, participants will be guided to attend solely to their breathing. As physical sensations, thoughts, and emotions begin to arise, participants will be taught to recognise, acknowledge, and accept the presence of the sensations or emotions and then to step back, release the thought or sensation, and refocus attention toward the breath. At the conclusion of each meeting, the meditation instructor will encourage participants to voluntarily engage in daily meditation practices. Behavioural: Reiki The Reiki intervention will be conducted for one hour per week for 6 weeks. Protocol for each session: Briefly meet with the Reiki practitioner to review experiences with symptoms of CIPN. Then, the participant will be directed to lie supine and fully clothed on a massage table. Beginning at the top of the head, the practitioner will move inferiorly and pause while holding their hands above, but facing the participant at each energy point until reaching the feet. Upon reaching the participant's feet, the participant will roll from the supine position to a prone position and the process repeated. After being guided to a seated position on the massage table, the practitioner will spend a few moments in conversation with the participation before ending the session. Other: Holistic Education The psychoeducational intervention will be presented in a traditional classroom format with weekly one hour meetings taking place during the six‐week study period. Each class meeting will address specific aspects of CIPN. Participants will be presented with content related to basic neuroanatomy, physiology, the effects of chemotherapy on peripheral nervous system, how available allopathic treatments (pharmacological/psychopharmacological) can be helpful, and psychosocial issues related to CIPN. The final week of the psychoeducational group will include the identification of complementary interventions that may be of help to people living with CIPN. |
| Outcomes | Primary Outcome Measures: FACT GOG‐ntx scale [Time Frame: change from baseline in quality of life and symptoms of neurotoxicity in 6 weeks ] [Designated as safety issue: No ]. This scale measures two outcomes: symptoms of neurotoxicity; and quality of life. The FACT GOG‐ntx combines the 27‐item general Functional Assessment of Cancer Therapy scale (FACT‐G) with an 11‐item neurotoxicity subscale. Completion of the FACT‐G does not require assistance and can be completed in less than five minutes. Cronbach's coefficient for each item on this scale has been demonstrated at 0.70 or higher, and the instrument is sensitive to respondent changes over time.
Secondary Outcome Measures: The Brief Symptom Inventory ‐ 18 (BSI‐18) [Time Frame: change from baseline in quality of life and symptoms of neurotoxicity in 6 weeks] [Designated as safety issue: No]. The BSI‐18 is an 18‐item brief psychological screening instrument that has been designed to measure distress and yields a global distress score as well as subscale scores for somatic concerns, anxiety, and depression. The BSI‐18 has been found to have good internal reliability with a Cronbach's alpha value of 0.89. Mindful Attention Awareness scale (MAAS) [Time Frame: change from baseline in quality of life and symptoms of neurotoxicity in 6 weeks] [Designated as safety issue: No]. The MAAS is a 15‐item scale that is self administered, requires no assistance to complete, and can be taken in five minutes or less. The instrument was developed to evaluate states of mindfulness or the respondent's capacity to simply observe and be aware of internal and external events in the present moment as a method of self regulation. Internal reliability of items on the MAAS has been established with Cronbach's Alpha coefficients at 0.80 or higher per item. |
| Starting date | May 2010 |
| Contact information | Paul Clark, PhD, Assistant Professor, George Mason University |
| Notes | Study is marked as finished. It had an end date of March 2012. It was registered in clinicaltrials.gov on March 29th, 2012. |
Differences between protocol and review
In the original protocol for this review, we planned to assess methodological quality of included studies by criteria sent out in the Cochrane Reviewers' Handbook (Alderson 2004); however, following the publication of the revised and expanded Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), we altered our plans and will now use the risk of bias tool.
The following methods were published in the original protocol for this review, but were not applicable to this version of the review.
Dealing with missing data: "missing dichotomous data will be managed through intention‐to‐treat (ITT) analysis, in which it will be assumed that patients who dropped out after randomisation had a negative outcome, although it is acknowledged that categorising dropouts as treatment failures may have overestimated the number of patients with a poor outcome. Best/worse case scenarios will also be calculated for the clinical response outcome. For missing continuous data, the method of 'last observation carried forward' (LOCF) will be used where possible, with due consideration of the potential bias and uncertainty introduced."
The types of participants section was modified, to make it clear that we included studies with a subset of relevant participants where the data for those participants was reported separately or the relevant information could be obtained from the authors.
Contributions of authors
Both authors had the idea for the systematic review. Both authors reviewed studies for eligibility, independently extracted data, and wrote the review.
Sources of support
Internal sources
-
GPH is an employee of the University of Otago, New Zealand.
Salary
External sources
No sources of support supplied
Declarations of interest
PH: none known
JJ is a Reiki teacher (but was not practicing during the period of the review)
New
References
References to studies included in this review
Beard 2011 {published and unpublished data}
- Beard C, Stason WB, Wang Q, Manola J, Dean‐Clower E, Dusek JA, et al. Effects of complementary therapies on clinical outcomes in patients being treated with radiation therapy for prostate cancer. Cancer 2011;117(1):96‐102. [DOI] [PubMed] [Google Scholar]
Bowden 2011 {published data only}
- Bowden D, Goddard L, Gruzelier J. A randomised controlled single‐blind trial of the efficacy of Reiki at benefitting mood and well‐being. Evidence‐Based Complementary and Alternative Medicine 2011;381862:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden D, Goddard L, Gruzelier J. A randomised controlled single‐blind trial of the efficacy of Reiki in benefitting mood and well‐being [abstract]. Neuroscience letters [abstracts of the 3rd biennial meeting of the society of applied neuroscience. 5‐8 may 2011, Thessaloniki Greece] 2011. [Google Scholar]
Richeson 2010 {published and unpublished data}
- Richeson NE, Spross JA, Lutz K, Peng C. Effects of Reiki on anxiety, depression, pain and physiological factors in community‐dwelling older adults. Research in Gerontological Nursing 2010;3(3):187‐99. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Assefi 2008 {published and unpublished data}
- Assefi N, Bogart A, Goldberg J, Buchwald D. Reiki for the Treatment of Fibromyalgia: A Randomized Controlled Trial. The Journal of Alternative and Complementary Therapies 2008;14(9):1115‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnett 2005 {published data only}
- Barnett D. The Effects on the Well‐being of Parents who learn and practise Reiki [PhD thesis]. San Francisco, CA: Institute of Transpersonal Psychology, 2005. [Google Scholar]
Bowden 2010 {published data only}
- Bowden D, Goddard L, Gruzelier J. A randomised controlled single‐blind trial of the effects of Reiki and positive imagery on well‐being and salivary control. Brain Research Bulletin 2010;81:66‐72. [DOI] [PubMed] [Google Scholar]
Catlin 2011 {published data only}
- Catlin A, Taylor‐Ford RL. Investigation of standard care versus sham Reiki placebo versus actual Reiki therapy to enhance comfort and well‐being in a chemotherapy infusion center. Oncology Nursing Forum 2011;38(3):E212‐E220. [DOI] [PubMed] [Google Scholar]
Clark 2012 {published data only}
- Clark P, Cortese‐Jimenez G, Cohen E. Using Reiki, Yoga, meditation or patient education to address physical and psychological symptoms related to chemotherapy‐induced peripheral neuropathy: A pilot study [conference abstract]. Psycho‐Oncology [abstracts from the 8th Annual Conference of the American Psychosocial Oncology Society Anaheim, CA United States. Feb 17‐19 2011]. 2011; Vol. 20 (Suppl 1):94‐5.
- Clark PG, Cortese‐Jimenez G, Cohen E. Effects of Reiki, Yoga or Meditation on the physical and psychological symptoms of chemotherapy‐induced peripheral neuropathy: A randomized pilot study. Journal of Evidence Based Complementary & Alternative Medicine 2012;17(3):161‐71. [Google Scholar]
Dressen 1998 {published data only}
- Dressen L, Singg S. Effects of Reiki on Pain and Selected Affective and Personality Variables of Chronically Ill Patients. Subtle Energies and Energy Medicine 1998;9(1):51‐82. [Google Scholar]
Fox 2006 {published data only}
- Fox J. Effects of Reiki on physiological consequences of acute stress. International Clinical Trials Registry (NCT00346671) 2006.
Gillespie 2007 {published data only}
- Gillespie E, Gillespie BW, Stevens M. Painful Diabetic Neuropathy: Impact of an Alternative approach. Diabetes Care 2007;30:999‐1001. [DOI] [PubMed] [Google Scholar]
MacKay 2004 {published data only}
- MacKay N, Hansen S, McFarlane M. Autonomic Nervous System Changes During Reiki Treatment: A Preliminary Study. The Journal of Alternative and Complementary Medicine 2004;10(6):1077‐81. [DOI] [PubMed] [Google Scholar]
Mansour 1999 {published data only}
- Mansour A, Beuche M, Laing G. A Study to test the effectiveness of placebo Reiki standardization procedures developed for a planned Reiki efficacy study. Journal of Alternative and Complementary Medicine 1999;5(2):153‐64. [DOI] [PubMed] [Google Scholar]
Miles 2003 {published data only}
- Miles P. Preliminary Report on the use of Reiki for HIV‐related pain and anxiety. Alternative Therapies in Health and Medicine 2003;9(2):36. [PubMed] [Google Scholar]
Olson 2003 {published data only}
- Olson K, Hanson J, Michaud M. A Phase II Trial of Reiki for the Management of Pain in Advanced Cancer Patients. Journal of Pain and Symptom Management 2003;26(5):990‐7. [DOI] [PubMed] [Google Scholar]
Potter 2007 {published data only}
- Potter, P. Breast Biopsy and Distress: Feasibility of Testing a Reiki Intervention. Journal of Holistic Nursing 2007;25:238‐48. [DOI] [PubMed] [Google Scholar]
Shiflett 2002 {published data only}
- Shiflett S, Nayak S, Bid C, Miles P, Agostinelli S. Effect of Reiki Treatments on Functional Recovery in Patients in Post stroke Rehabilitation: A Pilot Study. Journal of Alternative and Complementary Medicine 2002;8(6):755‐63. [DOI] [PubMed] [Google Scholar]
Shore 2004 {published data only}
- Shore AG. Long‐Term Effects of Energetic Healing on Symptoms of Psychological Depression and Self‐perceived Stress. Alternative Therapies in Health and Medicine 2004;10(4):42‐8. [PubMed] [Google Scholar]
- Shore ALG. Long‐term effects of energetic healing on symptoms of psychological depression and self perceived stress [PhD thesis]. Dissertation Abstracts International: Section B: The Sciences and Engineering 2002; Vol. 63, issue 3‐B:1575.
Thornton 1996 {published data only}
- Thornton L. A study of Reiki, an energy field treatment, using Roger's science. Rogerian Nursing Science News 1996;8(3):14‐5. [Google Scholar]
True 2002 {published data only}
- True G. The use of Reiki for Patients with advanced Aids. http://clinicaltrials.gov/ct2/show/NCT00032721 (accessed 4 November 2014).
- True G, Quinn J, Brown NA, Millar A, Tedaldi E, Phipps EJ, et al. Use of Reiki to Improve Quality of Life and Well‐being for Persons with Advanced HIV/AIDS[abstract #60484]. 131st Annual Meeting of the American Public Health Association (APHA). 2003 Nov 15‐19; San Francisco, CA https://apha.confex.com/apha/131am/techprogram/paper_60484.htm (accessed 4 November 2014).
Tsang 2007 {published data only}
- Tsang K, Carlson L, Olson K. Pilot Cross‐over Trial of Reiki versus Rest for Treating Cancer‐Related Fatigue. Integrated Cancer Therapies 2007;6:25‐35. [DOI] [PubMed] [Google Scholar]
Vitale 2006 {published data only}
- Vitale A, O'Connor P. The Effect of Reiki on Pain and Anxiety in Women with Abdominal Hysterectomies. Holistic Nursing Practice 2006;20(6):263‐71. [PubMed] [Google Scholar]
Wardell 2001 {published data only}
- Wardell D, Engebretson J. Biological correlates of Reiki touch healing. Journal of Advanced Nursing 2001;33(4):439‐45. [DOI] [PubMed] [Google Scholar]
Wetzell 1989 {published data only}
- Wetzel WS. Reiki Healing: A physiological perspective. Journal of Holistic Nursing 1989;7(1):47‐54. [Google Scholar]
Wirth 1994 {published data only}
- Wirth DP, Barrett MJ. Complementary Healing Therapies. International Journal of Psychosomatics 1994;41(1):61‐7. [PubMed] [Google Scholar]
Witte 2001 {published data only}
- Witte D, Dundes L. Harnessing life energy or wishful thinking?. Alternative and Complementary Therapy 2001;10:304‐9. [Google Scholar]
References to studies awaiting assessment
Fox 2005 {published data only}
- Fox J. Reiki energy healing on prostrate cancer. http://clinicaltrials.gov/ct2/show/NCT00065208 (accessed 4 November 2014).
Frost 2007 {published data only}
- Frost T. A randomised controlled pilot study to assess the benefit of using Reiki to treat chronic plaque psoriasis RAP. http://www.controlled‐trials.com/ISRCTN63003238 (accessed 4 November 2014).
Mauro 2001 {published data only}
- Mauro M. The Effects of Reiki Therapy on Maternal Anxiety Associated with Amniocentesis [masters thesis]. Edmonton, AB: Department of Nursing, University of Alberta, 2001. [Google Scholar]
Stevens 1998 {published data only}
- Stevens M. Effects of Reiki on painful neuropathy and cardiovascular risk factors. http://clinicaltrials.gov/ct2/show/NCT00010751 (accessed 4 November 2014).
References to ongoing studies
NCT01569269 {published data only}
- NCT01569269. Effects of Reiki, Yoga, Meditation, on the Physical and Psychological Symptoms of Chemotherapy‐Induced Peripheral Neuropathy. https://clinicaltrials.gov/show/NCT01569269 (accessed 19 January 2015).
Additional references
Alderson 2004
- Alderson P, Green S, Higgins JPT (editors). Cochrane Reviewers' Handbook 4.2.2. [updated March 2004]. Cochrane Collaboration, 2004. [Google Scholar]
Andrews 1998
- Andrews G. The burden of anxiety and depressive disorders. Current Opinion in Psychiatry 1998;11:121‐3. [Google Scholar]
APA 1980
- American Psychiatric Association. [American Psychiatric Association]. Diagnostic and Statistical Manual of Mental Disorders (DSM‐III). 3rd Edition. Washington, DC: American Psychiatric Association, 1980. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV). 4th Edition. Washington: American Psychiatric Association, 1994. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM‐IV‐TR. Washington, DC, USA: American Psychiatric Association, 2000. [Google Scholar]
Arroll 2009
- Arroll B, Elley CR, Fishman T, Goodyear‐Smith FA, Kenealy T, Blashki G, Kerse N, MacGillivray S. Antidepressants versus placebo for depression in primary care. Cochrane Database of Systematic Reviews 2009, Issue 3, Art. No.: CD007954. [DOI: 10.1002/14651858.CD007954] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bahadur 1978
- Bahadur KP. The wisdom of Saankhya. New Delhi: Sterling Publishers PVT Ltd, 1978. [Google Scholar]
Baldwin 2010
- Baldwin L, Vitale A, Brownell E, Scicinski J, Kearns M, Rand W. The Touchstone Process: An Ongoing Critical Evaluation of Reiki in the Scientific Literature. Holistic Nursing Practice 2010;24(5):260‐76. [DOI] [PubMed] [Google Scholar]
Barnes 2007
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. CDC National Health Statistics Report #12, 2008. [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Medelson M, Mock J, Erbaugh J. An Inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Berger 2013
- Berger L, Tavares M, Berger B. A Canadian experience of integrating complementary therapy in a hospital palliative care unit. Journal of Palliative Medicine 2013;16(10):1294‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohm 1994
- Bohm D. Thought as a system. Routledge, 1994. [Google Scholar]
Capra 2000
- Capra F. The Tao of Physics. 4th Edition. Berkeley, California, USA: Shambhala Publications, 2000. [Google Scholar]
Carrol 2012
- Carrol S. The particle at the end of the universe: How the hunt for the Higgs Boson leads us to the edge of a new world. Penguin Group (USA), 2012. [Google Scholar]
Chandra 1991
- Chandra R. The complete works of Ram Chandra. Vol. 111, Kolkata, India: Spiritual Hierarchy Publication Trust, 1991. [Google Scholar]
Chaoul 2010
- Chaoul MA, Cohen L. Rethinking Yoga and the application of Yoga in modern medicine. Crosscurrents 2010;60(2):144‐167. [Google Scholar]
Dasgupta 1989
- Dasgupta S. A study of Patanjali. New Dehli: India Council for Philosophical Research, 1989. [Google Scholar]
Depping 2010
- Depping AM, Komossa K, Kissling W, Leucht S. Second‐generation antipsychotics for anxiety disorders. Cochrane Database of Systematic Reviews 2010, Issue 12. [DOI: 10.1002/14651858.CD008120] [DOI] [PubMed] [Google Scholar]
Feuerstein 2002
- Feuerstein G. The Yoga tradition ‐ Its history, literature, philosophy and practice. Bhavana Books and Prints, 2002. [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurosurgery and Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, Available from www.cochrane‐handbook.org, 2011. [Google Scholar]
Ho 2007
- Ho DYC, Ho RTH. Measuring spirituality and spiritual emptiness: towards ecumenicity and transcultural applicability. Review of General Psychology 2007;11(1):62‐74. [Google Scholar]
Hossi 2006
- Hossu M, Rupert R. Quantum events of biophoton emission associated with complementary and alternative therapies: A descriptive pilot study. The Journal of Alternative and Complementary Medicine 2006;12(2):119‐24. [DOI] [PubMed] [Google Scholar]
Jain 2010
- Jain S, Mills PJ. Biofield therapies: Helpful or full of hype? A best evidence synthesis. International Journal of Behavioural Medicine 2010;17:1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kessler 2001
- Kessler RC, Soukup J, Davis RB, Foster DF, Wilkey SA, Rompay MI, Eisenberg DM. The use of complementary and alternative therapies to treat anxiety and depression in the United States. American Journal of Psychiatry 2001;158(2):289‐94. [DOI] [PubMed] [Google Scholar]
Kumar 2003
- Kumar R, Kurup P. Changes in the isoprenoid pathway with transcendental meditation and Reiki healing practices in seizure disorder. Neurology of India 2003;51(2):10‐28. [PubMed] [Google Scholar]
Kumar 2008
- Kumar A. Super Science of Yoga. New Delhi, India: Standard Publishers, 2008. [Google Scholar]
Lee 2008
- Lee MS, Pittler MH, Ernst E. Effects of Reiki in clinical practice: a systematic review of randomised clinical trials. International Journal of Clinical Practice 2008;62(6):947‐54. [DOI] [PubMed] [Google Scholar]
Lubeck 2001
- Lubeck W, Petter FA, Rand WL. The Spirit of Reiki. Lotus Press, April 23, 2001. [Google Scholar]
Mackay 2004
- Mackay N, Hansen S, McFarlane O. Autonomic nervous system changes during Reiki treatment: A preliminary study. The Journal of Alternative and Complementary Medicine 2004;10(6):1077‐81. [DOI] [PubMed] [Google Scholar]
McKenzie 1998
- McKenzie E. Healing Reiki (Hamlyn Health & Well Being). Hamlyn, 1998. [ISBN 0‐600‐60818‐2] [Google Scholar]
Nield‐Anderson 2000
- Nield‐Anderson L, Ameling A. The empowering nature of Reiki as a complementary therapy. Holistic Nursing Practise 2000;14(3):21‐9. [DOI] [PubMed] [Google Scholar]
Olsen 2003
- Olsen K, Hanson J, Michaud M. A phase II trial of Reiki for the management of pain in advanced cancer patients. Journal of Pain and Symptom Management 2003;26(5):990‐7. [DOI] [PubMed] [Google Scholar]
Potter 2003
- Potter P. What are the distinctions between Reiki and Therapeutic Touch?. Clinical Journal of Oncology Nursing 2003;7(1):1‐3. [DOI] [PubMed] [Google Scholar]
Prins 2008
- Prins MA, Verhaak PF, Bensing JM, Meer K. Health beliefs and perceived need for mental health care of anxiety and depression‐‐the patients' perspective explored. Clinical Psychology Review 2008;28(6):1038–58. [DOI] [PubMed] [Google Scholar]
Rand 2014
- Rand WL. Reiki in hospitals. http://www.reiki.org/healing/reiki_in_hospitalsold.html (accessed 26 April 2014).
Rein 2004
- Rein G. Bioinformation within the biofield: Beyond bioelectromagnetics. The Journal of Alternative and Complementary Medicine 2004;10(1):59‐68. [DOI] [PubMed] [Google Scholar]
Robinson 2007
- Robinson J, Biley FC, Dolk H. Therapeutic touch for anxiety disorders. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD006240.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosa 1998
- Rosa L, Rosa E, Sarner L, Barrett S. A close look at therapeutic touch. JAMA 1998;279(13):1005‐10. [DOI] [PubMed] [Google Scholar]
Rowney 2014
- Rowney J, Hermida T, Malone D. Anxiety Disorders. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/psychiatry‐psychology/anxiety‐disorder/ Accessed 25 April 2014.
Rubik 2002
- Rubik B. The biofield hypothesis: its biophysical basis and role in medicine. The Journal of Alternative and Complementary Medicine 2002;8(6):703‐17. [DOI] [PubMed] [Google Scholar]
Sedlmeier 2012
- Sedlmeier P, Eberth J, Schwarz M, Zimmermann D, Haarig F, Jaeger S, et al. The psychological effects of meditation: a meta‐analysis. Psychological Bulletin 2012;138(6):1139‐71. [DOI: 10.1037/a0028168] [DOI] [PubMed] [Google Scholar]
Spielberger 1983
- Spielberger CD. Manual for the State‐Trait Anxiety Inventory (Form Y). Palo Alto, CA: Consulting Psychologists Press, 1983. [Google Scholar]
Trepper 2013
- Trepper TS, Strozier A, Carpenter JE, Hecker LL. Introduction to Alternative and Complementary Therapies. Taylor and Francis, 2013. [Google Scholar]
vanderVaart 2009
- vanderVaart S, Gijsen VMGJ, Wildt SN, Koren G. A systematic review of the therapeutic effects of Reiki. The Journal of Alternative and Complementary Medicine 2009;15(11):1157‐69. [DOI] [PubMed] [Google Scholar]
Vitale 2007
- Vitale A. An integrative review of Reiki touch therapy research. Holistic Nursing Practice 2007;21(4):167‐79. [DOI] [PubMed] [Google Scholar]
Wardell 2004
- Wardell D, Weymouth K. Review of studies on Healing Touch. Journal of Nursing Scholarship 2004;36(2):147‐54. [DOI] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski, Gandek B. SF‐36 Health Survey: Manual and 1993 Interpretation Guide. Boston, MA: New England Medical Center, Health Institute, 1993. [Google Scholar]
WHO 1978
- World Health Organization. The Ninth Revision of the International Classification of Diseases and Related Health Problems (ICD‐9). Geneva: World Health Organization, 1978. [Google Scholar]
WHO 1992
- World Health Organization. The ICD‐10 Classification of Mental and Behavior Disorders. 10th Edition. Geneva: World Health Organization, 1992. [Google Scholar]
Yeh 2004
- Yeh CJ, Hunter CD, Madan‐Bahel A, Chiang L, Arora AK. Indigenous and Interdependent Perspectives of Healing: Implications for Counseling and Research. Journal of Counseling & Development 2004;82(4):410‐19. [Google Scholar]


