Abstract
Background.
Mortality associated with hepatitis C virus (HCV) has been well-documented nationally, but an examination across regions and jurisdictions may inform health-care planning.
Methods.
To document HCV-associated deaths sub-nationally, we calculated age-adjusted, HCV-associated death rates and compared death rate ratios (DRRs) for 10 US regions, 50 states, and Washington, D.C., using the national rate and described rate changes between 2016 and 2017 to determine variability. We examined the mean age at HCV-associated death, and rates and proportions by sex, race/ethnicity, and birth year.
Results.
In 2017, there were 17 253 HCV-associated deaths, representing 4.13 (95% confidence interval [CI], 4.07–4.20) deaths/100 000 standard population, in a significant, 6.56% rate decline from 4.42 in 2016. Age-adjusted death rates significantly surpassed the US rate for the following jurisdictions: Oklahoma; Washington, D.C.; Oregon; New Mexico; Louisiana; Texas; Colorado; California; Kentucky; Tennessee; Arizona; and Washington (DRRs, 2.87, 2.77, 2.24, 1.62, 1.57, 1.46, 1.36, 1.35, 1.35, 1.35, 1.32, and 1.32, respectively; P < .05). Death rates ranged from a low of 1.60 (95% CI, 1.07–2.29) in Maine to a high of 11.84 (95% CI, 10.82–12.85) in Oklahoma. Death rates were highest among non-Hispanic (non-H) American Indians/Alaska Natives and non-H Blacks, both nationally and regionally. The mean age at death was 61.4 years (range, 56.6 years in West Virginia to 64.1 years in Washington, D.C.), and 78.6% of those who died were born during 1945–1965.
Conclusions.
In 2016–2017, the national HCV-associated mortality declined but rates remained high in the Western and Southern regions and Washington, D.C., and among non-H American Indians/Alaska Natives, non-H Blacks, and Baby Boomers. These data can inform local prevention and control programs to reduce the HCV mortality burden.
Keywords: hepatitis C, deaths, mortality, jurisdiction, region
Hepatitis C virus (HCV) infection is a leading cause of liver-related morbidity and mortality in the United States [1–3]. In December 2013, all-oral direct-acting antiviral (DAA) therapies were licensed for chronic HCV infection curative treatment [4]. Trend analyses of US multiple cause-of-death (MCOD) data revealed that in 2012 and 2013, HCV-associated deaths exceeded deaths associated with 60 other infectious conditions that were nationally notifiable in 2013 [5]. From 2013–2016, a decline of 11.5% was observed in the HCV-associated death rate, with the majority of the decline occurring from 2015–2016 [6]. Planning for health systems also occurs sub-nationally, as variability in morbidity and mortality is evident across jurisdictions [7]. Efforts to eliminate HCV infection hinge on understanding these variabilities to inform local planning.
With changing HCV-associated death rate trends [5], it is imperative to examine the distribution of mortality at a finer geographic level to understand the health burden associated with HCV infection and mitigate that burden, particularly in jurisdictions with greater or increasing HCV-associated death rates. In 2017, the National Academies of Sciences, Engineering, and Medicine presented a strategy for eliminating HCV infection as a public health threat in the United States. The strategy indicated that aggressive case-finding and treating everyone with chronic HCV infection would reduce new US infections by 90% and deaths by 65% by 2030 [8]. In addition, the number of HCV infections has been growing among young adults, related to increases in injection drug use [6]. Death certificates provide data to track progress towards HCV treatment, and subsequently, elimination goals.
Using the most recent US death certificate data from 2017, the study objectives were to compare HCV-associated death rates and counts nationally and across 10 regions, 50 states, and Washington, D.C.; to describe the epidemiology of these deaths by examining demographic characteristics; and to assess whether death rate declines seen between 2015 and 2016 continued through 2017.
MATERIALS AND METHODS
Data Source
This study used 2016 and 2017 MCOD data files. The analysis made use of outputs from the “Multiple cause-of-death (Detailed Mortality)” module from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research [9] and microdata mortality files from the National Vital Statistics System. This study abstracted age, race/ethnicity, and sex as reported on the death certificate.
The death certificate is based on the US Standard Certificate of Death [10]. In 2016 and 2017, all jurisdictions used the latest 2003 revision [10], with the exception of West Virginia [11], which used the 1989 revision until August 2017 [12]. The main difference between the 2 revisions pertained to the ability to select more than 1 race in the 2003 revision, to align jurisdiction’s certificates with the Census decennial forms. Since West Virginia had not adopted the latest revision for most of this period, MCOD data files contained a race variable that bridged the races of multiple-race decedents to a single race, to make the 2 revisions comparable.
Case Definitions
State and Region of Decedent’s Residence
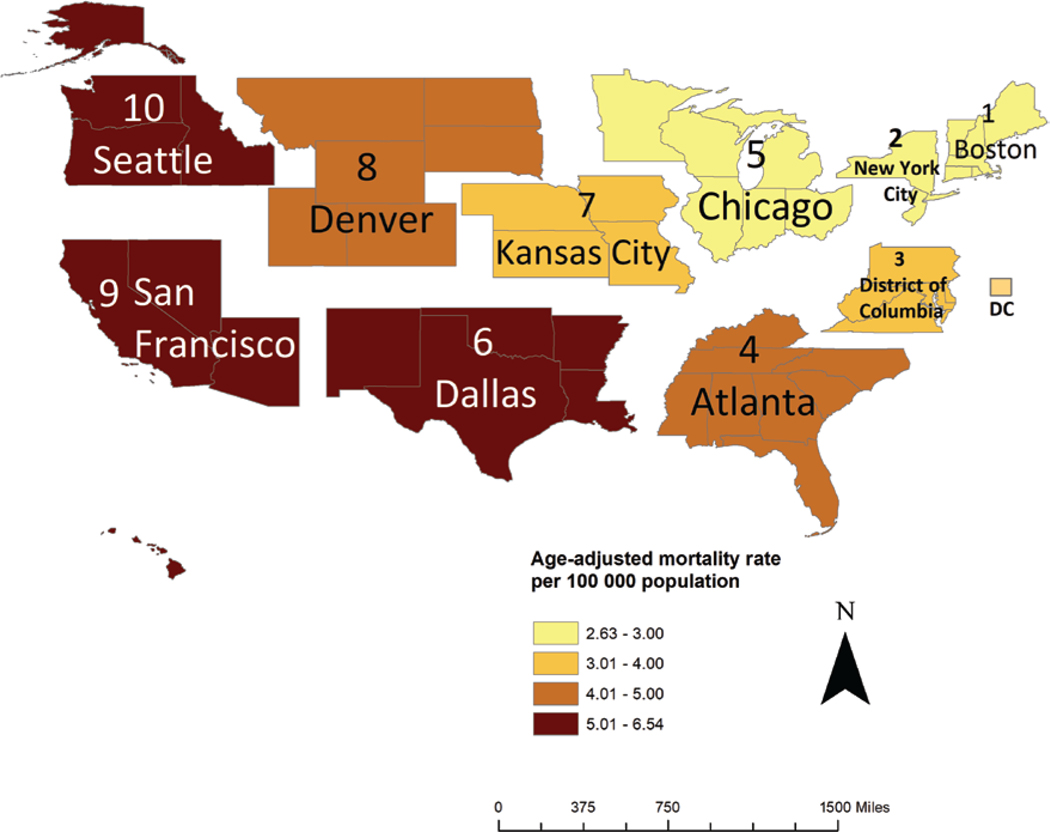
The variable “state of residence” (including Washington, D.C.) was examined, from which region- and jurisdiction-specific death rates were derived. Decedents whose place of residence was outside of the United States, including any of the US territories, were excluded. The region of a decedent’s residence was categorized according to the grouping of jurisdictions assigned under the 10 US Department of Health and Human Services (DHHS) regional offices that serve state and local organizations [13]. The 10 regional headquarters are Region 1: Boston; Region 2: New York City; Region 3: Philadelphia; Region 4: Atlanta; Region 5: Chicago; Region 6: Dallas; Region 7: Kansas City; Region 8: Denver; Region 9: San Francisco; and Region 10: Seattle.
Deaths Associated With Hepatitis C Virus
We used the International Classification of Diseases, Tenth Revision [14], cause-of-death codes B17.1 and B18.2, listed as any multiple causes of death, to identify HCV-associated deaths. The decision to use multiple causes of death, as opposed to the underlying cause of death, was based on the need to characterize all HCV-associated deaths, because HCV infection is often listed as a non-underlying cause of death [1].
Statistical Analyses
Death rates were calculated by dividing the number of HCV-associated deaths by the census population [15], and were adjusted to the age distribution of the 2000 US standard population using the direct method [16]. We calculated 95% confidence intervals (CIs) using 2 methods, based on the number of deaths for each category [17–19]. As a supplementary analysis, we examined the top 20 underlying causes of death where HCV infection was listed as a nonunderlying cause of death.
Relative comparisons of death rate ratios (DRRs) were calculated to compare age-adjusted, HCV-associated death rates in regions and jurisdictions with that of the United States as a whole, denoted by . The percent change in death rates from 2016 to 2017 was calculated using the following formula: . Z-score P values for DRRs, percent changes in rates from 2016 to 2017, and death rates by demographic characteristics for each region, compared to the United States as a whole, were examined to determine whether changes were significant, where P < .05 was considered statistically significant.
To increase the number of sufficient cell sizes, we aggregated 2016 and 2017 data to produce jurisdiction-level fractions for demographic characteristics. To adhere to the National Center for Health Statistics’ policy concerning small cell sizes, cells where values were ≤10 deaths were not presented. Interpreted differences for death rates across groups and time were statistically significant. We did not interpret proportions counts were less than or equal to 15, because of the instability associated with these fractions. Statistical analyses were conducted using SAS software, version 9.4 (Cary, NC). Aeronautical Reconnaissance Coverage Geographic Information System (Environmental Systems Research Institute, version 10.3. Redlands, CA) was employed to generate gradient color-coded death rates and count maps.
RESULTS
National, Regional, and Jurisdiction-level Mortality Rates Associated With Hepatitis C Virus
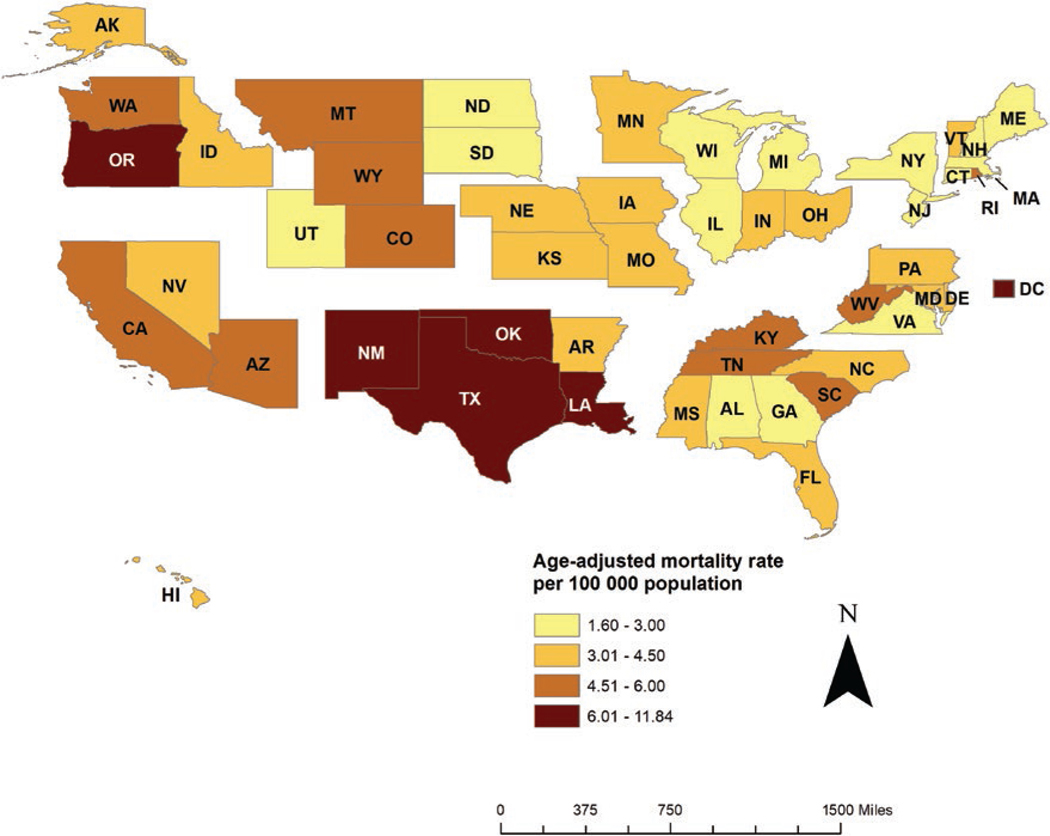
In 2017, there were 17 253 HCV-associated deaths among 325.7 million US residents and 2.8 million total deaths, representing an age-adjusted, HCV-associated death rate of 4.13 (95% CI, 4.07–4.20) deaths/100 000 standard population (Table 1). Of HCV-associated deaths, 4921 (28.5%) listed HCV infection as the underlying cause of death. Among the remaining 12 332 deaths where HCV infection was listed as a nonunderlying cause of death, the top 3 underlying causes of death were liver cell carcinoma (21.2%), alcoholic cirrhosis of the liver (9.8%), and unspecified malignant neoplasm of the liver (5.9%; Supplementary Table 1). Of 10 geographical regions, 3 had death rates that significantly surpassed the overall US rate: Region 6 (6.54), Region 10 (6.38), and Region 9 (5.37; Figure 1; Table 1). Death rates were significantly higher than the US death rate in Oklahoma; Washington, D.C.; Oregon; New Mexico; Louisiana; Texas; Colorado; California; Kentucky; Tennessee; Arizona; and Washington (P < .05; Table 1; Figure 2).
Table 1.
Death Counts and Rates Associated With Hepatitis C Virus Infection
| Jurisdiction | 2016 |
2017 |
2016–2017 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Count | Rate (95% CI)a | Count | Rate (95% CI)a | DRR (95% CI)b | P-Valuec | Mean Age at Death | % Change in Rate | P Valued | |
| United States | 18 093 | 4.42 (4.36–4.49) | 17 253 | 4.13 (4.07–4.20) | Reference | 61.4 | −6.56 | .00 | |
| Region 1: Boston | 616 | 3.10 (2.85–3.35) | 602 | 2.97 (2.72–3.21) | .72 (.66–.78) | .00 | 60.8 | −4.19 | .47 |
| Connecticut | 123 | 2.52 (2.06–2.97) | 130 | 2.61 (2.15–3.07) | .63 (.52–.74) | .00 | 61.1 | 3.57 | .79 |
| Maine | 40 | 1.87 (1.32–2.56) | 32 | 1.60 (1.07–2.29) | .39 (.25–.53) | .00 | 61.4 | −14.44 | .52 |
| Massachusetts | 261 | 2.98 (2.61–3.35) | 267 | 3.00 (2.63–3.37) | .73 (.64–.82) | .00 | 61.0 | .67 | .94 |
| New Hampshire | 68 | 3.57 (2.73–4.58) | 57 | 2.90 (2.16–3.80) | .70 (.52–.88) | .00 | 60.2 | −18.77 | .27 |
| Rhode Island | 89 | 6.57 (5.24–8.15) | 76 | 5.15 (4.02–6.50) | 1.25 (.97–1.53) | .08 | 59.2 | −21.61 | .13 |
| Vermont | 35 | 3.72 (2.56–5.22) | 40 | 4.44 (3.11–6.15) | 1.07 (.74–1.40) | .68 | 59.7 | 19.35 | .47 |
| Region 2: New York | 1167 | 3.12 (2.94–3.30) | 1043 | 2.76 (2.59–2.93) | .67 (.63–.71) | .00 | 63.6 | −11.54 | .00 |
| New Jersey | 378 | 3.24 (2.90–3.57) | 342 | 2.90 (2.58–3.21) | .70 (.63–.77) | .00 | 62.0 | −10.49 | .14 |
| New York | 789 | 3.06 (2.84–3.27) | 701 | 2.71 (2.50–2.91) | .66 (.61–.71) | .00 | 63.6 | −11.44 | .02 |
| Region 3: Philadelphia | 1478 | 3.68 (3.48–3.87) | 1441 | 3.53 (3.35–3.72) | .86 (.81–.91) | .00 | 61.0 | −4.08 | .27 |
| Delaware | 47 | 3.63 (2.65–4.85) | 49 | 3.80 (2.77–5.08) | .92 (.66–1.18) | .54 | 61.3 | 4.68 | .83 |
| District of Columbia | 95 | 13.37 (10.78–16.40) | 83 | 11.42 (9.09–14.18) | 2.77 (2.17–3.37) | .00 | 64.1 | −14.58 | .30 |
| Maryland | 327 | 4.32 (3.84–4.80) | 340 | 4.41 (3.93–4.89) | 1.07 (.96–1.18) | .23 | 60.8 | 2.08 | .79 |
| Pennsylvania | 564 | 3.28 (3.00–3.56) | 563 | 3.15 (2.88–3.42) | .76 (.70–.82) | .00 | 61.0 | −3.96 | .51 |
| Virginia | 327 | 3.03 (2.70–3.36) | 290 | 2.68 (2.36–2.99) | .65 (.57–.73) | .00 | 59.6 | −11.55 | .14 |
| West Virginia | 118 | 4.85 (3.93–5.76) | 116 | 4.94 (4.00–5.88) | 1.20 (.98–1.42) | .07 | 56.6 | 1.86 | .89 |
| Region 4: Atlanta | 3500 | 4.18 (4.03–4.32) | 3450 | 4.03 (3.89–4.16) | .97 (.93–1.01) | .10 | 60.2 | −3.59 | .14 |
| Alabama | 166 | 2.63 (2.22–3.05) | 188 | 2.97 (2.53–3.41) | .72 (.62–.82) | .00 | 60.9 | 12.93 | .27 |
| Florida | 1222 | 4.26 (4.01–4.50) | 1222 | 4.16 (3.92–4.40) | 1.01 (.95–1.07) | .74 | 61.7 | −2.35 | .57 |
| Georgia | 368 | 2.98 (2.67–3.29) | 344 | 2.66 (2.37–2.94) | .64 (.57–.71) | .00 | 61.0 | −10.74 | .14 |
| Kentucky | 269 | 5.05 (4.42–5.67) | 306 | 5.58 (4.94–6.23) | 1.35 (1.20–1.50) | .00 | 57.4 | 10.50 | .25 |
| Mississippi | 183 | 5.08 (4.33–5.84) | 159 | 4.38 (3.68–5.08) | 1.06 (.89–1.23) | .48 | 59.0 | −13.78 | .18 |
| North Carolina | 511 | 3.92 (3.57–4.26) | 460 | 3.44 (3.12–3.76) | .83 (.75–.91) | .00 | 59.6 | −12.24 | .05 |
| South Carolina | 299 | 4.51 (3.98–5.03) | 302 | 4.51 (3.98–5.03) | 1.09 (.97–1.21) | .15 | 60.3 | .00 | 1.00 |
| Tennessee | 482 | 5.89 (5.35–6.43) | 469 | 5.57 (5.05–6.09) | 1.35 (1.23–1.47) | .00 | 58.5 | −5.43 | .40 |
| Region 5: Chicago | 2064 | 3.01 (2.88–3.15) | 1846 | 2.63 (2.51–2.75) | .64 (.61–.67) | .00 | 61.5 | −12.62 | .00 |
| Illinois | 354 | 2.18 (1.95–2.41) | 288 | 1.72 (1.52–1.92) | .42 (.37–.47) | .00 | 62.7 | −21.10 | .00 |
| Indiana | 295 | 3.60 (3.18–4.02) | 269 | 3.16 (2.77–3.55) | .77 (.68–.86) | .00 | 60.1 | −12.22 | .13 |
| Michigan | 415 | 3.06 (2.75–3.36) | 368 | 2.61 (2.34–2.88) | .63 (.56–.70) | .00 | 62.1 | −14.71 | .03 |
| Minnesota | 240 | 3.28 (2.86–3.71) | 235 | 3.19 (2.78–3.61) | .77 (.67–.87) | .00 | 61.3 | −2.74 | .77 |
| Ohio | 546 | 3.58 (3.27–3.89) | 541 | 3.48 (3.17–3.78) | .84 (.77–.91) | .00 | 59.7 | −2.79 | .65 |
| Wisconsin | 214 | 2.70 (2.33–3.07) | 145 | 1.82 (1.52–2.12) | .44 (.37–.51) | .00 | 61.1 | −32.59 | .00 |
| Region 6: Dallas | 3194 | 6.69 (6.45–6.92) | 3169 | 6.54 (6.31–6.77) | 1.58 (1.52–1.64) | .00 | 60.6 | −2.24 | .37 |
| Arkansas | 184 | 4.91 (4.18–5.64) | 169 | 4.43 (3.74–5.11) | 1.07 (.91–1.23) | .40 | 59.9 | −9.78 | .35 |
| Louisiana | 383 | 6.60 (5.92–7.28) | 382 | 6.49 (5.82–7.16) | 1.57 (1.41–1.73) | .00 | 60.5 | −1.67 | .82 |
| New Mexico | 203 | 8.12 (6.96–9.28) | 175 | 6.70 (5.66–7.73) | 1.62 (1.38–1.86) | .00 | 59.1 | −17.49 | .07 |
| Oklahoma | 538 | 11.46 (10.47–12.46) | 555 | 11.84 (10.82–12.85) | 2.87 (2.63–3.11) | .00 | 59.4 | 3.32 | .60 |
| Texas | 1886 | 6.12 (5.84–6.40) | 1888 | 6.03 (5.76–6.31) | 1.46 (1.39–1.53) | .00 | 60.6 | −1.47 | .65 |
| Region 7: Kansas City | 593 | 3.31 (3.04–3.59) | 589 | 3.24 (2.97–3.51) | .78 (.72–.84) | .00 | 60.5 | −2.11 | .72 |
| Iowa | 109 | 2.67 (2.16–3.19) | 122 | 3.01 (2.46–3.56) | .73 (.60–.86) | .00 | 59.9 | 12.73 | .38 |
| Kansas | 148 | 4.20 (3.51–4.90) | 141 | 3.83 (3.18–4.48) | .93 (.78–1.08) | .37 | 59.3 | −8.81 | .45 |
| Missouri | 258 | 3.23 (2.82–3.63) | 247 | 3.06 (2.67–3.45) | .74 (.65–.83) | .00 | 60.5 | −5.26 | .55 |
| Nebraska | 78 | 3.25 (2.56–4.08) | 79 | 3.29 (2.59–4.13) | .80 (.62–.98) | .03 | 60.9 | 1.23 | .94 |
| Region 8: Denver | 640 | 4.69 (4.32–5.06) | 615 | 4.38 (4.02–4.73) | 1.06 (.97–1.15) | .17 | 61.2 | −6.61 | .24 |
| Colorado | 385 | 5.74 (5.16–6.33) | 386 | 5.62 (5.05–6.20) | 1.36 (1.22–1.50) | .00 | 61.4 | −2.09 | .77 |
| Montana | 75 | 5.71 (4.43–7.25) | 68 | 4.89 (3.73–6.29) | 1.18 (.90–1.46) | .21 | 58.7 | −14.36 | .38 |
| North Dakota | 20 | 2.25 (1.36–3.52) | 23 | 2.88 (1.78–4.40) | .70 (.41–.99) | .04 | 60.3 | 28.00 | .44 |
| South Dakota | 37 | 3.46 (2.41–4.81) | 29 | 2.56 (1.69–3.73) | .62 (.39–.85) | .00 | 60.1 | −26.01 | .24 |
| Utah | 85 | 2.98 (2.37–3.70) | 68 | 2.29 (1.77–2.92) | .56 (.43–.69) | .00 | 60.7 | −23.15 | .11 |
| Wyoming | 38 | 4.89 (3.43–6.77) | 41 | 5.50 (3.89–7.55) | 1.33 (.92–1.74) | .11 | 59.4 | 12.47 | .62 |
| Region 9: San Francisco | 3668 | 6.08 (5.88–6.28) | 3330 | 5.37 (5.19–5.56) | 1.30 (1.25–1.35) | .00 | 62.9 | −11.68 | .00 |
| Arizona | 500 | 5.81 (5.29–6.33) | 480 | 5.45 (4.95–5.95) | 1.32 (1.20–1.44) | .00 | 61.1 | −6.20 | .33 |
| California | 2917 | 6.33 (6.09–6.56) | 2630 | 5.58 (5.36–5.80) | 1.35 (1.29–1.41) | .00 | 62.8 | −11.85 | .00 |
| Hawaii | 70 | 3.75 (2.90–4.77) | 67 | 3.48 (2.68–4.44) | .84 (.64–1.04) | .12 | 63.7 | −7.20 | .67 |
| Nevada | 181 | 4.97 (4.23–5.70) | 153 | 4.00 (3.35–4.64) | .97 (.82–1.12) | .70 | 62.1 | −19.52 | .05 |
| Region 10: Seattle | 1173 | 6.56 (6.17–6.94) | 1168 | 6.38 (6.01–6.76) | 1.55 (1.46–1.64) | .00 | 62.0 | −2.74 | .51 |
| Alaska | 50 | 5.38 (3.95–7.15) | 38 | 4.38 (3.05–6.09) | 1.06 (.72–1.40) | .73 | 60.6 | −18.59 | .35 |
| Idaho | 115 | 5.40 (4.39–6.41) | 84 | 3.82 (3.03–4.75) | .92 (.72–1.12) | .43 | 61.5 | −29.26 | .02 |
| Oregon | 491 | 8.90 (8.09–9.70) | 518 | 9.24 (8.42–10.05) | 2.24 (2.04–2.44) | .00 | 61.6 | 3.82 | .56 |
| Washington | 517 | 5.53 (5.04–6.01) | 528 | 5.46 (4.99–5.94) | 1.32 (1.21–1.43) | .00 | 61.9 | −1.27 | .84 |
Data are shown by residence in the US states and the District of Columbia, sectioned by DHHS regions, 2016–2017. The region of a decedent’s residence was categorized according to the grouping of states assigned under each of the 10 DHHS regional offices that serve state and local organizations. Data Source: 2016 and 2017 US multiple cause-of-death data, National Vital Statistics System.
Abbreviations: CI, confidence interval; DHHS, US Department of Health and Human Services; DRR, death rate ratio; HCV, hepatitis C virus.
Death rates are per 100 000 population and adjusted to the age distribution of the 2000 US standard population.
DRRs were calculated to compare age-adjusted, HCV-associated death rates in DHHS regions and jurisdictions with the age-adjusted, HCV-associated death rate in US residents, denoted by .
Test to determine whether differences in age-adjusted, HCV-associated death rates in DHHS regions and jurisdictions were statistically significantly different from the age-adjusted, HCV-associated death rates among US residents, where a Z-score P value that was less than .05 was considered statistically significant.
Test to determine whether differences in age-adjusted, HCV-associated death rates in 2017 were statistically significantly different from the age-adjusted, HCV-associated death rates in 2016, where a Z-score P value that was less than .05 was considered statistically significant.
Figure 1.
Age-adjusted death rates associated with hepatitis C virus infection in the United States, by DHHS region of residence in the United States, 2017. Rates are per 100 000 population and adjusted to the age distribution of the 2000 US standard population. The region of a decedent’s residence was categorized according to the grouping of states assigned under each of the 10 US DHHS regional offices that serve state and local organizations. The map is segmented by the 10 DHHS regions and labeled accordingly. Data Source: 2017 US multiple cause-of-death data, National Vital Statistics System. Abbreviations: DC, Washington, D.C.; DHHS, Department of Health and Human Services;
Figure 2.
Age-adjusted death rates associated with hepatitis C virus infection in the United States, by state and District of Columbia, 2017. Rates are per 100 000 population and are adjusted to the age distribution of the 2000 US standard population. Data Source: 2017 US multiple cause-of-death data, National Vital Statistics System. Abbreviations: AK, Alaska; AR, Arkansas; AL, Alabama; AZ, Arizona; CA, California; CO, Colorado; CT, Connecticut; DC, Washington, D.C.; DE, Delaware; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming.
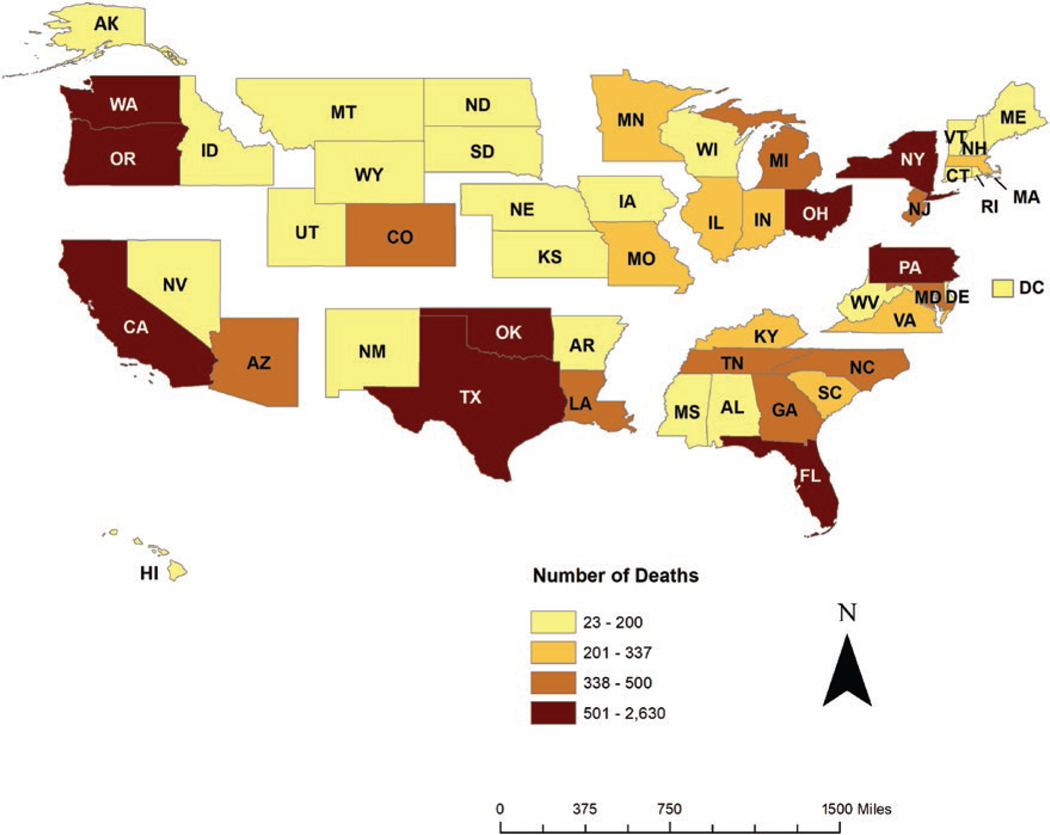
HCV-associated death counts in 18 jurisdictions surpassed the average number of deaths for all jurisdictions (n = 338 deaths). These jurisdictions were California, Texas, Florida, New York, Pennsylvania, Oklahoma, Ohio, Washington, Oregon, Arizona, Tennessee, North Carolina, Colorado, Louisiana, Michigan, Georgia, New Jersey, and Maryland. The sum of the deaths in these jurisdictions accounted for 73.7% of all HCV-associated deaths (Table 1; Figure 3).
Figure 3.
Number of deaths associated with hepatitis C virus infection in the United States, by state and District of Columbia, 2017. The lower end of the range of number of HCV-associated deaths in the third category level of 338 deaths was selected because it was the mean number of HCV-associated deaths among the 51 jurisdictions. Data Source: 2017 US multiple cause-of-death data, National Vital Statistics System Abbreviations: AK, Alaska; AR, Arkansas; AL, Alabama; AZ, Arizona; CA, California; CO, Colorado; CT, Connecticut; DC, Washington, D.C.; DE, Delaware; FL, Florida; GA, Georgia; HCV, hepatitis C virus; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming.
The lowest death rate was in Maine, with 1.60 deaths/100 000 standard population. Other jurisdictions with death rates ≤3.00 included Illinois, Wisconsin, Utah, South Dakota, Michigan, Connecticut, Georgia, Virginia, New York, North Dakota, New Hampshire, New Jersey, Alabama, and Massachusetts (Table 1; Figure 2).
Demographic Disparities
Mean Age and Year of Birth
The mean age at HCV-associated death in 2017 was 61.4 years, ranging in jurisdictions from 56.4 years in West Virginia to 64.7 years in Washington, D.C., and ranging more narrowly in regions, from 60.2 years in Region 4 to 63.6 years in Region 2 (Table 1).
Approximately three-fourths (78.6%) of US HCV-associated deaths were in people born during 1945–1965 (Table 2). The disparity observed at the national level occurred similarly in all regions, ranging from 75.6% in Region 2 to 82.2% in Region 10.
Table 2.
Percent Distribution and Death Rate Associated With Hepatitis C Virus Infection
| United States |
Region 1: Boston |
Region 2: New York |
Region 3: Philadelphia |
|||||
|---|---|---|---|---|---|---|---|---|
| Category | Rate (95% CI)a | %b | Rate (95% CI)a | %b | Rate (95% CI)a | %b | Rate (95% CI)a | %b |
| Overall | 4.13 (4.07–4.20) | ... | 2.97 (2.72–3.21) | ... | 2.76 (2.59–2.93) | ... | 3.53 (3.35–3.72) | ... |
| Sex | ||||||||
| Male | 6.12 (6.01–6.23) | 71.2 | 4.56 (4.12–5.00) | 73.3 | 4.11 (3.81–4.41) | 70.1 | 5.43 (5.10–5.76) | 74.7 |
| Female | 2.32 (2.26–2.39) | 28.8 | 1.55 (1.30–1.80) | 26.7 | 1.58 (1.40–1.76) | 29.9 | 1.82 (1.62–2.01) | 25.3 |
| Race/ethnicity | ||||||||
| Non-H White | 3.70 (3.63–3.78) | 63.0 | 2.52 (2.27–2.77) | 71.3 | 1.91 (1.73–2.09) | 46.3 | 2.82 (2.61–3.02) | 58.2 |
| Non-H Black | 7.03 (6.79–7.28) | 19.1 | 7.85 (6.18–9.82) | 13.3 | 5.73 (5.05–6.42) | 27.8 | 8.11 (7.40–8.82) | 36.6 |
| Hispanic | 5.29 (5.08–5.51) | 14.0 | 6.38 (4.99–8.05) | 12.9 | 4.92 (4.28–5.56) | 23.6 | 3.17 (2.31–4.26) | 3.4 |
| Non-H API | 1.86 (1.67–2.05) | 2.2 | 2.33 (1.20–4.07) | 2.2 | .80 (.50–1.23) | 2.2 | 1.54 (.91–2.43) | 1.4 |
| Non-H AIAN | 10.24 (9.04–11.44) | 1.7 | ... | ... | ... | ... | ... | ... |
| Year of birth | ||||||||
| Before 1945 | 6.52 (6.21–6.83) | 9.8 | 4.11 (3.00–5.21) | 8.8 | 6.75 (5.71–7.78) | 15.5 | 4.97 (4.11–5.83) | 9.0 |
| 1945–1965 | 16.90 (16.62–17.19) | 78.6 | 11.74 (10.68–12.81) | 77.9 | 10.88 (10.12–11.64) | 75.6 | 14.27 (13.44–15.10) | 79.0 |
| After 1965 | .91 (.87–.95) | 11.6 | .84 (.66–1.02) | 13.3 | .48 (.38–.58) | 8.8 | .86 (.73–.99) | 12.1 |
| Category | Region 4: Atlanta |
Region 5: Chicago |
Region 6: Dallas |
Region 7: Kansas City |
||||
| Rate (95% CI)a | %b | Rate (95% CI)a | %b | Rate (95% CI)a | %b | Rate (95% CI)a | %b | |
|
| ||||||||
| Overall | 4.03 (3.89–4.16) | ... | 2.63 (2.51–2.75) | ... | 6.54 (6.31–6.77) | ... | 3.24 (2.97–3.51) | … |
| Sex | ||||||||
| Male | 5.93 (5.69–6.17) | 71.0 | 3.85 (3.63–4.06) | 71.7 | 9.72 (9.32–10.13) | 72.0 | 4.68 (4.22–5.14) | 71.0 |
| Female | 2.32 (2.18–2.47) | 29.0 | 1.48 (1.34–1.61) | 28.3 | 3.59 (3.35–3.83) | 28.0 | 1.85 (1.56–2.13) | 29.0 |
| Race/ethnicity | ||||||||
| Non-H White | 4.35 (4.17–4.53) | 72.6 | 2.16 (2.04–2.29) | 67.3 | 6.23 (5.93–6.53) | 56.7 | 2.82 (2.55–3.09) | 76.4 |
| Non-H Black | 4.52 (4.18–4.86) | 20.9 | 7.13 (6.48–7.78) | 26.1 | 9.36 (8.58–10.15) | 18.5 | 8.78 (7.03–10.53) | 17.3 |
| Hispanic | 2.41 (2.05–2.78) | 5.0 | 2.44 (1.87–3.12) | 3.7 | 6.48 (5.97–6.98) | 21.1 | 3.29 (1.98–5.14) | 3.4 |
| Non-H API | 1.77 (1.15–2.62) | .8 | 1.66 (1.05–2.50) | 1.4 | 3.51 (2.53–4.74) | 1.5 | … | … |
| Non-H AIAN | 5.12 (3.03–8.09) | .6 | 8.83 (5.82–12.85) | 1.5 | 9.31 (7.20–11.84) | 2.2 | … | … |
| Year of birth | ||||||||
| Before 1945 | 4.62 (4.06–5.18) | 7.6 | 3.52 (2.96–4.08) | 8.2 | 9.86 (8.70–11.03) | 8.7 | 3.62 (2.54–4.70) | 7.3 |
| 1945–1965 | 16.18 (15.57–16.78) | 78.7 | 11.32 (10.75–11.89) | 82.2 | 26.36 (25.32–27.40) | 77.9 | 13.67 (12.45–14.90) | 81.3 |
| Category | Region 8: Denver |
Region 9: San Francisco |
Region 10: Seattle |
|||||
| Rate (95% CI)a | %b | Rate (95% CI)a | %b | Rate (95% CI)a | %b | |||
|
| ||||||||
| Overall | 4.38 (4.02–4.73) | ... | 5.37 (5.19–5.56) | ... | 6.38 (6.01–6.76) | ... | ||
| Sex | ||||||||
| Male | 5.75 (5.17–6.32) | 65.5 | 7.86 (7.54–8.19) | 70.2 | 9.20 (8.56–9.84) | 70.7 | ||
| Female | 3.02 (2.60–3.44) | 34.5 | 3.08 (2.88–3.27) | 29.8 | 3.69 (3.29–4.10) | 29.3 | ||
| Race/ethnicity | ||||||||
| Non-H White | 3.30 (2.97–3.64) | 65.1 | 5.14 (4.89–5.39) | 52.4 | 6.31 (5.90–6.72) | 83.2 | ||
| Non-H Black | 18.75 (13.83–24.86) | 8.7 | 11.16 (10.01–12.30) | 11.6 | 15.68 (11.91–20.27) | 5.3 | ||
| Hispanic | 8.49 (6.82–10.15) | 17.5 | 6.57 (6.14–7.01) | 28.6 | 6.04 (4.50–7.95) | 5.2 | ||
| Non-H API | 4.27 (2.05–7.86) | 1.8 | 1.82 (1.54–2.10) | 5.1 | 2.87 (1.89–4.17) | 2.4 | ||
| Non-H AIAN | 17.33 (12.44–23.52) | 6.9 | 13.43 (10.52–16.88) | 2.3 | 14.31 (10.31–19.34) | 3.9 | ||
| Year of birth | ||||||||
| Before 1945 | 6.25 (4.52–7.98) | 8.1 | 12.34 (11.22–13.46) | 14.0 | 9.00 (7.18–10.81) | 8.0 | ||
| 1945–1965 | 17.78 (16.20–19.37) | 78.7 | 21.63 (20.79–22.47) | 76.7 | 27.50 (25.76–29.24) | 81.8 | ||
| After 1965 | .96 (.75–1.17) | 13.2 | .87 (.78–.97) | 9.3 | 1.25 (1.03–1.48) | 10.2 | ||
Data are shown by DHHS Region of Residence, United States, 2017. The region of a decedent’s residence was categorized according to the grouping of states assigned under each of the 10 US DHHS regional offices that serve state and local organizations. Data Source: 2017 US multiple cause-of-death data, National Vital Statistics System.
Abbreviations: AIAN, American Indian/Alaska Native; API, Asian/Pacific Islander; CI, confidence interval; DHHS, US Department of Health and Human Services; HCV, hepatitis C virus; NH, non-Hispanic.
Rates are per 100 000 population. HCV-associated death rates for overall, sex, and race/ethnicity were adjusted to the age distribution of the 2000 US standard population.
Excluding missing values.
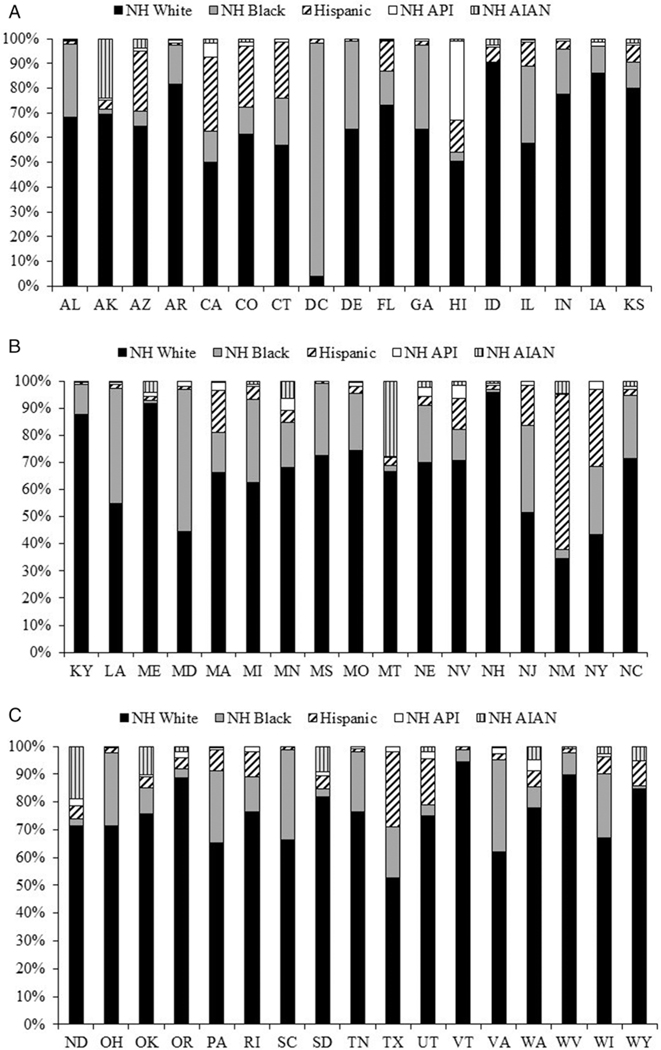
Race/Ethnicity
In 2017, the national, HCV-associated death rate by race/ethnicity (Table 2) was highest for non-Hispanic (non-H) American Indians/Alaska Natives (AIANs; 10.24), followed by non-H Blacks (7.03) and Hispanics (5.29). Rates for non-H Whites in Regions 4, 6, and 9 were significantly higher than the non-H White US death rate. Rates for non-H Blacks in Regions 3, 6, 8, 9, and 10 were significantly higher than the non-H Black US death rate. The rates for Hispanics in Regions 6, 8, and 9 were significantly higher than the Hispanic US death rate. The rate for non-H Asians/Pacific Islanders (APIs) in Region 6 was significantly higher than the non-H API US death rate. The rate for non-H AIANs in Region 8 was significantly higher than the non-H AIAN US death rate.
Of all HCV-associated deaths in 2017, 63.0% of decedents were NH White, 19.1% were non-H Black, and 14.0% were Hispanic (Table 2). Among regions, the highest proportion of deaths were in non-H White decedents. In Regions 1, 2, 3, 4, 5, and 7, non-H Blacks represented the second-highest proportion of deaths. In Regions 6, 8, and 9, Hispanics represented the second-highest proportion of deaths. The proportions were similar for non-H Blacks and Hispanics in Region 1, 2, 6, and 10.
In 2016 and 2017 together, the proportions of decedents who were non-H White were highest in all jurisdictions except for New Mexico, where Hispanics had the highest proportion (57.5%), and Washington, D.C., and Maryland, where non-H Blacks had the highest proportions (94.3% and 52.3%, respectively; Figure 4).
Figure 4.
Percent distribution of HCV-associated deaths by race/ethnicity for each of the US states and District of Columbia, 2016–2017. Data Source: 2016–2017 US multiple cause-of-death data, National Vital Statistics System. Abbreviations: AIAN, American Indian/Alaska Native; AK, Alaska; AL, Alabama; API, Asian/Pacific Islander; AR, Arkansas; AZ, Arizona; CA, California; CO, Colorado; CT, Connecticut; DC, Washington, D.C.; DE, Delaware; FL, Florida; GA, Georgia; HCV, hepatitis C virus; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MS, Mississippi; MO, Missouri; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; Non-H, non-Hispanic; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming.
Sex
In 2017, males had higher death rates when compared with females, across locations (Table 2).
Death Rate Changes Associated With Hepatitis C Virus From 2016 to 2017
From 2016 to 2017, there was a 6.56% decline in the HCV-associated death rate, from 4.42 in 2016 to 4.13 in 2017 (P < .05; Table 1). Death rate declines were observed in all regions, but the percentages in death rate declines were significant in Regions 2, 5, and 9. The death rates also declined in 36 jurisdictions, of which the declines were significant for Wisconsin, Idaho, Illinois, Michigan, California, and New York. For 14 jurisdictions, the HCV-associated death rate increased from 2016 to 2017, but the increases were not significant (P ≥ .05).
DISCUSSION
This study provided HCV-associated death rates and counts geographically in 2017, providing data in the curative-therapy era. We identified 3 regions and 12 jurisdictions, primarily in the Western and Southern regions, that had significantly higher death rates than the United States as a whole. This study also identified 18 jurisdictions that accounted for over 70% of the absolute number of HCV-associated deaths. The observed geographic discordances in death rates may be affected by parallel discordances in prevalence. However, because of the limitations of current prevalence data [20, 21], we cannot definitively confirm this. These parallels would not explain all discordances, though, because the HCV infection prevalences are shifting in some jurisdictions to younger adults who inject drugs. In these jurisdictions, the HCV-associated death rates would be lower. Discordances may be impacted by other factors, including (1) the distribution of subpopulations known to have disproportionate HCV-associated death rates (eg, AIANs, Blacks, and Baby Boomers); (2) geographic differences in the approval of Medicaid to cover treatment [22, 23]; (3) regional and rural/urban differences in DAA uptakes [24]; and (4) varying practices in reporting HCV infection as a cause of death [2, 25].
We observed jurisdictions with lower death rates that concurrently experienced higher acute HCV infection incidences. Of the 15 jurisdictions with lower death rates in 2017, Massachusetts, Utah, South Dakota, Maine, Wisconsin, New Jersey, Michigan, New York, Georgia, and Alabama had relatively higher acute HCV infection incidence rates in 2016 (ie, ≥ 0.7 cases/100 000 standard population) [6]. Massachusetts, Utah, and South Dakota reported the highest incidence rates per 100 000 population (6.2, 2.5, and 2.3, respectively), when compared to other reporting jurisdictions [6]. Jurisdictions that were experiencing lower HCV-associated death rates while simultaneously reporting higher acute HCV infection incidences may see higher death rates in future years. Comparing jurisdiction-specific incidence and mortality data has shown how the HCV infection epidemic is evolving and has spread to parts of the country not previously heavily affected. The continued monitoring of burden indicators may inform the experiences of HCV infections at the local level.
We identified disproportionate death rates in AIANs and Blacks, both nationally and regionally. The higher HCV-associated death rate in AIANs can potentially be explained by comorbidities (eg, cardiovascular disease, alcohol-related conditions, and chronic liver disease) [26–28] that may have accelerated any existing liver damage, leading to end-stage liver disease and mortality. Additionally, many American Indians, which comprised the majority of AIAN decedents in our study, lived in rural areas and faced additional challenges in accessing testing, treatment, and specialty care for their diseases [29]. On a positive note, the Cherokee Nation Health Services implemented a policy that resulted in programs that have been improving HCV testing and care [30]. The national HCV infection prevalence was 2.4 times higher in Whites than Blacks [31], while the HCV-associated death rate among Blacks was higher. An explanation is that African Americans had poorer responses to the pre-DAA regimen of interferon and ribavirin, because they were least likely to carry the CC genotype of the IL28B gene, which is a predictor of pre-DAA treatment-induced sustained virologic response [32]. The disproportionate death rate in this subpopulation still existed in 2016–2017 because only 3 years had elapsed since these DAAs became available, and population-based studies have found an association between DAA noninitiation and Black race/ethnicity versus White race/ethnicity [33, 34]. Evidence of these disparities highlights the need for increased efforts to improve linkage to the cure among populations experiencing disproportionate mortality.
The national recommendations for screening Baby Boomers prompted increases in the testing of this population [35, 36]. However, large numbers of HCV-infected Baby Boomers remain undiagnosed and not in care [37]. In spite of recommendations for testing Baby Boomers and non–birth cohort adults with identified risks, as well as the documented benefits of treatment on reducing mortality risks [38], reimbursement policies set forth by insurance plans and payers were restrictive in many jurisdictions, limiting treatment to only people with clinical evidence of moderate-to-severe liver disease and/or some period of abstinence from alcohol and injection drug use [22, 39, 40]. Indeed, 1 study found that Medicaid fee-for-service policies in 33 jurisdictions in 2014 required a demonstration of severe liver disease to qualify for treatment [22], while another study concluded that 24 jurisdictions in 2015–2016 had policies that required some period of sobriety before treatment [40]. The aforementioned study from 2014 found that Medicaid required moderate-to-severe liver damage before a patient would qualify for treatment in all 12 jurisdictions that were identified in our study as having the highest death rates, with the exception of Texas, which had unknown restrictions in 2014 [22] but required a minimum fibrosis score of F3 in 2017 [23]. Many jurisdictions have incrementally loosened treatment eligibility requirements from 2014 to 2017 [22, 23]. With the exception of Washington and New Mexico, jurisdictions with high death rates in 2017 that also had previously restrictive eligibility requirements in 2014 still required a fibrosis score of F2 or higher in 2017 [23].
National surveillance data indicated that from 2015–2016, a 9.37% decline in the HCV-associated death rate was observed [6]. In our study, from 2016–2017, a further, significant 6.56% decline was observed, with declines of varying extents in all regions and 36 jurisdictions and increases of varying extents in 14 jurisdictions. The decline in the death rate is potentially explained by the evolving nature of the HCV infection epidemic, as the incidence is now highest among younger people [6], and HCV-infected Baby Boomers with advanced liver disease have aged and may have already died of HCV-associated causes and other causes [41]. Approximately three-fourths of HCV-infected Baby Boomers, which account for nearly 80% of HCV-associated deaths, developed moderate-to-advanced liver disease [42]. It is also likely that the number of people cured of their HCV infection had begun to reduce the risk of progressive liver disease and mortality by 2016. A Veterans Administration study of DAA recipients with advanced liver disease through 2016 demonstrated a significant reduction in mortality in the first year after achieving a sustained virologic response [38]. Early testing has also been shown to improve linkage-to-cure rates [8, 43, 44]. Continued monitoring of HCV-associated mortality is important to track how effective treatment uptake efforts are being implemented.
There are important limitations to consider. First, demographic information on the death certificate is often collected from an informant, which could lead to misclassifications [45]; specifically, the misclassification of AIAN race has been common [46]. The National Longitudinal Study evaluated the percent agreement between self-identified race/ethnicity on the current population survey with reported race/ethnicity on the death certificate from 1979–2011 and found that while most groups had near 100% percent agreement, only 51.4–55.2% of self-identified AIANs from the most recent population survey were classified as such at death [46, 47]. The tendency to misclassify AIAN decedents as other race groups results in underrepresentation of AIANs, especially for conditions that disproportionately affect AIANs, like HCV infection [6]. Second, cause-of-death information is based on the certifying physician or medical examiner’s certification of causes of death [10]. Because the majority of HCV infections are asymptomatic [48] and could be undiagnosed, HCV infection is underreported as a cause of death. Even when an HCV infection is diagnosed, a cohort study of chronic HCV-infected patients in care concluded that only 19% of all deceased, chronic HCV-infected cohort members and only 30% of those with recorded liver disease in their medical record had HCV infection listed as a cause of death [25]. These findings were corroborated by 2 other studies [2, 49], 1 of which found that only 64% of deceased members of a large, managed-care health plan in California who had an HCV infection mentioned on the medical record had it cited as a cause of death, despite having a death associated with chronic liver disease [2]. Similarly, only 45.4% of deceased Connecticut residents with an HCV infection noted on their medical record had it cited as a cause of death, despite having a death confirmed as associated with chronic liver disease [49]. In spite of these limitations, MCOD data capture all registered deaths in a standardized way, and it is the only data source that can establish HCV-associated death estimates across jurisdictions.
In conclusion, this study identified subpopulations that have disproportionately higher HCV-associated mortality. The highest death rates were noted in the Western and Southern regions and Washington, D.C., and among non-H AIANs, non-H Blacks, and Baby Boomers. These results should be updated frequently, as the findings may inform programs in their targeted efforts to increase treatment uptake to reduce the HCV mortality burden and achieve goals for HCV elimination.
Supplementary Material
Acknowledgments.
The authors thank the staff of state and local health departments who provide death certificate data to the National Center for Health Statistics, and Dr Philip Spradling, Division of Viral Hepatitis, US Centers for Disease Control and Prevention; Dr Benedict Truman, National Center for Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome, Viral Hepatitis, Sexually Transmitted Disease, and Tuberculosis Prevention, US Centers for Disease Control and Prevention; and Dr Robert Anderson, Division of Vital Statistics, National Center for Health Statistics, US Centers for Disease Control and Prevention, for their helpful review and suggestions for the manuscript. The authors would like to acknowledge all 50 states and the District of Columbia who provide death certificate data to the National Center for Health Statistics.
Financial support.
This work was supported by employment through the US federal government.
Disclaimer.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention.
Footnotes
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Ly KN, Xing J, Klevens RM, Jiles RB, Holmberg SD. Causes of death and characteristics of decedents with viral hepatitis, United States, 2010. Clin Infect Dis 2014; 58:40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manos MM, Leyden WA, Murphy RC, Terrault NA, Bell BP. Limitations of conventionally derived chronic liver disease mortality rates: results of a comprehensive assessment. Hepatology 2007; 47:1150–7. [DOI] [PubMed] [Google Scholar]
- 3.Bell BP, Manos MM, Zaman A, et al. The epidemiology of newly diagnosed chronic liver disease in gastroenterology practices in the United States: results from population-based surveillance. Am J Gastroenterol 2008; 103:2727–36; quiz 2737. [DOI] [PubMed] [Google Scholar]
- 4.Seifert LL, Perumpail RB, Ahmed A. Update on hepatitis C: direct-acting antivirals. World J Hepatol 2015; 7:2829–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ly KN, Hughes EM, Jiles RB, Holmberg SD. Rising mortality associated with hepatitis C virus in the United States, 2003–2013. Clin Infect Dis 2016; 62:1287–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Viral hepatitis surveillance, United States, 2016. Available at: https://www.cdc.gov/hepatitis/statistics/2016surveillance/pdfs/2016HepSurveillanceRpt.pdf. Accessed 26 April 2018.
- 7.Association of State and Territorial Health Officials. Viral hepatitis epidemiologic profiles. Available at: http://www.astho.org/Viral-Hepatitis-Epi-Profiles/Map/. Accessed 21 March 2019.
- 8.The National Academies of Science Engineering and Medicine. A national strategy for the elimination of hepatitis B and C: phase two report. Available at: http://www.nationalacademies.org/hmd/reports/2017/national-strategy-for-the-elimination-of-hepatitis-b-and-c.aspx. Accessed 31 August 2018.
- 9.Centers for Disease Control and Prevention. CDC WONDER multiple cause of death data. Available at: https://wonder.cdc.gov/mcd.html. Accessed 5 April 2019.
- 10.Centers for Disease Control and Prevention. US standard certificate of death. Available at: https://www.cdc.gov/nchs/data/dvs/death11-03final-acc.pdf. Accessed 26 April 2018.
- 11.National Center for Health Statistics. Report of the panel to evaluate US standard certificates. Available at: https://www.cdc.gov/nchs/data/dvs/panelreport_acc.pdf. Accessed 15 March 2019.
- 12.Centers for Disease Control and Prevention. The 1989 revision of the US standard certificates and reports. Vital Health Stat 1991; 4:1–43. [PubMed] [Google Scholar]
- 13.US Department of Health and Human Services. Regional offices. Available at: https://www.hhs.gov/about/agencies/iea/regional-offices/index.html. Accessed 31 August 2018.
- 14.World Health Organization. International classification of diseases, 10th Revision. Geneva, Switzerland: World Health Organization, 1998. [Google Scholar]
- 15.National Center for Health Statistics. US census populations with bridged race categories. Available at: https://www.cdc.gov/nchs/nvss/bridged_race.htm. Accessed 8 January 2018.
- 16.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population. Healthy People 2010 Stat Notes 2001:1–10. [PubMed]
- 17.Centers for Disease Control and Prevention. Technical appendix from vital statistics of United States 1999 mortality. Available at: https://wonder.cdc.gov/wonder/help/CMF/TechnicalAppendix1999.pdf. Accessed 5 April 2019.
- 18.Breslow NE, Day NE. Statistical methods in cancer research: the design and analysis of cohort studies. IARC Scientific Publications, 1987; 2:65–68. [PubMed] [Google Scholar]
- 19.Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: final data for 2013. Natl Vital Stat Rep 2016; 64:1–119. [PubMed] [Google Scholar]
- 20.Moore MS, Greene SK, Bocour A, et al. Comprehensive nationwide chronic hepatitis C surveillance is necessary for accurate state-level prevalence estimates. J Viral Hepat 2019; 26:1124–6. [DOI] [PubMed] [Google Scholar]
- 21.Rosenberg ES, Rosenthal EM, Hall EW, et al. Prevalence of hepatitis C virus infection in US states and the District of Columbia, 2013 to 2016. JAMA Network Open 2018; 1:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canary LA, Klevens RM, Holmberg SD. Limited access to new hepatitis C virus treatment under state Medicaid programs. Ann Intern Med 2015; 163:226–8. [DOI] [PubMed] [Google Scholar]
- 23.National Viral Hepatitis Roundtable and the Center for Health Law and Policy Innovation of Harvard Law School. Hepatitis C: the state of Medicaid access. Available at: https://stateofhepc.org/wp-content/uploads/2017/10/State-of-HepC_2017_FINAL.pdf. Accessed 31 August 2018.
- 24.Njei B, Esserman D, Krishnan S, et al. Regional and rural-urban differences in the use of direct-acting antiviral agents for hepatitis C virus. Med Care 2019; 57:279–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahajan R, Xing J, Liu SJ, et al. Mortality among persons in care with hepatitis C virus infection: the Chronic Hepatitis Cohort Study (CHeCS), 2006–2010. Clin Infect Dis 2014; 58:1055–61. [DOI] [PubMed] [Google Scholar]
- 26.Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, Forquera RA. A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. Am J Public Health 2006; 96:1478–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: final data for 2017. Natl Vital Stat Rep 2019; 68:1–76. [PubMed] [Google Scholar]
- 28.Landen M, Roeber J, Naimi T, Nielsen L, Sewell M. Alcohol-attributable mortality among American Indians and Alaska Natives in the United States, 1999–2009. Am J Public Health 2014; 104:S343–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zuckerman S, Haley J, Roubideaux Y, Lillie-Blanton M. Health service access, use, and insurance coverage among American Indians/Alaska Natives and Whites: what role does the Indian Health Service play? Am J Public Health 2004; 94:53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mera J, Vellozzi C, Hariri S, et al. Identification and clinical management of persons with chronic hepatitis C virus infection - Cherokee Nation, 2012–2015. MMWR Morb Mortal Wkly Rep 2016; 65:461–6. [DOI] [PubMed] [Google Scholar]
- 31.Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med 2014; 160:293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ge D, Fellay J, Thompson AJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 2009; 461:399–401. [DOI] [PubMed] [Google Scholar]
- 33.Spradling PR, Xing J, Rupp LB, et al. Uptake of and factors associated with direct-acting antiviral therapy among patients in the Chronic Hepatitis Cohort Study, 2014 to 2015. J Clin Gastroenterol 2018; 52:641–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kanwal F, Kramer JR, El-Serag HB, et al. Race and gender differences in the use of direct acting antiviral agents for hepatitis C virus. Clin Infect Dis 2016; 63:291–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recomm Rep 2012; 61:1–18. [PubMed] [Google Scholar]
- 36.US Preventive Services Task Force. Hepatitis C screening: recommendation summary. 2013. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/hepatitis-c-screening. Accessed 31 August 2018.
- 37.Kasting ML, Giuliano AR, Reich RR, et al. Hepatitis C virus screening trends: serial cross-sectional analysis of the National Health Interview Survey population, 2013–2015. Cancer Epidemiol Biomarkers Prev 2018; 27:503–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Backus LI, Belperio PS, Shahoumian TA, Mole LA. Impact of sustained virologic response with direct-acting antiviral treatment on mortality in patients with advanced liver disease. Hepatology 2019; 69:487–97. [DOI] [PubMed] [Google Scholar]
- 39.Ward JW, Mermin JH. Simple, effective, but out of reach? Public health implications of HCV drugs. N Engl J Med 2015; 373:2678–80. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. State HCV incidence and policies related to HCV preventive and treatment services for persons who inject drugs — United States, 2015–2016. MMWR Weekly 2017; 66:465–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating prevalence of hepatitis C virus infection in the United States, 2013–2016. Hepatology 2018; 69:1020–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Klevens RM, Canary LA, X. H, et al. The burden of hepatitis C infection-related liver fibrosis in the United States. Clin Infect Dis 2016; 63:1049–55. [DOI] [PubMed] [Google Scholar]
- 43.American Association for the Study of Liver Diseases/Infectious Diseases Society of America. HCV guidance: recommendations for testing, managing, and treating hepatitis C. Available at: https://www.hcvguidelines.org/. Accessed 30 April 2018.
- 44.National Academies of Sciences E, and Medicine. Eliminating the public health problem of hepatitis B and C in the United States: phase one report. Washington, DC: The National Academies Press, 2016. doi: 10.17226/23407. [DOI] [PubMed] [Google Scholar]
- 45.Hahn RA, Wetterhall SF, Gay GA, et al. The recording of demographic information on death certificates: a national survey of funeral directors. Public Health Rep 2002; 117:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arias E, Heron M, Hakes JK. The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. National Center for Health Statistics. Vital Health Stat 2016; 2:1–21. Available at: https://www.cdc.gov/nchs/data/series/sr_02/sr02_172.pdf. [PubMed] [Google Scholar]
- 47.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. National Center for Health Statistics. Vital Health Stat 2008; 2:1–24. Available at: http://www.cdc.gov/nchs/data/series/sr_02/sr02_148.pdf. [PubMed] [Google Scholar]
- 48.Denniston MM, Klevens RM, McQuillan GM, Jiles RB. Awareness of infection, knowledge of hepatitis C, and medical follow-up among individuals testing positive for hepatitis C: National Health and Nutrition Examination Survey 2001–2008. Hepatology 2012; 55:1652–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ly KN, Speers S, Klevens RM, Barry V, Vogt TM. Measuring chronic liver disease mortality using an expanded cause of death definition and medical records in Connecticut, 2004. Hepatol Res 2014; 45:960–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.