Abstract
Purpose
The objective of this study is to evaluate the effect of intravenous acetaminophen on length of stay (LOS) in abdominal surgery patients.
Methods
This retrospective, cohort chart review evaluated patients who underwent colon resection or pancreaticoduodenectomy between January 1, 2010 and August 31, 2013. The primary outcome is postoperative LOS. Secondary outcomes include opioid use, pain scores, and naloxone or laxative use. Patients who received intravenous acetaminophen were compared to patients who did not.
Results
A total of 329 patients were included, with 269 in the non-acetaminophen group compared to 60 patients in the acetaminophen group. There was no difference in postoperative LOS (9.2 s vs 9.1 days; P = .90). Postoperative LOS was also similar when controlling for surgery type. The acetaminophen group had reduced opioid consumption in the first 24 hours postoperatively (P = .02). However, pain scores were higher in the acetaminophen group, both in the first 24 hours (P = .007) and throughout the hospital stay (P < .001). Other clinical outcomes were similar between groups.
Conclusion
Intravenous acetaminophen was not associated with a decreased postoperative LOS at our institution.
Keywords: acetaminophen, analgesia, internal medicine, pain management, surgery
The optimal strategy for treating postoperative pain has not been clearly defined. Multimodal approaches to analgesia may be more effective than addressing a single mechanism, as patients may benefit from the synergistic effects among analgesic agents.1,2 Multimechanistic analgesic regimens have conferred benefits such as improved postoperative pain relief, reduced opioid consumption, and potentially lower adverse events related to analgesia.3–7 Furthermore, recently updated pain, agitation, and delirium guidelines suggest that nonopioid analgesics be considered to decrease the amount of opioids administered and opioid-related side effects for patients in an intensive care unit (ICU) setting. 8
Acetaminophen is an analgesic and antipyretic with little anti-inflammatory effect. It is one of the most commonly used medications for pain relief, in both prescription and over-the-counter forms. Acetaminophen has long been available in oral and rectal dosage forms, but there has not been an injectable formulation for use in the United States until recently. Although easier to administer, oral acetaminophen may not be the ideal analgesic immediately after surgery when the oral route is not yet recommended. Rectal administration can result in unpredictable absorption, making it difficult to effectively control postoperative pain. When compared to nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen has a relatively safe adverse event profile at therapeutic doses, with the exception of hepatotoxicity, and has minimal drug interactions. 9 Intravenous acetaminophen was approved by the US Food and Drug Administration (FDA) in November 2010 and is indicated for the management of mild to moderate pain, the management of moderate to severe pain with adjunctive opioid analgesics, and the reduction of fever. The typical dose is 1 g every 6 hours or 650 mg every 4 hours for patients weighing greater than 50 kg. 10
Intravenous acetaminophen has shown to be safe and effective when used in conjunction with opioids for postoperative pain in patients following major surgery.1,11–15 In a randomized, double-blind study comparing intravenous acetaminophen to placebo in 151 patients after major orthopedic surgery, intravenous acetaminophen was associated with a significant improvement in pain relief in the first 6 hours, as well as a longer time to morphine rescue. 11 There was also an overall reduction in 24-hour morphine use in the intravenous acetaminophen group (38.3 ± 35.1 mg vs 57.4 ± 52.3 mg; P < .01). 11 A separate double-blind, placebo-controlled study evaluated 2 dosing strategies of intravenous acetaminophen in 244 patients after abdominal laparoscopic surgery. 12 Both acetaminophen groups were associated with a significant reduction in the 24-hour sum of pain intensity differences compared to placebo. 12 However, the authors found no difference in adverse events among groups as well as time to rescue medication or rescue medication consumption. 12 Zafar and colleagues 16 evaluated the outcomes of an accelerated recovery program after laparoscopic colon resection. The program consisted of patient and family education, minimal intravenous analgesia, and early mobilization. 16 Patients were consecutively enrolled into 1 of 3 groups: transversus abdominis plane (TAP) blocks plus intravenous acetaminophen and oral analgesics, intravenous acetaminophen plus oral analgesics, or morphine patient-controlled analgesia (PCA). 16 The authors found that the time to resumption of diet was reduced with both acetaminophen groups compared to PCA (12 vs 12 vs 36 hours, respectively; P < .001). 16 There was also a reduction in postoperative hospital stay with the non-PCA groups (2 vs 3 vs 5 days, respectively; P < .001). 16 Unfortunately, the authors concluded that they were unable to determine whether the reduction in hospital length of stay (LOS) was due to the intravenous acetaminophen, TAP analgesia, or the overall program itself.
Although relatively safe and effective at controlling pain, intravenous acetaminophen comes with a substantial cost increase when compared to opioids or NSAIDs. A pharmacoeconomic review published in 2013 reported that the wholesale acquisition cost (WAC) of intravenous acetaminophen as approximately 3-fold that of intravenous morphine ($45.60 per day compared to $15.40 per day). 17 As of June 2014, the current WAC for intravenous acetaminophen has increased to $136.15 per day. Even with the increased cost, intravenous acetaminophen provides significant pain relief without the increased incidence of nausea, vomiting, constipation, sedation, and respiratory depression associated with opioids or the gastrointestinal and renal adverse effects observed with NSAIDs. 18 These adverse effects may lead to prolonged hospitalization, further increasing health care costs. In another study, which used the 2002 Michigan State Inpatient Database, the authors demonstrated that a 1-day increase in LOS in a non-ICU/critical care unit bed equates to an increase in costs of $1,295. 19 Newer data from 2013 reveal the expenses per inpatient day in a non-ICU bed to be $2,157. 20 Therefore, any reduction in hospital LOS may have significant pharmacoeconomic impact.
To our knowledge, no prospective, randomized trial has shown a decrease in LOS using intravenous acetaminophen following major abdominal surgery. The primary aim of this study is to evaluate the effect of intravenous acetaminophen on postoperative LOS in patients after colon resection or pancreaticoduodenectomy at our institution. These procedures were chosen because they have a longer LOS compared to most abdominal surgeries. Second, we wanted to evaluate the clinical impact of utilizing intravenous acetaminophen.
Methods
This retrospective, cohort study was approved by the institutional review board at the University of Tennessee Graduate School of Medicine. All patients who underwent colon resection or pancreaticoduodenectomy during their hospitalization were identified via ICD-9 codes. Patients were included if they were 18 to 80 years old, received at least 4 scheduled doses of 1 g intravenous acetaminophen, and had their procedure performed at an academic medical center (University of Tennessee Medical Center) between January 1, 2010, and August 31, 2013. Our institutional policy restricts intravenous acetaminophen to 4 consecutive doses per order with the first dose administered intraoperatively. Patients were excluded for history of or current hepatic dysfunction, weight less than 50 kg, pregnancy, allergy or known hypersensitivity to acetaminophen, incomplete medical record, receipt of alvimopan during their hospitalization, or receipt of fewer than 4 doses of intravenous acetaminophen.
Patients were separated into 2 groups based upon the receipt of intravenous acetaminophen, regardless of surgery type. Institution medical records were reviewed for items such as patient demographics, surgery indication, American Society of Anesthesiologists (ASA) physical status, LOS, type of rescue medication, time to rescue medication, total acetaminophen dose, home opioid and laxative use, time to bowel movement, number of bowel movements, time to resumption of diet, and pain-related comorbidities to assess pain tolerance. Pain scores were assessed utilizing a visual analog scale ranging from 1 to 10. Laxative and naloxone use were collected to identify complications related to opioid use. Laxative use included receipt of bisacodyl, polyethylene glycol, lactulose, senna, magnesium hydroxide, magnesium citrate, methylnaltrexone, or an enema consisting of sorbitol, magnesium hydroxide, mineral oil, and glycerin. Naloxone was used as a surrogate for oversedation. Opioid consumption was converted to oral morphine equivalents, where 30 mg of oral morphine was equivalent to 0.1 mg of intravenous fentanyl, 1.5 mg of intravenous hydromorphone, 7.5 mg of oral hydromorphone, 10 mg of intravenous morphine, 20 mg of oral oxycodone, or 30 mg of oral hydrocodone.
Descriptive and frequency statistics were utilized to assess for outliers and meeting of statistical assumptions. Continuous data, such as LOS and opioid consumption, are presented as means with standard deviations. Categorical data are presented using percentages and cross-tabulations. We tested continuous variables utilizing independent sample t tests to evaluate significant effects between groups. Mann-Whitney U tests were used when violations of statistical assumptions occurred. Chi-square tests were used for comparison of categorical variables to yield unadjusted odds ratios with 95% confidence intervals. We employed a 2 × 2 fixed-effects analysis of variance (ANOVA) model to assess any interaction between type of surgery and group. Post hoc power was conducted using G*Power. Based on the means and standard deviations with an alpha of 0.05 and statistical power of 0.80, 131 patients would be needed per treatment group to detect a meaningful 12% reduction in LOS between groups. All inferential data analyses were conducted using IBM SPSS version 21 (IBM Corp., Armonk, NY). Statistical significance was assumed at an alpha value of 0.05.
Results
During the study evaluation period, a total of 438 patients underwent either colon resection or pancreaticoduodenectomy. Of the 438 eligible patients, 109 patients were excluded ( Figure 1 ). A total of 329 patients were included in the analysis; there were fewer patients in the intravenous acetaminophen group (n = 60) compared to the non-acetaminophen group (n = 269). There were also a greater number of patients who underwent colon resection (n = 271) compared to those who underwent pancreaticoduodenectomy (n = 58). Baseline characteristics are shown in Table 1 . The majority of patients were Caucasian with a median ASA physical status of III. Home opioid and laxative use was similar between groups. There were no statistical differences in baseline characteristics, with the exception of weight. Overall, patients in the intravenous acetaminophen group weighed less (78 vs 84 kg; P = .04).
Figure 1.
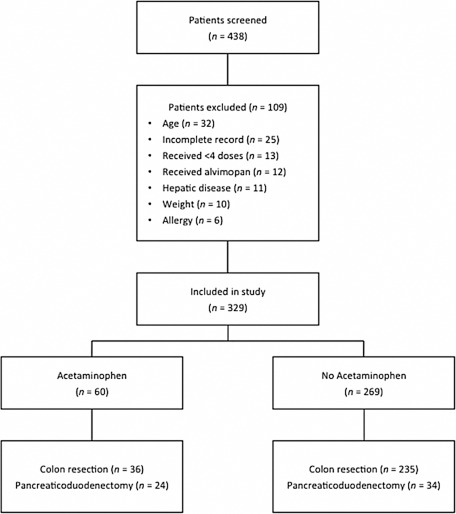
Patient enrollment and distribution.
Table 1.
Baseline demographic and clinical characteristics
| Variable | Acetaminophen (n = 60) | No acetaminophen (n = 269) | P |
|---|---|---|---|
| Age, mean ± SD, years | 60.1 ± 11.2 | 58.4 ± 14.5 | .28 |
| Male, n (%) | 30 (50) | 148 (55) | .38 |
| Caucasian, n (%) | 57 (95) | 253 (94) | .50 |
| Weight, mean ± SD, kg | 78.2 ± 17.3 | 84.5 ± 21.9 | .04 |
| ASA physical status, n (%) | |||
| I | 1 (1.7) | 1 (0.4) | |
| II | 10 (16.7) | 68 (25.2) | |
| III | 45 (75) | 164 (61) | .88 |
| IV | 4 (6.7) | 35 (13) | |
| V | 0 (0) | 1 (0.4) | |
| Home opioid use, n (%) | 13 (22) | 48 (18) | .35 |
| Home laxative use, n (%) | 1 (1.7) | 8 (3) | .46 |
Note: ASA = American Society of Anesthesiologists.
For the primary outcome of postoperative LOS, there was no difference between groups (intravenous acetaminophen group, 9.2 days vs non-acetaminophen group, 9.1 days; P = .90). There was also no difference in ICU LOS between groups ( Table 2 ). Postoperative LOS was similar when controlling for surgery type as well (P = .99).
Table 2.
Clinical outcomes for abdominal surgery patients: Intravenous administration of acetaminophen vs no acetaminophen groups
| Outcome | Acetaminophen (n = 60) | No acetaminophen (n = 269) | P |
|---|---|---|---|
| LOS, days | 9.2 ± 4.8 | 9.1 ± 5.3 | .90 |
| Colon resection | 9.2 ± 5.5 | 9.1 ± 5.5 | – |
| Pancreaticoduodenectomy | 9.3 ± 3.7 | 9.4 ± 3.6 | – |
| ICU LOS, days | 2.1 ± 2.5 | 2.2 ± 3.0 | .91 |
| 24 hour opioid use, mg a | 142.2 ± 118.8 | 207.2 ± 184.7 | .02 |
| Total opioid use, mg | 724.1 ± 686.7 | 757.9 ± 717.4 | .75 |
| 24 hour pain scores, VAS | 2.0 ± 1.6 | 1.5 ± 1.3 | .007 |
| Total pain scores, VAS | 2.2 ± 1.0 | 1.5 ± 1.3 | <.001 |
| Time to rescue, hours | 5.5 ± 2.7 | 4.9 ± 2.9 | .21 |
| Time to BM, hours | 86.2 ± 53.3 | 87.5 ± 51.3 | .87 |
| Time to diet, hours | 157.9 ± 89.7 | 133.8 ± 98.1 | .46 |
| >4 g/day of acetaminophen, n (%) | 15 (20) | 2 (0.7) | <.001 |
Note: Values given as mean ± SD, unless otherwise indicated. BM = bowel movement; ICU = intensive care unit; LOS = length of stay; VAS = visual analog scale.
Opioid use = oral morphine equivalents
In the first 24 hours postoperatively, we found a reduction in opioid consumption in the intravenous acetaminophen group (142 mg) compared to 207 mg of oral morphine equivalents (P = .02). However, there was no difference when assessing opioid consumption throughout the entire hospitalization. Unlike previous studies that showed effective pain relief, pain scores in the intravenous acetaminophen group were higher than the non-acetaminophen group, both in the first 24 hours (P = .007) and throughout the hospital stay (P < .001).
The majority of patients received morphine or hydromorphone patient-controlled analgesia (PCA) for breakthrough pain relief. In addition, all patients had as-needed acetaminophen-containing oral analgesics available. There was no difference in time to rescue pain medication between groups (P = .21). Time to bowel movement, number of bowel movements, and time to resumption of diet were also similar between groups ( Table 2 ). There was no difference in laxative use (P = .53) or naloxone use (P = .60). As expected, the total dose of acetaminophen from all dosage forms was higher in the intravenous acetaminophen group (P < .001). Of the 60 patients who received intravenous acetaminophen, 20% exceeded the 4 g per day threshold. However, we did not evaluate additional clinical outcomes in these patients.
Discussion
The data from our study suggest that the use of intravenous acetaminophen in patients undergoing colon resection or pancreaticoduodenectomy does not impact ICU or hospital LOS. We were unable to observe the reduction in LOS found in Zafar and colleagues' study 16 in patients following colorectal surgery in our facility. We also emphasize early mobilization and diet advancement postsurgery at our institution, similar to the Zafar study. There is potential to decrease health care costs tremendously with the reduction of hospital LOS. In a pharmacoeconomic review, the mean cost for a 5-day hospitalization was approximately $15,671. 17 A decrease in LOS of just 1 day would reduce costs greatly.
In the first 24 hours postsurgery, we were able to demonstrate a reduction in opioid consumption, similar to a previous study in orthopedic patients. 11 However, a randomized, double-blind, placebo-controlled study in adolescents after major spinal surgery did not find a reduction in opioid requirements. 15 Memis and colleagues 22 found a reduction in meperidine consumption with the use of propacetamol, a prodrug of paracetamol or acetaminophen, in ICU patients following major surgery. Nonetheless, it is unclear whether the utilization of intravenous acetaminophen consistently reduces opioid consumption throughout the hospitalization. In addition, there was no difference in opioid-related adverse effects with opioid use reduction from intravenous acetaminophen in our facility.
The requirement for breakthrough pain relief is commonly used to assess postoperative analgesia. Two previous studies, comparing intravenous acetaminophen to placebo, found increases in time to rescue medication. 11 We were unable to duplicate this finding in our study. Our study included patients undergoing major abdominal surgery, whereas the previous studies enrolled patients after orthopedic surgery.
In the present study, intravenous acetaminophen was associated with inferior pain control compared to traditional postoperative analgesia, consisting of a combination of opioids and NSAIDs. It is plausible that patients received intravenous acetaminophen because they were in greater pain. However, all of the patients receiving intravenous acetaminophen in our study were administered their first dose intraoperatively and continued for at least 24 hours thereafter. This finding is consistent with a recent study comparing intravenous and rectal acetaminophen in children following tonsillectomy. 23 In this randomized, double-blind study, rectal acetaminophen was associated with less postoperative pain and a longer duration to requesting breakthrough pain medication. 23 Nevertheless, further study is needed to determine whether rectal acetaminophen may be a more cost-effective analgesic agent compared to intravenous acetaminophen.
We used laxative use and naloxone use to assess for opioid-related adverse events. There was no difference in laxative or naloxone use between groups, suggesting that intravenous acetaminophen in the first 24 hours postoperatively does not reduce opioid-related adverse events in abdominal surgery patients in our facility. We did not assess antiemetic or antihistamine administration, which is often associated with opioid use, potentially leading to uncaptured adverse events. We were surprised to find that 20% of patients receiving intravenous acetaminophen exceeded the daily maximum dose of 4 g. The patients exceeding 4 g were due to either receiving a fifth dose of intravenous acetaminophen within 24 hours of the first dose or from as-needed oral acetaminophen-containing analgesics that were administered within the 24- hour window. At our institution, a policy was implemented to delay or discontinue all other forms of acetaminophen until 6 hours after the last dose of intravenous acetaminophen is infused. However, our electronic medical record system allows nurses to administer medications up to an hour before the scheduled time. The policy also restricts intravenous acetaminophen to 4 doses per order, to limit use and minimize costs, requiring physicians to reorder the medication the following day if they deem appropriate.
Our study has several limitations. It is retrospective and included only 329 patients, the majority of whom did not receive intravenous acetaminophen. Our patient groups were unmatched, both in surgery type and the receipt of acetaminophen. Our study was a single-institutional study, making it challenging to extrapolate our findings to other institutions. Intravenous acetaminophen was added to our formulary in April 2011. However, it was not routinely utilized by our surgeons until 2012, potentially leading to the group size disparity. In addition, all 12 of the patients excluded for receipt of alvimopan also received intravenous acetaminophen. Alvimopan, a peripherally acting opioid antagonist indicated to accelerate gastrointestinal recovery following bowel resections, was excluded in our study as a potential confounder. We also failed to achieve power with a goal of 131 patients per group. The majority of our patients underwent colon resection, making it difficult to extrapolate these findings to other types of surgeries. Although LOS was not different between the 2 surgeries evaluated, postoperative pain may be different between the types of surgeries. The most painful procedures appear to be orthopedic with major joints, thoracic, and open abdominal surgery; emergency, major, and abdominal surgery were found to have the highest analgesic consumption. 24 As previously mentioned, we did not assess liver function tests or clinical outcomes in the patients exceeding the maximum daily dose of acetaminophen. Hospital records were collected utilizing electronic medical records, which are subject to documentation errors. Finally, we were unable to account for postoperative complications, such as respiratory failure or infection, which may have prolonged patients' LOS.
Conclusion
Intravenous acetaminophen was not associated with a decreased LOS at our institution. While intravenous acetaminophen was associated with decreased opioid consumption in the first 24 hours postoperatively, it was associated with higher pain scores compared to the non-acetaminophen group. In addition to suboptimal pain relief, we did not find a reduction in opioid-related adverse events. Our results suggest there may be more cost-effective analgesics to control pain after colon resection or pancreaticoduodenectomy. However, a larger study is warranted to determine the true impact of intravenous acetaminophen after major abdominal surgery.
Acknowledgments
None of the authors have any conflicts of interest to disclose and no financial support or personal connections that could be perceived to bias their work.
References
- 1.Yaster M. Multimodal analgesia in children. Eur J Anaesthesiol. 2010; 27: 851–857. [DOI] [PubMed] [Google Scholar]
- 2.Khalili G. Janghorbani M. Saryazdi H. et al. Effect of pre-emptive and preventive acetaminophen on postoperative pain score: A randomized, double-blind trial of patients undergoing lower extremity surgery. J Clin Anesth. 2013; 25(3): 188–192. [DOI] [PubMed] [Google Scholar]
- 3.White P.F. Multimodal analgesia: Its role in preventing postoperative pain. Curr Opin Investig Drugs. 2008; 9: 76–82. [PubMed] [Google Scholar]
- 4.Fu P.L. Xiao J. Zhu Y.L. et al. Efficacy of a multimodal analgesia protocol in total knee arthroplasty: A randomized, controlled trial. J Int Med Res. 2010; 38: 1404–1412. [DOI] [PubMed] [Google Scholar]
- 5.Cho C.H. Song K.S. Min B.W. et al. Multimodal approach to postoperative pain control in patients undergoing rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2011; 19: 1744–1748. [DOI] [PubMed] [Google Scholar]
- 6.Koh I.J. Kang Y.G. Chang C.B. et al. Additional pain relieving effect of intraoperative periarticular injections after simultaneous bilateral TKA: A randomized, controlled study. Knee Surg Sports Traumatol Arthrosc. 2010; 18: 916–922. [DOI] [PubMed] [Google Scholar]
- 7.Hebl J.R. Dilger J.A. Byer D.E. et al. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg Anesth Pain Med. 2008; 33: 510–517. [PubMed] [Google Scholar]
- 8.Barr J. Fraser G.L. Puntillo K. et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41: 263–306. [DOI] [PubMed] [Google Scholar]
- 9.Macintyre P. Schug S. Acute Pain Management: A Practical Guide. 3rd ed. Edinburgh: Elsevier; 2007. [Google Scholar]
- 10.Ofirmev [package insert]. San Diego, CA: Cadence Pharmaceuticals, Inc.; November 2010. [Google Scholar]
- 11.Sinatra R.S. Jahr J.S. Reynolds L.W. et al. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005; 102: 822–831. [DOI] [PubMed] [Google Scholar]
- 12.Wininger S.J. Miller H. Minkowitz H.S. et al. A randomized, double-blind, placebo-controlled, multicenter, repeat-dose study of two intravenous acetaminophen dosing regimens for the treatment of pain after abdominal laparoscopic surgery. Clin Ther. 2010; 32: 2348–2369. [DOI] [PubMed] [Google Scholar]
- 13.Ong C.K. Seymour R.A. Lirk P. et al. Combining paracetamol (acetaminophen) with nonsteroidal anti-inflammatory drugs: A qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010; 110: 1170–1179. [DOI] [PubMed] [Google Scholar]
- 14.Wong I. St. John-Green C. Walker S.M. Opioid-sparing effects of perioperative paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) in children. Paediatr Anaesth. 2013; 23(6): 475–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hiller A. Helenius I. Nurmi E. et al. Acetaminophen improves analgesia but does not reduce opioid requirement after major spine surgery in children and adolescents. Spine. 2012; 37: E1225–E31. [DOI] [PubMed] [Google Scholar]
- 16.Zafar N. Davies R. Greenslade G.L. et al. The evolution of analgesia in an “accelerated” recovery programme for resectional laparoscopic colorectal surgery with anastomosis. Colorectal Dis. 2010; 12(2): 119–124. [DOI] [PubMed] [Google Scholar]
- 17.Jahr J.S. Filocamo P. Singh S. Intravenous acetaminophen: A review of pharmacoeconomic science for perioperative use. Am J Ther. 2013; 20(2): 189–199. [DOI] [PubMed] [Google Scholar]
- 18.Haas D.A. An update on analgesics for the management of acute postoperative dental pain. J Can Dent Assoc. 2002; 68: 476–482. [PubMed] [Google Scholar]
- 19.Candrilli S. Mauskopf J. How much does a hospital day cost? Presented at the International Society for Pharmacoeconomics and Outcomes Research Annual Meeting; May 22, 2006; Philadelphia, Pennsylvania. [Google Scholar]
- 20.Kaiser Family Foundation's State Health Facts. Data source: Hospital adjusted expenses per inpatient day. 2013. http://kff.org/other/state-indicator/expenses-per-inpatient-day/. Accessed October 2015.
- 21.Faul F. Erdfelder E. Buchner A. et al. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009; 41(4): 1149–1160. [DOI] [PubMed] [Google Scholar]
- 22.Memis D. Inal M.T. Kavalci G. et al. Intravenous paracetamol reduced the use of opioids, extubation time, and opioid-related adverse effects after major surgery in the intensive care unit. J Crit Care. 2010; 25: 458–462. [DOI] [PubMed] [Google Scholar]
- 23.Haddadi S. Marzban S. Karami M.S. et al. Comparing the duration of the analgesic effects of intravenous and rectal acetaminophen following tonsillectomy in children. Anesth Pain Med. 2014; 4(1): e13175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ip H.Y. Abrishami A. Peng P.W. et al. Predictors of postoperative pain and analgesic consumption: A qualitative systematic review. Anesthesiology. 2009; 111: 657–677. [DOI] [PubMed] [Google Scholar]


