Abstract
Background:
Opioids are recommended for pain management in patients being cared for and transported by Emergency Medical Services, but no specific guidelines exist for older adults with fall-related injury. Prior research suggests pre-hospital opioid administration can effectively manage pain in older adults, but less is known about safety in this population. We compared short-term safety outcomes, including delirium, disposition, and length of stay, among older adults with fall related injury according to whether they received pre-hospital opioid analgesia.
Methods:
We linked Medicare claims data with prehospital patient care reports for older adults (≥65) with fall-related injury in Illinois between January 1, 2014 and December 31, 2015. We used weighted regression models (logistic, multinomial logistic, Poisson) to assess the association between prehospital opioid analgesia and incidence of inpatient delirium, hospital disposition, and length of stay.
Results:
Of 28,150 included older adults, 3% received prehospital opioids. Patients receiving prehospital opioids (versus no prehospital opioids) were less likely to be discharged home from the emergency department (adjusted probability = 0.30 [95% CI: 0.25, 0.34] vs. 0.47 [95% CI: 0.46, 0.48]), more likely to be discharged to a non-home setting after an inpatient admission (adjusted probability = 0.43 [95% CI: 0.39, 0.48] vs. 0.30 [95% CI: 0.30, 0.31]), had inpatient length of stay 0.4 days shorter (p<0.001) and ICU length of stay 0.7 days shorter (p=0.045). Incidence of delirium did not vary between treatment and control groups.
Conclusions:
Few older adults receive opioid analgesia in the pre-hospital setting. Prehospital opioid analgesia may be associated with hospital disposition and length of stay for older adults with fall-related injury; however, our findings do not provide evidence of an association with inpatient delirium. These findings should be considered when developing guidelines for prehospital pain management specific to the older adult population.
Keywords: Traumatic injury, geriatric care, pain management, emergency medical services
Introduction
Three million US older adults experience a fall-related injury resulting in an emergency department (ED) visit or hospitalization each year, accounting for 32% of all injury-related ED encounters and 30% of trauma admissions.1 Emergency medical services (EMS) providers are often the first to treat older adults with fall-related injury.2,3 National EMS guidelines recommend opioid analgesia for prehospital pain management4 but do not include specific guidance for pain management in older patients.5
The scope of practice for paramedics (prehospital clinicians with Advance Life Support [ALS] training) in the US includes use of parenteral analgesia, which may include morphine sulfate, fentanyl, and ketamine, among others. In some jurisdictions, ALS personnel can administer opioids under standing orders and with some degree of independence, while other jurisdictions may require approval from EMS medical direction on a case-by-case basis or may prohibit use of opioids pain management entirely based on local protocols. Injured older adults are 20%–60% less likely to receive pain management interventions, compared to young adults with similar injuries6–10 and only 8% of injured older adults receive prehospital pain medication.11 There are many reasons older adults with fall-related injury may not receive prehospital pain medication. EMS providers may not recognize pain in older adults with cognitive impairment,12–14 may underestimate severity of injuries resulting from a fall,15 or may hesitate to use opioids to treat acute pain in older adults due to concerns about addiction or delirium.16,17 EMS providers’ concerns about opioid-induced delirium are grounded in evidence opioids increase risk of delirium for intensive care unit (ICU) patients.16,18,19 Paradoxically, poor management of pain increases risk of delirium in injured older adults.20,21 With delirium incidence between 7% and 46% among older adults treated in the ED,22 the dual relationship between opioid analgesia and delirium necessitates thoughtful pain management for injured older adults, including evidence-based guidelines for prehospital pain management.
Prior work from our group indicates prehospital opioid analgesia effectively reduces pain scores for injured older adults without increasing adverse events during the prehospital interval, as reported by EMS providers prior to ED arrival.11 To further understand safety of prehospital opioid analgesia for older adults with fall-related injury, we compared incidence of delirium diagnosis, hospital disposition, and hospital length of stay for older adults with fall-related injury, according to whether prehospital opioid analgesia was used.
Methods
Study Design
This was a retrospective cohort study using Medicare claims data from the Centers for Medicare and Medicaid Services (CMS) and EMS patient care reports (PCRs) from the Illinois Department of Public Health (IDPH). Institutional Review Boards at Mass General Brigham and IDPH, and the CMS privacy board reviewed and approved this study with a waiver of informed consent. Reporting of this study adheres to the guidelines for Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
Setting and Population
Our study population included Illinois residents who were Medicare fee-for-service beneficiaries, age ≥66, with an emergency department encounter for treatment of a fall-related traumatic injury between January 1, 2014 and December 31, 2015, and a corresponding prehospital encounter with an Illinois-based EMS company. Inclusion was set at age 66 to ensure one year of pre-injury data when estimating baseline health status. The data sets included 150 hospitals and 61 EMS agencies. We defined traumatic injury based on the National Trauma Data Standard (NTDS),23 including any emergency department or inpatient diagnosis for an injury in Medicare claims, as determined by International Classification of Disease (ICD) diagnosis codes (version 9 through September 2015, version 10 from October to January 2015). NTDS requires hospital admission or death in the ED for inclusion in the National Trauma Data Bank. We expanded this definition to include patients discharged from the ED. Due to Medicare classification of hospital stays up to 72 hours as outpatient/observation, we categorized ED/outpatient encounters with at least one overnight stay as inpatient admissions. We identified fall-related injury using ICD external cause of injury codes (ecode) indicating ground level fall according to the Centers for Disease Control and Prevention framework for categorizing injury mechanisms.24,25 A full list of ecodes is provided in Supplemental Methods 1. We linked Medicare claims with EMS PCRs using probabilistic matching based on age, sex, date of birth, race, injury mechanism, date of encounter and residential zip code (Supplemental Methods 2). Medicare beneficiaries with a hospital record indicating fall-related injury but no corresponding EMS record were excluded. Transferred patients were identified based on date of encounter and discharge disposition indicating transfer to another acute care facility. Data from transferring hospitals were consolidated into a single episode of care with diagnoses and claims from all ED encounters and inpatient admissions.
Outcomes and Covariates
Our primary exposure of interest was opioid analgesia delivered by EMS providers in the prehospital setting. EMS PCRs reported medication type, dosage, and mode of administration. At the time of data collection, morphine sulfate was the only opioid analgesic approved under the Illinois EMS scope of practice. We used opioid conversion factors from CMS26 to calculate morphine milligram equivalent (MME). When a patient received multiple opioid doses, total MMEs were calculated by aggregating MMEs across all doses. We measured prehospital opioid analgesia as a binary measure of any/no exposure and as total MMEs.
We examined hospital disposition, inpatient delirium, hospital length of stay, and ICU length of stay as outcomes. We categorized discharge disposition separately for patients discharged from the ED without an overnight stay, versus inpatient care, including those admitted or with observation stays of at least one night. We categorized hospital disposition as discharge home from the ED, ED discharge to a non-home destination, discharge home from inpatient/observation care, inpatient/observation discharge to a non-home destination, or deceased. We determined trauma center level and hospital disposition for transferred patients based on data from the final admitting hospital in the episode of care. We identified delirium based on ICD diagnoses27 (Supplemental Methods 3) present in inpatient claims, or in ED claims where the patient was held for observation over at least one night. We measured hospital length of stay as the number of days from initial ED arrival to hospital discharge for patients staying at the hospital at least one night, including both ED observation and inpatient days. Patients with same day discharges from the ED were excluded from length of stay and delirium analyses. We measured ICU length of stay as total days with claims for ICU care during the episode of care. Hospital and ICU length of stay for transferred patients included the total duration of the episode of care across all hospitals.
Demographic covariates of interest included patient age in years (continuous in propensity score algorithm, categorized as 65–74, 75–84, ≥85 for descriptive statistics), sex (male, female), and race (non-Hispanic White, non-White). Patient-level prehospital clinical covariates, measured as recorded in EMS PCRs, included and pre-hospital systolic blood pressure [SBP], Glasgow coma scale [GCS], respiratory rate [RR], pulse, and blood oxygenation. When PCRs had multiple recordings of a vital sign, we included the lowest reported value in analyses. Clinical covariates derived from Medicare data included comorbidities, frailty, injury severity, and traumatic brain injury (TBI). We used Charlson Comorbidity Index (CCI)28–30 to measure comorbidities and Claims Based Frailty Index (CFBI)31 to measure frailty. We calculated both indices based on all diagnosis codes in Medicare claims during the 365-day preceding injury diagnosis. We categorized CCI as no comorbidities, one mild comorbidity, multiple mild comorbidities or one moderate comorbidity, or multiple/complex comorbidities. CFBI scores range from 0 to 1, with scores ≤0.25 categorized as non-frail and score >0.25 categorized as frail. We measured injury severity using methods from ICD Programs for Injury Categorization (ICDPIC) to calculate Injury Severity Score (ISS).32,33 We then categorized ISS as mild (1–8), moderate (9–15), severe (16–25), and critical (≥26). We identified TBI based on Abbreviated Injury Scale (AIS) scores for head injury, calculated using methods from ICDPIC. Consistent with prior identification of TBI in administrative data,34 patients with head AIS ≥2 were considered to have a TBI. Treatment covariates included EMS scene time, drive time from scene to hospital, and hospital trauma center level. Both time variables were measured in minutes using time stamps in EMS PCRs. We determined trauma center level using data from the Trauma Information Exchange Program,35 linked with Medicare claims using American Hospital Association facility identification numbers. Hospitals were categorized as Level I/II, Level III, or non-trauma center using American College of Surgeons (ACS) verification levels and state designation levels. When hospitals had different ACS and state levels, we used the most advanced level.
Analyses
We assessed univariable distributions of categorical variables, median and interquartile range (IQR) of discrete variables, and mean and standard deviation (SD) of continuous variables. We used Kolmogorov-Smirnov tests to assess normality of continuous measures distributions.
Due to concerns about confounding, we used inverse probability of treatment weighting (IPTW) to balance the distribution of covariates likely to influence EMS decisions regarding opioid administration in our exposed and unexposed groups. We used multivariable probit regression to predict probability of prehospital opioid exposure for use in models examining opioid exposure as a binary variable, and multinomial probit regression to predict probability of opioid dosing categories for use in models examining dose effect. Predictions of opioid exposure and opioid dose categories were based on age, sex, race, comorbidities, frailty, injury severity, presence of TBI, prehospital vital signs, scene time, and prehospital travel time. Small rates of missingness were observed for race and prehospital vital signs. Missing data were coded using dummy variables and included in the IPTW algorithm. Weights were stabilized by using probability of treatment as the numerator when calculating inverse probability of treatment,36 and weights were trimmed at the 1st and 99th percentile to address outliers.37 We examined standardized mean differences for all covariates before and after weighting to assess balance. We then used the inverse of the predicted probability of prehospital opioid analgesia to weight each observation in subsequent analyses. We estimated the association between prehospital opioid analgesia and probability of delirium using logistic regression, probability of hospital disposition category using multinomial logistic regression, and hospital and ICU length of stay using Poisson regression. We estimated all outcomes as a function of binary exposure to prehospital opioid analgesia. In secondary analyses we measured exposure to prehospital opioid anesthesia in terms total prehospital MMEs administered. To support interpretation of results in the context of infrequent and multinomial outcomes, we estimated marginal mean probabilities of delirium and hospital disposition, and marginal mean length of hospital and ICU stay.
Sensitivity Analysis
TBI increases risk of poor outcomes in injured older adults, including diagnosis of delirium38 and mortality.39 While we included TBI in our IPTW algorithm, it is possible TBI modifies the relationship between prehospital opioid analgesia and outcomes; therefore, we conducted a sensitivity analysis with models stratified by presence of TBI. Similarly, overall injury severity, presence of hip fracture, and exposure to general anesthesia during surgical procedures may modify the relationship between prehospital opioids and short-term outcomes; therefore, we conducted sensitivity analyses stratified by injury severity (mild vs. moderate), hip fracture, and use of operative procedures requiring general anesthesia.
Results
We identified 28,150 older adults with ED or inpatient encounters for fall-related injury and corresponding EMS PCRs (Figure 1), of which 3.2% (95% CI: 2.9, 3.4) received prehospital opioids. Morphine sulfate was the only opioid form administered prehospital, with a median dose of 4 milligrams (IQR: 2–5). The cohort was predominantly non-Hispanic White (94.3%) and female (69.8%), 45.3% were age 85 or older, and 49.7% were discharged home from the ED. Table 1 presents overall cohort characteristics and bivariable analyses covariates. Patients receiving prehospital opioid analgesia were typically younger, female, had moderate injury severity, were less likely to have a TBI, and more likely to be treated at a non-trauma center. After weighting based on the inverse probability of treatment, standardized mean differences were less than 0.1 for all covariates, indicating sufficient balance of characteristics between patients with and without prehospital opioid analgesia (Supplemental Data 1).
Figure 1: Flow diagram of cohort development.
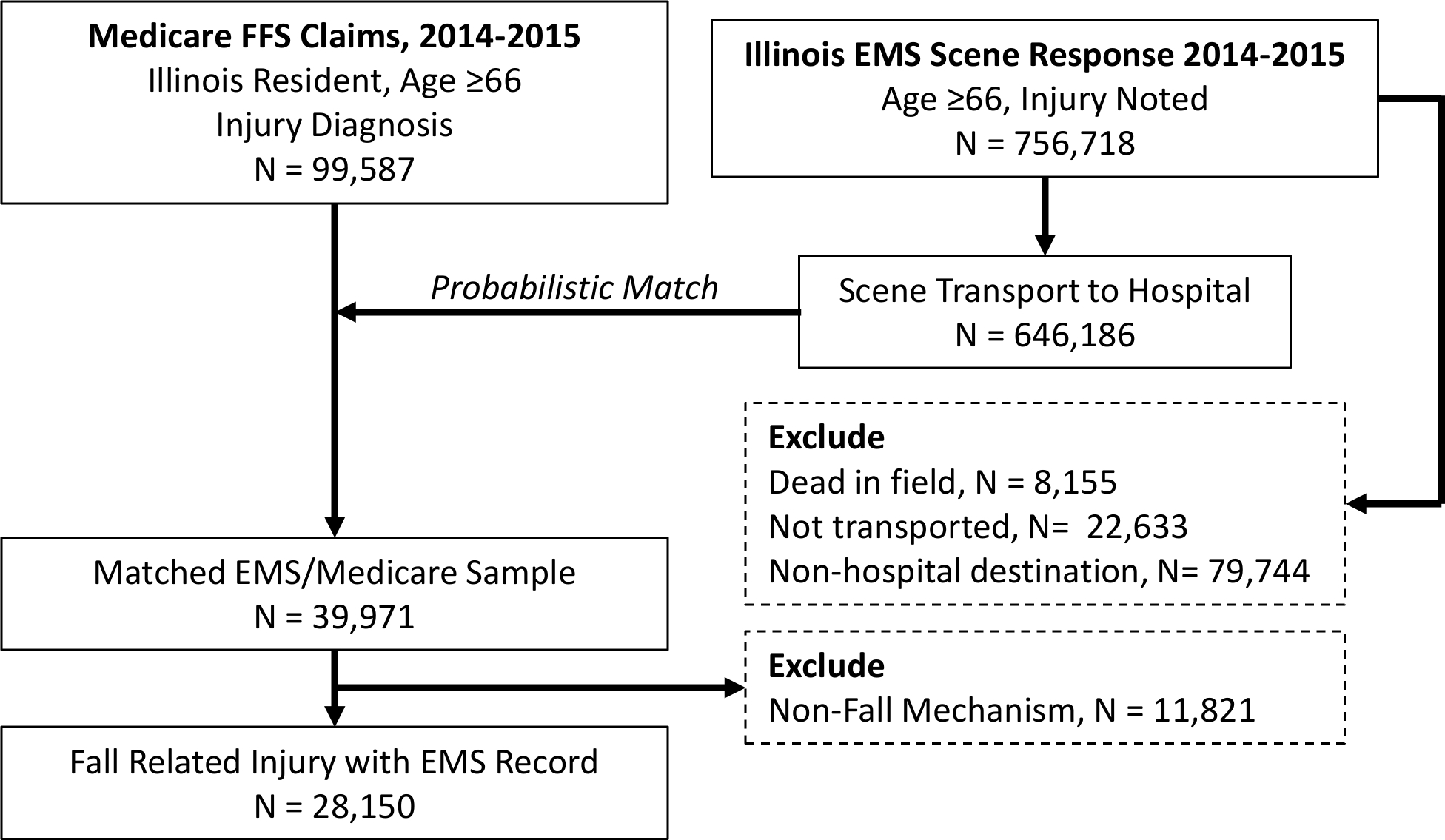
Medicare fee-for-service (FFS) claims and emergency medical services (EMS) patient care reports were linked using probabilistic matching. Medicare claims with fall-related injury diagnosis and linked with corresponding EMS records were included in analysis.
Table 1:
Distribution of patient characteristics, overall and by pre-hospital opioid exposure
| Variable | Total Population N = 28,150 | Opioid = No N = 27,260 (96.84%) | Opioid = Yes N = 890 (3.16%) |
|---|---|---|---|
| Age (%, N) | |||
| 65–74 | 20.0 (5,632) | 19.9 (5,410) | 24.9 (222) |
| 65–84 | 34.7 (9,769) | 34.7 (9,465) | 34.2 (304) |
| ≥85 | 45.3 (12,749) | 45.4 (12,385) | 40.9 (364) |
| Sex (%, N) | |||
| Female | 69.8 (19,640) | 69.5 (18,934) | 79.3 (706) |
| Male | 30.2 (8,510) | 30.5 (8,326) | 20.7 (184) |
| Race/Ethnicity (%, N) | |||
| Non-Hispanic White | 94.3 (26,537) | 94.1 (25,663) | 98.2 (874) |
| Race/Ethnicity other than White | 5.6 (1,572) | 5.7 (1,558) | 1.6 (14) |
| Unknown | 0.2 (41) | 0.1 (39) | <1.0 (<11) |
| Charlson Comorbidity Score (%, N) | |||
| 0 | 37.7 (10,622) | 37.9 (10,325) | 33.4 (297) |
| 1 | 23.0 (6,475) | 22.9 (6,263) | 23.8 (212) |
| 2 | 14.4 (4,054) | 14.3 (3,891) | 18.3 (163) |
| ≥3 | 24.9 (6,999) | 24.9 (6,781) | 24.5 (218) |
| Frailtya (%, N) | |||
| Not frail | 52.2 (14,691) | 52.1 (14,194) | 55.8 (497) |
| Frail | 47.8 (13,459) | 47.9 (13,066) | 44.2 (393) |
| Injury Severity Score (%, N) | |||
| 1–8 | 71.5 (20,132) | 72.6 (19,789) | 38.5 (343) |
| 9–15 | 24.2 (6,807) | 22.9 (6,267) | 60.7 (540) |
| 16–24 | 4.1 (1,165) | 4.3 (1,159) | <1.0 (<11) |
| ≥25 | 0.2 (46) | 0.2 (45) | <1.0 (<11) |
| Traumatic Brain Injury (%, N) | |||
| No | 76.0 (21,402) | 75.4 (20,562) | 94.4 (840) |
| Yes | 23.9 (6,748) | 24.6 (6,698) | 5.6 (50) |
| Hip Fracture (%, N) | |||
| No | 78.4 (22,071) | 79.4 (21,653) | 47.0 (418) |
| Yes | 21.6 (6,079) | 20.6 (5,607) | 53.0 (472) |
| Trauma Center Level (%, N) | |||
| Level I/II | 55.1 (15,519) | 55.9 (15,243) | 31.0 (276) |
| Level III | 0.9 (268) | 0.9 (254) | 1.6 (14) |
| Non-Trauma Center | 43.9 (12,363) | 43.2 (11,763) | 67.4 (600) |
| EMS Scene Time (mean minutes, SD) | 18.1 (35.2) | 18.0 (35.7) | 21.55 (7.95) |
| EMS Transport Time (mean minutes, SD) | 11.6 (23.6) | 11.4 (23.8) | 15.5 (13.9) |
| Prehospital Vital Signs | |||
| Lowest SPB (mean, SD) | 141.3 (28.6) | 141.3 (28.6) | 142.6 (28.2) |
| Missing SBP (%, N) | 3.9 (1,094) | 3.9 (1,088) | <1.0 (<11) |
| Lowest pulse (mean, SD) | 80.2 (18.9) | 80.2 (19.0) | 78.6 (15.4) |
| Missing pulse (%, N) | 2.8 (802) | 2.9 (800) | <1.0 (<11) |
| Lowest blood oxygenation (mean, SD) | 95.5 (16.1) | 95.6 (16.3) | 95.1 (9.1) |
| Missing blood oxygenation (%, N) | 16.6 (4,677) | 16.8 (4,587) | 10.1 (90) |
| Lowest respiratory rate (median, IQR) | 18 (16, 18) | 18 (16, 18) | 18 (16, 20) |
| Missing respiratory rate (%, N) | 2.9 (836) | 3.0 (827) | <1.0 (<11) |
| Lowest Glasgow Coma Score (median, IQR) | 15 (15, 15) | 15 (15, 15) | 15 (15, 15) |
| Missing Glasgow Coma Score (%, N) | 6.0 (1,698) | 5.9 (1,633) | 7.3 (65) |
| Delirium (%, N) | |||
| Yes | 6.4 (1,787) | 6.3 (1,725) | 6.9 (62) |
| No | 93.7 (26,363) | 93.7 (25,535) | 93.0 (828) |
| Hospital Disposition (%, N) | |||
| ED to home | 49.7 (14,015) | 50.7 (13,815) | 22.5 (200) |
| ED to non-home | 12.2 (3,446) | 12.1 (1,873) | 16.2 (144) |
| Inpatient to home | 6.8 (1,925) | 6.9 (1,873) | 5.8 (52) |
| Inpatient to non-home | 29.5 (8,290) | 28.7 (7,817) | 53.2 (473) |
| Deceased | 0.9 (239) | 0.9 (231) | <1.0 (<11) |
| Unknown | 0.8 (235) | 0.8 (222) | 1.5 (13) |
| Inpatient length of stay (median, IQR) | 4 (3, 6) | 4 (3, 6) | 4 (3, 6) |
| ICU length of stay (median, IQR) | 3 (1, 4) | 3 (1, 4) | 3 (2, 4) |
Frailty estimated using the Claims Based Frailty Score,31 which ranges from 0 to 1. Scores ≤0.25 were categorized as non-frail and scores >0.25 were categorized as frail
Figure 2 illustrates unadjusted and adjusted marginal probabilities of inpatient delirium and discharge disposition for patients with and without prehospital opioid analgesia. Figure 3 illustrates marginal probabilities by MME for patients who did receive prehospital opioid analgesia. There were no statistically significant differences in inpatient delirium and mortality. Patients receiving prehospital opioids were less likely to be discharged home from the ED (adjusted probability = 0.30 [95% CI: 0.25, 0.34] vs. 0.47 [95% CI: 0.46, 0.48]), and more likely to be discharged to a non-home setting after an inpatient admission (adjusted probability = 0.43 [95% CI: 0.39, 0.48] vs. 0.30 [95% CI: 0.30, 0.31]). The likelihood of discharge home from the ED decreased and likelihood of non-home discharge from inpatient care increased as prehospital MME increased.
Figure 2: Unadjusted and adjusted marginal probabilities of delirium and discharge disposition by prehospital binary opioid exposure.

Marginal probabilities of delirium and disposition status were compared for patients with and without prehospital opioid analgesia. Adjusted outcomes were modeled using inverse probability of treatment weights based on age, sex, race, comorbidities, frailty, injury severity, presence of TBI, prehospital vital signs, scene time, and prehospital travel time.
Figure 3: Unadjusted and adjusted marginal probabilities of inpatient delirium and discharge disposition by prehospital opioid exposure, dose effect.
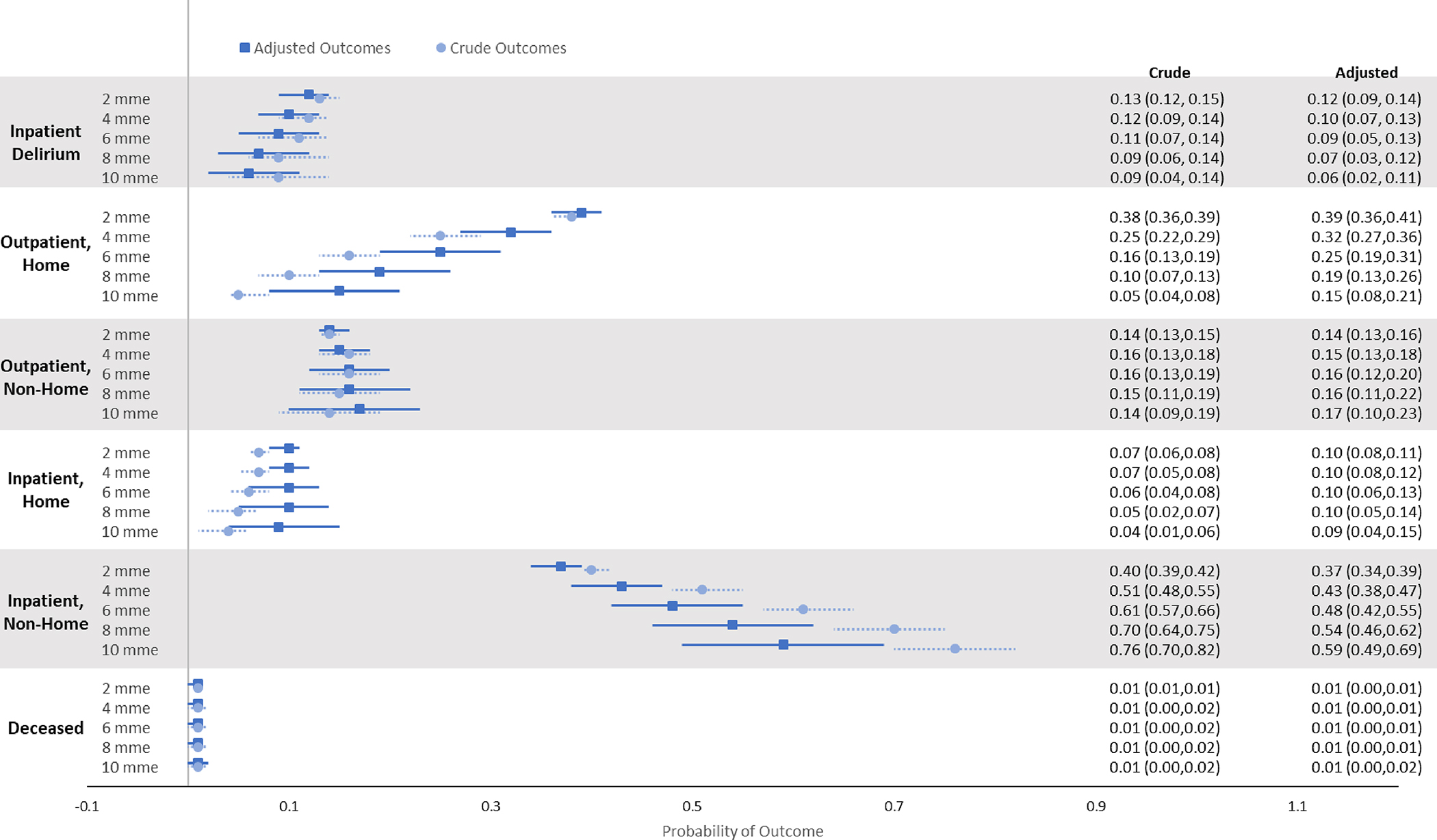
Marginal probabilities of delirium and disposition status were compared across prehospital opioid analgesia doses, measured in terms of morphine milligram equivalents (MMEs). Adjusted outcomes were modeled using inverse probability of treatment weights based on age, sex, race, comorbidities, frailty, injury severity, presence of TBI, prehospital vital signs, scene time, and prehospital travel time.
Unadjusted and adjusted marginal mean hospital length of stay and ICU length of stay are presented in Table 2. In adjusted analysis, average hospital length of stay was 0.4 days shorter (p<0.001) for patients receiving prehospital opioid analgesia, compared to those without. ICU length of stay was 0.7 days shorter (p=0.045) for those receiving prehospital opioid analgesia, compared to those without. Hospital and ICU length of stay were consistent across prehospital MME doses. Model parameters are reported in Supplemental Data 2.
Table 2:
Marginal medians for hospital and ICU length of stay by prehospital opioid exposure
| Mean Days (95% Confidence Interval) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | No Opioids | Any Opioids | p | 2 mme | 4 mme | 6 mme | 8mme | 10 mme | p |
| Hospital LOS | 4.9 (4.8, 5.1) | 4.9 (4.6, 5.1) | 0.68 | 4.9 (4.8, 4.1) | 4.9 (4.7, 5.1) | 5.0 (4.7, 5.2) | 5.0 (4.6, 5.3) | 5.0 (4.6, 5.4) | 0.73 |
| ICU LOS | 3.2 (2.9, 3.4) | 3.2 (2.7, 3.6) | 0.94 | 3.2 (2.9, 3.5) | 3.2 (2.8, 3.6) | 3.2 (2.6, 3.8) | 3.2 (2.4, 4.0) | 3.2 (2.2, 4.2) | 0.92 |
| Adjusted | |||||||||
| Hospital LOS | 5.1 (4.9, 5.3) | 4.7 (4.5, 4.9) | <0.01 | 4.9 (4.7, 5.1) | 4.8 (4.6, 4.9) | 4.7 (4.5, 4.9) | 4.6 (4.3, 4.9) | 4.6 (4.2, 4.9) | 0.06 |
| ICU LOS | 3.5 (3.1, 3.8) | 2.8 (2.3, 3.4) | 0.05 | 3.2 (2.8, 3.5) | 2.9 (2.4, 3.5) | 2.8 (2.0, 3.5) | 2.6 (1.7, 3.5) | 2.4 (1.3, 3.5) | 0.17 |
Adjusted outcomes modeled using inverse probability of treatment weights based on age, sex, race, comorbidities, frailty, injury severity, presence of TBI, prehospital vital signs, scene time, and prehospital travel time.
Sensitivity analysis
Results of models stratified by TBI, severity, hip fracture, and surgical status are presented in Supplemental Tables 3-10. Sensitivity analyses did not result in changes to the observed magnitude, direction, and statistical significance of associations between prehospital opioid analgesia.
Discussion
This single state, cohort study suggests prehospital use of opioid analgesia for pain management in older adults with fall-related injury is associated with higher likelihood of inpatient admission and decreased average length of stay for admitted patients; however, our findings do not provide evidence of an association between pre-hospital analgesia and likelihood of inpatient delirium. These findings, combined with our prior findings that prehospital opioids effectively reduce pain scores in older trauma patients without increasing incidence of adverse events in the prehospital interval,11 indicate use of prehospital opioid analgesia in injured older adults has both potential clinical benefits and implications for the course of subsequent care, highlighting the need for future investigation to inform specific guidelines for early pain management in this population.
These findings are especially relevant in the context of recently published guidelines for prehospital pain management, in which intravenous opioids were recommended over non-steroidal anti-inflammatory drugs and intravenous acetaminophen was recommended over opioids.4 Additionally, the recommendation for intravenous acetaminophen was tempered by concerns about costs and availability. The recent introduction of generic intravenous acetaminophen40 will likely result in increased use of acetaminophen for prehospital pain management. Ultimately, both recommendations were made with low certainty of evidence, and no specific recommendations were made for older adults, reinforcing the need for ongoing research regarding the safety and effectiveness of prehospital pain management.
Our analyses suggest prehospital opioid analgesia is associated with hospital disposition. The relationship between prehospital opioid analgesia and discharge home from the ED displayed a dose effect, with likelihood of discharge home decreasing incrementally with each 2 MME increase in opioid dose. Conversely, the likelihood of discharge to non-home settings from inpatient care increased with each 2 MME increase in prehospital opioid dose. Adjustment for confounding variables attenuated this relationship slightly, indicating the difference may partially be explained by differences in injury severity or other clinical characteristics that increase both apparent need for early pain management interventions and need for inpatient admission, as demonstrated in our prior work.11 Nevertheless, the residual dose effect in our adjusted analysis suggests use of prehospital opioid analgesia may necessitate inpatient admissions when discharge home from the ED would otherwise be possible. This highlights the need to better understand how to balance potential benefits of early pain control with implications for hospital admission and destination at discharge. Research addressing this potential tradeoff necessitates prospective data collection and should incorporate patient preferences and experiences to align clinical recommendations with patients’ priorities.
Our findings also point to shorter inpatient and ICU length of stay for older adults receiving opioids in the prehospital setting. In contrast with other outcomes examined, the relationship between length of stay and prehospital opioids does not appear to have a dose effect. Early pain control is associated with shorter ED length of stay among patients presenting with severe pain41 and those with traumatic injury.42 It is possible early pain management contributed to shorter inpatient and ICU stays in our study by facilitating faster ED throughput, and thus faster delivery of definitive inpatient interventions. Additionally, poor pain control contributes to delays in discharge for hip fracture patients,43 and early opioid pain management may contribute to shorter length of stay as part of a comprehensive pain management approach. Alternatively, as indicated by discharge disposition, prehospital opioids may necessitate inpatient admission or overnight observation for patients who would otherwise be discharged home from the ED. If this is the case, then average length of stay may be decreased due to admission of low acuity patients for short lengths of stay.
We did not find a statistically significant association between inpatient delirium diagnosis and prehospital opioid analgesia; however, our findings do indicate potential increase in incidence of delirium with higher opioid dosages. While not statistically significant, widening confidence intervals with increasing dosages suggest the lack of observed statistical significance may be due to small sample size at this dosage level. It is also possible prehospital opioid dose is correlated with other variables that increase risk of delirium, including pain severity. In this context, our findings are consistent with prior studies demonstrating increased risk of delirium in injured older adults with poor or delayed pain management in the ED setting.43,44
Our sensitivity analyses suggested the relationship between outcomes and prehospital opioid analgesia did not vary by TBI status, injury severity, hip fracture diagnosis, or use of general anesthesia; however, these analyses were limited by small sample size. Variation in clinical outcomes for subgroups examined in sensitivity analyses highlights the need to examine safety and effectiveness of prehospital opioid analgesia in specific patient populations. Data on the impact of prehospital opioids on TBI patients is especially critical to future pain management guidelines, given the complex relationship between TBI, pain, delirium, and dementia,43,45–47 as well as the prevalence of TBI among injured older adults.48
Notably, only 3% of patients in our sample received prehospital opioids, which is substantially lower than 8% observed in national data.11 There are many possible reasons for this difference. Medications administered by EMS personnel are limited both by credentials of personnel responding to the 911 call and by protocols in place in the EMS jurisdiction.49 In the US, use of opioids in the prehospital setting requires credentialling as an advanced emergency medical technician or paramedic. This level of care may not be available in all communities, or may have limited availability in communities with limited EMS resources. Prehospital opioid administration also requires standing orders or case-by-case consultation with the EMS medical director. Geographic variation in medication protocols and time burden may contribute to lower-than-expected use of opioid analgesia in our sample.
Limitations
This study used administrative data from a single state and relies on probabilistic matching to link data on prehospital care with hospital outcomes. As a result, non-Hispanic White patients and urban residents are overrepresented in analysis, compared to the population observed in national Medicare data (Supplemental Methods 2). This may limit generalizability of findings to patients from other racial groups and from rural communities. Data used in this study are from injuries occurring in 2014–2015. Analyses presented are not currently feasible with more recent data due to a prolonged data acquisition process, need for at least one-year of post-injury data for other planned analyses, and potential for historical effects introduced by the COVID-19 pandemic. It is possible prehospital practices have changed in intervening years; however, it is unlikely the relationship between prehospital opioids and clinical outcomes has changed. Our prior work indicated a correlation between pain scores and likelihood of prehospital opioid administration,11 raising concerns about confounding by indication. We used IPTW to reduce likelihood of bias from confounding by indication. We considered the EMS pain management decision process and selected variables that would be known to EMS clinicians and potentially influence pain management practices for inclusion in the IPTW algorithm. This process improved the balance of demographic and clinical characteristics between opioid exposed and unexposed groups; however, we cannot account for unmeasured covariates, specifically the intensity and duration of severe pain during the prehospital interval. Conceptually, pain intensity and duration increase the likelihood of exposure to prehospital opioids and the likelihood of delirium; therefore, we would expect the confounding to attenuate the association between prehospital opioids and incidence of delirium. We relied on external cause of injury codes to identify patients with fall-related injury, which may undercount patients, particularly those with severe injury requiring hospitalization;50 however this approach allows a higher degree of specificity in identification of fall-related injury, supporting a targeted approach to development of clinical guidelines. Finally, it is difficult to assess delirium using administrative diagnostic data. Delirium is underdiagnosed in inpatient settings.45 Underdiagnosis is likely consistent across treatment and control groups, having minimal impact on the observed associations. We also cannot assess timing of delirium diagnoses relative to onset of symptoms and other interventions that might contribute to development of delirium, including inpatient opioid analgesia and general anesthesia. Our sensitivity analyses stratifying by TBI, injury severity, hip fracture, and use of general anesthesia, all factors known to disrupt brain activity and increase risk of delirium, did not reveal substantial changes in the relationship between prehospital opioids and delirium.
Conclusion
The incidence of fall related injury will increase as the US population ages. Current guidelines for prehospital care of injured older adults are limited, leading to underutilization of available interventions. Our findings suggest use of opioid analgesia for management of pain in older adults with fall-related may be associated with discharge disposition, length of stay, and incidence of inpatient delirium. The association between prehospital opioid analgesia and outcomes varies by dose used, highlighting the need for prehospital pain management guidelines specific to the older adult population.
Supplementary Material
Additional supporting information can be found online in the Supporting Information section at the end of this article.
Supplemental Methods 1: Probabilistic Matching Procedures
Supplemental Methods 2: International Classification of Disease External Cause of Injury Codes for Ground Level Falls
Supplemental Methods 3: International Classification of Disease Diagnosis Codes for Delirium
Supplemental Data 1: Standardized Mean Differences, before and after weighting by inverse probability of treatment. (A) Binary opioid exposure; (B) Opioid Dose 0 vs 2 MME; (C) Opioid Dose 0 vs 4 MME; (D) Opioid Dose 0 vs 6 MME.
Supplemental Data 2: Parameters from inverse probability of treatment weighted regression models estimating outcomes by prehospital opioid exposure
Supplemental Data 3: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis, excluding patients with TBI
Supplemental Data 4: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis among patients with TBI
Supplemental Data 5: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis limited to mild injury (injury severity score [ISS] <9).
Supplemental Data 6: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis limited to moderate injury (ISS 9–15)
Supplemental Data 7: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis among patients with hip fracture
Supplemental Data 8: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis excluding patients with hip fracture
Supplemental Data 9: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis excluding patients with surgical procedure
Supplemental Data 10: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis among patients with surgical procedure
Keypoints:
Few injured older adults receive prehospital opioid analgesia
Prehospital opioid analgesia may be associated with hospital and post-acute care disposition and longer lengths of stay
Incidence of delirium was not associated with prehospital opioid analgesia
Why does this paper matter?
Associations between prehospital opioid analgesia and outcomes are mixed, highlighting the need for prehospital pain management guidelines specific to the older adult population.
Funding:
Research reported in this publication was supported by the National Institute of Aging of the National Institutes of Health under award number K01AG065414.
Sponsor’s Role:
The National Institute on Aging had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Footnotes
Conflicts of Interest: Authors report no conflicts of interest associated with this work.
References
- 1.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. doi: 10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- 2.Frederick PD. EMS Data Cube. NEMSIS. Accessed October 22, 2020. https://nemsis.org/view-reports/public-reports/ems-data-cube/ [Google Scholar]
- 3.Agency for Healthcare Research and Quality. HCUPnet Data Tools | AHRQ Data Tools. Accessed February 21, 2023. https://datatools.ahrq.gov/hcupnet
- 4.Lindbeck G, Shah MI, Braithwaite S, et al. Evidence-Based Guidelines for Prehospital Pain Management: Recommendations. Prehosp Emerg Care. 2023;27(2):144–153. doi: 10.1080/10903127.2021.2018073 [DOI] [PubMed] [Google Scholar]
- 5.National Association of State EMS Officials. National Model EMS Clincal Guidelines. Version 3.0. Published online March 2022. Accessed March 10, 2023. https://nasemso.org/wp-content/uploads/National-Model-EMS-Clinical-Guidelines_2022.pdf
- 6.Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US emergency department patients are less likely to receive pain medication than younger patients: results from a national survey. Ann Emerg Med. 2012;60(2):199–206. doi: 10.1016/j.annemergmed.2011.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Platts-Mills TF, Hunold KM, Weaver MA, et al. Pain treatment for older adults during prehospital emergency care: variations by patient gender and pain severity. J Pain. 2013;14(9):966–974. doi: 10.1016/j.jpain.2013.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terrell KM, Hui SL, Castelluccio P, Kroenke K, McGrath RB, Miller DK. Analgesic prescribing for patients who are discharged from an emergency department. Pain Med. 2010;11(7):1072–1077. doi: 10.1111/j.1526-4637.2010.00884.x [DOI] [PubMed] [Google Scholar]
- 9.Marra EM, Mazer-Amirshahi M, Mullins P, Pines JM. Opioid Administration and Prescribing in Older Adults in U.S. Emergency Departments (2005–2015). West J Emerg Med. 2018;19(4):678–688. doi: 10.5811/westjem.2018.5.37853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang U, Richardson LD, Harris B, Morrison RS. The quality of emergency department pain care for older adult patients. J Am Geriatr Soc. 2010;58(11):2122–2128. doi: 10.1111/j.1532-5415.2010.03152.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dalton MK, Semco RS, Ordoobadi AJ, et al. Opioid administration in the prehospital setting for patients sustaining traumatic injuries: An evaluation of national emergency medical services data. Injury. 2022;53(9):2923–2929. doi: 10.1016/j.injury.2022.03.068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herr K Pain in the older adult: an imperative across all health care settings. Pain Manag Nurs. 2010;11(2 Suppl):S1–10. doi: 10.1016/j.pmn.2010.03.005 [DOI] [PubMed] [Google Scholar]
- 13.Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med. 2001;17(3):457–478, vi. doi: 10.1016/s0749-0690(05)70080-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCleane G Pain perception in the elderly patient. Clin Geriatr Med. 2008;24(2):203–211, v. doi: 10.1016/j.cger.2007.12.008 [DOI] [PubMed] [Google Scholar]
- 15.Newgard CD, Holmes JF, Haukoos JS, et al. Improving early identification of the high-risk elderly trauma patient by emergency medical services. Injury. 2016;47(1):19–25. doi: 10.1016/j.injury.2015.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing. 2011;40(1):23–29. doi: 10.1093/ageing/afq140 [DOI] [PubMed] [Google Scholar]
- 17.Cavalieri TA. Management of pain in older adults. J Am Osteopath Assoc. 2005;105(3 Suppl 1):S12–17. [PubMed] [Google Scholar]
- 18.Dubois MJ, Bergeron N, Dumont M, Dial S, Skrobik Y. Delirium in an intensive care unit: a study of risk factors. Intensive Care Med. 2001;27(8):1297–1304. doi: 10.1007/s001340101017 [DOI] [PubMed] [Google Scholar]
- 19.Marcantonio ER, Juarez G, Goldman L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272(19):1518–1522. [PubMed] [Google Scholar]
- 20.American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57(8):1331–1346. doi: 10.1111/j.1532-5415.2009.02376.x [DOI] [PubMed] [Google Scholar]
- 21.AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205–224. doi: 10.1046/j.1532-5415.50.6s.1.x [DOI] [PubMed] [Google Scholar]
- 22.Oliveira J E Silva L, Berning MJ, Stanich JA, et al. Risk Factors for Delirium in Older Adults in the Emergency Department: A Systematic Review and Meta-Analysis. Ann Emerg Med. Published online June 11, 2021:S0196–0644(21)00194–3. doi: 10.1016/j.annemergmed.2021.03.005 [DOI] [PubMed] [Google Scholar]
- 23.American College of Surgeons Committee on Trauma. National Trauma Data Standard: Data Dictionary, 2015 Admissions. https://www.facs.org/-/media/files/quality-programs/trauma/ntdb/ntds/data-dictionaries/ntds-data-dictionary-2015.ashx
- 24.Recommended framework for presenting injury mortality data. MMWR Recomm Rep. 1997;46(RR-14):1–30. [PubMed] [Google Scholar]
- 25.Hedegaard H, Johnson RL, Garnett MF, Thomas KE. The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) External Cause-of-injury Framework for Categorizing Mechanism and Intent of Injury. Natl Health Stat Report. 2019;(136):1–22. [PubMed] [Google Scholar]
- 26.Centers for Medicare & Medicaid Services. Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors. Published online January 1, 2020. https://www.hhs.gov/guidance/document/opioid-oral-morphine-milligram-equivalent-mme-conversion-factors-0
- 27.Franks JA, Anderson JL, Bowman E, Li CY, Kennedy RE, Yun H. Inpatient Diagnosis of Delirium and Encephalopathy: Coding Trends in 2011–2018. J Acad Consult Liaison Psychiatry. 2022;63(5):413–422. doi: 10.1016/j.jaclp.2021.12.006 [DOI] [PubMed] [Google Scholar]
- 28.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 29.Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res. 2008;8:12. doi: 10.1186/1472-6963-8-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang JX, Iwashyna TJ, Christakis NA. The performance of different lookback periods and sources of information for Charlson comorbidity adjustment in Medicare claims. Med Care. 1999;37(11):1128–1139. doi: 10.1097/00005650-199911000-00005 [DOI] [PubMed] [Google Scholar]
- 31.Kim DH, Glynn RJ, Avorn J, et al. Validation of a Claims-Based Frailty Index Against Physical Performance and Adverse Health Outcomes in the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2019;74(8):1271–1276. doi: 10.1093/gerona/gly197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Statistical Software Components. Published online October 29, 2010. Accessed October 22, 2020. https://ideas.repec.org/c/boc/bocode/s457028.html [Google Scholar]
- 33.Wan V, Reddy S, Thomas A, et al. How Does Injury Severity Score Derived from ICDPIC Utilizing ICD-10-CM Codes Perform Compared to Injury Severity Score Derived from TQIP? J Trauma Acute Care Surg. Published online May 30, 2022. doi: 10.1097/TA.0000000000003656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Savitsky B, Givon A, Rozenfeld M, Radomislensky I, Peleg K. Traumatic brain injury: It is all about definition. Brain Inj. 2016;30(10):1194–1200. doi: 10.1080/02699052.2016.1187290 [DOI] [PubMed] [Google Scholar]
- 35.American Trauma Society. Trauma Information Exchange Program (TIEP) - American Trauma Society. Accessed October 22, 2020. https://www.amtrauma.org/page/tiep [Google Scholar]
- 36.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. doi: 10.1097/00001648-200009000-00011 [DOI] [PubMed] [Google Scholar]
- 37.Cole SR, Hernán MA. Constructing Inverse Probability Weights for Marginal Structural Models. Am J Epidemiol. 2008;168(6):656–664. doi: 10.1093/aje/kwn164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bryczkowski SB, Lopreiato MC, Yonclas PP, Sacca JJ, Mosenthal AC. Risk factors for delirium in older trauma patients admitted to the surgical intensive care unit. J Trauma Acute Care Surg. 2014;77(6):944–951. doi: 10.1097/TA.0000000000000427 [DOI] [PubMed] [Google Scholar]
- 39.Jarman MP, Jin G, Weissman JS, et al. Association of Trauma Center Designation With Postdischarge Survival Among Older Adults With Injuries. JAMA Netw Open. 2022;5(3):e222448. doi: 10.1001/jamanetworkopen.2022.2448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.New Generic Acetaminophen injection is Available. Pharmacy Times. Published December 9, 2020. Accessed January 24, 2024. https://www.pharmacytimes.com/view/new-generic-acetaminophen-injection-is-available [Google Scholar]
- 41.Sokoloff C, Daoust R, Paquet J, Chauny JM. Is adequate pain relief and time to analgesia associated with emergency department length of stay? A retrospective study. BMJ Open. 2014;4(3):e004288. doi: 10.1136/bmjopen-2013-004288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hughes JA, Brown NJ, Chiu J, Allwood B, Chu K. The relationship between time to analgesic administration and emergency department length of stay: A retrospective review. J Adv Nurs. 2020;76(1):183–190. doi: 10.1111/jan.14216 [DOI] [PubMed] [Google Scholar]
- 43.Morrison SR, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103(3):303–311. doi: 10.1016/S0304-3959(02)00458-X [DOI] [PubMed] [Google Scholar]
- 44.Daoust R, Paquet J, Boucher V, Pelletier M, Gouin É, Émond M. Relationship Between Pain, Opioid Treatment, and Delirium in Older Emergency Department Patients. Acad Emerg Med. 2020;27(8):708–716. doi: 10.1111/acem.14033 [DOI] [PubMed] [Google Scholar]
- 45.Israni J, Lesser A, Kent T, Ko K. Delirium as a predictor of mortality in US Medicare beneficiaries discharged from the emergency department: a national claims-level analysis up to 12 months. BMJ Open. 2018;8(5):e021258. doi: 10.1136/bmjopen-2017-021258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crane PK, Gibbons LE, Dams-O’Connor K, et al. Association of Traumatic Brain Injury With Late-Life Neurodegenerative Conditions and Neuropathologic Findings. JAMA Neurol. 2016;73(9):1062–1069. doi: 10.1001/jamaneurol.2016.1948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davis DHJ, Muniz-Terrera G, Keage HAD, et al. Association of Delirium With Cognitive Decline in Late Life: A Neuropathologic Study of 3 Population-Based Cohort Studies. JAMA Psychiatry. 2017;74(3):244–251. doi: 10.1001/jamapsychiatry.2016.3423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gelbard R, Inaba K, Okoye OT, et al. Falls in the elderly: a modern look at an old problem. Am J Surg. 2014;208(2):249–253. doi: 10.1016/j.amjsurg.2013.12.034 [DOI] [PubMed] [Google Scholar]
- 49.National Association of State EMS Officials. National EMS Scope of Practice Model. Accessed October 22, 2020. https://www.ems.gov/pdf/National_EMS_Scope_of_Practice_Model_2019.pdf
- 50.Mintz J, Duprey MS, Zullo AR, et al. Identification of Fall-Related Injuries in Nursing Home Residents Using Administrative Claims Data. J Gerontol A Biol Sci Med Sci. 2022;77(7):1421–1429. doi: 10.1093/gerona/glab274 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional supporting information can be found online in the Supporting Information section at the end of this article.
Supplemental Methods 1: Probabilistic Matching Procedures
Supplemental Methods 2: International Classification of Disease External Cause of Injury Codes for Ground Level Falls
Supplemental Methods 3: International Classification of Disease Diagnosis Codes for Delirium
Supplemental Data 1: Standardized Mean Differences, before and after weighting by inverse probability of treatment. (A) Binary opioid exposure; (B) Opioid Dose 0 vs 2 MME; (C) Opioid Dose 0 vs 4 MME; (D) Opioid Dose 0 vs 6 MME.
Supplemental Data 2: Parameters from inverse probability of treatment weighted regression models estimating outcomes by prehospital opioid exposure
Supplemental Data 3: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis, excluding patients with TBI
Supplemental Data 4: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis among patients with TBI
Supplemental Data 5: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis limited to mild injury (injury severity score [ISS] <9).
Supplemental Data 6: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis limited to moderate injury (ISS 9–15)
Supplemental Data 7: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis among patients with hip fracture
Supplemental Data 8: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis excluding patients with hip fracture
Supplemental Data 9: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis excluding patients with surgical procedure
Supplemental Data 10: Adjusted probabilities of delirium diagnosis and hospital disposition, and adjusted hospital and ICU length of stay, by prehospital opioid exposure from sensitivity analysis among patients with surgical procedure


