Abstract
Purpose of Review
Gluteus medius and minimus tears, or hip abductor tendon tears, are increasingly identified as a source of lateral hip pain. Once underappreciated and undertreated, they are now recognized as a cause of greater trochanteric pain syndrome and a pathology amenable to both nonoperative and operative modalities. This review summarizes relevant anatomy, clinical presentation, and treatment options for gluteus medius tears, focusing on surgical options.
Recent Findings
When surgical intervention is indicated, repair, reconstruction, or tendon transfer may be considered. Open and endoscopic repair techniques demonstrate similar outcomes with improvements in patient-reported outcomes and low complication and retear rates for both partial and full thickness tears. Variations in fixation construct and graft augmentations have been described, though clinical evidence remains limited to support specific techniques. Gluteus maximus transfer via open approach is a salvage option for the severely atrophied, retracted, or revision gluteus tendon; however, persistent limitations in abduction strength and gait abnormalities are common.
Summary
Emerging evidence continues to evolve our understanding of surgical decision-making for gluteus tendon tears. The current literature supports either open or endoscopic repair techniques and open tendon transfer as a salvAage option. Further study is needed to determine the optimal fixation construct, the role of graft augmentation, and patient-related factors that influence postoperative outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12178-024-09896-w.
Keywords: Gluteus tendon tear, Hip abductor tendon tear, Greater trochanteric pain syndrome, Endoscopic gluteus repair, Gluteus maximus transfer
Introduction
The gluteal tendons play a crucial role in facilitating movement, stability, and force transmission for the hip joint [1••, 2]. The gluteus medius and minimus function as the main abductors of the hip and structural compromise of these tendons, also collectively referred to as tears of the hip abductor complex (HAT), have gained much attention in the literature in recent years as a source of symptoms in greater trochanteric pain syndrome (GTPS) [3]. GTPS is a complex and debilitating clinical entity that encompasses the range of tendinopathy to tears of the abductor tendons, iliotibial band (ITB) syndrome, external coxa sultans, trochanteric bursitis, among other conditions [4]. Within the spectrum of these conditions, the identification and management of HAT have garnered increased concern given their potential to fail nonoperative management and require surgical intervention.
First dubbed, “the rotator cuff tears of the hip” by Bunker et al. in a series of patients with femoral neck fractures, gluteus tendon tears have been observed in several clinical scenarios [5–8]. The first are noted at the time of surgery for elective total hip arthroplasty (THA) or fracture, as in Bunker’s original series. The second are tears or avulsions after THA, particularly with direct lateral approaches. A third clinical scenario that may be encountered, less frequently, is acute traumatic ruptures [9–11]. Finally, chronic, degenerative tears with associated tendinopathy have been observed, as in GTPS. While initial studies regarding the surgical management of gluteus tears supported the use of primarily of open approaches to the first two clinical scenarios with fracture or arthroplasty, more recent approaches have supported the use of both open and endoscopic approaches to patients with GTPS or acute traumatic tears [1••, 12, 13].
The body of literature regarding diagnosis and management of gluteus tendon tears has rapidly evolved over the last several years. In particular, updated surgical techniques and outcome studies have become available. This review of HAT repairs will discuss the relevant anatomy, diagnosis and imaging, and treatment of gluteal tendon tears with a specific focus on contemporary surgical management.
Anatomy
The muscular support surrounding the hip joint has been compared to the rotator cuff of the shoulder, with the gluteus minimus and medius originating from the external iliac fossa and attaching onto the greater trochanter akin to the supraspinatus, infraspinatus, and teres minor tendons inserting on to the greater tuberosity [6, 14, 15]. More specifically, the gluteus medius muscle originates from the outer surface of the ilium and inserts onto the greater trochanter [16]. The gluteus minimus also originates from the outer surface of the ilium, deep to the medius and inserts onto the greater trochanter, deep and anterior to the medius tendon [15].
The greater trochanter has 4 distinct osseous facets that serve as tendon attachment and bursa sites: anterior, lateral, posterior, and superior-posterior [17]. The gluteus medius muscle has an anterior middle and posterior aspect, with the medius tendon inserting onto the greater trochanter on the lateral and superior-posterior facets [6, 14, 16]. The gluteus minimus tendon inserts onto the anterior facet of the greater trochanter, deep to the medius tendon, as well as onto the anterior and superior hip joint capsule [18, 19].
Radiological studies have demonstrated that gluteus minimus tears occur at the distal aspect of the tendon inserting onto the anterior aspect of the greater trochanter [18]. Similarly, tears of the medius are most commonly torn at their insertion point on the greater trochanter [6]. Both medius and minimus are innervated by the superior gluteal nerve and receive bloody supply from branches of the superior gluteal artery [15].
The major function of the gluteus medius and minimus is hip abduction and stabilization of the pelvis during ambulation [17]. Injury to these tendons can result in Trendelenburg gait, a pattern of gait characterized by dropping of the contralateral hemipelvis during the stance phase of ambulation. The mechanism for this pathological gait is due to inadequate hip abduction and stabilization, with patients dipping or leaning with their trunk to compensate [20]. Because the abductors are deficient (either due to a disruption along the musculo-tendinous unit or due to injury to the superior gluteal nerve), they cannot keep the ipsilateral pelvis close to the greater trochanter. The ipsilateral hemipelvis therefore rises relative to the trochanter during gait (or during single-limb stance). The trunk leans towards the affected side to prevent the center of gravity from shifting to the uninjured side, which would result in loss of balance [21].
The gluteus maximus is the most superficial and largest of the gluteal muscles and makes up the majority of the contour and form of the buttock and hip region [22, 23]. The gluteus maximus originates from the posterior iliac crest, sacrum and coccyx, with two insertion points: the superficial fibers insert into the iliotibial band (ITB) and the deep fibers insert onto the gluteal tuberosity between the vastus lateralis and adductor magnus [14]. The gluteal tuberosity acts as the proximal extension of the linea aspera on the posterior aspect of the femur. The gluteus maximus functions as the major extensor of the hip joint, though it also plays a role in hip abduction. Injuries to the gluteus maximus muscle can lead to difficulties in movements that necessitate hip extension, like lunging forward or rising from a squatting position, or going up and down stairs [24, 25]. Given that the gluteus maximus muscle is active in both hip abduction and extension, if the anterior portion of the tendon is directly attached to the greater trochanter through a tendon transfer, it is capable of actively abducting the hip joint [26]. The gluteus maximus is innervated by the inferior gluteal nerve and the blood supply is primarily from superior and inferior gluteal arteries [27].
Lastly, the proximal ITB begins as three distinct layers—superficial, intermediate, and deep IT layers—that course distally to converge at the level of the greater trochanter. The ITB goes on to extend over the lateral aspect of the lower extremity before inserting onto Gerdy’s tubercle on the lateral/proximal tibia [28].
Indications
Patients with atraumatic hip abductor tears often present with the symptoms of GTPS, namely an aching and dull pain of insidious onset on the lateral aspect of the hip that is exacerbated by weight-bearing palpation of the lateral hip and laying on the affected side [8, 29]. Women are more commonly affected by abductor tendon tears, in particular those between the ages from 40 to 60 [7]. Additionally, Meghpara et al. found that men who present with the symptoms of GTPS and hip abductor tears often present at an older age than women [29].
Treatment of degenerative HAT starts with a trial of nonoperative management, lasting approximately 3 months. Nonoperative interventions include activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, platelet-rich plasma injections, and corticosteroid injections [7, 8, 16, 29, 30]. The most common medications used to treat GTPS include NSAIDS and simple non-opioid analgesics. Opioids should be avoided, as their use could exacerbate balance issues, precipitating a fall [31]. With regard to physical therapy, exercise is recommended early in the course of treatment for gluteal tendinopathies, with eccentric exercise recognized as a superior protocol compared to a generic exercise approach [32].
When initial conservative treatment fails, corticosteroid injection into the lateral trochanteric bursa, immediately adjacent to the abductor tendons, has been shown to relieve pain in 60–100% of cases of GTPS [31, 33]. Additionally, platelet-rich plasma injections have been employed as treatments in many other tendinopathies as well as abductor tendon tears, though literature is mixed regarding its efficacy [34, 35]. One randomized controlled trial by Fitzpatrick et al. showed improved pain scores with PRP compared to corticosteroid injections, though existing literature is far from conclusive [7, 34].
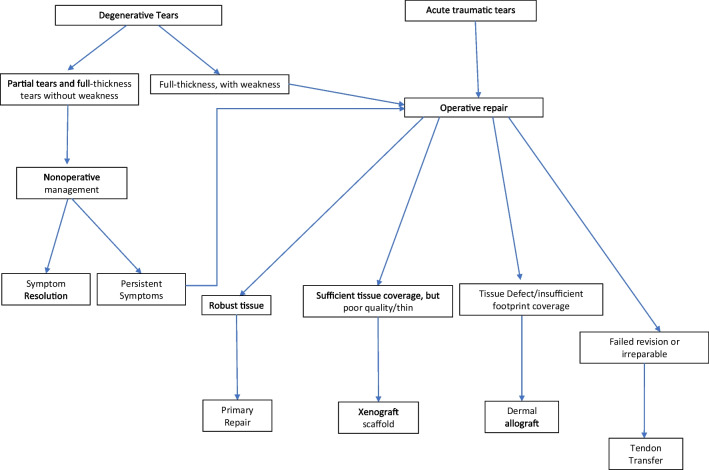
Operative indications for HAT are similar to that of rotator cuff tendon tears. Degenerative HAT is indicated for repair in the setting of persistent peritrochanteric hip pain that sufficiently interferes with activities of daily living despite nonoperative management [6, 7, 36]. Patients with degenerative full thickness tears of the abductor tendons without weakness can still undergo a trial of nonoperative management if symptoms are limited to pain. If there is associated weakness and/or gait abnormality, the threshold for surgical intervention should be much lower [7, 29]. A 2015 study by Chandrasekaran et al. demonstrated an odds ratio of 14 for requiring surgery in patients with full thickness gluteus medius tears and gait abnormalities compared to those without gait deviation [37]. This is because these deficits are less likely to be restored without re-establishing the muscle-tendon-bone unit. Similar to rotator cuff tears, chronic (typically full thickness) HAT may undergo fatty infiltration, compromising the quality of the muscle limiting the efficacy of repair, even if the tendon were to be successfully re-attached to the bone. Unlike degenerative tears, traumatic tears in younger patients should be considered for acute surgical intervention (Fig. 1).
Fig. 1.
Treatment algorithm for gluteal tendon tears
Surgical Techniques
Partial Tendon Tears
Existing evidence suggests an unexpected preponderance of patients undergoing abductor tendon repair have partial thickness injuries, comprising 63–89% of patients [12, 30, 38•, 39•]. These partial thickness tears are more often seen on the articular side of the tendon and have been referred to as partial articular gluteus tendon avulsions (PAGTA) [16, 40, 41]. This may be due to the fact that full thickness tears may be deemed irreparable and excluded from such reports, or because partial tears are so much more common than full thickness tears in general, even if most can be treated nonoperatively.
One challenge with partial tendon tears is how to access the footprint. Unlike a full thickness tear, where the tendon is elevated off of the footprint, a partial tear, particularly articular-sided, will not have an easily appreciable injury upon first inspection. Proper identification of the tear requires correlation with the MRI. One can also palpate the tendon and feel for an area of reduced thickness compared to the adjacent areas.
When addressing a partial thickness tear, both endoscopic and open techniques may be utilized, and various implants have been used successfully. Endoscopically, these tears are most commonly approached with a longitudinal split in the gluteus medius tendon and side to side repair with one or more anchors in the decorticated greater trochanter [12, 30, 42]. Historically, fixation techniques utilized loaded suture anchors secured with knot tying as described by Hartigan et al. in 2018 [43]. In their report of 25 patients with partial thickness undersurface tears of the abductor tendon treated with endoscopic HAT repair with knotted suture anchors, the group reported strong patient-reported outcomes (PROs) and no revisions or complications [43].
Knotless techniques have also been used successfully and confer several potential advantages. These include decreased surgical time and possible avoiding irritation of the overlying IT band from knot abrasion. Kirby et al. utilized a transtendinous approach in a cohort including partial and full thickness tears of the gluteus medius with a knotless construct. They demonstrated good PROs, with postoperative NAHS of 78.1 and mHHS of 75.8, where 90% of patients met the MCID and 0 complications [30].
A recent innovation made to help avoid the challenges of knot tying and suture shuttling, and even obviate the need for a transtendinous incision entirely, is the tendon compression bridge technique [44]. In the transtendinous technique, a longitudinal incision is made in the tendon, the torn fibers are debrided and lateral facet of the greater trochanter decorticated with a burr, and suture anchors placed. In the tendon compression technique, marrow stimulation with a microdrill or chondral pick is utilized rather than decortication with a burr, and the anchors are placed directly through the tendon in small stab incisions under fluoroscopy. The repair sutures are shuttled through the contralateral anchor to form a horizontal mattress configuration and compressed over the lateral facet. Prabhavalkar et al. report on a cohort of 48 patients undergoing this technique with similar rates of achieving the MCID and PASS for mHHS as well as patient satisfaction compared to a matched cohort undergoing endoscopic transtendinous fixation [45]. Of note, only tears involving less than 50% of the tendon were considered candidates for this technique while higher grade tears were addressed in a transtendinous fashion.
Open approaches to partial tendon tears are also commonly utilized. In a cohort of 9 patients with partial tendon tears, Day et al. utilized an open approach with bioinductive bovine collagen patch augmentation with MRI evidence of healing in 7 out of 9 patients at 6 months and improvements in mHHS, HOS-ADL, and iHOT that surpassed the MCID [46•]. Balazs et al. demonstrate good outcomes for open abductor repairs of both partial and full thickness tears utilizing single or double row techniques [47•]. Table 1 summarizes the most up to date systematic reviews regarding surgical outcomes for partial tendon tears and other surgical techniques described below.
Table 1.
Contemporary systematic reviews regarding surgical management of gluteal tendon tears
| Author | Variable of interest | Number of studies (Number of hips) |
Mean follow-up (mo) | Approach | Postoperative patient-reported outcomes | Retears (n, %) | Conclusions |
|---|---|---|---|---|---|---|---|
| Parker et al. (2020) | IT band sparing versus splitting techniques |
8 (174) Spare: 2 (141) Split: 3 (33) Both: 3 |
Spare: 29.72 ± 5.08 months Split: 28.33 ± 4.88 p = .16 |
Endoscopic |
VAS* Spare: 2.09 ± 0.28 Split: 2.97 ± 0.37 p < 0.01 mHHS* Spare: 81.49 ± 4.75 Split: 80.87 ± 2.94 p = 0.25 |
Spare: 4.75% Split: 3.67%* p = 0.04 |
Patients in ITB-sparing approach were significantly younger and more female. There is a lack of high-quality literature regarding ITB approach. |
| Longstaffe et al. (2021) | Endoscopic versus open gluteal repair techniques | 22 (611) | 27.3 | Open and endoscopic |
mHHS Open: 88 Endoscopic: 78.8 Gait deviation: 54% preoperative of which 70% resolved after repair |
Open: 4.1% Endoscopic: 3.4% |
77.9% of tears were partial thickness while 22.1% were full thickness. 53.3% were isolated involvement of the gluteus medius and 46.0% involved both medius and minimus. Both endoscopic and open approaches to gluteal tendon repair demonstrate improvement in patient-reported outcomes with low retear rate. |
| Ebert et al. (2022) | Post operative rehabilitation protocols | 17 (856) | N/A | Open and endoscopic | N/A | N/A |
Variation in postoperative rehabilitation protocols including weight-bearing restrictions, range of motion, and resistance exercises are reported. An evidence-based seven phase rehabilitation protocol is described. |
| Looney et al. (2022) | Fatty infiltration (FI) on repair outcomes | 4 (206) | 31.7-55.2 | Open and endoscopic |
mHHS*: High-grade FI showed less improvement than low or no FI p = .002 VAS score: No difference by FI p > .05 |
3.8% |
High-grade FI results in less improvement in mHHS though no difference in VAS scores after gluteal tendon repair. There was no difference between open and endoscopic repairs in FI-adjusted improvement, though open repair resulted in greater pain relief at each FI level. |
| Yee et al. (2023) | Intraoperative findings during endoscopic treatment of GTPS | 16 (743) | 5-109 | Endoscopic |
VAS: 10/12 studies report decrease mHHS: 11/13 report improvement NAHS: 8/9 report improvement 94% gluteal tendon tears (72% partial thickness, 20% full thickness) 4 studies reported findings of hip arthroscopy: 85% labral tears, 25% chondral lesions |
2–16% | Patients undergoing endoscopy for GTPS most commonly have partial thickness gluteus medius tendon tears. When concomitant hip arthroscopy is performed, labral tears and chondral lesions are often identified intraoperatively. |
| Song et al. (2023) | Outcomes after gluteus maximus transfer | 10 (125) | 40 | Open and endoscopic |
VAS: 3.1 ± 1.5 mHHS: 77.3 ± 18.5 Gait deviation: 85% preoperative of which 66% resolved after repair |
2.4% | Gluteus maximus transfer for irreparable gluteal tendon tears improves patient-reported outcomes with low retear rates. However, persistent Trendelenburg gait is noted in 33% of patients postoperatively. |
| Akhtar et al. (2024) | Outcomes after endoscopic tendon repair | 13 (272) | 16.4–46.7 | Endoscopic |
Trendelenburg gait persisted 0–13.6% MCID achievement in 50–93.3% PASS achievement in 40.7–75.0% |
0–33.3% | Endoscopic repairs have good-excellent patient-reported outcomes and low retear rates, though rates of MCID and PASS achievement are more variable. |
Partial Tears vs Full Thickness
Most literature across a heterogenous variety of approaches and fixation techniques has found no difference in outcomes between patients with partial and full thickness tears [30, 48–50]. In a study aimed at elucidating differences between full and partial thickness tears, Thaunat et al. reported greater improvement in mHHS in patients with partial tears, though no difference in NAHS was found [51•]. In a recent study reporting 5–10-year outcomes of 33 full thickness and 32 partial thickness tears repaired endoscopically, 92.2% of all patients achieved MCID with no difference in achievement between the full and partial thickness groups [52•].
Similarly, investigations of open tendon repair have similarly reported no difference in outcomes between partial and full thickness injuries [53]. In a cohort including 31% undergoing both arthroplasty and tendon repair, full thickness tears had higher VAS pain scores; however, no other outcome measures reached statistical significance between partial and full subgroups [54].
Importantly, across and within studies, partial tears are not treated in the same fashion as full thickness tears. Generally, low-grade tears may be treated with side to side, single row fixation while full thickness tears are more often treated with double row constructs. However, some high-grade partial tears may be completed intraoperatively for mobilization and double row fixation, and some full thickness tears deemed irreparable may not be represented in these repair cohorts as they are instead indicated for tendon transfer. Furthermore, despite attempts to classify partial thickness tears, studies heterogeneously report partial tears by size or reparability based on surgeon assessment, and multiple grading classifications have been described [51•, 55••, 56, 57]. Thus with repair constructs ultimately left to surgeon discretion, evidence-based guidelines for fixation construct by tear size remain undetermined.
Open Versus Endoscopic Approaches
Both open and endoscopic approaches have been successfully utilized for repair of gluteus medius tears [58–65, 66•] (Supplemental File 1). Open treatment of the hip abductor complex may utilize a direct lateral or posterolateral approach, while endoscopic treatment has risen in popularity since its initial description by Voos et al. in 2009 [1••, 47•, 48, 56].
Purported advantages of the open approach include greater visualization, easier tendon mobilization, and wider exposure for more thorough assessment of involved tendons and superior fixation. Importantly, it is more technically familiar to most orthopedic surgeons, as the approach is relatively simple, and similar to those used for most open hip procedures (like THA). Conversely, the endoscopic approach is unfamiliar for most surgeons, as this is not a frequently accessed endoscopic area. However, endoscopy affords less soft tissue violation and a much smaller wound, and early reports suggested there may be lower complication rates for experienced surgeon [67]. A 2021 systematic review of 22 studies with 611 hips evaluating outcomes between open and endoscopic approaches and indeed supported that while both resulted in improved patient-reported outcomes and similar retear rate (3.4% endoscopic vs 4.1% open), endoscopic repair demonstrated a decreased complication rate of 0.7% compared to 7.8% in open cases [1••]. However, open repair had a higher rate of resolution of Trendelenburg sign or gait with 76.1% resolution compared to 57.5% in endoscopic. Within endoscopic techniques, there is limited evidence to demonstrate superiority of IT band splitting versus sparing approaches [68].
Of note, in the years following these early reviews supporting endoscopic over open techniques, several recent works have reported notably higher retear rates in endoscopically treated cohorts. In a cohort of partial and/or full thickness tears treated endoscopically, Rice et al. reported a 10.9% retear or revision rate in 46 patients [38•]; Bitar et al. reported a 6% retear rate in 16 patients [69]; Thaunat et al. an 8% retear rate in 46 patients [12]; and Kocaoglu et al. a 26% retear rate in 50 patients [70]. Furthermore, complication rates vary widely by series and by definition; for example, while they reported no “major” complications, Della Rocca et al. report an 18.2% rate of minor complications in their endoscopically treated cohort, including postoperative hematoma and conservatively managed superficial wound dehiscence [71]. In a 2024 systematic review of 13 studies with 272 patients undergoing endoscopic hip abductor tendon repairs, a majority of studies reported 0% rates of retear, revision, and complication; however, some studies reported rates as high as 33.3%, 13.0%, and 18.2%, respectively [72••]. Three studies reported on Trendelenburg gait, which persisted in 0–13.5% of patients postoperatively [30, 71, 73]. Furthermore, while eight of nine studies reported improvements in PROs, the rates of achieving MCID and PASS ranged from 50.0 to 93.3%, representing a significant number of patients with suboptimal outcomes [72••].
These PRO findings are consistent with studies that included pooled cohorts of both endoscopic and open cases. In 84 patients treated via open or endoscopic methods, Meghpara et al. report the MCID was achieved for mHHS, NAHS, and HOS-SSS by 79.3%, 86.4%, and 70.2% of patients, respectively [42]. Similarly, in a 2023 report of 142 patients with open or endoscopically treated gluteus tendon tears, Allahabadi et al. report an overall success rate defined by revision-free survival and achievement of MCID/PASS, of 79% [55••]. In their cohort, there was no difference in outcomes between open and endoscopic approach on multivariate analysis. Factors that were independent predictors of clinical failure included preoperative smoking, lower back pain, presence of a limp or Trendelenburg gait, history of psychiatric diagnosis, and increased MRI classification grades. Thus, understanding risk factors for failure is crucial for preoperative planning and patient counseling.
One of the most commonly identified risk factors for failure is the degree of fatty infiltration. A 2022 investigation including both open and endoscopic repairs demonstrated association between fatty degeneration and worse patient-reported outcomes [74•], a finding that has been previously reported in both open only and endoscopic only cohorts [30, 75]. In a systematic review of four studies and 206 repairs both open and endoscopic, high-grade fatty infiltration was associated with significantly less improvement in mHHS compared to low or no fatty infiltration [76•]. While overall no difference was observed between open and endoscopic repair, the authors did note their analysis suggested patients with more severe fatty infiltration may benefit more from open repair where those without infiltration may benefit more from endoscopic treatment, which may inform the surgeon’s choice of approach.
Both endoscopic and open gluteus repairs provide good outcomes with low retear and revision rates, though a notable subset of patients will have persistent gait abnormality and may not return to their previous level of activity [1••, 42, 77•]. The literature does not clearly support superiority of open or endoscopic approach at this time. In their 2021 report, Uppstrom et al. comment that “in discussion with other hip preservation surgeons, we have observed a trend back towards the adoption of open abductor repair” [77•]. As endoscopic techniques have become more widely adopted, it may be that our attention should focus not on approach but instead other factors including those related to patient, fixation, and augmentation.
Repair Fixation Configurations
Fixation options for gluteus repair include single and double row constructs as well as, in open approaches, transosseous fixation. Based off of evidence from rotator cuff repair literature demonstrating lower retear rates using double row constructs, interest has grown in applying the same rationale to the abductor tendon complex [78]. From a biomechanical perspective, a cadaveric study, double row repair demonstrated greater footprint coverage of the lateral facet and higher mean yield load compared to single row repair, though this did not reach statistical significance [79].
Limited clinical evidence exists supporting one fixation configuration over another. Part of the challenge in delineating superiority is the differences in use between single and double row fixation. Many authors report using a single row for partial tendon tears and double row for high-grade partial or full thickness tears, preventing an apples-to-apples comparison [12, 38•, 42, 51•, 55••]. Kocaoglu et al. compared 50 patients treated endoscopically with single row, double row, and single row techniques with microfracture [70]. They reported the greatest improvement in PROMs in the single row with microfracture compared to either isolated single or double row cohorts. Regarding retear rates, they reported 31.3% in the double row cohort, 35.7% in the single row cohort, and 15.0% in the single row with microfracture cohort; while these findings suggest no difference between single and double row, these retear rates are notably higher than other modern reports. Additionally, the improvement with microfracture highlights the role of biologic factors and augmentation in repair.
Considering PROs, Derksen et al. reported a series of 43 patients after open, single row fixation [80]. While patients improved in VAS and PROs from pre to postoperatively, only 58.1% of their cohort were free of Trendelenburg gait. Additionally, mHHS and WOMAC scores were notably lower than other similar studies in the literature. While comparison across studies is difficult, the authors suggest their single row construct may have contributed to their relatively poor outcome. While using any suture anchor construct, surgeons should be aware that decortication, particularly in osteoporotic patients, decreases suture pullout strength [81].
An alternative to suture anchor fixation is transosseous tunnel fixation [75, 82]. Transosseous tunnels require open approaches and have been classically utilized in the setting of hip arthroplasty. In a cohort of 45 hips, 6 of whom had prior ipsilateral THA, Harper et al. report improvements in pain, gait, and muscle strength using tenodesis for partial minimus or medius tears and bone tunnel fixation for those involving the gluteus medius insertion [56]. Another report of 25 gluteal tendons repaired with transosseous suture fixation specifically investigated gait, reporting similar biomechanical gait characteristics compared to a healthy cohort [83]. No studies have specifically compared suture anchor to transosseous tunnel fixation in gluteal repairs. In the authors’ experience, suture anchors are easier to use than tunnels and can be utilized in both endoscopic and open cases, making them the fixation method of choice for the senior author. Additionally, while gluteus-specific clinical evidence is sparse, the authors’ preference is for double row fixation for high-grade partial or full thickness tears to maximize footprint coverage.
Augmentation Options
Numerous augmentation options have been described to supplement the fixation of gluteus repairs, informed by experience with such techniques in rotator cuff repair [84–89]. Described augmentation options include synthetics, xenografts, and allografts. Theoretically, autograft could also play a role, though no recent reports have been described.
Synthetic options primarily function by providing increased time-zero fixation strength. Initially developed for cruciate ligament reconstruction, the LARS ligament has been described with success by Ebert et al. [6, 90•, 91]. Ebert’s group utilizes a direct lateral approach, passing the LARS ligament through the deep surface of the abductor tendon through bone tunnels in the greater trochanter, affixed with an interference screw. In a long-term outcome study of 90 patients with at least 7–10-year follow-up, they found significant improvement in PROMs, 93% patient satisfaction, and an 8.2% failure rate [90•]. Requicha et al. report utilizing LARS in cases with significant degeneration or retraction; however, they do not report how frequently this was the case in their series, nor any LARS-specific outcomes [54]. The use of synthetic Mersilene mesh has also been reported. Maslaris et al. utilized mesh in a single patient with advanced fatty degeneration in their 38 patient series; however, they do not further characterize their technique or mesh-specific outcomes [74•].
Once limited by inflammatory responses, xenografts have become a viable option in tendon repair augmentation with improved preparation to serve as acellular extracellular scaffolds. Such bovine collagen patches offer no additional time-zero strength, but instead function as a scaffold to facilitate collagen migration and ultimately improve tissue quality. Both open and endoscopic techniques using these patches have been reported [92, 93]. In a study of open repair with bovine collagen patch augmentation, Day et al. describe an open, double row fixation technique after which point the patch was sutured over the repaired tendon. At 6 months postoperatively, they report no complications with 7/9 tendons healed on MRI and improvements in HOS-ADL, mHHS, and iHOT that met the MCID [46•].
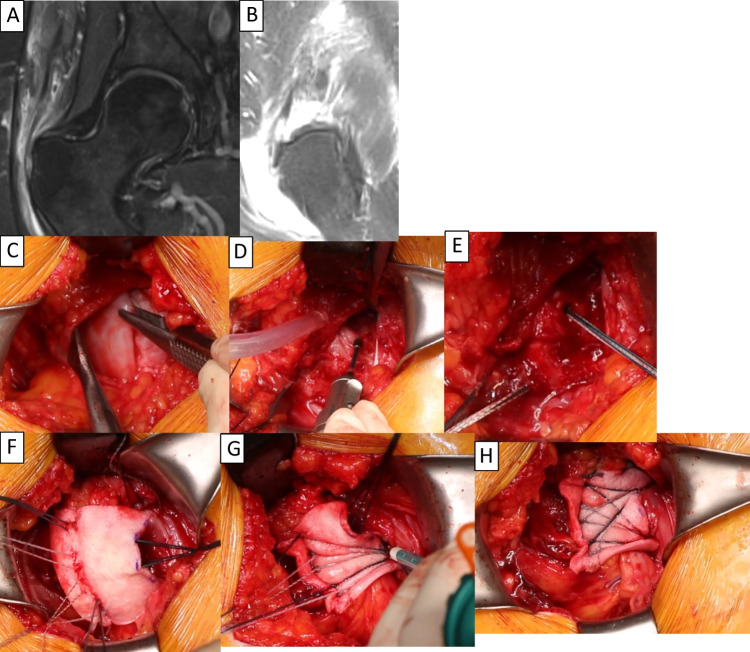
Allograft options include Achilles tendon grafts as well as acellular dermal grafts (Fig. 2). These function both to improve initial mechanical strength as well as improve the biologic environment for tendon to bone healing. Suppauksorn et al. describe an open, double row technique for tears with severe tendon loss using either acellular allograft or Achilles tendon allograft to fill in defects between the tendon and anchors [94]. Capurro et al. and Pascual-Garrido et al. describe similar open double row repair techniques with acellular dermal allograft [93, 95]. Additionally, Allahabadi et al. note in their surgical technique acellular human dermal allograft was used in cases of retraction or insufficient tissue quality, but do not further expound on technique or outcomes [55••]. In the same series in which they used Mersilene mesh in one case, Maslaris et al. utilized Achilles allograft in one case though they again do not detail their technique or outcomes for that case [74•].
Fig. 2.
Case demonstration of full thickness retracted gluteal tendon tear treated surgically with dermal allograft augmentation. A/B Coronal and sagittal MRI demonstrate full thickness gluteal tendon tear with tissue defect. C Tear in forceps. D Decortication of the greater trochanter. E Proximal row anchors. F Allograft on top of tear, with sutures passed through tendon and graft. G Suture limbs placed into first distal row anchor. H Completed double-row repair with allograft augmentation
Unfortunately, while these varied augmentation techniques have been described and are technically feasible, clinical outcome studies remain extremely limited. Theoretically, augmentation with synthetics, xenograft, or allograft may be of particular use in cases with severe degeneration or poor tissue quality, retraction, or revision procedures. However, further high-quality studies are needed to understand optimal indications, augmentation choice, and clinical outcomes.
Due to the limited studies to draw conclusions from, indications for the use of various augmentation products are ill-defined. In general, it is the senior author’s preference to consider bioinductive xenograft implants in partial tears where there is sufficient tendon coverage of the footprint, but the quality of the tissue is poor. Acellular dermal allografts are considered in full thickness tears, particularly where there is a tissue defect that the native tendon cannot bridge without undue tension. The decision to use a graft can be informed by preoperative patient and imaging characteristics, such as chronicity of the tear, amount of tendon retraction, tear width, and fatty infiltration; however, ultimately, the decision is typically based on intraoperative assessment after tendon debridement and mobilization.
Tendon Transfers
In cases of failed gluteus medius repair or those tears where the amount of retraction or fatty degeneration renders the tear irreparable, partial transfer of the gluteus maximus tendon may be considered (Supplemental File 2). Initially described by Whiteside in 2013 for the treatment of abductor deficiency in hip arthroplasty patients, tendon transfer techniques have subsequently been successfully applied to the native hip [26, 96]. Isolated gluteus maximus transfers and those with partial tensor fascia lata transfer have been described, as well as alongside partial gluteus medius repair when possible [97•, 98–103].
Generally, these transfers are accomplished through an open lateral incision and a longitudinal split through the IT band. The gluteus maximus, and medius/minimus if present, is identified, and the greater trochanter footprint is prepared. Either a portion of the glut max tendon in isolation or in combination with a portion of the TFL is transferred to the greater trochanter and fixed with suture anchors or transosseous drill holes. To ensure adequate tension, the transfer should be affixed in maximal abduction.
A 2023 systematic review of 10 studies, which included 125 hips that underwent either isolated gluteus medius transfer, or in combination with TFL transfer, demonstrated improved PROs at follow-up [104••]. The pooled results demonstrate an increase in mHHS by 30.1 (95% confidence interval: +15.5 to +46.5) and decrease in VAS by 4.1 (95% confidence interval: −7.1 to −1.0) [104••]. However, patients did not have significant improvement in abduction strength postoperatively and a third had persistent Trendelenburg gait. Additionally, there was a 5.6% complication and 2.4% retear rate. One three patient series from Jimenez-Tellaria et al., which supplemented their gluteus maximus transfer with synthetic mesh, improved limp and eliminated Trendelenburg sign in all three patients, though interpretation of these good results is limited given the extremely small series [105].
Since that review, a recent 8 patient series by Kaiser et al. echoed those results, with significant reduction in pain, but no increase in strength, with all patients demonstrating Trendelenburg sign postoperatively [100]. A more optimistic report of 22 hips from Lemme et al. showed, along with improvements in mHHS, VAS, and HOS-ADL, an improvement in hip abduction strength from 2.3 to 3.9/5, though this does reflect persistent weakness [101].
The vast majority of tendon transfers are performed in an open fashion, with limited endoscopic series reporting more concerning results. In a six patient series, Bauwens et al. report only three of six patients achieved satisfactory outcomes; of the failures, one required revision open surgery at 4 months and two had no improvement in pain or limp [97•]. Portet et al. reported on a series of 15 patients undergoing transfer [106]. The first six were performed endoscopically; however, after the report by Bauwen, the authors transitioned to an open approach. In their series, NAHS, mHHS, iHOT-12, VAS, and hip abduction strength improved postoperatively; however, 79% of patients had some persistent strength deficit and 57% had Trendelenburg sign. In this small series, they did not identify a difference between open and endoscopic cohorts [106].
While open tendon transfer remains a salvage option for the irreparable or revision gluteus medius repair, persistent postoperative strength and gait deficits are common. Early endoscopic reports are discouraging.
Postoperative Rehabilitation
Postoperative rehabilitation protocols vary in specifics; however, published plans follow the same principles and general timelines, regardless of repair technique or tendon transfer. In general, patients are non-weight-bearing or partial weight-bearing for 6 to 8 weeks. Range of motion is limited in the initial 3–6 weeks postoperatively, particularly flexion, adduction, and internal or external rotation. This may be accomplished with patient education, hip bracing, or casting.
As weight-bearing is advanced, so is activity and motion, with active abduction strengthening around 3 months and advancement to sport-specific activities around 6 months. Ebert et al. provide a comprehensive literature review of rehabilitation protocols and provide a seven phase protocol [107•]. Consideration may be made for more rapid or cautious activity advancement based on the surgeon’s intraoperative evaluation of repair quality and augmentation. Additionally, alterations may be required in cases of concomitant hip arthroscopy.
Conclusions
Gluteus medius tears, or hip abductor tendon tears, are an increasingly recognized source of lateral hip pain that may benefit from surgical management. Following a wave of interest in endoscopic repair approaches, more recent evidence suggests neither endoscopic nor open approach is superior and the choice should be based upon surgeon expertise. Generally, partial tendon tears are treated with side to side or single row repairs, while larger or full thickness tears may be addressed with double row constructs. Literature is lacking to confirm these trends result in superior patient-reported outcomes.
In spite of fixation variability, outcomes are similar between partial and full thickness tears. While patients undergoing gluteus repair experience improvements pre to postoperatively and good PROs, a proportion may not achieve the MCID. It is difficult to demonstrate variability in outcomes based upon surgical technique, with more evidence available to support variation in outcomes based upon patient factors such as fatty atrophy.
Full thickness tears with extensive retraction or atrophy are challenging to address. Augmentation and reconstruction strategies with synthetics, xenografts, and allografts have been described; however, minimal clinical outcomes demonstrate their clinical effect. Gluteus maximus tendon transfer offers a salvage option for failed repairs or those tears thought to be irreparable. Tendon transfers offer improvements in patient-reported outcomes, though less consistent improvements in abductor strength or Trendelenburg gait. Evidence in the surgical management of hip abductor tears has boomed in the past decade, and as larger series across longer term follow-up are reported, further refinement in techniques and recommendations may be made to provide to best outcomes for patients with gluteal tendon tears.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
A.M, M.M, K.D, A.B, J.B, T.Y, D.K wrote the main manuscript text and A.M, K.D and D.K prepared the figures and tables. All authors reviewed the manuscript.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of Interest
Allison Morgan, Michael Moore, Kendall Derry, Andrew Bi, and Daniel Kaplan declare that they have no conflicts of interest. Thomas Youm has received royalties and speaking fees from Arthrex, Inc.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Competing interests
Thomas Youm-Arthrex Inc.-Consulting Fees.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Longstaffe R, Dickerson P, Thigpen CA, Shanley E, Kissenberth MJ, Folk J, et al. Both open and endoscopic gluteal tendon repairs lead to functional improvement with similar failure rates: a systematic review. J ISAKOS Jt Disord Orthop Sports Med. 2021;6(1):28–34. doi: 10.1136/jisakos-2020-000474. [DOI] [PubMed] [Google Scholar]
- 2.Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Med Auckl NZ. 2015;45(8):1107–19. doi: 10.1007/s40279-015-0336-5. [DOI] [PubMed] [Google Scholar]
- 3.Ladurner A, Fitzpatrick J, O’Donnell JM. Treatment of gluteal tendinopathy: a systematic review and stage-adjusted treatment recommendation. Orthop J Sports Med. 2021;9(7):23259671211016850. doi: 10.1177/23259671211016850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strauss EJ, Nho SJ, Kelly BT. Greater trochanteric pain syndrome. Sports Med Arthrosc Rev. 2010;18(2):113–9. doi: 10.1097/JSA.0b013e3181e0b2ff. [DOI] [PubMed] [Google Scholar]
- 5.Bunker TD, Esler CN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997;79(4):618–20. doi: 10.1302/0301-620X.79B4.0790618. [DOI] [PubMed] [Google Scholar]
- 6.Ebert JR, Bucher TA, Ball SV, Janes GC. A review of surgical repair methods and patient outcomes for gluteal tendon tears. Hip Int J Clin Exp Res Hip Pathol Ther. 2015;25(1):15–23. doi: 10.5301/hipint.5000183. [DOI] [PubMed] [Google Scholar]
- 7.Dove JH, Lemme NJ, Modest JM, Talley-Bruns RC, Tabaddor RR, Fadale PD. A review of abductor tendon tears: the hidden lesion of the hip. JBJS Rev. 2022 Dec 1;10(12). [DOI] [PubMed]
- 8.Lachiewicz PF. Abductor tendon tears of the hip: evaluation and management. J Am Acad Orthop Surg. 2011;19(7):385–91. doi: 10.5435/00124635-201107000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Stanton MC, Maloney MD, Dehaven KE, Giordano BD. Acute traumatic tear of gluteus medius and minimus tendons in a patient without antecedant peritrochanteric hip pain. Geriatr Orthop Surg Rehabil. 2012;3(2):84–8. doi: 10.1177/2151458512441795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisher DA, Almand JD, Watts MR. Operative repair of bilateral spontaneous gluteus medius and minimus tendon ruptures. A case report. J Bone Joint Surg Am. 2007;89(5):1103–7. doi: 10.2106/00004623-200705000-00026. [DOI] [PubMed] [Google Scholar]
- 11.Godshaw B, Wong M, Ojard C, Williams G, Suri M, Jones D. Acute traumatic tear of the gluteus medius and gluteus minimus in a marathon runner. Ochsner J. 2019;19(4):405–9. doi: 10.31486/toj.18.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thaunat M, Pacoret V, Saad M, Saint-Etienne A, Morvan A. Francophone Arthroscopy Society (SFA). Endoscopic treatment of gluteus medius tendon tear. Orthop Traumatol Surg Res OTSR. 2022;108(8S):103393. doi: 10.1016/j.otsr.2022.103393. [DOI] [PubMed] [Google Scholar]
- 13.Lall AC, Schwarzman GR, Battaglia MR, Chen SL, Maldonado DR, Domb BG. Greater trochanteric pain syndrome: an intraoperative endoscopic classification system with pearls to surgical techniques and rehabilitation protocols. Arthrosc Tech. 2019;8(8):e889–903. doi: 10.1016/j.eats.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flack NAMS, Nicholson HD, Woodley SJ. The anatomy of the hip abductor muscles. Clin Anat N Y N. 2014;27(2):241–53. doi: 10.1002/ca.22248. [DOI] [PubMed] [Google Scholar]
- 15.Flack NAMS, Nicholson HD, Woodley SJ. A review of the anatomy of the hip abductor muscles, gluteus medius, gluteus minimus, and tensor fascia lata. Clin Anat. 2012;25(6):697–708. doi: 10.1002/ca.22004. [DOI] [PubMed] [Google Scholar]
- 16.LaPorte C, Vasaris M, Gossett L, Boykin R, Menge T. Gluteus medius tears of the hip: a comprehensive approach. Phys Sportsmed. 2019;47(1):15–20. doi: 10.1080/00913847.2018.1527172. [DOI] [PubMed] [Google Scholar]
- 17.Tsutsumi M, Nimura A, Akita K. The gluteus medius tendon and its insertion sites: an anatomical study with possible implications for gluteus medius tears. J Bone Joint Surg Am. 2019;101(2):177–84. doi: 10.2106/JBJS.18.00602. [DOI] [PubMed] [Google Scholar]
- 18.White LM, Oar DA, Naraghi AM, Griffin A, Safir OA. Gluteus minimus tendon: MR imaging features and patterns of tendon tearing. Skeletal Radiol. 2021;50(10):2013–21. doi: 10.1007/s00256-021-03745-4. [DOI] [PubMed] [Google Scholar]
- 19.Beck M, Sledge JB, Gautier E, Dora CF, Ganz R. The anatomy and function of the gluteus minimus muscle. J Bone Joint Surg Br. 2000;82-B(3):358–63. doi: 10.1302/0301-620X.82B3.0820358. [DOI] [PubMed] [Google Scholar]
- 20.Stevens WR, Jo CH, Tulchin-Francis K. Clinically derived biomechanical criteria for the Trendelenburg test. Clin Biomech Bristol Avon. 2020;78:105066. doi: 10.1016/j.clinbiomech.2020.105066. [DOI] [PubMed] [Google Scholar]
- 21.Bailey R, Selfe J, Richards J. The role of the Trendelenburg Test in the examination of gait. Phys Ther Rev. 2009;14(3):190–7. doi: 10.1179/174328809X452836. [DOI] [Google Scholar]
- 22.Carayannopoulos NL, S O, M P. The proximal origin of the gluteus maximus: a cadaveric study. J Clin Exp Orthop [Internet]. 2017 [cited 2024 Jan 31];03(01). Available from: http://orthopedics.imedpub.com/the-proximal-origin-of-the-gluteus-maximus-a-cadaveric-study.php?aid=18571
- 23.Serra F, Aboudib JH, Cedrola JPV, de Castro CC. Gluteoplasty: anatomic basis and technique. Aesthet Surg J. 2010;30(4):579–92. doi: 10.1177/1090820X10380389. [DOI] [PubMed] [Google Scholar]
- 24.Neto WK, Soares EG, Vieira TL, Aguiar R, Chola TA, de Sampaio VL, et al. Gluteus maximus activation during common strength and hypertrophy exercises: a systematic review. J Sports Sci Med. 2020;19(1):195–203. [PMC free article] [PubMed] [Google Scholar]
- 25.Muyor JM, Martín-Fuentes I, Rodríguez-Ridao D, Antequera-Vique JA. Electromyographic activity in the gluteus medius, gluteus maximus, biceps femoris, vastus lateralis, vastus medialis and rectus femoris during the Monopodal Squat, Forward Lunge and Lateral Step-Up exercises. PloS One. 2020;15(4):e0230841. doi: 10.1371/journal.pone.0230841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whiteside LA. Surgical technique: Transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop. 2012;470(2):503–10. doi: 10.1007/s11999-011-1975-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmadzadeh R, Bergeron L, Tang M, Morris SF. The superior and inferior gluteal artery perforator flaps. Plast Reconstr Surg. 2007;120(6):1551. doi: 10.1097/01.prs.0000282098.61498.ee. [DOI] [PubMed] [Google Scholar]
- 28.Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. J Anat. 2006;208(3):309–16. doi: 10.1111/j.1469-7580.2006.00531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meghpara MB, Bheem R, Haden M, Rosinsky PJ, Shapira J, Maldonado DR, et al. Differences in clinical presentations and surgical outcomes of gluteus medius tears between men and women. Am J Sports Med. 2020;48(14):3594–602. doi: 10.1177/0363546520966335. [DOI] [PubMed] [Google Scholar]
- 30.Kirby D, Fried JW, Bloom DA, Buchalter D, Youm T. Clinical outcomes after endoscopic repair of gluteus medius tendon tear using a knotless technique with a 2-year minimum follow-up. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2020;36(11):2849–55. doi: 10.1016/j.arthro.2020.07.022. [DOI] [PubMed] [Google Scholar]
- 31.Torres A, Fernández-Fairen M, Sueiro-Fernández J. Greater trochanteric pain syndrome and gluteus medius and minimus tendinosis: nonsurgical treatment. Pain Manag. 2018;8(1):45–55. doi: 10.2217/pmt-2017-0033. [DOI] [PubMed] [Google Scholar]
- 32.Harris-Love MO, Seamon BA, Gonzales TI, Hernandez HJ, Pennington D, Hoover BM. Eccentric exercise program design: a periodization model for rehabilitation applications. Front Physiol. 2017;8:112. doi: 10.3389/fphys.2017.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bessette MC, Olsen JR, Mann TR, Giordano BD. Intra-articular hip injections for lateral hip pain. J Hip Preserv Surg. 2014;1(2):71–6. doi: 10.1093/jhps/hnu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fitzpatrick J, Bulsara MK, O’Donnell J, Zheng MH. Leucocyte-rich platelet-rich plasma treatment of gluteus medius and minimus tendinopathy: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2019;47(5):1130–7. doi: 10.1177/0363546519826969. [DOI] [PubMed] [Google Scholar]
- 35.Jacobson JA, Yablon CM, Henning PT, Kazmers IS, Urquhart A, Hallstrom B, et al. Greater trochanteric pain syndrome: percutaneous tendon fenestration versus platelet-rich plasma injection for treatment of gluteal tendinosis. J Ultrasound Med Off J Am Inst Ultrasound Med. 2016;35(11):2413–20. doi: 10.7863/ultra.15.11046. [DOI] [PubMed] [Google Scholar]
- 36.Walsh MJ, Walton JR, Walsh NA. Surgical repair of the gluteal tendons: a report of 72 cases. J Arthroplasty. 2011;26(8):1514–9. doi: 10.1016/j.arth.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 37.Chandrasekaran S, Vemula SP, Gui C, Suarez-Ahedo C, Lodhia P, Domb BG. Clinical features that predict the need for operative intervention in gluteus medius tears. Orthop J Sports Med. 2015;3(2):2325967115571079. doi: 10.1177/2325967115571079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rice MW, Sivasundaram L, Hevesi M, Browning RB, Alter TD, Paul K, et al. Defining the minimal clinically important difference and patient acceptable symptom state after endoscopic gluteus medius or minimus repair with or without labral treatment and routine capsular closure at minimum 5-year follow-up. Am J Sports Med. 2022;50(10):2629–36. doi: 10.1177/03635465221105469. [DOI] [PubMed] [Google Scholar]
- 39.Yee C, Wong M, Cohen D, Kay J, Simunovic N, Duong A, et al. Labral tears and chondral lesions are common comorbidities identified during endoscopic repair of gluteal tendon tears for greater trochanteric pain syndrome: a systematic review. Arthrosc J Arthrosc Relat Surg. 2023;39(3):856–864.e1. doi: 10.1016/j.arthro.2022.06.031. [DOI] [PubMed] [Google Scholar]
- 40.Nho SJ, Grzybowski JS, Bogunovic L, Kuhns BD, Mather RC, Salata MJ, et al. Diagnosis, evaluation, and endoscopic repair of partial articular gluteus tendon avulsion. Arthrosc Tech. 2016;5(3):e425–431. doi: 10.1016/j.eats.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Domb BG, Nasser RM, Botser IB. Partial-thickness tears of the gluteus medius: rationale and technique for trans-tendinous endoscopic repair. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2010;26(12):1697–705. doi: 10.1016/j.arthro.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 42.Meghpara MB, Yelton MJ, Annin S, Rosinsky PJ, Shapira J, Maldonado DR, et al. Return to activity after gluteus medius repair in active patients older than 50 years. Orthop J Sports Med. 2021;9(1):2325967120967968. doi: 10.1177/2325967120967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hartigan DE, Perets I, Ho SW, Walsh JP, Yuen LC, Domb BG. Endoscopic repair of partial-thickness undersurface tears of the abductor tendon: clinical outcomes with minimum 2-year follow-up. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2018;34(4):1193–9. doi: 10.1016/j.arthro.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 44.Hartigan DE, Mansor Y, Perets I, Walsh JP, Mohr MR, Domb BG. Knotless “suture staple” technique for endoscopic partial thickness abductor tendon repair. Arthrosc Tech. 2018;7(10):e975–80. doi: 10.1016/j.eats.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Prabhavalkar ON, Carbone AD, Curley AJ, Padmanabhan S, Nerys J, Domb BG. Endoscopic tendon compression bridge technique for repair of partial-thickness gluteus medius tears with concomitant arthroscopy for labral tears: minimum 2-year outcomes with benchmark control group. Am J Sports Med. 2023;51(14):3764–71. doi: 10.1177/03635465231204314. [DOI] [PubMed] [Google Scholar]
- 46.Day MA, Hancock KJ, Selley RS, Swartwout EL, Dooley M, Shamrock AG, et al. Repair of gluteus medius tears with bioinductive collagen patch augmentation: initial evaluation of safety and imaging. J Hip Preserv Surg. 2022;9(3):185–90. doi: 10.1093/jhps/hnac031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balazs GC, Dooley M, Wang D, O’Sullivan E, Kelly BT. Clinical outcomes of open hip abductor tendon repair with minimum two-year follow-up. Hip Int J Clin Exp Res Hip Pathol Ther. 2022;32(4):516–22. doi: 10.1177/1120700020965487. [DOI] [PubMed] [Google Scholar]
- 48.Voos JE, Shindle MK, Pruett A, Asnis PD, Kelly BT. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med. 2009;37(4):743–7. doi: 10.1177/0363546508328412. [DOI] [PubMed] [Google Scholar]
- 49.Chandrasekaran S, Gui C, Hutchinson MR, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of endoscopic gluteus medius repair: study of thirty-four patients with minimum two-year follow-up. J Bone Joint Surg Am. 2015;97(16):1340–7. doi: 10.2106/JBJS.N.01229. [DOI] [PubMed] [Google Scholar]
- 50.Perets I, Mansor Y, Yuen LC, Chen AW, Chaharbakhshi EO, Domb BG. Endoscopic gluteus medius repair with concomitant arthroscopy for labral tears: a case series with minimum 5-year outcomes. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2017;33(12):2159–67. doi: 10.1016/j.arthro.2017.06.032. [DOI] [PubMed] [Google Scholar]
- 51.Thaunat M, de Saint VB, Caron E, Ingale PS. A comparison of outcomes after endoscopic repair of partial- versus full-thickness tears of the gluteus medius tendon. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2021;37(8):2465–72. doi: 10.1016/j.arthro.2021.02.020. [DOI] [PubMed] [Google Scholar]
- 52.Byrd JWT, Jones KS, Duncan S. Endoscopic hip abductor tendon repair results in successful outcomes with 5- to 10-year follow-up. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2023;S0749–8063(23):00980–5. doi: 10.1016/j.arthro.2023.11.031. [DOI] [PubMed] [Google Scholar]
- 53.Smith T, Matthews M, Weeks KD, Odum SM, Ellison BS. Early sears. J Surg Orthop Adv. 2023;32(2):75–82. [PubMed] [Google Scholar]
- 54.Requicha F, Edwards SM, Rickman MS, Comley AS. Outcomes analysis of anterior and lateral approach for open repair of hip abductor tendons. Hip Int J Clin Exp Res Hip Pathol Ther. 2023;33(5):812–8. doi: 10.1177/11207000221103440. [DOI] [PubMed] [Google Scholar]
- 55.Allahabadi S, Chapman RS, Fenn TW, Browning RB, Nho SJ. The Gluteus-Score-7 predicts the likelihood of both clinical success and failure following surgical repair of the hip gluteus medius and/or minimus. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2023;S0749–8063(23):00393–6. doi: 10.1016/j.arthro.2023.03.035. [DOI] [PubMed] [Google Scholar]
- 56.Harper KD, Park KJ, Rodriguez-Perez MA, Lambert BS, Gilcrease-Garcia B, Sullivan TC, et al. Clinical outcomes for open hip abductor repair using tenodesis and bone trough repair techniques. J Arthroplasty. 2022;37(7S):S444–8. doi: 10.1016/j.arth.2022.01.083. [DOI] [PubMed] [Google Scholar]
- 57.Browning RB, Fenn TW, Allahabadi S, Rice MW, Swindell HW, Ebersole JW, et al. Three-grade magnetic resonance imaging-based gluteus medius and/or minimus tear classification system provides excellent inter-rater reliability. Arthrosc Sports Med Rehabil. 2023;5(3):e773–82. doi: 10.1016/j.asmr.2023.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maslaris A, Vail TP, Zhang AL, Patel R, Jäger M, Bini SA. Equivalent mid-term results of open vs endoscopic gluteal tendon tear repair using suture anchors in forty-five patients. J Arthroplasty. 2020;35(6S):S352–8. doi: 10.1016/j.arth.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 59.Okoroha KR, Beck EC, Nwachukwu BU, Kunze KN, Nho SJ. Defining minimal clinically important difference and patient acceptable symptom state after isolated endoscopic gluteus medius repair. Am J Sports Med. 2019;47(13):3141–7. doi: 10.1177/0363546519877179. [DOI] [PubMed] [Google Scholar]
- 60.Paul KD, Hargreaves M, Manfredi JN, Cooke B, Crawford A, Evely T, et al. Patients with operative gluteus medius tears often present with a concomitant history of lumbar pathology. J Orthop. 2024;47:18–22. doi: 10.1016/j.jor.2023.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barrera M, Bothorel H, Poultsides L, Christofilopoulos P. Short-term outcomes following mini-open repair of chronic gluteus medius tendon tears using a double-row technique. J Hip Preserv Surg. 2021;8(2):202–8. doi: 10.1093/jhps/hnab060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Navas L, Zimmerer A, Hausschild M. Recreational activity after open hip abductor repair. Arch Orthop Trauma Surg. 2023;143(8):5143–8. doi: 10.1007/s00402-022-04734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zimmerer A, Navas L, Pfeil D, Hauschild M. Open hip abductor repair hitting the sack-abductor tendon repair significantly improves sleep quality. J Clin Med. 2021;10(21):5164. doi: 10.3390/jcm10215164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ratnayake RP, Shelton TJ, Wang J, Giordani M. Hip abductor repair improves patient outcome, function, and satisfaction in patients without and with total hip arthroplasty. J Orthop. 2020;17:59–62. doi: 10.1016/j.jor.2019.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.DeFroda S, Silverman A, Quinn M, Tabaddor R. Mini-open double row gluteus medius repair provides good short-term functional outcomes. J Hip Preserv Surg. 2019;hnz038.
- 66.Browning RB, Clapp IM, Alter TD, Nwachukwu BU, Wolfson T, Suppauksorn S, et al. Superior gluteal reconstruction results in promising outcomes for massive abductor tendon tears. Arthrosc Sports Med Rehabil. 2021;3(5):e1321–7. doi: 10.1016/j.asmr.2021.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chandrasekaran S, Lodhia P, Gui C, Vemula SP, Martin TJ, Domb BG. Outcomes of open versus endoscopic repair of abductor muscle tears of the hip: a systematic review. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2015;31(10):2057–2067.e2. doi: 10.1016/j.arthro.2015.03.042. [DOI] [PubMed] [Google Scholar]
- 68.Parker EA, Meyer AM, Laskovski JR, Westermann RW. Endoscopic gluteus medius repair with an itb-sparing versus itb-splitting approach: a systematic review and meta-analysis. Orthop J Sports Med. 2020;8(5):2325967120922196. doi: 10.1177/2325967120922196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bitar AC, Guimarães JB, Marques R, de Castro Trindade CA, Filho AGO, Nico MAC, et al. Clinical and radiological results after endoscopic treatment for gluteal tendon injuries with a minimum follow-up of 12 months. Arch Bone Jt Surg. 2023;11(10):641–8. doi: 10.22038/ABJS.2023.70495.3304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kocaoglu B, Paksoy AE, Cerciello S, Ollivier M, Seil R, Safran M. Arthroscopic repair of the hip abductor musculotendinous unit: the effect of microfracture on clinical outcomes. Am J Sports Med. 2021;49(6):1570–7. doi: 10.1177/0363546521999678. [DOI] [PubMed] [Google Scholar]
- 71.Della Rocca F, Di Francia V, Giuffrida A, Rosolani M, D’Ambrosi R, D’Addona A. Satisfactory results after endoscopic gluteus medius repair combined with selective gluteus maximus reflected tendon release for the treatment of a full-thickness tear of gluteus medius. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2023;31(5):2038–45. doi: 10.1007/s00167-022-07140-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.•• Akhtar M, Razick D, Aamer S, Baig O, Dhaliwal A, Kamran K, et al. Approximately 50% of patients report favorable clinical outcomes after endoscopic repair of hip abductor tendon tears: a systematic review. Arthrosc J Arthrosc Relat Surg. 2024;S074980632400001X. Endoscopic gluteal tendon repair results in good patient-reported outcomes and low retear rates; however, rates of MCID/PASS achievement vary.
- 73.Nazal MR, Abraham PF, Conaway WK, Quinlan NJ, Gillinov SM, Gibbs JS, et al. Endoscopic repair of full-thickness gluteus medius and minimus tears-prospective study with a minimum 2-year follow-up. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2020;36(8):2160–9. doi: 10.1016/j.arthro.2020.04.025. [DOI] [PubMed] [Google Scholar]
- 74.Maslaris A, Vail TP, Zhang AL, Patel R, Bini SA. Impact of fatty degeneration on the functional outcomes of 38 patients undergoing surgical repair of gluteal tendon tears. Arch Orthop Trauma Surg. 2022;142(9):2173–83. doi: 10.1007/s00402-021-03787-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fink B, Braun L. Treatment of extensive gluteus muscle tears with transosseous fixation and a nonresorbable collagen patch. J Arthroplasty. 2018;33(2):555–9. doi: 10.1016/j.arth.2017.08.045. [DOI] [PubMed] [Google Scholar]
- 76.Looney AM, Bodendorfer BM, Donaldson ST, Browning RB, Chahla JA, Nho SJ. Influence of fatty infiltration on hip abductor repair outcomes: a systematic review and meta-analysis. Am J Sports Med. 2022;50(9):2568–80. doi: 10.1177/03635465211027911. [DOI] [PubMed] [Google Scholar]
- 77.Uppstrom TJ, Sullivan SW, Burger JA, Ranawat AS, Kelly BT, Nwachukwu BU. Defining minimal clinically important difference after open hip abductor repair. Orthop J Sports Med. 2021;9(4):23259671211007740. doi: 10.1177/23259671211007740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23(4):586–97. doi: 10.1016/j.jse.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 79.Kahlenberg CA, Nwachukwu BU, Jahandar H, Meyers KN, Ranawat AS, Ranawat AS. Single- versus double-row repair of hip abductor tears: a biomechanical matched cadaver study. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2019;35(3):818–23. doi: 10.1016/j.arthro.2018.10.146. [DOI] [PubMed] [Google Scholar]
- 80.Derksen A, Lonnemann E, Budde S, Becker O, Wirries N, Haertlé M, et al. Clinical results after open gluteus medius repair in single-row technique. J Exp Orthop. 2022;9(1):55. doi: 10.1186/s40634-022-00483-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Putnam JG, Chhabra A, Castañeda P, Walker JB, Barber CC, Lendrum JA, et al. Does greater trochanter decortication affect suture anchor pullout strength in abductor tendon repairs? A biomechanical study. Am J Sports Med. 2018;46(7):1668–73. doi: 10.1177/0363546518759033. [DOI] [PubMed] [Google Scholar]
- 82.Incavo SJ, Harper KD. Open hip abductor tendon repair into a bone trough: improved outcomes for hip abductor tendon avulsion. JBJS Essent Surg Tech. 2020;10(2):e0042. doi: 10.2106/JBJS.ST.19.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sizeland TJB, Fearon AM, Perriman DM, Gilbert S, Lynch JT, Smith PN, et al. People after gluteal tendon repair have gait characteristics which are similar to those of a healthy cohort. Clin Biomech Bristol Avon. 2020;80:105176. doi: 10.1016/j.clinbiomech.2020.105176. [DOI] [PubMed] [Google Scholar]
- 84.Frazier LP, Quigley RA, Galvin JW, Waterman BR, Brusalis CM, Cole BJ. Put a patch on it!: When and how to perform soft-tissue augmentation in rotator cuff surgery. Oper Tech Sports Med. 2023;31(1):150984. doi: 10.1016/j.otsm.2023.150984. [DOI] [Google Scholar]
- 85.Cobb TE, Dimock RAC, Memon SD, Consigliere P, Ajami S, Imam M, et al. Rotator cuff repair with patch augmentation: what do we know? Arch Bone Jt Surg. 2022;10(10):833–46. doi: 10.22038/ABJS.2022.61345.3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bailey JR, Kim C, Alentorn-Geli E, Kirkendall DT, Ledbetter L, Taylor DC, et al. Rotator cuff matrix augmentation and interposition: a systematic review and meta-analysis. Am J Sports Med. 2019;47(6):1496–506. doi: 10.1177/0363546518774762. [DOI] [PubMed] [Google Scholar]
- 87.Chalmers PN, Tashjian RZ. Patch augmentation in rotator cuff repair. Curr Rev Musculoskelet Med. 2020;13(5):561–71. doi: 10.1007/s12178-020-09658-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mirzayan R, Weber AE, Petrigliano FA, Chahla J. Rationale for biologic augmentation of rotator cuff repairs. J Am Acad Orthop Surg. 2019;27(13):468–78. doi: 10.5435/JAAOS-D-18-00281. [DOI] [PubMed] [Google Scholar]
- 89.Acevedo DC, Shore B, Mirzayan R. Orthopedic applications of acellular human dermal allograft for shoulder and elbow surgery. Orthop Clin North Am. 2015;46(3):377–88. doi: 10.1016/j.ocl.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 90.Ebert JR, Jain M, Janes GC. Good clinical outcomes, a high level of patient satisfaction and an acceptable re-operation rate are observed 7–10 years after augmented hip abductor tendon repair. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2023;31(6):2131–9. doi: 10.1007/s00167-023-07382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ebert JR, Brogan K, Janes GC. A prospective 2-year clinical evaluation of augmented hip abductor tendon repair. Orthop J Sports Med. 2020;8(1):2325967119897881. doi: 10.1177/2325967119897881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kaplan DJ, Dold AP, Fralinger DJ, Meislin RJ. Endoscopic gluteus medius repair augmented with bioinductive implant. Arthrosc Tech. 2016;5(4):e821–5. doi: 10.1016/j.eats.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Capurro B, Kaplan DJ, Fenn TW, Chapman RS, Nho SJ. Open gluteus medius double-row repair with acellular allograft augmentation. Video J Sports Med. 2023;3(4):26350254231180629. doi: 10.1177/26350254231180629. [DOI] [Google Scholar]
- 94.Suppauksorn S, Nwachukwu BU, Beck EC, Okoroha KR, Nho SJ. Superior gluteal reconstruction for severe hip abductor deficiency. Arthrosc Tech. 2019;8(10):e1255–61. doi: 10.1016/j.eats.2019.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pascual-Garrido C, Schwabe MT, Chahla J, Haneda M. Surgical treatment of gluteus medius tears augmented with allograft human dermis. Arthrosc Tech. 2019;8(11):e1379–87. doi: 10.1016/j.eats.2019.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Whiteside LA. Surgical technique: Gluteus maximus and tensor fascia lata transfer for primary deficiency of the abductors of the hip. Clin Orthop. 2014;472(2):645–53. doi: 10.1007/s11999-013-3161-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bauwens PH, Haidar I, Thaunat M. Endoscopic transfer of gluteus maximus and tensor fasciae latae for massive gluteus medius tear: preliminary results. Orthop Traumatol Surg Res OTSR. 2021;107(8):102927. doi: 10.1016/j.otsr.2021.102927. [DOI] [PubMed] [Google Scholar]
- 98.Brenneis M, Flevas DA, Gayle LB, Boettner F, Sculco PK, Westrich GH. Gluteus maximus transfer for wound closure and treatment of abductor deficiency: a single-plastic surgeon series. Arch Orthop Trauma Surg. 2023;143(11):6927–33. doi: 10.1007/s00402-023-04968-x. [DOI] [PubMed] [Google Scholar]
- 99.Inclan PM, Schwabe MT, Song BM, Kuhn AW, Layon DR, Clohisy JC, et al. Gluteus maximus transfer for hip abductor deficiency. Arthrosc Tech. 2023;12(5):e671–6. doi: 10.1016/j.eats.2023.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kaiser D, Hoch A, Sutter R, Zingg PO. Gluteus maximus tendon transfer as a salvage option for painful chronic hip abductor insufficiency: clinical and MRI results with a minimum follow-up of 24 months. Hip Int J Clin Exp Res Hip Pathol Ther. 2023;5:11207000231197760. doi: 10.1177/11207000231197760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lemme NJ, Dworkin M, Morrissey PJ, Testa EJ, Kwan D, Roussel L, et al. Short-term outcomes following open gluteus maximus transfer for the management of hip abductor tears. J Hip Preserv Surg. 2023;10(3–4):143–8. doi: 10.1093/jhps/hnad014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maldonado DR, Annin S, Chen JW, Yelton MJ, Shapira J, Rosinsky PJ, et al. Combined transfer of the gluteus maximus and tensor fasciae latae for irreparable gluteus medius tear using contemporary techniques: short-term outcomes. JB JS Open Access. 2020;5(4):e20.00085. doi: 10.2106/JBJS.OA.20.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Christofilopoulos P, Kenanidis E, Bartolone P, Poultsides L, Tsiridis E, Kyriakopoulos G. Gluteus maximus tendon transfer for chronic abductor insufficiency: the Geneva technique. Hip Int J Clin Exp Res Hip Pathol Ther. 2021;31(6):751–8. doi: 10.1177/1120700020924330. [DOI] [PubMed] [Google Scholar]
- 104.Song BM, Inclan PM, Kuhn AW, Stronach BM, Pascual-Garrido C. Gluteus maximus transfer for irreparable hip abductor deficiency: a systematic review and meta-analysis. J Arthroplasty. 2023;S0883–5403(23):01082–3. doi: 10.1016/j.arth.2023.10.036. [DOI] [PubMed] [Google Scholar]
- 105.Jimenez-Telleria I, Foruria X, Moreta J, Bernuy L, Casado O, Martinez-de Los Mozos JL. Gluteus medius repair using a gluteus maximus flap augmented with synthetic polyethylene mesh: surgical technique and case series. Orthop Rev. 2022;14(3):31904. [DOI] [PMC free article] [PubMed]
- 106.Portet A, Lambrey PJ, Benhenneda R, Tanel L, Bauwens PH, Thaunat M. Short-term functional outcomes of Whiteside transfer for massive rupture of gluteus medius tendon in native hips. Int Orthop. 2024;48(1):57–64. doi: 10.1007/s00264-023-06050-y. [DOI] [PubMed] [Google Scholar]
- 107.Ebert JR, Fearon AM, Smith PN, Janes GC. Recommendations in the rehabilitation of patients undergoing hip abductor tendon repair: a systematic literature search and evidence based rehabilitation protocol. Arch Orthop Trauma Surg. 2022;142(11):3165–82. doi: 10.1007/s00402-021-03952-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.