Abstract
Background
We investigate the relationship between the supply of methamphetamine and overdose death risk in Ohio. Ohio and the overall US have experienced a marked increase in overdose deaths from methamphetamine combined with fentanyl over the last decade. The increasing use of methamphetamine may be increasing the risk of overdose death. However, if people are using it to substitute away from more dangerous synthetic opioids, it may reduce the overall risk of overdose death.
Methods
Ohio’s Bureau of Criminal Investigation’s crime lab data include a detailed list of the content of drug samples from law enforcement seizures, which are used as a proxy for drug supply. We use linear regressions to estimate the relationship between the proportion of methamphetamine in lab samples and unintentional drug overdose death rates from January 2015 through September 2021.
Results
Relatively more methamphetamine in crime lab data in a county-month has either no statistically significant relationship with overdose death rates (in small and medium population counties) or a negative and statistically significant relationship with overdose death rates (in large population counties). Past overdose death rates do not predict future increases in methamphetamine in crime lab data.
Conclusions
The results are consistent with a relatively higher supply of methamphetamine reducing the general risk of overdose death, possibly due to substitution away from more dangerous synthetic opioids. However, the supply of methamphetamine appears unrelated to the past illicit drug risk environment. The non-lethal and yet serious health effects of MA use were not explored and, thus, even if the presence of MA reduces the population-level overdose mortality rate, the rise of other adverse health effects may counteract any public health benefits of fewer deaths.
Keywords: Methamphetamine, Fentanyl, Overdose deaths, Ohio
Highlights
-
•
Methamphetamine in crime lab data not positively correlated with an increase in overdose death rates.
-
•
Methamphetamine a less deadly substitute for synthetic opioids.
-
•
Past overdose death rates do not predict the future presence of methamphetamine in crime lab data.
1. Introduction
Drug overdose deaths have been rising in several countries around the world. However, overdose death rates in the United States (US) remain substantially higher than any other country (Snowdon, 2022). This article focuses on the state of Ohio and seeks to understand the potential causes and consequences of the recent increase in availability of methamphetamine (MA) in an environment with a concurrent rise in synthetic opioid availability. The findings can help us to understand the broader US trend in drug supply of an increasing availability of MA and fentanyl (Cano et al., 2023). This research is relevant to other countries as well since MA supply is expanding around the globe (UNODC, 2023).
MA in the US is inexpensive and of high purity and potency (Drug Enforcement Administration, 2020). There has been a large increase in overdose deaths involving combinations of MA with fentanyl or other synthetic opioids (Ciccarone, 2021). Research has found that people who consume both MA and heroin are at higher risk of overdose than people only consuming heroin (Al-Tayyib et al., 2017). Thus, this increase in deaths may be due to purposeful co-use leading to higher overdose risk. However, Daniulaityte et al. (2023) found that among people reporting MA use in the past 30 days in Dayton, Ohio, some tested positive for fentanyl despite reporting they had not used fentanyl in the past 30 days. Hence, increasing contamination of the MA supply with fentanyl may also be raising the risk of overdose death.
This evidence would seem to indicate that the presence of MA increases, rather than decreases, the risk of overdose death. However, the positive correlation may be due to those at most risk of overdose increasing their MA use, not the MA use itself causing an increase in risk. And, thus, this statistical correlation could be present even if MA use itself somewhat reduces overdose risk. Relative to fentanyl, MA on its own has a substantially lower risk of overdose death. For people who co-use opioids and MA, a reduction in risk could be due to a reduction in the frequency of opioid use if MA is used to reduce withdrawal symptoms (Silverstein et al., 2021) or, as MA is a stimulant, it potentially provides some protection against overdose death. Some people who co-use opioids and MA believe there is a protective effect of MA (Daniulaityte et al., 2022, Clarke et al., 2022, Ondocsin et al., 2023). Animal study data show a bidirectional effect from amphetamines on the risk of fentanyl overdose, with small amounts of amphetamines increasing and larger amounts reducing risk (Elder et al., 2023). At a population level whether a greater supply of MA increases or decreases the risk of overdose death is an open question, particularly in a state with substantial numbers of synthetic opioid-related overdose deaths.
This article investigates the relationship between methamphetamine availability and overdose death using data from the Ohio Bureau of Criminal Investigation’s (BCI) Crime Labs as a measure of county-level illicit drug supply. Several other researchers have interpreted crime lab data in this way. For example, Cano et al. (2023) use the National Forensic Laboratory System (NFLIS), which includes data on drugs seized at a state level, to measure drug supply changes in the US, and Peterson et al. (2016) uses the NFLIS data to investigate changes in the drug supply in Ohio and Florida. Others, such as Hall et al. (2021), Rosenblum et al. (2020), and Zibbell et al. (2019) have used the BCI data as a measure of drug supply. State-level drug seizure data are a good proxy for drug supply, first, because the amounts seized are generally small, often less than a tenth of a gram. Thus, any individual seizure (or even 1000 s of small seizures) will not have a substantial impact on the overall illicit drug market. Second, assuming law enforcement intensity is similar from month to month within a county, changes in the composition of drugs over time, which is what we focus on, should reflect actual changes in the illicit drug market. In this article, we follow this interpretation of changes in crime lab data as changes in illicit drug supply. However, we acknowledge potential issues with this interpretation in our Limitations section.
Assuming crime lab data can be used as a reasonable measure of illicit drug supply, we can use existing data to examine the potential interrelationship between supply and demand. Our main empirical questions are: 1. Is there evidence that an increase in the amount of MA seized by law enforcement, relative to other illicit drugs, is correlated with a higher or lower overdose death rate? In other words, first, is the data consistent with MA exacerbating the overdose crisis in Ohio or does having more MA in the illicit drug supply in the presence of synthetic opioids correlate with a reduction in the risk of overdose death? 2. Does an increase in overdose deaths correlate with a future increase in the relative amounts of MA seized by law enforcement? In other words, is there evidence that people who use opioids respond to high levels of overdose risk by increasing their consumption of MA? In supply and demand terms, does an increased supply of MA reduce the risk of overdose death and does an increased risk of overdose death increase the demand for MA? We find evidence in support of the former, but not the latter. In addition, although we cannot show causal estimates of the effect of MA on overdose deaths, this latter finding shows that the estimates of the former are not being driven by MA supply preferentially going to locations with relatively high rates of overdose deaths in the recent past.
2. Methods
2.1. Data
To empirically test the relationship between the composition of the illicit drug supply and overdose death rates, the article builds on the analysis in Rosenblum et al. (2020) using updated data from the Ohio BCI Crime Labs. After extensively cleaning the crime lab data (e.g., correcting misspellings, dropping unclear or unknown lab results, and dropping duplicates), we have a dataset with 212,215 samples of illicit drugs that were seized between January 1, 2015 and September 30, 2021. We start the analysis in 2015, as this is when synthetic opioids and MA both began to appear in Ohio in substantial numbers. Our subsample includes all positive lab tests of prescription and illicit opioids (heroin, fentanyl, etc.), cocaine, MA, other synthetic stimulants (e.g. cathinones), MDMA and similar drugs, synthetic cannabis, benzodiazepines, psychedelics, PCP and variants (e.g. 3-HO-PCP), and other designer drugs. Cannabis and other miscellaneous drugs and substances are dropped from the analysis. There is a delay between drug seizure and drug testing, usually of one to two months, although in some cases substantially longer. For our current data, the BCI lab test date goes through February 14, 2022, with consistent numbers of observations for dates through September 2021. Thus, we limit our analysis to drugs seized through the third quarter of 2021.
The BCI data include information on what specific drugs are in the samples that are tested, but they do not include the specific amounts of each type of drug in the sample or the purity of these drugs. The data also do not include information on drug paraphernalia found with the drugs (e.g. syringes) or the form of the drug (e.g. powder, pill, liquid). One county out of eighty-eight, Hamilton County (which includes Cincinnati), has disproportionately few observations in the BCI data given its population size and was dropped from the analysis. Data are aggregated to the county-month or county-quarter level, yielding 7047 county-month observations and 2349 county-quarter observations.
The BCI data are linked to publicly available county-month (or quarter) rates per 100,000 of unintentional1 overdose deaths from the Ohio Department of Health (ODH)’s website (the Ohio Public Health Information Warehouse). We investigate both overall overdose deaths, which are less prone to error (Ruhm, 2018a), and psychostimulant-specific overdose deaths, which are how MA-related overdose deaths are classified. Changes in overall death rates will give us information about the overall change in the illicit drug risk environment, while psychostimulant-specific death rates will show us whether the types of overdose deaths are changing over time.
We use data from other sources to control for potential economic or health changes that may be differentially impacting overdose deaths in each county. We chose these controls due to data availability and acknowledge that there could still exist omitted variable bias from unobserved factors. The period of interest includes the COVID-19 pandemic, which may have changed the relative risk of overdose deaths differentially across counties. For example, Friedman and Akre (2021) find that early in the pandemic there was a substantial increase in overdose deaths. To account for this possibility, we use data from the ODH to control for COVID-19 cases, hospitalization, and death counts aggregated to the county-month (or quarter) level.
We control for the per capita amounts of licit prescription opioids. The presence of prescription opioids may raise or lower the risk of overdose death. On the one hand, the first wave of the opioid epidemic was driven by prescription opioids (Ciccarone, 2019) and may have increased the risk of overdose death. On the other hand, prescription opioids may offer a safer substitute relative to fentanyl and other illicit opioids. For example, Kim (2021) finds that Prescription Drug Monitoring Programs, which restrict the availability of prescription opioids, are correlated with higher heroin overdose deaths. Data for per capita amounts of prescription opioids and opioid treatment (i.e. buprenorphine) drugs dispensed at the county-quarter level are from the publicly available Ohio Automated RX Reporting System Quarterly County Data. Last, as economic conditions may affect the demand for illicit drugs (Ruhm, 2018b), we control for county-month unemployment rates from the US Bureau of Labor Statistics.
2.2. Overview of overdose and drug lab data in Ohio
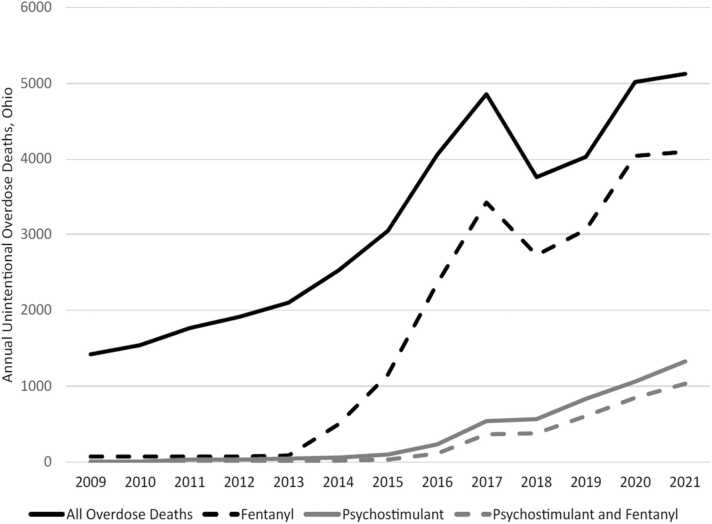
Similar to the pattern in the US as a whole, Ohio has experienced a large increase in unintentional overdose deaths over the last decade, mostly attributable to fentanyl and fentanyl analogs. We present these trends in Fig. 1. The spike in 2017 was largely due to an influx of the analog carfentanil (Jalal and Burke, 2021), which is far more deadly than fentanyl. Also similar to the overall US, there has been an increase in deaths related to psychostimulants (methamphetamine and related drugs). However, as can be seen in the figure, most of the psychostimulant deaths can be attributed to those using a combination of psychostimulants and synthetic opioids.
Fig. 1.
Annual unintentional overdose deaths in Ohio by drug-type. Fentanyl includes deaths where fentanyl and/or fentanyl analogs were associated with the death. Psychostimulant and Fentanyl deaths include both fentanyl (and/or a fentanyl analog) and a psychostimulant. Other drugs could be involved in each drug-type. Data Source: Ohio Department of Health.
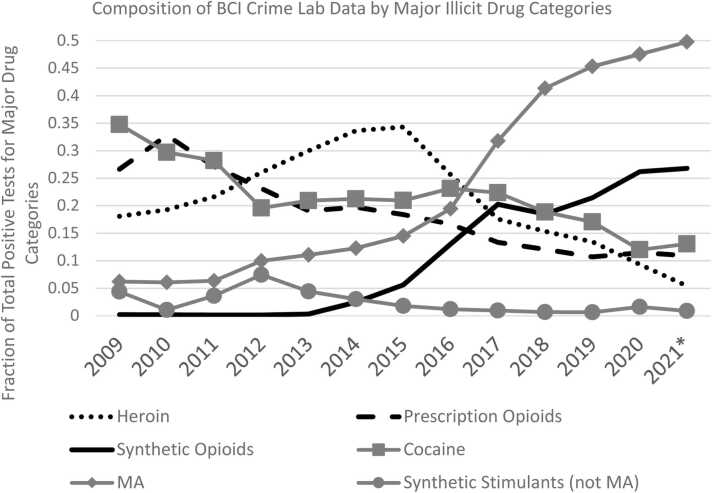
Fig. 2 shows how the BCI crime lab data have changed over time for the major categories of drugs. While the share of lab samples containing prescription opioids and heroin have been falling over time, synthetic opioids grew from about five percent of illicit drugs tested in 2015 to more than twenty-five percent in 2020 and 2021. Cocaine has been slowly declining, while MA has risen from a little more than 5 percent of the drugs tested in 2011 to about half in 2021. Thus, synthetic opioids, primarily fentanyl, and MA have become the dominant illicit drugs in Ohio.
Fig. 2.
Annual fractions of positive BCI lab tests from major drug classes that contain the specified drug class. The fraction of tests is calculated as the number of drug-specific tests divided by the sum of all positive tests that contain at least one of the major drug classes. Samples can test positive for multiple substances. Synthetic opioids include fentanyl and analogs as well as other illicit synthetic opioids such as U-47700 and etonitazene. Data Source: BCI Crime Lab Data, 2021 data are through September 2021.
In addition, although small as a total fraction of MA crime lab tests, MA combinations with opioids, primarily fentanyl, have been increasing. Approximately 4.5 percent of MA positive crime lab samples in 2020 and 2021 also contain fentanyl. The prevalence of MA and MA-opioid combinations varies by county population size, with larger population counties having relatively less of both, as well as fewer overdose deaths attributable to MA or MA-fentanyl combinations. To explore the potential heterogeneity in the relationship between MA and overdose deaths, the estimates below include sub-analyses of counties with small, medium, and large populations.
2.3. Estimation strategy
The estimates are implemented using linear regression analysis (OLS). To investigate whether an increase in MA in drug seizures is correlated with a contemporaneous higher or lower rate of overdose death, we estimate the following equation:
| Deathsit = β1MethNoSynthit + β2MethAnySynthit + β3SynthNoMethit+δXit + αi+γt+eit | (1) |
where Deathsit is the rate per 100,000 of unintentional overdose deaths in county i and month t.2 MethNoSynthit is the fraction of county-month BCI lab tests that are positive for MA, but not any synthetic opioids. MethAnySynthit is the fraction of county-month BCI lab tests that are positive for both MA and any synthetic opioid. SynthNoMethit is the county-month fraction of BCI lab tests that are positive for any synthetic opioid, but not MA. The separation of tests in this way clarifies the role MA in general is playing as opposed to MA combined with or contaminated with synthetic opioids. These three variables are the main independent variables of interest. Using the fraction of tests rather than the number of tests in a month helps to adjust for month-to-month differences in total lab tests and also makes counties of different sizes more comparable. Fractions also help to remove bias that may be occurring from any general increased intensity of law enforcement in a particular county in a particular month that would show up as higher absolute numbers of drug samples.
Xit is a vector of time-varying county-level controls: the county-month fraction of positive tests for other illicit and prescription drugs from the BCI crime lab data, prescribed opioid morphine milligram equivalent dose (MME) per capita for each quarter for non-buprenorphine opioids and also the mg per capita for prescribed buprenorphine each quarter, and monthly unemployment rates. We include controls for the presence of COVID-19, which is the county-month number of COVID-19 cases, hospitalizations, and fatalities. αi and γt are county and month fixed effects respectively. eit is the error term clustered by county. The time and location fixed effects control for general time trends in overdose deaths in Ohio as well as any time invariant county-specific differences in overdose deaths.
In addition, we perform estimates for the subsamples of small population counties (less than 50,000), medium population counties (between 50,000 and 100,0000), and large population counties (more than 100,000), to test whether locations with higher synthetic opioid availability (i.e. larger population counties) are differentially affected by increases in MA. For testing whether the presence of higher opioid overdose risk increases the future prevalence of MA, we aggregate the data by quarter rather than month, with the average monthly overdose death rate over a quarter as an independent variable and future fraction of lab tests containing MA as the dependent variable (1 quarter, 2 quarters, 3 quarters, and 4 quarters ahead).
3. Estimation results
Table 1 presents the correlation between the fraction of MA positive BCI crime lab tests and overall overdose death rates at the county-month level. We find that while there is no overall correlation, in large population counties there is a statistically significant correlation (p-value = 0.06): a 100 percentage point increase in MA is associated with a fall in the overdose death rate by about 0.5. To put this number in context, the average fraction of tests that are positive for MA in a county-month over the time period is about 0.23. If that fraction doubled it would be associated with a drop in the unintentional overdose death rate by about 0.1. The average monthly overdose death rate in large population counties is 2.87 per 100,000. Thus, this increase in MA supply would be correlated with a fall in the overdose death rate by about 3.5 percent. The combined population of the large population counties is approximately 8.9 million. Hence, this fall in the death rate translates into about 9 fewer deaths per month.
Table 1.
OLS: Relationship between the fraction of BCI crime lab tests containing MA and unintentional overdose death rates per 100,000, 2015–2021.
| All Counties | Small | Medium | Large | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| MA no Synthetic Opioids | -0.0893 | -0.0630 | 0.0591 | -0.4764* |
| (0.1599) | (0.2227) | (0.3852) | (0.2422) | |
| MA and Synthetic Opioids | 1.0697 | 1.2847 | 0.5027 | 0.3534 |
| (1.0566) | (1.6519) | (1.1676) | (0.6431) | |
| Synthetic Opioids no MA | 1.5451*** | 1.0764** | 1.8711** | 1.9837*** |
| (0.3402) | (0.4994) | (0.7798) | (0.6016) | |
| R-Squared | 0.25 | 0.18 | 0.37 | 0.49 |
| Observations | 7047 | 3159 | 1782 | 2106 |
Notes: Robust standard errors, clustered at the county level, are reported in parentheses. The estimates control for the fraction of monthly positive tests of cocaine, heroin, prescription opioids, synthetic cannibinoids, non-meth synthetic stimulants, PCP and PCP variants, psychedelics, barbiturates, and other designer drugs (each as a separate variable). See Appendix A for detailed definitions of drug categories. Other county-month controls: unemployment rate, COVID 19 case counts, hospitalizations, and deaths. County-quarter controls: per capita MME of prescription opioids, per capita mg of prescription buprenorphine. Estimates also include month and county fixed effects. Each observation is at the county-month level from 2015 through the 3rd quarter of 2021. Small Counties: population 50,000 or less. Medium Counties: population between 50,000 and 100,000. Large Counties: population more than 100,000. (* p<0.1, ** p<0.05, *** p<0.01).
Given the sizeable increase in overdose deaths in Ohio from psychostimulant-fentanyl combinations shown in Fig. 1, it is perhaps surprising that our estimates provide evidence in accord with the idea that the increased prevalence of MA is not driving an increase in overall overdose deaths. Instead, our estimates indicate that increases in MA supply do not increase the general risk of overdose death and, in the high population counties with the most fentanyl-related overdose deaths, it may even reduce the risk of overdose death.
In addition, as the variable is the fraction of crime lab tests, when MA tests rise, other drug types will fall. As synthetic opioids in the crime lab are the strongest predictor of overdose deaths, we can estimate what would happen to overdose deaths if all of the increase in MA reduced the fraction of synthetic opioids by a similar amount. If the fraction of synthetic opioids in the crime lab tests fell by 0.23, this would correlate with a reduction in the overdose death rate by about 0.46, a 16 percent fall in the overdose death rate, or about 41 fewer deaths per month. Thus, if MA supply increases cause a relative decline in the availability of synthetic opioids, we would expect overdose deaths to decline as well.
Synthetic opioids in crime lab tests are positively correlated with overdose deaths overall and across the subsamples of small, medium, and large counties. However, MA mixed with a synthetic opioid in crime lab tests are not associated with an increase or decrease in overall overdose death rates. In Table 2 where the outcome is psychostimulant death rates, there is also no statistically significant correlation between MA mixed with a synthetic opioid in crime lab tests and overdose death rates. For medium-size counties, there is a positive association, significant at the 5 % level, between MA without synthetic opioids and psychostimulant death rates. Since overall overdose death rates are uncorrelated with the fraction of MA in medium-size counties, this finding indicates that as MA deaths rose, other types of overdose deaths fell an equivalent amount.
Table 2.
OLS: Relationship between the fraction of BCI crime lab tests containing MA and unintentional psychostimulant overdose death rates per 100,000, 2015–2021.
| All Counties | Small | Medium | Large | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| MA no Synthetic Opioids | 0.0402 | -0.0542 | 0.4864** | 0.1326 |
| (0.0683) | (0.0658) | (0.2172) | (0.1095) | |
| MA and Synthetic Opioids | 0.6445 | 0.5359 | 0.8165 | 1.0366 |
| (0.6841) | (0.9906) | (1.2161) | (0.7389) | |
| Synthetic Opioids no MA | 0.2127 | 0.0568 | 0.9023*** | -0.0485 |
| (0.1336) | (0.1833) | (0.3159) | (0.1078) | |
| R-Squared | 0.22 | 0.18 | 0.36 | 0.38 |
| Observations | 7047 | 3159 | 1782 | 2106 |
Notes: Robust standard errors, clustered at the county level, are reported in parentheses. The estimates control for the number of monthly positive tests of cocaine, heroin, prescription opioids, synthetic cannibinoids, non-meth synthetic stimulants, PCP and PCP variants, psychedelics, barbiturates, and other designer drugs (each as a separate variable). See Appendix A for detailed definitions of drug categories. Other county-month controls: unemployment rate, COVID 19 case counts, hospitalizations, and deaths. County-quarter controls: per capita MME of prescription opioids, per capita mg of prescription buprenorphine. Estimates also include month and county fixed effects. Each observation is at the county-month level from 2010 through 2017. Small Counties: population 50,000 or less. Medium Counties: population between 50,000 and 100,000. Large Counties: population more than 100,000.
(* p<0.1, ** p<0.05, *** p<0.01).
These results are somewhat different than those found by Zibbell et al. (2022) who investigated the relationship between illicit stimulant-involved overdose deaths and MA and cocaine in the BCI crime lab data at the state level. Like us, they find no overall statistically significant correlation between MA-related overdose deaths and MA without synthetic opioids in BCI crime lab tests. However, unlike in our estimates, they find a statistically significant positive correlation between MA with synthetic opioids and MA-specific overdose deaths at the state level. This difference in findings may be due to their estimates being at the state level rather than the county level, since our estimates include month fixed effects that absorb any variation over time happening across the state of Ohio. Their estimates are also focused on death counts and crime lab test counts, rather than fractions and rates, which could yield different results.
While there may be an overall increase in the risk of overdose death in Ohio from COVID-19, which would be controlled for by our month fixed effect, we do not find a statistically significant correlation between county-level overdose death rates and the severity of COVID-19. This result is similar to the findings of DiGennaro et al. (2021) who investigate the effects of COVID-19 on overdose death trends in Massachusetts, but do not find measurable correlations between county-level COVID-19 deaths and overdose deaths.
The estimates in Table 1, Table 2 are robust to using a Poisson regression analysis with death counts instead of death rates as the dependent variable and either fractions of crime lab tests or crime lab test counts as independent variables. The estimates are robust to limiting the sample to the years 2015–2019, to avoid any potential effects of COVID-19. Under these restricted dates, there is a larger negative correlation between MA without synthetic opioids and overall drug death rates for large population counties (coefficient = −0.787), statistically significant at the 1 % level. Hence, it could be that COVID-19 itself affected the role of MA in reducing overdose deaths or it may be that the relatively lower overdose death rates in the presence of MA are diminishing over time. Additionally, in the pre-COVID-19 estimates the presence of MA is correlated with higher psychostimulant death rates overall, whereas in the main estimates there is no statistically significant correlation.
Table 3 displays estimation results that test whether a higher overdose death rate predicts higher fractions of MA in BCI lab tests in future quarters. We do not find a statistically significant relationship between current death rates and future MA in crime lab samples.3 There is a similar lack of correlation if death counts and drug counts are used in a Poisson regression. Estimates on the subsamples (not shown) of small, medium, and large population counties yield similar, not statistically significant, coefficients.
Table 3.
OLS: Relationship between unintentional overdose death rates per 100,000 and the future fraction of BCI lab drug tests containing MA (without synthetic opioids), 2015–2021.
| +1 Quarter | +2 Quarters | +3 Quarters | +4 Quarters | |
|---|---|---|---|---|
| Overall Overdose Death Rate | -0.0013 (0.0034) |
-0.0060* (0.0034) |
-0.0030 (0.0032) |
0.0004 (0.0043) |
| Fentanyl Overdose Death Rate | -0.0000 (0.0009) |
-0.0008 (0.0010) |
-0.0002 (0.0009) |
0.0009 (0.0012) |
| Observations | 2262 | 2175 | 2088 | 2001 |
Notes: The table shows coefficients for eight separate estimates with the independent variable of interest being Overall or Fentanyl-specific Overdose Death Rates and the dependent variable being the fraction of BCI lab tests that are positive for methamphetamine 1, 2, 3, or 4 quarters in the future. Robust standard errors, clustered at the county level, are reported in parentheses. Each observation is at the county-quarter level from 2015 through the third quarter of 2021. The estimates control for the quarterly average unemployment rate, quarterly COVID 19 case counts, hospitalizations, and deaths, as well as quarterly per capita MME of prescription opioids, and per capita mg of prescription buprenorphine. Estimates include quarter and county fixed effects.
(* p<0.1, ** p<0.05, *** p<0.01).
These findings on the relationship between past overdose death rates and future MA supply are important for two reasons. First, these estimates show that the MA market is not differentially responding to counties based on the relative overdose death risk. That is, we do not see evidence that MA supply is responding to demand for less deadly illicit drugs. Individuals may be consuming MA as a risk mitigation strategy, but if this is true, they are either only a small part of the population, and so we do not see this in the aggregate estimates, or MA is being used as a risk mitigation strategy across counties at similar rates regardless of the extent of overdose deaths in a specific county. Second, as the estimates in Table 1, Table 2 are non-causal, we may worry that the negative contemporaneous correlation between MA in lab tests and overdose death rates in large counties is due to MA supply preferentially going to counties which have slower increases in or even declining overdose death rates. However, the estimates in Table 3 do not support that hypothesis. Rather the estimates align with MA supply rising across counties in Ohio regardless of prior trends in overdose death rates and that the counties that happened to have relatively more MA (and less synthetic opioids) in their illicit drug supply have relatively fewer deaths.
4. Limitations
One of the limitations of the empirical findings in this article, and in general of empirical research on illicit drugs, is the lack of precise data on the supply, demand, and consequences of illicit drugs. Crime lab data can provide detailed information about what law enforcement is detecting. However, if law enforcement is targeting specific types of drugs and ignoring others, e.g. ignoring methamphetamine and focusing on fentanyl, then the crime lab data could be misleading about the actual state of the illicit drug market. As already mentioned, when multiple drugs are present in the same sample, we are not able to detect the relative quantities of each within the sample. It is for this reason that we separate MA and synthetic opioids into three distinct variables, combined and not combined. However, when interpreting the observations of MA combined with synthetic opioids, we may be estimating the null results because the variable is too imprecise: e.g. if we could have differentiated the samples that are mostly MA from those that are mostly opioids we may have found different results.
We may be misinterpreting the changes in crime lab data as changes in supply as it could instead reflect the consequences of differential incarceration or decreases in supply that could affect overdose deaths as was found by Ray et al. (2023) in Indiana. That is, if the police are arresting many more people with MA, it may have a substantial negative effect on the supply of MA, and, thus, we would interpret the negative correlation of MA in lab tests and death rates as a fall in MA supply leading to a fall in overdose deaths. However, given that there are relatively few monthly seizures in a county in Ohio, many typically less than a gram of drugs per seizure, these arrests should not have an appreciable affect on county-level drug supply. In any case, since we do not use the number of MA samples, but rather the relative amounts of MA samples compared to other types of drugs, our measure is not picking up intensity of arrests.
A related concern is that the estimates are really just detecting the number of incarcerated people who use MA, rather than the composition of the drug market. Hence, it may be that the overdose death rate is driven down in the short-run with a temporarily lower number of people who use MA, and the estimates are missing the long-term increases in overdose deaths that will occur when they are released from prison. We acknowledge that we are focused on contemporaneous estimates and are missing any long-term consequences that could be substantial. Although the BCI crime lab data is by no means a perfect measure of changes in the types of drugs available in the illicit drug market in Ohio, it is the best available data. Given our estimation strategy in which we control for time and county, as long as law enforcement is not changing their enforcement strategies differentially by county over time, the estimates should detect actual changes in the illicit drug market even if measured imprecisely.4
In addition to the crime lab data, mortality data may be imprecise about the specific cause of death. Some overdose deaths may be misclassified as other types of deaths or deaths due to psychostimulants or fentanyl may have undercounts. Within the fentanyl-specific deaths, which fentanyl analog if any was present is unknown. This issue is why we focus on overall overdose deaths. However, even if the overdose death data were entirely accurate, another issue is that the only health outcome we explore is overdose deaths. The non-lethal health effects of MA, e.g. psychosis, myocardial infarction, hypertension, etc. (Darke et al., 2008), are entirely absent from our estimates and, thus, even if the presence of MA reduces the population-level overdose mortality rate, the rise of other adverse health effects may more than counteract any public health benefits of fewer deaths.
5. Discussion
The estimates presented in this article find important evidence of the potential consequences of the rapid expansion of the MA supply in Ohio, which can help inform the public health consequences of a similar expansion across the US. We find that relatively more MA detected by crime labs is either unrelated to or associated with a small, but measurable decrease in the overall risk of unintentional overdose death. This is not to say that MA is safe or cannot cause overdose deaths. Our findings are not that the combination of MA and fentanyl is in fact safer than fentanyl on its own. As our estimates are only showing averages, it could certainly be the case that an increase in MA availability makes illicit drug consumption more deadly for some people or at particular dose levels. Rather, given the context of extremely dangerous synthetic opioids, our estimates should be interpreted as showing that a relative increase in the availability of less deadly drugs, especially if they are replacing synthetic opioids, may reduce the overall number of overdose deaths, at least in the short-run. Furthermore, we do not investigate the substantial, non-fatal health consequences of MA use such as psychosis and cardiovascular disease, which may be increasing even if deaths decline.
The exact mechanism linking MA to overdose deaths is not clear. Is it that MA use directly reduces the risk of overdose when used concurrently with opioids? If the animal data are applicable to humans, is MA co–use with fentanyl reducing opioid overdose risk at some doses and increasing it at others? Is it that MA use allows people to lengthen the duration between opioid use or substitute away from opioids entirely? This is supported by recent research showing that some people find MA helpful for managing opioid withdrawal (Ondocsin et al., 2023). Or is MA supply simply correlated with a reduction in overdose death, and we are missing a key unobservable omitted variable, such as greater migration to substance use treatment, that is positively correlated with MA supply?
Research carried out in 2019 by the qualitative arm of this study team in neighboring West Virginia (WV) found that uptake of MA among people who already used opioids was common. This adoption of MA was driven by supply factors, including the shift from locally produced to Mexican-sourced MA, as well as local economic and social factors. These included a low price-point relative to opioids and a desire for participation with others using MA alone or in combination with opioids (Ondocsin et al., 2023, Mars et al., 2024).
Interestingly, in a given area, MA supply is unrelated to past overdose deaths. That is, although individuals using MA with opioids may be doing so to reduce their overdose risk, we do not find evidence that at the population level, increases in the MA supply are being driven by overdose deaths in the vicinity. This finding is consistent with Mars et al. (2019) that argues that in North America, where fentanyl was sold as heroin, uptake was largely supply driven rather than demand driven. In recent years this has changed with the sale of fentanyl under its own name (Kral et al., 2021). Methamphetamine is also sold under its own identity but supply forces remain dominant.
Deaths from opioids and stimulants form the current ‘fourth wave’ of the US Overdose Epidemic, and there remain many unanswered questions about the contribution of these drugs to changing patterns of mortality (Ciccarone, 2021). By using both seizure data and overdose mortality data it is possible to estimate how the influx of methamphetamine into an area correlates with the risk environment. The resulting picture is one where, abundant low cost, high purity methamphetamine is not necessarily leading to an increase in overdose deaths and, given the prevalence of the relatively more deadly fentanyl, may even be slightly reducing them.
Funding
NIH-NIDA Grant R01DA054190; NIH-NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
CRediT authorship contribution statement
Daniel Ciccarone: Writing – review & editing, Funding acquisition. Sarah G. Mars: Writing – review & editing, Writing – original draft. Dennis Cauchon: Writing – review & editing, Writing – original draft, Data curation. Daniel Rosenblum: Writing – review & editing, Writing – original draft, Visualization, Methodology, Formal analysis, Data curation, Conceptualization. Jeffrey Ondocsin: Writing – review & editing, Writing – original draft.
Declaration of Competing Interest
Daniel Rosenblum, Jeffrey Ondocsin, Sarah G. Mars, and Daniel Ciccarone received funding for this study from NIH-NIDA Grant R01DA054190; NIH-NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Acknowledgments
We thank the editor and two anonymous referees for their valuable comments. We thank the Ohio Bureau of Criminal Investigation (BCI) for providing crime lab data. BCI had no further role in study design; analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. Funding for this study was provided by NIH-NIDA Grant R01DA054190; NIH-NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. Mortality and COVID-19 data are publicly available from the Ohio Department of Health. The Department specifically disclaims responsibility for any analyses, interpretations or conclusions.
Footnotes
Much of the literature on overdose deaths focuses on deaths classified as unintentional, meaning not due to suicide or undetermined intent. These types of deaths are distinguished from each other in the ICD-10 classification system: X40–44 (unintentional), X60–64 (suicide), and Y10-Y14 (undetermined). Suicide and undetermined overdose deaths are much fewer than unintentional overdose deaths and have remained relatively stable over recent years, while unintentional overdose deaths have risen markedly (Olfson et al., 2019).
Underlying cause of death ICD-10 codes X40-X44, unintentional drug overdose deaths.
The one exception is a small negative correlation between overdose death rates and MA in the lab tests two quarters later, which is statistically significant at the 10 percent level.
A similar rationale allows for the use of the Drug Enforcement Agency’s System to Retrieve Information from Drug Evidence (STRIDE) database to measure changes in the illicit drug market, which also suffers from the problem of being a non-random sample (Arkes et al., 2008).
Appendix A. Drug class definitions and descriptive statistics
Below is an updated version of Appendix A found in Rosenblum et al. (2020). We list below the definition of the drug classes that we created from the BCI crime lab. The drugs in the data are contained as a list of drugs in string format. We searched these strings for specific drug names to categorize below. The data were cleaned and corrected for misspellings (e.g. fentanyl is spelled as fetanyl, fenrtanyl, fenanyl, and fenatnyl) and to remove potential double counts (e.g. to ensure acetyl fentanyl was counted as a fentanyl analog, but not fentanyl itself).
Methamphetamine: Methamphetamine or amphetamine.
Synthetic Opioids: Fentanyl, fentanyl analogs (acetyl, acryl, benzyl, benzylfuranyl, benzylparaflouro, benzylparaflourocyclopropyl, buranyl, butyryl, carfentanil, crotonyl, cyclopropyl, 4-flouroisobutyryl, 2-furanyl, furanyl, 3-methyl, methoxy-acetyl, nmethylnor, ortho-fluoro, orthomethylacetyl, orthomethylfuranyl, paraflouro, paraflourofuranyl, paraflourovaleryl, phenyl fentanyl, tetrahydrofuran, thiophene, valeryl). Non-fentanyl synthetic opioids: (ANPP; U–47700, ISO–U47700, 4TFM–U47700, 2NAP–U47700, U– 48800, U–49900, U–51754; etodesnitazene, etonitazene, NP–etonitazene, isotonitazene, flunitazene, and piperidylthiambutene).
Cocaine: Cocaine.
Heroin: Heroin or 6-Monoacetylmorphine
Prescription Opioids: Buprenorphine, morphine, codeine, oxycodone, oxymorphone, hydromorphone, hydrocodone, tramadol, methadone, meperidine, diphenoxylate, pentazocine, propoxyphene, tapentadol, dihydrocodeine, dextropropoxyphene, dextromethorphan, levomethorphan.
Barbiturates: Aprobarbital, amobarbital, barbital, butalbital, pentobarbital, phenobarbital, and secobarbital.
Synthetic Cannibinoids: 75 different synthetic cannibinoids (e.g. AB-CHMINACA, AB-FUBINACA, etc.). A full list is available upon request.
Other Synthetic Stimulants: 79 different cathinones (e.g. pentedrone) and amphetamine-like drugs (e.g. phentermine). A full list is available upon request.
MDMA: MDMA, MDA, MDMC, and MDDMA.
Psychedelics: 25 different psychedelic drugs (Psilocybin, LSD, DMT, etc.). A full list is available upon request.
Other Designer Drugs: 25B-NBOMe, 25C-NBOMe, 25H-NBOMe, 25I-NBOMe, 25B-
NBOH, 25I-NBOH, Bk-2C-B, 2-CB, 2-CE, 2-CT-4, 2-CI, and 2-CP.
PCP: PCP, 3-Cl-PCP, 3-HO-PCP, 3-HO-PCE, 3-MeO-PCP, BTCP, and TCP.
Table A1.
Descriptive Statistics (County-Month Level) 2015–3rd Quarter of 2021
| Standard | ||||
|---|---|---|---|---|
| Variable | Mean | Deviation | Min | Max |
| All Overdose Deaths | 3.72 | 7.85 | 0 | 96 |
| Psychostimulant Overdose Deaths | 0.58 | 1.42 | 0 | 17 |
| Fentanyl Overdose Deaths | 2.57 | 6.31 | 0 | 89 |
| All Overdose Death Rate | 2.55 | 2.72 | 0 | 28 |
| Psychostimulant Overdose Death Rate | 0.60 | 1.36 | 0 | 15.4 |
| Fentanyl Overdose Death Rate | 1.66 | 2.23 | 0 | 26.5 |
| Meth and Synthetic Opioid | 0.33 | 0.88 | 0 | 11 |
| Meth no Synthetic Opioid | 10.50 | 13.74 | 0 | 137 |
| Synthetic Opioid no Meth | 5.36 | 8.68 | 0 | 139 |
| Cocaine | 4.49 | 9.97 | 0 | 93 |
| Heroin | 5.17 | 9.09 | 0 | 82 |
| Prescription Opioids | 3.99 | 5.96 | 0 | 78 |
| Barbiturates | 0.01 | 0.13 | 0 | 5 |
| Synthetic Cannibinoids | 0.30 | 1.15 | 0 | 22 |
| Other Synthetic Stimulants | 0.33 | 1.23 | 0 | 26 |
| MDMA | 0.17 | 0.86 | 0 | 31 |
| Psychedelics | 0.48 | 1.35 | 0 | 22 |
| Other Designer Drugs | 0.01 | 0.17 | 0 | 7 |
| PCP | 0.17 | 0.86 | 0 | 22 |
| Unemployment Rate(%*100) | 5.58 | 2.21 | 2.1 | 26.2 |
| Covid Case Count | 189.16 | 1016.52 | 0 | 26977 |
| Covid Hospitalizations | 10.24 | 49.35 | 0 | 1226 |
| Covid Deaths | 3.15 | 16.83 | 0 | 627 |
| Opioids MME Per Capita | 127.25 | 57.52 | 18.57 | 350.16 |
| Buprenorphine MG Per Capita | 422.35 | 356.16 | 6.44 | 3632.83 |
Notes: All Ohio counties except Hamilton county are included. There are 7047 observations in total. Drug categories are defined as above. Death rates are number of deaths per person multiplied by 100,000. Opioids MME Per Capita and Buprenorphine MG Per Capita are at the county-quarter level.
References
- Al-Tayyib Alia, Koester Stephen, Langegger Sig, Raville Lisa. Heroin and methamphetamine injection: an emerging drug use pattern. Subst. Use Misuse. 2017;52(8):1051–1058. doi: 10.1080/10826084.2016.1271432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arkes J., Pacula R.L., Paddock S.M., Caulkins J.P., Reuter P. National Bureau of Economic Research; 2008. Why the DEA Stride Data Are Still Useful for Understanding Drug Markets. Working Paper 14224. [Google Scholar]
- Cano, Manuel, Timmons Patricia, Hooten Madeline, Sweeney Kaylin. Drug supply measures and drug overdose mortality in the era of fentanyl and stimulants. Drug Alcohol Depend. Rep. 2023;9 doi: 10.1016/j.dadr.2023.100197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone Daniel. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int. J. Drug Policy. 2019;71:183–188. doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone Daniel. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr. Opin. Psychiatry. 2021;34(4):344. doi: 10.1097/YCO.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, Duhart Sarah E., Kral Alex H., Jon E.Zibbell. Consuming illicit opioids during a drug overdose epidemic: illicit fentanyls, drug discernment, and the radical transformation of the illicit opioid market. Int. J. Drug Policy. 2022;99 doi: 10.1016/j.drugpo.2021.103467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte Raminta, Ruhter Lance, Juhascik Matthew, Silverstein Sydney. Attitudes and experiences with fentanyl contamination of methamphetamine: exploring self-reports and urine toxicology among persons who use methamphetamine and other drugs. Harm Reduct. J. 2023;20(54):1–10. doi: 10.1186/s12954-023-00782-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte Raminta, Silverstein Sydney M., Getz Kylie, Juhascik Matthew, McElhinny Megan, Dudley Steven. Lay knowledge and practices of methamphetamine use to manage opioid-related overdose risks. Int. J. Drug Policy. 2022;99 doi: 10.1016/j.drugpo.2021.103463. [DOI] [PubMed] [Google Scholar]
- Darke Shane, Kaye Sharlene, McKetin Rebecca, Duflou Johan. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008;27(2):253–262. doi: 10.1080/09595230801923702. [DOI] [PubMed] [Google Scholar]
- DiGennaro, Catherine, Garcia Gian-Gabriel P., Stringfellow Erin J., Wakeman Sarah, Jalali Mohammad S. Changes in characteristics of drug overdose death trends during the COVID-19 pandemic. Int. J. Drug Policy. 2021;98 doi: 10.1016/j.drugpo.2021.103392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Enforcement Administration, 2020. National Drug Threat Assessment. Drug Enforcement Administration Strategic Intelligence Section, US Department of Justice. Published March, DEA-DCT-DIR-008-21, pp. 19–27.
- Elder, Harrison J., Varshneya Neil B., Matthew Walentiny D., Beardsley Patrick M. Amphetamines modulate fentanyl-depressed respiration in a bidirectional manner. Drug Alcohol Depend. 2023;243 doi: 10.1016/j.drugalcdep.2022.109740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman Joseph, Akre Samir. COVID-19 and the drug overdose crisis: uncovering the deadliest months in the United States, January-July 2020. Am. J. Public Health. 2021;111(7):1284–1291. doi: 10.2105/AJPH.2021.306256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall O.E., Hall O.T., Eadie J.L., Teater J., Gay J., Kim M., Cauchon D., Noonan R.K. Street-drug lethality index: a novel methodology for predicting unintentional drug overdose fatalities in population research. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalal Hawre, Burke Donald S. Carfentanil and the rise and fall of overdose deaths in the United States. Addiction. 2021;116(6):1593–1599. doi: 10.1111/add.15260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Bokyung. Must-access prescription drug monitoring programs and the opioid overdose epidemic: the unintended consequences. J. Health Econ. 2021;75 doi: 10.1016/j.jhealeco.2020.102408. [DOI] [PubMed] [Google Scholar]
- Kral, Alex H, Lambdin Barrot H., Browne Erica N., Wenger Lynn D., Bluthenthal Ricky N., Zibbell Jon E., Davidson Peter J. Transition from injecting opioids to smoking fentanyl in San Francisco, California. Drug Alcohol Depend. 2021;227 doi: 10.1016/j.drugalcdep.2021.109003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars Sarah G., Ondocsin Jeff, Holn Nicole, Ciccarone Daniel. The influence of transformations in supply on methamphetamine initiation among people injecting opioids in the United States. Harm Reduct. J. 2024;21(57):1–13. doi: 10.1186/s12954-024-00976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars Sarah G., Rosenblum Daniel, Ciccarone Daniel. Illicit fentanyls in the opioid street market: desired or imposed? Addiction. 2019;114(5):774–780. doi: 10.1111/add.14474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson Mark, Rossen Lauren M., Wall Melanie M., Houry Debra, Blanco Carlos. Trends in intentional and unintentional opioid overdose deaths in the United States, 2000-2017. JAMA. 2019;322(23):2340–2342. doi: 10.1001/jama.2019.16566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondocsin Jeff, Holm Nicole, Mars Sarah G., Ciccarone Daniel. The motives and methods of methamphetamine and ‘heroin’ co-use in West Virginia. Harm Reduct. J. 2023;20(1):1–9. doi: 10.1186/s12954-023-00816-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson A.B., Gladden R.M., Delcher C., et al. Increases in fentanyl-related overdose deaths: Florida and Ohio, 2013-2015. Morb. Mortal. Wkly. Rep. 2016;65(33):844–849. doi: 10.15585/mmwr.mm6533a3. [DOI] [PubMed] [Google Scholar]
- Ray Bradley, Korzeniewski Steven J., Mohler George, Carroll Jennifer J., Del Pozo Brandon, Victor Grant, Huynh Philip, Hedden Bethany J. Spatiotemporal analysis exploring the effect of law enforcement drug market disruptions on overdose, Indianapolis, Indiana, 2020–2021. Am. J. Public Health. 2023;113(7):750–758. doi: 10.2105/AJPH.2023.307291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum Daniel, Unick Jay, Ciccarone Daniel. The rapidly changing US illicit drug market and the potential for an improved early warning system: evidence from Ohio drug crime labs. Drug Alcohol Depend. 2020;208 doi: 10.1016/j.drugalcdep.2019.107779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm Christopher J. National Bureau of Economic Research; 2018. Deaths of Despair or Drug Problems? Working Paper 24188. [Google Scholar]
- Ruhm Christopher J. Corrected US opioid-involved drug poisoning deaths and mortality rates, 1999–2015. Addiction. 2018;113(7):1339–1344. doi: 10.1111/add.14144. [DOI] [PubMed] [Google Scholar]
- Silverstein, Sydney M., Raminta Daniulaityte, Kylie Getz, William Zule. It’s crazy what meth can help you do: lay beliefs, practices, and experiences of using methamphetamine to self-treat symptoms of opioid withdrawal. Subst. Use Misuse. 2021;56(11):1687–1696. doi: 10.1080/10826084.2021.1949612. [DOI] [PubMed] [Google Scholar]
- Snowdon John. Drug overdose death rates in different countries: who should be alarmed? Australas. Psychiatry. 2022;30(1):26–30. doi: 10.1177/10398562221075192. [DOI] [PubMed] [Google Scholar]
- UNODC . United Nations Publication; 2023. World Drug Report 2023; p. 2023. [Google Scholar]
- Zibbell J.E., Aldridge A.P., Cauchon D., DeFiore-Hyrmer J., Conway K.P. Association of law enforcement seizures of heroin, fentanyl, and carfentanil with opioid overdose deaths in Ohio, 2014-2017. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.14666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell Jon E., Clarke Sarah Duhart, Kral Alex H., Richardson Nicholas J., Cauchon Dennis, Aldridge Arnie. Association between law enforcement seizures of illicit drugs and drug overdose deaths involving cocaine and methamphetamine, Ohio, 2014–2019. Drug Alcohol Depend. 2022;232 doi: 10.1016/j.drugalcdep.2022.109341. [DOI] [PubMed] [Google Scholar]