Summary
Background
Parkinson's disease (PD) has become a public health concern with global ageing. However, comprehensive assessments of the temporal and geographical trend of PD disease burden in China remain insufficient. This study aimed to examine the burden of PD by age, gender, and geographical region in China during 1990–2021.
Methods
Using data from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2021, we analysed the incidence, prevalence, mortality, and DALY burden of PD in 33 Chinese provinces/regions. We compared the national figure with the global average and the corresponding estimates from the G20 countries. The estimated annual percentage change (EAPC) was used to quantify the temporal trends of PD burden during 1990–2021. We further assessed the PD burden by age and gender during 1990–2021. We used a decomposition analysis to investigate the changes in the number of new cases, patients, and deaths of PD during 1990–2021.
Findings
In 2021, China recorded the highest age-standardised incidence and prevalence of PD among the G20 countries, at 24.3 per 100,000 and 245.7 per 100,000, respectively, figures that were much higher than the global average. During 1990–2021, the age-standardised incidence of PD in China increased by 89.7%, and the age-standardised prevalence by 167.8%, both marking the largest increases among the G20 countries. In contrast, the age-standardised mortality for PD has significantly decreased since 1990, whereas the age-standardised DALY rate for PD has remained relatively unchanged since 1990. The PD burden gradually increased with age, especially in the elderly population aged ≥65 years. During 1990–2021, the burden in males consistently surpassed that in females, with the gender difference widening over time. The increase in new cases and patients of PD was primarily driven by changes in age-specific rates, while the rise in PD-related deaths was largely attributable to population ageing. The disease burden of PD varied considerably across the Chinese provinces. In 2021, age-standardised incidence and prevalence of PD were generally higher in China's southeastern coastal regions than in the western regions, and age-standardised DALY rates were higher in the northern regions than in other regions.
Interpretation
The disease burden of PD in China has consistently risen over the past three decades, particularly among elderly men. The increasing causative factors and population aging highlight the need for enhancing public health intervention and resource allocation, especially in etiological research, early diagnosis, preventive strategies, and region-specific management for PD.
Funding
Ministry of Science and Technology of the People's Republic of China (2022YFC2304900, 2022YFC2505100); National Key R&D Program of China (2022YFC2505100, 2022YFC2505103, 2018YFC1315300); Outstanding Young Scholars Support Program (grant number: 3111500001); Epidemiology modeling and risk assessment (grant number: 20200344), and Xi'an Jiaotong University Young Scholar Support Grant (grant number: YX6J004).
Keywords: Epidemiology, Parkinson's disease, Global burden of disease study, Incidence, Prevalence, Mortality, DALY
Research in context.
Evidence before this study
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2016 analysed the global burden of Parkinson's disease (PD) between 1990 and 2016, and showed that PD had become the fastest-growing brain disease in the world. We used keywords such as “Parkinson's disease”, “incidence”, “prevalence”, “mortality”, “DALY”, and “epidemiology” to search PubMed, Science Direct, Web of Science, and official websites of the Chinese Government and other institutions for studies and reports on PD in China published in English or Chinese until June 1, 2023. While previous studies have provided comprehensive national-level analyses of the PD burden in China, consistent and comparable assessments of temporal trends and regional differences at the provincial level have been lacking.
Added value of this study
Utilising the latest GBD 2021 data, this study provided a comprehensive assessment of the incidence, prevalence, mortality, and DALYs of PD in China and its provinces from 1990 to 2021, which offered a deeper understanding of the disease burden and epidemiological trends of PD among the Chinese population, contributing to the government's efforts in formulating more effective policies and allocating resources more rationally. Compared with the GBD 2016 study, the GBD 2021 China study incorporated major improvements in terms of expanded data sources, enhanced data accuracy, and improved model estimates.
Implications of all the available evidence
Our study reported the burden of PD in China and its provinces, emphasizing the importance of understanding epidemiological trends to guide medical and public health decision-making. Over the past three decades, the disease burden of PD in China has been consistently rising, especially among elderly men. Considering the complexity of PD pathogenesis, continuing research into etiological factors and therapeutic strategy development is crucial. Public health strategies should prioritise enhancing early diagnosis and prevention of PD, optimising the regional distribution of healthcare resources, and implementing effective environmental health policies. Additionally, rehabilitation and long-term care for PD patients deserve more attention.
Introduction
Parkinson's disease (PD), commonly observed in middle-aged and elderly populations, is pathologically characterised by the loss of dopaminergic neurons in the substantia nigra and the formation of Lewy bodies.1 This neural degeneration manifests not only in typical motor symptoms like resting tremor, bradykinesia, muscle stiffness, and abnormalities in posture and gait, but also in diverse non-motor symptoms, encompassing issues such as constipation, olfactory impairments, sleep disturbances, autonomic nervous dysfunction, and cognitive and psychiatric disorders.2 As the disease progresses, these symptoms worsen, greatly impacting patients' quality of daily life and functional activities. The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 estimated that over 8.5 million people worldwide suffer from PD.3 The World Health Organization (WHO) reported that in 2019, PD resulted in 5.8 million disability-adjusted life years (DALYs), an increase of 81% since 2000, and caused approximately 329,000 deaths, a more than 100% increase since 2000.4 PD has become the fastest-growing brain disease in the world.5 In response to this global challenge, the World Health Assembly endorsed the Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders 2022–2031.6 Additionally, the WHO released a technical brief on PD, outlining the global burden, treatment gaps and crucial action areas for PD.7
PD represents a significant public health concern in China. DALYs due to PD rank third out of all neurological disorders, next only to Alzheimer's disease and headache disorders.8 From 1990 to 2016, the age-adjusted prevalence of PD in China more than doubled, marking one of the largest increases worldwide.5 Although previous studies have provided comprehensive analyses at the national level regarding the burden of PD in China, detailed research on provincial differences and characteristics is still lacking.9, 10, 11, 12, 13 Most existing studies have been confined to specific cities or limited areas.10 Their relatively small sample sizes and methodological heterogeneity have impeded the broad comparability of statistical data. In recent years, China has undertaken several large-scale, cross-provincial studies on the prevalence of PD.12,13 However, these studies remained insufficient in providing comparative provincial-level data. Furthermore, epidemiological studies on PD incidence and mortality at the provincial level in China are even rarer.11 Given the significant socioeconomic and demographic changes in China over the past 30 years, it is crucial to monitor and understand the prevalence and trends of PD on a provincial scale to address this increasingly severe public health challenge.
Based on the most recent GBD 2021 data,8,14 our study provides a comprehensive assessment of the incidence, prevalence, mortality, and DALYs of PD in China and its provinces from 1990 to 2021. Our findings aim to provide essential information for government and health policymakers to identify priority areas for the prevention and control of PD, thereby facilitating more effective policy formulation and rational resource allocation.
Methods
Overview
This study analysed the burden of PD in China based on GBD 2021 data, covering a total of 33 provinces/regions, which includes all 31 mainland provinces, autonomous regions, municipalities, and the two special administrative regions of Hong Kong and Macao.8,14 GBD 2021 utilised a uniform and comparable method to comprehensively estimate the population, fertility, morbidity, and mortality for 204 countries and territories. Detailed information on this study can be found in GBD 2021.14
The National Centre for Chronic and Noncommunicable Disease Control and Prevention reviewed and approved this study. GBD 2021 complies with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations.15
Definitions
PD is a chronic, degenerative, and progressive neurological disorder typified by the loss of motor mobility and control, particularly tremors. The International Classification of Diseases tenth revision (ICD-10) codes for PD are G20, G21, and G22. According to GBD 2021, PD is defined by the presence of at least two of the following four primary symptoms: tremors or trembling, bradykinesia, stiffness of limbs and torso, and postural instability.
Data sources
Mortality data for PD in the GBD 2021 China study were mainly sourced from national disease surveillance point systems, death cause registration reporting systems, and maternal and child health surveillance websites. Data on non-fatal outcomes of PD were collected from population-based surveys and census data, as well as other published and unpublished studies and reports. Only data that met quality control criteria were included in the modelling estimation (Appendix p 1). Unlike most diseases in the Global Burden of Disease project, PD was characterised by marked discrepancies between the prevalence and cause-of-death data. Therefore, the GBD research team jointly modelled the mortality and morbidity estimates for PD to improve estimation accuracy. Further details can be found in the literature.3,5,14
Measures
The main outcome measures in our study were incidence, prevalence, mortality, years of life lost (YLLs), years lived with disability (YLDs), and DALYs associated with PD. The prevalence of a condition was defined as the proportion of the population with the condition at a specific time. All estimates were reported as counts per thousand and rates per 100,000 population. The 95% uncertainty interval (UI) was derived from the 2.5th and 97.5th percentiles of an ordered set of 1000 draws. GBD 2021 used HOEHN & YAHR stages to determine the severity of PD.16 YLDs were calculated by multiplying the prevalence of different severities by the corresponding disability weights. YLLs were calculated by multiplying the number of deaths in each age group by the remaining life expectancy in that age group. DALYs were the sum of YLLs and YLDs. Age-standardised populations were calculated by using the GBD world population age standard.
Data analysis
We analysed the age-standardised incidence, prevalence, mortality, and DALY rates of PD across China and its provinces in 2021, and then compared the estimates with the global average and the corresponding estimates of the Group of 20 (G20, an international economic cooperation forum composed of 20 major economies, from which we excluded the EU from our analysis and thus included only 19 countries). We used the estimated annual percentage change (EAPC) to quantify trends in PD burden from 1990 to 2021. A linear regression model was established to describe the relationship between time and the natural logarithm (ln) of the age-standardised rate: y = α + βx + ϵ, where y represents the ln (age-standardised rate), x is the calendar year, and ϵ is the error term. The EAPC was calculated using EAPC = 100 ×[exp(β)—1], with its 95% confidence interval (CI) derived from the regression model. An age-standardised rate is deemed statistically increasing if both the EAPC estimate and its 95% CI are greater than 0, and statistically decreasing if both are less than 0. If the EAPC estimate and its 95% CI include 0, the trend in the age-standardised rate is considered stable, indicating no significant change over time.
We further assessed the disease burden of PD by age and gender in China in 2021 as well as the trends in burden by gender from 1990 to 2021. Using the methodology developed by Das Gupta,17,18 we decomposed the changes in the number of new cases, patients, and deaths of PD in China and its provinces from 1990 to 2021 attributable to population growth, population structure, and age-specific rates. The observed net change in the total number of cases was equivalent to the combined changes in these three aspects. The decomposition analyses utilised counterfactual methods to calculate the number of cases. We first assumed that population growth was consistent with observations in 2021, while population structure and age-specific rates were consistent with 1990 (scenario one). We then assumed that both population growth and population structure were consistent with 2021, while age-specific rates were maintained at 1990 levels (scenario two). Consequently, the difference between the actual observed number of cases in 1990 and scenario one can be attributed to population growth; between scenario one and scenario two, to changes in population structure; and between scenario two and the actual observed cases in 2021, to shifts in age-specific rates. All analyses were performed using R software (version 4.3.1).
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study, and the corresponding author was responsible for the decision to submit for publication.
Results
In 2021, the age-standardised incidence rate of PD in China was the highest among the G20 countries, at 24.3 per 100,000 (95% UI 20.7–28.3), which was significantly higher than the global average of 15.6 per 100,000 (95% UI 14.0–17.4). From 1990 to 2021, the age-standardised incidence rate of PD in China increased by 89.7% (EAPC = 2.16%, 95% CI 2.10–2.21), representing the highest increase among the G20 countries and significantly exceeding the global average increase of 39.1% (EAPC = 1.09%, 95% CI 1.07–1.11). In terms of prevalence, the global average age-standardised prevalence of PD in 2021 was 138.6 per 100,000 (95% UI 123.1–157.6). However, in China, it reached 245.7 per 100,000 (95% UI 208.3–289.2), the highest among the G20 countries. The increase in the age-standardised prevalence of PD in China since 1990 was 167.8% (EAPC = 3.16%, 95% CI 3.03–3.30), significantly higher than that in Germany, which ranked second with an increase of 98.5% (EAPC = 2.11%, 95% CI 1.94–2.29). Based on EAPC, apart from Italy, Japan, and Russia, a general upward trend in age-standardised incidence and prevalence of PD was observed across the G20 countries (Table 1).
Table 1.
Age-standardised incidence, prevalence, mortality, and DALY rates of Parkinson's disease in 2021, and their percentage changes and EAPC from 1990 to 2021, 19 member countries of the G20 (the 20th member is the European Union) and the world.
 |
In 2021, the age-standardised mortality rate for PD in China was 5.0 per 100,000 (95% UI 4.2–5.9), ranking sixth among the G20 countries and close to the global average of 4.8 per 100,000 (95% UI 4.3–5.2). Contrary to the rising trends in incidence and prevalence, the age-standardised mortality rate for PD in China has shown a significant downward trend since 1990, with a decline of 17.7% (EAPC = −0.76%, 95% CI −0.93 to −0.60). In terms of disease burden, the age-standardised DALY rate for PD in China in 2021 was 108.0 per 100,000 (95% UI 91.1–125.5), ranking second highest among the G20 countries, following that in Saudi Arabia. However, compared to 1990, there was no significant change in the age-standardised DALY rate for PD in China. In 2021, the global age-standardised DALY rate for PD was 89.6 per 100,000 (95% UI 80.7–97.5), representing an increase of 9.9% (EAPC = 0.32%, 95% CI 0.28–0.36) from 1990 (Table 1).
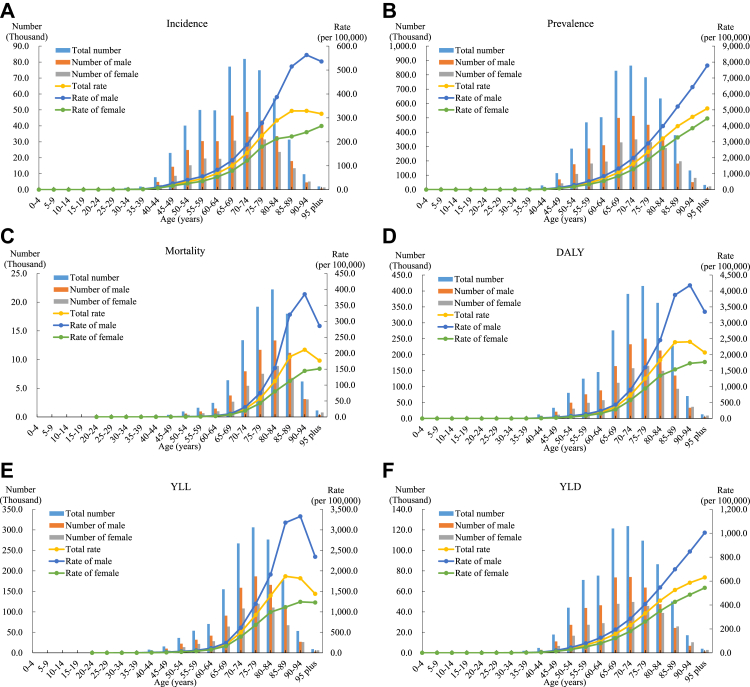
In 2021, there were 508.4 thousand new cases of PD in China, and the number of patients with PD was 5077.1 thousand. The incidence and prevalence rates of PD were 35.7 per 100,000 and 356.8 per 100,000, respectively (Fig. 1A and B). PD caused 92.0 thousand deaths, amounting to a mortality rate of 6.5 per 100,000 (Fig. 1C). PD also resulted in 2159.5 thousand DALYs, 1431.0 thousand YLLs, and 728.5 thousand YLDs in China. The DALY, YLL, and YLD rates for PD were 151.8 per 100,000, 100.6 per 100,000, and 51.2 per 100,000, respectively (Fig. 1D, E, F).
Fig. 1.
The incidence, prevalence, mortality, DALY, YLL, and YLD (in counts and crude rates) of Parkinson's disease by age and gender in China, 2021. DALY, disability-adjusted life-year; YLL, year of life lost; YLD, year lived with disability.
The incidence, prevalence, mortality, DALY, YLL, and YLD rates of PD in China in 2021 were all higher in males than in females. Starting from the age group of 20–24 years, the disease burden of PD gradually increased with age, especially in the elderly population aged 65 and above (Fig. 1). The number of new cases and patients of PD in each age group initially increased and then decreased, peaking at ages 70–74, while deaths peaked at ages 80–84. The prevalence of PD steadily rose with age, and the gender difference widened as age increased. The incidence and mortality rates of PD increased with age before declining, peaking in the 85–89 age group for incidence and in the 90–94 age group for mortality. The mortality rate of PD in females steadily increased with age, while in males aged 95 and above, there was a notable decline, yet it remained higher than that in females of the same age group (Fig. 1A–C). In 2021, the YLD rate due to PD increased with age, while the DALY and YLL rates peaked in the 85–89 age group before declining. Across all age groups for both males and females, starting from the 65–69 age group, the YLL burden due to PD was consistently twice as high as the YLD burden (Fig. 1D–F).
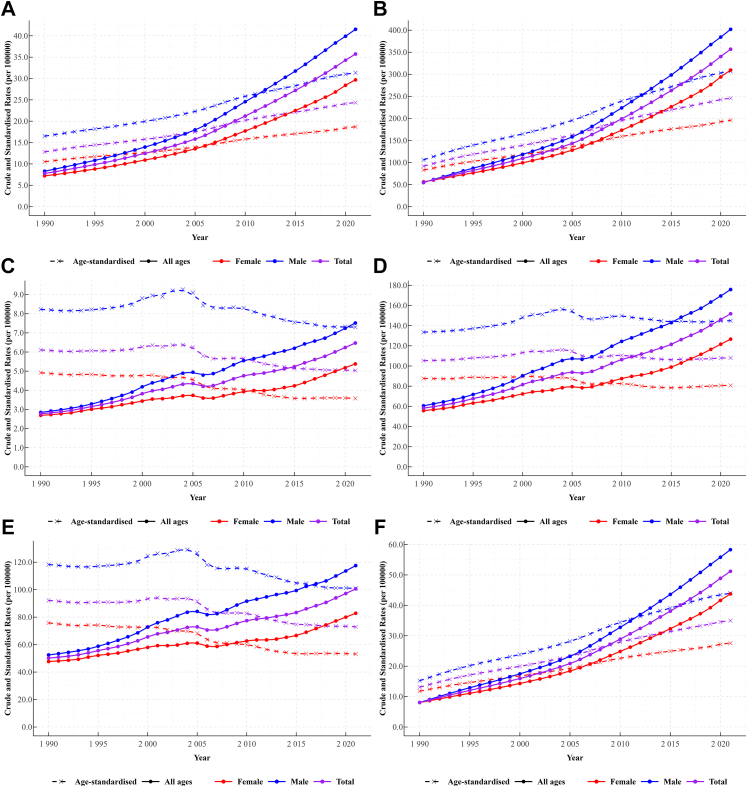
Fig. 2 showed that, from 1990 to 2021, the incidence, prevalence, mortality, DALY, YLL, and YLD rates of PD in China all followed a rising trend. The burden in males consistently surpassed that in females, with the gender difference widening over time. From the perspective of age-standardised rates, even after adjusting for population ageing, the age-standardised incidence and prevalence rates of PD continued to increase, while the age-standardised mortality rate initially rose slightly at 2000 before exhibiting a declining trend. For the disease burden caused by PD, the age-standardised YLL rate tended to decrease over time after an initial slight increase, while the age-standardised YLD rate continued to increase. The overall age-standardised DALY rate remained relatively stable over the past 30 years.
Fig. 2.
Temporal trends in crude and age-standardised rates of incidence, prevalence, mortality, DALY, YLL, and YLD for Parkinson's disease by gender in China from 1990 to 2021. DALY, disability-adjusted life-year; YLL, year of life lost; YLD, year lived with disability.
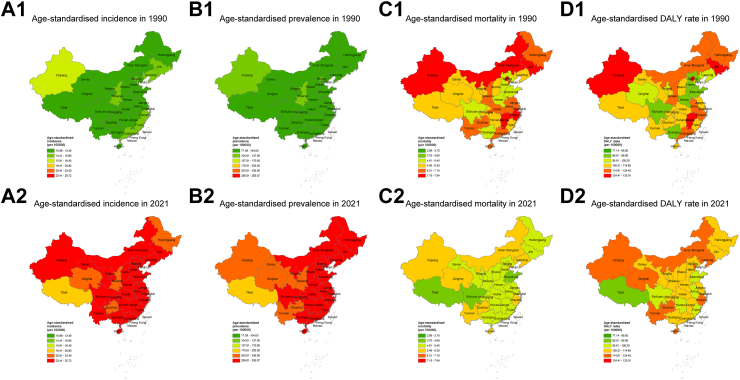
Regionally, from 1990 to 2021, there was a significant upward trend in the age-standardised incidence and prevalence rates of PD across all provinces in China (Fig. 3A and B, Appendix pp 2–4). In 2021, Fujian had the highest age-standardised incidence rate, followed by Zhejiang and Guangxi. Hong Kong, Zhejiang, Jiangsu, and Fujian had the highest age-standardised prevalence rates. In contrast, Tibet had the lowest age-standardised incidence and prevalence rates. Furthermore, the age-standardised incidence and prevalence rates of PD in the southeastern coastal regions of China were generally higher than those in the western regions. Since 1990, inland provinces, such as Henan, Hubei, Sichuan, and Chongqing, had a notably higher increase in age-standardised incidence and prevalence rates of PD compared to other areas.
Fig. 3.
Age-standardised incidence, prevalence, mortality, and DALY rates of Parkinson's disease by province in China, 1990 and 2021. DALY, disability-adjusted life-year.
Compared with 1990, a significantly decline in the age-standardised mortality rate of PD in 2021 was observed in most Chinese provinces, with the exceptions of Liaoning, Qinghai, Guangxi, and Hebei (Fig. 3C, Appendix pp 2–4). In 2021, age-standardised mortality rates for PD were higher in Zhejiang, Liaoning, Guizhou, and Qinghai, while those were the lowest in Macao, Hong Kong, and Tibet. Between 1990 and 2021, there were both increases and decreases in the age-standardised DALY rates of PD across the provinces in China (Fig. 3D, Appendix pp 2–4). In 2021, Zhejiang, Liaoning, and Qinghai had higher age-standardised DALY rates, with the lowest rates reported in Macao, Tibet, and Hong Kong. The age-standardised DALY rates for PD in the northern regions were higher than those in other areas.
The changes in the numbers of new cases, patients, and deaths of PD from 1990 to 2021 can be explained by population growth, population ageing, and changes in age-specific rates (Table 2). The number of new PD cases increased by 455.7%, with 20.9% attributed to population growth, 167.0% to population ageing, and 267.7% to increased age-specific incidence rates. The number of patients with PD increased by 678.9%, comprising 20.9% from population growth, 168.9% from population ageing, and 489.0% from increased age-specific prevalence rates. The number of PD deaths increased by 182.5%, with population growth contributing 20.9%, population ageing contributing 226.1%, and changes in age-specific mortality rates leading to a 64.6% decrease, which partially offset the overall increase. Changes in age-specific rates were the primary drivers for the increase in the number of new cases and patients of PD, while population ageing was the most important factor for the rise in PD deaths. Although the decline in age-specific mortality rates alleviated the increase in PD deaths, it could not completely counterbalance the combined effects of population growth and population ageing on the increase in PD deaths.
Table 2.
Decomposition of changes in the number of new cases, patients, and deaths (in thousands) of Parkinson's disease attributable to population growth, population ageing, and age-specific rates in China, 1990 and 2021.
| New cases | Patients | Deaths | |
|---|---|---|---|
| Observed number of people in 1990 | 91.5 | 651.8 | 32.6 |
| Number expected with 2021 population, 1990 population age structure, and 1990 rates | 110.6 | 788.3 | 39.4 |
| Number expected with 2021 population, 2021 population age structure, and 1990 rates | 263.5 | 1889.5 | 113.1 |
| Observed number of people in 2021 | 508.4 | 5077.1 | 92.0 |
| Percentage change from 1990 due to population growth | 20.9% | 20.9% | 20.9% |
| Percentage change from 1990 due to population ageing | 167.0% | 168.9% | 226.1% |
| Percentage change from 1990 due to change in age-specific rates | 267.7% | 489.0% | −64.6% |
| Observed percentage change from 1990 to 2021 | 455.7% | 678.9% | 182.5% |
Data are n or %, where n is in thousands.
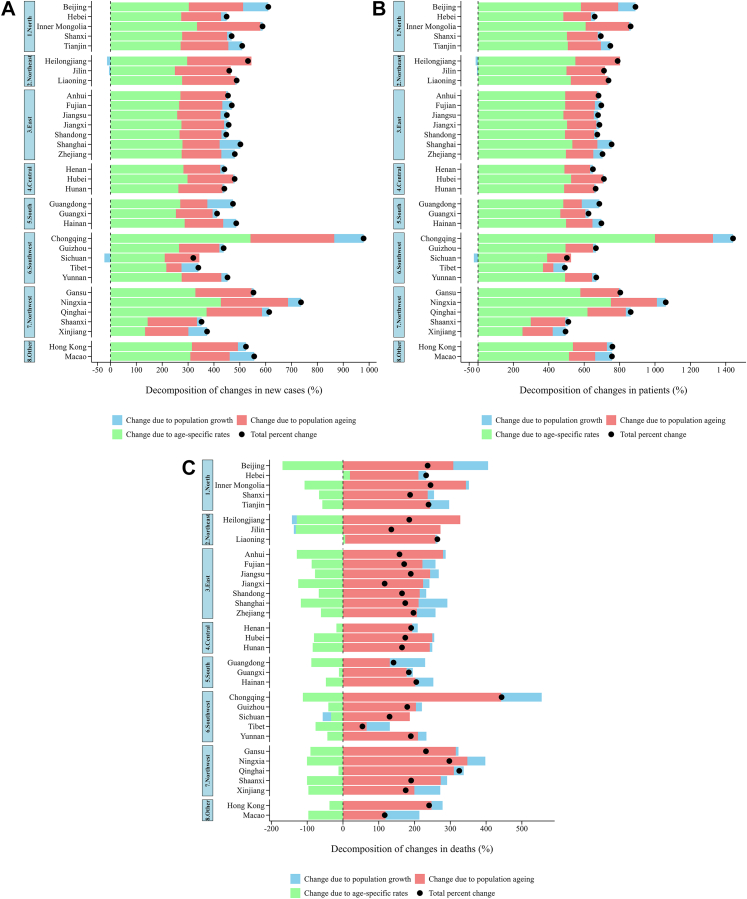
The decomposition of changes in the number of new cases, patients, and deaths of PD across Chinese provinces showed that population growth had a negative effect on PD in Sichuan, Heilongjiang, and Jilin, while all provinces experienced a positive impact on PD disease burden due to population ageing (Fig. 4, Appendix pp 5–7). The increase in age-specific rates was the key driver for the increase in the number of new cases and patients of PD in all provinces (Fig. 4A and B, Appendix pp 5 and 6). Regionally, intra-regional differences were smaller in the eastern and central areas, while larger internal disparities were observed within the southwest and northwest regions. Although all in the western region, the increase in age-specific prevalence rates contributed the most to the increase in the number of PD patients in Chongqing, Ningxia, and Qinghai, while its impact was relatively smaller in other western regions such as Xinjiang, Shaanxi, Tibet, and Sichuan. Population ageing was the main factor contributing to the increase in the number of PD deaths across all provinces (Fig. 4C, Appendix p 7). The increase in population ageing contributed the most to the increase in PD deaths in Chongqing, followed by Ningxia and Inner Mongolia, with the least impact in Tibet. It is noteworthy that only the age-specific mortality rates in Hebei and Liaoning contributed positively to the increase in the number of local PD deaths, while that in other provinces mitigated the increase in the number of local PD deaths to some extent.
Fig. 4.
Decomposition of changes in the number of new cases, patients, and deaths of Parkinson's disease attributable to population growth, population ageing, and age-specific rates by province in China, 1990 and 2021. We divided China into the following geographical regions (excluding Taiwan): 1. North: Beijing, Hebei, Inner Mongolia, Shanxi, Tianjin; 2. Northeast: Heilongjiang, Jilin, Liaoning; 3. East: Anhui, Fujian, Jiangsu, Jiangxi, Shandong, Shanghai, Zhejiang; 4. Central: Henan, Hubei, Hunan; 5. South: Guangdong, Guangxi, Hainan; 6. Southwest: Chongqing, Guizhou, Sichuan, Tibet, Yunnan; 7. Northwest: Gansu, Ningxia, Qinghai, Shaanxi, Xinjiang; 8. Other: Hong Kong, Macao.
Discussion
This study provided a comprehensive analysis of the PD burden in China from 1990 to 2021, revealing epidemiological trends and regional disparities, which are crucial for informing public health policies and resource allocation. We found that in 2021, China had the highest age-standardised incidence and prevalence of PD among the G20 countries (except the EU), with an increase from 1990 that was also the most significant and far exceeded the global average. The age-standardised mortality rate for PD in China has significantly declined compared to 1990, but the overall age-standardised DALY has not shown noticeable change. The increase in causative factors was the primary driver of the increase in the number of new PD cases and patients, while population ageing was the most important factor contributing to the increase in deaths associated with PD. Considering the rapid economic development and accelerated population ageing,19 the disease burden caused by PD in China is becoming increasingly heavy and requires more public health attention.
Previous studies had predicted that the number of PD patients in China would reach approximately 5 million by 2030, accounting for more than half of the global PD population.20 However, our research indicated that this figure had already been exceeded in 2021, reaching 5.08 million. Compared with 1990, the number of new cases and patients of PD in China had increased by 455.7% and 678.9%, respectively. This study found that the increase in the incidence and prevalence of PD was largely attributable to the accumulation of causative factors. The occurrence of PD has been confirmed to be mainly due to the degeneration and death of substantia nigra dopaminergic neurons. However, there is no clear evidence for the mechanism of neuronal degeneration and death.21,22 In addition to the immutable genetic and population ageing factors, agricultural and industrial toxins in environmental factors might be important changeable factors.11,23 Previous studies showed that pesticides ingested through agricultural use and food preservative residues might lead to various neurodegenerative diseases, including PD.24 Epidemiological studies also found that people frequently exposed to pesticides or herbicides had a significantly higher risk of PD.25 China is one of the largest producers of pesticides in the world. Although the Zero Growth Action of Fertilizer and Pesticide Use has been carried out recently, pesticide abuse is still widespread.26,27 In addition, the influence of heavy metals and industrial solvents on PD cannot be ignored.28 Studies have shown that people living in urban areas with high industrial metal emissions had a higher incidence of PD.29 Since the reform and opening up, with the development of the socialist market economic system, the industrialisation process in China has developed rapidly, and pesticide production has also become more diversified.30 Some studies have suggested that improved environmental health policies and land use planning have great potential for the prevention of PD.31 Furthermore, there is growing evidence of a negative correlation between smoking and the risk of PD.32,33 The prevalence of smoking in the Chinese population has been high,34 but its potential benefits to PD are insufficient to offset its harmful effects on health. Hence, it is important to strengthen epidemiological studies targeting risk and protective factors for PD in the Chinese population, especially in identifying and managing modifiable risk factors, in order to accumulate more epidemiological evidence to guide etiological control and risk management.
Different from the rising trend of age-standardised mortality of PD in other countries, the age-standardised mortality in China decreased from 1990 to 2021, but was still close to the global average. This might be attributed to the improvement of medical conditions in China in recent years, particularly the advancement in the knowledge about and the treatment protocols for PD.35,36 It is worth noticing that most patients with PD do not die directly from PD, but instead, complications such as lung infection caused by PD or accidental injuries such as falls may increase the risk of death in patients with PD to a certain extent.37,38 Therefore, it is important to pay attention to the prevention and treatment of the complications of PD as well.
DALY reflects the total healthy life years lost from disease onset to death. While the total age-standardised DALY rates in China have remained relatively stable over the past 30 years, the age-standardised YLD rates have been increasing, reflecting a gradual increase in the burden of disability due to PD. Patients with PD typically present with motor symptoms such as bradykinesia, resting tremor, muscle stiffness, postural gait disturbance, and non-motor symptoms such as cognitive-emotional disturbance, sleep disturbance, pain, and fatigue, which may occur sequentially or simultaneously,2,35 severely affecting the patient's working ability and quality of life. PD-related dysfunction and reduced quality of life become increasingly important health issues as patients' survival time increases. As PD is a chronic neurodegenerative disease with no current cure, existing treatments focus on symptomatic therapy to alleviate disease symptoms.21 Long-term rehabilitative therapy and nursing care are crucial for improving the self-care ability and quality of life of PD patients. Meanwhile, the development of new treatments and drugs is also important for improving the quality of life of patients. Currently, the treatment of PD mainly relies on drug therapy centred on dopamine metabolism, supplemented by deep brain electrical stimulation and surgical therapy.39 In recent years, China has also made some progress in the development of new therapies and effective drugs for PD.40 Therefore, continuing to increase financial support for basic and clinical research on PD is essential, which will deepen our understanding of PD's pathogenesis and promote the development of novel therapeutic approaches, such as gene therapy and cell therapy, providing more therapeutic options for PD patients.
In 2021, there were many new cases of PD in China between the ages of 50 and 85, accounting for about 85% of the total number of new cases. For people under 90 years of age, age is an obvious influencing factor in the risk of PD. The incidence, prevalence, or mortality of PD all increased with age, especially in the population aged 65 years and older. This was consistent with the findings of other countries.41,42 The decline in the death burden after the age of 90 might be due to underdiagnosis or the presence of other fatal complications.5 In terms of gender, the disease burden of PD in males of all ages in China was higher than that in females. Moreover, for people under 90 years old, the gender difference grew wider with the increase of age. A national study in France also found this age-dependent relationship between PD and gender, the mechanism of which remained unclear.43 Potential mechanisms such as the role of the X chromosome in PD, more frequent occupational exposure in males, or the neuroprotective effect of estrogen in females have been suggested but still need to be further studied.44
Improving health equity and reducing health inequalities among regions have long been important policy objectives of the Chinese government.45 However, precise guidance of public health investments and resource allocation at the provincial level can only be achieved by basing these investments on adequate and detailed health data information. To address this need, we focused on analysing the disease burden of PD across different provinces in China. Our study indicated that although the age-standardised incidence and prevalence of PD across all regions of China showed a significant upward trend, the disease burden varied considerably across provincial-level areas. In 2021, the age-standardised incidence and prevalence of PD were higher in the southeastern coastal regions than in the western regions. Nevertheless, with the exception of Zhejiang, the age-standardised mortality and DALY rates of PD were generally lower in most eastern regions than in central and western regions. This might be due to the higher levels of economic, industrial, and agricultural development in the eastern regions, which might be accompanied by more severe environmental pollution, leading to a higher incidence of PD.46 In contrast, the economic development of the southeastern coastal region also brings more adequate medical resources and higher public health awareness, potentially promoting early diagnosis and timely treatment of PD, thereby improving the prognosis of patients. Additionally, high-level medical services and health management have also helped patients to better control their disease and slow down its progression to a certain extent, reducing the mortality rate. In Zhejiang, the age-adjusted prevalence and mortality burden of PD have remained consistently high from 1990 to 2021. The precise mechanisms underlying this trend are not yet clear. Region-specific genetic factors might provide a possible explanation,47 but further research is needed. In terms of changes in the number of patients and deaths due to PD, the intraregional disparities in China's eastern and central regions were relatively small, whereas those in the southwestern and northwestern regions were apparently larger. Particularly in the western region, the increase in causative factors contributed the most to the increase in the number of patients with PD in Chongqing, Ningxia, and Qinghai, but had relatively lesser impact in other western regions such as Xinjiang, Shaanxi, Tibet, and Sichuan. This suggests that even within regions with similar geographical and economic conditions, the epidemiological patterns and influencing factors of PD might still exhibit apparent differences. These differences might result from a combination of factors specific to each area, such as environment, genetics, medical resources, and public health strategies. Therefore, conducting in-depth epidemiological surveys in targeted areas to obtain more detailed and specific regional data is key to unravelling the mechanisms behind the regional differences in PD, as well as to understanding and responding to this uneven distribution. This will provide more evidence to support the government in adopting more precise preventive and control measures in accordance with local conditions.
This study has several limitations. First, data within each iteration of GBD were comparable, but due to inherent limitations in the GBD methodology, results from different iterations, even for the same year, were not comparable. Differences in the GBD outcomes between iterations could be attributed to updates in data sources and improvements in methodology. Second, GBD 2021 mainly estimated the disease burden of PD through all available provincial-level data and previous literature in China. Unfortunately, high-quality epidemiological studies on PD in China were very limited, especially in some provinces with a lack of relevant data, which might introduce some bias in the model's estimation. Third, since 1990, changes in screening and diagnosis methods, as well as a better understanding of PD by patients and physicians, might have led to an increase in the reporting rate of PD, which could potentially impact the analysis of PD incidence trends. Fourth, although this study set the minimum onset age for PD at 20 years, the overall burden was measured based on the entire population, which might underestimate the actual burden of PD in the middle-aged and older population to some extent. Furthermore, this study did not adequately consider the overlap between atypical Parkinsonism and idiopathic PD when analysing the epidemiological trends of PD, which could lead to a biased estimation of the disease burden of PD. Therefore, current epidemiological findings on PD need to be interpreted with caution and further validated in future research.
In conclusion, the disease burden of PD in China has been consistently rising over the past three decades, particularly among elderly men. Considering the complexity of PD pathogenesis, the focus of current research should be on the etiological research and the development of therapeutic strategies. Public health strategies need to enhance early diagnosis and prevention of PD, as well as optimise the regional distribution of healthcare resources and implement effective environmental health policies. Research on the epidemiology of PD in the Chinese population should be strengthened, particularly focusing on differentiated management and precise prevention and control strategies for various regions, genders, and age groups. Meanwhile, rehabilitation and long-term care for PD patients require greater attention to improve patients' quality of life and reduce the burden on society and the healthcare system.
Contributors
TX, and MZ conceived the ideas for this research and provided overall guidance.
TX, ZW, LZ, and MZ prepared the first draft and finalised the manuscript based on comments from all other authors.
All other authors contributed to the analysis and approved the manuscript.
Data sharing statement
To download GBD data used in the analyses in this article please visit the Global Health Data Exchange GBD 2021 website.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
We declare no competing interests.
Acknowledgements
This study was supported by the Ministry of Science and Technology of the People's Republic of China (2022YFC2304900, 2022YFC2505100); National Key R&D Program of China (2022YFC2505100, 2022YFC2505103, 2018YFC1315300); Outstanding Young Scholars Support Program (grant number: 3111500001); Epidemiology modeling and risk assessment (grant number: 20200344), and Xi’an Jiaotong University Young Scholar Support Grant (grant number: YX6J004).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2024.101078.
Contributor Information
Lei Zhang, Email: lei.zhang1@monash.edu.
Maigeng Zhou, Email: maigengzhou@126.com.
Appendix A. Supplementary data
References
- 1.Kalia L.V., Lang A.E. Parkinson's disease. Lancet. 2015;386(9996):896–912. doi: 10.1016/S0140-6736(14)61393-3. [DOI] [PubMed] [Google Scholar]
- 2.Leite Silva A.B.R., Gonçalves de Oliveira R.W., Diógenes G.P., et al. Premotor, nonmotor and motor symptoms of Parkinson's disease: a new clinical state of the art. Ageing Res Rev. 2023;84 doi: 10.1016/j.arr.2022.101834. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Global health estimates: leading causes of DALYs. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/global-health-estimates-leading-causes-of-dalys
- 5.GBD 2016 Parkinson’s disease Collaborators Global, regional, and national burden of Parkinson’s disease, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2018;17(11):939–953. doi: 10.1016/S1474-4422(18)30295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization Intersectoral global action plan on epilepsy and other neurological disorders. https://www.who.int/publications/i/item/9789240076624
- 7.World Health Organization . World Health Organization; Geneva: 2022. Parkinson disease: a public health approach. Technical brief. [Google Scholar]
- 8.Institute for Health Metrics and Evaluation Global health data exchange. https://ghdx.healthdata.org/
- 9.Zheng Z., Zhu Z., Zhou C., et al. Burden of Parkinson disease in China, 1990-2019: findings from the 2019 global burden of disease study. Neuroepidemiology. 2023;57(1):51–64. doi: 10.1159/000527372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li G., Ma J., Cui S., et al. Parkinson's disease in China: a forty-year growing track of bedside work. Transl Neurodegener. 2019;8:22. doi: 10.1186/s40035-019-0162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim S.Y., Tan A.H., Ahmad-Annuar A., et al. Parkinson's disease in the western pacific region. Lancet Neurol. 2019;18(9):865–879. doi: 10.1016/S1474-4422(19)30195-4. [DOI] [PubMed] [Google Scholar]
- 12.Qi S., Yin P., Wang L., et al. Prevalence of Parkinson's disease: a community-based study in China. Mov Disord. 2021;36(12):2940–2944. doi: 10.1002/mds.28762. [DOI] [PubMed] [Google Scholar]
- 13.Song Z., Liu S., Li X., et al. Prevalence of Parkinson's disease in adults aged 65 years and older in China: a multicenter population-based survey. Neuroepidemiology. 2022;56(1):50–58. doi: 10.1159/000520726. [DOI] [PubMed] [Google Scholar]
- 14.GBD 2021 Demographics Collaborators Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950-2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the global burden of disease study 2021. Lancet. 2024;S0140-6736(24):00476–00478. doi: 10.1016/S0140-6736(24)00476-8. [DOI] [PubMed] [Google Scholar]
- 15.Stevens G.A., Alkema L., Black R.E., et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388(10062):e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 16.Hoehn M.M., Yahr M.D. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427–442. doi: 10.1212/wnl.17.5.427. [DOI] [PubMed] [Google Scholar]
- 17.Das Gupta P. US Bureau of the Census; Washington, DC: 1993. Standardization and decomposition of rates: a user's manual. [Google Scholar]
- 18.Xu T., Wang B., Liu H., et al. Prevalence and causes of vision loss in China from 1990 to 2019: findings from the global burden of disease study 2019. Lancet Public Health. 2020;5(12):e682–e691. doi: 10.1016/S2468-2667(20)30254-1. [DOI] [PubMed] [Google Scholar]
- 19.Fang E.F., Scheibye-Knudsen M., Jahn H.J., et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24(Pt B):197–205. doi: 10.1016/j.arr.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dorsey E.R., Constantinescu R., Thompson J.P., et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68(5):384–386. doi: 10.1212/01.wnl.0000247740.47667.03. [DOI] [PubMed] [Google Scholar]
- 21.Bloem B.R., Okun M.S., Klein C. Parkinson's disease. Lancet. 2021;397(10291):2284–2303. doi: 10.1016/S0140-6736(21)00218-X. [DOI] [PubMed] [Google Scholar]
- 22.Masato A., Plotegher N., Boassa D., et al. Impaired dopamine metabolism in Parkinson's disease pathogenesis. Mol Neurodegener. 2019;14(1):35. doi: 10.1186/s13024-019-0332-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ascherio A., Schwarzschild M.A. The epidemiology of Parkinson's disease: risk factors and prevention. Lancet Neurol. 2016;15(12):1257–1272. doi: 10.1016/S1474-4422(16)30230-7. [DOI] [PubMed] [Google Scholar]
- 24.Kamel F., Hoppin J.A. Association of pesticide exposure with neurologic dysfunction and disease. Environ Health Perspect. 2004;112(9):950–958. doi: 10.1289/ehp.7135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanner C.M., Kamel F., Ross G.W., et al. Rotenone, paraquat, and Parkinson's disease. Environ Health Perspect. 2011;119(6):866–872. doi: 10.1289/ehp.1002839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ministry of Agriculture and Rural Affairs of the people's Republic of China Notice of the Ministry of agriculture and rural affairs on printing and distributing the action plan for Zero growth of fertilizer use by 2020 and the action plan for Zero growth of pesticide use by 2020. http://www.moa.gov.cn/nybgb/2015/san/201711/t20171129_5923401.htm
- 27.Sun S., Hu R., Zhang C., et al. Do farmers misuse pesticides in crop production in China? Evidence from a farm household survey. Pest Manag Sci. 2019;75(8):2133–2141. doi: 10.1002/ps.5332. [DOI] [PubMed] [Google Scholar]
- 28.De Miranda B.R., Goldman S.M., Miller G.W., et al. Preventing Parkinson's disease: an environmental agenda. J Parkinsons Dis. 2022;12(1):45–68. doi: 10.3233/JPD-212922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Willis A.W., Evanoff B.A., Lian M., et al. Metal emissions and urban incident Parkinson disease: a community health study of Medicare beneficiaries by using geographic information systems. Am J Epidemiol. 2010;172(12):1357–1363. doi: 10.1093/aje/kwq303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang X., Wang F., Luo H. Spatio-temporal characteristics of environment pollution of China from 1978 to 2018: a study using news reports from the people's Daily. Geogr Res. 2021;40(4):1134–1145. [Google Scholar]
- 31.Yuchi W., Sbihi H., Davies H., et al. Road proximity, air pollution, noise, green space and neurologic disease incidence: a population-based cohort study. Environ Health. 2020;19(1):8. doi: 10.1186/s12940-020-0565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mappin-Kasirer B., Pan H., Lewington S., et al. Tobacco smoking and the risk of Parkinson disease: a 65-year follow-up of 30,000 male British doctors. Neurology. 2020;94(20):e2132–e2138. doi: 10.1212/WNL.0000000000009437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang C., Zhou C., Guo T., et al. Association between cigarette smoking and Parkinson's disease: a neuroimaging study. Ther Adv Neurol Disord. 2022;15 doi: 10.1177/17562864221092566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang M., Luo X., Xu S., et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7(1):35–45. doi: 10.1016/S2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 35.Chinese Society of Parkinson's Disease and Movement Disorders Parkinson's disease and movement disorder section of neurologist branch of Chinese medical doctor association. Chinese guidelines for the treatment of Parkinson's disease (fourth edition) Chin J Neurol. 2020;53(12):973–986. [Google Scholar]
- 36.Nan H.T., Chen H.B., Li S.H., et al. Effect of Parkinson's disease treatment guideline on medicine treatment. Chin J Geriatr. 2014;33(9):937–940. [Google Scholar]
- 37.Xu J., Gong D.D., Man C.F., et al. Parkinson's disease and risk of mortality: meta-analysis and systematic review. Acta Neurol Scand. 2014;129(2):71–79. doi: 10.1111/ane.12201. [DOI] [PubMed] [Google Scholar]
- 38.Karceski S. Parkinson disease and mortality: understanding how the two are connected. Neurology. 2018;91(22):e2106–e2108. doi: 10.1212/WNL.0000000000006565. [DOI] [PubMed] [Google Scholar]
- 39.Poewe W., Seppi K., Tanner C.M., et al. Parkinson disease. Nat Rev Dis Primers. 2017;3 doi: 10.1038/nrdp.2017.13. [DOI] [PubMed] [Google Scholar]
- 40.Chen Y., Hong Z., Wang J., et al. Circuit-specific gene therapy reverses core symptoms in a primate Parkinson's disease model. Cell. 2023;186(24):5394–5410.e18. doi: 10.1016/j.cell.2023.10.004. [DOI] [PubMed] [Google Scholar]
- 41.Pringsheim T., Jette N., Frolkis A., et al. The prevalence of Parkinson's disease: a systematic review and meta-analysis. Mov Disord. 2014;29(13):1583–1590. doi: 10.1002/mds.25945. [DOI] [PubMed] [Google Scholar]
- 42.Brakedal B., Toker L., Haugarvoll K., et al. A nationwide study of the incidence, prevalence and mortality of Parkinson's disease in the Norwegian population. NPJ Parkinsons Dis. 2022;8(1):19. doi: 10.1038/s41531-022-00280-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moisan F., Kab S., Mohamed F., et al. Parkinson disease male-to-female ratios increase with age: French nationwide study and meta-analysis. J Neurol Neurosurg Psychiatry. 2016;87(9):952–957. doi: 10.1136/jnnp-2015-312283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cerri S., Mus L., Blandini F. Parkinson's disease in women and men: what's the difference? J Parkinsons Dis. 2019;9(3):501–515. doi: 10.3233/JPD-191683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.The State Council of the People’s Republic of China The "healthy China 2030" planning outline. https://www.gov.cn/zhengce/2016-10/25/content_5124174.htm
- 46.Sing T.F., Wang W., Zhan C. Tracking industry pollution sources and health risks in China. Sci Rep. 2023;13(1) doi: 10.1038/s41598-023-49586-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zheng Z., Qiu C., Zheng Z., et al. Studies of mutations and polymorphism of PINK1 gene in patients with Parkinson's disease in littoral of Zhejiang Province. Chin J Neurol. 2012;45(8):581–585. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.