Abstract
Background
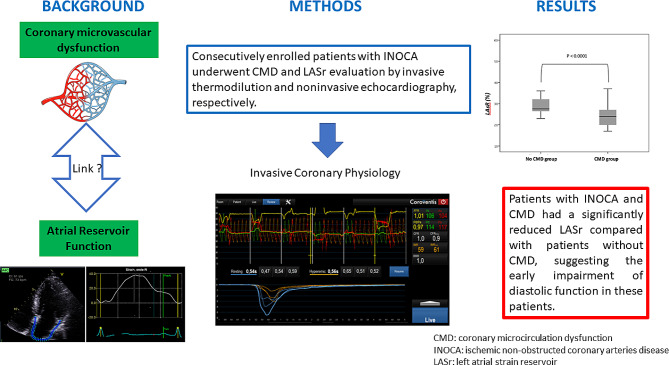
Coronary microvascular dysfunction (CMD) refers to structural and functional abnormalities of the coronary microcirculation, which may be diagnosed using invasive coronary physiology. CMD is responsible for impaired diastolic cardiac function. It has recently been suggested that left atrial strain (LASr) represents a highly sensitive tool for detecting cardiac diastolic function abnormalities. Accordingly, the aim of this study was to investigate the relationship between CMD and LASr.
Methods
Consecutively enrolled patients with non-obstructed coronary arteries (NOCA) underwent CMD and LASr evaluation by invasive thermodilution and noninvasive echocardiography, respectively.
Results
Forty-two (42) patients were included, out of which 26 presented with CMD. There were no significant differences between CMD-positive and negative patients in terms of clinical and echocardiographic characteristics. LASr was significantly reduced in patients with CMD (24.6% ± 6.1 vs. 30.3 ± 7.8%, p = 0.01). A moderate correlation was observed between coronary flow reserve and LAsr (r = 0.47, p = 0.002). A multivariate logistic regression analysis demonstrated that CMD was independently associated with LASr (OR = 0.88, 95%CI 0.78–0.99.135, p = 0.04). A LASr cut-off of 25.5% enabled an optimal classification of patients with or without CMD.
Conclusion
Patients with NOCA and CMD had a significantly reduced LASr compared with patients without CMD, suggesting the early impairment of diastolic function in these patients.
Keywords: Coronary microvascular dysfunction, Left atrial strain reservoir
Introduction
Coronary microvascular dysfunction (CMD) corresponds to structural and/or functional damage to small (< 400 μm) coronary vessels. Patients with CMD experience a reduction in coronary flow reserve, leading to abnormal flow at rest or an altered coronary response to stress. Recent studies reported that 47–60% of patients with typical angina-like symptoms and no significant epicardial lesions according to coronary angiography have CMD [1, 2]. The diagnosis of CMD has been standardized based on clinical criteria and invasive and/or non-invasive imaging tests [3, 4]. Studies have shown that CMD is associated with an increased incidence of cardiovascular events including myocardial infarction, stroke and hospitalization for heart failure [1]. The role of CMD in heart failure with preserved ejection fraction (HFpEF) has also recently been described by a number of studies, including its role in the development of diastolic disorders characterizing this pathology [5–7].
Technological advances in echocardiography allow the analysis of myocardial contraction and deformation through left atrial strain (LAS). LAS allows the assessment of all three aspects of left atrial function, namely reservoir (LASr), conduit and pump [8–10]. The LASr technique is robust, easy to use, has low intra- and inter-observer variation [11, 12], and is used in a variety of cardiac pathologies [10–12]. LASr is now proposed as part of the algorithm used for the assessment of left ventricular filling pressures [8, 13]. It is also considered as a prognostic biomarker, especially in atrial fibrillation where it indicates the probability of success of an external electric shock, and it is a predictive factor for stroke [12, 14–16].
The aim of this study was to analyze the relationship between LASr and CMD as assessed by invasive coronary physiology.
Methods
Study population
The present prospective and single-centered study recruited consecutive patients referred for coronary angiography upon clinically appropriate indications (ClinicalTrials.gov identifier: NCT04560829). The study included men and women with chest pain suggestive of angina and/or positive ischemic test and non-obstructed coronary arteries (NOCA), who underwent invasive coronary physiology studies between September 2020 to June 2023. Exclusion criteria were (a) contraindications to adenosine (asthma, second or third-degree AV block or sick sinus syndrome without a pacemaker, methyl xanthenes medication within the last 12 h prior to the test, and known hypersensitivity to adenosine); (b) previous percutaneous coronary intervention or coronary artery bypass graft surgery; (c) previous myocardial infarction; (d) pregnancy; (e) low ejection fraction < 50%; (f) known cardiomyopathy or severe valvular disease; (g) coronary stenosis > 50% or fractional flow reserve (FFR) < 0.8. A total of 42 patients satisfied the inclusion criteria (Fig. 1) and constituted the final study population. The institutional review board approval was obtained as per current regulations. The sponsor of the trial was our University Hospital. The study protocol was in accordance with the Declaration of Helsinki.
Fig. 1.
Flow Chart. TTE: Trans-Thoracic echocardiography
Invasive coronary physiology
Selective conventional invasive coronary angiography (ICA) was performed using standard techniques using the Judkins technique and a radial approach with 6-French catheters (Philips Allura Xper FD10, Philips Healthcare). After selection of patients with no stenosis > 50% by angiography, left ventriculography, as ultrasound was performed after the invasive examination, was performed to ensure that there is no alteration of the left ejection fraction, and that there are no abnormalities in filling (N ≤ 10 mmHg) in accordance of the expert consensus [4]. This process it is important because Many patients with HFpEF would fulfil these criteria: dyspnoea, no obstructive CAD and impaired CFR. FFR, CFR and IMR were determined mainly on the left anterior descending artery (LAD). The IMR was assessed using a coronary pressure wire (PressureWire X, Abbott, IL, USA) at maximal hyperemia induced by intravenous adenosine (140 µg/kg/min). The coronary pressure wire was flushed. Following calibration to zero pressure, the coronary pressure wire was equalized to the guide catheter pressure with the sensor positioned at the ostium of the coronary artery. The pressure sensor was then positioned at the distal segment of a target vessel, and intracoronary nitrate (100 or 200 mg) was administered before each measurement. Resting mean transit time (Tmn) was obtained in triplicate by rapid intracoronary manual administrations of a 3 mL bolus of saline at room temperature. Hyperemia was induced by intravenous adenosine (140 µg/kg/min) during at least 3 min via a peripheral or central vein. Hyperemic mean aortic pressure (Pa), distal intracoronary pressure (Pd), and hyperemic Tmn were measured in triplicate during sustained hyperemia. FFR was calculated as the mean Pd – to - mean Pa ratio. CFR was calculated as the resting-to-hyperemic Tmn ratio and IMR was calculated as Pd*hyperemic Tmn. When the pressure sensor was pulled back in the guiding catheter, both pressures were checked to exclude any drift of the transducers. A final aortic-to-distal pressure difference within ± 2 mmHg was considered acceptable. Normalization and physiological assessment were repeated for larger pressure offsets. Patients were classified into the reference group (CFR ≥ 2.5), functional CMD group (CFR < 2.5; IMR < 25), or structural CMD group (CFR < 2.5; IMR ≥ 25) [17].
Echocardiography
All patients benefited from a standard echocardiographic examination using a commercially available machine (Vivid E95, General Electric Medical Systems, Horten, Norway) and a 2.5 MHz transducer. Images were acquired in the left lateral decubitus position. Blood pressure was recorded using a digital blood pressure monitor with a brachial cuff. A complete M-mode and two-dimensional gray scale echocardiography, including the 3 standard apical views (4, 3 and 2 chambers) using high frame rates (> 60 frames/s), were performed for each patient. All echocardiographic data were synchronized to the electrocardiogram. Image analysis was independently performed by a single blinded observer unaware of coronary status. The following measurements were recorded according to the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACVI) guidelines [18]: LV end-diastolic and end-systolic volumes and ejection fraction using Simpson’s biplane method from apical 2- and 4-chamber views, left atrial volume index using a biplane area-length formula at end-systole. LV diastolic function was evaluated with E/e’ ratio, derived from the pulsed wave tissue Doppler images (TDI) at the lateral mitral annulus. Tricuspid annular plane systolic excursion was evaluated by applying M-mode in the apical 4-chamber view and used as a measure of RV systolic function. Systolic pulmonary artery pressure was estimated as the sum of the peak tricuspid regurgitation and right atrium pressure derived from the inferior vena cava diameter and inspiratory collapse. Color Doppler and pulsed wave Doppler were used to explore for the presence of valvular regurgitation, while continuous wave Doppler was used to quantify valvular stenosis obstruction. Commercially available software (EchoPAC PC version 203; GE Medical Systems, Milwaukee, WI, United States) with a speckle-tracking technology was used to measure LASr. As recommended by the European Association of Cardiovascular Imaging and the American Society of Echocardiography task force for deformation imaging, strain was evaluated on a non-foreshortened apical 4-chamber view with zero reference set at end-diastole (i.e., R-R gating) [19]. The LA endocardial border was automatically drawn followed by manual adjustment if required.
Statistics
Continuous variables are expressed as mean +/- SD for normally distributed variables and as median (25th–75th percentile) for non-normally distributed variables. Discontinuous variables were presented as percentages. Data comparisons between the two patient groups were carried out for continuous variables using a Student’s t-test for parametric series, or a non-parametric Mann-Whitney test in the case of non-normal distributions and using Chi 2 or Fischer test for discrete variables. Pearson’s correlation coefficient was used for bivariate correlation analysis. Univariate and multivariate logistic regression analyses were used to quantify the association between CMD and the independent variables using odds ratios (OR) and 95% confidence intervals (CIs). Factors clinically recognized risk factors were included in the multivariate analysis (age, high blood pressure, body weight Index, diabetes, smoker). ROC curve analysis was used to assess the ability of LASr to predict CMD. Coefficient of variation was used to determine the variablity of data. The intra-observer and inter-observer variabilities of LASr measurements were quantified by calculating the intra-class correlation coefficient (ICC). Inter-observer variability was assessed using a two-way randomized single-measure ICC analysis. Intra-observer variability was assessed using a one-way random two-measure ICC analysis. For all statistical tests, the alpha threshold was set at 5%. Statistical analysis and graphs were performed using SPSS 24.0 (IBM Software).
Results
A total of 42 patients were included in the analysis, out of which 26 had CMD, while the remaining 16 were free of microcirculatory involvement. Clinical parameters were comparable between the two groups, with a majority of women in both. Population characteristics are summarized in Table 1. No patient presented parossistic or permanent atrial fibrillation.
Table 1.
Population characteristics
| Parameters | CMD | Control group | p value |
|---|---|---|---|
| n = 26 | n = 16 | ||
| Male Sex (% male) | 11 (42) | 5 [31] | 0.4 |
| Age, years (± SD) | 62.9 ± 9.07 | 59.6 ± 11.7 | 0.3 |
| Body weight Index (Kg/m2) | 27.9 ± 4.99 | 25.8 ± 4.92 | 0.19 |
| Smoker (n, %) | 8 [30] | 5 [31] | 0.97 |
| Diabetes (n, %) | 13 (50) | 4 [25] | 0.10 |
| Hyperlipidemia (n, %) | 9 (56) | 15 (58) | 0.92 |
| High blood pressure (n, %) | 11 (42) | 6 (38) | 0.75 |
| Coronary heredity (n, %) | 2 [8] | 0 (0) | 0.51 |
| Renal clearance, ml/mn/m2 (± SD) | 81.9 ± 19.0 | 87.5 ± 18.5 | 0.35 |
| Symptoms according to Diamond and Forrester | |||
| Typical angina | 11 (42) | 0 (0) | 0.003 |
| Atypical angina | 9 (35) | 13 (81) | 0.003 |
| Non anginal | 1 [4] | 0 (0) | 0.6 |
| Dyspnea | 18 (69) | 3 [19] | 0.001 |
Coronary microcirculation dysfunction
The results are presented in Table 2. All patient in the CMD group presented with structural CMD.
Table 2.
Invasive coronary physiology
| CMD (n = 26) | Control group (n = 16) | p value | |
|---|---|---|---|
| Systolic blood pressure (mmHg) | 125.3 ± 25.5 | 127.3 ± 11.5 | 0.77 |
| Diastolic blood pressure (mmHg) | 73.1 ± 8.51 | 70.5 ± 10.5 | 0.38 |
| Heart rate (bpm) | 68.5 ± 12,1 | 67.8 ± 9.27 | 0.88 |
| Rate Pressure product | 8522 ± 2226 | 8633 ± 1340 | 0.85 |
| Baseline Tmn (s) | 0.86 ± 0.33 | 0.55 ± 0.21 | 0.002 |
| Hyperhemic Tmn (s) | 0.50 ± 0.25 | 0.16 ± 0.06 | 0.001 |
| Pa hyperhemic (mmHg) | 84.0 ± 22.3 | 90.6 ± 14.2 | 0.03 |
| Pd hyperhemic (mmHg) | 77.1 ± 12.9 | 86.8 ± 9.39 | 0.03 |
| FFR | 0.91 ± 0.04 | 0.91 ± 0.03 | 0.63 |
| CFR | 1.78 ± 0.49 | 3.48 ± 1.03 | 0.0001 |
| IMR (mmHg x s) | 29.5 (28.2–43) | 15 (10.7–17.7) | 0.0001 |
FFR: fractional flow reserve; CFR: coronary flow reserve; IMR: index of microcirculatory resistance, Pa: aortic pressure; Pd: distal coronary pressure, Tmn: mean transit time at rest
Echocardiographic analysis
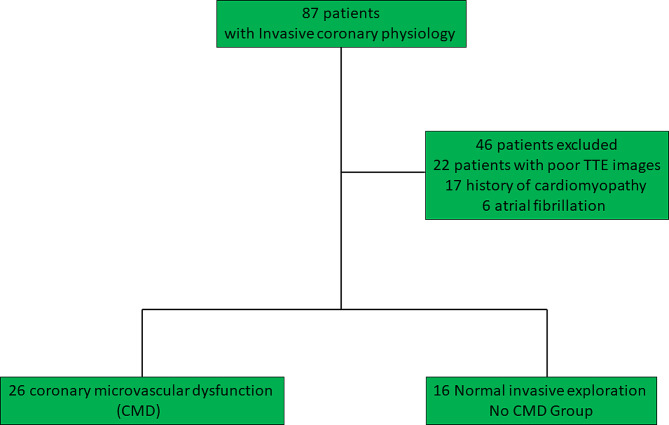
There were no significant differences between CMD-positive and negative patients on the basis of classic echocardiographic functional and structural parameters. LASr was significantly reduced in the CMD group in comparison with the control group (24.6% ± 6.1 vs. 30.3 ± 7.8%, p = 0.01) (Fig. 2). Echocardiographic characteristics are summarized in Tables 3, 4.
Fig. 2.
Comparison between CMD and No CMD groups. CMD: Coronary microvascular dysfunction; LASr: Left atrial strain reservoir
Table 3.
Echocardiographic characteristics of patients
| CMD (n = 26) | Control group (n = 16) | p value | |
|---|---|---|---|
| LVWT (cm) | 0.86 ± 0.17 | 0.88 ± 0.15 | 0.67 |
| LVMI (g/m2) | 79.3 ± 18.6 | 73.2 ± 17.6 | 0.29 |
| LVDI (ml/m2) | 52.7 ± 13.9 | 50.1 ± 10.4 | 0.37 |
| LVEF (%) | 63.1 ± 6.67 | 63.0 ± 5.09 | 0.39 |
| E (m/s) | 7.25 ± 3.02 | 6.44 ± 1.33 | 0.32 |
| A (m/s) | 6.92 ± 2.81 | 7.8 ± 2.24 | 0.28 |
| E/A | 0.90 ± 0.29 | 0.86 ± 0.22 | 0.69 |
| E’(cm/s) | 10.5 ± 4.55 | 9.01 ± 3.81 | 0.25 |
| E/E’ | 6.95 ± 2.95 | 6.58 ± 2.86 | 0.68 |
| PAPS (mmHg) | 24.6 ± 6.64 | 20.4 ± 4.58 | 0.06 |
| TAPSE (mm) | 23.6 ± 4.63 | 21.8 ± 3/03 | 0.16 |
| Peak S Annular tricuspid (cm/s) | 12.4 ± 2.42 | 12.0 ± 1.41 | 0.49 |
| LAVI (ml/m2) | 31.0 ± 12.8 | 28.0 ± 6.44 | 0.39 |
| LASr (%) | 24.6 ± 6.14 | 30.3 ± 7.79 | 0.01 |
LAVI: left atrial volume index, LASr: left atrial strain reservoir function, LVDI: LV dimensions at end-diastole index, LVEF: left ventricle ejection fraction, LVMI: left ventricular masse index, LVWT: left ventricular wall thickness, PAPS: pulmonary artery pressure systolic, TAPSE: Tricuspid annular plane systolic excursion
Table 3.
Univariate and multivariate logistic regression analysis for coronary microvascular dysfunction
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Age | 1.033 (0.970–1.101) | 0.309 | ||
| Body weight Index | 1.095 (0.954–1.257) | 0.19 | ||
| High blood pressure | 1.22 (0.341–4.381) | 0.75 | ||
| Smoker | 0.97 (0.255–3.75) | 0.97 | ||
| Diabetes | 3.00 (0.764–11.78) | 0.15 | ||
| LASr | 0.87 (0.78–0.98) | 0.02 | 0.88 (0.78–0.99) | 0.04 |
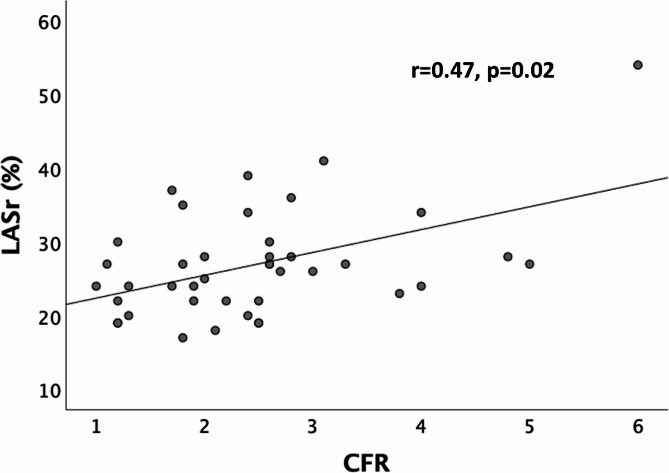
CMD and LASr
There was a moderate yet significant positive correlation between LASr and CFR (r = 0.47, p=0.002) (Fig. 3). With regards to diagnostic performance, the ROC curve presented in Fig. 4 indicated an area under the curve of 0.76 (0.62-0.90) (95% CI), corresponding to a parameter with relatively high discriminatory potential. The LASr cut-off value was 25.5%, enabling better classification of patients with or without CMD.
Fig. 3.
Correlation between LASr and CFR. CFR: Coronary flow reserve; LASr: Left atrial strain reservoir
Fig. 4.
ROC curve for the assessment of the diagnostic performances of LASr for CMD
Reproducibility
Intra- and inter-observer variability of LASr assessment was good. The results are summarized in Table 5.
Table 4.
Assessment of inter- and intra-observer reproducibility
| Intra-observer reproducibility | Inter-observer reproducibility | |||
|---|---|---|---|---|
| Coefficient of variation % | ICC | Coefficient of variation % | ICC | |
| LASr | 26.6 | 0.92 (0.86–0.96) | 27 | 0.82 (0.67–0.90) |
Discussion
The main result of this study was that patients with CMD had a significantly lower LASr than patients without CMD and a multivariate logistic regression analysis demonstrated that CMD was independently associated with LASr.
The strength of this study is that coronary microcirculation was assessed using a robust method validated by international consensus [3, 4, 20, 21]. We showed that LASr was the only TTE parameter to be significantly more altered in the CMD group than in the control group. Advantages of LASr over standard diastolic function parameters include independence of the acquisition from the measurement angle, low influence of loading conditions, and excellent inter- and intra-individual measurement reproducibility. Studies have shown thar LASr diagnostic performance was actually superior to that of other parameters. As demonstrated in the work by Reddy et al., LASr appeared to be the most discriminating parameter in the diagnosis of diastolic dysfunction in patients with HFpEF [22]. Compared with standard multiparametric measurements of diastolic function, LASr evaluation is rapid and easy for expert investigators. It provides information on a gradual, linear impairment of left atrial function [9, 11].
Patients with cardiovascular risk factors such as obesity, hypertension and diabetes exhibit low-grade systemic inflammation. These factors lead to lesions of the coronary endothelium and, consequently, to structural and functional abnormalities of the microcirculation [7, 23]. Structural CMD correspond to a reduction in vessel lumen due to hypertrophy of vascular smooth muscle cells, hypertrophy of myocyte cells, interstitial fibrosis, vasodilatory impairment, and/or hyperreactivity to vasoconstrictor stimuli. Functional CMD correspond to abnormal vasodilation at rest [24]. In our study, structural CMD was only observed. Interesting, no patient in this prospective cohort presented parossistic or permanent atrial fibrillation. This may be explained by the screening method, which targets INOCA patients with a systematic LV end-diastolic pressure measure in accordance of expert consensus [4]. All patients had normal LV end-diastolic pressure (≤ 10 mmHg). This information is important because it was not available in the other studies on the subject, and enables a mechanistic hypothesis to be made. In the case of INOCA, CMD is responsible for an early disorder of diastolic function, with a relaxation disorder but no increase in filling pressures. Relaxation is an active phenomenon, due, at cellular level, to the relaxation of fibers by release of actin and myosin bridges, which requires reuptake of intracellular Calcium into the sarcoplasmic reticulum by the Sarcoendoplasmic Reticulum Calcium ATPase (SERCA) pump. This is an energy-consuming process, which explains the early diastolic disturbances seen in ischemia. For certain teams, INOCA represents a pre-HFpEF state. An increase over time in structural anomalies of the coronary microcirculation leads to ventricular filling disorders due to impaired myocardial compliance which can in turn lead to the development of HFpEF [7, 25]. Several data show correlation between CMD and HFpEF [26]. As shown by the PROMIS-HFpEF study, up to 75% of HFpEF patients have CMD [5]. Anatomopathological studies revealed that patients with HFpEF had decreased capillary density and increased fibrosis compared to subjects without heart disease [27]. A recently published meta-analysis concluded that the diagnostic and prognostic values of LASr were convincing in HFpEF [28]. European cardiac imaging guidelines now suggest the inclusion of LASr results in the new algorithm designed for the estimation of left ventricular filling pressures [29].
Our results contribute to demonstrating the link between left ventricular diastolic abnormalities and CMD in NOCA patients without HFpEF. In the literature, the link between reduced LASr and CMD has already been explored. Keulards et al. concluded that there was a correlation between increased coronary microvascular resistance and impaired LASr. A relationship was also observed between the intensity of microcirculatory damage and altered strain [30]. The authors used continuous thermodilution, whereas bolus thermodilution was used in our study. The former method has been shown to be less prone to measurement variations. However, it requires the use of a dedicated microcatheter (Rayflow®, Hexacath, France), making the procedure more time-consuming, and for the time being, cut off decisions and international expert recommendations recommend the use of bolus thermodilution [4]. Similarly, Konerman et al. found a correlation between altered LASr and CMD as assessed by positron emission tomography. The results also showed that left ventricular systolic parameters such as global longitudinal strain (GLS) did not discriminate between patients with and without CMD [31]. In addition to confirming such data, our results indicate that the use of bolus thermodilution is suitable to evidence the relationship between LASr and CMD. If the present results will be confirmed by several larger studies, LAsr could be used for two purposes in the CMD field. First, LASr could help to classify NOCA patients at high risk of CMD. Second, LASr as an easily measurable, noninvasive and reproducible parameter may ultimately enable the therapeutic monitoring of CMD.
Limitations
This study was monocentric and included a relatively small cohort of patients. The results therefore require further validation on a larger sample. Unfortunately for the LV GLS, the number of non-analyzable segments was too large to provide a robust data set, and we preferred not to analyze these data. In addition, it is important to mention that the echocardiographic study was performed at rest. It should also be noted that strain analysis was carried out on a single equipment while strain values may vary according to the manufacturer.
Conclusion
LASr represent an easily measurable, reliable, and reproducible indicator of diastolic function. LASr was significantly impaired in patients with CMD, indicating diastolic function impairment. LASr could be integrated into the screening, diagnosis, and follow-up of CMD patients.
Acknowledgements
Not applicable.
Abbreviations
- BMI
Body Mass Index
- CFR
Coronary Flow Reserve
- COVADIS
Coronary Vasomotor Disorders International Study
- CMD
Coronary Microvascular Dysfunction
- ESC
European society of Cardiology
- FFR
Fractional Flow Reserve
- GFR
Glomerular Filtration Rate
- HFpEF
Heart Failure with preserves ejection fraction
- HTA
Hypertension
- IMR
Index of microcirculatory resistance
- LASr
Left atrial strain reservoir
- LDLc
Low-Density lipoprotein cholesterol
- LA
Left atrium LAVI left atrial volume index
- LVEF
Left ventricular ejection fraction
- LVWT
left ventricular wall thickness
- LVMI
left ventricular masse index
- LV
dimensions at end-diastole index (LVDI)
- PAPs
Pulmonary arterial systolic pressure
- RPP
Rate Pressure Product
- SBP
Simpson Biplan
- TAPSE
Tricuspid Annular Plane Systolic Excursion
- TTE
Trans-thoracic echocardiography
Author contributions
Barone-Rochette G conceived of the presented idea. La Mela J collected and performed analysis. Barone-Rochette G verified the analytical methods. La Mela J wrote the paper under the supervision of Riou Land Barone-Rochette G. All authors collected the data and discussed the final manuscript.
Funding
Not applicable.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Declarations
Ethics approval and consent to participate
We further confirm that any aspect of the data collection covered in this manuscript that has involved our patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Consent for publication
We guarantee that the contribution to the work has not been previously published elsewhere, or that if it has been published in whole or in part, any permission necessary to publish it in the work has been obtained.
Competing interests
GBR has received research grants from Merck Sharp and Dohme, Abbott vascular, Pfizer, and consulting fees from Bayer, General electric, Boehringer Ingelheim, MEDIS medical imaging, Abbott vascular, Novo Nordisk, Sanofi, Novartis and AMGEN. The other authors have no conflict of interest.
Authors’ information
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen C, Wei J, AlBadri A, Zarrini P, Bairey Merz CN. Coronary microvascular dysfunction - epidemiology, Pathogenesis, prognosis, diagnosis, risk factors and therapy. Circ J. 2017;81:3–11. doi: 10.1253/circj.CJ-16-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradley C, Berry C. Definition and epidemiology of coronary microvascular disease. J Nucl Cardiol. 2022;29:1763–75. doi: 10.1007/s12350-022-02974-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ong P, Camici PG, Beltrame JF, Crea F, Shimokawa H, Sechtem U, et al. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol Janv. 2018;250:16–20. doi: 10.1016/j.ijcard.2017.08.068. [DOI] [PubMed] [Google Scholar]
- 4.Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas AHEM, et al. An EAPCI Expert Consensus Document on Ischaemia with non-obstructive coronary arteries in collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504–20. doi: 10.1093/eurheartj/ehaa503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan RS, et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J. 2018;39:3439–50. doi: 10.1093/eurheartj/ehy531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dryer K, Gajjar M, Narang N, Lee M, Paul J, Shah AP, et al. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am J Physiol-Heart Circ Physiol. 2018;314:H1033–42. doi: 10.1152/ajpheart.00680.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options. J Am Coll Cardiol. 2018;72:2625–41. doi: 10.1016/j.jacc.2018.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venkateshvaran A, Tureli HO, Faxén UL, Lund LH, Tossavainen E, Lindqvist P. Left atrial reservoir strain improves diagnostic accuracy of the 2016 ASE/EACVI diastolic algorithm in patients with preserved left ventricular ejection fraction: insights from the KARUM haemodynamic database. Eur Heart J - Cardiovasc Imaging. 2022;23:1157–68. doi: 10.1093/ehjci/jeac036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh A, Addetia K, Maffessanti F, Mor-Avi V, Lang RM. LA Strain for categorization of LV Diastolic Dysfunction. JACC Cardiovasc Imaging. 2017;10:735–43. doi: 10.1016/j.jcmg.2016.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas L, Marwick TH, Popescu BA, Donal E, Badano LP. Left atrial structure and function, and left ventricular diastolic dysfunction. J Am Coll Cardiol. 2019;73:1961–77. doi: 10.1016/j.jacc.2019.01.059. [DOI] [PubMed] [Google Scholar]
- 11.Sun BJ, Park JH. Echocardiographic Measurement of Left Atrial Strain ― A key requirement in clinical practice. Circ J. 2021;24:6–13. doi: 10.1253/circj.CJ-21-0373. [DOI] [PubMed] [Google Scholar]
- 12.Moreno-Ruiz LA, Madrid-Miller A, Martínez-Flores JE, González-Hermosillo JA, Arenas-Fonseca J, Zamorano-Velázquez N, et al. Left atrial longitudinal strain by speckle tracking as independent predictor of recurrence after electrical cardioversion in persistent and long standing persistent non-valvular atrial fibrillation. Int J Cardiovasc Imaging. 2019;35:1587–96. doi: 10.1007/s10554-019-01597-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by Echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 14.Tan TS, Akbulut IM, Demirtola AI, Serifler NT, Ozyuncu N, Esenboga K, et al. LA reservoir strain: a sensitive parameter for estimating LV filling pressure in patients with preserved EF. Int J Cardiovasc Imaging. 2021;37:2707–16. doi: 10.1007/s10554-021-02235-x. [DOI] [PubMed] [Google Scholar]
- 15.Yuda S. Current clinical applications of speckle tracking echocardiography for assessment of left atrial function. J Echocardiogr. 2021;19:129–40. doi: 10.1007/s12574-021-00519-8. [DOI] [PubMed] [Google Scholar]
- 16.Kuppahally SS, Akoum N, Badger TJ, Burgon NS, Haslam T, Kholmovski E, et al. Echocardiographic left atrial reverse remodeling after catheter ablation of atrial fibrillation is predicted by preablation delayed enhancement of left atrium by magnetic resonance imaging. Am Heart J. 2010;160:877–84. doi: 10.1016/j.ahj.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demir OM, Boerhout CKM, de Waard GA, et al. Comparison of Doppler Flow Velocity and Thermodilution Derived indexes of coronary physiology. JACC Cardiovasc Interv. 2022;15:1060–70. doi: 10.1016/j.jcin.2022.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–70. doi: 10.1093/ehjci/jev014. [DOI] [PubMed] [Google Scholar]
- 19.Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using twodimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018;19:591–600. doi: 10.1093/ehjci/jey042. [DOI] [PubMed] [Google Scholar]
- 20.Barbato E. Validation of coronary flow reserve measurements by thermodilution in clinical practice. Eur Heart J. 2004;25:219–23. doi: 10.1016/j.ehj.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Ford TJ, Ong P, Sechtem U, Beltrame J, Camici PG, Crea F, et al. Assessment of Vascular Dysfunction in patients without obstructive coronary artery disease. JACC Cardiovasc Interv. 2020;13:1847–64. doi: 10.1016/j.jcin.2020.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reddy YNV, Obokata M, Egbe A, Yang JH, Pislaru S, Lin G, et al. Left atrial strain and compliance in the diagnostic evaluation of heart failure with preserved ejection fraction. Eur J Heart Fail. 2019;21:891–900. doi: 10.1002/ejhf.1464. [DOI] [PubMed] [Google Scholar]
- 23.Camici PG, d’Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015;12:48–62. doi: 10.1038/nrcardio.2014.160. [DOI] [PubMed] [Google Scholar]
- 24.Rahman H, Demir OM, Khan F, Ryan M, Ellis H, Mills MT, et al. Physiological stratification of patients with Angina due to coronary microvascular dysfunction. J Am Coll Cardiol. 2020;75:2538–49. doi: 10.1016/j.jacc.2020.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paulus WJ, Tschöpe C. A Novel paradigm for heart failure with preserved ejection fraction. J Am Coll Cardiol. 2013;62:263–71. doi: 10.1016/j.jacc.2013.02.092. [DOI] [PubMed] [Google Scholar]
- 26.Giamouzis G, Schelbert EB, Butler J. Growing evidence linking Microvascular Dysfunction with Heart failure with preserved ejection fraction. J Am Heart Assoc. 2016;5:e003259. doi: 10.1161/JAHA.116.003259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohammed SF, Hussain S, Mirzoyev SA, Edwards WD, Maleszewski JJ, Redfield MM. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation. 2015;131:550–9. doi: 10.1161/CIRCULATIONAHA.114.009625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan MS, Memon MM, Murad MH, Vaduganathan M, Greene SJ, Hall M, et al. Left atrial function in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail. 2020;22:472–85. doi: 10.1002/ejhf.1643. [DOI] [PubMed] [Google Scholar]
- 29.Smiseth OA, Morris DA, Cardim N, Cikes M, Delgado V, Donal E, et al. Multimodality imaging in patients with heart failure and preserved ejection fraction: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J - Cardiovasc Imaging. 2022;23:e34–61. doi: 10.1093/ehjci/jeab154. [DOI] [PubMed] [Google Scholar]
- 30.Keulards DCJ, Bouwmeester S, de Vos AMJ, Dekker LRC, Pijls NHJ, Houthuizen P. High microvascular resistance and reduced left atrial strain in patients with coronary microvascular dysfunction: the micro-strain study. Int J Cardiol. 2021;333:21–8. doi: 10.1016/j.ijcard.2021.02.055. [DOI] [PubMed] [Google Scholar]
- 31.Konerman MC, Greenberg JC, Kolias TJ, Corbett JR, Shah RV, Murthy VL, et al. Reduced myocardial Flow Reserve is Associated with Diastolic Dysfunction and decreased left atrial strain in patients with normal ejection Fraction and Epicardial Perfusion. J Card Fail. 2018;24:90–100. doi: 10.1016/j.cardfail.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.