CASE PRESENTATION
A woman with invasive ductal carcinoma was hospitalized due to a locally infected thoracic ulcer. Topical metronidazole was prescribed. One month later, she developed mental confusion. There were no metabolic causes to justify her altered mental state. Brain magnetic resonance imaging revealed T2/fluid attenuated inversion recovery (FLAIR) hyperintensities in the dentate nuclei [Figures 1 and 2]. Cerebrospinal fluid and electroencephalogram showed no significant changes.
Figure 1.
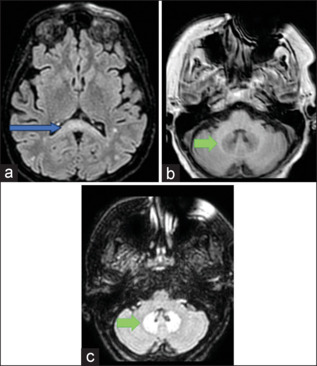
(a) Axial FLAIR scan illustrating hyperintensity within the corpus callosum (blue arrow). (b) Axial T1 imaging with bilateral dentate nuclei hypointensity (green arrow), opposite to FLAIR hyperintensity shown on (c) (green arrows). FLAIR = fluid attenuated inversion recovery
Figure 2.
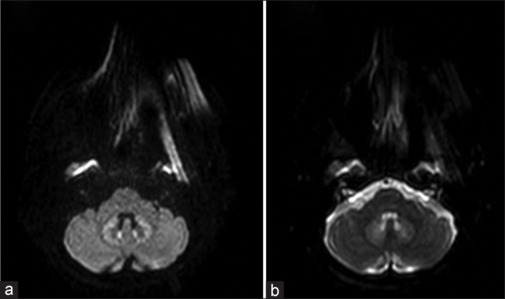
Hyperintensity on bilateral dentate nuclei on diffusion-weighted imaging (DWI) (a), with no corresponding restriction on ADC maps (b)
Most cases of metronidazole-induced brain toxicity present with T2/FLAIR hyperintensities in the dentate nuclei.[1,2] This is the second case report in international literature of encephalopathy related to topical metronidazole.[3] Due to the extent of the ulcer being treated [Figure 3], there was probably cutaneous absorption and metronidazole intoxication.[1,2,3] She improved completely after the antibiotic was stopped.
Figure 3.

Large thoracic ulcer being treated with topic metronidazole for approximately 1 month before symptoms occurred
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bond KM, Brinjikji W, Eckel LJ, Kallmes DF, McDonald RJ, Carr CM. Dentate update: Imaging features of entities that affect the dentate nucleus. AJNR Am J Neuroradiol. 2017;38:1467–74. doi: 10.3174/ajnr.A5138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oliveira AM, Paulino MV, Vieira APF, McKinney AM, da Rocha AJ, Dos Santos GT, et al. Imaging patterns of toxic and metabolic brain disorders. Radiographics. 2019;39:1672–95. doi: 10.1148/rg.2019190016. [DOI] [PubMed] [Google Scholar]
- 3.Mathew RP, Kunhimohammed SP. A case of topical metronidazole–induced encephalopathy. JAMA Neurol. 2020;77:1318–9. doi: 10.1001/jamaneurol.2020.2596. [DOI] [PubMed] [Google Scholar]


