Abstract
Objectives:
To examine changes in presence of methamphetamine in toxicology testing among outpatients receiving healthcare in Boston, Massachusetts.
Methods:
A serial cross-sectional study of oral fluid drug test results over a 6-year period of all patient specimens submitted for testing as part of routine care across an academic medical center in Boston, Massachusetts and affiliated primary care practices which has roughly 48,000 admissions and 500,000 primary care visits per year. All samples were subjected to definitive drug testing by liquid chromatography–tandem mass spectrometry for fentanyl, 6-mono-acetylmorphine (6-MAM, metabolite of heroin), benzoylecgonine (metabolite of cocaine), cocaine, and methamphetamine. We compared positive rates and change over time across the same calendar months (February to July) of 6 consecutive years from 2014 to 2019.
Results:
Total of 17,303 oral fluid samples collected from outpatients receiving routine healthcare across 6 years were analyzed. Samples showing presence of methamphetamine, cocaine, and fentanyl increased over the study period, whereas 6-MAM presence decreased. From 2014 to 2019 samples with methamphetamine present increased from 0.9% to 5.1% and samples with 6-MAM present decreased from 9.5% to 2.8%. Fentanyl was added to the testing panel in 2017. In 2019, 15.7% of samples had fentanyl present. Polysubstance use was common; 44% of samples with methamphetamine also showed cocaine or benzoylecgonine, 25% showed fentanyl, and 3% showed 6-MAM presence.
Conclusions:
Presence of methamphetamine in oral fluid toxicology tests increased from 2014 to 2019 across a sample of outpatients receiving healthcare in Boston, Massachusetts. Regions of the country with high rates of opioid overdose may need to integrate harm reduction and addiction treatment resources for stimulant use disorder in addition to opioid use disorder.
Keywords: fentanyl, heroin, methamphetamine, overdose crisis, stimulant, toxicology
The North American drug overdose crisis continues to evolve as its supply and demand drivers are in flux (Ciccarone, 2019). Although illicitly manufactured fentanyl is a main driver of drug overdose deaths, most opioid-related deaths now cooccur with a nonopioid drug (Gladden, 2019). Deaths involving an opioid and a stimulant have also been increasing in recent years and one-third of the 70,237 drug overdose deaths in 2017 involved cocaine, psychostimulants, including drugs such as methamphetamine, or both (Kariisa et al., 2019). Morbidity testing shows some parallels. Among a large sample of urine drug screens submitted to a national toxicology testing company, nonprescribed fentanyl was increasingly found among samples testing positive for either cocaine or methamphetamine, with an 1850% increase among cocaine- and a 798% increase among methamphetamine-positive samples from 2013 to 2018 (LaRue et al., 2019).
Historically, US geographic disparities have been noted both in stimulant supply and medical consequences related to stimulant use. For example, methamphetamine supply and use problems are typically greater in the western US and lower in the Northeast (Centers for Disease Control and Prevention, 2018; U.S. Drug Enforcement Administration, Diversion Control Division, 2019). More recently, an increase in methamphetamine use was found among people with opioid use disorder seeking treatment, from 2011 to 2017, with the greatest increase in the western part of the United States (Ellis et al., 2018). The Northeast United States has been a hotspot for opioid-related overdoses, but historically has not been a region with high rates of methamphetamine overdose, however this may be shifting (Jalal et al., 2018). Understanding drug use trends could be valuable in designing interventions, particularly in areas of the country which have already been impacted by the opioid overdose crisis. This study examined changes in the presence of methamphetamine in toxicology testing among patients receiving healthcare in Boston, Massachusetts.
METHODS
We conducted a serial cross-sectional study of oral fluid drug test results of patient specimens submitted for testing by health care providers as part of routine care. This analysis used a sample of all specimens submitted for oral fluid toxicology as a part of routine healthcare in the outpatient setting across an academic medical center in Boston, Massachusetts and affiliated primary care practices which has roughly 48,000 admissions and 500,000 primary care visits per year. All samples were subjected to definitive drug testing by liquid chromatography–tandem mass spectrometry. Analyte concentrations at or greater than: fentanyl, 1.0 ng/mL; 6-monoacetylmorphine (6-MAM, a metabolite of heroin), 2.0 ng/mL; benzoylecgonine, 2.0 ng/mL or cocaine, 2.0 (2014–2018); 4.0 (2019) ng/mL; or methamphetamine, 10.0 ng/mL, were considered positive. We compared positive rates and change over time across the same calendar months (February to July) of 6 consecutive years from 2014 to 2019. Because fentanyl testing was added on March 6, 2017, fentanyl results were not available for all of the study years.
This study was approved by the Partners Healthcare institutional review board.
RESULTS
A total of 17,303 oral fluid samples collected across 6 years were included and analyzed (Table 1). We found increases over time in the percent of samples which showed the presence of methamphetamine, cocaine, and fentanyl and a parallel decrease in the percent of samples showing the presence of 6-MAM (heroin) (Fig. 1). From 2014 to 2019 there was an increase in the presence of methamphetamine in samples from 0.9% to 5.1% and in the presence of cocaine or benzoylecgonine from 19.7% to 22.1%. Over the same time-period there was decrease in the presence of 6-MAM (heroin) from 9.5% to 2.8%. Fentanyl was added to the routine testing panel in March of 2017. In 2018 and 2019, respectively, 13.8% and 15.7% of samples showed the presence of fentanyl. We also explored combinations of methamphetamine with other drugs. In the period February 1, 2019 to July 31, 2019 there were 272 samples with presence of methamphetamine from 117 different patients. One hundred and nineteen of the 272 (44%) methamphetamine samples also showed the presence of cocaine or benzoylecgonine, 67 (25%) showed the presence of fentanyl, and 7 (3%) showed 6-MAM (heroin) presence.
TABLE 1.
Toxicology Results Among Outpatients Seen for Routine Care in an Academic Medical Center in Boston, Massachusetts and Affiliated Primary Care Practices
| Feb to July Period, Year | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|
| Total samples tested | 1077 | 1326 | 1719 | 3012 | 4812 | 5357 |
| BZE positive, n (%) | 161 (14.9) | 175 (13.2) | 249 (14.5) | 501 (16.6) | 821 (17.1) | 914 (17.1) |
| COC positive, n (%) | 191 (17.7) | 212 (16.0) | 321 (18.7) | 614 (20.4) | 1139 (23.7) | 1093 (20.4)† |
| BZE or COC positive, n (%) | 212 (19.7) | 245 (18.5) | 350 (20.4) | 679 (22.5) | 1198 (24.9) | 1184 (22.1)† |
| Fentanyl positive, n (%) | TNP | TNP | TNP | 282* (9.4) | 665 (13.8) | 839 (15.7) |
| 6-MAM positive, n (%) | 102 (9.5) | 148 (11.2) | 119 (6.9) | 129 (4.3) | 130 (2.7) | 150 (2.8) |
| Methamphetamine positive, n (%) | 10 (0.9) | 13 (1.0) | 20 (1.2) | 79 (2.6) | 106 (2.2) | 272 (5.1) |
| Methamphetamine and BZE or COC positive, n (%) | 1 (0.001) | 3 (0.002) | 6 (0.003) | 34 (0.011) | 48 (0.010) | 119 (0.021) |
| Methamphetamine and fentanyl positive, n (%) | TNP | TNP | TNP | TNP | 31 (0.006) | 67 (0.013) |
| Methamphetamine and 6-MAM positive, n (%) | 1 (0.001) | 1 (0.0008) | 3 (0.002) | 9 (0.003) | 5 (0.001) | 7 (0.001) |
Fentanyl testing started 3/6/17.
COC cutoff was 2.0 ng/ml until 2019 when it was changed to 4.0 ng/ml.
6-MAM, 6-monoacetylmorphine; BZE, Benzoylecgonine; COC, Cocaine; TNP, test not performed.
FIGURE 1.
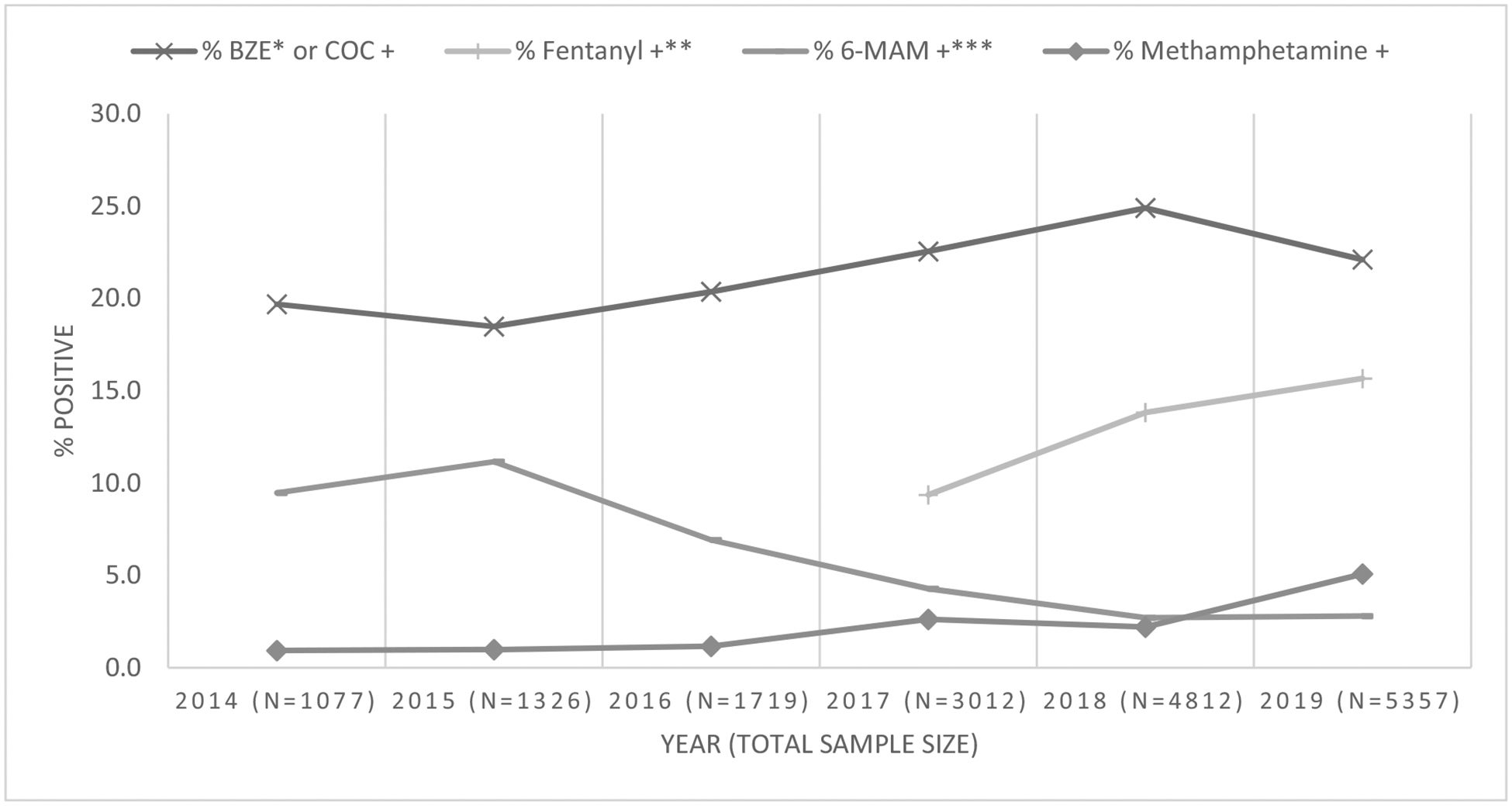
Percent positivity by drug or metabolite. * BZE: benzoylecgonine, metabolite of cocaine. ** There is no data for fentanyl from 2014 to 2016 as fentanyl was not added to the testing panel until March 6, 2017. *** 6-MAM: 6-monoacetylmorphine, metabolite of heroin.
DISCUSSION
In this serial cross-sectional study of toxicology testing in an academic health center in Boston, Massachusetts we found a 467% increase in the presence of methamphetamine in samples from 2014 to 2019. In addition, we noted a decrease in heroin presence and a growth in fentanyl presence in samples. These findings mirror changes seen in national mortality data showing increases in fentanyl and stimulant related overdose deaths and treatment admissions in the Western region of the United States. These findings are novel from prior studies in 2 main ways. First, testing was conducted among patients as a part of routine healthcare across primary and behavioral healthcare settings affiliated with a large academic medical center in contrast to prior samples limited to people who use drugs or to commercial testing companies (Hayashi et al., 2018). Second, these findings, being limited to the Northeast, demonstrate a break from the historic norm of low methamphetamine availability and consequences in the Northeast region of the United States.
These findings have important public health and clinical implications, particularly for regions like the Northeast where substance-related interventions have focused largely on opioids. With intense attention on the opioid overdose crisis relatively fewer resources have been dedicated to other substances and combinations. There is a critical necessity for integrating comprehensive polysubstance addiction treatment resources into healthcare settings. Incorporating harm reduction principles and practice is key, including tools for drug checking given the contamination and unpredictability of the illicit drug supply. In addition, increased awareness in the medical and public health community about changing use patterns could help advance prevention and clinical care models. For example, for people using methamphetamine, healthcare settings may be particularly challenging where excessive stimuli, involvement of hospital security, and monitoring by medical staff may worsen agitation seen with intoxication. Protocols which focus on reducing agitation and retaining patients who use methamphetamine in medical settings are needed. In addition, these findings emphasize the importance of moving away from substance specific interventions and instead focusing on holistic prevention and intervention efforts that are grounded in the medical evidence base to effectively manage substance use disorders using the principles of chronic disease management. Stigma reduction efforts are an additional important part of the public health response.
There are limitations to these findings. First, the decision to order toxicology tests was not random and thus findings may not generalize to the wider population. Second, toxicology tests were ordered on patients engaged in healthcare and this population is likely different from people who use drugs who do not receive healthcare. Third, we did not examine patient or practice level factors. Fourth, this is only a descriptive study and we did not do statistical testing for trends. Lastly, as this study was limited to toxicology results, we were not able to assess whether use was intentional or the result of drug supply contamination.
CONCLUSIONS
Methamphetamine presence in toxicology tests increased from 2014 to 2019 across a sample of outpatients receiving healthcare in Boston, Massachusetts. This may indicate a need for harm reduction and addiction treatment resources for stimulant use disorder in addition to opioid use disorder in areas of the country with high rates of opioid overdose.
Acknowledgments
Dr. Wakeman has previously received personal fees from Optum Labs and serves currently as a scientific advisor to Celero Systems. Dr. Ciccarone serves currently as a scientific advisor to Celero Systems and Arbour Pharmaceuticals. For the remaining authors none were declared. Dr. Wakeman has received research support through Massachusetts General Hospital from the National Institutes of Health (1R01DA044526-01A1), the National Institute on Drug Abuse (3UG1DA015831-17S2), the Substance Abuse and Mental Health Services Administration (1H79TI081442-01), the Laura and John Arnold Foundation, received salary support from OptumLabs, and serves as a scientific advisor to Celero Systems. Dr. Ciccarone acknowledges research support from the National Institutes of Health, National Institute on Drug Abuse (R01DA037820) and also serves as scientific advisor to Celero Systems and Arbour Pharmaceuticals.
REFERENCES
- Ciccarone D The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy 2019;71:183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladdden RM, O’Donnell J, Mattson CL, Seth P. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine and methamphetamine- 25 states, July-December 2017 to January-June 2018. MMWR Morb Mortal Wkly Rep 2019;68:737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. MMWR Morb Mortal Wkly Rep 2019;68:388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRue L, Twillman RK, Dawson E, et al. Rate of fentanyl positivity among urine drug test results positive for cocaine or methamphetamine [published correction appears in JAMA Netw Open. 2019 Oct 2;2(10):e1916040]. JAMA Netw Open 2019;2(4):e192851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2018. Annual Surveillance Report of Drug-Related Risks and Outcomes — United States. Surveillance Special Report. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Published August 31, 2018. Available at: https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf. Accessed December 2, 2019. [Google Scholar]
- U.S. Drug Enforcement Administration, Diversion Control Division. National Forensic Laboratory Information System: NFLIS-Drug 2018 Annual Report. Springfield, VA: U.S. Drug Enforcement Administration; 2019. [Google Scholar]
- Ellis MS, Kasper ZA, Cicero TJ. Twin epidemics: the surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend 2018;193:14–20. [DOI] [PubMed] [Google Scholar]
- Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science 2018;361(6408): eaau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi K, Milloy MJ, Lysyshyn M, et al. Substance use patterns associated with recent exposure to fentanyl among people who inject drugs in Vancouver, Canada: a cross-sectional urine toxicology screening study. Drug Alcohol Depend 2018;183:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


