Key Points
Question
Do text messages with or without financial incentives promote weight loss in men with obesity?
Findings
In this randomized trial that included 585 men with obesity, text messaging with behavioral messages combined with a financial incentive resulted in a 5% weight loss at 12 months, compared with weight loss of 3% for text messaging alone, and 1% for the control group. The difference in weight loss was statistically significant for the comparison between text messaging with financial incentives and the control group but not between the text messaging alone and the control group.
Meaning
In men with obesity, a 12-month intervention consisting of text messaging with financial incentives resulted in modest but statistically significant weight loss compared with control.
Abstract
Importance
Effective weight loss interventions are needed for men with obesity.
Objective
To determine whether an intervention that combined text messaging with financial incentives attained significant weight loss at the 12-month follow-up compared with the control group and whether an intervention of text messaging alone attained significant weight loss at the 12-month follow-up compared with the control group.
Design, Setting, and Participants
An assessor-blinded randomized clinical trial conducted in Belfast, Bristol, and Glasgow areas in the UK. A total of 585 men with body mass index (BMI) of 30 or more were enrolled between July 2021 and May 2022. Final follow-up occurred June 2023.
Interventions
Participants were randomly assigned to 12 months of behavioral focused text messages combined with financial incentives (n = 196), 12 months of behavioral focused text messages alone (n= 194), or a waiting list (control group; n= 195). The financial incentive consisted of a monetary reward that was lost if weight loss targets were not met. All participants received weight management information and a pedometer at baseline.
Main Outcomes and Measures
The 2 primary comparisons were the 12-month comparison of within-participant weight change between the text messaging with financial incentive group and the control group and the comparison between the text messaging alone group and the control group (minimum clinically important difference, 3%). The P value defined for statistical significance was P < .025 for each comparison.
Results
Of the 585 men (mean [SD] age, 50.7 [13.3] years; mean weight, 118.5 [19.9] kg; mean BMI, 37.7 [5.7]; 525 [90%] White), 227 (39%) lived in postal code areas with lower socioeconomic status, and 426 (73%) completed the 12-month follow-up. At the 12-month follow-up, compared with the control group, the mean percent weight change was significantly greater in the text messaging with financial incentive group (mean difference, −3.2%; 97.5% CI, −4.6% to −1.9%; P < .001) but was not significantly greater in the text messaging alone group (mean difference, −1.4%; 97.5% CI, −2.9% to 0.0, P = .05). The mean (SD) weight changes were −5.7 (7.4) kg for the text messaging with financial incentives group, −3.0 (7.5) kg for the text messaging alone group, and −1.5 (6.6) kg for the control group. The 12-month mean (SD) percentage weight changes from baseline were −4.8% (6.1%) for the text messaging with financial incentives group, −2.7% (6.3%) for text messaging alone group, and −1.3% (5.5%) for the control group. Of 366 adverse events reported, the most common were infections (83 [23%]). Of the 23 serious adverse events (6.3%), 12 (52%) occurred in the text messaging with financial incentives group, 5 (22%) in the texts messaging alone group, and 6 (26%) in the control group. None were considered related to participating in a trial group.
Conclusion and Relevance
Among men with obesity, an intervention with text messaging with financial incentive significantly improved weight loss compared with a control group, whereas text messaging alone was not significantly better than the control condition. These findings support text messaging combined with financial incentives to attain weight loss in men with obesity.
Trial Registration
isrctn.org Identifier: ISRCTN91974895
This randomized clinical trial assesses whether text messaging combined with financial incentives or text messages alone could help men with obesity lose weight at 12 months.
Introduction
Obesity increases rates of type 2 diabetes, heart disease, stroke, mobility impairment, and some cancers and affects approximately 800 million people worldwide.1,2 Approximately 26% of UK adult men have obesity.3 However, men are less likely than women to participate in weight loss interventions.4,5 Effective interventions to attain weight loss in men are needed.6
Behavior change interventions delivered with text messaging can be effective and scalable components of weight loss programs. A systematic review that included 12 randomized clinical trials reported that text messaging–based weight loss interventions were associated with a mean weight change of −2.3 kg (95% CI, −3.2 to −1.4 kg) compared with control.7 However, in this systematic review, only 3 clinical trials reported weight loss at 12 months (mean intervention duration 6 months), and no trials included a large proportion of men. Financial incentives can help men with overweight and obesity to lose weight8,9 and adding behavior change techniques and economic theory may enhance effectiveness.10,11,12
The Game of Stones clinical trial was designed to assess whether text messaging combined with financial incentives could help men with obesity lose weight at 12-month follow-up, compared to a control group. This clinical trial also evaluated whether text messaging alone could attain significant weight loss at 12 months’ follow-up compared with a control group.
Methods
Trial Design
We conducted a 3-group assessor-blind superiority randomized clinical trial in 3 UK areas around Belfast, Bristol, and Glasgow. Enrollment was between July 2021 and May 2022. Final follow-up occurred June 2023. The trial protocol can be found in Supplement 113 and the statistical analysis plan in Supplement 2. Eligible men were randomized to 1 of 3 groups: text messaging with financial incentives for 12 months; text messaging alone for 12 months, or waiting list (control) for 12 months. The control group could receive the first 3 months of text messages at the end of the clinical trial. Ethical approval was provided by North of Scotland Research Ethics Committee 2 [20/NS/0141]. All participants provided written informed consent. This trial is reported using the Consolidated Standards of Reporting Trials Extension (CONSORT Extension) to CONSORT 2010 guidelines for multiarm, parallel-group, randomized trials and the CONSORT harms statement 2022 (https://www.equator-network.org/).
Participants
We recruited participants through letters sent by general family practices and through the community, such as information stands in supermarkets, leaflets, posters, social media, and word of mouth.14,15
Men 18 years or older with a body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) of 30 or higher were eligible. Men were excluded if they did not have a mobile phone, were unable to understand English, planned to move from the area or have bariatric surgery within 12 months, had participated in a weight loss intervention less than 6 months ago, or had a terminal or severe psychiatric illness.
Men were randomly allocated 1:1:1 by researchers within each area using a secure remote web-based system to 12 months of automated text messages with financial incentives, text messages alone, or a control group. Randomization was stratified by area using permuted blocks of random sizes of 3, 6, or 9.
Interventions
Text messages and financial incentives were developed with feedback from potentially eligible men and health care clinicians and were designed to promote inclusivity, sustainability, minimal effort from participants and clinical staff, and to have a low risk of harm.16,17
Text Messages
Daily text messages were identical for the 2 intervention groups and did not mention financial incentives. They incorporated weight management evidence, website links to information resources, and theory-based behavior change techniques based on the Health Action Process Approach,18 self-determination theory,19 and the behavior change maintenance model.20 Examples are provided in the Box and eTable 1 in Supplement 3. Text messages commenced within a week of randomization, with options for participants to pause, restart, or reduce frequency. The total number of text messages that a participant could receive was 370, of which 364 were behavioral, 3 were weight appointment reminders, and 3 were notifications of weight goal attainment. Participants could respond to text messages but were advised that they would usually not receive a reply unless a participant safety issue was identified.
Box. Example Text Messagesa.
Baseline: “OK, here’s the deal. Some texts will be useful and others maybe won’t. Just pick whatever works for you and ignore the rest. If you want to reply to any of the texts please do. We read every text but usually we won’t be able to write back. Sorry.”
3 months: “Rick says that when he’s got a special occasion coming up, he prepares for it and makes sure he has a period where you are doing well before making loads of sensible eating choices—this way you will have earned it even more.”
6 months: “That’s the 6 months mark! Two things are important now: Keep off any weight lost and have your 1-year goal in mind. How confident are you that you can manage this?”
9 months: “Weekend coming up, finally! Remember Gavin’s tip: the power of meal prep. Helps you stay ahead. Time for another batch prep session?”
Automated incentive calculation text with {algorithm}:
12 months:
“Thanks for attending the weigh-in. You lost {0} kg ({1} st {2} lb}), or {3}% of your starting weight. You have secured £{4} and lost £{5}. Well done! Your total Game of Stones payment is £{3m + 6m + 12m} Look forward to seeing you in 12 months’ time.”
Financial Incentives
Participants allocated to the text messaging with the financial incentives group were told that £400 (US $490) had been placed in a study account for them that they could access at the end of the clinical trial, but that money would be lost if weight loss goals were not attained. The goals were 5% weight loss from baseline at 3 months (£50 [$64] secured), 10% from baseline at 6 months (£150 [$191] secured), and maintaining 10% weight loss at 12 months (£200 [$254] secured) (eMethods in Supplement 3). If all goals were met, participants could retain £400 [$490] if they were weighed in person at community venues of family practices within 23 days of their follow-up due date on the study scales. For each 1% of weight lost between 5% and 10% at 6 and 12 months, additional money was secured. Information about the amount of money due was automatically calculated from the weight data and sent to participants by text after each weight assessment (Box and eTable 2 in Supplement 3) and participants were paid after the 12-month follow-up through bank transfer.
Interventions Received by All 3 Groups
All participants received a pedometer and access to a study website with evidence-based information about weight management (eMethods in Supplement 3). Participants in intervention groups had personal login accounts that allowed them to track their weight and step count and access information about local weight management and physical activity services. Study staff directed participants to study materials rather than giving weight management advice.
Primary Outcome
The 2 primary outcomes are within-participant weight change expressed as a percentage of baseline weight at 12 months comparing the text messaging with financial incentives vs the control group and comparing the text messaging alone vs the control group.
Secondary Outcomes
Secondary outcomes at the 12-month follow-up compared with baseline were as follows: absolute weight change in kilograms; the percent of participants with any weight loss, the percent of participants achieving weight loss of 5% or more, or achieving weight loss of 10% or more; categories of weight loss were defined as 0 to less than 5%, 5% or more to less than 10%, 10% or more; percent of participants gaining weight; the EuroQol 5-Dimension 5-level (EQ-5D-5L); Warwick-Edinburgh Mental Well-Being Score (WEMWBS); and Weight Self-Stigma Questionnaire (WSSQ). The following secondary outcomes were added after the trial start: EQ-5D-5L Anxiety/Depression Dimension (EQ-5D-5L-AD), Patient Health Questionnaire (PHQ-4), and all possible categories for percent weight change from baseline were specified. Baselin data collection for PHQ-4 began November 2021 during enrollment and before collection of 12-month follow-up data. No outcome data were reviewed prior to adding these secondary outcomes.
Exploratory Outcomes
The exploratory outcomes (no minimally important clinical difference defined) consisted of program satisfaction assessed using a 0- to 100-point scale, (100 was most satisfied); satisfaction with weight loss progress assessed using 7 categories 1 (very unhappy) to 7 (very happy); and publicly funded weight management services including “yes” or “no” for medication and meal replacements used. Behavioral exploratory outcomes will be reported separately and consist of weight management strategies; self-monitoring weight; self-monitoring steps; physical activity; alcohol use; smoking status; confidence in ability to lose weight; and confidence in ability to maintain weight loss long term.
Assessments
Staff measuring weight and analyzing outcomes, harms and benefits data were unaware of group allocations. Weight was measured in-person within 3 weeks of the target date for follow-up using study scales and verified independently by another researcher. If the participant was not able to return for measurement of weight in person, participants were offered a video call to measure weight on study scales delivered to their home. If participants declined or did not respond to this option, they were mailed a letter requesting email or postal return of a questionnaire with self-reported weight on their own scale. Weights were measured at baseline and 12 months for all 3 groups, and the 2 intervention groups at 3 and 6 months. Staff asked participants at each assessment about helpful or harmful consequences of taking part in the study and about adverse events including serious adverse events (eMethods in Supplement 3).
Self-report questionnaires at baseline included socioeconomic measures consistent across UK countries obtained from the UK Office for National Statistics.21 Data on racial and ethnic group were collected to assess the potential generalizability of results to UK regions with different populations. Participants were asked to select one of the following 6 options: African; Asian or Asian British; Black, Black British, or Caribbean; White; mixed or multiple ethnic groups; and other ethnic group or prefer not to say.
Power Calculation
The sample size calculation was based on detecting a target difference in weight between the intervention groups and the control group of at least 3.3 kg, assuming an SD of 8 kg.7,14 The 3.3 kg was based on 3% of the mean baseline weight of 109 kg in the feasibility study and the National Institute of Health and Care Excellence guidance.22 We required outcome data on 146 participants per group for 90% power with a 2-sided α of 2.5% (to account for 2 comparisons). We increased this to 169 per group (total sample size, 585 participants) to allow for 25% loss to follow-up.
Statistical Analyses
All participants (including those with missing primary outcome data) were included in the primary analysis according to treatment group allocation, regardless of adherence to their assigned group. For the primary outcome, 2 analyses estimated the mean differences in percentage weight change at 12 months between groups (text messaging with financial incentives group vs control group; and text messaging alone group vs control group) using a linear regression model adjusted for the recruitment areas and recruitment route (general practice or community), with missing data accounted for using multiple imputation under a missing at random assumption. The P value for statistical significance was defined as P < .025. The imputation model used baseline weight, recruitment method, area deprivation quintile using country-specific Index of Multiple Deprivation (eMethods in Supplement 3), recruitment area, height, and age to impute missing weights at 12 months for each group. In sensitivity analyses, analyses were repeated among people with 12-month weight values obtained in person (including video) if on study scales within 23 days of the target date, with missing data imputed using the model above. Additional sensitivity analyses used the same analysis model on all observed data (a missing-completely-at-random assumption) and 2 missing-not-at-random models with either baseline observations carried forward or last observation carried forward (for the intervention groups only). Stata statistical software version 16 was used for all analyses (StataCorp).
Secondary and Exloratory Analyses
Secondary and exploratory outcomes were analyzed in a similar manner as the primary outcome, using a generalized linear model suitable for the outcome distribution and effect sizes presented with 97.5% CIs. Statistical significance was P<.025.
Post Hoc Analyses
An exploratory post hoc analysis repeated the primary analyses after excluding participants who reported taking weight loss medications or meal replacements at any point during the trial.
Results
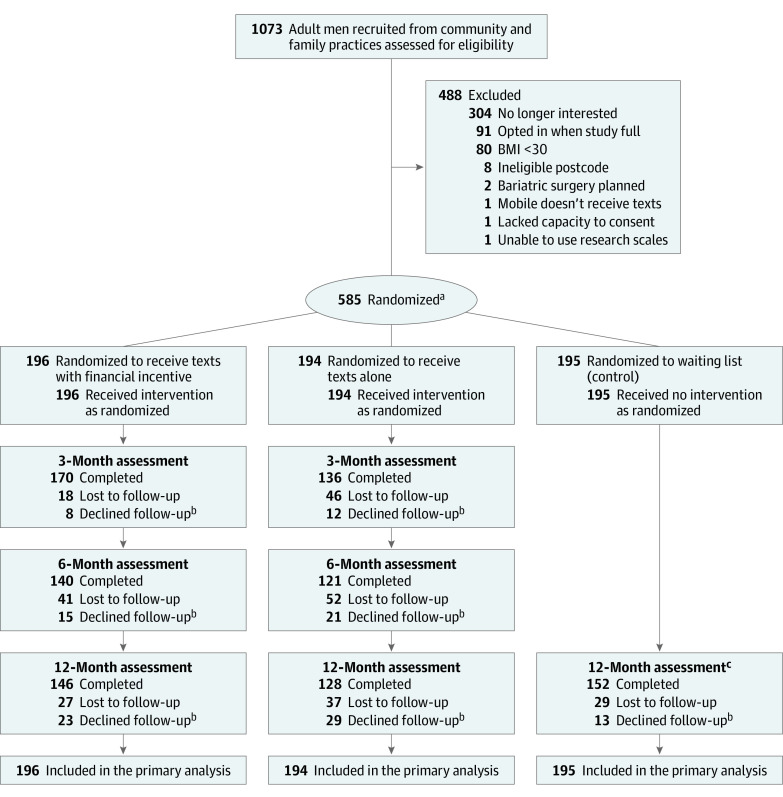
Between July 2021 and May 2022, 1073 men expressed interest in enrolling, of whom 93 were ineligible, 304 declined participation, 91 expressed interest after enrollment was completed, and 585 were randomized: 196 to text messaging with financial incentives group, 194 to text messaging alone group, and 195 to the control group (Figure 1). Weight at 12 months was completed by 426 participants (73%): 146 (75%) in the text messaging with financial incentives group, 128 (66%) in the text messaging alone group, and 152 (78%) in the control group. Overall, 397 (68%) completed the 12-month weight measurement on study scales within 23 days of the target date, consisting of 137 participants (70%) in the text messaging with financial incentives group, including 1 participant who followed up by video; 118 (61%) in the text messaging alone group; and 142 (73%) in the control group (eTable 3 in Supplement 3). Nineteen participants (3%) provided written weight by questionnaire, consisting of 4 in the text messaging with incentives group, 8 in the text messages alone group, and 7 in the control group. Weight assessments at 3 months were completed by 170 men (87%) in the text messaging with financial incentives group and 136 (70%) in the text messaging alone group. Weight assessments at 6 months were completed by 140 men (71%) in the text messages with incentives group compared with 121 (63%) in the text messaging alone group (eTable 4 in Supplement 3). The reasons for the 66 men (11%) declining follow-up were comparable across groups (eTable 5 in Supplement 3).
Figure 1. Participant Flow Through the Game of Stones Study.
aRandomization was stratified by area using permuted blocks of random sizes of 3, 6, or 9.
beTable 5 reports reasons for declining follow-up.
cThere were no 3- or 6-month follow-up sessions for the control group.
Baseline characteristics were similar across trial groups (mean age, 50.7 [SD, 13.3] years; 525 White (90%) (Table 1; eTables 6 and 7 in Supplement 3). Overall, 227 (39%) lived in the 2 more disadvantaged quintile areas, 416 (71%) self-reported an obesity-related health condition, 104 (18%) had diabetes, 235 (40%) had multiple long-term conditions, and 165 (29%) reported a physical or mental health disability (Office for National Statistics definition). The mean body weight was 118.5 (SD, 19.9) kg and the mean BMI was 37.7 (SD, 5.7). More participants were recruited through community strategies (368 [63%]) than through general practices (217 [37%]).
Table 1. Baseline Characteristics.
| Text messages with financial incentives (n = 196) | Text messages alone (n = 194) | Control group (n = 195) | |
|---|---|---|---|
| Recruitment strategya | |||
| General practice, No. (%) | 74 (38) | 79 (41) | 64 (33) |
| Community, No. (%) | 122 (62) | 115 (59) | 131 (67) |
| Age, mean (SD) [No.], yb | 50.0 (12.7) [195] | 51.7 (13.3) [194] | 50.2 (13.9) [195] |
| Deprivation category, No. (%)c | n = 195 | n = 192 | n = 194 |
| Most deprived | 48 (25) | 36 (19) | 50 (26) |
| More deprived | 28 (14) | 37 (19) | 28 (14) |
| Deprived | 25 (13) | 33 (17) | 29 (15) |
| Less deprived | 39 (20) | 40 (21) | 31 (16) |
| Least deprived | 55 (28) | 46 (24) | 56 (29) |
| Ethnic group, No. (%)b | n = 190 | n = 186 | n = 188 |
| Asian/Asian British | 2 (1.1) | 3 (1.6) | 6 (3.2) |
| Black/African/Caribbean/Black British | 3 (1.6) | 3 (1.6) | 3 (1.6) |
| White | 179 (94) | 174 (94) | 172 (92) |
| Mixed or multiple ethnic groups | 2 (1.1) | 4 (2.1) | |
| Other | 3 (1.6) | 3 (1.6) | 2 (1.1) |
| Prefer not to say | 1 (0.5) | 3 (1.6) | 1 (0.5) |
| Relationship status, No. (%)b | n = 193 | n = 191 | n = 190 |
| Married or civil partnership | 126 (64) | 116 (60) | 113 (56) |
| Cohabiting | 25 (13) | 34 (18) | 37 (19) |
| Single (never married; never in a civil partnership) | 30 (16) | 19 (9.8) | 27 (14) |
| Divorced | 5 (2.6) | 8 (4.1) | 6 (3.1) |
| Separated | 5 (2.6) | 6 (3.1) | 3 (1.5) |
| Widowed | 0 | 3 (1.5) | 3 (1.5) |
| Prefer not to say | 2 (1.0) | 5 (2.6) | 1 (0.5) |
| Comorbidities, No. (%)b,d | n = 196 | n = 193 | n = 194 |
| High blood pressure | 93 (47) | 83 (43) | 86 (44) |
| Mental health condition | 51 (26) | 46 (24) | 49 (25) |
| Arthritis | 40 (20) | 55 (28) | 47 (24) |
| Possible latent mental health condition | 50 (26) | 48 (25) | 44 (23) |
| Diabetes | 37 (19) | 38 (20) | 29 (15) |
| Heart condition | 29 (15) | 34 (18) | 28 (14) |
| Stroke (including ministroke) | 9 (4.6) | 3 (1.5) | 8 (4.1) |
| Cancer | 6 (3.1) | 8 (4.1) | 5 (2.6) |
| ≥1 Comorbidity | 136 (69) | 136 (70) | 144 (74) |
| Multiple long-term conditionb | 82 (42) | 82 (42) | 71 (36) |
| Including self-reported diabetesb | 33 (17) | 34 (18) | 23 (12) |
| Physical or mental disabilitya,e | n = 193 | n = 193 | n = 192 |
| Disability, No. (%) | 60 (31) | 47 (24) | 58 (30) |
| Measured weight | n = 196 | n = 194 | n = 195 |
| Weight, mean (SD), kg | 120.3 (20.1) | 117.2 (17.9) | 118.1 (21.6) |
| BMI, mean (SD) | 38.2 (5.9) | 37.3 (4.7) | 37.8 (6.4) |
Abbreviation: BMI, body mass index, calculated as weight in kilograms divided by height in meters squared.
See eTables 6 and 7 in Supplement 3 for more detail.
Self-reported.
To measure disadvantage participant postcodes of residence were looked up in the following country-specific databases and assigned an index of multiple deprivation quintile (see eMethods in Supplement 3): Scotland: https://www.gov.scot/publications/scottish-index-of-multiple-deprivation-2020v2-postcode-look-up; England: https://imd-by-postcode.opendatacommunities.org/imd/2019; Northern Ireland: https://www.nisra.gov.uk/publications/central-postcode-directory-jul-2023-downloads.
In the questionnaire, participants were asked, “Has a doctor ever told you that you have/had? (Please tick all that apply)” followed by the following list of obesity-related conditions: a stroke or ministroke, high blood pressure, a heart condition such as angina or atrial fibrillation, diabetes, cancer, arthritis, a mental health condition, or none of the above. Multiple long-term conditions were defined as ticking 2 or more of the conditions listed above. Derivation of the category a possible latent mental health condition is described in the statistical analysis plan (Supplement 2).
Disability was measured using the Harmonised standards and guidance, Government Statistical Service, Office for National Statistics, 2021. In the questionnaire, participants were asked: “Do you have any physical or mental health conditions or illnesses lasting or expected to last 12 months or more? If you answered, ‘Yes’ to the question above, do any of your conditions or illnesses reduce your ability to carry out day-to-day activities? (Please tick one).” The choices were yes, a lot; yes, a little; or not at all. To be categorized as disabled, participants must have answered yes to the first question and yes to the second question.
Of a maximum of 370 texts over 12 months, the mean number sent to participants was 332.4 (SD, 80.9) in the text messaging with financial incentives group and 317.3 (SD, 100.8) in the text messaging alone group. The mean number of responses to the text messages received was 8.8 (SD, 18.9) in the text messaging with financial incentives group and 8.6 (SD, 33.8) in the text messaging alone group (eTable 8 in Supplement 3). The number of participants who visited the trial website are listed in eTables 9 and 10 in Supplement 3.
A mean of £128 ($159) was paid per participant randomized to text messaging with financial incentives for meeting weight loss goals (eTable 4 in Supplement 3). Of 146 participants who provided a 12-month weight, 90 men (62%) adhering to the payment protocol received payments (eMethods in Supplement 3), with 5 men missing either 3- or 6-month targets but paid for attaining 5% or more weight loss at 12 months. Six participants met 3- and/or 6-month targets of 5% or more but received no money because their 12-month weight was greater than at baseline. Twenty-seven of 196 men (14%) randomized to the text messaging with incentives group received the full £400 ($490).
Primary Outcome
At the 12-month follow-up, the mean (SD) percent weight change was −4.8% (6.1%) for the text messaging with financial incentives group, −2.7% (6.3%) for the text messaging alone group, and −1.3% (5.5%) for the control group. Compared with the control group, the text messaging with incentive group had significantly greater weight loss (mean difference in percentage change from baseline, −3.2%;97.5% CI, −4.6 to −1.9; P < .001), but the text messaging alone group did not have significantly greater weight loss (mean difference in percentage change from baseline, −1.4%; 97.5% CI, −2.9% to −0.0; P = .05; Figure 2; eTable 11 in Supplement 3).
Figure 2. Weight Change and Percent Weight Change From Baseline to 12 Months .
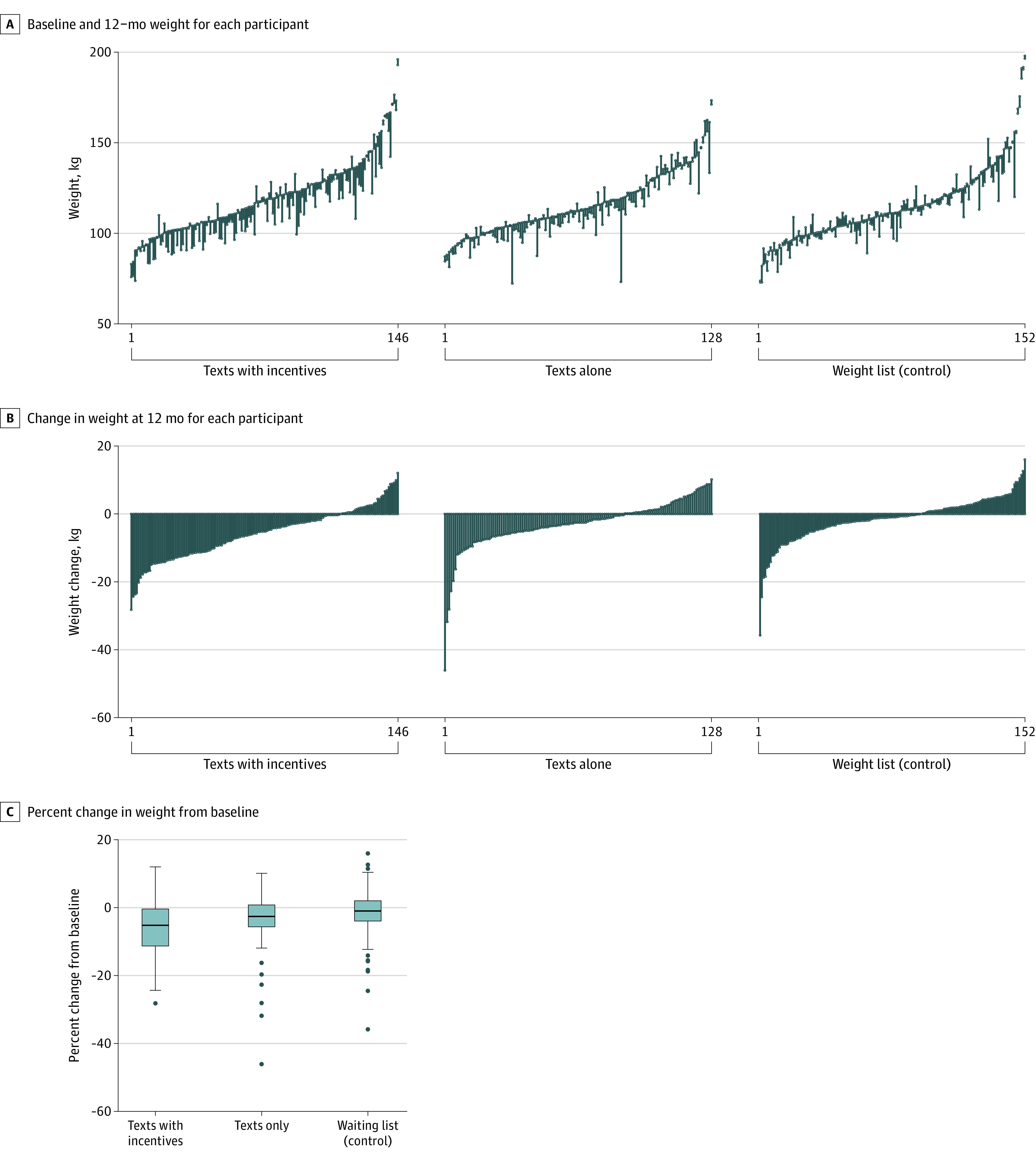
The thick lines in the boxes represent the median; the bottom and top of the box, the first and third quartiles, respectively; whiskers, an additional 1.5 times the IQR lower than the first quartile and higher than the third quartile; and dots, more extreme values that lie outside 1.5 times the IQR.
Secondary Outcomes
Participants lost a mean (SD) of 5.7 (7.4) kg in the text messaging with financial incentives group, 3.0 (7.5) kg in the text messaging alone group, and 1.5 (6.5) kg in the control group (eTable 12 in Supplement 3). At the 12-month follow-up, 114 of 146 participants (78%) in the text messaging with financial incentives group lost some weight compared with 86 of 128 (67%) in the text messaging alone group, and 92 of 152 (61%) in the control group (Table 2). At least 5% weight loss was attained by 65 of 146 participants (45%) in the text messaging with financial incentives group compared with 32 of 128 (25%) in the text messaging alone group and 28 of 152 (18%) in the control group. Compared with the control group, the odds ratio (OR) for weight loss of at least 5% in the text messaging with incentive group was 3.6 (97.5% CI, 2.0-6.6; P<.001). For the text messaging alone group compared with the control group, the OR was 1.5 (97.5% CI, 0.8-2.9; P=.2). At least 10% weight loss was attained by 40 of 146 (27%) in the text messaging with financial incentives group, 8 of 128 (6%) in the text messaging alone group, and 11 of 152 (7%) in the control group. Figure 3 shows weight loss over time with weight outcomes at 3 and 6 months (eTable 13 in Supplement 3). There were no statistically significant differences in EQ-5D-5L; EQ-5D-5L-AD; WEMWBS; PHQ-4; WSSQ scores between the text messaging with financial incentives group and the control group or between the text messaging alone group and the control group (eTable 14 in Supplement 3). Data for the PHQ-4 scores were missing for 291 participants, 163 of whom did not receive the question at baseline. Those in the text messaging with financial incentives group significantly improved the EQ-5D visual analogue scale score by 5.00 (97.5% CI, 0.76 to 9.25; P = .008) compared with the control group. The text messaging alone group improved the EQ-5D visual analog scale score by 3.71 (97.5% CI, −0.75 to 8.16, P = .06) compared with the control group, but the difference was not statistically significant.
Table 2. Secondary Outcomes at 12 Months.
| Weight at 12 mo | Texts with incentives (n = 146) | Texts alone (n = 128) | Waiting list control (n = 152) | Risk differences (97.5% CI) | Odds ratios (97.5% CI) [P value] | ||||
|---|---|---|---|---|---|---|---|---|---|
| Texts with incentives vs control | Texts alone vs control | Texts with incentives vs control | P value | Texts alone vs control | P value | ||||
| Weight loss | |||||||||
| Any weight loss, % | 114 (78) | 86 (67) | 92 (61) | 17 (5.6 to 29)a | 6.2 (6.6 to 19)a | 2.3 (1.3 to 4.2)a | .001 | 1.3 (0.7 to 2.3)a | .28 |
| ≥5 | 65 (45) | 32 (25) | 28 (18) | 26 (15 to 38)a | 6.9 (4.2 to 18)a | 3.6 (2.0 to 6.6)a | <.001 | 1.5 (0.8 to 2.9)a | .16 |
| ≥10 | 40 (27) | 8 (6.3) | 11 (7.2) | 20 (11 to 30)a | −0.8 (−5.9 to 7.6)a | 4.9 (2.2 to 11.1)a | <.001 | 0.9 (0.3 to 2.6)a | .78 |
| Weight change categories, No. (%) | |||||||||
| Gain | 32 (22) | 42 (33) | 60 (39) | 3.2 (2.0 to 5.3)b | <.001 | 1.3 (0.8 to 2.2)b | .20 | ||
| Loss, % | |||||||||
| 0 to 5 | 49 (34) | 54 (42) | 64 (42) | ||||||
| ≥5 to <10 | 25 (17) | 24 (19) | 17 (11) | ||||||
| ≥10 | 40 (27) | 8 (6.3) | 11 (7.2) | ||||||
Odds ratio from a binary logistic regression, adjusting for area and method of recruitment and using all observed outcome data, the absolute risk difference and confidence intervals were also estimated from this model and presented as a percentage.
Odds ratio from an ordered categories logistic regression adjusting for area and method of recruitment and using all observed outcome data.
Figure 3. Weight Change in Kilograms Over Time .
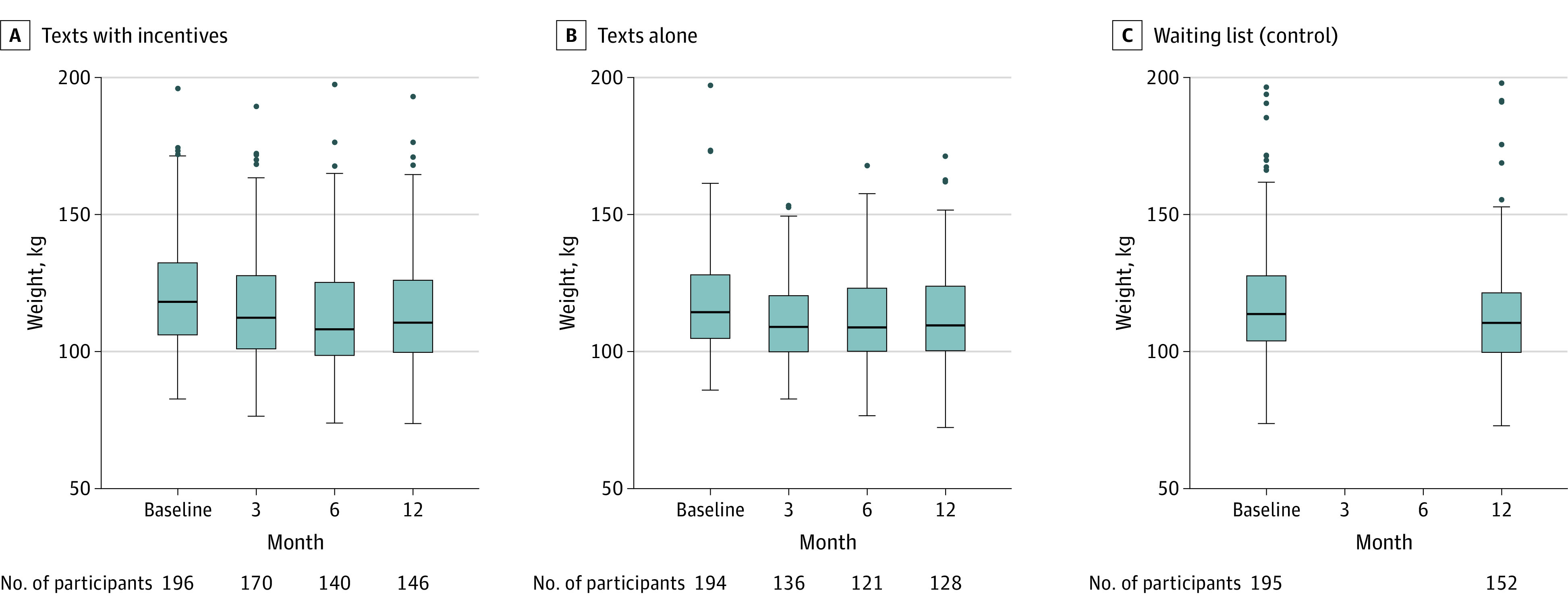
The thick lines in the boxes represent the median; the bottom and top of the box, the first and third quartiles, respectively; whiskers, an additional 1.5 times the IQR lower than the first quartile and higher than the third quartile; and dots, more extreme values that lie outside 1.5 times the IQR.
Number Needed to Treat
For the outcome of weight loss of 5% or more, the number needed to treat for the text messaging with financial incentives group at 12 months was 4 (97.5% CI, 3-8), for a weight loss of 10% or more, 5 (97.5% CI, 4-10). The number needed to treat with text messaging alone for a weight loss of 5% or more at 12 months was 15 (97.5% CI, NNT[harm] 33 to ∞ to NNT[benefit] 6) and for ≥10% weight loss it was NNT[harm] 102 (97.5% CI, NNT[harm] 15 to ∞ to NNT[benefit] 18).
Exploratory Outcomes
Compared with the control group, the text messaging with financial incentives group significantly improved the satisfaction scale by 18.6 (97.5% CI, 11.4-25.8; P < .001) and the text messaging alone group improved the satisfaction scale by 10.3 points (97.5% CI, 2.7-17.8; P = .002; eTable 15 in Supplement 3). Compared with the control group, the text messaging with financial incentives group significantly improved satisfaction with weight loss by 1.7 (97.5% CI, 1.0-2.6; P = .02) and the text messaging alone group improved the satisfaction scale for weight loss by 1.3 points (97.5% CI, 0.8-2.1; P = .18).
Sensitivity Analyses
All sensitivity analyses for missing data are reported in eTable 16 in Supplement 3. In analyses limited to participants weighed on study scales within 23 days of the target date (in person or video) compared with the control group, the text messaging with financial incentives group changed percentage weight by −3.6% (97.5% CI, −5.2% to −2.0%; P < .001) and the text messaging alone group changed percentage weight by −1.5% (97.5% CI, −3.2% to 0.2%; P = .05).
Post Hoc Analyses
Fifty-one participants reported taking weight-loss medications, including injectable therapies or meal replacements (eTable 17 in Supplement 3). In a post hoc exploratory analysis for which the observed 12-month follow-up data for these 51 participants were removed and then imputed, text messaging with financial incentives significantly improved weight loss compared with the control group (mean difference, −2.7%; 97.5% CI, −4.2% to −1.1%; P = .001), whereas the text messaging alone group was not significantly different compared with the control group (mean difference, −1.1%; 97.5% CI, −2.7% to 0.5%; P = .19; eFigure 1 and eTable 18 in Supplement 3).
Adverse Events
Overall, 366 adverse events were reported including 83 infections (23%), 58 social harms (17%, eg, bereavement, employment problems, illness of a family member, relationship problems); and 39 musculoskeletal and connective tissue adverse events (11%); 160 adverse events (44%) were in the text messaging with financial incentives group, 137 (37%) in the text messaging alone group, and 69 (19%) in the control group. Of the 366 adverse events, 23 (6.3%) were classified as serious adverse events, including 12 (52%) in the texts messaging with incentives group; 5 (22%) in the texts messaging alone group, and 6 (26%) in the control group. None were considered associated with participation in the clinical trial (eTables 19-22 in Supplement 3).
Discussion
In this randomized clinical trial involving 585 men with obesity, behavioral text messages combined with financial incentives reduced weight by 3.2% compared with a control group. Text messaging alone did not significantly reduce weight compared with the control group. This study included 39% of men from lower socioeconomic backgrounds who have typically been under represented in clinical trials of weight loss in people with obesity.23
Although 5% weight loss is typically considered clinically meaningful, some evidence has suggested that weight loss of less than 5% may be clinically important.24,25 Providing participants with cash that they could retain if they met study goals may have facilitated enrollment of participants with lower incomes, in contrast to deposit contract financial incentives where participants risk losing their own money.10,11 Including men with obesity living in disadvantaged areas in making decisions about the design of the incentives, number of assessments, goals, and text messages16,17 may have contributed to the effectiveness of the text messaging with the financial incentives intervention. A meta-analysis recommended 12 in-person contacts for individual or group behavioral weight-management interventions.26 In addition, NICE (National Institute for Health and Care Excellence)27 recommends weekly or fortnightly sessions, including a weigh-in at each weight management session, for at least 3 months. In contrast, interventions for the current study included 4 weight assessments, which could reduce costs and burden for participants and staff.
Limitations
This study had several limitations. First, generalizability to women, diverse ethnic groups, people without mobile phone access, and people with low literacy, poor vision, or inability to attend weight assessments is uncertain. Second, the drop-out rate was higher among men in the group with text messaging alone compared with the other 2 groups. Third, weight regain is common following weight loss trials and may be greater for financial incentive interventions.28 Follow-up weight beyond 12 months is not yet available for this study. Fourth, because the clinical trial did not include a 2 × 2 factorial design, it is not possible to know whether text messaging with financial incentives was more effective than financial incentives alone in this population. Fifth, harms were collected more frequently in the intervention groups than in the control group and might have influenced rates of adverse events.
Conclusions
Among men with obesity, a text-messaging with an endowment financial incentive intervention significantly improved weight loss compared with a control group; however, text messaging alone was not significantly better than the control condition. These findings support text messaging combined with financial incentives to attain weight loss in men with obesity.
Educational Objective: To identify the key insights or developments described in this article.
-
This study sought to assess whether text messaging combined with financial incentives could help men lose weight. How were participants recruited to the program?
A combination of letters to family practices and community notifications including leaflets, posters, social media, and word of mouth.
From online advertising keyed to searches for bariatric surgery, high-carbohydrate foods, and diet advice.
Through referral from medicated and surgical weight loss programs.
-
The group assigned to text messaging and financial incentives had awards allocated based on weight loss goals at 3 months, 6 months, and 12 months. How much money did participants in this group receive?
All men received a minimum payment of £50 ($64) because all men made the early 3-month weight target but only 27 also met the 12-month goal and obtained the full payment of £400 ($490).
A mean of £128 ($159) per participant.
Ninety-eight men (50%) received the full £400 ($490) possible.
-
What was the result for the primary outcome of percent weight change at 12 months?
All groups lost ≥5% of body weight, an amount typically considered clinically meaningful.
Both text messaging groups experienced statistically significant weight loss compared with the control group, regardless of financial incentives.
Only the text messaging plus financial incentive group lost a statistically significant amount of weight compared with the control group.
Trial Protocol
Statistical Analysis Plan
eTable 1. Sample texts for baseline, 3 months, 6 months and 9 months
eTable 2. Texts sent to participants in texts within incentive group following weight measurements
eTable 3. Weight assessment methods for men retained in the trial at 12 months
eTable 4. Weight loss targets met by intervention groups between baseline and 12 months
eTable 5. Reasons for declining follow-up
eTable 6. Baseline characteristics by treatment allocation
eTable 7. Baseline characteristics by recruitment strategy
eTable 8. Text messages delivered and replied to by intervention group participants
eTable 9. Post-randomization website engagement by all trial participants over 12 months
eTable 10. Intervention group engagement with website self-monitoring and local resources webpage over 12 months
eTable 11. Primary outcome: percentage weight change at 12 months from baseline
eTable 12. Weight change in kilograms at 12 months from baseline
eTable 13. Weight change at 3 months and 6 months from baseline for intervention groups
eTable 14. Secondary outcomes by trial group
eTable 15. Participant satisfaction with the Game of Stones trial and weight loss progress at 12 months
eTable 16. Sensitivity analyses for the primary outcome
eTable 17. Use of publicly funded weight loss services, weight loss medications or meal replacements in previous 12 months
eTable 18. Sensitivity analyses for participants not taking weight loss medications or meal replacements
eTable 19. Harms reported by participants since last seen
eTable 20. Participants reporting or harms at one or more time point
eTable 21. MedDRA System Organ Classification of harms
eTable 22. Unexpected benefits reported by participants.
eFigure. Sensitivity analysis for participants not taking weight loss medications or meal replacements
eMethods
Data Sharing Statement
Footnotes
eTable 1 in Supplement 3 provides more examples of daily text messages and the embedded behavior change techniques; eTable 2 in Supplement 3 provides more examples of the automated texts with {algorithms} for the money secured and lost following each weight assessment.
References
- 1.World Health Organization . WHO acceleration plan to stop obesity. Published July 3, 2023. Accessed February 20, 2024. https://www.who.int/publications/i/item/9789240075634
- 2.Afshin A, Forouzanfar MH, Reitsma MB, et al. ; GBD 2015 Obesity Collaborators . Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13-27. doi: 10.1056/NEJMoa1614362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Obesity profile: short statistical commentary May 2023. Office for Health Improvement and Disparities . Published May 3, 2023. Accessed February 20, 2024. https://www.gov.uk/government/statistics/obesity-profile-update-may-2023/obesity-profile-short-statistical-commentary-may-2023
- 4.Knowlden AP, Wilkerson AH, Dunlap KB, Stellefson M, Elijah OA. Systematic review of electronically delivered behavioral obesity prevention interventions targeting men. Obes Rev. 2022;23(9):e13456. doi: 10.1111/obr.13456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMahon J, Thompson DR, Pascoe MC, Brazil K, Ski CF. eHealth interventions for reducing cardiovascular disease risk in men: a systematic review and meta-analysis. Prev Med. 2021;145:106402. doi: 10.1016/j.ypmed.2020.106402 [DOI] [PubMed] [Google Scholar]
- 6.Robertson C, Avenell A, Boachie C, et al. Should weight loss and maintenance programmes be designed differently for men? a systematic review of long-term randomised controlled trials presenting data for men and women: the ROMEO project. Obes Res Clin Pract. 2016;10(1):70-84. doi: 10.1016/j.orcp.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 7.Skinner R, Gonet V, Currie S, Hoddinott P, Dombrowski SU. A systematic review with meta-analyses of text message-delivered behaviour change interventions for weight loss and weight loss maintenance. Obes Rev. 2020;21(6):e12999. doi: 10.1111/obr.12999 [DOI] [PubMed] [Google Scholar]
- 8.Ananthapavan J, Peterson A, Sacks G. Paying people to lose weight: the effectiveness of financial incentives provided by health insurers for the prevention and management of overweight and obesity—a systematic review. Obes Rev. 2018;19(5):605-613. doi: 10.1111/obr.12657 [DOI] [PubMed] [Google Scholar]
- 9.Ali R, Ho TH, Lim N, et al. Cash incentives for weight loss work only for males. Behav Public Policy. 2021;8(2):279-299. [Google Scholar]
- 10.Sykes-Muskett BJ, Prestwich A, Lawton RJ, Armitage CJ. The utility of monetary contingency contracts for weight loss: a systematic review and meta-analysis. Health Psychol Rev. 2015;9(4):434-451. doi: 10.1080/17437199.2015.1030685 [DOI] [PubMed] [Google Scholar]
- 11.Boonmanunt S, Pattanaprateep O, Ongphiphadhanakul B, et al. Evaluation of the effectiveness of behavioral economic incentive programs for goal achievement on healthy diet, weight control and physical activity: a systematic review and network meta-analysis. Ann Behav Med. 2023;57(4):277-287. doi: 10.1093/abm/kaac066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glanz K, Shaw PA, Kwong PL, et al. Effect of financial incentives and environmental strategies on weight loss in the healthy weigh study: a randomized clinical trial. JAMA Netw Open. 2021;4(9):e2124132. doi: 10.1001/jamanetworkopen.2021.24132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Macaulay L, O’Dolan C, Avenell A, et al. Effectiveness and cost-effectiveness of text messages with or without endowment incentives for weight management in men with obesity (Game of Stones): study protocol for a randomised controlled trial. Trials. 2022;23(1):582. doi: 10.1186/s13063-022-06504-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dombrowski SU, McDonald M, van der Pol M, et al. Game of Stones: feasibility randomised controlled trial of how to engage men with obesity in text message and incentive interventions for weight loss. BMJ Open. 2020;10(2):e032653. doi: 10.1136/bmjopen-2019-032653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McDonald MD, Dombrowski SU, Skinner R, et al. ; Game of Stones team . Recruiting men from across the socioeconomic spectrum via GP registers and community outreach to a weight management feasibility randomised controlled trial. BMC Med Res Methodol. 2020;20(1):249. doi: 10.1186/s12874-020-01136-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dombrowksi SU, McDonald M, Van Der Pol M, et al. Text messaging and financial incentives to encourage weight loss in men with obesity: the Game of Stones feasibility RCT. Public Health Res (Southampt). 2020;8(11). [Google Scholar]
- 17.van der Pol M, McDonald M, Collacott H, et al. Designing financial incentives for health behaviour change: a mixed-methods case study of weight loss in men with obesity. J Public Health (Berl). 2022;32:65-77. doi: 10.1007/s10389-022-01785-1 [DOI] [Google Scholar]
- 18.Schwarzer R, Luszczynska A. How to overcome health-compromising behaviors: the health action process approach. Eur Psychol. 2008;13(2):141-151. doi: 10.1027/1016-9040.13.2.141 [DOI] [Google Scholar]
- 19.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68-78. doi: 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 20.Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev. 2016;10(3):277-296. doi: 10.1080/17437199.2016.1151372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Classifications and harmonisation. Office for National Statistics . Accessed February 20, 2024. https://www.ons.gov.uk/methodology/classificationsandstandards
- 22.Obesity: identification, assessment and management: clinical guideline. National Institute for Health and Care Excellence . Published November 27, 2014. Accessed February 20, 2024. Updated July 26, 2023. https://www.nice.org.uk/guidance/cg189
- 23.McDonald MD, Hunt K, Sivaramakrishnan H, et al. A systematic review examining socioeconomic factors in trials of interventions for men that report weight as an outcome. Obes Rev. 2022;23(7):e13436. doi: 10.1111/obr.13436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;320(11):1172-1191. doi: 10.1001/jama.2018.7777 [DOI] [PubMed] [Google Scholar]
- 25.Hartmann-Boyce J, Theodoulou A, Oke JL, et al. Long-term effect of weight regain following behavioral weight management programs on cardiometabolic disease incidence and risk: systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2023;16(4):e009348. doi: 10.1161/CIRCOUTCOMES.122.009348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Madigan CD, Graham HE, Sturgiss E, et al. Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2022;377:e069719. doi: 10.1136/bmj-2021-069719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weight management: lifestyle services for overweight or obese adults. National Institute for Health and Care Excellence. Published May 28, 2014. Accessed April 24, 2024. https://www.nice.org.uk/guidance/ph53
- 28.Hartmann-Boyce J, Theodoulou A, Oke JL, et al. Association between characteristics of behavioural weight loss programmes and weight change after programme end: systematic review and meta-analysis. BMJ. 2021;374:n1840. doi: 10.1136/bmj.n1840 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
Statistical Analysis Plan
eTable 1. Sample texts for baseline, 3 months, 6 months and 9 months
eTable 2. Texts sent to participants in texts within incentive group following weight measurements
eTable 3. Weight assessment methods for men retained in the trial at 12 months
eTable 4. Weight loss targets met by intervention groups between baseline and 12 months
eTable 5. Reasons for declining follow-up
eTable 6. Baseline characteristics by treatment allocation
eTable 7. Baseline characteristics by recruitment strategy
eTable 8. Text messages delivered and replied to by intervention group participants
eTable 9. Post-randomization website engagement by all trial participants over 12 months
eTable 10. Intervention group engagement with website self-monitoring and local resources webpage over 12 months
eTable 11. Primary outcome: percentage weight change at 12 months from baseline
eTable 12. Weight change in kilograms at 12 months from baseline
eTable 13. Weight change at 3 months and 6 months from baseline for intervention groups
eTable 14. Secondary outcomes by trial group
eTable 15. Participant satisfaction with the Game of Stones trial and weight loss progress at 12 months
eTable 16. Sensitivity analyses for the primary outcome
eTable 17. Use of publicly funded weight loss services, weight loss medications or meal replacements in previous 12 months
eTable 18. Sensitivity analyses for participants not taking weight loss medications or meal replacements
eTable 19. Harms reported by participants since last seen
eTable 20. Participants reporting or harms at one or more time point
eTable 21. MedDRA System Organ Classification of harms
eTable 22. Unexpected benefits reported by participants.
eFigure. Sensitivity analysis for participants not taking weight loss medications or meal replacements
eMethods
Data Sharing Statement