Abstract
Background and Aim:
Infant mortality is a widely reported indicator of population health and a leading public health concern. In this systematic review and meta-analysis, we review the available literature for epidemiologic evidence of the association between short-term air pollution exposure and infant mortality.
Methods:
Relevant publications were identified through PubMed and Web of Science databases using comprehensive search terms and screened using predefined inclusion/exclusion criteria. We extracted data from included studies and applied a systematic rubric for evaluating study quality across domains including participant selection, outcome, exposure, confounding, analysis, selective reporting, sensitivity, and overall quality. We performed meta-analyses, using both fixed and random-effect methods, and estimated pooled odds ratios (ORs) and 95 % confidence intervals (95%CI) for pollutants (nitrogen dioxide (NO2), sulfur dioxide (SO2), coarse particulate matter (PM10), fine particulate matter (PM2.5), ozone (O3), carbon monoxide (CO)) and infant mortality, neonatal mortality, or postneonatal mortality.
Results:
Our search returned 549 studies. We excluded 490 studies in the abstract screening phase and an additional 37 studies in the full text screening phase, leaving 22 studies for inclusion. Among these 22 studies, 14 included effect estimates for PM10, 13 for O3, 11 for both NO2 and CO, 8 for SO2, and 3 for PM2.5. We did not calculate a pooled OR for PM2.5 due to the limited number of studies available and demonstrated heterogeneity in the effect estimates. The pooled ORs (95%CI) with the greatest magnitudes were for a 10-ppb increase in SO2 or NO2 concentration in the days before death (1.07 [95%CI: 1.02, 1.12], 1.04 [95%CI: 1.01, 1.08], respectively). The pooled OR for PM10 was 1.02 (95%CI: 1.00, 1.03), and the pooled ORs for CO and O3 were 1.01 (95%CI: 1.00, 1.02) and 0.99 (95%CI: 0.97, 1.01).
Conclusions:
Increased exposure to SO2, NO2, PM10, or CO is associated with infant mortality across studies.
Keywords: Air pollution, Infant mortality, Systematic review, Meta-analysis, Short-term
1. Introduction
Infant mortality is a widely reported indicator of population health and a leading public health concern. Generally, infant mortality is defined as a death occurring in the first year of life and is commonly divided into two sub-types: neonatal mortality (i.e., death during the first 28 days) and postneonatal mortality (i.e., death after day 28 of life and before 1 year of age). About two-thirds of infant deaths occur in the neonatal period (NCHS, 2023). Birth defects are the most common cause of infant mortality, accounting for about 21 % of infant deaths, while sudden infant death syndrome (SIDS) accounts for about 6 % of infant deaths (Ely and Driscoll, 2021). Associations between environmental quality, especially air pollution, and infant deaths suggest that environmental pollutants may also play a role in the etiology of infant mortality (Patel et al., 2018).
There are well-documented associations between short-term exposure to air pollution (on the order of hours to days) and respiratory and cardiovascular health effects, as well as mortality. For example, short-term exposure to fine particulate matter (PM2.5) causes mortality in adults (U.S. EPA, 2019), though the evidence is less certain for other criteria pollutants (e.g., ozone (O3), nitrogen dioxide (NO2), sulfur dioxide (SO2), and carbon monoxide (CO)). Compared to the extensive body of evidence that has evaluated the association between short-term air pollution exposure and mortality among adults, the number of studies that has evaluated infant mortality is relatively few. Though infant mortality rates have been declining in the United States (U.S.) –5.58 per 1000 live births in 2019, the lowest reported rate in U.S. history (Ely and Driscoll, 2021) – U.S. rates of infant mortality are among the highest of high-income countries (Thakrar et al., 2018).
Short-term exposure to air pollutants can result in respiratory tract inflammation and oxidative stress (Gong et al., 2005) or activation of sensory nerves that modulate the autonomic nervous system (ANS) (Ghelfi et al., 2008). Inflammatory mediators (e.g., cytokines) produced in the respiratory tract can enter the bloodstream, where they may amplify an initial inflammatory response (Steenhof et al., 2014; Delfino et al., 2009), leading to a variety of downstream effects including coagulation (Croft et al., 2017; Strak et al., 2013), thrombosis (Lucking et al., 2011), impaired vascular function (Ljungman et al., 2014; Madrigano et al., 2010), and ischemia (Delfino et al., 2011). Epidemiologic studies provide evidence for associations between short-term air pollution exposure and respiratory effects (e.g., asthma exacerbations), cardiovascular effects (e.g., heart attacks), some birth outcomes (e.g., preterm birth), and mortality. There is a relatively large and growing body of evidence for associations between short-term air pollution exposure and mortality among adults, including older adults. The evidence for infant mortality is relatively sparse in comparison. Given the potential for a biological mechanism by which air pollution exposure could trigger an acute response that contributes to infant mortality and the relatively limited evidence characterizing such associations, an examination of the relationship between short-term air pollution exposure and infant mortality may help to better characterize the role of short-term air pollution exposure in the etiology of infant mortality.
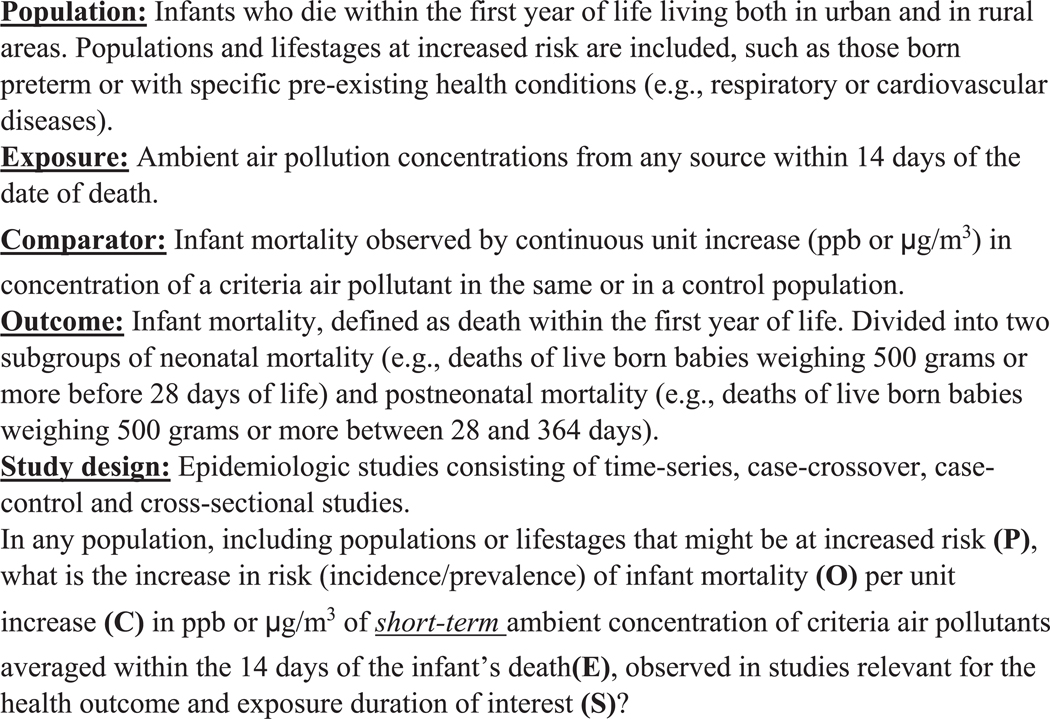
In this systematic review and meta-analysis, we summarize and evaluate the available literature for epidemiologic evidence of the association between short-term criteria air pollution exposure and infant mortality. Relevant publications were identified through PubMed and Web of Science databases using comprehensive search terms. Articles were chosen based on an established Population, Exposure, Comparison, Outcome, Study Design (PECOS) statement (Morgan et al., 2018) that specified the inclusion and exclusion criteria shown in Fig. 1.
Fig. 1.
Population, Exposure, Comparator, Outcome, Study Design (PECOS) statement used to define scope of systematic review.
2. Methods
2.1. Data sources and searches
We searched PubMed and Web of Science literature databases, without beginning time restriction through May 24, 2022, using combinations of keywords related to air pollution and infant mortality. Keywords for exposure included “air pollution”, “particulate matter”, “ozone”, “PM2.5”, “O3”, “NO2”, “nitrogen dioxide”, “nitrogen oxide”, “sulfur dioxide”, “SO2”, and “carbon monoxide”, while keywords for the outcome included “infant mortality”, “neonatal mortality”, “post neonatal mortality”, “perinatal mortality”, and “SIDS”. Exact search terms used to query each database are provided in supplemental materials (Supplemental Table S1). In addition, the reference lists of included studies were screened for any potentially relevant studies not previously identified in this review.
2.2. Study selection
After duplicate studies were removed from the initial query results, two investigators (TL, FN, KP, AW, SZ) independently performed title and abstract screening using SWIFT-ActiveScreener (SWIFT-AS; Howard et al., 2020). The same two investigators did not screen each title and abstract; five investigators performed title-abstract screening and each title and abstract was screened by at least two independent investigators. We excluded studies if they did not examine short-term exposure (i.e., days to weeks) to a criteria air pollutant, did not examine infant mortality as an outcome, were not time-series, case-crossover, case-control, or cross-sectional study design, were literature reviews or abstract-only, or were not English language. Studies with unclear designations were kept for full-text screening. Full-text screening relied on a scoping tool to explicitly define the relevant Population, Exposure, Comparison, Outcome and Study design (PECOS; Fig. 1) serving as criteria for inclusion/exclusion decisions. Two investigators (TL, AK, KP, AW, SZ) then performed a full-text screen using the PECOS statement to retain studies assessing continuous exposure to a criteria air pollutant during the first year of life (either during the neonatal period (first 30 days after birth), postneonatal period (between 1 month and 1 year after birth), or the during the first year after birth). The same two investigators did not screen each full text; five investigators performed full text screening and each full text was screened by at least two independent investigators. Studies that solely considered gestational exposure only were excluded.
2.3. Data extraction
Data from included studies were extracted into a spreadsheet independently by two investigators (TL, AW). Extracted information included: study design, cohort or study name, study population details (e.g., registry or vital records), study size, study location, timing of study, definition of infant mortality used, exposure assessment method, exposure timing, air pollution averaging method (e.g., 8 h-max, 24 h avg., etc.), distribution of air pollution concentrations, confounders examined, co-pollutant correlations, multi-pollutant models evaluated and with which co-pollutants, effect measure, exposure contrast/increment, effect estimates, upper and lower confidence bounds, and modifiers or sub-strata examined. We requested quantitative results from the authors when articles indicated that analyses were performed but were not reported in the manuscript or supplemental materials or were only presented in figures.
2.4. Study quality evaluation
Using a modified Office of Health Assessment and Translation framework (Rooney et al., 2014), we developed guidance for evaluating study quality across domains including participant selection, outcome, exposure, confounding, analysis, selective reporting, sensitivity, and overall quality. Quality levels for individual domains were “good”, “adequate”, “deficient”, and “critically deficient” for all domains except sensitivity, which had levels of “adequate” or “deficient” only. Overall quality was rated as “high confidence”, “medium confidence”, “low confidence”, or “uninformative”. Guidance tables are presented in supplemental materials (Supplemental Table S2). Each study was independently evaluated by two investigators (TL, AK, AW, SZ), notes and decisions were extracted into the Health Assessment Workspace Collaborative (HAWC) tool (Shapiro et al., 2018), and any conflicts were resolved in group discussion, with one investigator making the final decision (KR). The same two investigators did not conduct study quality evaluations for each study; four investigators conducted study quality evaluations and each study quality evaluation was conducted by at least two independent investigators.
2.5. Statistical analysis
For the purposes of meta-analysis, a single effect estimate was selected from each study and standardized to an incremental increase in exposure (1 ppm for CO, 10 μg/m3 for PM10 and PM2.5, 10 ppb for O3, NO2, SO2); preferentially, we chose the estimate that included the full study population from Gouveia and Junger (2018). Different sub-types of infant mortality were reported across the included studies. There were insufficient numbers of effect estimates for us to conduct meta-analyses on different infant mortality sub-types. We preferentially chose all infant mortality, then postneonatal mortality, then neonatal mortality. If the only sub-type of infant mortality included in a study was SIDs, it was selected for inclusion in the meta-analysis. When different lag days of exposure were reported across studies, we preferentially chose effect estimates for the average of 1–3 days, or the lag closest to this. Because few studies reported co-pollutant adjusted effect estimates, we only used effect estimates from single pollutant models. Effect estimates were standardized to reflect an incremental increase by dividing natural logged effect estimates (and confidence limits) by the original exposure increment reported in the manuscript, multiplying by 1 (for CO) or 10 (for all other pollutants) and exponentiating the product.
We then performed meta-analyses, using both fixed and random-effect methods, and estimated pooled odds ratios (OR) and 95 % confidence intervals (95 % CI) for infant mortality and each criteria pollutant for which there were at least four studies with effect estimates using the metafor package in R with RStudio (Allaire, 2012; Team, 2013; Viechtbauer, 2010). When observed heterogeneity was above “moderate” (I2 > 40 %) and statistically significant (Cochran’s Q, alpha 0.05), random effects were presented. We also estimated 95 % prediction intervals for each pollutant-outcome pair – these convey where we expect to see future study results given the observed results.
Publication bias was assessed through funnel plots and Egger’s regression tests, and when appropriate, trim and fill methods were used to assess the potential impact of publication bias. Leave-one-out analyses were performed as sensitivity analyses to identify potential outliers and influential studies.
We conducted sensitivity analyses using fixed effects methods and estimated pooled ORs and 95 % CI for sub-types of infant mortality and each criteria pollutant for which there were at least four studies with effect estimates.
3. Results
Fig. 2 presents the literature flow diagram for study inclusion. Our search of PubMed and Web of Science databases returned 589 studies. In the abstract screening phase, we excluded 525 studies for either not meeting the criteria of examining ambient air pollution (k = 171), not examining infant mortality (k = 213), or having a study design outside of consideration (k = 168); this left 64 studies. In the process of full-text screening, 21 studies were excluded based on study design, exposure period, not including air pollution as the main exposure, or not including infant mortality. An additional 21 studies were excluded from this systematic review because they evaluated long-term exposure, and not short-term exposure. Twenty-two studies were identified for inclusion (Carbajal-Arroyo et al., 2011; Chen et al., 2021; Currie et al., 2009; Dales et al., 2004; Gouveia and Junger, 2018; Greenberg et al., 1973; Hajat et al., 2007; He et al., 2022; Hwang et al., 2019; Klonoff-Cohen et al., 2005; Lin et al., 2004; Litchfield et al., 2018; Loomis et al., 1999; Ritz et al., 2006; Romieu et al., 2004; Scheers et al., 2011; Son et al., 2008; Tsai et al., 2006; Wang et al., 2019; Yang et al., 2006; Yorifuji et al., 2016). In reviewing references of included studies, it was determined that any potentially relevant references had been identified during the initial screening process and were excluded or included appropriately; no additional studies were identified by screening cited references in included studies.
Fig. 2.
Flow chart of study inclusion for systematic review and meta-analysis of short-term air pollution exposure and infant mortality.
Two of the studies identified for inclusion (Greenberg et al., 1973; Klonoff-Cohen et al., 2005) could not be included in the meta-analyses because they provided effect estimates for categorical exposures only, which could not be combined with effect estimates from other studies in the meta-analysis. Two additional studies provided quantitative results but could not be included in the meta-analyses. Wang et al. (2019) provided results in figures only and Son et al. (2008) did not include the unit increase associated with the effect estimates. We attempted to contact the corresponding authors from each of these studies requesting additional information but have not received a response.
3.1. Study quality evaluation
A summary of study evaluations is presented in Fig. 3 and additional details can be obtained by accessing the HAWC project page at https://hawcprd.epa.gov/assessment/100500287/. One study received an overall rank of high confidence, with the rest receiving ranks of medium (k = 4) or low confidence (k = 15) overall (Fig. 3). In individual domains, deficient metric scores were often due to a lack of stated reasoning or underlying information within the text. Several lower scores were due to restrictions of the data, for example, exposure assessment scores were frequently lower when a single home residence from the time of birth was used to assign postnatal exposure without knowledge of residential mobility between infant birth and infant death.1
Fig. 3.
Study quality evaluation visualization showing metric scores for individual domains and confidence score for overall quality for studies with quantitative results.
3.2. Overall confidence
We also evaluated the overall confidence in the body of evidence (Table 1). We found no factors that were influential enough to decrease or increase overall confidence, leading to a final designation of moderate overall confidence. In general, we believe that in evaluating causality, inference should be drawn across multiple lines of evidence, for example across epidemiology, toxicology, and human exposure studies (when possible). While we rate our overall confidence here, it is important to note that this is for the studies included on the very specific topic of interest.
Table 1.
Evaluation of overall confidence in body of evidence.
| Initial confidence by key features of study design | Factors increasing confidence | Factors decreasing confidence | Confidence in the body of the evidence |
|---|---|---|---|
| Moderate Features: exposure occurs prior to outcome, individual outcome data, and comparison groups used | Risk of Bias – no studies were uninformative, half were considered low confidence, and half were medium to high (1) confidence (=) | Residual confounding – studies examining co-pollutant confounding did not observe an impact on observed associations. Not possible to evaluate if other residual confounding would bias toward or away from null without more information (=) | Moderate |
| Publication bias expected to have minimal impact (=) | Concentration response - not evaluated (=) | ||
| Indirectness – studies are of relevant populations and examine ambient exposures of interest (=) | Consistency – while there was substantial heterogeneity, associations are not so dissimilar to change interpretation, study design and population size did not contribute to heterogeneity (=) | ||
| Imprecision – confidence intervals are generally of reasonable to narrow range, except in very small study populations (=) | Magnitude of effect – magnitudes are small, as would be expected in epidemiology studies of environmental exposures and infant mortality (=) |
3.3. Overall results
The study characteristics, including pollutants included, infant mortality sub-types examined, study design and study location, are displayed in Fig. 4. Additional details for each study, including quantitative results, are included in Supplemental Table S3. PM10 was the pollutant most often evaluated (k = 16 studies) while PM2.5 was included in the fewest studies (k = 4 studies). There was substantial variability in the sub-types of infant mortality evaluated, with postneonatal mortality included in the most studies (k = 10 studies). Case-crossover and time-series studies were the most common study designs used, and the majority of studies were conducted in Asia, followed by Latin America, the U.S./Canada, and Europe.
Fig. 4.
Characteristics of included studies of short-term postnatal air pollution exposure and infant mortality.
The results of the random effect pooled ORs for each pollutant are displayed together in Fig. 5. Generally, positive pooled ORs were observed for all the pollutants except for O3. The highest magnitude pooled ORs were observed for SO2 and NO2, though these confidence intervals were the widest for these two pollutants, indicating less precision in the estimates. Forest plots representing each of the studies contributing to the pooled ORs are shown in Fig. 6 and summary statistics for each of the meta-analyses are presented in Table S4 in Supplemental Materials.
Fig. 5.
Summary results for meta-analysis of air pollutants and infant mortality. Random effects (Any Infant Mortality) and fixed effects (Postneonatal Mortality and Postneonatal Respiratory Mortality) for pooled odds ratios and 95 % confidence intervals for SO2, NO2, PM10, CO, and O3.
Fig. 6.
Forest plots for associations between short-term air pollution exposure and odds of infant mortality, with pooled odds ratio from random effects model for (A) PM10, (B) O3, (C), NO2, (D) SO2, (E) CO. Effect estimates standardized to a 10-μg/m3 increase in PM10 concentration, a 10-ppb increase in O3, NO2, or SO2 concentration, or a 1-ppm increase in CO concentration using the formula: standardized effect estimate = EXP(ln(reported effect estimate)*(10/reported increase in pollutant)). This formula is also used to standardize reported upper and lower confidence intervals. Standardized ORs may not match ORs reported in paper due to standardization.
We conducted sensitivity analyses for postneonatal mortality for five pollutants (PM10, O3, NO2, SO2, CO) and for postneonatal respiratory mortality for two pollutants (PM10, O3). Forest plots representing each of the studies contributing to the pooled ORs are shown in Figs. S11 and S12, respectively, in Supplemental Materials.
3.3.1. PM10 – infant mortality
Sixteen studies (Ha et al., 2003; Lin et al., 2004; Carbajal-Arroyo et al., 2011; Gouveia and Junger, 2018; Hajat et al., 2007; Scheers et al., 2011; Chen et al., 2021; Ritz et al., 2006; Romieu et al., 2004; Currie et al., 2009; Hwang et al., 2019; Litchfield et al., 2018; Yang et al., 2006; Tsai et al., 2006; Son et al., 2008; Wang et al., 2019) evaluated the association between short-term exposure to PM10 and infant mortality. Fourteen of these studies contributed effect estimates to the meta-analysis; the random effect pooled estimate for PM10 was 1.02 (95 % CI: 1.00, 1.03) (Fig. 6, panel A), and the prediction interval was 0.98–1.05. We chose to present the random effect pooled estimate because the I2 statistic (66 %) and the Q statistic p-value (<0.0005) indicated heterogeneity. The majority of the studies evaluating PM10 used a case-crossover study design (k = 7), with other study designs including time-series (k = 4), case-control (k = 2) and cross-sectional (k = 1). Most of the PM10 studies included in the pooled estimate were conducted in Asia (k = 7), followed by Latin America (k = 4), Europe (k = 3), and the U.S. (k = 2).
The studies included in the pooled estimate reported effect estimates for several different infant mortality sub-types: postneonatal (k = 5), SIDS (k = 2), neonatal (k = 1), postneonatal-respiratory (k = 1), postneontal-SIDS (k = 1), infant mortality-respiratory (k = 1) and any infant mortality (k = 3). The individual effect estimates for each infant mortality subtype from each study and additional study details are available in Supplemental Table S3.
Examination of the funnel plot and Egger’s test (p = 0.40) indicated the absence of potential publication bias, as did a rank correlation test (p = 0.75); trim and fill analyses estimated no missing studies (Supplemental Fig. S1). In leave-one-out sensitivity analyses, pooled effect estimates ranged from 1.01 to 1.02 (Supplemental Fig. S2) indicating that no one single study had a substantial influence on the pooled estimate.
In sensitivity analyses, we calculated pooled fixed effect estimates for PM10 and postneonatal mortality (k = 7) and postneonatal respiratory mortality (k = 5). For postneonatal mortality, the fixed effect pooled estimate for PM10 was 1.03 (95 % CI: 1.02, 1.03) (Supplemental Fig. S11, panel A), and for postneonatal respiratory mortality, the fixed pooled estimate for PM10 was 1.03 (0.97, 1.10) (Supplemental Fig. S12, panel A).
3.3.2. O3 – infant mortality
Fifteen studies (Carbajal-Arroyo et al., 2011; Lin et al., 2004; Gouveia and Junger, 2018; Hajat et al., 2007; Loomis et al., 1999; Currie et al., 2009; Romieu et al., 2004; Litchfield et al., 2018; Ritz et al., 2006; Chen et al., 2021; Yang et al., 2006; Tsai et al., 2006; Son et al., 2008; Wang et al., 2019) evaluated the association between short-term exposure to O3 and infant mortality. Thirteen of these studies contributed effect estimates to the meta-analysis; the random effect pooled estimate for O3 was 0.99 (0.97, 1.01) (Fig. 6, panel B), and the prediction interval was 0.94–1.04. We chose to present the random-effect pooled estimate because the I2 statistic (93 %) and the Q statistic p-value (<0.001) indicated heterogeneity. The majority of the studies evaluating O3 used a time-series (k = 7) or case-crossover study design (k = 6), with other study designs including case-control (k = 2) and cross-sectional (k = 1). Most of the O3 studies included in the pooled estimate were conducted in Asia (k = 6), followed by Latin America (k = 3), Europe (k = 2), and U. S./Canada (k = 2).
The studies included in the pooled estimate reported effect estimates for several different infant mortality sub-types: postneonatal (k = 5), infant mortality (k = 3), neonatal (k = 1), SIDS (k = 1), postneonatal-respiratory (k = 1), postneonatal-SIDS (k = 1), and infant mortality-respiratory (k = 1). The individual effect estimates for each infant mortality subtype from each study and additional study details are available in Supplemental Table S3.
Examination of the funnel plot and Egger’s test (p = 0.23) indicated the absence of potential publication bias, as did a rank correlation test (p = 0.95); trim and fill analyses estimated no missing studies (Supplemental Fig. S3). In leave-one-out sensitivity analyses, pooled effect estimates ranged from 0.99 to 1.00 (Supplemental Fig. S4) indicating that no single study had a substantial influence on the pooled estimate.
In sensitivity analyses, we calculated pooled fixed effect estimates for O3 and postneonatal mortality (k = 6) and postneonatal respiratory mortality (k = 5). For postneonatal mortality, the fixed effect pooled estimate for O3 was 0.99 (95 % CI: 0.99, 1.00) (Supplemental Fig. S11, panel B), and for postneonatal respiratory mortality, the fixed pooled estimate for O3 was 1.00 (0.99, 1.00) (Supplemental Fig. S12, panel B).
3.3.3. NO2 – infant mortality
Fourteen studies (Lin et al., 2004; Hajat et al., 2007; Ha et al., 2003; Loomis et al., 1999; Litchfield et al., 2018; Dales et al., 2004; Ritz et al., 2006; Chen et al., 2021; Hwang et al., 2019; Yang et al., 2006; Tsai et al., 2006; Son et al., 2008; Wang et al., 2019; Klonoff-Cohen et al., 2005) evaluated the association between short-term exposure to NO2 and infant mortality. Eleven of these studies contributed effect estimates to the meta-analysis; the random-effect pooled estimate for NO2 was 1.04 (1.01, 1.08) (Fig. 6, panel C), and the prediction interval was 0.96–1.13. We chose to present the random effect pooled estimate because the I2 statistic (87 %) and the Q statistic p-value (<0.002) indicated heterogeneity. The studies evaluating NO2 used a time-series (k = 7) or case-crossover (n = 5) study design, with two additional studies using a case-control study design. Seven of the O3 studies included in the pooled estimate were conducted in Asia, with Europe, Latin America, and U.S./Canada each contributing an additional two studies.
The studies included in the pooled estimate reported effect estimates for postneonatal mortality (k = 3), SIDS (k = 3), infant mortality (k = 1), neonatal mortality (k =1), postneonatal respiratory mortality (k =1), or postneonatal SIDS (k =1). The individual effect estimates for each infant mortality subtype from each study and additional study details are available in Supplemental Table S3.
Examination of the funnel plot and Egger’s test (p < 0.001) indicated the presence of potential publication bias, while a rank correlation test did not (p = 0.76); trim and fill analyses estimated five missing studies and resulted in a pooled odds ratio of 1.01 (1.00, 1.01) (Supplemental Fig. S5). In leave-one-out sensitivity analyses, pooled effect estimates ranged from 1.01 to 1.05 (Supplemental Fig. S6) and showed some influence by Dales et al. (2004) and Loomis et al. (1999); when either of these two studies was left out, the observed outcome was attenuated toward the null with more precise confidence intervals.
In sensitivity analyses, we calculated pooled fixed effect estimates for NO2 and postneonatal mortality (k =4). The fixed effect pooled estimate for NO2 was 1.01 (95 % CI: 0.99, 1.03) (Supplemental Fig. S11, panel C).
3.3.4. SO2 – infant mortality
Eleven studies (Hajat et al., 2007; Lin et al., 2004; Ha et al., 2003; Dales et al., 2004; Litchfield et al., 2018; Hwang et al., 2019; Yang et al., 2006; Tsai et al., 2006; Son et al., 2008; Wang et al., 2019) evaluated the association between short-term exposure to SO2 and infant mortality. Eight of these studies contributed effect estimates to the meta-analysis; the random-effect pooled estimate for SO2 was 1.07 (1.02, 1.12) (Fig. 6, panel D), and the prediction interval was 0.97–1.17. We chose to present the random-effect pooled estimate because the I2 statistic (61 %) and the Q-statistic p-value (<0.05) indicated heterogeneity. The majority of the studies evaluating SO2 used time-series (k = 6) or case-crossover study designs (n = 5), with one study conducting a case-control analysis. Seven of the SO2 studies included in the pooled estimate were conducted in Asia, with two additional studies conducted in Europe, one study conducted in Latin America, and one study from the U.S./Canada.
The studies included in the pooled estimate reported effect estimates for postneonatal mortality (k = 3), SIDS (k = 3), infant mortality (k = 1), and neonatal mortality (k = 1). The individual effect estimates for each infant mortality subtype from each study and additional study details are available in Supplemental Table S3.
Examination of the funnel plot and Egger’s test (p = 0.37) indicated the absence of potential publication bias, as did a rank correlation test (p = 0.72); trim and fill analyses estimated one missing study and resulted in a pooled odds ratio of 1.07 (1.02, 1.12) (Supplemental Fig. S7). In leave-one-out sensitivity analyses, pooled effect estimates ranged from 1.05 to 1.08 (Supplemental Fig. S8) indicating that no single study had a substantial influence on the pooled estimate.
In sensitivity analyses, we calculated pooled fixed effect estimates for SO2 and postneonatal mortality (k = 4). The fixed effect pooled estimate for SO2 was 1.06 (95 % CI: 1.02, 1.10) (Supplemental Fig. S11, panel D).
3.3.5. CO – infant mortality
Fourteen studies (Chen et al., 2021; Currie et al., 2009; Hwang et al., 2019; Lin et al., 2004; Hajat et al., 2007; Ha et al., 2003; Ritz et al., 2006; Dales et al., 2004; Litchfield et al., 2018; Yang et al., 2006; Tsai et al., 2006; Son et al., 2008; Wang et al., 2019; Klonoff-Cohen et al., 2005) evaluated the association between short-term exposure to CO and infant mortality. Eleven of these studies contributed effect estimates to the meta-analysis; the random-effect pooled estimate for CO was 1.01 (1.00, 1.02) (Fig. 6, panel E), and the prediction interval was 0.99–1.03. We chose to present the random-effect pooled estimate because the I2 statistic (54 %) and the Q-statistic p-value (<0.0002) indicated heterogeneity. In calculating the random-effect pooled odds ratio for CO, the ratio of the largest to smallest sampling variance was extremely large and may have affected the stability of the estimate. This is likely due to the extremely wide confidence interval associated with the standardized estimate from Tsai et al. (2006) (i.e., 0.02, 64.09) compared to the extremely narrow confidence interval associated with the standardized estimate from Chen et al. (2021) (i.e., 1.00, 1.00).
The studies evaluating CO used a time-series (k = 6) or case-crossover (k = 5) study design, with two additional studies using a case-control study design and one study conducting a cross-sectional analysis. Seven of the CO studies included in the pooled estimate were conducted in Asia, with the U.S./Canada contributing an additional three studies, two studies conducted in Europe, and one study from Latin America.
The studies included in the pooled estimate reported effect estimates for infant mortality (k = 3), SIDS (k = 3), postneonatal mortality (k = 2), neonatal mortality (k =1), postneonatal respiratory mortality (n =1), or postneonatal SIDS (n = 1). The individual effect estimates for each infant mortality subtype from each study and additional study details are available in Supplemental Table S3.
Examination of the funnel plot and Egger’s test (p < 0.001) indicated the presence of potential publication bias, while a rank correlation test did not (p = 0.88); trim and fill analyses estimated five missing studies and resulted in a pooled odds ratio of 1.01 (1.00, 1.01) (Supplemental Fig. S9). In leave-one-out sensitivity analyses, pooled effect estimates ranged from 1.01 to 1.04 (Supplemental Fig. S10) and showed some influence by Currie et al. (2009) and Hwang et al. (2019); when either of these two studies was left out, the magnitude of the observed outcome was higher with less precise confidence intervals.
In sensitivity analyses, we calculated pooled fixed effect estimates for CO and postneonatal mortality (k = 4). The fixed effect pooled estimate for CO was 1.05 (95 % CI: 0.98, 1.12) (Supplemental Fig. S11, panel E).
3.3.6. PM2.5 – infant mortality
Four studies (He et al., 2022; Loomis et al., 1999; Yorifuji et al., 2016; Wang et al., 2019) evaluated the association between short-term PM2.5 exposure and infant mortality. Three of these studies included effect estimates suitable for inclusion in a meta-analysis. We are not presenting pooled effect estimates for short-term PM2.5 exposure and infant mortality due to the limited number of studies available (k = 3) and demonstrated heterogeneity in the effect estimates from those studies (Q-statistic p-value = 0.13). The studies evaluating PM2.5 used a case-crossover (k = 2) or time-series (k = 1) study design. Two of the PM2.5 studies were conducted in Asia, with the other conducted in Latin America. The studies reported effect estimates for infant mortality (k = 2) or postneonatal mortality (k = 1). The individual effect estimates for each infant mortality subtype from each study and additional study details are available in Supplemental Table S3.
3.3.7. Additional studies
Two studies provided quantitative results but could not be included in the meta-analyses. Wang et al. (2019) evaluated PM10, PM2.5, O3, NO2, SO2, and CO and infant mortality and provided results in figures only. Son et al. (2008) evaluated PM10, O3, NO2, SO2, and CO and postneonatal mortality and did not include the unit increase associated with the effect estimates. Though we could not statistically evaluate the quantitative results presented in these studies, the results reported in these two studies generally appear to be near or within the range of effect estimates included in the meta-analyses for each of the pollutants.
An additional two studies could not be included in the meta-analyses based on the nature of the exposure assessment or statistical analyses of the data. Klonoff-Cohen et al. (2005) observed a positive association between SIDS and relatively higher NO2 concentrations (lag 0–2 days) when compared with relatively lower NO2 concentrations and an inverse association (i.e., OR < 1.0) between SIDS and relatively higher CO concentrations (lag 0–2 days) when compared with relatively lower CO concentrations. Greenberg et al. (1973) did not observe a positive association between SO2 and SIDS in their analyses. Generally, these results appear to be consistent with the range of effect estimates included in the meta-analyses for these pollutants.
4. Discussion
Outdoor air pollution is a complex mixture of gases, liquids, and particulate matter that contributes to adverse impacts on human health, affecting multiple organ systems, and can result in death. The State of Global Air 2020 (Health Effects Institute, 2020) estimated 6.67 million deaths worldwide were attributable to air pollution, and infants and children are among the most vulnerable (Sang et al., 2022). Infant mortality rates worldwide have declined substantially over the last few decades but remain an important contributor to childhood mortality (WHO, 2022). Previous reviews of air pollution and infant mortality have demonstrated stronger associations between PM and some causes of infant mortality (e.g., postneonatal respiratory mortality, SIDS) (Glinianaia et al., 2004; Kihal-Talantikite et al., 2020). In these reviews, authors combined and synthesized evidence from studies evaluating both short-term (i.e., days preceding death) and long-term (i.e., months preceding death) air pollution exposure. They also evaluated gestational exposures as well as postnatal exposure periods. To increase the comparability of effect estimates and reduce potential heterogeneity in study characteristics, we focused our review on short-term air pollution exposures during early life (i.e., postnatal) and infant mortality.
We identified 22 studies for inclusion in our systematic review, 18 of which were appropriate for inclusion in meta-analyses. Among the studies included in the meta-analyses, PM10 was the pollutant most commonly included (n = 14), while PM2.5 was included in the fewest studies (n = 3), and the pooled estimate is not presented. We generally observed positive associations between ambient air pollution concentrations and the odds of infant mortality with the highest magnitude associations observed for SO2 and NO2. The exception to this was a modest, negative association observed between short-term O3 exposure and infant mortality. In sensitivity analyses in which we restricted to specific sub-types of infant mortality, we observed similar pooled odds ratios for PM10 and O3 with postneonatal mortality and postneonatal respiratory mortality compared to the odds ratios for any infant mortality calculated in the main analyses. For NO2, SO2 and CO there were four studies included in the postneonatal infant mortality sensitivity analyses; pooled odds ratios were relatively unchanged for SO2, attenuated, but still positive for NO2, and elevated, though imprecise for CO compared to the pooled estimates in the main analysis.
Most of the effect estimates included in the meta-analyses were from studies that used a time-series or case-crossover design and corresponding analyses, though one cross-sectional and two case-control studies contributed effect estimates to the meta-analyses. The majority of studies included in the meta-analyses was conducted in Asia, followed by Latin America and Europe, with the fewest from the U.S. or Canada. There was variability in the types of infant mortality evaluated by the studies in this systematic review. Some studies reported effect estimates for all infant mortality, some divided infant mortality into the neonatal and postneonatal periods, and others reported infant mortality by cause of death. Due to the relatively low number of studies in each of these categories, we were unable to conduct meta-regression analyses to characterize potential sources of heterogeneity. In meta-analyses, we focused on random-effect models, since the effect estimates are taken from a series of sub-populations, and differences between these populations, and structures within these populations, may contribute to heterogeneity.
Globally, there is geographic variability in infant mortality rates, with the highest rates observed in parts of Africa (e.g., Sierra Leone), followed by the Middle East (e.g., Afghanistan), Asia (e.g., India), and the Pacific Islands (e.g., Indonesia) (Hill et al., 2012). No studies included in our systematic review or meta-analysis were conducted in the countries with the highest infant mortality rates. This is likely due to the lack of established, government-funded monitoring systems in these countries that contribute exposure data with the necessary spatial and temporal resolution to effectively conduct these types of analyses. In addition, a lack of well-maintained, well-funded, and accessible vital records may influence the feasibility of conducting epidemiologic research on infant mortality in some countries with high infant mortality rates. Recently, global air pollution models have been utilized for assigning long-term exposure in epidemiologic studies of air pollution, but these models are less useful for evaluating the effect of day-to-day changes in air pollution concentrations necessary for the types of analyses included in this systematic review.
There are a number of risk factors and potential confounders relating to infant mortality that could lead to bias estimates, which we attempted to minimize. The leading causes of infant mortality are birth defects, other adverse birth outcomes (e.g., preterm birth, low birth weight), and maternal pregnancy complications (CDC, 2022). By restricting the studies in this review to air pollution exposures occurring in the postnatal period, and specifically in the days preceding death, we reduce the likelihood that these risk factors are contributing to infant death in our meta-analyses. Further, when effect estimates for multiple sub-types of infant mortality were available from the same study, we preferentially chose postneonatal mortality over neonatal mortality for inclusion in the meta-analyses to help distinguish the effects of short-term early life air pollution exposure from effects related to adverse birth outcomes or pregnancy complications. In addition, many of the studies included in this systematic review were time-series or case-crossover studies. These study designs inherently control for time-invariant potential confounders or other unmeasured risk factors. The included studies generally controlled for other risk factors or potential confounders, such as weather-related variables and flu or other infectious disease prevalence, that could vary over shorter time periods.
During the neonatal and postneonatal periods, the developing lung is highly sensitive to environmental toxicants. There are two commonly-proposed biological mechanisms by which short-term exposure to air pollutants could lead to infant mortality: (1) respiratory tract inflammation and oxidative stress (Gong et al., 2005) that leads to downstream effects in the cardiovascular system or (2) activation of sensory nerves that modulate the ANS (Ghelfi et al., 2008). Either of these initiating events may eventually lead to respiratory effects (e.g., asthma exacerbations), cardiovascular effects (e.g., heart attacks), and mortality. There is the potential for different biological mechanisms to contribute to different infant mortality sub-types. Neonatal mortality is more likely to occur due to pregnancy complications or adverse birth outcomes and is common among infants who never left the hospital after birth (Woodruff et al., 2008). Though relatively little is known about the biological mechanism responsible for SIDS, there are hypotheses that disruptions in autonomic control may play a role (Lavezzi, 2015). Thus, it is plausible that air pollution’s ability to modulate the ANS could contribute to cases of SIDS. There is the potential that the inflammation and oxidative stress pathway or the activation of the sensory nerve pathway could contribute to postneonatal mortality. Currently, the evidence base is too limited for a meaningful evaluation of the differences in the effect of short-term postnatal air pollution exposure on different infant mortality subtypes.
This systematic review and meta-analyses considers multiple criteria air pollutants and focuses on short-term exposure during the postnatal period. By focusing on air pollution exposure on the days immediately preceding death, we hope to reduce some heterogeneity in the effect estimates due to different or combined exposure durations. Due to the limited evidence base for short-term air pollution exposure and infant mortality, the scope of our systematic review was relatively large. We included multiple criteria air pollutants and infant mortality sub-types. Generally, I2 statistics and Q statistic p-values indicated heterogeneity in the effect estimates available for most of the criteria pollutants. Despite this, we observed relatively consistent effect estimates in meta-analyses for each pollutant (i.e., narrow range in central estimate values), even when effect estimates for different infant mortality sub-types were combined. As the evidence base grows, a more refined approach focusing on specific infant mortality sub-types may be informative.
One of the strengths of this systematic review is the focus on short-term exposure durations during the postnatal period. This differentiates our review and meta-analyses from previous studies that have combined both short- and long-term exposure durations during gestation and/or the postnatal period (Glinianaia et al., 2004; Kihal-Talantikite et al., 2020). In addition, because little is known about the association between air pollution and infant mortality, we conducted a broad literature search intended to identify studies on any of the criteria air pollutants. Previous reviews have focused mainly on PM and infant mortality (Glinianaia et al., 2004). Our results suggest the potential for associations between gaseous air pollutants, specifically NO2 and SO2, and infant mortality that have not been highlighted in systematic reviewspreviously. Finally, we developed guidance and evaluated study quality across multiple domains for each study, and overall quality was rated as “high confidence”, “medium confidence”, “low confidence”, or “uninformative”. There were no factors that were influential enough to decrease or increase overall confidence, leading to a final designation of moderate overall confidence for this evidence base. It is unlikely that specific biases present in an individual study or across studies had a substantial impact on the results of our meta-analyses.
There were several limitations inherent in the evidence base. Few of the individual studies included in the systematic review controlled for potential co-pollutant confounding. Criteria air pollutants can be highly correlated in ambient air, and it is difficult to disentangle the effect of one pollutant from another. Co-pollutant models are one tool commonly used to address this. However, few studies in this systematic review presented co-pollutant models (Carbajal-Arroyo et al., 2011; Dales et al., 2004; Loomis et al., 1999; Ritz et al., 2006; Yorifuji et al., 2016). Further, it is difficult to separate environmental exposures from social determinants of health. Few studies included in this systematic review considered effect measure modification by social determinants of health. For example, there is clear evidence that infant mortality rates vary by gestational parent race/ethnicity, with the highest rates for non-Hispanic Black individuals and lower rates for Hispanic, non-Hispanic White, and non-Hispanic Asian individuals (Ely and Driscoll, 2021). Few studies conducted analyses stratified by race (as an indicator of racism), and we could not evaluate potential differences in the effect of air pollution on infant mortality by different social determinants of health. Another limitation in the evidence base supporting this systematic review is that the included studies focus on linear models to describe the relationship between short-term air pollution exposure and infant mortality. Little is known about the concentration-response relationship between air pollution and infant mortality and the potential for a non-linear relationship. This is especially important considering recent evidence suggesting the potential for non-linear (e.g., supra-linear) relationships between PM2.5 and cardiovascular mortality among adults (US EPA, 2019). Finally, while there is some evidence to support a biological pathway by which postnatal air pollution exposure could lead to infant mortality specifically through the inflammation and oxidative stress or ANS pathways, a clear mechanism for infant mortality, and specific infant mortality sub-types (e.g., SIDS) have yet to be identified.
5. Conclusion
Overall, the results of this systematic review and meta-analysis, based on 22 studies identified for overall inclusion, support an elevated risk of infant mortality associated with short-term air pollution exposure during early life. Positive associations were observed in meta-analyses for PM10, NO2, SO2, and CO. The notable exception to this was O3, for which a negative association was observed in the meta-analysis. The elevated pooled estimates from our meta-analyses were generally robust to trim-and-fill methods that account for potential publication bias, though the pooled estimate from the trim-and-fill method indicated an attenuated OR for NO2. While we were able to focus on a specific exposure duration (i.e., short-term exposure in the days preceding death) and exposure period (postnatal exposure), there are still uncertainties that remain, especially related to the potential for heterogeneity due to sub-types of infant mortality. Further exploration in studies of air pollution and infant mortality could address uncertainties, particularly with more complete consideration of other infant mortality sub-types and potential heterogeneity in different geographic locations.
Supplementary Material
Acknowledgements
We acknowledge Ms. Danielle Moore for assistance in designing and conducting literature searches. The authors would like to thank Drs. Stephanie Deflorio-Barker and David Dillon for comments on an early version of the manuscript.
Funding information
All funding for this study was provided by the U.S. Environmental Protection Agency. The funder had no role in the study design, data collection, analysis, interpretation, or manuscript writing. This research was supported, in part, by appointments to the Research Participation Program for the U.S. Environmental Protection Agency, Office of Research and Development, administered by the Oak Ridge Associated Universities (ORAU) and the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and Environmental Protection Agency. This work was performed as part of normal duties by EPA employees and contractors.
Footnotes
Disclaimer
The research described in this article has been reviewed by the Center for Public Health and Environmental Assessment, U.S. EPA, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the Agency, nor does the mention of trade names of commercial products constitute endorsement or recommendation for use.
CRediT authorship contribution statement
Thomas J. Luben: Conceptualization, Methodology, Investigation, Validation, Data curation, Writing – original draft, Supervision. Adrien A. Wilkie: Investigation, Validation, Data curation, Writing – review & editing. Alison K. Krajewski: Methodology, Investigation, Validation, Data curation, Writing – review & editing, Visualization. Fanny Njie: Investigation, Validation, Data curation, Visualization. Kevin Park: Validation, Data curation, Visualization. Sarah Zelasky: Validation, Data curation, Visualization. Kristen M. Rappazzo: Methodology, Software, Investigation, Validation, Formal analysis, Writing – review & editing, Supervision.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Adrien Wilkie reports financial support was provided by Oak Ridge Institute for Science and Education. Fanny Njie, Kevin Park, Sarah Zelasky reports financial support was provided by Oak Ridge Associated Universities.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2023.165522.
No studies evaluated the effect of residential mobility between the date of birth and the date of death on exposure assignment.
Data availability
All data used are publicly available
References
- Allaire J, 2012. Rstudio: Integrated development environment for r 770, 394. [Google Scholar]
- Carbajal-Arroyo L, Miranda-Soberanis V, Medina-Ramón M, Rojas-Bracho L, Tzintzun G, Solís-Gutiérrez P, Méndez-Ramírez I, Hurtado-Díaz M, Schwartz J, Romieu I, 2011. Effect of PM10 and O3 on infant mortality among residents in the Mexico City metropolitan area: a case-crossover analysis, 1997–2005. J. Epidemiol. Community Health 65, 715–721. 10.1136/jech.2009.101212 (HERO ID: 667773). [DOI] [PubMed] [Google Scholar]
- CDC (2022) Infant Mortality. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm Last accessed January 30, 2023.
- Chen YT; Liu CL; Chen CJ; Chen MH; Chen CY; Tsao PN; Chou HC; Chen PC (2021) Association between short-term exposure to air pollution and sudden infant death syndrome doi: 10.1016/j.chemosphere.2020.129515 HERO ID: 10288170. [DOI] [PubMed] [Google Scholar]
- Croft DP, Cameron SJ, Morrell CN, Lowenstein CJ, Ling F, Zareba W, Hopke PK, Utell MJ, Thurston SW, Thevenet-Morrison K, Evans KA, Chalupa D, Rich DQ, 2017. Associations between ambient wood smoke and other particulate pollutants and biomarkers of systemic inflammation, coagulation and thrombosis in cardiac patients. Environ. Res. 154, 352–361. 10.1016/j.envres.2017.01.027 (HERO ID: 3603596). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J, Neidell M, Schmieder JF, 2009. Air pollution and infant health: lessons from New Jersey. J. Health Econ. 28, 688–703. 10.1016/j.jhealeco.2009.02.001HEROID:597382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dales R, Burnett RT, Smith-Doiron M, Stieb DM, Brook JR, 2004. Air pollution and sudden infant death syndrome. Pediatrics 113, e628–e631. 10.1542/peds.113.6.e628HEROID:87342. [DOI] [PubMed] [Google Scholar]
- Delfino RJ, Staimer N, Tjoa T, Gillen DL, Polidori A, Arhami M, Kleinman MT, Vaziri ND, Longhurst J, Sioutas C, 2009. Air pollution exposures and circulating biomarkers of effect in a susceptible population: clues to potential causal component mixtures and mechanisms. Environ. Health Perspect. 117, 1232–1238. 10.1289/ehp.0800194HEROID:1006561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, Gillen DL, Tjoa T, Staimer N, Polidori A, Arhami M, Sioutas C, Longhurst J, 2011. Electrocardiographic ST-segment depression and exposure to traffic-related aerosols in elderly subjects with coronary artery disease. Environ. Health Perspect. 119, 196–202. 10.1289/ehp.1002372. HERO ID: 677632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely DM, Driscoll AK. (2021) Infant mortality in the United States, 2019: data from the period linked birth/infant death file. National Vital Statistics Reports; vol 70 no 14. Hyattsville, MD: National Center for Health Statistics. 2021. DOI: 10.15620/cdc:111053. [DOI] [PubMed] [Google Scholar]
- Ghelfi E, Rhoden CR, Wellenius GA, Lawrence J, Gonzalez-Flecha B, 2008. Cardiac oxidative stress and electrophysiological changes in rats exposed to concentrated ambient particles are mediated by TRP-dependent pulmonary reflexes. Toxicol. Sci. 102, 328–336. 10.1093/toxsci/kfn005HEROID:1079446. [DOI] [PubMed] [Google Scholar]
- Glinianaia FV, Rankin J, Bell R, Pless-Mulloli T, Howel D, 2004. Does particulate air pollution contribute to infant death? A systematic review. Environmental Health Perspectives 112, 1365–1371. 10.1289/ehp.6857 [Review] (HERO ID: 87898). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong H, Linn WS, Clark KW, Anderson KR, Geller MD, Sioutas C, 2005. Respiratory responses to exposures with fine particulates and nitrogen dioxide in the elderly with and without COPD. Inhal. Toxicol. 17, 123–132. 10.1080/08958370590904481. HERO ID: 87921. [DOI] [PubMed] [Google Scholar]
- Gouveia N, Junger WL, ESCALA investigators, 2018. Effects of air pollution on infant and children respiratory mortality in four large Latin-American cities. Environmental Pollution 232, 385–391. 10.1016/j.envpol.2017.08.125. HERO ID: 4166467. [DOI] [PubMed] [Google Scholar]
- Greenberg MA; Nelson KE; Carnow BW (1973) A study of the relationship between sudden infant death syndrome and environmental factors doi: 10.1093/oxfordjournals.aje.a121570 HERO ID: 10288200. [DOI] [PubMed] [Google Scholar]
- Ha EH; Lee JT; Kim H; Hong YC; Lee (2003) Infant susceptibility of mortality to air pollution in Seoul, South Korea, Pediatrics 111:284–290. doi: 10.1542/peds.111.2.284 HERO ID: 42552. [DOI] [PubMed] [Google Scholar]
- Hajat S, Armstrong B, Wilkinson P, Busby A, Dolk H, 2007. Outdoor air pollution and infant mortality: analysis of daily time-series data in 10 English cities. J. Epidemiol. Community Health 61, 719–722. 10.1136/jech.2006.053942 (HERO ID: 93276). [DOI] [PMC free article] [PubMed] [Google Scholar]
- He C; Liu C; Chen R; Meng Xia; Wang W; Ji J; Kang L; Liang J; Li X; Liu Y; Yu Xue; Zhu Jun; Wang Y; Kan H (2022) Fine particulate matter air pollution and under-5 children mortality in China: a national time-stratified case-crossover study Environment International 159. doi: 10.1016/j.envint.2021.107022 HERO ID: 10288201. [DOI] [PubMed] [Google Scholar]
- Health Effects Institute, 2020. State of Global Air 2020. Special Report. Health Effects Institute, Boston, MA. [Google Scholar]
- Hil K, You D, Inoue M, Oestergaard MZ, Technical Advisory Group of United Nations Inter-agency Group for Child Mortality Estimation (2012) Child mortality estimation: accelerated progress in reducing global child mortality, 1990–2010 doi: 10.1371/journal.pmed.1001303 HERO ID: 10693818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard BE, Phillips J, Tandon A, Maharana A, Elmore R, Mav D, Sedykh A, Thayer K, Merrick BA, Walker V, Rooney A, Shah RR, 2020. SWIFT-active screener: accelerated document screening through active learning and integrated recall estimation. Environ. Int. 138, 105623 10.1016/j.envint.2020.105623. HERO ID: 6570105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang MJ, Cheong HK, Kim JH, 2019. Ambient air pollution and sudden infant death syndrome in Korea: a time-stratified case-crossover study. Int. J. Environ. Res. Public Health 16. 10.3390/ijerph16183273 (HERO ID: 10288205). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kihal-Talantikite W, Marchetta GP, Deguen S, 2020. Infant mortality related to NO2 and PM exposure: systematic review and Meta-analysis. Int. J. Environ. Res. Public Health 17. 10.3390/ijerph17082623 (HERO ID: 8342519). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonoff-Cohen H, Lam PK, Lewis A, 2005. Outdoor carbon monoxide, nitrogen dioxide, and sudden infant death syndrome archives of disease in. Childhood 90, 750–753. 10.1136/adc.2004.057091 (HERO ID: 89445). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavezzi AM (2015) A new theory to explain the underlying pathogenetic mechanism of sudden infant death syndrome doi: 10.3389/fneur.2015.00220 HERO ID: 10693821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CA, Pereira LAA, Nishioka DC, Conceicao GMS, Graga ALF, Saldiva PHN, 2004. Air pollution and neonatal deaths in Sao Paulo, Brazil. Braz. J. Med. Biol. Res. 37, 765–770. . [DOI] [PubMed] [Google Scholar]
- Litchfield IJ, Ayres JG, Jaakkola JJK, Mohammed NI, 2018. Is ambient air pollution associated with onset of sudden infant death syndrome: a case-crossover study in the UK. British Medical Journal Open 8, e018341. 10.1136/bmjopen-2017-018341. HERO ID: 7497675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljungman PL, Wilker EH, Rice MB, Schwartz J, Gold DR, Koutrakis P, Vita JA, Mitchell GF, Vasan RS, Benjamin EJ, Mittleman MA, Hamburg NM, 2014. Short-term exposure to air pollution and digital vascular function. Am. J. Epidemiol. 180, 482–489. 10.1093/aje/kwu161HEROID:2353698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomis D, Castillejos M, Gold DR, Mcdonnell W, Borja-Aburto VH, 1999. Air pollution and infant mortality in Mexico City. Epidemiology 10, 118–123. 10.1097/00001648-199903000-00006HEROID:87288. [DOI] [PubMed] [Google Scholar]
- Lucking AJ, Lundbäck M, Barath SL, Mills NL, Sidhu MK, Langrish JP, Boon NA, Pourazar J, Badimon JJ, Gerlofs-Nijland ME, Cassee FR, Boman C, Donaldson K, Sandstrom T, Newby DE, Blomberg A, 2011. Particle traps prevent adverse vascular and prothrombotic effects of diesel engine exhaust inhalation in men. Circulation 123, 1721–1728. 10.1161/circulationaha.110.987263. HERO ID: 1256938. [DOI] [PubMed] [Google Scholar]
- Madrigano J, Baccarelli A, Wright RO, Suh H, Sparrow D, Vokonas PS, Schwartz J, 2010. Air pollution, obesity, genes and cellular adhesion molecules. Occup. Environ. Med. 67, 312–317. 10.1136/oem.2009.046193 (HERO ID: 625445). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan RL; Whaley P; Thayer KA; Schünemann HJ (2018) Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes doi: 10.1016/j.envint.2018.07.015 HERO ID: 7514150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS, (2023). National Center for Health Statistics, final mortality data, 1990–1994 and period linked birth/infant death data, 1995-present. Retrieved February 13, 2023, from www.marchofdimes.org/peristats.
- Patel AP; Jagai JS; Messer LC; Gray CL; Rappazzo KM; Deflorio-Barker SA; Lobdell DT (2018) Associations between environmental quality and infant mortality in the United States, 2000–2005 doi: 10.1186/s13690-018-0306-0 HERO ID: 10288113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritz B, Wilhelm M, Zhao Y, 2006. Air pollution and infant death in southern California, 1989–2000. Pediatrics 118, 493–502. 10.1542/peds.2006-0027 (HERO ID: 89819). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romieu I, Ramirez-Aguilar M, Moreno-Macias H, Barraza-Villarreal A, Miller P, Hernandez-Cadena L, Carbajal-Arroyo LA, Hernandez-Avila M, 2004. Infant mortality and air pollution: modifying effect by social class. J. Occup. Environ. Hyg. 46, 1210–1216. 10.1097/01.jom.0000147224.35351.08. HERO ID: 93074. [DOI] [PubMed] [Google Scholar]
- Rooney AA, Boyles AL, Wolfe MS, Bucher JR, Thayer KA, 2014. Systematic review and evidence integration for literature-based environmental health science assessments. Environ. Health Perspect. 122, 711–718. 10.1289/ehp.1307972. HERO ID: 2520120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sang S; Chu C; Zhang T; Chen H; Yang X (2022) The global burden of disease attributable to ambient fine particulate matter in 204 countries and territories, 1990–2019: a systematic analysis of the Global Burden of Disease Study 2019 doi: 10.1016/j.ecoenv.2022.113588 HERO ID: 10692784. [DOI] [PubMed] [Google Scholar]
- Scheers H, Mwalili SM, Faes C, Fierens F, Nemery B, Nawrot TS, 2011. Does air pollution trigger infant mortality in Western europe? A case-crossover study. Environmental Health Perspectives 119, 1017–1022. 10.1289/ehp.1002913. HERO ID: 749664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro AJ, Antoni S, Guyton KZ, Lunn RM, Loomis D, Rusyn I, Jahnke GD, Schwingl PJ, Mehta SS, Addington J, Guha N, 2018. Software tools to facilitate systematic review used for cancer hazard identification. Environ. Health Perspect. 126, 104501 10.1289/ehp4224HEROID:6570074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son JY, Cho YS, Lee JT, 2008. Effects of air pollution on postneonatal infant mortality among firstborn infants in Seoul, Korea: case-crossover and time-series analyses. Arch. Environ. Occup. Health 63, 108–113. 10.3200/aeoh.63.3.108-113 (HERO ID: 190323). [DOI] [PubMed] [Google Scholar]
- Steenhof M, Janssen NA, Strak M, Hoek G, Gosens I, Mudway IS, Kelly FJ, Harrison RM, Pieters RH, Cassee FR, Brunekreef B, 2014. Air pollution exposure affects circulating white blood cell counts in healthy subjects: The role of particle composition, oxidative potential and gaseous pollutants. RAPTES project Inhalation Toxicology 26, 141–165. 10.3109/08958378.2013.861884. HERO ID: 2230058. [DOI] [PubMed] [Google Scholar]
- Strak M, Hoek G, Godri KJ, Gosens I, Mudway IS, van Oerle R, Spronk HM, Cassee FR, Lebret E, Kelly FJ, Harrison RM, Brunekreef B, Steenhof M, Janssen NA, 2013. Composition of PM affects acute vascular inflammatory and coagulative markers - the RAPTES project. PLoS One 8, e58944. 10.1371/journal.pone.0058944. HERO ID: 1519608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team, R.C., 2013. R: A language and environment for statistical computing. Vienna, Austria. [Google Scholar]
- Thakrar AP, Forrest AD, Maltenfort MG, Forrest CB, 2018. Child Mortality in the US and 19 OECD Comparator Nations: A 50-Year Time-Trend Analysis. 10.1377/hlthaff.2017.0767. HERO ID: 10706130. [DOI] [PubMed] [Google Scholar]
- Tsai SS, Chen CC, Hsieh HJ, Chang CC, Yang CY, 2006. Air pollution and postneonatal mortality in a tropical city: Kaohsiung, Taiwan. Inhalation Toxicology 18, 185–189. 10.1080/08958370500434214HEROID:90709. [DOI] [PubMed] [Google Scholar]
- U.S. EPA (2019) Integrated Science Assessment (ISA) for particulate matter (final report, Dec 2019) (EPA/600/R-19/188). Washington, DC: U.S. Environmental Protection Agency, [EPA Report] https://cfpub.epa.gov/ncea/isa/recordisplay.cfm?deid=347534 HERO ID: 6591812. [Google Scholar]
- Viechtbauer W, 2010. Conducting meta-analyses in r with the metafor package. Journal of Statistical Software 36, 1–48. [Google Scholar]
- Wang J, Cao H, Sun D, Qi Z, Guo C, Peng W, Sun Y, Xie Y, Liu X, Li B, Luo Y, Pan Y, Li Y, Zhang L, 2019. Associations between ambient air pollution and mortality from all causes, pneumonia, and congenital heart diseases among children aged under 5 years in Beijing, China: a population-based time series study. Environmental Research 176, 108531. 10.1016/j.envres.2019.108531. HERO ID: 5438404. [DOI] [PubMed] [Google Scholar]
- WHO (2022). Newborn mortality fact sheet. https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021#:~:text=Globally%202.4%20million%20children%20died,up%20from%2040%25%20in%201990. Last accessed January 30, 2023.
- Woodruff TJ, Darrow LA, Parker JD, 2008. Air pollution and postneonatal infant mortality in the United States, 1999–2002. Environmental Health Perspectives 116 (1), 110–115. 10.1289/ehp.10370. HERO ID: 98386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang CY, Hsieh HJ, Tsai SS, Wu TN, Chiu HF, 2006. Correlation between air pollution and postneonatal mortality in a subtropical city: Taipei, Taiwan. Journal of Toxicology and Environmental Health, Part A: Current Issues 69, 2033–2040. 10.1080/15287390600746181. HERO ID: 90760. [DOI] [PubMed] [Google Scholar]
- Yorifuji T, Kashima S, Doi H, 2016. Acute exposure to fine and coarse particulate matter and infant mortality in Tokyo, Japan (2002− 2013). Sci. Total Environ. 551–552, 66–72. 10.1016/j.scitotenv.2016.01.211 (HERO ID: 3120028). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used are publicly available