Abstract
Meige syndrome is a rare neurological disease characterized by segmental dystonia, specifically blepharospasm and oromandibular dystonia. These symptoms are often accompanied by complex movements of the eyelids, lower facial muscles, mandible, and neck muscles. Bilateral blepharospasm is the most common feature of this disease. In this case report, we present the successful treatment of refractory blepharospasm in a 72-year-old woman with Meige syndrome via 2 incisions resulting from myectomy and in situ surgery.
Keywords: Meige syndrome, blepharospasm, myectomy, myotomy
Introduction
Meige syndrome is a rare neurological disorder classified as a type of segmental dystonia that was initially described by the French neurologist Henri Meige in 1910. It is characterized by the presence of blepharospasm and oromandibular dystonia and is often accompanied by complex movements involving the eyelids, lower facial muscles, mandible, and neck muscles. 1 The exact pathogenesis of this condition is unknown; however, several hypotheses have been proposed, including dysfunction of gamma-aminobutyric acid neurons, cholinergic hyperactivity, dopamine receptor hypersensitivity, and an imbalance in dopaminergic neurotransmitters. 1 Meige syndrome is generally more prevalent in individuals aged 30 to 70 years, with a higher incidence observed in females than in males. 1
Bilateral blepharospasm is the predominant characteristic of Meige syndrome and results in dystonic sustained eyelid spasms and apraxia of eyelid opening. These symptoms severely impair patients’ functionality and significantly impact their quality of life. Current treatment options for blepharospasm in patients with Meige syndrome include focal muscle weakening with botulinum toxins (BTx), deep brain stimulation (DBS), and surgical myectomy. While BTx injections can provide temporary relief of blepharospasm, many patients do not experience sufficient improvement with this treatment alone. Factors such as apraxia of eyelid opening, disease progression, or development of immunoresistance to BTx can contribute to this complication. 2 DBS, which involves stimulating the bilateral pallidal tract, has shown effectiveness but requires further evaluation to assess the long-term and potential side effects. 3 Surgical myectomy, which specifically targets the orbicularis oculi and corrugator supercilii muscles, is an effective treatment option for refractory blepharospasm in patients with Meige syndrome. 4 It can be performed in combination with BTx injections or as a standalone procedure. The myectomy procedure typically involves the resection of only the muscles in the upper eyelids but can involve resection of the muscles in both the upper and lower eyelids. In this case report, we present the surgical outcomes of selective orbicularis oculi myectomy and in situ corrugator supercilii muscle myotomy on the upper eyelids for refractory blepharospasm in patients with Meige syndrome.
Case Presentation
A 72-year-old female patient presented with involuntary tics affecting both eyes accompanied by mandibular muscle spasms that had been ongoing for 10 years. Additionally, she reported a 2-year history of an inability to keep her eyes open. The patient had previously undergone treatment with Botulinum toxin (BTx) injections for both eyes, which provided temporary relief for only 1 month. She declined further injection therapy. There was no history of surgical procedures or traumatic events, and the patient had no known systemic disease.
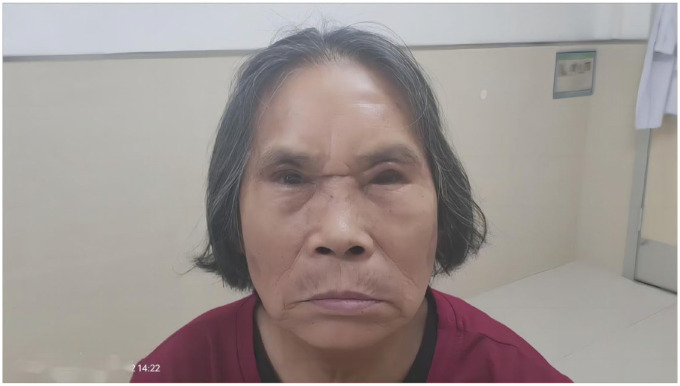
During the ocular examination, the patient exhibited uncorrected visual acuity of 8/20 in the right eye (OD) and 6/20 in the left eye (OS). Slit-lamp microscopy revealed the presence of cataracts extending from the ocular surface to the fundus area. No other specific findings were observed. The patient displayed normal extraocular eye movements and no evidence of nystagmus or relative afferent pupillary defects. However, she presented with symmetrical and involuntary movements of her eyelids, difficulty keeping her eyes open, partially blocked eyelid gland opening, and pursing of her lips. These symptoms were indicative of oromandibular dystonia, as depicted in Figure 1 and Supplemental Video 1. The diagnosis for this patient included Meige syndrome, senile cataract in both eyes, and dry eye disease in both eyes.
Figure 1.
Displays the preoperative state, showing the symmetrical and involuntary movements of the eyelids. This was further emphasized in Supplemental Video 1.
These procedures can be performed under local anesthesia and are briefly described as follows:
The surgery required 2 incisions, a subbrow incision and a double eyelid line incision. Local anesthesia was administered to all surgically involved areas. Excess upper eyelid skin was removed. Selective myectomy is performed by resecting the orbicularis oculi muscle (OOM) between the subbrow incision and a double eyelid line incision. Two to three sutures with 5-0 nylon thread were placed to fix the eyebrow tissue under the eyebrow bone periosteum. The nasal skin was incised, the eyebrow muscle and procerus were separated, and the eyebrows and procerus were cut. The patient’s orbital midriff fat was filled with middle broken ends, and 6-0 beauty stitches were used to interrupt the suturing of the skin.
Following the surgery, the patients were able to open their eyes without assistance and experienced relief from blepharospasm. At the 6-month follow-up visit, the patient could open their eyes without assistance and reported sustained significant relief from blepharospasm, as shown in Figure 2 and Supplemental Video 2. The patient’s quality of life improved significantly.
Figure 2.
Represents the postoperative follow-up at 6 months, revealing satisfactory functional and cosmetic outcomes. This is corroborated in Supplemental Video 2.
Discussion
Meige syndrome is a rare neurological disorder with unclear etiology. However, it is believed that emotional stress may play a significant role in its development. Approximately 33% of Meige syndrome patients also experience symptoms of anxiety, depression, and sleep disturbances. 5 The diagnosis of Meige syndrome relies primarily on clinical evaluation. The presence of bilateral blepharospasm accompanied by involuntary contractions of other facial or oromandibular muscles is considered a common manifestation of this syndrome.
Treatment for Meige syndrome should be individualized, taking into consideration factors such as patient willingness, severity of the condition and etiology to ensure treatment effectiveness. The involved etiological factors are complex and affect the type of treatment. In one case report, Meige syndrome was found to be related to the use of vortioxetine. 6 In another case report, Meige syndrome was induced by atypical antipsychotic effects caused by the long-term use of blonanserin in a 37-year-old woman. 7 Additionally, a case study by Nguyen and Hoegerl 8 described the successful treatment of Meige syndrome using oral baclofen in an 87-year-old man. However, a rare case of multiple system atrophy associated with Meige syndrome was reported by Liang et al. 9 The authors found that, based on their experience, a combination of local BTx injections and intrathecal injections of umbilical cord-derived mesenchymal stem cells was an effective treatment approach.
However, unlike the aforementioned reported cases, the pathogenesis of many other instances of Meige syndrome remains unclear. Persistent blepharospasm is a prominent issue that can weaken the function of protractors, creating a vicious cycle that exacerbates blepharospasm and leads to functional disability. This approach could help increase the success rate of orbicularis myectomy in patients with blepharospasm. Upper eyelid myectomy surgery is commonly performed to improve the condition of blepharospasm patients with associated apraxia of lid opening (ALO) who do not respond to botulinum toxin (BTx) injections. 2 The choice of surgical technique is based on 4 factors: ALO associated with benign essential blepharospasm (BEB), blepharospasm-associated deformities, unresponsiveness or refractoriness to BTx, and inability or refusal to undergo BTx injections. 5 In 2020, Lai et al 4 presented the myotomy in situ for essential BEB refractory to BTx. The research conclusion indicates that the efficacy and cosmetic outcomes of upper eyelid myotomy in situ are similar to that of full myectomy for patients with BEB who are refractory to BTx treatment. 4 However, studies on blepharospasm in Meige syndrome patients are rare. Unlike the one incision made in the reported article, 10 we made 2 surgical incisions, both of which were hidden and thus did not affect the patient’s aesthetic appearance; moreover, the view of the operative field is better, allowing a simpler procedure. Moreover, our surgery required the eyebrow to be raised to allow deep fixation of the brow to prevent eyebrow prolapse, which can subsequently delay peri-orbital aging. For Meige syndrome patients with more severe refractory blepharospasm, Lai et al 10 in 2023 recommened an upper eyelid protractor as well as lower eyelid tightening may be necessary.The conclusion that selective myectomy and myotomy in situ of eyelid protractors combining blepharoplasty correction and lower eyelid tightening can lead to long-term functional and aesthetic outcomes with refractory Meige syndrome.
Meanwhile, it should be pointed out that our follow-up period was 6 months, and the long-term effects are still unclear. A recent literature report 11 that upper eyelid surgery still faces many challenges in the long-term follow up. Long-term blepharospasm management seems still difficult to be performed adequately and new therapeutical approaches are still needed.
Conclusions
Myectomy and myotomy in situ through 2 surgical incisions might be considered viable options for managing refractory blepharospasm in Meige syndrome patients. However, further studies including long-term follow up are needed to confirm these findings in patients with Meige syndrome.
Footnotes
Author contribution: Ming-ming Li wrote the main manuscript text and prepared Figures. Zhi-min Cen revised the article. Huang Zhang have checked and prepared Videos. Zhong-ling Luo is the surgeon and participated in polishing this manuscript. All authors reviewed the manuscript.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: In compliance with the ICMJE uniform disclosure form, all the authors declare the following: Payment/services info: All the authors declare that no financial support was received from any organization for the submitted work. Financial relationships: All the authors declare that they have no financial relationships at present or established within the previous 3 years with any organizations that might have an interest in the submitted work. Other relationships: All the authors declare that there are no other relationships or activities that could appear to have influenced the submitted work.
Human Subjects: Consent was obtained from all participants in this study.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Pandey SSS. Meige’s syndrome: history, epidemiology, clinical features, pathogenesis and treatment. J Neurol Sci. 2017;372:162-170. [DOI] [PubMed] [Google Scholar]
- 2. Yen MT. Surgical myectomy for essential blepharospasm and hemifacial spasm. Int Ophthalmol Clin. 2018;58:63-70. [DOI] [PubMed] [Google Scholar]
- 3. Reese R, Gruber D, Schoenecker T, et al. Long-term clinical outcome in meige syndrome treated with internal pallidum deep brain stimulation. Movement Disord. 2011;26:691-698. [DOI] [PubMed] [Google Scholar]
- 4. Lai H, Chen AD, Lee S, Lin Y, Lai C. Myotomy in situ for essential blepharospasm refractory to botulinum toxin. Ann Plas Surg. 2020;84:S74-S79. [DOI] [PubMed] [Google Scholar]
- 5. Pariseau B, Worley MW, Anderson RL. Myectomy for blepharospasm 2013. Curr Opin Ophthalmol. 2013;24:488-493. [DOI] [PubMed] [Google Scholar]
- 6. Şahin ŞK, Elboga G, Altindag A. Meige syndrome related to vortioxetine in 2 sisters. J Clin Psychopharmacol. 2015;39:679-681. [DOI] [PubMed] [Google Scholar]
- 7. Kim JE, Jung JW. Refractory dry eye disease associated with Meige’s syndrome induced by long-term use of an atypical antipsychotic. BMC Ophthalmol. 2020;20:474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nguyen K, Hoegerl C. A case of Meige syndrome treated with baclofen. Cureus J Med Sci. 2020;12(9): e10570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liang J, He X, Lu J. Multiple system atrophy associated with Meige syndrome: a rare case report. Radiol Case Rep. 2023;18:3192-3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lai C, Wang Y, Ramachandran S, Chang Y, Huang S, Hsieh MW. Selective myectomy and myotomy in situ for the management of refractory blepharospasm in Meige syndrome. Ann Plast Surg. 2023;90:S84-S88. [DOI] [PubMed] [Google Scholar]
- 11. Trinchillo A, Cuomo N, Habetswallner F, Esposito M. The long-term response to botulinum toxin injections in patients with blepharospasm undergoing upper eyelid surgery. Parkinsonism Relat Disord. 2024;119:105958. [DOI] [PubMed] [Google Scholar]