Abstract
Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health. Historically, most health inequities have been caused by societal injustices, and these causal factors must be considered when conducting biomedical research–including human genomics. However, the field of human genomics has fallen short when it comes to equity, in large part because the diversity of the human population has been inadequately reflected among participants of genomics research, human genome reference sequences, and, as a result, the content of genomic data resources. This lack of diversity leads to disparities that can have scientific and clinical consequences such as the lack of generalizability of research results and inaccurate reference ranges. Like the larger biomedical research enterprise, the genomics community is becoming increasingly focused on enhancing equity in genomics. Achieving health equity related to genomics will require greater effort in addressing inequities within the field. As part of the National Human Genome Research Institute’s (NHGRI) commitment to advancing health equity, it convened experts in genomics and health equity research to make recommendations and performed a review of current literature to identify the landscape of gaps and opportunities at the interface between human genomics and health equity research. This perspective describes these findings and examines the meaning of health equity within the context of human genomics and genomic medicine.
Existing Inequities
Achieving health equity is a significant challenge globally1, as the conditions in which people are born, grow, live, and work influence health and quality-of-life outcomes — yet these conditions are far from equal among individuals and populations. Such disparate conditions play a large part in propagating health inequities amongst different populations2. While the use of genomic information and genomic technologies holds great potential to improve human health, not all individuals, groups, and populations have benefitted equally from genomic advances to date (https://www.ashg.org/publications-news/ashg-news/statement-american-society-of-human-genetics-board-of-directors-on-the-report-of-the-ashg-facing-our-history-building-an-equitable-future-initiative/). In fact, the growing awareness of structural inequality, including the impacts of interpersonal and structural racism and discrimination, has brought significant visibility to the socioeconomic, racial, ethnic, and other disparities associated with the design and outcomes of human genomics studies3.
Why is health equity in genomics vital?
Genomics offers great promise for both elucidating disease mechanisms and improving prevention, diagnosis, and treatment of diseases. However, the genome does not operate in isolation. It has long been established that genomic contributions to health and disease should be assessed in the context of a person’s broader environment. It is only recently that the social environment, particularly elements of structural inequities, such as systemic racism and inadequate accessibility to healthcare, has been considered in genomics research.
Moreover, genomics research does not occur in a vacuum, and achieving health equity relies on recognizing and removing the many structural barriers that lead to disparities in underserved populations. In this perspective, we seek to define health equity in the genomics context and make recommendations on how to move toward health equity in genomics research and genomic medicine. Health equity in genomics means that all groups, populations, social contexts, and environments are considered in all aspects of human genomics research—from the development of genomic technologies and the design of genomics studies to the provision of access to genomic data and the implementation of genomic medicine. In short, a health equity lens must be applied to all aspects of genomics research. Policies such as the expansion of insurance programs that promote access to healthcare have taught us important lessons about the path toward health equity. These and other lessons must be considered by the genomics community to ensure that genomic advances benefit all (https://www.medicare.gov/basics/costs/help/medicaid). In addition, guidelines and practices should be established for researchers and clinicians to increase equity in the use of genomics in medicine4.
Exploration of Current Challenges
Recognizing the need to obtain new perspectives and specific recommendations from the scientific community about enhancing health equity in human genomics research, the NHGRI Training, Diversity, and Health Equity Office (TiDHE; https://www.genome.gov/about-nhgri/Office-of-the-Director/Training-Diversity-and-Health-Equity-Office) led a 1. workshop and a 2. literature landscape review.
1. Future Directions of Genomics and Health Equity Workshop
In April 2022, NHGRI hosted a virtual, public workshop, titled Future Directions of Genomics and Health Equity Workshop, that aimed to identify research gaps and opportunities that will improve health equity in genomics (https://www.genome.gov/sites/default/files/media/files/2022-05/Genomics-and-Health-Equity-Workshop-Meeting-Summary.pdf). The workshop had the following objectives:
1st: leverage what has been learned in health disparities research to identify areas in human genomics that are important to advancing health equity;
2nd: identify research and partnerships needed to understand and address structural factors that influence health equity in genomics; and
3rd: define measurements of success in terms of attaining health equity in genomics.
The two-day workshop was attended by over 300 individuals from academic and non-academic backgrounds, representing broad areas of expertise and perspectives. A series of presentations, panel discussions, and breakout group discussions were used to achieve the objectives of the workshop by offering different methods for participants to share their research, expertise, and diverse perspectives. Presentations focused on the following: NHGRI’s mission regarding health equity and diversity; the vision for health equity and genomics; moving forward from health disparities to health equity in genomics and genomic medicine; current research in genomics and health equity; and current challenges in genomics research and genomic medicine that can lead to health disparities. After each presentation, a panel of experts responded to the research and thoughts presented as well as questions presented by workshop attendees. Workshop participants were then separated into five breakout groups based on their expertise and experiences in the topic areas and were asked to give recommendations for future research aimed at improving health equity in genomics and genomic medicine. The attendees considered all recommendations and voted on the top recommendations to pursue.
Although the recommendations of advancing health equity and partnerships helped to accomplish the first two workshop objectives, workshop attendees agreed that metrics were needed to measure success in increasing health equity in genomics (see workshop summary at: https://www.genome.gov/event-calendar/future-directions-in-genomics-and-health-equity-research). As a result of the workshop, NHGRI developed two funding opportunities: the Investigator-Initiated Research in Genomics and Health Equity R01 (Research Project Grant) Funding Opportunity (https://grants.nih.gov/grants/guide/rfa-files/RFA-HG-23-017.html) to develop approaches, generate and disseminate data, and implement metrics and/or interventions that will advance the equitable use of genomics to improve health and the Investigator-Initiated Research in Genomics and Health Equity R21 (Exploratory/Development Research Grant) Funding Opportunity (https://grants.nih.gov/grants/guide/rfa-files/RFA-HG-23-018.html) to support pilot and feasibility studies, secondary analysis of existing data, small, self-contained research projects, development of research methodology, and development of new research technology that addresses genomics and health equity.
2. Understanding Elements Needed for Health Equity in Genomics
To build upon the workshop, we also conducted a literature review using PubMed Central (https://www.ncbi.nlm.nih.gov/pmc/) specifically with the search phrases “genomics and health equity”, “health equity”, “health equity in research”, and “underrepresented populations and genomics”. We restricted the search to articles that were published from June 2013 to June 2023. A combination of the following terms was used to maximize search specificity and sensitivity: “genomics AND health equity,” “genomics AND health disparities,” “health equity research,” “underrepresented populations AND genomics,” and “health disparities.” The search identified more than 800 papers. Results were further screened by title and abstract. Articles specific to disease areas or specific research areas in genomics as well as papers that only referred to rather than focused on health equity, genomics, and/or underrepresented populations were then excluded. This resulted in 189 identified research articles. We then removed papers that focused on the cause of health disparities rather than ways to increase health equity, which yielded 72 articles for the literature review. Major themes and recommendations were coded according to frequency of occurrence. Resulting themes were equitable participation, increasing workforce diversity, building partnerships, developing metrics of health equity and policy development. Suggestions resulting from the workshop and review of these papers led to the following overarching recommendations (Table 1).
Table 1.
Genomics and Health Equity Workshop and Literature Review Recommendations*
| Recommendations | Workshop | Literature Review |
|---|---|---|
| Diversify the genomics workforce | ✔ | ✔ |
| Address the lack of population diversity in genomics research and biobanks | ✔ | ✔ |
| Assess how the lack of diversity in populations and communities comprising genomic research cohorts impacts health disparities | ✔ | |
| Address outcomes important to all communities | ✔ | |
| Address the inappropriate use of racial and ethnic categories in genomics research | ✔ | ✔ |
| Increase the utilization of genomic markers rather than racial and ethnic categories in clinical algorithms | ✔ | |
| Include contextual variables and diverse settings in genomics research | ✔ | ✔ |
| Build partnerships with diverse communities to build trust, get feedback, and conduct research in an equitable fashion | ✔ | ✔ |
| Respect views and autonomy of participants and communities | ✔ | ✔ |
| Develop metrics of health equity and apply those metrics across genomics studies | ✔ | ✔ |
| Develop policies to address health disparities | ✔ |
Check marks indicate whether the recommendation came from the Genomics and Health Equity Workshop and/or literature review.
Consideration of major themes in genomics and health equity
Equitable Participation
Currently, there are many populations that are underrepresented in genomics research; the majority of research cohorts are composed of participants that are mainly of European descent, therefore the outcomes from research using these cohorts are not generalizable. Inclusion of diverse populations, including populations often underrepresented in genomics research, helps to ensure research outcomes and clinical algorithms apply to all populations. Moving towards health equity requires a shift in how we think about equitable participation in genomics and precision medicine research. Specifically, equitable participation must reflect not just factors such as age, race, ethnicity, and sex, but also other sociodemographic characteristics such as sexual orientation, sex identity, (dis)ability, socioeconomic status, and geographic residence.
The interplay of genomics in relation to broader systemic issues of poverty, racism, and discrimination should be examined. There is thus a need to take an intersectional approach that both promotes diverse and equitable inclusion in genomics research and conducts research that addresses outcomes important to all communities. It is essential that this focus on representation does not focus on the study of differences among groups or reinforce the misconception that race is biologically determined; instead, it should aim to make genomics research more applicable and generalizable to diverse communities5.
Take, for example, two groups often excluded – Indigenous communities and people with disabilities. When conducting genomics research that involves Indigenous communities in the United States, investigators must respect the sovereignty that federally recognized tribes have as Native Nations. This reality must not be separated from discussions about design, data ownership, and dissemination since tribes have and exert their authority to regulate research6.
People with disabilities are often excluded from research unless that research focuses on specific disabilities7. In addition, genomics research has sometimes been viewed as aiming to eradicate disability communities, especially in the contexts of prenatal screening and gene editing. Workshop participants expressed concerns that genomics research has sometimes been used in the past to ‘cure’ disabilities. These communities expressed concerns that research to ‘cure’ disabilities gives the impression that researchers would like to eliminate people with disabilities. Through community engagement it was learned that often persons with disabilities are not interested in cures but would like the genomics community to focus on accessibility and inclusion. In the design and implementation of genomics studies, researchers must consider and respect the views and perceptions of disability communities, including appropriate engagement to ensure transparent communication.
Enhancing the Diversity of the Genomics Workforce
Currently, the genomics workforce does not reflect the diversity of the United States population. Enhancing the diversity of the genomics workforce is imperative for achieving health equity in genomics. One route for this is intentionally including institutions that serve underserved communities, such as minority-serving institutions, in genomics research, which will help in reaching individuals and groups underrepresented in the biomedical research workforce.
The inclusion of Historically Black Colleges and Universities (HBCU), Hispanic-serving institutions, Tribal colleges, and community colleges in genomics research has been shown to increase access to and inclusion of diverse trainees and investigators. The inclusion of individuals at all career stages and from different scientific disciplines [including those studying the ethical, legal, and social implications (ELSI) of genomic advances] is also critical for expanding the diversity of thought and perspectives in genomics research.
In addition, the early engagement of trainees from diverse backgrounds is important to diversifying investigators in genomics research. Without diverse voices, there is potential for over- and/or underestimating participant risk and personal agency, which can lead to research harms and limited research benefits. Workshop participants agreed that including individuals from diverse backgrounds and scientific disciplines among genomics researchers will increase the diversity of methods and outcomes and thus decrease genomics research’s exacerbation of health disparities.
Building Partnerships to Ensure Health Equity in Genomics
Although we seek advice from experts in the field, the genomics community often calls on the same experts to guide future research. The Future Directions in Genomics and Health Equity Workshop was held to hear from experts in genomics and health disparities that NIH has not traditionally included in an advisory capacity. However, it is important to integrate community engagement with all communities in all stages of genomics research to understand and address structural inequities. Many of the challenges involved in ensuring that genomics research is aligned with community values and practices can be addressed by meaningful community engagement, community-informed and culturally tailored genomics education, and community-engaged research strategies that recognize the importance of context and external validity of research interventions8. Community engagement may not always end with the identification of mutually beneficial ways to address both community and research needs, but community values and contributions should always be respected. In addition, engagement with participants and communities may ultimately result in concerns not being alleviated and thus individuals and/or communities deciding not to participate in genomics research. The decision not to participate must also be respected and treated as a learning opportunity.
Communities are also ideal places from which research staff can be recruited, trained, and supported, which will strengthen the links between community engagement and workforce diversity. These activities can be enhanced by a rigorous review of proposed community engagement plans as part of the review of genomics research applications.
Community-researcher partnerships are recommended to translate genomics research into public benefit and to address the needs of diverse and under-resourced communities9. Such partnerships can promote equity between and among institutions and community members. Community-based approaches can also facilitate co-learning, power sharing, mutual contributions to decision making, and priority setting by all partners, with the core goal of minimizing inequities in social and health outcomes often faced by underserved populations and communities8. These approaches have been beneficial in genomics research programs such as the Implementing Genomics in Practice (IGNITE) Network10 and the Clinical Sequencing Evidence-Generating Research (CSER) consortium11, in which community input and recommendations were integrated into study designs of the programs. In addition, resources are needed to help the genomics community disseminate information that promotes health equity as being central to all aspects of genomics research and genomic medicine implementation12. Workshop attendees strongly recommended that there be sufficient time and equitable resource distribution and funding for appropriate community engagement.
Measuring Health Equity
Although one of the guiding principles of the 2020 NHGRI Strategic Vision (https://www.genome.gov/2020SV) is to maximize the utility of genomics for all members of the public, equity is often not at the forefront of genomics research. An equity lens should be applied to all research, including genomics research, to assess how social, constructed, and natural environments influence health and how these environments influence biomedical research findings and health outcomes2. As recommended in the workshop, genomics research should include a robust understanding of contextual variables and emphasize diverse settings, as well as include clear and measurable metrics to assess health equity in genomics research and genomic medicine. Ensuring genomics has a positive effect on health equity should cross the whole spectrum of NHGRI’s research portfolio. This includes equitably selecting populations for research to understand the biology of genomes, increasing diversity in genomics databases, leveraging computational tools to facilitate access to and analysis of genomic data across all populations, assessing the ethical, legal, and social implications of genomic advances, and equitably implementing genomics research and its technology.
As genomic researchers and clinicians move forward with using a health equity lens, there will be challenges to not only achieving but also measuring health equity in the context of genomics1. Standardized measures and funding to develop new outcome measurements are needed to help the genomics community review, examine, and identify the effects of genomics research and genomic medicine implementation on health equity9. Assessing health equity should also include establishing the adequacy in including diverse populations, providing access to genomic testing, and ensuring high-quality clinical use of genomic findings.
Measuring health equity should account for the imbalance and harm caused by oppression and biases including racism, ableism, sexism, heterosexism, sex binarism, etc.13. There should also be integration of social vulnerability metrics within the measurement plans, assessment of the effects of public policies on public health, and consideration of the immediate and sustained benefit of genomics research for diverse, low-resourced, and underserved communities, as well as other communities that may be considered vulnerable9. Studies should measure the interrelationships among different social determinants of health and physical health and include such standardized measures in all genomics studies14. In addition, there should be proper analytical tools to facilitate accurate interpretation of these data15.
Braveman and colleagues recommend a systematic approach to measuring health equity, such as comparing the population group of interest for a health indicator with groups that are in the most advantaged social position16. Disadvantaged groups represent a large portion of the population, and this approach compares the disadvantaged groups largely with themselves, thereby underestimating the size of the gap between the disadvantaged and the advantaged. This is something that could be implemented as the field assesses the impact of genomics research on health equity. In addition, pathways and processes influencing structural determinants of health should be defined when measuring health equity. Consistent with these ideas, workshop attendees recommended that training on the collection and analysis of social or structural determinants of health be included. Longer-term training opportunities on the analysis of social determinants of health in underrepresented populations were also recommended.
Policy Development
Historically, genomics research often used race as a surrogate for describing human genomic variation, although race is fluid and was developed as a social concept17. The use of race reinforces the view that humans can be classified into discrete, innate categories, which is fundamentally incorrect. Genomics researchers continue to use race as a proxy for social and environmental factors, but it is recommended that researchers incorporate such factors into their analyses and use variables that capture more precise information. If population descriptors are used, the recommendations from the literature review and the workshop explicitly encourage genomics researchers to explain why and how population descriptors were selected and consider using multiple descriptors for each study participant to improve clarity (https://doi.org/10.17226/26902). As recommended by the 2023 NASEM Consensus Study on Population Descriptors, policies are needed to ensure that race and ethnicity are not incorrectly used in genomics research (https://nap.nationalacademies.org/catalog/26902/using-population-descriptors-in-genetics-and-genomics-research-a-new).
Millions of dollars are spent on genomics research every year, but policies do not exist to ensure that genomics increases equity in health rather than exacerbating existing disparities. System-level approaches are needed to reduce health disparities and advance health equity in genomics. These should include advancing genomic literacy, decreasing barriers in genomics, and increasing access to genomic testing and genomic information. Organizations that are leaders in genomics, such as NHGRI, must contribute to the development of goals, objectives, and strategies to move towards health equity in hand with genomic advances. In addition, policies are needed that encourage institutions and health systems to develop and implement strategies focused on health equity and that are informed by diverse groups18.
Institutions should encourage partnerships and involve organizational leaders to maximize the potential for effective impact for institutional and systemic change to achieve health equity. Workshop attendees recommended research agencies provide funding to evaluate health equity and integrate health equity considerations into genomic research programs. The workshop discussion also addressed the need for policies related to funding diverse research, including calling to increase funding for investigators from diverse backgrounds as well as diverse institutions and settings, such as minority-serving institutions. Funding to build infrastructure and increase capacity for technology development, as well as generating, storing, analyzing, and using genomic data from underserved populations, is also needed. To ensure that the impact of genomics research on health equity is assessed going forward, evaluation of health equity impact should be included in funding applications and incorporated into scores during scientific review. Moreover, the importance of conducting research and practicing medicine through a health equity lens should be taught as core competencies in education and training (https://public.csr.nih.gov/AboutCSR/Address-Bias-in-Peer-Review). The appropriate training of reviewers and funders about diversity, cultural awareness and sensitivity, and inclusion is important for mitigating bias in peer review and funding decisions.
Conclusion
Genomic research has led to many advancements in clinical care, yet inequities still remain. This paper recommends needed components and tools to direct genomics research to have a positive impact on health equity. The consensus of both the workshop and literature review is that research is needed to understand both the effects of genomics on health equity and how to disseminate and implement genomic strategies to increase health equity. A revision to the policies and practices in genomics research cannot resolve health disparities alone, rather we need to more fully account for historical, cultural, social, and economic forces that shape the unequal implementation of genomics in diverse communities. Designing optimal dissemination models should account for factors that likely influence intervention uptake and effectiveness in different groups, including under-resourced populations. Growing the capacity for technology development and genomic data generation, storage, and analyses in underserved institutions and populations is also needed. Such advances require organizational commitment and resources.
Ensuring health equity in genomics will require new investments, creative partnerships, improved policies, and a prioritization in all aspects of genomics research. It will also require the inclusion of diverse populations as both active research participants and members of the genomics workforce, thereby bringing diverse perspectives and novel ideas. Genomics investigators should seek cross-disciplinary expertise to incorporate knowledge of social and structural factors and to engage underserved populations in the development, design, and evaluation of the research being conducted. Genomics research should also account for the various facets of diversity inherent to the communities and populations where the burden of health disparities and mortality is particularly high.
In summary, genomics research can make important contributions to health equity if designed and conducted appropriately. Regardless of the primary goal of the study, genomics research should endeavor to design and implement research practices and findings in a manner that does not exacerbate health disparities. For example, study designs should consider the current environment of structural inequality that exists in today’s society. This can include measuring social determinants of health and evaluating whether genomic advances are increasing or decreasing health equity. Through such efforts, health equity becomes an important lens through which all research activities, analyses, and outcomes are viewed. Conducting genomics research with a health equity lens will increase the generalizability of research results and thus lead to inclusive implementation and improved genomic medicine opportunities. This in turn will help genomics research move towards achieving health equity.
Figure 1.
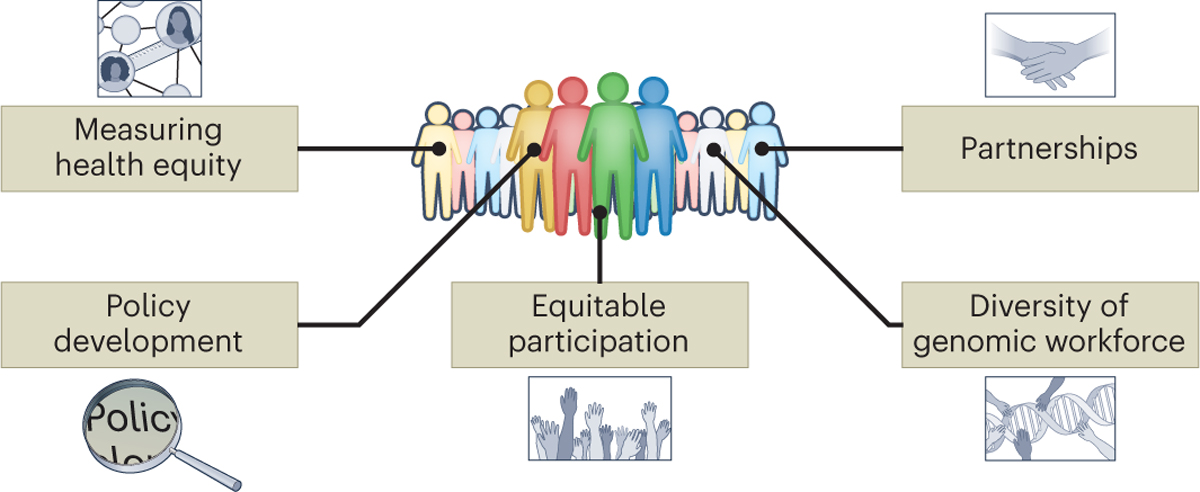
Elements Needed to Increase Health Equity in Genomics Courtesy: National Human Genome Research Institute: www.genome.gov
Created by Darryl Leja, NHGRI
This figure includes graphical illustrations of the elements needed to increase health equity in genomics: measuring health equity, policy development, equitable participation, diversity of the genomics workforce, and partnerships.
Box 1. Definitions.
Health disparity is “a health difference that adversely affects defined disadvantaged populations, based on one or more health outcomes.” The National Institute of Minority Health and Health Disparities (https://www.nimhd.nih.gov/)
Health equity is the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, sex identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes. The Centers for Medicare and Medicaid Services (https://www.cms.gov/pillar/health-equity).
Interpersonal relates to relationships or interactions between people.
Population is a group of people that are identified by a chosen shared characteristic or shared characteristics.
Structural racism are the “ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care and criminal justice” (https://www.ama-assn.org/delivering-care/health-equity/what-structural-racism).
Systemic racism is the oppression of a racial group to the advantage of another as perpetuated by inequity within interconnected systems such as political, economic, and social systems (https://www.merriam-webster.com/dictionary/systemic%20racism).
Acknowledgments
We would like to thank the attendees of the Future Directions in Genomics and Health Equity Workshop, the NHGRI TiDHE Office, and the NHGRI Office of Communication for their expertise, assistance, and thoughtful perspectives and recommendations.
E.B.M. took the lead in writing the manuscript with input from all authors. V.L.B., E.D.G., E.J.P-S., L.A.H., and S.S-J.L. made major contributions and performed critical revisions to the manuscript. R.L.B., N.C.L., and M.S. have given critical feedback and edits to the manuscript. T.H.A., K.E.B., E.G.B., J.D.C., N.J.C., V.D.F., D.A.D., F.E.F., S.M.F., N.A.G., V.H. C.M.H-A., J.E.K.H., C.R.H., C.A.H.H., M.I., A.J., R.A.K., L.G.L., J.T.L., N.A.L., E.O.O., L.S., L.E.S., J.L.T., B.S.W., G.W. and J.H.C. have made content recommendations that helped shape the manuscript. All authors provided critical feedback and helped shape the manuscript.
Footnotes
Competing Interest Statement: M.S. is a member of the Institutional Review Board for the All of Us Research Program. M.I. is a trustee of the Public Health Genomics (PHG) Foundation, member of the Scientific Advisory Board of Open Targets, and has research collaborations with AstraZeneca, Nightingale Health, and Pfizer (unrelated to the work of the manuscript). All other authors confirm that there are no financial or non-financial interests that may bias the conclusions, implications, or opinions stated.
References
- 1.Carnethon MR, Kershaw KN, & Kandula NR Disparities Research, Disparities Researchers, and Health Equity. JAMA 323, 3 (2020). [DOI] [PubMed] [Google Scholar]
- 2.Gomez CA Dushanka, Kleinman V, Pronk N, Wrenn Gordon GL, Ochiai E, Blakey C, Johnson A, & Brewer KH Addressing Health Equity and Social Determinants of Health Through Healthy People 2030. J of Public Health Manag Pract 27, S249–S257 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Westfall JM, Roper R Gaglioti A, & Nease DE Jr. Practice-based Research Networks: Strategic Opportunities to Advance Implementation Research for Health Equity. Ethnicity & Disease, 29 (Suppl 1), 113–118 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jooma S, Hahn MJ, Hindorff LA & Bonham VL Defining and Achieving Health Equity in Genomic Medicine. Ethnicity & Disease 29 (Suppl 1):173–178 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonham VL Examining How Race, Ethnicity, and Ancestry Data Are Used in Biomedical Research. JAMA 320 (15), 1533–1534 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saunkeah B, Beans JA, Peercy MT, Hiratsuka VY, & Spicer P Extending Research Protections to Tribal Communities. American Journal of Bioethics 21 (20), 5–12 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDonald KE, Schwartz AE, & Sabatello M Eligibility criteria in NIH-funded clinical trials: Can adults with intellectual disability gen in? Disabil Health J. 15(4),101368 (2022). [DOI] [PubMed] [Google Scholar]
- 8.Dickson E, Magarati M, Boursaw B, Oetzel J Devia C Ortiz K, & Wallerstein N Characteristics and Practices Within Research Partnerships for Health and Social Equity. Nursing Research 69 (1), 51–61 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castillo EG & Harris C Directing Research Toward Health Equity: a Health Equity Research Impact Assessment. J Gen Intern Med 36(9):2803–2808 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horowitz CR, Ferryman K, Negron R, Sabin T, Rodriguez M Zinberg RF, Böttinger E & Robinson M Race, Genomics and Chronic Disease: What Patients with African Ancestry Have to Say. J Health Care Poor Underserved 28(1):248–260 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Daniel JM, Ackerman S, Desrosiers LR, Rego S, Knight SJ, Mollison L, Byfield G, Anderson KP, Danila MI, Horowitz CR, Joseph G, Lamoure G, Lindberg NM, McMullen CK, Mittendorf KF, Ramos MA, Robinson M, Sillari C, Madden EB: CSER Stakeholder and Engagement Work Group. Genet Med 24(5):1108–1119 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liburd LC, Hall JE, Mpofu JJ, Williams SM, Bouye K, & Penman-Aguilar A Addressing Health Equity in Public Health Practice: Frameworks, Promising Strategies, and Measurement Considerations. Annu. Rev. Public Health 41, 417–432 (2020). [DOI] [PubMed] [Google Scholar]
- 13.Krieger N Measures of Racism, Sexism, Heterosexism, and Gender Binarism for Health Equity Research: From Structural Injustice to Embodied Harm—An Ecosocial Analysis Annu Rev Public Health 41, 37–62 (2020). [DOI] [PubMed] [Google Scholar]
- 14.Dover DC & Belon AP The health equity measurement framework: a comprehensive model to measure social inequities in health. Int J Equity Health 18, 36 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, & Beckles G Measurement of Health Disparities, Health Inequities, and Social Determinants of Health to Support the Advancement of Health Equity. J Public Health Manag Pract. 22(Suppl 1) S33–S42 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braveman P, Arkin E, Orleans T, Proctor D, Acker J & Plough A What is Health Equity? Behavioral Science & Policy 4 (1), 1–14 (2018). [Google Scholar]
- 17.Byeon YJJ, Islamaj R, Yeganova L, Wilbur WJ, Lu Z, Brody LC & Bonham VL Evolving use of ancestry, ethnicity, and race in genetics research-A survey spanning seven decades. Am J Hum Genet 108 (12), 2215–2223 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mulder NJ, Adebiyi E, Adebiyi M, Adeyemi S, Ahmed A, Ahmed R, Akanle B, Alibi M, Armstrong DL, Aron S, Ashano E, Baichoo S, Benkahla A, Brown DK, Chimusa ER, Fadlelmola FM, Falola D, Fatumo S, Ghedira K, Ghouila A, Hazelhurst S, Isewon I, Jung S, Kassim SK, Kayondo JK, Mbiyavanga M, Meintjes A, Mohammed S, Mosaku A, Moussa A, Muhammad M, Mungloo-Dilmohamud Z, Nashiru O, Odia T, Okafor A, Oladipo O, Osamor V, Oyelade J, Sadki K, Salifu SP, Soyemi J, Panji S, Radouani F, Souiai O, Bishop ÖT; H3ABioNet Consortium, as members of the H3Africa Consortium. Development of Bioinformatics Infrastructure for Genomics Research. Glob Heart 12(2):91–98 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]


