Key Teaching Points.
-
•
Cardiovascular magnetic resonance imaging (CMR) is a critical component of disease surveillance in pediatric heart disease, but diagnostic quality is limited in the setting of a cardiac implantable electronic device (CIED).
-
•
Wideband CMR sequences can reduce artifact to produce diagnostically acceptable image quality in a pediatric patient with a CIED.
-
•
Wideband late gadolinium enhancement and perfusion CMR can be a safe and effective way to assess myocardial scar, perfusion defects, and cardiac function in a pediatric patient with a CIED.
-
•
Further studies are warranted to fully evaluate the performance of wideband pulse sequences in a larger cohort of patients, including those with epicardial CIED systems.
Introduction
Cardiac implantable electronic devices (CIEDs) such as pacemakers and implantable cardioverter defibrillators (ICDs) are a critical component of pediatric cardiac care, particularly in congenital heart disease.1 CIEDs can be life saving, increase longevity, and improve quality of life. Some children may even receive a CIED within the first few hours of life. Children with CIEDs frequently require cardiovascular magnetic resonance imaging (CMR) for disease surveillance and therapeutic management, including surgical planning.2 Decisions regarding preferred imaging modality and CIED implantation techniques are complex and require consideration of possible risks and benefits.
Current consensus statements support that magnetic resonance imaging (MRI) can be performed with manageable risks on pediatric patients with a CIED.2, 3, 4 Even in MRI-conditional CIED systems, however, image artifact owing to the CIED can decrease the diagnostic yield. This artifact may be intensified in pediatric patients, as the generator is typically closer to the heart and imaging is acquired at faster heart rates.
The utility of “wideband” late gadolinium enhanced pulse sequences for suppressing image artifacts induced by the generator of a CIED has been reported at 1.5T and 3T MRI scanners.5,6 Our group has previously shown less image artifact using wideband late gadolinium enhancement (LGE) in a patient with a subcutaneous ICD compared with standard LGE.7 Our group has also developed the first wideband cardiac perfusion and cardiac T1 mapping MRI protocol in adults; however, this wideband sequence has not previously been adapted for children.8,9
The capability of wideband CMR to suppress image artifacts in a pediatric patient with a magnetic resonance (MR)-conditional device is unknown. This case report demonstrates that wideband CMR pulse sequences in a pediatric patient with a transvenous MR-conditional CIED can produce diagnostically acceptable image quality.
Case report
A 15-year-old female patient with a transvenous dual-chamber pacemaker for atrioventricular (AV) conduction disease was referred in 2021 for CMR to further evaluate the etiology of new left ventricular dysfunction on echocardiogram. She was below the 1st percentile in height (55.5 inches/141 cm) and at the 35th percentile in weight (50.3 kg). The patient was diagnosed with medulloblastoma at 4 years of age for which she underwent chemotherapy per ACNS 0331, craniospinal radiation (2340 CSI with PF boost to 5400 cGy), and tumor resection in 2009. Post tumor resection, she developed hypothyroidism. From a rhythm perspective, she initially developed left axis deviation and right bundle branch block in 2015 at 9 years of age and then presented with persistent hemodynamically stable complete AV block in 2017 at 11 years of age with a junctional escape rhythm of 30–50 beats per minute. She underwent left-sided transvenous dual-chamber pacemaker implantation in 2017 at 12 years of age with an MR-conditional (1.5T and 3T) Medtronic Advisa model A2DR01 generator in a standard left-sided subclavicular position and 2 MR-conditional Medtronic 5076 pacing leads (Figure 1).
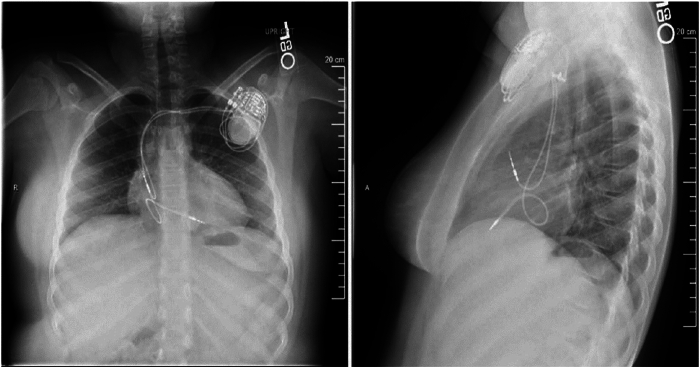
Figure 1.
Anterior-posterior (left) and lateral (right) radiographs at the time of cardiac implantable electronic device (CIED) implant demonstrating the location of the CIED leads and pulse generator.
Prior to pacemaker insertion, a baseline CMR demonstrated normal biventricular size and function, no regional wall motion abnormalities, no LGE, and normal T1, T2, and extracellular volume values. Following pacemaker insertion, the patient was followed with serial echocardiograms to monitor ventricular chamber sizes and function. Her echocardiogram 1 year after pacemaker implant showed normal biventricular function, but her echocardiogram 3 years after implant showed severely depressed left ventricular function. The differential diagnosis for her ventricular dysfunction included metabolic and thyroid abnormalities, pacemaker-induced cardiomyopathy, and chemotherapy-related cardiotoxicity. She was referred for CMR for further diagnostic evaluation. At the time of referral, the patient was deemed to be pacemaker dependent and required ventricular pacing 100% of the time.
Per institutional clinical practice, a physician obtained written consent. The patient was scanned on a 1.5T MRI scanner (Aera; Siemens Healthcare, Erlangen, Germany) under general anesthesia. The imaging protocol included CIED interrogation and programming before and after MRI by electrophysiology staff, vital sign and hemodynamic monitoring throughout the scan by anesthesia staff, and specific absorption rate <2.0 W/kg.
CMR pulse sequences tailored for scanning patients with a CIED was used. Specific pulse sequences included cine [function, volumes], resting perfusion, and LGE [scar]. Pertinent imaging parameters are summarized in Table 1.
Table 1.
Relevant parameters for wideband late gadolinium enhancement and perfusion cardiac magnetic resonance pulse sequences
| Parameters | Wideband perfusion | Standard/wideband LGE |
|---|---|---|
| Field of view | 300 mm × 300 mm | 300 mm × 225 mm |
| Acquisition matrix | 192 × 192 | 256 × 192 |
| Spatial resolution | 1.6 mm × 1.6 mm | 1.2 mm × 1.2 mm |
| Slice thickness | 8 mm | 7 mm |
| TE/TR | 1.3/2.5 ms | 1.9/4.3 ms |
| k-space lines per readout | 33 | 24 |
| Readout duration per image per heartbeat | 82.5 ms | 103.2 ms |
| TS or TI | 100 ms | 300 ms |
| Number of slices per heartbeat | 3 | |
| Receiver bandwidth | 1002 Hz/pixel | 501 Hz/pixel |
| Flip angle | 15° | 20° |
| Acceleration factor | 5.8 | 1.8 |
| Number of repetitions | 100 | 1 |
| Total scan time | 100 heartbeats | 9 heartbeats |
Wideband perfusion images were reconstructed using compressed sensing, whereas wideband LGE images were reconstructed using Generalized Autocalibrating Partially Parallel Acquisitions (GRAPPA). The perfusion scan was conducted during free breathing, whereas the LGE scan was performed with the respirator turned off (ie, breath-hold). The main difference between standard and wideband LGE pulse sequences was the frequency bandwidth of the inversion pulse: 1 kHz for standard and 4 kHz for wideband. LGE = late gadolinium enhancement; TE = echo time; TI = inversion time; TR = repetition time; TS = time from saturation pulse to sample the center of k-space.
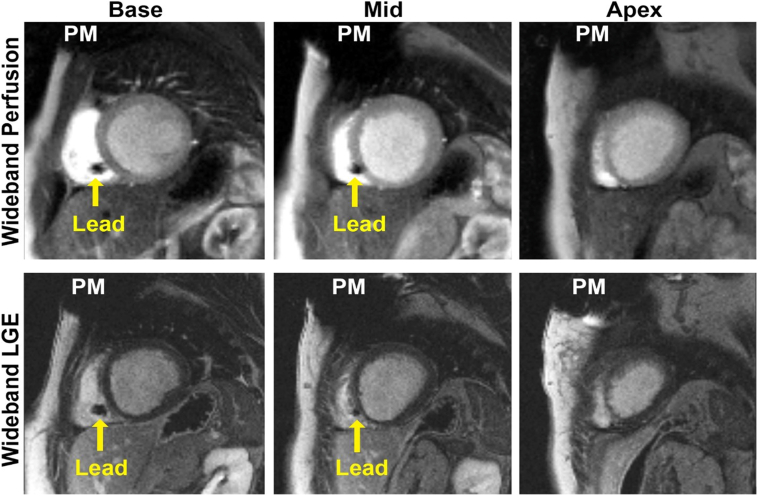
CMR revealed a severely dilated left ventricle (end-diastolic volume = 184 mL; end-diastolic volume indexed for body surface area = 131 mL/m2), a top normal left ventricular mass with normal wall thicknesses, and moderately to severely depressed global left ventricular systolic function (ejection fraction = 26%). There were regional wall motion abnormalities, including an akinetic inferior wall and hypokinetic septum with paradoxical motion from the base to mid left ventricular chamber, which was new from the baseline CMR 4 years prior. There was no evidence of rest perfusion abnormalities or LGE. The right ventricular size and systolic function were normal. Significant dyssynchrony was noted between the right and left ventricles, presumably due to pacing. As shown in Figure 2, there were no pacemaker-induced image artifacts involving the myocardium for wideband perfusion or wideband LGE. The only CIED image artifacts were signal voids within the left lateral chest wall and along the trajectory of the intracardiac leads without obstructing myocardial tissue.
Figure 2.
Cardiac magnetic resonance images using wideband perfusion and late gadolinium enhancement (LGE). Image artifact in these projections is signal void. The majority of signal void is in the small area surrounding the pacemaker (PM) pulse generator. There is a small area of signal void surrounding each lead (yellow arrows). Neither artifact interferes with visualization of myocardial wall.
There were no patient or device complications during the scan. There were no heart rate or rhythm disturbances detected during the CMR or in the post-anesthesia monitoring period by an external patient monitoring device or by the patient’s CIED. The device interrogations immediately after CMR and during serial evaluations from 2 months to 2.5 years after CMR showed appropriate device function, expected battery life, and stable lead characteristics, including sensing, impedance, and capture thresholds.
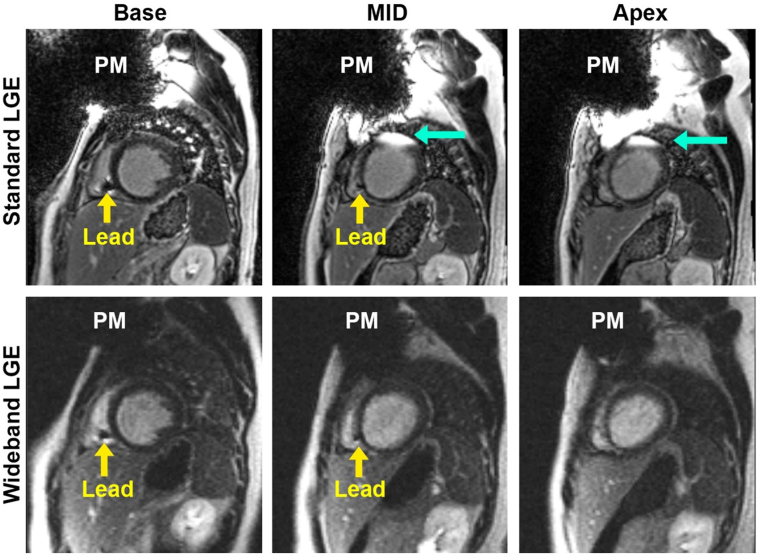
The patient underwent a follow-up CMR 31 months later. As shown in Figure 3, standard LGE produced considerable image artifacts induced by the CIED generator, whereas wideband LGE effectively suppressed the image artifacts.
Figure 3.
The same patient (shown in Figure 2) underwent follow-up cardiovascular magnetic resonance imaging 31 months later: (top row) standard late gadolinium enhancement (LGE) and (bottom row) wideband LGE. As shown, standard LGE produced hyperintense image artifacts caused by the generator (cyan arrows), whereas wideband LGE suppressed the image artifacts.
Discussion
To our knowledge, this is the first utilization of wideband LGE and perfusion CMR pulse sequences in a pediatric patient with a CIED. This case report provides 2 unique contributions to the literature. First, wideband sequences produced minimal image artifacts and enabled readers to evaluate for myocardial scar and rest perfusion abnormalities. The artifact-free images permitted direct comparison of function, chamber sizes, and myocardial characterization to the baseline CMR obtained prior to CIED placement. Second, wideband sequences were clinically safe in a pediatric patient. Our patient was pacemaker dependent, but there were no complications during the scan, and the CIED system had stable characteristics at up to 2.5 years follow-up.
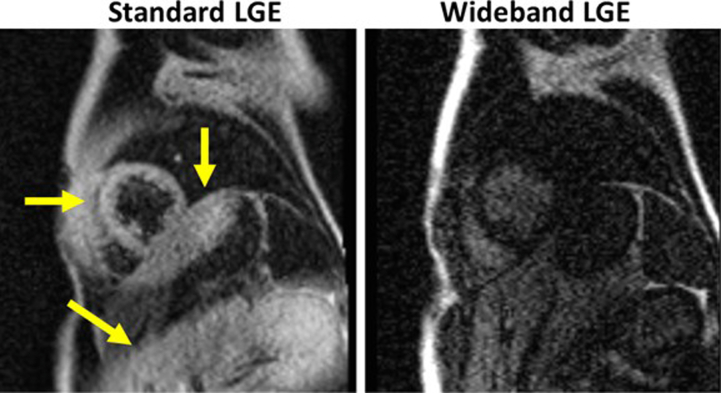
CIED pulse generators can cause artifacts during conventional CMR, including hyperintense signals in LGE and perfusion images and geometric image distortions and signal loss in the slices including and surrounding the CIED. This is caused by an alteration in the local magnetic field.10,11 The ideal way to reduce imaging artifact is to acquire images as far away from the CIED as possible, but this strategy is limited when obtaining cardiac imaging in small, pediatric patients.11,12 A recently published pediatric study found that 6 of 9 patients with uninterpretable MRI were <18 years of age.4 As patient factors (eg, body shape and size, anatomy) and device factors (eg, model, size, shape, position in the body) cannot be changed, we propose that wideband sequencing is an alternative strategy to reduce potential image artifact. One limitation of this work is that a 15-year-old patient at the 1st percentile of height is still a transitional step between adult patients and small children. Moving forward, we hope to apply this technology in smaller patients and epicardial systems. Our preliminary study involving an 11-year-old female volunteer with an ICD pulse generator taped on her abdomen to mimic an epicardial CIED system suggests that wideband LGE is superior to standard LGE in suppressing image artifacts induced by the ICD (see Supplemental Materials for details on the experiment and results).
There are urgent clinical implications for the ability of wideband LGE and perfusion imaging to suppress image artifacts in pediatric patients with a CIED. Current guidelines state it is appropriate for a pediatric patient with an MR-conditional CIED and normal cardiac anatomy to undergo CMR following the appropriate procedural recommendations.2 This includes patients with conduction abnormalities like our patient and those with either acquired or inherited cardiomyopathies who often need CIEDs.1, 2, 3, 4 Conduction abnormalities and tachyarrhythmias necessitating CIED can also be related to congenital heart disease, and CMR in these patients can be used for disease surveillance and therapeutic planning. Specifically, CMR can evaluate cardiac anatomy, surgical repair outcomes, cardiac chamber sizes and function, and myocardial characteristics. Owing to concern for device artifact reducing the diagnostic utility of CMR, many children with CIEDs who require cross-sectional imaging undergo computed tomography resulting in increased radiation exposure.
Conclusion
In summary, this case report demonstrates wideband LGE and perfusion CMR is a safe and effective way to assess myocardial scar, perfusion defects, and cardiac function in a pediatric patient with an MR-conditional transvenous pacemaker. Further studies are warranted to fully evaluate the performance of wideband pulse sequences in a larger cohort of patients of different sizes and device types. This includes patients with epicardial CIED systems who are typically smaller and have generators in closer proximity to the heart.
Disclosures
The authors have no conflicts of interest to report.
Acknowledgments
Funding Sources
This work was supported by the National Institutes of Health’s National Heart, Lung, and Blood Institute (R01HL151079), National Institutes of Health’s National Center for Advancing Translational Sciences (KL2TR001424), and the Brett Boyer Foundation.
Footnotes
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hrcr.2024.02.003.
Appendix. Supplementary Data
Supplementary Figure 1.
References
- 1.Shah M.J., Silka M.J., Silva J.N.A., et al. 2021 PACES expert consensus statement on the indications and management of cardiovascular implantable electronic devices in pediatric patients. Heart Rhythm. 2021;18:1888–1924. doi: 10.1016/j.hrthm.2021.07.038. [DOI] [PubMed] [Google Scholar]
- 2.Indik J.H., Gimbel J.R., Abe H., et al. 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Heart Rhythm. 2017;14:e97–e153. doi: 10.1016/j.hrthm.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 3.Pulver A.F., Puchalski M.D., Bradley D.J., et al. Safety and imaging quality of MRI in pediatric and adult congenital heart disease patients with pacemakers. Pacing Clin Electrophysiol. 2009;32:450–456. doi: 10.1111/j.1540-8159.2009.02304.x. [DOI] [PubMed] [Google Scholar]
- 4.Gakenheimer-Smith L., Etheridge S.P., Niu M.C., et al. MRI in pediatric and congenital heart disease patients with CIEDs and epicardial or abandoned leads. Pacing Clin Electrophysiol. 2020;43:797–804. doi: 10.1111/pace.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rashid S., Rapacchi S., Vaseghi M., et al. Improved late gadolinium enhancement MR imaging for patients with implanted cardiac devices. Radiology. 2014;270:269–274. doi: 10.1148/radiol.13130942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranjan R., McGann C.J., Jeong E.K., et al. Wideband late gadolinium enhanced magnetic resonance imaging for imaging myocardial scar without image artefacts induced by implantable cardioverter-defibrillator: a feasibility study at 3 T. Europace. 2015;17:483–488. doi: 10.1093/europace/euu263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahsepar A.A., Collins J.D., Knight B.P., Hong K., Carr J.C., Kim D. Wideband LGE MRI permits unobstructed viewing of myocardial scarring in a patient with an MR-conditional subcutaneous implantable cardioverter-defibrillator. Clin Imaging. 2018;50:294–296. doi: 10.1016/j.clinimag.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong K., Collins J.D., Knight B.P., Carr J.C., Lee D.C., Kim D. Wideband myocardial perfusion pulse sequence for imaging patients with a cardiac implantable electronic device. Magn Reson Med. 2019;81:1219–1228. doi: 10.1002/mrm.27458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hong K., Jeong E.K., Wall T.S., Drakos S.G., Kim D. Wideband arrhythmia-insensitive-rapid (AIR) pulse sequence for cardiac T1 mapping without image artifacts induced by an implantable-cardioverter-defibrillator. Magn Reson Med. 2015;74:336–345. doi: 10.1002/mrm.25712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sommer T., Naehle C.P., Yang A., et al. Strategy for safe performance of extrathoracic magnetic resonance imaging at 1.5 tesla in the presence of cardiac pacemakers in non-pacemaker-dependent patients: a prospective study with 115 examinations. Circulation. 2006;114:1285–1292. doi: 10.1161/CIRCULATIONAHA.105.597013. [DOI] [PubMed] [Google Scholar]
- 11.Sasaki T., Hansford R., Zviman M.M., et al. Quantitative assessment of artifacts on cardiac magnetic resonance imaging of patients with pacemakers and implantable cardioverter-defibrillators. Circ Cardiovasc Imaging. 2011;4:662–670. doi: 10.1161/CIRCIMAGING.111.965764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carroll C., Litt H. Patient and device related factors affecting artifact size and cardiac visualization when performing cardiac MRI in patients with implanted defibrillators. J Cardiovasc Magn Reson. 2011;13:P357. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.