Abstract
Ischemic stroke (IS) is one of the leading causes of death and disability. Complicated mechanisms are involved in the pathogenesis of IS. Immunomodulatory mechanisms are crucial to IS. Acupuncture is a traditional non-drug treatment that has been extensively used to treat IS. The exploration of neuroimmune modulation will broaden the understanding of the mechanisms underlying acupuncture treatment. This review summarizes the immune response of immune cells, immune cytokines, and immune organs after an IS. The immunomodulatory mechanisms of acupuncture treatment on the central nervous system and peripheral immunity, as well as the factors that influence the effects of acupuncture treatment, were summarized. We suggest prospects and future directions for research on immunomodulatory mechanisms of acupuncture treatment for IS based on current progress, and we hope that these will provide inspiration for researchers. Additionally, acupuncture has shown favorable outcomes in the treatment of immune-based nervous system diseases, generating new directions for research on possible targets and treatments for immune-based nervous system diseases.
Keywords: immunomodulatory mechanism, acupuncture treatment, ischemic stroke, research progress, future direction, prospects
1. Introduction
Ischemic stroke (IS) is an acute cerebrovascular disease in which blood cannot be supplied to the brain due to a sudden blockage of cerebral vessels (1). IS continues to be the third-leading cause of mortality and disability worldwide, accounting for 5.7% of all deaths and 11.6% of all disabilities worldwide (2). IS survivors often suffer from disabilities that cause a poor quality of life and a heavy economic burden (3). In addition, several comorbidities caused by IS, such as melancholy, epilepsy, exhaustion, and pain, further impair the quality of life of patients (4–7).
An increasing number of studies have shown that the immune response is a double-edged sword in the pathophysiology of IS and has become a breakthrough target in treatment strategies (8). IS induces a series of peripheral and central immune reactions that are crucial to the pathophysiology of development, acute damage cascades, and the chronic course after an IS (9). The acute and chronic phases of IS and the long-term effects of stroke are greatly affected by the immune system (10). The immune response after IS involves innate and adaptive immunity in the central and peripheral nervous systems (11). Targeting regulatory immunity is a promising approach for reducing stroke-related dysfunction.
Acupuncture is a traditional non-pharmacological treatment that dates back thousands of years. It uses needles to penetrate the skin at specific acupoints on the body, head, and ears. Patients with IS receive acupuncture as a complementary medical treatment in various countries, including China, Korea, and the USA (12, 13). Numerous lines of evidence indicated that acupuncture was effective and safe for IS and its complications (14, 15). In addition, acupuncture has been shown to modulate immune responses, particularly neuroimmune responses (16, 17). However, no review has outlined the immunomodulatory mechanisms underlying the effects of acupuncture in the treatment of IS.
In this review, we summarize the immune response following an IS, as well as the immunomodulatory effects of acupuncture in the treatment of IS and its consequences. In addition, we propose some new considerations for the future research direction of acupuncture for IS to provide a new strategy for stroke rehabilitation based on neuroimmune.
2. Immune responses after an ischemic stroke
2.1. Immune cell response after an ischemic stroke
Immune cells are the primary components of the central immune system. Immune cells play a vital role in regulating the progression of IS. These immune cells include microglia, astrocytes, oligodendrocytes (OLs), neutrophils, T cells, B cells, dendritic cells, and macrophages.
2.1.1. Microglia—the first line of defense
Microglia are frequently found as resident immune cells in the central nervous system (CNS) and affect pathological processes such as neuronal healing, antigen presentation, and poststroke inflammation (18). The functions of microglia and monocytes/macrophages in cleaning debris, triggering neuroinflammation, causing tissue damage, and encouraging tissue recovery are believed to be a double-edged sword (19). After an IS, with the release of damage-associated molecular patterns (DAMPs) and cytokines, the microglia are activated and react. The activation of microglia from the brain and macrophages from the blood composes the first line of defense, which is the innate immune response (20). The two main types of microglia, M1-like and M2-like, can be distinguished based on their biological role and the cytokines and chemokines they secrete (21). Two types of microglia play different roles. Clearing cellular debris, secreting anti-inflammatory substances, promoting angiogenesis, enhancing angiogenesis, and synaptic remodeling are performed by M2-like microglia (22, 23). M2-like microglia inhibited inflammatory damage to protect the blood–brain barrier (BBB) by releasing interleukin (IL)-4, IL-10, and transforming growth factor-β1 (TGF-β1) (24). Ischemic neurons cause M1-like microglia to become polarized, and M1-like microglia release proinflammatory substances that wreak havoc in the nervous system and harm neurons (25). M1-like microglia play a hazardous role after IS, such as damaging the BBB and aggravating the harmful inflammation response (26). Most of the activated microglia in the subacute and chronic phases of stroke are M1-like, which is detrimental to brain regeneration, while M2-like microglia predominate in the first 24 h following stroke (27, 28). Some research has verified that the regulation of microglial polarization can be a promising target to treat IS (29, 30).
2.1.2. Astrocytes—double-edged sword for modulation
The most prevalent glial cell type in the CNS, astrocytes, has an essential function (31). Similar to microglia, damaged brain tissues with the secretion of cytokines and DAMPs stimulated the receptors of astrocytes to differentiate phenotype (32). Astrocytes are actived into two polarization states after an IS, named A1 and A2, facilitating the understanding of the reactive state of astrocytes. Numerous processes are related to astrocytes, including homeostasis, neuronal and synaptic development, control of cerebral blood flow, and vascular remodeling and repair (33, 34). A2-subtype astrocytes secrete substances that facilitate the recovery of neurons, including neurotrophic factors, glutamic acid, homocysteine, and cholesterol (35). Nevertheless, A1-subtype astrocyte development is detrimental to neurons, as it prevents effective axonal regeneration (36). M1-like microglia can promote astrocyte activation (34). More in vivo and in vitro research should be conducted to explore astrocyte pathways in the case of IS.
2.1.3. Oligodendrocytes—for preserving axonal integrity
OLs, which create myelin, are discovered in white matter (37). When OLs are affected by ischemic damage, OLs produce tissue demyelination and axonal instability, resulting in various neurological deficits (38). Damaged OLs were replaced to restore saltatory conduction and relieve motor function after an IS. Increasing myelin production, augmenting synaptogenesis, promoting oligodendrogenesis, promoting OLs maturation, and suppressing remyelination are the strategies to target OLs for the treatment of IS (39).
2.1.4. Neutrophils—infiltration from blood
Neutrophils are the first immune cells transported to the CNS from the peripheral immune system after stroke (40). The enhancement in neutrophils results in the disruption of cerebral edema, brain injury, and the BBB after an IS (41). Neutrophils also impact thrombosis and atherosclerosis, which are high risk factors of IS (42, 43). Neutrophils invade the brain during the hyperacute, acute, and subacute phases (44). Importantly, circulating neutrophils are related to stroke severity, stroke outcomes, and stroke prognosis (45). The responses of neutrophils after an IS include three parts: (1) neutrophil activation and recruitment, (2) neutrophil adhesion to endothelial cells, and (3) neutrophil transmigration and neurovascular interactions (46). Cytokines, chemokines, and DAMPs act on neutrophils, which cause the recruitment of neutrophils to the site of injury and the delivery of adhesion molecules (47). Neutrophils are key modulators of IS injury. Thus, researchers show a great interest in neutrophils as treatment targets to prevent IS and relieve ischemic brain injury. The processes of neutrophil recruitment and transmigration can also be potential targets to influence stroke severity in detail (48).
2.1.5. T lymphocytes—their conflicting roles in ischemic stroke
T lymphocytes, which are adaptive immune cells, exacerbate ischemic–reperfusion injury in acute IS, in both an antigen-dependent and an antigen-independent manner (49). T lymphocytes release interferon-gamma (IFN-γ), IL-21, and IL-17, which cause harmful effects in IS (50). On the basis of cell functions, T cells are divided into multiple types marked by CD3 expression, including CD8+ cytotoxic T lymphocytes, CD4+ T helper cells, regulatory T cells (Tregs), and γδ T cells (51). CD4+ T cells are the main effector T cells, which modulate brain inflammation through releasing cytokines after an IS (52). CD4+ T cells play a double-edged role in inflammation regulation after a stroke, with anti-inflammatory and proinflammatory effects. CD8+ T cells play a cytotoxic role and promote cell apoptosis by recognizing antigens on T-cell receptors and releasing granzyme and perforin subsequently after an IS (53). Tregs are a type of T cell that influences immune responses after an IS (54). Tregs secrete anti-inflammatory cytokines, inhibit proinflammatory cytokines, induce cell lysis, promote neural regeneration, and modulate microglial and macrophage polarization after an IS (54). It is currently uncertain if Tregs are helpful or harmful in IS, as well as how they affect IS at different phases. Peripheral γδ T cells infiltrated the lesion site after an IS and aggravated BBB injury (55). Numerous γδ T cells infiltrate the ischemic penumbra, and knockout of γδ T cells relieves motor dysfunction and significantly reduces infarction and BBB damage (55). Though the major function of T cells has already been discovered, their specific role and the mechanism of T cells after a stroke need more attention.
In conclusion, the summary of the type and function of immune cells in IS is shown in Table 1 .
Table 1.
Summary of type and function of immune cells in ischemic stroke.
| Immune cell type | Phenotype | Function |
|---|---|---|
| Microglia | M1-like microglia | Damaging the blood–brain barrier, aggravating the harmful inflammation response, and harming neurons |
| M2-like microglia | Clearing cellular debris, secreting anti-inflammatory substances, promoting angiogenesis, inhibiting inflammatory damage, and protecting the blood–brain barrier | |
| Astrocytes | A1 subtype astrocytes | Preventing effective axonal regeneration |
| A2 subtype astrocytes | Facilitating the recovery of neurons and releasing neurotrophic factors, glutamic acid, homocysteine, and cholesterol | |
| Oligodendrocytes | / | Creating myelin and producing tissue demyelination and axonal instability |
| Neutrophils | / | Destroying neurons and the blood–brain barrier |
| T cells | CD4+ T cells | Exerting anti-inflammatory and proinflammatory effects |
| CD8+ T cells | Playing a cytotoxic role and promoting cell apoptosis | |
| Regulatory T cells | Secreting anti-inflammatory cytokines, inhibiting pro-inflammatory cytokines, inducing cell lysis, promoting neural regeneration, and modulating microglial and macrophage polarization | |
| γδ T cells | Aggravating the blood–brain barrier injury |
2.2. Immune cytokines’ responses after an ischemic stroke
Immune cytokines secreted by immune cells are promising prognostic and predictive biomarkers for predicting stroke outcomes and therapeutic targets in patients with IS (56). They affect infarct and edema volumes (57). The classification of immune cytokines includes proinflammatory and anti-inflammatory cytokines on the basis of their function.
2.2.1. Proinflammatory cytokines
The proinflammatory cytokines mediate brain tissue destruction after an IS. Tumor necrosis factor (TNF), IL-1β, IL-6, IFN-γ, and IL-17 are classical and well-known proinflammatory cytokines (58). TNF-α is produced by various immune cell types and is related to various physiological events, including endothelial necroptosis, breakdown of the BBB, and the results of stroke (26). After a stroke, the expression of TNF-α, IL-1β, and IL-6 increased, aggravating the brain injury (59). IFN-γ, which is a proinflammatory cytokine, is pivotal for activating microglia into neurotoxic phenotypes that induce oxidative stress, severe dysfunction, and neuron death (60). The level of IL-17 increased in patients with IS. IL-17 accelerates neutrophil recruitment to the ischemic hemisphere (61).
2.2.2. Anti-inflammatory cytokines
IL-10, TGF-β1, and IL-4 are classical anti-inflammatory cytokines that mediate neuroprotection. IL-10 has a role in clear vascular endothelial protective properties and neuronal protection after brain injury (62). Once the level of TGF-β1 was upregulated, the apoptosis of neurons was suppressed (63). IL-4 modulates the proliferation of B cells and T cells, and the differentiation of B cells. Enhancing signaling through the IL-4 receptor may alleviate inflammation after ischemia and attenuate sensorimotor and cognitive deficits (64).
2.2.3. Multiple effects cytokines
The current study considers that IL-21 is an anti-inflammatory cytokine after an IS. IL-21R-deficient mice had reduced collateral vascular connections and increased brain infarct volume after ischemic brain injury. Moreover, the IL-21 receptor exerts neuroprotective effects in IS mice (65). However, IL-21 promotes the proinflammatory effects of macrophages during respiratory infection (66).
2.3. Immune organ responses after an ischemic stroke
Immune-related organs include the spleen, bone marrow, thymus, lymph nodes, lungs, liver, adrenal glands, and gut (67). The bone marrow exudes plenty of proinflammatory cells and cytokines, resulting in exacerbating peripheral inflammation (68). The gut changes intestinal dysbiosis to affect peripheral inflammation via regulating the gut–brain axis (69). The liver metabolism takes part in immunosuppression, inflammation, and oxidative stress after an IS (70). IS causes pulmonary damage, harmful inflammation, and reduction of alveolar macrophage phagocytic capability, which is related to the brain–lung axis (71). Most studies focus on the changes in the spleen and thymus after an IS, but the research depth is insufficient. Additionally, the function and change of bone marrow, lymph glands, lungs, and intestines after an IS should receive more attention.
2.3.1. The spleen
Spleen weight and size dramatically decreased in middle cerebral artery occlusion (MCAO) rats and mice, and spleen atrophy and cell death occurred after ischemia (72–74). The number of serum leukocytes is adversely linked to changes in spleen size in patients (75). At 24 h after ischemia, MCAO rats with splenectomies had lower levels of proinflammatory cytokines, fewer T cells, neutrophils, and macrophages in the brain tissue, and higher levels of anti-inflammatory factor IL-10, resulting in a smaller infarct size in the brain (76).
2.3.2. The thymus
At 3, 7, and 13 days after reperfusion, the number of CD8α+ T cells in the spleen and thymus of 90-min ischemia–reperfusion (I/R) rats decreased significantly, the TUNEL+ apoptotic cells in the spleen increased significantly, and the numbers of Iba1+ macrophages, CD68+ macrophages, and Ki67+ proliferating cells decreased significantly in the spleen and thymus of 90-min I/R rats and increased in brain tissue (77). The number of CD3+ T cells in the spleen and thymus of 30-min I/R mice was enhanced 24 h after stroke (78). The number of microglia, the level of TNF-α, and the inflammatory microbiota in the spleen and thymus of 60-min I/R rats increased significantly (79).
3. The mechanism of acupuncture treatment regulating immunity in ischemic stroke
In this review, acupuncture treatment includes electroacupuncture (EA) and manual acupuncture (MA). Acupuncture treatment stimulates acupoints to modulate the neuroendocrine–immune network (80). When dealing with various pathological conditions, acupuncture treatment can modulate immune system function, immune cell motivation and phenotypic metamorphosis, and immune cytokine expression. In this section, the mechanism of acupuncture treatment on immunity after an IS was extracted and summarized. As shown in Tables 2 , 3 , authors, animal model, acupoint selection, acupuncture method, stimulation parameter, treatment course, and neuroimmune molecular and cellular results were extracted and summarized ( Tables 2 , 3 ).
Table 2.
Summary of studies exploring the effects of acupuncture treatment on ischemic stroke by modulating the central nervous system.
| Author | Animal model | Acupoint | Acupuncture method | Stimulation parameter | Treatment course | Neuro-immune molecular and cellular results |
|---|---|---|---|---|---|---|
| Han B 2015 | MCAO male Wistar model rats | Neiguan (PC6), Quchi (LI11), Diji (SP8) | EA | 2/15 Hz, 1 mA, 1.5 seconds | 30 min/days, for consecutive 5 days. | Downgrade: TLR4, HMGB1, TRAF6, IKKβ, NF-κB p65 in microglia; TNF-α, IL-1β, IL-6 in brian tissues |
| Cao Y 2020 | CCH male Wistar model rats | Zusanli (ST36), Baihui (GV20) | MA | Twirling reinforcing manipulation | once daily for 2 weeks (continued for 6 days and 1 day of rest) from the third day after surgery |
Downgrade: Iba-1, TNF-α, IL-6 in the hippocampus Upgrade: α7nAChR in neurons, JAK2, STAT3 in Hippocampus |
| Yang J 2019 | CMi male Wistar model rats | Zusanli (ST36) | MA | Twirling reinforcing manipulation | once daily for 2 weeks (with a rest every seventh day) | Downgrade: NF-κB p65 nuclear translocation, hydroxyl radical generation, Ca2+ homeostasis |
| Jittiwat J 2019 | pMCAO male Wistar model rats | Baihui (GV20) | LA | a laser spot diameter of 100 μm, with a laser module output of 100 mW |
Once daily for 14 days | Downgrade: IL-6 in the hippocampus Upgrade: GSH-Px, SOD |
| Li Z 2020 | pMCAO male SD model rats | Baihui (GV20) | MA | The needle was rotated for 1 min at a frequency of 200 rpm and twirled once an hour for 2 hours. | Once daily for three weeks | Downgrade: TNF-α, IL-1β, ROS in the hippocampus Upgrade: BDNF, S100b, GFAP in the hippocampus |
| Xu H 2014 | 2h CIRI male SD model rats | Baihui (GV20), Zusanli (ST36) | EA | continuous-wave, 2Hz, 1mA | once a day for 6 days | Downgrade: TNF-α, HSP70 in serum |
| Xu H 2014② | 2h CIRI male SD model rats | Baihui (GV20), Zusanli (ST36) | MA; EA | MA: twisted 180 degrees at a rate of 10065 twists per min for 1 min, with the twisting procedure repeated at 10-min intervals; EA: continuous-wave, 2Hz, 1mA |
Twice befor euthanasia | Downgrade: MMP2, AQP4, AQP9, MPO+ and CD68+ cell in the ischemic penumbra and the core zone |
| Liu R 2020 | pMCAO male SD model rats | Baihui (GV20), Dazhui (GV24) | EA | sparse-dense, 20Hz, 1-2mA, 30min | Once per day for three days | Downgrade: TNF-α, IL-1β, NF-κB, Iba-1, CD11b |
| Lan L 2013 | 2h I/R male SD model rats | Quchi (LI11), Zusanli (ST36) | EA | 1/20Hz; an intensity of the muscle twitch threshold |
30min, twice | Downgrade: TLR4, NF-κB p65, IκB, TNF-α, IL-1β, IL-6 |
| Wang W 2016 | 2h I/R male SD model rats | Baihui (GV20), Shuigou (GV26) | EA | 2/150Hz; 3mA | 30min, once every 12h, for 3 consecutive days | Upgrade: TGF-β1 |
| Zhou X 2020 | 2h I/R male SD model rats | Baihui (GV20), Hegu (LI4), Taichong (LR3) | EA | 20Hz for 5min and 2Hz for 30min; 1mA | 35min; once a day for 72h | Upgrade: ABIN1 in the peri-infarct cortex, Downgrade: NF-κB, TNF-α, IL-1β, MCP-1 in the peri-infarct cortex |
| Ma Z 2019 | pMCAO male SD model rats | Baihui (GV20) | EA pretreatment | dense-disperse frequency of 2/15 Hz; 1mA; | 30 min; once per day for 5 days before operation | Upgrade: α7nAChR, Arg-1, TGF-β1, IL-10 in the ischemic penumbra Downgrade: iNOS, IL-1β, TNF-α in the ischemic penumbra |
| Lin X 2021 | 2h I/R male SD model rats | Baihui (GV20), Hegu (LI4), Taichong (LR3) | EA | 20Hz for 5min and 2Hz for 30min; 1mA | 35min; once a day for 72h | Upgrade: ym1, arg1, fizz, CD206+/Iba+ cell, CX3CL1+/CX3CR1+ cell, CX3CL1, Downgrade: iNOS, IL-1β, TNF-α, iNOS+/Iba+cell, NLRP3, CX3CR1 |
| Tao J 2015 | 2h I/R male SD model rats | Zusanli (ST36), Quchi (LI11) | EA | a dense disperse wave of 1 or 20 Hz | 30min; once a day for 3 days | Upgrade: GFAP/Vimentin, GFAP/Nestin, the co-expression of GFAP and BrdU, Cyclin D1, CDK4, p-Rb in peri-infarct cortex and striatum |
| Xiao Y 2013 | MCAO male SD model rats | Zusanli (ST36), Quchi (LI11) | EA | 15, 30, 100Hz | 30 min; once a day for 5 days | maintain the structural integrity |
| Liu J 2017 | 2h I/R male SD model rats | Baihui (DU20), Shenting (DU24) | EA | disperse-dense waves of 2-10 Hz; 2-4 mA | 30min; once a day for 7 days, start 2 days after ischemia | Upgrade: α7nAChR in the hippocampus Downgrade: GFAP, Iba1, TNF-α, IL-1β |
| Yang J 2021 | 1h I/R male C57BL/6J model mice | Baihui (GV20) | EA pretreatment | 2/15Hz; 1 mA | 30min; once a day for 5 days | Upgrade: ambient endocannabinoid, astroglial cannabinoid type 1 receptors |
| Lu Y 2015 | MCAO male Wistar model rats | Neiguan (PC6), Quchi (LI11) | EA | 2/15Hz; 1 mA | 20min; once daily for 7 days | Upgrade: GFAP, MCT1 in the ischemic brain tissue |
| Luo Y 2011 | MCAO male Wistar model rats | Baihui (GV20), Dazhui (GV14) | EA | 4/20Hz; 1-3 mA | 30min; once a day for 1, 3, 7, and 21 days each group | Upgrade: EAAT2, CX43 Downgrade: GFAP, Ca2+ in Astrocytes |
| Wang SJ 2003 | 90min I/R male Wistar model rats | D group: Baihui (GV20), Shuigou (GV26); G group: Hanyan (GB4), Xuanlu (GB5), Xuanli (GB6), Qubin (GB7) | EA | 3/20 Hz; 3 mA | 30min; once every other day | Upgrade: VEGF in astrocytes |
| Han X 2010 | MCAO male Wistar model rats | Baihui (GV20), Dazhui (GV14) | EA | 20 Hz; 1-2 mA | 30min; once a day for 28 days | Upgrade: GFAP-immunoreactive cells in the peri-infarct region |
| Ahn SM 2016 | BCAS male C57BL/6 model mice | Baihui (GV20), Dazhui (GV14) | EA | 2 Hz; 2 V | 20min; once daily for 7 consecutive days | Downgrade: neural/glial antigen 2 (NG2) and platelet-derived growth factor receptor-α (PDGFRα) Upgrade: 2,3-cyclic nucleotide-3-phosphodiesterase (CNPase), NT4/5, TrkB, CREB phosphorylation |
| Lee HJ 2022 | 40min I/R male C57BL/6 model mice | Sishencong (EX-HN1), Baihui (GV20) | EA | 2 Hz; 1 mA | 20min; once every other day | Upgrade: NG2-expressing cells, ERK, Akt, BDNF, TGFβ, NT3, pTrkB |
| Liu W 2016 | 2h I/R male SD model rats | Quchi (LI11), Zusanli (ST36) | EA | 1-20 Hz; 0.2 mA | 30min; once a day for three days | Downgrade: Iba-1, ED1 positive microglia, NF-κB p65, IκB-α, p38 MAPK, MyD88 in the peri-infract sensorimotor cortex, TNF-α, IL-1β, IL-6 in serum |
| Zou J 2021 | 60min I/R male C57BL/6 model mice | Shuigou (GV26), Chengjiang (CV24) | EA | 4/16 Hz; initial voltage 1V with a 1V increase every 10min; terminal tension 3V | 30min; both pre- and post-MCAO |
Upgrade: ANXA1, Arg-1, BDNF Downgrade: IL-1β, iNOS, TNF-α |
| Jiang J 2017 | 2h I/R male SD model rats | Baihui (GV20), Hegu (LI4), Taichong (LR3) | EA | 20 Hz and 2 Hz | 35min; once a day for 72h | Upgrade: CYLD Downgrade: NF-κB p65, TNF-α, IL-1β, neuronal CX3CL1 |
| Xu H 2018 | 2h I/R male SD model rats | Baihui (GV20), Hegu (LI4), Taichong (LR3) | EA | 2/20 Hz; 1 mA | 30min; once a day for 72h | Upgrade: TREM2, p-PI3K/PI3K, p-Akt/Akt, p-NF-kB/NF-kB, Arg-1, IL-10 in the ischemic penumbra Downgrade: TNF-α, IL-1β, IL-6 in the ischemic penumbra |
| Chen S 2023 | MCAO male SD model rats | Shuigou (GV26) | EA | 4/20 Hz; 1-3 mA; | 30min; twice a day for 24h | Downgrade: Iba-1, IL-1β, IL-6, Lnc826 |
| Wang F 2013 | 2h I/R male SD model rats | Baihui (GV20) | EA pretreatment | 2/15 Hz; 1 mA | 30min; once a day for 5 days | Downgrade: NDRG2, TUNEL+ |
| Jin Z 2013 | 90min I/R MCPIP1 knockout and C57/BL6 model mice | Baihui (GV20) | EA pretreatment | 2/15 Hz; 1 mA | 30min; once a day for 2 days | Upgrade: monocyte chemotactic protein-induced protein 1 Downgrade: TNF-α, IL-1β, IL-6, MCP-1, NF-κB |
| Lin W 2016 | 2h I/R male SD model rats | Zusanli (ST36), Quchi (LI11) | EA | 1/20 Hz; | 30min; once a day for 72h | Upgrade: miR-9, IκBα Downgrade: NF-κB p65, TNF-α, IL-1β |
| Wang Q 2012 | 2h I/R male SD model rats | Baihui (GV20) | EA | 2/15 Hz; 1 mA | 30min; once a day for 5 days | Upgrade: α7nAChR in ischemic penumbra Downgrade: HMGB1 |
MCAO, middle cerebral artery occlusion; SD, Sprague–Dawley; EA, electroacupuncture; TLR4, toll-like receptor 4; HMGB1, high mobility group box 1; TRAF6, TNF receptor-associated factor 6; IKKβ, inhibitor of kappa B kinase beta; NF-κB, nuclear factor kappa-B; TNF-α, tumor necrosis factor alpha; IL-1β, interleukin-1beta; Iba-1, ionized calcium binding adapter molecule-1; α7nAChR, α7 nicotinic acetylcholine receptor; JAK2, janus kinase 2; STAT3, signal transducer and activator of transcription 3; CCH, chronic cerebral hypoperfusion; CMi, cerebral multi-infarction; GSH-Px, glutathione peroxidase; SOD, superoxide dismutase; MA, manual acupuncture; ROS, reactive oxygen species; BDNF, brain-derived neurotrophic factor; S100B, S100 calcium binding protein B; GFAP, glial fibrillary acidic protein; HSP70, 70-kDa heat shock proteins; CIRI, cerebral ischemia–reperfusion injury; MMP2, matrix metalloproteinase 2; AQP4, aquaporin protein-4; IκB, inhibitor of NF-κB; ABIN1, A20-binding inhibitor of NF-kappaB 1; MCP-1, monocyte chemotactic protein-1; I/R, ischemia–reperfusion; Arg-1, arginase-1; TGF-β1, transforming growth factor-β1; iNOS, inducible nitric oxide synthase; CX3CL1, CX3C motif chemokine ligand 1; CX3CR1, CX3C motif chemokine receptor 1; NLRP3, NOD-like receptor thermal protein domain associated protein 3; MCT1, monocarboxylate transporter 1; EAAT2, excitatory amino acid transporter 2; CX43, connexin 43; VEGF, vascular endothelial growth factor; NG2, neural/glial antigen 2; PDGFRα, platelet-derived growth factor receptor-α; CNPase, 2,3-cyclic nucleotide-3-phosphodiesterase; ERK, extracellular regulating kinase; TrkB, tyrosine kinase receptor B; MAPK, mitogen-activated protein kinase; MyD88, myeloid differentiation primary response gene 88; ANXA1, annexin A1; CYLD, cylindromatosis; TREM2, triggering receptor expressed on myeloid cells-2; NDRG2, n-myc downstream-regulated gene 2; LA, laser acupuncture; MCT1, monocarboxylate transporter 1; VEGF, vascular endothelial growth factor; NDRG2, N-Myc downstream-regulated gene 2; BCAS, bilateral common carotid artery stenosis.
Table 3.
Summary of studies exploring the effects of acupuncture treatment on ischemic stroke by modulating peripheral immunity.
| Author | Animal model | Acupoint | Acupuncture method | Stimulation parameter | Treatment course | Neuro-immune molecular and cellular results |
|---|---|---|---|---|---|---|
| Deng P 2022 | MCAO male C57BL/6 model mice | Baihui (GV20), Zusanli (ST36) | EA | 2Hz; 1mA | 30min; Once daily for 48h | Downgrade: IFNγ+ Th cells, IL-17+ Th cells, IL-33+ cells, ST2+ cells |
| Wang YL 2023 | 2h I/R male SD model rats | Baihui (GV20) | EA | 2/15Hz; 1mA | 20min, 2h and 24h after ischemia | Downgrade: TNF-α and IL-1β in the brain, serum, and small intestine, CXCL1, CXCL2 expression in small intestine, the percentage of the CD4+ cells, TCRγδ+ cells, γδT cells in small intestine, IL-17A in the peri-ischemic cortex and small intestine Upgrade: IL-10 in serum and small intestine, Tregs percentage, Foxp3+ cells %, and the ratio of Treg to γδT cells in small intestine |
| Wang Y 2023 | 2h I/R male SD model rats | Baihui (GV20) | EA | 2/15Hz; 1mA | 20min, once daily for three days | Downgrade: TNF-α, IL-1β, in the peri-ischemic cortex, ischemic hemisphere, and small intestine; Cxcl1, Cxcl2 in ischemic hemisphere, IL-17A in the peri-ischemic cortex and small intestine, TCRγδ+ cells in ischemic hemisphere and small intestine Upgrade: IL-10 in the peri-ischemic cortex and small intestine, Foxp3+ cells %, The ratio of Treg/γδ T cells in ischemic hemisphere and small intestine |
| Qin L 2022 | severe stroke patients | Old Ten Needles | MA | / | once daily for seven days | Upgrade: albumin, prealbumin, hemoglobin, total lympho-cyte count in peripheral blood |
| Jin L 2021 | Cerebral ischemic stroke patients | Baihui (GV20), Shenting (GV24), Sishencong (EX-HN1), Sanyinjiao (SP6), Zusanli (ST36), Neiguan (PC6), Shenmen (HT7) | MA | / | 30min, once daily, for 14 days | Downgrade: CD8+ cell %, CRP, TNF-α, IL-6 in peripheral blood Upgrade: CD3+ cell %, CD4+ cell %, CD4+ cell %/CD8+ cell % in peripheral blood |
IFN-γ, interferon-gamma; TH cell, helper T cell; TCR, T-cell receptor; Tregs, regulatory cells; CRP, C-reactive protein.
3.1. The immunomodulatory effect of acupuncture treatment on the central nervous system
3.1.1. The immunomodulatory effect of acupuncture treatment on immunocytes
3.1.1.1. Microglia
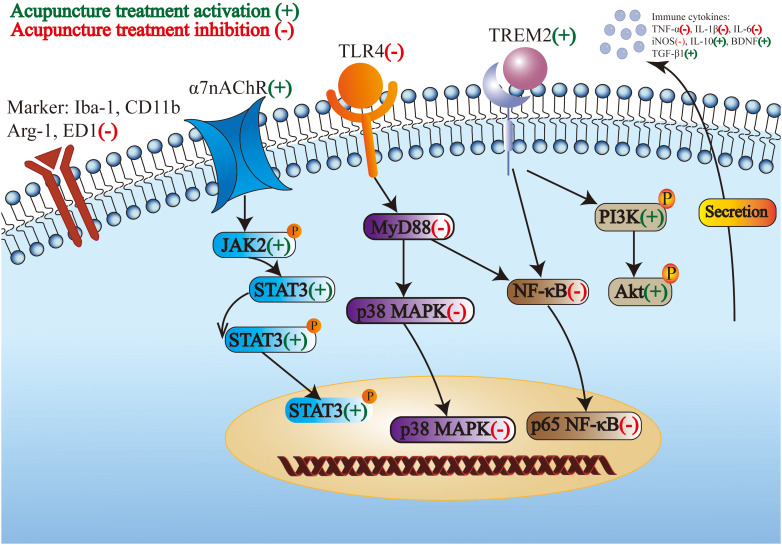
Acupuncture improves stroke by modulating microglial polarization and morphology. Moreover, acupuncture treatment regulates microglial markers, receptors, and signaling pathways. A study showed that EA at GV26 and CV24 relieved neurological deficits by enhancing the expression of annexin A1 and its receptor formyl peptide receptor, promoting M2-like microglia polarization and the levels of arginase-1 (Arg-1) and brain-derived neurotrophic factor (BDNF), and reducing the levels of IL-1β, inducible nitric oxide synthase (iNOS), and TNF-α in the cerebral cortex (81). The nuclear factor kappa-B (NF-κB) is a key nuclear transcription factor, which plays a crucial role in the inflammation and immune responses of cells (82). EA at GV20 and GV24 regulated brain injury-induced inflammation by inhibiting NF-κB activation and decreasing the expression of ionized calcium binding adapter molecule-1 (Iba-1), CD11b, TNF-α, and IL-1β, indicating that EA suppressed the activation of microglia and the inflammatory response in brain tissues (83). EA at LI11 and ST36 reduced infarct volume by attenuating the overactivation of Iba-1 and ED1-positive microglia in the peri-infract sensorimotor cortex, decreasing the level of TNF-α, IL-1β, and IL-6 in serum, and preventing the nucleus translocation of NF-κB p65 and the expression of p38 mitogen-activated protein kinase (p38 MAPK) and myeloid differentiation primary response gene 88 (MyD88) in the peri-infract sensorimotor cortex. These outcomes indicated that EA recovered motor impairment by inhibiting microglia-mediated neuroinflammation (84). EA at PC6, LI11, and SP8 in MCAO rats suppressed the toll-like receptor 4/NF-κB (TLR4/NF-κB) signaling pathway to alleviate microglia activation and inflammation in brain tissues (85). EA at GV20, LI4, and LR3 inhibits neuroinflammatory damage by increasing the A20-binding inhibitor of NF-kappaB 1 (ABIN1) and suppressing NF-κB activation in the peri-infarct cortex, mediating the modulation of microglial polarization (86). EA activated the microglia-specific receptor triggering receptor expressed in myeloid cells 2 (TREM2) through PI3K/AKT and NF-κB signaling pathways to decrease inflammation in the CNS (87).
The cholinergic-anti-inflammatory pathway is the efferent arm of the inflammatory reflex, which mediates the prevention of systemic inflammation by stimulating the vagus nerve (88). The cholinergic anti-inflammatory system involves neuroimmune interactions that produce systemic and anti-inflammatory effects through the α7 nicotinic acetylcholine receptor (α7nAChR). EA pretreatment reduced infarct volume and improved neurological deficits by activating the α7nAChR-mediated phenotypic conversion of microglia, thus reducing the inflammatory response in the ischemic penumbra (89). MA at ST36 and GV20 promoted cognitive function and protected neurons in CCH rats via downregulating the expression of TNF-α and IL-6 and reducing the number of microglia in the hippocampus by activating the janus kinase 2/signal transducer and activator of transcription 3 (JAK2/STAT3) pathway by targeting α7nAChR (90). EA pretreatment inhibits high mobility group box 1 (HMGB1) release by α7nAChR activation in I/R rats (91).
Crosstalk between microglia and neurons is a potential target for neuroimmune regulation (92). EA at GV20, LI4, and LR3 plays anti-inflammatory and neuroprotective roles by upregulating cylindromatosis (CYLD) and CX3C motif chemokine ligand 1 (CX3CL1) expression and downregulating CX3C motif chemokine receptor 1 (CX3CR1) expression, suggesting that the crosstalk between microglia and neurons is regulated. Therefore, M1-like microglial polarization is suppressed, and M2-like microglia polarization is prompted (93). Jiang et al. found that EA at GV20, LI4, and LR3 relieved neurological deficits by upregulating CYLD in neurons, preventing the nucleus translocation of NF-κB p65 in neurons and microglia polarization, and downregulating the expression of TNF-α, IL-1β, and neuronal CX3CL1 in the peri-ischemic area (94). EA at GV26 modulates microglial polarization through the Lnc826-mediated hippo/YAP pathway in the cortex (95).
Above all, M1-like microglia is suppressed, M2-like microglia is prompted, and the crosstalk between microglia and neurons is regulated by acupuncture treatment stimulation. In addition, acupuncture treatment inhibits the proinflammatory pathway and activates the anti-inflammatory pathway to modulate the phenotype and morphology of microglia and microglial markers and receptors. Subsequently, the proinflammatory cytokines secreted by microglia decreased and the anti-inflammatory cytokines secreted by microglia increased. The regulation of microglia in the CNS by acupuncture treatment for the treatment of IS through multiple targets is shown in Figure 1 .
Figure 1.
The regulation of microglia in the central nervous system by acupuncture treatment for the treatment of ischemic stroke through multiple targets.
3.1.1.2. Astrocytes
EA improves stroke by regulating the proliferation of astrocytes and the cytokines secreted by astrocytes. EA at ST36 and LI11 maintains the structural integrity of astrocytes in brain tissue (96). Owing to the special double-edged sword function of astrocytes, two opposing results were observed. EA at GV20 and GV14 recovered post-ischemic behavioral dysfunction by activating astrocytes and preventing excess reactive gliosis (97). EA at ST36 and LI11 exerted neuroprotective effects by enhancing the proliferation of astrocytes and increasing the secretion of BDNF from reactive astrocytes in the peri-infarct cortex and striatum (98). Therefore, more research should be conducted to explore the conditions required for astrocyte activation or inhibition. EA at DU20 and DU24 reduced the neuroinflammatory response by activating α7nAChR and decreasing the number of astrocytes (99). EA pretreatment at GV20 upregulated ambient endocannabinoid (eCB) expression and activated ischemic penumbral astroglial cannabinoid type 1 receptors (CB1R) in the ischemic penumbra, protecting neurons from ischemia (100). EA at PC6 and LI11 activated lactate metabolism in resident astrocytes for the use of injured neurons around the ischemic area by enhancing lactate transporter (monocarboxylate transporter 1, MCT1) expression (101). EA at GV20 and GV14 regulated the activation of astrocytes, increased the expression of excitatory amino acid transporter-2 (EAAT2) and connexin 43 (CX43), decreased Ca2+ in astrocytes, and promoted beneficial interactions between astrocytes and synapses in brain tissues (102). EA at GB4, GB5, GB6, and GB7 enhanced the induction of vascular endothelial growth factor in astrocytes of the peri-infarct area after reperfusion (103). EA pretreatment at GV20 attenuated the expression and cellular translocation of the N-Myc downstream-regulated gene 2 (NDRG2) in astrocytes in the ischemic penumbra (104).
In summary, the proliferation and structural integrity of astrocytes were enhanced, excess reactive gliosis is prevented, and the release of beneficial neurotransmitters secreted by astrocytes increased through acupuncture treatment stimulation. Receptors and pathways in astrocytes play an important anti-inflammatory role in these effects.
3.1.1.3. Neutrophils, monocytes/macrophages, and oligodendrocytes
The following studies focused on the regulation of neutrophils, monocytes, macrophages, and OLs. EA and MA at GV20 and ST36 exerted neuroprotective actions in MCAO rats by decreasing the number of immune cells, including neutrophils and monocytes/macrophages (105). EA pretreatment at GV20 reduced inflammatory cytokine production and leukocyte infiltration by inducing the expression of monocyte chemotactic protein-induced protein 1 (MCPIP1) in monocytes in brain tissues (106).
EA at EX-HN1 increased the percentage of CC1-positive cells, indicating that EA promotes the survival and differentiation of OLs (107). EA at GV20 and GV14 ameliorated memory impairment by strengthening OL differentiation from OL precursor cells and by upregulating the Neurotrophin 4/5-tyrosine kinase receptor B (NT4/5-TrkB) pathway in OLs (108).
Few studies focused on the effects of neutrophils, monocytes, macrophages, and OLs after an IS stimulated by acupuncture treatment. These immune cells were believed to be promising targets for the treatment of IS. Hence, these immune cells deserve further study in the future.
3.1.2. Acupuncture treatment effects on immune cytokines
Studies have shown that cytokines are the core mediators of neuroimmune regulatory mechanisms (109, 110). Acupuncture bidirectionally modulates the release of immune cytokines, forming a complex network with multiple effects on IS. Acupuncture regulates immune cytokines from immune cells to control multiple immune responses after an IS. The scalp acupuncture at GV20 was determined to counteract ischemic brain injury through downregulation of TNF-α and IL-1b in the hippocampi (111). EA at GV20 and ST36 exerted neuroprotective properties in CIRI rats by reducing TNF-α and 70-kDa heat shock proteins (HSP70) (112). EA at GV20 and GV26 improved neurological function by increasing the serum level of TGF-β1 (113). LA at GV20 alleviated cognitive and motor deficits by reducing the expression of IL-6 and improving glutathione peroxidase (GSH-Px) and superoxide dismutase (SOD) activity in the hippocampus (114).
The NF-κB signaling pathway is a well-known nuclear transcription factor and the most studied proinflammatory biomarker and target of IS. MA at ST36 protected cognitive function in cerebral multi-infarction rats by suppressing NF-κB p65 nuclear translocation in hippocampal tissues (115). EA at ST36 and LI11 prevented neuroinflammation by regulating the miR-9-mediated NF-κB signaling pathway in the ischemic cortex (116). EA at LI11 and ST36 on the paralyzed limb showed neuroprotective activity by exhibiting the TLR4/NF-κB pathway (117).
Hence, proinflammatory cytokines were reduced, anti-inflammatory cytokines were upregulated, and the proinflammatory signaling pathway was suppressed by acupuncture treatment stimulation.
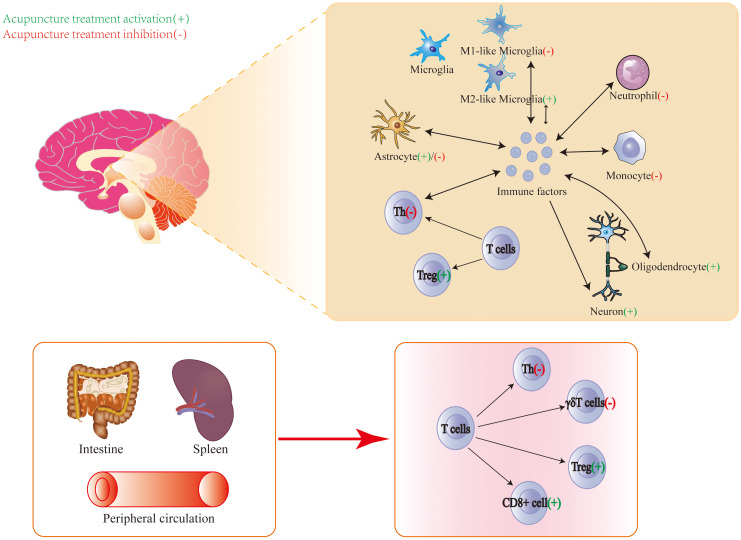
3.2. The immunomodulatory effect of acupuncture treatment on peripheral immunity
Acupuncture treatment regulates peripheral immunity, especially immune cells in the peripheral blood and immune cells in the spleen. EA at GV20 and ST36 improved motor function and brain damage in MCAO rats by decreasing IFNγ+ Th cells and IL-17+ Th cells in spleen tissues and peripheral blood (118). EA at GV20 alleviated cerebral injury by reducing the level of TNF-α and IL-1β in the brain, serum, and small intestine; reducing IL-17A, CXCL1, and CXCL2 expression, and the percentage of CD4+ cells, TCRγδ+ cells, and γδT cells in the small intestine; increasing the level of IL-10 in the serum and small intestine; and increasing Tregs percentage and the ratio of Treg to γδT cells in the small intestine (119, 120). Those studies indicated that EA regulated the differentiation of T-cell subsets in the small intestine and promoted the balance of Treg/γδ T cells toward Tregs. MA increased the total lymphocyte count in IS patient’s peripheral blood (121). MA increased IS patient’s CD8+ cell percentage and the level of CRP, TNF-α, and IL-6 in peripheral blood, and decreased CD3+ cell percentage, CD4+ cell percentage, the ratio of CD4+ cell percentage, and CD8+ cell percentage in peripheral blood (122). Therefore, major studies focus on suppressing harmful T cells in spleen tissues and peripheral blood, decreasing the expression of proinflammatory cytokines in serum and the small intestine, increasing the expression of anti-inflammatory cytokines in serum and the small intestine, and increasing the beneficial T cells in peripheral blood.
Above all, the central and peripheral immune modulation by acupuncture treatment for the treatment of IS is shown in Figure 2 .
Figure 2.
Central and peripheral immune modulation by acupuncture treatment for the treatment of ischemic stroke.
4. Factors influencing acupuncture treatment effect
The operation time of acupuncture is an important factor that influences the efficacy of acupuncture treatment. Gao et al. found that for stroke patients, acupuncture was more effective in the morning than in the afternoon (123). The effect of EA at GV20 and GV14 in the subacute phase was better than that of EA in the acute phase (124). Needle retention time had a significant effect on the efficacy of acupuncture treatment. He et al. considered the time–effect relationship between needle retention time and acupuncture efficacy for patients with IS (125). The efficacy of the 60-min needle retention time was better than that of the 40-min and 20-min needle retention times (125). A similar conclusion was reached in MCAO rats. When comparing neural function recovery, neurobehavioral scores were greater in the 48-h group than in the 12-h group and in the 24-h group (126). The output frequency of the EA instrument affects its efficacy. The efficacy of EA at 15 and 30 Hz was better than the efficacy of EA at 100 Hz in MCAO rats (96). The perceived stimulation intensity of MA had a differential effect on cerebral activation and cardiovascular reflex response (127). Additionally, EA and MA have different efficacy for IS. The efficacy of EA is better than the efficacy of MA for recovering nerve defects, improving quality of life (128), and strengthening limb motor function (129).
Acupoints are associated with the specificity of the acupuncture effect, and acupoint application is one of the factors that influence efficacy. MA at Neiguan (PC6) for 60 s was more effective than that at 5 s and 180 s in MCAO rats (130). The EA at Hanyan (GB4), Xuanlu (GB5), Xuanli (GB6), and Qubin (GB7) showed more significant recovery than at Baihui (GV20) and Shuigou (GV26) (103). Another study showed that acupuncture at Neiguan (PC6) was more effective than acupuncture at Chize (LU5) and Shuigou (GV26) (131). Zhang et al. used cluster analysis to illustrate that the Neiguan (PC6), Weizhong (BL40), Chize (LU5), Sanyinjiao (SP6), and Shuigou (GV26) groups had the most valid and suitable acupuncture parameters (132). Acupoint selection in the current study was unsystematic, because little attention was paid for the accurate stimulation of neurons. More research is needed to explore the most effective acupoints to accurately stimulate the corresponding neural signaling pathways.
Overall, different types of acupuncture treatment, duration, operation time, retention, output frequency, and acupoint selection will affect the effect of acupuncture treatment.
5. Prospect and future direction
Immune responses are complicated cascade reactions after an IS. However, current studies about immune organs, cells, and cytokine responses remain shallow. The immune mechanisms of IS are appealing and deserve to be explored. For example, myeloid cells that take on a foamy appearance are a key driver of the inflammatory response after an IS. Targeting lipid accumulation in foam cells may be a promising strategy for accelerating recovery from IS (133).
A phase III trial indicated that the tumor necrosis factor receptor-immunoglobulin G1, which controls a single inflammatory cytokine, was ineffective in the incidence or resolution of organ dysfunction (134). Programmed cell death protein 1 (PD-1) inhibitors, which are immune checkpoint inhibitors, can regulate cellular immunity in patients with cancer. However, PD-1 inhibitors cause endocrine autoimmune diseases, gastrointestinal discomfort, hepatotoxicity, rashes, and thyroid dysfunction at the same time (135). The inflammatory cascade reaction after ischemia is produced by multiple cytokines and not by a single cytokine; therefore, successful treatment of IS requires inhibition of multiple cytokines. Acupuncture improves disease by modulating the release of multiple biomolecules into the microenvironment, where they can activate the neuroendocrine–immune network to achieve holistic modulation (136). Therefore, acupuncture is a promising potential treatment for IS through the regulation of the immune network. The underlying mechanisms of acupuncture in IS require further exploration.
The vagus nerve and hypothalamic–pituitary–adrenal (HPA) axis are important components of neuroimmune interactions because they control immune function and inflammatory responses. The hypothesis of acupuncture neuroimmune regulation in the IS model by eliciting the vagal–adrenal and spinal–sympathetic axes has been raised. Ma et al. confirmed the neuroanatomy of EA at ST36 with low intensity driving the vagal–adrenal axis to produce anti-inflammatory effects (137), while EA at ST25 with high intensity activates NPY splenic noradrenergic neurons via the spinal–sympathetic axis (138). In particular, the current intensity is critical. EA at ST36 improved inflammatory arthritis in Lyme disease-susceptible C3H mice by stimulating the sciatic–vagal nerve (139). Since current studies on the neuroimmune regulation mechanism in acupuncture treatment for IS have not focused on the vagus nerve, HPA axis, or splenic sympathetic nerve, they will be a promising target.
Natural killer (NK) cells are cytotoxic lymphocytes of the innate immune system. Acupuncture also regulates NK cells by modulating the expression of the NK cell receptor CD94, protein tyrosine kinase, adhesion molecule vascular cell adhesion molecule-1 (VCAM-1), and protein tyrosine phosphatase (140). There has been no research on the mechanism of acupuncture that focuses on the modulation of NK cells. Therefore, NK cells are a promising target for exploration.
Immunoregulators can be used to treat IS, offering a new therapeutic approach to IS treatment. Acupuncture aims to restore and maintain the dynamic equilibrium of the immune system instead of strengthening or inhibiting the immune system. These evidences show that acupuncture is a potential adjunct to immune regulation in IS, which has not been previously proposed in published reviews.
6. Conclusion
Acupuncture treatment is an ancient non-drug treatment, and it shows fewer side effects and beneficial therapeutic effects. This review summarizes the progress in understanding the immunomodulatory mechanisms of acupuncture treatment for IS and provides a theoretical framework for further mechanism research. In summary, the above evidences suggest that acupuncture has the potential to modulate the immune response induced by IS, which is related to its neuroprotective effects. The exploration of the mechanisms of acupuncture promotes its global impact.
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Shenzhen Science and Technology Program (Grant Numbers JCYJ20220818100803007 and JCYJ20210324120804012).
Author contributions
HK: Conceptualization, Investigation, Writing – original draft. XZ: Funding acquisition, Methodology, Supervision, Writing – review & editing. HC: Supervision, Writing – review & editing. HT: Data curation, Writing – original draft. HZ: Funding acquisition, Investigation, Methodology, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Feske SK. Ischemic stroke. Am J Med. (2021) 134:1457–64. doi: 10.1016/j.amjmed.2021.07.027 [DOI] [PubMed] [Google Scholar]
- 2. GBD 2019 Stroke Collaborators . Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/s1474-4422(21)00252-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cerniauskaite M, Quintas R, Koutsogeorgou E, Meucci P, Sattin D, Leonardi M, et al. Quality-of-life and disability in patients with stroke. Am J Phys Med rehabilitation. (2012) 91:S39–47. doi: 10.1097/PHM.0b013e31823d4df7 [DOI] [PubMed] [Google Scholar]
- 4. De Doncker W, Dantzer R, Ormstad H, Kuppuswamy A. Mechanisms of poststroke fatigue. J neurology neurosurgery Psychiatry. (2018) 89:287–93. doi: 10.1136/jnnp-2017-316007 [DOI] [PubMed] [Google Scholar]
- 5. Yang S, Chang MC. Poststroke pain. Semin neurology. (2021) 41:67–74. doi: 10.1055/s-0040-1722641 [DOI] [PubMed] [Google Scholar]
- 6. Altman K, Shavit-Stein E, Maggio N. Post stroke seizures and epilepsy: from proteases to maladaptive plasticity. Front Cell Neurosci. (2019) 13:397. doi: 10.3389/fncel.2019.00397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Medeiros GC, Roy D, Kontos N, Beach SR. Post-stroke depression: A 2020 updated review. Gen Hosp Psychiatry. (2020) 66:70–80. doi: 10.1016/j.genhosppsych.2020.06.011 [DOI] [PubMed] [Google Scholar]
- 8. Chauhan C, Kaundal RK. The role of cGAS-STING signaling in ischemic stroke: From immune response to therapeutic targeting. Drug Discovery Today. (2023) 28:103792. doi: 10.1016/j.drudis.2023.103792 [DOI] [PubMed] [Google Scholar]
- 9. Endres M, Moro MA, Nolte CH, Dames C, Buckwalter MS, Meisel A. Immune pathways in etiology, acute phase, and chronic sequelae of ischemic stroke. Circ Res. (2022) 130:1167–86. doi: 10.1161/circresaha.121.319994 [DOI] [PubMed] [Google Scholar]
- 10. Iadecola C, Buckwalter MS, Anrather J. Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J Clin Invest. (2020) 130:2777–88. doi: 10.1172/jci135530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shi SX, Vodovoz SJ, Xiu Y, Liu N, Jiang Y, Katakam PVG, et al. T-lymphocyte interactions with the neurovascular unit: implications in intracerebral hemorrhage. Cells. (2022) 11. doi: 10.3390/cells11132011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chang H, Kwon YD, Yoon SS. Use of acupuncture therapy as a supplement to conventional medical treatments for acute ischaemic stroke patients in an academic medical centre in Korea. Complementary therapies Med. (2011) 19:256–63. doi: 10.1016/j.ctim.2011.07.003 [DOI] [PubMed] [Google Scholar]
- 13. Gong CZ, Liu W. Acupuncture and the opioid epidemic in america. Chin J Integr Med. (2018) 24:323–7. doi: 10.1007/s11655-018-2989-z [DOI] [PubMed] [Google Scholar]
- 14. Zhang S, Wu B, Liu M, Li N, Zeng X, Liu H, et al. Acupuncture efficacy on ischemic stroke recovery: multicenter randomized controlled trial in China. Stroke. (2015) 46:1301–6. doi: 10.1161/strokeaha.114.007659 [DOI] [PubMed] [Google Scholar]
- 15. Jiang C, Yang S, Tao J, Huang J, Li Y, Ye H, et al. Clinical efficacy of acupuncture treatment in combination with rehaCom cognitive training for improving cognitive function in stroke: A 2 × 2 factorial design randomized controlled trial. J Am Med Directors Assoc. (2016) 17:1114–22. doi: 10.1016/j.jamda.2016.07.021 [DOI] [PubMed] [Google Scholar]
- 16. Gong Y, Li N, Lv Z, Zhang K, Zhang Y, Yang T, et al. The neuro-immune microenvironment of acupoints-initiation of acupuncture effectiveness. J leukocyte Biol. (2020) 108:189–98. doi: 10.1002/jlb.3ab0420-361rr [DOI] [PubMed] [Google Scholar]
- 17. Li N, Guo Y, Gong Y, Zhang Y, Fan W, Yao K, et al. The anti-inflammatory actions and mechanisms of acupuncture from acupoint to target organs via neuro-immune regulation. J Inflammation Res. (2021) 14:7191–224. doi: 10.2147/jir.S341581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Arcuri C, Mecca C, Bianchi R, Giambanco I, Donato R. The pathophysiological role of microglia in dynamic surveillance, phagocytosis and structural remodeling of the developing CNS. Front Mol Neurosci. (2017) 10:191. doi: 10.3389/fnmol.2017.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dudvarski Stankovic N, Teodorczyk M, Ploen R, Zipp F, Schmidt MHH. Microglia-blood vessel interactions: a double-edged sword in brain pathologies. Acta neuropathologica. (2016) 131:347–63. doi: 10.1007/s00401-015-1524-y [DOI] [PubMed] [Google Scholar]
- 20. Xiong XY, Liu L, Yang QW. Functions and mechanisms of microglia/macrophages in neuroinflammation and neurogenesis after stroke. Prog neurobiology. (2016) 142:23–44. doi: 10.1016/j.pneurobio.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 21. Xu S, Lu J, Shao A, Zhang JH, Zhang J. Glial cells: role of the immune response in ischemic stroke. Front Immunol. (2020) 11:294. doi: 10.3389/fimmu.2020.00294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang J, Xing H, Wan L, Jiang X, Wang C, Wu Y. Treatment targets for M2 microglia polarization in ischemic stroke. Biomedicine pharmacotherapy = Biomedecine pharmacotherapie. (2018) 105:518–25. doi: 10.1016/j.biopha.2018.05.143 [DOI] [PubMed] [Google Scholar]
- 23. Var SR, Shetty AV, Grande AW, Low WC, Cheeran MC. Microglia and macrophages in neuroprotection, neurogenesis, and emerging therapies for stroke. Cells. (2021) 10. doi: 10.3390/cells10123555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Candelario-Jalil E, Dijkhuizen RM, Magnus T. Neuroinflammation, stroke, blood-brain barrier dysfunction, and imaging modalities. Stroke. (2022) 53:1473–86. doi: 10.1161/strokeaha.122.036946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jurga AM, Paleczna M, Kuter KZ. Overview of general and discriminating markers of differential microglia phenotypes. Front Cell Neurosci. (2020) 14:198. doi: 10.3389/fncel.2020.00198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen AQ, Fang Z, Chen XL, Yang S, Zhou YF, Mao L, et al. Microglia-derived TNF-α mediates endothelial necroptosis aggravating blood brain-barrier disruption after ischemic stroke. Cell Death disease. (2019) 10:487. doi: 10.1038/s41419-019-1716-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cherry JD, Olschowka JA, O'Banion MK. Neuroinflammation and M2 microglia: the good, the bad, and the inflamed. J neuroinflammation. (2014) 11:98. doi: 10.1186/1742-2094-11-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kolosowska N, Keuters MH, Wojciechowski S, Keksa-Goldsteine V, Laine M, Malm T, et al. Peripheral administration of IL-13 induces anti-inflammatory microglial/macrophage responses and provides neuroprotection in ischemic stroke. Neurother J Am Soc Exp NeuroTherapeutics. (2019) 16:1304–19. doi: 10.1007/s13311-019-00761-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang W, Xu H, Li C, Han B, Zhang Y. Exploring Chinese herbal medicine for ischemic stroke: insights into microglia and signaling pathways. Front Pharmacol. (2024) 15:1333006. doi: 10.3389/fphar.2024.1333006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhang W, Tian T, Gong SX, Huang WQ, Zhou QY, Wang AP, et al. Microglia-associated neuroinflammation is a potential therapeutic target for ischemic stroke. Neural regeneration Res. (2021) 16:6–11. doi: 10.4103/1673-5374.286954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta neuropathologica. (2010) 119:7–35. doi: 10.1007/s00401-009-0619-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fan YY, Huo J. A1/A2 astrocytes in central nervous system injuries and diseases: Angels or devils? Neurochemistry Int. (2021) 148:105080. doi: 10.1016/j.neuint.2021.105080 [DOI] [PubMed] [Google Scholar]
- 33. Williamson MR, Fuertes CJA, Dunn AK, Drew MR, Jones TA. Reactive astrocytes facilitate vascular repair and remodeling after stroke. Cell Rep. (2021) 35:109048. doi: 10.1016/j.celrep.2021.109048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shen XY, Gao ZK, Han Y, Yuan M, Guo YS, Bi X. Activation and role of astrocytes in ischemic stroke. Front Cell Neurosci. (2021) 15:755955. doi: 10.3389/fncel.2021.755955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Allen NJ, Eroglu C. Cell biology of astrocyte-synapse interactions. Neuron. (2017) 96:697–708. doi: 10.1016/j.neuron.2017.09.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sims NR, Yew WP. Reactive astrogliosis in stroke: Contributions of astrocytes to recovery of neurological function. Neurochemistry Int. (2017) 107:88–103. doi: 10.1016/j.neuint.2016.12.016 [DOI] [PubMed] [Google Scholar]
- 37. Hernández IH, Villa-González M, Martín G, Soto M, Pérez-Álvarez MJ. Glial cells as therapeutic approaches in brain ischemia-reperfusion injury. Cells. (2021) 10. doi: 10.3390/cells10071639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dewar D, Underhill SM, Goldberg MP. Oligodendrocytes and ischemic brain injury. J Cereb Blood Flow Metab. (2003) 23:263–74. doi: 10.1097/01.Wcb.0000053472.41007.F9 [DOI] [PubMed] [Google Scholar]
- 39. Huang S, Ren C, Luo Y, Ding Y, Ji X, Li S. New insights into the roles of oligodendrocytes regulation in ischemic stroke recovery. Neurobiol disease. (2023) 184:106200. doi: 10.1016/j.nbd.2023.106200 [DOI] [PubMed] [Google Scholar]
- 40. Wanrooy BJ, Wen SW, Wong CH. Dynamic roles of neutrophils in post-stroke neuroinflammation. Immunol Cell Biol. (2021) 99:924–35. doi: 10.1111/imcb.12463 [DOI] [PubMed] [Google Scholar]
- 41. Ansari J, Gavins FNE. Neutrophils and platelets: immune soldiers fighting together in stroke pathophysiology. Biomedicines. (2021) 9. doi: 10.3390/biomedicines9121945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kapoor S, Opneja A, Nayak L. The role of neutrophils in thrombosis. Thromb Res. (2018) 170:87–96. doi: 10.1016/j.thromres.2018.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Döring Y, Drechsler M, Soehnlein O, Weber C. Neutrophils in atherosclerosis: from mice to man. Arteriosclerosis thrombosis Vasc Biol. (2015) 35:288–95. doi: 10.1161/atvbaha.114.303564 [DOI] [PubMed] [Google Scholar]
- 44. Beuker C, Strecker JK, Rawal R, Schmidt-Pogoda A, Ruck T, Wiendl H, et al. Immune cell infiltration into the brain after ischemic stroke in humans compared to mice and rats: a systematic review and meta-analysis. Trans stroke Res. (2021) 12:976–90. doi: 10.1007/s12975-021-00887-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. El Amki M, Glück C, Binder N, Middleham W, Wyss MT, Weiss T, et al. Neutrophils obstructing brain capillaries are a major cause of no-reflow in ischemic stroke. Cell Rep. (2020) 33:108260. doi: 10.1016/j.celrep.2020.108260 [DOI] [PubMed] [Google Scholar]
- 46. Dimasi D, Sun WY, Bonder CS. Neutrophil interactions with the vascular endothelium. Int immunopharmacology. (2013) 17:1167–75. doi: 10.1016/j.intimp.2013.05.034 [DOI] [PubMed] [Google Scholar]
- 47. Metzemaekers M, Gouwy M, Proost P. Neutrophil chemoattractant receptors in health and disease: double-edged swords. Cell Mol Immunol. (2020) 17:433–50. doi: 10.1038/s41423-020-0412-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jickling GC, Liu D, Ander BP, Stamova B, Zhan X, Sharp FR. Targeting neutrophils in ischemic stroke: translational insights from experimental studies. J Cereb Blood Flow Metab. (2015) 35:888–901. doi: 10.1038/jcbfm.2015.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Stoll G, Nieswandt B. Thrombo-inflammation in acute ischaemic stroke - implications for treatment. Nat Rev Neurology. (2019) 15:473–81. doi: 10.1038/s41582-019-0221-1 [DOI] [PubMed] [Google Scholar]
- 50. Rayasam A, Kijak JA, Kissel L, Choi YH, Kim T, Hsu M, et al. CXCL13 expressed on inflamed cerebral blood vessels recruit IL-21 producing T(FH) cells to damage neurons following stroke. J neuroinflammation. (2022) 19:125. doi: 10.1186/s12974-022-02490-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lei TY, Ye YZ, Zhu XQ, Smerin D, Gu LJ, Xiong XX, et al. The immune response of T cells and therapeutic targets related to regulating the levels of T helper cells after ischaemic stroke. J neuroinflammation. (2021) 18:25. doi: 10.1186/s12974-020-02057-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Liu Y, Dong J, Zhang Z, Liu Y, Wang Y. Regulatory T cells: A suppressor arm in post-stroke immune homeostasis. Neurobiol disease. (2023) 189:106350. doi: 10.1016/j.nbd.2023.106350 [DOI] [PubMed] [Google Scholar]
- 53. Cai W, Shi L, Zhao J, Xu F, Dufort C, Ye Q, et al. Neuroprotection against ischemic stroke requires a specific class of early responder T cells in mice. J Clin Invest. (2022) 132. doi: 10.1172/jci157678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wang H, Wang Z, Wu Q, Yuan Y, Cao W, Zhang X. Regulatory T cells in ischemic stroke. CNS Neurosci Ther. (2021) 27:643–51. doi: 10.1111/cns.13611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Dong X, Zhang X, Li C, Chen J, Xia S, Bao X, et al. γδ T cells aggravate blood-brain-barrier injury via IL-17A in experimental ischemic stroke. Neurosci letters. (2022) 776:136563. doi: 10.1016/j.neulet.2022.136563 [DOI] [PubMed] [Google Scholar]
- 56. Doll DN, Barr TL, Simpkins JW. Cytokines: their role in stroke and potential use as biomarkers and therapeutic targets. Aging disease. (2014) 5:294–306. doi: 10.14336/ad.2014.0500294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Martha SR, Cheng Q, Fraser JF, Gong L, Collier LA, Davis SM, et al. Expression of cytokines and chemokines as predictors of stroke outcomes in acute ischemic stroke. Front neurology. (2019) 10:1391. doi: 10.3389/fneur.2019.01391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zhu H, Hu S, Li Y, Sun Y, Xiong X, Hu X, et al. Interleukins and ischemic stroke. Front Immunol. (2022) 13:828447. doi: 10.3389/fimmu.2022.828447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mo ZT, Zheng J, Liao YL. Icariin inhibits the expression of IL-1β, IL-6 and TNF-α induced by OGD/R through the IRE1/XBP1s pathway in microglia. Pharm Biol. (2021) 59:1473–9. doi: 10.1080/13880209.2021.1991959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kann O, Almouhanna F, Chausse B. Interferon γ: a master cytokine in microglia-mediated neural network dysfunction and neurodegeneration. Trends neurosciences. (2022) 45:913–27. doi: 10.1016/j.tins.2022.10.007 [DOI] [PubMed] [Google Scholar]
- 61. Backes FN, de Souza A, Bianchin MM. IL-23 and IL-17 in acute ischemic stroke: Correlation with stroke scales and prognostic value. Clin Biochem. (2021) 98:29–34. doi: 10.1016/j.clinbiochem.2021.09.003 [DOI] [PubMed] [Google Scholar]
- 62. Garcia JM, Stillings SA, Leclerc JL, Phillips H, Edwards NJ, Robicsek SA, et al. Role of interleukin-10 in acute brain injuries. Front neurology. (2017) 8:244. doi: 10.3389/fneur.2017.00244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Zhu H, Gui Q, Hui X, Wang X, Jiang J, Ding L, et al. TGF-β1/smad3 signaling pathway suppresses cell apoptosis in cerebral ischemic stroke rats. Med Sci monitor Int Med J Exp Clin Res. (2017) 23:366–76. doi: 10.12659/msm.899195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Huang Y, Li K, Dai Q, Pang H, Xu Z, Luo X, et al. SCH 644343 alleviates ischemic stroke-induced neuroinflammation by promoting microglial polarization via the IL-4/SREBP-1 signaling pathway. Eur J Pharmacol. (2023) 958:176033. doi: 10.1016/j.ejphar.2023.176033 [DOI] [PubMed] [Google Scholar]
- 65. Lee HK, Keum S, Sheng H, Warner DS, Lo DC, Marchuk DA. Natural allelic variation of the IL-21 receptor modulates ischemic stroke infarct volume. J Clin Invest. (2016) 126:2827–38. doi: 10.1172/jci84491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yang S, Zeng J, Hao W, Sun R, Tuo Y, Tan L, et al. IL-21/IL-21R Promotes the Pro-Inflammatory Effects of Macrophages during C. muridarum Respiratory Infection. Int J Mol Sci. (2023) 24. doi: 10.3390/ijms241612557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Godinho-Silva C, Cardoso F, Veiga-Fernandes H. Neuro-immune cell units: A new paradigm in physiology. Annu Rev Immunol. (2019) 37:19–46. doi: 10.1146/annurev-immunol-042718-041812 [DOI] [PubMed] [Google Scholar]
- 68. Courties G, Herisson F, Sager HB, Heidt T, Ye Y, Wei Y, et al. Ischemic stroke activates hematopoietic bone marrow stem cells. Circ Res. (2015) 116:407–17. doi: 10.1161/circresaha.116.305207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Xie X, Wang L, Dong S, Ge S, Zhu T. Immune regulation of the gut-brain axis and lung-brain axis involved in ischemic stroke. Neural regeneration Res. (2024) 19:519–28. doi: 10.4103/1673-5374.380869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Inderhees J, Schwaninger M. Liver metabolism in ischemic stroke. Neuroscience. (2024). doi: 10.1016/j.neuroscience.2023.12.013 [DOI] [PubMed] [Google Scholar]
- 71. Samary CS, Ramos AB, Maia LA, Rocha NN, Santos CL, Magalhães RF, et al. Focal ischemic stroke leads to lung injury and reduces alveolar macrophage phagocytic capability in rats. Crit Care (London England). (2018) 22:249. doi: 10.1186/s13054-018-2164-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ajmo CT, Jr., Collier LA, Leonardo CC, Hall AA, Green SM, Womble TA, et al. Blockade of adrenoreceptors inhibits the splenic response to stroke. Exp neurology. (2009) 218:47–55. doi: 10.1016/j.expneurol.2009.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Jin R, Zhu X, Liu L, Nanda A, Granger DN, Li G. Simvastatin attenuates stroke-induced splenic atrophy and lung susceptibility to spontaneous bacterial infection in mice. Stroke. (2013) 44:1135–43. doi: 10.1161/strokeaha.111.000633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Yu H, Cai Y, Zhong A, Zhang Y, Zhang J, Xu S. The "Dialogue" Between central and peripheral immunity after ischemic stroke: focus on spleen. Front Immunol. (2021) 12:792522. doi: 10.3389/fimmu.2021.792522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Sahota P, Vahidy F, Nguyen C, Bui TT, Yang B, Parsha K, et al. Changes in spleen size in patients with acute ischemic stroke: a pilot observational study. Int J stroke. (2013) 8:60–7. doi: 10.1111/ijs.12022 [DOI] [PubMed] [Google Scholar]
- 76. Zhang BJ, Men XJ, Lu ZQ, Li HY, Qiu W, Hu XQ. Splenectomy protects experimental rats from cerebral damage after stroke due to anti-inflammatory effects. Chin Med J (Engl). (2013) 126:2354–60. [PubMed] [Google Scholar]
- 77. Tan C, Wang Z, Zheng M, Zhao S, Shichinohe H, Houkin K. Responses of immune organs after cerebral ischemic stroke. J Nippon Med School = Nippon Ika Daigaku zasshi. (2021) 88:228–37. doi: 10.1272/jnms.JNMS.2021_88-308 [DOI] [PubMed] [Google Scholar]
- 78. Glab JA, Puthalakath H, Zhang SR, Vinh A, Drummond GR, Sobey CG, et al. Bim deletion reduces functional deficits following ischemic stroke in association with modulation of apoptosis and inflammation. Neuromolecular Med. (2022) 24:405–14. doi: 10.1007/s12017-022-08703-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kingsbury C, Shear A, Heyck M, Sadanandan N, Zhang H, Gonzales-Portillo B, et al. Inflammation-relevant microbiome signature of the stroke brain, gut, spleen, and thymus and the impact of exercise. J Cereb Blood Flow Metab. (2021) 41:3200–12. doi: 10.1177/0271678x211039598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Ding SS, Hong SH, Wang C, Guo Y, Wang ZK, Xu Y. Acupuncture modulates the neuro-endocrine-immune network. QJM monthly J Assoc Physicians. (2014) 107:341–5. doi: 10.1093/qjmed/hct196 [DOI] [PubMed] [Google Scholar]
- 81. Zou J, Huang GF, Xia Q, Li X, Shi J, Sun N. Electroacupuncture promotes microglial M2 polarization in ischemic stroke via annexin A1. Acupunct Med. (2022) 40:258–67. doi: 10.1177/09645284211057570 [DOI] [PubMed] [Google Scholar]
- 82. Lawrence T. The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harbor Perspect Biol. (2009) 1:a001651. doi: 10.1101/cshperspect.a001651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Liu R, Xu NG, Yi W, Ji C. Electroacupuncture attenuates inflammation after ischemic stroke by inhibiting NF-κB-mediated activation of microglia. Evidence-Based complementary Altern Med eCAM. (2020) 2020:8163052. doi: 10.1155/2020/8163052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Liu W, Wang X, Yang S, Huang J, Xue X, Zheng Y, et al. Electroacupunctre improves motor impairment via inhibition of microglia-mediated neuroinflammation in the sensorimotor cortex after ischemic stroke. Life Sci. (2016) 151:313–22. doi: 10.1016/j.lfs.2016.01.045 [DOI] [PubMed] [Google Scholar]
- 85. Han B, Lu Y, Zhao H, Wang Y, Li L, Wang T. Electroacupuncture modulated the inflammatory reaction in MCAO rats via inhibiting the TLR4/NF-κB signaling pathway in microglia. Int J Clin Exp Pathol. (2015) 8:11199–205. [PMC free article] [PubMed] [Google Scholar]
- 86. Zhou X, Lu W, Wang Y, Li J, Luo Y. A20-binding inhibitor of NF-κB 1 ameliorates neuroinflammation and mediates antineuroinflammatory effect of electroacupuncture in cerebral ischemia/reperfusion rats. Evidence-Based complementary Altern Med eCAM. (2020) 2020:6980398. doi: 10.1155/2020/6980398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Xu H, Mu S, Qin W. Microglia TREM2 is required for electroacupuncture to attenuate neuroinflammation in focal cerebral ischemia/reperfusion rats. Biochem Biophys Res Commun. (2018) 503:3225–34. doi: 10.1016/j.bbrc.2018.08.130 [DOI] [PubMed] [Google Scholar]
- 88. Okusa MD, Rosin DL, Tracey KJ. Targeting neural reflex circuits in immunity to treat kidney disease. Nat Rev Nephrology. (2017) 13:669–80. doi: 10.1038/nrneph.2017.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ma Z, Zhang Z, Bai F, Jiang T, Yan C, Wang Q. Electroacupuncture pretreatment alleviates cerebral ischemic injury through α7 nicotinic acetylcholine receptor-mediated phenotypic conversion of microglia. Front Cell Neurosci. (2019) 13:537. doi: 10.3389/fncel.2019.00537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Cao Y, Wang L, Lin LT, Wang XR, Ma SM, Yang NN, et al. Acupuncture attenuates cognitive deficits through α7nAChR mediated anti-inflammatory pathway in chronic cerebral hypoperfusion rats. Life Sci. (2021) 266:118732. doi: 10.1016/j.lfs.2020.118732 [DOI] [PubMed] [Google Scholar]
- 91. Wang Q, Wang F, Li X, Yang Q, Li X, Xu N, et al. Electroacupuncture pretreatment attenuates cerebral ischemic injury through α7 nicotinic acetylcholine receptor-mediated inhibition of high-mobility group box 1 release in rats. J neuroinflammation. (2012) 9:24. doi: 10.1186/1742-2094-9-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Haidar MA, Ibeh S, Shakkour Z, Reslan MA, Nwaiwu J, Moqidem YA, et al. Crosstalk between microglia and neurons in neurotrauma: an overview of the underlying mechanisms. Curr neuropharmacology. (2022) 20:2050–65. doi: 10.2174/1570159x19666211202123322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Lin X, Zhan J, Jiang J, Ren Y. Upregulation of neuronal cylindromatosis expression is essential for electroacupuncture-mediated alleviation of neuroinflammatory injury by regulating microglial polarization in rats subjected to focal cerebral ischemia/reperfusion. J Inflammation Res. (2021) 14:2061–78. doi: 10.2147/jir.S307841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Jiang J, Luo Y, Qin W, Ma H, Li Q, Zhan J, et al. Electroacupuncture suppresses the NF-κB signaling pathway by upregulating cylindromatosis to alleviate inflammatory injury in cerebral ischemia/reperfusion rats. Front Mol Neurosci. (2017) 10:363. doi: 10.3389/fnmol.2017.00363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Chen S, Wang L, Yuan Y, Wen Y, Shu S. Electroacupuncture regulates microglia polarization via lncRNA-mediated hippo pathway after ischemic stroke. Biotechnol Genet Eng Rev. (2023) 9:1–17. doi: 10.1080/02648725.2023.2177046 [DOI] [PubMed] [Google Scholar]
- 96. Xiao Y, Wu X, Deng X, Huang L, Zhou Y, Yang X. Optimal electroacupuncture frequency for maintaining astrocyte structural integrity in cerebral ischemia. Neural regeneration Res. (2013) 8:1122–31. doi: 10.3969/j.issn.1673-5374.2013.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Han X, Huang X, Wang Y, Chen H. A study of astrocyte activation in the periinfarct region after cerebral ischemia with electroacupuncture. Brain injury. (2010) 24:773–9. doi: 10.3109/02699051003610482 [DOI] [PubMed] [Google Scholar]
- 98. Tao J, Zheng Y, Liu W, Yang S, Huang J, Xue X, et al. Electro-acupuncture at LI11 and ST36 acupoints exerts neuroprotective effects via reactive astrocyte proliferation after ischemia and reperfusion injury in rats. Brain Res bulletin. (2016) 120:14–24. doi: 10.1016/j.brainresbull.2015.10.011 [DOI] [PubMed] [Google Scholar]
- 99. Liu J, Li C, Peng H, Yu K, Tao J, Lin R, et al. Electroacupuncture attenuates learning and memory impairment via activation of α7nAChR-mediated anti-inflammatory activity in focal cerebral ischemia/reperfusion injured rats. Exp Ther Med. (2017) 14:939–46. doi: 10.3892/etm.2017.4622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Yang C, Liu J, Wang J, Yin A, Jiang Z, Ye S, et al. Activation of astroglial CB1R mediates cerebral ischemic tolerance induced by electroacupuncture. J Cereb Blood Flow Metab. (2021) 41:2295–310. doi: 10.1177/0271678x21994395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Lu Y, Zhao H, Wang Y, Han B, Wang T, Zhao H, et al. Electro-acupuncture up-regulates astrocytic MCT1 expression to improve neurological deficit in middle cerebral artery occlusion rats. Life Sci. (2015) 134:68–72. doi: 10.1016/j.lfs.2015.05.014 [DOI] [PubMed] [Google Scholar]
- 102. Luo Y, Xu NG, Yi W, Yu T, Yang ZH. Study on the correlation between synaptic reconstruction and astrocyte after ischemia and the influence of electroacupuncture on rats. Chin J Integr Med. (2011) 17:750–7. doi: 10.1007/s11655-011-0754-7 [DOI] [PubMed] [Google Scholar]
- 103. Wang SJ, Omori N, Li F, Jin G, Hamakawa Y, Sato K, et al. Functional improvement by electro-acupuncture after transient middle cerebral artery occlusion in rats. Neurological Res. (2003) 25:516–21. doi: 10.1179/016164103101201751 [DOI] [PubMed] [Google Scholar]
- 104. Wang F, Gao Z, Li X, Li Y, Li X, Zhong H, et al. NDRG2 is involved in anti-apoptosis induced by electroacupuncture pretreatment after focal cerebral ischemia in rats. Neurological Res. (2013) 35:406–14. doi: 10.1179/1743132813y.0000000159 [DOI] [PubMed] [Google Scholar]
- 105. Xu H, Zhang Y, Sun H, Chen S, Wang F. Effects of acupuncture at GV20 and ST36 on the expression of matrix metalloproteinase 2, aquaporin 4, and aquaporin 9 in rats subjected to cerebral ischemia/reperfusion injury. PloS One. (2014) 9:e97488. doi: 10.1371/journal.pone.0097488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Jin Z, Liang J, Wang J, Kolattukudy PE. Delayed brain ischemia tolerance induced by electroacupuncture pretreatment is mediated via MCP-induced protein 1. J neuroinflammation. (2013) 10:63. doi: 10.1186/1742-2094-10-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Lee HJ, Jung DH, Kim NK, Shin HK, Choi BT. Effects of electroacupuncture on the functionality of NG2-expressing cells in perilesional brain tissue of mice following ischemic stroke. Neural regeneration Res. (2022) 17:1556–65. doi: 10.4103/1673-5374.330611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Ahn SM, Kim YR, Kim HN, Shin YI, Shin HK, Choi BT. Electroacupuncture ameliorates memory impairments by enhancing oligodendrocyte regeneration in a mouse model of prolonged cerebral hypoperfusion. Sci Rep. (2016) 6:28646. doi: 10.1038/srep28646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Stone TW, Clanchy FIL, Huang YS, Chiang NY, Darlington LG, Williams RO. An integrated cytokine and kynurenine network as the basis of neuroimmune communication. Front Neurosci. (2022) 16:1002004. doi: 10.3389/fnins.2022.1002004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Loftis JM, Huckans M, Morasco BJ. Neuroimmune mechanisms of cytokine-induced depression: current theories and novel treatment strategies. Neurobiol disease. (2010) 37:519–33. doi: 10.1016/j.nbd.2009.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Li Z, Meng X, Ren M, Shao M. Combination of scalp acupuncture with exercise therapy effectively counteracts ischemic brain injury in rats. J stroke cerebrovascular Dis. (2020) 29:105286. doi: 10.1016/j.jstrokecerebrovasdis.2020.105286 [DOI] [PubMed] [Google Scholar]
- 112. Xu H, Sun H, Chen SH, Zhang YM, Piao YL, Gao Y. Effects of acupuncture at Baihui (DU20) and Zusanli (ST36) on the expression of heat shock protein 70 and tumor necrosis factor α in the peripheral serum of cerebral ischemia-reperfusion-injured rats. Chin J Integr Med. (2014) 20:369–74. doi: 10.1007/s11655-014-1800-z [DOI] [PubMed] [Google Scholar]
- 113. Wang WB, Yang LF, He QS, Li T, Ma YY, Zhang P, et al. Mechanisms of electroacupuncture effects on acute cerebral ischemia/reperfusion injury: possible association with upregulation of transforming growth factor beta 1. Neural regeneration Res. (2016) 11:1099–101. doi: 10.4103/1673-5374.187042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Jittiwat J. Baihui point laser acupuncture ameliorates cognitive impairment, motor deficit, and neuronal loss partly via antioxidant and anti-inflammatory effects in an animal model of focal ischemic stroke. Evidence-Based complementary Altern Med eCAM. (2019) 2019:1204709. doi: 10.1155/2019/1204709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Yang JW, Wang XR, Ma SM, Yang NN, Li QQ, Liu CZ. Acupuncture attenuates cognitive impairment, oxidative stress and NF-κB activation in cerebral multi-infarct rats. Acupunct Med. (2019) 37:283–91. doi: 10.1136/acupmed-2017-011491 [DOI] [PubMed] [Google Scholar]
- 116. Liu W, Wang X, Zheng Y, Shang G, Huang J, Tao J, et al. Electroacupuncture inhibits inflammatory injury by targeting the miR-9-mediated NF-κB signaling pathway following ischemic stroke. Mol Med Rep. (2016) 13:1618–26. doi: 10.3892/mmr.2015.4745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Lan L, Tao J, Chen A, Xie G, Huang J, Lin J, et al. Electroacupuncture exerts anti-inflammatory effects in cerebral ischemia-reperfusion injured rats via suppression of the TLR4/NF-κB pathway. Int J Mol Med. (2013) 31:75–80. doi: 10.3892/ijmm.2012.1184 [DOI] [PubMed] [Google Scholar]
- 118. Deng P, Wang L, Zhang Q, Chen S, Zhang Y, Xu H, et al. Therapeutic potential of a combination of electroacupuncture and human iPSC-derived small extracellular vesicles for ischemic stroke. Cells. (2022) 11. doi: 10.3390/cells11050820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Wang Y, Chen Y, Meng L, Wu B, Ouyang L, Peng R, et al. Electro-acupuncture treatment inhibits the inflammatory response by regulating γδ T and Treg cells in ischemic stroke. Exp neurology. (2023) 17:114324. doi: 10.1016/j.expneurol.2023.114324 [DOI] [PubMed] [Google Scholar]
- 120. Wang YL, Meng LL, Chen YL, OuYang L, Wu BF, Peng R, et al. Electro-acupuncture treatment ameliorates intestinal inflammatory injury in cerebral ischemia-reperfusion rats via regulating the balance of Treg / γδ T cells. Brain Res. (2023) 6:148233. doi: 10.1016/j.brainres.2023.148233 [DOI] [PubMed] [Google Scholar]
- 121. Qin L, Zhang XX, Jin X, Cui CH, Tang CZ. The effect of acupuncture on enteral nutrition and gastrointestinal dynamics in patients who have suffered a severe stroke. Curr neurovascular Res. (2022) 19:275–81. doi: 10.2174/1567202619666220822123023 [DOI] [PubMed] [Google Scholar]
- 122. Jin L, Han C. Effects of acupuncture on clinical outcome and helper T cell distribution and abundance in patients with convalescent ischemic stroke. Am J Trans Res. (2021) 13:8118–25. [PMC free article] [PubMed] [Google Scholar]
- 123. Gao Y, Lin Z, Tao J, Yang S, Chen R, Jiang C, et al. Evidence of timing effects on acupuncture: A functional magnetic resonance imaging study. Exp Ther Med. (2015) 9:59–64. doi: 10.3892/etm.2014.2056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Young-Wook P, Gi Yoon H, Min Jae K, Seo-Yeon L, Byung Tae C, Hwa Kyoung S. Subacute electroacupuncture at Baihui (GV 20) and Dazhui (GV 14) promotes post-stroke functional recovery via neurogenesis and astrogliosis in a photothrombotic stroke mouse model. J Tradit Chin Med. (2019) 39:833–41. [PubMed] [Google Scholar]
- 125. He Y, Han B, Hu J, Yuan L, Chen Z, Li J, et al. An observation on the acupuncture treatment of ischemic wind-stroke with different lengths of needle-retaining time. J Tradit Chin Med. (2006) 26:83–7. [PubMed] [Google Scholar]
- 126. Chang XB, Fan XN, Wang S, Yang S, Yang X, Zhang YN, et al. Influence of acupuncture on neural movement function in rats with middle cerebral artery occlusion–a randomized controlled trial. J Tradit Chin Med. (2012) 32:105–9. doi: 10.1016/s0254-6272(12)60041-7 [DOI] [PubMed] [Google Scholar]
- 127. Bäcker M, Hammes MG, Valet M, Deppe M, Conrad B, Tölle TR, et al. Different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity, arterial blood pressure and heart rate in human subjects. Neurosci letters. (2002) 333:203–6. doi: 10.1016/s0304-3940(02)01109-6 [DOI] [PubMed] [Google Scholar]
- 128. Tian L, Du X, Wang J, Sun R, Zhang Z, Yuan B, et al. [Comparative study on the effects between manual acupuncture and electroacupuncture for hemiplegia after acute ischemic stroke]. Zhongguo Zhen Jiu. (2016) 36:1121–5. doi: 10.13703/j.0255-2930.2016.11.001 [DOI] [PubMed] [Google Scholar]
- 129. Yang JS, Gao X, Sun R, Wang X, Wang H, Zhang JC, et al. [Effect of electroacupuncture intervention on rehabilitation of upper limb motor function in patients with ischemic stroke]. Zhen Ci Yan Jiu. (2015) 40:489–92. doi: 10.13702/j.1000-0607.2015.06.012 [DOI] [PubMed] [Google Scholar]
- 130. Zhang C, Wen Y, Fan XN, Tian G, Zhou XY, Deng SZ, et al. Therapeutic effects of different durations of acupuncture on rats with middle cerebral artery occlusion. Neural regeneration Res. (2015) 10:159–64. doi: 10.4103/1673-5374.150727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Chang XB, Fan XN, Wang S, Meng ZH, Yang X, Shi XM. Cluster analysis for acupoint specificity of acupuncture effect based on cerebral infarction rat model. Chin J Integr Med. (2013) 19:853–8. doi: 10.1007/s11655-013-1530-7 [DOI] [PubMed] [Google Scholar]
- 132. Chang XB, Wang S, Meng ZH, Fan XN, Yang X, Shi XM. Study on acupuncture parameters impacting on the acupuncture effect using cluster analysis in a rat model with middle cerebral artery occlusion. Chin J Integr Med. (2014) 20:130–5. doi: 10.1007/s11655-013-1584-6 [DOI] [PubMed] [Google Scholar]
- 133. Zbesko JC, Stokes J, Becktel DA, Doyle KP. Targeting foam cell formation to improve recovery from ischemic stroke. Neurobiol disease. (2023) 181:106130. doi: 10.1016/j.nbd.2023.106130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Abraham E, Laterre PF, Garbino J, Pingleton S, Butler T, Dugernier T, et al. Lenercept (p55 tumor necrosis factor receptor fusion protein) in severe sepsis and early septic shock: a randomized, double-blind, placebo-controlled, multicenter phase III trial with 1,342 patients. Crit Care Med. (2001) 29:503–10. doi: 10.1097/00003246-200103000-00006 [DOI] [PubMed] [Google Scholar]
- 135. Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, et al. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. (2017) 8:561. doi: 10.3389/fphar.2017.00561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Cui J, Song W, Jin Y, Xu H, Fan K, Lin D, et al. Research progress on the mechanism of the acupuncture regulating neuro-endocrine-immune network system. Veterinary Sci. (2021) 8. doi: 10.3390/vetsci8080149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Liu S, Wang Z, Su Y, Qi L, Yang W, Fu M, et al. A neuroanatomical basis for electroacupuncture to drive the vagal-adrenal axis. Nature. (2021) 598:641–5. doi: 10.1038/s41586-021-04001-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Liu S, Wang ZF, Su YS, Ray RS, Jing XH, Wang YQ, et al. Somatotopic organization and intensity dependence in driving distinct NPY-expressing sympathetic pathways by electroacupuncture. Neuron. (2020) 108:436–450.e7. doi: 10.1016/j.neuron.2020.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Akoolo L, Djokic V, Rocha SC, Ulloa L, Parveen N. Sciatic-vagal nerve stimulation by electroacupuncture alleviates inflammatory arthritis in lyme disease-susceptible C3H mice. Front Immunol. (2022) 13:930287. doi: 10.3389/fimmu.2022.930287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Johnston MF, Ortiz Sánchez E, Vujanovic NL, Li W. Acupuncture may stimulate anticancer immunity via activation of natural killer cells. Evidence-Based complementary Altern Med eCAM. (2011) 2011:481625. doi: 10.1093/ecam/nep236 [DOI] [PMC free article] [PubMed] [Google Scholar]