Abstract
Background
Patient monitoring devices are critical for alerting of potential cardiac arrhythmias during hospitalization; however, there are concerns of alarm fatigue due to high false alarm rates.
Objective
The purpose of this study was to evaluate the sensitivity and false alarm rate of hospital-based continuous electrocardiographic (ECG) monitoring technologies.
Methods
Six commonly used multiparameter bedside monitoring systems available in the United States were evaluated: B125M (GE HealthCare), ePM10 and iPM12 (Mindray), Efficia and IntelliVue (Philips), and Life Scope (Nihon Kohden). Sensitivity was tested using ECG recordings containing 57 true ventricular tachycardia (VT) events. False-positive rate testing used 205 patient-hours of ECG recordings containing no cardiac arrhythmias. Signals from ECG recordings were fed to devices simultaneously; high-severity arrhythmia alarms were tracked. Sensitivity to true VT events and false-positive rates were determined. Differences were assessed using Fisher exact tests (sensitivity) and Z-tests (false-positive rates).
Results
B125M raised 56 total alarms for 57 annotated VT events and had the highest sensitivity (98%; P <.05), followed by iPM12 (84%), Life Scope (81%), Efficia (79%), ePM10 (77%), and IntelliVue (75%). B125M raised 20 false alarms, which was significantly lower (P <.0001) than iPM12 (284), Life Scope (292), IntelliVue (304), ePM10 (324), and Efficia (493). The most common false alarm was VT, followed by nonsustained VT.
Conclusion
We found significant performance differences among multiparameter bedside ECG monitoring systems using previously collected recordings. B125M had the highest sensitivity in detecting true VT events and lowest false alarm rate. These results can assist in minimizing alarm fatigue and optimizing patient safety by careful selection of in-hospital continuous monitoring technology.
Keywords: Alarm fatigue, Electrocardiogram, Electrocardiographic monitoring, False alarm, Outcomes, Sensitivity, Specificity, Ventricular tachycardia
Key Findings.
-
•
Our results indicate significant performance differences in the ventricular tachycardia (VT) detection sensitivity and false-positive alarm rate of 6 commonly used multiparameter bedside monitoring systems.
-
•
When tested using electrocardiographic (ECG) recordings, the B125M system displayed the highest sensitivity in alarming true VT events (98%; P <.05), followed by iPM12 (84%) and Life Scope (81%).
-
•
In the false alarm testing using 205 patient-hours of ECG recordings containing no cardiac arrhythmias, the B125M had the lowest number of false alarms (20; P <.0001), followed by iPM12 (284 alarms) and Life Scope (292).
-
•
These sensitivity and false alarm data can inform clinical practice regarding continuous ECG monitoring and help improve patient safety by optimizing VT detection and reducing alarm fatigue among health care providers.
Introduction
Patient monitoring devices are a critical component of the decision-making repertoire of health care personnel in caring for patients in the hospital environment, including directing the course of treatment and delivering lifesaving therapies. Bedside and central stations display waveforms, including electrocardiograms (ECGs), pulse rate, noninvasive blood pressure, invasive hemodynamic pressures (eg, arterial, pulmonary artery, central venous, and intracranial), respiratory rate, and peripheral oxygen saturation, among other parameters. ECG signals are the primary method for real-time monitoring of patient cardiac rhythm. The visual and auditory alarms created by these monitors play an integral part in patient care, and the response rate of health care personnel is dependent on the perceived credibility and accuracy of the systems.
Patient monitors are not intended to replace close observation of the patient by clinical staff, but a monitor that alerts for a potential cardiac arrhythmia is a useful tool to assist staff in monitoring patient conditions.1 Ventricular tachycardia (VT) is a common and dangerous arrhythmia that occurs during continuous ECG patient monitoring.2 Timely assessment and treatment of suspected VT is critical because untreated VT can result in severe, and in some cases fatal, complications. High VT burden can lead to syncope, electrical storm, cardiogenic shock, and cardiac arrest, and up to 10% of sustained VTs may degenerate into ventricular fibrillation (VF).3, 4, 5 Additional arrhythmias that require active monitoring include VF, nonsustained ventricular tachycardia (NSVT), accelerated ventricular rhythm, and asystole. Therefore, ventricular arrhythmia detection in a patient monitoring device must be optimized for sensitivity because uncaptured events will have an increasingly deleterious effect on patient outcomes.
As many as 90% of all arrhythmia alarms and 87% of VT alarms occur due to nonarrhythmia events, such as motion artifacts.2,6 Consequently, health care personnel are exposed to a high volume of physiological monitor alarms throughout their shifts, resulting in an excessively noisy environment that is perceived as the normal working atmosphere of a hospital.7 When health care personnel are required to address a high proportion of false alarms, they may become less likely to respond in a timely manner, or at all, to future events because of a perception that the alarm has a high probability of being nonactionable and because the alarm burden exceeds their capacity to respond. This phenomenon is defined as alarm fatigue, an important patient safety concern in which health care personnel become desensitized to alarm sounds.8 As a consequence of alarm fatigue, alarms may be silenced at the central station without checking the patient or may be totally ignored by health care personnel who find the repetitive notifications disruptive and noncontributory to patient care.
Over-alarming leads to nuisance and stress for health care personnel and patients, and alarm fatigue increases the risk of failure to actively monitor all alarms with potentially missed changes in patient condition and severe adverse events.9,10 Consequently, maintaining alarm value and utility is an important challenge for health care personnel and device manufacturers, creating a need for technology that maximizes sensitivity and specificity to critical cardiac events.2,11 Previous work has shown that certain features of different ECG monitoring systems, such as greater number of leads, are associated with increased sensitivity and retainment of high specificity in the detection of a range of adverse cardiac events.12, 13, 14, 15 However, there has not been a comprehensive evaluation of hospital-based continuous ECG patient monitoring technologies to advance clinical understanding of the strengths and weaknesses of the systems’ ventricular arrhythmia sensitivity and specificity and potential ventricular arrhythmia-based alarm fatigue.
Thus, the objective of this study was to compare the performance of 6 patient monitoring systems in the detection of ventricular arrhythmias during hospitalization using an annotated reference dataset. The sensitivity reference dataset was specific to VT and the false-positive reference dataset had no VT events, which enabled precise analysis of VT event detection and issuance of false VT alarms. The analysis of the monitoring systems was conducted by assessing (1) their ability to detect and alarm true VT events using verified VT event recordings; and (2) their false alarm rate and corresponding alarm fatigue burden using recordings with difficult ECG traces and no arrhythmia events.
Materials and methods
In this study, we determined the sensitivity and false alarm rate of various patient monitoring systems in order to inform clinical decision-making and help to optimize patient care. We tested 6 commonly used multiparameter bedside monitoring systems (Table 1).
Table 1.
Patient monitoring devices
| Device | Software version | First approval date | Manufacturer (location) |
|---|---|---|---|
| B125M | EK-Pro algorithm v14, VSP 3.0 | April 1, 2022 | GE HealthCare (Chicago, Illinois, USA) |
| ePM10 | V2 | June 8, 2020 | Mindray (Shenzhen, China) |
| iPM12 | V5.0 (05.27.00-01 SVN:44952) | July 3, 2013 | |
| Life Scope VS BSM-3000 | 05-20 (v0520t00) | May 2, 2021 | Nihon Kohden (Tokyo, Japan) |
| Efficia CM120 | A.01.00 (064) | January 26, 2016 | Philips (Amsterdam, Netherlands) |
| IntelliVue MX430 | M.04.00-149 | July 1, 2016 |
Data source
For this retrospective, observational study, 2 fully anonymized datasets were used to evaluate the devices, one for sensitivity testing and one for false alarm testing. Data were accessed for research purposes from January 2018 to August 2023. For the sensitivity testing, the dataset was collected by 8 different intensive care units in Europe and the United States (for details see Supplemental Table 1), which shared de-identified raw binary waveform ECG recording files with the study team under data sharing agreements. The recording files were from 29 individuals and included 57 VT arrhythmia events that were preselected and annotated by independent expert cardiologists based on the waveform graphs.
For the false alarm testing, the dataset comprised fully anonymized raw ECG binary waveform datafiles from the MADDEC (Mass Data in Detection and Prevention of Serious Adverse Events in Cardiovascular Disease) database, which includes electronic health record and biosignal data from a study population of approximately 73,000 individuals treated between 2007 and 2017 at the TAYS Heart Hospital in Finland.16 As a retrospective registry study, MADDEC did not require formal ethical approval, but the researchers obtained approval from the local authority overseeing the use of registry data as required by Finnish legislature.17
For this study, we selected Holter monitor recordings collected from 41 long-term post–percutaneous coronary intervention patients with a history of myocardial infarction (MI) who were monitored in a stepdown unit. All recordings had data from at least 4 leads collected: leads I, II, and III were always collected, and additional data were collected from either lead V1 or lead V5. The recordings had abnormal morphology on ECG, such as small QRS, high T-wave or P-wave, conduction abnormalities, significant damage caused by MI, or significantly noisy ECGs caused by patient movement. These recordings did not include any significant VT events, according to hospital patient records. The original recordings were 24 hours long, but because of time limitations for testing, only the first 5 hours of data was used for testing, resulting in a total of 205 hours of testing. Due to the retrospective nature of this study and the use of fully anonymized data, formal ethical approval and informed consent were not required. This study was conducted according to the ethical principles of the Declaration of Helsinki on the use of human data.
Test setup
All monitors were configured to their default settings, and the VT and asystole criteria were set as close to identical as possible (Table 2). The VT criteria were set to 6 premature ventricular contractions in all but the Life Scope (set to 9) because it did not allow changing the value without administrative privileges that were not available during the test. VT rate was 100 for all the monitors. Asystole duration was set to 5 seconds in all but the IntelliVue, which was set to its maximum value of 4 seconds. QRS threshold settings were not modified from the default values (Table 2).
Table 2.
Settings used in testing
| Settings | B125M | ePM10 | iPM12 | Life Scope | Efficia | IntelliVue |
|---|---|---|---|---|---|---|
| Default QRS threshold (mV) | ∼0.3∗ | 0.15 | 0.15 | 0.15 | 0.2 | 0.15 |
| ASY delay (s) | 5 | 5 | 5 | 5 | 5 | 4† |
| VT rate (bpm) | 100 | 100 | 100 | 100 | 100 | 100 |
| VT length (PVCs) | 6 | 6 | 6 | 9‡ | 6 | 6 |
ASY = asystole; PVC = premature ventricular contraction; VT = ventricular tachycardia.
The B125M default QRS threshold setting is approximately ∼0.3 mV, labeled on the device as “normal.”
Maximum value.
Setting unchangeable.
Tracked alarms
We tracked alarms for arrhythmias that would be considered potentially life-threatening events and would trigger a high severity alarm by all the monitors. Selecting alarms based on level of severity allowed us to track those alarms that would be expected to contribute the largest burden on health care providers to respond and thereby could contribute to alarm fatigue if raised erroneously. These included VT, VF/VT, NSVT, accelerated ventricular rhythm, asystole, and ventricular beat runs (VRUN). The criteria for each alarm type are given in Supplemental Table 2; false alarms were tracked separately by type. All “ventricular run” alarms that included >2 ventricular beats in a row with a heart rate above the ventricular bradycardia threshold were included. Alarms that were not turned on as part of the default settings on each device (ie, those that were optional) were not included.
Testing protocol
Digitized signals from the datasets of ECG recordings were converted to electric signals using a “data playback device.” All monitors were connected to the “data playback device” at the same time using their own lead wires simulating the patient. The devices used the beginning of each record as a learning period, which was excluded from the analysis. For sensitivity testing, the recordings with true VT events were fed to the devices simultaneously, alarm notifications were collected from the event histories of each device, and then alarms were compared to the reference annotations on true VT events. We note that in addition to VT events, the B125M has VF alarms labeled as “VF/VT” because VF events may also have sections of VT. Therefore, the VT/VF and the VF alarms given by other devices were classified as correct VT alarms for comparison. For false-positive testing, the false alarm recordings were fed to devices simultaneously and alarm notifications were collected to determine the number of false alarms. If >1 similar false alarm occurred within 3 seconds, they were calculated as 1 alarm only to most accurately count unique alarm events when a small gap (of approximately 1 correctly classified normal beat) was present between false alarm runs.
Statistical analysis
The sensitivity of each device was calculated by dividing the number of correct alarms by the total number of true VT events. Non-VT alarms for VT events were counted separately to acknowledge the clinical response and potential intervention that a non-VT alarm would trigger, prompting the health care personnel to check the status of the patient. The false-positive rate was computed by dividing the number of false alarms by the total testing time of 205 hours. An approach in which false alarms (False Positives) were compared to True Negative events was not applicable in this context, as True Negatives cannot meaningfully be defined when monitoring and analyzing continuous signals. Sensitivity is reported as percentage, with odds ratios (OR) and 95% confidence interval (CI). Comparisons of sensitivities were carried out using the “exact 2×2” package in R Version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria).
In order to make statistical comparisons of performance, one of the devices was selected to serve as the referent group. We selected the most recently approved of the study devices as the basis for comparisons (B125M), but the referent group was not used outside of these statistical comparisons or as a standard for determining correct or false annotations. The false-positive rate ratio was calculated as the ratio of the false-positive rate for each device to the false-positive rate of the referent group. The 95% CI of the false-positive rate ratio was calculated based on the distribution of the log-transformed rate ratio, which was approximately normal. To detect statistically significant differences, Fisher exact tests were used for sensitivities and Z-tests were used for false-positive rates. P <.05 was considered significant. Comparisons of false-positive rates and tests for significance were performed using SAS Version 9.4 (SAS Institute Inc., Cary, NC).
Results
In total, the sensitivity testing used data from 29 patients with 57 true VT events that resulted in 338 cumulative alarms from the 6 monitors. The false alarm testing used 5 hours of data from each of 41 patients for 205 patient-hours of recordings, which generated 1717 total false alarms across all 6 monitors. Our analyses indicated that different systems had statistically significant differences in sensitivity and false-positive rates that may inform the choice of technology for patient monitoring. The B125M displayed both the highest sensitivity and the lowest false alarm rate of all monitors tested. The iPM12 and Life Scope had the second and third highest sensitivity and lowest false alarm rate, respectively. The IntelliVue had the lowest sensitivity of all 6 monitoring devices under study; the Efficia had the highest false-positive rate.
Sensitivity
The B125M raised 56 total alarms for 57 investigated VT events for sensitivity of 98% (Table 3). Of these alarms, 49 were true VT alarms and 7 were non-VT alarms (3 AV and 4 NSVT). The iPM12 had the second-highest sensitivity (84%); it raised 31 true VT alarms and 17 non-VT alarms (15 NSVT and 2 VRUN). The Life Scope raised true VT alarms for 19 events and VRUN alarms for the other 27 alarmed VT events. We note that the Life Scope’s true VT alarm rates were not directly comparable to other monitors because of its less sensitive setting in VT length. The Efficia had the next-highest sensitivity (79%), alarming 45 of 57 VT events with no non-VT alarms. The ePM10 raised 33 VT and 11 non-VT alarms (8 NSVT and 3 VRUN). The IntelliVue had the lowest sensitivity to VT events, raising alarms for 43 of 57 events (75%) with no non-VT alarms. Data analysis indicated that the sensitivity of the B125M was significantly higher than all study comparators (P <.05).
Table 3.
Analysis of device sensitivity
| Device | Detected events | Not detected events | Sensitivity | Odds ratio∗ (95% confidence interval) | P value† |
|---|---|---|---|---|---|
| B125M | 56 | 1 | 0.98 | — | — |
| ePM10 | 44 | 13 | 0.77 | 0.06 (0.00–0.42) | <.001 |
| iPM12 | 48 | 9 | 0.84 | 0.10 (0.00–0.64) | .016 |
| Life Scope | 46 | 11 | 0.81 | 0.08 (0.00–0.55) | .004 |
| Efficia | 45 | 12 | 0.79 | 0.07 (0.00–0.48) | .002 |
| IntelliVue | 43 | 14 | 0.75 | 0.06 (0.00–0.37) | <.001 |
B125M device was used as the referent group.
False alarms
The B125M generated the lowest (P <.0001) number of false alarms (20), of which the majority (52%) were NSVT alarms (Tables 4 and 5). The iPM12 generated 284 false alarms, followed by the Life Scope with 292 alarms. The IntelliVue and the ePM10 had a moderate number of false alarms (304 and 324, respectively), and the Efficia had the highest number of false alarms (494). False alarms raised by the IntelliVue and the Efficia were almost exclusively VT alarms (97% and 96%, respectively).
Table 4.
False-positive rate analysis
| Device | False alarm count | FPR∗ | FPR ratio† (95% CI) | P value† |
|---|---|---|---|---|
| B125M | 20 | 0.10 | — | |
| ePM10 | 324 | 1.58 | 16.20 (10.31–25.45) | <.0001 |
| iPM12 | 284 | 1.39 | 14.20 (9.02–22.35) | <.0001 |
| Life Scope | 292 | 1.42 | 14.60 (9.28–22.97) | <.0001 |
| Efficia | 493 | 2.40 | 24.65 (15.76–38.55) | <.0001 |
| IntelliVue | 304 | 1.48 | 15.20 (9.67–23.90) | <.0001 |
FPR = false-positive rate; FPR ratio = ratio of the false-positive rate for each device to the false-positive rate of the referent group.
Count per person per hour.
B125M was used as the standard for comparisons.
Table 5.
False alarms by type
| Alarm | B125M | ePM10 | iPM12 | Life Scope | Efficia | IntelliVue |
|---|---|---|---|---|---|---|
| VT | 4 | 36 | 34 | 1 | 475 | 294 |
| VF/VT∗ | 0 | 106 | 84 | 56 | 4 | 3 |
| NSVT† | 11 | 173 | 164 | 0 | 0 | 0 |
| AVR | 3 | 0 | 0 | 0 | 0 | 0 |
| Asystole | 2 | 9 | 2 | 8 | 14 | 7 |
| VRUN | 0 | 0 | 0 | 227 | 0 | 0 |
| Total | 20 | 324 | 284 | 292 | 493 | 304 |
AVR = accelerated ventricular rhythm; NSVT = nonsustained ventricular tachycardia; VF = ventricular fibrillation; VRUN = ventricular beat runs; VT = ventricular tachycardia.
Labeled as VF on Life Scope.
Labeled as VT >2 on the B125M.
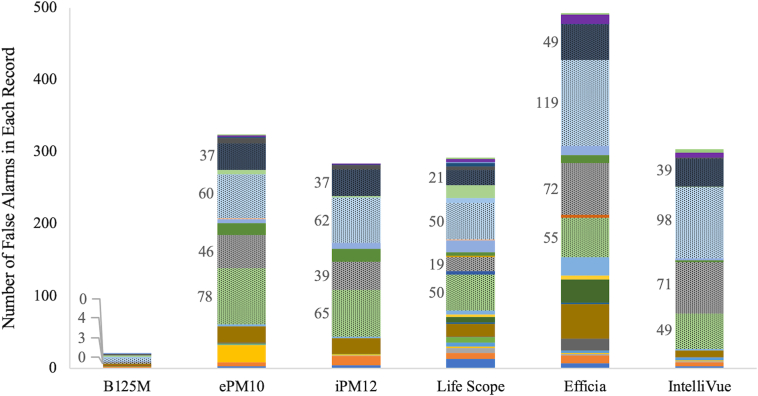
In considering the distribution of the false alarms according to their cases, 4 recordings were responsible for the majority of alarms (Figure 1). These were particularly noisy recordings with a consistently low signal-to-noise ratio that had been selected to challenge the monitors. The false alarms did not occur within a certain short episode in each of these recordings but were widely distributed across the total recording time.
Figure 1.
Distribution of false alarms in each record, across all devices. Each color represents the number of false alarms in 1 record across all the devices. Labeled bars indicate the 4 recordings with the greatest number of false alarms across all devices.
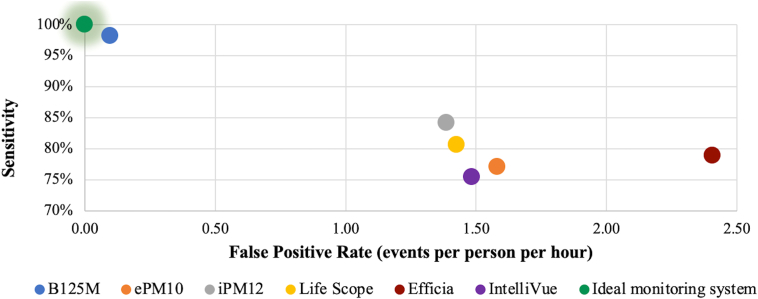
Combined examination of sensitivity and false alarm rate revealed that 4 of the examined devices had similar overall performance, clustered at the center of the plot: iPM12, Life Scope, IntelliVue, and ePM10 (Figure 2). These devices had moderate sensitivities (75%–84%) and false-positive rates around 1.5 events per patient per hour. The Efficia and B125M devices were removed from this central cluster because the Efficia had a higher false-positive rate (2.40 events per person per hour) that moved it to the right of the plot, and the B125M had a lower false-positive rate and higher sensitivity, bringing it closest to the ideal monitoring system at the top left of the plot. The ideal patient monitoring system has 0 false alarms and 100% sensitivity.
Figure 2.
Combined representation of sensitivity and false alarm rate. The ideal monitoring system is shown as the green dot at the top left.
Discussion
To the best of our knowledge, this is the first study to compare the sensitivity and false-positive rate of the ECG algorithms of 6 multiparameter bedside systems that are commonly used in clinical practice for in-hospital continuous patient monitoring to detect serious cardiac ventricular arrhythmias. We used a large sample of VT event recordings annotated by independent, expert cardiologists while managing patients with a history of acute MI to test sensitivity, resulting in highly controlled and interpretable data output. The monitors were challenged with >200 hours of difficult recordings to assess false alarms, a critically important performance characteristic in our current era of safety concerns surrounding alarm fatigue. Our results indicate that distinct systems have statistically significant differences in sensitivity and false-positive rates that may inform the choice of technology for patient monitoring.
The B125M monitor had the highest sensitivity (98%). It alarmed 56 of 57 VT events during the testing period, and 49 of the alarms were correctly labeled as VT. This sensitivity is comparable to the 97% achieved in a recent report of a machine learning–based algorithm for classification of VT.18 The other 5 monitors had variable but still moderately high sensitivity, ranging from 75%–84%. All monitors except the IntelliVue and Efficia had a proportion of non-VT alarms triggered for VT events, which may be associated with a slower reaction of the health care personnel. However, these alarms, although not correctly labeled, will likely achieve the desired outcome by capturing the attention of the health care provider, triggering assessment of the patient. Timely detection and treatment of cardiac arrhythmia are essential for patient monitoring given the potentially severe impact of undetected events on patient outcomes. Ventricular arrhythmias are major complications associated with poor in-hospital and long-term outcomes, including increased mortality.19, 20, 21
The monitors also performed differently in terms of the number of false alarms raised during the 205-hour testing period. The B125M had the lowest with 20 false alarms, which was strikingly lower than other study devices: iPM12 (284), Life Scope (292), IntelliVue (304), ePM10 (324), and Efficia (493). The majority of these rates align with estimates suggesting that nurses are responsible for responding to 150–400 alarms per patient per day.22,23 In contrast, the B125M may significantly lower the false-alarm response burden, with its rate of 2.4 alarms per patient per day (0.10 per patient per hour), as measured in this study. High alarm counts are an important consideration in patient care management because they are associated with large increases in subjective nurse-reported workload that should be minimized where possible.24 The most common type of false alarm varied by device and was more likely to occur during recordings that were particularly noisy or complex. This aligns with previous research that has shown ECG signal corruption can be due to a variety of sources, including muscle artifact, baseline wander, instrumentation noise, and power line interference, all of which can lead to false alarms.25,26 Although certain false alarms may be less meaningful in the context of signal noise, such as false alarms for asystole, these alarms still would be expected to contribute to the burden on health care providers when they occur in clinical practice and so were tracked accordingly in our study.
The hardware and software of these medical devices are complex, and the details are not publicly available. However, there are distinctions among the devices that may explain some of our results. For example, the B125M uses simultaneous 4-lead analysis, compared to 2- or 3-lead algorithms commonly used in the other devices.27 Recommendations from the American Heart Association stipulate that 2 or preferably 3 or more leads should be displayed and monitored simultaneously,28 as using multiple leads can increase the sensitivity of the algorithm because the QRS amplitude can be low in only 1 lead but normal in others, or the obviousness of ventricular beats can be more pronounced in a single lead but have only minor morphologic changes in other leads. In previous research, greater number of ECG leads has been associated with increased sensitivity and retainment of high specificity in the detection of a range of adverse cardiac events.12, 13, 14, 15 Therefore, algorithms that use more leads conceivably may improve the differentiation of arrhythmias from noise and artifacts and/or enable uninterrupted ECG monitoring in the event of an electrode failure. There may be a tradeoff in the slightly increased nursing workload associated with the application and maintenance of additional leads, but this must be balanced against the workflow advantages of improved sensitivity and alarm fatigue avoidance. Similarly, any tradeoff in cost associated with adoption of technology with higher sensitivity and lower false alarm rates must be balanced against the long-term potential to minimize alarm fatigue and optimize the workload of health care personnel. Because alarm fatigue may be associated with detrimental consequences for health care personnel, including nurse burnout and secondary traumatic stress,29 the impacts of reducing alarm fatigue may be substantial. Similarly, reduction of false alarms could reduce negative consequences experienced by patients, such as disrupted sleep or periods of instability that are missed by health care providers.8,30,31
It is important to select devices with sensitive and precise alerts to optimize patient care and avoid alarm fatigue by alarming only truly severe events and minimizing incorrect alarms. In 2023, reduction of patient harm associated with clinical alarm systems and alarm fatigue was identified by The Joint Commission as a National Patient Safety Goal.32 Reducing unnecessary alarm noise in order to avoid desensitization of staff was recommended to preserve the usefulness of alarms in alerting caregivers of potential patient problems. Optimized monitoring technology could be further coupled with additional interventions that have been shown to reduce alarm burden, such as adjusting alarm thresholds from their default settings to best suit the patient population.33 Such interventions also may be used in clinical settings where accessible devices have lower sensitivity or higher false alarm rates, in order to manage alarm burden when optimized monitoring technology is not available. Ultimately, ensuring that patients are monitored in line with best practices and using the optimal available technologies will benefit both patient safety outcomes and the burden on health care personnel.
Our findings suggest that careful selection of a patient monitoring system that optimizes sensitivity to critical arrhythmias while minimizing false alarms can be a key element in achieving these patient safety goals. The B125M system had significantly higher sensitivity (98%; P <.05) to VT events and the lowest false alarm event rate (0.10 events per person per hour; P <.0001) vs other commonly used patient monitoring systems. These results can inform decision-making by health care providers responsible for responding to patient alarms and managing potentially severe VT events, ultimately helping them to achieve patient safety goals. Additional research, particularly clinical studies, is needed to validate these findings in a clinical setting, and further technical assessments are necessary to understand the mechanisms of the devices as underpinning these significant differences in performance.
Study limitations
First, the full recordings used for sensitivity testing were not visually examined, so the sensitivity testing dataset may have contained ventricular arrhythmias that were not annotated, including possibly even missed VT arrhythmia events. A separate dataset known to contain no ventricular arrhythmias was used for false alarm testing in order to minimize the impact of this limitation. Second, the data were limited to the clinical settings described in the Methods and may not be generalizable to other contexts. Third, in the dataset used for false alarm testing, clinical notes were used to determine that no ventricular arrhythmias were detected, but false alarms were not separately verified by experts. Fourth, the set of monitors selected for testing represents a set of devices in common clinical use that were available to the researchers but does not include all available multiparameter monitors. Finally, these results should be interpreted in light of the controlled laboratory testing conditions of this analysis. Artifacts due to patient movement and shifting of electrode placement could be different in a hospital environment. However, the ECG recordings used here were collected in a hospital setting and thus contain the signal noise that would be expected in a real-world setting, and the direct comparison approach of this study is helpful in drawing meaningful conclusions. Overall, the trends in performance among monitors observed here are useful to assist health care personnel in selecting the most sensitive technology to optimize diagnosis and management of VT.
Conclusion
In comparing ventricular arrhythmia performance across 6 patient monitoring solutions, significant differences were found among devices in a laboratory-based assessment based on previously collected data. The B125M monitor was shown to have the highest sensitivity in detection of true VT events, with the lowest false alarm rate. These results provide important information to assist health care personnel in minimizing alarm fatigue and optimizing patient safety by careful selection of continuous monitoring technology.
Acknowledgment
Writing and editorial support was provided by Sarah Colton at Boston Strategic Partners, Inc.
Funding Sources
This work was supported by GE HealthCare, United States.
Disclosures
René Coffeng, Heikki Vaananen, and Dr Beard are employees of GE HealthCare. Dr Zhang, Dr Farrar, and Dr Yapici are employees of Boston Strategic Partners, Inc. Dr Cosentino discloses honoraria and/or consultation fees from Eli-Lilly, Sanofi, Novo Nordisk, GE HealthCare, Boehringer Ingelheim, Abbott, Bayer, and Menarini, and acknowledges grants from the Ministry of Health, Italy (RF GR-2019-12370197 and PNRR-MAD-2022-12376295).
Authorship
All authors attest they meeting ICMJE criteria for authorship.
Patient Consent
Due to the retrospective, observational nature of this study and the use of fully anonymized data, formal ethical approval and informed consent were not required.
Ethics Statement
This study was conducted according to the ethical principles of the Declaration of Helsinki on the use of human data.
Data Availability
Data cannot be shared publicly because of licensing restrictions. Fully anonymized data underlying the results presented in the study can be requested from the corresponding author (john.beard@ge.com).
Footnotes
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.cvdhj.2024.02.002.
Appendix. Supplementary data
References
- 1.Ellis J.E., Shah M.N., Briller J.E., Roizen M.F., Aronson S., Feinstein S.B. A comparison of methods for the detection of myocardial ischemia during noncardiac surgery: automated ST-segment analysis systems, electrocardiography, and transesophageal echocardiography. Anesth Analg. 1992;75:764–772. doi: 10.1213/00000539-199211000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Drew B.J., Harris P., Zègre-Hemsey J.K., et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS One. 2014;9 doi: 10.1371/journal.pone.0110274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buxton A.E., Calkins H., Callans D.J., et al. ACC/AHA/HRS 2006 key data elements and definitions for electrophysiological studies and procedures: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (ACC/AHA/HRS Writing Committee to Develop Data Standards on Electrophysiology) Circulation. 2006;114:2534–2570. doi: 10.1161/CIRCULATIONAHA.106.180199. [DOI] [PubMed] [Google Scholar]
- 4.Junaid Z., Sharad A. Management of ventricular tachycardia storm. Heart. 2021;107:1671. doi: 10.1136/heartjnl-2019-316192. [DOI] [PubMed] [Google Scholar]
- 5.Rüppel R., Schlüter C.A., Boczor S., et al. Ventricular tachycardia during follow-up in patients resuscitated from ventricular fibrillation: experience from stored electrograms of implantable cardioverter-defibrillators. J Am Coll Cardiol. 1998;32:1724–1730. doi: 10.1016/s0735-1097(98)00430-6. [DOI] [PubMed] [Google Scholar]
- 6.Harris P.R., Zègre-Hemsey J.K., Schindler D., Bai Y., Pelter M.M., Hu X. Patient characteristics associated with false arrhythmia alarms in intensive care. Ther Clin Risk Manag. 2017;13:499–513. doi: 10.2147/TCRM.S126191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou Y., Zhao G., Li J., et al. A contrastive learning approach for ICU false arrhythmia alarm reduction. Sci Rep. 2022;12:4689. doi: 10.1038/s41598-022-07761-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sendelbach S., Funk M. Alarm fatigue: a patient safety concern. AACN Adv Crit Care. 2013;24:378–386. doi: 10.1097/NCI.0b013e3182a903f9. quiz 87–88. [DOI] [PubMed] [Google Scholar]
- 9.Graham K.C., Cvach M. Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms. Am J Crit Care. 2010;19:28–34. doi: 10.4037/ajcc2010651. [DOI] [PubMed] [Google Scholar]
- 10.Lewandowska K., Weisbrot M., Cieloszyk A., Mędrzycka-Dąbrowska W., Krupa S., Ozga D. Impact of alarm fatigue on the work of nurses in an intensive care environment—a systematic review. Int J Environ Res Public Health. 2020;17:8409. doi: 10.3390/ijerph17228409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandau K.E., Funk M., Auerbach A., et al. Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation. 2017;136:e273–e344. doi: 10.1161/CIR.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 12.Perron A., Lim T., Pahlm-Webb U., Wagner G.S., Pahlm O. Maximal increase in sensitivity with minimal loss of specificity for diagnosis of acute coronary occlusion achieved by sequentially adding leads from the 24-lead electrocardiogram to the orderly sequenced 12-lead electrocardiogram. J Electrocardiol. 2007;40:463–469. doi: 10.1016/j.jelectrocard.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Ho D.S., Denniss R.A., Uther J.B., Ross D.L., Richards D.A. Signal-averaged electrocardiogram. Improved identification of patients with ventricular tachycardia using a 28-lead optimal array. Circulation. 1993;87:857–865. doi: 10.1161/01.cir.87.3.857. [DOI] [PubMed] [Google Scholar]
- 14.Tragardh E., Claesson M., Wagner G.S., Zhou S., Pahlm O. Detection of acute myocardial infarction using the 12-lead ECG plus inverted leads versus the 16-lead ECG (with additional posterior and right-sided chest electrodes) Clin Physiol Funct Imaging. 2007;27:368–374. doi: 10.1111/j.1475-097X.2007.00761.x. [DOI] [PubMed] [Google Scholar]
- 15.Zalenski R.J., Cooke D., Rydman R., Sloan E.P., Murphy D.G. Assessing the diagnostic value of an ECG containing leads V4R, V8, and V9: the 15-lead ECG. Ann Emerg Med. 1993;22:786–793. doi: 10.1016/s0196-0644(05)80792-9. [DOI] [PubMed] [Google Scholar]
- 16.Hernesniemi J.A., Mahdiani S., Lyytikäinen L.-P., et al., editors. Cohort Description for MADDEC—Mass Data in Detection and Prevention of Serious Adverse Events in Cardiovascular Disease. Springer Singapore; Singapore: 2018. [Google Scholar]
- 17.Syyli N., Hautamäki M., Antila K., et al. Left ventricular ejection fraction adds value over the GRACE score in prediction of 6-month mortality after ACS: the MADDEC study. Open Heart. 2019;6 doi: 10.1136/openhrt-2019-001007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ansari S., Belle A., Ghanbari H., Salamango M., Najarian K. Suppression of false arrhythmia alarms in the ICU: a machine learning approach. Physiol Meas. 2016;37:1186–1203. doi: 10.1088/0967-3334/37/8/1186. [DOI] [PubMed] [Google Scholar]
- 19.Cronin E.M., Bogun F.M., Maury P., et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Heart Rhythm. 2020;17:e2–e154. doi: 10.1016/j.hrthm.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Masuda M., Nakatani D., Hikoso S., et al. Clinical impact of ventricular tachycardia and/or fibrillation during the acute phase of acute myocardial infarction on in-hospital and 5-year mortality rates in the percutaneous coronary intervention era. Circ J. 2016;80:1539–1547. doi: 10.1253/circj.CJ-16-0183. [DOI] [PubMed] [Google Scholar]
- 21.Mehta R.H., Starr A.Z., Lopes R.D., et al. Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA. 2009;301:1779–1789. doi: 10.1001/jama.2009.600. [DOI] [PubMed] [Google Scholar]
- 22.Keller J.P. Clinical alarm hazards: a “top ten” health technology safety concern. J Electrocardiol. 2012;45:588–591. doi: 10.1016/j.jelectrocard.2012.08.050. [DOI] [PubMed] [Google Scholar]
- 23.Schondelmeyer A.C., Brady P.W., Goel V.V., et al. Physiologic monitor alarm rates at 5 children's hospitals. J Hosp Med. 2018;13:396–398. doi: 10.12788/jhm.2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rasooly I.R., Kern-Goldberger A.S., Xiao R., et al. Physiologic monitor alarm burden and nurses' subjective workload in a children's hospital. Hosp Pediatr. 2021;11:703–710. doi: 10.1542/hpeds.2020-003509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Satija U., Ramkumar B., Manikandan M.S. A review of signal processing techniques for electrocardiogram signal quality assessment. IEEE Rev Biomed Eng. 2018;11:36–52. doi: 10.1109/RBME.2018.2810957. [DOI] [PubMed] [Google Scholar]
- 26.Bashar S.K., Ding E., Walkey A.J., McManus D.D., Chon K.H. Noise detection in electrocardiogram signals for intensive care unit patients. IEEE Access. 2019;7:88357–88368. doi: 10.1109/access.2019.2926199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.GE HealthCare B1x5M and B1x5P Patient Monitors. https://www.gehealthcare.com/en-my/products/patient-monitoring/b1x5m-and-b1x5p Updated 2023.
- 28.Mirvis D.M., Berson A.S., Goldberger A.L., et al. Instrumentation and practice standards for electrocardiographic monitoring in special care units. A report for health professionals by a Task Force of the Council on Clinical Cardiology, American Heart Association. Circulation. 1989;79:464–471. doi: 10.1161/01.cir.79.2.464. [DOI] [PubMed] [Google Scholar]
- 29.Dehghan M., Mokhtarabadi S., Rashidi E., Rahiminejad E., Asadi N. Correlation between professional quality of life and alarm fatigue symptoms among intensive care unit nurses. Health Sci Rep. 2023;6:e1583. doi: 10.1002/hsr2.1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Winters B.D., Cvach M.M., Bonafide C.P., et al. Technological distractions (part 2): a summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit Care Med. 2018;46:130–137. doi: 10.1097/CCM.0000000000002803. [DOI] [PubMed] [Google Scholar]
- 31.Hravnak M., Pellathy T., Chen L., et al. A call to alarms: current state and future directions in the battle against alarm fatigue. J Electrocardiol. 2018;51(6S):S44–S48. doi: 10.1016/j.jelectrocard.2018.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The Joint Commission National Patient Safety Goals: Effective July 2023 for the Hospital Program, March 29, 2023. https://www.jointcommission.org/standards/national-patient-safety-goals/hospital-national-patient-safety-goals/
- 33.Turmell J.W., Coke L., Catinella R., Hosford T., Majeski A. Alarm fatigue: use of an evidence-based alarm management strategy. J Nurs Care Qual. 2017;32:47–54. doi: 10.1097/NCQ.0000000000000223. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared publicly because of licensing restrictions. Fully anonymized data underlying the results presented in the study can be requested from the corresponding author (john.beard@ge.com).