Summary
This paper outlines the process undertaken by Asian National Cancer Centers Alliance (ANCCA) members in working towards an Asian Code Against Cancer (ACAC). The process involves: (i) identification of the criteria for selecting the existing set of national recommendations for ACAC (ii) compilation of existing national codes or recommendations on cancer prevention (iii) reviewing the scientific evidence on cancer risk factors in Asia and (iv) establishment of one or more ACAC under the World Code Against Cancer Framework. A matrix of national codes or key recommendations against cancer in ANCCA member countries is presented. These include taking actions to prevent or control tobacco consumption, obesity, unhealthy diet, physical inactivity, alcohol consumption, exposure to occupational and environmental toxins; and to promote breastfeeding, vaccination against infectious agents and cancer screening. ANCCA will continue to serve as a supportive platform for collaboration, development, and advocacy of an ACAC jointly with the International Agency for Research on Cancer/World Health Organization (IARC/WHO).
Keywords: Asia, Code, Cancer, Prevention, Risk factors, Non-communicable diseases, ANCCA, ACAC
Introduction
Asia is the largest and most populated geographical region in the world, with 4.6 billion people or 60% of the world’s population. An estimated 9.5 million new cancer cases were diagnosed in Asia in 2020, accounting for almost half of all cancers diagnosed globally.1 Nearly 6 million deaths were caused by cancer in the region in the same year, accounting for 58% of global cancer deaths.1 The current cancer burden in Asia is expected to rise significantly by 2030 due to a combination of factors including population growth, ageing population, industrialisation and increasing exposure to environmental and occupational carcinogens and unhealthy lifestyles.2,3 A multipronged approach across prevention, early detection, treatment, and palliative care is needed to control the growing cancer burden.4 Evidence-based recommendations are needed to guide successful cancer prevention, tailored to the disease epidemiology of the population according to their cancer burden, established risk factors, and health care systems.5
The International Agency for Research on Cancer (IARC/WHO) and its partners launched the World Code Against Cancer Framework in 2022 to promote cancer prevention globally and to provide evidence-based recommendations through the development of Regional Codes Against Cancer.6 This Framework was inspired by the European Code Against Cancer (ECAC) which was first created in 1987 as a set of recommendations to advise European Union (EU) populations on cancer prevention.7 The ECAC was developed through EU experts’ assessment of systematic reviews of the scientific literature on cancer risk factors and effective preventive measures. The ECAC 4th edition was the first to be developed using the new IARC/WHO methodology later proposed to guide the World Code Against Cancer Framework.7 The ECAC consists of three levels of information: (i) The 12 recommendations for avoiding or reducing exposure to specific carcinogenic agents, adopting healthy behaviours, and encouraging participation in vaccination and screening programmes7,8; (ii) Supplementary information in questions-and-answers (Q&As), explaining and providing contextual and additional information on the 12 recommendations as well as on areas of cancer prevention not covered by the ECAC and of interest for the general public7,8; and (iii) Peer-reviewed open access publications summarizing the project, methodology and the scientific justification of each recommendation.9 More recently, the Latin American and Caribbean (LAC) region has started developing the three levels of information that form the basis for the Latin American and the Caribbean Code Against Cancer. The LAC Code is directed at the general public, health providers and policymakers, in Spanish, Portuguese, and English languages, with IARC/WHO as coordinator, and follow the guidelines and methodology of the World Code Against Cancer Framework.6
In 2021, as part of its consolidation of priorities to address gaps in cancer control, the Asian National Cancer Centers Alliance (ANCCA) recognised the importance of developing a set of cancer prevention recommendations for Asia.10 The main objective of this paper is to provide a status overview of cancer prevention recommendations currently in place in Asian countries. This paper also outlines the initial processes undertaken by ANCCA in formulating the essential criteria, for selecting the existing set of national codes or recommendations against cancer for Asia based on the World Code Against Cancer Framework. The paper documents the work-in-progress among ANCCA members in assessing the key preventive measures against cancer and compilation of the cancer prevention recommendations and control plans already in place among ANCCA members. Our overarching aim is to develop an Asian Code Against Cancer (ACAC) with potential sub-chapters to account for the large and diverse population of the Asian region, following the rigorous review process of scientific evidence defined in the IARC/WHO World Code Against Cancer Framework and criteria. ACAC’s development will be jointly steered by IARC/WHO and ANCCA, and disseminated by ANCCA and other regional cancer control stakeholders.
Process in working towards an ACAC
ANCCA initiated several rounds of virtual consultations and engagements with its members and associates in 2021. The aims of the consultations were to (i) review and collate country-specific data on cancer burden and existing cancer control strategies, (ii) compile country-specific key recommendations or national codes already available on cancer prevention and (iii) summarise existing scientific evidence on cancer risk factors. Webinar and virtual meetings were held with experts from IARC/WHO to share the World Code Against Cancer Framework and EU’s and LAC’s experience and methods in developing the respective Codes Against Cancer. In addition, ANCCA members identified and discussed challenges and opportunities in the development of ACAC within this Framework, the review of scientific evidence and the formulation of future recommendations in consideration of the regional cancer prevention mechanisms and structures. Each ANCCA member presented a snapshot of their national cancer burden and cancer control program and existing national codes or recommendations for cancer prevention in their country.
ANCCA conducted several rounds of virtual monthly meetings with its members from Bangladesh (BD), Bhutan (BH), Brunei Darussalam (BN), Cambodia (CM), China (CN), India (IN), Indonesia (ID), Iran (IR), Japan (JP), Korea (KR), Laos (LA), Malaysia (MY), Mongolia (MN), Myanmar (MM), Nepal (NP), Pakistan (PK), Philippines (PH), Singapore (SG), Sri Lanka (SL), Thailand (TH) and Vietnam (VN). These countries met ANCCA membership requirements and agreed to engage in ANCCA initiatives on a voluntary basis. Surveys and voting polls were developed for ANCCA members to provide feedback and comments.
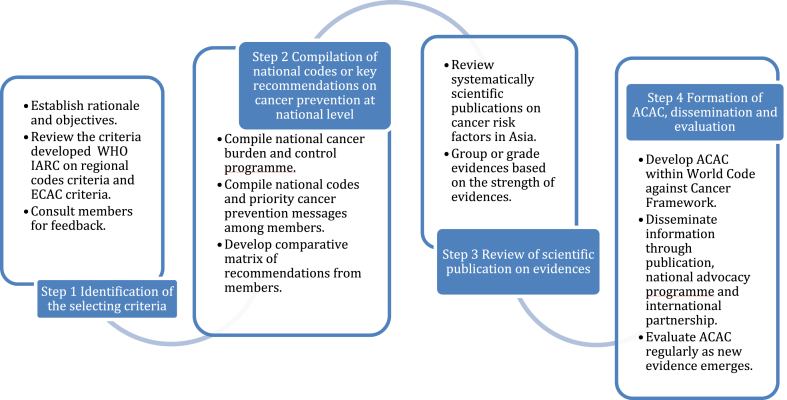
The overall development can be summarised as a 4-step process (Fig. 1), consisting of step 1: identification of the criteria for selecting the existing set of recommendations against cancer for Asia, based on the criteria defined by the World Code Against Cancer Framework; step 2: compilation of existing national codes or key recommendations on cancer prevention at national level; step 3: scientific literature review of cancer risk factors in Asia. The outcome will feed into ACAC development within the World Code Against Cancer Framework and the development of step 4: establishment of an ACAC or sub-regional ACACs and continuous dissemination, evaluation and update as new evidence emerges. This paper reports on the preparatory work from step 1 and step 2 on the development process of ACAC, resulting in a repository on cancer prevention recommendations among ANCCA members to inform the development of the ACAC; and also, the preliminary findings from step 3 reviewing literature on cancer risk factors in Asia.
Fig. 1.
Process in working towards an Asian Code Against Cancer (ACAC) as part of the World Code Against Cancer Framework. Note: Step 1 and 2 and preliminary Step 3 are outlined in this paper. IARC, International Agency for Research on Cancer; ECAC, European Code Against Cancer.
In step 1, selecting criteria for guiding the relevance of existing recommendations were reviewed by ANCCA members based on the World Code Against Cancer Framework6 methodology and the more detailed criteria published under the ECAC.7 Criterion V describes the different target audiences,5 and criterion VI defines the rationale of Regional Codes to be tailored to their target population under risk.5
ANCCA member countries share many common cancer-related risk factors, but some cancer risk factors are more prevalent or even unique to certain countries, and some preventive measures are prioritised over others. Therefore, the criteria for selecting each recommendation for this compilation of existing recommendations were identified and agreed upon by the members. A list of criteria for selecting existing cancer prevention recommendations for Asia and reviewing implemented cancer prevention strategies among ANCCA member countries, based on the IARC/WHO methodology as defined in the World Code Against Cancer Framework and the ECAC, has been assembled in Table 1.5,7
Table 1.
List of criteria to guide inclusion of cancer prevention recommendations in the Asian Code Against Cancer (ACAC), based on the World Code Against Cancer Framework.
| Criteria | Description |
|---|---|
| I | The recommendation is supported by robust scientific evidence for public to adopt healthy lifestyle, or participate in public health activities such as vaccination, screening and avoid exposure to harmful agents in order to reduce the individual’s risk of developing cancer. |
| II | The recommendation is suitable for a broad target population affected by a risk factor that causes significant cancer burden. |
| III | The recommendation is action based, where risks and benefits are assessed and balanced out to allow individuals to do something to reduce their cancer risk; the actions should not involve difficult decisions for the individual. |
| IV | The recommendation can be communicated to the public in simple language, clear succinct and instructive language, without hectoring. |
| V | The recommendation can be framed at several levels to address or influence various target groups including the general population, policymakers, clinicians, and healthcare professionals. |
| VI | The recommendation is relevant for the region in terms of epidemiological, socioeconomic, and cultural conditions in Asia, and adapted to the availability and accessibility of healthcare services and interventions. |
Recommendations on cancer prevention at national level among ANCCA members
In step 2 on compilation of existing national codes or recommendations on cancer prevention, ANCCA members shared their national cancer prevention themes and rationale for prioritising the selected cancer prevention messages in their countries. A comparative matrix of national codes or recommendations was compiled, based on the prioritised cancer or non-communicable disease (NCD) preventive measures from the ANCCA members. Table 2 provides a matrix of the existing national codes or recommendations on cancer prevention at national level among participating ANCCA countries. Of the 21 countries which submitted responses to the survey, three countries (China, Japan and Korea) have national codes against cancer. Only the Korean cancer prevention recommendations have been formally approved by the government.
Table 2.
ANCCA member countries’ key recommendations or national codes on cancer prevention.
| Cancer risk reduction actions | BD | BH | BN | CM | CN | IN | ID | IR | JP | KR | LA | MY | MM | MN | NP | PK | PH | SG | SL | TH | VN |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Existence of national official codes against cancer | N | N | N | N | Y | N | N | N | Y | Y | N | N | N | N | N | N | N | N | N | N | N |
| 1. Say no to any tobacco product. Do not smoke. Take action to quit smoking. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ |
| • Keep your environment, home, and workplace smoke free. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||
| 2. Maintain a healthy body weight. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| 3. Be active every day. Avoid sedentary lifestyle. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| 4. Eat balanced healthy meals | |||||||||||||||||||||
| • Eat more fruit and vegetables, whole grains, and legumes. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |
| • Reduce intake of sugary food and drinks. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| • Reduce intake of processed and red meat and salty foods. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||||
| 5. Avoid or minimise alcohol intake. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||
| 6. Avoid or reduce exposure to carcinogens in the workplace and ensure use of personal protective equipment (PPE). | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||
| 7. Take action to reduce environmental pollutants including air pollution, pesticides, radiation. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||
| 8. Take part in vaccination programs for: | |||||||||||||||||||||
| • Hepatitis B | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| • Human papillomavirus (HPV) | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||
| 9. Participate in cancer screening programs: | |||||||||||||||||||||
| • Bowel cancer | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||
| • Breast cancer | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| • Cervical cancer | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| • Other cancer screening (including gastric, oral, thyroid) | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||
| 10. Encourage and support mothers to breastfeed. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||
| 11. Other common cancer prevention recommendations: | |||||||||||||||||||||
| • Manage stress and take care of mental health. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||
| • Avoid unsafe sex. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||
| • Protect yourself from ultraviolet radiation from the sun. | ✔ | ✔ | ✔ | ✔ | |||||||||||||||||
| • Use hormone replacement therapy (HRT) with caution in consultation with a clinician. | ✔ | ✔ | ✔ |
Abbreviations for ANCCA member countries: BD, Bangladesh; BH, Bhutan; BN, Brunei Darussalam; CM, Cambodia; CN, China; IN, India; ID, Indonesia; IR. Iran; JP, Japan; KR, Korea; LA, Laos; MY, Malaysia; MN, Mongolia; MM, Myanmar; NP, Nepal; PK, Pakistan; PH, Philippines; SG, Singapore; SL, Sri Lanka; TH, Thailand; and VN, Vietnam.
N, No; Y, Yes.
Notes: Korea: codes approved by the Ministry of Health, National Cancer Center, Scientific and academic groups.
The matrix presents key recommendations adapted from the 4th edition of the European Code Against Cancer (Schuz et al., 2015).
The text in column 1 is exemplar for the topic but the exact wording may vary across national recommendations.
Smoking, a leading cause of cancer, is the only recommendation which was part of the set of national recommendations in all participating countries. However, differences were seen in the recommendation on smoke-free workplaces and homes, 11 of the 21 countries highlighted this as a national recommendation to prevent cancer. Avoiding alcohol was highlighted in 15 countries. Reducing the intake of red or processed meat and food high in salt as diet-specific national recommendations were highlighted in nine countries. Recommendations related to the promotion of breastfeeding are present in 14 countries, while only three countries specified advice on hormone replacement therapy (HRT) as a recommendation for cancer prevention.
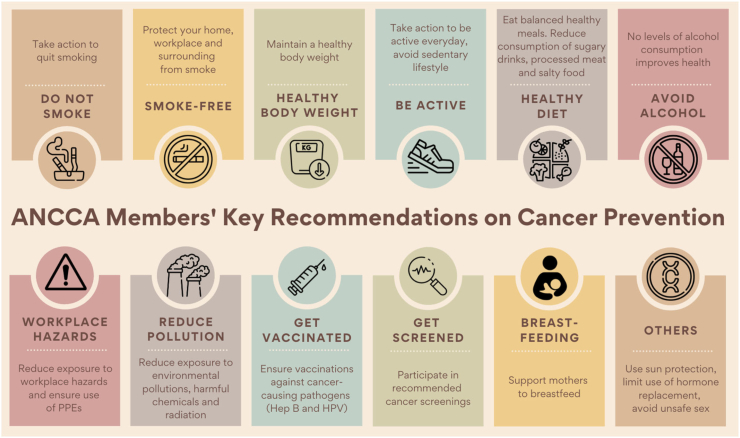
Most participating Asian countries have recommendations which are not included in the 4th edition of the ECAC.7 For example, taking care of mental health was shared by many ANCCA members as one of the key recommendations as part of general healthy lifestyle priority messages. Several ANCCA members shared subregion-specific cancer risk factors such as exposure to air pollution, chewing tobacco, pesticide and chemical fertilizer use, intake of food containing trans-fat, consumption of arsenic from ground water, lack of personal protective equipment (PPE) and unsafe sex; these were highlighted as key cancer prevention messages in some of the Asia subregions where prevalence was high. These additional factors were identified as priority cancer prevention messages or recommendations shared by ANCCA members. ANCCA members have compiled a pictorial summary of the matrix (Table 2) for easier visualisation of the information, and to support further work towards developing codes against cancer in the region and among the member countries (Fig. 2). Fig. 2 is an overview of key cancer risk factors compiled by ANCCA and is not the final ACAC for the region.
Fig. 2.
ANCCA members’ key recommendations on cancer prevention. ∗Note: Fig. 2 is a pictorial summary of cancer risk factors and does not represent the final code for the region. PPE, personal protective equipment; Hep B, hepatitis B; HPV, human papillomavirus.
Most Asian countries currently do not have national codes or recommendations specifically addressing cancer prevention. The national cancer prevention messages in Asian countries typically are embedded within the more general messages to promote healthy lifestyle to prevent NCDs. This can dilute the efforts to increase cancer prevention awareness among the public. Inadequate health literacy or an inability to comprehend health information has been linked to unfavourable lifestyles and health choices, in turn leading to poorer health outcomes.11 This effect is more evident in developing countries in Asia compounded by gaps in healthcare such as inadequate accessibility to health information, scarcity of resources and underdeveloped infrastructure.12
China, Japan and Korea have developed their national codes against cancer. The development of specific codes against cancer has allowed streamlining of cancer prevention messages across different populations, thereby strengthening cancer prevention awareness among the public. This also facilitates developing programs for risk factor surveillance leading to other benefits including formulation and implementation of public policies. They could also serve as a beacon for providing a template to guide cancer prevention in other countries in the region including the formulation of an acceptable ACAC with sub-chapters for Asian sub-regions.
Cancer burden and risk factors among ANCCA members
An initial literature review on cancer risk factors in Asia (step 3) was conducted by ANCCA members, and ANCCA member countries were invited to share scientific literature on evidence of cancer risks that were utilised in their countries to guide cancer control and preventive measures. Selected studies were discussed i webinars where participants were encouraged to adopt an internationally established grading system to assess the strength of evidence of the scientific literature identified.
Cancer incidence and mortality are diverse across and within countries in Asia.12 Cancer incidence and mortality rates using the most recent estimates from GLOBOCAN for ANCCA member countries are shown in Table 3. The age standardised (World Standard Population)1 cancer incidence rates ranged from 80.9 in Nepal to 285.1 in Japan per 100,000 population. The age standardised cancer mortality rate ranged from 54.8 in Nepal to 176.2 in Mongolia per 100,000 population.1 The population of these countries ranged from 433,000 in Brunei Darussalam to over 1.4 billion in China.13
Table 3.
Age standardized cancer incidence and mortality rates for Asian National Cancer Centers Alliance (ANCCA) member countries.
| ANCCA members and associates | Population (thousand)13 | ASIR1 | ASMR1 |
|---|---|---|---|
| Bangladesh (BD) | 163,046 | 106.2 | 75.3 |
| Bhutan (BH) | 763 | 81.9 | 66.6 |
| Brunei (BN) | 433 | 224.0 | 107.8 |
| Cambodia (CM) | 16,487 | 135.3 | 97.0 |
| China (CN) | 1,433,784 | 204.8 | 129.4 |
| India (IN) | 1,366,418 | 97.1 | 63.1 |
| Indonesia (ID) | 270,626 | 141.1 | 85.1 |
| Iran (IR) | 82,914 | 152.7 | 94.0 |
| Japan (JP) | 126,860 | 285.1 | 81.5 |
| Korea (KR) | 51,225 | 242.7 | 75.5 |
| Laos (LA) | 7169 | 165.8 | 117.8 |
| Malaysia (MY) | 31,950 | 143.9 | 87.3 |
| Mongolia (MN) | 3225 | 215.6 | 176.2 |
| Nepal (NP) | 28,609 | 80.9 | 54.8 |
| Philippines (PH) | 108,117 | 162.0 | 100.0 |
| Pakistan (PK) | 216,565 | 110.4 | 74.3 |
| Singapore (SG) | 5804 | 233.0 | 111.5 |
| Sri Lanka (SL) | 21,324 | 105.4 | 57.2 |
| Thailand (TH) | 69,626 | 164.0 | 100.5 |
| Turkey (TR) | 83,430 | 231.5 | 120.4 |
| Vietnam (VN) | 96,462 | 159.7 | 106.0 |
ASIR, age standardised incidence rate of cancer per 100,000 population.
ASMR, age standardised mortality rate of cancer per 100,000 population.
Asia has a diverse socioeconomic and cultural landscape that is closely intertwined with its disease pattern. Asian populations share many similarities in terms of risk factors for cancer,14, 15, 16, 17 notably some that are widely shared around the world. Modifiable cancer risk factors can be clustered into distinct but overlapping groups: behavioural, infectious, environmental and occupational.18 A substantial proportion of newly diagnosed cancers in Asia are potentially preventable as they are attributable to modifiable risk factors.2,19 Most common cancers in Asia have been linked to specific behavioural or lifestyle risks such as tobacco use; alcohol consumption; obesity, and infectious agents such as Helicobacter pylori (H. pylori), hepatitis B virus and human papillomavirus (HPV).18
Key scientific evidence from peer-reviewed literature which supported the national codes or key recommendations on cancer prevention at national level were identified. Summative findings from the literature review are presented in the section below.
Tobacco and second-hand smoking
The average rate of tobacco use among people aged 15 years and older in South-East Asia decreased from 50% in 2000 to 29% in 2020.20 However, the region still has the highest average rate of tobacco use compared to all other WHO regions.20 Additionally, vaping and smokeless tobacco including chewing betel nut remain as important risk factors in the region.21 In many Asian countries, exposure to second-hand smoke is common at home and in public places and can be as high as 85%.22 The prevalence of second-hand smoke exposure among adolescents (defined as people smoked in their presence on one or more days in the past week) from the South East Asia and Western Pacific regions were reported to be as high as 37.0% at home and 70% in public places.23
Obesity
Studies have identified obesity as a risk factor for 16 site-specific cancers, and there is a stronger adverse effect of obesity on breast cancer risk reported for women of Asian ethnicity than for women of Hispanic, African, or non-Hispanic White ancestry.2 The prevalence of overweight and obesity (BMI ≥ 25 kg/m2) among men and women in countries making up the Association of Southeast Asian Nations (ASEAN) ranges from 20.3% in Cambodia to 62.8% in Brunei.24
Physical activity
Physical activity is associated with reduced risks of bladder, breast, colon, endometrial, oesophageal (adenocarcinoma), renal and gastric cancers, with relative risk reductions up to 25%.2 In some regions of Asia, the prevalence of insufficient physical activity is higher among women. In the ASEAN region, countries have reported prevalence of insufficient physical activity ranging from 8 to 40% in the adult population and 76–93% among adolescents aged 11–17 years.24
Diet
Broad heterogeneity is observed in dietary patterns across countries in Asia. A significant proportion of the Southeast Asian population reported inadequate consumption of fruit and vegetables—91.7% in Brunei, 95.5% in Indonesia, 95.0% in Malaysia and 67.0% in Vietnam.24 According to 2015 Organisation for Economic Co-operation and Development (OECD) data, Korea had the highest daily vegetable intake globally.25 A systematic review on diet and colorectal cancer in Asia has identified components of diet including meat, fat, salt and sugar to be associated with increased risk of gastro-intestinal tract cancers, while lower cancer risks were seen with very high intakes of vegetable, fruit, fibre and micronutrients.26
Alcohol use
Alcohol intake is causally related to several cancer sites (oral cavity, pharynx, larynx, oesophagus [squamous cell carcinoma], female breast, liver, colon and rectum).2 The eastern Asian region has the highest estimated population attributable fraction (PAF) of cancer incidence at 5.7% (8.6% for men and 2.1% for women) attributable to alcohol consumption (worldwide PAF of 4.1% [6.1% for men and 2.0% for women]).27 In Asia, Mongolia and China have the highest fractions attributable to alcohol of cancer incidence estimated at 15.0% and 9.6% respectively among men.27
Environmental pollution and occupational exposure to carcinogenic substances
A large number of environmental pollutants are released from various sources, affecting populations through diverse routes of exposure, with air pollution as a major contributor to cancer burden.2 Every year, increasing numbers of newly-created chemicals are introduced into workplaces, and very few of them have been comprehensively assessed for carcinogenicity.28 East and South Asia regions have reported the highest cancer burden due to the thirteen occupational carcinogens (arsenic, asbestos, benzene, beryllium, cadmium, chromium, diesel engine exhaust, formaldehyde, nickel, polycyclic aromatic hydrocarbons, silica, sulphuric acid, and trichloroethylene).29 Asbestos and silica exposure were highest in some Asian countries. Some countries have banned the use of asbestos but many including China continue to mine or import and use it widely.29 Most countries have enacted counter regulations, but enforcement usually concentrates on the immediate risks, which results in a gap for prevention of long-term conditions such as cancer. Improper disposal and management of industrial waste, from methods like incineration, can result in the release carcinogenic chemicals including dioxins and heavy metals. These chemicals are endocrine disrupters interfering with the body’s hormone production and regulation, and have been associated with the development of breast and testicular cancer.2
Vaccination against cancer
Prevalence of HPV, varies among Asian countries, were reported at 21% in Iran30 (for oral mucosal lesions), 20% in Korea31 (with 74% being HPV16/18) and 19.0–84.4% in China.32,33 In a 2017 meta-analysis34 conducted in Asian populations, HPV vaccines significantly enhanced HPV16 and HPV18-specific antibody levels. In a 2022 systematic review,35 HPV vaccination was found to be cost-effective for implementation in high-income, middle-income, and low-income countries in Asia. In many Asian countries, the coverage of HPV vaccine remains low due to several barriers such as high cost and lack of a national HPV vaccination program.
Cancer screening
Lack of awareness and knowledge about cancer prevention and screening, and psychosocial-related factors remain significant barriers to screening uptake in Asian communities.36 Health education through primary healthcare workers was found to be a crucial facilitator in increasing uptake of screening.36,37 In addition, selected cancers found to have higher burden in a particular Asian setting may warrant consideration of targeted cancer screening of high-risk populations. For example, screening and treatment of H. pylori to prevent gastric cancer have been recommended in some settings such as Japan and Korea.38 H. pylori is significantly associated with gastric cancer in Asia with significant regional variation in terms of Disability-Adjusted Life-Years (DALYs). The DALYs ranged from 298.9 thousand in China to 1.9 thousand in Malaysia. The average prevalence of H. pylori in the studied Asian populations (China, Iran, Japan, Korea and Malaysia) was estimated to be 56.3%.39
Breastfeeding
There is an established inverse association between breastfeeding and risk of endometrial cancer, with a relative risk of 0.57 (95% confidence interval (CI) 0.37 to 0.87).40 A longer duration of breastfeeding is associated with a stronger protective effect against ovarian41 and breast cancers.2 The rate of exclusive breastfeeding of infants in the first six months of life ranged from 21% in China to 82% in Sri Lanka.42 The WHO Global Nutrition Targets have included exclusive breastfeeding rate in the first six months to reach at least 50% by 2025, while the current global average is estimated at 37%.43
Other risk factors associated with cancer in Asia
The Global Burden of Disease Study (2019) has attributed unsafe sex as the second leading cancer risk factor for females, responsible for 8·2% of all female cancer DALYs in 2019.44 Sexually transmitted infections, including HPV, Hepatitis and HIV, have been found to cause oral, prostate and cervical cancer, hepatocellular carcinoma and Kaposi sarcoma2,45,46
The relationship between mental illness and cancer risk warrants further study and review. Some studies have linked mental illnesses with the development of certain cancers including breast, colorectal and lung cancers. Higher cancer mortality has also been associated with poorer adherence to screening or treatment among patients with mental illnesses.47, 48, 49
Menopausal hormone replacement therapy is associated with increased ovarian cancer risk, with a pooled relative risk of 1.76 in a meta-analysis involving Asian populations.50 Exposure to radiation is also an established risk factor for several types of solid cancers with a dose response relationship.51 Specifically, UV radiation exposure has been causally linked to skin cancers including melanoma,2 and is one of the recommendations in ECAC. In Asian populations, prevalence of malignant skin cancer is lower compared to those of European ancestry,2 and avoiding sun exposure was considered lower in priority among the list of cancer prevention recommendations by ANCCA members.
Diabetes is emerging as a potential cancer risk factor. A pooled analysis of over 771,000 individuals in the Asia Cohort Consortium study found that diabetes was associated with 26% increased risk of death from any cancer in Asians.52 Studies have revealed higher incidence of diabetes among South Asian populations,53 and further studies are required to ascertain the underlying biological mechanisms linking diabetes to cancer risk.
ANCCA members have proposed that certain country-specific risk factors, still warrant discussion and documentation to encourage further research and synthesis of evidence. For instance, aflatoxin may have a contributory role in up to one-third54 of all global hepatocellular carcinoma which is reported to be the third most common cause of cancer death in the Asia–Pacific region. Staples in many Asian diets consist of crops susceptible to fungal infection and aflatoxin accumulation. Food and water contaminants, such as nitrates and acrylamide, are potential carcinogens and have been linked to the development of breast and colorectal cancer.2 Use of charcoal for indoor cooking and heating is another example that is related to significant cancer burden in some Asian populations.2 These will be among factors to be further reviewed in line with the methodology of the World Code Against Cancer Framework during the process of developing a future ACAC.
As part of step 3 leading to step 4, evidence review for ACAC will be conducted, which will follow the methodology established by IARC/WHO as part of the World Code Against Cancer Framework, which includes a rigorous and validated process to review, assess and grade the latest evidence and assist experts to draw conclusions and formulate recommendations, taking into account contextual factors, communications strategies and enabling international policies. Systematic review of the published literature in Asia will be published in subsequent manuscripts in relation to development of ACAC.
Opportunities, challenges, strategies and future perspectives
To the best of our knowledge, this is the first overview on cancer prevention recommendations in developing codes against cancer in Asia. Our paper includes information, literatures, survey responses and input received from 21 countries in the region on their respective cancer burden, prevention, and control measures. For this overview, we conducted consultations and survey data extraction from ANCCA members who are focal points of respective national cancer centres or health agencies.
This collaboration amongst ANCCA members, the rigorous review of evidence, and the development of an ACAC will encourage more public health agencies, policymakers, clinicians, and cancer researchers to continue analysing the evidence to produce more specific cancer prevention recommendations that meet the needs of each region or country in Asia. Thus, ACAC will serve as a tool to facilitate and contribute to the United Nations Sustainable Development Goal 3 (SDG 3.4) in reducing premature mortality associated with NCDs, which is to counteract the rising burden due to NCDs, including cancer and its associated socioeconomic impact.55 There are a number of challenges and potential barriers which could affect the development and implementation of ACAC. The current ANCCA working group comprises policymakers, health administrators, epidemiologists, oncologists, and cancer researchers. For ACAC to represent the Asian populations, this working group will be expanded to include more countries outside of the current ANCCA membership, stakeholders beyond cancer treatment groups, experts on specific risk factor prevention, as well as consumers, and to collaborate with other cancer or NCD prevention networks.
Health inequalities across the Asian continent, which are also linked to the heterogeneity of cancer burden, economic development, health literacy and access to health services, have significant impact on the implementation of cancer prevention initiatives. Despite the potential challenges, the working group remains optimistic that there are opportunities and strengths identified even in resource constrained settings. Community participation, national programme compliance and bottom up initiatives have been reported in many settings in Asia.55
In addition to the differing distribution of cancer risk factors across sub-populations in Asian subregions, geopolitical and economic factors could potentially have an impact on the finalisation and implementation of ACAC. For instance, the ECAC is an initiative of the European Commission, developed by the IARC/WHO whereas there are several sub-regional Asian political bodies and economic bloc including ASEAN, WHO WPRO, WHO SEARO, SAARC and APEC. Effective collaboration among these networks and stakeholders will be key to ensuring a smoother progress towards ACAC.
A key public health strategy of the IARC/WHO has been to empower the public by providing necessary knowledge on common cancer-causing risk factors and behavioural changes to reduce cancer risk. This involves providing simple and easy-to-understand messages or recommendations (referred to as codes) which can be communicated rapidly to large and diverse target audiences.8 Having an ACAC, based on the World Code Against Cancer Framework adapted to the regional needs, will guide healthcare professionals and policymakers in strengthening the key aspects of primary and secondary prevention of cancer. Providing easy-to-understand messages, with illustrations, to schools or target high-risk groups, will enhance public awareness on cancer prevention from an early stage. Technology serves as an accelerator in the dissemination of information to raise awareness regarding cancer prevention. For instance, the National Cancer Center of China has published an easy-to-understand handbook with cartoon illustrations to raise awareness on primary prevention of cancer.56 They have also developed the Smart Health Management Digital Platform for Primary Cancer Prevention (SmartHMDP-PCP),57 to collect data on potential cancer risk factors longitudinally, provide individualised risk prediction and interventional feedback messages, and build databases for cancer research to identify optimal strategies for cancer prevention.
In addition to public health education, an ACAC will provide the groundwork for more elaborate cancer prevention tools such as the development of national policies and enactment of certain codes into law. Many effective preventive measures against diseases involve legal and fiscal methods. For instance, tobacco control laws in the WHO Framework Convention on Tobacco Control (FCTC) enable the creation of a smoke free healthy environment and prevention of lung cancer. In term of fiscal measures, innovative financing measures to encourage health enabling environment and reduce unhealthy behaviours included taxation on sugar sweetened beverages or carbon emissions. The ACAC will serve as a key reference from the region for policymakers in Asian countries to develop national codes against cancer and measures which may include introducing regulations to reduce the exposure to potential carcinogens in the environment. ANCCA members are currently at varying stages of development and implementation of cancer prevention and cancer control measures in their respective countries. It is anticipated that obtaining national authority approval for the endorsement of the ACAC may be a potentially long but necessary process. Nevertheless, ANCCA initiatives are expected to serve as a bridge as links are put in place with Ministry of Health (MoH) and other focal points participating in ANCCA. The MoHs play a pivotal role in aligning the national and regional cancer control strategies and taking a proactive role in allocating budget and resources for the conduct of scientific research on cancer risk factors and the formulation of healthcare policies on cancer prevention. With guidance from the World Code Against Cancer Framework, an IARC/WHO initiative, ANCCA will support the development of the governance for ACAC to establish the respective regional scientific committee and working groups of experts towards developing an ACAC. This will also include active promotion of ANCCA among new members in Asia through publications in scientific journals, national and international partnerships with the WHO, IARC/WHO and the Union for International Cancer Control (UICC) and through media, audio-visual formats, and social media.
In formulating an ACAC, future consultations and review will consider (i) having sub-regional chapters of ACAC, given the large and diverse population of the Asian region—the compilation of national recommendations conducted by this paper is crucial, as it highlights many similarities across the entire region, with some regional aspects; (ii) reaching out to other countries in Asia who are currently not ANCCA members yet, to participate in the development process of ACAC; and (iii) collaborating more closely with all relevant stakeholders, as development and implementation of ACAC require significant support from the political and health decision-makers, the medical and health agencies or associations, academics, researchers and experts in the development and implementation of cancer prevention and control measures. Effective cancer prevention recommendations are supported by scientific evidence. The evaluation of scientific evidence includes peer review, systematic review, documentation, classification of the strength of the evidence and rigorous decision-making based on expert consensus. Sociodemographic transitions over time may result in changing landscape of cancer risk factors. As new evidence emerges, codes or recommendations are to be reviewed on a regular basis and updated where necessary.
Conclusions
This paper is a status report on the current cancer prevention recommendations in Asia, with 21 countries participating in this first multinational ANCCA initiative. While few countries have comprehensive cancer recommendations (or national codes) and cancer control plans in place, many are still in the process of developing recommendations and will benefit from having structured and evidence-based approaches. It is hoped that all countries in Asia will benefit from working towards an ACAC which may have sub-regional sets of recommendations given the size of the Asian population and its diversity. Our review found that substantial cancer prevention strategies are already in place in many ANCCA member countries that can be integrated into the process of developing the ACAC according to the methodology of the World Code Against Cancer Framework of IARC/WHO. Multi-stakeholder collaboration between governments, policymakers, clinicians, and researchers, and the public is essential in the development and implementation of an ACAC. Rising cancer burden is a global challenge and the implementation of successful cancer prevention interventions benefits from international collaboration. An ACAC will be part of the IARC/WHO World Code Against Cancer Framework in the global fight against cancer.
Contributors
SKO, SKA, MI, and TM conceived and designed the study. SKO, SKA, GLGP, HJ, JK, LG, JSH, AS, CC, NSBIT, SNY actively participated in the working group consultations and contributed to drafting the manuscript. SKO, SKA, KT, YZ, SZK, CSP, MS, GNH, TTTH, KKP, SNY critically interpreted the findings. SKO, SKA, CC, KTs, TD, SS, EN, TB, JH, SWN, AR, JSI, EYP, MB, AY, CV, YYM, KKK, MSR, EF, SNY, NSBIT and BR contributed country specific data for Table 3. MTBJ created the infographic in consultation with lead authors. JS and CE critically appraised the manuscript, particularly on the methodological aspects. BS and WH advised and provided guidance for the study. All authors confirm that they had access to the data and accept responsibility to submit for publication. All authors agree to the submission and the final form of the manuscript.
Data sharing statement
Data from Asia–Global Cancer Observatory, GLOBOCAN Summary Statistics 2020 data published by International Agency for Research on Cancer is publicly available.
Declaration of interests
Where authors are identified as personnel of the International Agency for Research on Cancer/WHO and other organisations, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/WHO or respective organisations. HJ receives funding from Australian National Health and Medical Research Council ([NHMRC] GNT1163120, 2018–2023) and World Cancer Research Fund ([WCRF] IIG_FULL_2022_011, 2023–2025). This study was supported by the Japanese National Cancer Center Research and Development Fund (2022-A-21) provided to SKA. The funders had no role in study design, data collection, analysis, interpretation or writing of the report. The authors declare no other conflicts of interest.
Contributor Information
Sok King Ong, Email: sokking.ong@ubd.edu.bn.
Sarah K. Abe, Email: saabe@ncc.go.jp.
References
- 1.Ferlay J.E.M., Lam F., Colombet M., et al. Global cancer observatory: cancer today. 2020. https://gco.iarc.fr/today
- 2.Wild C.P., Weiderpass E., Stewart B.W. World cancer report: cancer research for cancer prevention. 2020. http://publications.iarc.fr/586 [PubMed]
- 3.Lin L., Li Z., Yan L., Liu Y., Yang H., Li H. Global, regional, and national cancer incidence and death for 29 cancer groups in 2019 and trends analysis of the global cancer burden, 1990-2019. J Hematol Oncol. 2021;14(1):197. doi: 10.1186/s13045-021-01213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seventieth World Health Assembly Cancer prevention and control in the context of an integrated approach. 2017. http://apps.who.int/gb/ebwha/pdf_files/WHA70/A70_R12-en.pdf
- 5.Espina C., Herrero R., Sankaranarayanan R., Krug E., Wild C.P., Schuz J. Toward the World Code Against Cancer. J Glob Oncol. 2018;4:1–8. doi: 10.1200/JGO.17.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO IARC . 2022. World Code Against Cancer Framework.https://cancer-code-world.iarc.who.int/wcac-framework/about/ Accessed April 20, 2022. [Google Scholar]
- 7.Schuz J., Espina C., Villain P., et al. European Code Against Cancer 4th edition: 12 ways to reduce your cancer risk. Cancer Epidemiol. 2015;39(Suppl 1):S1–S10. doi: 10.1016/j.canep.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Minozzi S., Armaroli P., Espina C., et al. European Code Against Cancer 4th Edition: process of reviewing the scientific evidence and revising the recommendations. Cancer Epidemiol. 2015;39(Suppl 1):S11–S19. doi: 10.1016/j.canep.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 9.WHO IARC . 2016. European Code Against Cancer scientific justification.https://cancer-code-europe.iarc.fr/index.php/en/scientific-justification Accessed July 24, 2022. [Google Scholar]
- 10.Gatellier L., Matsuda T., Sabapathy K., et al. An asian body to tackle cancers in Asia - the asian national cancer centers alliance. Asian Pac J Cancer Prev. 2020;21(5):1207–1212. doi: 10.31557/APJCP.2020.21.5.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madeeha M.R.Z.Z., Azhar H. Health literacy as a global public health concern: a systematic review. J Pharmacol Clin Res. 2017;4(2) [Google Scholar]
- 12.Sankaranarayanan R., Ramadas K., Qiao Y.L. Managing the changing burden of cancer in Asia. BMC Med. 2014;12:3. doi: 10.1186/1741-7015-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United Nations DoEaSA. Population Division . 2019. World population prospects 2019, Volume I: Comprehensive Tables (ST/ESA/SER.A/426) [Google Scholar]
- 14.Inoue M., Hirabayashi M., Abe S.K., et al. Burden of cancer attributable to modifiable factors in Japan in 2015. Glob Health Med. 2022;4(1):26–36. doi: 10.35772/ghm.2021.01037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen T.P., Luu H.N., Nguyen M.V.T., et al. Attributable causes of cancer in Vietnam. JCO Glob Oncol. 2020;6:195–204. doi: 10.1200/JGO.19.00239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang J.B., Jiang Y., Liang H., et al. Attributable causes of cancer in China. Ann Oncol. 2012;23(11):2983–2989. doi: 10.1093/annonc/mds139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korea NCC Attributable causes of cancer in Korea in the year. 2009. https://www.ncc.re.kr/sub07_Publications.ncc?isgubun=A&searchKey=title&searchValue=&pageNum=1
- 18.WHO IARC Monographs on the identification of carcinogenic hazards to humans. https://monographs.iarc.who.int/
- 19.GBD Diseases Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . 4th ed. World Health Organization; Geneva, Switzerland: 2021. WHO global report on trends in prevalence of tobacco use 2000-2025. [Google Scholar]
- 21.Azeem N., Sarfraz Z., Sarfraz A., Hange N., Sarfraz M., Cherrez-Ojeda I. Vaping and smokeless tobacco control in South Asia: a policy review. Ann Med Surg (Lond) 2022;81 doi: 10.1016/j.amsu.2022.104285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Asma S., Mackay J., Song S.Y., et al. The GATS atlas: global adult tobacco survey. 2015. http://gatsatlas.org/
- 23.Ma C.H.E., Li Z., Zhao M., Liang Y., Xi B. Global trends in the prevalence of secondhand smoke exposure among adolescents aged 12-16 years from 1999 to 2018: an analysis of repeated cross-sectional surveys. Lancet Glob Health. 2021;9(12):e1667–e1678. doi: 10.1016/S2214-109X(21)00365-X. [DOI] [PubMed] [Google Scholar]
- 24.ASEAN. UNITED WFP . UNICEF; Jakarta, Indonesia: 2022. ASEAN food and nutrition security report 2021, volume 1 and 2. [Google Scholar]
- 25.OECD . OECD Publishing; Paris, France: 2017. Daily vegetable eating among adults, 2015 (or nearest year) [Google Scholar]
- 26.Azeem S., Gillani S.W., Siddiqui A., Jandrajupalli S.B., Poh V., Syed Sulaiman S.A. Diet and colorectal cancer risk in asia--a systematic review. Asian Pac J Cancer Prev. 2015;16(13):5389–5396. doi: 10.7314/apjcp.2015.16.13.5389. [DOI] [PubMed] [Google Scholar]
- 27.Rumgay H., Shield K., Charvat H., et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22:1071–1080. doi: 10.1016/S1470-2045(21)00279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fritschi L. Future of work and occupational cancer. 2019. https://www.ilo.org/global/topics/safety-and-health-at-work/events-training/events-meetings/world-day-for-safety/33thinkpieces/WCMS_681591/lang--en/index.htm
- 29.Li N., Zhai Z., Zheng Y., et al. Association of 13 occupational carcinogens in patients with cancer, individually and collectively, 1990-2017. JAMA Netw Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aghaeipour F., Salehiniya H., Abbaszadeh H. Prevalence of human papillomavirus (HPV) in oral mucosal lesions in Iran: a systematic review and meta-analysis. J Med Virol. 2021;93(11):6089–6099. doi: 10.1002/jmv.27161. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y.T., Serrano B., Lee J.K., et al. Burden of Human papillomavirus (HPV)-related disease and potential impact of HPV vaccines in the Republic of Korea. Papillomavirus Res. 2019;7:26–42. doi: 10.1016/j.pvr.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang J., Cheng K., Wang Z. Prevalence and distribution of human papillomavirus genotypes in cervical intraepithelial neoplasia in China: a meta-analysis. Arch Gynecol Obstet. 2020;302(6):1329–1337. doi: 10.1007/s00404-020-05787-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li K., Li Q., Song L., Wang D., Yin R. The distribution and prevalence of human papillomavirus in women in mainland China. Cancer. 2019;125(7):1030–1037. doi: 10.1002/cncr.32003. [DOI] [PubMed] [Google Scholar]
- 34.Setiawan D., Luttjeboer J., Pouwels K.B., Wilschut J.C., Postma M.J. Immunogenicity and safety of human papillomavirus (HPV) vaccination in Asian populations from six countries: a meta-analysis. Jpn J Clin Oncol. 2017;47(3):265–276. doi: 10.1093/jjco/hyw192. [DOI] [PubMed] [Google Scholar]
- 35.Zhu K., Tian Y., Dong X., et al. The cost-effectiveness of bivalent, quadrivalent, and nine-valent HPV vaccination in Asia: a systematic review. Arch Gynecol Obstet. 2022;306(1):173–187. doi: 10.1007/s00404-021-06309-y. [DOI] [PubMed] [Google Scholar]
- 36.Hatamian S., Hadavandsiri F., Momenimovahed Z., Salehiniya H. Barriers and facilitators of colorectal cancer screening in Asia. Ecancermedicalscience. 2021;15:1285. doi: 10.3332/ecancer.2021.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chua B.M.V., Asjes C., Lim A., Mohseni M., Wee H.L. Barriers to and facilitators of cervical cancer screening among women in Southeast Asia: a systematic review. Int J Environ Res Public Health. 2021;18(9):4586. doi: 10.3390/ijerph18094586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu J.Y., Lee Y.C., Graham D.Y. The eradication of Helicobacter pylori to prevent gastric cancer: a critical appraisal. Expert Rev Gastroenterol Hepatol. 2019;13(1):17–24. doi: 10.1080/17474124.2019.1542299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ji X., He G., Wang K., Zhang Y., Yin J., Wang K. Estimation of gastric cancer burden attributable to Helicobacter pylori infection in Asia. J Public Health (Oxf) 2022;45(1):40–46. doi: 10.1093/pubmed/fdab410. [DOI] [PubMed] [Google Scholar]
- 40.Zhan B., Liu X., Li F., Zhang D. Breastfeeding and the incidence of endometrial cancer: a meta-analysis. Oncotarget. 2015;6(35):38398–38409. doi: 10.18632/oncotarget.5049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li D.P., Du C., Zhang Z.M., et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev. 2014;15(12):4829–4837. doi: 10.7314/apjcp.2014.15.12.4829. [DOI] [PubMed] [Google Scholar]
- 42.OECD/WHO . OECD Publishing; 2020. Health at a glance: asia/pacific 2020: measuring progress towards universal health coverage.https://www.oecd-ilibrary.org/sites/b2997366-en/index.html?itemId=/content/component/b2997366-en [Google Scholar]
- 43.WHO . 2014. Comprehensive implementation plan on maternal, infant and young child nutrition. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.GBD 2019 Cancer Risk Factors Collaborators The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400:563–591. doi: 10.1016/S0140-6736(22)01438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chung S.D., Lin Y.K., Huang C.C., Lin H.C. Increased risk of prostate cancer following sexually transmitted infection in an Asian population. Epidemiol Infect. 2013;141(12):2663–2670. doi: 10.1017/S0950268813000459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kitamura T., Suzuki M., Shigehara K., Fukuda K. Prevalence and risk factors of human papillomavirus infection among Japanese female people: a nationwide epidemiological survey by self-sampling. Asian Pac J Cancer Prev. 2021;22(6):1843–1849. doi: 10.31557/APJCP.2021.22.6.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shim E.J., Lee J.W., Cho J., et al. Association of depression and anxiety disorder with the risk of mortality in breast cancer: a National Health Insurance Service study in Korea. Breast Cancer Res Treat. 2020;179(2):491–498. doi: 10.1007/s10549-019-05479-3. [DOI] [PubMed] [Google Scholar]
- 48.Chen M.H., Tsai S., Su T.P., et al. Cancer risk in patients with bipolar disorder and unaffected siblings of such patients: a nationwide population-based study. Int J Cancer. 2022;150(10):1579–1586. doi: 10.1002/ijc.33914. [DOI] [PubMed] [Google Scholar]
- 49.Rahman T., Sahrmann J.M., Olsen M.A., et al. Risk of breast cancer with prolactin elevating antipsychotic drugs: an observational study of US women (ages 18-64 Years) J Clin Psychopharmacol. 2022;42(1):7–16. doi: 10.1097/JCP.0000000000001513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu Y., Ma L., Yang X., et al. Menopausal hormone replacement therapy and the risk of ovarian cancer: a meta-analysis. Front Endocrinol (Lausanne) 2019;10:801. doi: 10.3389/fendo.2019.00801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grant E.J., Brenner A., Sugiyama H., et al. Solid cancer incidence among the life span study of atomic bomb survivors: 1958-2009. Radiat Res. 2017;187(5):513–537. doi: 10.1667/RR14492.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen Y., Wu F., Saito E., et al. Association between type 2 diabetes and risk of cancer mortality: a pooled analysis of over 771,000 individuals in the Asia Cohort Consortium. Diabetologia. 2017;60:1022–1032. doi: 10.1007/s00125-017-4229-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Narayan K.M.V., Kondal D., Daya N., et al. Incidence and pathophysiology of diabetes in South Asian adults living in India and Pakistan compared with US blacks and whites. BMJ Open Diabetes Res Care. 2021;9(1) doi: 10.1136/bmjdrc-2020-001927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu Y., Wu F. Global burden of aflatoxin-induced hepatocellular carcinoma: a risk assessment. Environ Health Perspect. 2010;118(6):818–824. doi: 10.1289/ehp.0901388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nations U. 2015. UN General assembly, transforming our world : the 2030 Agenda for sustainable development. A/RES/70/1. [Google Scholar]
- 56.He J., Zhang Y. People’s Medical Publishing House; China: 2022. Education manual for primary prevention of cancer (in Chinese) [Google Scholar]
- 57.Huang H., Sun P.Y., Zou K.Y., He J., Zhang Y.W. Current status and prospects of primary prevention of cancer in China. Zhonghua Zhong Liu Za Zhi. 2022;44(9):942–949. doi: 10.3760/cma.j.cn112152-20220209-00083. [DOI] [PubMed] [Google Scholar]