Summary
Background
Cancer survival data from Population Based Cancer Registries (PBCR) reflect the average outcome of patients in the population, which is critical for cancer control efforts. Despite decreasing incidence rates, cervical cancer is the second most common female cancer in India, accounting for 10% of all female cancers. The objective of the study is to estimate the five-year survival of patients with cervical cancer diagnosed between 2012 and 2015 from the PBCRs in India.
Methods
A single primary incidence of cervical cancer cases of 11 PBCRs (2012–2015) was followed till June 30, 2021 (n = 5591). Active follow-ups were conducted through hospital visits, telephone calls, home or field visits, and public databases. Five-year Observed Survival (OS) and Age Standardised Relative Survival (ASRS) was calculated. OS was measured by age and clinical extent of disease for cervical cancers.
Findings
The five-year ASRS (95% CI) of cervical cancer was 51.7% (50.2%–53.3%). Ahmedabad urban (61.5%; 57.4%–65.4%) had a higher survival followed by Thiruvananthapuram (58.8%; 53.1%–64.3%) and Kollam (56.1%; 50.7%–61.3%). Tripura had the lowest overall survival rate (31.6%; 27.2%–36.1%). The five-year OS% for pooled PBCRs was 65.9%, 53.5%, and 18.0% for localised, regional, and distant metastasis, respectively.
Interpretation
We observed a wide variation in cervical cancer survival within India. The findings of this study would help the policymakers to identify and address inequities in the health system. We re-emphasise the importance of awareness, early detection, and increase the improvement of the health care system.
Funding
The National Cancer Registry Programme is funded through intra-mural funding by Indian Council of Medical Research, Department of Health Research, India, Ministry of Health & Family Welfare.
Keywords: Cervical cancer, India, Cervix survival, Disparity, Stage survival
Research in context.
Evidence before this study
Cervical cancer is the fourth most common cancer worldwide, and the second most common cancer among females in India. Cervical cancer is associated with prevalence of human papillomavirus and lower socioeconomic status. It currently accounts for about 10% of all female cancers, though the incidence is decreasing. The first population based survival study from Bangalore, India reported a 5-year cervical cancer suvival rate of 38.3%. A recent SurvCan-3 study reported a 5-year cervival cancer survival rate in India, ranging between 38.6% and 63.9%. These previous studies were from limited number of geographic areas. A larger and more disturbed updated population-based survival study on cervical cancer from India is helpful to assess the country's cervical cancer control efforts.
Added value of this study
This PBCS study from India compares survival from 11 different population based cancer registries (PBCR). In India, the overall pooled data of cervical cancer five-year survival was 51.7%. The survival rate of 11 PBCRs ranged from 31.6% in Tripura PBCR to 61.5% in Ahmedabad PBCR. The study found heterogeneity in cervical cancer survival across the country, with urban registries having higher survival than predominantly rural and northeastern registries. The results of this study demonstrated that cervical cancer survival rates have increased over time, but registry disparities have persisted. It also revealed that the 5-year survival rate of cervical cancer in India is lower than in high-income countries.
Implications of all the available evidence
The findings of this study would help policymakers to identify and address inequities in the health-care system. The effectiveness of the cervical cancer elimination programmes may be monitored with the help of PBCS studies conducted throughout the region and reporting changing survival over time.
Introduction
Cervical cancer ranks fourth in the world in terms of both incidence and mortality, while it ranks second in India.1 Despite decreasing incidence rates, cervical cancer is the second most common female cancer in India, accounting for 10% of all female cancers.2,3 Cervical cancer is linked to lower socioeconomic status and high human papillomavirus (HPV) prevalence.4 In India, infections with HPV types 16 and 18 are responsible for four out of every five cervical cancers reported.5, 6, 7
The National Cancer Registry Programme (NCRP) was established in 1981 by the Indian Council of Medical Research (ICMR) for the systematic collection of data on cancer through the population based cancer registries (PBCRs) and hospital-based cancer registries (HBCRs) in various parts of the country. Despite the systematic collection of incidence data, there is inadequate follow-up information on outcome of cancer patients registered by the PBCRs. Obtaining follow-up of cancer patients in India poses numerous challenges due to cancer not being a notified disease, lack of complete nationwide cause of death registration and its linkages with the registry. The Government of India has implemented screening for oral, breast, and cervical cancers throughout the country.8 India is committed to meeting the WHO’s target of eliminating cervical cancer.9 Population based survival data are used to assess the efficiency and effectiveness of cancer diagnostic, treatment and follow-up services in the region. In 2017, the study on Population Based Cancer Survival (PBCS) on breast (females), cervical, and head and neck cancers in India was launched across 25 PBCR under NCRP. Currently, this study reports cervical cancer survival statistics from 11 PBCRs under NCRP in various parts of the country. The outcomes will aid in determining the existing situation and future assessment in improving cervical cancer survival in India.
PBCR and its survival are representative of the population covered and critical for cancer control efforts. PBCS calculates the average survival rate of cancer patients in a specific geographic area. In general, many factors influence cancer survival, including type of cancer, time of diagnosis, gender, stage of disease, and treatment. It measures cancer control activities in the region and provides overall efficiency of cancer health care services.10 The global survival range for cervical cancer remains wide (50–70%).11 India had a five-year Age Standardised Relative Survival (ASRS) rate of 46% for those patients diagnosed between 1990 and 2001.12 According to our knowledge, the first PBCS study was published in India in 1995, followed by several individual registry and international collaboration publications.13, 14, 15, 16, 17, 18 In comparison to earlier studies, this study involves a larger population and a higher number of PBCRs. It is crucial to assess India's cervical cancer survival rate and pattern due to the heterogeneity in cancer incidence and pattern.2
The study aimed to estimate the five-year survival of patients with cervical cancer diagnosed between 2012 and 2015 in India from PBCRs under NCRP and, to estimate five-year overall survival based on age and clinical extent of disease.
Methods
Study population
There are currently 38 PBCRs functioning under NCRP. The NCRP 2020 report included cancer incidence and mortality data from 28 PBCRs and of which 25 PBCRs agreed to take part in this study for cervical cancer cases diagnosed between 2012 and 2015.19 The survival analysis was taken up on cervical cancer data from PBCRs, with a follow-up rate of at least 70% among total cases. Eleven PBCRs had follow-up information for at least 70% of their respective patients as of June 30, 2021, and were taken up for analysis and reporting. The incidence of cancer with a behavior code 3 defined by the International Classification of Diseases for Oncology, 3rd Edition and the International Statistical Classification of Diseases and Related Health Problems (10th revision; ICD-10) of the cervical cancer (ICD10: C53) of single primary cases was included in this study.20 During this time period, 22 (0.4%) of the 5591 cases reported apart from first primary cancer were also included. However, the earliest primary cancer in these patients were not reported during this time period. From 2012 to 2015, a single primary incidence of cervical cancer cases from 11 PBCRs (Kollam, Thiruvananthapuram, Mumbai [2012–2014], Wardha, Ahmedabad urban, Kamrup urban, Manipur, Mizoram, Sikkim, Tripura, and Pasighat) was followed until June 30, 2021 (n = 5591). Individuals were right-censored at the time they were lost to follow-up or the cut-off date. Manipur, Mizoram, Sikkim, and Tripura PBCRs cover the entire state population (Appendix 1).
Data collection process
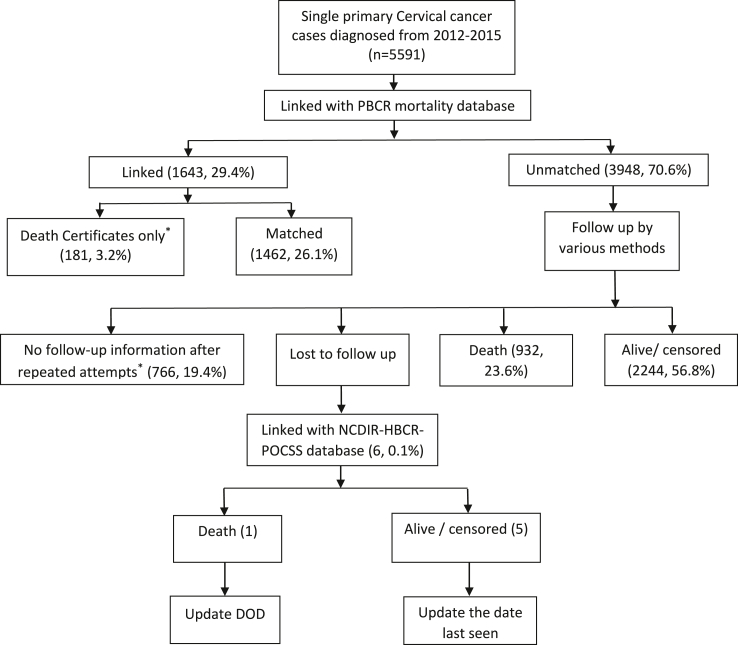
In India, cancer is not a nationally notifiable disease. To collect data on a standardised core form, trained registry staff visits various sources such as hospitals, diagnostic labs, vital registration to register cancer cases. Unlike incidence, the mortality data collection is incomplete in cancer registries due to incomplete or incorrect certification of cause of death. In addition to the normal operations of PBCR, this PBCS study focused on the follow-up of cancer patients to update their vital status (dead or alive). The registered cancer cases were mostly tracked using active methods on a yearly basis. Following up and updating the patient's vital status were done by registry-trained staff. First, the registry collected death records from the mortality registration system or municipal corporation and other active procedures as well. To update the date of death (DOD), mortality (including all-cause) cases were matched with incidence records (based on name, address, ICD-10, etc). This mortality database was termed as PBCR mortality database. Second, unmatched cases were actively pursued through PBCS study by contacting registration or collaborating hospital departments, telephone calls, home or field visits, and public databases (voter list or insurance). At each interval, attempts were made again to obtain the vital status for the cases that lost to follow-up cases and follow-back of Death Certificate Only (DCO) cases. To update the vital status of the remaining cases (no or unknown follow-up), they were linked with the NCDIR-NCRP database of Hospital Based Cancer Registry (HBCR)–Pattern of Care and Survival Studies (POCSS) (Fig. 1).
Fig. 1.
Outline of the Population Based Cancer Survival study under National Cancer Registry Programme (NCRP). ∗Excluded in survival study. DOD, date of death; NCDIR, National Centre for Disease Informatics; HBCR, Hospital Based Cancer Registry; POCSS, Patterns of Cancer Care and Survival Study.
Instrumentation or measures
The PBCS form was created as a software module that was deployed to each PBCR for uniform data entry. NCDIR held regular training and review meetings with the PBCRs team. Data quality indices such as the proportion of microscopically verified (MV%), DCO, no or unknown follow-up%, and quality control checks (consistency, range, duplicate, incompatible date, invalid date) were performed. Each clarification, as well as unknown or insufficient follow-up, was communicated to PBCRs for updation. The survival analysis excluded cases with a DCO and those with no or unknown follow-up.
Data analysis
The difference between the date of first diagnosis (DFD) and the DOD (any cause of death) or loss to follow-up or censoring is used to compute survival time (closing date). Observed Survival (OS) was estimated using the actuarial survival method.21 It was assumed that the individuals who were lost to follow-up were not severely ill or died. Relative survival is the ratio of cancer patients' OS to the expected survival of a comparable group of the general population. The Ederer-II method was used to estimate expected survival based on the general population mortality experience of India's life table from the UN.22,23 ASRS estimates are the weighted average of age-specific relative survival and the standard population (age distribution of cancer patients from NCRP [2012–2016], India).19,24 The vital status distribution and pattern of lost to follow-up statistics are computed. Survival analysis was performed for each PBCR as well as by clinical extent of disease. Pooled survival estimates were calculated by combining all 11 PBCRs. Survival analyses were not performed for groups (age or stage) with less than 25 observations. The Age Adjusted Rate (AAR) per 100,000 population was calculated using the world standard population.25 Commands "ltable," and "strs" in STATA 14 were used for the survival analysis. This study was approved by the Institutional Ethics Committee (Ref: NCDIR/IEC/2017/7). Prior to the study, each PBCRs obtained Institutional Ethical Clearances.
Role of the funding source
The funders had no role in the design, data collection, analysis of the study, nor the decision to publish or prepare this manuscript.
Results
Table 1 details on the population, the total number of cervical cancer cases, and data quality indicators for the years 2012–2015 are provided. In total, 11 PBCRs contributed to (n = 5591) cervical cancer cases. Mumbai (1531) and Ahmedabad urban (817) PBCRs contributed most of the cases. The median age at diagnosis ranged from 45 (Pasighat) to 60 (Thiruvananthapuram) years. MV% exceeded 85.0% in each PBCRs with the exception of Wardha (78.4%). The overall DCO% was 3.2%, with Wardha having the highest (20.4%). In 8 PBCRs, the percentage of unknown follow-up was less than 20.0%. Mizoram had the highest (AAR per 100,000 population) of 23.3, followed by Pasighat (20.1), and Manipur had the lowest incidence rate of 6.4.
Table 1.
Estimated population, total number of cervical cancer cases and data quality indices for the years 2012–2015.
| Population |
Total cases | Median age | AAR | MV |
Excluded cases (Number, %) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Urbana (%) | Rurala (%) | Number (%) | DCOs (%) | Follow-up Unk (%) | Total number (%) | ||||
| PBCR | ||||||||||
| Kollam | 5,615,045 | 45.0 | 55.0 | 514 | 60 | 6.8 | 456 (88.7) | 0 (0.0) | 7 (1.4) | 7 (1.4) |
| Thiruvananthapuram | 6,943,052 | 53.7 | 46.3 | 624 | 60 | 6.7 | 578 (92.6) | 0 (0.0) | 60 (9.6) | 60 (9.6) |
| Mumbaib | 17,447,872 | 100.0 | 0.0 | 1531 | 55 | 8.7 | 1345 (87.9) | 103 (6.7) | 301 (19.7) | 404 (26.4) |
| Wardha | 25,70,309 | 32.5 | 67.5 | 245 | 55 | 8.5 | 192 (78.4) | 50 (20.4) | 14 (5.7) | 64 (26.1) |
| Ahmedabad urban | 11,626,485 | 100.0 | 0.0 | 817 | 50 | 7.1 | 778 (95.2) | 4 (0.5) | 87 (10.6) | 91 (11.1) |
| Kamrup urban | 2,499,807 | 100.0 | 0.0 | 316 | 53 | 14.2 | 295 (93.4) | 14 (4.4) | 33 (10.4) | 47 (14.9) |
| Manipur | 6,139,804 | 29.2 | 70.8 | 322 | 53 | 6.4 | 310 (96.3) | 3 (0.9) | 27 (8.4) | 30 (9.3) |
| Mizoram | 2,315,829 | 52.1 | 47.9 | 455 | 46 | 23.3 | 430 (94.5) | 7 (1.5) | 103 (22.6) | 110 (24.2) |
| Sikkim | 1,193,426 | 25.2 | 74.8 | 95 | 51 | 10.4 | 95 (100.0) | 0 (0.0) | 25 (26.3) | 25 (26.3) |
| Tripura | 7,500,573 | 26.2 | 73.8 | 627 | 50 | 9.3 | 614 (97.9) | 0 (0.0) | 97 (15.5) | 97 (15.5) |
| Pasighat | 1,194,944 | 25.4 | 74.6 | 45 | 45 | 20.1 | 45 (100.0) | 0 (0.0) | 12 (26.7) | 12 (26.7) |
| India (Pooled) | 65,047,146 | 5591 | 54 | 5138 (91.9) | 181 (3.2) | 766 (13.7) | 947 (16.9) | |||
MV, microscopic verification; DCO, death certificate only; Unk, unknown.
As per 2011 Census.
Year of Diagnosis-2012–2014.
Table 2 shows the number and proportions (%) of cervical cancer cases with vital status and the pattern of follow-up from 2012 to 2015. In total, 83.1% (n = 4644) of the cases were included in the survival analysis. Kollam had the highest percentage of inclusion (98.6%), while Pasighat PBCR had the lowest (73.3%). During the 5-year follow-up period, 68.1% and 41.0% of patients died in Tripura (high) and Ahmedabad urban (low), respectively. Except for Thiruvananthapuram and Kamrup urban, all PBCRs had more than 90% of five-year follow-ups. During the first three years, 1.6% of patients were lost to follow-up.
Table 2.
Number and proportions (%) of cervical cancer cases with vital status and pattern of follow-up for the years 2012–2015.
| Included cases | Deaths within 5 years of diagnosis |
Alive 5-years from diagnosis |
Complete follow-up (upto 5 years)a | Incomplete follow-up (Lost to follow-up) |
|||
|---|---|---|---|---|---|---|---|
| Number (%) | |||||||
| Number (%) | Number (%) | <1 year | 1–3 year | 3–5 year | |||
| PBCR | |||||||
| Kollam | 507 (98.6) | 258 (50.9) | 247 (48.7) | 99.6 | 0 | 0 | 2 |
| Thiruvananthapuram | 564 (90.4) | 250 (44.3) | 221 (39.2) | 83.5 | 19 | 20 | 54 |
| Mumbai | 1127 (73.6) | 572 (50.8) | 468 (41.5) | 92.3 | 0 | 5 | 82 |
| Wardha | 181 (73.9) | 108 (59.7) | 65 (35.9) | 95.6 | 0 | 0 | 8 |
| Ahmedabad urban | 726 (88.9) | 298 (41.0) | 405 (55.8) | 96.8 | 13 | 7 | 3 |
| Kamrup urban | 269 (85.1) | 159 (59.1) | 75 (27.9) | 87.0 | 2 | 4 | 29 |
| Manipur | 292 (90.7) | 169 (57.9) | 123 (42.1) | 100.0 | 0 | 0 | 0 |
| Mizoram | 345 (75.8) | 165 (47.8) | 178 (51.6) | 99.4 | 0 | 0 | 2 |
| Sikkim | 70 (73.7) | 37 (52.9) | 30 (42.9) | 95.7 | 0 | 0 | 3 |
| Tripura | 530 (84.5) | 361 (68.1) | 120 (22.6) | 90.8 | 2 | 0 | 47 |
| Pasighat | 33 (73.3) | 18 (54.5) | 14 (42.4) | 97.0 | 0 | 0 | 1 |
| India (Pooled) | 4644 (83.1) | 2395 (51.6) | 1946 (41.9) | 93.5 | 36 (0.8) | 36 (0.8) | 231 (5.0) |
Calculated from the total included cases.
Table 3 displayed the five-year OS% (95% CI) of Cervical cancer across the 11 PBCRs. OS% of 1-year, 3-year, and 5-year pooled data was 77.8%, 57.0%, and 47.6%. The absolute difference between 1-year and 5-year survival is 30.2%. For Ahmedabad urban, the 1-year, 3-year, and 5-year OS% were higher being 84.0%, 66.5%, and 58.1%, respectively. The 5-year OS% in Ahmedabad urban was higher (58.1%), followed by Thiruvananthapuram (53.2%) and Mizoram (52.2%). Tripura has lower 3-year and 5-year survival rates of 43.4% and 30.8%, respectively.
Table 3.
Observed Survival (with 95% CI) for cervical cancer across the 11 Population Based Cancer Registries (PBCRs) for the years 2012–2015.
| Observed survival (95% CI) for cervical cancer cases |
|||
|---|---|---|---|
| 1 year | 3 year | 5 year | |
| PBCR | |||
| Kollam | 80.7 (77.0–83.9) | 60.2 (55.8–64.3) | 49.1 (44.7–53.4) |
| Thiruvananthapuram | 81.1 (77.6–84.1) | 59.5 (55.2–63.5) | 53.2 (48.8–57.4) |
| Mumbai | 71.4 (68.7–74.0) | 56.1 (53.1–58.9) | 48.9 (46.0–51.8) |
| Wardha | 74.6 (67.6–80.3) | 49.7 (42.3–56.8) | 39.9 (32.7–47.0) |
| Ahmedabad urban | 84.0 (81.1–86.5) | 66.5 (62.9–69.8) | 58.1 (54.4–61.6) |
| Kamrup urban | 79.5 (74.1–83.8) | 50.0 (43.8–55.8) | 39.3 (33.3–45.2) |
| Manipur | 82.5 (77.7–86.4) | 57.5 (51.7–63.0) | 42.1 (36.4–47.7) |
| Mizoram | 80.9 (76.3–84.6) | 61.5 (56.1–66.4) | 52.2 (46.8–57.3) |
| Sikkim | 74.3 (62.3–83.0) | 54.3 (42.0–65.1) | 47.0 (35.0–58.1) |
| Tripura | 73.4 (69.4–76.9) | 43.4 (39.1–47.6) | 30.8 (26.8–34.8) |
| Pasighat | 72.7 (54.1–84.8) | 54.6 (36.3–69.6) | 45.3 (28.0–61.1) |
| India (Pooled) | 77.8 (76.6–79.0) | 57.0 (55.5–58.4) | 47.6 (46.2–49.1) |
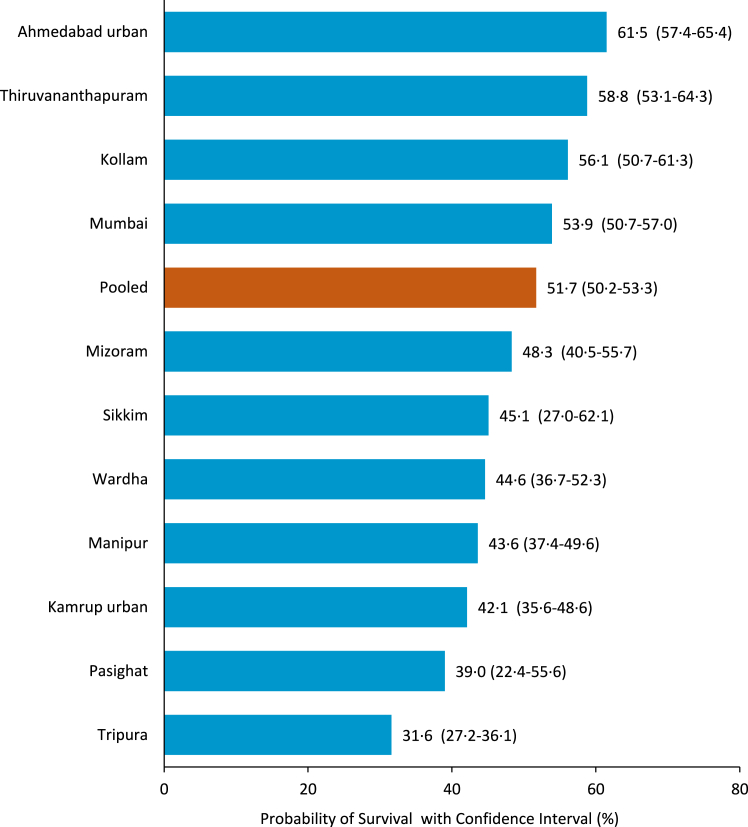
Fig. 2 describes the five-year ASRS by cervical cancer across the 11 PBCRs. The overall pooled data of the cervical cancer survival was 51.7%. Ahmedabad urban had the highest 5-year ASRS (61.5%), followed by Thiruvananthapuram (58.8%) and Kollam (56.1%). Survival rates were lower in Tripura (31.6%) and Pasighat (39.0%). The survival rate in the North East (NE) region and Wardha PBCR was less than 50%.
Fig. 2.
Five-year Age Standardised Relative Survival (ASRS) with Confidence Interval (95% CI) for cervical cancer across the 11 PBCRs for the years2012–2015.
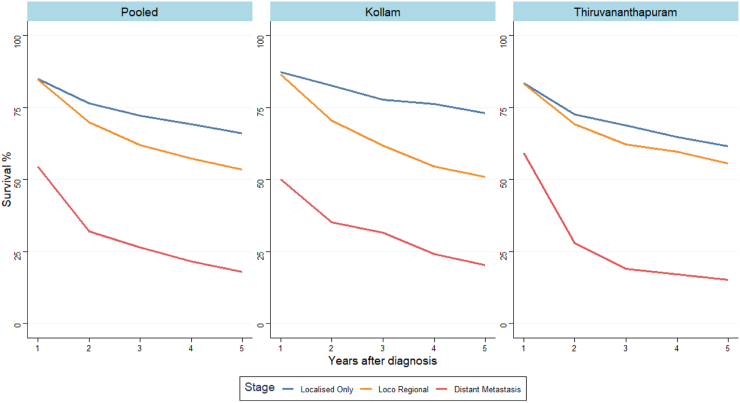
Fig. 3 depicted the OS (%) for cervical cancers based on clinical extent of disease. The five-year OS% for pooled PBCRs was 65.9, 53.5, 18.0 for localized, regional, and distant metastasis, respectively. The one-year survival rate for distant metastasis was 54.5%, falling to 18.0% after five years. The stage-wise survival was only conducted for Kollam and Thiruvananthapuram based on the quality and completeness of the data. Kollam PBCR five-year OS% was (73.0, 50.8, 20.4) for localised, regional, and distant metastasis, respectively. Thiruvananthapuram PBCR five-year OS% was 61.5, 55.6 and 15.3 for localised, regional, and distant metastasis, respectively.
Fig. 3.
Observed survival (OS) by clinical extent of disease for cervical cancer across the PBCRs for the year 2012–2015. Note: Pooled from Kollam and Thiruvananthapuram.
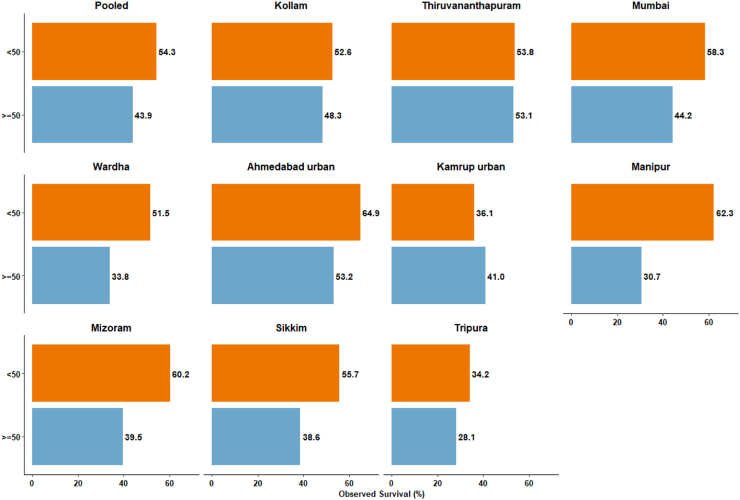
Fig. 4 describes the Five-year OS% by age group (<50, ≥50) for cervical cancer across the 11 PBCRs. The pooled five-year OS% were 54.3% and 43.9% for those younger than 50 and older than or equal to 50 at the time of diagnosis, respectively. Ahmedabad urban had the highest rate of survival (64.9%), followed by Manipur (62.3%) in people under the age of 50. Tripura had the lowest survival rates at both ages (34.2% and 28.1%). Among PBCRs from NE region, Kamrup urban had a higher survival rate in those over 50 (41.0%) but a lower survival rate in those under 50 (36.1%). The 5-year survival rate in Thiruvananthapuram is similar for both age groups (53.8% and 53.1%). When compared to other PBCRs, the difference in 5-year survival between 50 and ≥50 years of age was substantial in Manipur.
Fig. 4.
Five-year Observed survival (OS) by age group for cervical cancer across the 11 PBCRs for the year 2012–2015. Note: Pooled from 11 PBCRs.
Appendix 2 shows the number and proportions (%) of cervical cancer deaths and patterns of follow-up for the years 2012–2015. Among the death cases, 42.8% died within a year and 40.0% died within the next 1–3 years. Appendix 3 summarises the number and proportions of cervical cancer follow-up methods used across the 11 PBCRs from 2012 to 2015. Patients were contacted several times to update their vital status. The telephone method (30.8%) was preferred, followed by linking with a PBCR mortality database (26.1%).
Discussion
This is the largest population level comparative survival study on cervical cancer from India. It covers 65 million person-years female population in India from various geographical regions. The analysis of survival included 83.1% of the 5591 cases of cervical cancer. More than 90% of the cases in Kollam, Thiruvananthapuram and Manipur were included. PBCRs tried to ascertain the patient’s vital status using a variety of techniques, and higher proportion of the patients had five-year follow up. Overall, MV accounted for 91.9% of cases, with DCO accounting for 3.2%. Though both urban and rural PBCRs in India showed a declining trend in cervical cancer incidence, the estimated incidence rate for cervical cancer in 2020 was 10.9 per 100,000.2 Concurrently, the five-year survival rate for cervical cancer is 51.7%.
Survival was low in the NE region, particularly in PBCRs in Tripura, Pasighat, and Kamrup urban. This region's survival rate was lower than the national or pooled average. Furthermore, a hospital-based survival study from the NE region revealed a lower 5-year overall survival rate of 40.7% (all stages) with early stage (47.7%) and advanced stage (29.4%).26 In comparison to urban PBCRs (Ahmedabad, Mumbai), the Wardha PBCR population, which is predominantly rural, had a lower rate of survival. In south India, a similar result was observed in a rural district vs an urban district.18 The cervical cancer survival in India was comparable with other WHO South-East Asia Region (SEAR) countries like Thailand and Indonesia (Appendix 4).11,17 NE region has lacked health care infrastructure, treatment facilities, and human resources.27 The access to diagnostic and effective treatment services has varied across the populations. This could explain the disparity in survival rates across the population. The metro cities of Mumbai and Ahmedabad had much better access to diagnostic and therapeutic services than the NE region. Major sources of secondary and tertiary level hospitals were limited (≤5) in these PBCRs (Tripura, Pasighat, Manipur, Sikkim, Mizoram, and Wardha) and considerably high (≥10) in Thiruvananthapuram, Kollam, Ahmedabad urban, Kamrup urban, and Mumbai.19 Distance from a clinical care facility, travel costs, co-morbidity, and poverty all increase the likelihood of not undergoing a follow-up examination and completing treatment, resulting in lower survival.17
Similar statistical methods and study design are employed in our study as done in SurvCan. This study presented a 5-year ASRS for selected PBCRs in India from 1991 to 1999.17 In India, the comparison of SurvCan and the current study revealed an increase in cervical cancer survival (46.0% vs 51.7%). Bangalore PBCR reported a 5-year relative survival rate of 46.3% from 1987 to 1989.10 The survival rate of patients diagnosed between 1982 and 1986 in the Mumbai PBCR was 47.7%, and it gradually decreased as the clinical extent of the disease increased.15 A higher 5-year survival rate of 54.0% was recorded in Chennai between 1990 and 1999.18 The first survival study from Bangalore reported a 5-year survival rate of 38.3% (1982–1989).13 Appendix 5 contains survival information on previous studies conducted in India. Although the survival rate for individual PBCRs has improved since previous studies (Kollam & Mumbai), disparities between PBCRs remain. CONCORD-3 study estimated cervical cancer 5-year survival as 59.0% based on two PBCRs from India.11 Nonetheless, survival rates in India are lower than in high-income countries. In the United States, the 5-year survival rate for cervical cancer was 66.7%.28
Cancer stage was a significant predictor of survival. As in previous studies, an inverse relationship between survival probability and clinical extent of disease or stage was observed.13,14,17 For localized, regional, and distant metastasis, the five-year OS% for India (SurvCan) was 73.2, 47.2 and 7.4, respectively.12 Our study found that regional (53.5%) and distant metastasis (18.0%) stages had slightly higher survival rates. However, stage misclassification due to incomplete or inaccurate documentation cannot be ruled out. In the United States, the higher five-year OS% was observed for localized, regional, and distant metastasis (91.8, 59.4, 17.1).28 In total, 9.6% of cases were missing stage information. Due to the small number of samples and limitations in the misclassification of clinical extent of the disease, the remaining PBCRs were not analysed. The findings from south India revealed that individuals with lower levels of education are more likely to be diagnosed with advanced cancer and have shorter survival.29 Several studies from India revealed that people with early stage cancer detected through screening had a higher chance of survival.30, 31, 32 The Health Technology Assessment of Strategies for Cervical Cancer Screening in India concluded that visual inspection with acetic acid is the most cost-effective screening method and reduces treatment costs.33 A collaborative approach to implementing state-wide cervical cancer control and HPV vaccination will yield effective result.34 National Technical Advisory Group for Immunization (NTAGI) has recommended introduction of HPV Vaccine in the Universal Immunization Programme (UIP) with a one-time catch-up for 9–14 year-old adolescent girls followed with routine introduction at 9 years.35 To improve survival, it is essential to increase screening and early detection of cervical cancer. To eliminate cervical cancer by 2030, ensure that 90% of girls are fully vaccinated with HPV vaccine, 70% of women are screened using a high-performance test by 35 years of age, and again by 45 years of age and 90% of women identified with cervical disease get treated.9 The effectiveness of the screening and management of cases will get reflected as an improvement in the survival of the patients. Therefore, expanding PBCS studies across the region and reporting survival over time aids in monitoring the effectiveness of the cervical cancer elimination programme.
The main strength of this study is the analysis of large volume of quality data. The incidence data was processed in accordance with International Association of Cancer Registries or International Agency for Research on Cancer standards and published in CI-5 volumes and the NCRP report.36 Patients were actively followed-up, and 5-year follow-up was available for 93.5% of the patients. In low-income and middle-income countries, this method would produce more reliable cancer survival estimates than the passive method.37 The main limitation of the study is six of the 11 PBCRs from the NE region of four states, with the remaining four PBCRs from Kerala and Maharashtra state. It might limit the generalizability of the results for India. Around 17% of cases were excluded. This could potentially bias survival (upward or downward) across the PBCRs and should be considered when interpreting the results. The Kollam PBCR had the least bias, with an exclusion of 1.4%, while Mumbai, Wardha, Sikkim, and Pasighat had exclusion of around 26% cases. In this study, various methods of follow-up were used to obtain the vital status. The accuracy of survival estimation is dependent on the accuracy and completeness of the public or mortality database. In this study, no imputation techniques were used to address missing data. It is also limited by a lack of data on treatment status, socioeconomic status, comorbidities, and stage information, all of which are important contributors to cancer survival. The considerable diversity in lifestyle across the Indian population, coupled with disparities in healthcare resource accessibility in both urban and rural settings, significantly influences cervical cancer survival rates. The PBCRs, encompassing both urban and rural demographics, were not segregated for separate analysis due to inaccuracies in coding urban and rural designations.
A good quality PBCR data would be comparable, valid, complete, and timely.38,39 It is essential for accurate and reliable cancer surveillance, research, and policy formulation. It is crucial in improving cancer early detection, survival rates, and disparities. Missing or inadequate data from PBCRs in demographics, stage, and treatment limit cancer research and public health planning. Efforts are being made to address the missing data by providing continuous education and training to the registries, as well as revising the questionnaire. Registries should devise a strategy for collecting missing data from healthcare providers and connecting it to other health and administrative databases.
In conclusion, we observed the disparity in cervical cancer survival within India. The disparity in survival between the populations could explain the overall effectiveness of the health care system. This informs the policymakers to identify and address inequities in the health system. The population-based survival study should be expanded and continued to assess cancer survival trends as well as the impact of cancer control activities such as screening programme. We emphasise the importance of promoting awareness, early detection, and improving the health-care system.
Contributors
PM: Conceptualisation, supervision, writing review & editing. KS: Conceptualisation, data curation, formal analysis, visualisation, writing original draft. JS: Formal analysis, writing original draft. AM, RAN, NG, SK, DB, SP, GM, VD, EZ, TWB, KJ, PSG, SM, RL, AS, SD, SK, LP, PDP, GJ: Data curation, validation, writing review & editing. MC: Data curation, writing review & editing. PD: Software, writing review & editing. All authors agreed with the final version of the manuscript.
Data sharing statement
De-identified data collected for this study are available upon a reasonable request over email to the corresponding author.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None. The National Cancer Registry Programme is funded through intra-mural funding by Indian Council of Medical Research, Department of Health Research, Ministry of Health & Family Welfare.
Acknowledgements
The authors acknowledge the contribution of the Population Based Cancer Registries under the National Cancer Registry Programme contributed data.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100296.
Appendix A. Supplementary data
References
- 1.Ferlay J., Ervik M., Lam F., et al. International Agency for Research on Cancer; Lyon, France: 2020. Global cancer observatory: cancer today.https://gco.iarc.fr/today [cited 2022 August 5]. Available from: [Google Scholar]
- 2.Mathur P., Sathishkumar K., Chaturvedi M., et al. Cancer statistics, 2020: report from National Cancer Registry Programme, India. JCO Glob Oncol. 2020;6:1063–1075. doi: 10.1200/go.20.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kulothungan V., Sathishkumar K., Leburu S., et al. Burden of cancers in India: estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on National Cancer Registry Program. BMC Cancer. 2022;22:527. doi: 10.1186/s12885-022-09578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sankaranarayanan R., Ramadas K. In: Socioeconomic factors and cancer prevention in India. Wild C.P., Weiderpass E., Stewart B.W., editors. IARC Scientific Publications; Lyon, France: 2020. World cancer report 2020. Cancer research for cancer prevention; pp. 258–265. [Google Scholar]
- 5.Basu P., Roychowdhury S., Bafna U.D., et al. Human papillomavirus genotype distribution in cervical cancer in India: results from a multi-center study. Asian Pac J Cancer Prev. 2009;10(1):27–34. [PubMed] [Google Scholar]
- 6.Senapati R., Nayak B., Kar S.K., Dwibedi B. HPV genotypes distribution in Indian women with and without cervical carcinoma: implication for HPV vaccination program in Odisha, Eastern India. BMC Infect Dis. 2017;17(1):30. doi: 10.1186/s12879-016-2136-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramamoorthy T., Sathishkumar K., Das P., Lakshminarayana S.K., Mathur P. Epidemiology of human papillomavirus related cancers in India: findings from the National Cancer Registry Programme. ecancer. 2022;16:1444. doi: 10.3332/ecancer.2022.1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of Health and Family Welfare, Government of India . 2022. National Programme for prevention & control of cancer, diabetes, cardiovascular diseases & stroke (NPCDCS): National Health Mission.https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604 [cited 2022 September 24]. Available from: [Google Scholar]
- 9.Global strategy towards the elimination of cervical cancer as a public health problem. Word Health Organization; Geneva: 2020. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 10.Jensen O.M., Parkin D.M., MacLennan R., Muir C.S., Skeet R.G., editors. Cancer registration: principles and methods. No. 95. IARC Scientific Publications; Lyon, France: 1991. pp. 1–288. [Google Scholar]
- 11.Allemani C., Matsuda T., Di Carlo V., et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075. doi: 10.1016/s0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sankaranarayanan R., Swaminathan R., Brenner H., et al. Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol. 2010;11:165–173. doi: 10.1016/s1470-2045(09)70335-3. [DOI] [PubMed] [Google Scholar]
- 13.Nandakumar A., Anantha N., Venugopal T.C. Incidence, mortality and survival in cancer of the cervix in Bangalore, India. Br J Cancer. 1995;71(6):1348–1352. doi: 10.1038/bjc.1995.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sankaranarayanan R., Black R.J., Swaminathan R., Parkin D.M. In: Cancer survival in developing countries. Sankaranarayanan R., Black R.J., Parkin D.M., editors. Vol. 145. IARC Sci Publ.; 1998. An overview of cancer survival in developing countries; pp. 135–173. [PubMed] [Google Scholar]
- 15.Yeole B.B., Sankaranarayanan R., Jussawalla D.J. Long-term survival from uterine cervical cancer in Mumbai (Bombay), India. Int J Cancer. 1998;78(3):394–395. doi: 10.1002/(sici)1097-0215(19981029)78:3%3C394::aid-ijc25%3E3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 16.Yeole B.B., Kumar A.V., Kurkureet A., Sunny L. Population-based survival from cancers of breast, cervix and ovary in women in Mumbai. Asian Pac J Cancer Prev. 2004;5(3):308–315. http://journal.waocp.org/article_24274_285b6b99fbc4962837b2d27f7f4e5852.pdf [PubMed] [Google Scholar]
- 17.Sankaranarayanan R., Swaminathan R., World Health Organization, International Agency for Research on Cancer, editors. Cancer survival in Africa, Asia, the Caribbean and Central America. International Agency for Research on Cancer, World Health Organization; IARC Scientific Publications; Lyon, France: 2011. p. 291. [Google Scholar]
- 18.Swaminathan R., Selvakumaran R., Esmy O.P., et al. Cancer pattern and survival in a rural district in South India. Cancer Epidemiol. 2009;33(5):325–331. doi: 10.1016/j.canep.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 19.ICMR-National Centre for Disease Informatics and Research (ICMR-NCDIR) ICMR-NCDIR; 2020. Report of National Cancer Registry Programme 2020. Bengaluru (India)https://ncdirindia.org/All_Reports/Report_2020/default.aspx Available from: [Google Scholar]
- 20.World Health Organization (WHO) WHO; Geneva (Switzerland): 1994. International statistical classification of diseases and related health problems. [Google Scholar]
- 21.Cutler S.J., Ederer F. Maximum utilization of the life table method in analysing survival. J Chron Dis. 1958;8:699–712. doi: 10.1016/0021-9681(58)90126-7. [DOI] [PubMed] [Google Scholar]
- 22.Ederer F., Axtell L.M., Cutler S.J. The relative survival rate: a statistical methodology. Natl Cancer Inst Monogr. 1961;6:101–121. [PubMed] [Google Scholar]
- 23.United Nations, Department of Economic and Social Affairs, Population Division . 2022. World population prospects 2022: methodology of the United Nations population estimates and projections (UN DESA/POP/2022/TR/NO. 4) [Google Scholar]
- 24.Brenner H., Arndt V., Gefeller O., Hakulinen T. An alternative approach to age adjustment of cancer survival rates. Eur J Cancer. 2004;40:2317–2322. doi: 10.1016/j.ejca.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Segi M. The Department of Public Health, Tohoku University School of Medicine; 1960. Cancer mortality for selected sites in 24 countries 1950-1957. Sendai, Japan. [Google Scholar]
- 26.Kataki A.C., Sharma J.D., Krishnatreya M., et al. A survival study of uterine cervical patients in the North East India: hospital-cancer registry-based analysis. J Cancer Res Ther. 2018;14:1089–1093. doi: 10.4103/0973-1482.184516. [DOI] [PubMed] [Google Scholar]
- 27.Ngaihte P., Zomawia E., Kaushik I. Cancer in the NorthEast India: where we are and what needs to be done? Indian J Public Health. 2019;63(3):251. doi: 10.4103/ijph.IJPH_323_18. [DOI] [PubMed] [Google Scholar]
- 28.An interactive website for SEER cancer statistics. Surveillance research program, National Cancer Institute. https://seer.cancer.gov/statistics-network/explorer/ [cited 2021 September 21]. Available from:
- 29.Mathew A., George P.S., Kunnambath R., et al. Educational status, cancer stage, and survival in south India: a population-based study. JCO Glob Oncol. 2020;6:1704–1711. doi: 10.1200/go.20.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sankaranarayanan R., Ramadas K. Early detection of cancer in primary care in less-developed countries. Cancer Control. 2013:68–72. http://cancercontrol.info/wp-content/uploads/2014/08/cc2013_66-72-Sankaranarayanan-incl-T-page_2012.pdf [Google Scholar]
- 31.Jayant K., Sankaranarayanan R., Thorat R.V., et al. Improved survival of cervical cancer patients in a screened population in rural India. Asian Pac J Cancer Prev. 2016;17(11):4837–4844. doi: 10.22034/apjcp.2016.17.11.4837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thulaseedharan J.V., Malila N., Swaminathan R., et al. Effect of screening on variation in cervical cancer survival by socioeconomic determinants-a study from rural south India. Asian Pac J Cancer Prev. 2015;16(13):5237–5242. doi: 10.7314/apjcp.2015.16.13.5237. [DOI] [PubMed] [Google Scholar]
- 33.Health technology assessment of strategies for cervical cancer screening in India. https://dhr.gov.in/health-technology-assessment-strategies-cervical-cancer-screening-india School of Public Health Postgraduate Institute of Medical Education and Research Chandigarh (India). Available from:
- 34.Mehrotra R., Yadav K. Cervical cancer: formulation and implementation of Govt of India guidelines for screening and management. Indian J Gynecol Oncol. 2022;20(1):4. doi: 10.1007/s40944-021-00602-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centre urges States to create awareness and take steps for prevention of cervical cancer among girl students. https://pib.gov.in/PressReleseDetailm.aspx?PRID=1885597 Available from:
- 36.Bray F., Ferlay J. In: Cancer incidence in five continents, No. 166. Volume XI. Bray F., Colombet M., Mery L., et al., editors. IARC Scientific Publications; Lyon, France: 2017. [Google Scholar]
- 37.Swaminathan R., Rama R., Shanta V. Lack of active follow-up of cancer patients in Chennai, India: implications for population-based survival estimates. Bull World Health Organ. 2008;86:509–515. doi: 10.2471/BLT.07.046979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bray F., Parkin D.M. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45:747–755. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 39.Parkin D.M., Bray F. Evaluation of data quality in the cancer registry: principles and methods. Part II: completeness. Eur J Cancer. 2009;45:756–764. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.