Summary
Background
Available data on cost of cancer treatment, out-of-pocket payment and reimbursement are limited in India. We estimated the treatment costs, out-of-pocket payment, and reimbursement in a cohort of breast cancer patients who sought treatment at a publicly funded tertiary cancer care hospital in India.
Methods
A prospective longitudinal study was conducted from June 2019 to March 2022 at Tata Memorial Centre (TMC), Mumbai. Data on expenditure during each visit of treatment was collected by a team of trained medical social workers. The primary outcome variables were total cost (TC) of treatment, out-of-pocket payment (OOP), and reimbursement. TC included cost incurred by breast cancer patients during treatment at TMC. OOP was defined as the total cost incurred at TMC less of reimbursement. Reimbursement was any form of financial assistance (cashless or repayment), including social health insurance, private health insurance, employee health schemes, and assistance from charitable trusts, received by the patients for breast cancer treatment.
Findings
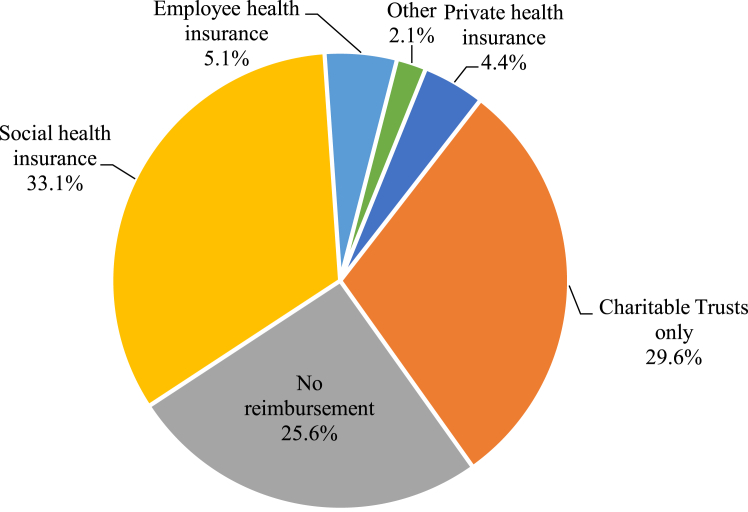
Of the 500 patients included in the study, 45 discontinued treatment (due to financial or other reasons) and 26 died during treatment. The mean TC of breast cancer treatment was ₹258,095/US$3531 (95% CI: 238,225, 277,934). Direct medical cost (MC) accounted for 56.3% of the TC. Systemic therapy costs (₹50,869/US$696) were higher than radiotherapy (₹33,483/US$458) and surgery costs (₹25,075/US$343). About 74.4% patients availed some form of financial assistance at TMC; 8% patients received full reimbursement. The mean OOP for breast cancer treatment was ₹186,461/US$2551 (95% CI: 167,666, 205,257), accounting for 72.2% of the TC. Social health insurance (SHI) had a reasonable coverage (33.1%), followed by charitable trusts (29.6%), employee health insurance (5.1%), private health insurance (4.4%) and 25.6% had no reimbursement. But SHI covered only 40.1% of the TC of treatment compared to private health insurance that covered as much as 57.1% of it. Both TC and OOP were higher for patients who were younger, belonged to rural areas, had a comorbidity, were diagnosed at an advanced stage, and were from outside Maharashtra.
Interpretation
In India, the cost and OOP for breast cancer treatment are high and reimbursement for the treatment flows from multiple sources. Though many of the patients receive some form of reimbursement, it is insufficient to prevent high OOP. Hence both wider insurance coverage as well as higher cap of the insurance packages in the health insurance schemes is suggested. Allowing for the automatic inclusion of cancer treatment in SHI can mitigate the financial burden of cancer patients in India.
Funding
This work was funded by an extramural grant from the Women’s Cancer Initiative and the Nag Foundation and an intramural grant from the International Institute of Population Sciences, Mumbai.
Keywords: Breast cancer, Oncology, Health policy, Health economics, Cancer costs, OOP, Health care expenditure, Health insurance, Reimbursement
Research in context.
Evidence before this study
Estimates of the economic burden of cancer treatment in India are primarily drawn from cross-sectional health surveys conducted by the National Sample Survey. Various small-scale studies have provided estimates of cost of treatment, out-of-pocket payment (OOP), and insurance coverage for specific cancer sites. Evidence from these studies suggests that OOP for cancer treatment is large due to the long duration of treatment, the high cost of treatment and low insurance coverage. Based on data from the latest round of NSS, 2017–2018, the OOP for any cancer treatment was estimated at ₹85,595 (USD 1171) for hospitalization.1 Jain and Mukherjee (2016)2 estimated that the major mode of financing for breast cancer treatment was OOP (91%), with only 9% of the patients covered by any health insurance.
Added value of this study
Our study followed a longitudinal approach to collect data on cost of treatment of breast cancer. In our sample, 86.0% patients were treated as subsidized patients (general or non-chargeable) and 14.0% were treated as non-subsidized patients (private). Our estimated total cost (TC) of treatment at TMC was ₹258,095/USD 3531 (95% CI: 238,255, 277,934) and the mean out-of-pocket payment (OOP) was ₹186,461/USD 2551 (95% CI: 167,666, 205,257). The TC and OOP for subsidized patients were ₹210,246/USD 2876 (95% CI: 195,308, 225,183) and ₹149,315/USD 2043 (95% CI: 135,179, 163,451), respectively. For non-subsidized patients, the TC was ₹552,368/USD 7556 (95% CI: 478,449, 626,287) and the OOP was ₹414,910/USD 5676 (95% CI: 331,623, 498,197). Systemic therapy was found to be the largest contributor to the direct medical cost of treatment, while accommodation and travel were the two major non-medical costs for patients. Reimbursement from state funded healthcare payments (insurance and welfare schemes) was to the tune of 40.1% of TC, while that from private and employee health insurance was to the tune of 58.5% and 57.1%, respectively. We observed marked variations in OOP and reimbursements across different socio-demographic and economic subgroups in the study cohort. Reimbursement at current level was insufficient to protect the breast cancer patients from financial hardship.
Implications of all the available evidence
To our knowledge, this study is the first to longitudinally capture costs incurred by patients undergoing breast cancer treatment in India. The knowledge of different treatment modalities and of the economic burden of treatment, especially in the changing landscape of treatment, is necessary to guide healthcare spending such that it benefits the underserved optimally. There is certainly a need to increase the reimbursement limits within the purview of state sponsored health insurance and to increase awareness of different insurance schemes among patients. Reduction of OOP for cancer patients can increase their financial protection and achieve the health-related sustainable development goals (SDGs).
Introduction
The incidence and prevalence of breast cancer has been increasing worldwide. Globally, breast cancer is the leading type of cancer, accounting for 2.3 million of the 19 million new cancer cases.3 In low- and middle-income countries (LMICs), a majority of breast cancer patients are in the reproductive age group, are diagnosed at an advanced stage, and experience high mortality.4, 5, 6 Economic hardship due to breast cancer treatment is high as treatment is expensive in middle-income countries, including India, and the cost of treatment has been increasing over time.7, 8, 9 Households often borrow or sell assets to meet the high out-of-pocket payment (OOP) for cancer treatment.10 In many LMICs, the financial protection mechanism systematically excludes cancer treatment from its ambit, leading to financial catastrophe.11
Breast cancer treatment involves long-term care. The treatment begins with identification of symptoms and evaluation for diagnosis, followed by an appropriate treatment and follow-up visits to monitor the disease status regularly.12 Multimodal treatment that includes surgery, radiation therapy, and systemic therapies is needed as the treatment spreads over a year. Breast cancer treatment adversely affects the economic condition of the households as they often resort to borrowing from social networks, taking loans at high interest rates, selling assets, pawning jewellery, and other such measures. In addition, the patients and their accompanying person suffer from loss of daily wages and exhaustion of paid leaves.13,14 The nature and degree of cost of and OOP for breast cancer treatment vary across countries. Chemotherapy is the largest contributor to the total cost in stage V of the disease and the lowest contributor at the initial stage.15 Most of the OOP is made towards medication, transportation, and physician visits.16 Evidences suggest that place of residence, patient age, stage at diagnosis, use of multiple therapies, type of institutional facility (public vs. private), and extent of insurance coverage are the primary drivers of treatment cost.15,17, 18, 19
In India in 2020, breast cancer accounted for 14% of the total cancer cases diagnosed and 22% of the disease adjusted life years (DALY) related to cancer.20,21 The prevalence of breast cancer has been increasing in the country. Delivery of complex cancer care requires specialist cancer centers, 95% of which are located in urban India, while 68.8% of the Indian population lives in rural areas.22 The concentration of cancer care centers in the northern and eastern regions of India is low, often leading to patients travelling long distances for treatment.9,23 In addition to this, the cancer statistics are limited to screening, prevalence, and incidence of cancer. The cancer registry provides number of cases, new cases, and deaths by type of cancer, broad age groups, and sex. With limited geographical coverage; 15% of the population in urban areas and 1% in rural areas implying larger urban representation.24,25 Population-based national-level surveys like the National Sample Survey (NSS) are cross-sectional and provide very limited information on cancer.26 Another national-level survey, the National Family Health Survey (NFHS), collected data on the screening prevalence of only breast, cervical, and oral cancer in its last two rounds (NFHS-4 and 5).27,28
Studies on the economic burden of breast cancer in India are few and based on small-scale and unrepresentative data. A household-based study from the state of Punjab showed that medicines and hospitalization accounted for over 60% of the total cost of breast cancer treatment.2 The NSS data does not segregate cost of or OOP for treatment by type and stage of cancer; rather it only provides inpatient and outpatient expenditure for any cancer treatment by household. In 2018, the mean OOP for hospitalisation for any cancer treatment in India was estimated at ₹85,595. The mean OOP for treatment was lower in public (₹38,859) hospitals compared to private hospitals (₹115,771)1; the estimates were similar to those of earlier studies.29,30 As the breast cancer treatment is multimodal and multifaceted, the estimates derived from cross-sectional studies underestimate the cost of treatment and OOP owing to recall bias in self-reported data. In this paper, we estimated of the cost of treatment of and OOP for breast cancer from a prospective longitudinal study carried out at a publicly funded tertiary cancer care center in India.
Methods
Study design and setting
We conducted a prospective study in a cohort of patients with breast cancer who were registered at Tata Memorial Centre (TMC), Mumbai. Patients who were partially/fully investigated outside TMC were eligible for the study; however, patients who had begun any part of cancer directed treatment outside the centre were not included. The study was reviewed and approved by the Institutional Ethics Committee of TMC. Patient accrual was initiated after the registration of the patients in the Clinical Trials Registry-India (CTRI/2019/07/020142). All patients were newly diagnosed, histologically confirmed cases of breast cancer that were treatment naïve. Recurrent cases were excluded. Consecutive patients seeking treatment at TMC were screened from the outpatient department. The patients were enrolled from June 2019 to August 2021 after written informed consent and followed up till March 2022. The study was a joint collaborative study between TMC and the International Institute for Population Sciences (IIPS), Mumbai. The study site, design, and setting have been elaborated in Supplementary Texts S1 and S2. Details of the study design and sample design, including inclusion and exclusion criteria, can be found elsewhere.31
Data collection and follow-up
A structured data collection tool was developed to record various demographic and socio-economic characteristics of the households and patients. The process of data collection for capturing direct medical and direct non-medical costs was a continuous one from the time of registration (baseline) to treatment completion (endline/conclusion). After obtaining consent for the study, information on the socio-demographic and economic condition of the household was collected during a 40-min to 1-h long interview of the patient/relative by a trained social worker using the structured data collection tool. The cost of treatment prior to registration at TMC was also recorded. During the subsequent hospital visits up to treatment completion, only cost data was collected. Cost data collection was carried out by verifying the billing data produced by the patient/relative or the data was drawn up from the electronic hospital records. Some patients sought some specific treatment from another health center due to the long waiting period at TMC. Data on the costs incurred by the patients on such treatment were recorded during the patients’ visit to TMC. As financial matters were often handled equally by the patients and their caregivers, we did not mandate the patient’s interview over the relative’s or vice versa (Supplementary Text S2).
Study outcome
The primary outcome variables included the total cost (TC) of treatment at TMC, out-of-pocket payment (OOP), and reimbursement. Reimbursement is an umbrella term that includes the expenses recovered by patients either in full or partially by financial assistance from sources such as social health insurance schemes, private health insurance, employee health insurance schemes, and charitable trusts. Many of the schemes provides cashless claim and in fact, treatment for cancer starts only after receiving in principle approval from the insurer. Patients received reimbursement from single as well as from multiple sources. The TC included direct medical costs and direct non-medical costs. The direct medical costs of treatment consisted of costs incurred on registration, consultation, admission, investigation, medicine, surgery, systemic therapy, and radiotherapy, whereas direct non-medical costs included food, travel and accommodation costs. We did not include indirect costs such as loss of wage or salary to the patient and the accompanying person in the estimation of TC. Data on source(s) (public or private health insurance schemes, charitable trust funding, etc.) and amount of reimbursement was collected at the time of treatment conclusion. The OOP was defined as TC less of reimbursement.
Independent variables
The study used a broad set of socio-demographic, economic, and household variables. Patients’ characteristics included standard demographic variables like age (up to 45 years, over 45 years), marital status (currently married, others), and educational level (never attended school, primary, secondary, higher secondary, higher secondary and above). Type of patient (general or non-chargeable, private), place of treatment (TMC, at least one outside TMC), comorbidity (no comorbidity, at least one comorbidity), duration of treatment (<9 months (M), 9 M–12 M, >12 M), and stage of breast cancer (early stage (I/II), advanced stage (III/IV)) were included as disease-specific variables. For household characteristics, we used religion (Hindu/Muslim/Others), caste (general, Other Backward Class (OBC), Scheduled Caste (SC) or Scheduled Trible (ST), other), location of residence (urban, rural), distance from native place to Mumbai (<500 kilometres (kms), 501–1500 kms, >1500 kms), major source of income (agriculture, labour, self-employed, service), and monthly per capita expenditure (MPCE) (poorest, poorer, middle, richer, richest). The MPCE variable did not include the expenditure on health care as used elsewhere, the reason being that cancer households spend a large amount of money on cancer treatment, which may distort the estimates of their true MPCE. A brief description of these variables is given in Supplementary Text S3.
The variables were described using frequency tables and percentages along with mean and 95% confidence interval (CI), the median, and interquartile range (IQR). Continuous outcomes (TC and OOP) were compared between groups using the non-parametric Kruskal–Wallis test.32 We used the Generalised Linear Models (GLMs) to estimate OOP across socio-economic and disease characteristics. Using a GLM allowed the OOP estimates to handle skewness,33 heteroskedastic errors, and non-linear responses to covariates.34 We considered GLMs like Gaussian family with log link, gamma family with log link, gamma inverse, etc. A model fitting algorithm was used to choose the best regression model to estimate OOP for breast cancer treatment. The model with the minimum AIC (Akkaike Information Criterion) and BIC (Bayesian Information Criterion) was chosen as the best regression model (Supplementary Table S1), which happened to be the GLM model with gamma distribution and log-link. The model is given as follows:
where the variance function of OOP is quadratic (), denotes the various socio-demographic and economic characteristics considered in the model, is the intercept, and are the K + 1 regression coefficients.
We reported the coefficients (Supplementary Table S7) and fitted an interaction model of MPCE quintile and type of insurance (Supplementary Table S8). The analysis was performed using the Stata (16.0) software.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit the report for publication.
Results
Patient characteristics
The baseline data consisted of 500 patients who were registered for treatment at TMC. Of them, 429 had successfully completed treatment and were interviewed at the end of the treatment (referred as endline). A total of 71 patients did not complete the treatment due to death or financial and other reasons.31 Supplementary Table S2 shows the summary characteristics of the 429 patients in the concluded sample. A majority of the patients were married and from rural areas. The mean age of the study cohort was 47 years and the mean years of schooling was 7 years. About one-fourth (24%) of the patients belonged to households whose income primarily came from daily wage labour. Thirty-one percent of the patients had a comorbidity. Two-thirds of the patients were diagnosed at an advanced stage, and 90% of all the patients completed the treatment within one year. On average, a cancer patient traveled 1066 kms for treatment. The study cohort comprised a higher proportion of patients from the subsidized payment category (non-chargeable/general) than those belonging to the full payment category (private).
Treatment cost
Table 1 presents a systematic breakdown of TC of breast cancer treatment. The average TC was ₹258,095 (95% CI: 238,255, 277,934). The primary factor of cost before coming to TMC was investigation for breast cancer diagnosis. The pattern of cost of treatment before coming to TMC was different from the pattern during treatment at TMC (Supplementary Table S3). Out of the TC, 56% could be attributed to direct medical cost and 44% to direct non-medical cost. The segmentation of TC further suggests that systemic therapy accounted for the largest share (19.7%), followed by accommodation (18.6%), travel (17.9%), and radiotherapy (13%) (Fig. 1). The breakdown of the direct medical cost suggests that systemic therapy (35.0%) was the most expensive form of treatment, while surgery (17.3%) was the least expensive form. Radiotherapy accounted for 23.1% of the direct medical cost, while investigation made up 14.6% of it. The largest proportion of direct non-medical treatment cost was composed of accommodation (42.7%) and food (40.9%) related costs (Supplementary Figure S1). The direct non-medical cost of cancer treatment increased from ₹1011 (95% CI: 832, 1191) prior to TMC to ₹112,707 (95% CI: 100,578, 124,835) during treatment at TMC (Supplementary Table S3).
Table 1.
Mean costs (in ₹) segregation of breast cancer treatment at TMC, Mumbai.
| Type of costs | During treatment at TMC |
||
|---|---|---|---|
| Mean cost (in ₹) | 95% CI | % Shareb | |
| 1. Total medical cost | 145,388 | (133,402, 157,375) | 56.3 |
| Registration cost | 247 | (180, 313) | 0.1 |
| Consultation cost | 1684 | (1265, 2104) | 0.7 |
| Admission cost | 4833 | (4116, 5550) | 1.9 |
| Investigation cost | 21,239 | (19,486, 22,993) | 8.2 |
| Medicine cost | 7751 | (6720, 8782) | 3.0 |
| Surgery costa | 25,075 | (21,385, 28,766) | 9.7 |
| Systemic therapy costa | 50,869 | (44,391, 57,346) | 19.7 |
| Radiotherapy costa | 33,483 | (28,873, 38,092) | 13.0 |
| 2. Total non-medical cost | 112,707 | (100,578, 124,835) | 43.7 |
| Food cost | 46,149 | (41,926, 50,372) | 17.9 |
| Travel cost | 18,460 | (16,198, 20,723) | 7.2 |
| Accommodation cost | 48,097 | (39,689, 56,505) | 18.6 |
| 3. Total cost (1 + 2) | 258,095 | (238,255, 277,934) | 100.0 |
Note: 1 US$ = ₹73.1 at 2020 prices.
Only treatment naïve cases were accrued.
The percentage share of each cost component (registration, admission, investigation…etc) was calculated out of the total cost (100%).
Fig. 1.
Percent distribution in cost of breast cancer by component at TMC,Mumbai.
Table 2 shows the socio-economic differentials in TC, OOP, and share of OOP to TC. The mean OOP was ₹186,461 (95% CI: 167,666, 205,257), accounting for 72.2% of the TC. The median OOP and median TC are shown in Supplementary Table S4. The socio-economic gradient of TC and OOP showed a significant association. The OOP (p < 0.001) increased linearly with the economic condition of the households (measured by MPCE quintile), distance to Mumbai (p < 0.001) from the native place, stage of cancer (p = 0.044), and duration of treatment (p < 0.001). The pattern was similar for TC. The mean OOP for the richest quintile was more than thrice higher than for the poorest quintile (p < 0.001). OOP as a share of TC varied from 61.1% in the poorest quintile to 78.4% in the richest quintile. The mean OOP for patients in the early stage of cancer was ₹164,721 (95% CI: 136,915, 192,527), which accounted for 71.2% of the TC. Patients in the advanced stage of cancer had a mean OOP of ₹195,395 (95% CI: 173,880, 223,639), which accounted for 72% of the TC. Patients who underwent less than nine months of treatment incurred almost half as much OOP as patients who were treated for more than one year (p < 0.001). Patients who completed the full course of treatment at TMC had a lower OOP (<0.001) and a lower TC (<0.001) compared to those who underwent at least one modality of treatment (surgery, systemic therapy, or radiotherapy) outside TMC. The pattern of cost segregation by stage showed a higher cost for systemic therapy in the advanced stage compared to the early stage (Supplementary Table S5). Over 84% patients had taken three modes of treatment and their cost was higher than those who taken only a single mode of treatment (Supplementary Table S6).
Table 2.
Socio-economic differentials in the cost of treatment at TMC (in ₹), out-of-pocket payment (in ₹) and out-of-pocket payment as a share of total cost at TMC for breast cancer at TMC, Mumbai.
| SES variables | N | Cost of treatment at TMC (in ₹) |
OOP (in ₹) |
OOP as a share of TC |
||||
|---|---|---|---|---|---|---|---|---|
| Mean | 95% CI | p-value | Mean | 95% CI | p-value | % | ||
| Age of patients | 0.026 | 0.177 | ||||||
| Up to 45 years | 202 | 266,258 | (237,607, 294,909) | 188,367 | (161,950, 214,784) | 70.7 | ||
| Over 45 years | 227 | 250,831 | (223,170, 278,492) | 184,765 | (157,948, 211,582) | 73.7 | ||
| Marital status | 0.009 | 0.046 | ||||||
| Other | 63 | 192,676 | (156,627, 228,725) | 124,540 | (96,088, 152,993) | 64.6 | ||
| Currently married | 366 | 269,355 | (247,094, 291,617) | 197,120 | (175,791, 218,449) | 73.2 | ||
| Location of residence | <0.001 | <0.001 | ||||||
| Urban | 196 | 206,389 | (182,637, 230,142) | 131,193 | (110,802, 151,584) | 63.6 | ||
| Rural | 233 | 301,590 | (271,993, 331,187) | 232,953 | (204,088, 261,818) | 77.2 | ||
| Education level | <0.001 | 0.002 | ||||||
| Never attended | 99 | 236,252 | (201,359, 271,145) | 166,617 | (136,225, 197,009) | 70.5 | ||
| Primary | 36 | 235,438 | (163,538, 307,339) | 176,455 | (106,896, 246,014) | 74.9 | ||
| Secondary | 167 | 209,950 | (188,041, 231,860) | 141,081 | (120,760, 161,401) | 67.2 | ||
| Higher secondary | 50 | 275,740 | (214,278, 337,202) | 214,277 | (156,430, 272,124) | 77.7 | ||
| Above HS | 77 | 389,730 | (322,750, 456,711) | 297,013 | (229,610, 364,417) | 76.2 | ||
| Religion | 0.239 | 0.082 | ||||||
| Hindu | 332 | 263,135 | (239,598, 286,673) | 189,326 | (167,232, 211,421) | 72.0 | ||
| Muslim | 80 | 252,210 | (212,125, 292,296) | 193,549 | (153,028, 234,070) | 76.7 | ||
| Others | 17 | 187,350 | (115,262, 259,439) | 97,149 | (44,797, 149,501) | 51.9 | ||
| Caste | 0.007 | 0.007 | ||||||
| General | 226 | 287,088 | (256,362, 317,814) | 214,131 | (184,973, 243,289) | 74.6 | ||
| OBC | 145 | 239,628 | (209,348, 269,908) | 168,999 | (140,702, 197,297) | 70.5 | ||
| SC/ST/Other | 58 | 191,289 | (157,426, 225,152) | 122,299 | (88,868, 155,730) | 63.9 | ||
| Distance to Mumbai | <0.001 | <0.001 | ||||||
| <500 kms | 185 | 164,606 | (144,749, 184,463) | 95,887 | (80,337, 111,437) | 58.3 | ||
| 501–1500 kms | 60 | 348,865 | (292,630, 405,100) | 290,706 | (230,106, 351,306) | 83.3 | ||
| >1500 kms | 184 | 322,493 | (289,199, 355,787) | 243,534 | (211,893, 275,176) | 75.5 | ||
| Income source | 0.055 | 0.028 | ||||||
| Agriculture | 54 | 280,074 | (234,368, 325,780) | 214,717 | (171,665, 257,770) | 76.7 | ||
| Labour | 103 | 216,336 | (186,723, 245,950) | 150,144 | (123,667, 176,620) | 69.4 | ||
| Self-employed | 66 | 300,722 | (232,620, 368,824) | 230,801 | (168,221, 293,382) | 76.7 | ||
| Service | 206 | 259,556 | (229,884, 289,227) | 183,007 | (154,103, 211,911) | 70.5 | ||
| MPCE | <0.001 | <0.001 | ||||||
| Poorest | 83 | 147,955 | (126,233, 169,677) | 90,430 | (72,868, 107,993) | 61.1 | ||
| Poorer | 78 | 175,336 | (148,825, 201,846) | 115,596 | (89,997, 141,196) | 65.9 | ||
| Middle | 89 | 218,674 | (191,974, 245,374) | 152,673 | (125,935, 179,412) | 69.8 | ||
| Richer | 89 | 293,421 | (244,702, 342,140) | 215,062 | (166,951, 263,173) | 73.3 | ||
| Richest | 90 | 435,442 | (380,660, 490,225) | 341,569 | (288,275, 394,863) | 78.4 | ||
| Type of patient | <0.001 | <0.001 | ||||||
| General/Non-chargeable | 369 | 210,246 | (195,308, 225,183) | 149,315 | (135,179, 163,451) | 71.0 | ||
| Private | 60 | 552,368 | (478,449, 626,287) | 414,910 | (331,623, 498,197) | 75.1 | ||
| Stage of cancer | 0.017 | 0.044 | ||||||
| Early stage (I/II) | 155 | 231,335 | (200,106, 262,564) | 164,721 | (136,915, 192,527) | 71.2 | ||
| Advance stage (III/IV) | 274 | 273,233 | (247,714, 298,751) | 195,395 | (173,880, 223,639) | 72.0 | ||
| Comorbidities | 0.735 | 0.435 | ||||||
| No comorbidity | 296 | 251,805 | (230,358, 273,252) | 182,909 | (162,108, 203,710) | 72.6 | ||
| At least 1 comorbidity | 133 | 272,093 | (229,086, 315,101) | 194,367 | (154,802, 233,931) | 71.4 | ||
| Place of treatment | <0.001 | <0.001 | ||||||
| TMC | 243 | 217,448 | (193,008, 241,888) | 148,239 | (125,711, 170,767) | 68.2 | ||
| At least one outside TMC | 186 | 311,198 | (279,777, 342,619) | 236,397 | (205,794, 267,000) | 76.0 | ||
| Duration of treatment | <0.001 | <0.001 | ||||||
| <9 M | 214 | 232,674 | (207,563, 257,786) | 156,228 | (134,364, 178,092) | 67.1 | ||
| 9 M−12 M | 174 | 262,883 | (232,652, 293,115) | 196,180 | (166,389, 225,971) | 74.6 | ||
| 12 M | 41 | 370,456 | (275,925, 464,987) | 303,018 | (208,908, 397,128) | 81.8 | ||
| Total | 429 | 258,095 | (238,255, 277,934) | 186,461 | (167,666, 205,257) | 72.2 | ||
Note: 1 US$ = ₹73.1 at 2020 prices.
Table 3 presents the mean reimbursement and percentage reimbursed by socio-economic characteristics. Almost three-fourths of the breast cancer patients received some reimbursement, and the mean reimbursement amount was ₹71,724 (95% CI: 61,747, 81,701). The median reimbursement is shown in Supplementary Table S4. Patients belonging to the richest MPCE quintile received the highest reimbursement (₹94,040; 95% CI: 60,510, 127,569), while those belong to the poorest quintile received the lowest amount (₹57,526; 95% CI: 43,531, 71,522). Compared to their respective counterparts, the share of reimbursement to total cost was higher among patients belonging to the poorest MPCE quintile (79.5%), urban patients (42%), patients belonging to SC/ST/other category (40%), patients who had labour and service as the major sources of household income (each 33%), patients whose cancer was diagnosed at an early stage (31%), and patients who completed treatment in less than nine months (37%).
Table 3.
Percentage reimbursed and mean reimbursement (in ₹) by socio-economic characteristics.
| SES variables | % Reimbursed |
Reimbursement (in ₹) |
|
|---|---|---|---|
| % | Mean | 95% CI | |
| Age of patients | |||
| Up to 45 years | 76.2 | 77,999 | (61,564, 94,435) |
| Over 45 years | 72.7 | 66,140 | (54,163, 78,117) |
| Marital status | |||
| Others | 82.5 | 68,216 | (44,658, 91,774) |
| Currently married | 73.0 | 72,328 | (61,318, 83,338) |
| Location of residence | |||
| Urban | 79.1 | 75,339 | (59,936, 90,743) |
| Rural | 70.4 | 68,683 | (55,569, 81,797) |
| Education level | |||
| Never attended | 77.8 | 69,705 | (52,443, 86,966) |
| Primary | 69.4 | 59,091 | (25,870, 92,312) |
| Secondary | 82.6 | 68,952 | (56,111, 81,793) |
| Higher secondary | 72.0 | 61,514 | (33,127, 89,901) |
| Above HS | 55.8 | 92,869 | (56,505, 129,234) |
| Religion | |||
| Hindu | 72.3 | 73,892 | (61,943, 85,841) |
| Muslim | 81.3 | 58,780 | (42,773, 74,826) |
| Others | 82.4 | 90,202 | (26,453, 153,950) |
| Caste | |||
| General | 70.4 | 73,049 | (57,761, 88,337) |
| OBC | 79.3 | 70,739 | (55,895, 85,583) |
| SC/ST/Other | 77.6 | 69,024 | (44,603, 93,445) |
| Distance to Mumbai | |||
| <500 kms | 82.7 | 68,764 | (53,994, 83,534) |
| 501–1500 kms | 58.3 | 58,415 | (32,170, 84,659) |
| >1500 kms | 71.2 | 79,040 | (63,121, 94,960) |
| Income source | |||
| Agriculture | 74.1 | 65,515 | (42,288, 88,743) |
| Labour | 86.4 | 66,247 | (51,728, 80,766) |
| Self-employed | 65.2 | 69,954 | (43,373, 96,535) |
| Service | 71.4 | 76,657 | (60,001, 93,313) |
| MPCE | |||
| Poorest | 79.5 | 57,526 | (43,531, 71,522) |
| Poorer | 83.3 | 59,803 | (45,601, 74,006) |
| Middle | 79.8 | 66,063 | (48,773, 83,353) |
| Richer | 71.9 | 78,506 | (54,580, 102,433) |
| Richest | 58.9 | 94,040 | (60,510, 127,569) |
| Type of patient | |||
| General/Non-chargeable | 78.3 | 61,023 | (53,760, 68,375) |
| Private | 50.0 | 137,538 | (84,038, 191,037) |
| Stage of cancer | |||
| Early stage (I/II) | 71.0 | 66,725 | (47,871, 85,579) |
| Advance stage (III/IV) | 76.3 | 74,552 | (63,056, 86,048) |
| Comorbidities | |||
| No comorbidity | 74.3 | 68,988 | (57,688, 80,288) |
| At least 1 comorbidity | 74.4 | 77,813 | (57,533, 98,093) |
| Place of treatment | |||
| TMC | 77.6 | 74,827 | (57,531, 92,123) |
| At least one outside TMC | 71.8 | 69,349 | (57,625, 81,073) |
| Duration of treatment | |||
| <9 M | 68.3 | 76,586 | (60,034, 93,138) |
| 9 M−12 M | 71.0 | 66,754 | (54,694, 78,815) |
| 12 M | 77.0 | 67,438 | (36,549, 98,326) |
| Total | 74.4 | 71,724 | (61,747, 81,701) |
Note: 1 US$ = ₹73.1 at 2020 prices.
Fig. 2 presents the state-wise variation in OOP and reimbursement as a share of TC among breast cancer patients. OOP was the highest for patients from Uttar Pradesh and higher for those from the other states compared to patients from Maharashtra. In contrast, the share of reimbursement was higher for patients from Maharashtra compared to patients from outside Maharashtra.
Fig. 2.
Out-of-pocket payment and reimbursement as a percentage of total cost for breast cancer treatment at TMC by state oforigin.
Table 4 and Fig. 3 show the sources of reimbursement. Social health insurance (SHI) schemes were the biggest source of reimbursement (33.1%), followed by charitable trusts (29.6%) and employee health insurance (5.1%). 25.6% of the patients received no reimbursement, whereas 8% received full reimbursement. Employee health insurance (58.5%) was the source of highest reimbursement as a share of TC, followed by private health insurance (57.1%) and SHI schemes like Swasthya Sathi (38.3%), MJPJAY (32.0%), and PM-JAY (28.9%).
Table 4.
Type of reimbursement and its share to total cost of treatment at TMC.
| Type of reimbursement | N (%) | Reimbursement (in ₹) |
TC of treatment (in ₹) |
Reimbursement as share of TC |
||
|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | % Share | ||
| No reimbursement | 110 (25.6) | NA | NA | 335,152 | (289,330, 380,975) | NA |
| Social health insurance | 142 (33.1) | 59,088 | (50,582, 67,594) | 147,249 | (130,563, 163,935) | 40.1 |
| PM-JAY/& trusta | 11 (2.6) | 71,968 | (42,690, 101,247) | 249,360 | (156,910, 341,810) | 28.9 |
| MJPJAY only | 74 (17.2) | 36,386 | (29,724, 43,499) | 113,867 | (96,257, 131,478) | 32.0 |
| MJPJAY, trust & ESISb | 50 (11.7) | 82,649 | (65,715, 99,582) | 154,399 | (128,589, 180,208) | 53.5 |
| Swasthya Sathi (WB)c | 7 (1.6) | 110,542 | (53,695, 167,390) | 288,618 | (187,659, 389,577) | 38.3 |
| Employee health insurance | 22 (5.1) | 196,632 | (117,595, 275,669) | 336,048 | (238,931, 433,166) | 58.5 |
| Private health insurance | 19 (4.4) | 308,152 | (207,099, 409,205) | 539,710 | (351,655, 727,765) | 57.1 |
| Charitable trust/s only | 127 (29.6) | 89,594 | (75,652, 103,535) | 260,799 | (234,177, 287,421) | 34.4 |
| Othersd | 9 (2.1) | 110,542 | (53,695, 167,390) | 241,950 | (124,592, 359,308) | 45.7 |
| Total | 429 | 71,724 | (61,747, 81,701) | 258,095 | (238,255, 277,934) | 27.8 |
Note: PM-JAY: Pradhan Mantri Jan Arogya Yojana; MJPJAY: Mahatma Jyotirao Phule Jan Arogya Yojana; ESIS: Employee State Insurance Scheme, Charitable Funds includes financial help from all philanthropic sources.
1 US$ = ₹73.1 at 2020 prices.
Contains 5 cases where patients got reimbursement from ABY and Trust.
There were 2 cases of patients where they got reimbursement from ESIS & Trust along with MJPJAY, respectively.
Contains 4 cases where patients got reimbursement from Swasthya Sathi as well as Trust.
Others contain unspecified sources.
Fig. 3.
Percent distribution of source of reimbursement received by patients atTMC.
Table 5 provides the adjusted and unadjusted mean OOP for breast cancer treatment. Controlling for the covariates, the adjusted mean OOP for breast cancer treatment was ₹188,666 (95% CI: 169,526, 207,805), higher than the unadjusted mean OOP of ₹186,461 (95% CI: 167,666, 205,257). Patients who were older, were living in urban areas, had low educational levels, belonged to the poorest or poorer quintiles, had SHI, and were in the advanced stage of cancer had a higher adjusted mean OOP than the unadjusted mean OOP. Private category patients had an adjusted mean OOP of ₹283,897 (95% CI: 228,486, 339,308), which was lower than the unadjusted mean OOP. Patients with SHI belonging to the poorest and poorer quintiles had 45% and 40% less OOP, respectively, than patients with no reimbursement in the poorest quintile. Patients with no reimbursement in the richest quintile were more likely to have more OOP than patients with no reimbursement in the poorest quintile (Supplementary Table S8). The predicted OOP was higher among patients with SHI in the poorest quintile than patients with employee/private health insurance and financial assistance from trusts. Among patients with SHI in the richer and richest quintiles, the predicted OOP was much lower than their counterparts (Supplementary Figure S2).
Table 5.
Adjusted and unadjusted mean out-of-pocket payment (in ₹) for breast cancer treatment at TMC, Mumbai.
| SES characteristics | Adjusted OOP (in ₹) |
Unadjusted OOP (in ₹) |
||
|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | |
| Age of patients | ||||
| Up to 45 years | 184,686 | [160,444, 208,927] | 188,367 | [161,950, 214,784] |
| Over 45 years | 192,660 | [169,007, 216,313] | 184,765 | [157,948, 211,582] |
| Marital status | ||||
| Others | 175,919 | [141,987, 209,850] | 124,540 | [96,088, 152,993] |
| Currently married | 190,168 | [170,473, 209,863] | 197,120 | [175,791, 218,449] |
| Location of residence | ||||
| Urban | 170,817 | [146,730, 194,904] | 131,193 | [110,802, 151,584] |
| Rural | 198,348 | [175,631, 221,065] | 232,953 | [204,088, 261,818] |
| Education level | ||||
| Never attended | 178,103 | [148,014, 208,192] | 166,617 | [136,225, 197,009] |
| Primary | 158,774 | [116,543, 201,006] | 176,455 | [106,896, 246,014] |
| Secondary | 182,539 | [157,280, 207,798] | 141,081 | [120,760, 161,401] |
| Higher secondary | 187,841 | [150,360, 225,323] | 214,277 | [156,430, 272,124] |
| Above HS | 215,471 | [176,608, 254,335] | 297,013 | [229,610, 364,417] |
| Religion | ||||
| Hindu | 185,915 | [165,792, 206,038] | 189,326 | [167,232, 211,421] |
| Muslim | 202,814 | [166,814, 238,815] | 193,549 | [153,028, 234,070] |
| Others | 174,479 | [101,775, 247,182] | 97,149 | [44,797, 149,501] |
| Caste | ||||
| General | 187,182 | [164,219, 210,145] | 214,131 | [184,973, 243,289] |
| OBC | 198,823 | [170,438, 227,207] | 168,999 | [140,702, 197,297] |
| SC/ST/Other | 167,290 | [131,086, 203,493] | 122,299 | [88,868, 155,730] |
| Distance to Mumbai | ||||
| <500 kms | 134,055 | [109,552, 158,557] | 95,887 | [80,337, 111,437] |
| 501–1500 kms | 208,742 | [174,152, 243,333] | 290,706 | [230,106, 351,306] |
| >1500 kms | 213,587 | [189,068, 238,106] | 243,534 | [211,893, 275,176] |
| Income source | ||||
| Agriculture | 210,442 | [170,178, 250,707] | 214,717 | [171,665, 257,770] |
| Labour | 192,860 | [159,770, 225,949] | 150,144 | [123,667, 176,620] |
| Self-employed | 190,780 | [152,429, 229,130] | 230,801 | [168,221, 293,382] |
| Service | 180,268 | [157,630, 202,905] | 183,007 | [154,103, 211,911] |
| MPCE | ||||
| Poorest | 111,003 | [89,752, 132,254] | 90,430 | [72,868, 107,993] |
| Poorer | 144,909 | [117,291, 172,526] | 115,596 | [89,997, 141,196] |
| Middle | 188,945 | [156,284, 221,606] | 152,673 | [125,935, 179,412] |
| Richer | 177,612 | [150,478, 204,746] | 215,062 | [166,951, 263,173] |
| Richest | 263,544 | [227,612, 299,477] | 341,569 | [288,275, 394,863] |
| Type of insurance | ||||
| Social health insurance | 143,041 | [117,509, 168,574] | 88,275 | [74,516, 102,034] |
| Employee health insurance | 122,682 | [69,179, 176,184] | 139,551 | [65,120, 213,982] |
| Private health insurance | 130,019 | [69,044, 190,994] | 231,558 | [59,926, 403,190] |
| Trust and other | 161,473 | [139,628, 183,318] | 169,940 | [146,374, 193,507] |
| No insurance | 267,036 | [236,175, 297,896] | 335,229 | [289,397, 381,061] |
| Type of patient | ||||
| General | 164,067 | [147,932, 180,203] | 149,315 | [135,179, 163,451] |
| Private | 283,897 | [228,486, 339,308] | 414,910 | [331,623, 498,197] |
| Stage of cancer | ||||
| Early stage (I/II) | 166,050 | [143,449, 188,651] | 164,721 | [136,915, 192,527] |
| Advance stage (III/IV) | 200,312 | [177,373, 223,251] | 198,759 | [173,880, 223,639] |
| Comorbidities | ||||
| No comorbidity | 190,653 | [169,407, 211,898] | 182,909 | [173,880, 223,639] |
| At least 1 comorbidity | 184,574 | [157,102, 212,045] | 194,367 | [162,108, 203,710] |
| Place of treatment | ||||
| TMC | 203,004 | [178,060, 227,947] | 148,239 | [125,711, 170,767] |
| At least one outside TMC | 173,350 | [150,795, 195,906] | 236,397 | [205,794, 267,000] |
| Duration of treatment | ||||
| <9 M | 161,312 | [141,224, 181,400] | 156,228 | [134,364, 178,092] |
| 9 M−12 M | 196,092 | [170,784, 221,401] | 196,180 | [166,389, 225,971] |
| 12 M | 293,824 | [232,568, 355,080] | 303,018 | [208,908, 397,128] |
| Total | 188,666 | [169,526, 207,805] | 186,461 | [167,666, 205,257] |
Discussion
This is the first ever prospective study in India that provides estimates of the cost of, OOP for, and reimbursement of cost of breast cancer treatment using a longitudinal design from the patient perspective. Our approach to data collection over multiple visits during treatment is likely to have minimized the recall bias (common in cross-sectional surveys) and double counting. The study was comprehensive as it had an adequate sample size for disaggregated analyses by socio-economic, demographic, and disease-specific characteristics. The following are the salient findings of the study.
First, breast cancer treatment is expensive. The average cost of breast cancer treatment, OOP payment, and reimbursement showed a strong socio-economic gradient and variation by disease characteristics. TC, OOP, and reimbursement were higher for better educated patients, those belonging to the general social group, younger patients, rural inhabitants, patients who came from states other than Maharashtra, treated as private patients, those who were diagnosed at an advance stage, and those who had co-morbidities. Second, medical cost accounted for 56.3% of the total cost of treatment at TMC. Out of the direct medical cost, the cost was the highest for systemic therapy, followed by radiation and surgery. The main contributors to the direct non-medical cost were accommodation and travel costs. Third, about three-fourths of patients got reimbursement, but it did not reduce the high OOP burden. Reimbursement accounted for 58.9% of TC for patients in the richest MPCE quintile compared to 79.5% among patients in the poorest MPCE quintile. OOP accounted for 72.2% of the total cost of treatment. Fourth, patients relied on multiple sources to get support for breast cancer treatment. Only one-third of the patients were covered by SHI schemes, which are publicly funded; only 5% patients had a private health insurance and one-fourth of all patients did not have any form of reimbursement. SHI had a larger coverage compared to private and employee health insurance, but reimbursement as a share of total cost was higher among patients with private and employee health insurance. About one-third patients were reimbursed by charitable organizations and trusts.
Finally, after controlling for socio-demographic correlates, type of insurance, co-morbidities, type of patient, economic status, stage of cancer, and duration of treatment emerged as significant predictors of OOP for breast cancer treatment.
We provide some plausible explanations in support of these findings. The high TC of and OOP for breast cancer among the richer, more educated, and non-Scheduled Caste/Tribe patients may be attributed to their ability to pay. These patients were more likely to be treated as private patients and incurred a higher direct non-medical cost. However, our finding as to higher TC and OOP among rural residents and patients from states other than Maharashtra was possibly due to distance, non-familiarity with place of treatment, and lack of social networking.35 Patients from rural areas and those with a co-morbidity may have had limited access to insurance. The high mean and median TC and OOP observed in our study confirm the findings of previous studies that TC and OOP increase with advancing stage of the disease.2,36, 37, 38 Advanced stage patients may need intense/additional treatment that is likely to increase the cost. Moreover, stage IV patients receive multiple lines of treatment either due to lack of adequate control of disease or due to disease recurrence. Hence their existing insurance scheme is likely to cover treatment costs only partially.
An interesting finding in our study was with regard to the respective share of cost of systemic, radiation, and surgical modalities of treating cancer, with the cost of systemic therapy being the highest, followed by the cost of radiation and surgery in that order, while most previous studies often place radiation therapy at the bottom of the list of contributors to costs of breast cancer treatment.2,39 The higher contribution of radiation therapy to costs in comparison to previous studies in India can be explained by the adoption of newer techniques by breast radiation oncologists and, more often, curative treatment of oligometastatic disease with ablative radiation. The high contribution of systemic therapy can be explained by the increased use of targeted therapies which have been shown to contribute to 67% of the drug costs, of which trastuzumab alone accounts for 94%.39 Hormone therapy, on the other hand, has been shown to contribute to 30% of the total spend on drugs, with letrozole and fulvestrant contributing to 65% of it in one study.39
Our finding as to non-medical costs accounting for 45% of the total cost is consistent with literature.40, 41, 42 One way of interpreting the high non-medical costs in the current study could be in terms of relocation of most of the patient population to metropolitan cities for treatment, where the cost of living is higher. This is supported by the fact that 55.2% patients at TMC came from other states of India, largely the states of West Bengal, Bihar, and Uttar Pradesh. Another reason may be the frequent number of visits required for cancer treatment, which made patients choose accommodation close to the hospital that may have been expensive.40
An important means of affordability of health care across all social strata is coverage via insurance/welfare schemes. Almost three-fourths of the patients in our cohort were covered under various insurance/welfare schemes or reimbursed by charitable trusts, which is very important with regard to financial risk protection. The most common source of reimbursement was social health insurance (SHI) schemes such as MJPJAY, which is a popular flagship insurance program of the Maharashtra State Government that covers any hospitalization or treatment cost up to ₹150,000 per family per year. Other such welfare schemes include PM-JAY and state-specific health schemes offered to residents by their respective states. The SHI schemes were the biggest source of reimbursement. One-third of patients undergoing treatment at our centre who were eligible for financial aid were supported by multiple charity sources, a few of which include the Tata Trusts, the Nargis Dutt Foundation, the Madat Foundation, and different funds of the Indian Cancer Society.
The share of reimbursement to TC was found to be about 27.8% in our study. This can be explained by the higher costs of cancer care and the lower cap for reimbursement under different schemes. Patients in our study were characterised by diverse socio-cultural backgrounds, educational status, and awareness/health attitudes and by residence in various states when compared to a former study which was conducted within a single state. Private insurance coverage in India has not seen a great rise in last two decades.28,43 The low reimbursement rates among patients in our breast cancer cohort corroborate the findings of previous studies. Our study was conducted during a period when PM-JAY had just been rolled out and did not cover most of the states. Under recent changes in PM-JAY, the cap has been enhanced to ₹500,000, which may be sufficient for breast cancer treatment.
We strongly believe this work can serve as an index measure to define the breadth of monetary coverage in SHI schemes, which, at present, does not lower the OOP reasonably. India’s public health care expenditure has remained abysmally low but has increased since the launch of PM-JAY due to which the coverage of SHI schemes has increased significantly among the poorer and marginalised population in the country.44 There is a need for automatic inclusion of cancer treatment in PM-JAY. Our work also sensitises breast cancer physicians in clinics across the country to the ongoing financial toxicity pandemic and the need to arrange for subsidies/philanthropic help locally for the vulnerable populations so that they are able to continue treatment. We suggest systematic collection of data by the National Sample Survey in the form of inclusion of cancer types, stage of disease, treatment cost, and supportive care costs. We suggest taking into consideration the rising cancer care costs, which prohibit oncologists in India from offering what is called ‘standard of care’ treatments in the developed nations while framing the sum insured for SHI policies. A majority of our patients came to Mumbai from the other states of India to avail treatment, which raised their non-treatment costs. In this context, there is an argument that OOP could have been lower had patients availed treatment at their local place. Future research on breast cancer may focus on multicentric study and estimate the economic impact of breast cancer in the long run.
Although a longitudinal study that captured data over multiple visits, our study is not without limitations. One of the important limitations is that our study was based on a single centre that operates on a health economic model that is characterised by widespread financial help, subsidies, and social support. Few cancer institutes in the country offer financial support for patient care at such a large scale as TMC while dealing with the same cost of treatment. Such disparity in the provision of healthcare is a common occurrence in LMICs and impedes the generalisability of our findings for patients in other parts of the country. We also acknowledge that our sample may have suffered from selection bias as there was a lower representation of patients from the higher socioeconomic stratum. Such patients may have opted for treatment from private health centres, which was beyond our scope. However, even in the presence of selection bias, our estimates of cost of and OOP for treatment provide at best the lower bounds of the true estimates. Another limitation is that we included systemic therapy, which encompasses targeted therapy, hormonal therapy, and chemotherapy, which may have led to higher systemic therapy cost compared to radiotherapy and surgery costs. Lastly, we did not consider indirect costs like wage and productivity loss of patients and accompanying persons in estimation.
Contributors
TW and SKM equally contributed to the study, and both share first authors. TW is the corresponding author. The study was conceptualized by TW & SKM. The data was collected by NP & SS and analyzed by SS & SM. The first draft was prepared by SKM, SS, TW, SM, & TS. This was followed by editing of the final draft by SM, SKM, TW, TS, SG, RS, & VP. The project administration was done by TW and SKM. All the authors read the final version of the manuscript. (SKM: Sanjay K Mohanty, SM: Suraj Maiti).
Data sharing statement
All the authors involved in the study have access to the data collected as part of this project. Sharing of the data with outside parties is at the discretion of the corresponding author and may be considered on request.
Declaration of interests
The authors declare no conflict of interest.
Acknowledgements
We are thankful for the extramural grant from the Women’s Cancer Initiative and the Nag Foundation as well as for the intramural grant from the International Institute of Population Sciences, Mumbai. The content of the article is solely the responsibility of the authors and does not necessarily represent the views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of manuscript.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100346.
Contributor Information
Tabassum Wadasadawala, Email: twadasadawala@actrec.gov.in.
Sanjay K. Mohanty, Email: sanjayiips@yahoo.co.in.
Soumendu Sen, Email: sen.soumendu16@gmail.com.
Tejaswi S. Kanala, Email: tejashvisreevatsavak@gmail.com.
Suraj Maiti, Email: suraj.yunique@gmail.com.
Namita Puchali, Email: namitaumesh1937@gmail.com.
Sudeep Gupta, Email: sudeepgupta04@yahoo.com.
Rajiv Sarin, Email: drrajivsarin@gmail.com.
Vani Parmar, Email: vaniparmar@gmail.com.
Appendix A. Supplementary data
References
- 1.Goyanka R. Economic and non-economic burden of cancer: a propensity score matched analysis using household health survey data of India. Cancer Res Stat Treat. 2021;4:29–36. [Google Scholar]
- 2.Jain M., Mukherjee K. Economic burden of breast cancer to the households in Punjab, India. Int J Med Public Health. 2016;6:13. [Google Scholar]
- 3.Sung H., Ferlay J., Siegel R.L., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 4.Sen S., Khan P.K., Wadasadawala T., Mohanty S.K. Socio-economic and regional variation in breast and cervical cancer screening among Indian women of reproductive age: a study from National Family Health Survey, 2019-21. BMC Cancer. 2022;22:1279. doi: 10.1186/s12885-022-10387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim Y.X., Lim Z.L., Ho P.J., Li J. Breast cancer in Asia: incidence, mortality, early detection, mammography programs, and risk-based screening initiatives. Cancers. 2022;14:4218. doi: 10.3390/CANCERS14174218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bidoli E., Virdone S., Hamdi-Cherif M., et al. Worldwide age at onset of female breast cancer: a 25-year population-based cancer registry study. Sci Rep. 2019;9 doi: 10.1038/S41598-019-50680-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Natarajan A., Mehra N., Rajkumar T. Economic perspective of cancer treatment in India. Med Oncol. 2020;37:101. doi: 10.1007/S12032-020-01424-3. [DOI] [PubMed] [Google Scholar]
- 8.Prasad V., De Jesús K., Mailankody S. The high price of anticancer drugs: origins, implications, barriers, solutions. Nat Rev Clin Oncol. 2017;14:381–390. doi: 10.1038/nrclinonc.2017.31. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhuri S., Goel A., Awasthi A., et al. Disparity between Metro-Centric Cancer Care and Rural Outreach in India: situational analysis and future trends in context of developing countries. J Glob Oncol. 2018;4:59s. [Google Scholar]
- 10.Kasahun G.G., Gebretekle G.B., Hailemichael Y., Woldemariam A.A., Fenta T.G. Catastrophic healthcare expenditure and coping strategies among patients attending cancer treatment services in Addis Ababa, Ethiopia. BMC Public Health. 2020;20:1–10. doi: 10.1186/s12889-020-09137-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donkor A., Atuwo-Ampoh V.D., Yakanu F., et al. Financial toxicity of cancer care in low- and middle-income countries: a systematic review and meta-analysis. Support Care Cancer. 2022;30:7159–7190. doi: 10.1007/s00520-022-07044-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nair N., Shet T., Parmar V., et al. Breast cancer in a tertiary cancer center in India - an audit, with outcome analysis. Indian J Cancer. 2018;55:16–22. doi: 10.4103/ijc.IJC_484_17. [DOI] [PubMed] [Google Scholar]
- 13.Zheng A., Duan W., Zhang L., et al. How great is current curative expenditure and catastrophic health expenditure among patients with cancer in China? A research based on “System of Health Account 2011”. Cancer Med. 2018;7:4036–4043. doi: 10.1002/cam4.1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frieden T.R., Harold Jaffe D.W., Kent C.K., et al. Medical costs and productivity losses of cancer survivors — United States, 2008–2011. MMWR Morb Mortal Wkly Rep. 2014;63:505. [PMC free article] [PubMed] [Google Scholar]
- 15.Blumen H., Fitch K., Polkus V. 2016. Comparison of treatment costs for breast cancer, by tumor stage and type of service.www.AHDBonline.com [PMC free article] [PubMed] [Google Scholar]
- 16.Arozullah A.M., Calhoun E.A., Wolf M., et al. The financial burden of cancer care: estimates from a study of insured women with breast cancer. J Support Oncol. 2004;2:271–278. [PubMed] [Google Scholar]
- 17.Pramesh C.S., Badwe R.A., Borthakur B.B., et al. Delivery of affordable and equitable cancer care in India. Lancet Oncol. 2014;15:e223–e233. doi: 10.1016/S1470-2045(14)70117-2. [DOI] [PubMed] [Google Scholar]
- 18.Afkar A., Jalilian H., Pourreza A., Mir H., Sigaroudi A.E., Heydari S. Cost analysis of breast cancer: a comparison between private and public hospitals in Iran. BMC Health Serv Res. 2021;21:1–11. doi: 10.1186/s12913-021-06136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoang V.M., Pham C.P., Vu Q.M., et al. Household financial burden and poverty impacts of cancer treatment in Vietnam. BioMed Res Int. 2017;2017 doi: 10.1155/2017/9350147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehrotra R., Yadav K. Breast cancer in India: present scenario and the challenges ahead. World J Clin Oncol. 2022;13:209. doi: 10.5306/wjco.v13.i3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kulothungan V., Sathishkumar K., Leburu S., et al. Burden of cancers in India - estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on National Cancer Registry Program. BMC Cancer. 2022;22:1–12. doi: 10.1186/s12885-022-09578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Population finder | Government of India. https://censusindia.gov.in/census.website/data/population-finder
- 23.Singh M., Prasad C.P., Singh T.D., Kumar L. Cancer research in India: challenges & opportunities. Indian J Med Res. 2018;148:362. doi: 10.4103/ijmr.IJMR_1711_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhatia A., Victora C.G., Beckfield J., Budukh A., Krieger N. ‘Registries are not only a tool for data collection, they are for action’: cancer registration and gaps in data for health equity in six population-based registries in India. Int J Cancer. 2021;148:2171–2183. doi: 10.1002/ijc.33391. [DOI] [PubMed] [Google Scholar]
- 25.Behera P., Patro B.K. Population based cancer registry of India - the challenges and opportunities. Asian Pac J Cancer Prev. 2018;19:2885–2889. doi: 10.22034/APJCP.2018.19.10.2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NSSO . 2018. Key indicators of social consumption in India, health: NSSO 75st round (July 2017-June 2018)http://microdata.gov.in/nada43/index.php/catalog/152 New Delhi. [Google Scholar]
- 27.International Institute for Population Sciences (IIPS) and ICF . National Family Health Survey (NFHS-4), 2015-16. IIPS; Mumbai, India: 2017. [Google Scholar]
- 28.International Institute for Population Sciences (IIPS) and ICF . National Family Health Survey (NFHS-5), 2019-21. vol. I. IIPS; Mumbai, India: 2021. [Google Scholar]
- 29.Rajpal S., Kumar A., Joe W. Economic burden of cancer in India: evidence from cross-sectional nationally representative household survey, 2014. PLoS One. 2018;13 doi: 10.1371/journal.pone.0193320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kastor A., Mohanty S.K. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS One. 2018;13 doi: 10.1371/journal.pone.0196106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mohanty S., Wadasadawala T., Sen S., Khan P. Socio-economic variations of breast cancer treatment and discontinuation: a study from a public tertiary cancer hospital in Mumbai, India. BMC Womens Health. 2023;23:113. doi: 10.1186/s12905-023-02275-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lalanne C., Mesbah M. Biostatistics and computer-based analysis of health data using stata. 2016. Measures of association, comparisons of means and proportions for two samples or more; pp. 25–57. [Google Scholar]
- 33.Deb P., Norton E.C. Modeling health care expenditures and use. Annu Rev Public Health. 2018;39:489–505. doi: 10.1146/annurev-publhealth-040617-013517. [DOI] [PubMed] [Google Scholar]
- 34.Jones A. HEDG, Department of Economics, University of York, Health, Econometrics and Data Group (HEDG) Working Papers; 2010. Models for health care. [DOI] [Google Scholar]
- 35.Goyanka R., Yadav J., Sharma P. Financial burden and coping strategies for cancer care in India. Clin Epidemiol Glob Health. 2023;20 [Google Scholar]
- 36.Mittmann N., Porter J.M., Rangrej J., et al. Health system costs for stage-specific breast cancer: a population-based approach. Curr Oncol. 2014;21:281–293. doi: 10.3747/co.21.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Capri S., Russo A. Cost of breast cancer based on real-world data: a cancer registry study in Italy. BMC Health Serv Res. 2017;17:84. doi: 10.1186/S12913-017-2006-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pakseresht S., Ingle G.K., Garg S., Singh M.M. Expenditure audit of women with breast cancer in a tertiary care hospital of Delhi. Indian J Cancer. 2011;48:428–437. doi: 10.4103/0019-509X.92263. [DOI] [PubMed] [Google Scholar]
- 39.Alghamdi A., Balkhi B., Alqahtani S., Almotairi H. The economic burden associated with the management of different stages of breast cancer: a retrospective cost of illness analysis in Saudi Arabia. Healthcare. 2021;9:907. doi: 10.3390/HEALTHCARE9070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nair K.S., Raj S., Tiwari V.K., Piang L.K. Cost of treatment for cancer: experiences of patients in public hospitals in India. Asian Pac J Cancer Prev. 2013;14:5049–5054. doi: 10.7314/apjcp.2013.14.9.5049. [DOI] [PubMed] [Google Scholar]
- 41.Cocquyt V., Moeremans K., Annemans L., Clarys P., Van Belle S. Long-term medical costs of postmenopausal breast cancer therapy. Ann Oncol. 2003;14:1057–1063. doi: 10.1093/annonc/mdg280. [DOI] [PubMed] [Google Scholar]
- 42.Justo N., Wilking N., Jönsson B., Luciani S., Cazap E. A review of breast cancer care and outcomes in Latin America. Oncologist. 2013;18:248. doi: 10.1634/theoncologist.2012-0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.International Institute for Population Sciences (IIPS) and, Macro International. National Family Health Survey (NFHS-3), 2005–06. vol. I. IIPS; Mumbai, India: 2007. [Google Scholar]
- 44.Mohanty S.K., Upadhyay A.K., Maiti S., et al. Public health insurance coverage in India before and after PM-JAY: repeated cross-sectional analysis of nationally representative survey data. BMJ Glob Health. 2023;8 doi: 10.1136/bmjgh-2023-012725. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.