Abstract
Aim
To evaluate the effectiveness of Rapid Cycle Deliberate Practice (RCDP) compared to traditional instruction or other forms of learning on resuscitation training outcomes and on clinical and/or patient-related outcomes.
Methods
As part of the continuous evidence evaluation process of the International Liaison Committee on Resuscitation it was conducted this review and searched Medline, Embase and Cochrane from inception to Feb 12th, 2024. Risk of bias assessment was performed with the Risk of Bias in Non-randomized Studies of Interventions assessment tool and the Revised Cochrane risk-of-bias tool for randomized trials. The GRADE approach was used to evaluate the overall certainty of evidence for each outcome.
Results
4420 abstracts were retrieved by the initial search and 10 additional studies were identified through other resources. Sixty-five studies were selected for eligibility and nine simulated studies met the inclusion criteria. A meta-analysis was performed on three outcomes: time to chest compressions, time to defibrillation and time to first epinephrine given, which showed that RCDP had significantly shorter time to defibrillation and time to administration of epinephrine than controls. The overall certainty of evidence was very low across all outcomes due to risk of bias, inconsistency, indirectness, and imprecision.
Conclusion
It may be reasonable to include RCDP as an instructional design feature of basic and advanced life support training. However, substantial variations of delivering RCDP exist and there is no uniform use of RCDP. Further research is necessary on medium/long-term effects of RCDP training, and on the effects on different target groups of training.
Keywords: Medical education, Simulation, Debriefing, Basic life support, Advance cardiac life support, Learning, Rapid Cycle Deliberate Practice, Resuscitation
Introduction
Simulation-based training has become well established within healthcare education,1 as it allows learning in a controlled environment without putting patients or trainees at risk.2 Specifically in resuscitation training it facilitates context-related learning of both, technical and non-technical skills for lay people to highly professional resuscitation teams.3
Although some aspects related to simulation training were studied and effectiveness proved such as the use of high-fidelity manikins[3], [4] or debriefing,5 other instructional design factors should be addressed and investigated.6 In this regard, for such simulation-based resuscitation training, Hunt et al.7 designed a competency-based curriculum named “Rapid Cycle Deliberate Practice” (RCDP). Applying RCDP means the simulations scenario is stopped at certain points, when the facilitator gives the learners feedback on the task performed until the stop. Thus, learners received short specific feedback during the scenario and not after its completion. RCDP creates a safe environment, giving multiple opportunities to “do it right” with ample time for repetition to improve performance, creating muscle memory for the “right way”.7 RCDP is much more than a new type of debriefing, accurately it is a simulation instructional method.
The aim of this systematic review was to evaluate the use of RCDP as an instructional design method compared with other forms of learning, and determine the impact of RCDP on educational, clinical, and/or patient-related outcomes.
Methods
This systematic review was conducted as part of the continuous evidence evaluation process of the International Liaison Committee on Resuscitation (ILCOR) Education, Implementation and Teams (EIT) Task Force.[8], [9] It was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Supplementary file 1),10 and the study protocol was published in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42023468862).
Search strategy
The search was conducted through the following databases: Medline, Embase, Cochrane Database of Systematic Reviews (CDSR) and Cochrane Central Register of Controlled Trials (CCRCT) (Supplementary file 2). The addition of the Cochrane databases was decided after discussion within the Task Force, after the protocol registration. It was the only deviation from the registered protocol. Grey literature was not searched. Reference lists of included studies and review articles were revised to identify potential additional publications. The research question was structured in the PICOST format (Population, Intervention, Comparison, Study design, Timeframe) showed in Table 1.
Table 1.
Research according PICOST structure.
| Population | Learners training in basic or advanced life support (laypersons/students/healthcare providers). |
| Intervention | Instruction using RCDP. |
| Comparison | Compared to traditional instruction or other forms of learning without RCDP. |
| Outcomes | Patients’ survival (CRITICAL), knowledge acquisition and retention (IMPORTANT), skills acquisition and retention (IMPORTANT), skill performance in real CPR (IMPORTANT), process outcomes such as costs, resources (NOT IMPORTANT). |
| Study design | Randomized controlled trials (RCTs) and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies) and research letters were eligible for inclusion. |
| Timeframe | All years and all languages were included as long as there was an English abstract; unpublished studies (e.g., conference abstracts, trial protocols) were excluded. Literature search was performed from inception to Feb 12th, 2024. |
CPR: Cardiopulmonary resuscitation; RCDP: Rapid Cycle Deliberate Practice.
Definitions
For the purposes of this systematic review, we defined RCDP as an instructional design method with rapid cycling between deliberate practice and directed feedback until skill mastery is achieved.7 Training scenarios are interrupted at predetermined points; during the interruptions the facilitator gives formative and/or corrective feedback on tasks performed to that point. Thus, the debriefing in RCDP is done in brief and frequent ‘doses’ during the scenario and not in a summative fashion after the scenario is completed. The key points of rapid cycle deliberate practice are: 1) there is a goal to achieve; 2) Stop-and-go practice with immediate feedback on the performance, pausing the scenario when observing errors; 3) Ample time for repetition to improve performance; 4) “Safe” environment, fostering an atmosphere where students have no fear to make mistakes and receive feedback from a constructive perspective.
Study selection, data extraction, and risk of bias assessment
Both screening and eligibility were independently performed by two pairs of authors to minimize potential bias (CAG and AC; AD and TS) using Rayyan software.11 If there were disagreements, both reviewers discussed to reach consensus. Data extraction of the final inclusions was performed by one reviewer (CAG) and checked and ratified by co-authors (AC, AD, TS).
Risk of bias assessment was performed with the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I)12 assessment tool and the Revised Cochrane Risk-of-Bias tool for randomized trials (RoB 2).13 The evaluation of risk of bias was appraised by two reviewers (CAG and AD). When there were disagreements, consensus was reached by discussion. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to evaluate the overall certainty of evidence for each outcome.
Data extraction, risk of bias assessment and GRADE tables were presented and discussed by the EIT Task Force members during several virtual meetings.
Data analysis
We used meta-analysis to synthesize evidence of those outcomes reported by more than two articles. The analysis was carried out using the standardized mean difference as summary statistics for meta-analysis. A random-effects model was fitted to the data. Statistical heterogeneity was measured with I2 statistic. The analysis was performed using Jamovi 2.5 (https://www.jamovi.org).
Results
Study characteristics
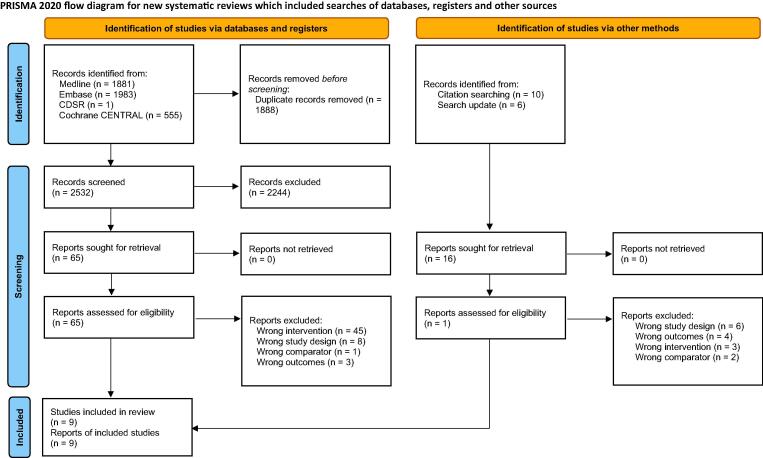
The initial search retrieved 4420 abstracts and 10 additional studies were identified through checking the list of references (Fig. 1). After removing duplicates, 2532 records were screened. Sixty-five articles were selected for eligibility, and nine studies were identified that addressed the PICOST question comparing Rapid Cycle Deliberate Practice (RCDP) with other approaches.[7], [14], [15], [16], [17], [18], [19], [20], [21]
Fig. 1.
PRISMA flow diagram.
Eight studies were carried out in United States[7], [14], [15], [16], [19], [20], [21] and one in Brazil.18 Study cohorts were comprised of residents,[7], [15], [20] interns,[16], [17], [21] physicians,18 medical students,19 and a mix of fellows, nurses and respiratory therapists,14 who were involved in adult,[18], [19], [21] pediatric,[7], [14], [15], [17], [20] and neonatal16 simulated scenarios. Most of the studies reported comparisons between RCDP and other approaches (e.g. after-event debriefing) after a single session of simulation-based training, lasting 20–75 min.[14], [15], [16], [18], [19], [20], [21]
Eight were randomized studies with parallel-group[15], [16], [17], [18], [19], [20], [21] or crossover14 designs and one an observational study with a before-after design7; all of them were simulated studies. Table 2 shows the characteristics of the studies including the population, description of the studies, intervention, and comparator, as well as the relevant key findings, and the supplementary file 3 provides more information on the primary endpoints, results, conclusions, and comments on the limitations. Eight of the studies referred directly to RCDP, 7,14-18,20,21 the other one used an “in-simulation debriefing” during the clinical scenario meeting the key components of the RCDP.19 No studies reported clinical or patient-related outcomes, or other outcomes related to process outcomes.
Table 2.
Data extraction of the nine studies included (simulated studies).
| First author; Year; Country |
Study design |
Sample size, intervention, and comparator | Population | Description of methods | Key relevant findings |
|---|---|---|---|---|---|
| Hunt; 2014; USA7 | Observational; Before-after design | 121 participants Intervention: High-fidelity pediatric simulations with RCDP (post-RCDP). (n = 51) Comparator: High-fidelity simulation with debriefing after the resolution of the case (pre-RCDP). (n = 70) |
Pediatric residents from the tertiary care, academic Johns Hopkins hospital |
BLS during intern orientation, PALS and monthly in situ mock-codes on the wards and sporadic mock codes on other rotations. Multiple sessions (pediatric simulations) |
RCDP curriculum was associated with improved performance by pediatric residents during simulated pediatric cardiopulmonary arrest. |
| Lemke; 2019; USA14 | Randomized crossover trial | 30 participants split into 8 teams Intervention: 45-min each of the three simulated pediatric resuscitation scenarios with RCDP intervention. (n = 30; 4 teams) Comparator: 45-min each of the three simulated pediatric resuscitation scenarios with after-event debriefing. (n = 30; 4 teams) |
Pediatric emergency medicine fellows, nurses, and respiratory therapist from the Texas Children’s Hospital | One scenario as pre- and post-assessment with three training scenarios. After 3-month wash-out, teams received training with the other methodology. 45-min single session (pediatric simulations) |
This study showed a trend toward greater improvement in team performance for RCDP. |
| Lemke; 2021; USA15 | RCT | 229 participants split into 41 teams Intervention: Simulated pediatric resuscitation scenario with RCDP intervention. (n = 108; 20 teams) Comparator: Simulated pediatric resuscitation scenario with after-event debriefing using the PEARLS method. (n = 112; 21 teams) |
Pediatric and emergency residents from the Texas Children’s Hospital | 1-h single session (pediatric simulations) |
Teams trained using RCDP were faster to defibrillate and demonstrated less frustration and workload. |
| Magee; 2018; USA16 | RCT | 34 participants Intervention: Simulated neonatal resuscitation scenario with RCDP intervention. (n = 17) Comparator: Simulated neonatal resuscitation scenario with after-event debriefing. (n = 17) |
Pediatric interns with Neonatal Resuscitation Program certification | 45-min single session (neonatal simulations) | Pediatrics interns had improved observed abilities and decreased time to perform critical interventions in NR simulation immediately following RCDP as compared to those trained with the after-event debriefing method. Neither approach was superior in improving confidence level and recall 4 months later. |
| Raju; 2020; USA17 | RCT | 22 participants Intervention: RDCP booster session at 9 months after initial session. Comparator: booster session with standard plus/delta debriefing at 9 months. |
Pediatric and internal medicine/pediatric postgraduate year 1 (PGY) at the Children's of Alabama, University of Alabama at Birmingham |
All subjects did initial sessions (pre-training followed by RDCP training) and a 6-month test scenario with plus/delta debriefing. 20–30 min single session (pediatric simulations) |
Initial RDCP session was effective; booster session at 9 months did not influence performance at 12 months. |
| Teixeira de Castro; 2022; Brazil18 | RCT | 76 participants split into 10 teams Intervention: Simulated adult CA scenario with RCDP intervention. (n = 42; 5 teams) Comparator: Simulated CA scenario with after-event debriefing using the PEARLS method. (n = 34; 4 teams) |
Physicians enrolled in the Emergency Medicine post-graduate Course of the Hospital Israelita Albert Einstein |
Theoretical training in emergency cardiovascular care and discussion regarding the management of CA (common part). 40-min single session (adult simulations) |
RCDP strategy is associated with better performance of resuscitation teams in critical actions during care for CA. |
| Van Heukelom; 2010; USA19 | RCT | 161 participants Intervention: Simulated adult ACLS scenario with in-simulation intervention. (n = 84) Comparator: Simulated adult ACLS scenario with after-event debriefing intervention. (n = 77) |
Third year medical students enrolled in the “Clinical Procedures Rotation” at the Medical College of Wisconsin | 20-min single session (adult simulations) | Simulation was an effective learning tool that significantly increases the confidence in the ability to perform critical care skills of third medical students. After-event debriefing was better rated by the participants than in-simulation intervention. |
| Won; 2022; USA20 | RCT | 32 participants Intervention: Simulated pediatric resuscitation scenario with RCDP intervention. (n = 16) Comparator: Simulated pediatric resuscitation scenario with after-event debriefing using the PEARLS method. (n = 16) |
Pediatric and emergency residents from the Texas Children’s Hospital |
1-h single session (pediatric simulations) | Residents trained using RCDP were more likely to achieve defibrillation faster and perform more effectively as team leader than those trained using after-event debriefing. |
| Raper; 2024; USA21 | RCT | 55 participants Intervention: Simulated adult resuscitation scenario with RCDP intervention. (n = 28) Comparator: Immersive simulation with after-event debriefing. (n = 27) |
Internal and emergency medicine PGY-1 at University of Alabama at Birmingham | 45–75-min single session (adult simulations) | Although it was observed a trend in favor of RCDP group to decrease time to perform ACLS interventions, only differences were found in one of the time intervals assessed. |
ACLS: Advanced cardiac life support; BLS: Basic life support; CA: Cardiac arrest; PALS: Pediatric advanced life support; PEARLS: Promoting Excellence and Reflective Learning in Simulation; RCDP: Rapid Cycle Deliberate Practice; RCT: Randomized control trial; STAT: Simulation Team Assessment Tool.
The risk of bias assessment is shown in Table 3. The observational study included was assessed as at overall serious risk of bias due to cofounding.7 In six of the randomized studies some concerns were found,[14], [17], [18], [19], [20], [21] mainly for randomization processes.[14], [17], [19] One randomized study was assessed as overall serious risk of bias due to the randomization process, missing data, and measurement of outcomes.16
Table 3.
Risk of Bias assessment.
| Non-randomized studies (ROBINS-1). | ||||||||
|---|---|---|---|---|---|---|---|---|
| First author; year | Confounding | Selection of participants | Classification of interventions | Deviations from intended interventions | Missing data | Measurement of outcomes | Selection of reported results | Overall |
| Hunt; 201477 | Serious | Low | Low | Low | Low | Moderate | Low | Serious |
| Randomized studies (RoB 2). | ||||||||
| First author; year | Randomization process | Deviation from intended interventions | Missing outcome data | Measurement of outcomes | Selection of reported results | Overall | ||
| Lemke; 201914 | Some concerns | Low | Low | Low | Low | Some concerns | ||
| Lemke; 202115 | Low | Low | Low | Low | Low | Low | ||
| Magee; 201816 | Some concerns | Low | Some concerns | Some concerns | Low | High | ||
| Raju; 202117 | Some concerns | Low | Low | Low | Low | Some concerns | ||
| Teixeira de Castro; 202218 | Low | Low | Low | Low | Some concerns | Some concerns | ||
| Van Heukelom; 201019 | Some concerns | Low | Low | Some concerns | Low | Some concerns | ||
| Won; 202220 | Low | Low | Low | Some concerns | Low | Some concerns | ||
| Raper; 202421 | Low | Low | Low | Low | Low | Some concerns | ||
The overall certainty of evidence was very low across all outcomes due to risk of bias, inconsistency, indirectness, and imprecision. GRADE summary tables are provided in supplementary file 4.
Meta-analysis on the time to tasks performance in simulated scenarios
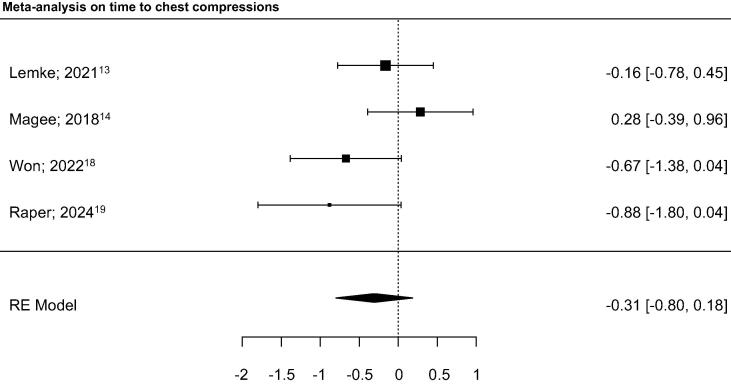
We were able to perform meta-analysis only for the outcomes time to chest compressions, time to defibrillation and time to first epinephrine due to the low number of studies per outcome, heterogeneity in the study designs and the reported outcome measures.
Time to chest compressions was included in four randomized studies,[15], [16], [20], [21] and the observational study,7 and showed no benefit from the use of RCDP compared to after-event debriefing (Fig. 2). There was low to moderate heterogeneity (I2 = 46.7 %). The observational study reported significantly less time between the onset of pulseless ventricular tachycardia and initiation of chest compressions for participants in the RCDP group.7
Fig. 2.
Time to chest compression. The estimated standardized mean difference did not differ significantly from zero (z = -1.2230, p = 0.2213). I2 = 46.7 %.
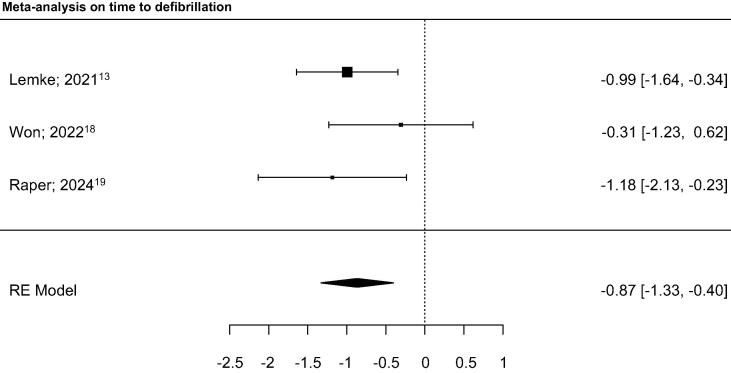
Time to defibrillation was assessed by five studies (four randomized[15], [18], [20], [21] and the observational7) of which three were included in the meta-analysis,[15], [20], [21] showing that RCDP group had significantly less time between recognition of the rhythm and defibrillation (Fig. 3). There was low heterogeneity (I2 < 1.0 %). The RCT not included in the meta-analysis due to reported outcome measures found that RCDP trained participants needed significantly lower time to recognize the rhythm and to defibrillation.18 The same was found for the observational study.7 RCDP trained participants needed significantly less time to detect pulseless ventricular tachycardia and to execute defibrillation and had 1.65 times the odds of defibrillating within two minutes (p = 0.04).7 In another RCT, RCDP participants had more than five times the odds of defibrillation occurring within three minutes (p = 0.04).20
Fig. 3.
Time to defibrillation. The estimated standardized mean difference differs significantly from zero (z = -3.6620, p < 0.001) in favor of RCDP. I2 < 1.0 %.
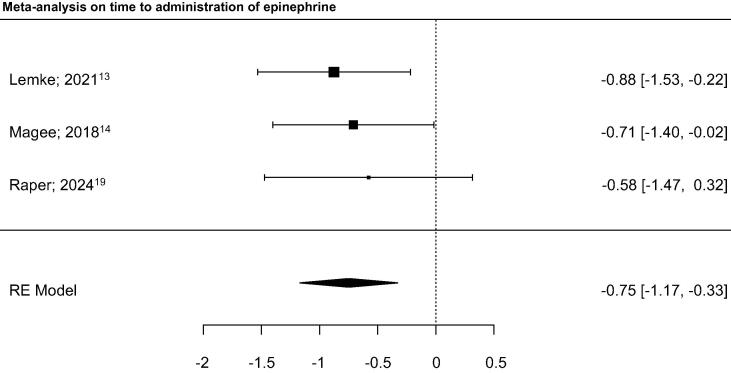
Time to the administration of the first epinephrine was assessed in three randomized studies,[15], [16], [21] showing that RCDP participants had significantly shorter time to the administration of epinephrine than controls (Fig. 4). There was low heterogeneity (I2 < 1.0 %).
Fig. 4.
Time to administration of epinephrine. The estimated standardized mean difference differs significantly from zero (z = -3.4868, p < 0.001) in favor of RCDP. I2 < 1.0 %.
Time to recognize cardiac arrest reported in one RCT found no differences between groups.18 In another RCT, participants with RCDP initiated positive pressure ventilation within one minute more frequently than controls (p = 0.05),16 while the observational study showed no differences on time to use bag-valve mask.7.
Cardiopulmonary resuscitation and defibrillation
One RCT reported compression fraction,18 while the observational study no-flow and no-ventilation fraction (proportion of time a pulseless patient received no respiratory support).7 Both favor the performance of RCDP participants.
One RCT18 and the observational study7 reported defibrillation pre-pause and found that RCDP participants registered significantly shorter defibrillation pre-pause.
Adherence to guidelines
Three randomized studies evaluated quality of performance with different tools.[14], [16], [17] RCDP participants reached higher performance scores using the Megacode Assessment Form,16 but no differences were found with the Simulation Team Assessment Tool12 or Pediatric Advance Life Support performance.17
Other outcomes
One RCT showed higher scores in the RCDP group for team leader performance.20 Workload was reported in another RCT, with lower weighted score in RCDP participants compared to participants having after-event debriefing (p = 0.02).15 Stress experienced was significantly lower in RCDP participants compared with controls in an RCT (p = 0.01).21 A RCT found high-median scores for teaching effectiveness in three of the eight questions (help to learn effectively, help to understand the correct actions, effectiveness of the debriefing) in the after-event debriefing group compared to the RCDP group.19 Retention of skills was reported in one RCT (4-month follow-up) without any significant difference between groups in any variable.16
Discussion
This systematic review represents the most up-to-date evidence synthesis on the effect of Rapid Cycle Deliberate Practice on resuscitation education. All the included articles compared RCDP training with training having after-event debriefing. The evidence from this systematic review shows several favorable outcomes that supports training effectiveness with the use of RCDP in resuscitation simulation training.7,14-18,20,21 However, no evidence was found about the effect of RCDP on clinical and patient-related outcomes. A meta-analysis was possible on three outcomes, showing evidence in favor of RCDP for skill acquisition of time to defibrillate and time to administer first epinephrine, but not for time to chest compressions.
RCDP aims to maximize the time of practice during scenario simulation, creating multiple opportunities to “do it right”.7 In addition, corrective feedback is given by instructors in a ‘just-in-time’ fashion throughout the scenario, supporting immediate reflection and correction.[7], [22] Therefore, RCDP is more than another type of debriefing, and according to Hunt et al.,7 it is a simulation instructional method.22
From an andragogical perspective, RCDP recommends scaffolding the progression of complexity of skills or scenario simulations. That can be achieve either by progressing and increasing difficulty using the same scenario;[14], [15], [18], [20] or across different scenarios.7
Repeated practice without feedback from an instructor may lead incorrect performance or the cultivation of suboptimal habits.22 Although learners should be allowed to make mistakes and errors,23 RCDP forces instructors to stop the scenario when those happened.22 Interestingly, several studies included in this systematic review reported that scenarios were divided in different cycles, having assigned to each cycle different goals to be achieved. More and more steps were added until the final cycle, in which participants had to perform the whole set of skills and participants received feedback from instructors.[14], [15], [18], [20]
As awareness and experience with this method has increased over time, RCDP has become an instructional design element in an increasing number of resuscitation-related curriculums in recent years.[24], [25], [26] Originally, the essence of the RCDP instructional method was that the instructor intervenes when an error is noticed. However, others used RCDP by stopping the scenario only at the end cycle,[27], [28] gave feedback at the end of the case and then re-run the scenario,29 or allowed any learner to stop scenarios at any moment.30 This heterogeneity in the use of the term “RCDP” and its application differs in some aspects such as the use (or not) of round/cycles or stop-and-go approaches. In contrast to this, a systematic review in 2017 and a scoping review in 2021 about RCDP in medical education agree that RCDP definition is consistent across the literature.[31], [32]
Limitations
Our systematic review relied on a relatively limited number of databases, although we also applied snowballing method by reviewing reference lists of included studies and the recent systematic reviews about RCDP. In addition, this review had narrow inclusion criteria, since only studies about resuscitation were included. Additionally, studies that lacked a comparator group (i.e. studies that compared RCDP to no other type of intervention) were excluded. Our systematic review found more pronounced differences in favor of RCDP compared to after-event debriefing, although most of the studies had trainees as participants, making difficult to generalize the findings to other groups. Due to the heterogeneous study designs we could only perform meta-analysis on three outcomes, and more studies are needed to provide more evidence on the effect of RCDP on resuscitation related outcomes. Finally, most studies reported that the simulations lasted only for one session,[14], [15], [16], [18], [19], [20], [21] which might reduce the effect of the RCDP training in comparison with curriculums based on RCDP.
Knowledge gaps
We identified several knowledge gaps with the use of RCDP on resuscitation training. As mostly RCDP was studied in single sessions, the effect of the implementation of entire curriculums based on RCDP is unknown, especially on clinical outcomes and patient survival. Hunt et al. evaluated the effect of the integration of a cardiac arrest contextual curriculum into a basic life support course, reporting improvements on performance on hospital-specific quality measures on RCDP participants compared with controls trained with a traditional American Heart Association course.33 However, we excluded this article because we were unable to isolate the effect of RCDP from other instructional elements also included in the intervention.
The effect of RCDP after medium/long-term follow-up is another knowledge gap. Only one study included in this systematic review reported medium-term effect after four months without differences between RCDP participants and controls on quality of performance and confidence level.16
The effect of the use of RCDP in other populations beyond health care students, such as lay people, community first responders, or experienced healthcare providers, and the resources required and costs of implementation in simulation-based training curriculum of health care providers and other populations is also unknown.
The effectiveness of RCDP depends on feedback mechanisms, realism of the simulation, and integration of RCDP principles into the overall training program. Therefore, it will not only be essential to tailor resources such as simulation equipment (manikins, software), instructors training (expertise in debriefing and feedback), curriculum development, and educational and evaluation tools, but also to report these factors in RCTs to allow proper comparisons and analysis of such educational interventions. Finally, there is substantial heterogeneity in the use of the term RDCP and there is no standardized use of RDCP.
Conclusions
Based on the summary of the evidence found in this systematic review it may be reasonable to include Rapid Cycle Deliberate Practice as an instructional design feature of basic and advanced life support training. However, substantial variations of delivering Rapid Cycle Deliberate Practice exist and there is no uniform use of this instructional design. Further research is necessary on medium/long-term effects of Rapid Cycle Deliberate Practice training, and on the effects on different target groups of training.
Funding
This Systematic Review was funded by the American Heart Association, on behalf of The International Liaison Committee on Resuscitation (ILCOR).
CRediT authorship contribution statement
Cristian Abelairas-Gómez: Writing – original draft, Visualization, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Andrea Cortegiani: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Taylor Sawyer: Writing – review & editing, Methodology, Investigation, Data curation, Conceptualization. Robert Greif: Writing – review & editing, Supervision, Project administration, Methodology, Funding acquisition, Conceptualization. Aaron Donoghue: Writing – review & editing, Methodology, Investigation, Data curation, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: CAG is member of ILCOR’s Task Force on Education, Implementation, and Teams, and ERC Basic Life Support Science and Education Committee member. AC, AD and TS are members of ILCOR’s Task Force on Education, Implementation, and Teams. RG is the ERC Director of Guidelines and ILCOR, Chair of ILCOR’s Task Force on Education, Implementation, and Teams, and Editorial Board member of Resuscitation Plus.
Acknowledgements
The authors acknowledge the assistance provided by Mary-Doug Wright, Informational Specialist at Apex Information, Vancouver, Canada, for building up the searching strategy. The following ILCOR EIT Task Force members are acknowledged as collaborators in this systematic review: Natalie Anderson, Farhan Bhanji, Jan Breckwoldt, Adam Cheng, Kathryn Eastwood, Barbara Farquharson, Ming-Ju Hsieh, Ying-Chih Ko, Elina Koota, Kasper Lauridsen, Yiquin Lin, Andrew Lockey, Sabine Nabecker, Kevin Nation, Tasuku Matsuyama, Alexander Olaussen, Sebastian Schnaubelt, Chih-Wei Yang, Joyce Yeung.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100648.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Kneebone R. Evaluating clinical simulations for learning procedural skills: A theory-based approach. Acad Med. 2005;80:549–553. doi: 10.1097/00001888-200506000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Perkins G.D. Simulation in resuscitation training. Resuscitation. 2007;73:202–211. doi: 10.1016/j.resuscitation.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Greif R., Lockey A., Breckwoldt J., et al. European resuscitation council guidelines 2021: education for resuscitation. Resuscitation. 2021;161:388–407. doi: 10.1016/j.resuscitation.2021.02.016. [DOI] [PubMed] [Google Scholar]
- 4.Greif R., Bhanji F., Bigham B.L., et al. On behalf of the education, implementation, and teams collaborators. education, implementation, and teams: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142:S222–S283. doi: 10.1161/CIR.0000000000000896. [DOI] [PubMed] [Google Scholar]
- 5.Sawyer T., Eppich W., Brett-Fleegler M., Grant V., Cheng A. More than one way to debrief: a critical review of healthcare simulation debriefing methods. Simul Healthc. 2016;11:209–217. doi: 10.1097/SIH.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 6.Cheng A., Lockey A., Bhanji F., et al. The use of high-fidelity manikins for advanced life support training—A systematic review and meta-analysis. Resuscitation. 2015;93:142–149. doi: 10.1016/j.resuscitation.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Hunt E.A., Duval-Arnould J.M., Nelson-McMillan K.L., et al. Pediatric resident resuscitation skills improve after “rapid cycle deliberate practice” training. Resuscitation. 2014;85:945–951. doi: 10.1016/j.resuscitation.2014.02.025. [DOI] [PubMed] [Google Scholar]
- 8.Peter T., Morley P.T., Atkins D.L., Fin J.C., et al. Evidence evaluation process and management of potential conflicts of interest: 2020 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A23–A34. doi: 10.1016/j.resuscitation.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 9.Peter T., Morley P.T., Atkins D.L., Fin J.C., et al. Evidence evaluation process and management of potential conflicts of interest: 2020 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142:S28–S40. doi: 10.1161/CIR.0000000000000891. [DOI] [PubMed] [Google Scholar]
- 10.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sterne J.A., Hernan M.A., Reeves B.C., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355 doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sterne J.A.C., Savovic J., Page M.J., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366 doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 14.Lemke D.S., Fielder E.K., Hsu D.C., Doughty C.B. Improved team performance during pediatric resuscitations after rapid cycle deliberate practice compared with traditional debriefing. A Pilot Study. Pediatr Emer Care. 2019;35:480–486. doi: 10.1097/PEC.0000000000000940. [DOI] [PubMed] [Google Scholar]
- 15.Lemke D.S., Young A.L., Won S.K., et al. Rapid-cycle deliberate practice improves time to defibrillation and reduces workload: A randomized controlled trial of simulation-based education. AEM Educ Train. 2021;5 doi: 10.1002/aet2.10702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magee M.J., Farkouh-Karolesk C., Rosen T.S. Improvement of immediate performance in neonatal resuscitation through rapid cycle deliberate practice training. J Grad Med Educ. 2018;10:192–197. doi: 10.4300/JGME-D-17-00467.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raju S.S., Tofil N.M., Gaither S.L., et al. The impact of a 9-month booster training using rapid cycle deliberate practice on pediatric resident PALS skills. Simul Healthc. 2021;16:e168–e175. doi: 10.1097/SIH.0000000000000538. [DOI] [PubMed] [Google Scholar]
- 18.Teixeira de Castro L., Melo Coriolano A., Burckart K., et al. Rapid cycle deliberate practice versus after event debriefing clinical simulation in cardiopulmonary resuscitation: a cluster randomized trial. Advances. Simulation. 2022;7:43. doi: 10.1186/s41077-022-00239-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Heukelom J.N., Begaz T., Treat R. Comparison of postsimulation debriefing versus in-simulation debriefing in medical simulation. Simul Healthc. 2010;5:91–97. doi: 10.1097/SIH.0b013e3181be0d17. [DOI] [PubMed] [Google Scholar]
- 20.Won S.K., Doughty C.B., Young A.L., et al. Rapid cycle deliberate practice improves retention of pediatric resuscitation skills compared with postsimulation debriefing. Simul Healthc. 2022;17:e20–e27. doi: 10.1097/SIH.0000000000000568. [DOI] [PubMed] [Google Scholar]
- 21.Raper J.D., Khoury C.A., Marshall A., et al. Rapid Cycle Deliberate Practice training for simulated cardiopulmonary resuscitation in resident education. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health. 2024 doi: 10.5811/westjem.60319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perretta J.S., Duval-Arnould J., Poling S.M., et al. Best practices and theoretical foundations for simulation instruction using rapid-cycle deliberate practice. Simul Healthc. 2020;15:356–362. doi: 10.1097/SIH.0000000000000433. [DOI] [PubMed] [Google Scholar]
- 23.McKenzie I., Ohayon D., Li H., et al. Motor skill learning requires active central myelination. Science. 2014;346:318–322. doi: 10.1126/science.1254960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lemke D.S. Rapid cycle deliberate practice for pediatric intern resuscitation skills. MedEdPORTAL. 2020;16:11020. doi: 10.15766/mep_2374-8265.11020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zern S.C., Marshall W.J., Shewokis P.A., et al. Use of simulation as a needs assessment to develop a focused team leader training curriculum for resuscitation teams. Adv Simul. 2020;5:6. doi: 10.1186/s41077-020-00124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yan D.H., Slidell M.B., McQueen A. Using rapid cycle deliberate practice to improve primary and secondary survey in pediatric trauma. BMC Med Educ. 2020;20:131. doi: 10.1186/s12909-020-02038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosman S.L., Nyirasafari R., Bwiza H.M., et al. Rapid cycle deliberate practice vs. traditional simulation in a resource-limited setting. BMC Med Educ. 2019;19:314. doi: 10.1186/s12909-019-1742-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang S.-Y., Oh Y.-H. Development and effectiveness of a rapid cycle deliberate practice neonatal resuscitation simulation program: A quasi-experimental study. Healthcare. 2024;12:104. doi: 10.3390/healthcare12010104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tucker G., Urwin C., Tomietto M., Unsworth J. The impact of rapid cycle simulation deliberate practice on nursing student's resuscitation self-efficacy: A quasi-experimental study. Nurse Educ Pract. 2023;73 doi: 10.1016/j.nepr.2023.103841. [DOI] [PubMed] [Google Scholar]
- 30.Nichols B.E., McMichael A.B.V., Volk A.P.D., Davis M.D., Bhaskar P., Bowens C.D. CPR during COVID-19: use of expert-driven rapid cycle deliberate practice to implement PALS guidelines. Pediatr Qual Saf. 2021;6:e374. doi: 10.1097/pq9.0000000000000374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taras J., Everett T. Rapid cycle deliberate practice in medical education - a systematic review. Cureus. 2017;19:e1180. doi: 10.7759/cureus.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ng C., Primiani N., Orchanian-Cheff A. Rapid cycle deliberate practice in healthcare simulation: a scoping review. Med Sci Educ. 2021;31:2105–2120. doi: 10.1007/s40670-021-01446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hunt E.A., Duval-Arnould J.M., Chime N.O., et al. Integration of in-hospital cardiac arrest contextual curriculum into a basic life support course: a randomized, controlled simulation study. Resuscitation. 2017;114:127–132. doi: 10.1016/j.resuscitation.2017.03.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.