Abstract
Propylene glycol (PG) is a diol (a double alcohol) that is commonly used as a food additive to preserve shelf life and enhance flavors, texture, and appearance. Although PG makes up only a small percentage of cornstarch, ingestion of large doses can cause lactic acidosis leading to hyperosmolarity, high anion gap metabolic acidosis (HAGMA), and a sepsis‐like syndrome.
A 17‐year‐old female presented to our emergency department (ED) with chronic chest pain, dyspnea, nausea, and vomiting. Laboratory testing showed an elevated anion gap of 18 mEq/L with no osmolar gap. Toxicology screening was negative. Twelve hours after ED arrival, she admitted to consuming one box of cornstarch daily for the past 6 months. She was admitted to the intensive care unit (ICU) with multisystem organ failure due to propylene glycol toxicity. After empiric treatment with fomepizole and continuous renal replacement therapy, her clinical status gradually improved. This case highlights the importance of obtaining a thorough dietary history in patients with suspected toxicities, especially when laboratory values demonstrate an unexplained HAGMA and/or lactic acidosis. Prompt recognition and therapeutic intervention with fomepizole, a potent inhibitor of alcohol dehydrogenase, is essential in reducing life‐threatening sequelae following toxic alcohol ingestions.
Keywords: anion gap metabolic acidosis, cornstarch, lactic acidosis, propylene glycol, toxic alcohol
1. INTRODUCTION
Propylene glycol (PG) is a diol (a double alcohol) that is commonly used as a food additive to preserve shelf life and enhance flavors, texture, and appearance. 1 PG is generally recognized as safe by the US Food and Drug Administration. 1 , 2 Ingested PG is readily absorbed and then partially excreted by the kidneys and partially metabolized. 3 Oxidation, primarily via alcohol and aldehyde dehydrogenase, generates both the D and L optical isomers of lactic acid (see Figure 1). 3 Cornstarch contains PG; unfortunately, the exact amount in various cornstarch products is not well defined and often will not be provided by the manufacturer. We report the case of a young woman who developed profound high anion gap metabolic acidosis (HAGMA), which we believe was secondary to chronic cornstarch ingestion.
FIGURE 1.
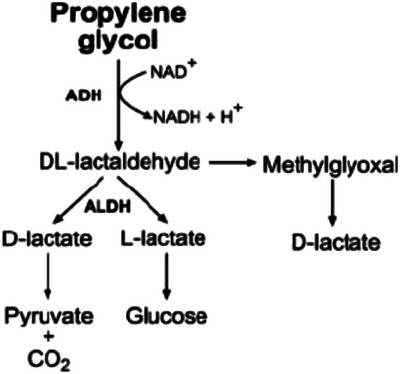
Metabolic pathway of propylene glycol. ADH, alcohol dehydrogenase; ALDH, aldehyde dehydrogenase.
2. CASE REPORT
A 17‐year‐old woman presented to the emergency department (ED) with chronic chest pain, dyspnea, nausea, and vomiting. The chest pain had been present for about 6 months, was intermittent, and relieved with rest. Two days prior to ED arrival, the pain became more severe and constant and was described as a non‐radiating burning sensation. She had a history of asthma and heavy, irregular menstrual periods. On presentation, she was afebrile (36.7°C), normotensive (95/54 mmHg), tachycardic (111 beats per minute), and tachypneic (39 respirations per minute). Oxygen saturation was 100% on room air. The primary abnormality noted on physical examination was tachycardia. Electrocardiogram (ECG) revealed sinus tachycardia without repolarization changes. She was given 1 L of IV lactated ringer's solution, 4 mg of ondansetron, 10 mg of IV ketorolac, and 1000 mg of acetaminophen.
Initial laboratory tests are shown in Table 1. Serum ethanol and acetaminophen levels were undetectable. Salicylate level was undetectable (< 0.7 mg/dL) and beta‐hydroxybutyrate level was <0.5 mmol/L. Comprehensive drug screen results are shown in Table 2. Blood cultures were drawn, and empiric vancomycin and cefepime were initiated. Bedside transthoracic echocardiogram, chest x‐ray, computed tomography angiogram (CTA) chest, and CTA abdomen/pelvis showed no abnormalities. d‐dimer levels were within the accepted reference range and qualitative β‐human chorionic gonadotropin (hCG) level was negative.
TABLE 1.
Laboratory analysis.
| Parameter | Initial values | Values at pediatric hospital | Reference values |
|---|---|---|---|
| Hemoglobin (g/dL) | 9.4 | NA | 12–16 |
| Hematocrit (%) | 29.1 | NA | 36–47 |
| Mean corpuscular volume (µm3) | 72.2 | NA | 80–99 |
| High‐sensitivity troponin (ng/L) | 26 | 4832.90 | <14 |
| Sodium (mEq/L) | 138 | 136 | 136–145 |
| Potassium (mEq/L) | 4 | 5.7 | 3.5‐5.1 |
| Chloride (mEq/L) | 106 | 105 | 98–107 |
| CO2 (mEq/L) | 14 | <10 | 18–31 |
| Serum anion gap (mEq/L) | 18 | Unable to calculate | 6–16 |
| Serum osmolarity (mOsm/kg) | 290 | 338 | 275–296 |
| Serum osmolar gap (mOsm/kg) | <10 | 57 | <10 |
| pH | 7.25 | 6.87 | 7.25–7.45 |
| pO2 (mmHg) | 54 | 61 | 30–40 |
| pCO2 (mmHg) | 17 | 10 | 41–51 |
| HCO3 (mEq/L) | 7 | 2 | 21–26 |
| l‐Lactic acid (mg/dL) | 63.96 | 173.69 | 8.11–15.32 |
| Urine d‐lactic acid (mmol/L) | N/A | 1.04 | 0.0–0.25 |
| BUN (mg/dL) | 6 | 8 | 5–18 |
| Creatine (mg/dL) | 0.76 | 1.38 | 0.60–0.88 |
| Glucose (mg/dL) | 102 | 109 | 60–99 |
| Alkaline phosphatase (U/L) | 111 | 121 | 42–110 |
Abbreviations: BUN, blood urea nitrogen; N/A, not available.
TABLE 2.
Comprehensive drug screen.
| Drug component | Result |
|---|---|
| Analgesics | Naproxen |
| Cannabinoids | Marijuana |
| Opioids/opiates | Morphine, morphine‐3‐glucuronide, tramadol |
| Stimulants | Cotinine |
| Antiemetics | Ondansetron |
| Tox Screen | Ketorolac, cefepime |
On further questioning, she stated that she had been consuming one box of cornstarch daily for the past 6 months. She appeared clinically stable, and arrangements were made for transfer to a pediatric hospital. However, en route her clinical status deteriorated, and she presented there in shock, hypotensive, and hypothermic. Laboratory studies are shown in the table.
She was admitted to the ICU with multi‐organ system failure where she required initiation of norepinephrine. Given a history of cornstarch ingestion coupled with a profound metabolic acidosis and the large osmolar gap, she was started on fomepizole (1.11 g administered at 200 mL/h, followed by 0.74 g every 12 h for four doses) and continuous renal replacement therapy was initiated. A volatile screen was negative for ethylene glycol, methanol, isopropanol, and acetone. Therefore, a presumptive diagnosis of PG toxicity was made. Her condition gradually improved and she was discharged.
3. DISCUSSION
We believe this patient developed D&L lactic acidosis as a result of propylene glycol toxicity secondary to chronic, large‐quantity cornstarch ingestion. This may have been related to iron deficiency anemia that can generate amylophagia, a subtype of pica that causes patients to compulsively ingest large amounts of cornstarch. 4 A similar case of PG toxicity from chronic cornstarch ingestion was reported in a 29‐year‐old female who consumed a 16 oz box of cornstarch every 2 days for several years. She presented to the ED with altered mental status and several weeks of fatigue and arthralgias; however, despite aggressive therapy, that patient died. 5
Ingested PG is partly excreted by the kidneys (25%–45%) unchanged or as a glucuronide conjugate. 3 The remainder is metabolized, primarily by sequential hepatic alcohol dehydrogenase and aldehyde dehydrogenase to form both d and l isomers of lactate. 6 Normally, l‐lactate is metabolized via conversion to pyruvate and is oxidized via the Krebs cycle, while d‐lactate metabolism is much slower. 3 , 7 At high concentrations, proximal tubular secretion of PG reaches a transport maximum resulting in higher blood levels and accelerated generation of both L and D lactic acid. 7 These effects combine to generate a HAGMA, which may be associated with renal and liver dysfunction. 7
Following ingestion of most toxic alcohols, an inverse relationship exists between the development of an osmolar gap and an anion gap metabolic acidosis. 8 Early after initial ingestion, the osmolar gap is elevated and as time progresses, the osmolar gap progressively declines and the anion gap increases. 8 Therefore, the absence of a large osmolar gap and/or anion gap does not exclude the possibility of a toxic alcohol ingestion. It remains uncertain why the patient's laboratory tests initially showed a HAGMA with a normal osmolar gap, and then a large osmolar gap plus an even greater anion gap metabolic acidosis when she was re‐evaluated after transfer. Two plausible possibilities are as follows: (1) she was ingesting cornstarch after her arrival at the first ED, or (2) she may have absorbed a bolus of propylene glycol from her gastrointestinal tract en route to the accepting facility.
Our patient initially denied any toxin ingestions; we only later discovered that she had been ingesting one box of cornstarch daily. This case highlights the importance of obtaining a thorough dietary history in patients with suspected toxicities, especially when laboratory values demonstrate an unexplained HAGMA and/or lactic acidosis. Prompt recognition and therapeutic intervention with fomepizole, a potent inhibitor of ADH, is essential in reducing life‐threatening sequelae following toxic alcohol ingestions. 9
The U.S. Food and Drug Administration classifies PG as being “generally recognized as safe” if the daily intake does not exceed 25 mg/kg body weight. 2 , 10 However, PG can make up to 5% of alcoholic beverages, 24% of confections and frostings, 2.5% of frozen dairy products, and 97% of seasonings and flavorings. 2 Ingestion of large quantities of such products can generate toxicity. We have been unable to determine the exact amount of PG our patient was ingesting, but we believe it was the cause of her HAGMA and multisystem organ dysfunction.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Downey K, Keklik R, Morrissey B, Barnes R, Reyner K, Emmett M. Propylene glycol toxicity in an adolescent secondary to chronic cornstarch ingestion. JACEP Open. 2024;5:e13188. 10.1002/emp2.13188
Supervising Editor: Karl Sporer, MD
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Okolie JA. Insights on production mechanism and industrial applications of renewable propylene glycol. iScience. 2022;25(9):104903. doi: 10.1016/j.isci.2022.104903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Food and Drug Administration . GRAS status of propylene glycol and propylene glycol monostearate. Fed Regist. 1982;47:27810. 21 CFR 184.1666. [Google Scholar]
- 3. Fowles JR, Banton MI, Pottenger LH. A toxicological review of the propylene glycols. Crit Rev Toxicol. 2013;43(4):363‐390. doi: 10.3109/10408444.2013.792328 [DOI] [PubMed] [Google Scholar]
- 4. Maksoud C, Dhadham GC, Kothari S, Elfarra H. Amylophagia in iron deficiency anemia: uncommon and commonly missed: 698. Am J Gastroenterol. 2010;105:S253. [Google Scholar]
- 5. Peterson J, Stadlen R, Radke J. Propylene glycol toxicity from compulsive corn starch ingestion. Am J Emerg Med. 2022;53:286.e1‐286.e3. doi: 10.1016/j.ajem.2021.09.054 [DOI] [PubMed] [Google Scholar]
- 6. Zosel A, Egelhoff E, Heard K. Severe lactic acidosis after an iatrogenic propylene glycol overdose. Pharmacotherapy. 2010;30(2):219. doi: 10.1592/phco.30.2.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zar T, Graeber C, Perazella MA. Recognition, treatment, and prevention of propylene glycol toxicity. Semin Dial. 2007;20(3):217‐219. doi: 10.1111/j.1525-139X.2007.00280.x [DOI] [PubMed] [Google Scholar]
- 8. Iqbal A, Glagola JJ, Nappe TM. Ethylene glycol toxicity. In: StatPearls. StatPearls Publishing;2023. https://www.ncbi.nlm.nih.gov/books/NBK537009/ [PubMed] [Google Scholar]
- 9. Agency for Toxic Substances and Disease Registry (ATSDR) . Toxicological profile for ethylene glycol. U.S. Department of Health and Human Services, Public Health Service; 2010. [PubMed] [Google Scholar]
- 10. Joint FAO/WHO Expert Committee on Food Additives (JECFA) . Toxicological evaluation of some food additives including anticaking agents, antimicrobials, antioxidants, emulsifiers and thickening agents. WHO Food Additives; 1974. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


