Abstract
Objectives: Congruence between the preferred and actual place of death is recognised as an important quality indicator in end-of-life care. However, there may be complexities about preferences that are ignored in summary congruence measures. This article examined factors associated with preferred place of death, actual place of death, and congruence for a sample of patients who had received specialist palliative care in the last three months of life in Ireland. Methods: This article analysed merged data from two previously published mortality follow-back surveys: Economic Evaluation of Palliative Care in Ireland (EEPCI); Irish component of International Access, Rights and Empowerment (IARE I). Logistic regression models examined factors associated with (a) preferences for home death versus institutional setting, (b) home death versus hospital death, and (c) congruent versus non-congruent death. Setting: Four regions with differing levels of specialist palliative care development in Ireland. Participants: Mean age 77, 50% female/male, 19% living alone, 64% main diagnosis cancer. Data collected 2011-2015, regression model sample sizes: n = 342-351. Results: Congruence between preferred and actual place of death in the raw merged dataset was 51%. Patients living alone were significantly less likely to prefer home versus institution death (OR 0.389, 95%CI 0.157-0.961), less likely to die at home (OR 0.383, 95%CI 0.274-0.536), but had no significant association with congruence. Conclusions: The findings highlight the value in examining place of death preferences as well as congruence, because preferences may be influenced by what is feasible rather than what patients would like. The analyses also underline the importance of well-resourced community-based supports, including homecare, facilitating hospital discharge, and management of complex (eg, non-cancer) conditions, to facilitate patients to die in their preferred place.
Keywords: place of death, location of death, congruence, preference, palliative care (MeSH), end-of-life care (MeSH)
Introduction
Congruence between preferred and actual place of death has gained recognition as a quality indicator in end-of-life care.1–3 This reflects a shift away from focusing on home death as a quality-of-care indicator, 4 recognising that while many people with terminal illness would prefer to die at home,2,5–7 others prefer a non-home setting such as hospital, hospice, or nursing home.6,8,9 While it is agreed that congruence is a more appropriate measure, there may be complexities about preferences that are ignored in summary measures.6,10
Several systematic reviews have summarised the factors associated with place of death preferences, place of death, and congruence.1,2,5,11–13 Factors are typically categorised according to Andersen's model of health service use (predisposing, enabling, need, system-level characteristics)14,15 or grouped broadly as illness, individual or environmental factors. 1 Studies vary in methodology, target population (eg, cancer-specific), sample size, and overall quality8,11 and an internationally consistent profile of factors strongly associated with place of death preferences is lacking. 5 A multi-centre study of older patients (>65 years) with advanced disease in New York, London, and Dublin found that cancer diagnosis and living with someone were significantly associated with preference for a home death. 6 There is greater consistency in the factors associated with place of death. Home death is linked with patient's preferences, low functional status, intensive homecare, living with someone, extended family support, cancer diagnosis, and early access to palliative care.11,13 Key factors associated with congruence include functional status, treatments, cancer, age, sex, marital status, living arrangements, end-of-life preferences, and availability of health and palliative care although patterns, and levels of congruence, vary across studies.1,2
In Ireland, there is a strong preference for dying at home among the general public, 16 although in reality 40% of people die in hospital.17,18 There is limited understanding of the factors associated with place of death outcomes for those with terminal illness in the Irish context6,15,19 yet analysis from 33 countries suggests there is greater heterogeneity in place of death preferences among patients than the general public. 8 Thus, this article examines the factors associated with preferred place of death, actual place of death, and congruence between the two, for a sample of terminally ill patients receiving specialist palliative care (SPC) in four regions within Ireland. Specifically, we examined factors associated with preferences for home death compared with an institutional setting (hospital/hospice/nursing home), factors associated with home death compared with hospital death, and factors associated with a congruent compared with a non-congruent death. SPC delivery varies across the country19,20 and so this study was also able to examine if different modes of SPC delivery were associated with differences in place of death outcomes. Thus, this article contributes to international and national discussions on place of death for patients with serious illness.
Methods
Design
This article undertook a secondary analysis of merged data from two sister mortality follow-back surveys in Ireland: The Economic Evaluation of Palliative Care in Ireland study (EEPCI) and the Irish component of the International Access, Rights and Empowerment study (IARE I).19,21
Setting
Approximately 80% of deaths in Ireland are from conditions considered to have palliative care needs. 22 Ireland is committed to universal palliative care access 23 but available evidence highlights geographic variation in service provision 15 and uneven policy implementation. 20 Larger urban areas have advanced services where SPC is provided in dedicated SPC inpatient units (in-patient beds, day hospice, out-patient services, bereavement services), in people's homes, and in hospitals (eg, Dublin (Capital), Cork (South), Limerick (Mid-West)) while other areas continue to lack a SPC inpatient unit. 20
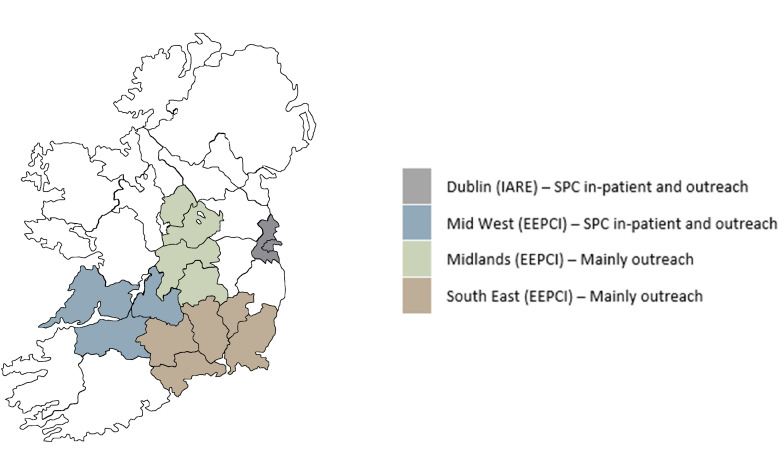
This article examined four comparator areas (Figure 1) reflecting differing levels of SPC development and to an extent, different models of care.6,19,20 These are: Dublin (City and County) and the Mid-West (Counties Clare, Limerick, North Tipperary) which have long-established dedicated SPC inpatient units, hospital SPC services, as well as outreach services (ie, SPC provided in people's homes), the Midlands (Counties Laois, Offaly, Longford, Westmeath), and South-East (Counties South Tipperary, Waterford, Wexford) where SPC services are mainly provided on an outreach basis in people's homes.6,19,24 A new in-patient facility opened in the South-East in 2021 (not captured in the data in this study) and an in-patient facility is planned for 2025 in the Midlands.
Figure 1.
Study sites.
Data
The EEPCI and the Irish component of IARE I had comparable study design and data collection tools, published already with full details.19,21,24,25 The Irish component of IARE I collected data in Dublin. Reference to IARE I data in this paper refers only to the Dublin sample. Both studies administered mortality follow-back surveys of key informants (usually relatives and carers) of decedents identified by palliative care services in Dublin (IARE I), the Midlands, the Mid-West, and South-Eastern areas in Ireland (EEPCI). Survey data were collected during telephone (and a small number of face-to-face) interviews (EEPCI) or by postal survey (IARE I). Eligible participants included cancer and non-cancer patients who had died 3-10 months prior to survey date, had accessed SPC, aged 18+ (EEPCI), or ≥65 years (IARE I). Ethical approval was granted for both studies and data were analysed anonymously.24,25 Data were collected between 2011 and 2015 with final samples of 215 (EEPCI) and 282 (IARE I – Dublin) participants. The questionnaires included a Client Service Receipt Inventory 26 to capture healthcare use, quality of care ratings using Likert-type scales, health-related quality of life using EQ-5D-3L, and questions about place of death preferences. This article made use of the comparability of questions across the two surveys (eg, Supplemental Table 1).
Descriptive Analysis
We compared demographic and clinical characteristics of patients across each site (Dublin, Midlands, Mid-West, South-East), checking for significant differences using independent samples t tests/chi-square tests.
Regression Analysis
We ran logistic regressions for each of three core outcome variables of interest (Supplemental Table 1):
- Preferences for home death versus an institutional death. ‘Home’ included home of a relative/friend plus a small number of patients whose home was a nursing/residential home.
- Death at home versus death in a hospital. Sample sizes were too small to permit comparisons of death at home versus death in hospice or nursing/residential home.
- Congruence between preferred and actual place of death.
We selected explanatory variables drawing on relevant literature,1,2,5,6,11–13 and on availability of variables in the data. Variables were categorised as predisposing (age, sex), enabling (informal care, living arrangements, carer demographics), need (cancer/non-cancer diagnosis, functional ability), and system (healthcare use, study site) characteristics according to Andersen's model.14,27
Explanatory variables were checked for collinearity. Within functional ability measures (mobility, self-care, usual activities), responses were collinear, and mobility at 3 months was retained to reflect functional ability in the models.
Final logistic regression models were selected using AIC and BIC criteria. Robust standard errors were adjusted to allow for clustering by study (EEPCI and IARE). Statistical analysis was undertaken in StataSE 17.
Missing Data
Sixteen percent of the sample without an expressed place of death preference or location of death were excluded from the analyses. Observations with missing data on the independent variables were excluded from the analysis. Percentage of missing data was <3% for most independent variables although higher for the functional ability variables (6-9%).
Sensitivity Analysis
For sensitivity, the regression models were run on the separate unmerged IARE and EEPCI samples.
To contextualise the patterns observed in the multivariate models, we examined details on living arrangements throughout the last year of life (EEPCI) and at place of death (IARE I).
Ethical Considerations
The data used in this article were from two mortality follow-up surveys that were conducted with full ethical approval. The EEPCI study received approval from the Health Policy and Management and Centre for Global Health Research Ethics Committee at Trinity College Dublin (Ref: TCD 07/2012/05), and the Research Ethics Committees at HSE Midlands (Ref: 060612SS), Mid-West (Ref: 18/04/2012), and South-East (Ref: 06/06/2012). The IARE I study received ethical approval from the Research Ethics Committee in Dulwich, London in England (Ref. 12/LO/0044); the ethics committees of the Mater Misericordiae University Hospital (Ref. 1/378/1456) and Beaumont Hospital (Ref. 12/07) in Ireland; the Institutional Review Board of the Icahn School of Medicine at Mount Sinai (Ref. GCO#11) and the University of California, San Francisco (UCSF; Ref. 13-1099) in the United States.
Results
Primary Outcome Variables
The raw merged dataset included 497 patients. We had outcome data on both preference and location of death for 417 cases, of whom 51% died in their preferred place.
The final analysis sample sizes for the regression models, excluding cases with missing values in independent variables, were 347 (preference for home vs institutional death), 342 (death at home vs death in hospital), and 351 (congruence between preferred and actual place of death). Of those who expressed a preference, 79% preferred to die at home rather than in an institutional setting. In actuality, 38% died at home, 47% died in a hospital, 9% died in a hospice, and 6% died in a nursing home. The level of congruence in the congruence regression sample was 56% with variations in congruence by place (eg, 48% of those who preferred to die at home had a congruent death, compared with 98% of those who preferred to die in hospital) (Table 1).
Table 1.
Congruence Between Preferred and Actual Place of Death, EEPCI/IARE I Merged Data.
| Congruence between preferred and actual place | Actual place of death, % | |||||
|---|---|---|---|---|---|---|
| Home a | Hospital | Hospice | Nursing home/other | Total | ||
| Preferred place of death, % | Home a | 48 | 44 | 5 | 4 | 100 |
| Hospital | – | 98 | – | 3 | 100 | |
| Hospice | 8 | 20 | 68 | 4 | 100 | |
| Nursing home/other | – | 11 | – | 89 | 100 | |
Source: EEPCI and IARE I.
Home including home of relative/friend. Plus, a small number of patients were living in a nursing/residential home full-time and for these patients, nursing/residential home was interpreted as ‘home’.
There are some significant differences in decedent profiles across the sites, underlining the importance of controlling for demographic, need, enabling, and system-level characteristics in the regressions (Supplemental Table 2).
Explanatory Variables
Table 2 presents the explanatory variables categorised by each outcome variable. The mean age ranged from 74 to 77 across the regression models, with a relatively balanced number of men and women in each model (percentage of women ranged from 49% in the preferences model to 53% in the congruence model).
Table 2.
Explanatory Variables by Outcome Variables and Full Sample, EEPCI/IARE Merged Data.
| Explanatory variables | Pref for home death n = 274 |
Home death n = 141 |
Died in preferred place n = 196 |
Full sample n = 351 |
|---|---|---|---|---|
| Patient age | ||||
| Mean | 77.7 | 74.7 | 74.3 | 77.0 |
| 95% CI | [76.392-79.097] | [72.628-76.762] | [72.508-76.012] | [75.807-78.250] |
| Women, % | 48.9 | 51.8 | 52.6 | 50.4 |
| Number of informal carers, % | ||||
| 0 informal carer | 4.0 | 1.4 | 2.0 | 4.0 |
| 1 informal carer | 27.7 | 29.8 | 32.1 | 29.1 |
| 2/more informal carers | 68.3 | 68.8 | 65.8 | 67.0 |
| Living alone, % | 16.4 | 9.9 | 15.8 | 18.8 |
| Female carer, % | 68.3 | 68.8 | 66.8 | 66.7 |
| Carer age | ||||
| Mean | 56.5 | 56.1 | 56.4 | 56.8 |
| 95% CI | [54.945-57.974] | [54.029-58.213] | [54.633-58.225] | [55.443-58.169] |
| Main diagnosis cancer, % | 63.1 | 75.9 | 75.5 | 64.4 |
| Mobility at 3 months, % | ||||
| No problems | 17.9 | 16.3 | 16.3 | 17.7 |
| Some/lots of problems | 82.1 | 83.7 | 83.7 | 82.3 |
| Pain at 3 months, % | ||||
| No pain | 32.9 | 36.9 | 38.8 | 33.6 |
| Some/lots of pain | 67.2 | 63.1 | 61.2 | 66.4 |
| Anxiety at 3 months, % | ||||
| No anxiety | 38.7 | 42.1 | 41.0 | 39.4 |
| Some/lots of anxiety | 61.3 | 57.9 | 59.0 | 60.6 |
| Healthcare utilisation last 3 months, % | ||||
| Inpatient – one/more nights | 75.2 | 71.2 | 73.0 | 76.6 |
| Hospice – one/more nights | 9.5 | 9.9 | 14.3 | 12.5 |
| Nursing home – one/more nights | 15.0 | 16.3 | 17.4 | 16.5 |
| Homecare – one/more hours per week | 32.5 | 36.9 | 34.2 | 30.5 |
| Site, % | ||||
| Dublin | 44.5 | 22.0 | 28.6 | 45.6 |
| Midlands | 22.6 | 34.0 | 29.6 | 21.1 |
| Mid-West | 18.6 | 24.8 | 24.0 | 19.1 |
| South-East | 14.6 | 19.2 | 17.9 | 14.3 |
Source: EEPCI and IARE I merged dataset.
Notes: Descriptive statistics on the explanatory variables by each of the outcome variables are based on the sample of observations included in each of the regressions in Table 3. Descriptive statistics on the explanatory variables for the full sample is based on the analysis sample included in the congruence regression model, excluding observations with missing values on outcome and explanatory variables, total n = 351.
Regression Analysis
Predisposing, enabling, and system factors were significantly associated with place of death preferences (home vs institution) (Table 3a). Older patients were significantly more likely to prefer to die at home (OR 1.042, 95% CI 1.037-1.048) while women and those living alone were significantly less likely to prefer home death (OR 0.759, 95% CI 0.646-0.892; OR 0.389, 95% CI 0.157-0.961). Hospital and nursing home use (one/more nights in last 3 months of life) were significantly associated with preference for dying in an institutional setting rather than at home (OR 0.472, 95% CI 0.393-0.567; OR 0.306, 95% CI 0.172-0.545).
Table 3.
Factors Associated with Preferences on Place of Death, Actual Place of Death, and Congruence, Logit Results.
| 3a. Preference for home death versus institutional death (base = formal) | 3b. Home death versus hospital death (base = hospital death) | 3c. Congruence between preferred and actual place of death (base = not congruent) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | P > z | [95% conf. interval] | Odds ratio | P > z | [95% conf. interval] | Odds ratio | P > z | [95% conf. interval] | ||||
| Patient age | 1 . 042 | 0.000 | 1.037 | 1.048 | 1.011 | 0.203 | 0.994 | 1.028 | 0.967 | 0.017 | 0.941 | 0.994 |
| Women (base: men) | 0.759 | 0.001 | 0.646 | 0.892 | 1.317 | 0.110 | 0.940 | 1.845 | 1.347 | 0.000 | 1.262 | 1.437 |
| Number of informal carers (base: no informal carer) | ||||||||||||
| 1 informal carer | 0.739 | 0.403 | 0.363 | 1.502 | 2.328 | 0.003 | 1.326 | 4.088 | 1.294 | 0.161 | 0.902 | 1.855 |
| 2/more informal carers | 0.883 | 0.106 | 0.758 | 1.027 | 2.556 | 0.000 | 2.099 | 3.113 | 1.238 | 0.194 | 0.897 | 1.709 |
| Living alone (base: not living alone) | 0.389 | 0.041 | 0.157 | 0.961 | 0.383 | 0.000 | 0.274 | 0.536 | 1.107 | 0.554 | 0.791 | 1.547 |
| Female carer (base: male carer) | 0.901 | 0.530 | 0.651 | 1.248 | ||||||||
| Carer age | 0.982 | 0.303 | 0.948 | 1.017 | 0.985 | 0.001 | 0.976 | 0.994 | 1.005 | 0.613 | 0.987 | 1.023 |
| Main diagnosis cancer | 0.735 | 0.482 | 0.312 | 1.733 | 3.052 | 0.001 | 1.540 | 6.049 | 1.621 | 0.000 | 1.395 | 1.883 |
| Mobility at 3 months (base: no problems) | ||||||||||||
| Some/Lots of problems | 0.816 | 0.370 | 0.523 | 1.273 | 0.513 | 0.451 | 0.090 | 2.917 | 0.636 | 0.517 | 0.161 | 2.503 |
| Pain at 3 months (base: no pain) | ||||||||||||
| Some/lots of pain | 1.079 | 0.728 | 0.703 | 1.657 | 1.674 | 0.484 | 0.395 | 7.096 | 0.990 | 0.987 | 0.321 | 3.058 |
| Anxiety at 3 months (base: no anxiety) | ||||||||||||
| Some/lots of anxiety | 1.166 | 0.336 | 0.853 | 1.596 | ||||||||
| Healthcare utilisation last 3 months | ||||||||||||
| Inpatient – one/more nights | 0.472 | 0.000 | 0.393 | 0.567 | 0.164 | 0.000 | 0.146 | 0.186 | 0.494 | 0.000 | 0.431 | 0.566 |
| Hospice – one/more nights | 0.181 | 0.202 | 0.013 | 2.505 | 65.582 | 0.181 | 0.142 | 30 294 | 0.906 | 0.876 | 0.262 | 3.133 |
| Nursing home – one/more nights | 0.306 | 0.000 | 0.172 | 0.545 | 0.951 | 0.921 | 0.347 | 2.607 | 0.774 | 0.678 | 0.231 | 2.597 |
| Homecare – one/more hours per week | 1.425 | 0.120 | 0.911 | 2.229 | 1.508 | 0.022 | 1.062 | 2.141 | 1.559 | 0.000 | 1.293 | 1.879 |
| Site (base: Mid-West) | ||||||||||||
| Dublin | 0.332 | 0.277 | 0.045 | 2.430 | 0.018 | 0.000 | 0.004 | 0.080 | 0.257 | 0.000 | 0.200 | 0.332 |
| South-East | 0.614 | 0.502 | 0.148 | 2.550 | 0.164 | 0.000 | 0.107 | 0.253 | 0.999 | 0.998 | 0.648 | 1.542 |
| Midlands | 0.802 | 0.809 | 0.135 | 4.785 | 0.584 | 0.000 | 0.533 | 0.639 | 2.027 | 0.006 | 1.229 | 3.342 |
| Number of obs | 347 (274 pref home; 73 pref institution) | 342 (141 died at home; 201 died in hosp) | 351 (196 congruent; 155 not congruent) | |||||||||
| Log likelihood | −156.570 | −141.841 | −198.539 | |||||||||
| Pseudo R2 | 0.123 | 0.388 | 0.176 | |||||||||
Source: EEPCI and IARE I merged dataset.
Significant at 5% level are presented in boldface.
Enabling, need, and system factors were significantly associated with place of death (home vs hospital) (Table 3b). Patients with more informal care supports including ≥1 informal carer (OR 2.328, 95% CI 1.326-4.088; OR 2.556; 95% CI 2.099-3.113), younger carers (OR 0.985, 95% CI 0.976-0.994), and higher homecare use (OR 1.508, 95% CI 1.062-2.141) were significantly more likely to die at home than in hospital. Patients living alone (OR 0.383, 95% CI 0.274-0.536) were significantly less likely to die at home than in hospital. Cancer patients were significantly more likely to die at home (OR 3.052, 95% CI 1.540-6.049). Hospital use in the last 3 months of life was significantly associated with dying in a hospital setting rather than at home (OR 0.164, 95% CI 0.146-0.186). Patients in the Mid-West were significantly more likely to die at home than in the other regions.
Predisposing, need, and system factors were significantly associated with congruence between preferred and actual place of death (Table 3c). Older patients were significantly less likely to die in their preferred setting (OR 0.967, 95% CI 0.941-0.994), while women were significantly more likely to achieve congruence (OR 1.347, 95% CI 1.262-1.437). Cancer patients were significantly more likely to achieve congruence (OR 1.621, 95% CI 1.395-1.883). Patients with higher hospital use were significantly less likely to achieve congruence (OR 0.494, 95% CI 0.431-0.566) while those with higher homecare use were more likely (OR 1.559, 95% CI 1.293-1.879). Patients in Dublin were significantly less likely to achieve congruence than in the other regions.
Missing Data Analysis
Absence of a stated preferred place of death was the main source of missing data (n = 70 missing values). Supplemental Table 3 compares the predisposing, enabling, need, and system characteristics of the patients with missing preference data (n = 70) with the profile of the patients included in the place of death preference regression model (n = 347). The missing cases were not found to be statistically significantly different from those included in the regression model with two exceptions: a higher proportion of missing preference data were found in the Dublin sample than in the other three regions (Χ2 = 16.24, p = 0.001), and cases with missing preference data were less likely to have a cancer diagnosis (51.4%) compared with those included in the regression model (65.1%, Χ2 = 4.68, p = 0.03).
Sensitivity Analyses
IARE Versus EEPCI
For the non-significant findings in the models based on the merged dataset, there are some differences in coefficient sign (±) in the separate IARE and EEPCI models but for the significant findings the overall patterns are consistent across all models (Supplemental Table 4(a)–(c)). Results from the merged dataset models only are reported here for ease of presentation.
Living Arrangements in Last Year of Life
In the last year of life, EEPCI data showed most adjustments in living arrangements were between home and institutional settings with 89% of all moves being to/from/between institutional settings, 8% within a home (eg, relative/friend moving in or out), and 4% own home to home of relative (Supplemental Figures 1 and 2).
Drawing on the IARE I sample, Table 4 shows the length of time spent (in weeks) at the place of death.
Table 4.
Length of Time Spent at Place of Death (IARE I Sample).
| Home | Hospice | Hospital | Nursing home | Total | |
|---|---|---|---|---|---|
| % | % | % | % | % | |
| <1 week | 18 | 63 | 14 | 0 | 16 |
| 1-3 weeks | 20 | 13 | 45 | 0 | 40 |
| 4 weeks + | 63 | 25 | 41 | 100 | 44 |
| Total | 100 | 100 | 100 | 100 | 100 |
Source: IARE I survey.
Notes: Cell sizes are small for Hospice and Nursing Home categories.
Discussion
Main Findings
This article provides important detail on the factors associated with place of death outcomes for a sample of patients who received SPC before they died. A high proportion of patients preferred a home death but died in hospital, consistent with national and international profiles7,16,17,18 and overall congruence in the raw merged dataset was just over 51% suggesting a substantial gap in facilitating patients to die in their preferred place in Ireland.
Key Lessons
The analysis underlines the importance of analysing place of death preferences per se despite the recent shift in focus towards congruence as a key end-of-life quality indicator. Living situation was shown here to be significantly associated with preferred and actual place of death, but not with congruence. Patients who lived alone were significantly less likely to choose to die at home, suggesting that preferences were influenced by pragmatic considerations. The fact that those who lived alone were less likely to choose home as well as being less likely to die at home, could explain why they were not significantly less likely to achieve congruence. The specific challenges facing people living alone towards the end of life have been well-documented.4,28 Patients with hospital and nursing home use in the last 3 months of life were significantly less likely to choose to die at home, further supporting the observation that preferences are influenced by system characteristics (eg, experience of alternative options) and not just by predisposing characteristics. Although congruence may be the more important summary end-of-life quality indicator, it is still valuable to examine factors associated with preferences, especially if patients shape their preferences based on what they think is feasible rather than what they would like. This is consistent with observations by Higginson et al (2017) that end-of-life care choices are nuanced and ‘further work is needed to understand whether not wanting to die at home is a positive choice, or a reaction against failures in care’.6,10 Future qualitative analysis could explore what drives place of death preferences and how alternative places are ranked so that patients are helped, at the very least, to avoid dying in their least preferred place of death.
Second, the regression findings are consistent with international evidence that a range of predisposing, enabling, need, and system factors are associated with place of death outcomes6,11,13 but the Irish context highlights the important role of community-based supports in the observed patterns:
- Informal care supports (number of, younger aged, informal carers) and homecare were significantly associated with home versus hospital deaths, and homecare was also significantly associated with congruent deaths. This is consistent with previous findings from population-based survey data. 29 As illustrated in Table 2, patients who died at home and had congruent deaths each had higher homecare hours and to some extent higher proportions of informal care providers compared with the rest of the sample. These could reflect greater needs, or better access to homecare and there is detailed evidence of insufficient and unequal homecare access for older populations in Ireland.30,31
- Consistent with other studies,2,13 cancer patients were significantly more likely to die in their preferred place (home). This finding is consistent with evidence that people with other life-limiting illnesses have different trajectories of needs, often with distressing and difficult-to-manage symptoms (eg, pain, breathlessness). There can be more exacerbations and unpredictable events that lead to hospital use, and it can be difficult to discharge these patients back home. 32 Although detailed diagnostic data are unavailable, non-cancer patients in the merged data were more likely to have an ED visit (54% vs 33%) and to have some/lots of pain compared with cancer patients (73% vs 67%). It may also reflect the fact that SPC supports have traditionally been more focused on cancer diagnoses, and there is greater capacity to manage care needs at home.20,33 Cancer diagnosis may be capturing some of the system-level influence in our data.
- The significant association between prior hospital use and hospital death, and between prior hospital use and non-congruence, could be capturing residual complexity of need. However, it may also reflect well-documented barriers to moving patients from hospital to appropriate levels of community care (including homecare as discussed above) in Ireland. 30 The analysis of time in place of death using Dublin only data sheds light on this (Table 4). For those who died at home, the majority (63%) were there for longer than 4 weeks suggesting that a home death is not typically set up quickly. While for those who died in hospice, 63% (albeit a small sample size) were there for less than 1 week. For those who died in hospital, 14% were there for less than a week while 45% were there for 1-3 weeks, and a further 41% were there for >4 weeks. This suggests the pattern was not necessarily that patients were transferred to hospital to die, but that they were not being transferred out of hospital in time to die elsewhere. This is further supported by the finding that older patients were significantly less likely to achieve congruence consistent with known gaps and inequalities in community-based supports for older people.30,31,34
- Thus, while these patterns are likely capturing unobserved needs to some extent, when taken altogether they also consistently point to under-resourced community-based supports for older people in Ireland and it is likely that both factors are at play. These findings further strengthen the call for progress in Irish policy reforms to enhance community-based care. 23
Third, the significance of the region warrants further examination and should be interpreted with caution. The Midlands had significantly higher congruence than in the other three areas suggesting that the model of SPC based mainly on outreach in people's homes may be more successful in helping patients to die in their preferred place but equally this could be reflecting an absence of choice (there is no inpatient SPC facility in the Midlands). Overall, congruence was significantly less likely in Dublin compared with the other regions which may point to health system pressures in Dublin or an unobserved urban/rural dimension. It could also reflect differences in sampling methods between IARE and EEPCI with the former more focused on recruiting participants from hospital-based SPC teams while EEPCI included both hospital and outreach teams.
Strengths and Weaknesses
This study examined merged data from two rich SPC datasets to examine place of death outcomes but the sample size was still relatively small and we were restricted to focusing on preferences for home versus non-home deaths, and on factors associated with home versus hospital deaths. While the focus on these two places is valid because they accounted for most patient preferences, and death places in the data, further analysis of hospice, nursing home, and other places is needed. Moreover, analysis is needed of changes in preferences over time, 35 and of missing preferences 10 to further enrich our understanding of preferences in the Irish context.
Previous analysis of place of death preferences indicates that the home of a relative should not be considered an equal alternative to a patient's own home. 6 We merged these two categories to maximise sample size. Analysis of living patterns within the last year of life suggested that the more important distinctions in these data were between home and institutional settings, with moves between own home and home of relative/friend accounting for just 4% of all moves in the last year of life.
While the data allowed for a range of predisposing, enabling, need, and system-level characteristics in the models, there may be residual omitted variable bias particularly around diagnosis and the implications of different levels of SPC intensity for place of death outcomes.
Finally, there were unavoidable delays that prevented data merging until now. There is no evidence to suggest that SPC structures in the study sites have radically altered since the data were collected (the new South-East inpatient SPC facility only came on stream in 2021 and the Midlands SPC inpatient unit is not planned until 2025). Thus, inferences made about factors affecting place of death outcomes are relevant to current SPC delivery both in Ireland and internationally.
Conclusions
To conclude, despite the recent shift in focus towards congruence between preferred and actual place of death as the more important summary end-of-life quality indicator, this study highlights the value in also examining factors associated with place of death preferences, because patients may be shaping their preferences based on what is feasible rather than what they would like. The findings also underline the importance of well-resourced community-based supports, including homecare, facilitating hospital discharge, and management of complex (eg, non-cancer) conditions, to facilitate patients to die in their preferred place.
Supplemental Material
Supplemental material, sj-docx-1-pal-10.1177_08258597241231042 for Place of Death for Adults Receiving Specialist Palliative Care in Their Last 3 Months of Life: Factors Associated With Preferred Place, Actual Place, and Place of Death Congruence by Samantha Smith, Aoife Brick, Bridget Johnston, Karen Ryan, Regina McQuillan, Sinead O’Hara, Peter May, Elsa Droog, Barbara Daveson, R. Sean Morrison, Irene J. Higginson and Charles Normand in Journal of Palliative Care
Supplemental material, sj-docx-2-pal-10.1177_08258597241231042 for Place of Death for Adults Receiving Specialist Palliative Care in Their Last 3 Months of Life: Factors Associated With Preferred Place, Actual Place, and Place of Death Congruence by Samantha Smith, Aoife Brick, Bridget Johnston, Karen Ryan, Regina McQuillan, Sinead O’Hara, Peter May, Elsa Droog, Barbara Daveson, R. Sean Morrison, Irene J. Higginson and Charles Normand in Journal of Palliative Care
Acknowledgements
We would like to acknowledge gratefully the dedication, skill, and expertise that all the members of the participating specialist palliative care teams brought to their project inputs. We would also like to acknowledge those relatives who took time to tell us about their experiences. For the EEPCI study, we would also like to thank the interviewers for their kind, sensitive approach to the interviews.
The IARE I study was part of BuildCARE, an international research programme supported by Cicely Saunders International (CSI) and The Atlantic Philanthropies, led by Irene J Higginson at King's College London, Cicely Saunders Institute of Palliative Care, Policy & Rehabilitation, UK. We thank all collaborators and advisors including service-users. BuildCARE members: Emma Bennett, Francesca Cooper, Barbara Daveson, Susanne de Wolf-Linder, Mendwas Dzingina, Clare Ellis-Smith, Catherine Evans, Taja Ferguson, Lesley Henson, Irene J Higginson, Bridget Johnston, Paramjote Kaler, Pauline Kane, Lara Klass, Peter Lawlor, Paul McCrone, Regina McQuillan, Diane Meier, Susan Molony, R Sean Morrison, Fliss Murtagh, Charles Normand, Caty Pannell, Steve Pantilat, Anastasia Reison, Karen Ryan, Lucy Selman, Melinda Smith, Katy Tobin, Rowena Vohora, Gao Wei and Deokhee Yi. Finally, we would like to thank two anonymous reviewers for their invaluable feedback on the paper.
Footnotes
Authors’ Note: Author contributions are categorised using the CRediT author taxonomy (https://credit.niso.org/ [last accessed 02/07/2023]. S.S. led the conceptualisation, data curation, formal analysis, and writing (original draft) of this article. A.B., B.J., K.R., R.McQ., S.O.H., P.M., E.D., B.D., I.J.H., and C.N. each contributed to writing (review and editing) of the article. S.S., A.B., B.J., and B.D. were involved in data curation, methodology, and project administration in the source studies (S.S. and A.B.: EEPCI) and (B.J. and B.D.: IARE I). K.R. and R.McQ. were involved in methodology and supervision of the source studies (K.R.: EEPCI and IARE I; R.McQ.: IARE I). S.O.H. and E.D. were involved in data curation in the source EEPCI study. I.J.H. and C.N. led funding acquisition and supervised the two source studies, EEPCI and IARE I. All authors read and approved the final version of this article.
Data Management and Sharing: The merged dataset used in this article draws on data from two studies, EEPCI and IARE I. The ethical agreements governing the EEPCI data do not permit sharing of the data but the final report from the EEPCI study contains detailed tables and metadata from the study and is publicly available. 19 Anonymised data for the IARE I study are available on request from the corresponding authors of the core IARE I study publications. 20
Declaration of Conflicts of Interest: The authors declare that there are no conflicts of interest with respect to the research, authorship, or publication of this paper.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Cicely Saunders International, and The Atlantic Philanthropies (grant number 18744).
Research Ethics and Patient Consent: The data used in this article were from two mortality follow-back surveys that were conducted with full ethical approval. The EEPCI study received ethical approval from the Health Policy and Management and Centre for Global Health Research Ethics Committee at Trinity College Dublin (Ref: TCD 07/2012/05), and the Research Ethics Committees at HSE Midlands (Ref: 060612SS), Mid-West (Ref: 18/04/2012), and South-East (Ref: 06/06/2012). The study was introduced to eligible participants by a member of the local palliative care team. Where the eligible participant agreed to receive further information, they were sent an information booklet and were asked to sign a consent form if they agreed to participate in a phone interview (if specifically requested by the participant a small number of face-to-face interviews were facilitated). The IARE I study received ethical approval from the Research Ethics Committee in Dulwich, London in England (Ref. 12/LO/0044); the ethics committees of the Mater Misericordiae University Hospital and Beaumont Hospital in Ireland (Ref. 1/378/1456 and Ref. 12/07, respectively) and the Institutional Review Board of the Icahn School of Medicine at Mount Sinai (Ref. GCO#11) and the University of California, San Francisco (UCSF; Ref. 13-1099) in the United States. Eligible participants were sent study information and a postal questionnaire with a pre-paid envelope addressed to the research team. Consenting respondents returned a self-completed questionnaire, pre-piloted in all countries.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Garcia-Sanjuan S, Fernandez-Alcantara M, Clement-Carbonell V, et al. Levels and determinants of place-of-death congruence in palliative patients: a systematic review. Front Psychol. 2022;12(Jan 13):807869. doi: 10.3389/fpsyg.2021.807869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Billingham MJ, Billingham SJ. Congruence between preferred and actual place of death according to the presence of malignant or non-malignant disease: a systematic review and meta-analysis. BMJ Support Palliat Care. 2013;3(2):144-154. doi: 10.1136/bmjspcare-2012-000292 [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Bhadelia A, Goh C, et al. Cross country comparison of expert assessments of the quality of death and dying 2021. J Pain Symptom Manage. 2022;63(4):e419-e429. doi: 10.1016/j.jpainsymman.2021.12.015 [DOI] [PubMed] [Google Scholar]
- 4.Kieninger J, Wosko P, Pleschberger S. Support towards the end of life and beyond: Non-kin care commitment for older people living alone in Austria. Health Soc Care Community. 2022;30(6):e5196-e5203. doi: 10.1111/hsc.13937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fereidouni A, Rassouli M, Salesi M, et al. Preferred place of death in adult cancer patients: A systematic review and meta-analysis. Front Psychol. 2021;12(Aug 27):704590. doi: 10.3389/fpsyg.2021.704590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higginson IJ, Daveson BA, Morrison RS, et al. Social and clinical determinants of preferences and their achievement at the end of life: Prospective cohort study of older adults receiving palliative care in three countries. BMC Geriatr. 2017;17(1):271. doi: 10.1186/s12877-017-0648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiang J, May P. Proportion of deaths in hospital in European countries: Trends and associations from panel data (2005-2017). Eur J Public Health. 2021;31(6):1176-1183. doi: 10.1093/eurpub/ckab169. [DOI] [PubMed] [Google Scholar]
- 8.Gomes B, Calanzani N, Gysels M, et al. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care. 2013;12(1):7. doi: 10.1186/1472-684X-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tay RY, Choo RWK, Ong WY, et al. Predictors of the final place of care of patients with advanced cancer receiving integrated home-based palliative care: A retrospective cohort study. BMC Palliat Care. 2021;20(1):164. doi: 10.1186/s12904-021-00865-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoare S, Morris ZS, Kelly MP, et al. Do patients want to die at home? A systematic review of the UK literature, focused on missing preferences for place of death. PLoS One. 2015;10(11):e0142723. doi: 10.1371/journal.pone.0142723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: Systematic review. Br Med J. 2006;332(7540):515-521. doi: 10.1136/bmj.38740.614954.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nilsson J, Blomberg C, Holgersson G, et al. End-of-life care: Where do cancer patients want to die? A systematic review. Asia Pac J Clin Oncol. 2017;13(6):356-364. doi: 10.1111/ajco.12678. [DOI] [PubMed] [Google Scholar]
- 13.Costa V, Earle CC, Esplen MJ, et al. The determinants of home and nursing home death: A systematic review and meta-analysis. BMC Palliat Care. 2016;15(1):8. doi: 10.1186/s12904-016-0077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36(1):1-10. [PubMed] [Google Scholar]
- 15.May P, Roe L, McGarrigle CA, et al. End-of-life experience for older adults in Ireland: Results from the Irish longitudinal study on ageing (TILDA). BMC Health Serv Res. 2020;20(1):118. doi: 10.1186/s12913-020-4978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weafer J. Irish Attitudes to Death, Dying and Bereavement 2004-2014. Dublin: Irish Hospice Foundation; 2014. [Google Scholar]
- 17.Matthews S, Pierce M, O'Brien Green S, et al. Dying and Death in Ireland: What Do We Routinely Measure, How Can We Improve? Dublin: Irish Hospice Foundation; 2021. [Google Scholar]
- 18.CSO. VSDO Vital Statistics Deaths Occurrence (Final). Cork: Central Statistics Office; 2023. [Google Scholar]
- 19.Brick A, Normand C, O'Hara S, et al. Economic Evaluation of Palliative Care in Ireland. Report prepared for The Atlantic Philanthropies. Dublin: Trinity College Dublin; 2015. [Google Scholar]
- 20.Johnston BM, Ní Chéileachair F, Burke S, et al. Review of the Implementation of the 2001 Report of the National Advisory Committee on Palliative Care as it relates to Adult Palliative Care. Dublin: Department of Health; 2022. [Google Scholar]
- 21.Higginson IJ, Yi D, Johnston BM, et al. Associations between informal care costs, care quality, carer rewards, burden and subsequent grief: The international, access, rights and empowerment mortality follow-back study of the last 3 months of life (IARE I study). BMC Med. 2020;18(1):344. doi: 10.1186/s12916-020-01768-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kane PM, Daveson BA, Ryan K, et al. The need for palliative care in Ireland: A population-based estimate of palliative care using routine mortality data, inclusive of nonmalignant conditions. J Pain Symptom Manage. 2015;49(4):726-733, e721. DOI: 10.1016/j.jpainsymman.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 23.Houses of the Oireachtas Committee on the Future of Healthcare. Sláintecare Report. Dublin: Houses of the Oireachtas; 2017. [Google Scholar]
- 24.Brick A, Smith S, Normand C, et al. Costs of formal and informal care in the last year of life for patients in receipt of specialist palliative care. Palliat Med. 2017;31(4):356-368. doi: 10.1177/0269216316686277. [DOI] [PubMed] [Google Scholar]
- 25.Yi D, Johnston BM, Ryan K, et al. Drivers of care costs and quality in the last 3 months of life among older people receiving palliative care: a multinational mortality follow-back survey across England, Ireland and the United States. Palliat Med. 2020;34(4):513-523. doi: 10.1177/0269216319896745. [DOI] [PubMed] [Google Scholar]
- 26.Beecham J, Knapp M. Costing psychiatric interventions. In: Thornicroft G. ed. Measuring Mental Health Needs. 2nd ed. Cambridge: Cambridge University Press, 2001:200-224. [Google Scholar]
- 27.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208-220. [PMC free article] [PubMed] [Google Scholar]
- 28.Rolls L, Seymour JE, Froggatt KA, et al. Older people living alone at the end of life in the UK: Research and policy challenges. Palliat Med. 2011;25(6):650-657. doi: 10.1177/0269216310373165. [DOI] [PubMed] [Google Scholar]
- 29.Burns CM, Abernethy AP, Dal Grande E, et al. Uncovering an invisible network of direct caregivers at the end of life: A population study. Palliat Med. 2013;27(7):608-615. doi: 10.1177/0269216313483664. [DOI] [PubMed] [Google Scholar]
- 30.Walsh B, Lyons S, Smith S, et al. Does formal home care reduce inpatient length of stay? Health Econ. 2020;29(12):1620-1636. doi: 10.1002/hec.4158. [DOI] [PubMed] [Google Scholar]
- 31.Keane C, Lyons S, Regan M, et al. Home Support Services in Ireland: Exchequer and Distributional Impacts of Funding Options. ESRI Survey and Statistical Report Series; 2022. [Google Scholar]
- 32.Bone AE, Evans CJ, Henson LA, et al. Influences on emergency department attendance among frail older people with deteriorating health: A multicentre prospective cohort study. Public Health. 2021;194(May):4-10. doi: 10.1016/j.puhe.2021.02.031 [DOI] [PubMed] [Google Scholar]
- 33.Jang H, Lee K, Kim S, et al. Unmet needs in palliative care for patients with common non-cancer diseases: A cross-sectional study. BMC Palliat Care. 2022;21(1):151. doi: 10.1186/s12904-022-01040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith S, Walsh B, Wren MA, et al. Geographic inequalities in non-acute healthcare supply: Evidence from Ireland. HRB Open Res. 2021;4(Oct):111. doi: 10.12688/hrbopenres.13412.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheridan R, Roman E, Smith AG, et al. Preferred and actual place of death in haematological malignancies: A report from the UK haematological malignancy research network. BMJ Support Palliat Care. 2021;11(1):7-16. doi: 10.1136/bmjspcare-2019-002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pal-10.1177_08258597241231042 for Place of Death for Adults Receiving Specialist Palliative Care in Their Last 3 Months of Life: Factors Associated With Preferred Place, Actual Place, and Place of Death Congruence by Samantha Smith, Aoife Brick, Bridget Johnston, Karen Ryan, Regina McQuillan, Sinead O’Hara, Peter May, Elsa Droog, Barbara Daveson, R. Sean Morrison, Irene J. Higginson and Charles Normand in Journal of Palliative Care
Supplemental material, sj-docx-2-pal-10.1177_08258597241231042 for Place of Death for Adults Receiving Specialist Palliative Care in Their Last 3 Months of Life: Factors Associated With Preferred Place, Actual Place, and Place of Death Congruence by Samantha Smith, Aoife Brick, Bridget Johnston, Karen Ryan, Regina McQuillan, Sinead O’Hara, Peter May, Elsa Droog, Barbara Daveson, R. Sean Morrison, Irene J. Higginson and Charles Normand in Journal of Palliative Care