ABSTRACT
Streptococcus suis is a major bacterial pathogen in pigs and an emerging zoonotic pathogen. Different S. suis serotypes exhibit diverse characteristics in population structure and pathogenicity. Surveillance data highlight the significance of S. suis serotype 4 (SS4) in swine streptococcusis, a pathotype causing human infections. However, except for a few epidemiologic studies, the information on SS4 remains limited. In this study, we investigated the population structure, pathogenicity, and antimicrobial characteristics of SS4 based on 126 isolates, including one from a patient with septicemia. We discovered significant diversities within this population, clustering into six minimum core genome (MCG) groups (1, 2, 3, 4, 7-2, and 7-3) and five lineages. Two main clonal complexes (CCs), CC17 and CC94, belong to MCG groups 1 and 3, respectively. Numerous important putative virulence-associated genes are present in these two MCG groups, and 35.00% (7/20) of pig isolates from CC17, CC94, and CC839 (also belonging to MCG group 3) were highly virulent (mortality rate ≥ 80%) in zebrafish and mice, similar to the human isolate ID36054. Cytotoxicity assays showed that the human and pig isolates of SS4 strains exhibit significant cytotoxicity to human cells. Antimicrobial susceptibility testing showed that 95.83% of strains isolated from our labs were classified as multidrug-resistant. Prophages were identified as the primary vehicle for antibiotic resistance genes. Our study demonstrates the public health threat posed by SS4, expanding the understanding of SS4 population structure and pathogenicity characteristics and providing valuable information for its surveillance and prevention.
KEYWORDS: Streptococcus suis serotype 4, population structure, pathogenicity, antimicrobial susceptibility, prophage, integrative and conjugative elements
Introduction
Streptococcus suis is an important pathogen in the pig industry, causing septicemia, meningitis, and sudden death in pigs, imposing substantial economic losses on the industry [1]. Moreover, S. suis is an emerging zoonotic pathogen that can be transmitted to humans by contact with diseased animals or contaminated raw pork products [2,3]. Indeed, human cases of S. suis have been reported worldwide. Particularly in Vietnam and Thailand, S. suis was responsible for thousands of human disease cases and has been identified as one of the most prevalent causes of adult bacterial meningitis [2,4,5]. Based on the capsular polysaccharide (CPS) antigenicity variation, S. suis can be classified into 29 serotypes (1–19, 21, 23–25, 27–31, 1/2) [6,7]. Also, serotype Chz and 27 novel cps loci (NCLs) have been identified from non-typeable isolates based on differences in the cps gene cluster [8–13]. To date, 11 serotypes have been documented as capable of inducing human infections, consisting of serotypes 1, 2, 4, 5, 7, 9, 14, 16, 21, 24, and 31 [14,15].
Although the distribution of serotypes in clinical cases may vary across geographic locations, S. suis serotype 2 is universally recognized as the most prevalent pathotype in both swine and humans worldwide [1]. Therefore, most studies have focused on S. suis serotype 2. However, different serotypes exhibit diverse characteristics in population structure and pathogenicity. In recent years, we have noticed an increase in the isolation rate of S. suis serotype 4 in pig populations. In addition, the report of the first human case caused by serotype 4 dated back to 1988 in the Netherlands, and the second human case caused by ST94 strain of serotype 4 was reported in 2018 in Thailand [16,17]. Notably, S. suis serotype 4 has been identified as one of the most prevalent serotypes in diseased pigs in Asia, and strains of this serotype have also been detected in healthy and diseased pigs in specific European and North American nations [6,18–21]. In a recent study, Murray et al. identified 10 pathogenic lineages of S. suis based on isolates sampled from healthy and diseased pigs, wild boar, and humans, from Asia, North America, Europe, and Australia [22]. They revealed that 80.36% of S. suis serotype 4 isolates (90/112) belong to these pathogenic lineages [22]. These findings highlight the significance of S. suis serotype 4 in swine streptococcusis. However, except for the information in human case reports and a few epidemiologic studies, the information on S. suis serotype 4 remains exceedingly limited.
In this study, a total of 126 S. suis serotype 4 genomes from eight different countries were analyzed, including one isolate from a patient with septicemia. A systematic bioinformatic analysis was conducted to investigate their population structure, phylogenetic relationship, putative virulence-associated genes, antibiotic resistance genes, and dissemination vehicles of antibiotic resistance genes. Additionally, animal infection experiments, human cell cytotoxicity assays, and antimicrobial susceptibility testing were performed on S. suis serotype 4 strains isolated from pigs and human to assess their pathogenicity and resistance characteristics. This study contributes to our understanding of S. suis serotype 4 and provides valuable information for the surveillance and prevention of this serotype.
Materials and methods
Bacterial strains and culture conditions
To investigate the characteristics of S. suis serotype 4 population, 48 strains isolated from our labs and 78 genomes from NCBI database were used in this study, as shown in Table 1. The 48 strains were collected from diseased and healthy pigs in China between 2014 and 2022. All strains were confirmed to be S. suis by analyzing their 16S rRNA gene sequences [23] and recN gene [24]. Furthermore, these strains were identified as serotype 4 by the PCR method based on the serotype 4 specific wzy gene [25] and the agglutination test using serotype 4 specific serum purchased from Statens Serum Institute (Copenhagen, Denmark). In addition, 78 S. suis serotype 4 genomes downloaded from the NCBI database originated from eight different countries, consisting of 30 from UK, 21 from China, ten from Canada, seven from Thailand, four from the Netherlands, four from the USA, and one each from Denmark and Spain. These genomes harboured S. suis serotype 4 specific wzy gene and were isolated from 1991 to 2019. The human strain ID36054 was isolated from a patient with septicemia reported in 2018 [17,26]. Strains were cultured in Todd-Hewitt broth (THB, Hope Bio-Technology Co., Ltd, China) and plated on THB agar containing 5% sheep blood at 37°C and 5% CO2.
Table 1.
The information of S. suis serotype 4 strains used in this study.
| Lineages | Strains | Accession number | ST | CC | MCG | Country | Date | Host | Isolation | Source |
|---|---|---|---|---|---|---|---|---|---|---|
| Lineage 1 | CPD27 | SAMN12784764 | 17 | 17 | 1 | China | 2010 | Pig | / | NCBI |
| LSSP193 | SAMN26554949 | 17 | 17 | 1 | China | 2017 | Pig | / | NCBI | |
| SC5B93 | SAMN14687788 | 17 | 17 | 1 | China | 2019 | Pig | / | NCBI | |
| ND7 | SAMN34237859 | 17 | 17 | 1 | China | 2014 | Diseased pig | Lung | This study | |
| ND83 | SAMN34237860 | 17 | 17 | 1 | China | 2014 | Diseased pig | Lung | This study | |
| ND84 | SAMN34237861 | 17 | 17 | 1 | China | 2014 | Diseased pig | Lung | This study | |
| ND90 | SAMN34237862 | 17 | 17 | 1 | China | 2014 | Diseased pig | Lung | This study | |
| WUSS270 | SAMN34237819 | 17 | 17 | 1 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS304 | SAMN34237824 | 17 | 17 | 1 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS388 | SAMN34237830 | 17 | 17 | 1 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS406 | SAMN34237833 | 17 | 17 | 1 | China | 2017 | Healthy pig | Tonsil | This study | |
| 2018WUSS011 | SAMN34237836 | 17 | 17 | 1 | China | 2018 | Healthy pig | Tonsil | This study | |
| CPD30 | SAMN12784768 | 850 | 17 | 1 | China | 2011 | Pig | / | NCBI | |
| WUSS303 | SAMN34237823 | 850 | 17 | 1 | China | 2017 | Healthy pig | Tonsil | This study | |
| 2021WUSS074 | SAMN34237846 | 2224 | 17 | 1 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2021WUSS078 | SAMN34237850 | 2224 | 17 | 1 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2021WUSS076 | SAMN34237848 | 2224 | 17 | 1 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2021WUSS079 | SAMN34237851 | 2224 | 17 | 1 | China | 2021 | Healthy pig | Tonsil | This study | |
| CPD39 | SAMN12784777 | 2235 | 17 | 1 | China | 2010 | Pig | / | NCBI | |
| CPD29 | SAMN12784766 | 2235 | 17 | 1 | China | 2010 | Pig | / | NCBI | |
| LSSP132 | SAMN26111036 | 2236 | 17 | 1 | China | 2017 | Pig | Brain | NCBI | |
| GD-0057 | SAMEA3595235 | 17 | 17 | 1 | Netherlands | 2004 | Diseased pig | CSF | NCBI | |
| GD-0073 | SAMEA3595242 | 17 | 17 | 1 | Netherlands | 2005 | Diseased pig | CSF | NCBI | |
| GD-0098 | SAMEA3595254 | 17 | 17 | 1 | Netherlands | 2006 | Diseased pig | CSF | NCBI | |
| MA6 | SAMN21439331 | 17 | 17 | 1 | Netherlands | 2017 | Diseased pig | Brain/blood | NCBI | |
| MA2 | SAMN21439327 | 17 | 17 | 1 | Canada | 2016 | Pig | Tonsil | NCBI | |
| DB1V3-4A | SAMN14932575 | 17 | 17 | 1 | Canada | 2016 | Pig | / | NCBI | |
| 40439 | SAMN13975665 | 17 | 17 | 1 | USA | 2017 | Pig | / | NCBI | |
| 40458 | SAMN13975647 | 17 | 17 | 1 | USA | 2016 | Pig | / | NCBI | |
| JT9 | SAMN29093732 | 17 | 17 | 1 | Spain | 2018 | Pig | Brain | NCBI | |
| Lineage 2 | SS967 | SAMN14933159 | 23 | 87 | 2 | UK | 2010 | Pig | / | NCBI |
| SS1048 | SAMN14932752 | 23 | 87 | 2 | UK | 2010 | Pig | / | NCBI | |
| LSS20 | SAMN14932632 | 23 | 87 | 2 | UK | 2010 | Pig | / | NCBI | |
| S14O | SAMEA3234013 | 23 | 87 | 2 | UK | 2010 | Diseased pig | Lung | NCBI | |
| S97A | SAMEA3234092 | 23 | 87 | 2 | UK | 2010 | Pig | Lung | NCBI | |
| LS0M | SAMEA3233887 | 23 | 87 | 2 | UK | 2010 | Healthy pig | Tonsil | NCBI | |
| SS967_2 | SAMEA1316593 | 23 | 87 | 2 | UK | 2012 | Pig | / | NCBI | |
| SS1048_2 | SAMEA1316599 | 23 | 87 | 2 | UK | 2012 | Pig | / | NCBI | |
| LSS20_2 | SAMEA1316631 | 23 | 87 | 2 | UK | 2012 | Pig | / | NCBI | |
| TMW-SS042 | SAMN14933224 | 23 | 87 | 2 | UK | 2013 | Pig | / | NCBI | |
| LSS94 | SAMN14932706 | 862 | 87 | 2 | UK | 2011 | Pig | / | NCBI | |
| LS4P | SAMEA3233921 | 862 | 87 | 2 | UK | 2011 | Healthy pig | Tonsil | NCBI | |
| LSS94_2 | SAMEA1316533 | 862 | 87 | 2 | UK | 2012 | Pig | / | NCBI | |
| 6407a | SAMN02905150 | 54 | 54 | 3 | Denmark | / | Pig | / | NCBI | |
| Lineage 3 | 942 | SAMN08295926 | 94 | 94 | 3 | China | 2013 | Pig | Tonsil | NCBI |
| 944 | SAMN08295927 | 94 | 94 | 3 | China | 2013 | Pig | Tonsil | NCBI | |
| 1044 | SAMN08295942 | 94 | 94 | 3 | China | 2013 | Pig | Tonsil | NCBI | |
| SH1510 | SAMN09460428 | 94 | 94 | 3 | China | 2015 | Pig | Lung | NCBI | |
| LSSP204 | SAMN26554953 | 94 | 94 | 3 | China | 2017 | Pig | / | NCBI | |
| LSSP213 | SAMN26554957 | 94 | 94 | 3 | China | 2018 | Pig | / | NCBI | |
| LSSP237 | SAMN28125328 | 94 | 94 | 3 | China | 2018 | Pig | / | NCBI | |
| ND6 | SAMN34237858 | 94 | 94 | 3 | China | 2014 | Diseased pig | Lung | This study | |
| WUSS026 | SAMN34237817 | 94 | 94 | 3 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS273 | SAMN34237820 | 94 | 94 | 3 | China | 2017 | Healthy pig | Tonsil | This study | |
| 2021WUSS075 | SAMN34237847 | 94 | 94 | 3 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2021WUSS077 | SAMN34237849 | 94 | 94 | 3 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2021WUSS080 | SAMN34237852 | 94 | 94 | 3 | China | 2021 | Healthy pig | Tonsil | This study | |
| WUSS326 | SAMN34237826 | 1175 | 94 | 3 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS329 | SAMN34237827 | 1175 | 94 | 3 | China | 2017 | Healthy pig | Tonsil | This study | |
| 2018WUSS156 | SAMN34237840 | 2220 | 94 | 3 | China | 2018 | Diseased pig | / | This study | |
| SS1042 | SAMN14932750 | 911 | 94 | 3 | UK | 2010 | Pig | / | NCBI | |
| SS1041 | SAMN14932749 | 911 | 94 | 3 | UK | 2010 | Pig | / | NCBI | |
| SS1040 | SAMN14932748 | 911 | 94 | 3 | UK | 2010 | Pig | / | NCBI | |
| S14J | SAMEA3234009 | 911 | 94 | 3 | UK | 2010 | Diseased pig | Lung | NCBI | |
| S14K | SAMEA3234010 | 911 | 94 | 3 | UK | 2010 | Diseased pig | Lung | NCBI | |
| S14L | SAMEA3234011 | 911 | 94 | 3 | UK | 2010 | Diseased pig | Lung | NCBI | |
| SS1042_2 | SAMEA1316637 | 911 | 94 | 3 | UK | 2012 | Pig | / | NCBI | |
| SS1041_2 | SAMEA1316538 | 911 | 94 | 3 | UK | 2012 | Pig | / | NCBI | |
| SS1040_2 | SAMEA1316654 | 911 | 94 | 3 | UK | 2012 | Pig | / | NCBI | |
| TMW-SS070 | SAMN14933250 | 911 | 94 | 3 | UK | 2014 | Pig | / | NCBI | |
| TRG6 | SAMN31277175 | 94 | 94 | 3 | Thailand | 2010 | Diseased pig | Lung | NCBI | |
| ID36054 | SAMN31277174 | 94 | 94 | 3 | Thailand | 2011 | Homo sapiens | Blood | NCBI | |
| ID34693 | SAMN31277178 | 94 | 94 | 3 | Thailand | 2011 | Pig | Tonsil | NCBI | |
| ID34704 | SAMN31277179 | 94 | 94 | 3 | Thailand | 2011 | Pig | Tonsil | NCBI | |
| ID34545 | SAMN31277176 | 1689 | 94 | 3 | Thailand | 2011 | Pig | Tonsil | NCBI | |
| ID34553 | SAMN31277177 | 1689 | 94 | 3 | Thailand | 2011 | Pig | Tonsil | NCBI | |
| ID34572 | SAMN31277173 | 1689 | 94 | 3 | Thailand | 2011 | Healthy pig | Tonsil | NCBI | |
| 1602956 | SAMN14932473 | 94 | 94 | 3 | Canada | 2014 | Pig | / | NCBI | |
| 1665814 | SAMN14932502 | 1175 | 94 | 3 | Canada | 2014 | Pig | / | NCBI | |
| CPD36 | SAMN12784774 | 485 | 839 | 3 | China | 2013 | Pig | / | NCBI | |
| LSSP145 | SAMN26111047 | 485 | 839 | 3 | China | 2017 | Pig | Lung | NCBI | |
| LSSP144 | SAMN26111046 | 485 | 839 | 3 | China | 2017 | Pig | Lung | NCBI | |
| WUSS346 | SAMN34237829 | 485 | 839 | 3 | China | 2017 | Healthy pig | Tonsil | This study | |
| 2018WUSS160 | SAMN34237841 | 485 | 839 | 3 | China | 2018 | Diseased pig | Spleen | This study | |
| MY1C3-3C | SAMN14932601 | 839 | 839 | 3 | Canada | 2016 | Pig | / | NCBI | |
| MA4T3-4C | SAMN14932592 | 839 | 839 | 3 | Canada | 2016 | Pig | / | NCBI | |
| 40436 | SAMN13975668 | 839 | 839 | 3 | USA | 2016 | Pig | / | NCBI | |
| D16-010378 | SAMN14932573 | 977 | 108 | 3 | Canada | / | Pig | / | NCBI | |
| 1652716 | SAMN14932497 | 977 | 108 | 3 | Canada | 2014 | Pig | / | NCBI | |
| 1607743 | SAMN14932477 | 977 | 108 | 3 | Canada | 2014 | Pig | / | NCBI | |
| WUSS390 | SAMN34237831 | 977 | 108 | 3 | China | 2017 | Healthy pig | Tonsil | This study | |
| Lineage 4 | LOLA-SS006 | SAMN14932618 | 856 | 28 | 4 | UK | 2010 | Pig | / | NCBI |
| LL-U | SAMEA3233876 | 856 | 28 | 4 | UK | 2010 | Diseased pig | Lung | NCBI | |
| 91-178-2215 | SAMN14932532 | 2233 | 1372 | 4 | Canada | 1991 | Pig | / | NCBI | |
| Lineage 5 | WUSS435 | SAMN34237834 | 1067 | / | 7-2 | China | 2017 | Diseased pig | / | This study |
| WUSS436 | SAMN34237835 | 1067 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| 2019WUSS015 | SAMN34237842 | 2221 | / | 7-2 | China | 2019 | Healthy pig | Tonsil | This study | |
| 2019WUSS016 | SAMN34237843 | 2221 | / | 7-2 | China | 2019 | Healthy pig | Tonsil | This study | |
| 2020WUSS060 | SAMN34237845 | 2223 | / | 7-2 | China | 2020 | Healthy pig | Tonsil | This study | |
| 2022WUSS016 | SAMN34237853 | 2225 | / | 7-2 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2022WUSS017 | SAMN34237854 | 2226 | / | 7-2 | China | 2021 | Healthy pig | Tonsil | This study | |
| WUSS228 | SAMN34237818 | 2237 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS309 | SAMN34237825 | 2237 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS285 | SAMN34237821 | 2238 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS299 | SAMN34237822 | 2238 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS333 | SAMN34237828 | 2238 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| WUSS399 | SAMN34237832 | 2239 | / | 7-2 | China | 2017 | Healthy pig | Tonsil | This study | |
| CPD3 | SAMN12784778 | 935 | / | 7-3 | China | 2014 | Pig | / | NCBI | |
| HA1003 | SAMN09460429 | 1006 | / | 7-3 | China | 2010 | Healthy pig | Tonsil | NCBI | |
| 1367 | SAMN08295994 | 2229 | / | 7-3 | China | 2013 | Pig | Tonsil | NCBI | |
| 1369 | SAMN08295995 | 2229 | / | 7-3 | China | 2013 | Pig | Tonsil | NCBI | |
| 2018WUSS056 | SAMN34237837 | 2218 | / | 7-3 | China | 2018 | Healthy pig | Tonsil | This study | |
| 2018WUSS108 | SAMN34237838 | 2219 | / | 7-3 | China | 2018 | Healthy pig | Tonsil | This study | |
| 2018WUSS109 | SAMN34237839 | 2219 | / | 7-3 | China | 2018 | Healthy pig | Tonsil | This study | |
| 2020WUSS059 | SAMN34237844 | 2222 | / | 7-3 | China | 2020 | Healthy pig | Tonsil | This study | |
| 2022WUSS018 | SAMN31099739 | 2057 | / | 7-3 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2022WUSS019 | SAMN34237855 | 2227 | / | 7-3 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2022WUSS020 | SAMN34237856 | 2057 | / | 7-3 | China | 2021 | Healthy pig | Tonsil | This study | |
| 2022WUSS056 | SAMN34237857 | 2228 | / | 7-3 | China | 2022 | Healthy pig | Tonsil | This study | |
| 2022WUSS141 | SAMN31099758 | 2066 | / | 7-3 | China | 2022 | Healthy pig | Tonsil | This study | |
| LSS33 | SAMN14932646 | 895 | / | 7-3 | UK | 2011 | Pig | / | NCBI | |
| LS3A | SAMEA3233909 | 895 | / | 7-3 | UK | 2011 | Pig | / | NCBI | |
| SS1028 | SAMEA1316687 | 908 | / | 7-3 | UK | 2012 | Pig | / | NCBI | |
| S12X | SAMEA3233997 | 908 | / | 7-3 | UK | 2010 | Diseased pig | Brain | NCBI | |
| 270-6A | SAMN14933322 | 2234 | / | 7-3 | UK | 2013 | Pig | / | NCBI | |
| 32052 | SAMN13975691 | 1209 | / | 7-3 | USA | 2015 | Pig | / | NCBI |
/: unassigned.
Except for strain 6407, the remaining genomes from MCG group 3 were assigned to lineage 3.
Bioinformatic analysis of S. suis serotype 4 genomes
The draft genomes of 48 strains isolated from our labs were sequenced using Illumina NovaSeq PE150 at Beijing Novogene Bioinformatics Technology Co., Ltd (China). The multilocus sequence type (MLST) and the minimum core genome (MCG) groups of 126 S. suis serotype 4 genomes were determined using the PubMLST database [27] and a previously established approach [28], respectively. Additionally, the global optimal eBURST (goeBURST) analysis [29] was employed to classify clonal complexes (CCs). Bowtie 2 was used to identify single-nucleotide polymorphisms (SNPs) within S. suis serotype 4 genomes, using the genome sequence of SC84 (accession number FM252031) as a reference. The mutational SNP sites were selected based on the procedure described in a previous study [28], and the phylogenetic tree was constructed using the maximum likelihood method by FastTree v2.1.10. As an outgroup, Streptococcus pneumoniae ATCC 700669 (NC_011900) was used to root the tree, and tree visualization was completed using tvBOT v2.5.2 [30]. The distribution of 35 putative virulence-associated genes of S. suis, as described in previous reports [31,32] (listed in Table S1), was investigated among the 126 S. suis serotype 4 genomes. Genes with coverage <80% or a nucleotide sequence identity <80% were determined to be absent. Antibiotic resistance gene analysis was performed using ResFinder 4.1 [33]. The whole genome sequencing data was input for ResFinder 4.1, with parameters set at ≥ 80% identity over ≥ 80% coverage of the reference gene. Prophages were predicted using PHASTER [34]. The prophage is incomplete if the score is less than 60, questionable if it is between 70 and 90, and intact if it is greater than 90 [34]. The integrative and conjugative elements (ICEs) analysis based on the major insertion hotspots rplL and rum loci was conducted according to a previous study [35]. The conjugative plasmids carrying antibiotic resistance genes were predicted using VRprofile2 [36] and oriTfinder [37]. The obtained mobile genetic element (MGE) sequences were further annotated using an online RAST server [38], followed by comparison and visualization using the BLASTn programme inserted within Easyfig 2.2.3 software [39].
Animal infection experiments
Animal infection experiments were conducted at the Laboratory Animal Center of Nanjing Agricultural University (Permit number: SYXK (Su) 2021-0086). According to the population structure of S. suis serotype 4, we selected 34 of 48 strains isolated from our labs, along with the human isolate ID36054, for the zebrafish infection experiment. The infection protocol for zebrafish was described in our previous studies [40,41]. Briefly, bacteria were collected during the mid-log phase, washed twice in PBS, and then adjusted to the proper infection concentrations in PBS. Each experimental group comprised 15 zebrafish, with each fish receiving an intraperitoneal injection containing 3 × 106 CFU of S. suis in 20 µL of PBS. The mortality was recorded from 12 h until 96 h after the challenge. Then, strains highly pathogenic to zebrafish (mortality rate ≥ 80%) were chosen for the mouse infection experiment. Six-week-old BALB/c mice were purchased from the Shanghai SLAC Laboratory Animal Co., Ltd (China). Each experimental group comprised 10 mice, and they were intraperitoneally injected with 3 × 108 CFU of S. suis per mouse. After infection, the mortality of the mice was monitored for 10 days. In the animal infection experiments, the highly virulent S. suis serotype 2 strain SC070731 [42], non-virulent S. suis serotype 9 strain SH040917 [43], and an equivalent volume of PBS were included as controls. According to our previous reports [14,40,41], a strain with a mortality rate ≥ 80% in zebrafish and mice was defined as highly virulent. The Log-rank (Mantel–Cox) test was used to compare the survival curves of zebrafish and mice infected with S. suis strains.
Human cell cytotoxicity assays
Human lung adenocarcinoma cells (A549) and human brain microvascular endothelial cells (hBMEC) were used for cell cytotoxicity assays, according to previous reports [26,44–46]. The human isolate ID36054 and four pig isolates 2021WUSS075, 2018WUSS156, ND90, and 2018WUSS160, with a mortality rate of ≥ 80% in zebrafish and mice, were selected for cell cytotoxicity assays. Strains were cultured and collected during the mid-log phase and were prepared at a concentration of 1 × 107 CFU/mL in THB medium. The A549 and hBMEC cell lines were purchased from the Cell Resource Center, IBMS, CAMS/PUMC (Beijing, China) and cultured in F12/DMEM (Gibco, Carlsbad, USA) and DMEM (Hyclone, Beijing, China), respectively, each supplemented with 10% fetal bovine serum, and maintained at 37°C in an atmosphere of 5% CO2. For each experiment, A549 or hBMEC cells were plated into 24-well flat-bottom plates at 3 × 105 cells/well in 1 mL corresponding medium and maintained in 5% CO2 at 37°C for 48 h to allow cell confluence. Then, the cell number reached approximately 1 × 106 cells/well before the infection assays. The medium was changed every 24 h. In the cytotoxicity assay, S. suis (1 × 107 CFU/well) were added to A549 or hBMEC cells at the multiplicity of infection (MOI) of 10, incubated for 3 and 6 h at 37°C with 5% CO2, respectively. Following the manufacturer's instructions, the supernatant was collected to measure lactate dehydrogenase (LDH) release using the LDH Cytotoxicity Assay-Fluorescence Kit (Thermo Fisher). The unpaired t-test was used to compare the percentage of cytotoxicity of S. suis serotype 4 strains. This experiment has been performed with a minimum of three independent biological replicates.
Antimicrobial susceptibility testing
Minimum inhibitory concentrations (MICs) were determined using the broth microdilution method following the guidelines outlined in the Clinical and Laboratory Standards Institute (CLSI) document (M31-A3). The following 23 antibiotics of 11 categories were tested: β-lactam antibiotics (penicillin, cefotaxime, and amoxicillin), rifamycin (rifampin), glycopeptide (vancomycin), quinolones (marbofloxacin and enrofloxacin), oxazolidinone (linezolid), amphenicols (chloramphenicol and florfenicol), macrolides (tilmicosin, azithromycin, and erythromycin), pleuromutilins (valnemulin and tiamulin), aminoglycosides (gentamicin, streptomycin, kanamycin, and spectinomycin), lincosamides (clindamycin and lincomycin), and tetracyclines (doxycycline and tetracycline). These antibiotics were tested at concentrations ranging from 0.5–256 µg/mL, with breakpoints for resistance according to the CLSI document (VET08-ED4) and guidelines provided by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) (https://www.eucast.org/), as listed in our previous study [41].
Results
Population structure and phylogenetic relationship of S. suis serotype 4
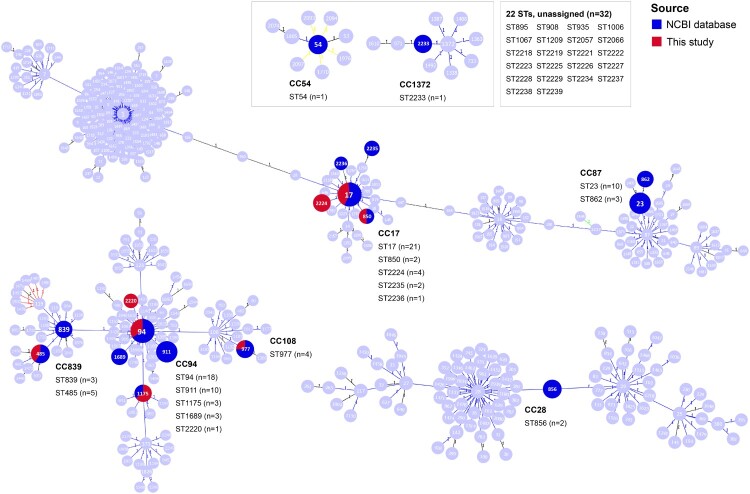
MLST analysis showed that the S. suis serotype 4 population exhibited significant genetic diversity, with 40 distinct sequence types (STs) found throughout 126 genomes (Table 1). Most prevalent were ST17 (n = 21) and ST94 (n = 18), followed by ST23 (n = 10), ST911 (n = 10), ST485 (n = 5), ST977 (n = 4), ST2224 (n = 4), ST839 (n = 3), ST862 (n = 3), ST1175 (n = 3), ST1689 (n = 3), and ST2238 (n = 3). Each of the remaining ST54, ST850, ST856, ST895, ST908, ST935, ST1006, ST1067, ST1209, ST2057, ST2066, ST2218-2223, ST2225-2229, ST2233-2237, and ST2239 consisted of two or one genomes. As shown in Figure 1, 18 STs (94/126 genomes, 74.60%) belonged to eight CCs, consisting of CC94 (ST94, ST911, ST1175, ST1689, and ST2220), CC17 (ST17, ST850, ST2224, ST2235, and ST2236), CC87 (ST23 and ST862), CC839 (ST839 and ST485), CC108 (ST977), CC28 (ST856), CC54 (ST54), and CC1372 (ST2233). In contrast, the remaining 22 STs (32/126 genomes, 25.40%) did not belong to any CCs. As shown in Figure 2, according to MCG analysis, 126 genomes belonged to six MCG groups, including MCG groups 1, 2, 3, 4, 7-2, and 7-3. Notably, two main CCs, CC17 (30/126 genomes, 23.81%) and CC94 (35/126 genomes, 27.78%), belonged to MCG groups 1 and 3, respectively. Most strains isolated from diseased pigs belonged to these two CCs. Moreover, the strain ID36054, responsible for human infections, also belonged to CC94. Based on an evolutionary tree constructed from SNPs in core genomes, the 126 genomes were divided into five lineages (Figure 2). Lineages 1 and 2 comprised MCG groups 1 and 2, respectively. Except for strain 6407, the remaining genomes from MCG group 3 were assigned to lineage 3. Lineage 4 was composed of MCG group 4. MCG groups 7-2 and 7-3 were collectively categorized as lineage 5.
Figure 1.
A goeBURST analysis of STs of the S. suis serotype 4 population. Numbers in circles indicate partial STs in S. suis MLST database. Deep blue circles and red circles indicate STs identified in the S. suis serotype 4 genomes downloaded from the NCBI database and sequenced in this study, respectively. “n” indicates the number of genomes. STs connected by a line mean that they have six identical alleles. Clusters of linked STs correspond to CCs.
Figure 2.
The phylogenetic tree and information of STs, CCs, MCG groups, and putative virulence-associated genes (VAGs) for the S. suis serotype 4 population. The superscripts “D” and “P” indicate strains originating from diseased pigs and human patients, respectively. The phylogenetic tree was constructed based on the SNPs of the core genome. The S. pneumoniae ATCC 700669 (NC_011900) was used as an outgroup to root the tree.
Distribution of putative virulence-associated genes in S. suis serotype 4
Thirty-five putative virulence-associated genes preferentially present in highly pathogenic S. suis serotype 2 strains [31,32] were analyzed among S. suis serotype 4 genomes. As shown in Figure 2, 18 of 35 putative virulence-associated genes were present in all S. suis serotype 4 genomes. The genes atl_2 (124/126, 98.41%), SSU05_1311 (124/126, 98.41%), and abpb (124/126, 98.41%) were present in most S. suis serotype 4 genomes. The remaining 14 of 35 putative virulence-associated genes showed distribution correlated with the MCG groups. All genomes within MCG group 1 exhibited the genotype of ef+/mrp+/sly+. For MCG groups 2 and 3, all genomes exhibited the genotype of ef-/mrp+/sly+. For MCG group 4, all genomes exhibited the genotype of ef-/mrp+/sly-. However, all three classical virulence marker genes were absent in MCG groups 7-2 and 7-3. Based on variation in the central region of the gene, mrp was classified as EU, NA1, and NA2 subtypes [14]. MCG groups 1 and 2 are all subtype NA2, while MCG groups 3 and 4 are mostly NA1 (Figure 2). Genes dltA, IdeSsuis, igdE, ofs, and sao were widespread in serotype 4 genomes, except for MCG groups 7-2 and 7-3. In contrast, the sbp2 gene was primarily distributed in MCG group 1, and hp0197 and hp0272 were only present in MCG groups 1 and 2. The regulatory genes rgg and revs were predominantly distributed in MCG group 1, and the tran gene was present in MCG groups 1 and 3. Importantly, it should be noted that all 35 putative virulence-associated genes were found to be present in MCG group 1 (Figure 2).
The results of animal infection experiments
To assess the virulence of the S. suis serotype 4 population, we selected 35 representative strains based on their distribution in the phylogenetic tree and their host for the zebrafish infection experiment. One strain ID36054 originated from a patient, eight strains (ND7, ND83, ND84, ND90, ND6, 2018WUSS156, 2018WUSS160, and WUSS435) originated from diseased pigs, and the remaining from healthy pigs (Table 2). As shown in Table 2, the mortality rate of zebrafish infected with nine strains (ID36054, WUSS406, 2018WUSS011, ND84, ND90, 2021WUSS075, 2018WUSS156, WUSS346, and 2018WUSS160) reached or exceeded 80%, classified as highly virulent strains. The survival curves of zebrafish infected with strains ID36054, 2018WUSS011, ND84, 2021WUSS075, WUSS346, and 2018WUSS160 showed no significant difference compared to zebrafish infected with the highly virulent control strain SC070731. Notably, strains WUSS406, 2018WUSS011, 2021WUSS075, and WUSS346 were isolated from healthy pigs. The abovementioned nine strains belonged to CC17 (4/11 representatives, 36.36%), CC94 (3/8 representatives, 37.50%), and CC839 (2/2 representatives, 100.00%), respectively. They belong to MCG groups 1 and 3, and harbour numerous crucial genes associated with virulence (Figure 2). There are also five strains (WUSS270, WUSS388, ND83, WUSS303, and WUSS026) with mortality rates between 50% and 80%, which also belong to CC17 and CC94. The mortality rate of zebrafish infected with the remaining strains, including all representative strains of MCG groups 7-2 and 7-3 (13/13 representatives, 100.00%), was <50%, classified as lowly virulent strains (Table 2). The gross pathology of zebrafish infected with highly virulent, moderately virulent, lowly virulent, and non-virulent strains of S. suis serotype 4 is shown in Figure S1.
Table 2.
The results of the zebrafish infection experiment.
| Strains | ST | CC | Hosta | Deaths at different post-infection time points | Total deaths | Mortality rate (%) | P value | Significanceb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12 h | 24 h | 36 h | 48 h | 60 h | 72 h | 84 h | 96 h | ||||||||
| WUSS270 | 17 | 17 | H | 0 | 4 | 3 | 1 | 1 | 0 | 0 | 0 | 9 | 60.00 | 0.0008 | *** |
| WUSS304 | 17 | 17 | H | 0 | 2 | 3 | 0 | 0 | 0 | 0 | 0 | 5 | 33.33 | <0.0001 | **** |
| WUSS388 | 17 | 17 | H | 0 | 7 | 4 | 0 | 0 | 0 | 0 | 0 | 11 | 73.33 | 0.0051 | ** |
| WUSS406 | 17 | 17 | H | 0 | 9 | 1 | 0 | 0 | 0 | 1 | 1 | 12 | 80.00 | 0.0225 | * |
| 2018WUSS011 | 17 | 17 | H | 2 | 8 | 4 | 0 | 0 | 0 | 0 | 0 | 14 | 93.33 | 0.1408 | ns |
| ND7 | 17 | 17 | D | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 6.67 | <0.0001 | **** |
| ND83 | 17 | 17 | D | 10 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 11 | 73.33 | 0.8457 | ns |
| ND84 | 17 | 17 | D | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 13 | 86.67 | 0.0921 | ns |
| ND90 | 17 | 17 | D | 0 | 8 | 3 | 0 | 1 | 0 | 0 | 0 | 12 | 80.00 | 0.0142 | * |
| WUSS303 | 850 | 17 | H | 0 | 2 | 5 | 1 | 0 | 0 | 0 | 0 | 8 | 53.33 | 0.0001 | *** |
| 2021WUSS076 | 2224 | 17 | H | 1 | 1 | 4 | 0 | 0 | 1 | 0 | 0 | 7 | 46.67 | 0.0002 | *** |
| ID36054 | 94 | 94 | P | 5 | 2 | 5 | 1 | 1 | 0 | 0 | 0 | 14 | 93.33 | 0.2186 | ns |
| WUSS026 | 94 | 94 | H | 1 | 3 | 4 | 1 | 1 | 0 | 0 | 0 | 10 | 66.67 | 0.0026 | ** |
| WUSS273 | 94 | 94 | H | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 4 | 26.67 | <0.0001 | **** |
| 2021WUSS075 | 94 | 94 | H | 6 | 5 | 1 | 2 | 0 | 0 | 0 | 0 | 14 | 93.33 | 0.8088 | ns |
| 2021WUSS077 | 94 | 94 | H | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 3 | 20.00 | <0.0001 | **** |
| ND6 | 94 | 94 | D | 3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 4 | 26.67 | 0.0007 | *** |
| WUSS329 | 1175 | 94 | H | 0 | 0 | 3 | 0 | 1 | 0 | 0 | 0 | 4 | 26.67 | <0.0001 | **** |
| 2018WUSS156 | 2220 | 94 | D | 0 | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 13 | 86.67 | 0.0405 | * |
| WUSS346 | 485 | 839 | H | 8 | 2 | 4 | 0 | 0 | 0 | 0 | 0 | 14 | 93.33 | 0.8375 | ns |
| 2018WUSS160 | 485 | 839 | D | 0 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 15 | 100.00 | 0.0979 | ns |
| WUSS390 | 977 | 108 | H | 0 | 9 | 1 | 0 | 0 | 0 | 0 | 0 | 10 | 66.67 | 0.0080 | ** |
| WUSS285 | 2238 | / | H | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 4 | 26.67 | 0.0002 | *** |
| WUSS309 | 2237 | / | H | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 20.00 | 0.0003 | *** |
| WUSS399 | 2239 | / | H | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 4 | 26.67 | <0.0001 | **** |
| WUSS435 | 1067 | / | D | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 3 | 20.00 | <0.0001 | **** |
| 2018WUSS056 | 2218 | / | H | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** |
| 2018WUSS108 | 2219 | / | H | 1 | 2 | 1 | 1 | 1 | 0 | 0 | 0 | 6 | 40.00 | 0.0004 | *** |
| 2020WUSS059 | 2222 | / | H | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 13.33 | <0.0001 | **** |
| 2022WUSS016 | 2225 | / | H | 4 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 7 | 46.67 | 0.0057 | ** |
| 2022WUSS017 | 2226 | / | H | 1 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 5 | 33.33 | 0.0004 | *** |
| 2022WUSS018 | 2057 | / | H | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** |
| 2022WUSS019 | 2227 | / | H | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 3 | 20.00 | <0.0001 | **** |
| 2022WUSS056 | 2228 | / | H | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** |
| 2022WUSS141 | 2066 | / | H | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 13.33 | <0.0001 | **** |
| SC070731 | 7 | 1 | D | 5 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 93.33 | – | – |
| SH040917 | / | / | H | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** |
| PBS | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** | |||
H indicates healthy pig, D indicates diseased pig, and P indicates human patient.
The survival outcome of serotype 4 strains for zebrafish was compared with that of the highly pathogenic strain SC070731 using the Log-rank (Mantel-Cox) test. * indicates p < 0.05, ** indicates p < 0.01, *** indicates p < 0.001, **** indicates p < 0.0001, and “ns” indicates no significant difference.
/: unassigned.
The mouse infection experiment was performed further to validate the virulence of S. suis serotype 4 strains. Nine strains with ≥ 80% mortality to zebrafish and two strains with no mortality to zebrafish were selected for BALB/c mice infection. As shown in Table 3, the mortality rate of mice infected with eight strains with ≥ 80% mortality to zebrafish was also ≥ 80%. The survival curves of mice infected with strains ID36054, WUSS406, ND90, 2021WUSS075, 2018WUSS156, WUSS346, and 2018WUSS160 showed no significant difference compared to mice infected with the highly virulent control strain SC070731. Strain ND84, with 86.67% mortality to zebrafish, exhibited 60% mortality to mice. Two strains with no mortality to zebrafish also showed no mortality to mice. The results of mice and zebrafish infection experiments were consistent. In summary, 35.00% (7/20) of representative pig isolates of CC17, CC94, and CC839 were highly virulent in zebrafish and mice (mortality rate ≥ 80%), similar to the human isolate ID36054 (belonging to CC94) (Table 3). Thus, S. suis serotype 4 strains of CC17 (ST17), CC94 (ST94, ST2220), and CC839 (ST485) are potentially pathogenic.
Table 3.
The results of the BALB/c mice infection experiment.
| Strains | Mortality rate (%)a | CC | Deaths at different post-infection time points | Total deaths | Mortality rate (%)b | P value | Significancec | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 d | 2 d | 3 d | 4 d | 5 d | 6 d | 7 d | 8 d | 9 d | 10 d | |||||||
| WUSS406 | 80.00 | 17 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 100.00 | 0.3173 | ns |
| 2018WUSS011 | 93.33 | 17 | 5 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 8 | 80.00 | 0.0111 | * |
| ND84 | 86.67 | 17 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 60.00 | 0.0317 | * |
| ND90 | 80.00 | 17 | 7 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 80.00 | 0.1512 | ns |
| ID36054 | 93.33 | 94 | 9 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 100.00 | >0.9999 | ns |
| 2021WUSS075 | 93.33 | 94 | 9 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 100.00 | >0.9999 | ns |
| 2018WUSS156 | 86.67 | 94 | 6 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 80.00 | 0.0863 | ns |
| WUSS346 | 93.33 | 839 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 100.00 | 0.3173 | ns |
| 2018WUSS160 | 100.00 | 839 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 90.00 | 0.5567 | ns |
| 2022WUSS018 | 0.00 | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** |
| 2022WUSS056 | 0.00 | / | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** |
| SC070731 | 93.33 | 1 | 9 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 100.00 | - | - |
| PBS | 0.00 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.00 | <0.0001 | **** | |
Mortality rate of each strain in zebrafish.
Mortality rate of each strain in BALB/c mice.
The survival outcome of serotype 4 strains for mice was compared with that of the highly pathogenic strain SC070731 using the Log-rank (Mantel-Cox) test. * indicates p < 0.05, ** indicates p < 0.01, *** indicates p < 0.001, **** indicates p < 0.0001, and “ns” indicates no significant difference.
/: unassigned.
Cell cytotoxicity
To evaluate the cell cytotoxicity of highly virulent S. suis serotype 4 strains on human cells, the human isolate ID36054 and four pig isolates belonging to CC17, CC94, and CC839 were selected for cell cytotoxicity assays, and the mortality rate of these strains in both zebrafish and mice is ≥ 80%. As shown in Figure 3(A), the human strain ID36054 exhibited significant cytotoxicity to A549 at 3 h incubation with 93.04% cytotoxicity, and the pig isolates showed 88.67%−100.00% cytotoxicity. As shown in Figure 3(B), the human strain ID36054 exhibited significant cytotoxicity to hBMEC at 6 h incubation with 66.42% cytotoxicity, and the pig isolates showed 45.25%−67.41% cytotoxicity. These data indicate that the human and pig isolates of S. suis serotype 4 exhibit significant cytotoxicity to human cells.
Figure 3.
Human cell cytotoxicity assays of S. suis serotype 4 highly virulent strains. Cell cytotoxicity of S. suis strains on A549 (A) for 3 h and hBMEC (B) for 6 h. The percentage of cytotoxicity of S. suis serotype 4 strains was compared with that of the human reference strain ID36054 using an unpaired t-test. A summary of the p-values is provided, with an asterisk indicating a significant difference (p < 0.05) and “ns” denoting no significant difference.
Distribution and dissemination vehicles of antibiotic resistance genes in S. suis serotype 4
The distribution of antibiotic resistance genes in 126 S. suis serotype 4 genomes was investigated. We identified twenty-two distinct antibiotic resistance genes, which showed ≥ 95% identity in nucleotide sequence across over 90% coverage of the reference gene. They were classified into six categories: tetracyclines, macrolides-lincosamides-streptogramin B (MLSB), aminoglycosides, lincosamides, oxazolidinones, and chloramphenicol (Figure 4). The distribution of tetracycline resistance genes was found to be highest at a rate of 81.75% (103/126), corresponding to the phenotypes of resistance to doxycycline and tetracycline, with tet(O) being the predominant gene (77/126, 61.11%), followed by tet(M) (22/126, 17.46%), tet(40) (7/126, 5.56%), tet(O/W/32/O) (6/126, 4.76%), and tet(L) (3/126, 2.38%). Ninety-two genomes (73.02%) possess the MLSB resistance gene erm(B), corresponding to the phenotypes of resistance to erythromycin, azithromycin, lincomycin, and clindamycin. Other lincosamides resistance genes lsaE (20/126, 15.87%), lnuB (20/126, 15.87%), and lnuC (2/126, 1.59%) were also found in 22 genomes (17.46%). Nine types of aminoglycoside resistant genes were found among 53 genomes (42.06%), consisting of ant(6)-Ia (51/126, 40.48%), aac(6′)-aph(2″) (36/126, 28.57%), aph(3′)-III (6/126, 4.76%), as well as one each of ant(6)-Ib, aph(2″)-Ia, aph(2″)-Ic, aph(3′)-IIa, aph(4)-Ia, and aac(3)-IV. The florfenicol and linezolid resistance gene optrA (12/126, 9.52%), chloramphenicol resistance gene cat (8/126, 6.35%), and efflux pump gene mef(A) (6/126, 4.76%) were also found in the S. suis serotype 4 genomes.
Figure 4.
The distribution of antibiotic resistance genes (ARGs), prophages, and ICEs for S. suis serotype 4 genomes. Color-filled square boxes on the periphery indicate the presence of antibiotic resistance genes-associated prophages and ICEs, and unfilled boxes indicate their absence.
Our investigation successfully identified an intact prophage with a score of 100 in one genome. Moreover, questionable prophages with predicted scores of 90 and 80 were present in seven and fifteen genomes, respectively (Figure 4). Integration analysis revealed that these prophages were primarily inserted into the rum locus. However, prophages ΦSsuWUSS303 and ΦSsuCPD30 were inserted into the comEC locus instead. It is worth mentioning that the MLSB resistance gene erm(B), aminoglycosides resistance genes ant(6)-Ia and aac(6′)-aph(2″), tetracyclines resistance genes tet(O), tet(O/W/32/O), and tet(40), and other resistance genes optrA, mef(A), lsaE, lnuB, lnuC, and cat were detected within prophages (Figure 5(A)). In addition, nine different ICEs were distributed in 12 genomes, containing five ICEs inserted into the rplL locus and four ICEs inserted into the rum locus (Figure 4). These ICEs predominantly carried erm(B) and tet(O) genes (Figure 5(B)). We utilized online analysis platforms to detect conjugative plasmids carrying antibiotic resistance genes in the strains studied. The results indicate that no conjugative plasmids carrying antibiotic resistance genes were found. This discovery implies that prophages were the primary vehicle of antibiotic resistance genes and played a crucial role in disseminating MLSB, tetracyclines, aminoglycosides, and linezolid resistance genes. Additionally, the presence of ICEs further facilitated the dissemination of MLSB and tetracycline resistance genes. We also observed that genomes harbouring prophages associated with antibiotic resistance genes were exclusively isolated from China, whereas those harbouring ICEs associated with antibiotic resistance genes were discovered mainly in other nations (Figure 4).
Figure 5.
Genetic context of antibiotic resistance genes-associated prophages and ICEs in S. suis serotype 4 genomes. The direction of transcription for each gene is denoted by arrows, and distinct colours represent the various genes. (A) Prophages with scores of 100, 90, and 80 by PHASTER analysis. (B) ICE structure predicted by ICEfinder software. T4SS, type IV secretion system; T4CP, type IV coupling protein.
Antimicrobial susceptibility profiles of S. suis serotype 4 strains
We detected the antibiotic resistance phenotypes of 48 S. suis serotype 4 strains isolated from our labs using the broth microdilution method. The MIC values of 23 antimicrobials tested for 48 strains are listed in Table S2. As shown in Figure 6(A), all strains were resistant to lincomycin and clindamycin, and most strains were also resistant to erythromycin (97.92%), azithromycin (97.92%), doxycycline (93.75%), and tetracycline (87.50%). The presence of the genes erm(B) (89.58%), lsaE (20.83%), and lnuB (20.83%) conferred resistance to lincosamides and macrolides, and the presence of the genes tet(O) (60.42%), tet(M) (33.33%), and tet(O/W/32/O) (8.33%) conferred resistance to tetracyclines (Figure 4, Table S2). The resistance rate for kanamycin, streptomycin, gentamicin, tilmicosin, tiamulin, spectinomycin, florfenicol, and valnemulin was 64.58%, 62.50%, 60.42%, 35.42%, 31.25%, 25.00%, 22.92%, and 18.75%, respectively. The carriage of the genes aac(6′)-aph(2″) (64.58%) and aph(3′)-III (6.25%) led to high-level resistance to gentamicin and kanamycin, while the presence of the gene ant(6)-Ia (72.92%) resulted in high-level resistance to streptomycin (Figure 4, Table S2). All S. suis serotype 4 strains displayed susceptibility to amoxicillin, cefotaxime, and vancomycin. There was a low resistance rate to enrofloxacin (14.58%), marbofloxacin (14.58%), penicillin (10.42%), linezolid (10.42%), chloramphenicol (8.33%), and rifampin (4.17%). It is worth noting that 95.83% (46/48) of the strains were resistant to ≥3 classes of antimicrobial agents (Figure 6(B)) and were classified as multidrug-resistant. Most strains were resistant to four or five classes of antimicrobial agents.
Figure 6.
The antimicrobial susceptibility profiles in S. suis serotype 4 strains isolated from our labs. (A) The resistance rates of 48 strains to 23 antibiotics. PEN, Penicillin; AMO, Amoxicillin; CTX, Cefotaxime; RIF, Rifampin; VAN, Vancomycin; LNZ, Linezolid; ENR, Enrofloxacin; MAR, Marbofloxacin; CHL, Chloramphenicol; FLO, Florfenicol; LIN, Lincomycin; CLI, Clindamycin; TIA, Tiamulin; VAL, Valnemulin; GEN, Gentamicin; KAN, Kanamycin; STR, Streptomycin; SPE, Spectinomycin; TIM, Tilmicosin; ERY, Erythromycin; AZM, Azithromycin; DOX, Doxycycline; TET, Tetracycline. (B) The resistance rates of 48 strains to 11 categories of antibiotics.
Discussion
Serotyping is vital for gaining insights into bacterial epidemiology, such as its prevalence across different geographic regions and transmission dynamics. Identifying specific serotypes or STs linked to outbreaks offer invaluable information for epidemiologists to comprehend disease spread and implement targeted control measures. Currently available vaccines against S. suis infection are mainly bacterins, which are supposed to confer serotype-specific protection. Thus, serotyping helps to develop serotype-specific vaccines based on epidemiological data.
In the recent study by Murray et al., ten pathogenic lineages of S. suis were identified, among which disease-associated serotypes 1, 1/2, 2, 3, 4, 5, 6, 7, 8, 9, and 14 were found to be prevalent [22]. However, different S. suis serotypes exhibit diverse population structure and pathogenicity characteristics. Therefore, for the pathogenicity of S. suis, it is important to not only focus on disease-associated serotypes but also ST [1,6]. S. suis serotype 2 is the most prevalent pathotype in both swine and humans worldwide [1]. The common pathogenic ST of S. suis serotype 2 are ST1, ST7, ST20, ST25, ST28, and ST104. Notably, ST1 strains belonging to MCG group 1 are globally distributed and demonstrate the highest pathogenicity in humans and pigs [6]. Besides this serotype, S. suis serotype 9 has emerged as the predominant serotype among diseased pigs in Western Europe; ST16 strains showed a zoonotic potential [1,47,48]. S. suis serotype 7, a non-negligible pathotype with the most predominant STs being ST29, ST373, and ST94, prevalent in Europe, China, and North America, respectively; ST373 strains were responsible for septicemia in humans and widely prevalent in China [14]. S. suis serotype 8, as one of the main pathogenic serotypes causing clinical diseases in pigs, was frequently isolated from clinical cases in Asia, North America, South America, and Europe [1,49,50]. Among the isolates of serotype 8 in China, the predominant STs included ST308, ST198, and ST1241, with the ST1241 strains showing significant pathogenicity in zebrafish and mice [40]. The main purpose of population structure analysis for different S. suis serotypes is to identify the high-pathogenic sub-lineages from the whole population and provide important information to precisely prevent the infection caused by the high-pathogenic sub-lineage strains.
Between 2002 and 2013, in China and South Korea, S. suis serotype 4 ranked as the third most predominant serotype isolated from infected pigs, accounting for 5.6% [1]. In Canada, there was an increasing trend in the proportion of S. suis serotype 4 among isolates from diseased pigs between 2009 and 2011, rising from 3.7% to 5.9% [18]. In Germany, S. suis serotype 4 accounted for 10% and 10.3% of S. suis isolates identified between 1996–2004 and 2015–2016, respectively [20]. In this study, the results of animal infection experiments showed that among the representative strains of CC17 (ST17), CC94 (ST94, ST2220), and CC839 (ST485), 66.67% (14/21) of the strains exhibited a mortality rate exceeding 50% in zebrafish (Table 2). Therefore, S. suis serotype 4 is a non-negligible pathotype.
In a recent study, Hatrongjit et al. analyzed the genome of seven serotype 4 strains belonging to CC94 and group 3 [26]; they performed cytotoxicity assays using human cell lines and demonstrated that CC94 serotype 4 strains are potentially virulent [26]. However, the virulence of those strains was not validated in animal models, and only seven strains were analyzed in their study. In the present study, we investigated the population structure and pathogenicity of the S. suis serotype 4 population based on 126 isolates from eight different countries. Within the S. suis serotype 4 population, CC17 and CC94, which belong to MCG group 1 and MCG group 3, respectively, exhibited the highest proportions. Chen et al. reported seven MCG groups among S. suis population; MCG group 1 included all the highly virulent isolates of ST1, the epidemic isolates of ST7, and all isolates from human infections and outbreaks [28]. Notably, S. suis serotype 4 strain ID36054 causing human infection belongs to CC94. In this study, the results of animal infection experiments showed that 35.00% (7/20) of pig isolates from CC17, CC94, and CC839 (also belonging to MCG group 3) were highly virulent in zebrafish and mice, similar to the human isolate ID36054. We found a correlation between the virulence phenotype and the distribution of putative virulence-related genes. These highly virulent strains harbour numerous crucial genes associated with virulence, particularly including mrp, sly, IdeSsuis, igdE, sbp2, hp0197, hp0272, rgg, and tran which have been identified as potential zoonotic virulence factors in a recent study [51]. In addition, we found that the genotype of S. suis classical virulence markers in highly virulent strains was ef+/mrpNA2/sly+ or ef-/mrpNA1/sly+. Notably, the genotype of ef+/mrpNA2/sly+ was prevalent in human infection strains [52,53]. In contrast, all strains from MCG groups 7-2 and 7-3 were lowly virulent in zebrafish. Compared to the highly virulent strains, they lack several crucial virulence genes, including ef, mrp, sly, ofs, sao, dltA, IdeSsuis, igdE, revS, rgg, and tran. Furthermore, cell cytotoxicity assays confirmed that the human and pig isolates of S. suis serotype 4 exhibit significant cytotoxicity to human cells A549 and hBMEC. Thus, S. suis serotype 4 strains of CC17, CC94, and CC839 exhibit significant threat to humans and pigs and should be monitored.
Previous studies have shown S. suis to be a reservoir of clinically significant antibiotic resistance genes for major streptococcal pathogens [35,54,55]. In this study, we observed that 95.83% S. suis serotype 4 strains isolated from our labs were multidrug-resistant. The presence of erm(B), tet genes, ant(6)-Ia, aac(6′)-aph(2″), and optrA were the main reasons for the prevalent resistance phenotypes to macrolides, lincosamides, tetracyclines, aminoglycosides, and linezolid in serotype 4 strains. Prophages were identified as their primary vehicle, and ICEs further facilitated the dissemination of erm(B) and tet(O). In Streptococcus species, the dissemination of antibiotic resistance genes is primarily facilitated through the horizontal gene transfer of ICEs and prophages [35,56–60]. However, major vehicles may differ for S. suis serotypes. For example, prophages were the primary vehicle of antibiotic resistance genes in serotype 31 strains [41]. In serotype 7 and 8 strains, antibiotic resistance genes were mainly disseminated by integrative and mobilizable elements (IMEs) [40]. We found that S. suis serotype 4 genomes containing prophages associated with antibiotic resistance genes were mainly isolated from China, while those containing ICEs associated with antibiotic resistance genes were mainly discovered in other countries, suggests that the predominant vehicles for the spread of antibiotic resistance genes may vary by nation or region.
In conclusion, S. suis serotype 4 exhibited a distinct population structure. 61.90% of strains (78/126) were clustered into MCG groups 1 and 3, with potential pathogenicity in humans and pigs, particularly strains belonging to CC17, CC94, and CC839. S. suis serotype 4 strains showed multidrug-resistant, with prophages crucial in disseminating antibiotic resistance genes. Our study expands the understanding of the S. suis serotype 4 population and provides valuable information for the surveillance and prevention of this serotype.
Supplementary Material
Funding Statement
This work was supported by grants from the National Key Research and Development Program of China [2021YFD1800402], the National Natural Science Foundation of China [32172859], Open Project Program of Jiangsu Key Laboratory of Zoonosis [R2103], and Open Project Program of Engineering Research Center for the Prevention and Control of Animal Original Zoonosis, Fujian Province University [2021ZW001].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethical approval
Animal infection experiments were conducted at the Laboratory Animal Center of Nanjing Agricultural University (Permit number: SYXK (Su) 2021-0086). This study and the application of the animal experiments were reviewed and approved by the Experimental Animal Welfare and Ethics Committee of Nanjing Agricultural University and were performed according to Animal Welfare Agency Guidelines.
References
- 1.Goyette-Desjardins G, Auger JP, Xu J, et al. Streptococcus suis, an important pig pathogen and emerging zoonotic agent-an update on the worldwide distribution based on serotyping and sequence typing. Emerg Microbes Infect. 2014 Jun;3(6):e45. doi: 10.1038/emi.2014.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Segura M, Fittipaldi N, Calzas C, et al. Critical Streptococcus suis virulence factors: are they all really critical? Trends Microbiol. 2017 Jul;25(7):585–599. doi: 10.1016/j.tim.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 3.Gottschalk M, Xu J, Calzas C, et al. Streptococcus suis: a new emerging or an old neglected zoonotic pathogen? Future Microbiol. 2010 Mar;5(3):371–391. doi: 10.2217/fmb.10.2 [DOI] [PubMed] [Google Scholar]
- 4.van Samkar A, Brouwer MC, Schultsz C, et al. Streptococcus suis meningitis: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2015;9(10):e0004191. doi: 10.1371/journal.pntd.0004191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wertheim HF, Nguyen HN, Taylor W, et al. Streptococcus suis, an important cause of adult bacterial meningitis in northern Vietnam. PLoS One. 2009 Jun 22;4(6):e5973. doi: 10.1371/journal.pone.0005973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Segura M, Aragon V, Brockmeier SL, et al. Update on Streptococcus suis research and prevention in the era of antimicrobial restriction: 4th international workshop on S. suis. Pathogens. 2020 May 14;9(5). doi: 10.3390/pathogens9050374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okura M, Osaki M, Nomoto R, et al. Current taxonomical situation of Streptococcus suis. Pathogens. 2016 Jun 24;5(3). doi: 10.3390/pathogens5030045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bojarska A, Janas K, Pejsak Z, et al. Diversity of serotypes and new cps loci variants among Streptococcus suis isolates from pigs in Poland and Belarus. Vet Microbiol. 2020 Jan;240:108534. doi: 10.1016/j.vetmic.2019.108534 [DOI] [PubMed] [Google Scholar]
- 9.Huang J, Liu X, Chen H, et al. Identification of six novel capsular polysaccharide loci (NCL) from Streptococcus suis multidrug resistant non-typeable strains and the pathogenic characteristic of strains carrying new NCLs. Transbound Emerg Dis. 2019 Mar;66(2):995–1003. doi: 10.1111/tbed.13123 [DOI] [PubMed] [Google Scholar]
- 10.Pan Z, Ma J, Dong W, et al. Novel variant serotype of streptococcus suis isolated from piglets with meningitis. Appl Environ Microbiol. 2015 Feb;81(3):976–985. doi: 10.1128/AEM.02962-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng H, Qiu X, Roy D, et al. Genotyping and investigating capsular polysaccharide synthesis gene loci of non-serotypeable Streptococcus suis isolated from diseased pigs in Canada. Vet Res. 2017 Feb 20;48(1):10. doi: 10.1186/s13567-017-0417-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu X, Bai X, Lan R, et al. Novel capsular polysaccharide loci and new diagnostic tools for high-throughput capsular gene typing in Streptococcus suis. Appl Environ Microbiol. 2016 Dec 15;82(24):7102–7112. doi: 10.1128/AEM.02102-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zheng H, Ji S, Liu Z, et al. Eight novel capsular polysaccharide synthesis gene loci identified in nontypeable Streptococcus suis isolates. Appl Environ Microbiol. 2015 Jun 15;81(12):4111–4119. doi: 10.1128/AEM.00315-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liang P, Wang M, Gottschalk M, et al. Genomic and pathogenic investigations of Streptococcus suis serotype 7 population derived from a human patient and pigs. Emerg Microbes Infect. 2021 Dec;10(1):1960–1974. doi: 10.1080/22221751.2021.1988725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatrongjit R, Fittipaldi N, Jenjaroenpun P, et al. Genomic comparison of two Streptococcus suis serotype 1 strains recovered from porcine and human disease cases. Sci Rep. 2023 Apr 3;13(1):5380. doi: 10.1038/s41598-023-27709-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arends JP, Zanen HC.. Meningitis caused by Streptococcus suis in humans. Rev Infect Dis. 1988 Jan-Feb;10(1):131–137. doi: 10.1093/clinids/10.1.131 [DOI] [PubMed] [Google Scholar]
- 17.Kerdsin A, Akeda Y, Takeuchi D, et al. Genotypic diversity of Streptococcus suis strains isolated from humans in Thailand. Eur J Clin Microbiol Infect Dis. 2018 May;37(5):917–925. doi: 10.1007/s10096-018-3208-8 [DOI] [PubMed] [Google Scholar]
- 18.Gottschalk M, Lacouture S, Bonifait L, et al. Characterization of Streptococcus suis isolates recovered between 2008 and 2011 from diseased pigs in Quebec, Canada. Vet Microbiol. 2013 Mar 23;162(2-4):819–825. doi: 10.1016/j.vetmic.2012.10.028 [DOI] [PubMed] [Google Scholar]
- 19.Hadjirin NF, Miller EL, Murray GGR, et al. Large-scale genomic analysis of antimicrobial resistance in the zoonotic pathogen Streptococcus suis. BMC Biol. 2021 Sep 7;19(1):191. doi: 10.1186/s12915-021-01094-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prufer TL, Rohde J, Verspohl J, et al. Molecular typing of Streptococcus suis strains isolated from diseased and healthy pigs between 1996 and 2016. PLoS One. 2019;14(1):e0210801. doi: 10.1371/journal.pone.0210801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Werinder A, Aspan A, Backhans A, et al. Streptococcus suis in Swedish grower pigs: occurrence, serotypes, and antimicrobial susceptibility. Acta Vet Scand. 2020 Jun 24;62(1):36. doi: 10.1186/s13028-020-00533-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray GGR, Hossain A, Miller EL, et al. The emergence and diversification of a zoonotic pathogen from within the microbiota of intensively farmed pigs. Proc Natl Acad Sci U S A. 2023 Nov 21;120(47):e2307773120. doi: 10.1073/pnas.2307773120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chatellier S, Harel J, Zhang Y, et al. Phylogenetic diversity of Streptococcus suis strains of various serotypes as revealed by 16S rRNA gene sequence comparison. Int J Syst Bacteriol. 1998 Apr;48(Pt 2):581–589. doi: 10.1099/00207713-48-2-581 [DOI] [PubMed] [Google Scholar]
- 24.Tien LHT, Nishibori T, Nishitani Y, et al. Reappraisal of the taxonomy of Streptococcus suis serotypes 20, 22, 26, and 33 based on DNA-DNA homology and sodA and recN phylogenies. Vet Microbiol. 2013 Mar 23;162(2–4):842–849. doi: 10.1016/j.vetmic.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 25.Liu Z, Zheng H, Gottschalk M, et al. Development of multiplex PCR assays for the identification of the 33 serotypes of Streptococcus suis. PLoS One. 2013;8(8):e72070. doi: 10.1371/journal.pone.0072070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hatrongjit R, Boueroy P, Jenjaroenpun P, et al. Genomic characterization and virulence of Streptococcus suis serotype 4 clonal complex 94 recovered from human and swine samples. PLoS One. 2023;18(7):e0288840. doi: 10.1371/journal.pone.0288840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jolley KA, Bray JE, Maiden MCJ.. Open-access bacterial population genomics: BIGSdb software, the PubMLST.org website and their applications. Wellcome Open Res. 2018;3:124. doi: 10.12688/wellcomeopenres.14826.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen C, Zhang W, Zheng H, et al. Minimum core genome sequence typing of bacterial pathogens: a unified approach for clinical and public health microbiology. J Clin Microbiol. 2013 Aug;51(8):2582–2591. doi: 10.1128/JCM.00535-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Francisco AP, Bugalho M, Ramirez M, et al. Global optimal eBURST analysis of multilocus typing data using a graphic matroid approach. BMC Bioinformatics. 2009 May 18;10:152. doi: 10.1186/1471-2105-10-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xie J, Chen Y, Cai G, et al. Tree Visualization By One Table (tvBOT): a web application for visualizing, modifying and annotating phylogenetic trees. Nucleic Acids Res. 2023 Jul 5;51(W1):W587–W592. doi: 10.1093/nar/gkad383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Segura M, Calzas C, Grenier D, et al. Initial steps of the pathogenesis of the infection caused by Streptococcus suis: fighting against nonspecific defenses. FEBS Lett. 2016 Nov;590(21):3772–3799. doi: 10.1002/1873-3468.12364 [DOI] [PubMed] [Google Scholar]
- 32.Tram G, Jennings MP, Blackall PJ, et al. Streptococcus suis pathogenesis-A diverse array of virulence factors for a zoonotic lifestyle. Adv Microb Physiol. 2021;78:217–257. doi: 10.1016/bs.ampbs.2020.12.002 [DOI] [PubMed] [Google Scholar]
- 33.Bortolaia V, Kaas RS, Ruppe E, et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J Antimicrob Chemother. 2020 Dec 1;75(12):3491–3500. doi: 10.1093/jac/dkaa345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arndt D, Grant JR, Marcu A, et al. PHASTER: a better, faster version of the PHAST phage search tool. Nucleic Acids Res. 2016 Jul 8;44(W1):W16–W21. doi: 10.1093/nar/gkw387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang J, Ma J, Shang K, et al. Evolution and diversity of the antimicrobial resistance associated mobilome in Streptococcus suis: a probable mobile genetic elements reservoir for other streptococci. Front Cell Infect Microbiol. 2016;6:118. doi: 10.3389/fcimb.2016.00118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang M, Goh YX, Tai C, et al. VRprofile2: detection of antibiotic resistance-associated mobilome in bacterial pathogens. Nucleic Acids Res. 2022 Jul 5;50(W1):W768–W773. doi: 10.1093/nar/gkac321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li X, Xie Y, Liu M, et al. oriTfinder: a web-based tool for the identification of origin of transfers in DNA sequences of bacterial mobile genetic elements. Nucleic Acids Res. 2018 Jul 2;46(W1):W229–W234. doi: 10.1093/nar/gky352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Overbeek R, Olson R, Pusch GD, et al. The SEED and the rapid annotation of microbial genomes using subsystems technology (RAST). Nucleic Acids Res. 2014 Jan;42(Database issue):D206-14. doi: 10.1093/nar/gkt1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sullivan MJ, Petty NK, Beatson SA.. Easyfig: a genome comparison visualizer. Bioinformatics. 2011 Apr 1;27(7):1009–1010. doi: 10.1093/bioinformatics/btr039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu Z, Xu Q, Liang P, et al. The characteristics of population structure and antimicrobial resistance of Streptococcus suis serotype 8, a non-negligible pathotype. Transbound Emerg Dis. 2022 Sep;69(5):e2495–e2505. doi: 10.1111/tbed.14592 [DOI] [PubMed] [Google Scholar]
- 41.Wang X, Sun J, Bian C, et al. The population structure, antimicrobial resistance, and pathogenicity of Streptococcus suis cps31. Vet Microbiol. 2021 Aug;259:109149. doi: 10.1016/j.vetmic.2021.109149 [DOI] [PubMed] [Google Scholar]
- 42.Wu Z, Wang W, Tang M, et al. Comparative genomic analysis shows that Streptococcus suis meningitis isolate SC070731 contains a unique 105 K genomic island. Gene. 2014 Feb 10;535(2):156–164. doi: 10.1016/j.gene.2014.04.041 [DOI] [PubMed] [Google Scholar]
- 43.Wu Z, Zhang W, Lu C.. Comparative proteome analysis of secreted proteins of Streptococcus suis serotype 9 isolates from diseased and healthy pigs. Microb Pathog. 2008 Sep;45(3):159–166. doi: 10.1016/j.micpath.2008.04.009 [DOI] [PubMed] [Google Scholar]
- 44.Pan Z, He P, Zhang Y, et al. SssP1, a Fimbria-like component of Streptococcus suis, binds to the vimentin of host cells and contributes to bacterial meningitis. PLoS Pathog. 2022 Jul;18(7):e1010710. doi: 10.1371/journal.ppat.1010710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y, Lu P, Pan Z, et al. Sssp1, a Streptococcus suis Fimbria-like protein transported by the SecY2/A2 system, contributes to bacterial virulence. Appl Environ Microbiol. 2018 Sep 15;84(18). doi: 10.1128/AEM.01385-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lalonde M, Segura M, Lacouture S, et al. Interactions between Streptococcus suis serotype 2 and different epithelial cell lines. Microbiology (Reading). 2000 Aug;146(Pt 8):1913–1921. doi: 10.1099/00221287-146-8-1913 [DOI] [PubMed] [Google Scholar]
- 47.Kerdsin A, Hatrongjit R, Gottschalk M, et al. Emergence of Streptococcus suis serotype 9 infection in humans. J Microbiol Immunol Infect. 2017 Aug;50(4):545–546. doi: 10.1016/j.jmii.2015.06.011 [DOI] [PubMed] [Google Scholar]
- 48.Zheng H, Du P, Qiu X, et al. Genomic comparisons of Streptococcus suis serotype 9 strains recovered from diseased pigs in Spain and Canada. Vet Res. 2018 Jan 9;49(1):1. doi: 10.1186/s13567-017-0498-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oh SI, Jeon AB, Jung BY, et al. Capsular serotypes, virulence-associated genes and antimicrobial susceptibility of Streptococcus suis isolates from pigs in Korea. J Vet Med Sci. 2017 Apr 20;79(4):780–787. doi: 10.1292/jvms.16-0514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gottschalk M, Canada LS.. Distribution of Streptococcus suis (from 2012 to 2014) and Actinobacillus pleuropneumoniae (from 2011 to 2014) serotypes isolated from diseased pigs. Can Vet J. 2015 Oct;56(10):1093–1094. [PMC free article] [PubMed] [Google Scholar]
- 51.Roodsant TJ, Van Der Putten BCL, Tamminga SM, et al. Identification of Streptococcus suis putative zoonotic virulence factors: a systematic review and genomic meta-analysis. Virulence. 2021 Dec;12(1):2787–2797. doi: 10.1080/21505594.2021.1985760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Callejo R, Zheng H, Du P, et al. Streptococcus suis serotype 2 strains isolated in Argentina (South America) are different from those recovered in North America and present a higher risk for humans. JMM Case Rep. 2016 Oct;3(5):e005066. doi: 10.1099/jmmcr.0.005066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang M, Du P, Wang J, et al. Genomic epidemiology of Streptococcus suis sequence type 7 sporadic infections in the Guangxi Zhuang autonomous Region of China. Pathogens. 2019 Oct 12;8(4):187. doi: 10.3390/pathogens8040187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haenni M, Lupo A, Madec JY.. Antimicrobial resistance in Streptococcus spp. Microbiol Spectr. 2018 Mar;6(2). doi: 10.1128/spectrum.00315-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Palmieri C, Varaldo PE, Facinelli B.. Streptococcus suis, an emerging drug-resistant animal and human pathogen. Front Microbiol. 2011;2:235. doi: 10.3389/fmicb.2011.00235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Arnold BJ, Huang IT, Hanage WP.. Horizontal gene transfer and adaptive evolution in bacteria. Nat Rev Microbiol. 2022 Apr;20(4):206–218. doi: 10.1038/s41579-021-00650-4 [DOI] [PubMed] [Google Scholar]
- 57.Huang J, Dai X, Wu Z, et al. Conjugative transfer of streptococcal prophages harboring antibiotic resistance and virulence genes. ISME J. 2023 Sep;17(9):1467–1481. doi: 10.1038/s41396-023-01463-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baquero F, Martinez JL, FL V, et al. Evolutionary pathways and trajectories in antibiotic resistance. Clin Microbiol Rev. 2021 Dec 15;34(4):e0005019. doi: 10.1128/CMR.00050-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Partridge SR, Kwong SM, Firth N, et al. Mobile genetic elements associated with antimicrobial resistance. Clin Microbiol Rev. 2018 Oct;31(4). doi: 10.1128/CMR.00088-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Libante V, Nombre Y, Coluzzi C, et al. Chromosomal conjugative and mobilizable elements in Streptococcus suis: major actors in the spreading of antimicrobial resistance and bacteriocin synthesis genes. Pathogens. 2019 Dec 25;9(1). doi: 10.3390/pathogens9010022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.